4
Action Agenda to Support the Consumer–Provider Partnership
CHAPTER SUMMARY
A key step in improving the safety of the medication-use process is establishing a consumer–provider partnership. The consumer of health care—the patient—is the person with the greatest stake in identifying and preventing medication errors. The chapter addresses ways in which both consumers and providers (including physicians, nurses, and pharmacists) can strengthen the consumer– patient partnership. There are also many areas for improvement in consumer-oriented drug information.
According to a 2004 survey by the Kaiser Family Foundation, 48 percent of Americans are concerned about the safety of the medical care they and their families receive, and 55 percent are dissatisfied with the quality of the nation’s health care—up from 44 percent who expressed this view in a survey conducted 4 years ago (KFF, 2004). Results of other national and international surveys indicate that 34 to 40 percent of individuals have experienced a medical error themselves or know of a family member or friend who has (CMWF 2005; NPSF, 1997). A National Patient Safety Foundation survey found that among those who had personally experienced an error, 40 percent of the errors were due to mistakes in diagnosis and wrong treatments. Medication errors accounted for 28 percent of the errors, while 22 percent were the result of mistakes during surgery. In a six-country survey by the Commonwealth Fund, 28 to 32 percent of patients in
each country said treatment risks had not been completely explained during their hospital stay. In addition, 55 to 64 percent of patients said physicians had not always reviewed all their medications during the past year, and 47 to 69 percent stated that physicians did not always explain the side effects of medications (CMWF, 2005).
Usually, people are not told about an error unless injury or death occurs. In a nationally representative survey of hospital risk managers, the vast majority reported that their hospital’s practice was to disclose harm at least some of the time, although only one-third of hospitals actually had board-approved policies for doing so in place (Lamb et al., 2003). More than half of respondents stated that they would always disclose a death or serious injury; when presented with actual clinical scenarios, however, respondents revealed they were much less likely to disclose preventable harm than to disclose nonpreventable harm of comparable severity. In a 2004 survey by the Premier Safety Institute, no respondents indicated that disclosures of errors causing serious or short-term harm were never given; 57 percent said such errors were frequently disclosed to patients or families, while 37 percent said such disclosures were always made (PSI, 2004).
The following is an example of a medication error that resulted in a fatality:
Eighteen-month-old Josie King was admitted to the hospital for first- and second-degree burns received when she climbed into a hot tub. She spent 10 days in the pediatric intensive care unit, with her mother being vigilant as to the details of her care. Josie was recovering and was transferred to an intermediate care floor for a few more days. After her central line was removed, however, her condition worsened. Although her mother expressed concern about Josie’s new symptoms, which at one point included sucking avidly on a wet washcloth, those concerns were not addressed by the shift nurses. Moreover, despite a doctor’s order that no narcotics be administered to the child, and over the objections of her mother, Josie received a narcotic pain medication 2 days before she was to go home. She then experienced cardiac arrest. In retrospect, the child’s symptoms reflected progressive dehydration. Josie’s mother is among the many individuals, parents, and surrogates whose voices are often ignored by providers (JKF, 2002).
The following are examples of medication errors with the potential to result in death or serious harm:
A child with leukemia was discharged from the hospital with a nasogastric tube in place for intermittent enteral feeding. While readmitted for chemotherapy, he developed an infection and had a peripherally inserted central catheter (PICC) emplaced for the administration of antibiotics. He recovered from the infection and was discharged. Shortly thereafter, the
PICC line clotted. His mother called the home care nurse. When the nurse arrived, she found that the mother was about to use a syringe of ginger ale to clear the PICC line and prevented a serious error. Having been taught to clear the child’s feeding tube with ginger ale, the mother thought the same could be done with the PICC line. She is just one example of the many caretakers who do not receive adequate discharge counseling (Cohen, 2000).
A middle-aged man with newly developed asthma was prescribed an inhaler, but was not responding to treatment. During a follow-up visit, he described how he was using the inhaler. He would squirt two puffs in the air and breathe deeply for 15 minutes. He said he’d been instructed to do this by his doctor, who had picked up an inhaler, held it in the air, and released two puffs to demonstrate its use. The doctor had given the man no further instructions. The man had not read the instructions on the package because he was functionally illiterate. He is an example of the millions of Americans who do not receive adequate medication instructions and have difficulty with basic reading and writing (Cohen, 2000).
Each of the above cases illustrates the potentially lethal consequences of inadequate and ineffective interactions between consumers (patients or surrogates) and providers. The cases underscore the most common complaint about providers—they fail to take the time to listen and to explain. Some communication problems have been attributed to the fact that many health care providers focus on diseases and their management rather than on people, their lives, and their health issues (Lewin at al., 2005). Other issues concern the lack of understanding and respect for patients’ rights to be informed and to play an active role in their and their family members’ care. Unfortunately, such circumstances are commonplace (Annas, 2004; KFF, 2004; CMWF, 2005). Care delivered without good communication and follow-through on patient rights is provider-centric when in truth, consumers want and increasingly expect care that is patient-centered (Cleary, 1993). The Institute for Healthcare Improvement’s program on Patient and Family Voices has identified key aspects of patient-centered care desired by consumers (see Box 4-1).
FOUNDATION FOR IMPROVEMENT
Improving safety and quality in the medication-use system requires a shift from the conventional approach to care toward a patient-centered model based on consumer–provider partnership and communication. The foundation for this change has several elements discussed in this chapter. First, all participants in the health care delivery system need to acquire a thorough understanding of what patient-centered care really entails in terms of both the consumer–provider relationship and the culture of the health
|
BOX 4-1 Patients’ Expectations of Their Providers
SOURCE: IHI, 2005. |
care organization. Second, consumers need to be empowered to play an active role in their care through the establishment of patient rights that are ensured at all points along the medication-use continuum, enhancing the presence, power, and participation of consumers in their relationships with providers. Third, certain basic, definitive actions can be taken to minimize and prevent medication errors and other safety issues; for example, the consumer can carry a medication list, and the provider can regularly practice medication reconcilation. Fourth, participants in the health care delivery system should seek to understand and address barriers to patient-centered care, patient–provider communication, and consumer medication self-management. Finally, resources need to be developed to support partnership, communication, and self-management. The first two of these elements are discussed below; the others are addressed in the remainder of the chapter.
Understanding Patient-Centered Care
Understanding patient-centered care is critical to quality and safety in medication use. Patient-centered care is an approach that adopts perspective of patients—what matters to them, what affects them either positively or negatively, and their experience of illness (Gerteis et al., 1993). The aim is to see people in their biopsychosocial entirety, understanding the whole person, sharing power and responsibility, and drawing attention to
patients’ individual identities (Armstrong, 1982; Stewart, 1995; Stewart et al., 1995; Mead and Bower, 2000). The approach recognizes that important aspects of the patient’s experience have just as much to do with the quality of care delivery during interactions with medical staff as the actual medical care itself (Frampton et al., 2003). It focuses attention on the heart of the patient–provider relationship—communication during each clinical encounter, whether a consultation, intervention, or simple exchange. Patient-centered care that embodies both effective communication and technical skill is necessary to achieve safety and quality of care (Griffin et al., 2004).
Although a number of definitions have been presented in the academic and clinical literature (Frampton et al., 2003; Lewin et al., 2005), the Committee on Identifying and Preventing Medication Errors uses the multifaceted definition developed by Gerteis and colleagues (1993) and espoused in previous Institute of Medicine (IOM) reports. This definition encompasses seven primary dimensions of patient-centered care, as described in Box 4-2: (1) respect for patients’ values, preferences, and expressed needs; (2) coordination and integration of care; (3) information, communication, and education; (4) physical comfort; (5) emotional support and alleviation of fear and anxiety; (6) involvement of family and friends; and (7) transition and continuity. Effective, patient-centered communication along these dimensions supports a more collaborative consumer– provider relationship whereby the joint definition of problems, treatment goals, and management strategies can be accomplished (Von Korff et al., 1997; Wolpert and Anderson, 2001). This collaboration, in turn, can lead to improved patient satisfaction, engagement in decision making, participation in prevention activities (Flach et al., 2004), better self-management of chronic conditions (Heisler et al., 2002), and adherence to medication regimens (Safran et al., 1998).
Even though the benefits of patient-centered communication are well understood, they have not been well implemented across health care settings, institutions, and practices (IOM, 2001). In today’s health care system, such communication is sometimes sacrificed as a result of the intrusion of business into clinical practice, the pressures of limited time for office visits, the culture of medicalization, and the often all-consuming focus on technology (Teutsch, 2003). There is a misconception that supportive interactions require more staff or more time and are therefore more costly (Frampton et al., 2003). This is not necessarily the case. Rather, it could be argued that negative interactions (e.g., alienating patients, being unresponsive to their needs, or limiting their sense of control) can be very costly in terms of lost patient revenues, poor health outcomes, and, in some cases, increased likelihood of litigation (Frampton et al., 2003). For example, insufficient communication about medications can lead to nonadherence
|
BOX 4-2 Dimensions of Patient-Centered Care
SOURCE: Gerteis et al., 1993. |
and increased hospitalization (DiMatteo, 2004). Conversely, good communication can obviate the need for extensive discussions about the medication regimen with every patient during every visit.
Methods for incorporating patient-centered communication about medications into day-to-day clinical practice can be drawn from the Chronic Care Model (as well as others employed to develop consumers’ self-management skills). The Chronic Illness Care Breakthrough Series Collaboratives established by the Institute for Healthcare Improvement and Associates in Process Improvement developed a five-component model of key steps to patient-centered self-management support (Glasgow et al., 2002) (see Figure 4-1). It is designed to organize evidence-based intervention components into an integrated and understandable iterative process appropriate for incorporation into busy primary care practices. The five components are as follows: (1) current self-management beliefs and behaviors are assessed, with feedback for both providers and patients; (2) the feedback prompts collaborative goal setting between patients and provider(s); (3) a personal action plan for self-management is developed; (4) initial self-management goals are refined and informed through the identification of anticipated barriers to and supports for the achievement
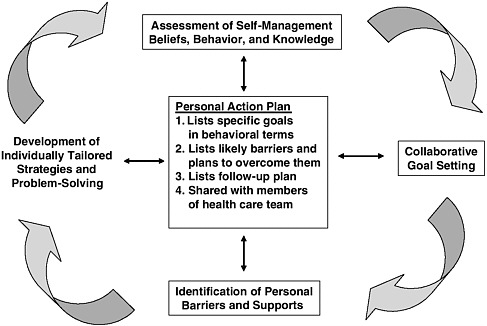
FIGURE 4-1 The Chronic Care Model: Key steps to patient-centered, self-management support.
SOURCE: Glasgow et al., 2002.
of those goals and a better understanding of the patient’s perspective and the social environment in which self-management must be conducted; and (5) individually tailored strategies and problem-solving approaches are developed to enhance self-efficacy and provide patients with strategies for overcoming the barriers identified (Glasgow et al., 2002). These steps are repeated in an iterative, ongoing, flexible way at future encounters. Glasgow and colleagues (2002) believe this model is different from that used in most health care settings in that it is patient-centered, individualized, and self-correcting, and encompasses the overall care of a patient’s health conditions rather than being an isolated activity.
Self-management education programs have been found to improve patient health outcomes (IOM, 2003). For example, a study that investigated the effects of self-management education and regular practitioner review for adults with asthma demonstrated a statistically significant reduction in the proportion of subjects reporting hospitalizations and emergency room visits, unscheduled physician visits, days lost from work, and episodes of nocturnal asthma (Gibson et al., 2000).
The above steps outlined for chronic care could easily be adapted to patient-centered care for improved medication self-management. In fact, Svarstad and colleagues (1999) developed a brief medication questionnaire for patients as a means of identifying those who need assistance with their medications, assessing their concerns, evaluating new ways to assist them, and monitoring their progress (including adherence). Additional research could be undertaken to develop methods for adapting the components of the Chronic Care Model to general medication self-management and the resources required to support patients and providers in a patient-centered, collaborative partnership.
Empowering Consumers in Their Health Care
The second critical element of the foundation for improving the safety and quality of the medication-use process through an emphasis on patient-centered care is the empowerment of consumers as equal partners in their health care. Equalizing and empowering consumers in their relationship with their providers requires assurance of their rights as patients in all health care settings. Embracing a set of basic patient rights that are endorsed and enforced by health care provider, accreditation, and regulatory organizations to support patient-centered medication management, informed decision making, and prevention of errors is necessary to improve the safety of medication use and the quality of care overall. As seen in the examples quoted earlier, patient rights are not important only in the abstract; they can literally save lives (Annas, 2004).
Many rights that empower consumers and protect them from harm have been instituted through codes, regulations, and laws governing informed consent prior to receipt of a medication, treatment, or procedure during an experimental clinical study or during clinical care. Informed consent is the fundamental ethical and legal doctrine that protects patients’ rights to personal autonomy and bodily self-determination (Ridley, 2001). Where informed consent is relevant, the physician is required to discuss and disclose the following (AMA, 1998):
-
Patient’s diagnosis, if known
-
Nature and purpose of a proposed medication, treatment, or procedure
-
Risks and benefits of a proposed medication, treatment, or procedure
-
Alternatives (including medication options), regardless of their cost or the extent to which they are covered by health insurance
-
Risks and benefits of an alternative medication, treatment, or procedure
-
Risks and benefits of not receiving or undergoing a treatment or procedure
Patients are also entitled to the opportunity to ask questions so they can elicit a better understanding of their treatment plan (medication or procedure) before proceeding with or refusing a proposed medical intervention.
Regulations of the U.S. Food and Drug Administration (FDA) govern informed consent requirements for participation in clinical trials. Vulnerable populations—children, pregnant women, those with mental illnesses, those of reduced competency, and prisoners—are given special consideration and, in some cases, extra protection by the federal government (Getz and Borfitz, 2002). As part of licensing, certification, and regulatory authority, state medical boards govern informed consent requirements in hospitals and ambulatory practice. Informed consent provisions are based on the American Medical Association’s Code of Medical Ethics and standards set by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO). While most state laws regarding informed consent are written for hospital care, precedent set by extensive case law applies these provisions equally to ambulatory care. In the realities of clinical practice, however, consumers are often not adequately informed to participate as partners in their care. For example, many aspects of medication therapy that should be discussed as fully as in an informed consent discussion are not. Often lacking is discussion of contraindications, side effects, adverse reactions, how to distinguish side effects and adverse reactions from the symptoms of disease, and what to do about them (Kerzman et al., 2005; Safran, 2003). Not all patients need a full discussion at every clinical encounter, especially if they are familiar with their medication(s), but such discussion should be recognized as a patient’s fundamental right. This raises another
core issue: a formal set of patient rights applicable in all health care settings has never been instituted at the federal or state level. Federal legislative attempts in the 1990s to pass a comprehensive patient bill of rights that would apply to health care services did not succeed, with the exception of consumers’ right to sue their insurance payer for denial of benefits.
Health care provider and accreditation organizations have, however, been leaders in promulgating statements of patient rights. For example, the American Hospital Association recently recrafted its 1992 Patient’s Bill of Rights to include principles of the patient care partnership, a model that represents a shift to patient-centered care. Those principles state what patients can expect during a hospital stay in terms of the hospital environment, participation in their care, protection of privacy, discharge preparation, and help with billing. JCAHO evaluates compliance with standards for ethics, rights, and responsibilities in hospital and ambulatory care settings. The purpose of these standards is to ensure that care, treatment, and services are provided in a way that respects and fosters patient dignity, autonomy, positive self-regard, civil rights, and involvement (JCAHO, 2005). Consideration is given to patients’ abilities and resources; their cultural, psychosocial, and spiritual values; the relevant demands of their environment; and their wishes regarding the involvement of family members in their care. Other efforts to raise awareness of patient rights include those of the Tavistock Group—a group of experts representing health care stakeholders that developed a set of shared ethical principles to guide decision making in an integrated health care delivery system (Smith et al., 1999). Certain states have instituted a patient bill of rights, but provisions are not comprehensive, nor do they cover all health care settings (see Table 4-1 for examples).
While these efforts are steps in the direction of patient-centered care and patient rights, they do not go far enough. The committee believes that establishment of a basic set of patient rights—presented in Box 4-3—is essential to achieve patient-centered care, consumer activation and partnership, and improvements in safety and quality. Many but not all of these rights are established broadly in the U.S. Constitution (Amendments I and XIV1) and have been articulated by the courts through common law. Nonetheless, they remain difficult to enforce for patients and providers alike, especially for sick individuals (Annas, 2004). One important point listed in Box 4-3 that is not specifically provided for in the law is the right to be told
TABLE 4-1 Examples of State Patient Rights Statutes
|
State |
Provision |
Providers/Facilities Covered |
|
Alaska |
Patient Medical Rights Alaska Stat. § 47.30.825 (2006) |
Mental health facilities |
|
California |
Patients’ Bill of Rights Cal. Health & Safety Code § 1599 (2006) |
Nursing homes |
|
Florida |
Patient’s Bill of Rights and Responsibilities Fla. Stat. § 381.026 |
Medical doctors, osteopaths, podiatrists, hospitals, and other health care facilities |
|
Maryland |
Patient Bill of Rights Md. HEALTH-GENERAL Code Ann. § 19-342 |
Hospitals |
|
Massachusetts |
Patients’ Bill of Rights Annotated Laws of Michigan, ch. 111, § 70E (2005) |
Hospitals, clinics, nursing homes |
|
Mississippi |
Patients Rights Miss. Code Ann. § 41-21-102 |
Mental health facilities |
|
BOX 4-3 Improving Medication Safety: Actions for Nurses
|
when an adverse event occurs. For example, if a patient is administered the wrong drug but is not injured, he or she should be told that the error occurred and what is being done to correct it. Thus, the committee believes disclosure of clinically significant errors should be included as an essential patient right. Enumerating patients’ essential rights in one document would facilitate consumers’ and providers’ understanding and exercise of these rights and thereby improve the safety and quality of medication use. It also would clarify how the rights are to be applied day-to-day in clinical practice and ensure equality in application of the rights across health care settings.
COMPONENTS OF THE PATIENT–PROVIDER PARTNERSHIP FOR MEDICATION SAFETY
This section outlines components of the consumer–provider partnership that can contribute to the safety and quality of medication use. Components for consumers include activation and partnership, carrying a medication list, safety practices for self-care, and knowing where to find quality health and medication information. Components for providers include regular practice of medication reconciliation, patient education about medications, increased opportunities for consultation, respect for designated surrogates, and disclosure of errors.
Recommendation 1: To improve the quality and safety of the medication-use process, specific measures should be instituted to strengthen patients’ capacities for sound medication self-management. Specifically:
-
Patients’ rights regarding safety and quality in health care and medication use should be formalized at the state and/or federal levels and ensured at every point of care.
-
Patients (or their surrogates) should maintain an active list of all prescription drugs, over-the-counter (OTC) drugs, and dietary supplements they are taking; the reasons for taking them; and any known drug allergies. Every provider involved in the medication-use process for a patient should have access to this list.
-
Providers should take definitive action to educate patients (or their surrogates) about the safe and effective use of medications. They should provide information about side effects, contraindications, and how to handle adverse reactions, as well as where to obtain additional objective, high-quality information.
-
Consultation on their medications should be available to patients at key points in the medication-use process (during clinical
-
decision making in ambulatory and inpatient care, at hospital discharge, and at the pharmacy).
Components for Consumers
Consumers’ awareness of health care quality and safety issues is growing, but fundamental principles related to the consumer’s roles in addressing these issues are not widely known or implemented (NPSF, 2000). Several organizations, such as the Institute for Healthcare Improvement, Planetree, and the former Foundation for Accountability are developing strategies designed to advance patient-centered care (FACCT, 2001b; Frampton et al., 2003; IHI, 2005; Markle Foundation, 2005). One key element of these strategies is the empowerment and activation of consumers. Consumers who have already been activated with regard to medication safety generally gained this knowledge as the result of personal experience with an adverse event in either their own care or that of a family member or friend. Thus a sizable portion of the population does not know what constitutes appropriate and safe medication use, quality health care, and patient safety, or what practical steps consumers can take to protect themselves and their loved ones (NPSF, 2000).
Interventions that promote consumer empowerment and the acquisition of self-management skills emphasize the crucial role of patients in setting goals, establishing action plans, and identifying and overcoming barriers to effective self-management.
Consumer Activation and Partnership
Engagement of consumers in activities and behaviors that promote their health, well-being, and safety is an important component of current initiatives to redesign the health care system (Hibbard, 2004). Ideally, as informed and engaged partners in their health care, consumers contribute to efforts that improve the safety and quality of care while reducing costs to the system (IOM, 2001). In this role, they help produce desired health outcomes to the best of their ability. They make informed decisions about when to seek care; how to work with providers in selecting among treatment options on the basis of their own values and needs; how to work with providers in managing their conditions; what information to provide about their health and functioning to aid in diagnosis and treatment; and how to follow through on agreed-upon treatment plans, recommended lifestyle changes, and preventive actions (Hibbard, 2003).
Research has revealed that being an engaged and active participant in one’s own care is linked to better health outcomes (Safran et al., 1998; Ansell, 1999; Lorig et al., 1999; Sawicki, 1999; Bodenheimer et al., 2002; Heisler et al., 2003; Flach et al., 2004). Some of the best research on
patients’ capability for self-management given adequate support and education stems from models developed for chronic conditions such as heart disease, stroke, lung disease, arthritis, and diabetes (see the earlier discussion of the Chronic Care Model). In these studies, providers educated patients about managing the symptoms and problems associated with their conditions and taught good medication self-management practices and healthful behaviors. For example, patients with vascular disease demonstrated high self-efficacy in medication use, exercise, and weight control when interventions emphasized the importance of self-management, supplied information on visible physiological changes and performance accomplishments, and used nursing staff for patient support and communications (Sol et al., 2006). Hartigan (2003) studied cancer patients receiving oral chemotherapy agents and noted their success with medication safety, optimal dosing, and adherence to the treatment plan when instructed by an oncology nurse in self-assessment, management of symptoms and medication side effects, and use of compliance aids (e.g., diaries, calendars, pill-boxes with alarms). Nurses also provided telephone follow-up and triage to patients, reinforcing this support (Hartigan, 2003).
However, the ability and willingness of patients to assume this partnership role can vary depending on their health status. Many patients trust their health care providers and prefer that providers make appropriate decisions for them (Kravitz et al., 2003). In one study, for example, up to 34 percent of women recently diagnosed with breast cancer wanted to delegate all decision making to their provider (Degner et al., 1997). Another study found that 69 percent of patients with chronic conditions preferred such delegation of medical decisions (Arora and McHorney, 2000). The likelihood of preferring an active role increases with level of education and decreases significantly with age and severity of illness (Ende et al., 1989; Stiggelbout and Kiebert, 1997; Mansell et al., 2000).
Thus, consumer engagement should be viewed on a continuum from those who prefer a highly active role to those who prefer a more passive role (RWJF, 2000). For some individuals, their level of activation will change over time. Nevertheless, respect for patients’ decisions about their care and level of partnership is paramount. No less important is respect for the level of participation desired by patient surrogates when patients themselves are unable to participate.
Carrying a Medication List
The single most important contribution consumers can make to medication safety and good medication self-management is maintaining an up-to-date medication list that includes prescription medications, OTC drugs, and dietary supplements; the reasons for taking these products; and all
known drug and/or food allergies. Information about each drug should include its name, strength, dose, and frequency of administration. Patients should bring this list with them each time they visit their provider and have the provider verify the list with them. Ideally, they should carry it with them at all times in the event emergency care is needed. Indeed, patients have a responsibility to provide this information to their providers and designated surrogates to help prevent adverse drug events (ADEs) such as drug–drug interactions (Cohen, 2000). The medication list is especially important for those who have chronic conditions; see multiple providers; or take multiple medications, OTCs, and dietary supplements. Consumers should exercise their right to ask their prescriber questions if they do not understand their drug treatment regimen, especially side effects and contraindications, and communicate with their caregivers about any adverse changes in the way they feel after initiating a new medication. Providers should be sure that their patients understand the regimen and whom to contact if they have any further questions once they are at home.2
Many consumers do not know that their providers are supposed to reconcile their medications as they transition between different health care settings and patient care units. Carrying a medication list can help greatly in the reconciliation process. In particular, providers should reconcile patients’ medications at each ambulatory encounter, at each admission to a hospital or readmission to long-term care, at each point of transfer between hospital units, and at hospital discharge.
Medication Safety Practices for Self-Care
When consumers become informed and engaged partners, they can decrease the probability that they will experience a medication error (Cohen, 2000). Actions range from the simple and routine, such as double-checking their prescription when dropping it off and picking it up from the pharmacy, to the more involved, such as maintaining an accurate personal medication record and a partnership with their provider in health care. The following are examples of actions consumers can take as empowered partners in their care:
|
2 |
Examples of medication lists can be found at: (1) The Joint Commission for the Accreditation of Health Care Organizations (http://www.jcaho.org/general+public/gp+speak+up/speak up_brochure_meds.pdf and http://www.jcaho.org/general+public/gp+speak+up/speakup_ card_meds.pdf); and (2) Institute for Healthcare Improvement (http://www.ihi.org/IHI/Topics/PatientSafety/MedicationSystems/Tools/MedicationReconciliationGuidelinesAndHome MedicationListLutherMidelfort.htm, http://www.ihi.org/IHI/Topics/PatientSafety/Medication Systems/Tools/Tools/WhatYouNeedtoKnowAboutMedicationSafety.htm, and http://www. ihi.org/IHI/Topics/PatientSafety/MedicationSystems/Tools/TheMedForm.htm). |
-
Ask questions and insist on answers from providers to guide their decision making on medication and nonmedication treatment options based on their personal values and needs.
-
Insist that providers clarify specific aspects of the medication regimen (e.g., purpose, drug name, dosage, strength), identify possible side effects and what actions to take should they occur, and understand possible interactions with other medications and/or foods.
-
Ensure that providers give them or direct them to written information about the drug appropriate to their level of health literacy, age, and language, and that they know where to obtain additional information about their medication(s) and health condition(s).
-
Understand and retain their right to disagree and to say no—no to taking on a more active role, no to a particular provider’s counsel, and no to medication therapy.
-
Seek information and counseling to make informed self-care decisions when self-prescribing and administering OTC medications, herbal remedies, and dietary supplements.
Along with knowing their rights as patients and maintaining a medication list, understanding a basic set of practices for each step in the medication-use system can help consumers contribute to medication safety. These practices are outlined in Box 4-4 and discussed further later in the chapter.
Finding Quality Health and Medication Information
Consumers should become knowledgeable about where to find quality health and medication information to support them in self-care. They should know where and how to find this information at the public library, if these resources exist, and where to find the best information on the Internet (e.g., the National Library of Medicine’s [NLM] MedlinePlus program) (see the section on actions for government and other stakeholders later in the chapter). In addition, they should keep a list of these references that they can refer to quickly and easily.
Components for Providers
Patient-centered care in the medication-use system requires improvement in many of the dynamics affecting the provider–patient relationship. Provider responsibilities in this regard include medication reconciliation, patient education, availability of counseling, respect for surrogates, and disclosure of errors. Just as important, consumers and surrogates can develop their understanding of the appropriate expectations they should have
|
BOX 4-4 Consumer Actions to Improve Medication Safety
|
of their providers for engaging in activities that promote quality and safety, and hold them accountable for meeting those expectations.
Medication Reconciliation
Medication reconciliation is a process designed to prevent medication errors at patient transition points. It is a multistep process that entails obtaining a complete and accurate list of the medications a patient is taking (including nonprescription and alternative medications) and comparing this list with both documentation in the patient’s medical record during ambulatory care visits and the physician’s admission, transfer, and/or discharge orders in inpatient settings (IHI, 2004). The purpose of the reconciliation process is to avoid or minimize errors of transcription, omission, duplication of therapy, and drug–drug and drug–disease interactions. Discrepancies are brought to the attention of the provider, and if appropriate, changes are made to the record or orders. The overarching goal is to facilitate continuity of care (Nickerson et al., 2005).
Several studies have shown that a significantly high number of discrepancies can be detected through the medication reconciliation process (Pronovost et al., 2003). Nickerson and colleagues (2005) found that of 481 drug therapy problems detected, 83.8 percent had a potentially significant or somewhat significant clinical impact. Another study of inpatient medical records found that the details of current medication use were either nonexistent or incorrect 85 percent of the time (Rozich and Resar, 2001). Bikowski and colleagues (2001) also demonstrated high rates of discrepancies in family practice. In 74 percent of cases studied, the patient was taking at least one medication that the physician was unaware of, or that the physician was aware of but was not actually part of the treatment regimen. Along with these statistics on medication incongruence, about 60 percent of medication errors in patient records occurred when patients were admitted, discharged, or transferred (Rozich and Resar, 2001).
Medication reconciliation has proven to be an effective means of achieving significant reductions in such discrepancies. The introduction of a series of reconciliation interventions in one hospital during a 7-month period decreased the rate of errors by 70 percent and that of adverse drug events by 15 percent (Rogers et al., 2006; Rozich et al., 2004). Pharmacy technicians in another hospital reduced the potential for medication errors by 80 percent within 3 months by obtaining a medication history from patients scheduled for surgery (Haig, 2003).
The Institute for Healthcare Improvement has simplified medication reconciliation into three steps applicable in all health care settings (IHI, 2004):
-
Verification (collection of medication history/list)
-
Clarification (ensuring that the medications and doses are appropriate)
-
Reconciliation (documentation of changes)
The medication reconciliation process can be implemented in several ways. One method, especially when multiple providers are involved in a patient’s care, is for health care organizations to maintain a system that allows each member of the care team (e.g., physician, nurse, pharmacist) access to the patient’s medication list and medication administration record. Electronic health information systems (as discussed in Chapter 5) may be an efficient means to this end. During handoffs between sites of care (e.g., hospital to home) or between professionals (e.g., change in medical services or rotation of residents or attending physicians), the clinician receiving the patient should review and reconcile the patient’s medication plan to ensure its completeness and accuracy. The Institute for Healthcare Improvement’s Getting Started Kit: Prevent Adverse Drug Events (Medication Reconciliation)—How-to-Guide provides several strategies for implementing medication reconciliation processes within health care organizations (IHI, 2004).
Even though medication reconciliation is recognized as an effective means of preventing medication errors (Gleason et al., 2004; Ketchum et al., 2005), often it is overlooked and not performed (IHI, 2004: Rogers et al., 2006). Several barriers to implementing medication reconciliation were identified by Rodehaver (2005), who proposed actions that could be taken to overcome these barriers (see Table 4-2). Rather than continuing to leave reconciliation as a voluntary process, in 2003 JCAHO incorporated medication reconciliation as a key expectation for compliance with its National Patient Safety Goals (JCAHO, 2004). The intent is that by 2006, hospitals will implement reconciliation activities at all transition points, including transitions from the intensive care unit to medical or surgical units. The patient’s updated medication regimen and list should be communicated to the “next provider of service” at all interfaces of care, and upon admission to and discharge from the facility. At admission and discharge, reconciliation activities should involve discussions with the patient or designated person (e.g., family member, significant other, surrogate decision maker). Implementing comprehensive medication reconciliation activities at all points of care as requested by JCAHO is a complex undertaking that may require remodeling of inpatient flow, provider workflow, and organizational information management. Studies should be undertaken to determine the most efficient and effective means of implementing the JCAHO requirements.
TABLE 4-2 Overcoming Barriers to the Implementation of Medication Reconciliation
|
Barrier |
Actions to Overcome Barriers |
|
Medical staff acceptance |
|
|
Concerns related to the accuracy of the solicited medication list |
|
|
Ownership for medication oversight |
|
|
Attitude that “my patient type is unique” and “you just don’t understand” |
|
|
Inconsistency among residents and physician extenders |
|
|
Organizational climate versus small test of change |
|
|
SOURCE: Rodehaver, 2005. |
|
Patient Education
Consumers should expect to be adequately educated by their providers about their medications and about appropriate medication self-management. Enhancing individuals’ knowledge of and capacity for medication self-management requires, above all, high-quality communications with providers. Providers must be able and willing to understand and respond to the patient’s implicit and explicit messages (Sundin and Jansson, 2003). They should attempt to elicit the patient’s ideas, feelings, and preferences regarding health problems and possible treatments, daily routines, and the information needed to support self-management. Providers should understand that patients need different kinds of information at different times and for different purposes (Raynor et al., 2004). Moreover, they should understand that some points may be easily understood, while others may need to be reiterated, especially when the patient’s receptivity is limited by physical debility or psychological/ emotional states (Scott and Thompson, 2003). The information relayed should be accurate and complete relative to the patient’s level of understanding (Reiser, 1980).
Part of the problem has been physician training—until recently, undergraduate and postgraduate training paid little attention to ensuring that doctors acquire the skills necessary to communicate well with patients (Maguire and Pitceathly, 2002). In the 1990s, medical schools sharpened their focus on communication skills (AAMC, 1999). The Association of American Medical Colleges (AAMC) initiated the Medical Schools Objectives Project to facilitate the process of enhancing teaching and assessment of communication skills. As a result of this and other efforts,3 interpersonal skills and communication are one of six core competencies of graduate medical education required as part of the United States Medical Licensing Examination (Batalden et al., 2002; FSMB and NBME, 2005). However, there is significant variation among medical schools in the way and the extent to which communication skills are taught and assessed (AAMC, 1999; Makoul, 2003). Regardless of what method is used,4 the reliability and effectiveness of observation and feedback can be compromised unless grounded in a coherent structured framework (Makoul, 2003).
The development of competency in communication has been a focus of nursing education for over 50 years. Nursing education programs are required to demonstrate attention to this core competency as part of the accreditation process (AACN, 1998). On many health care teams with excellent patient outcomes, nurses and nurse practitioners are used as the primary providers who listen, communicate with and educate patients and families, and coordinate care.
Even though some communication training has been incorporated in medical school curricula, most patient complaints about providers are related to problems with communication rather than clinical competency— specifically, that doctors do not listen to them (Richards, 1990). A study of the literature on patients’ priorities for general practitioners found the most highly rated aspect of care to be “humanness,” followed by competence/ accuracy (Wensing et al., 1998). For some patients, the humanness element means the physician really listens and does not hurry them (Carroll et al., 1998). Patients’ ratings of physicians’ communication skills are strongly related to trust, but trust does not equate to unquestioning faith (Coulter, 2002). Patients need empathy, support, and reassurance, all essential features of the therapeutic relationship, but they also need honest information about their condition, options for treatment, and clinicians who listen to their concerns and preferences (Mechanic and Meyer, 2000).
It is widely recognized that provider–patient communications, including those regarding medications, typically are provider-oriented (e.g., the provider talking more than listening and asking few open-ended questions) (Berry et al., 2003). As a result, patients fail to receive all the information they need and desire about their medications, especially that related to risks, adverse side effects, and contraindications (Caress et al., 2002; Scott and Thompson, 2003; Garfield et al., 2004). Patients increasingly want more and better information about their condition and the expected outcome, more openness about medication side effects, and advice on what they can do for themselves (Meryn, 1998). Recognizing that some patients find it difficult to articulate their information needs or are reluctant to ask questions during medical visits, practitioners (physicians, nurse practitioners, physician assistants, pharmacists, nurses) should have the requisite training in communication to elicit their patients’ understanding of the medication regimen and educational needs (Sleath et al., 1999). Box 4-5 outlines the core information that research indicates patients should receive about their medications (Sleath et al., 1999; Caress et al., 2002; Scott and Thompson, 2003; Garfield et al., 2004; Morrow et al., 2005).
The ability of providers to communicate medication information in an understandable manner is critical to adequately informing, educating, and empowering patients. In particular, both discussions and written information about medications should be appropriate to the patient’s level of lit-
eracy, age, language, and culture. Providers must have resources available to manage the knowledge, practical, and attitudinal barriers that affect provider–patient communication. Information should be easy for patients to understand and follow when they are at home self-managing their regimen. For example, providers should be aware that the majority of individuals with literacy problems have difficulty following prescription directions and will require communication consistent with their literacy level (Safeer and Keenan, 2005). Patients may misunderstand the instruction to “take a tablet X times a day” but understand “take a tablet every X hours.” When necessary, providers should have resources available to facilitate the patient’s understanding of medication information orally and in writing. Such resources may include translation services for patients. Ambulatory care providers can have a nurse or technician on staff with the language skills necessary to support the needs of the practice’s patient population, develop a partnership with a local pharmacist that can assist certain patients in confirming details of their medication regimen in their native language, or utilize centrally located telephone translation services.
Opportunities for Consultation
Successful medication self-management requires that consumers have multiple opportunities to gain knowledge about safe and effective medication use. Such consultations with providers should be readily available to consumers in all health care settings and at key points along the medication-use continuum. Specifically, consultations should take place during clinical decision making in ambulatory and hospital care, at hospital discharge, and at the time of dispensing by the local community pharmacy. Telephone consultations may be used to provide additional support to patients as they manage problems with and the effects of their medications. Access to consultation at these critical points in the medication-use continuum creates, in effect, a chain of communication that serves as the medication self-management support system. Conversely, poor communication at any of these points can lead to medication errors due to misunderstanding, inaccurate or incomplete information, or nonadherence (Morrow et al., 1988).
Because most health care is provided in community settings, the chain of communication begins with provider–patient consultations during ambulatory care. As discussed earlier, primary care providers play a crucial role in educating patients about the safe and effective use of prescription and nonprescription medications. Thus during ambulatory care consultations, providers must allow sufficient time for consultations with patients or surrogates about medication management (Raynor et al., 2004). Providers should be able to adapt to information needs that shift over time and
|
BOX 4-5 Core Information for Educating Patients About Their Medications
|
with changes in patients’ health status. They should follow up closely on their patients’ success or difficulties with a medication regimen so as to overcome the barriers to self-management discussed above and facilitate desired health outcomes. And it is essential that primary care providers function as the chief coordinator and record keeper of their patients’ medication regimens from multiple providers.
Hospital providers also serve as important sources of patient education both during inpatient care and at discharge. Research shows that many patients desire more information about their health conditions, treatments, and procedures than they currently receive (Wilson et al., 2002; Scott and Thompson, 2003). During an inpatient stay, however, the extent to which patients want to be educated about their medications may vary according to individual preferences, severity of illness, or other factors. Patients or their surrogates should have access to regular consultations with physicians, nurses, and pharmacists to gain knowledge about the medications involved in the treatment plan. Evidence supports a team approach among these providers as a successful means of improving patient safety, quality of
|
care, and health outcomes (Connor et al., 2002; Kaissi et al., 2003; Reiling et al., 2004). Providers should be particularly vigilant about educating patients at discharge, as many providers tend to overestimate patients’ understanding of the medication regimen and its potential side effects (Kerzman et al., 2005). Discharge from the hospital is also a prime time for problems with medication reconciliation. Providers may overlook the need to resume medications that were suspended during hospitalization, and providers inside and outside of the hospital may inadvertently prescribe different medications for the same condition.
The quality of discharge planning and communication is an important determinant of patients’ capacity for self-management and of overall health outcomes (Calkins et al., 1997). Registered nurses spend a large amount of time integrating patient care as part of planning for patients’ discharge from hospitals or other health care facilities to enable continued care in the home, school, or long-term care facility; educating the patient and family about the patient’s disease, course of therapy, medications, self-care activities, and other areas of concern to the patient; and preventing discontinuities
in care (IOM, 2004d). Discharge communication is also an important factor affecting coordination of care during transitions from inpatient care to another setting. Hospital providers must ensure that both patients and their primary ambulatory care providers receive comprehensive information about the discharge plan, including the prescribed medication regimen, disease management if a chronic condition is present, and self-care activities to improve health status.
Another critical link in the chain of communication to support medication self-management is the local community pharmacist. Pharmacists have expertise in many aspects of medication use, yet are often underutilized in both hospital and community settings. Pharmacists are required by state law to provide consumers with medication consultation unless an individual waives his or her right. Because many consumers do not know that they have the right to utilize pharmacists in this capacity, they may unknowingly sign documents waiving consultation services. Pharmacists generally provide consultation upon request, but few serve as active facilitators of medication self-management. A daily workload characterized by a high volume of prescriptions to fill, large percentages of time (up to 85 percent) dedicated to claims adjudication, and staffing shortages inhibit pharmacists’ ability to do so (Knowlton and Penna, 2003; Manasse and Thompson, 2005). Training pharmacy technicians to take over claims adjudication and bottle filling, as well as implementing robotics and other automated pharmacy systems, would allow pharmacists more time for counseling patients. Reducing costs in the above manner would generate some of the resources necessary to support medication management services for the general population, although additional resources may also be needed. Initial efforts to this end are included in the provisions of Part D of the Medicare Prescription Drug Improvement and Modernization Act of 2003, which requires pharmaceutical benefit plans to make available medication therapy management programs and pay pharmacists for these services. These medication therapy management programs are available only for certain beneficiaries—those using multiple medications, with multiple chronic conditions, and with expected drug expenditures of $4,000 annually. Pharmaceutical benefit plans provide the services through their own in-house staff and a toll-free 800 telephone number, rather than under fee-for-service contracts with community pharmacists. Medication therapy management is addressed further in Chapter 8.
Respect for Patient Surrogates
In compliance with existing laws, including those established through living wills, power of medical attorney, and other state and federal laws (Annas, 2004), providers should be aware of and strictly follow patients’
arrangements for designated surrogates. If patients are unable or unwilling to make decisions on their own, providers must adhere to their alternative arrangements for health care decision making (PCSEPMBBR, 1982). Capacity for decision making is specific to a particular situation or episode and best understood from a functional perspective: the presence or absence of capacity does not depend on a person’s health status or on the decision made, but on the individual’s actual functioning in the decision-making process. Clearly, incoherent, unconscious, or otherwise incapacitated patients cannot make informed treatment decisions because they cannot receive a full and current explanation of their health problems and treatment options (Johnstone, 2000). Some patients may be technically capable of decision making but choose to defer to others, and this choice should be respected. Even if patients possess no decision-making capacity, ethical principles for protecting vulnerable populations dictate that providers speak to and inform them out of respect, beneficence, and justice (PCSEPMBBR, 1982; Getz and Borfitz, 2002). For example, someone with Parkinson’s disease may be fully alert but unable to speak understandably or function physically. Nonetheless, providers should inform such a patient of decisions made by surrogates as care proceeds.
Patients should have the right to have someone of their choosing present whenever medications are being prescribed, administered, or monitored. Family members, friends, and significant others can have a far greater impact on patients’ experiences with their illness, their safety, and their long-term health and happiness than any clinician (Gerteis et al., 1993). Relatives and friends take care of patients, offer love and support, remind patients to take medications, and monitor doctors’ orders and nursing care. Patients may choose to have a family member, friend, or other person present for any number of other reasons important to them, such as assistance with health decision making, language translation, and emotional support. They may choose to have that person participate actively or passively. For example, at the patient’s request, the designated person might be asked to double-check the dosage of a chemotherapy agent prepared for administration by a hospital nurse or to hold the patient’s hand in prayer during the cycle of administration. Health care providers must expand their thinking about family from including only next of kin to encompassing other family members, friends, or designated others; recognize that involvement of these individuals is critical to patient-centered care; and be knowledgeable about laws that support such involvement (Gerteis et al., 1993).
Disclosure of Errors
Disclosure of medical errors signifies respect for both patient autonomy and ethical standards (Gerteis et al., 1993; Gallagher et al., 2003) and should
be required of any medical practice. The majority (90 percent) of patients want and expect to be told about errors, particularly those that cause them harm (Wu et al., 1997; Brazeau, 1999; Blendon et al., 2002; Millenson, 2003; Mazor et al., 2004a; Gallagher and Levinson, 2005). However, rates of disclosure by providers have been quite low (about 30 percent)—this despite general agreement among providers that patients should be told about errors, as well as disclosure requirements outlined in hospital accreditation standards and some state laws (Sweet and Bernat, 1997; Blendon et al., 2002). The primary reasons for nondisclosure are fear of a malpractice suit, damage to the provider’s or hospital’s reputation, and the negative effect on provider–patient relationships. In reality, lack of disclosure is associated with lower levels of patient satisfaction, less trust of physicians, a more negative emotional response to care, and greater likelihood of a malpractice suit (Gallagher et al., 2003; Lamb, 2004; Mazor et al., 2004b).
Results of a number of studies confirm that patients want detailed explanations—they want to know what happened, what implications the error has for their health, why it happened, how the resulting problem will be corrected, and how future errors will be prevented (Gallagher et al., 2003; Mazor et al., 2004b; Manser and Staender, 2005). Just as important is the way an error is disclosed. Honesty and compassion in disclosure, along with a sincere apology, result in a more positive emotional response from the patient (Mazor et al., 2004b; Gallagher and Levinson, 2005). Health care providers must understand that disclosure of errors is part of a patient’s fundamental rights and quality of care. Moreover, all providers should be trained in good communication skills related to error disclosure. Materials and programs to help accomplish this are starting to become available in the form of courses and educational videos (see, e.g., http:// www.jhsph.edu/removinginsult/from/injury). Some organizations, such as the Veterans Health Administration (VHA), already are implementing policies for the disclosure of errors to patients or their representatives. The VHA published a directive in October 2005 stating that VHA facilities and individual VHA providers have an obligation to disclose adverse events to patients who have been harmed in the course of their care, including cases in which the harm may not be obvious or severe, or may be evident only in the future (VHA, 2005). The Harvard Medical School teaching institutions also have implemented guidelines for responding to adverse events (Harvard, 2006). The patient is free to involve family members in the disclosure process. Likewise, the University of Michigan Health System has instituted a disclosure program and has since seen reductions in legal costs (Wu, 2005). The “Sorry Works” Coalition also aims to promote error disclosure as an ethical imperative (SWC, 2005). However, these initiatives are not enough. Because there is no formal statute that dictates the seriousness of errors warranting disclosure, each health care organization defines
this independently. To resolve these differences and respect the intent of patient rights, the committee believes patients have the right to know about any clinically significant error.
UNDERSTANDING AND OVERCOMING BARRIERS EXPERIENCED BY CONSUMERS AND PROVIDERS
In the current health care system, a number of barriers affect the ability of consumers to engage in safe and effective self-management of their medications and the ability of health care practitioners to change their day-to-day practices to support new consumer-oriented activities. These barriers can be classified into three main areas: knowledge deficits, practical barriers, and attitudinal factors (Cohen, 2000).
According to the Institute of Safe Medication Practices (ISMP), many of these barriers are the root cause of nonadherence (Baird et al., 1984; Ansell, 1999; Sawicki, 1999; Tamada et al., 1999; Cummings et al., 2000). Nonadherence to a recommended treatment regimen, both intentional and unintentional, is defined as not filling a prescription initially, not having a prescription refilled, omitting doses, taking the wrong dose, stopping a medication without the provider’s consultation or advice, taking a medication incorrectly, taking a medication at the wrong time, or taking someone else’s medication (Cohen, 2000). Box 4-6 summarizes statistics on nonadherence among patients in the U.S. population.
For providers, barriers can present themselves as factors contributing to errors in all phases of the medication-use system (many of which were summarized in Chapter 2). Factors that directly impact the consumer– provider relationship and consumers’ capacity for medication self-management include the following:
-
Inadequate continuing education programs and overreliance on marketing materials for new knowledge about medications
-
Lack of patient educational materials and resources to support providers in this capacity
-
Use of free samples without appropriate documentation or in lieu of other, more appropriate treatment options (medication and nonmedication) for a particular patient
-
Complex, burdensome, time-consuming, and changing requirements associated with multiple payers and regulators
-
Poor workflow design, inadequate continuity of care, and lack of systems approaches and information technologies, which compromise efficiency, effectiveness, and safety
-
Lack of the support and leadership required to change from the current system to a patient-centered delivery system and a culture of safety
|
BOX 4-6 Rates of Inaccurate Medication Use by Consumers Problems with adherence exist in all populations but tend to be somewhat more prevalent among vulnerable groups, such as those with low literacy, low English proficiency, or cognitive impairment; the uninsured; those over age 70; and those with polypharmaceutial regimens (NQF, 2005). The effects of nonadherence are substantial both for patients and in terms of costs to the health care system. A recent meta-analysis of 569 studies found that the average nonadherence rate was 25 percent, resulting in as many as 188 million visits to health care providers (including hospitalizations). Analysis by disease estimates nonadherence at 8.4 million for hypertension, 7.6 million for diabetes, and 4.5 million for cancer. Analysis by regimen suggests 112.2 million for medication, 49.4 million for diet, and 22.6 for exercise recommendations. Based on these rates, the costs of nonadherence could be very high (billions of dollars per year) (DiMatteo, 2004). Individual studies have estimated significantly higher nonadherence rates. The University of Pennsylvania reported that about 50 percent of older adults have problems adhering to their prescribed regimen, and more than 10 percent of these cases result in hospital admissions (Schlenk et al., 2004). Other estimates of hospital admissions due to adverse drug events (ADEs) resulting from nonadherence are much higher: 23.5 percent for seniors (Michalsen et al., 1998) and 33 percent for all groups (McDonnell and Jacobs, 2002). Gurwitz and colleagues (2003) cite problems with patient adherence as a contributing factor in more than 20 percent of preventable ADEs that occurred at the prescribing and monitoring stages. A study of patients with hypertension and dyslipidemia who were prescribed a medication for each condition found that only 44.7 percent were adhering to their regimen 3 months after starting treatment, with a drop to 36 percent at 6 months and 1 year—a 64 percent nonadherence rate (Chapman et al., 2005). Other studies found that 20 to 71 percent of patients failed to take the prescribed dose, while 29 percent omitted taking the medication altogether (Bedell et al., 2000; Barat et al., 2001). Some interventions designed to address adherence have been evaluated (e.g., interventions specific to a disease, dose simplification, reminders); these evaluations have not found consistent outcomes among patient groups. Part of the reason for this is that the issue of patient adherence has received very little attention in the literature on patient safety relevant to preventing ADEs. A recent report of the National Quality Forum recommends the development of a set of standardized steps designed to improve adherence that could be implemented by providers as part of quality and safety improvement efforts (NQF, 2005). Where nonadherence is intentional and the result of informed patient preference, providers (and health care systems) need to understand these preferences and pursue other treatment options. |
This section provides an overview of key issues underlying knowledge deficits, practical barriers, and attitudinal factors that constitute barriers for consumers and providers. Resources and strategies for adequately addressing these issues are necessary to achieve patient-centered care and the consumer–provider partnership envisioned in this report.
Knowledge Deficits
The single greatest barrier to patient education and good medication self-management is insufficient knowledge about the safe and effective use of medications. Both providers and patients often are forced to make decisions in spite of knowledge deficits and take calculated risks as they weigh the pros and cons of medication regimens.
At the most global level, there may be insufficient knowledge available about the risks, benefits, and use of a drug, particularly in certain patient populations. Issues that affect the development of an adequate knowledge base for providers and patients are discussed in Chapters 2 and 6. Providers themselves may lack up-to-date pharmacologic facts, especially given the volume of products on the market and frequently changing safety information (IOM, 2004c; Schultz and Perrier, 1976). As cited by Woolsey (2000), for example, a two-page package insert for cisapride, when printed in a 12-point font on 8.5 × 11 paper, is more than 10 pages long and contains more than 470 facts about the drug (PDR, 2000). Prescribers would have difficulty mastering all of this information for even a single drug, much less the 40 to 100 medications that they regularly prescribe (Woolsey, 2000). Most can manage simply the basic facts, including when to prescribe a drug; in which quantity, dose, and frequency; how to counsel patients about taking the drug; what to look for when monitoring for effects; and how to handle patient abuse of a drug (Horvatich and Schnoll, 1991). In addition, drug information may not be presented in a way that accommodates the needs of different providers (physicians, nurses, pharmacists) within the scope of different time-sensitive uses (e.g., emergency care, surgery, clinical practice, home care) or decision-support systems (IOM, 2004c).
Systems to assist physicians, nurses, pharmacists, and the public in dealing with the overwhelming volume of information on drugs have not been identified or are not being implemented (Woolsey, 2000). Poorly developed continuing education programs and methods of incorporating new information into day-to-day clinical practice are major factors contributing to providers’ limited knowledge of medications (Balas et al., 1996; Blumenthal, 2004; Brennan et al., 2006). For example, physicians have little specific training or continuing education in prescribing medications for the elderly even though there is clear scientific evidence that these patients’ physiological differences affect drug metabolism and safety (Avorn, 1990; Pereles and Russell, 1996; Peterson et al., 2005). Further lacking are specific methods for teaching older adults how to self-manage medications, as well as prevent such common errors as mixing OTC and prescription medications, discontinuing prescriptions, taking wrong doses, using incorrect techniques, and consuming inappropriate foods with specific medications (Curry et al., 2005). Another obstacle to better patient education and self-management is the tendency of the medical establishment to organize
medical training and chronic disease management programs around single diseases and conditions despite the need for care that addresses those with multiple conditions taking multiple medications (Schroeder et al., 1986; Mullan, 1998). Lastly, use of complementary and alternative medications by consumers has increased dramatically, with a growing proportion requesting that these products be integrated into their treatment regimens (IOM, 2005). Except for selected hospitals, educational programs and licensure and credentialing requirements for integrated treatment with these products remain insufficient for the average practitioner (Cohen et al., 2005; IOM, 2005).
At the patient level, knowledge deficits are usually due to misunderstanding or the receipt of faulty or incomplete information about the medication regimen. Often such deficits are the product of limited provider–patient communications, low levels of literacy or English proficiency on the part of the patient, or inadequate educational materials and resources. The unfortunate result is that consumers’ actual knowledge about illness, illness prevention, and the function of medications is generally quite low (Haugbolle et al., 2002). For example, in as many as 62 percent of patients, misunderstanding or forgetting instructions from health care providers or printed medication materials is an important reason for non-adherence and poor health outcomes (Jenkins et al., 2003; Skoglund et al., 2003). A study of medication misadventures resulting in emergency room visits found that 30 percent of patients had no understanding and another 30 percent only some understanding of proper medication use (Schneitman-McIntire et al., 1996). Another study demonstrated that 73 percent of patients discharged from the hospital were aware of the course and purpose of their medication, but were unaware of side effects, needed lifestyle changes, and correct medication schedules (Kerzman et al., 2005). Clearly, when consumers do not understand information about their medications, safety may be compromised (Cohen, 2000).
In other instances, misunderstandings in provider–patient communications are attributable to the patient’s own lack of participation in the consultation, which can lead to inaccurate guesses and assumptions on the part of both provider and patient. Patients can also be confused by conflicting advice from their providers and other sources of information, such as pharmacy leaflets and the Internet (Bitten et al., 2000). One study of asthma patients found multiple examples of partial or total failure to understand drug information, even though patients had actively sought such information from a variety of professional and lay sources (Raynor et al., 2004).
Issues related to consumers’ health literacy, in terms of low levels of both general literacy and English proficiency, and providers’ cultural competence contribute further to deficits in knowledge about medications. Ac-
cording to the National Adult Literacy Survey, nearly half of all American adults (90 million people) have difficulty understanding and acting upon health information (IOM, 2004a). Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services as necessary to make appropriate health decisions (Ratzan and Parker, 2000). Functional literacy is the ability to use literacy to perform a task. It includes speech and speech comprehension (e.g., communicating symptoms to a doctor, discussing medication use), reading and writing (e.g., reading and understanding a prescription label, completing a medical history questionnaire), and basic math skills (e.g., calibrating a home care medical device, calculating the proper dose of a medicine). Even those with high general literacy skills may find health information difficult to obtain, understand, or use (IOM, 2004a); those Americans (40 million) with limited literacy and/or English proficiency, many of whom are poor, members of ethnic or cultural minorities, or with less than a high school education, are at a severe disadvantage in their ability to understand and act upon such information. For example, a Spanish-speaking patient may have an English-speaking physician who prescribes a heart medication to be taken once per day. Without an interpreter available, this patient, whose prescription has been filled in English, may translate the English words “once per day” as meaning “eleven times per day” in Spanish.
Another major factor contributing to the gap in knowledge, awareness, and understanding of medications among both high- and low-literacy groups is the inadequacy of drug information materials that are intended to supplement provider–patient communications and self-management. Few materials and resources are available to support providers in educating patients about their medications. Generally, educational exchanges with the provider are verbal; the provision of literature is relegated to the pharmacy, yet pharmacy leaflets vary in comprehensibility, utility, and design quality (Krass et al., 2002). The average pharmacy leaflet is written at a college reading level, four grade levels above the average reading comprehension level (grades 11–12) (Rolland, 2000), and lacks important information about precautions, drug–drug interactions, and symptoms of certain adverse reactions (Svarstad and Mount, 2001). Moreover, most pharmacies do not provide leaflets in commonly spoken languages to accommodate consumers with low English proficiency (Svarstad and Mount, 2001; Krass et al., 2002; IOM, 2004a). Knowledge deficits can be overcome by providing patients with more information or providing them with information in a more understandable forms, tailored to their level of education and their cultural/ethnic background (FACCT, 2001a; IOM, 2004a; AMA, 2005; AskMe3, 2005).
Practical Barriers
Practical barriers for providers generally can be classified as problems stemming from the health system itself, such as limited time for interactions with patients, prescribing requirements associated with multiple formularies, and lack of systems approaches and health information technology to improve workflow.
Providers are constrained in the amount of time they can spend with each patient for a number of reasons. Most visits to the doctor end with a prescription being written in the last 30 seconds, with limited discussion about the medication and the scope of important facts necessary for safe and effective medication use (George and Rabin, 1993; Gallagher et al., 2003; IOM, 2000). In a busy office practice, physicians often find it difficult to engage in lengthy discussions with patients about self-management, including medication use (Debusk et al., 1999; Ditmyer et al., 2003; Trude, 2003). Increased time pressures associated with clinical practice have been observed—patients waiting longer for appointments and more physicians reporting having inadequate time with patients (Trude, 2003). Constrained capacity also is the result of changes in the nature and prevalence of diseases in the population. Medical advances mean more treatment options are available to patients (Trude, 2003). People are living longer with chronic conditions that require more time to discuss treatment options and disease management, more complex coordination with other caregivers, and greater emphasis on preventive services (Trude, 2003). Some physician practices have employed physician assistants, nurse practitioners, nurse midwives, and clinical nurse specialists to counter the pressures of time and capacity. However, most ambulatory physicians cannot afford to hire additional office staff to assist them with patient education and counseling (Woolsey, 2000).
Prescribing requirements associated with multiple payers and formularies are another practical barrier affecting providers in their day-to-day practice activities. Some aspects of managing multiple different formulary requirements can be alleviated with the use of information technology.
For consumers, practical barriers to medication self-management inhibit an individual’s ability to follow through on a prescribed medication regimen because of physiological, functional, or financial constraints. Such barriers include visual, hearing, and cognitive impairment; the inability to act on one’s own behalf; complex medication regimens and adverse drug side effects; medication labeling and packaging that are difficult to read or use; and a lack of health insurance and the cost of drugs (Cohen, 2000). Seniors are particularly vulnerable as many of them are challenged by several of these barriers (NCHS, 1995).
Estimates of the number of people in the United States with visual
difficulty (even wearing their usual eyeglasses) range from 7 to 20 million for all ages; 1.5 to 2.0 million are estimated to have severe visual impairment (i.e., near-total or total blindness) (AFB, 2004). Of particular concern is that four of the five major causes of vision impairment and blindness are associated with aging,5 and the population of seniors is expected to double by 2030. Compromised ability to read instructions printed on drug containers or pharmacy leaflets creates a high potential for errors in self-managing medications. Consumers use a range of solutions, based generally on the severity of their impairment. For example, they may rely on friends or family members to read information on bottles or in leaflets, memorize the shape of a pill as it feels in their hand, use extra lighting and magnifiers, use a technological device (e.g., talking pill bottles, glucose meters with alerts) or a computer program that can convert printed information to Braille, or rely on their memory of oral communications (AFB, 2004). Nonetheless, methods for meeting the medication safety needs of individuals with various levels of visual impairment need to be more fully developed and widely distributed. Moreover, manufacturers need to make the printed information on prescription bottles easier to read for consumers in general.
Hearing-impaired individuals are compromised in their verbal communications with providers and pharmacists, which can lead to misunderstandings in the execution of the prescribed medication regimen. Since they are able to obtain and read written medication information, however, errors can be prevented more easily than for those with visual impairment.
Medication management requires not only a defined set of mental and physical skills, but also higher-level cortical processing and integration (Edelberg et al., 1999). With cognitive impairment, certain areas of the brain involved in thinking and higher-level executive functions (e.g., memory, language, reasoning, judgment, perception, attention, learning) are compromised to the point of interfering with the conduct of daily activities (NIMH, 2000; IOM, 2006). Even mild impairment, such as memory changes associated with the normal aging process, or fluctuating impairment, such as that associated with type II diabetes, can be a barrier to safe and effective medication self-management, especially when the ability to generate problem-solving strategies is required (Asimakopoulou and Hampson, 2002). Various interventions—psychosocial (e.g., caregivers, behavioral modification), technological (e.g., weekly pill organizers, electronic pagers), and others—can be effective in enhancing cognition and support for those with such impairment (Albert et al., 2003; Andrade et al., 2005).
The inability to perform self-care is another barrier to medication management when the impairment is high, when individuals are too sick to care for themselves, or when they are rendered unconscious. In such cases, individuals must rely completely on providers and other caregivers (e.g., family members, friends, surrogates) for medication management, safety, and error prevention. In these circumstances, informal caregivers require adequate training, education, and emotional support to carry out this role, whether for a short period, such as when a patient is postoperative, or for chronic conditions that require long-term care. Such caregivers can experience a significant burden that affects their quality of life and mental and physical health (McCullagh et al., 2005; Schrag et al., 2005; Vanderwerker et al., 2005), which in turn can result in medication errors.
It must be stressed that any policy or provider action that prevents a patient from having a designated surrogate present whenever the patient is receiving medication can be considered a barrier to safe and effective medication management. Given the amount of evidence for the occurrence of medication errors in hospitals, surrogates should be encouraged to question any professional about medications, routes of administration, and doses, and should be partners in reporting side effects patients may not be able to report themselves.
Another practical barrier to medication self-management can be the difficulty of opening a pill bottle or container, especially if an individual’s manual dexterity has been compromised by his or her condition (e.g., arthritis, broken arm, disability). Such individuals may give up trying to open the bottle and simply not take the medicine.
Undesirable drug side effects (expected or not) distress patients, add to the burden of their illness, and increase the costs of care (Barsky et al., 2002). They may result in nonadherence or discontinuation of an otherwise appropriate therapy, or they may increase the complexity of the regimen as drug(s) are added to treat the side effects. Polypharmacy contributes significantly to the likelihood of adverse drug reactions and drug–drug interactions. Difficulties with side effects are exacerbated in those that have impaired renal and hepatic function as a result of either age (e.g., seniors) or illness (e.g., HIV) (Cohen, 2000; Murray and Kroenke, 2001). Drug toxicity can manifest as a decline in functional status (e.g., problems in performing activities of daily living, confusion, drowsiness, and depression) or a more pronounced acute or long-term reaction (e.g., vomiting, heart arrhythmia) (LeSage, 1991).
The inability to pay for medications (or for health care in general) is one of the most frequently cited practical barriers to medication adherence, as well as to overall self-management of health conditions (Safran et al., 2005; Piette et al., 2006). To minimize out-of-pocket costs for drugs, individuals who are uninsured or underinsured may not fill a prescriptions at
all, skip doses, or take smaller doses to make the medication last longer (Cohen, 2000). Problems related to the cost of drugs are widespread; a recent poll showed that one of every three families has difficulty paying for prescriptions (AP, 2004). The elderly and those in lower income brackets are particularly affected by drug prices (Prutting et al., 1998), as are those subject to formularies that require high copayments even if no generic equivalent is available (Kamal-Bahl and Briesacher, 2004). Growing numbers of consumers are using the Internet to purchase lower-priced drugs, which may raise safety concerns (see Chapter 2).
Overcoming practical barriers requires a concerted effort to assist patients on the part of providers and other stakeholders. Providers should develop an understanding of how a medication regimen fits into the patient’s life, including the practical barriers likely to arise. Providers should be able to direct patients and their surrogates to the appropriate resources for further assistance with medication management. They also should follow up with patients to see how they are handling the effects of their medication and whether they are encountering any barriers that could interfere with adherence. Pharmacists, drug manufacturers, and regulators should redesign product labels and instructions to make them easier to read and understand, and should redesign product containers so they are easier to use.
Attitudinal Factors
At the provider level, attitudinal factors that influence caregiving range from organizational leadership, culture, and priorities to individual providers’ personal values. Improvements in patient safety (including medication safety and error prevention) are best achieved when health care organizations adopt a culture of safety (IOM, 2004c). A culture of safety6 can be defined as an integrated pattern of individual and organizational behavior, based upon shared beliefs and values, that continuously seeks to minimize patient harm that may result from the processes of care delivery (Kizer, 1999). Several studies have documented that the existing health care culture is likely the greatest barrier to improving patient safety (Leape, 1998; O’Leary, 1998; Cohen et al., 2003; Manasse and Thompson, 2005). Patient safety and patient-centered care have not been made a priority (Gerteis et al., 1993; Manasse et al., 2002). Most events are handled within the con-
text of a bureaucratic culture where errors are dealt with on an isolated, local basis, and lessons from failures are not integrated throughout the organization for purposes of improvement (Manasse and Thompson, 2005). The attitudes embodied in a culture of safety are not widely present within the majority of current health care organizations. To bring a culture of safety and quality to health care, fundamental change is required at both the organizational and individual practitioner levels (Bodenheimer, 1999). A core element of culture change is the patient-centered approach to care (Gerteis et al., 1993).
Patient-centeredness is an expression of organizational culture. While every health care organization’s and practitioner’s purpose is to serve patients, those that have successfully implemented a patient-centered approach to care have done so through a clear articulation of this mission of service, specific definition of the components of such service, and espousal of the approach by top management (Gerteis et al., 1993). Patient-centered care, then, permeates every facet of institutional life and practitoners’ interactions with patients. Some organizational environments are more conducive to patient-centered care than others.7 Chief attitudinal barriers to the adoption of patient-centered care from the organizational perspective are the failure to make patient-centered care a priority and redesign processes to support its multiple dimensions, lax or ineffective managerial intervention when such intervention can shape the quality of patient-centered care (e.g., efforts to attract, retain, and motivate the right people and socialize them into the institutional culture), and a lack of methods for measuring patients’ perceptions (Gerteis et al., 1993). At the level of the individual provider, attitudinal barriers to patient-centered care are associated with a belief that the care being given is patient-centered, whereas the provider in fact may not fully understand the components of such interaction; external factors that negatively impact the provider–patient relationship;8 preferences for formal sources of information (e.g., randomized controlled trials) for clinical decision making rather than patient preferences; frustration with poor
patient adherence to medical regimens rather than taking an empathetic approach to understand patient challenges; and challenges of the provider’s own work environment (e.g., long hours).
Consumer-related attitudinal factors that affect medication self-management are rooted in the individual’s belief system, culture, ethnicity, family, personal values, and previous experience with the health system (Cohen, 2000). Such factors affect everything from health beliefs to preferences regarding treatment, advance directives, organ donation, and disclosure, as well as truth telling (Berger, 1998). For example, cultural and religious beliefs can determine an individual’s role preference in decision making. African Americans place greater emphasis on security, survival, and community than do white Americans, who place greater value on personal autonomy, empowerment, and control (Murray, 1992). Asian and Hispanic cultures emphasize family support and involvement in decision making, as well as high regard for and deference to the physician (Blackhall et al., 1995). Euthanasia is broadly accepted in the Netherlands, and nondisclosure of a cancer diagnosis is common practice in Italy and Japan (Berger, 1998).
According to Berger (1998), assessment of both good and harm is culturally mediated, and acceptance of medication varies by ethnic group. In fact, the influence of attitudinal factors is so strong that some health care interventions are unsuccessful because of the provider’s failure to account for these factors. For instance, Afro-Caribbeans are less than half as likely as whites to take an antihypertensive medication (Morgan, 1995). White Americans are more likely to accept narcotic analgesics even if life is unintentionally shortened (Caralis et al., 1993). Herbal remedies are used commonly by Puerto Ricans to treat asthma and by Hispanics to treat diabetes (Zaldivar and Smolowitz, 1994; Pachter et al., 1995). Providers’ recognition of the cultural and religious contexts of their patients’ illnesses can thus be essential to a successful therapeutic relationship (Berger, 1998).
Culture and ethnicity aside, patients’ personal experiences related to their health condition can influence their attitudes toward treatment and self-management. A growing portion of the population—36 percent in a recent survey (NCCAM, 2004)—uses complementary and alternative medications as part of the treatment plan or as a first step prior to the use of conventional medications. (Some organizations, such as the Dana Farber Cancer Institute, refer to these as integrative therapies.) Patients’ preferences for these medications may engender a conflict between medical paternalism (the desire to do what is best for patients and protect them from foolish decisions) and patient autonomy (IOM, 2005). Moreover, individuals with serious and terminal illnesses may feel they are unable to tolerate any further traditional medicines with significant noxious side effects and prefer to seek relief with complementary and alternative therapies. Practi-
tioners should demonstrate willingness, at the very least, to maintain a professional knowledge base on such medications, including results of the latest research studies, from which they can counsel their patients, guide decision making, and protect patient autonomy.
Individuals may have negative attitudes about prescription medicines and/or health care providers in general that may affect their willingness to follow a treatment regimen (Getz and Borfitz, 2002). Educated consumers may be cautious because providers have prescribed drugs in the past that turned out to be dangerous to people’s health or have failed to prevent an ADE. They may also be aware that new drugs are not tested sufficiently to ensure that there will be no negative sequelae once the drugs are used outside of tightly controlled clinical trials in relatively healthy populations. Negative attitudes may be shaped as well by dislike of a medication’s side effects or delivery method, concern about the perceived risk of using a particular medication, or a general reluctance to take any medication (Osman, 1997).
Conversely, people may overvalue the potential benefits of medications while ignoring or minimizing their risks. A recent article in the New York Times highlighted young people’s sharing of psychiatric prescription medicines obtained from providers, their parents’ medicine cabinets, and the Internet (Harmon, 2005). Youths are trading unused drugs with each other not to get high, but to feel more focused, better rested, less stressed, and less depressed. They also believe that general practitioners are too pressed for time to be familiar with the increasing inventory of psychiatric drugs and are happy to take suggestions from their friends. While they understand the risks of illegal drugs, such as cocaine and heroin, they have no grasp of the potential danger of misusing or overusing prescription drugs (Harmon, 2005). Additionally, older individuals struggling to pay for prescription drugs will often trade drugs with their friends to save money (Schommer et al., 2003).
The IOM’s recent report on mental health and substance-use health care (IOM, 2006) expounds on the negative effects of stigma and discrimination on providers’ recognition of the capacity of individuals with these conditions for self-efficacy in making decisions about and managing their illness and its care. In fact, stigma and discrimination act as direct impediments to patient-centered care. Those with mental health or substance-use conditions can experience stigma (negative attitudes about members of a group) and discrimination (behaviors that result from these attitudes) from society at large or from unenlightened clinicians. Such stereotypes (1) lessen patients’ ability to participate in the management of their illness and achieve the desired outcomes; (2) encourage pessimistic and nontherapeutic attitudes and behaviors among clinicians, making them less likely to foster and support patients’ self-management efforts;
and (3) promote discriminatory public policies that create barriers to patient-centered care and recovery. In the present context, because mental health care in America is highly medication-dependent, stigma and discrimination may affect deliberations about medication choice, administration modality, and who will monitor for side effects and determine the level of satisfaction with treatment outcomes.
Religious beliefs can affect medical treatment in such areas as prenatal and end-of-life decision making, as well as in more common decisions about medication use. In these situations, conflicts with medical recommendations are less about the clinical facts than about the meaning of the facts and their implications for further action (Curlin et al., 2005). Individuals who decline treatment for religious reasons do so more often in situations of relative uncertainty and under conditions in which treatment modalities offer modest benefit over faith in God for healing. However, some religions require that all medical interventions be declined, while others preclude the use of only certain treatments or medications (e.g., antidepressants). Regardless of the individual’s reasons, courts have long held that patients have the right to refuse both medical treatment (Schloendorff v. Society of N.Y. Hospital, 211 N.Y. 125, 105 N.E. 92, 93 [1914]; Cobbs v. Grant, 502 P.2d 1, 12 [Cal 1972]), and mental health treatment or psychiatric medications (Cruzan v. Director, Missouri Department of Health, 497 U.S. 261 [1990]). For the majority of states, this includes the right of parents or guardians to refuse medical treatment for a child in their care based on religious beliefs without prosecution under federal laws governing abuse and neglect.9 In life-or-death situations, however, a physician or hospital can obtain a court order to proceed with treatment for the child (Annas, 2004).
Attitudinal factors are more difficult to address than the other barriers discussed above as they embody an individual’s personal beliefs and values, protected by the U.S. Constitution. Unless safety is seriously compromised (e.g., by youngsters trading drugs), most attitudinal factors should be taken into consideration when a medication regimen is being designed.
RESOURCES TO SUPPORT THE CONSUMER–PROVIDER PARTNERSHIP
Activating consumers on a national scale will require the development and refinement of resources to provide support at all stages of the medication-use process across all health care settings. Specifically, health and medication information and educational tools must be revised to have consumer-friendly formats; a variety of supportive interventions for medication safety and self-management education should be developed and tested; systems that provide around-the-clock access to clinical support should be developed; information technology tools should incorporate programs that support medication management and general self-care; and regulatory councils should expand consumer participation. All stakeholders in the health system (e.g., government regulators, payers, employers, industry) should make contributions to the development and implementation of these means of support for consumers and providers.
Recommendation 2: Government agencies (i.e., the Agency for Healthcare Research and Quality [AHRQ], the Centers for Medicare and Medicaid Services [CMS], the Food and Drug Administration [FDA], and the National Library of Medicine [NLM]) should enhance the resource base for consumer-oriented drug information and medication self-management support. Such efforts require standardization of pharmacy medication information leaflets, improvement of online medication resources, establishment of a national drug information telephone helpline, the development of personal health records, and the formulation of a national plan for the dissemination of medication safety information.
-
Pharmacy medication information leaflets should be standardized to a format designed for readability, comprehensibility, and usefulness to consumers. The leaflets should be made available to consumers in a manner that accommodates their individual needs, such as those associated with variations in literacy, language, age, and visual acuity.
-
The NLM should be designated as the chief agency responsible for Internet health information resources for consumers. Drug information should be provided through a consumers’ version of the DailyMed program, with links to the NLM’s Medline Plus program for general health and additional drug information.
-
CMS, the FDA, and the NLM, working together, should undertake a full evaluation of various methods for building and funding a national network of drug information helplines.
-
CMS, the FDA, and the NLM should collaborate to confirm a minimum dataset for personal health records and develop requirements for vendor self-certification of compliance. Vendors should take the initiative to improve the use and functionality of personal health records by incorporating basic tools to support consumers’ medication self-management.
-
A national plan should be developed for widespread distribution and promotion of medication safety information. Health care provider, community-based, consumer, and government organizations should serve as the foundation for such efforts.
Pharmacy Leaflets
Written information about prescription drugs for consumers is available in various forms (e.g., medication guides, pharmacy leaflets, patient package inserts,10 websites). Consumers rely primarily on pharmacy-distributed documents (i.e., medication guides and leaflets) for basic information and instructions about their medications. Medication guides (as defined in Chapter 2) are pharmaceutical company–produced and FDA-approved labels that are required to be provided to consumers for drugs that pose a serious and significant public health concern if certain circumstances exist.11 While the law (21 Code of Federal Regulations Part 208) requiring distribution of medication guides was not formally passed until 1999 (NARA, 1999), the FDA began requiring additional warnings and consumer-oriented information for certain high-risk drugs, such as isoproterenol products, in the late 1960s and for oral contraceptives (by means of patient package inserts) in the 1970s (DHHS, 1996). Through these early initiatives, the FDA recognized the benefit of such information to safe, effective medication use. At several points in subsequent decades, the FDA sought to pass formal regulations requiring the provision of consumer-oriented information for all prescription drugs; each time, however, the
legislation failed.12 Instead, Public Law 104-180 was passed in 1996, establishing a process for voluntary development and distribution of medication information for consumers in the form of pharmacy leaflets.
Pharmacy leaflets (also known as consumer medication information or CMI)—the computerized printouts that are attached to or placed in the prescription bag at the pharmacy—are now the most common form of medication information received by consumers. Neither the FDA nor state boards of pharmacy regulate the content of the leaflets, although the FDA did produce the Keystone report (DHHS, 1996), which provides guidance on leaflet design and content. If written in a clear, understandable manner, leaflets can be an important supplement to provider–patient communications. They can help bridge information gaps, clarify specific instructions, reinforce safety precautions, and increase adherence (Bernardini et al., 2000). For such results to occur, however, the leaflets must be easy to read, understand, and act upon (Gustafsson et al., 2003).
Unfortunately, a number of studies have confirmed that the quality of pharmacy leaflets remains inadequate, and varies widely from one pharmacy vendor to another and from one drug to another (Morrow et al., 1988; Svarstad and Mount, 2001; USP, 1999). Primary problems include a lack of standardized consumer-friendly nomenclature, incomplete or inaccurate information, inadequate layout and design for readability, and a lack of regulatory review and approval prior to use. A U.S. Pharmacopeia (USP) study found that these and various cognitive features can affect consumers’ ability to find, understand, remember, and use the information provided (USP, 1999). Many types of health information, ranging from informed consent forms and public health information to prescription instructions and health education materials, are provided in written form characterized by jargon and technical language that make them unnecessarily difficult for consumers to use (Rudd et al., 2000). Cultural, language, and age differences exacerbate problems with comprehension, particularly since leaflets cannot be adjusted to accommodate individual needs (Gustafsson et al., 2003). There have been exceptions (such as the USP MedCoach leaflets with gender-specific and easy-to-read versions), but they have proved difficult to maintain. Research has found that key information deemed by consumers to be most important to them but missing or deficient in the leaflets is that related to risks (i.e., contraindications and drug interactions), followed by administration (i.e., directions and precautions) (Meryn, 1998; Svarstad and Mount, 2001; Garfield et al., 2004; Raynor et al., 2004).
A major part of the problem has been follow-through on the processes established by Public Law 104-180. Specifically, the law set basic standards for content and design, and there are plans to study the extent of leaflet distribution at two specific target dates (2001/2002 and 2006/2007). However, the standards were never fully developed or implemented, and the most extensive studies on content and design have been undertaken by other organizations, such as USP, and individuals. As a result, most pharmacies distribute leaflets, but the only standard is a de facto one set by the market. To move forward with leaflet design, the FDA published a draft guidance document in May 2005 describing how vendors should implement the Keystone criteria. However, those criteria need further improvement to address critical barriers experienced by consumers when trying to read, understand, and act on medication information in the leaflets. Remaining concerns about leaflet readability, comprehensibility, and usefulness to the consumer must be resolved to support safe and effective medication use.
Additional work on human and cognitive factors engineering aspects of content and design should be undertaken for the various consumer information sources (i.e., pharmacy leaflets, medication guides). Expanded studies should be based on well-known cognitive principles identified in the USP (1999) study, including the following:
-
Information load (i.e., the amount of information presented)
-
Study time (i.e., the limited amount of time someone will actually spend reading the information)
-
Depth of processing (i.e., the way information can be processed to increase memory and understanding)
-
Chunking (i.e., breaking up items into smaller, more manageable pieces)
-
Linguistic coding (i.e., internal ways of naming or coding information to increase memory and understanding)
-
Prior knowledge and knowledge structures from previous experiences that may make it easier to learn and recall new information
-
Cognitive task scenarios that test the ability to utilize the information in problem solving situations (USP, 1999).
Along with work on human and cognitive factors, studies should be undertaken to develop and evaluate pictograms that could be used in leaflets to accommodate certain populations. Some studies have evaluated the use of pictograms to improve readability and comprehensibility, but their findings do not support major improvements in the comprehensibility of leaflet information (TGA, 2002; Hameen-Anttila et al., 2004; USP, 1999). In one study, reasons for neutral results included disconnects between pictograms and leaflet information, nonuse of text within pictograms to rein-
force the message, and too many visual elements (USP, 1999). For example, pictograms meant to convey “ask/tell your doctor if you are pregnant” were interpreted as “don’t use this drug if you are pregnant;” other pictograms meant to convey “don’t drive” and “don’t share medicines” did not translate at all. Researchers agree, however, that standardized, well-designed, and comprehensively tested pictograms would be valuable and safe to use for intended patient populations, particularly those in vulnerable groups (e.g., children, the elderly, those with poor sight or low literacy skills) (Hameen-Anttila et al., 2004).
Implementation of the leaflets designs can be relatively simple. Pharmacy database vendors can develop software programs that allow the pharmacist to generate a leaflet according to selected characteristics to accommodate the individual needs of consumers.
Lastly, the lack of an established regulatory review prior to distribution has compromised the effectiveness of leaflets. The committee believes FDA leadership is necessary to ensure that leaflet content and design promote safe and effective medication use and accommodate the needs of all consumer populations. The FDA could establish an advisory council for this purpose. Box 4-7 outlines specific tasks for leaflet improvement that encompass but go beyond those identified in the Keystone report (DHHS, 1996).
Pharmacy Container Labels
Along with pharmacy leaflets, the labels applied to medication containers dispensed at the pharmacy warrant significant improvement. Container labels that are difficult to read or easy to confuse with those for other medications increase the likelihood that an error will occur (Cohen, 2000). (Issues concerning the external packaging and labeling generated by drug manufacturers, which affect health care providers, are discussed in Chapter 6; the discussion here focuses on bottle labels generated at the pharmacy, which affect consumers.)
At the community pharmacy, almost all medications are dispensed in similar-looking brown, bottle-shaped containers with white labels providing basic drug information. Warnings (e.g., may cause drowsiness, take with food) are placed horizontally on the containers on yellow stickers that may include a pictogram. Typically for drug information and warnings, the point size is quite small (i.e., 10 or smaller), and the labels may contain abbreviations, acronyms, or other terms that are difficult for consumers to read and understand. Moreover, the readability of label information is compromised when the label is placed horizontally so that it can be read only by turning the bottle around, and when characters are compressed to fit the small space of the label (Wogalter and Vigilante, 2003).
|
BOX 4-7 Principles for Improving Pharmacy Medication Information Sheets (Leaflets) The FDA and the National Library of Medicine should:
The FDA should:
|
Sometimes warning labels are stuck on the bottles over other important information or each other. These problems of readability and comprehensibility are compounded for those individuals with visual or hearing impairment, memory problems, or language or literacy difficulties (Drummond et al., 2004). Moreover, opening containers with safety caps
can be problematic for older individuals, exacerbating their difficulties in taking their medications (Beckman et al., 2005).
Several studies of all types of labeling have demonstrated the importance of label format—point size, font type, font compression, design/ layout, and terminology (including acronyms)—for readability, comprehensibility, and usefulness to consumers (Cramer, 1998; Cohen, 2000; Wogalter and Vigilante, 2003). For example, Drummond and colleagues (2004) noted significant improvements in comprehension and adherence among older adults when the label font was Arial 22 or the equivalent— almost three times the point size normally used on medication labels. Adjusting the format of pharmacy bottle labels is one of the simplest, lowestcost means of improving consumer understanding of the information presented (Wogalter and Vigilante, 2003).
Some pharmacies are experimenting with new designs for the shape of medication containers and for labels. For example, the new bottle and label design implemented by pharmacies at Target™ retail stores, called Clear Rx™, is an upside-down bottle made from red clear plastic with flat front back surfaces for printed information, including up to five warnings (Hafferty, 2005). Removable colored rings can be added around the bottle opening to differentiate family members’ medications or an individual’s different medications. On the label, light blue bands separate each item of labeling information. The name of the prescription is in bold and all capital letters, highlighted by a light gray background. Below the drug name are the instructions for use, followed by a colored band, then secondary information, such as the number of tablets/capsules, date, number of refills, prescriber’s name, drug routing information, and pharmacy phone numbers (Hafferty, 2005). Additional information about side effects and warnings are printed on a small card that slips under the back portion of the label.
The FDA is now exploring the development of a general set of requirements for redesigning pharmacy containers and labels to improve their safety and quality. Comparative studies of different designs should be undertaken to determine those optimally useful to consumers. Such efforts should incorporate the principles of human factors engineering and include thorough testing in the general population. As with pharmacy leaflets, attention should be given to the needs of various consumer groups; different designs may be necessary to accommodate these varying needs.
Drug Information on the Internet
The proliferation of Internet-based health information over the last decade has given consumers immediate access to valuable resources such as medical journals and libraries, disease management guidelines, medication
information, and treatment alternatives, and consumers are increasing their use of the Internet to obtain this information. The proportion of adults who have sought health information online grew from 27 percent (54 million) in 1998 to 53 percent (117 million) in 2005 (HI, 2005). Many consumers believe that Internet health information is highly reliable (37 percent) or somewhat reliable (53 percent). In reality, however, the quality of health and drug information on the Internet remains quite variable (Griffiths and Christensen, 2000; Berendt et al., 2001; Eysenbach et al., 2002; Risk and Petersen, 2002). This variability stems from the multitude of sources of information and differing standards (or the lack thereof) for developing content (Silberg et al., 1997; Berland et al., 2001; Eysenbach et al., 2002).
Most drug information on the Internet is not peer reviewed, but is developed from lay or commercial sources. Those sources may include other Internet sites that attempt to provide medical information for all needs (e.g., http://www.drkoop.com, webmd.com), that target specific health and medication information needs (e.g., American Cancer Society [http://www.cancer.org], http://www.hopkins-aids.edu), or that are maintained by health care providers and pharmaceutical companies (Gawande and Bates, 2000). Much drug information from nonpeer-reviewed sources tends to be poor and on occasion can even be harmful (Doupi and van der Lei, 1999; Boyer et al., 2001; Crocco et al., 2002). Many Internet pharmacies that sell prescription drugs, OTCs, dietary supplements, and complementary and alternative medications are particularly known for presenting inadequate, inaccurate, misleading, or fraudulent information (Eysenbach et al., 2002; Bessell et al., 2003; Molassiotis, 2004; Oakley, 2005). Yet in many cases, these sources are the first retrieved from Internet search engines (Peterson et al., 2003). The commercial website of a drug’s pharmaceutical manufacturer, which highlights the drug’s benefits and downplays its risks, tends to be one of the first retrieved as well. Because most consumers do not go beyond the first page of search results, they are not easily or automatically accessing the highest-quality or most objective drug information from the most respected sources, such as the National Library of Medicine (NLM). They may not know exactly where to find the best information or how to evaluate the quality of information from various sites. Moreover, the most respected sources of drug information— the NLM, the FDA, other government sources, peer-reviewed journals, health care provider organizations, consumer organizations, and pharmaceutical companies—are available online in multiple formats, at various levels of detail, and often with data that conflict with each other, further confusing consumers (Eysenbach et al., 2002).
Government agencies are collaborating to develop reliable, high-quality, consumer-friendly health and medication information available to the general public online through the NLM. In particular, NLM’s MedlinePlus
program provides information online in English that is easy to read, with interactive tutorials and voice recordings to facilitate learning (Personal communication, E. Humphreys, 2003). The tutorials, available for more than 150 health topics, are a popular feature in part because they are suitable for those with low levels of literacy. In addition to providing standardized health information, the NLM has a leadership role in the development of standardized electronic drug information for providers through the DailyMed program. The DailyMed database, as its name suggests, is intended to provide updates of medication information to the public on a daily basis (Brown et al., 2003). The NLM’s MedlinePlus program does provide consumer-oriented drug information developed by several sources. However, greater standardization is needed. On MedlinePlus, consumers should have access to the electronic versions of standardized pharmacy leaflets and consumer-oriented versions of product package inserts (or patient information sheets). The FDA has been working with pharmaceutical companies to standardize the latter inserts (see Chapter 6), but more work is needed on current versions to employ more consumer-friendly nomenclature.
An important aspect of raising public awareness of quality information available at the NLM website is ensuring that this information is placed as the first to be retrieved when consumers search the Internet for health and medication information. Such placement of the NLM’s resources and peer-reviewed literature is critical to improving consumer education and access to information resources. The NLM, search engine developers, and Internet service providers should collaborate to develop mechanisms that support the NLM’s placement as a top resource for Internet health information.
The committee believes continued leadership by the NLM and the FDA is necessary to make health and medication information widely available to the public in standardized form and everyday language. The NLM should receive funding for several specific tasks aimed at advancing the online availability of quality health and medication information (see Box 4-8).
Telephone Helpline
Telephone intervention and helpline support programs in several countries have proven to be a successful resource for consumers seeking medical advice and information. Consumers can receive advice around the clock about general self-care and self-management of symptoms related to their health condition, medication, or drug side effects, as well as information about their health and prescription drug benefits. Helplines are an important supplement to provider services, giving consumers immediate access to effective care when they are unsure how best to care for themselves or for another as a designated surrogate. Such interventions have resulted in im-
|
BOX 4-8 Tasks the National Library of Medicine Should Undertake to Develop Quality Internet Resources for Drug Information
|
proved health outcomes, decreased provider and emergency room visits, and ultimately reduced health care expenditures (Reigel et al., 2002; Bosworth et al., 2005; Caithain et al., 2005). Self-confidence and self-efficacy in handling one’s own health problems are also noted benefits of telephone interventions (Brooks et al., 2004).
Currently, most telephone helplines are available through health care providers and target certain health conditions, such as cancer (Jefford et al., 2005), chronic heart failure (Reigel et al., 2002), rheumatoid arthritis (Hughes et al., 2002), hypertension (Bosworth et al., 2005), and mental health problems (De Leo et al., 2002). Some address the needs of specific patient populations (e.g., pediatric patients) and are manned by physicians who share resources (Poole et al., 1993). For providers, the Physicians’ Desk Reference (PDR, 2005) provides lists of toll-free numbers for pharmaceutical companies staffed by nurses and pharmacists well qualified to provide drug information.
In Western Australia, nurses provide health information associated with general practice by telephone statewide (Turner et al., 2002); similar services are offered nationally in Canada (Robb, 1996), Denmark (Christensen and Olesen, 1998), and the United Kingdom (Caithain et al., 2005). The National Health Service (NHS) in the United Kingdom has by far the most
well-developed telephone intervention and helpline support system in the world—NHS Direct (Caithain et al., 2005). Individuals can call the service and receive advice for a per minute fee; the average call costs £18.00 or roughly US$31.00. In all cases, nurses are the primary health professionals providing telephone intervention and helpline support (Greatbatch et al., 2005). Strict protocols and standards for evaluating consumers’ health needs, along with clinical decision-support software, guide the helpline consultations.
In the United States, consumers receive telephone assistance with questions about their prescription medications by directly contacting their health care provider, local pharmacist, or prescription benefit manager or going to the emergency room. This approach may not be able to meet the growing health demands and information needs and the changing demographics of the U.S. population. Use of all medications has increased tremendously in recent decades, now representing 11 percent of overall health care expenditures (NCHS, 2005). Of these expenditures, ADEs are the largest safety-related cost to the health system. Many of these events are the result of misunderstanding proper use of a drug. There are also enormous gaps in timely access to advice and information about medications, particularly for the 43 million Americans who are uninsured (IOM, 2004b) and those with literacy and language difficulties (IOM, 2004a).
Consumers need quick, easy access to drug information, advice about minor problems, and information on what to do about side effects and adverse reactions for the range of products on the market. The committee believes establishing a national drug information telephone helpline (a “drugline”) could serve this purpose. The drugline would give consumers a third option for obtaining information about proper medication use, complementing paper and online sources they may not be able to access, read, or understand. In particular, establishing the drugline would accelerate the availability of medication assistance to consumers with health literacy, language, and other barriers. However, it will take significant time and funding to expand existing online resources. Building a national drugline similar to that in the United Kingdom would be expensive. In fiscal year 2002– 2003, the cost of the NHS Direct program was £124 million (US$216.6 million). Thus, leveraging the existing health care and public health infrastructure may be the best option for developing the drugline and trimming the overall costs for doing so.
One possibility may be the expansion of poison control centers to include drug safety counseling. Several centers have collaborated with nearby universities and already initiated expansion in this capacity. For example, the Arizona Poison and Drug Information Center operates as part of the University of Arizona, Health Sciences Center, College of Pharmacy, providing accessible poison- and medication-related emergency treatment
advice; referral assistance; and comprehensive information on poisons and toxins, poison prevention, and the safe and proper use of medications (APDIC, 2005). As another example, along with counseling on poison-related events, the Rocky Mountain Poison and Drug Center provides health and safety information on the safe and effective use of medications, adverse reactions, drug interactions, and drug use during pregnancy and lactation (RMPDC, 2006). Pharmaceutical companies contract with the center to provide their customers 24-hour access to medical information, to collect information on adverse drug events, and to meet other regulatory requirements. The Denver Health Nurse Line also is part of the Rocky Mountain Poison and Drug Center, providing 24-hour access to medical triage for health concerns. Potentially, a combination of existing funds from local, state, and private sources could be used, together with additional allocations from private and federal sources, to finance such expansion of poison control centers nationwide.
A drawback to this approach may be the question of whether most poison control centers are adequately funded and structured to handle drug information and counseling services. Currently most are not, but they can be. The 2004 IOM report Forging a Poison Prevention and Control System highlighted many of the issues involved, citing financial instability, lack of network or systems infrastructure (each operates independently), lack of effective links to the nation’s public health system, and data collection that operates through a proprietary system (IOM, 2004e). The report made several recommendations for improvement, many of which have yet to be implemented. Policy makers should revisit the recommendations of this report in evaluating possibilities for development of the proposed drugline.
The federal government should undertake a full evaluation of various methods for building a national network of drug information helplines and develop strategies for their ongoing funding and financing. Knowledge gained from the successful telephone intervention and helpline support programs mentioned above can be incorporated into the strategy for developing these centers, along with other guidance outlined in Box 4-9. The druglines should include a mechanism for consumers to report ADEs and medication errors.
Personal Health Records
Emerging information and communications technologies have great potential to improve consumers’ self-management of their health and health conditions (Markle Foundation, 2005). Over the last 5 years, several initiatives have been launched to develop and market computerized personal health records (PHRs) as a viable technology to support self-management. In general, PHRs were intended to function as an extension of electronic health
|
BOX 4-9 Guidelines for a National Drugline The drugline should:
|
records (EHRs) that would allow individuals to access certain portions of their health record (e.g., medication record, laboratory test results) through a secure portal. Individuals would also be able to enter information in the PHR/EHR system, such as that related to diet, exercise, adherence to treatment/medication plans, and OTC medications. However, slow adoption of EHRs by providers overall and some concerns about the privacy and security of health information on the part of consumers have resulted in several different types of web-based and stand-alone systems (Waegemann, 2002): (1) offline PHRs are composed of health-related documents carried in paper-based files or booklets, or electronically on a CD-ROM or smart card; (2) commercial PHRs store a consumer’s health information on a secure webpage; (3) functional/purpose-based PHRs are web-based records accessible for a specific service, such as emergency care; (4) provider-based PHRs are those for which the provider or health plan makes portions of personal health information available through the provider’s website/portal; and (5) partial PHRs allow an individual to keep an electronic file of health information and literature about diseases and conditions downloaded from the web, and also can be used by the web provider for marketing purposes.
Most PHRs function simply as a file of data; only a few have capabilities to support self-management. Yet even a holding file plus some modest upgrades can be useful to facilitate medication self-management. Specifically, the following functionality should be required for PHRs: information about safe medication use; printable medication record sheets with areas for listing drug allergies; patient safety reporting forms; and links to online
drug libraries, drug interaction checkers, and medication adherence tools. The Markle Foundation Connecting for Health Initiative identified components of a minimum dataset for PHRs: (1) personal and emergency contact information, (2) physician and insurance information, (3) health condition information, (4) medications, (5) allergies, (6) immunization history, (7) certain test results, (8) surgical history, (9) health risks, (10) lifestyle information, and (11) advance directives (Markle Foundation, 2003).
Innovative tools designed for specific patient populations (e.g., seniors) to support medication adherence and self-monitoring of medication effects could prove highly useful to increase compliance. Eventually, PHRs and more comprehensive disease management programs can be integrated; at this time, however, they remain independent.
Information Dissemination
Important information and resources must be readily accessible to consumers to increase their awareness, knowledge, and active involvement with regard to medication safety on a national scale. Consumers should be able to obtain information not only from their providers, but also through community-based resources, consumer organizations, and public health networks. The information available should include general medication safety practices or tips, as well as guidelines for specific medications and polypharmacy regimens, medication self-management strategies, and methods for reporting ADEs and medication errors. Also, information should be available in both paper and electronic format, with variations to accommodate the consumer’s individual needs and preferences. The lack of an overall strategy and resources for dissemination of information on medication use and safety has resulted in limited consumer knowledge and activation. Thus, the broad array of organizations already interacting with the medication-use system should develop strategic plans and leverage their resources to disseminate such information more broadly to consumers. Some examples of organizations that have developed consumer-friendly brochures or leaflets on general safe medication practices that providers can distribute to patients or consumers can print from the Internet are highlighted in Box 4-10.
Along with brochures, other means of disseminating information should be used, such as the development of health information resource centers. For example, retail pharmacies could set up medication kiosks for consumers13 who would like to look up or print out additional information about
|
BOX 4-10 Examples of Consumer Medication Safety Materials The National Council on Patient Information and Education (NCPIE) has developed several brochures describing what consumers can do to improve medication safety and prevent errors. Examples are Be MedWise: Use Over-the-Counter Medicines Wisely (http://www.bemedwise.org/brochure/bemedwise_english_brochure.pdf) and Prescription Pain Medicines: What You Need to Know (http://www.talkaboutrx.org/assocdocs/TASK/18/pain_bro.pdf). The Massachusetts Coalition for the Prevention of Medical Errors has published a guide for patients and families titled Your Role in Safe Medication Use (http://www.mhalink.org/public/prodserv/Docs/consumerguide.pdf). The FDA collaborated with the Council on Family Health to produce such brochures as Be an Active Member of Your Health Care Team (http://www.fda.gov/cder/consumerinfo/Active12panel.pdf) and Medicines and You: A Guide for Older Adults (http://www.fda.gov/cder/consumerinfo/MedandYouEng.pdf). The American Pharmacists Association has developed a brochure on Avoiding Medication Errors (http://www.pharmacyandyou.org/aboutmedicine/med.html). The Institute for Safe Medication Practices has produced a pamphlet titled Be an Informed Consumer (http://www.ismp.org/Consumer/Brochure.html). The above materials are a good start for information on safe medication use, but their dissemination is not as widespread as is needed. Moreover, the materials need to specify where to find additional information about health and medications, such as the NLM’s MedlinePlus website (http://medlineplus.gov), and how to report problems or ADEs through the FDA’s MedWatch Program (http://www.fda.gov/medwatch). |
their medications. Public libraries could establish health resource areas for consumers interested in obtaining health and medication information or leaflets. School health programs and libraries could distribute child- or adolescent-oriented materials on safe medication use and what to do should a problem occur. Waiting areas in ambulatory care offices could serve as venues for patient education through videotapes, computers, and/or paper-based information on health conditions and on good medication self-management practices. The waiting area could display lively posters explaining the patient’s rights and responsibilities with regard to medication safety (e.g., why it is important for the doctor to know if the patient is taking herbal or other dietary supplements).
Communication networks already in place, such as those associated with the public health infrastructure, should be utilized for medication safety initiatives. The Centers for Disease Control and Prevention recently completed the consolidation of its dissemination activities into one center—the National Center for Health Marketing (NCHM). The goal of NCHM is to help people actively use accessible, accurate, relevant, and timely health information and interventions to protect and promote their
|
BOX 4-11 Actions to Disseminate Medication Information and Resources
NOTE: Medication information used for dissemination activities should be scientifically accurate, useful, and comprehensible to patients and their families, rather than the type of information used for commercial purposes. |
health and that of their families and communities (CDC, 2005). The center has a number of divisions that could be employed for dissemination of medication safety information, including the divisions of Public and Private Partnerships, Consumer Services, and State and Local Public Health Systems. Other federal communication networks affiliated with the FDA, the NLM, and CMS could provide additional resources to broaden dissemination activities. Consumer organizations (e.g., Consumers Union, American Association of Retired Persons) could also serve as valuable resources. As membership-based organizations, they have extensive networks reaching out to millions of Americans and offering significant opportunities to expand communications about medication safety. Their members have access to information through online and paper publications that often include health and medication information. These organizations also provide telephone information helplines to assist their members in understanding important information, such as that on drug benefit plans. Actions the committee believes should be taken to better disseminate information and resources on medication safety are summarized in Box 4-11.
REFERENCES
AACN (American Association of Colleges of Nursing). 1998. The Essentials of Baccalaureate Education for Professional Nursing Practice. Washington, DC: AACN.
AAMC (Association of American Medical Colleges). 1999. Report III: Contemporary Issues in Medicine: Communication in Medicine. Washington, DC: AAMC.
ACF (Administration for Children and Families). 2005. Overview of Abuse and Neglect. [Online]. Available: http://nccanch.acf.hhs.gov/topics/overview/index.cfm [accessed March 27, 2006].
AFB (American Foundation for the Blind). 2004. Submission to the FDA for the Medicare Prescription Drug Improvement and Modernization Act of 2003: Study on Making Prescription Pharmaceutical Information Accessible for Blind and Visually Impaired Individuals. Docket 2004N-0221, June 25, 2004.
Albert SM, Flater SR, Clouse R, Todak G, Stern Y, Marder K. 2003. Medication management skill in HIVL I. Evidence for adaptation of medication management strategies in people for cognitive impairment. II. Evidence for a pervasive lay model of medication efficacy. AIDS and Behavior 7(3):329–338.
AMA (American Medical Association). 1998. Informed Consent. [Online]. Available: http:// www.ama-assn.org/ama/pub/category/4608.html [accessed December 2005].
AMA. 2005. Helping Your Patients Understand. [Online]. Available: http://www.ama-assn. org/ama/pub/category/9913.html [accessed February 6, 2006].
Andrade AS, McGruder HF, Wu AW, Celano SA, Skolasky RL, Selnes OA, Huang IC, McArthur JC. 2005. A programmable prompting device improves adherence to highly active antiretroviral therapy in HIV-infected subjects with memory impairment. Clinical and Infectious Diseases 41(6):875–882.
Annas GJ. 2004. The Rights of Patients: The Authoritative ACLU Guide to the Rights of Patients. 3rd ed. New York: New York University Press.
Ansell JE. 1999. Empowering patients to monitor and manage oral anticoagulation therapy. Journal of the American Medical Association 281(2):182–183.
AP (Associated Press). 2004. Almost a Third of Americans Say Paying for Drugs Is a Problem in Their Families. [Online]. Available: http://www.ipsos-na.com/news/pressrelease.cfm?id= 2064 [accessed November 15, 2005].
APDIC (Arizona Poison and Drug Information Center). 2005. Arizona Poison and Drug Information Center. [Online]. Available: http://uanews.org/cgi-bin/WebObjects/UAMaster Calendar.woa/2/wa/goPrint?EventID=1232 [accessed March 21, 2006].
Armstrong D. 1982. The doctor-patient relationship: 1930-1980. In: Wright P, Treacher A, eds. The Problems of Medical Knowledge. Examining the Social Construction of Medicine. Edinburgh, Scotland: Edinburgh University Press.
Arora NK, McHorney A. 2000. Patient preferences for medical decision making: Who really wants to participate? Medical Care 38(3):325–341.
Asimakopoulou K, Hampson SE. 2002. Cognitive functioning and self-management in older people with diabetes. Diabetes Spectrum 15(2):116–121.
AskMe3, Partnership for Clear Health Communication. 2005. Information for Patients. [Online]. Available: http://www.askme3.org [accessed February 6, 2006].
Avorn J. 1990. The elderly and drug policy: Coming of age. Health Affairs 9(3):6–19.
Baird MG, Bentley-Taylor MM, Carruthers SG, Dawson KG, Laplante LE, Larochelle P, MacCannell KL, Marquez-Julio A, Silverberg LR, Talbot P. 1984. A study of efficacy, tolerance and compliance of once-daily versus twice-daily metoprolol (Betaloc) in hypertension. Betaloc Compliance Canadian Cooperative Study Group. Clinical and Investigative Medicine 7(2):95–102.
Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. 1996. The clinical value of computerized information services. A review of 98 randomized clinical trials. Archives of Family Medicine 5(5):271–278.
Barat I, Andreasen F, Damsgaard EMS. 2001. Drug therapy in the elderly: What doctors believe and patients actually do. British Journal of Clinical Pharmacology 51:615–622.
Barsky AJ, Saintfort R, Rogers MP, Borus JF. 2002. Nonspecific medication side effects and the nocebo phenomenon. Journal of the American Medical Association 287(5):622–627.
Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. 2002. General competencies and accreditation in graduate medical education. Health Affairs 21(5):103–111.
Beckman AGK, Parker MG, Thorslund M. 2005. Can elderly people take their medicine? Patient Education and Counseling 59:186–191.
Bedell SE, Jabbour S, Goldberg R, Glaser H, Gobble S, Young-Xu Y, Graboys TB, Ravid S. 2000. Discrepancies in the use of medications: Their extent and predictors in an outpatient practice. Archives of Internal Medicine 160(14):2129–2134.
Berendt M, Schaefer B, Heglund MJ, Bardin C. 2001. Telehealth for effective disease state management. Home Care Provider 6(2):67–72.
Berger J. 1998. Culture and ethnicity in clinical care. Archives of Internal Medicine 158:2085– 2090.
Berland GK, Elliott MN, Morales LS, Algazy JI, Kravitz RL, Broder MS, Kanouse DE, Munoz JA, Puyol JA, Lara M, Watkins KE, Yang H, McGlynn EA. 2001. Health information on the Internet: Accessibility, quality, and readability in English and Spanish. Journal of the American Medical Association 285(20):2612–2621.
Bernardini C, Ambrogi V, Perioli L, Tiralti MC, Fardella G. 2000. Comprehensibility of the package leaflets of all medicinal products for human use: A questionnaire survey about the use of symbols and pictograms. Pharmacological Research 41(6):679–688.
Berry DL, Wilkie DL, Thomas CR, Fortner P. 2003. Clinicians communicating with patients experiencing cancer pain. Cancer Investigation 21(3):374–381.
Bessell TL, Anderson JN, Silagy CA, Sanson LN, Hiller JE. 2003. Surfing, self-medicating, and safety: Buying nonprescription and complimentary medicines via the Internet. Quality and Safety in Health Care 12:88–92.
Bikowski RM, Ripsin CM, Lorraine VL. 2001. Physician-patient congruence regarding medication regimens. Journal of the American Geriatrics Society 49(10):1353–1357.
Bitten N, Stevensen FA, Barry CA, Barber N, Bradley C. 2000. Misunderstandings in prescribing decisions in general practice: Qualitative study. British Medical Journal 320:484–488.
Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. 1995. Ethnicity and attitudes towards patient autonomy. Journal of the American Medical Association 274:820–825.
Blendon R, DesRochies C, Brodie M, Benson JM, Rosen AB, Schneider E, Altman DE, Zapert K, Herrmann M, Steffenson AE. 2002. Views of practicing physicians and the public on medical errors. New England Journal of Medicine 347(24):1933–1940.
Blumenthal D. 2004. Doctors and drug companies. New England Journal of Medicine 351(18):1885–1890.
Bodenheimer T. 1999. The American health care system: The movement for improved quality in health care. New England Journal of Medicine 340(6):488–492.
Bodenheimer T, Lorig K, Holman H, Gumbach K. 2002. Patient self-management of chronic disease in primary care. Journal of the American Medical Association 288(19):2469– 2475.
Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, Oddone EZ. 2005. Nurse administered telephone intervention for blood pressure control: A patient-centered multifactoral intervention. Patient Education and Counseling 57(1):5–14.
Boyer EW, Shannon M, Hibberd PL. 2001. Web sites with misinformation about illicit drugs. New England Journal of Medicine 345(6):469–471.
Brazeau C. 1999. Disclosing the truth about a medical error. American Family Physician 60:1013–1014.
Brennan TA, Rothman DJ, Blank L, Blumenthal D, Chimonas SC, Cohen JJ, Goldman J, Kassirer JP, Kimball H, Naughton J, Smelser N. 2006. Health industry practices that create conflicts of interest: A policy proposal for academic medical centers. Journal of the American Medical Association 295(4):429–433.
Brooks D, Fancott CA, Falter LB, McFarlane A, Nonoyama ML. 2004. The development of a helpline for chronic obstructive pulmonary disease. Patient Education and Counseling 54:329–336.
Brown SH, Levin R, Lincoln MJ, Kolodner RM, Nelson SJ. 2003. United States Government Progresses Toward a Common Information Infrastructure for Medications. Bethesda, MD: National Library of Medicine.
Caithain AO, Goode J, Luff D, Strangleman T, Hanlon G, Greatbatch D. 2005. Does NHS Direct empower patients? Social Science and Medicine 61:1761–1771.
Calkins DR, Davis RB, Reiley P, Phillips RS, Pinco KLC, Delbance TL, Iezzoni LI. 1997. Patient-physician communication at hospital discharge and patients’ understanding of the postdischarge treatment plan. Archives of Internal Medicine 157:1026–1030.
Caralis PV, Davis B, Wright K, Marcial E. 1993. The influence of ethnicity and race on attitudes toward advance directives, life prolonging treatments, and euthanasia. Journal of Clinical Ethics 4:155–165.
Caress AL, Luker K, Woodcock A, Beaver K. 2002. An exploratory study of priority information needs in adult asthma patients. Patient Education and Counseling 47:319–327.
Carroll L, Sullivan FM, Colledge M. 1998. Good health care: Patient and professional perspectives. British Journal of General Practice 48:1507–1508.
CDC (Centers for Disease Control and Prevention). 2005. Health Marketing and Communication at the New CDC. [Online]. Available http://cdc.confex.com/cdc/nic2006/ techprogram/P11748.HTM [accessed May 8, 2006].
Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, Schwartz S. 2005. Predictors of adherence with antihypertensive and lipid-lowering therapy. Archives of Internal Medicine 165(10):1147–1152.
Christensen MB, Olesen F. 1998. Out of hours service in Denmark: Evaluation five years after reform. British Medical Journal 316:1502–1505.
Cleary PD, Edgman-Levitan S, Walker JD, Gerteis M, Delbanco TL. 1993. Using patient reports to improve medical care: A preliminary report from 10 hospitals. Quality Management in Health Care 2(1):31–38.
CMWF (The Commonwealth Fund). 2005. Commonwealth International Survey on Sicker Adults. New York: CMWF.
Cohen MH, Hrbek A, Davis RB, Schachter SC, Eisenberg DM. 2005. Emerging credentialing practices, malpractice liability policies, and guidelines governing complimentary and alternative medical practices and dietary supplement recommendations: A descriptive study of 19 integrative health care centers in the United States. Archives of Internal Medicine 165(3):289–295.
Cohen MM, Eustis MA, Gribbins RE. 2003. Changing the culture of patient safety: Leadership’s role in health care quality improvement. Joint Commission Journal on Quality and Safety 29(7):329–335.
Cohen MR. 2000. Medication Errors: Causes, Prevention, and Risk Management. Sudbury, MA: Jones and Bartlett Publishers.
Connor M, Ponte PR, Conway J. 2002. Multidisciplinary approaches to reducing error and risk in a patient care setting. Critical Care Nursing Clinics of North America 14(4): 359–367.
Coulter A. 2002. Patients’ views of the good doctor: Doctors have to earn trust. British Medical Journal 325:668–669.
Cramer JA. 1998. Enhancing patient compliance in the elderly: Role of packaging aids and monitoring. Drug Therapy 12(1):7–15.
Crocco AG, Villasis-Keever M, Jadad AR. 2002. Two wrongs don’t make a right: Harm aggravated by inaccurate information on the Internet. Pediatrics 109(3):522–523.
Cummings SR, Palermo L, Browner W, Marcus R, Wallace R, Pearson J, Blackwell T, Eckert S, Black D. 2000. Monitoring osteoporosis therapy with bone densitometry: Misleading changes and regression to the mean. Journal of the American Medical Association 283(10):1318–1321.
Curlin FA, Roach CJ, Gorawara-Bhat R, Lantos JD, Chin MH. 2005. When patients choose faith over medicine: Physician perspectives on religiously related conflicts in the medical encounter. Archives of Internal Medicine 165:88–91.
Curry LC, Walker C, Hogstel MO, Burns P. 2005. Teaching older adults to self-manage medications: Preventing adverse drug reactions. Journal of Gerontological Nursing 31 (4):32–42.
De Leo D, Buono MD, Dwyer J. 2002. Suicide among the elderly: The long-term impact of a telephone support and assessment intervention in northern Italy. British Journal of Psychiatry 181:226–229.
Debusk RF, West JA, Miller NH, Taylor CB. 1999. Chronic disease management: Treating the patient with disease(s) vs treating disease(s) in the patient. Archives of Internal Medicine 159(22):2739–2742.
Degner LF, Kristjanson LJ, Bowman D, Sloan A, Carriere KC, O’Neil J, Bilodeau B, Watson P, Mueller B. 1997. Information needs and decisional preferences in women with breast cancer. Journal of the American Medical Association 277(18):1485–1492.
DHHS (U.S. Department of Health and Human Services). 1996. Action Plan for the Provision of Useful Prescription Medicine Information: Steering Committee for the Collaborative Development of a Long-Range Action Plan for the Provision of Useful Prescription Medicine Information. Washington, DC: DHHS.
DiMatteo MR. 2004. Variations in patients’ adherence to medication recommendations: A qualitative review of 50 years of research. Medical Care 42(3):200–209.
Ditmyer MM, Price JH, Telljohann SK, Rogalski F. 2003. Pediatricians’ perceptions and practices regarding prevention and treatment of Type 2 diabetes mellitus in children and adolescents. Archives of Pediatric and Adolescent Medicine 157(9):913–918.
Doupi P, van der Lei J. 1999. Rx medication information for the public and the WWW: Quality issues. Medical Informatics and the Internet Medicine 24(3):171–179.
Drummond SR, Drummond RS, Dutton GN. 2004. Visual acuity and the ability of the visually impaired to read medication instructions. British Journal of Othamology 88:1541–1542.
Edelberg HK, Shallenberger E, Wei JY. 1999. Medication management capacity in highly functioning community-living older adults: Detection of early deficits. Journal of the American Geriatrics Society 47(5):592–596.
Ende J, Kazis L, Ash A, Moskowitz MA. 1989. Measuring patients’ desire for autonomy: Decision making and information-seeking preferences among medical patients. Journal of General Internal Medicine 4:23–30.
Ernst E. 2001. Informed consent in complimentary and alternative medicine. Archives of Internal Medicine 161:2288–2292.
Eysenbach G, Powell J, Kuss O, Sa ER. 2002. Empirical studies assessing the quality of health information for consumers on the World Wide Web. Journal of the American Medical Association 287(20):2691–2700.
FACCT (Foundation for Accountability). 2001a. Consumers and Quality. What Do They Know? What Do They Want? Results from FACCT Consumer Research 1996–2000. Portland, OR: FAACT and New York: Markle Foundation.
FACCT. 2001b. Development of a Consumer Communications Toolkit: Report and Findings from the Leapfrog Group’s 2001 Focus Groups. Portland, OR: FAACT and New York: Markle Foundation.
FDA (U.S. Food and Drug Administration). 2005. Patient Labeling and Risk Communication. [Online] Available: http://www.fda.gov/cder/Offices/ODS/labeling.htm [accessed January 2, 2006].
Flach SD, McCoy KD, Vaughn TE, Ward MM, Bootsmiller BJ, Doebbeling BN. 2004. Does patient-centered care improve provision of preventive services? Journal of General Internal Medicine 19:1019–1026.
Frampton SB, Gilpin L, Charmel PA. 2003. Putting Patients First: Designing and Practicing Patient-Centered Care. San Francisco, CA: Jossey-Bass.
FSMB (Federation of State Boards of Medicine) and NBME (National Board of Medical Examiners). 2005. United States Medical Licensing Examination. [Online]. Available: http://www.usmle.org [accessed March 23, 2006].
Fusco R, Whiteside J. 2005. Kiosks win patient kudos and speed registration. Healthcare Benchmarks and Quality Improvement 12(2):20–21.
Gallagher TH, Levinson W. 2005. Disclosing harmful medical errors to patients. Archives of Internal Medicine 165:1819–1824.
Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. 2003. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. Journal of the American Medical Association 289(8):1001–1007.
Garfield S, Francis SA, Smith FJ. 2004. Building concordant relationships with patients starting antidepressant medication. Patient Education and Counseling 55:241–246.
Gawande AA, Bates DW. 2000. The Use of Information Technology in Improving Medical Performance: Part III. Patient-Support Tools. [Online]. Available: http://www.medscape. com/viewarticle/408035 [accessed November 7, 2005].
George CF, Rabin KH. 1993. Improving Patient Information and Education on Medicines. Geneva, Switzerland: International Medical Benefit/Risk Foundation-RAD-AR.
Gerteis M, Edgman-Levitan S, Daley J, Delbanco T. 1993. Through the Patient’s Eyes: Understanding and Promoting Patient-Centered Care. San Francisco, CA: Jossey-Bass.
Getz K, Borfitz D. 2002. Informed Consent: A Guide to the Risks and Benefits of Volunteering for Clinical Trials. Boston, MA: Thomson CenterWatch.
Gibson PG, Coughlan J, Wilson AJ, Abramson M, Bauman A, Hensley MJ, Walters EH. 2000. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Systematic Review (2):CD001005.
Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. 2002. Self-management aspects of the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Annals of Behavioral Medicine 24(2): 80–87.
Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. 2004. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. American Journal of Health System Pharmacists 61(16):1689–1695.
Goldschmidt L, Goodrich GL. 2004. Development and evaluation of a point-of-care interactive patient education kiosk. Journal of Telemedicine and Telecare 10(Supplement 1):30–32.
Greatbatch D, Hanlon G, Goode J, Caithain AO, Strangleman T, Luff D. 2005. Telephone triage, expert systems, and clinical expertise. Sociology of Health and Illness 27(6): 802–830.
Griffin SJ, Kinmonth AL, Veltman MWM, Gillard S, Grant J, Stewart M. 2004. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: A systematic review of trials. Annals of Family Medicine 2(6):595–608.
Griffiths KM, Christensen H. 2000. Quality of Web-based information on treatment of depression: Cross sectional survey. British Medical Journal 321(7275):1511–1515.
Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, Cadoret C, Fish LS, Garber L, Kelleher M, Bates DW. 2003. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. Journal of the American Medical Association 289(9):1107–1116.
Gustafsson J, Kalvemark S, Nilsson G, Nilsson JLG. 2003. A method to evaluate patient information leaflets. Drug Information Journal 37:115–125.
Hafferty E. 2005. Clear Rx: Design on Drugs. [Online]. Available: http://www.brand channel.com/print_page.asp?”ar_id=248§ion=profile [accessed December 27, 2005].
Haig K. 2003. One Hospital’s Journey Toward Patient Safety–A Cultural Revolution. Medscape Money and Medicine 4(2). [Online]. Available: http://www.medscape.com/view article/460721 [accessed May 8, 2006].
Hameen-Anttila K, Kemppainen K, Enlund H, Bush PJ, Marja A. 2004. Do pictograms improve children’s understanding of medicine leaflet information? Patient Education and Counseling 55:371–378.
Harmon A. 2005. Young, assured and playing pharmacist to friends. New York Times. p. 16.
Hartigan K. 2003. Patient education: The cornerstone of successful oral chemotherapy treatment. Clinical Journal of Oncology Nursing 7(6):21–24.
Harvard. 2006. When Things Go Wrong: Responding to Adverse Events. A Consensus Statement of the Harvard Hospitals. [Online]. Available: http://macoalition.org/documents/ respondingToAdverseEvents.pdf [accessed April 13, 2006].
Haugbolle LS, Sorensen EW, Henriksen HH. 2002. Medication- and illness-related factual knowledge, perceptions, and behavior in angina pectoris patients. Patient Education and Counseling 47:281–289.
Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. 2002. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self management. Journal of General Internal Medicine 17(4):243–252.
Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. 2003. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? Journal of General Internal Medicine 18:893–902.
HI (Harris Interactive). 2005. Number of Cyberchondriacs: U.S. Adults Who Go Online for Health Information Increases to Estimated 117 Million. [Online]. Available: http:// harrisinteractive.com/news/newsletters/healthnews/HI_HealthCareNews2005Vol5_ Iss08.pdf [accessed November 5, 2005].
Hibbard JH. 2003. Engaging health care consumers to improve the quality of care. Medical Care 41(1):I-61–I-70.
Hibbard JH. 2004. New roles for patients and consumers in assuring high quality care. Virtual Mentor: Ethics Journal of the American Medical Association 6(6). [Online]. Available: http://www.ama-assn.org/ama/pub/category/12500.html [accessed September 26, 2006].
Horvatich PK, Schnoll SH. 1991. Filling the knowledge gap: A continuing medical education course on prescribing drugs with abuse potential. New York State Journal of Medicine 91(11):40S–42S.
Hughes RA, Carr ME, Thwaites CEA. 2002. Review of the function of a telephone helpline in the treatment of outpatients with rheumatoid arthritis. Annals of the Rheumatic Disease 61:341–345.
IHI (Institute for Healthcare Improvement). 2004. Getting Started Kit: Prevent Adverse Drug Events (Medication Reconciliation). How-To-Guide. Boston MA: IHI.
IHI. 2005. Consumer Involvement. [Online]. Available: http://www.ihi.org/IHI/Topics/ HIVAIDS/ConsumerInvolvement.htm [accessed February 8, 2006].
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2003. Priority Areas for National Action Transforming Health Care Quality. Washington, DC: The National Academies Press.
IOM. 2004a. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press.
IOM. 2004b. Insuring America’s Health. Washington, DC: The National Academies Press.
IOM. 2004c. Patient Safety: Achieving a New Standard for Care. Washington, DC: The National Academies Press.
IOM. 2004d. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: The National Academies Press.
IOM. 2004e. Forging a Poison Prevention and Control System. Washington, DC: The National Academies Press.
IOM. 2004f. Ethical Conduct of Clinical Research Involving Children. Washington, DC: The National Academies Press.
IOM. 2005. Complementary and Alternative Medicines in the United States. Washington, DC: The National Academies Press.
IOM. 2006. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: The National Academies Press.
JCAHO (Joint Commission on Accreditation of Healthcare Organizations). 2004. 2005 Joint Commission National Patient Safety Goals. [Online]. Available at: http://www.jcipatient safety.org/show.asp?durki=9344&site=164&return=9335 [accessed May 26, 2005].
JCAHO. 2005. Ethics, Rights, and Responsibilities. 2005 Hospital Accreditation Standards. Chicago, IL: JCAHO.
Jefford M, Kirke B, Grogan S, Yeoman G, Boyes A. 2005. Australia’s cancer helpline: An audit and caller profile. Australian Family Physician 34(5):393–394.
Jenkins L, Britten N, Stevenson F, Barber N, Bradley C. 2003. Developing and using quantitative instruments for measuring doctor-patient communication about drugs. Patient Education and Counseling 50:273–278.
JKF (Josie King Foundation). 2002. Sorrel’s Speech to IHI Conference. [Online]. Available: http://www.josieking.org/speech.html [accessed February 1, 2006].
Johnson MW, Mitch WE, Sherwood J, Lopes L, Schmidt A, Hartley H. 1986. The impact of a drug information sheet on the understanding and attitude of patients about drugs. Journal of the American Medical Association 256(19):2722–2724.
Johnstone MJ. 2000. Informed consent and the betrayal of patient’s rights. Australian Nursing Journal 8(2):1320–1385.
Kaissi A, Johnson T, Kirschbaum MS. 2003. Measuring teamwork and patient safety attitudes of high-risk areas. Nursing Economics 21(5):211–218.
Kamal-Bahl, S, Briesacher B. 2004. How do incentive-based formularies influence drug selection and spending for hypertension? Health Affairs 23(1):227–236.
Kerzman H, Baron-Epel O, Toren O. 2005. What do discharged patients know about their medication? Patient Education and Counseling 56:276–282.
Ketchum K, Grass CA, Padwojski A. 2005. Medication reconciliation: Verifying medication orders and clarifying discrepancies should be standard practice. American Journal of Nursing 105(11):78–79.
KFF (Kaiser Family Foundation). 2004. National Survey on Consumers’ Experiences with Patient Safety and Quality Information. Menlo Park, CA: KFF.
Kizer KW. 1999. Large System Change and a Culture of Safety. Enhancing Patient Safety and Reducing Errors in Health Care. Chicago, IL: National Patient Safety Foundation.
Knowlton CH, Penna RP. 2003. Pharmaceutical Care. 2nd ed. Bethesda, MD: American Society of Health System Pharmacists.
Krass I, Svarstad BL, Bultman D. 2002. Using alternative methodologies for evaluating patient education leaflets. Patient Education and Counseling 47:29–35.
Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH. 2003. Direct observation of requests for clinical services in office practice: What do patients want and do they get it? Archives of Internal Medicine 163(14):1673–1678.
Lamb RM. 2004. Open disclosure: The only approach to medical error. Quality Health Care 13:3–5.
Lamb RM, Studdert DM, Bohmer RMJ, Berwick DM, Brennan TA. 2003. Hospital disclosure practices: Results of a national survey. Health Affairs 22(2):73–83.
Leape LL. 1998. Creating a Culture of Safety. Paper presented at: Enhancing Patient Safety and Reducing Errors in Health Care, Rancho Mirage, CA.
LeSage J. 1991. Polypharmacy in geriatric patients. Nursing Clinics of North America 26(2): 273–290.
Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. 2005. Interventions for Providers to Promote a Patient-Centered Approach in Clinical Consultations (Review). The Cochrane Collaboration.
Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, Gonzalez VM, Laurent DD, Holman HR. 1999. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care 39(1):5–14.
Maguire P, Pitceathly C. 2002. Key communication skills and how to acquire them. British Medical Journal 325:697–700.
Makoul G. Communication skills education in medical school and beyond. 2003. Journal of the American Medical Association 289(1):93.
Manasse HR, Thompson KK. 2005. Medication Safety: A Guide for Health Care Facilities. Bethesda, MD: American Society of Health System Pharmacists.
Manasse HR, Turnbull JE, Diamond LH. 2002. Patient safety: A review of the contemporary American experience. Singapore Medical Journal 43(5):254–262.
Mansell D, Poses RM, Kazis L, Duefield CA. 2000. Clinical factors that influence patients’ desire for participation in decisions about illness. Archives of Internal Medicine 160:2991–2996.
Manser T, Staender S. 2005. Aftermath of an adverse event: Supporting health care professionals to meet patient expectations through open disclosure. Acta Anaesthesiologica Scandinavica 49:728–734.
Markle Foundation. 2003. The Personal Health Working Group: Final Report. Connecting for Health: A Public-Private Collaborative. New York: Markle Foundation.
Markle Foundation. 2005. Connecting Americans to Their Health Care: Empowered Consumers, Personal Health Records, and Emerging Technologies. New York: Markle Foundation.
Mazor KM, Simon SR, Gurwitz JH. 2004a. Communicating with patients about medical errors. Archives of Internal Medicine 164:1690–1697.
Mazor KM, Simon SR, Yood RA, Martinson BC, Gunter MJ, Reed, GW, Gurwitz JH. 2004b. Health plan members’ views about disclosure of medical errors. Annals of Internal Medicine 140(6):409–418.
McCullagh E, Brigstocke G, Donaldson N, Kalra L. 2005. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke 36(10):2181–2186.
McDonnell PJ, Jacobs MR. 2002. Hospital admissions resulting from preventable adverse drug reactions. Annals of Pharmacotherapy 36(9):1331–1336.
Mead N, Bower P. 2000. Patient-centeredness: A conceptual framework and review of empirical literature. Social Science and Medicine 51(7):1087–1110.
Mechanic D, Meyer S. 2000. Concepts of trust among patients with serious illness. Social Science and Medicine 51:657–658.
Meryn S. 1998. Improving doctor-patient communication. British Medical Journal 316:1922– 1930.
Michalsen A, Konig G, Thimme W. 1998. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart 80:437–441.
Millenson M. 2003. The silence. Health Affairs 22(3):103–112.
Molassiotis A. 2004. Quality and safety issues of web-based information about herbal medicines in the treatment of cancer. Complementary Therapies in Medicine 12(4):217–227.
Morgan M. 1995. The significance of ethnicity for health promotion: Patients’ use of antihypertensive drugs in inner London. International Journal of Epidemiology 24:S79–S84.
Morrow DG, Leirer V, Sheikh J. 1988. Adherence and medication instructions: Review and recommendations. Journal of the American Geriatrics Society 36:1147–1160.
Morrow DG, Weiner M, Young J, Steinley D, Deer M, Murray MD. 2005. Improving medication knowledge among older adults with heart failure: A patient-centered approach to instruction design. The Gerontologist 45(4):545–552.
Mullan F. 1998. Eugene McGregor, MD: A legacy of general practice. Journal of the American Medical Association 279(14):1117–1120.
Murray MD, Kroenke K. 2001. Polypharmacy and medication adherence: Small steps on a long road. Journal of General Internal Medicine 16(2):137–139.
Murray RF. 1992. Minority perspectives on biomedical ethics. In: Pellegrino E, Mazzarella P, Corsi P, eds. Transcultural Dimensions in Medical Ethics. Frederick, MD: University Publishing Group.
NARA (National Archives and Records Administration). 1999. Title 21–Food and Drugs: Chapter I–Food and Drug Administration, Department of Health And Human Services. Part 208–Medication Guides for Prescription Drug Products (Effective 6-1-99). [Online]. Available: http://www.access.gpo.gov/nara/cfr/waisidx_99/21cfr208_99.html. Notes: 21 CFR 208 [accessed March 23, 2006].
NCCAM (National Center for Complimentary and Alternative Medicine). 2004. The Use of Complementary and Alternative Medicine in the United States. [Online]. Available: http:// nccam.nih.gov/news/camsurvey_fs1.htm#use [accessed February 6, 2006].
NCHS (National Center for Health Statistics). 1995. National Health Interview Survey on Disability. [Online]. Available: http://www.cdc.gov/nchs/about/major/nhis_dis/nhis_dis. htm [accessed November 15, 2005].
NCHS. 2005. Health, United States, 2005. Hyattsville, MD: NCHS.
Nickerson A, MacKinnon NJ, Roberts N, Saulnier L. 2005. Drug-therapy problems, inconsistencies, and omissions identified during a medication reconciliation and seamless care service. Healthcare Quarterly 8:65–72.
NIMH (National Institute of Mental Health). 2000. Cognitive Research. Bethesda, MD: NIMH.
NPSF (National Patient Safety Foundation). 1997. National Patient Safety Foundation at the AMA. North Adams, MA: NPSF.
NPSF. 2000. National Agenda for Action: Patients and Families in Patient Safety. Chicago, IL: NPSF.
NQF (National Quality Forum). 2005. Improving Use of Prescription Medications: A National Action Plan. Wu HW, Nishimi RY, Kizer KW, eds. Washington, DC: NQF.
O’Leary DS. 1998. Organization, Evaluation, and a Culture of Safety. Paper presented at: Enhancing Patient Safety and Reducing Errors in Health Care, Rancho Mirage, CA.
Oakley A. 2005. Focus on: Information technology. Online drug information for dermatology patients. Journal of Drugs and Dermatology 4(1):108–113.
Osman LM. 1997. How do patients’ views about medication affect their self management in asthma? Patient Education and Counseling 32:S43–S49.
Pachter LM, Cloutier MM, Bernstein BA. 1995. Ethnomedical (folk) remedies for childhood asthma in a mainland Puerto Rican community. Archives of Pediatric and Adolescent Medicine 149:982–988.
PCSEPMBBR (President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research). 1982. Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. New York: U.S. Government Printing Office.
PDR (Physicians’ Desk Reference). 2000. Physicians’ Desk Reference. Montvale, NJ: Medical Economics Co.
PDR. 2005. Physicians’ Desk Reference, edition 2006. Montvale, NJ: Thomson PDR.
Pereles I, Russell ML. 1996. Needs for CME in geriatrics. Part 2: Physician priorities and perceptions of community representatives. Canadian Family Physician 42:632–640.
Peterson G, Aslani P, Williams KA. 2003. How do consumers search for and appraise information on medicines on the Internet? A qualitative study using focus groups. Journal of Medical Internet Research 5(4):e33.
Peterson JF, Kuperman GJ, Shek C, Patel M, Avorn J, Bates DW. 2005. Guided prescription of psychotropic medications for geriatric inpatients. Archives of Internal Medicine 165(7):802–807.
Piette JD, Heisler M, Horne R, Alexander GC. 2006. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Social Science and Medicine 62(4):846–857.
Poole SR, Schmitt BD, Carruth T, Peterson-Smith A, Slusarski M. 1993. After-hours telephone coverage: The application of an area-wide telephone triage and advice system for pediatric practices. Pediatrics 92:670–679.
Pronovost P, Weast B, Schwarz M, Wyskiel RM, Prow D, Milanovich SN, Berenholtz S, Dorman T, Lipsett P. 2003. Medication reconciliation: A practical tool to reduce the risk of medication errors. Journal of Critical Care 18(4):201–205.
Prutting SM, Cerveny JD, MacFarlane LI, Wiley MK. 1998. An interdisciplinary effort to help patients with limited prescription drug benefits afford their medication. Prescription Drug Assistance 91(9):815–820.
PSI (Premier Safety Institute). 2004. Survey on Disclosure Practices. Oak Brook, IL: PSI.
Ratzan SC, Parker RM. 2000. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker RM, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. NLM Pub. No. CBM2000-1. Bethesda, MD: National Institute of Health, U.S. Department of Health and Human Services.
Raynor DK, Savage I, Knapp P, Henley J. 2004. We are the experts: People with asthma talk about their medicine information needs. Patient Education and Counseling 53:167–174.
Reigel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. 2002. Effect of standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Archives of Internal Medicine 162:705–712.
Reiling JG, Knutzen BL, Wallen TK, McCullough S, Miller R, Chernos S. 2004. Enhancing the traditional hospital design process: A focus on patient safety. Joint Commission Journal on Quality and Safety 30(5):233.
Reiser S. 1980. Words as scalpels: Transmitting evidence in the clinical dialogue. Annals of Internal Medicine 92:837–842.
Richards T. 1990. Chasms in communication. British Medical Journal 301:1407–1408.
Ridley DT. 2001. Informed consent, informed refusal, informed choice: What is it that makes a patient’s medical treatment decisions informed? Medical Law 20(2):205–214.
Risk A, Petersen C. 2002. Health information on the Internet: Quality issues and international initiatives. Journal of the American Medical Association 287(20):2713–2715.
RMPDC (Rocky Mountain Poison and Drug Center). 2006. Organization History. [Online]. Available: http://www.rmpdc.org/history/index.cfm [accessed March 21, 2006].
Robb N. 1996. Telecare acting as an “electronic grandmother” for New Brunswickers. Canadian Medical Association Journal 154(6):903–904.
Rodehaver C. 2005. Medication reconciliation in acute care: Ensuring an accurate drug regimen on admission and discharge. Joint Commission Journal on Quality and Patient Safety 31(7):406–413.
Rogers G, Alper E, Brunelle D, Federico F, Fenn CA, Leape LL, Kirle L, Ridley N, Clarridge BR, Bolcic-Jankovic D, Griswold P, Hanna D, Annas CL. 2006. Reconciling medications at admission: Safe practice recommendations and implementation strategies. Joint Commission Journal on Quality and Patient Safety 32(1):37–50.
Rolland PD. 2000. Reading level of drug information printouts: A barrier to effective communication of patient medication information. Drug Information Journal 34:1329–1338.
Rozich JD, Resar RK. 2001. Medication safety: One organization’s approach to the challenge. Journal of Clinical Outcomes Management 8:27–34.
Rozich JD, Howard RJ, Justeson JM, Macken PD, Lindsay ME, Resar RK. 2004. Standardization as a mechanism to improve safety in health care: Impact of sliding scale insulin protocol and reconciliation of medications initiatives. Joint Commission Journal on Quality and Safety 30(1):5–14.
Rudd RE, Colton T, Schact R. 2000. An Overview of Medical and Public Health Literature Addressing Literacy Issues: An Annotated Bibliography. Report #14. Cambridge, MA: National Center for the Study of Adult Learning and Literacy.
RWJF (Robert Wood Johnson Foundation). 2000. Patient Education and Consumer Activation in Chronic Disease. Princeton, NJ: RWJF.
Safeer RS, Keenan J. 2005. Health literacy: The gap between physicians and patients. American Family Physician 72(3).
Safran DG. 2003. Defining the future of primary care: What can we learn from patients? Annals of Internal Medicine 138(3):248–255.
Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. 1998. Linking primary care performance to outcomes of care. Journal of Family Practice 47(3):213–220.
Safran DG, Neuman P, Schoen C, Kitchman MS, Wilson IB, Cooper B, Li A, Chang H, Rogers WH. 2005. Prescription drug coverage and seniors: Findings from a 2003 National Survey. Health Affairs (Millwood) W5-152–W5-166.
Sawicki PT. 1999. A structured teaching and self-management program for patients receiving oral anticoagulation: A randomized controlled trial. Journal of the American Medical Association 281(2):145–150.
Schlenk EA, Dunbar-Jacob J, Engberg S. 2004. Medication nonadherence among older adults: A review of strategies and interventions for improvement. Journal of Gerontologic Nursing 30(7):33–43.
Schneitman-McIntire O, Farnen TA, Gordon N, Chan J, Toy WA. 1996. Medication misadventures resulting in emergency department visits at an HMO medical center. American Journal of Health-System Pharmacy 53(12):1416–1422.
Schommer JC, Mott DA, Hansen RA, Cline RR. 2003. Selected characteristics of senior citizens prescription drug payment and procurement in 1998 and 2001. Journal of Managed Care Pharmacy 9(5):453–456.
Schrag A, Hovis A, Morley D, Quinn N, Jahanshahi M. 2005. Caregiver burden in Parkinson’s disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism and Related Disorders 12(1):35–41.
Schroeder SA, Showstack JA, Gerbert B. 1986. Residency training in internal medicine: Time for a change? Annals of Internal Medicine 104(4):554–561.
Schuerenberg BK. 2005. Kiosks serve up e-Rx convenience. Health Data Management 13(11): 56, 58.
Schultz PE, Perrier CV. 1976. Inadequacy of information about drugs. International Journal of Clinical Pharmacology 14(4):255–258.
Scott JT, Thompson DR. 2003. Assessing the information needs of post-myocardial infarction patients: A systemic review. Patient Education and Counseling 50:167–177.
Silberg WM, Lundberg GD, Musacchio RA. 1997. Assessing, controlling, and assuring the quality of medical information on the Internet. Journal of the American Medical Association 277(15):1244–1245.
Skoglund P, Isacson D, Kjellgren KI. 2003. Analgesic medication: Communication at pharmacies. Patient Education and Counseling 51:155–161.
Sleath B, Roter D, Chewning B, Svarstad B. 1999. Asking questions about medication: Analysis of physician-patient interactions and physician perceptions. Medical Care 37(11): 1169–1173.
Smith R, Hiatt H, Berwick D. 1999. Shared ethical principles for everyone in healthcare: A working draft from the Tavistock Group. British Medical Journal 318(7178):248–251.
Sol BG, van der Graaf Y, van der Bijl JJ, Goessens NB, Visseren FL. 2006. Self-efficacy in patients with clinical manifestations of vascular diseases. Patient Education and Counseling 61(3):443–448.
Stewart M. 1995. Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal 152(9):1423–1433.
Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR. 1995. Patient-Centered Medicine: Transforming the Clinical Method. Thousand Oaks, CA: Sage.
Stiggelbout AM, Kiebert GM. 1997. A role for the sick role. Patient preferences regarding information and participation in clinical decision-making. Canadian Medical Association Journal 157(4):383–389.
Sundin K, Jansson L. 2003. Understanding and being understood as a creative caring phenomenon in care of patients with stroke and aphasia. Journal of Clinical Nursing 12: 107–116.
Svarstad BL, Mount JK. 2001. Evaluation of Written Prescription Information Provided in Community Pharmacies. Rockville, MD: FDA.
Svarstad BL, Chewning BA, Sleath BL, Claesson C. 1999. The brief medication questionnaire: A tool for screening patient adherence and barriers to adherence. Patient Education and Counseling 37(2):113–124.
SWC (Sorry Works Coalition). 2005. Homepage: Sorry Works Coalition. [Online]. Available: http://www.sorryworks.net [accessed March 22, 2006].
Sweet MP, Bernat JL. 1997. A study of the ethical duty of physicians to disclose errors. Journal of Clinical Ethics 8:341–348.
Tamada JA, Garg S, Jovanovic L, Pitzer KR, Fermi S, Potts RO. 1999. Noninvasive glucose monitoring: Comprehensive clinical results. Journal of the American Medical Association 282(19):1839–1844.
Teutsch C. 2003. Patient-doctor communication. The Medical Clinics of North America 87(5):1115–1145.
TGA (Therapeutic Goods Administration). 2002. Review of the Labelling Requirements for Medicines: Consumer-Focused Labelling—A Way Forward? Australia: Commonwealth Department of Health and Ageing.
Trude S. 2003. So Much to Do, So Little Time: Physician Capacity Constraints 1997-2001. Tracking Report: Results from the Community Tracking Study. Washington, DC: Center for Studying Health System Change.
Turner VF, Bentley PJ, Hodgson SA, Collard PJ, Drimitis R, Rabune C, Wilson AJ. 2002. Telephone triage in Western Australia. Medical Journal of Australia 176:100–103.
USP (U.S. Pharmacopeia). 1999. Optimizing Patient Comprehension Through Medicine Information Leaflets. Rockville, MD: USP.
Vanderwerker LC, Laff RE, Kadan-Lottick NS, McColl S, Prigerson HG. 2005. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. Journal of Clinical Oncology 23(28):6899–6907.
VHA (Veterans Health Administration). 2005. Disclosure of Adverse Events to Patients. VHA Directive 2005-049. Washington, DC: VHA.
Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. 1997. Collaborative management of chronic illness. Annals of Internal Medicine 127(12):1097–1102.
Waegemann CP. 2002. The vision of electronic health records. Journal of Medical Practice Management 18(2):63–65.
Wensing M, Jung HP, Mainz J, Olesen F, Grol R. 1998. A systematic review of the literature on patient priorities for general practice care. Part 1: Description of the research domain. Social Science and Medicine 47:1573–1588.
Wilson IB, Ding L, Hays RD, Shapiro MF, Bozette SA, Cleary PD. 2002. HIV patients’ experiences with inpatient and outpatient care. Medical Care 40(12):1149–1160.
Wogalter MS, Vigilante WJ. 2003. Effects of label format on knowledge acquisition and perceived readability by younger and older adults. Ergonomics 46(4):327–344.
Wolpert HA, Anderson BJ. 2001. Management of diabetes: Are doctors framing the benefits from the wrong perspective? British Medical Journal 323(7319):994–996.
Woolsey RL. 2000. Drug labeling revisions—Guaranteed to fail? Journal of the American Medical Association 284(23):3047–3049.
Wu AW. 2005. Removing Insult from Injury—Disclosing Adverse Events. [Online]. Available: http://www.sorryworks.net/article28.phtml [accessed March 22, 2006].
Wu AW, Cavanaugh TA, McPhee SJ, Lo B, Micco GP. 1997. To tell the truth: Ethical and practical issues in disclosing medical mistakes to patients. Journal of General Internal Medicine 12:770–775.
Zaldivar A, Smolowitz J. 1994. Perceptions of the importance placed on religion and fold remedies by nonMexican American Hispanic adults with diabetes. Diabetes Educator 20:303–306.






































































