5
Advancing System Infrastructure
Emergency medical services (EMS) personnel rely on many different types of equipment to provide timely and effective treatment to patients requiring emergency care. This equipment ranges from basic transport vehicles, such as ambulances and helicopters; to medical devices, such as defibrillators and heart monitors; to communications equipment that allows for transmission of patient information between ambulance and hospital or among first responders in the case of a significant disaster event. In addition, patients rely on effective communications systems that enable them to summon help when needed and ensure that care is on the way.
Over time, technological advances have led to improvements in the delivery of EMS. Automatic crash notification (ACN) technology enables immediate notification of emergency responders when a car crash has occurred. Devices provide instant, audible warnings to ambulance drivers if their driving becomes unsafe. And systems are under development that may eventually allow prehospital EMS personnel in the field to view complete patient health records and potentially replace paper-based ambulance “run records” with electronic data submissions.
Set against this backdrop of evolving technology, however, is the basic reality that most EMS systems do not have the resources needed to make major system upgrades. A significant percentage of the communications equipment currently in use by ambulances was purchased in the 1970s with federal financial assistance. Revamping EMS voice and data communications capabilities, including the infrastructure required to support an electronic health record (EHR) system, would almost certainly require a significant investment on the part of the federal government. Moreover,
not all local EMS providers agree that newer, more sophisticated technology necessarily translates into better or more efficient patient care. The end result is that the infrastructure supporting EMS personnel across the country is highly variable and uneven. In many areas there is a growing gap between the type of equipment now available and that which is actually in use. This chapter details key areas in which technology can play a role in supporting effective EMS response: emergency notification and dispatch, equipment for emergency response, and communications and data systems.
EMERGENCY NOTIFICATION AND DISPATCH
The development and implementation of a single nationwide number to call in emergency situations was a major advance for the U.S. emergency and trauma care system. Before 9-1-1 was fully adopted, states and localities had in place a vast array of 7-digit telephone numbers for citizens to call in the case of an emergency. In the early 1970s, for example, Nebraska had 184 different ambulance service phone numbers in use in various parts of the state (NAS and NRC, 1978; IOM, 1993). Designating a simple 3-digit, standardized number to call in emergencies helped avoid the confusion and delays that inevitably occurred with having so many different numbers for so many different types of emergencies in various parts of the country.
One of the early catalysts for the development of the 9-1-1 system in the United States occurred in 1957 when the National Association of Fire Chiefs recommended the use of a single number for reporting fires. In addition, the 1966 report Accidental Death and Disability contained a recommendation that there be “active exploration of the feasibility of designating a single nationwide telephone number to summon an ambulance” (NAS and NRC, 1966).
In 1967, a presidential commission recommended that a uniform number be used to reach emergency response agencies. The following year, AT&T announced that it would establish 9-1-1 as the emergency code throughout the United States. The first 9-1-1 call was placed in February 1968 (NENA, 2004). In 1973, the Department of Transportation recommended that the universal emergency number be 9-1-1 and provided model legislation for states to use in implementing this system (DOT Wireless E9-1-1 Steering Council, 2002). Implementation of the 9-1-1 system occurred very unevenly across the country, however. By 1992, a number of states, including California and Connecticut, had 100 percent of their populations covered by a 9-1-1 system. In that same year, however, other states had less than 50 percent access, while some, including Maine and Vermont, had only 25 percent coverage (IOM, 1993). Such disparities in the management of 9-1-1 systems nationwide persist today.
To improve federal coordination and communication on 9-1-1 activities,
the ENHANCE 9-1-1 Act was enacted in 2004. The act established a national 9-1-1 Implementation Coordination Office. In addition to improving federal coordination, this office will develop and disseminate information concerning practices, procedures, and technology used in the implementation of 9-1-1 services and will also administer a grant program to enable 9-1-1 call centers to upgrade their equipment. The National 9-1-1 Office is housed within the National Highway Traffic Safety Administration’s (NHTSA) Office of EMS, which will partner with the National Telecommunications and Information Administration, located within the Department of Commerce (NHTSA Office of EMS, 2006).
The Current 9-1-1 System
Americans place an estimated 200 million 9-1-1 calls each year (NENA, 2004). An estimated 85 percent of those calls are directed to the police, while the remaining 15 percent are divided between fire departments and EMS (NENA, 2001). In recent years, the number of EMS calls relative to fire department calls has been increasing. According to the National Fire Protection Association, 80 percent of fire service calls are EMS-related (National Fire Protection Association, 2005).
The 9-1-1 system is locally based and operated, and its structure varies widely across the country. Today there are over 6,000 public safety answering points (PSAPs), or 9-1-1 call centers, nationwide. Various approaches are used to fund these local 9-1-1 systems, including state or local taxes and state or local telephone subscriber fees. Implementation has generally been managed by individual counties or other local governmental units that try to coordinate public resources and work with public safety agencies and telephone companies to help finance and operate the system (IOM, 1993).
While basic 9-1-1 service enables callers to contact an emergency dispatcher, newer, enhanced 9-1-1 (E9-1-1) has the added feature of enabling the dispatcher to identify the telephone number and location of callers using fixed telephone lines (see Table 5-1). This is accomplished through automatic number identification and automatic location identification technologies. These features allow dispatchers to obtain a call-back number in case the call is cut off, as well as immediate access to the caller’s location, which speeds ambulance dispatch. Currently, 93 percent of counties that have basic 9-1-1 have E9-1-1; however, there remain 350 counties without automatic location information and access to a call-back number (NENA, 2004).
Impact of Wireless Technology
An estimated one-third of 9-1-1 calls are now made on cell phones (GAO, 2003), and in some jurisdictions that figure is as high as 50 percent
TABLE 5-1 Types of 9-1-1 Call Capacity
|
Basic 9-1-1 |
Enhanced 9-1-1 |
Wireless Phase I |
Wireless Phase II |
Next-Generation 9-1-1 |
|
9-1-1 is dialed, and a public safety answering point (PSAP) dispatcher answers the call. |
A 9-1-1 call is selectively routed to the proper PSAP. The PSAP has access to the caller’s phone number and address. |
The 9-1-1 call taker automatically receives the wireless phone number and the location of the cell tower handling the call, but not the exact location of the caller. |
The 9-1-1 call taker receives both the caller’s wireless phone number and present location. |
Dispatch will be able to receive voice, text, or video transmissions and will have advanced data capabilities. |
|
SOURCE: NENA, 2004. |
||||
(DOT Wireless E9-1-1 Steering Council, 2002). The movement toward wireless technology has had a significant impact on 9-1-1 systems because the location of the wireless caller cannot be identified as easily as with a landline phone. This can be medically dangerous because in many emergency situations, callers are incapacitated or unable to speak, or they are unaware of their exact location. The inability to pinpoint the caller’s location has resulted in a number of widely reported incidents in which victims have died because rescue workers were not able to arrive in time, even though considerable resources were mobilized to find the caller (DOT Wireless E9-1-1 Steering Council, 2002).
Efforts are under way to ensure that the location of emergency callers can be automatically identified, even if they are using a wireless cell phone. Currently, this capability involves either locating the caller using triangulation of the signal among cell towers or locating the caller by Global Positioning System (GPS) satellite technology. The transition of the telecommunications industry to an E9-1-1 system that is able to detect the location of cellular calls is being directed by the Federal Communications Commission (FCC) and is occurring in two phases. Phase I requires carriers, upon the request of the PSAP, to provide technology that allows the call taker to receive the caller’s wireless phone number automatically. This is important in the event that the wireless phone call is dropped, and may allow PSAP employees to work with the wireless company to identify the wireless subscriber. Phase I also delivers the location of the cell tower handling the call. The call is routed to a PSAP based on cell site/sector information. Phase II requires wireless carriers to provide more precise location information in
addition to the caller’s wireless phone number (DOT Wireless E9-1-1 Steering Council, 2002).
Wireless E9-1-1 capacity is currently being developed nationwide, although its uptake has been sporadic. In 1996, the FCC adopted rules requiring wireless carriers to provide E9-1-1 service. For wireless E9-1-1 to work, however, three parties—the wireless carriers, the PSAPs, and the local exchange carriers (which are the local wireline carriers)—must interconnect and install the equipment necessary to locate wireless callers. These collaborations have been lacking in some areas of the country.
Moreover, the cost of building the required infrastructure is substantial. In 2003, the U.S. Government Accounting Office (GAO; now the Government Accountability Office) estimated the cost of implementation to be at least $8 billion over 5 years. No federal funding has been provided to states or localities to make those upgrades. Wireless carriers have raised funds by charging customers $0.05 to $1.50 more per month for 9-1-1 service, although GAO has reported that states or localities have often appropriated these funds for other purposes, slowing rates of uptake in those jurisdictions (GAO, 2003).
In addition to financial concerns and the difficulties of establishing collaboration among various participants, there is a regulatory vacuum at the federal level. The FCC can regulate carriers, but it has no authority to regulate the PSAPs, which are under state and local jurisdiction. Thus, for example, as of 2005 carriers are required to provide location information for all wireless 9-1-1 calls, but this requirement is contingent on whether the local PSAP is equipped to receive and use that information (Medical Subcommittee of the ITS America Public Safety Advisory Group, 2002). Consequently, the FCC does not have the ability to establish an ultimate nationwide deadline for full implementation of wireless E9-1-1 services (GAO, 2003). Implementation will take place in a piecemeal fashion based on the timeframes established by local entities.
Despite these concerns, however, uptake of wireless E9-1-1 has been proceeding at a fairly rapid pace. Table 5-2 illustrates the gap in wireless E9-1-1 that persists, as well as the degree to which Phase II wireless E9-1-1
TABLE 5-2 Progress Toward Universal Wireless Enhanced 9-1-1 (February 2006)
|
|
Phase I |
Phase II |
|
U.S. Population |
85 percent |
71 percent |
|
Public Safety Access Points (PSAPs) |
80 percent |
59 percent |
|
Counties |
71 percent |
45 percent |
|
SOURCE: NENA, 2006. |
||
continues to trail Phase I implementation. Yet the figures also represent a significant increase in the coverage now available as compared with 2 to 3 years ago.
As of October 2003, only 18 percent of PSAPs were receiving Phase II information, compared with 59 percent in 2006. In addition, only 65 percent of PSAPs were receiving Phase I information, as compared with 80 percent in 2006 (GAO, 2003; NENA, 2006). A Department of Transportation survey released in 2003 showed that only 33 of the nation’s 3,136 local jurisdictions had wireless call location capability in December 2002, whereas 643 local jurisdictions had that capability in May 2003 (DOT Wireless E9-1-1 Steering Council, 2002). These figures demonstrate substantial growth in wireless E9-1-1 capacity over the past few years.
The committee supports the nationwide adoption of E9-1-1 and wireless E9-1-1. To ensure more rapid adoption, the committee believes that the charges for wireless E9-1-1 services should be bundled with the overall wireless plan rate, rather than allowing 9-1-1 to be listed as a separate option that raises the monthly fee.
Voice over Internet Protocol (VoIP)
Americans are increasingly moving to alternative communications services, and this presents challenges for the 9-1-1 system. VoIP allows customers to make telephone calls using a computer network and the Internet. VoIP converts the voice signal from the telephone into a digital signal that travels over the Internet, then converts it back at the other end so that customers can speak to anyone with a regular phone number. With regard to emergency notification, however, this new type of communications service has limitations similar to those of wireless calls.
In May 2005, the FCC released VoIP E9-1-1 rules. These rules require VoIP providers to (1) deliver all 9-1-1 calls to the customer’s local emergency operator, (2) give emergency operators the call-back number and location of their customers if the emergency operator is capable of receiving that information, and (3) inform their customers of their E9-1-1 capabilities and the limitations of the service. The FCC gave VoIP providers 120 days to furnish this information to customers and to receive acknowledgment from customers that they had received the information. The FCC informed VoIP carriers that they would have to disconnect from service those customers who had not provided this acknowledgment (FCC, 2006).
Next-Generation 9-1-1
The 9-1-1 system currently in place was not designed to handle the challenges of multimedia communications in a wireless, mobile society. As
TABLE 5-3 Next-Generation 9-1-1
|
Today’s 9-1-1 |
Future 9-1-1 |
|
Primarily voice calls via telephone |
Voice, text, or video from many types of communications devices |
|
Minimal data |
Advanced data capabilities |
|
Local access, transfer, and backup |
Long-distance access, transfer, and backup |
|
Limited emergency notification |
Location-specific emergency alerts possible for any networked device |
|
SOURCE: DOT Intelligent Transportation Systems, 2006. |
|
noted, it is based on 1970s technology and focused on wireline phones. To address this gap, the Department of Transportation is now sponsoring an initiative that would adapt the basic 9-1-1 infrastructure to 21st-century communications technology. The next-generation 9-1-1 initiative, funded by Intelligent Transportation Systems (ITS) and managed by NHTSA’s Office of EMS, will establish a 9-1-1 system that is compatible with any communications device and serve as the foundation for public emergency services in a wireless environment (see Table 5-3).
NHTSA’s Office of EMS is managing a research initiative that will produce a high-level system architecture and deployment plan for the next-generation 9-1-1 system. The goal of the initiative is to establish the infrastructure for transmission of voice, data, and photographs from different types of communications devices to PSAPs and then to emergency responder networks (NHTSA Office of EMS, 2006).
Automatic Crash Notification
Each year, approximately 5 million Americans are injured in 17 million crashes involving 28 million vehicles (Champion et al., 1999). Of those 28 million vehicle crashes, approximately 250,000 result in serious injuries to passengers and/or drivers. For vehicle occupants who sustain serious injuries in vehicle crashes, the time that elapses between the moment of the crash and the moment medical care arrives is crucial. Over the last decade, ACN has emerged as a new technology that can reduce the time between a crash and initial notification of the local PSAP, thereby reducing likely fatalities. NHTSA has estimated that ACN systems may result in up to a 20 percent reduction in fatalities due to vehicle crashes (Bachman and Preziotti, 2001).
The broad availability of cell phones has helped reduce the time it takes for 9-1-1 to be notified of a vehicle crash. However, many crashes occur at times and in places where there are no witnesses to call 9-1-1. In addition, victims of crashes often do not have cell phones available, or they may be
incapacitated and unable to place a 9-1-1 call. ACN technology allows notification of a crash to be sent automatically to ACN call centers, which then notify 9-1-1 dispatchers. This eliminates the need for bystanders or victims themselves to provide notification to the emergency call center.
In 1996, General Motors (GM) introduced ACN technology in a selected number of vehicles through its OnStar program. By 2005, OnStar was available for more than 50 GM models, as well as other vehicle makes such as Saturn and Saab. In addition, ACN programs that use other telematics service providers are available from other car manufacturers, such as Acura, BMW, and Mercedes.
This first-generation ACN technology was able to notify 9-1-1 of the location of a vehicle in which an airbag had been deployed. However, first-generation ACN units were not able to indicate the severity of the accident recorded. GM recently introduced a second-generation technology called advanced ACN (AACN). This more advanced version is able to capture additional information, including speed at impact, occupants’ seatbelt status, direction of impact, and whether the vehicle rolled over. This information provides much more detail regarding the severity of the crash and the likely condition of the vehicle occupants. However, the condition of the occupants may still be uncertain (for example, if seatbelts were secured and airbags deployed, but the crash occurred at a fairly high speed).
In recent years, NHTSA has funded the development of URGENCY Decision Assist software, which is able to translate the data collected in the car’s event data recorder into information that may be able to improve the triage of crash victims. URGENCY estimates the probability of fatality due to a vehicle crash using telemetric data in a predictive model. In the future, these data may allow dispatch operators to make more informed decisions about deployment of resources and may enhance the EMS provider’s ability to make effective triage decisions.
Currently, ACN calls go through a call center, where operators assess the situation and contact emergency personnel if necessary. However, the verbal exchange between the telematics call center and the 9-1-1 call taker is time-consuming and can be prone to information gaps and errors. New technology (recently tested in Minnesota) addresses this issue by allowing electronic data to be transferred directly to PSAPs and then on to EMS responders and emergency department (ED) personnel—providing them with a better picture of the type of incident and possible injuries.
URGENCY software is in the public domain; however, its uptake has been slow, in part because PSAPs would need the technology to receive data transmission, a capability many PSAPS currently lack. In addition, there is no definitive research demonstrating which data elements have clinical utility. Telematics services appear to be moving toward furnishing automatic, instantaneous notification of emergency events to multiple emergency care
providers, including EMS ground and air medical services, heavy rescue services, trauma centers, and others. The committee believes evaluations should be conducted to determine whether emergency dispatchers should transmit that information selectively to local emergency providers to enable more efficient allocation of regional assets, or crash scene data should be integrated directly into EMS and hospital ED data systems.
Nonemergency Calls
The 9-1-1 emergency number is familiar to most Americans and is recognized as being highly responsive (NENA, 2001). Because the number is so widely recognized and remembered, however, it is often used in situations that are not true emergencies, such as property crimes no longer in progress, minor vehicle crashes resulting in no injuries, and some situations involving animal control. Use of the 9-1-1 system for questions or concerns that are nonemergent in nature may produce delays in the response provided for true emergencies, which can place victims in danger.
Because of increasing reports of inappropriate 9-1-1 use, some communities have established alternative phone lines for citizens with non-emergency concerns. In some cases, the phone lines devoted to less urgent calls are regular 7-digit telephone numbers. However, these numbers are more difficult for citizens to remember or to access easily. As a result, some communities have established 3-digit numbers—often 3-1-1—that can be used in nonemergency situations. Operators receiving such calls are able to make triage decisions and if necessary refer a call to a 9-1-1 call center; they can also refer calls to other appropriate government agencies. The hope is that this system will improve the processing of both emergency and nonemergency calls.
Because callers cannot always discern which number is most appropriate to call, 9-1-1 call takers and EMS dispatchers may need to exercise the option of transferring callers to a 3-1-1 system, a nonemergency transport service, or a local nurse advice line if they determine that the caller’s problem does not require immediate EMS attention. This strategy may help keep the 9-1-1 system open and preserve ambulance capacity for serious or life-threatening calls. However, evaluations are needed to assess the feasibility, impact, and risks of this approach.
EQUIPMENT FOR EMERGENCY RESPONSE
Once a PSAP has been notified that help is needed, the dispatcher can summon an array of equipment and personnel to respond: a fire or rescue vehicle bringing first responders (Key et al., 2003), an ambulance carrying EMTs or paramedics, or an air ambulance bringing additional EMS per-
TABLE 5-4 Fire Department Responses (2003)
|
Type of Response |
Number |
Percent Change from 2002 |
|
Fire |
1,584,500 |
–6.1 |
|
Medical Aid |
13,631,500 |
+5.6 |
|
False Alarm |
2,189,500 |
+3.5 |
|
Mutual Aid/Assistance |
987,000 |
+11.1 |
|
Hazardous Material (hazmat) |
349,500 |
–3.2 |
|
Other Hazard (e.g., arcing wires, bomb removal) |
660,500 |
+9.4 |
|
Other (e.g., smoke scares, lockouts) |
3,003,500 |
+9.5 |
|
Total |
22,406,000 |
+5.2 |
|
SOURCE: U.S. Fire Administration, 2005. |
||
sonnel or rescue or other equipment. Using protocols, emergency medical dispatchers must determine whether ground or air ambulance capacity is required for a given emergency call. The default position for dispatchers is to assume that a ground ambulance is needed. Air ambulances are not typically called until an emergency responder on the ground (police, first responder, or emergency medical technician [EMT]) has confirmed the need.
Fire department first responders often provide support for patients before other EMS units can respond. Fire stations are generally well distributed across a given jurisdiction, especially in urban and suburban areas, and are often the first responders able to arrive at the scene of a medical emergency. Although statistics from the U.S. Fire Administration indicate that medical aid calls outnumber fire calls by 9 to 1 (see Table 5-4), fire equipment is typically geared to fighting fires rather than treating sick or injured patients. As a result, it is not uncommon for large fire trucks to carry first responders or EMS personnel to the scene of an incident.
Ground Ambulance Capacity and Safety Issues
Today more than 12,000 ambulance services operate about 24,000 ground ambulance vehicles in the United States (AAA, 2006). Typically, ambulances must be licensed by the state to ensure that they meet specific trained staffing and equipment requirements. Although these requirements vary by state, basic life support (BLS) units typically carry EMS personnel, as well as equipment such as oxygen tanks, equipment to stabilize fractures, airway supplies (including suction devices and manual and automatic ventilators), and often automated external defibrillators (AEDs). Advanced life support (ALS) units carry paramedics, as well as all BLS equipment, plus medications, intravenous fluids, advanced airway adjuncts, portable pulse oximetry, manual heart monitors/defibrillators (some of which are capable
of acquiring and transmitting a 12-lead electrocardiogram), and external pacing.
A major function of state EMS offices is ambulance credentialing and inspection. In 2003, 41 state offices were involved in credentialing ambulances, while 42 state offices were engaged in ambulance inspections. Typically, states require EMS vehicles to be recredentialed every 1 to 2 years (Mears et al., 2003). The federal government also requires that all federal agencies—as well as other public and private services that use federal funding to purchase ambulances—comply with what are known as the KKK standards. Some states have adopted these standards as well and require their service to purchase KKK-compliant ambulances. However, these state and federal requirements typically address only basic ambulance capacity, not health and safety issues, which have become an increasingly significant problem.
From the standpoint of the EMS worker, the basic ambulance design is highly problematic. An assessment of EMS working conditions inside ambulances revealed that more than 40 percent of the working postures associated with high-frequency EMS tasks—including oxygen administration, heart monitoring, and blood pressure checks—create excessive musculoskeletal strain that requires corrective measures from an ergonomic perspective (Ferreira and Hignett, 2005). Ambulances are also unsafe for workers because they create an environment in which airborne and bloodborne pathogens can easily be transmitted.
In addition to these dangers, crashes involving ground ambulances are a major concern because of the frequency of high-speed, lights-and-siren driving; the transport of vulnerable patients and family members; and the poor restraint positions of EMS personnel. According to the Centers for Disease Control and Prevention (CDC), 300 fatal crashes involving ambulances occurred in the United States between 1991 and 2000. These crashes resulted in 357 fatalities, 275 of which were occupants of other vehicles or pedestrians (CDC, 2003). These data highlight the major threat posed by ambulances to their crews, their patients, and others on the road.
A number of solutions have been proposed to address these hazards. For example, some ambulances are now equipped with harnesses that allow EMS personnel to work in the back of the ambulance while still providing them with a restraint in the event of a crash or a sudden stop. Newer ambulance designs also include features that prevent patients from being projected through to the main compartment in the event of a crash.
There are also a number of efforts under way to reduce accident rates for ambulances. NHTSA has developed an Emergency Vehicle Operators Course (EVOC) National Standard Curriculum that some states require their providers to complete before being able to drive an ambulance. Other states, local EMS agencies, and even some insurance carriers require their
ambulance drivers to complete a driver training course that is often derived from the NHTSA course. EVOC thus represents an important step toward ensuring ambulance safety on the roads. In addition to training improvements, technology has been developed that provides ambulance drivers with automatic, audible feedback when they are not driving according to standards. This technology uses sophisticated on-board computers that are able to monitor speed, revolutions per minute (RPMs), and braking. Other new capabilities, such as “drive cams” and intelligent transportation highway designs (e.g., lane-centering devices in blizzard conditions) can also have a significant impact on safety. The committee supports the exploration of additional technological applications to increase patient and provider safety in ambulances, including the Federal Highway Safety Intelligent Transportation System Public Safety initiative.
Finally, ambulance safety is being addressed through protocols that dictate whether lights and sirens are appropriate to use in given situations. Operating with lights and sirens (i.e., “running hot”) can be helpful in navigating through traffic, but numerous studies indicate that doing so leads to increased danger (NAEMSP and NASEMSD, 1994; Hunt et al., 1995; Lacher and Bausher, 1997; Overton, 2001). A central question, then, is whether the use of lights and sirens is justified given the health care needs of the patient. Hunt and colleagues (1995) determined that on average, the use of lights and sirens saved only 43.5 seconds in transporting patients from the scene of an emergency to the hospital. The authors argued that such a small improvement in transport time would be clinically meaningful only in very rare situations. Lacher and Bausher (1997) found that nearly 40 percent of pediatric 9-1-1 responders inappropriately used lights and sirens when the patient was stable. They concluded that limited use of lights and sirens, dictated by strong protocols, could reduce the dangers associated with inappropriate use (Lacher and Bausher, 1997).
Air Medical Services
Air medical operations, including those involving both rotor-wing helicopters and fixed-wing aircraft, have become an increasingly significant component of U.S. medical capabilities (Helicopter Association International, 2005). The air medical industry began in the United States in the early 1970s, following the Vietnam War (Blumen and UCAN Safety Committee, 2002). During the war, the U.S. military used helicopters to transport soldiers from the front lines to mobile army surgical hospitals. After soldiers had been stabilized, the military deployed fixed-wing aircraft to transport them home. In Vietnam, the time it took for soldiers to be transported from the combat theater to a stateside medical hospital averaged approximately 45 days. During the Afghanistan and Iraq wars, transport time for wounded
soldiers has been reduced to as little as 36 hours, with medical care provided throughout (Gawande, 2004).
Air ambulance operations for U.S. civilians have traditionally followed the military model of “trauma medevac,” which emphasizes speed—moving the patient away from the site of the injury and to definitive care. However, a growing trend in the air medical industry is to bring more of the assets of the trauma center directly to the patient (Judge, 2005). One of the long-recognized goals of EMS is to deliver patients to definitive care within the “golden hour” (Lerner and Moscati, 2001), and in most cases this remains a primary objective. Air ambulance providers play a key role, especially in rural areas, where trauma centers are typically farther away from the scene of an incident. Branas and colleagues (2005) estimated that medical helicopters provide access for 81.4 million Americans who otherwise would not be able to reach a trauma center within an hour.
The Atlas and Database of Air Medical Services (ADAMS)—developed by academic researchers and supported by the Federal Highway Administration and NHTSA—now provides a map of available air medical service areas across the United States. ADAMS indicates that air medical providers have a heavy presence in many urban and suburban areas of the country, but that coverage is sparse in many rural locales. While it is inherently difficult to provide timely care to these remote areas, they have a particular need for greater coverage by air ambulance providers. Data indicate that in 2001, about 39 percent of vehicle-miles traveled were on rural roads, but 61 percent of all crash fatalities occurred on these roads (Flanigan et al., 2005).
In addition to concerns about access, there are concerns regarding safety. As noted earlier, there has recently been an increase in the number of air ambulances involved in crashes and this has prompted greater scrutiny from the media and regulators. The Federal Aviation Administration (FAA) is responsible for certifying the safety of air ambulance programs operating in the United States. However, because of a decrease in the number of FAA inspectors, along with a rapid increase in the number of air medical providers, safety checks have not been sufficiently rigorous in recent years according to print media reports (Davis, 2005; Meier, 2005). This comes at a time when Medicare reimbursements for air medical transport have increased, and competition within the industry has grown substantially (Meier, 2005). In response to growing concerns regarding air ambulance safety, the FAA released guidelines in August 2005 instructing air ambulance firms to implement safety measures, such as using checklists to ensure that maintenance steps have been completed and improving decision making about whether to launch in unsafe weather conditions (Davis, 2005).
The Airline Deregulation Act of 1978 gave the FAA, rather than the states, regulatory authority over the operations of this industry. Court cases between states and the federal government involving air ambulance opera-
tions have centered largely on state efforts to control growth in air medical capacity through the certificate-of-need process. However, other questions regarding the federal preemption of state law have not been definitively resolved. Pennsylvania recently established a protocol requiring air ambulance operations to transport patients to the nearest trauma center, rather than to the base hospital. The air medical provider contested the protocol, saying that it was preempted by federal law. However, the FAA acknowledged in a letter to the state that it had never intended to regulate the medical aspects of air medical operations, and the case was never taken to court.
Some states currently have no regulatory framework in place to govern the medical care aspects of air ambulance providers. However, a key objective for state regulatory agencies should be to ensure coordination and improve the allocation of available assets, including air ambulances. Currently, ground EMS and 9-1-1 dispatch centers sometimes call for air medical support without coordination, resulting in more than one air medical provider being dispatched to a scene. This is a problem especially where there are multiple air medical services competing in the same coverage area. These providers typically market their services to EMS agencies, and when multiple EMS agencies are dispatched to the same event, they may each call for the air medical provider best known to them, resulting in multiple responses.
In light of the above issues, the committee recommends that states assume regulatory oversight of the medical aspects of air medical services, including communications, dispatch, and transport protocols (5.1). The regulatory authority of the FAA should extend to helicopters, fixed-wing aircraft, pilots, and company sponsors; however, the state should regulate the medical aspects of the operations, including personnel on board (nurses, paramedics, physicians), medical equipment, and transport protocols regarding hospitals and trauma centers. In addition, states should establish dispatch protocols for air medical response and should incorporate air medical providers into the broader emergency and trauma care system through improved communications. These measures are essential to more coordinated and efficient use of air capacity.
Interfacility Transport
In addition to transport from the scene of an incident directly to a medical facility, air medical helicopters are used extensively to transport patients from a hospital to a definitive care location. This often occurs, for example, with patients suffering a myocardial infarction or stroke, or pediatric patients who are critically ill or injured. This type of interfacility transport is probably the most common use of air medical services today.
Ground and air ambulances may also be used for nonemergency trans-
ports, such as those from nursing homes to hospitals for medical treatment or from hospitals to nursing homes following discharge. Unlike emergency calls, these trips can be scheduled in advance. With the aging of the population, these trends are likely to continue and may result in increasing call volumes for such transport operations.
Advances in Medical Technologies
Emerging medical and communications technologies are enabling real-time voice and video links between ambulance crews and emergency physicians. Some cities, such as San Antonio and Seattle, have established systems in which ambulances carry portable computers, video cameras, and microphones to transmit information to physicians. The technology allows physicians to view the patient, assess the extent of the injury, and determine possible treatment options while the patient is still en route (Medical Subcommittee of the ITS America Public Safety Advisory Group, 2002).
Many ambulance units are now equipped with technologies that allow for the direct transmission of patient data to hospital EDs. For example, 12-lead electrocardiograms enable physicians to view a patient’s heart readings prior to arrival at the hospital, and this capability has been shown to reduce door-to-treatment intervals significantly (Cannon, 1999; Woollard et al., 2005). In addition, providing this information to the physician allows for the administration of prehospital thrombolytic therapy, which in some studies has been shown to improve outcomes, although relatively few patients are eligible for the treatment (Boersma et al., 2000).
In addition to these emerging technologies, numerous other advances in medical treatment are likely to impact the level of care EMS personnel are able to provide to patients. For example, a study involving 20 level I trauma centers is currently under way to test the efficacy of an experimental oxygen-carrying blood substitute in increasing the survival of critically injured and bleeding trauma patients. Under the study protocol, treatment begins before arrival at the hospital, either at the scene of the injury, in the ambulance, or in an air ambulance. Because blood is not currently carried in ambulances, use of the blood substitute in these settings has the potential to address a critical unmet medical need. The introduction of saline, the current standard of care, helps restore a patient’s blood pressure but does not deliver oxygen, which is critical to preventing damage in the brain, heart, lungs, and other organs.
Emerging communications technologies and clinical treatments should be evaluated to determine their impact on treatment cost, quality of care, and patient outcomes. New technologies are often offered at a high cost that is beyond the reach of many EMS systems across the country. Moreover, there is growing evidence that simpler interventions performed effectively in
a timely manner may be most important in ensuring good outcomes. Indeed, that was the conclusion of a recent World Health Organization report on prehospital trauma care systems (Sasser et al., 2005). In addition, research, including the Ontario Prehospital Advanced Life Support study, has raised serious questions about the value of ALS beyond early defibrillation and administration of aspirin and oxygen to patients suffering myocardial infarction. Technologies that simplify the job of the prehospital provider, such as AEDs and newly developed airway adjuncts, have been shown to improve outcomes. The appropriate roles of other, more complex technologies have not been well established (Bunn et al., 2001; Sasser et al., 2005).
COMMUNICATIONS AND DATA SYSTEMS
Communications among EMS and other public safety and health care providers are still very limited. Antiquated and incompatible voice communications systems often result in a lack of coordination among emergency personnel as they respond to incidents. As mentioned earlier, many EMS systems rely on voice communications equipment that was purchased in the 1970s with federal financial assistance and has never been upgraded. This equipment frequently suffers from dead spots, interference, and other technical problems (Public Safety Wireless Network Program, 2005) (see Figure 5-1). However, upgrading to new equipment is often prohibitively expensive for local communities.
Advanced data and information systems are now available in the commercial market; however, adoption of these systems has been uneven across the country. Most ambulance systems continue to rely on paper-based run records rather than electronic systems. Similarly, technologies that enable direct transmission of patient information (e.g., vital signs) to hospitals prior to the arrival of an ambulance have not been uniformly adopted. Consequently, there is a growing gap between the types of EMS data and information systems available and those commonly used in the field.
These issues are compounded by the significant variation in EMS operational structures at the local and regional levels. EMS agencies may be operated by local governments, fire departments, private companies, or other entities. This makes communications and data integration difficult, even among EMS providers within a given local area. Communications among EMS, public safety, public health, and other hospital providers are even more problematic given the technical challenges associated with developing interoperable networks. As a result of these challenges and the need for improved coordination, the committee recommends that hospitals, trauma centers, emergency medical services agencies, public safety departments, emergency management offices, and public health agencies develop integrated and interoperable communications and data systems (5.2). Each
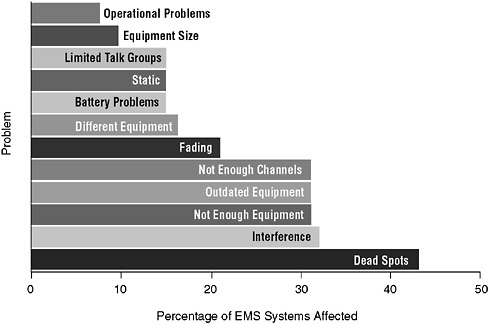
FIGURE 5-1 Problems with existing land mobile radio systems.
SOURCE: Public Safety Wireless Network Program, 2005.
state and local system should have communications plans for EMS that provide for interoperability and interconnectivity with other public service and health providers. A number of states are moving forward in developing wireless interoperable networks with assistance from the National Governors Association (National Governors Association Center for Best Practices, 2005). In addition, Maryland has developed a model communications system, described in Chapter 3. Such efforts need to be expanded nationwide.
Public Safety Communications
Voice communications improvements initiated by the federal government in the aftermath of the terrorist attacks of September 11 have focused on fire and police but have often overlooked EMS (Center for Catastrophe Preparedness and Response NYU, 2005). For example, interoperability of EMS and fire communications systems remains a significant problem. In a survey conducted by the Public Safety Wireless Network Program, 30 percent of responding fire and EMS agencies indicated that the lack of wireless communications interoperability has, at some time in the past, hampered their ability to respond to incidents. EMS agencies were the most adversely
affected by this lack of interoperability, with 53 percent indicating that it had limited their response capabilities. In addition, 43 percent of local fire and EMS agencies indicated that a lack of interoperability had affected their ability to communicate with agencies in surrounding jurisdictions (Public Safety Wireless Network Program, 2005).
As with other first responders, there are a number of barriers to improving the EMS system’s communications capabilities, including the absence of communications standards, significant technological barriers, and a lack of funding (Center for Catastrophe Preparedness and Response NYU, 2005). In addition, the above survey of EMS and fire agencies identified a number of additional obstacles to communications interoperability (see Figure 5-2). For example, 39 percent of local fire and EMS agencies rated political or turf issues as a severe obstacle. These factors have impeded progress toward a more effective communications system.
GAO reported in 2004 that federal leadership was needed to facilitate interoperable communications between first responders. The report asserted that jurisdictional boundaries and the unique missions of public safety agencies were hindrances to collaboration, and that the federal government should provide the leadership, long-term commitment, and focus to help state and local governments achieve interoperability. Specifically, GAO advised the federal government to assist in this effort by creating a national architecture for interoperable communications, establishing a standard database to coordinate frequencies, and allocating communications spectrum for public safety use (GAO, 2004).
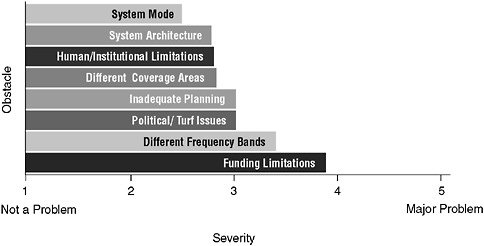
FIGURE 5-2 Obstacles to interoperability.
SOURCE: Public Safety Wireless Network Program, 2005.
The technical challenges to establishing an effective public safety communications system have been a focus of attention for over a decade. In 1996, the Public Safety Wireless Advisory Committee presented a report to the FCC and the National Telecommunications and Information Administration (NTIA) indicating the crucial need to promote interoperability and advocating the allocation of spectrum for the use of public safety agencies (The SAFECOM Project, 2004).
In 1997, Congress instructed the FCC to allocate 24 MHz of spectrum for public safety radio communications operations. However, the spectrum cannot be used in most heavily populated areas until local residents transition to digital television, and no firm date has been set for this transition. In the interim, many public safety agencies are continuing to operate with congested radio systems, and some have postponed the activation of fully interoperable radio networks in their regions (Alliance in Support of America’s First Responders, 2005).
To direct the federal government’s efforts at establishing an interoperable public safety communications system, the Office of Management and Budget established the Wireless Public Safety Interoperable Communications Program (SAFECOM), housed within the Department of Homeland Security. SAFECOM’s purpose is to help local, tribal, state, and federal public safety agencies improve public safety response through more effective and efficient interoperable wireless communications. In 2004, SAFECOM released its Statement of Requirements, focused on the functional needs of public safety first responders to communicate and share information effectively. The document served as a first step toward establishing base-level communications and interoperability standards for all 50,000 public safety agencies across the United States (The SAFECOM Project, 2004). The document describes several scenarios involving first responders, including a future scenario in which an EMS unit responds to a heart attack call. The PSAP responding to the call is equipped with displays indicating likely ambulance response times given current traffic conditions. Computer-activated voice technology assists the ambulance driver in selecting the fastest traffic lanes. On scene, a radio frequency identification (RFID) bracelet worn by the patient allows paramedics to determine the patient’s allergies to medicines. Data from the 12-lead electrocardiogram are transmitted wirelessly to the hospital through a public safety communications device (PSCD). All medical monitors are attached wirelessly to the patient, and the encounter is entirely paperless.
Health Care Data Systems
NHTSA’s Emergency Medical Services Agenda for the Future set forth five goals for the EMS information system of the future: (1) adopt uniform
data elements and definitions, and incorporate them into information systems; (2) develop mechanisms for generating and transmitting data that are valid, reliable, and accurate; (3) develop information systems that are able to describe an entire EMS event; (4) develop information systems that are integrated with other health care providers, public safety agencies, and community resources; and (5) provide feedback to those who generate data (NHTSA, 1996). Efforts are under way to achieve each of these objectives through the National EMS Information System (NEMSIS).
The availability of uniform, reliable EMS data has been a long-standing concern that emerged as major priority during the development of the Emergency Medical Services Agenda for the Future: Implementation Guide in the late 1990s. The availability of such data was cited as fundamental to a number of the Agenda’s goals, such as determining the costs and benefits of EMS and improving EMS research. GAO’s investigation of state and local EMS agencies in 2001 found unanimous agreement that greater availability of data and improved information systems were needed to monitor the agencies’ own performance and to quantify and justify system needs to the local public and decision makers (GAO, 2001).
Federal government efforts to improve EMS data systems date back more than a decade. In 1993, the Department of Health and Human Services, NHTSA, and the U.S. Fire Administration cosponsored a conference that resulted in the development of a model set of EMS data elements and definitions that could be used by states and local systems as the basis for creating their own information systems (GAO, 2001). This Uniform Prehospital EMS Dataset contained a wide array of data elements, including patient characteristics, dispatch and incident data, financial information, EMS system demographic data, and others.
NEMSIS, managed by NHTSA in coordination with the Health Resources and Services Administration, is a continuation of this work. NEMSIS is geared toward improving data standardization and linking disparate EMS databases at the federal, state, and local levels (Mears et al., 2003). It will serve as a national EMS database that can be used to evaluate patient and EMS system outcomes, benchmark performance, facilitate research efforts, develop nationwide EMS training curricula, determine national fee schedules, and address disaster preparedness resource issues. The database will be able to supply information at the national level, such as the total number and types of EMS calls, average response times, and the most widely used medications and procedures. Currently, all of the states except New York and Vermont have elected to participate in the project. By the end of 2006, 6–7 states are expected to be fully operational in the program and will be submitting state-level data to the national EMS database; this number is expected to increase by 17 by the end of 2007. Becoming fully operational means that states are collecting and submitting NEMSIS-compliant data from
the individual EMS provider agencies within their respective states. NHTSA houses NEMSIS at its National Center for Statistics and Analysis.
In addition, the American College of Surgeons administers the National Trauma Data Bank (NTDB), the largest single injury database in the country. The NTDB contains over 1.5 million records from 405 trauma centers in the United States and Puerto Rico. Its goal is to inform the medical community, the public, and decision makers about a wide variety of issues that characterize the current state of care for injured persons. The information contained in the NTDB has implications in many areas, including epidemiology, injury control, research, education, acute care, and resource allocation (American College of Surgeons, 2006).
In addition to the development of data systems, new technology now in use by the military has the potential to streamline data collection in the field. The Battlefield Medical Information System Tactical (BMIST) device is a handheld unit that enables military health care providers to record, store, retrieve, and transmit the essential elements of clinical encounters at the point of care (Onley, 2004). The device provides diagnostic and treatment decision aids and has the capability to incorporate new procedures and protocols. In addition, it can retrieve a patient’s complete medical records, including drug allergies, immunization status, and dental records. Significant obstacles exist to the adoption of this type of technology in the commercial market, especially with respect to the availability of a patient’s complete medical records. However, companies selling to the civilian market are developing formal field tests of similar technology (TeleMedic Systems, 2001).
In addition, the transition to a National Health Information Infrastructure (NHII) for the United States is currently under way. In 2004, the Bush Administration called for widespread adoption of interoperable EHRs within 10 years and designated a National Coordinator for Health Information Technology. Since then, the coordinator has sought to develop common technology standards and broader consensus among the public and private stakeholders involved in this effort. However, discussions regarding the NHII have frequently excluded prehospital emergency care. The initial focus of the effort centered on hospitals, ambulatory care providers, pharmacies, and other more visible components of the health care system. Given the role played by prehospital EMS in providing essential and often lifesaving treatment to patients, this has been a significant oversight. Therefore, the committee recommends that the Department of Health and Human Services fully involve prehospital emergency medical services leadership in discussions about the design, deployment, and financing of the National Health Information Infrastructure (5.3).
In addition to this national effort, local areas have moved forward with initiatives to support regional health information sharing. For example, the Santa Barbara County Care Data Exchange project allows for the ap-
propriate sharing of clinical information among medical groups, hospitals, clinics, laboratories, pharmacies, and payers (IOM, 2003; SBCCDE, 2006). Approximately 75 percent of the health care providers in the county are involved in the project. There is also an EMS component to the effort. The Santa Barbara County EMS Information Systems Project has sought to develop accurate EMS information systems that are integrated with other health care providers, public safety agencies, and community resources (Santa Barbara County Public Health Department, 2003). This project has the following objectives: (1) to ensure that the times at which calls are received by the PSAP are recorded; (2) to ensure that all providers have synchronized times based on Coordinated Universal Time (UTC); (3) to integrate information from the various providers into a comprehensive EMS response patient care record; and (4) to provide feedback to individual service providers regarding patient outcomes and provider performance. This project meets a number of the goals established by the Emergency Medical Services Agenda for the Future and can serve as a model for other communities across the United States.
Efforts to improve health information technology are aimed at improving the effectiveness, efficiency, and safety of health care interventions. The goal is to link all relevant providers so that communication of vital patient data is smooth, and patient hand-offs are seamless. A key component of that linkage is the hand-off between EMS personnel and hospital-based providers. Therefore, the committee believes there should be improved interface and connectivity between EMS electronic patient records and hospital electronic records, with the goal of transmitting EMS electronic information to EDs in real time.
In addition to patient data, there is often a need for EMS-to-hospital communications regarding the current status of hospital facilities. Ambulance units frequently transport patients to facilities that are on diversion or do not have the necessary subspecialists on call to handle the type of emergency patient they are transporting. Units then must travel to another facility, wasting valuable time in the process. Emerging technology will enable ambulance providers to have ready access to data indicating the current status of hospitals in the local area. Systems in use in Richmond, San Diego, and elsewhere allow ambulance providers to see the diversion status of hospitals throughout the region. This type of information could also assist in detailing recurring diversion patterns at various regional facilities.
SUMMARY OF RECOMMENDATIONS
5.1: States should assume regulatory oversight of the medical aspects of air medical services, including communications, dispatch, and transport protocols.
5.2: Hospitals, trauma centers, emergency medical services agencies, public safety departments, emergency management offices, and public health agencies should develop integrated and interoperable communications and data systems.
5.3: The Department of Health and Human Services should fully involve prehospital emergency medical services leadership in discussions about the design, deployment, and financing of the National Health Information Infrastructure.
REFERENCES
AAA (American Ambulance Association). 2006. Ambulance Facts. [Online]. Available: http://www.the-aaa.org/media/AmbulanceFacts.htm [accessed January 5, 2006].
Alliance in Support of America’s First Responders. 2005. Support America’s First Responders. [Online]. Available: http://www.apcointl.com/supportamericasfirstresponders/index.htm [accessed November 1, 2005].
American College of Surgeons. 2006. National Trauma Data Bank. [Online]. Available: http://www. facs.org/trauma/ntdb.html [accessed February 7, 2006].
Bachman LR, Preziotti GR. 2001. Automated Collision Notification (ACN) Field Operational Test (FOT) Evaluation Report. Springfield, VA: National Technical Information Service.
Blumen IJ, UCAN Safety Committee. 2002. A Safety Review and Risk Assessment in Air Medical Transport. Salt Lake City, UT: Air Medical Physician Association.
Boersma E, Akkerhuis M, Simoons ML. 2000. Primary angioplasty versus thrombolysis for acute myocardial infarction. New England Journal of Medicine 342(12):890–891; author reply 891–892.
Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. 2005. Access to trauma centers in the United States. Journal of the American Medical Association 293(21):2626–2633.
Bunn F, Kwan I, Roberts I, Wentz R. 2001. Effectiveness of Pre-Hospital Trauma Care. London, England: London School of Hygiene & Tropical Medicine.
Cannon CP. 1999. Advances in the medical management of acute coronary syndromes. Journal of Thrombosis & Thrombolysis 7(2):171–189.
CDC (Centers for Disease Control and Prevention). 2003. Ambulance crash-related injuries among emergency medical services workers––United States, 1991–2002. Morbidity & Mortality Weekly Report 52(8):154–156.
Center for Catastrophe Preparedness and Response NYU. 2005. Emergency Medical Services: The Forgotten First Responder: A Report on the Critical Gaps in Organization and Deficits in Resources for America’s Medical First Responders. New York: Center for Catastrophe Preparedness and Response, New York University.
Champion H, Augenstein J, Blatt AJ, Cushing B, Digges KH, Hunt RC, Lombardo LV, Siegel JH. 1999. Reducing Highway Deaths and Disabilities with Automatic Wireless Transmission of Serious Injury Probability Ratings from Vehicles in Crashes to EMS, Paper 406. Presentation at the meeting of the Proceedings of the 18th ESV Conference. [Online]. Available: http://www-nrd.nhtsa.dot.gov/pdf/nrd-01/esv/esv18/CD/Files/18ESV-000406.pdf [accessed August 4, 2006].
Davis R. 2005, August 11. Air ambulance firms warned. USA Today. P. 1A.
DOT (U.S. Department of Transportation) Intelligent Transportation Systems. 2006, February 10. Today’s 9-1-1 vs. Future 9-1-1. [Online]. Available: http://www.its.dot.gov/ng911/ng911_future.htm [accessed February 25, 2006].
DOT Wireless E9-1-1 Steering Council. 2002. Wireless E9-1-1 Priority Action Plan. Washington, DC: DOT Intelligent Transportation Systems Joint Program Office (HOIT).
FCC (Federal Communications Commission). 2006. VoIP and 911 Services: VoIP 911 Background. [Online]. Available: http://www.voip911.gov [accessed February 25, 2006].
Ferreira J, Hignett S. 2005. Reviewing ambulance design for clinical efficiency and paramedic safety. Applied Ergonomics 36(1):97–105.
Flanigan M, Blatt A, Lombardo L, Mancuso D, Miller M, Wiles D, Pirson H, Hwang J, Thill J, Majka K. 2005. Assessment of air medical coverage using the atlas and database of air medical services and correlations with reduced highway fatality rates. Air Medical Journal 24(4):151–163.
GAO (U.S. Government Accountability Office). 2001. Emergency Medical Services: Reported Needs Are Wide-Ranging, with a Growing Focus on Lack of Data. Washington, DC: Government Printing Office.
GAO. 2003. Uneven Implementation of Wireless Enhanced 911 Raises Prospect of Piecemeal Availability for Years to Come. Washington, DC: Government Printing Office.
GAO. 2004. Homeland Security: Federal Leadership Needed to Facilitate Interoperable Communications between First Responders. Washington, DC: Government Printing Office.
Gawande A. 2004. Casualties of war––military care for the wounded from Iraq and Afghanistan. New England Journal of Medicine 351(24):2471–2475.
Helicopter Association International. 2005. White Paper: Improving Safety in Helicopter Emergency Medical Services (HEMS) Operations. Alexandria, VA: Helicopter Association International.
Hunt RC, Brown LH, Cabinum ES, Whitley TW, Prasad NH, Owens CF Jr, Mayo CE Jr. 1995. Is ambulance transport time with lights and siren faster than that without? Annals of Emergency Medicine 25(4):507–511.
IOM (Institute of Medicine). 1993. Emergency Medical Services for Children. Washington, DC: National Academy Press.
IOM. 2003. Patient Safety: Achieving a New Standard for Care. Washington, DC: The National Academies Press.
Judge T. 2005, April. Contemporary Air Medicine in the USA––Briefing for Institute of Medicine. Unpublished.
Key CB, Pepe PE, Persse DE, Calderon D. 2003. Can first responders be sent to selected 9-1-1 emergency medical services calls without an ambulance? Academic Emergency Medicine 10(4):339–346.
Lacher M, Bausher J. 1997. Lights and siren in pediatric 911 ambulance transports: Are they being misused? Annals of Emergency Medicine 29(2):223–227.
Lerner EB, Moscati RM. 2001. The golden hour: Scientific fact or medical “urban legend”? Academic Emergency Medicine 8(7):758–760.
Mears G, Kagarise J, Raisor C. 2003. 2003 Survey and Analysis of EMS Scope of Practice and Practice Settings Impacting EMS Services in Rural America: Executive Brief and Recommendations. Chapel Hill, NC: University of North Carolina at Chapel Hill Department of Emergency Medicine.
Medical Subcommittee of the ITS America Public Safety Advisory Group. 2002. Recommendations for ITS Technology in Emergency Medical Services. Washington, DC: ITS America.
Meier B. 2005, May 3. Air ambulances are multiplying, and costs rise. The New York Times. P. A1.
NAEMSP, NASEMSD (National Association of Emergency Medical Services Physicians, National Association of State EMS Directors). 1994. Use of warning lights and siren in emergency medical vehicle response and patient transport. Prehospital & Disaster Medicine 9(2):133–136.
NAS, NRC (National Academy of Sciences, National Research Council). 1966. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: NAS.
NAS, NRC. 1978. Emergency Medical Services at Midpassage. Washington, DC: NAS.
National Fire Protection Association. 2005. Fire Department Calls. Quincy, MA: National Fire Protection Association.
National Governors Association Center for Best Practices. 2005. Policy Academy on Wireless Interoperability. [Online]. Available: http://www.nga.org/portal/site/nga/menuitem.9123e83a1f6786440ddcbeeb501010a0/?vgnextoid=93d31a37ab8e4010VgnVCM1000001a01010aRCRD/ [accessed April 20, 2006].
NENA (National Emergency Number Association). 2001. Report Card to the Nation: The Effectiveness, Accessibility and Future of America’s 9-1-1 Service. Columbus, OH: RCN Commission/NENA.
NENA. 2004. The Development of 9-1-1. [Online]. Available: http://www.nena.org/PR_Pubs/Devel_of_911.htm [accessed September 28, 2004].
NENA. 2006. 9-1-1 Fast Facts. Arlington, VA: NENA.
NHTSA (National Highway Traffic Safety Administration). 1996. Emergency Medical Services Agenda for the Future. Washington, DC: Department of Transportation.
NHTSA Office of EMS. 2006. EMS Update. [Online]. Available: http://www.nvfc.org/pdf/2006-ems-upate.pdf [accessed May 1, 2006].
Onley DS. 2004, November 22. Electronic medical records go into combat. Government Computer News. [Online]. Available: http://www.gcn.com/print/23_33/27923-1.html [accessed January 27, 2007].
Overton J. 2001. Ambulance design and safety. Journal of Prehospital and Disaster Medicine 16(3).
Public Safety Wireless Network Program. 2005. Information Brief: Fire and EMS Communications Interoperability. Washington, DC: Department of Justice and Department of the Treasury.
The SAFECOM Project. 2004. Statement of Requirements for Public Safety Wireless Communications & Interoperability. Washington, DC: Department of Homeland Security.
Santa Barbara County Public Health Department. 2003. EMS Information Systems Project. [Online]. Available: http://www.sbcphd.org/ems/isdisaster.html [accessed December 1, 2005].
Sasser S, Varghese M, Kellermann A, Lormand JD. 2005. Prehospital Trauma Care Systems. Geneva, Switzerland: World Health Organization.
SBCCDE (Santa Barbara County Care Data Exchange). 2006. Background Information & Recent Quotes. [Online]. Available: http://www.sbccde.org/bginfo.htm [accessed January 5, 2006].
TeleMedic Systems. 2001. Home Page. [Online]. Available: http://www.telemedicsystems.com/corpsite/ [accessed February 1, 2006].
U.S. Fire Administration. 2005. Fire Departments. [Online]. Available: http://www.usfa.fema.gov/statistics/departments/ [accessed February 1, 2006].
Woollard M, Pitt K, Hayward AJ, Taylor NC. 2005. Limited benefits of ambulance telemetry in delivering early thrombolysis: A randomised controlled trial. Emergency Medicine Journal 22(3):209–215.


























