6
Preparing for Disasters
On August 29, 2005, Hurricane Katrina struck the U.S. Gulf Coast, leaving over 1,300 people dead, countless injured, and over 1 million displaced. The aftermath of the hurricane created a humanitarian crisis unparalleled in the nation’s history, with federal disaster declarations covering 90,000 square miles (GAO, 2005). While the scope of Hurricane Katrina extended far beyond typical disaster scenarios, it illustrated the heavy demands that can be placed upon emergency workers in the event of a major crisis.
The term “disaster” denotes a low-probability but high-impact event that causes a large number of individuals to become ill or injured. The International Federation of Red Cross and Red Crescent Societies defines a disaster as an event that causes more than 10 deaths, affects more than 100 people, or leads to an appeal for assistance by those affected (Bravata et al., 2004). Disaster events overwhelm a community’s emergency response capacity (Waeckerle et al., 1994) and create an imbalance between the supply of available resources and the need for those resources (Noji, 1996).
Even in responding to day-to-day demands, however, the emergency and trauma care system in the United States is often stretched beyond its capacity. This is evidenced by the frequency with which hospitals are placed on diversion and ambulances are required to find alternative receiving hospitals (GAO, 2003a). The capacity shortages that are observable on a day-to-day basis in many areas of the country are magnified considerably in the event of a disaster. Given the existing challenges, there is substantial evidence that the emergency and trauma care system is not well prepared for larger-scale disaster events (Schur et al., 2004).
Emergency medical services (EMS) personnel are always among the first
to respond in the event of a disaster. However, they are also the least supported in fulfilling this role among all public safety personnel nationwide, lacking both adequate training and proper equipment for disaster response. According to New York University’s Center for Catastrophe Preparedness and Response, more than half of emergency medical technicians (EMTs) and paramedics have received less than 1 hour of training in dealing with biological and chemical agents and explosives since the terrorist attacks of September 11, and 20 percent have received no such training. In 25 states, moreover, fewer than 50 percent of EMTs and paramedics have adequate equipment to respond to a biological or chemical attack (Center for Catastrophe Preparedness and Response NYU, 2005).
In the aftermath of September 11, President Bush promulgated a set of Homeland Security Presidential Directives designed to ensure a coordinated response to a national emergency. But the absence of effective federal, state, and local coordination following Hurricane Katrina demonstrated just how far we have to go in this regard. The integration of emergency care, trauma systems, and EMS into the overall disaster planning process has proven even more problematic. EMS providers and state and local EMS directors are often excluded from critical disaster planning efforts (Center for Catastrophe Preparedness and Response NYU, 2005). Federal programs dealing with medical aspects of disaster preparedness are dispersed among multiple agencies, including the Department of Homeland Security (DHS), the National Highway Traffic Safety Administration (NHTSA), and the Department of Health and Human Services (DHHS). And there are no EMS-specific standards and guidelines for the training and equipment necessary to respond effectively to a terrorist attack or disaster (Center for Catastrophe Preparedness and Response NYU, 2005).
This lack of coordination is reflected in the haphazard funding of preparedness initiatives. EMS and trauma systems have consistently been underfunded relative to their presence and role in the field (Rudman et al., 2003; Center for Catastrophe Preparedness and Response NYU, 2005). Recent audits have found that EMS systems have received only 4–6 percent of federal disaster preparedness funds from DHS and DHHS (GAO, 2003b; Center for Catastrophe Preparedness and Response NYU, 2005). One recent survey revealed that 58 percent of responding ambulance agencies had not been allocated any federal funding for terrorism preparedness. Nearly 60 percent stated that their organization had not benefited from indirect access to items purchased with federal funds. Fully 82.8 percent of respondents had encountered either extreme difficulty or difficulty in obtaining federal funding and access to items purchased with federal funding (AAA, 2004).
This chapter reviews the array of threats faced by the United States and describes the medical responses to recent disasters both here and abroad.
Against this background, the committee details measures that can be taken to improve the nation’s EMS-related disaster preparedness.
THE ARRAY OF THREATS
Worldwide, disasters occur almost daily; in the past 20 years, they have claimed nearly 3 million lives and adversely affected 800 million more (Waeckerle, 2000; Chan et al., 2004). Such events can be either naturally occurring catastrophes or, increasingly, intentional (terrorist) or unintentional man-made disasters (see Table 6-1). Recent experience demonstrates the frequency with which disasters can strike and the tremendous impact they can have on the residents of stricken areas.
TABLE 6-1 Recent Disaster Events (United States and Worldwide)
|
Type |
Category |
Location |
Deaths |
|
Naturally Occurring |
Hurricane (Katrina) Avian influenza Earthquake Tsunami Severe acute respiratory syndrome (SARS) Earthquake |
Louisiana (especially New Orleans), Mississippi, Alabama (2005–2006) 6 countries (2005–2006) Kashmir (2005) 12 countries (2004) 25 countries (2002–2003) Northridge, California (1994) |
1,326 118 (as of 10/20/05) 73,000 (69,000 injured) 212,611 774 57 (5,000+ injured) |
|
Man-made, Intentional (Terrorist) or Unintentional |
Train bombings Nightclub fire Nightclub bombing Anthrax attacks Terrorist attacks of September 11 Embassy bombings Sarin gas attack |
London (2005) Madrid (2004) Rhode Island (2003) Bali (2002) Washington, D.C. (2001) New York/Washington, D.C. (2001) Nairobi and Tanzania (1998) Tokyo, Japan (1995) |
52 (700 injured) 191 (2,000 injured) 100 (200+ injured) 202 5 (13 injured) 2,752 224 (4,000+ injured) 12 (5,000 injured) |
|
SOURCE: Accountability Review Boards on the Embassy Bombings in Nairobi and Dar es Salaam, 1999; CNN.com, 2003, 2005a,b; Hirschkorn, 2003; Gutierrez de Ceballos et al., 2004; IOM, 2004; Rand Corporation, 2004; BBC News, 2005, 2006a,b; Times Foundation, 2005; Associated Press, 2006a,b; Insurance Information Network of California, 2006. |
|||
Naturally Occurring Disasters
The nation is vulnerable to a wide range of natural disasters, including earthquakes, extreme heat, forest fires, wildfires, floods, hurricanes, mudslides, thunderstorms, tornadoes, tsunamis, volcanoes, and winter storms/extreme cold (DHS READYAmerica, 2005). Responders in areas that are prone to certain types of disasters (e.g., search and rescue teams in cities along the San Andreas Fault in California) are generally well prepared and cognizant of the risks involved. As with Hurricane Katrina, however, responders may be unprepared for the magnitude of the crisis in a worst-case scenario. Such events can overwhelm local resources and require additional help from neighboring areas, adjoining states, or, in many cases, the federal government.
Historically, flooding has been the nation’s most common natural disaster, having occurred in every state (DHS READYAmerica, 2005). Earthquakes, regarded as a West Coast phenomenon, in fact pose a moderate to high risk to the majority of states. Tornados are focused primarily in states located in “tornado alley” in the Midwest. Hurricanes form in the southern Atlantic Ocean, Caribbean Sea, Gulf of Mexico, and eastern Pacific Ocean and affect coastal states in those areas (DHS READYAmerica, 2005).
Disease outbreaks also pose a significant risk to the United States. In 2003, severe acute respiratory syndrome (SARS) spread quickly from China to several countries in Asia and to Toronto, Canada, representing a potential threat to the United States (Augustine et al., 2004). Infected travelers spread the disease before public health officials in China were able to recognize its significance. SARS is highly infectious and is transmitted through close personal contact. The outbreak illustrated how quickly such an event can get out of control when health care workers themselves become not only victims, but also transmitters of the disease. The spread of SARS was contained in 2003; however, public health officials in the United States have warned that the possibility of another outbreak remains.
In addition to the threat posed by SARS, world health officials continue to issue warnings about the potential for avian influenza (H5N1) to mutate and become transmissible from human to human, potentially resulting in a global pandemic. There are widespread fears that this strain of influenza could result in deaths of the magnitude experienced during the 1918–1919 Spanish flu pandemic, which by some estimates claimed the lives of 500,000 Americans and more than 20 million people worldwide (Fee and Parry, 2005; IOM, 2005).
The United States is seeking to stockpile sufficient quantities of vaccines and antivirals to protect against the threat of pandemic influenza, but a scenario in which the government is unable to stop the spread of the disease remains highly plausible. Currently, common influenza causes the deaths of
approximately 36,000 Americans each year. A pandemic occurs when there is a major change in the influenza virus such that most or all of the world’s population has never been exposed to and therefore is vulnerable to the virus (IOM, 2005). Vaccine manufacturers are ramping up capacity to produce a vaccine that will be effective against H5N1, but it will take 6–9 months to produce an adequate supply, and the effectiveness of a vaccine will depend on how the virus mutates.
In the event of an outbreak of pandemic influenza, emergency medical responders will potentially be called upon to treat and transport thousands of afflicted individuals. However, there are a number of concerns regarding the nation’s preparedness for and potential response to such an event, including (1) the overwhelming number of afflicted individuals who would require hospitalization or outpatient medical care, stretching an already overburdened emergency and trauma care system; (2) the fact that communities across the country would be affected simultaneously, limiting the ability of any jurisdiction to provide support and assistance to other areas; and (3) disruptions that would occur in public safety and emergency and trauma care systems as their personnel fell ill and even succumbed to the disease (IOM, 2005). These challenges call into question U.S. readiness for a catastrophic public health emergency.
Unintentional Man-Made Disasters
While terrorist attacks are a constant concern, an array of other manmade disasters threaten communities and have the potential to strain or exceed the capacity of local emergency and trauma care resources. These include train wrecks, plane crashes, and fires (which may also be intentionally set). For example, the 2003 nightclub fire in West Warwick, Rhode Island, killed 100 people and injured 200 others, placing a strain on the local emergency care system, as well as area firefighters. This type of incident illustrates the need for effective surge capacity in the emergency and trauma care system and the value of an “all hazards” approach to disaster preparedness.
Terrorist Threats
Concerns regarding the likelihood of terrorist attacks increased dramatically in the wake of September 11, 2001. Recent terrorist events overseas, including the Madrid train bombings in 2004 and the London transit bombings of 2005, have added to those concerns. Terrorist attacks on the United States could take a number of different forms (see Box 6-1). Threats emanate from chemical, biological, radiological, nuclear, and explosive (CBRNE) sources and could be directed against a range of targets, includ-
|
BOX 6-1 Examples of Major Terrorist Threats to the United States Explosives
Chemical
Biological
Radiological
Nuclear
SOURCE: CDC, 2006a. |
ing our transportation systems, government institutions, and food supplies, among others.
Explosions are by far the most common cause of casualties associated with terrorism. From 1991 to 2000, 93 reported terrorist attacks resulted in more than 30 casualties, and 88 percent of those attacks involved explosions (Arnold et al., 2004). Over the past 25 years, explosives or firearms have been used to commit countless acts of terrorism in Israel, Egypt, Kenya, Argentina, Colombia, Bali, Yemen, Russia, the United Kingdom, Germany, France, Italy, the United States, and many other countries. Every week, if not every day, another suicide bombing, car bombing, or improvised explosive device claims the lives of innocent victims. This threat of terrorism involving conventional weapons is especially prevalent in large urban areas. Yet even though traumatic injury is likely to be the primary result of these types of
explosive attacks, the federal government recently eliminated the Health Resources and Service Administration’s (HRSA) Trauma-EMS Systems Program and the grants it provided to states to develop and maintain trauma systems. There are presently 52 Centers for Public Health Preparedness supported by federal funding that focus on various aspects of bioterrorism, but not one federally funded center is focused on the civilian consequences of terrorist bombings (CDC, 2006b).
Although explosive devices are the most commonly used terrorist weapon, there is evidence that terrorists have also sought to develop chemical, biological, and radiological weapons, such as the following:
-
Mustard gas is a blister agent that poses a threat through direct contact or inhalation. Inhalation of mustard gas damages the lungs, causes breathing difficulties, and leads to death by suffocation in severe cases as a result of water in the lungs (DHS, 2003).
-
Sarin disrupts a victim’s nervous system by blocking the transmission of nerve signals. Exposure to nerve agents causes constriction of the pupils, salivation, and convulsions that can lead to death (DHS, 2003).
-
Ricin is a plant toxin that is 30 times more potent than the nerve agent VX. There is no treatment for ricin poisoning once the agent has entered the bloodstream (DHS, 2003).
-
Inhaled anthrax is usually fatal unless antibiotic treatment is started prior to the onset of symptoms. Anthrax can be disseminated in aerosol form or used to contaminate food or water. The anthrax attacks in the United States in 2001 involved placing aerosolized anthrax in letters sent to U.S. Congressmen and impacted postal workers near the nation’s capitol (DHS, 2003).
-
Smallpox is a contagious and often fatal infectious disease. Although it was eradicated from human populations through a globally coordinated program of vaccination, there are concerns that the virus could still be used in a terrorist attack. Stockpiles of the virus exist in the United States and Russia, and some fear that they could be stolen by terrorists. One study showed that if 100 people were initially infected with smallpox, a 15-day delay in control measures could result in over 15,000 excess cases after 1 year (Henning, 2003; CDC, 2004).
-
A dirty bomb is designed to disperse radioactive material. While unlikely to cause mass casualties or extensive destruction, such a device would lead to fear, injuries, and possibly levels of contamination requiring costly and time-consuming cleanup (DHS, 2003).
In addition to these and other well-known threats, an increasing number of “next-generation” bioterrorist agents are emerging. A recent National Academy of Sciences report, Global Effort Needed to Anticipate
and Prevent Potential Misuse of Advances in Life Sciences, asserted that intelligence agencies are too focused on specific lists of bacteria and viruses and should place more emphasis on dangerous emerging threats, such as RNA interference, synthetic biology, and nanotechnology (IOM and NRC, 2006). Nevertheless, more basic weapons, including conventional bombs and improvised explosive devices, appear to be the primary terrorist threats facing the United States today.
RESPONSES TO RECENT DISASTERS
Responding to a disaster requires preparation and also adaptability on the part of emergency responders. In many crisis situations, such as a natural disaster or terrorist incident, communications equipment may become inoperable, leaving rescue workers and emergency managers without any effective means of transmitting information. The chaotic flow of events in an evolving disaster can produce an effect that has been likened to “the fog of war” (Horwitz and Davenport, 2005; U.S. House of Representatives, 2006).
Emergency workers themselves may be victims of the catastrophic event and unable to respond. Some may be among the wounded, killed, or infected; others may have to respond to the needs of their own families. Those who are able to respond confront an array of challenges. During Hurricane Katrina, many roads were flooded and impassable, leaving personnel without an adequate means to reach those in need. In the case of Katrina, as well as other past catastrophes, working situations became unsafe as law and order began to break down. While serving as an EMT or paramedic typically involves a number of dangers, such as transporting patients at high speeds and entering scenes of recent violence (see Chapter 4), these dangers are amplified during a large-scale disaster.
Managing patients in a large-scale disaster is also extremely challenging. Although disaster planners frequently assume that casualties will be transported to hospitals by ambulance, research shows that most arrive by other means, including private cars, police vehicles, buses, taxis, or on foot (Auf der Heide, 2006). This frequently results in the crowding of nearby hospitals and reduced system efficiency since patients are not immediately directed to facilities that are open and ready. In most instances, the patients first arriving, who have “self-triaged” themselves from the scene, are often less seriously ill or injured than those that follow. This contributes to the chaos and confusion that mass casualty incidents typically produce.
Following a mass-casualty incident, there are often calls for policy changes that will produce more effective means of dealing with crisis events. Such changes may involve restructuring government bureaucracy or improving the way help from neighboring cities and states is utilized. These types
of reforms have been introduced subsequent to a number of major disaster events in U.S. history, including September 11 and the Oklahoma City bombing, as well as disasters that have taken place in foreign countries.
Terrorist Attacks of September 11
The terrorist attacks on the World Trade Center and the Pentagon on September 11, 2001, represented a seminal event in U.S. history. The damage suffered that day increased awareness of the threat posed by terrorist groups and the potential for future attacks. The crisis spawned a series of actions on the part of the U.S. government to mitigate the possibility of such a disaster happening again.
EMS played a vital role in the emergency response to the attacks. Along with fire, police, and other rescue workers, EMS personnel were among the first to respond. According to the New York State Department of Health, 2,500 EMS personnel from 345 ambulance services responded to the World Trade Center attack, and 8 EMS workers were killed (Hall, 2005).
In addition to the bombing victims who were treated on scene by EMS personnel and transported to area hospitals, a large number of the injured either walked or were transported by other means to nearby hospitals. Two affiliated hospitals in lower Manhattan reported that 85 percent of the patients they received were “walking wounded” (Cushman et al., 2003). Beekman Hospital, a 170-bed facility 4 blocks from the disaster site, was overwhelmed with more than 500 patients in the first 24 hours, in addition to approximately 1,000 walk-ins seeking shelter from the dust (Pesola et al., 2002). This situation illustrates the challenge regarding overutilization of the most proximate hospitals in the event of a crisis.
In addition to direct transports from ground zero to area hospitals, ambulances were called upon to transport patients from overburdened local hospitals to other area hospitals with more available capacity. Following initial triage, patients were transported to other hospitals on the basis of their condition (e.g., burn victims, head trauma patients, and orthopedic patients). Because communications systems were disabled, however, ambulances had to transport the patients without advance communication with the destination hospitals (Pesola et al., 2002). As was the case with other first responders who participated in ground zero rescue efforts, EMS personnel struggled with faulty communications systems during the peak hours of the crisis.
Experience with the 1993 World Trade Center bombing provided some of the basis for New York City’s response to the attack of September 11. A review of that incident conducted by the U.S. Fire Administration concluded with a recommendation that hospital transport decisions be made on an incident-wide basis, rather than by individuals on a case-by-case basis (Fire
Engineering, 2004). However, the number of “self-referred” victims, as well as communications challenges, made this approach extremely problematic on September 11. The U.S. Fire Administration report also concluded that “the need for a medical incident command system cannot be overstated” and that both medical and fire operations required extensive management. The report suggested that “fire departments that have EMS responsibility should closely examine their medical management procedures to ensure their ability to manage both major elements simultaneously” (Fire Engineering, 2004).
In response to the attacks of September 11, the U.S. government initiated a massive restructuring of the federal bureaucracy by establishing DHS. This restructuring involved the consolidation of dozens of federal agencies involved in homeland security functions (The White House, 2002). Agencies such as the Transportation Security Administration, the Federal Emergency Management Agency (FEMA), the National Disaster Medical System (NDMS), the U.S. Coast Guard, and many others were consolidated under DHS. The development of this new department coincided with a significant increase in homeland security spending.
In addition, in February 2003 President Bush issued Homeland Security Presidential Directive (HSPD)-5, which directed the Secretary of Homeland Security to develop and administer the National Incident Management System (NIMS). NIMS, released in March 2004, was intended to establish a more coherent incident command structure to handle all potential hazards facing the United States. It represented a significant shift in the nation’s approach to incident management—from event- and discipline-specific incident response to an all-hazards, cooperative, multiagency approach (Walsh and Christen, 2005). In addition, the NIMS Integration Center (NIC) was established to provide strategic direction and oversight for NIMS. The NIC, which operates with FEMA as lead, aims to ensure that the all-hazards approach is an integral part of response training. It is also working to develop and facilitate national standards for NIMS education and training and to refine the system over time.
HSPD-5 also directed DHS to develop a National Response Plan (NRP) that builds on the basic framework provided by NIMS. Released in December 2004, the NRP represents “a concerted national effort to prevent terrorist attacks within the United States; reduce America’s vulnerability to terrorism, major disasters, and other emergencies; and minimize the damage and recover from attacks, major disasters, and other emergencies that occur” (DHS, 2004).
One central premise of the NRP is that incidents should be handled at the lowest possible jurisdictional level. However, incidents of national significance—such as situations in which the resources of state and local authorities have been overwhelmed and federal assistance has been request-
ed—would result in a full federal response. In such cases, federal actions would be taken in conjunction with state, local, tribal, nongovernmental, and private-sector entities (DHS, 2004).
The NRP identifies specific emergency support functions (ESFs) that are required in a crisis event. ESF-8 is the health and medical component of the plan, which is overseen by DHHS. ESF-8 identifies four major necessities for a medical response effort: (1) facilities in which to provide care (which may require building field hospitals since other facilities may have been damaged); (2) personnel to provide the care (which involves licensure issues for those coming from outside areas to help); (3) supplies and medications (including chronic care medications); and (4) the ability to move victims away from the impacted area (Alson, 2005). Disputes regarding the authority provided by ESF-8 hindered relief efforts during Hurricane Katrina (see below).
Hurricane Katrina
Hurricane Katrina was the first major disaster handled by FEMA after its relocation within DHS. The agency was severely criticized for its slow response to the crisis, and the director of relief operations at FEMA subsequently resigned from office. State and city managers also received a significant share of criticism. Local government officials were taken to task for having no effective incident command system in place to handle the crisis that ensued following the hurricane (Lindstrom and Losavio, 2005).
Although planners had anticipated that the city of New Orleans would be particularly vulnerable to a major hurricane, the magnitude of the crisis overwhelmed emergency responders and government officials at the federal, state, and local levels. Years prior to Katrina, FEMA had developed a disaster simulation, referred to as Hurricane Pam, illustrating the significant potential for damage from a major hurricane in New Orleans (CNN, 2005c; U.S. House of Representatives, 2006). However, this preparation did not result in an effective disaster operation. Instead, extreme chaos descended upon New Orleans, as well as some of the other affected areas in Louisiana, Mississippi, and Alabama.
A central criticism of the federal government was its failure to act proactively as weather reports indicated that a category 4 hurricane was headed for the Gulf Coast. The result was the loss of several critical days vital to the response effort and additional hardships for hurricane victims. In addition, while considerable federal resources were eventually brought to bear, these resources were not adequately coordinated, resulting in added confusion. Despite the tremendous organizational failures that occurred at each level of government, care providers on scene did the best they could to supply adequate care. The U.S. House of Representatives report on Katrina concluded
that “ultimately, public health and medical support services were effectively but inefficiently delivered” (U.S. House of Representatives, 2006).
FEMA was essentially created as a disaster recovery agency that could coordinate the efforts of various federal departments. Its focus historically was on logistics and recovery distribution. However, Hurricane Katrina presented a number of additional challenges, including major evacuations and search and rescue operations, as well as issues of health care delivery and public health. The NDMS, housed within FEMA, took a primary role in mobilizing medical care for hurricane victims. According to FEMA testimony, the agency’s Disaster Medical Assistance Teams (DMATs) treated over 100,000 patients during the crisis (Burris, 2005). The various disaster response teams within the NDMS are detailed in Box 6-2.
DMATs are medical units designed to complement state and local medical resources. They consist of approximately 35 individuals with a range of health care skills, as well as support personnel serving communications, logistics, and security functions. Fully operational DMATs have the ability
|
BOX 6-2 National Disaster Medical System (NDMS) Assets
SOURCE: FEMA, 2005. |
to triage and treat up to 250 patients per day for up to 3 days without resupply. DMAT team members are community-based volunteers and can be federalized upon the team’s activation. This provides the team members with licensure and certification anywhere in the federal domain and addresses liability and compensation issues (Mediccom.org, 2006). In addition, DMATs may be used by states for emergencies within their borders. Thus there is a need for close coordination between the federal government and the states when the teams are deployed. During Katrina, many DMAT teams were moved around the country multiple times without ever setting up operations and seeing patients. Teams that did set up had difficulty being resupplied or being integrated within the local health care system. These problems limited the effectiveness of the teams in responding to the crisis.
Along with FEMA, the NDMS was moved from DHHS to DHS in 2003. According to the U.S. House of Representatives report on Katrina, however, some DHHS officials believe their agency assumes functional jurisdiction over the NDMS in the event of a disaster, based on authority provided under ESF-8 (U.S. House of Representatives, 2006). This uncertainty regarding appropriate authority contributed to confusion during the Katrina crisis. Following a review of the events, the White House report on Katrina, released in 2006, recommended that the NDMS be moved from DHS back to DHHS (The White House, 2006). Also in 2006, a congressional committee proposed a major restructuring of FEMA to expand its responsibilities while keeping it within DHS (Lipton, 2006).
In Hancock County, Mississippi, identified as Katrina’s epicenter, a medical assistance team supported by HRSA Hospital Preparedness grants set up a 120-bed mobile hospital in the parking lot of a large shopping center. Beds, medical equipment, and provider training were made available through the HRSA grant program. As of early October 2005, the 450 medical personnel who staffed the unit on a rotating basis had treated 7,000 local residents (HRSA, 2005).
In addition to federal support, New Orleans and the other affected areas received assistance from states through the Emergency Management Assistance Compact (EMAC), an arrangement for interstate mutual aid that is managed by the National Emergency Management Association (NGA Center for Best Practices, 2005). Currently, 49 states participate in the arrangement. Through EMAC, states undergoing a disaster can immediately request assistance from other member states without the need for a federal disaster declaration. Issues related to licensure, liability, and reimbursement are resolved in advance. States that are prepared to provide assistance must wait for a formal request from a state in need. Including civilian personnel (19,481) and National Guard troops (48,477), Hurricanes Katrina and Rita resulted in the largest deployment of mutual aid through EMAC to date (Emergency Management Assistance Compact, 2005). The 2006 report of
the U.S. House of Representatives concluded that EMAC “successfully provided unprecedented levels of response and recovery personnel and assets to the Gulf coast in record time following Hurricane Katrina” (U.S. House of Representatives, 2006). However, the system also suffered from significant disorganization during the crisis. In many cases, physicians were brought in and never used, while in others, physicians were used but not provided with any relief.
One of the significant challenges presented by a disaster of Katrina’s magnitude is managing the flood of volunteers who arrive on scene wanting to provide help. Authorities are often unable to distinguish those who are qualified to provide care from who are unqualified but well intentioned. HRSA was charged by Congress with establishing a national system for identifying, authenticating, and credentialing responders under a program called Emergency Systems for Advance Registration of Volunteer Health Professionals (ESAR-VHP); however, this system had not been sufficiently developed to provide help during Hurricane Katrina.
During Katrina, air ambulance crews also played an important role, assisting in evacuating survivors from flooded areas. Overall, 27 civilian EMS helicopters were involved in evacuating Tulane Medical Center, Charity Hospital, and other facilities (Lindstrom and Losavio, 2005). In many cases, the helicopters used the roof of the hospital parking garage as a landing zone, and patients were brought upstairs to meet them. Despite these efforts, however, which took place largely without the aid of FEMA (U.S. House of Representatives, 2006), evacuations from these facilities were highly disorganized and agonizingly slow.
Patients who survived the evacuation were treated initially and then transported via buses and airplanes to hospitals in other cities for definitive care. However, this process also suffered from significant disorganization and delays. Many patients were evacuated to the airport but were left there for hours or days before being transported. Others were sent to distant cities with little or no information about where they were going or how they could find out about the location of their families. The NDMS did a poor job of allocating the patient load. Some cities, such as Houston and Atlanta, were inundated with patients, while others, such as Winston Salem, North Carolina, and Augusta, Georgia, received very few.
In Houston and Dallas, the Metropolitan Medical Response System (MMRS) was activated to coordinate the provision of shelter and medical care to evacuees. The MMRS was founded in 1996 by DHHS in response to the increased terrorist threat demonstrated by the Tokyo subway sarin attack in March 1995 and the Oklahoma City bombing in April 1995. The program was designed to enhance and coordinate local and regional response capabilities for highly populated areas that could be targeted by a terrorist attack using weapons of mass destruction. The MMRS concept
and resources can also be applied to the management of large-scale incidents such as accidents involving hazardous materials, epidemic disease outbreaks, and natural disasters requiring specialized and carefully coordinated medical preparation and response. The MMRS became part of the new DHS in 2003 (DHS, 2005).
Following Katrina, both the Dallas Convention Center and the Reunion Arena were transformed into makeshift shelters for evacuees. Medical teams established a field hospital in the basement of the Dallas Convention Center and triaged individuals as they exited buses arriving from New Orleans. This helped ease the burden on local trauma centers. However, hospitals receiving large numbers of NDMS evacuees likely were filled to capacity, causing crowding in hospital emergency rooms, ambulance diversions, and reductions in access to emergency and trauma care.
After the initial blow and immediate aftermath of Hurricane Katrina, emergency health workers increasingly shifted their focus to the treatment of chronic illnesses. Patients suffering from conditions such as congestive heart failure and asthma required treatment, and patients with diabetes needed glucose monitors, syringes, insulin, and other medications. Emergency response teams were unequipped for these needs in many cases (Lindstrom and Losavio, 2005). In addition to a lack of adequate supplies and medications, no system was in place to verify the prescriptions of these patients. Moreoever, acute health issues unrelated to the hurricane, such as heart attacks and high-risk pregnancies, had to be addressed as well as possible by the emergency workers on the ground.
Terrorist Bombings in London and Madrid
On July 7, 2005, three bombs were detonated nearly simultaneously in London’s Underground subway system. A short time later, a fourth bomb exploded on a double-decker bus at street level. Together, these explosions killed more than 50 people and injured more than 700.
In response to the September 11 terrorist attacks in the United States, London had planned for a possible mass casualty incident on its own soil, and EMS personnel had been trained accordingly. On the day of the bombings, emergency services set up a command structure and a triage area in the concourse of the rail station to determine the type of care required by each victim.
The London Ambulance Service (LAS) called for mutual aid from neighboring ambulance services and from voluntary agencies, which staged at previously agreed-upon locations. In total, more than 250 EMS personnel and 100 ambulances were mobilized to provide assistance (Hines et al., 2005). Altogether, LAS treated 45 patients for serious and critical injuries (e.g., burns, amputations, and chest and blast injuries) and approximately
300 patients for minor injuries (e.g., lacerations, smoke inhalation, and bruises). An additional 300 people went on their own to local London hospitals (Hines et al., 2005).
On March 11, 2004, Madrid experienced a similar but even more deadly terrorist attack. Ten bombs exploded nearly simultaneously in four commuter trains during rush hour, killing 191 people and injuring 2,000. Spain launched a massive emergency operation, mobilizing (according to government information) over 70,000 health personnel, 291 ambulances, 200 firemen, and 500 volunteers to assist in rescue and recovery operations and subsequent treatment (Gutierrez de Ceballos et al., 2004). According to one analysis, overtriage to the closest hospital was likely the largest problem with the rescue operations, making it more difficult to ensure that all patients were triaged appropriately.
Rhode Island Nightclub Fire
In February 2003, a fire erupted in a West Warwick, Rhode Island, nightclub when a band attempted to light pyrotechnics inside the club. The fire killed 100 people and injured more than 200 others. At the scene, two senior EMS officers provided triage. Victims were first assigned to one of two categories: dead or not dead. The fatalities were moved to a separate mass fatality management area. The remaining victims were brought by various means (e.g., walking or through the use of a backboard) to the primary triage site 100 feet from the nightclub. A captain scanned patients for signs of severe smoke inhalation and burns to the face, neck, torso, and upper extremities and directed the most critically injured to the next available EMS vehicle. Ambulances were lined up nearby, and pickups occurred in less than 5 minutes according to reports. Less critical patients were directed to a second triage area where another captain reassessed and retriaged them as necessary. EMS personnel reportedly transported 186 seriously injured persons from the incident site to 10 Rhode Island hospitals in less than 2 hours (CNN.com, 2003; Suburban Emergency Management Project, 2005).
Israeli Building Collapse
Israel frequently confronts mass casualty incidents, including suicide bombings and other incidents involving improvised explosive devices. One of its most serious recent mass casualty events occurred in May 2001 at a wedding celebration involving 700 participants, when the third floor of the wedding hall suddenly collapsed, causing 23 fatalities and 315 injuries (Avitzour et al., 2004).
In response to this disaster, more than 30 ambulances from the Jerusalem region were dispatched immediately to the scene, and additional units
from other regions were mobilized. Approximately 600 EMTs, 40 paramedics, and 15 physicians operating 97 basic life support (BLS) ambulances, 18 mobile intensive care vehicles, and 6 mobile first aid stations were mobilized. On site, the senior paramedic assumed command of all medical teams and established a triage and resuscitation center. Casualties were dispatched to hospitals after receiving immediate necessary life support on site. The distribution of casualties to hospitals was controlled by the medical commander on site and coordinated by the area dispatch center, given that citywide communications were still in operation. The ambulances had a turnover time of 30 minutes and evacuated 42 percent of the victims within the first hour and an additional 33 percent in the next hour. Avitzour and colleagues (2004) found that a unified medical command system facilitated rapid response on scene, full utilization of all medical resources, and early evacuation and triage of casualties to nearby hospitals. Because of the crowding caused at the scene, however, the authors concluded that the automatic dispatching of a large number of ambulances to the incident site was ill advised (Avitzour et al., 2004).
Additional Experience from the Iraq War
Experience from the Iraq war and previous conflicts has led to improvements in the delivery of health care services to wounded American soldiers. The U.S. military is now able to provide high levels of medical care to soldiers much more quickly than was possible in the past. Medical assets are closer to the front lines, and air medical capabilities have been improved (Miles, 2005). The U.S. Marine Corps and Navy introduced forward resuscitative surgery systems (FRSSs)—small, mobile trauma surgical teams of eight individuals (including two surgeons and support staff) designed to provide tactical surgical intervention for combat casualties in the forward area (Chambers et al., 2005). The units can erect a battlefield hospital with two operating tables and four ventilator-equipped beds in less than 1 hour (Gawande, 2004). New medical technologies, such as compact ultrasound and x-ray machines, generators that extract pure oxygen from the air, and computerized diagnostic equipment, have allowed the teams to provide fairly sophisticated care (Barnes et al., 2005). With these new surgical teams, the U.S. military’s strategy is to conduct damage control in the field (e.g., stopping bleeding and keeping patients warm), leaving definitive care to physicians at a hospital. Surgeons in the forward areas provide intermediate treatment, limiting surgery to 2 hours or less and sending the patient off to the next level of care.
Air medical evacuation procedures and equipment have improved to allow rapid transport of a critically injured solider. Because of those advances, the Air Force is transporting patients that never would have been
moved in previous wars (Miles, 2005). From the field surgery teams, patients are brought by helicopter to a larger combat support hospital in Iraq. Air medical evacuations are now lighter and more adaptable; patient support pallets can be moved from one aircraft to another, and medical teams carry much of their equipment in backpacks. If a soldier is critically wounded, a critical care air transport (CCAT) team joins the air medical evacuation to help transport the patient to a combat hospital in Iraq with additional equipment.
Lessons Learned
Experience gained from recent domestic and international incidents such as those described above demonstrates that many commonly held assumptions about disasters do not correspond to the research evidence (Auf der Heide, 2006). Typically, events unfolding in the aftermath of a disaster are likely to be much more chaotic than what is optimal from an emergency management standpoint. In disaster events, emergency response units from neighboring communities and states often self-dispatch, which can overwhelm the ability of local managers to process them; casualties at the scene of the disaster are likely to self-triage and self-transport; and nearby hospitals are likely to be overwhelmed with patients arriving at their doors (see Table 6-2). Although emergency responders play an essential role in caring for victims at the scene of a disaster, previous experience shows that the overall response is likely to be more disorganized than planners would hope.
IMPROVING EMS-RELATED DISASTER PREPAREDNESS IN THE UNITED STATES
The array of threats facing the United States is substantial. Existing dangers, such as natural calamities and the potential for disease outbreaks, are now compounded by the threat of terrorism. Many disaster scenarios involve the disruption or destruction of local emergency care assets and institutions and the need for immediate help from outside the affected area. Other scenarios involve broader threats that potentially could challenge emergency systems throughout the country.
Since September 11, considerable resources have been devoted to preparing for large-scale disasters. Homeland security spending, which is estimated to have been below $10 billion in the mid-1990s, rose to nearly $50 billion subsequent to September 11 and the establishment of DHS in 2002 (see Figure 6-1). These homeland security funds were directed to a number of different areas, including border security, aviation security, and bioterrorism. However, very little funding has been directed to strengthen-
TABLE 6-2 Commonly Held Misconceptions About Disasters
|
Assumption |
Research Observation |
|
Dispatchers will hear of the disaster and send response units to the scene. |
Emergency response units, both local and distant, will often self-dispatch. |
|
Trained emergency personnel will carry out field search and rescue. |
Most initial search and rescue is carried out by the survivors themselves. |
|
Trained EMS personnel will carry out triage, provide first aid or stabilizing medical care, and decontaminate casualties before patient transport. |
Casualties are likely to bypass on-site triage, first-aid, and decontamination stations and go directly to hospitals. |
|
Casualties will be transported to hospitals by ambulance. |
Most casualties are not transported by ambulance. They arrive by private car, police vehicle, bus, taxi, on foot, etc. |
|
Casualties will be transported to hospitals appropriate to their needs, and no hospital will receive a disproportionate share. |
Most casualties are transported to the closest or most familiar hospitals. |
|
Authorities in the field will ensure that area hospitals are promptly notified of the disaster and the numbers, types, and severities of casualties they will receive. |
Hospitals may be notified by the first arriving victims or the news media rather than authorities in the field. Often, information and updates about incoming casualties are insufficient or lacking. |
|
The most serious casualties will be the first to be transported to hospitals. |
The least serious casualties often arrive first. |
|
SOURCE: Auf der Heide, 2006. |
|
ing the nation’s trauma care system or its capacity to respond to terrorism involving conventional weapons. In fiscal year 2003, just 9 percent of homeland security spending was directed to first responders, including fire, police, and EMS (see Figure 6-2). Programs through which EMS providers received preparedness funding included the Urban Area Security Initiative Grant, Assistance to Firefighters Grant, and Homeland Security Grant programs. (The issue of funding for EMS in disaster planning is discussed further below.)
In some limited respects, the nation may be better prepared for disasters now than it was in the past (e.g., in the case of aviation security). However, these gains have been extremely uneven. For example, federal disaster planning has focused much more on biological and chemical threats than on explosive attacks by terrorists. And prior to Hurricane Katrina, much more attention had been focused on terrorism than on natural disasters (Arkin, 2005; Kellermann, 2005). Of the 15 national planning scenarios introduced
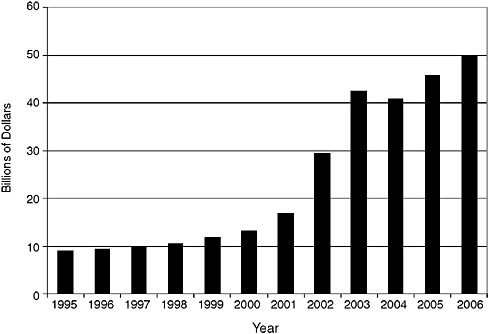
FIGURE 6-1 Trend in homeland security spending, fiscal years 1995 through 2006.
SOURCE: Reprinted, with permission, from de Rugy, 2005.
by DHS to guide disaster preparation efforts, only two involve natural disasters and only one attack uses explosives (see Box 6-3).
Following Hurricane Katrina, DHS did alter the selection criteria for its Urban Area Security Initiatives grants to ensure that the program would give as much weight to cities under threat from natural disasters as those that are likely targets of terrorism (Jordan, 2006). This shift reflected an effort on the part of the Secretary of Homeland Security to increase the emphasis on the department’s all-hazards mission.
Local Capacity and Day-to-Day Readiness
The challenges facing the federal government in improving preparedness are matched by those facing local communities that provide the immediate response to disaster events. In the field of emergency management, it is axiomatic that all response is local and that state and federal governments assist only as needed. However, local emergency and trauma care systems across the country face sizable day-to-day challenges, even without the additional responsibilities that might be placed upon them in the event of a
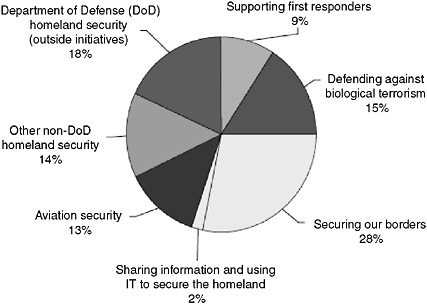
FIGURE 6-2 Distribution of homeland security funding in fiscal year 2003 request by activity.
NOTE: IT = information technology.
SOURCE: The White House, 2003.
major crisis. As described earlier, ED crowding is common in most cities and ambulance diversions occur regularly, even under normal operating conditions (GAO, 2003a). In terms of physical capacity, EMS, hospital EDs, and trauma centers in most cities have limited or no surge capacity, especially for pediatric and critical patients. Even multivehicle highway crashes can stretch local systems to their limit. The committee maintains that to be adequately prepared for disaster events, it is necessary first to establish strong and highly efficient emergency and trauma care systems that work smoothly on a day-to-day basis.
In addition, local systems should be prepared and equipped for specific potential disaster events. The training and equipment and emergency planning currently under way in most areas are inadequate. Few EMS personnel have any training or experience in assessing the scene of a terrorist bombing or evaluating casualties for a range of potential injuries. A serious natural or man-made biological threat—one that required sophisticated surveillance, highly coordinated communications and planning, decontamination, negative pressure suites, and staff equipped and trained in the use of personal protective equipment—would seriously challenge even the most well-
|
BOX 6-3 The Department of Homeland Security’s 15 National Planning Scenarios
SOURCE: Homeland Security Council, 2004. |
prepared community today. Given the enormous deficiencies in preparation for disasters in communities throughout the United States, the committee maintains that DHS and other agencies should enhance the equipment, training, and surge capacity of local emergency and trauma care systems in order to prepare for both day-to-day spikes in demand and mass-casualty disaster events. Mass-casualty preparations should heavily emphasize the most likely disaster scenarios.
Recognizing EMS as an Equal Partner in Disaster Planning and Funding
EMS and trauma systems have to a large extent been overlooked in disaster preparedness planning at both the state and federal levels (NASEMSD, 2003). This is due in part to the fact that EMS is often regarded as a subset of fire response, though the medical role that would be undertaken by EMS personnel in the event of a major emergency is distinct from the role of fire suppression teams (Fire Engineering, 2004). Given the specific homeland security threats that confront the United States, most of which have a heavy medical component, the committee recommends that
the Department of Health and Human Services, the Department of Transportation, the Department of Homeland Security, and the states elevate emergency and trauma care to a position of parity with other public safety entities in disaster planning and operations (6.1). These care providers represent a critical component of the broader, multiagency response to a major crisis, whether a natural disaster, terrorist incident, or other public health emergency, and should be included in all preparedness activities.
The fact that EMS has not been adequately included in disaster preparations is evidenced by the small share of disaster-related funding received by EMS from the federal government since September 11. Although they represent a third of the nation’s first responders, EMS providers received only 4 percent of the $3.38 billion distributed for emergency preparedness by DHS in 2002 and 2003 (see Figure 6-3). Similarly, EMS received only 5 percent of the Bioterrorism Hospital Preparedness Grant, a program administered by DHHS (Center for Catastrophe Preparedness and Response NYU, 2005). To date, the vast majority of these federal resources have been directed at law enforcement, fire response, hospitals, and public health systems. Few resources have been directed at EMS except through these means (NASEMSD, 2004).
The final version of the fiscal year 2006 Homeland Security Appropriations report included language calling for greater recognition of EMS
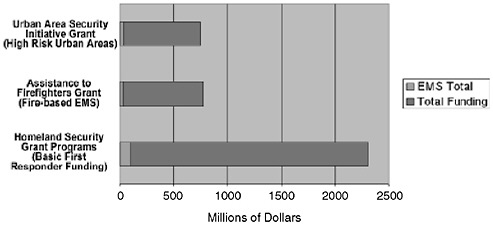
FIGURE 6-3 EMS receives only 4 percent of first responder funding.
SOURCE: Reprinted, with permission, from the Center for Catastrophe Preparedness and Response. 2005. Emergency Medical Services: The Forgotten First Responder—A Report on the Critical Gaps in Organization and Deficits in Resources for America’s Medical First Responders. New York, NY: Center for Catastrophe Preparedness and Response, New York University.
in homeland security funding distributions. The report stated that “the conferees are very concerned with the lack of first responder grant funding being provided to the Emergency Medical Services (EMS) community.” The conferees directed DHS’s Office of Domestic Preparedness (ODP) to require state and local governments to include EMS representatives in planning committees as an equal partner and to facilitate a nationwide needs assessment. While the conferees did not mandate that a specific percentage of grant funds be allocated to each type of first responder, they directed ODP to evaluate how much money goes to EMS. The conferees also inserted a requirement that a state provide an explanation if it does not award at least 10 percent of its grant funding to EMS providers to enhance training and equipment (Advocates for EMS, 2006).
While significant federal funds are available to states and localities for disaster preparedness, emergency care in general has not been able to secure a meaningful share of these funds because they have been folded into other pubic safety functions in which emergency medical care is considered a low priority. To address the serious deficits in health-related disaster preparedness, the committee recommends that Congress substantially increase funding for emergency medical services–related disaster preparedness through dedicated funding streams (6.2). These funding streams could be directed through the states to regional systems and localities based on priorities established through the regional planning process, thus ensuring that resources would be allocated according to the real needs identified by communities.
In budgeting for disaster preparedness, the committee believes it critical to separate medical functions from other public safety functions by establishing them as a separate line item. Without this separation, politics and culture will always pose a threat to the commitment to the medical component.
Finally, changes in the disaster preparedness grant process should also be considered. A 2003 survey conducted by the National Association of State EMS Directors (NASEMSD) found that its membership believed the federal grant process needs to be simplified and state EMS offices to have more support and involvement in the process. In addition, NASEMSD advocated the identification of specific funding streams for EMS, including non-fire-related EMS (NASEMSD, 2004).
Equipment, Education, and Training
One consistent challenge for disaster responders is communication and information management. Effective response requires the transmission of real-time information to assess needs and available resources, which can change suddenly and unexpectedly (Chan et al., 2004). On September 11,
communications failures led to chaos and confusion, and by one estimate resulted in more problems than all other factors combined (Simon and Teperman, 2001; Martinez and Gonzalez, 2001). The U.S. House of Representatives report on Hurricane Katrina likewise concluded that destruction of communications capability hindered command and control and severely limited situational awareness. The report concluded that “one of the most common and pervasive themes in the response to Hurricane Katrina has been a systematic failure of communications at the local, state, and federal levels” (U.S. House of Representatives, 2006).
Current disaster preparedness efforts have focused on creating interoperable communications systems among first responders, which is an urgent priority for EMS providers. This type of system will be essential in avoiding a repeat of the experience of September 11, as well as other disaster events in which communications links have been a central problem. However, the systems now being developed are primarily public safety communications networks; they are not designed to meet medical communication needs. The committee recommends that a greater focus be placed on developing an effective interoperable medical communications system that works efficiently on a day-to-day basis and can be employed in the event of a major disaster. In addition to voice communications systems, DHS could contribute to emergency preparedness by providing financial support for improving the nation’s health information technology infrastructure.
The International Association of Fire Chiefs, the International Association of Chiefs of Police, and the National League of Cities have pointed to congested radio communications systems as a key problem and have advocated a consumer transition to digital television to free up additional spectrum for public safety agencies. They have called for the creation of a single command and control center that would coordinate federal, state, and local officials in times of emergency. However, these recommendations are focused on public safety emergencies that are distinct from the provision of health care, including the transmission of medical data.
In addition to the central challenge of ensuring effective communications, providers currently lack appropriate equipment for specific disaster events, such as chemical and biological attacks. The use of personal protective equipment (PPE) is one method of protecting providers from biological or chemical hazards, but very few emergency medical professionals have been provided with such equipment or trained in its proper use. As mentioned above, in 25 states fewer than 50 percent of EMTs and paramedics have reported having adequate equipment to respond to these types of attacks. Only 1 state has reported that adequate personal protective equipment would be immediately available for all EMS personnel statewide in the event of a biological or chemical event (Center for Catastrophe Preparedness and Response NYU, 2005). These deficiencies must be addressed to prevent
emergency responders from becoming victims themselves and to enable a meaningful response in the event of a major terrorist attack.
Ultimately, disasters are characterized by many people trying to do quickly what they do not ordinarily do, in an environment with which they are not familiar (Chan et al., 2004). Regardless of the quality of disaster plans, efforts will be ineffective if personnel are not well trained in executing them. Currently, the lack of this type of training is a serious deficiency of the national disaster preparedness effort. Most hospitals have disaster plans, but providers have not been adequately instructed in how to execute those plans. Disaster training has been equally deficient among EMS professionals, as evidenced by the following facts:
-
During the past year, fewer than 33 percent of EMTs and paramedics have participated in a drill simulating a radiological, biological, or chemical attack.
-
Fire department EMTs and paramedics have received an average of 4.5 hours of training in homeland security and disaster management since September 11, 2001. EMTs and paramedics not affiliated with fire departments have received an average of less than 1 hour of such training.
-
EMTs and paramedics in urban areas have received less than 3.5 hours of training in homeland security and disaster management since September 11 (Center for Catastrophe Preparedness and Response NYU, 2005).
Moreover, in rural areas, training for more commonly occurring disasters (including weather-related incidents and unintentional man-made disasters) has declined over the past few years in favor of terrorism preparedness (Furbee et al., in press). These findings indicate that U.S. EMS personnel are not well prepared to handle a catastrophic emergency such as a major earthquake, bioterrorist attack, or pandemic influenza outbreak. Adequate funding directed specifically to emergency medical personnel is required to address this deficiency.
Establishing effective training in disaster preparedness for EMS personnel will require a coordinated and well-funded national effort that involves both professional and continuing education. The committee therefore recommends that professional training, continuing education, and credentialing and certification programs for all the relevant professional categories of emergency medical services personnel incorporate disaster preparedness into their curricula and require the maintenance of competency in these skills (6.3). These changes would ensure that emergency personnel would remain up to date on essential disaster skills and would bolster preparedness efforts.
Finally, state and federal response to a national disaster is hindered by inconsistent standards for the licensure of all emergency care providers and a lack of adequate reciprocity agreements between states. For example, state EMS scope of practice and professional licensure standards, designations, and educational requirements vary widely (Center for Catastrophe Preparedness and Response NYU, 2005). To facilitate improved response to a disaster, each state should adopt consistent standards for the licensure of all emergency care providers and enter into reciprocity agreements with all other states. The adoption by states of the National EMS Scope of Practice Model, a component of NHTSA’s Emergency Medical Services Education Agenda for the Future, would be a major step in this direction (see Chapter 4). This would enable state and federal agencies to quickly identify and deploy EMS personnel, physicians, nurses, and other critical professionals across state lines in the event of a major disaster.
Coordination of Government Disaster Response
Hurricane Katrina illustrated the breakdowns that can occur among local, state, and federal governments in a time of crisis. Critical delays in bringing relief supplies to stranded New Orleans residents, an extremely faulty incident command structure, and a breakdown in law and order resulted in the exchange of blame among officials involved at each level of government. Criticisms often centered on how and when requests for help were made by local officials and why help did not arrive sooner. These conflicts demonstrate the challenge of delineating the roles and responsibilities of each level of government given the right of local self-determination and the need to ensure that sufficient resources are brought to bear in the event of a major catastrophe.
In the aftermath of Hurricane Katrina, the federal government moved to assert more control over future disaster situations, proposing greater utilization of the U.S. military and other federal resources (NEMA, 2005). In October 2005, however, the National Governors Association (NGA) responded with a position statement calling for continued respect for the central role of the state. NGA stated that “following the tragedies inflicted on the citizens of the gulf coast by hurricanes Katrina and Rita, local, state and federal government must examine the way the three levels of government communicate and coordinate their response. The possibility of the federal government pre-empting the authority of states or governors in emergencies, however, is opposed by the nation’s governors.” NGA indicated that “governors are responsible for the safety and welfare of their citizens and are in the best position to coordinate all resources to prepare for, respond to and recover from disasters.” At the same time, NGA acknowledged that
federal aid and assistance are sometimes necessary, and said that a dialogue between state and federal officials about how best to achieve these goals should continue (NGA Center for Best Practices, 2005).
Managing large-scale disasters continues to be a challenge for officials at each level of government. The responses to September 11 and Hurricane Katrina demonstrate that there is a significant gap between the dangers that now present themselves and the nation’s readiness to address them effectively. From the EMS perspective, significant deficiencies in education, training, and equipment reflect a lack of funding directed to preparing for the emergency medical component of likely disaster events. These deficiencies will need to be addressed if the nation is to be well prepared for the next major disaster.
SUMMARY OF RECOMMENDATIONS
6.1: The Department of Health and Human Services, the Department of Transportation, the Department of Homeland Security, and the states should elevate emergency and trauma care to a position of parity with other public safety entities in disaster planning and operations.
6.2: Congress should substantially increase funding for emergency medical services–related disaster preparedness through dedicated funding streams.
6.3: Professional training, continuing education, and credentialing and certification programs for all the relevant professional categories of emergency medical services personnel should incorporate disaster preparedness into their curricula and require the maintenance of competency in these skills.
REFERENCES
AAA (American Ambulance Association). 2004. AAA Terrorism Preparedness Survey. [Online]. Available: http://64.233.161.104/search?q=cache:yCdVtVqLUTIJ:www.the-aaa.org/Members_Only/Oncapitolhill/4%2520Summary%2520AAA%2520Terrorism%2520Prep%2520Survey.doc+AAA+Terrorism+Preparedness+Survey&hl=en&gl=us&ct=clnk&cd=1 [accessed May 2, 2006].
Accountability Review Boards on the Embassy Bombings in Nairobi and Dar es Salaam. 1999. Report of the Accountability Review Boards on the Embassy Bombings in Nairobi and Dar es Salaam on August 7, 1998. Washington, DC.
Advocates for EMS. 2006. Language Included in the Final FY 2006 Homeland Security Appropriations Report. [Online]. Available: http://www.advocatesforems.org/Library/upload/EMS_HS_conference_ report_language.pdf [accessed May 25, 2006].
Alson RL. 2005. Medical Response to Catastrophic Events. Statement at the October 20, 2005, Hearing of the Subcommittee on Subcommittee on Prevention of Nuclear and Biological Attack, Committee on Committee on House Homeland Security, Washington, DC.
Arkin WM. 2005. Michael Brown Was Set Up: It’s All in the Numbers. [Online]. Available: http://blogs.washingtonpost.com/earlywarning/2005/09/michael_brown_w.html [accessed November 1, 2005].
Arnold JL, Halpern P, Tsai MC, Smithline H. 2004. Mass casualty terrorist bombings: A comparison of outcomes by bombing type. Annals of Emergency Medicine 43(2):263–273.
Associated Press. 2006a. Four Bodies Found Since Dec. 21; Katrina Death Toll Now 1,326. [Online]. Available: http://www.katc.com/global/story.asp?s=4317545&ClientType=Printable [accessed May 1, 2006].
Associated Press. 2006b. Band Ex-Manager Sentenced to Four Years in R.I. Club Fire Case. [Online]. Available: http://www.usatoday.com/news/nation/2006-05-09-fire-hearing_x.htm [accessed May 11, 2006].
Auf der Heide E. 2006. The importance of evidence-based disaster planning. Annals of Emergency Medicine 47(1):34–49.
Augustine J, Kellermann A, Koplan J. 2004. America’s emergency care system and severe acute respiratory syndrome: Are we ready? Annals of Emergency Medicine 43(1):23–26.
Avitzour M, Libergal M, Assaf J, Adler J, Beyth S, Mosheiff R, Rubin A, Feigenberg Z, Slatnikovitz R, Gofin R, Shapira SC. 2004. A multicasualty event: Out-of-hospital and in-hospital organizational aspects. Academic Emergency Medicine 11(10):1102–1104.
Barnes J, Roane K, Szegedy-Maszak M. 2005, April. 5. Stemming the fatalities with a modern touch. Sydney Morning Herald. [Online]. Available: http://www.smh.com.au/articles/2003/04/04/1048962935279.html?oneclick=true [accessed January 29, 2007].
BBC News. 2005. Sarin Attack Remembered in Tokyo. [Online]. Available: http://news.bbc.co.uk/2/hi/asia-pacific/4365417.stm [accessed May 1, 2006].
BBC News. 2006a. Bali Death Toll Set at 202. [Online]. Available: http://news.bbc.co.uk/1/hi/in_depth/asia_pacific/2002/bali/default.stm [accessed May 1, 2006].
BBC News. 2006b. Q&A: Bird Flu. [Online]. Available: http://news.bbc.co.uk/2/hi/health/3422839.stm [accessed May 1, 2006].
Bravata DM, McDonald K, Owens DK. 2004. Regionalization of Bioterrorism Preparedness and Response. [Online]. Available: http://www.ahrq.gov/clinic/epcsums/bioregsum.pdf [accessed May 25, 2006].
Burris K. 2005. Legislative Proposals in Response to Hurricane Katrina. Statement at the October 3, 2005, Hearing of the Subcommittee on Economic Development, Public Buildings and Emergency Management, Committee on House Transportation and Infrastructure, Washington, DC.
CDC (Centers for Disease Control and Prevention). 2004. Smallpox Fact Sheet. [Online]. Available: http://www.bt.cdc.gov/agent/smallpox/overview/disease-facts.asp [accessed January 29, 2007].
CDC. 2006a. Emergency Preparedness and Response: Agents, Disease, & Other Threats. [Online]. Available: http://www.bt.cdc.gov [accessed February 1, 2006].
CDC. 2006b. Emergency Preparedness & Response: Training, Centers for Public Health Preparedness (CPHP) Program. [Online]. Available: http://www.bt.cdc.gov/training/cphp/ [accessed February 1, 2006].
Center for Catastrophe Preparedness and Response NYU. 2005. Emergency Medical Services: The Forgotten First Responder—A Report on the Critical Gaps in Organization and Deficits in Resources for America’s Medical First Responders. New York: Center for Catastrophe Preparedness and Response, New York University.
Chambers LW, Rhee P, Baker BC, Perciballi J, Cubano M, Compeggie M, Nace M, Bohman HR. 2005. Initial experience of US Marine Corps forward resuscitative surgical system during Operation Iraqi Freedom. Archives of Surgery 140(1):26–32.
Chan TC, Killeen J, Griswold W, Lenert L. 2004. Information technology and emergency medical care during disasters. Academic Emergency Medicine 11(11):1229–1236.
CNN.com. 2003. At Least 96 Killed in Nightclub Inferno, Governor: DNA Might Be Only Clue to Identity of Some Victims. [Online]. Available: http://www.cnn.com/2003/US/Northeast/02/21/deadly.nightclub.fire [accessed May 1, 2006].
CNN.com. 2005a. Tsunami Deaths Soar Past 212,000. [Online]. Available: http://www.cnn.com/2005/WORLD/asiapcf/01/19/asia.tsunami [accessed May 1, 2005].
CNN.com. 2005b. Four Sought in Attempted Attacks: Police Say Man Shot and Killed in Underground Not One of Four. [Online]. Available: http://www.cnn.com/2005/WORLD/europe/07/22/london.tube/index.html [accessed May 1, 2006].
CNN.com. 2005c. Chertoff: Katrina Scenario Did Not Exist. [Online]. Available: http://www.cnn.com/2005/US/09/03/katrina.chertoff [accessed January 7, 2006].
Cushman JG, Pachter HL, Beaton HL. 2003. Two New York city hospitals’ surgical response to the September 11, 2001, terrorist attack in New York City. Journal of Trauma-Injury Infection & Critical Care 54(1):147–154; discussion 154–155.
de Rugy V. 2005. What Does Homeland Security Spending Buy? Washington, DC: American Enterprise Institute for Public Policy Research.
DHS (U.S. Department of Homeland Security). 2003. Homeland Security Information Bulletin: Chemical, Biological, Radiological and Nuclear (CBRN) Materials and Effects. [Online]. Available: http://www.iwar.org.uk/homesec/resources/dhs-bulletin/cbrn.htm [accessed May 25, 2006].
DHS. 2004. National Response Plan. [Online]. Available: http://www.dhs.gov/interweb/assetlibrary/NRP_FullText.pdf [accessed March 2, 2006].
DHS. 2005. Metropolitan Medical Response System (MMRS) the First Decade (1995–2005). [Online]. Available: http://mmrs.fema.gov/press/2005/pr2005-07-05.aspx [accessed February 10, 2006].
DHS READYAmerica. 2005. Be Informed: Natural Disasters. [Online]. Available: http://www.ready.gov/america/natural_disasters.html [accessed January 15, 2006].
Emergency Management Assistance Compact. 2005. EMAC Home Page. [Online]. Available: http://www.emacweb.org [accessed January 7, 2006].
Fee E, Parry M. 2005. Dangerous illusions: Cautionary tales in the history of medicine. Health Affairs 24(4):1178–1179.
FEMA (Federal Emergency Management Agency). 2005. FEMA News: FEMA Disaster Medical Assistance Teams Hard at Work; Federal Teams Have Treated More Than 100,000 Patients. [Online]. Available: http://www.fema.gov/news/newsrelease.fema?id=19304 [accessed November 1, 2005].
Fire Engineering. 2004. The World Trade Center Bombing: Report and Analysis. Emmitsburg, MD: Federal Emergency Management Agency/U.S. Fire Administration National Fire Data Center.
Furbee PM, Coben JH, Smyth SK, Manley WG, Summers DE, Sanddal ND, Sanddal TL, Helmkamp JC, Kimble RL, Althouse RC, Kocsis AT. In press. Realities of rural emergency medical services disaster preparedness. Prehospital and Disaster Medicine 21.
GAO (U.S. Government Accountability Office). 2003a. Hospital Emergency Departments: Crowded Conditions Vary among Hospitals and Communities. Washington, DC: GAO.
GAO. 2003b. Hospital Preparedness: Most Urban Hospitals Have Emergency Plans but Lack Certain Capacities for Bioterrorism Response. Washington, DC: GAO.
GAO. 2005. Hurricane Katrina: Providing Oversight of the Nation’s Preparedness, Response, and Recovery Activities. [Online]. Available: http://www.gao.gov/new.items/d051053t.pdf [accessed March 29, 2006].
Gawande A. 2004. Casualties of war––military care for the wounded from Iraq and Afghanistan. New England Journal of Medicine 351(24):2471–2475.
Gutierrez de Ceballos JP, Turegano-Fuentes F, Perez–Diaz D, Sanz-Sanchez M, Martin-Llorente C, Guerrero-Sanz JE. 2004. 11 March 2004: The terrorist bomb explosions in Madrid, Spain: An analysis of the logistics, injuries sustained and clinical management of casualties treated at the closest hospital. Critical Care 8.
Hall M. 2005, March 10. Report: EMS lacks terrorism training, equipment. USA Today. Nation.
Henning KJ. 2003. Syndromic surveillance. In: Microbial Threats to Health: Emergence, Detection, and Response. Washington, DC: The National Academies Press.
Hines S, Payne A, Edmondson J, Heightman AJ. 2005. Bombs under London: The EMS response plan that worked. Journal of Emergency Medical Services 23(8).
Hirschkorn P. 2003. New York Reduces 9/11 Death Toll by 40. [Online]. Available: http://www.cnn.com/2003/US/Northeast/10/29/wtc.deaths [accessed May 1, 2006].
Homeland Security Council. 2004. Planning Scenarios: Executive Summaries. [Online]. Available: http://www.globalsecurity.org/security/library/report/2004/hsc-planning-scenarios-jul04_exec-sum.pdf [accessed May 1, 2006].
Horwitz S, Davenport C. 2005, September 11. Terrorism could hurl D.C. area into turmoil: Despite efforts since 9/11, response plans incomplete. The Washington Post. P. A01.
HRSA. 2005. HRSA Hospital Preparedness Grantee in N.C. Takes Mobile Hospital, Staff to Miss. to Help Hurricane Victims. [Online]. Available: http://www.hrsa.gov/katrina/updatehrsa1011/htm [accessed January 7, 2006].
Insurance Information Network of California. 2006. Earthquakes. [Online]. Available: http://iinc.org/pdf/EQ percent20Kit percent20final.updated.pdf [accessed May 1, 2006].
IOM (Institute of Medicine). 2004. Learning from SARS: Preparing for the Next Disease Outbreak. Workshop Summary. Washington, DC: The National Academies Press.
IOM. 2005. The Threat of Pandemic Influenza: Are We Ready? Workshop Summary. Washington, DC: The National Academies Press.
IOM, NRC (Institute of Medicine, National Research Council). 2006. Globalization, Biosecurity, and the Future of the Life Sciences. Washington, DC: The National Academies Press.
Jordan LJ. 2006, January 2. Homeland security to re-prioritize grants. Washington Dateline.
Kellermann A. 2005, August 5. Still not ready in the ER. The Washington Post. P. A15.
Lindstrom A-M, Losavio K. 2005. Chaos of Katrina: EMS maintains composure in the midst of anarchy. Journal of Emergency Medical Services 23(11).
Lipton, E. 2006, April 27. Senate panel urges FEMA dismantling. The New York Times. P. A22.
Martinez C, Gonzalez D. 2001. The World Trade Center attack. Doctors in the fire and police services. Critical Care 5(6):304–306.
Mediccom.org. 2006. The NDMS Disaster Medical Assistance Teams. [Online]. Available: http://mediccom.org/public/tadmat/ndms/dmat.html [accessed January 7, 2006].
Miles D. 2005, August 10. Aeromedical evacuation improvements saving lives. DefenseLink News. [Online]. Available: http://www.defenselink.mil/news/Aug2005/20050810_2386.html [accessed January 30, 2007].
NASEMSD (National Association of State EMS Directors). 2003. Linkages of Acute Care and EMS with State and Local Prevention Programs, Part 3: Status of State EMS System Funding. Falls Church, VA: NASEMSD.
NASEMSD. 2004. NASEMSD Survey: Identification of Obstacles to EMS Terrorism Preparedness. Falls Church, VA: NASEMSD.
NEMA (National Emergency Management Association). 2005. NEMA Policy Position on the Role of the Military in Disaster Response. Lexington, KY: NEMA.
NGA Center for Best Practices. 2005. Beyond EMAC: Legal Issues in Mutual Aid Agreements for Public Health Practice. Issue Brief, Washington, DC.
Noji EK. 1996. Disaster epidemiology. Emergency Medical Clinics of North America 14(2):289–300.
Pesola GR, Dujar A, Wilson S. 2002. Emergency preparedness: The World Trade Center and Singapore airline disasters. Academic Emergency Medicine 9(3):220–222.
Rand Corporation. 2004. Rand Study Shows Compensation for 9/11 Terror Attacks Tops $38 Billion; Businesses Receive Biggest Share. [Online]. Available: http://www.rand.org/news/press.04/11.08b.html [accessed May 1, 2006].
Rudman WB, Clarke RA, Metzl JF. 2003. Emergency Responders: Drastically Underfunded, Dangerously Unprepared. New York, NY: Council on Foreign Relations.
Schur CL, Berk ML, Mueller CD. 2004. Perspectives of Rural Hospitals on Bioterrorism Preparedness Planning. Bethesda, MD: NORC Walsh Center for Rural Health Analysis.
Simon R, Teperman S. 2001. The World Trade Center attack. Lessons for disaster management. Critical Care (London) 5(6):318–320.
Suburban Emergency Management Project. 2005. SEMP Biot #250: What Is “Graceful Degradation”? [Online]. Available: http://www.semp.us/biots/biot_250.html [accessed February 1, 2006].
Times Foundation. 2005. Kashmir Earthquake—A Situation Report. India: The Times Group.
U.S. House of Representatives. 2006. A Failure of Initiative: Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina. Washington, DC: Government Printing Office.
Waeckerle JF. 2000. Domestic preparedness for events involving weapons of mass destruction. Journal of the American Medical Association 283(2):252–254.
Waeckerle J, Lillibridge S, Burkle F, Noji E. 1994. Disaster medicine: Challenges for today. Annals of Emergency Medicine 23(4):715–718.
Walsh DW, Christen H. 2005. The National Incident Management System fully interfaces EMS operations in disaster and MCI responses. Journal of Emergency Medical Services 23(4).
The White House. 2003. Securing the Homeland, Strengthening the Nation. [Online]. Available: http://www.whitehouse.gov/homeland/homeland_security_book.pdf [accessed May 25, 2006].
The White House. 2006. Federal Response to Hurricane Katrina: Lessons Learned. [Online]. Available: http://www.whitehouse.gov/reports/katrina-lessons-learned.pdf [accessed May 25, 2006].
































