9
Ethical Considerations in Living Donation
The demand for solid organs far exceeds the number of organs available from deceased donors. Not surprisingly, instead of facing years on the transplantation waiting list, some patients, often with the encouragement of transplantation teams, seek to identify relatives or others who would be willing to donate the needed organ or partial organ directly or, in some cases, through a donor exchange program. Still other donors offer a kidney or a partial organ to patients whose stories have become known to them, perhaps through the media, whereas still others make a nondirected donation of a kidney to the transplantation system for use by any patient who needs it.
Organ donation by living donors clearly saves lives, improves transplantation outcomes under some circumstances, and reduces recipients’ waiting times. It also increases opportunities for patients without living donors to receive organs from deceased donors. However, it raises a series of ethical questions that have not been fully addressed.
The transplantation of organs from living donors seems to violate the traditional first rule of medicine—primum non nocere (above all, do no harm)—because it involves the removal of a healthy organ from one person for implantation into another person. One person becomes a patient to benefit another person who is already a patient. In a survey of 100 liver transplant surgeons, Cotler and colleagues (2003) found that 77 percent experienced a moral dilemma in placing a living donor at risk. Nevertheless, 72 percent also agreed that transplant centers had a duty to offer their patients the possibility of transplantation using living donors.
Because the committee’s mandate calls for primary attention to ways to increase the rates of organ donation from deceased donors, this report will not provide a detailed discussion of the scientific, clinical, and ethical issues involved in organ donation by living donors. However, the committee believes that it is important that living donation be the subject of intense discussion and study. This chapter can do little more than flag a number of issues and concerns that warrant further attention.
The committee believes that it would be appropriate for the Health Resources and Services Administration (HRSA), perhaps in conjunction with other organizations, to establish an appropriate mechanism to conduct this full and long overdue review, a portion of which has been undertaken by the U.S. Department of Health and Human Services (DHHS) Advisory Committee on Transplantation (ACOT). Nevertheless, even before a full review is conducted, the committee finds warrant for two recommendations to increase and improve the available data and to protect donors’ rights and welfare (see Summary and Recommendations below).
This chapter begins with an overview of the statistics regarding living donation followed by a discussion highlighting a number of the ethical issues. The chapter concludes by focusing on the need for further examination of this issue and on the committee’s recommendations to provide independent donor advocate teams and to follow up on the health of living donors.
BACKGROUND
The first successful organ transplantations involved living donors. In 1954, surgeons at Peter Brent Brigham Hospital in Boston removed a kidney from a young man and implanted it in his identical twin brother (Merrill et al., 1956). Through the 1960s developments in transplantation technology enabled kidney transplantation to evolve into a viable alternative to hemodialysis (Surman et al., 2005). As developments in immunosuppressive medication allowed the use of organs from unrelated deceased donors—at first from individuals declared dead by the use of circulatory criteria and subsequently from individuals declared dead by the use of neurologic criteria—it also expanded the pool of potential living donors of kidneys (Abecassis et al., 2000; Surman et al., 2005). Transplant centers initially allowed only genetically related family members to donate kidneys. Over the years, however, more and more patients have received kidneys from emotionally related donors (those who do not have a genetic link to the donor but who are nevertheless close, e.g., spouses and friends), from acquaintances, and even from altruistic strangers (those who are not currently known by the recipient) (HRSA and SRTR, 2006).
Because the identification of a living donor is an ad hoc process that largely involves the actions of the potential recipient, government oversight of the living donation process is limited. Individual transplant centers have largely borne the responsibility for living organ donation (Steinbrook, 2005). Although the Organ Procurement and Transplantation Network (OPTN) has collected and analyzed data regarding deceased donors, its data on the living donation process and on its effects on living donors over time are quite limited. Perhaps one reason for this imbalance is that the National Organ Transplant Act of 1984, which established the OPTN, did not address living donation. At that time, living donation was not as significant a percentage of donation as it has since become. Hence, there are huge gaps in the available data on living donation and its effects on the donors. OPTN has, however, recently taken steps to increase and improve the data on living donors (Steinbrook, 2005).
Living donation has become more frequent in recent years (Figure 9-1), with significant increases in the number of unrelated donors in the past 10 years (Figure 9-2). From 1988 through December 2005 over 77,000
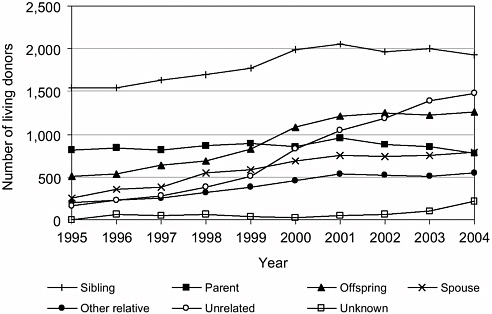
FIGURE 9-1 Relationships between living donors and recipients, 1995 to 2004.
SOURCE: HRSA and SRTR (2006, Table 2.8).
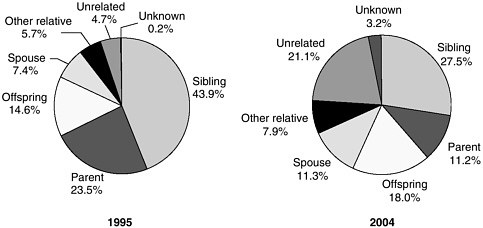
FIGURE 9-2 Relationships between living donors and recipients, 1995 and 2004.
SOURCE: HRSA and SRTR (2006).
living donations occurred (OPTN, 20061). Most organs donated by living donors are kidneys, which constituted 95 percent of the organs from living donors transplanted in 2005 (OPTN, 2006). In 1988, of the 8,873 kidneys transplanted, about 20 percent (1,812 kidneys) came from living donors (OPTN, 2006). A total of 16,477 kidney transplants were performed in 2005, with 9,915 (60.2 percent) of the transplants resulting from deceased donations and 6,562 (39.8 percent) resulting from living donations (OPTN, 2006).
From 2001 to 2003 the number of living donors slightly outnumbered the number of deceased donors (although the latter provided more organs). This trend reversed in 2004 and 2005 due to substantial increases in the number of deceased donors (Chapter 2). Over the last decade and a half, it has become possible for living donors to donate organs other than kidneys, including partial liver, partial lung, and, most recently, parts of the small bowel. Hence, organ donation by living donors is not a single kind of activity because of the different organs that can be involved, the different ratios of the potential benefit to the risk, the variety of possible relationships between the donor and the recipient, and other factors.
The relationship between the donor and the recipient often has a bearing on the donor’s motivation for giving an organ. The living related donor is genetically related to the recipient. Duties and obligations associated with
|
1 |
Data are provided from the National Data Reports on the OPTN website (http://www.optn.org). The data used in this chapter are current as of March/April 2006; data on the website are continuously updated. |
family relationships and roles often weigh heavily on the decision to donate, as do emotional bonds within the family, because the living related donor is usually also an emotionally related one as well. Major ethical concerns about organ donation by living related donors focus on the possibility of undue influence and emotional pressure and coercion.
By contrast, the living unrelated donor lacks genetic ties to the recipient. The living unrelated donor and recipient may be emotionally related (e.g., a spouse or a friend), they may be known to each other but not emotionally close (e.g., coworkers), or they may be complete strangers. Living unrelated donors respond to a need that may come to their attention in various ways. They may become aware of a person’s need for an organ through a shared personal story of a coworker, teacher, church member, or friend of the family; through a story in the media; or through a public solicitation, such as on a billboard, in an advertisement, or on the Internet. Although organ donations in such cases are usually directed donations, that is, the organ is directed to a specific patient in need, there are some cases of nondirected donation. For example, in response to the shortage of transplantable organs, a living unrelated donor may simply wish to donate an organ or part of an organ anonymously to save a life or enhance the quality of life of another person (Matas et al., 2000; Jacobs et al., 2004; Gilbert et al., 2005; Truog, 2005).
Other models have emerged to address situations in which a donor wants to provide a kidney to a particular individual but cannot do so because of incompatibility. The paired donor exchange is a quid pro quo situation in which two donors provide a kidney, each to the other’s intended recipient, because their tissue or blood type is incompatible with that of the originally intended recipient. The donor’s motivation here is ensuring the best outcome for his or her originally intended recipient.
Another arrangement involves a living undirected donation to the pool of transplantable kidneys with the explicit expectation that the donor’s loved one will receive priority for a kidney from a deceased donor. For instance, Region 1 of the United Network for Organ Sharing has devised a live donor list exchange. In this system, a living donor who wants to provide a kidney to a patient but who cannot do so because of blood type or cross-match incompatibility provides a kidney to the system, and the originally intended recipient then receives a kidney from a deceased donor (Delmonico et al., 2004).
In some circumstances it is possible to perform “domino transplantations” in which medical circumstances allow the transplant recipient’s kidney or liver to be donated to another individual on the waiting list. This can occur with specific medical conditions (e.g., familial amyloid polyneuropathy) or with some heart-lung transplantations.
The varieties of recipient-donor relationships raise a number of specific
ethical issues. For example, the solicitation of living donors has become an area of concern and discussion following some widely publicized cases of solicitation for organs through billboards, newspaper advertisements, and the Internet (e.g., through MatchingDonors.com) (Steinbrook, 2005; Truog, 2005). In such cases, as well as in some other types of donation by living unrelated donors, the ethical concerns focus on the possibility of the buying and selling of organs as well as on the impact on the equitable allocation of organs (Steinbrook, 2005).
RISK-BENEFIT RATIOS
The ethical justification for the use of organs from living donors begins with a consideration of the potential benefits, mainly to the recipient but also to the donor, balanced against the risks to the donor, understood in terms of both the probability and the magnitude of harm. Before a potential living organ donor makes the decision to donate, she or he needs to have an accurate understanding of the risks and the potential benefits associated with the donation. However, as this chapter will emphasize, the information disclosed to potential donors to increase their understanding of the risks involved is inevitably inadequate because, for instance, the long-term health outcomes of living donation are only beginning to be explored, particularly for nonrenal organs.
An acceptable risk-benefit ratio is a precondition for a living organ donation. Even though the term “risk-benefit ratio” is common, a more precise formulation is risk-probable benefit ratio. Because the term “risk” reflects both the probability and the magnitude of harm, cost, or burden, the comparable language for benefit needs to include probability as well as magnitude; hence, the ratio is between risk (probability and magnitude of harm, cost, or burden) and probable benefit. Therefore, when this chapter uses the common formulation “risk-benefit ratio,” this interpretation is operative.
A complication in determining a risk-benefit ratio for living organ donation is that the donor bears almost all of the risks. The recipient, on the other hand, is the primary beneficiary because of the reduced waiting time for an organ, survival, and improved health and quality of life if the transplantation is successful. The donor may be a secondary beneficiary, perhaps gaining the psychosocial benefits that result from donating an organ to someone in need. In short, the living donor accepts the risks of major surgery for another’s medical benefit and any psychosocial benefits to himself or herself (Spital, 2004). In this situation, a risk-benefit analysis is thus complicated and difficult to conduct.
Nevertheless, the transplantation team and, ideally, an independent donor advocate team must make a judgment about the acceptability of the
risk-benefit ratio for particular potential donors, who must also make their own assessment. The transplantation team and donor advocate team must be comfortable with the risk-benefit ratio before proceeding. For instance, they may view the risks as excessive to a particular potential donor because of some preexisting medical problem, such as a condition that might increase the risk that his or her remaining kidney may fail in subsequent years. The donor also needs to weigh information on the medical condition of the potential recipient and the potential for a successful transplantation. Even if these teams agree that the risk-benefit ratio is acceptable, the potential donor, whose subjective evaluation is crucial to the decision, must still make his or her own judgment. A negative judgment by either party precludes the donation. Nevertheless, the potential donor’s decision often reflects, at least in part, his or her relationship to the potential recipient.
Living donors often report that they receive important psychological and social benefits from exercising their autonomy to become a living donor. The kinds of benefits, both those that are anticipated and those that are actually experienced, vary to some extent according to the type of relationship between the donor and the recipient. When the donor is biologically and emotionally related to the recipient, donors may experience increased self-esteem for making such a gift, gratitude from the recipient, praise by others, and so forth. Similarly, even when the donor is unrelated to the recipient, donors may experience the gratification of having performed an altruistic act and may receive the praise of others (Spital, 2004).
However, it is difficult for transplantation teams, independent donor advocate teams, and prospective donors themselves to perform their analyses and assessments of risks, benefits, and risk-benefit ratios because of incomplete data about the health outcomes of living donation. Even for the more than 67,000 living donors who donated a kidney through 2004, the data on short-term health outcomes are not comprehensive, and there has been little long-term follow-up to determine the physical and psychosocial effects of living donation over time (Ellison et al., 2002; Matas et al., 2003; Davis and Delmonico, 2005; Ingelfinger, 2005). An example of the need for follow-up data is the number of patients who after donating a kidney later need kidney transplant; as of 2002, an analysis of the OPTN database identified 56 living donors who had subsequently received a kidney transplant or were on the waiting list for renal transplant (Ellison et al., 2002).
For those who have donated parts of their liver, lung, or intestines, the data on the health outcomes of donation come from recent, short-term studies that are not comprehensive; little is known about the long-term effects of these donations (see, for example, Renz and Roberts, 2000; Beavers et al., 2001; Bowdish and Barr, 2004; Bowdish et al., 2004).
Nevertheless, on the basis of the currently available data, it is apparent that the risk-benefit ratio largely depends on the organ or organ part to be
donated because the risks of mortality and morbidity as a result of donation vary greatly by the organ or organ part that is donated. The risk-benefit ratio also depends on the donor’s motivation, which is closely connected to the kind of relationship that exists between the donor and the recipient. A highly motivated donor may derive significant psychological benefit from his or her donation and may thus be willing to incur more risk. Regardless of the organ that is donated, however, complications may occur at the time of the donor workup, during and shortly after the surgery, or long after donation.
In addition, the act of donation may result in some negative psychosocial consequences. For example, lingering health problems could delay or prevent a return to work, and may create difficulties in obtaining life, health, and disability insurance (Russo and Brown, 2003). Furthermore, the donor may confront significant financial costs. These costs, which may be a major disincentive to prospective donors, include lost wages as well as travel, lodging, and other expenses. For these reasons, the federal government and transplantation organizations have begun to take steps to make organ donation as financially neutral as possible. In 1999, the U.S. Congress enacted the Organ Donor Leave Act (Public Law 106-56). This law allows federal employees to take 7 days of paid leave to be a bone marrow donor and 30 days of paid leave to be a solid-organ donor. A number of states and many private-sector businesses have followed suit and have created similar leave provisions for their employees (Davis and Delmonico, 2005; NCSL, 2006). Efforts are also under way to implement the provision of the Organ Donation and Recovery Improvement Act (Public Law 108-216) that provides for the implementation of programs that would grant reimbursement for travel and subsistence expenses and incidental nonmedical expenses incurred by living organ donors (Davis and Delmonico, 2005).
OTHER ETHICAL CONSIDERATIONS
In addition to the ethical considerations involved in risk-benefit analyses and assessments, living organ donation raises several other ethical concerns. Whatever the relationship between the potential donor and the recipient, it is crucial that the potential donor be adequately informed and that the decision be made in an environment that is conducive to thoughtful decision making without undue influence or coercion.
Informed Consent
Ethically justifiable living organ donation presupposes the competent donor’s voluntary informed consent. Competence or capacity in this context refers to the prospective donor’s ability to understand the relevant
information in relation to his or her personal values and interests and, on that basis, to make a thoughtful decision about donation. When the individual being evaluated for living donation lacks the capacity to make such a decision, he or she cannot, strictly speaking, be a “donor,” that is, one who competently decides to donate. Such an individual can only be a “source” of the organs, even though sometimes such a source of organs is loosely called a “donor.” Although children and some adults who are incompetent or doubtfully competent to make complex health-related decisions are sometimes involved in living donation, with the decisions made by others, such donations are difficult to justify ethically and, at a minimum, must satisfy special substantive and procedural conditions. Discussions on the issues regarding children as living organ donors continue (see, for example, Ross, 1998; Abecassis et al., 2000; Delmonico and Harmon, 2002; Holm, 2004; Jansen, 2004; Ladd, 2004; Zinner, 2004).
Nevertheless, even when individuals are competent, problems with communication may compromise the process of informed consent in living donation as well as in other settings, such as therapy and research (Beauchamp and Childress, 2001) (Chapter 3). In addition, the close affective ties in most donations involving related donors may lead the prospective donor to make a decision to donate before he or she fully receives and understands all the pertinent information, particularly about the risks involved (Simmons et al., 1987). The knowledge that a loved one needs a life-saving or life-enhancing transplant may be powerful enough by itself to lead the individual to agree to donate an organ or part of an organ without extensive deliberation.
The goal of the informed-consent process in living donation is adequately informed consent. Even if the individual immediately agrees to donate, it is appropriate to provide the range of relevant information and to ask the potential donor questions to ensure that he or she has an adequate understanding of the act of donation and its possible and probable effects. In light of the potential donor’s desire to help a loved one, the transplantation team and the donor advocacy team need to indicate to the potential donor as clearly as possible the prospective recipient’s need, possible medical alternatives, and the chances for a successful outcome. The patient’s perceived need is important in the prospective donor’s risk-benefit calculus, but so is the patient’s probable outcome.
Nevertheless, adequate understanding (i.e., understanding adequate for informed consent to living donation) may be difficult and perhaps impossible for prospective donors to achieve because of the incomplete and limited data about donor outcomes. Robust informed consent thus remains an elusive ideal because the data about specific health and other risks have not been rigorously collected and analyzed. For example, little is known about the time to recovery; the nature and extent of subsequent morbidities and
complications, or even death; the financial consequences of living donation, including out-of-pocket costs; or the impact of living donation on obtaining or maintaining health and life insurance. Hence, it is important to develop registries that can track such outcomes for living donors.
A few years ago the DHHS Advisory Committee on Transplantation made several recommendations about living donation that called for the creation of a database with data on the health outcomes of all living donors (ACOT, 2005). In May 2005, ACOT noted the continuing lack of a donor registry and reiterated its concern “that provisions in living donor informed consent cannot be fulfilled without the existence of a living donor registry” (ACOT, 2005).
Voluntary Consent
General ethical concerns focus on a potential donor’s competence, level of understanding, and voluntary choice, whatever the relationship between the donor and the recipient. When the prospective donor is related to the recipient, which usually involves close affective ties as well as the genetic relationship, specific concerns focus on the dangers of undue influence, pressure, and coercion, even if he or she is competent, has received adequate information, and appears to understand that information.
It is important to develop mechanisms and procedures to ensure the voluntariness of the prospective donor’s decision. Because the potential donor’s interests may sometimes conflict with the potential recipient’s interests (and, perhaps, with the interests of the recipient’s family, which is also the potential donor’s family), a confidential process is needed for the evaluation and selection of donors, with particular attention to their willingness to donate. Potential donors sometimes feel trapped in a process that they do not know how to stop without jeopardizing their relationships with members of their family or other people. A donor advocate can often be helpful in such circumstances. The transplantation team or donor advocate may sometimes believe that it is justifiable to offer a medical excuse to enable the potential donor to escape the pressure of donation and still protect his or her relationships with the family and others who have an interest in the transplantation. For example, in a survey of 100 liver transplant surgeons, 87 percent indicated that “they would provide a medical or technical reason that precluded donation” if the potential donor changed his or her mind regarding donation (Cotler et al., 2003, p. 640).
Transplantation teams and donor advocates also need to recognize that, for poorly understood reasons, a striking gender imbalance exists in living renal transplantation: women donate kidneys at a significantly higher rate than men. For example, in 2005, 59.2 percent of living kidney donors were women, continuing a long-term trend in which women constitute 56
to 59 percent of the living kidney donations each year (OPTN, 2006). Examining the data for living kidney transplants between 1990 and 1999, Kayler and colleagues (2003, p. 15) observed that “The higher incidence of end-stage renal disease among males and the slight predominance of females in the general population did not explain these gender disparities…. Gender disparities in living donor transplantation result from a higher proportion of wife-to-husband donations and disproportionate female-to-male donations among biological relatives and unrelated pairs.” This quotation describes but does not explain why women donate more often. A much earlier study, which needs to be updated, indicated that men and women donate at roughly the same rates when they are asked to do so and suggested that women were asked more often (Simmons, 1981). Transplantation and donor advocacy teams need to attend to any factors, such as power imbalances, that might lead to the singling out of particular individuals as prospective donors and to pressure on them to donate.
Donations, Not Sales
An ethical concern about living unrelated donation that frequently arises is that the organ is actually being sold or, at least, that financial incentives partially motivate the donation. For example, such concerns have arisen with regard to solicitations on the Internet (Steinbrook, 2005). Money may be a factor in living related donations, too. Whatever the context, compensation for organs is illegal under Section 301 of the National Organ Transplant Act: “It shall be unlawful for any person to knowingly acquire, receive, or otherwise transfer any human organ for valuable consideration” (Public Law 98-507). Compensating living donors opens up the possibility of exploiting poor and underprivileged people and also increases the risk that potential donors will withhold relevant medical information.
The committee’s reasons for rejecting a market in organs from deceased individuals (Chapter 8) apply with even greater force to a market involving organs from living people. These reasons hold even though a few analysts argue that it would be effective and cost-effective to pay individuals as much as $90,000 to provide a kidney for transplantation and even propose changes in the laws to permit such a payment in a regulated market (Matas and Schnitzler, 2003; Matas, 2004). These proposals have yet to gain traction in the United States because they are incompatible with the fundamental values and norms that govern transplantation (Delmonico et al., 2002) and because international markets in organs from living individuals appear to involve the exploitation of relatively impoverished people and inadequately informed and perhaps manipulated consent, as well as, in many cases, adverse consequences for both sellers and purchasers. Although the
direct sale of organs has been debated for several decades, it has been condemned by most national and international governmental organizations and professional societies because of concerns about human rights abuses; the inability to obtain adequately informed consent; and the exploitation of vulnerable people, who are often vulnerable because of poverty (Marshall and Daar, 1998). Although some contend that a regulated market would be a better solution than prohibition, critics doubt that it could avoid all of those negative consequences. Furthermore, they worry about the broader societal impact of the commodification of organs on human dignity.
These ethical concerns also apply to markets for organs that operate, often illegally, in other countries and attract an international clientele (Scheper-Hughes, 2000). Goyal and colleagues (2002) conducted a cross-sectional survey of 305 individuals in Chennai, India, who had sold one of their kidneys. Ninety-six percent of the respondents stated that paying off debt was their motivation; however, selling a kidney did not produce any long-term economic benefit among those interviewed. The results of the study demonstrated a one-third decline in family income, and the majority of participants were still in debt and living below the poverty line at the time of the survey (on average, 6 years after they had sold their kidney). Eighty-six percent of those interviewed reported deterioration in their health status following the nephrectomy.
In addition to the risks to the sellers of a kidney, so-called medical tourism often creates problems for the buyers. A 2005 study of the health outcomes of 16 individuals (mainly from Macedonia) 10 years after they had purchased organs from living unrelated donors (mainly in India) found relatively poor outcomes and several deaths as a result of severe pulmonary infections because of sepsis, hepatitis B with liver cirrhosis, and other complications. Two patients died in the first month, and two patients died at the end of the first year after transplantation (Ivanovski et al., 2005). These results suggest that surgical and medical complications arising from such transplantation practices may outweigh the benefits, all other ethical issues aside (Ivanovski et al., 2005).
NEXT STEPS
Although the committee believes that the whole practice of organ donation by living donors now needs a careful review and assessment on its own, in the interim the committee makes a few specific recommendations, building on ethical concerns and proposals already present within the transplantation community and drawing on the ethical perspectives that inform this report (Chapter 3). Ethical needs include the generation of better information (through a registry for living nonrenal donors and a registry or rigor-
ous sample studies for renal donors) for improved risk-benefit analyses by transplantation teams, donor advocates, and the potential donors themselves; a clinical commitment to the welfare of the donor as a patient before, during, and after the donation; vigorous efforts to ensure fairness and nonexploitation in the selection of donors and to ensure the prospective donor’s understanding and voluntary decision; and the increased use of independent donor advocate teams. The specific recommendations that follow are particularly important for partial liver transplantation and partial lung transplantation because of their greater medical risks and inadequate data about those risks, but they would also be valuable in the context of kidney transplantation. Indeed, these recommendations are crucial to promoting and protecting the potential donor’s voluntary and informed consent in a nonexploitative context.
Independent Donor Advocate Team
In determining which potential living donors will be accepted, transplantation teams serve as ethical gatekeepers, with less societal oversight than occurs in much of transplantation. Additionally, they may have an inherent conflict of interest because they seek to obtain an organ for patients on the waiting list while assuming major responsibilities to potential and actual donors.
The development and use of an independent donor advocacy team that focuses on the donor’s needs is of paramount importance. Such a team can best protect the donor if it offers the multidisciplinary expertise needed to address the whole range of medical, ethical, social, and psychological questions and issues. Each team should include a clinician with experience in transplantation, a social worker or other mental health professional with experience in interpreting donor motivations and addressing intrafamilial conflict, and a nurse. Whether these healthcare professionals or another group of healthcare professionals are involved, the goal is to provide the expertise and skills necessary to ensure (1) that the potential donor adequately understands the risks that surround his or her donation and recognizes the uncertainties involved, especially in the absence of comprehensive data about outcomes, and (2) that the potential donor is making a voluntary decision regarding donation without undue pressure or coercion by family members or by anyone else. Focusing on the welfare and rights of the donor, the donor advocacy team can also act as a safety valve by providing a confidential way out for prospective donors who believe that they are being pressured or coerced to donate.
Living Donor Follow-Up
As this chapter has stressed repeatedly, more information is needed about the short-term and long-term health and other effects of living organ donation, particularly the donation of nonrenal organs. For the most part, living donation developed on an ad hoc basis in various transplant centers and has never had the central oversight and supervision that has marked practices of donation by deceased individuals. As a result there is no national infrastructure for gathering information and for ensuring accountability as there is for donation by deceased individuals.
Establishing registries of living donors would be a first step in developing the infrastructure needed for follow-up studies. Registries are particularly important for nonrenal transplants, and they could be developed without excessive cost because the numbers are small: there are just over 300 living liver donors and about 30 living lung donors (for about 15 lung transplants) each year (HRSA and SRTR, 2006). It could be argued that such a registry is not needed for living kidney donors because this procedure has been used for decades and many thousands of living donors have provided a kidney. However, it is important to start the process of registering all living donors and then to determine, through an appropriate mechanism, what data should be collected after the first year, at what intervals, and for how long, balancing the costs and probable benefits of the data collection.
Important concerns for registries and for sample studies include the long-term effects as well as the short-term effects of donation on physical and mental health and on financial resources, insurability, and other relevant issues. OPTN could be the locus for data collection and management because it is well situated for managing large data sets relating to transplantation. In addition, placing the responsibility for the collection of long-term data on living donors within OPTN would effectively bring living donation under the general scrutiny of the transplantation community and the public.
The committee further observes that many of the available studies of the decision-making process about living donation by potential donors were conducted years ago with living kidney donors (see, for example, the work of Simmons et al., 1977; Sanner, 2005). In addition to continuous quality improvement in the process of selecting, informing, and ensuring the voluntariness of the decisions of prospective donors, transplantation and donor advocacy teams need information from rigorous studies of their processes and of donor and nondonor decision making.
SUMMARY AND RECOMMENDATIONS
The realistic goal of the recommendations developed in this report is to reduce the gap between the supply and the demand for transplantable
organs by increasing the rates of organ donation by deceased persons. One important effect of the reduction of this gap would be the reduction in the need for organs from living donors because such donations are often ethically problematic in view of the risks to donors, particularly in nonrenal transplants, and the difficulty of ensuring voluntary, informed consent.
The committee urges further scrutiny of the complex ethical issues related to living donation and, in the interim, offers two specific recommendations designed to enhance the assessment of donors’ risks and their voluntary, informed consent.
Recommendation 9.1 Protect Living Donors.
Hospitals that perform living-donor transplantations should provide each potential living donor with an independent donor advocacy team to ensure his or her voluntary and informed decision making.
Recommendation 9.2 Facilitate Living Donor Follow-Up.
HRSA, OPTN, and transplant centers should work to establish registries of living donors that would facilitate studies of both short-term and long-term medical and other outcomes of living donation.
REFERENCES
Abecassis M, Adams M, Adams P, Arnold RM, Atkins CR, Barr ML, Bennett WM, Bia M, Briscoe DM, Burdick J, Corry RJ, Davis J, Delmonico FL, Gaston RS, Harmon W, Jacobs CL, Kahn J, Leichtman A, Miller C, Moss D, Newmann JM, Rosen LS, Siminoff L, Spital A, Starnes VA, Thomas C, Tyler LS, Williams L, Wright FH, Youngner S. 2000. Consensus statement on the live organ donor. Journal of the American Medical Association 284(22):2919–2926.
ACOT (Advisory Committee on Organ Transplantation), U.S. Department of Health and Human Services. 2005. Recommendations. [Online]. Available: http://www.organdonor.gov/acotrecs.html [accessed February 23, 2006].
Beauchamp TL, Childress JF. 2001. Principles of Biomedical Ethics, 5th ed. New York: Oxford University Press.
Beavers KL, Sandler RS, Fair JH, Johnson MW, Shrestha R. 2001. The living donor experience: Donor health assessment and outcomes after living donor liver transplantation. Liver Transplantation 7(11):943–947.
Bowdish ME, Barr ML. 2004. Living lobar lung transplantation. Respiratory Care Clinics of North America 10(4):563–579.
Bowdish ME, Barr ML, Schenkel FA, Woo MS, Bremner RM, Horn MV, Baker CJ, Barbers RG, Wells WJ, Starnes VA. 2004. A decade of living lobar lung transplantation: Perioperative complications after 253 donor lobectomies. American Journal of Transplantation 4(8):1283–1288.
Cotler SJ, Cotler S, Gambera M, Benedetti E, Jensen DM, Testa G. 2003. Adult living donor liver transplantation: Perspectives from 100 liver transplant surgeons. Liver Transplantation 9(6):637–644.
Davis CL, Delmonico FL. 2005. Living-donor kidney transplantation: A review of the current practices for the live donor. Journal of the American Society of Nephrology 16(7):2098–2110.
Delmonico FL, Harmon WE. 2002. The use of a minor as a live kidney donor. American Journal of Transplantation 2(4):333–336.
Delmonico FL, Arnold R, Scheper-Hughes N, Siminoff LA, Kahn J, Youngner SJ. 2002. Ethical incentives—not payment—for organ donation. New England Journal of Medicine 346(25):2002–2005.
Delmonico FL, Morrissey PE, Lipkowitz GS, Stoff JS, Himmelfarb J, Harmon W, Pavlakis M, Mah H, Goguen J, Luskin R, Milford E, Basadonna G, Chobanian M, Bouthot B, Lorber M, Rohrer RJ. 2004. Donor kidney exchanges. American Journal of Transplantation 4(10):1628–1634.
Ellison MD, McBride MA, Taranto SE, Delmonico FL, Kauffman HM. 2002. Living kidney donors in need of kidney transplants: A report from the Organ Procurement and Transplantation Network. Transplantation 74(9):1349–1351.
Gilbert JC, Brigham L, Batty DSJ, Veatch RM. 2005. The nondirected living donor program: A model for cooperative donation, recovery and allocation of living donor kidneys. American Journal of Transplantation 5(1):167–174.
Goyal M, Mehta RL, Schneiderman LJ, Sehgal AR. 2002. Economic and health consequences of selling a kidney in India. Journal of the American Medical Association 288(13):1589–1593.
Holm S. 2004. The child as organ and tissue donor: Discussions in the Danish Council of Ethics. Cambridge Quarterly of Healthcare Ethics 13(2):156–160.
HRSA (Health Resources and Services Administration) and SRTR (Scientific Registry of Transplant Recipients). 2006. 2005 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1995–2004. [Online]. Available: http://www.optn.org/AR2005/default.htm [accessed March 3, 2006].
Ingelfinger JR. 2005. Risks and benefits to the living donor. New England Journal of Medicine 353(5):447–449.
Ivanovski N, Popov Z, Cakalaroski K, Masin J, Spasovski G, Zafirovska K. 2005. Living-unrelated (paid) renal transplantation—ten years later. Transplantation Proceedings 37(2):563–564.
Jacobs CL, Roman D, Garvey C, Kahn J, Matas AJ. 2004. Twenty-two nondirected kidney donors: An update on a single center’s experience. American Journal of Transplantation 4(7):1110–1116.
Jansen LA. 2004. Child organ donation, family autonomy, and intimate attachments. Cambridge Quarterly of Healthcare Ethics 13(2):133–142.
Kayler LK, Rasmussen CS, Dykstra DM, Ojo AO, Port FK, Wolfe RA, Merion RM. 2003. Gender imbalance and outcomes in living donor renal transplantation in the United States. American Journal of Transplantation 3(4):452–458.
Ladd RE. 2004. The child as living donor: Parental consent and child assent. Cambridge Quarterly of Healthcare Ethics 13(2):143–148.
Marshall PA, Daar AS. 1998. Cultural and psychological dimensions of human organ transplantation. Annals of Transplantation 3(2):7–11.
Matas AJ. 2004. The case for living kidney sales: Rationale, objections and concerns. American Journal of Transplantation 4(12):2007–2017.
Matas AJ, Schnitzler M. 2003. Payment for living donor (vendor) kidneys: A cost-effectiveness analysis. American Journal of Transplantation 4(2):216–221.
Matas AJ, Garvey CA, Jacobs CL, Kahn JP. 2000. Nondirected donation of kidneys from living donors. New England Journal of Medicine 343(6):433–436.
Matas AJ, Bartlett ST, Leichtman AB, Delmonico FL. 2003. Morbidity and mortality after living kidney donation, 1999–2001: Survey of United States transplant centers. American Journal of Transplantation 3(7):830–834.
Merrill JP, Murray JE, Harrison JH, Guild WR. 1956. Successful homotransplantation of the human kidney between identical twins. Journal of the American Medical Association 160(4):277–282.
NCSL (National Conference of State Legislatures). 2006. State Leave Laws Related to Medical Donors. [Online]. Available: http://www.ncsl.org/programs/employ/Leave-medicaldonors.htm [accessed March 27, 2006].
OPTN (Organ Procurement and Transplantation Network). 2006. National Data Reports. [Online]. Available: http://www.optn.org/latestData/step2.asp? [accessed March 29, 2006].
Renz JF, Roberts JP. 2000. Long-term complications of living donor liver transplantation. Liver Transplantation 6(Suppl 2):S73–S76.
Ross LF. 1998. Children, Families and Healthcare Decision Making. Oxford, UK: Clarendon Press.
Russo MW, Brown RS Jr. 2003. Financial impact of adult living donation. Liver Transplantation 9(10):S12–S15.
Sanner MA. 2005. The donation process of living kidney donors. Nephrology, Dialysis, and Transplantation 20(8):1707–1713.
Scheper-Hughes N. 2000. The global traffic in human organs. Current Anthropology 41(2): 191–224.
Simmons RG. 1981. Psychological reactions to giving a kidney. In: Levy NB, ed. Psychonephrology 1: Psychological Factors in Hemodialysis and Transplantation. New York: Plenum Medical.
Simmons RG, Marine SK, Simmons RL. 1977. Gift of Life: The Social and Psychological Impact of Organ Transplantation. New York: Wiley.
Simmons RG, Marine SK, Simmons RL. 1987. Gift of Life: The Effect of Organ Transplantation on Individual, Family, and Societal Dynamics. New Brunswick, NJ: Transaction Books.
Spital A. 2004. Donor benefit is the key to justified living organ donation. Cambridge Quarterly of Healthcare Ethics 13(1):105–109.
Steinbrook R. 2005. Public solicitation of organ donors. New England Journal of Medicine 353(5):441–444.
Surman OS, Fukunishi I, Allen T, Hertl M. 2005. Live organ donation: Social context, clinical encounter, and the psychology of communication. Psychosomatics 46(1):1–6.
Truog RD. 2005. The ethics of organ donation by living donors. New England Journal of Medicine 353(5):444–446.
Zinner S. 2004. Cognitive development and pediatric consent to organ donation. Cambridge Quarterly of Healthcare Ethics 13(2):125–132.


















