4
Arming the Emergency Care Workforce with Pediatric Knowledge and Skills
This chapter provides an overview of the emergency care workforce. The review focuses on the level of pediatric education and training that providers receive and evidence of their ability to treat children appropriately. What becomes clear from the discussion is that pediatric care represents a relatively limited component of educational requirements for many emergency care providers; moreover, many emergency care providers treat critically ill or injured pediatric patients infrequently and therefore may be unable to maintain the requisite level of skill. The result is that some emergency care providers are ill prepared to address the broad spectrum of ailments that children encounter, from common to critical injuries and illnesses. This is a long-standing problem that has improved somewhat over time, but naturally has led to continued concerns about the ability of the emergency care workforce to care properly for pediatric patients. To reduce the consequences of illness and injury, the workforce must have the knowledge and skills necessary to deliver appropriate pediatric emergency care. The committee offers several recommendations for enhancing and supporting providers’ ability to deliver quality care to children.
PREHOSPITAL EMERGENCY CARE
The term “first responder” is often used to identify the first care provider on the scene. In the mid-1990s, the term was used by the National Highway Traffic Safety Administration (NHTSA) in its formal classification of emergency medical services (EMS) responders. First responders represent the most basic level of EMS response and are trained to provide basic emer-
gency medical care. They have more training than first aid, but less than an emergency medical technician (EMT). A certification exists for first responders, and many firefighters, police officers, and other emergency workers have first responder training, which is useful since they may arrive on the scene before an EMT. First responders use a limited amount of equipment to perform initial assessment and intervention and are trained to assist EMTs once the EMTs arrive on the scene (NHTSA and MCHB, 1995; Bureau of Labor Statistics and U.S. Department of Labor, 2004).
EMTs are the backbone of prehospital emergency care in the United States as they are usually the first providers of direct medical care to patients needing emergency treatment. There are generally three levels of EMT: EMT-B (Basic), EMT-I (Intermediate), and EMT-P (Paramedic).
EMT-Bs are those trained to provide basic, noninvasive prehospital care, although their scope of practice varies by state and may include certain invasive procedures in some states. EMT-Bs provide care to patients at the scene of a medical emergency (e.g., car crash) and during transport to the hospital. They perform the following tasks:
-
Examine victims to determine the nature and scope of their injury or illness.
-
Administer basic life support (BLS), including providing oxygen or performing cardiopulmonary resuscitation (CPR).
-
Use automated or semiautomated defibrillators to administer lifesaving shocks to a stopped heart.
-
Upon arrival at the hospital or medical center, help the staff provide preadmittance treatment and obtain patient medical histories (Bureau of Labor Statistics, 2002; State of California Employment Development Department Labor Market Information Division, 1995).
EMT-Ps are the most highly skilled EMTs, and they provide the most extensive care. Paramedics are trained in all phases of emergency prehospital care, including advanced life support (ALS) treatment. In addition to the tasks performed by EMT-Bs, they may also:
-
Administer drugs (usually intravenously).
-
Administer intravenous fluids.
-
Use manual defibrillators to administer lifesaving shocks to a stopped heart.
-
Use advanced airway techniques and equipment to assist those patients experiencing a respiratory emergency.
-
Perform endotracheal intubations and perhaps other invasive airway maneuvers.
-
Interpret the results of heart-monitoring equipment (Bureau of Labor
-
Statistics, 2002; State of California Employment Development Department Labor Market Information Division, 1995).
Most states recognize a level of practice between that of EMT-Bs and EMT-Ps. Sometimes known as EMT-I, this level encompasses all the tasks of an EMT-B, but also may include some of the tasks of a paramedic. The scope of practice of these EMT-Is varies by state, but is always broader than that of an EMT-B in the same state and narrower than that of an EMT-P.
The EMT profession is different from most medical occupations in that a substantial number of workers serve in a volunteer capacity. According to data gathered from a sample of members of the National Registry of Emergency Medicine Technicians (NREMT), 36.5 percent of registered EMTs are volunteers. The vast majority of volunteer EMTs are EMT-Bs (89.5 percent), while paid EMTs are much more likely to be registered as EMT-Ps (46.3 percent) (NREMT, 2003). Volunteer personnel have traditionally been the lifeblood of rural EMS agencies. Since the development of EMS systems began in the 1960s, millions of hours of time and effort have been donated by rural EMTs to the care of their neighbors, friends, and complete strangers.
Staffing Challenges
Working conditions for EMTs tend to be very challenging, leading to high rates of turnover. EMTs may experience burnout, or even post-traumatic stress disorder, as a result of the emotional and psychological stressors of their job. Many EMTs work irregular hours, and some are not well compensated in salary or retirement benefits. The work of EMTs is also occasionally dangerous, as they must respond to unpredictable and uncontrolled situations and may be exposed to the threat of violence or infectious disease (Franks et al., 2004). Moreover, there is no well-defined career ladder for EMTs, and those in fire department–based services sometimes must leave EMS work for other duties to advance within their organization. Many individuals work as an EMT as a step toward becoming a physician assistant, registered nurse (RN), or physician.
Recruitment and retention are a constant problem for EMS agencies; at a recent EMS conference, administrators ranked recruitment and retention as a top priority (EMS Insider, 2005). Anecdotal reports indicate that many regions are facing shortages of prehospital personnel. Some reports indicate a critical shortage of EMTs in rural areas, but even some urban areas struggle. For example, the District of Columbia Fire and EMS Service Department reported a shortage of EMS personnel that had driven staffing levels below half of what is needed to staff the city’s fleet of ambulances. In 2005, 57 of the 166 paramedic positions in the District of Columbia were
vacant. As a result, the city is staffing ALS ambulances with a paramedic and a lesser-trained EMT rather than two paramedics (Wilber, 2005). Reports indicate that staffing shortfalls appear to be most pronounced at the paramedic level. This is likely due to the increased education required for this level of EMT and attrition of personnel to fire services (Personal communication, M. Williams, March 27, 2006).
Demand for EMTs will continue to be strong in rural and smaller metropolitan areas (Bureau of Labor Statistics, 2002). Volunteer staffing has become increasingly more difficult to maintain in rural areas for a variety of reasons. Decades ago it was common for volunteers to be on call virtually 24 hours a day. Today, increased time demands due to the need for two-income family support and vying interests create an environment in which volunteers may donate just one specific weeknight or a few hours on a weekend. Rural EMS agencies face particular volunteer staffing shortages during the weekday work hours.
Pediatric Training
Although there are National Standard Curricula for all levels of EMT training, those curricula are not mandatory, so training requirements for certification vary across states. A written exam is required in most states, and some require an additional practical exam to obtain certification. Generally, the national standards for BLS are a minimum of 110 hours of instructional training with additional field training requirements that vary by state. For ALS, training at the paramedic level entails 1,000–1,200 hours of didactic training beyond the EMT-B level (DOT, 1998), with additional practicum time. Certification in all states needs to be renewed (every 2 years for most states). Renewal usually requires completion of continuing education, verification of skills by a medical director, and current affiliation with an EMS agency.
Pediatric care has traditionally been a small component of EMT training. In a mid-1980s survey of EMT training programs nationwide, Seidel (1986) found that 41 percent of such programs offered 10 hours or less of didactic training in pediatrics; 5 percent of programs offered none. All EMTs received on average 8 hours of didactic training in pediatrics; paramedics received 15 hours. Seidel also identified wide variation in the pediatric topics covered in the curriculum. Most training programs covered epiglottitis (98 percent of agencies), croup (98 percent), respiratory distress (98 percent), asthma (97 percent), and seizures (95 percent). However, half of programs did not offer pediatric field simulation, half did not cover pediatric dysrhythmias, 36 percent did not cover hypotension, 26 percent did not cover drowning, 22 percent did not cover pediatric ALS, and 16 percent did not cover neonatal resuscitation.
Since the early 1990s, a number of efforts have been made to improve pediatric training opportunities for EMTs. Among the earliest courses designed specifically for EMTs was the Prehospital Trauma Life Support course, developed in 1990 by the National Association of EMTs in cooperation with the American College of Surgeons’ (ACS) Committee on Trauma. This continuing education course incorporates material on prehospital pediatric assessment and stabilization. It is an intensive 16- to 20-hour course attended by all levels of EMTs.
In 1992, the first national consensus curriculum on prehospital pediatrics was published by the California Pediatric Emergency and Critical Care Coalition, the California Emergency Medical Services for Children (EMS-C) Project, and the American College of Emergency Physicians (ACEP). The initiative grew, and in 1995 a task force produced the Pediatric Education for Paramedics (PEP) course, which built on the work of several state projects funded by the federal EMS-C program (AAP, 2005a). That course was eventually expanded by a steering committee assembled by the American Academy of Pediatrics (AAP) to serve both BLS and ALS EMTs. The result was the Pediatric Education for Prehospital Providers (PEPP) course. The BLS course consists of a minimum of 7 hours, while the ALS course is a minimum of 13 hours. In developing course recommendations, the steering committee reviewed the most current data on efficacy, safety, and feasibility. Where scientific data were not available, the steering committee used expert opinion and clinical experience in hospitals, emergency departments (EDs), and pediatric ambulatory settings to shape the course content. The course is subject to the steering committee’s ongoing review (AAP, 2005a). The first edition of the PEPP manual sold more than 100,000 copies, and the program extends into nine countries and includes more than 5,000 instructors worldwide (PEPP Program, 2006).
In the 1990s, the Maternal and Child Health Bureau (MCHB) worked with and supported NHTSA in revising the Department of Transportation’s (DOT) National Standard Curricula to ensure that the needs of children would be addressed during initial EMT education and refresher courses. The curricula for first responders, EMT-Bs, EMT-Is, and EMT-Ps were all revised. Table 4-1 shows the content of the National Standard Curricula specific to pediatrics for first responders, EMT-Bs and EMT-Is. It should be noted that there are more cognitive, affective, and psychomotor objectives related to pediatrics included in other parts of the curriculum. For example, a module on assessment-based management may include instruction related to pediatrics. Still, the number of hours dedicated to pediatrics appears low.
The National Standard Curriculum for Paramedics was developed in 1998, but the hours specific to each module are not specified. Instead, the curriculum emphasizes meeting educational objectives. The curriculum
TABLE 4-1 Recommended Pediatric Education in the Current U.S. Department of Transportation National Standard Curricula
|
Content |
Recommended Minimum Hours |
|
First Responder (1995) |
|
|
Infants and Children |
2 |
|
Practical Lab: Children and Childbirth |
1 |
|
Evaluation: Children and Childbirth |
1 |
|
Emergency Medical Technician-Basic (1994) |
|
|
Infants and Children |
3 |
|
Practical Skills Lab: Infants and Children |
3 |
|
Evaluation: Infants and Children |
1 |
|
Emergency Medical Technician-Intermediate (1999) |
|
|
Neonatal Resuscitation |
2 |
|
Practical Lab: Neonatal Resuscitation |
2 |
|
Pediatrics |
8 |
|
Practical Lab: Pediatrics |
4 |
|
SOURCE: Personal communication, D. Bryson, NHTSA, 2006. |
|
includes the following modules that address pediatric issues: pharmacology, venous access and medication administration, life span development, neonatology, pediatrics, abuse and assault, patients with special challenges, acute interventions for the chronic care patient, and assessment-based management (Personal communication, D. Bryson, January 26, 2006).
The National Standard Curricula, which many but not all states follow, are likely to be replaced in the future by the National EMS Education Standard. It will be updated on a 2- or 3-year cycle as a new national approach to EMT education is developed (NHTSA, 2006).
When the DOT National Standard Curricula were developed, there was concern that many EMS instructors did not have the knowledge or clinical experience to teach the new pediatric components of the curriculum adequately (MCHB, 1996). As a result, the EMS-C program awarded a grant to New York University to develop the Teaching Resource for Instructors in Prehospital Pediatrics (TRIPP). TRIPP, originally published in 1997, is an encyclopedic resource manual for instructors who teach the pediatric sections of the EMT-B National Standard Curriculum. In 2002, the developers of TRIPP released another version for instructors of ALS.
The National Association of Emergency Medical Technicians (NAEMT) also established its own Pediatric Prehospital Care (PPC) course in 2000 after recognizing a need by EMTs for additional training to better understand the anatomical, physiological, and communication challenges surrounding the treatment of children. The course is overseen primarily by EMTs, with strong guidance from a pediatric emergency medicine physician. Some EMS
systems adopt the course as their only pediatric training program (NAEMT, 2005). However, the pediatric continuing education courses required by EMS agencies still vary considerably. Those commonly required include Pediatric Airway Management for the Prehospital Professional, Pediatric Advanced Life Support, and Advanced Pediatric Life Support. A review of the literature revealed no studies that have evaluated whether EMS training in these courses has led to changes in patient outcomes.
Perhaps the newest course for the prehospital professional is one that focuses on children with special health care needs. The EMS-C program funded the development of Special Children’s Outreach and Prehospital Education (SCOPE), designed to teach EMTs how to care for children with special health care needs. This curriculum is particularly important since special needs children are frequent users of the prehospital system. The curriculum, created in 2003, provides basic information on various chronic medical conditions, as well as on the technologies and equipment that may be necessary for the survival of children with these conditions (MCHB, 2003).
Despite advances in educational opportunities and materials, pediatric issues continue to be a challenge for EMTs. According to a NREMT newsletter, in 1996, nearly one-third of individuals taking the NREMT EMT-P examination failed on their first attempt. Of those who failed, two-thirds failed the pediatric/obstetrics section; the failures related primarily to the pediatric questions within that section (Glaeser et al., 2000).
Limited studies of pediatric training for EMTs have continued to show deficiencies, though many of these studies are dated. A survey of EMS agencies in North Carolina revealed that only 11 percent of agencies provided more than 10 hours of basic training in pediatric emergency care (Zaritsky et al., 1994). A similar survey of EMS agencies in Oklahoma found that more than half did not address pediatric topics in continuing education (Graham et al., 1993). According to the 2003 EMS-C National Grantee Survey Assessment, pediatric education requirements were a condition for recertification for EMT-Bs in 24 states and for EMT-Ps in 31 states (MCHB, 2004a).
A survey of nationally registered EMTs revealed that mandatory continuing education was not required for 35 percent of EMT-Bs, 40 percent of EMT-Is, and 25 percent of EMT-Ps. In the 2 years prior to the survey, 24 percent of EMT-Bs, 20 percent of EMT-Is, and 6 percent of EMT-Ps received 0–3 hours of pediatric continuing education. Still, continuing education was the main source of pediatric knowledge and skills for 42 percent of EMT-Bs, 56 percent of EMT-Is, and 60 percent of EMT-Ps. More than three-fourths of all EMTs surveyed said they supported a state or national mandate for required continuing education in pediatrics beyond what they currently received (Glaeser et al., 2000). Of those EMTs surveyed who sup-
ported mandated pediatric continuing education, approximately half said there were no barriers to obtaining this training. However, 23 percent of EMT-Bs, 21 percent of EMT-Is, and 13 percent of EMT-Ps said that continuing education was not available. Other common barriers cited included costs of continuing education courses, which are frequently borne by the EMTs themselves rather than their EMS agency, and the distance to the courses. Only a small percentage of EMTs said their medical director was not interested in increasing pediatric continuing education or that pediatric facilities were not cooperative (Glaeser et al., 2000).
Maintenance of Pediatric Skills
Exercising skills in real life is important to reinforce training (Wood et al., 2004). One of the challenges faced by EMTs in keeping their pediatric skills sharp is that they rarely have the opportunity to practice lifesaving procedures in real situations (Gausche-Hill, 2000). Children represent only 5–10 percent of all prehospital calls (Seidel et al., 1984; Federiuk et al., 1993); of those pediatric calls, only 12 percent involve the need for pediatric ALS (PALS) (Seidel et al., 1984). Only a small percentage of EMTs identify field experience as the main source for their pediatric knowledge and skills. This is not surprising considering that fewer than 3 percent of all EMTs care for more than 15 pediatric patients during a typical month, and perhaps only 1 of these patients needs ALS care. In one survey, 87 percent of EMT-Bs, 84 percent of EMT-Is, and 60 percent of EMT-Ps said they treated fewer than 4 pediatric patients per month (Glaeser et al., 2000).
Several studies have revealed how infrequently EMTs have the opportunity to practice certain interventions in the field. In an analysis of ALS prehospital provider calls in Boston, Massachusetts, Babl and colleagues (2001) found that ALS providers delivered on average one bag mask ventilation every 1.7 years, one intubation every 3.3 years, and one intraosseous access (placement of a needle into a bone to give fluid for resuscitation) every 6.7 years (Babl et al., 2001). Similarly, Gausche (1997) concluded that it would take at least 20 years for every paramedic in 11 counties in California to perform bag-valve-mask ventilation at least once on a pediatric patient (Seidel et al., 1991).
Quality of Care
Lack of initial and continuing pediatric education, coupled with the low frequency with which EMTs encounter critical pediatric patients, results in a lower level of care than should be expected of the nation’s prehospital emergency care system. Several studies have documented deficiencies in treatment for pediatric patients. In the 1980s, Seidel and colleagues (1984) found
that death rates from trauma were significantly higher for children than for adults (highest for infants), and that deaths occurred more commonly in areas where there were no pediatric centers. The study findings suggest that the needs of children in the prehospital setting were not being met (Seidel et al., 1984). In a study of 100 pediatric trauma deaths, Ramenofsky and colleagues (1984) found that 53 could have survived if the EMS/trauma system had functioned properly; errors were found in nearly 80 percent of those cases (Ramenofsky et al., 1984). Several studies have shown that EMTs have greater success rates in intubating adults compared with children (Mishark et al., 1992; Boswell et al., 1995; Doran et al., 1995).
Underutilization of acquired skills can cause an EMT to feel fearful or reluctant about performing an intervention in a time of crisis (Orr et al., 2006). And in fact, children tend to be undertreated in comparison with adults (Gausche et al., 1998; Orr et al., 2006). There are several examples. A study of children in respiratory distress found that 44 percent received inappropriate interventions. Oxygen and medications were underused, while vascular access, a procedure that paramedics perform frequently, was overused (Scribano et al., 2000). Another study found that paramedics are less likely to perform basic resuscitation procedures for pediatric patients than for equally critical adults (Su et al., 1997). In one Canadian study, half of children under age 6 who required intravascular access did not receive an intravenous line (Lillis and Jaffe, 1992).
Comfort in Caring for Pediatric Patients
Studies indicate that many EMTs are less comfortable caring for pediatric patients, particularly infants, than for adult patients. An example is that paramedics reported being very comfortable terminating CPR on adults, but very uncomfortable doing so with children (Hall et al., 2004). A study that examined job satisfaction among paramedics found that pediatric calls were among the most stressful because of the low volume of pediatric cases typically encountered (Federiuk et al., 1993).
Although the majority of EMTs in the survey of Glaeser and colleagues (2000) said they were comfortable to some degree with their own and their EMS system’s ability to care for a critical pediatric patient, they indicated that critical care infants were the patients of greatest concern. Indeed, 94 percent of respondents were more uncomfortable with treating infants and toddlers than any other age group (Glaeser et al., 2000). This is an important finding considering that infants tend to use prehospital and ED services at higher rates than older children. In a 1999 study of EMS transports in Kansas City, Missouri, Murdock and colleagues (1999) found that infants younger than 1 year of age had the highest transport rates (47 transports per 1,000 persons), followed by those aged 1–4 (26 per 1,000 persons),
10–14 (18 per 1,000 persons), and 5–9 (17 per 1,000 persons) (Murdock et al., 1999).
Another problem associated with the lack of practice in the field is that certain skills deteriorate rather quickly if not used. Training in pediatric resuscitation can boost knowledge and skills initially, but one study found that this knowledge and these skills decay significantly after 6 months (Su et al., 2000). Deterioration of skills is a concern even for paramedics with years of experience. Two years after taking a PALS course, a majority of experienced paramedics could not pass a test on PALS concepts (Wolfram et al., 2003).
More troubling, EMTs’ confidence is not necessarily a good indication of ability. Henderson (1998) showed that 95 percent of paramedics who failed both bag-valve-mask and endotracheal intubation attempts reported a feeling of confidence in and a lack of anxiety about their ability to perform those tasks (Henderson, 1998; Orr et al., 2006). Training increases EMTs’ perception of their ability, and their confidence declines slowly over time. Unfortunately, their actual skill performance declines more quickly than perceived (Gausche-Hill, 2000).
EMERGENCY DEPARTMENT CLINICIANS
A number of different types of clinicians deliver care to children in EDs. Not just physicians and nurses, but also pharmacists, nurse practitioners, physician assistants, and others play an important role in many EDs.
ED Physicians
There were approximately 32,000 physicians working in EDs in 1999, an average of nearly 8 physicians per ED (Moorhead et al., 2002). Emergency physicians evaluate the presenting problems of patients, make diagnoses, and initiate treatment. They must be prepared for a wide variety of medical emergencies and must be well versed in such diverse subjects as anesthesia, cardiology, critical care, environmental illness, neurosciences, obstetrics/gynecology, ophthalmology, pediatrics, psychiatry, neonatology, resuscitation, toxicology, trauma, and wound management. In addition, they often represent the sole source of primary care for patients whose only access to care is through EDs. ED physicians also have duties beyond their scheduled clinical time; they spend several hours per week performing unscheduled clinical duties, administrative work, teaching, and/or research (Moorhead et al., 2002). In small hospitals that lack in-house physician support at night, many emergency physicians are required to provide backup support to the hospital from the ED.
A medical specialty of emergency medicine (EM) was created to enhance
the training and skills of physicians wishing to practice in the ED. EM residency training involves a minimum of 3 years of specialized training after medical school. Board certification is granted by the American Board of Emergency Medicine (ABEM) or its osteopathic equivalent, the American Osteopathic Board of Emergency Medicine (AOBEM). Largely as a result of the steady growth in EM residency training programs, the number of self-identified EM physicians in the United States has increased substantially since 1979, when EM was first recognized as a specialty. Growth in EM has been much stronger than growth in medicine overall. The number of self-identified EM physicians in the United States increased from 14,000 in 1990 to more than 25,500 in 2002, an increase of 79 percent. During the same period, the number of all physicians increased by 39 percent (AMA, 2003).
Despite the growth in EM physicians, only 38 percent of practicing ED physicians in the United States are residency trained and board certified in the specialty of EM. The majority of those ED physicians who are not residency trained or board certified in EM have completed a residency in another specialty, most often family practice or internal medicine. Only 3 percent of practicing emergency physicians are residency trained or board certified in pediatrics (Moorhead et al., 2002). Many rural hospitals hire “moonlighting” residents to provide physician coverage in their EDs. Moonlighting—traditionally the unsupervised practice of residents before the completion of their residency (Armon and Coren, 2005)—has stirred considerable controversy among medical organizations (Kaji and Stevens, 2002). In any case, moonlighting physicians are not likely to have extensive training or experience in either EM or pediatrics.
Residency-trained EM physicians and pediatricians have the option of pursuing subspecialty fellowship training and board certification in pediatric emergency medicine. Alternatively, graduating medical students can enroll in a joint EM–pediatrics residency program, an option established in 1992 by the American Board of Pediatrics (ABP) and ABEM. Pediatric emergency medicine is now a recognized subspecialty of the American Board of Medical Specialties. Creation of the pediatric emergency medicine subspeciality grew from the recognition that the pediatric population is a distinct group of patients requiring trained staff to respond to their unique needs (Tamariz et al., 2000). A subspecialist in pediatric emergency medicine is a physician who has completed training in either pediatrics or EM, and then secured additional training in pediatric emergency medicine in an accredited fellowship program (ABMS, 2002). At present, the total number of pediatric emergency medicine physicians is quite small. In fact, the number of EM physicians and pediatricians choosing to subspecialize in pediatric emergency medicine has declined significantly, from a high of 355 in 1996–1997 to a low of 121 in 2002–2003. However, the large number of physicians who received their
certification in the mid-1990s reflects those individuals who did so before the grandfather provision for the subspecialty ran out. The figure since that time indicates a rather stable number of trainees in pediatric emergency medicine. Most of the slots in these fellowship programs are being awarded to graduates of pediatric residency programs. As a result, the vast majority of pediatric emergency medicine subspecialists (89 percent of the total between 1994 and 2003) hold their primary board certification in pediatrics rather than EM (see Figure 4-1) (ABMS, 2003).
The average hospital is likely to have a board-certified EM physician attending, but unlikely to have a pediatric emergency medicine physician attending. Approximately 23 percent of EDs have a pediatric emergency medicine physician attending. Children’s hospitals and hospitals with large volumes of pediatric patients (more than 7,500 pediatric ED visits per year) are more likely to have a pediatric emergency medicine physician attending than the average hospital (Middleton and Burt, 2006). Among those hospitals without a pediatric emergency medicine physician attending, just over half have a board-certified pediatrician attending, and 20 percent have a written protocol for calling a pediatrician; 17 percent of EDs have no EM, pediatric emergency medicine, or pediatric attending physician.
The physicians who work in the ED have varying degrees of training in pediatrics. Those with the most formal training are those who have completed a fellowship in pediatric emergency medicine. The goal of the fellowship program in this subspecialty is to produce physicians who are clinically proficient in the practice of pediatric emergency medicine, especially in the management of the acutely ill or injured child, in the ED (ACGME, 2004). The training period for pediatric emergency medicine subspecialty residents is 2 years for EM physicians and 3 for pediatricians. The Accreditation Council for Graduate Medical Education (ACGME) specifies that the curriculum must include at least 12 months of seeing children in an ED that treats children for the full spectrum of illnesses and injuries. The training
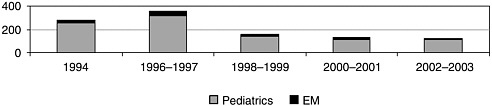
FIGURE 4-1 Number of subspecialty certificates in pediatric emergency medicine, United States, 1994–2003.
SOURCE: ABMS, 2003.
also includes 4 months in the reciprocal specialty from which the resident enters the training program. For example, pediatric graduates must spend 4 months in adult care rotations. The core content of the curriculum must include training in EMS, administration, ethics, legal issues, research, and procedures. Certification is limited according to the physician’s primary board—7 years for the American Board of Pediatrics, 10 years for the American Board of Emergency Medicine (ACGME, 2004).
EM resident physicians are required to receive training in pediatric emergency care. In the early 1980s, there was considerable concern about the level and quality of pediatric emergency care training provided in these programs. Pediatric emergency care training accounted for approximately 16 percent of training time for EM residents, even though pediatric patients represented about 25 percent of all ED visits (Ludwig et al., 1982). In a survey, 42 percent of residency program directors expressed dissatisfaction with the pediatric training component of the EM residency (Ludwig et al., 1982; Christopher, 2000). Since that time, there has been increased involvement of pediatric emergency medicine physicians in EM residencies. Additionally, more EM residencies include specific training experience in pediatric emergency care, and more EM residency programs are affiliated with pediatric centers (AAP, 2000; Tamariz et al., 2000; Christopher, 2000).
Nonetheless, a more recent assessment of pediatrics in emergency medicine residency programs indicates that progress has been mixed. Pediatric training in EM residency programs continues to represent a relatively small percentage of training time. Today, approximately 13 percent of training time is spent on pediatric electives (Tamariz et al., 2000). EM residents may see children during nonpediatric rotations and certainly during their 18-plus months of supervised training on ED rotations, but the amount of pediatric contact time on these rotations is difficult to determine. At the same time, the confidence of residency directors in their pediatric curriculum has improved. The majority of directors indicated that they were either very or somewhat confident in the areas of trauma, intensive care, airway management, and urgent care. This confidence likely reflects the relatively large exposure of emergency residents to pediatric patients in EDs, pediatric EDs, pediatric intensive care units, and urgent care or fast-track clinics. In the area of neonatal resuscitation, most residency directors were somewhat confident or not very confident, suggesting that emphasis on this skill should be increased in the curriculum (Tamariz et al., 2000).
To be board certified in EM, a physician must pass an exam in that specialty. Approximately 8 percent of the EM board exam focuses on pediatric topics (ABEM, 2004). However, an individual need answer only 75 percent of the total questions correctly to pass. Therefore, an individual can answer all of the pediatric questions incorrectly and still receive a passing score on the exam.
Unfortunately, the majority of physicians practicing in the ED have not had residency training in either EM or pediatric emergency medicine (Moorhead et al., 2002). An assessment conducted in the late 1990s found that the supply of EM physicians was simply not sufficient to staff all ED physician positions, and not all EDs had access to a pediatric emergency medicine physician on staff (Holliman et al., 1997). This appears to be the case today as well (Moorhead et al., 2002). Therefore, physicians in some of the other disciplines (e.g., internal medicine, family practice) are needed to fill positions in EDs. It is difficult to determine the level of pediatric and EM training these physicians have received. Certainly those ED physicians who are pediatricians are familiar with children, but their formal training in EM may be limited. Likewise, ED physicians in such disciplines as internal medicine and family practice may have little formal training in either EM or pediatrics. Nevertheless, these ED physicians presently represent an essential component of ED staffing in many hospitals. Many may possess a high level of competency in pediatric emergency care, but it was gained through on-the-job experience rather than through formal training in a supervised setting.
As stated above, 3 percent of ED physicians are board certified in pediatrics. The committee is concerned not only about ED physicians lacking substantial training in pediatrics, but also about some pediatricians working in the ED lacking sufficient training in EM. According to the Residency Review Committee’s requirements for pediatric residency programs, pediatric residents must spend a minimum of 4 months receiving training in emergency and acute illness, but only 2 of those 4 months must be in EM (National Capital Consortium Pediatrics Residency, 2004). This means that some pediatricians practicing in the ED may have spent only 5.5 percent of their 3-year residency on EM, although again, many of these physicians may possess a high level of competency in EM based on their experience in the ED. Another concern is that sick children access care through their pediatricians, who may find it difficult to detect certain emergency conditions, such as meningococcemia, among their patients. A pediatrician who received little training in EM and who spends the majority of his or her time on well-child visits may have difficulty recognizing and addressing an emergency condition.
Beyond initial specialty training, physicians have a number of opportunities to obtain training in pediatric emergency care. Different hospitals have their own requirements in terms of continuing education for ED physicians. However, the most popular pediatric continuing education courses are PALS and advanced pediatric life support (APLS). These courses are often required during initial training as well; for example, the PALS course is required in 78 percent of EM residency programs and APLS in 17 percent of programs (Tamariz et al., 2000). Additionally, professional societies help
member physicians comply with continuing education requirements from state medical boards. For example, ACEP, which represents EM physicians, has a number of educational offerings designed to help members earn 150 hours of continuing education credits every 3 years. Of the 800 courses approved for credit, 23 percent are on pediatric topics, the most popular being PALS and APLS. Several other pediatric courses are offered at the ACEP annual meeting. According to a 1997 ACEP survey, however, 17 states had not offered APLS, PALS, or other similar pediatric courses in the previous 2 years (Santamaria et al., 1997). Having to travel a long distance to attend a pediatric training course naturally places an added burden on physicians who might wish to obtain the training.
Pediatric and Trauma Surgeons
The other medical specialties of particular relevance to pediatric emergency care are the surgical subspecialties of trauma surgery and pediatric surgery. In a 5-year residency training program in general surgery, surgeons receive training in a number of specialty areas, including trauma and pediatric surgery, after which they are expected to be able to manage the commonly encountered and less complex cases associated with these content areas (The American Board of Surgery, 2004). They may subsequently choose to undertake advanced training in trauma surgery or pediatric surgery (The American Board of Surgery, 2005).
Trauma surgeons perform emergent surgical procedures, usually but not exclusively involving life- or limb-threatening injuries to the neck, chest, abdomen, pelvis, and vasculature. Trauma surgeons generally complete 2 years of fellowship training in trauma surgery and surgical critical care following the completion of the 5-year surgical residency. The ACS estimates that there are about 3,000 trauma surgeons practicing in the United States today (Personal communication, C. Williams, February 17, 2006). Trauma surgeons tend to focus their practice in trauma centers.
The American Board of Surgery awards Certification in Pediatric Surgery to surgeons who complete a 2-year fellowship in pediatric surgery and pass an examination in pediatric surgery following the 5-year surgical residency (The American Board of Surgery, 2004). Pediatric surgery residents are required to meet specific curricular goals and objectives in pediatric trauma care and must help provide definitive pediatric trauma care to large numbers of pediatric trauma patients.
On-Call Specialists
Hospitals that offer specialist services, such as neurosurgery and orthopedic surgery, to inpatients must also have the same services available
to patients who present at the ED (Glabman, 2005). ED physicians rely on and consult these specialists for advice or admission, as well as to arrange follow-up care after discharge, to relay information about a patient, and/or to request specific procedures or treatment for patients (Macasaet and Zun, 2005). Some of these specialist physicians have obtained advanced training in their specialty area after completing a pediatric residency (e.g., pediatric neurology or cardiology) or residency training in the specialty area followed by specialized pediatric training (e.g., pediatric surgery, orthopedics, or plastic surgery).
The salient problem with specialists is their availability. Over the past several years, many hospitals have experienced great difficulty in securing specialists for ED patients of all ages when needed. In a 2004 survey by ACEP, two-thirds of ED medical directors reported shortages of on-call specialists at their hospitals (ACEP, 2004; Vanlandingham et al., 2005). Numerous other studies and surveys have investigated the shortage of on-call specialists, finding that the problem extends across many different specialties and all regions of the country, and that it appears to be worsening (Green et al., 2005; O’Malley et al., 2005).
Part of the problem is a general shortage of pediatric subspecialists. The number and proportion of pediatric residents choosing advanced training have declined (Health Resources and Services Administration Council on Graduate Medical Education, 2002; O’Leary, 2002). This decline can be attributed at least in part to managed care’s focus on primary care, which has led to reduced support for specialist fellowships and less reimbursement income for specialists (O’Leary, 2002). The American Academy of Pediatrics has called the supply of pediatric subspecialists “a pressing concern” (AAP, 2003).
In August 2001, the National Association of Children’s Hospitals and Related Institutions (NACHRI) surveyed member hospitals to gauge perceptions about the supply of pediatric subspecialists, both nationally and within each hospital’s own market, and to assess hospitals’ physician recruitment and retention efforts. With a 34 percent response rate, the survey showed that the overall vacancy rate for pediatric subspecialists was 11.1 percent, with endocrinology, pulmonology, and neurology being the specialties with the highest vacancy rates. Respondents noted that the most difficult specialties to recruit were neurology, gastroenterology, anesthesiology, and pulmonology. The reasons given for the difficulty most frequently were an overall shortage of qualified candidates, competition from other provider organizations, and low pay relative to job demands. Reasons cited for the perceived shortage of pediatric subspecialists were residents’ reduced interest in the subspecialties and reimbursement and compensation issues (O’Leary, 2002). Indeed, issues surrounding compensation are an important factor. A study by the California Medical Association showed that more than 50 percent
of physicians said they had difficulty receiving reimbursement for insured patients at least 50 percent of the time; the problem of payment is greatly exacerbated when the patient is uninsured. To encourage subspecialists to continue taking ED call, some hospitals have begun paying for this service (Steiger, 2005).
Other forces also contribute to the shortage of on-call specialists to care for patients of all ages. Some speculate that the younger generation of specialists may be less inclined to take call than their more experienced colleagues out of a desire to improve their work–life balance (Salsberg, 2005). Hospital by-laws often require physicians to take ED call for a certain period of time, for example, 15 years, in exchange for admitting privileges. Historically, this arrangement has worked well; it allows hospitals to fill their on-call panel and gives young specialists an opportunity to build up their practices. But with the movement of specialists to large, multispecialty groups, younger physicians no longer need to rely on ED call to supply patients. Hospitals have less leverage in linking admitting privileges to ED call, and many physician groups discourage members from taking ED call (Taheri and Butz, 2004).
Still other physicians drop ED call because of liability concerns. Pediatric emergency cases are especially risky because the patient is often seriously ill or injured; medical records may be scant or nonexistent; treatment may be rendered after hours, when resources for care are less readily available; and the doctor lacks an established relationship with the child and his or her family. The rapidly rising cost of malpractice insurance is a powerful disincentive for specialists to assume liability by treating unknown emergency patients, many of whom are uninsured, may be noncompliant with discharge instructions, and may be difficult to contact regarding follow-up (Green et al., 2005). Seventy-five percent of neurosurgeons no longer operate on children because of liability concerns, sharply reducing the availability of those services for pediatric patients (Glabman, 2005).
The availability of on-call specialists is an issue discussed at length in the committee’s companion report, Hospital-Based Emergency Care: At the Breaking Point, which offers specific recommendations for addressing the problem. One option being discussed by specialty societies is the creation of a specialty in emergency surgery or acute care surgery in which a board-certified general surgeon would receive fellowship training in elective and emergency general surgery, trauma surgery, and surgical critical care. In addition to treating what is conventionally considered “general trauma” (neck, thoracic, and abdominal injuries), the new acute care surgical specialist could also perform selected and limited neurosurgical and orthopedic procedures, with support from fellow surgical specialists (The Committee to Develop the Reorganized Specialty of Trauma Surgical Critical Care and Emergency Surgery, 2005). It is anticipated that acute care surgeons would
treat both adult and pediatric patients. The proposed curriculum for the new specialty was under development at the time of this writing, but pediatric surgery is likely to be an elective option within the fellowship training.
Nurses
There are between 75,000 and 100,000 nurses working in EDs. According to the Emergency Nurses Association (ENA), emergency RNs perform the following tasks: triage, assessment, analysis, nursing diagnosis, planning, implementation of interventions and procedures, administration of medications and other therapies, monitoring of patient status, outcome identification, evaluation of responses, triage and prioritization, preparedness for emergency operations, stabilization and resuscitation, patient education, and crisis intervention for unique patient populations (e.g., sexual assault survivors) (ENA, 1999).
Nurses in EDs are predominantly female (86 percent), have a median age of 40, and are largely non-Hispanic white (88.5 percent). They generally have worked in nursing for less time than other nurses; approximately 30 percent graduated in the last 5 years, compared with 20.6 percent of other nurses. Only 11 percent graduated 26 or more years ago, compared with 22.6 percent of all nurses (DHHS, 2000). Nurses in EDs report feeling that they are under great stress significantly more often than do RNs in other settings: in one study, 37 percent of ED RNs reported feeling under great stress “almost every day,” compared with 30 percent of other RNs. Surveys show that nurses in the ED tend to be more pressed for time and have heavier workloads than those working in other settings (New York State Education Department, 2003).
Training
To become a nurse, an individual typically completes one of two courses of study, an associate degree nurse (ADN) or a bachelor of science nurse (BSN). The ADN course is typically a 2-year degree program focused on the practical applications of nursing. The BSN is a 4-year program that expands into the theoretical realms of patient care. In recent years there has been a push to mandate that the BSN be a minimum requirement for being a professional nurse; this issue is still under debate. After graduation from one of these programs, nurses must take the board examination to become an RN.
Courses mandated at the basic level include hazardous materials awareness, fire and safety, CPR, and infection control. Requirements for more advanced coursework vary from hospital to hospital, although almost all require advanced cardiac life support for ED nurses working in resuscitation
areas or administering intravenous (IV) sedation. Some hospitals require new ED hires to take a critical care course, depending upon their previous experience.
ED nurses wishing to obtain additional credentials in emergency nursing may become certified emergency nurses (CENs), awarded to nurses that pass the qualifying examination by the Board of Certification for Emergency Nursing. However, most nurses working in EDs are not certified as CENs. In 2004, 13,115 nurses nationwide were credentialed as CENs. There are also other advanced degree options for nurses, including masters and doctoral degree programs with various areas of specialization and practice. Many nursing management positions require advanced degrees.
Some ED nurses specialize in caring for children and may work in pediatric EDs, but there is no certification available in pediatric emergency nursing, and very little data exist regarding these nurses. State boards of nursing may require PALS or APLS for nurses providing sedation. Pediatric EDs are likely to require advanced pediatric courses for their nurses, and may even require advanced training in neonatal resuscitation. Some ED nurses may participate in a number of other pediatric continuing education courses, including the emergency nursing pediatric course. It is unclear how many nurses are required to participate in pediatric continuing education and how often.
Staffing Challenges
The nursing shortage in both hospital and nonhospital settings has been the subject of press reports and research articles for years (GAO, 2001; Gerson and Oliver, 2005). Although there have been nursing shortages in the past, many believe that the current one is different in that it is not rooted in cyclical changes (Schriver et al., 2003). Today, fewer individuals are choosing nursing as a profession than in the past, in part because of the increased professional opportunities for women and the limited number of nursing education slots resulting from a shortage of nursing faculty. The nursing shortage has led to problems for hospitals and medical centers in all units, and the problem is only expected to worsen in the future as the demand for nursing services increases with the aging of the population. The importance of an adequate-sized nursing staff cannot be overstated. A number of robust research studies have shown a direct link between nurse staffing levels and patient outcomes (Aiken et al., 2002a,b; Needleman et al., 2002).
EDs are not immune to the nursing shortage. Nationwide, it is estimated that 12 percent of nursing positions for which hospitals are actively recruiting are in EDs. This makes the ED the third most common source of nursing position openings in hospitals (following general medical/surgical and critical care units). In a survey of hospitals in New York City, 83 percent
reported that they were actively recruiting for nurses in their ED (Greater New York Hospital Association, 2004). A 2005 survey of EDs by the ENA found that 26 percent of EDs had an RN vacancy rate of 10 percent or higher (ENA, 2006).
The impact of the nursing shortage on ED patient care has not been effectively evaluated; however, many speculate that the shortage has a negative impact for two reasons. First, as with other areas of the hospital, if the ED lacks appropriate nursing levels, patients will not receive the proper care or attention. For example, a triage nurse may be overwhelmed by the number of patients he or she has to evaluate and may miss an important sign of a severe illness or injury. Moreover, procedures performed on children less than 5 years of age, for example, IV starts and catheterizations, generally require more staffing to keep the child calm and manageable. Second, the nursing shortage adds to the problem of ED crowding. If nurses are not available to staff inpatient beds, admitted patients from the ED may become boarders, waiting for an available bed.
Other Medical Professionals in the ED
A number of other medical professionals may deliver care to children in the ED. Some might be surprised to hear that nearly 9 percent of ED patients are seen by an EMT (McCaig and Burt, 2005). These EMT-trained ED technicians are able to perform basic emergency care in the ED setting, allowing nurses and physicians more time to treat complex cases and perform more intensive procedures. The scope of practice for such personnel is limited, but has increased in some EDs to include intravenous infusions, splinting, and phlebotomy (Franks et al., 2004).
Approximately 7 percent of ED patients are seen by a physician assistant (PA), generally in addition to seeing a physician and/or nurse. PAs provide medical care to patients under the supervision of a physician, and their specialty is the same as that of their supervising physician. PAs must be granted clinical privileges at the hospital in which they work and can prescribe medication in most states. There are three PA educational programs in the United States offering specializations in emergency medicine, although PAs do not need to graduate from such a program to practice in EDs. In 2003, approximately 4,508 PAs (9.8 percent) worked in EDs. More than 4,600 PAs had a primary specialty in emergency medicine (10 percent). The majority of PAs working in EDs are emergency medicine specialists (93.6 percent); fewer than 1 percent are pediatric specialists (2003 Physician Assistant Census Survey, calculations by American Association of Physician Assistants staff).
Only about 2 percent of patients see a nurse practitioner (NP) during their ED visit (McCaig and Burt, 2005). NPs are master’s-prepared RNs
who provide significant medical care to patients. Some states require NPs to work under the supervision of a physician, while others do not. There is no national certification in emergency care for NPs, but they may obtain training in emergency care skills through university-based programs, continuing education, and work experiences (Cole et al., 1999). Advanced practice nurses (APNs) in emergency settings were most likely to report certification as a family NP (43 percent), acute care NP (13 percent), adult care NP (12 percent), critical nurse specialist (CNS) (9 percent), or pediatric NP (7 percent) (ENA, 2003).
In the 1970s, a limited number of hospitals began integrating pharmacists into their ED staff. Clinical pharmacy specialists (CPSs) who work in EDs typically have a doctor of pharmacy degree and have completed a 1-year residency. Traditionally, CPSs in EDs helped with medication billing and inventory control, but in recent years their role in the ED has expanded. With the growing number of drugs available and the increased complexity of drug selection, administration, and monitoring, some EDs use a pharmacist as part of the care team. Such use of pharmacists offers the potential to reduce the high number of medication errors that occur in that environment.
Still, the prevalence of pharmacists, particularly full-time pharmacists, in EDs remains low. A 2001 survey of directors of pharmacy in hospitals with at least one accredited pharmacy residency program was conducted to ascertain the prevalence and characteristics of pharmaceutical services in EDs nationwide. Only 3 percent of respondents reported having a dedicated pharmacist in an ED satellite pharmacy, while 14 percent reported having a dedicated pharmacist who provided services to ED patients (Thomasset and Faris, 2003). But the demand for pharmacists may grow over the next few years as a result of the Joint Commission on Accreditation of Health Care Organizations’ (JCAHO) 2005 National Patient Safety Goals and Requirements, which call for complete and accurate medication reconciliation across the continuum of care (JCAHO, 2005).
Efforts to integrate clinical pharmacists into the ED care team have shown some success. For example, one study assessed the impact of having a clinical pharmacist integrated into the care team at a level I trauma center. Responsibilities of this pharmacist included clinical consultations, patient education, order screening, dispensing of drugs, medication preparation, resuscitation response, staff education, patient care, and emergency preparedness. Inclusion of the clinical pharmacist on the care team resulted in improved medical care (reduction in voluntary reporting of medical errors) and the imparting of knowledge to ED personnel. It also reduced institutional expenditures; by encouraging physicians to modify prescribing practices, the pharmacist reduced the ordering of high-cost medications, for an estimated savings of $100,000 over 1 year (Fairbanks et al., 2004).
Another study compared the effectiveness of having a pharmacist collect patients’ medication histories with that of the institution’s standard approach of a nurse-obtained medication history. Results showed that when the pharmacist obtained the history, more discrepancies between patients’ reported home medications and initial hospital orders were identified, and a higher percentage of patients received clinical interventions. Having pharmacists take medical histories was also more time-efficient (Nester and Hale, 2002). At another hospital, ED cost savings were realized when pharmacists performed clinical interventions, such as medication selection and dosing changes. Cost savings were also realized by reducing the ED satellite inventory; pharmacists noted that duplicate medications in the same drug class were unwarranted for a single- or double-dose regimen (Levy, 1993).
Some pediatric facilities (typically children’s hospitals and general hospitals with advanced pediatric capabilities) also employ suture technicians to assist with pediatric wound repair (Apolo and DiCocco, 1988). These technicians, often EMTs or nurses, receive training with general, reconstructive, and plastic surgeons on wound repair and use a variety of techniques to reduce pain and anxiety in children needing suturing. Because these technicians provide a large number of sutures (one hospital estimated that suture technicians provided 450–700 sutures per month), they are able to attain a high skill level in suturing. Additionally, the use of suture technicians helps free up the time of ED physicians so they can provide care to other patients (Akron Children’s Hospital, 2005).
Skill Retention and Performance
As with EMTs, skill retention for ED providers can be a problem. Only about 10 percent of pediatric patients in the ED are classified as “emergent,” meaning that care must be provided within 15 minutes (McCaig and Burt, 2005). Therefore, only a small percentage of ED visits are critical pediatric cases. As a result, deterioration of skills can be a problem. Many ED providers have infrequent contact with and rarely perform life support interventions for children. Research confirms this concern; 1 year after CPR training, for example, physician and nurse retention of CPR skills deteriorates and can even fall to pretraining levels (Gass and Curry, 1983; Mancini and Kaye, 1985).
It is difficult to say precisely how well ED providers deliver care to pediatric patients in the absence of reliable data. The limited information available on physician performance tends to focus on intubation of pediatric patients in the ED. Some findings indicate that EM and pediatric emergency medicine fellows are generally successful in performing pharmacologically assisted intubation, an airway intervention that is frequently used in the ED (Tayal et al., 1999; Sagarin et al., 2002). However, success rates for
neonatal endotracheal intubation were found to be low, despite providers’ high levels of confidence in performing the procedure (Falck et al., 2003; Leone et al., 2005). Additionally, a study of pediatric patient encounters during EM residents’ pediatric emergency medicine rotation found deficiencies in critical care procedures, resuscitations, child abuse evaluations, and neonatal evaluations (Chen et al., 2004). Again, though, the majority of ED physicians are not EM or pediatric emergency medicine physicians, and it is difficult to assess their performance.
As mentioned in Chapter 2, it is known that the care children receive in the ED can vary considerably. Substantial variations exist among physicians of different specialties in the management of a number of illnesses and injuries, including fever (Isaacman et al., 2001), croup (Hampers and Faries, 2002), splenic injury (Davis et al., 2005), diabetic ketoacidosis (Glaser et al., 1997), bronchiolitis (Mansbach et al., 2005), and febrile seizures (Hampers et al., 2000), as well as in sedation treatment (Babl et al., 2005). These variations may be due to differences in specialty training. In some cases, guidelines are available to help in treatment decisions, but most are not used by the physician (Isaacman et al., 2001; Han et al., 2003; Orr et al., 2006).
SUPPORTING THE WORKFORCE TO IMPROVE PEDIATRIC EMERGENCY CARE
The committee is concerned about the problem of ensuring an adequate supply of highly trained professionals for every category of emergency care provider. In its companion reports on prehospital and ED care, the committee recommends that that the federal government undertake a detailed assessment of the capacity, trends, and future needs of the emergency care workforce, including providers with pediatric expertise. In this report, however, the committee focuses on the need to support providers in their ability to deliver appropriate pediatric emergency care, for which it proposes a three-pronged approach.
Increasing Pediatric Training
There are no national standards for the core competencies of training in pediatric emergency care. Residency programs, medical schools, nursing schools, states, EMS agencies, and hospitals have varying pediatric education and training requirements and opportunities for providers. In some cases, pediatric training is intensive; as discussed above, however, pediatric training often makes up a small portion of total training time.
The committee believes all emergency care providers should possess a certain level of competency to deliver care to children. Research has shown
that pediatric training works, at least initially, to improve both the competency and confidence of providers in caring for pediatric patients. Improving the confidence of providers may reduce the reluctance of some to administer treatment to children, thereby eliminating some of the disparities in care between adult and pediatric patients. But continuing education is also essential to maintain these skills and competencies. To increase the pediatric emergency care training that providers receive, the committee recommends that every pediatric- and emergency care–related health professional credentialing and certification body define pediatric emergency care competencies and require practitioners to receive the level of initial and continuing education necessary to achieve and maintain those competencies (4.1). The major professional organizations that create and update core content specific to the emergency medicine curriculum (ACEP, Society for Academic Emergency Medicine [SAEM], Council of Emergency Medicine Residency Directors [CORD], ABEM, Emergency Medicine Residents Association [EMRA], and Residency Review Committee for Emergency Medicine [RRC-EM]) should ensure that EM residents receive the training necessary to meet a defined pediatric competency level considering the frequency with which children seek care in EDs. Similar improvements are needed in the EM curriculum for pediatric residents. The ENA should define a pediatric competency level, review the amount of pediatric training nurses currently receive, and address any gaps. States should adopt the national standard curriculum developed by NHTSA, which includes pediatric training and pediatric continuing education components. Residency programs, medical and nursing schools, and states should ensure that individuals with pediatric expertise conduct the pediatric training. Further, states and provider organizations should ensure that all certification examinations are designed to test providers’ pediatric competencies. Individuals who answer all pediatric questions incorrectly should not receive certification. All of these organizations should also explore ways to test pediatric competencies at regular intervals.
Despite the strong growth of EM residency programs, a large number of emergency physicians, particularly in rural EDs, have not undergone EM residency training. Many nurses working in EDs, particularly in rural settings, have not sought CEN certification and have not taken the emergency nursing pediatric course. To ensure that these professionals receive proper pediatric emergency medicine education, JCAHO and state licensing bodies should evaluate ED staff’s pediatric training for certification; similarly, pediatricians working in the ED should be assessed on their EM training.
Provider organizations, such as hospitals and EMS agencies, must also ensure that their workforce is well prepared to handle pediatric patients. Strategies for continuing education should be developed by provider organizations and should reflect the type of setting in which providers work. For example, the continuing education needed at a dedicated pediatric ED may
be very different from that needed at a general ED. Continuing education classes must be conducted regularly, as skill maintenance declines over a relatively short time period. Furthermore, courses should include a major focus on the care of infants and young children, given that they constitute the largest single group making pediatric ED visits and require care that is most different from that of adults.
Continuing education courses are critical for all emergency care providers, particularly those who rarely see children, as well as for hospitals that lack pediatric specialists. Even if critically ill pediatric patients are transported to dedicated pediatric EDs, ED staff at all hospitals need to maintain a basic level of competency to recognize and stabilize those who are critically ill or injured until transport to a higher level of care is available. High-fidelity simulation models, to the extent available, should be used for continuing education to provide as realistic an event as possible.
Developing Clinical Practice Guidelines for Pediatric Emergency Care
Treatment patterns for pediatric patients can vary widely among providers. In some cases, this variation is due to providers’ lack of education. Often, however, it is the result of the absence of evidence-based clinical guidelines for pediatric patients.
Clinical practice guidelines assist providers in decision making regarding the appropriate care for specific clinical circumstances, and their use has been shown to improve the quality of care (Grimshaw and Russell, 1993). Ideally, practice guidelines are based on scientific evidence or predictability. The Institute of Medicine’s (IOM) Committee on Clinical Practice recommended the implementation of evidence-based clinical practice guidelines because of their potential to improve care. However, only a limited number of nationally recognized pediatric emergency care practice guidelines exist; a 2001 review of the 1,053 practice guidelines in the national Guidelines Clearinghouse found only 15 (Moody-Williams et al., 2002).
The committee believes clinical guidelines should be science-based through use of an evidence evaluation process for several reasons. First, research indicates that clinical guidelines based on research evidence are more likely to be used than those developed in the absence of such evidence (Grol et al., 1998). Moreover, an evidence evaluation process helps ensure that clinical guidelines and standards are based on scientific evidence that is most likely to be correct. Under this process, all research studies in a particular area, for example, asthma care in the ED, are reviewed and ranked according to the validity of study findings. Studies using randomized controlled trials are ranked higher than those based on expert opinion. These rankings are then tied to grades of recommendations. For example, a systematic review documenting homogeneity of results from a large number of high-quality
randomized controlled trials yields the least biased estimate of the effect of an intervention; those results are assigned a high recommendation grade and then used in the development of clinical practice guidelines and standards of care. Reviews of studies using less rigorous methods are given a lower recommendation grade and are not used to develop guidelines.
Use of a formal or systematic evidence evaluation process for emergency care research has been limited. In 1998 and again in 2005, however, the Neonatal Resuscitation Program Steering Committee of the AAP and the National Pediatric Resuscitation Subcommittee of the American Heart Association undertook a review of the scientific literature on pediatric resuscitation. They evaluated the quality of the evidence supporting practices employed at the time and changes to those practices. The first evidence evaluation process culminated in the publication of Guidelines 2000 for Emergency Cardiovascular Care and Resuscitation: International Consensus on Science (AAP, 2005b). The second set of guidelines was released in January 2006.
In 2001, the Health Resources and Services Administration (HRSA), NHTSA, and The Robert Wood Johnson Foundation convened a panel of experts in managed care, quality improvement, and EMS to review the literature and discuss critical issues related to practice guidelines and performance measurement in pediatric emergency care. The panel recommended the development of pediatric emergency care guidelines and suggested how the guidelines should be developed (e.g., a broad consensus process and a scientific approach), as well as what characteristics the guidelines should have (e.g., they should be flexible and not unduly complex). In 2002, the EMS-C program initiated the Clinical Practice Guidelines for Pediatric Emergency Care demonstration project, which provided funding for two projects to help develop practice guidelines. One project is investigating rehydration of children with moderate dehydration due to acute gastroenteritis; the other is evaluating the use of the National Heart, Lung and Blood Institute’s pediatric asthma guideline in five adult EDs and investigating patient outcomes (MCHB, 2004b). The committee believes more such efforts are necessary. The committee therefore recommends that the Department of Health and Human Services collaborate with professional organizations to convene a panel of individuals with multidisciplinary expertise to develop, evaluate, and update clinical practice guidelines and standards of care for pediatric emergency care (4.2). A number of agencies within the Department of Health and Human Services (DHHS) could lead this effort, including the Food and Drug Administration (FDA), HRSA, and the Agency for Healthcare Research and Quality (AHRQ). Funding for the effort should be provided by DHHS. It will be up to the specialists from various professional organizations to evaluate the evidence in order to develop, evaluate, and update the clinical practice guidelines and standards for pediatric emergency
care. The effort should be multidisciplinary and multiorganizational to promote consensus and uniformity. The more organizations are involved in the development, the more likely it will be that the guidelines will be used in practice in various disciplines.
Unless there is a commitment to funding pediatric emergency medicine research, however, there will not be an adequate evidence base from which to derive practice guidelines. The issue of research and research funding is discussed in depth in Chapter 7.
Providing Pediatric Leadership in EMS Agencies and EDs
Simply recommending more training and the development of guidelines is not enough. Someone must be responsible at the provider level for ensuring that continuing education opportunities are available and well attended. Similarly, the development of clinical guidelines is useless unless their widespread adoption by providers is ensured. To these ends, the committee believes pediatric leadership within each provider organization is needed. Therefore, the committee recommends that emergency medical services agencies appoint a pediatric emergency coordinator and hospitals appoint two pediatric emergency coordinators—one a physician—to provide pediatric leadership for the organization (4.3). Hospitals could choose personnel for the two coordinator positions based on available resources; often they will be filled by a physician and a nurse, but other models are possible (e.g., a physician and an EMT-P). The activities of the pediatric coordinators should be a component of medical oversight.
The pediatric coordinator position is not necessarily intended to be full-time, but instead a shared role. Still, the coordinators would have a number of responsibilities that would include ensuring adequate skill and knowledge among fellow ED or EMS providers; overseeing pediatric quality improvement initiatives; ensuring the availability of pediatric medications, equipment, and supplies; ensuring that fellow providers are following clinical practice guidelines; representing the pediatric perspective in the development of hospital or EMS protocols or procedures, for example, for family-centered care; participating in pediatric research efforts; and developing prevention programs for the hospital or EMS agency. The pediatric coordinator would monitor pediatric care issues and present concerns to the organization’s leadership when a problem with pediatric care was identified. For example, if medication errors for children in the ED appeared to be rising, the pediatric coordinator should bring this to the attention of hospital administrators. Additionally, pediatric coordinators would liaison in quality improvement efforts and education with community hospitals lacking pediatric resources.
There are two reasons why it is important for hospitals to have two
pediatric coordinators. First, as noted, the coordinator positions would not be full-time. However, the committee envisions the coordinator role as encompassing many responsibilities—enough that two coordinators would be necessary. Second, it is important for hospitals to have a physician serve as a pediatric coordinator rather than having the role filled by a lone nurse or EMT. While the nurse–physician relationship has generally evolved over time from an authoritarian to a collaborative one (Pavlovich-Danis et al., 2005), remnants of the old dynamic may prevent some physicians from taking suggestions for improving pediatric care amiably from nurses or EMTs and vice versa. Certainly both coordinators should collaborate on pediatric improvement initiatives within the ED.
The concept of a pediatric coordinator is not new. In fact, since 1983 all Los Angeles hospitals designated as emergency departments approved for pediatrics (EDAPs) have been required to have a pediatric liaison nurse (PdLN) on staff, similar to the pediatric coordinator proposed here. Additionally, the AAP/ACEP 2001 Guidelines for Preparedness for the Care of Children in the Emergency Department contain a recommendation regarding the use of a physician coordinator and a nurse coordinator for pediatric care. The guidelines stipulate that the physician coordinator may be a staff physician with other responsibilities in the ED, but should meet the criteria for credentialing as a specialist in emergency care, pediatric emergency medicine, or pediatrics and have a special interest, knowledge, and skill in emergency medical care of children. The guidelines stipulate further that the nurse coordinator should have an interest, knowledge, and skill in emergency care and resuscitation of infants and children as demonstrated by training, clinical experience, or focused continuing nursing education. The position includes such duties as coordinating pediatric quality improvement, serving as a liaison to in-hospital and out-of-hospital pediatric care committees, and facilitating nursing continuing education in pediatrics (AAP, 2001). Pediatric coordinators for EMS agencies appear to be less common, but are necessary to advocate for improved competencies and the availability of resources for pediatric patients. Preferably, prehospital pediatric coordinators would be EMT-Ps with the interest, knowledge, and skills necessary to deliver care to children. EMS pediatric coordinators would have many of the same responsibilities as physician and nurse pediatric coordinators.
One children’s hospital currently employs two full-time coordinators who are responsible for both EMS and hospital-based emergency care services. The hospital-based coordinator, an EMT-P, spends the majority of his time coordinating the PALS and other education programs within the hospital. He also leads a task force that examines all resuscitation events and reviews policies and procedures for resuscitation. His duties include making sure that resuscitation equipment is available and that all crash carts are uniform across all hospital floors. The coordinator reports to
the administrator of the ED, as well as to the division chief of emergency medicine. The second coordinator focuses primarily on coordinating PALS and other continuing education courses for prehospital providers (Personal communication, D. LaCovey, March 13, 2006).
Approximately 18 percent of hospitals have a pediatric physician coordinator on staff; 12 percent have a nurse coordinator (Gausche-Hill et al., 2004). In Los Angeles, however, the hospitals that are best prepared for pediatric emergencies—those designated as EDAPs—are required to have pediatric coordinator positions. But pediatric coordinators are arguably most important for smaller EDs and EMS agencies that lack strong pediatric expertise; these are the facilities most in need of immediate pediatric leadership. They may not be able to staff the pediatric coordinator position with a physician that is an EM physician or a physician with pediatric expertise; however, the position should be assigned to a physician with the interest and desire to improve pediatric emergency care within the facility.
SUMMARY OF RECOMMENDATIONS
4.1 Every pediatric- and emergency care–related health professional credentialing and certification body should define pediatric emergency care competencies and require practitioners to receive the level of initial and continuing education necessary to achieve and maintain those competencies.
4.2 The Department of Health and Human Services should collaborate with professional organizations to convene a panel of individuals with multidisciplinary expertise to develop, evaluate, and update clinical practice guidelines and standards of care for pediatric emergency care.
4.3 Emergency medical services agencies should appoint a pediatric emergency coordinator, and hospitals should appoint two pediatric emergency coordinators—one a physician—to provide pediatric leadership for the organization.
REFERENCES
AAP (American Academy of Pediatrics). 2000. Access to pediatric emergency medical care. Pediatrics 105(3 Pt. 1):647–649.
AAP. 2001. Care of children in the emergency department: Guidelines for preparedness. Pediatrics 107(4):777–781.
AAP. 2003. Council of Medical Specialty Societies: Workforce Questions. Washington, DC: AAP.
AAP. 2005a. About PEPP: History of PEPP. [Online]. Available: http://www.peppsite.com/about_history.cfm [accessed October 31, 2005].
AAP. 2005b. Evidence-based Guidelines Process. [Online]. Available: http://www.aap.org/nrp/science/science_evidenceguide.html [accessed March 9, 2005].
ABEM (American Board of Emergency Medicine). 2004. Written Certification Examination Description and Content Specifications. [Online]. Available: http://www.abem.org/public/portal/alias_Rainbow/lang_en-US/tabID_3368/DesktopDefault.aspx#one [accessed August 23, 2004].
ABMS (American Board of Medical Specialties). 2002. Which Medical Specialist Is for You? Evanston, IL: ABMS.
ABMS. 2003. ABMS Annual Report and Reference Handbook. Evanston, IL: ABMS.
ACEP (American College of Emergency Physicians). 2004. Two-Thirds of Emergency Department Directors Report On-Call Specialty Coverage Problems. [Online]. Available: http://www.acep.org/1,34081,0.html [accessed September 28, 2004].
ACGME (Accreditation Council for Graduate Medical Education). 2004. Program Requirements for Residency Education in Pediatric Emergency Medicine. [Online]. Available: http://www.acgme.org/downloads/RRC_progReq/114pr698.pdf [accessed August 20, 2004].
Aiken LH, Clarke SP, Sloane DM. 2002a. Hospital staffing, organization, and quality of care: Cross-national findings. International Journal for Quality in Health Care 14(1):5–13.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. 2002b. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association 288(16):1987–1993.
Akron Children’s Hospital. 2005. Suture Program. [Online]. Available: http://www.akronchildrens.org/cms/site/d0d9e25d302b66b8/index.html [accessed February 27, 2006].
AMA (American Medical Association). 2003. Physician Characteristics and Distribution in the U.S.: 2004 Edition. Chicago, IL: AMA.
The American Board of Surgery. 2004. Booklet on Certification in Surgical Specialties: Information Regarding Requirements and Examinations 2004–2005. Philadelphia, PA: The American Board of Surgery.
The American Board of Surgery. 2005. Booklet of Information 2005. Philadelphia, PA: The American Board of Surgery.
Apolo JO, DiCocco D. 1988. Suture technicians in a children’s hospital emergency department. Pediatric Emergency Care 4(1):12–14.
Armon BD, Coren JS. 2005. Basking in the moonlight. Unique Opportunities. [Online]. Available: http://www.uoworks.com/articles/legal.moonlighting.html [accessed January 31, 2007].
Babl FE, Vinci RJ, Bauchner H, Mottley L. 2001. Pediatric per-hospital advanced life support care in an urban setting. Pediatric Emergency Care 17(1):5–9.
Babl FE, Puspitadewi A, Barnett P, Oakley E, Spicer M. 2005. Preprocedural fasting state and adverse events in children receiving nitrous oxide for procedural sedation and analgesia. Pediatric Emergency Care 21(11):736–743.
Boswell W, McElveen N, Sharp M, Boyd CR, Frantz EI. 1995. Analysis of prehospital pediatric and adult intubation. Air Medical Journal 14:125–127.
Bureau of Labor Statistics. 2002. Occupational Outlook Handbook, 2002–2003 Edition: Emergency Medical Technicians and Paramedics. Washington, DC: U.S. Department of Labor.
Bureau of Labor Statistics, U.S. Department of Labor. 2004. Emergency medical technicians and paramedics. In: Occupational Outlook Handbook, 2004–2005 Edition. Washington, DC: U.S. Department of Labor.
Chen EH, Shofer FS, Baren JM. 2004. Emergency medicine resident rotation in pediatric emergency medicine: What kind of experience are we providing? Academic Emergency Medicine 11(7):771–773.
Christopher N. 2000. Pediatric emergency medicine education in emergency medicine training programs. Academic Emergency Medicine 7(7):797–799.
Cole FL, Ramirez E, Luna-Gonzales H. 1999. Scope of Practice for the Nurse Practitioner in the Emergency Setting. Des Plaines, IL: ENA.
The Committee to Develop the Reorganized Specialty of Trauma Surgical Critical Care and Emergency Surgery. 2005. Acute care surgery: Trauma, critical care, and emergency surgery. The Journal of Trauma 58(3):614–616.
Davis DH, Localio AR, Stafford PW, Helfaer MA, Durbin DR. 2005. Trends in operative management of pediatric splenic injury in a regional trauma system. Pediatrics 115(1):89–94.
DHHS (U.S. Department of Health and Human Services). 2000. National Sample Survey of Registered Nurses. Rockville, MD: HRSA, Bureau of Health Professions, National Center for Health Workforce Analysis.
Doran JV, Tortella BJ, Drivet WJ, Lavery RF. 1995. Factors influencing successful intubation in the prehospital setting. Prehospital Disaster Medicine 10(4):259–264.
DOT (Department of Transportation). 1998. EMT-Paramedic: National Standard Curriculum. Washington, DC: DOT.
EMS Insider. 2005. EMS Employers Struggle with Paramedic Shortages. [Online]. Available: http://www.jems.com/insider/4_04.html [accessed April 4, 2005].
ENA (Emergency Nurses Association). 1999. Scope of Emergency Nursing Practice. Des Plains, IL: ENA.
ENA. 2003. Advanced Practice in Emergency Nursing. Des Plains, IL: ENA.
ENA. 2006. ENA 2005 National Emergency Department Benchmark Guide. Des Plaines, IL: ENA.
Fairbanks RJ, Hays DP, Webster DF, Spillane LL. 2004. Clinical pharmacy services in an emergency department. American Journal of Health-System Pharmacy 61(9):934–937.
Falck AJ, Escobedo MB, Baillargeon JG, Villard LG, Gunkel JH. 2003. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics 112(6): 1242–1247.
Federiuk CS, O’Brien K, Jui J, Schmidt TA. 1993. Job satisfaction of paramedics: The effects of gender and type of agency of employment. Annals of Emergency Medicine 22(4):657–662.
Franks PE, Kocher N, Chapman S. 2004. Emergency Medical Technicians and Paramedics in University of California. San Francisco, CA: San Francisco Center for the Health Professions.
GAO (General Accountability Office). 2001. Emerging Nurse Shortage. Washington, DC: General Accountability Office.
Gass DA, Curry L. 1983. Physicians’ and nurses’ retention of knowledge and skill after training in cardiopulmonary resuscitation. Canadian Medical Association Journal 128(5):550–551.
Gausche M. 1997. Differences in the out-of-hospital care of children and adults: More questions than answers. Annals of Emergency Medicine 29(6):776–779.
Gausche M, Tadeo R, Zane M, Lewis R. 1998. Out-of-hospital intravenous access: Unnecessary procedures and excessive cost. Academic Emergency Medicine 5(9):878–882.
Gausche-Hill M. 2000. Pediatric continuing education for out-of-hospital providers: Is it time to mandate review of pediatric knowledge and skills? Annals of Emergency Medicine 36(1):72–74.
Gausche-Hill M, Lewis R, Schmitz C. 2004. Survey of US Emergency Departments for Pediatric Preparedness: Implementation and Evaluation of Care of Children in the Emergency Department: Guidelines for Preparedness. Unpublished results.
Gerson J, Oliver T. 1995. Addressing the Nursing Shortage. Washington, DC: Kaiser Family Foundation.
Glabman M. 2005. Specialist shortage shakes emergency rooms; more hospitals forced to pay for specialist care. The Physician Executive 6–11.
Glaeser P, Linzer J, Tunik M, Henderson D, Ball J. 2000. Survey of nationally registered emergency medical services providers: Pediatric education. Annals of Emergency Medicine 36(1):33–38.
Glaser NS, Kuppermann N, Yee CK, Schwartz DL, Styne DM. 1997. Variation in the management of pediatric diabetic ketoacidosis by specialty training. Archives of Pediatrics & Adolescent Medicine 151(11):1125–1132.
Graham CJ, Stuemky J, Lera TA. 1993. Emergency medical services preparedness for pediatric emergencies. Pediatric Emergency Care 9(6):329–331.
Greater New York Hospital Association. 2004. Survey of Nurse Staffing in GNYHA Member Hospitals, 2003. [Online]. Available: http://www.gnyha.org/pubinfo/2005_Nurse_Staffing_Survey.pdf [accessed May 2006].
Green L, Melnick GA, Nawathe A. 2005. On-Call Physicians at California Emergency Departments: Problems and Potential Solutions. Oakland, CA: California Healthcare Foundation.
Grimshaw JM, Russell IT. 1993. Effect of clinical guidelines on medical practice: A systematic review of rigorous evaluations. Lancet 342(8883):1317–1322.
Grol R, Dalhuijsen J, Thomas S, Veld C, Rutten G, Mokkink H. 1998. Attributes of clinical guidelines that influence use of guidelines in general practice: Observational study. British Medical Journal 317(7162):858–861.
Hall WL II, Myers JH, Pepe PE, Larkin GL, Sirbaugh PE, Persse DE. 2004. The perspective of paramedics about on-scene termination of resuscitation efforts for pediatric patients. Resuscitation 60(2):175–187.
Hampers LC, Faries SG. 2002. Practice variation in the emergency management of croup. Pediatrics 109(3):505–508.
Hampers LC, Trainor JL, Listernick R, Eddy JJ, Thompson DA, Sloan EP, Chrisler OP, Gatewood LM, McNulty B, Krug SE. 2000. Setting-based practice variation in the management of simple febrile seizure. Academic Emergency Medicine 7(1):21–27.
Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME, Orr RA. 2003. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics 112(4):793–799.
Health Resources and Services Administration Council on Graduate Medical Education. 2002. 2002 Summary Report. Rockville, MD: Health Resources and Services Administration.
Henderson DP. 1998. Education of paramedics in pediatric airway management effects of different retaining methods on self-efficacy and skill retention. Academic Emergency Medicine 5(5):429.
Holliman CJ, Wuerz RC, Chapman DM, Hirshberg AJ. 1997. Workforce projections for emergency medicine: How many emergency physicians does the United States need? Academic Emergency Medicine 4(7):725–730.
Isaacman DJ, Kaminer K, Veligeti H, Jones M, Davis P, Mason JD. 2001. Comparative practice patterns of emergency medicine physicians and pediatric emergency medicine physicians managing fever in young children. Pediatrics 108(2):354–358.
JCAHO (Joint Council on Accreditation of Healthcare Organizations). 2005. 2005 Hospitals’ National Patient Safety Goals. [Online]. Available: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_hap.htm [accessed August 9, 2005].
Kaji A, Stevens C. 2002. Moonlighting and the emergency medicine resident. Annals of Emergency Medicine 40(1):63–66.
Leone TA, Rich W, Finer NN. 2005. Neonatal intubation: Success of pediatric trainees. The Journal of Pediatrics 146(5):638–641.
Levy DB. 1993. Documentation of clinical and cost-saving pharmacy interventions in the emergency room. Hospital Pharmacy 28(7):624–627, 630–634.
Lillis KA, Jaffe DM. 1992. Prehospital intravenous access in children. Annals of Emergency Medicine 21(12):1430–1434.
Ludwig S, Fleisher G, Henretig F, Ruddy R. 1982. Pediatric training in emergency medicine residency programs. Annals of Emergency Medicine 11(4):170–173.
Macasaet A, Zun A. 2005. The on-call physician. Emedicine.Com. [Online.] Available: http:// www.emedicine.com/emerg/topic878.htm [accessed January 31, 2007].
Mancini ME, Kaye W. 1985. The effect of time since training on house officers’ retention of cardiopulmonary resuscitation skills. American Journal of Emergency Medicine 3(1):31–32.
Mansbach JM, Emond JA, Camargo CA Jr. 2005. Bronchiolitis in U.S. emergency departments 1992 to 2000: Epidemiology and practice variation. Pediatric Emergency Care 21(4):242–247.
McCaig LF, Burt CW. 2005. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. Hyattsville, MD: National Center for Health Statistics.
MCHB (Maternal and Child Health Bureau). 1996. Emergency Medical Services for Children, Annual Report, FY 1996. Rockville, MD: MCHB.
MCHB. 2003. Emergency Medical Services for Children, Annual Report, FY 2003. Rockville, MD: MCHB.
MCHB. 2004a. Emergency Medical Services for Children. Five Year Plan 2001–2005: Midcourse Review. Washington, DC: EMS-C National Resource Center.
MCHB. 2004b. Emergency Medical Services for Children FY 2003 Highlights. [Online]. Available: http://www.mchb.hrsa.gov/programs/emsc/highlights03.htm [accessed December 3, 2005].
Middleton KR, Burt CW. 2006. Availability of Pediatric Services and Equipment in Emergency Departments: United States, 2002–03. Hyattsville, MD: National Center for Health Statistics.
Mishark KJ, Vukov LF, Gudgell SF. 1992. Airway management and air medical transport. Journal of Air Medical Transport 11(3):7–9.
Moody-Williams JD, Krug S, O’Connor R, Shook JE, Athey JL, Holleran RS. 2002. Practice guidelines and performance measures in emergency medical services for children. Annals of Emergency Medicine 39(4):404–412.
Moorhead JC, Gallery ME, Hirshkorn C, Barnaby DP, Barsan WG, Conrad LC, Dalsey WC, Fried M, Herman SH, Hogan P, Mannle TE, Packard DC, Perina DG, Pollack CV Jr, Rapp MT, Rorrie CC Jr, Schafermeyer RW. 2002. A study of the workforce in emergency medicine: 1999. Annals of Emergency Medicine 40(1):3–15.
Murdock TC, Knapp JF, Dowd MD, and Campbell JP. 1999. Bridging the emergency medical services for children information gap. Archives of Pediatric Adolescent Medicine 153(3):281–285.
NAEMT (National Association of Emergency Medical Technicians). 2005. About PPC. [Online]. Available: http://www.naemt.org/PPC/aboutPPC/ [accessed November 4, 2005].
National Capital Consortium Pediatrics Residency. 2004. Pediatric Program Requirements: Residency Review Committee. [Online]. Available: http://www.nccpeds.com/Chief%20Files/RRC%20Requirements.doc [accessed January 11, 2006].
NHTSA (National Highway Traffic Safety Administration). 2006. National Standard Curricula. [Online]. Available: http://www.nhtsa.dot.gov/people/injury/ems/nsc.htm [accessed January 25, 2006].
NHTSA, MCHB (National Highway Traffic Safety Administration, Maternal and Child Health Bureau). 1995. First Responder: National Standard Curriculum. Washington, DC: DOT, DHHS.
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. 2002. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine 346(22):1715–1722.
Nester TM, Hale LS. 2002. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. American Journal of Health-System Pharmacy 59(22):2221.
New York State Education Department. 2003. Registered Nurses in New York State, 2002, Survey Data. Albany, NY: USNY State Education Department.
NREMT (National Registry of Emergency Medical Technicians). 2003. Longitudinal Emergency Medical Technician Attributes and Demographics Survey (LEADS) Data. [Online]. Available: http://www.nremt.org/about/lead_survey.asp [accessed February 24, 2006].
O’Leary K. 2002. The shortage of pediatric subspecialists. Children’s Hospitals Today. Winter 2002. [Online]. Available: http://www.childrenshospitals.net/AM/Template.cfm?Section=Home&CONTENTID=10936&TEMPLATE=/CM/ContentDisplay.cfm [accessed January 31, 2007].
O’Malley AS, Gerland AM, Pham HH, Berenson RA. 2005. Rising Pressure: Hospital Emergency Departments: Barometers of the Health Care System. Washington, DC: The Center for Studying Health System Change.
Orr RA, Han YY, Roth K. 2006. Pediatric transport: Shifting the paradigm to improve patient outcome. In: Fuhrman B, Zimmerman J, eds. Pediatric Critical Care (3rd edition). Mosby, Elsevier Science Health. Pp. 141–150.
Pavlovich-Danis S, Forman H, Simek PP. 2005. The nurse-physician relationship: Can it be saved? Nursing Spectrum 8(5):14–15.
PEPP Program. 2006. What’s new with PEPP 2? PEPP Talk. [Online]. Available: http://www.peppsite.com/newsletter/n_06_January_2006.htm [accessed January 31, 2007].
Ramenofsky ML, Luterman A, Quindlen E, Riddick L, Curreri PW. 1984. Maximum survival in pediatric trauma: The ideal system. The Journal of Trauma 24(9):818–823.
Sagarin MJ, Chiang V, Sakles JC, Barton ED, Wolfe RE, Vissers RJ, Walls RM. 2002. Rapid sequence intubation for pediatric emergency airway management. Pediatric Emergency Care 18(6):417–423.
Salsberg E. 2005. Physician Workforce Issues and Trends: Implications for Surgical Specialties. Presentation at the ACS Meeting on Workforce Issues, Chicago, IL.
Santamaria JP, Abrunzo TJ, Murray R. 1997. Assessment of the Current Status of Continuing Education Training in Pediatric Emergency Care in Emergency Medicine. Washington, DC: ACEP.
Schriver J, Talmadge R, Chuong R, Hedges J. 2003. Emergency nursing: Historical, current, and future roles. Academic Emergency Medicine 10(7):798–804.
Scribano PV, Baker MD, Holmes J, Shaw KN. 2000. Use of out-of-hospital interventions for the pediatric patient in an urban emergency medical services system. Academic Emergency Medicine 7(7):745–750.
Seidel JS. 1986. Emergency medical services and the pediatric patient: Are the needs being met? II. Training and equipping emergency medical services providers for pediatric emergencies. Pediatrics 78(5):808.
Seidel JS, Hornbein M, Yoshiyama K, Kuznets D, Finklestein JZ, St Geme JW Jr. 1984. Emergency medical services and the pediatric patient: Are the needs being met? Pediatrics 73(6):769–772.
Seidel JS, Henderson DP, Ward P, Wayland BW, Ness B. 1991. Pediatric prehospital care in urban and rural areas. Pediatrics 88(4):681.
State of California Employment Development Department Labor Market Information Division. 1995. California Occupational Guide Number 550 (Interest Area 13). [Online]. Available: http://www.calmis.ca.gov/file/occguide/PARAMED.HTM [accessed April 2005].
Steiger B. 2005. ACEP poll: Physician leaders distressed by specialist shortage; on call pay controversial. The Physician Executive 31(3):14–18.
Su E, Mann NC, McCall M, Hedges JR. 1997. Use of resuscitation skills by paramedics caring for critically injured children in Oregon. Prehospital Emergency Care 1(3):123–127.
Su E, Schmidt TA, Mann NC, Zechnich AD. 2000. A randomized controlled trial to assess decay in acquired knowledge among paramedics completing a pediatric resuscitation course. Academic Emergency Medicine 7(7):779–786.
Taheri PA, Butz DA. 2004. Specialist On-Call Coverage of Palm Beach County Emergency Departments. MD Content Report Commissioned by the Palm Beach County Medical Society Services, December 13, 2004.
Tamariz VP, Fuchs S, Baren JM, Pollack ES, Kim J, Seidel JS. 2000. Pediatric emergency medicine education in emergency medicine training programs. SAEM Pediatric Education Training Task Force. Society for Academic Emergency Medicine. Academic Emergency Medicine 7(7):774–778.
Tayal VS, Riggs RW, Marx JA, Tomaszewski CA, Schneider RE. 1999. Rapid-sequence intubation at an emergency medicine residency: Success rate and adverse events during a two-year period. Academic Emergency Medicine 6(1):31–37.
Thomasset KB, Faris R. 2003. Survey of pharmacy services provision in the emergency department. American Journal of Health-System Pharmacy 60(15):1561–1564.
Vanlandingham BD, Powe NR, Diener-West M, Marone B, Rubin H. 2005. Patient Insurance Status and Specialist On-Call Coverage in U.S. Hospital Emergency Departments: A National Study. Presentation at the Academy Health Conference, Boston, MA.
Wilber DQ. 2005, May 7. D.C. paramedic shortage causes concern. The Washington Post. P. B03.
Wolfram RW, Warren CM, Doyle CR, Kerns R, Frye S. 2003. Retention of pediatric advanced life support (PALS) course concepts. Journal of Emergency Medicine 25(4):475–479.
Wood D, Kalinowski EJ, Miller DR. 2004. Pediatric continuing education for EMTs: Recommendations for content, method, and frequency. The National Council of State Emergency Medical Services Training Coordinators. Pediatric Emergency Care 20(4):269–272.
Zaritsky A, French JP, Schafermeyer R, Morton D. 1994. A statewide evaluation of pediatric prehospital and hospital emergency services. Archives of Pediatrics & Adolescent Medicine 148(1):76–81.




































