2
History and Current State of Pediatric Emergency Care
Before setting forth a vision for emergency care in the future, it is important to understand the system that exists today and how it evolved. This chapter describes the development and current state of the emergency care system with respect to children.
The first part of the chapter provides a historical overview of pediatric emergency care. The field is surprisingly young and has trailed the development of the broader emergency care system by a decade or two. In this review, attention is focused on two important topics: (1) the creation, activities, and achievements of the Emergency Medical Services for Children (EMS-C) program, a federal program that aims to ensure essential emergency medical care for ill or injured children and adolescents, and (2) the 1993 Institute of Medicine (IOM) report Emergency Medical Services for Children, which represented the first comprehensive look at the need for and effectiveness of pediatric emergency care services in the United States. An understanding of the development of pediatric emergency care provides a sense of progress, as well as greater insight into the system’s resources, challenges, successes, and failures. In fact, many of the challenges facing the system today are the same ones that existed more than a decade ago.
The second part of the chapter focuses in detail on pediatric emergency care in 2006. It begins with an overview of illness and injury in children based on the most recent national data available. This is followed by a discussion of trends in emergency care use by children.
The chapter continues with an assessment of how well the emergency care system works today. The committee concludes that while considerable progress has been made over the past two decades, the system falls short of
consistently providing quality emergency care to children, and that continued efforts are needed to address its deficiencies.
The chapter concludes with a look at the financing of pediatric emergency care services. This review highlights a number of issues surrounding reimbursement for pediatric services and/or reimbursement at children’s hospitals that have become a growing problem for some providers.
DEVELOPMENT OF EMERGENCY CARE FOR CHILDREN
1940s–1960s: The Beginning of the Modern Emergency Care System
The modern emergency room developed at a time when the specialization of medical practice swept the nation after World War II. As the number of house calls from general physicians declined, patients increasingly turned to the local hospital for treatment. This trend was reinforced by the development of private insurance plans, which geared payments toward hospitals and away from home visits (Rosen, 1995). The development of the emergency room also reflects the passage of the Hill-Burton Act of 1946, which gave states federal grants to build hospitals provided that the states met a variety of conditions, including a community service obligation. Among other things, the community service obligation required hospitals that received the federal funding to maintain an emergency room. This requirement applies to the vast majority of nonprofit U.S. hospitals in operation today (Rosenblatt et al., 2001).
Emergency care as a field advanced as the result of several forces that drew attention to emergency care in the 1950s and 1960s. One was new knowledge about the value of prompt prehospital treatment and transport derived from military experience in Korea. During that conflict, technical innovations such as the creation of battalion aid stations and rapid transport by helicopter to mobile field hospitals were introduced and resulted in dramatically improved survival rates for battle-wounded soldiers. Experience in Vietnam led to advances in trauma care. Surgeons returning to the United States from Korea and Vietnam recognized that the systems developed by the Army for triage, transport, and field surgery could surpass anything available to civilians at home (Rosen, 1995), and they believed that similar innovations could and should be applied to civilian care. Around the same time, advances in cardiac care, such as the creation of “mobile coronary care units,” improved the survival rate of patients prior to reaching the hospital (Pantridge and Geddes, 1967).
Another major turning point was the publication of the landmark National Academy of Sciences (NAS)/National Research Council (NRC) report Accidental Death and Disability: The Neglected Disease of Modern Society
in 1966 (NAS and NRC, 1966). The report described the epidemic of injuries and deaths from automobile crashes and other causes in the United States and lamented the deplorable system for treating those injuries nationwide. In 1966, prehospital and hospital services were largely inadequate or nonexistent. Although a few communities were providing ambulance services through their fire or police departments, it is estimated that morticians provided about half of such services. No specific training was required for ambulance attendants. Most emergency rooms could offer only advanced first aid, and only a few hospitals appeared to have the infrastructure necessary to provide complete care for the critically ill and injured.
The 1970s: Rapid Development of EMS Systems
The 1966 NAS/NRC report stimulated a flood of public and private initiatives designed to enhance highway safety and improve the medical response to accidental injuries. These initiatives included the development of the national trauma system, the creation of the specialty of emergency medicine, and the establishment of federal programs to enhance the nation’s emergency care infrastructure and research base. Perhaps most significant was passage of the Emergency Medical Services Systems (EMSS) Act of 1973 (P.L. 93-154), which created a categorical grant program that led to the nationwide development of about 300 regional EMS systems (IOM, 1993). Despite these achievements, the need to treat pediatric emergencies in a unique way was not fully appreciated at the time. The EMSS Act led to the development of systems that were focused primarily on adult trauma and adult cardiac care. Specialized pediatric needs received little attention; indeed, only limited expertise in pediatric emergency medicine existed (Foltin and Fuchs, 1991).
Nonetheless, some initial efforts were made in the 1970s in certain geographic areas to incorporate the needs of children into emergency medicine and EMS systems. Dedicated pediatric emergency departments (EDs) began to develop, staffed by pediatricians who were willing to devote their full attention to emergency care. Also, some hospitals established pediatric intensive care units (PICUs) and began conducting research on pediatric emergency care. In 1975, Maryland established a regional pediatric trauma center, one of the first in the country. Physicians in Los Angeles, along with local professional societies and the county EMS agency, developed a pediatric-focused training curriculum for paramedics and management guidelines for pediatric emergency care (IOM, 1993). The level of sophistication of emergency rooms generally improved during this time, and the term shifted from “emergency room” to “emergency department” as emergency services began to constitute a full department within hospitals.
The 1980s: Pediatric Emergency Care in Its Infancy
The burgeoning EMS system suffered a setback in 1981 when Congress passed legislation that indirectly resulted in a sharp loss of funding for state EMS activities. Categorical federal funding that had been dedicated to EMS was replaced by the Preventive Health and Health Services Block Grant, which essentially shifted responsibility for EMS from the federal to the state level. Because the states were given greater discretion regarding the use of funds and EMS was a relative newcomer without a significant political constituency, most states chose to spend the money in other areas of need. The immediate impact of the shift to block grants was a considerable reduction in total funding allocated to EMS (Office of Technology Assessment, 1989).
Conversely, attention to pediatric emergency care grew dramatically throughout the 1980s as initial data on this domain of care became available. For example, studies indicated that children represented about 10 percent of all ambulance runs (Seidel et al., 1984); that young children were likely to suffer from respiratory distress, whereas older children were likely to need trauma care (Fifield et al., 1984); and that up to half of pediatric deaths due to trauma might be preventable (Ramenofsky et al., 1984). Studies also indicated that children’s outcomes, given the same severity of injury, tended to be worse than those of adults (Seidel et al., 1984; Seidel, 1986a). For example, a study of 88 general acute care hospitals in Los Angeles County found nearly twice as many deaths among children with serious traumatic injuries as among adults with similar injuries (Seidel et al., 1984). Most of the deaths occurred in areas lacking pediatric tertiary care centers. The studies also revealed that prehospital personnel generally had little training in pediatric care. Also, most lacked the equipment needed to treat children (Seidel, 1986b).
Findings of these early studies led to recognition of the need to address pediatric emergency care and of the existence of a distinct body of knowledge that should be applied in so doing. This recognition stimulated action on several fronts. First, there were advances in resources for care. In the 1980s, several cities designated pediatric trauma centers. Advocates for pediatric emergency care in Los Angeles developed a new two-tiered approach for organizing such care. Under this system, seriously ill or injured children were to be treated only at hospitals that had been certified as meeting a certain set of requirements and capabilities for pediatric care. Perhaps the most significant development for pediatric emergency care was the establishment in 1984 of the federal EMS-C program, a grant program that assists states in addressing pediatric deficiencies within their emergency care systems. The first federal funding for EMS-C was made available in 1985, and later appropriation acts continued to increase funding for the program. The EMS-C program is discussed in detail later in the chapter.
Second, there were advances in resources for information. In the early 1980s, the U.S. Department of Education, through the National Institute of Disability and Rehabilitation Research, funded the development of the National Pediatric Trauma Registry. The registry enabled researchers to identify the demographics of pediatric trauma. Data from the registry revealed that automobile crashes were the primary source of pediatric trauma, that injuries were most often blunt, and that an injured child stood a 3 percent chance of dying from trauma. Data from the registry were also used to develop the Pediatric Trauma Score, a system used to help EMTs determine the facility to which an injured child should be transported (Harris, 1987).
Third, professional societies began to give greater attention to pediatric emergency care. In the late 1970s, pediatricians who worked in EDs began to discuss issues in pediatric emergency care; the result was the formation of a section on pediatric emergency medicine within the American Academy of Pediatrics (AAP) in 1981 (Pena and Snyder, 1995; AAP, 2000). In 1983, the American College of Emergency Physicians (ACEP) held an interspecialty conference on childhood emergencies that led to the establishment of a joint AAP/ACEP Task Force on Pediatric Emergency Medicine the following year (AAP, 2000). ACEP also formed a member section on pediatric emergency medicine in 1998 (Pena and Snyder, 1995). In 1985, a Provisional Committee on Pediatric Emergency Medicine was created within AAP; it became a full committee in 1998 (AAP, 2000). Both the Emergency Nurses Association (ENA) and the National Association of EMS Physicians (NAEMSP) had established pediatric sections by the end of the 1980s (IOM, 1993).
Fourth, there were important advances in pediatric emergency medicine. By the early 1980s, many physicians had recognized that emergency care for children was not as well advanced as that for adults and that specialized resources for the training of providers in pediatric emergency care was needed. The longest-running pediatric emergency medicine fellowship was established in 1980 (Pena and Snyder, 1995; Macias, 2005). Early experts in the field began to synthesize knowledge in the area and make it more widely available. The first pediatric emergency care textbook was published in 1983, and the first journal devoted to pediatric emergency care was launched in 1985.
A number of training courses were developed as well. In 1988, the American Heart Association and the AAP initiated the Pediatric Advanced Life Support (PALS) course. The AAP and ACEP joint task force developed and sponsored the Advanced Pediatric Life Support (APLS) manual, published in 1989. Some courses were also developed locally. An example is the Pediatric Emergency Medical Services Training Program (PEMSTP) at Children’s National Medical Center in Washington, D.C., which prepared EMT instructors to teach pediatric aspects of emergency care. Progress continued in the early 1990s when the ENA developed standardized training for
emergency nurses with its Emergency Nursing Pediatric Course (ENPC). All of these efforts helped develop an emergency care workforce with enhanced pediatric skills.
Finally, injury prevention efforts, which had gained momentum in the 1970s, expanded greatly in the 1980s. The Poison Prevention Packaging Act of 1970 required manufacturers of toxic, corrosive, or irritative substances to use child-resistant closures (Harborview Injury Prevention and Research Center, 2006). The first state law requiring the use of child safety seats was enacted by Tennessee in 1978; by 1985, however, all states had passed such legislation (Traffic Safety Center, 2002). Additionally, state and local laws were passed to establish requirements for the installation of smoke detectors, window guards, and pool fencing. Concern about the prevention of injury and illness was reflected in national health promotion and disease prevention goals first published in 1980 and updated in 1990 and 2000 (DHHS, 1980, 1990, 2000). The 1985 IOM report Injury in America highlighted the heavy toll of injuries and called for more research in prevention and improved care. Much as the NAS/NRC report Accidental Death and Disability led to the passage of the EMSS Act of 1973, Injury in America: A Continuing Health Problem led to the creation of an injury prevention program at the Centers for Disease Control and Prevention (CDC), which later became CDC’s National Center for Injury Prevention and Control (IOM, 1993).
Today, the incidence of sudden infant death syndrome (SIDS) and pediatric cardiac arrest has declined as parents have learned the proper sleep position for infants (AAP, 1992; Willinger, 1995). Injury prevention efforts, such as the poison prevention packaging law, bicycle helmet requirements, child passenger restraint requirements, smoke detector promotion programs, and drowning prevention programs, are beginning to decrease morbidity and mortality due to injury in children (Clarke and Walton, 1979; Rivara et al., 1997; Stenklyft, 1999; Haddix et al., 2001; Macpherson and MacArthur, 2002; Mittelstaedt and Simon, 2004). Many of these prevention efforts were spearheaded by programs such as the National Safe Kids Campaign, founded in 1987.
In addition to injury, prevention efforts targeted reducing pediatric illness. In 1980, for example, Starko and colleagues (1980) produced a study indicating that the use of aspirin may be associated with the onset of Reye’s syndrome, a deadly disease most common in children that affects all organs of the body and occurs after a viral infection, such as the flu or chickenpox (National Institute of Neurological Disorders and Stroke, 2006). As parents learned of the link between aspirin and Reye’s syndrome, there was a decline in both the use of children’s aspirin and the number of Reye’s syndrome cases reported to CDC (Arrowsmith et al., 1987; Belay et al., 1999).
Prevention efforts have successfully changed the scope of pediatric illness seen in the ED. For example, the Hemophilus influenzae (Hib) vac-
cine, introduced in 1990, has nearly eliminated epiglottitis in children and markedly decreased the incidence of meningitis, sepsis, and septic shock (Subedar and Rathore, 1995; Stenklyft, 1999). And the introduction of the PCV7 vaccine has reduced the number of invasive pneumococcal infections among children (Kaplan et al., 2004).
The 1990s: Birth of a New Subspecialty
The number of pediatric emergency medicine fellowships had begun to increase, although most of these had been developed at children’s hospitals under the leadership of pediatricians. In the late 1980s, representatives from the American Board of Emergency Medicine (ABEM) and the American Board of Pediatrics collaborated to ensure that such fellowships would be accessible to both pediatricians and emergency medicine physicians. Together, the two organizations submitted a proposal to the American Board of Medical Specialties that pediatric emergency care be a recognized subspecialty (Pena and Snyder, 1995). The proposal was approved, and in 1992, the first subspecialty certifying exam in pediatric emergency medicine was administered (Stenklyft, 1999). In 1998, pediatric emergency medicine fellowships became accredited. Most fellowship programs are now 3 years in duration and include a research component (Stenklyft, 1999). By 1999, the nation had approximately 1,000 board-certified subspecialists in pediatric emergency medicine.
In 1993, the IOM released findings from its comprehensive study on the need for and effectiveness of pediatric emergency care (IOM, 1993). Despite the advances in pediatric emergency care that had occurred through the 1980s and early 1990s, the study identified gaps in several major areas, including education and training; appropriate equipment and supplies; communications; funding; and planning, evaluation, and research. In response to these findings, the Maternal and Child Health Bureau (MCHB) within the Health Resources and Services Administration (HRSA) and the National Highway Traffic Safety Administration (NHTSA) published a 5-year plan for pediatric emergency care in 1995. That plan was revised and updated in 2000 (DHHS et al., 2000), and a new plan was published in 2001 (DHHS et al., 2001). Additionally, ACEP and the AAP published recommended equipment guidelines for prehospital units and emergency departments (Guidelines for Pediatric Equipment, 1996; AAP, 2001).
Pediatric Emergency Care in 2006
If there is one word to describe pediatric emergency care in 2006, it is uneven. As mentioned in Chapter 1, the specialized resources available to treat seriously ill or injured children vary greatly based on location. Some
children have access to children’s hospitals and hospitals with separate pediatric inpatient capabilities, which tend to be well prepared for pediatric emergencies; others must rely on hospitals with limited pediatric medical expertise and equipment (Middleton and Burt, 2006). Requirements for pediatric continuing medical education for EMTs vary greatly across states. Some states and communities have organized trauma systems and designated pediatric facilities, while others do not. As a result, not all children have access to the same quality of care. While data on system performance are not routinely collected, it appears that where a child lives has an important impact on whether the child can survive a serious illness or injury.
The day-to-day presentation of pediatric patients is challenging enough for emergency care systems in some areas; addressing new and emerging threats to children’s health may be beyond the capabilities of the current system. Experience has shown that the outbreak and management of contagious diseases, such as new strains of influenza and severe acute respiratory syndrome (SARS), can cause a major disruption in the emergency care system (Augustine et al., 2004). The effect of these new health threats on children is not yet well understood. Several case studies of SARS have been published, but most of the clinical, laboratory, and radiological information available is based on adult patients (Bitnun et al., 2003). Some case studies suggest that while children are susceptible to SARS, symptoms of the disease may be milder in young children as compared with adolescents and adults (Fong et al., 2004; Leung et al., 2004). However, these studies are based on a very small sample. The efficacy of pediatric treatment for SARS requires additional evaluation; indeed, no pediatric treatment regime for SARS currently exists (Leung et al., 2004).
Avian influenza is another emerging threat that could put children at particular risk. Children may be more susceptible to the disease because of their increased proximity to one another at schools and day care centers. They may also be more likely to come into contact with poultry or bird fecal matter while playing. It is unknown whether immunity differences in children have any significance in their susceptibility to avian influenza, since it is presumed that the vast majority of humans have no immunity against the H5N1 virus, the strain of greatest concern (U.S. Department of State, 2006).
Development of Pediatric Trauma Care
Trauma represents a particular kind of medical emergency. It is typically defined as having a physical wound caused by force or impact, such as a fall or automobile accident; burns and other severe wounds are also deemed a form of trauma. Other life-threatening medical conditions caused by preexisting conditions are generally not considered trauma. Trauma
care is distinguished from care received in a general ED by the specialized diagnostic and treatment procedures necessary to care for the traumatically injured patient. Trauma centers are designed to meet the complex surgical demands of critically ill patients immediately. To qualify as a trauma center, a hospital must have a number of capabilities, including a resource-intensive ED, a high-quality intensive care ward, and an operating room that is functional at all times. Ideally, traumatically injured children are cared for in a pediatric trauma center, a facility with the personnel, equipment, space, and other resources required to provide the necessary care 24 hours a day, 7 days a week (Ramenofsky, 2006). The American College of Surgeons’ (ACS) Committee on Trauma has defined the term “pediatric trauma center” in its categorization of trauma centers into levels based on their capabilities. A level I pediatric trauma center, the highest level, is a children’s hospital or an adult center with pediatric expertise (Ramenofsky, 2006).
Given that the development of pediatric emergency care has lagged behind that of adult emergency care, it is surprising that the first pediatric trauma center was established in 1962—5 years before the first adult trauma center was established (Ramenofsky, 2006). In 1970, the American Pediatric Surgical Association (APSA) was founded; 2 years later, one of the members requested greater emphasis on trauma, and the association established a Committee on Trauma, which continues today. Also in 1972, the APSA joined the American Medical Association, the ACS, the American Academy of Orthopedic Surgeons, and the American Association for the Surgery of Trauma in sponsoring the American Trauma Society (ATS) (Personal communication, M. Stanton, March 12, 2006). The ATS, established in the late 1960s, was an advocate for the EMSS Act of 1973. Today it works to promote trauma care and prevention, serving as an advocate for trauma victims and their families and for optimal care for all trauma victims (ATS, 2006).
However, advanced resources for the care of pediatric trauma patients were largely unavailable until the 1980s. In 1982, the Journal of Trauma published the first description of resources necessary to treat the injured child. Others followed. In 1984, the ACS Committee on Trauma included an appendix on pediatric trauma care in its standards manual, which was the first document to define the standards of care necessary to treat trauma patients. A chapter on pediatric trauma appeared in the ACS resource manual in 1987 (Ramenofsky, 2006).
Today, most regions have dedicated trauma facilities, board-certified surgeons have training and experience in trauma care and pediatric surgery, and most states have organized trauma systems. Injuries are no longer viewed as “accidents” but as predictable events that can be prevented through the application of harm reduction strategies (Cooper, 2006). As detailed later in the chapter, however, unintentional injury continues to be the leading cause of death in children over age 1 and an important source of
ED visits. While this report is focused on the emergency care system and the pediatric component of that system, the committee emphasizes that greater effort is needed to build a comprehensive injury control strategy or system to reduce injuries among both children and adults.
The Emergency Medical Services for Children Program
The creation of the federal EMS-C program in 1984 grew at least in part out of policy makers’ personal experiences with the pediatric emergency care system. Several congressional staff members had had disturbing experiences with the emergency care system’s ability to care for their children. Their experiences highlighted serious shortcomings of a typical ED’s capacity to care for children in crisis. Around the same time, emergency physicians began approaching federal lawmakers to tell them that children were arriving at the ED in worse condition than adults. As a result, Senators Daniel Inouye (D-HI), Orrin Hatch (R-UT), and Lowell Weicker (R-CT) sponsored the creation of the EMS-C demonstration grant program under the Health Services, Preventive Health Services, and Home Community Based Services Act of 1984 (IOM, 1993; CPEM, 2001).
The goal of the EMS-C program is to reduce child and youth morbidity and mortality resulting from severe illness or trauma by supporting injury prevention programs and improvements in the quality of medical care received by children. The program aims to ensure (1) that state-of-the-art emergency medical care is available for ill or injured children and adolescents; (2) that pediatric services are well integrated into an EMS system backed by optimal resources; and (3) that the entire spectrum of emergency services—including illness and injury prevention, acute care, and rehabilitation—is provided to children and adolescents as well as adults (Perez, 1998). While this report is focused on pediatric EMS and hospital-based pediatric emergency care, the EMS-C program covers a broader continuum of care, from illness and injury prevention to bystander care, dispatch, prehospital EMS, definitive hospital care, rehabilitation, and return to the community (see Figure 2-1). The EMS-C program is the only federal program that specifically supports essential emergency medical care for ill or injured children and adolescents. The program is administered by HRSA with support from NHTSA.
The program initially focused on providing grants to states and accredited schools of medicine for needs assessments and demonstration projects (Advocates for EMS, 2004; Krug and Kuppermann, 2005). Its original authorization provided $2 million in funding for fiscal year 1985 (IOM, 1993). That funding supported four state partnership demonstration projects that created some of the first strategies for addressing important pediatric emergency care issues, such as disseminating education programs for pre-

FIGURE 2-1 Continuum of care of the Emergency Medical Services for Children program.
hospital and hospital-based providers, establishing data collection processes to identify significant pediatric issues in the EMS system, and developing tools for assessing critically ill or injured children (CPEM, 2001).
Growth of the EMS-C Program
Funding for the EMS-C program has grown since its inception, as have the number and types of initiatives funded. Reauthorization of the program in 1988 lifted the initial limit of four grants per year and provided funding of $3 million for fiscal year 1989, $4 million for fiscal year 1990, and $5 million for fiscal year 1991 (IOM, 1993).
The program underwent several changes in 1991. First, the focus of the state grants shifted from demonstration to implementation projects (IOM, 1993). The objective of implementation projects is to put into place what is known to work (HRSA, 1994). Second, the program introduced new Targeted Issues Grants. These grants target specific issues related to the de-
velopment of pediatric emergency care capacity, with the intent of providing potential national models. Examples of such grants awarded to date are an investigation of the psychosocial impact of emergencies on children and the development of new pediatric information systems (IOM, 1993).
States that receive EMS-C grants are expected to share ideas or products with other interested states, and the EMS-C National Resource Center was created to assist with such knowledge sharing. As states create new programs, the center provides technical assistance with strategic planning, program development, problem solving, identification of national resources, and program evaluation. The center also promotes understanding of pediatric issues in the EMS system through the development of reports and special materials for the states. Its library contains more than 1,000 products that address illness and injury prevention, patient care training and safety, equipment guidelines, medical direction, and public policy. Additionally, the National EMSC Data Analysis Resource Center (NEDARC) in Salt Lake City, Utah, specializes in providing grantees with technical assistance in data collection and analysis (Perez, 1998).
The program continued to expand and mature in the mid-1990s. In response to the recommendations of the 1993 IOM report Emergency Medical Services for Children, HRSA and NHTSA sponsored a meeting to help translate those recommendations into objectives and specific actions. The result was the EMS-C 5-Year Plan, a comprehensive, long-range strategy for the EMS-C program for 1995–2000 (DHHS et al., 1995). That plan was updated in 2000 and continued to guide the program through 2005 (DHHS et al., 2001). The program has partnered with a number of professional organizations to address the objectives in the plan (Krug and Kuppermann, 2005).
In recent years, the EMS-C program has also supported the infrastructure for pediatric emergency care research. In 2001, the program collaborated with the Research Branch of HRSA’s MCHB to develop the Pediatric Emergency Care Applied Research Network (PECARN), the first federally funded multi-institutional network for research in pediatric emergency care. Funding for the infrastructure for PECARN has come through EMS-C program appropriations. PECARN consists of five cooperative agreements with academic medical centers. Its goal is to conduct meaningful and rigorous multi-institutional research on the prevention and management of acute illnesses and injuries in children and youths across the continuum of emergency medicine health care (PECARN, 2004). PECARN provides leadership and infrastructure to promote multicenter studies, support research collaboration among researchers in pediatric EMS, and encourage information exchanges between pediatric emergency care investigators and providers (DHHS, 2004).
Congress should be commended for recognizing the importance of the
EMS-C program and supporting its development.1 Despite the program’s growth, however, it continues to be funded at a relatively modest level. Fiscal year 2005 funding for the program was $19.86 million2; details on the program’s expenditures are provided in Table 2-1. Note that administrative expenses are low in part because the two full-time staff overseeing the program at the national level are not funded from the program’s budget, but from the MCHB’s Program Management Fund.
Impact of the EMS-C Program
In 2005, the EMS-C program celebrated its twentieth anniversary. The program’s accomplishments are numerous even with its modest level of appropriations. The program has broadly advanced the state of pediatric emergency care nationwide. It has improved the availability of child-size equipment in ambulances and EDs; initiated hundreds of programs to prevent injuries; and provided thousands of hours of training to EMTs, paramedics, and other emergency medical care providers. Educational materials covering every aspect of pediatric emergency care have been developed under the EMS-C program, and a formal partnership (the EMS-C Partnership for Children Stakeholder Group) has been forged with numerous national and professional organizations to help achieve the program’s goals (MCHB, 2005a). Findings resulting from Targeted Issues Grants have enhanced the use of ketamine and analgesia for pediatric orthopedic emergencies (Graff et al., 1996) and led to improved understanding of pediatric intubation in the prehospital environment (Gausche-Hill et al., 2000) and pediatric airway management (MCHB, 2004b).
The EMS-C program’s guidance and resources have led to important changes in pediatric emergency care at the state level. For example:
-
Twelve states have adopted and disseminated pediatric guidelines that characterize acute care facilities (pediatric trauma care or critical care facilities or EDs approved for pediatrics) according to the equipment, drugs, trained personnel, and facilities necessary to provide varying levels of pediatric emergency care.
-
Twenty states have pediatric emergency care statutes.
TABLE 2-1 EMS-C Program Expenditures for Fiscal Year (FY) 2005
|
Program Component |
Description |
Approximate FY 05 Funding |
|
State Partnership Grants |
|
$5.6 million |
|
Network Development Demonstration |
|
$3.5 million |
|
Targeted Issues Grants |
|
$3.1 million |
|
National Resource Center |
|
$2.2 million |
|
National EMSC Data Analysis Resource Center (NEDARC) |
|
$1.2 million |
|
Interagency Agreements |
|
$800,000 |
|
Regional Symposia |
|
$239,000 |
|
Other Activities |
|
$3 million |
-
Twenty-seven states, tribal reservations, or federal territories have conducted a pediatric emergency care needs assessment within the last 5 years.
-
Thirty-six of the 42 states having statewide computerized data collection systems now produce reports on pediatric EMS using statewide data.
-
Forty-one states use pediatric guidelines for identification of acute care facilities, ensuring that children are transported to the right hospital in a timely manner.
-
Forty-four states employ pediatric protocols for on-line medical direction of EMTs and paramedics at the scene of an emergency.
-
Forty-eight states identify and require all essential pediatric EMS equipment on advanced life support (ALS) ambulances (Advocates for EMS, 2004; MCHB, 2005b).
While the program is focused on pediatric emergency care, many of its initiatives benefit patients of all ages. An example is an interagency agreement with NHTSA to support the development of the National EMS Research Agenda, the National EMS Information System, and the infrastructure for the National Association of State EMS Officials.
The 1993 IOM Report on Emergency Medical Services for Children
The activities of the EMS-C program were the subject of considerable congressional interest during the program’s first decade. In response to this interest, in 1991 HRSA requested that the IOM undertake a study of pediatric EMS to examine the issues involved more broadly than was possible through the EMS-C program’s individual demonstration projects (IOM, 1993). Previously the National Academy of Sciences, National Research Council, and IOM had conducted several other studies related to emergency care, but few had given much attention to pediatric emergency care. The findings and recommendations of the IOM study were published in the 1993 report Emergency Medical Services for Children. The report presented recommendations in five areas: education and training; essential tools; communication and 9-1-1 systems; planning, evaluation, and research; and federal and state agencies and funding. The report garnered considerable attention from emergency care providers, professional organizations, policy makers, and the public. Since its release, progress has been made in each of the recommendation areas, yet the issues raised have not been fully addressed. Examples are described below.
Education and Training
Concern in 1993 regarding emergency providers’ knowledge about the proper care of pediatric patients remains salient today. Maintenance of
skills is a challenge because many providers have infrequent contact with critically ill and injured children; only rarely do they perform ALS interventions on children. Surveys indicate that prehospital providers find the age group birth to 3 years most concerning and support increased continuing education in pediatric emergency care (Glaeser et al., 2000). Additionally, the majority of pediatric visits occur at general EDs (Gausche et al., 1995), which are less likely than specialized facilities to have providers specifically trained in pediatric emergency medicine. Anecdotal accounts of physicians expressing doubt about their skills to care for a critically ill or injured child are not uncommon (Frush and Hohenhaus, 2004). The abilities of emergency care providers to address the needs of children are discussed further in Chapter 4.
Essential Tools
The IOM committee that developed the 1993 report was concerned by reports that emergency providers lacked the equipment necessary to care properly for children and recommended that pediatric equipment and supplies be made more widely available. Since the release of the 1993 report, professional organizations have continued to update guidelines on essential and recommended equipment and supplies, and many states have used funding from the EMS-C program to purchase pediatric equipment. While some progress has been made, however, deficiencies in pediatric equipment and supplies remain a problem for some providers. The average ED has about 80 percent of the recommended pediatric supplies, and only 6 percent of the nation’s EDs are fully equipped to care for children (Middleton and Burt, 2006). Some data indicate that there was no increase in the availability of pediatric equipment in EDs between 1998 and 2002 (Middleton, 2005).
Research on the availability of the pediatric supplies and equipment recommended for prehospital providers has been limited primarily to studies of regions or states, and no recent data are available. A 1993 study of EMS ambulance agencies in Oklahoma found that deficiencies in equipment needed for pediatric emergencies were common (Graham et al., 1993). A 1998 study of compliance with the guidelines of the Committee on Ambulance Pediatric Equipment and Supplies in Kansas revealed that only 5 percent of ambulance services reported having essential equipment on all vehicles; 92 percent of agencies failed to achieve compliance with the guidelines on any vehicle. The most frequently lacking pediatric basic life support (BLS) items were stethoscopes (58 percent), traction splints (53 percent), and non-rebreather masks (45 percent). The most frequently lacking pediatric ALS items were nasogastric tubes (75 percent), monitor electrodes (50 percent), and Magill forceps (41.7 percent) (Moreland et al., 1998). Again, there is
scant evidence regarding the impact on patient outcomes of not having all essential pediatric equipment; however, having this equipment available is an essential element of preparedness.
The 1993 IOM report also recommended that states address the issue of categorization and regionalization in overseeing the development of pediatric emergency care. In many states, however, hospitals are not categorized based on their ability to care for critically ill or injured children. Additionally, many hospitals lack transfer agreements in case a critically ill or injured child arrives at a hospital that lacks pediatric expertise (Middleton and Burt, 2006). This issue is discussed further in the next chapter.
Planning, Evaluation, and Research
One of the great successes of the EMS-C program has been that all states now have an EMS-C coordinator, whose job it is to oversee grant funding received from the program. In many states, the coordinator position is full-time and involves other activities, including making sure that the state EMS system considers children’s needs. However, there are still signs of deficiencies in trauma and disaster planning (MCHB, 2004a; NAEMSD, 2004). As mentioned earlier, about half of hospitals that lack a separate pediatric ward also lack written interfacility transfer agreements (Middleton and Burt, 2006). Moreover, although most state disaster plans address the need for pediatric equipment and medications at hospitals, only six states report that hospitals have those resources in place (NAEMSD, 2004).
Certainly there has been some expansion of pediatric emergency care research since 1993, but efforts to track patient outcomes have been hampered by the absence of an infrastructure for the systematic collection of a uniform set of data elements and by the inability to link datasets of different providers (prehospital, ED, others) as recommended in the 1993 IOM report. Research funding for pediatric emergency care is also highly limited. It is of note that the annual appropriation for the entire EMS-C program is less than the annual cost of some single large-scale National Institutes of Health (NIH) clinical trials (National Center for Complementary and Alternative Medicine, 2002; National Cancer Institute, 2005). As a result of the dearth of funding for emergency care research, many emergency medical interventions that are regularly provided to children have not been subjected to rigorous scientific trials. This issue is discussed further in Chapter 7.
PEDIATRIC EMERGENCY CARE IN 2006
This section describes the emergency care system for children in 2006. The focus is on the need for and use of pediatric emergency care.
Threats to Children’s Health
Data from CDC’s 2003 National Health Interview Survey indicate that children in the United States are generally in good health. Approximately 83 percent of parents described their children as being in “excellent” or “very good” health. Not surprisingly, children in two-parent families, families with higher incomes, and those covered by private insurance tended to be in better health than children living with their mothers only, children from poor families, and children without insurance (Dey and Bloom, 2005).
Threats to children’s health and safety remain prevalent in our society. Injuries are the leading cause of death among those aged 1–19, and rates of childhood injury in the United States are considerably higher than those in other developed countries (United Nations Children’s Fund, 2001; CDC, 2004). Illnesses, particularly asthma and infectious disease, impose a high burden on American children and their parents. In fact, approximately 20 million children in the United States suffer from at least one chronic condition, leaving them more susceptible to medical emergencies (AHRQ, 2002). Moreover, violence in our society remains prevalent; many children witness or are directly exposed to violence in their families and/or communities. The result is that millions of Americans rely on the emergency medical system to provide care for children when they need it most.
Injury
Statistics on childhood injury are available from a variety of sources, but perhaps the most comprehensive are from CDC’s National Vital Statistics Reports and ACS’s National Trauma Data Bank (NTDB). CDC collects data on injury deaths by cause; those data are displayed in Table 2-2, while data from the NTDB are shown in Table 2-3. The two datasets are somewhat different because the NTDB includes not just deaths, but all injured patients seen at one of the 474 participating trauma centers in 43 states (Fildes, 2005).
Both datasets show what has been known for many years: the most common cause of injury deaths and injury visits to trauma centers is motor vehicle crashes. According to NHTSA, more than half of children aged 0–14 who were killed in such crashes in 2003 were not restrained (CDC, 2005). More than a quarter of occupant deaths among children aged 0–14 involved a driver who was drinking (Shults, 2004).
Other threats to safety vary by age group. Young children aged 1–4 are at great risk of injury as they explore their environment. They are more likely than older children to fall into a pool and drown or swallow pills unintentionally. Indeed, drowning is the second leading cause of death in this age group. Young children also lack coordination, which makes them
TABLE 2-2 Number of Deaths from Selected Causes, by Age
|
Cause of Death |
Age in Years |
Total Deaths |
|||
|
Under 1 |
1–4 |
5–14 |
15–24 |
||
|
Injury |
|||||
|
Unintentional Injury |
946 |
1,641 |
2,718 |
15,412 |
20,717 |
|
Motor Vehicle Accident |
123 |
610 |
1,614 |
11,459 |
13,806 |
|
Accidental Poisoning/Exposure to Noxious Substances |
26 |
31 |
43 |
1,679 |
1,779 |
|
Drowning |
63 |
454 |
321 |
629 |
1,467 |
|
Exposure to Smoke, Fire, or Flames |
36 |
221 |
253 |
193 |
703 |
|
Fall |
16 |
37 |
42 |
247 |
342 |
|
Firearm Discharge |
1 |
11 |
48 |
210 |
270 |
|
Assault (Homicide) |
303 |
423 |
356 |
5,219 |
6,301 |
|
Suicide |
NA |
NA |
264 |
4,010 |
4,274 |
|
SOURCE: National Center for Health Statistics, 2004. |
|||||
TABLE 2-3 Percentage of Total Pediatric Patients Presenting at a Trauma Center, by Mechanism of Injury
more susceptible to falls. Approximately 2.4 million cases of human poison exposures were reported to poison control centers in 2003; 44 percent of those cases occurred in children aged 1–4 (Watson et al., 2003). Additionally, these children may be at much higher risk of abuse (inflicted injuries) or neglect, particularly because of their dependency and their inability to communicate the abuse (National Center for Injury Prevention and Control, 2001).
Children aged 5–14 are often injured because of their impulsiveness and inability to judge the safety of a situation. They may run into the street without looking or give unwanted attention to animals (2.5 percent of children are bitten by dogs each year). They are also susceptible to bicycle crashes. In fact, 140,000 children are seen in the ED each year for traumatic brain injuries sustained while riding a bicycle; one-third of all bicyclists killed in crashes are children. Small size contributes to these children’s risk of injury—motorists may not be able to see them in the road. The risk of violence, including child sexual abuse, is high in this age group. Emotional stress and social changes may contribute to the increased risk of suicide attempts and completed suicides involving adolescents (National Center for Injury Prevention and Control, 2001).
Teenagers and young adults between the ages of 15 and 19 are involved in violence more than any other age group. They are also at high risk for suicide. Developmental factors that result in impulsiveness and risk-taking behaviors may contribute to these risks. Motor vehicle crashes are most likely to occur among teenaged drivers, particularly during the first year behind the wheel; teenagers are more likely to speed, ride with an intoxicated driver, or drive after using alcohol or drugs than those in other age groups (National Center for Injury Prevention and Control, 2001).
Although the prevalence of childhood injury is high, trend data indicate improvement over time for unintentional injuries and some categories of intentional injuries. The unintentional injury death rate among children aged 0–14 declined 41 percent between 1987 and 2001; death rates fell for motor vehicle injury, bicycle injury, pedestrian injury, drowning, fire and burn injury, poisoning, and fall injury during the period (National Safe Kids Campaign, 2004). This improvement is likely the result of prevention efforts, such as laws and campaigns aimed at increased use of child safety seats, bicycle helmets, and smoke alarms.
Rates of intentional injury, homicide, suicide, and firearm-related fatality among teenagers all dropped from the mid-1990s through 2002 (the most recent year for which data are available). Between 1973 and 1993, the homicide rate for teenagers doubled from 8.1 to 20.7 deaths per 100,000, but the rate subsequently declined, falling to 9.3 in 2002. The rate of adolescent suicide also rose dramatically between 1970 and the mid-1990s (from
5.9 to 11.1 deaths per 100,000), but has since fallen to 7.4 (Child Trends Databank, 2004).
Trends in child abuse are more difficult to discern because of underrecognition and underreporting. There has been a slight increase in the number of child abuse cases reported to child protective services (Peddle and Wang, 2002) and in child abuse fatalities reported by the National Child Abuse and Neglect Data System (National Clearinghouse on Child Abuse and Neglect Information, 2004), but it is unclear whether these increases are a result of improved reporting or increased abuse. Regardless, child abuse and neglect remains a serious problem.
Illness
Children suffer from a myriad of illnesses, but not all types of illnesses are likely to lead to an experience with the emergency care system. For example, congenital abnormalities and birth-related conditions are among the leading causes of death among infants, yet they are rarely the reason for an ED visit (Table 2-4). Data from the Agency for Healthcare Research and Quality’s (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Emergency Department Database (SEDD) include the most frequent diagnoses for all pediatric ED visits in 12 states. Table 2-5 shows the primary diagnosis for treat and release ED visits for various pediatric age groups. Approximately 4 percent of all ED visits result in admission to the hospital (2002 NHAMCS data, calculations by IOM; 2002 SEDD data provided by AHRQ staff); Table 2-6 shows the primary diagnosis for such ED visits.
The illnesses most frequently responsible for an ED visit tend to be rather minor. Among children treated and released from the ED, the most common non-injury-related diagnosis for all age groups is upper respiratory infection (not including asthma, acute bronchitis, or pneumonia), which includes conditions such as the common cold, croup, and sinusitis. Otitis media, or ear infection, is another common illness responsible for many ED visits among younger children; three of four children experience this condition by the time they reach age 3 (National Institute on Deafness and Other Communication Disorders, 2002).
Among ED visits that result in hospital admission, the illnesses responsible vary considerably based on age group. Younger children tend to be hospitalized for serious upper respiratory infections, including acute bronchitis, pneumonia, and asthma. Infants and young children tend to have greater vulnerability to these illnesses than older children and nonelderly adults. Children whose parents or siblings smoke are especially susceptible to these three conditions (MayoClinic.com, 2005).
Of note, mood disorders are the most frequent diagnosis for children
TABLE 2-4 Ten Leading Causes of Death in Children and Number of Deaths, by Age Group (in years), 2002
|
|
Less than 1 |
Ages 1–4 |
Ages 5–9 |
Ages 10–14 |
Ages 15–24 |
|
1. |
Congenital anomalies 5,623 |
Unintentional injury 1,641 |
Unintentional injury 1,176 |
Unintentional injury 1,542 |
Unintentional injury 15,412 |
|
2. |
Short gestation 4,673 |
Congenital anomalies 530 |
Malignant neoplasms 537 |
Malignant neoplasms 535 |
Homicide 5,219 |
|
3. |
Sudden infant death syndrome (SIDS) 2,295 |
Homicide 423 |
Congenital anomalies 199 |
Suicide 260 |
Suicide 4,010 |
|
4. |
Maternal pregnancy complications 1,708 |
Malignant neoplasms 402 |
Homicide 140 |
Congenital anomalies 218 |
Malignant neoplasms 1,730 |
|
5. |
Placenta cord membranes 1,028 |
Heart disease 165 |
Heart disease 92 |
Homicide 216 |
Heart disease 1,022 |
|
6. |
Unintentional injury 946 |
Influenza and pneumonia 110 |
Benign neoplasms 44 |
Heart disease 163 |
Congenital anomalies 492 |
|
7. |
Respiratory distress 943 |
Septicemia 79 |
Septicemia 42 |
Chronic lower respiratory disease 95 |
Chronic lower respiratory disease 192 |
|
8. |
Bacterial sepsis 749 |
Chronic lower respiratory disease 65 |
Chronic lower respiratory disease 41 |
Cerebrovascular disease 58 |
HIV 178 |
|
9. |
Circulatory system disease 749 |
Complications of perinatal period 65 |
Influenza and pneumonia 38 |
Influenza and pneumonia 53 |
Cerebrovascular disease 171 |
|
10. |
Intrauterine hypoxia 583 |
Benign neoplasms 60 |
Cerebrovascular disease 33 |
Septicemia 53 |
Diabetes mellitus 171 |
|
SOURCE: CDC, 2004. |
|||||
TABLE 2-5 Ten Leading Primary Diagnoses for Treat and Release ED Cases in Selected States, by Age Group (in years)
|
|
Less than 1 |
Ages 1–4 |
Ages 5–9 |
Ages 10–14 |
Ages 15–17 |
|
1. |
Other upper respiratory infections (18%) |
Other upper respiratory infections (14%) |
Other upper respiratory infections (13%) |
Superficial injury, contusion (12%) |
Sprains and strains (13%) |
|
2. |
Otitis media (14%) |
Otitis media (13%) |
Superficial injury, contusion (9%) |
Sprains and strains (11%) |
Superficial injury, contusion (11%) |
|
3. |
Fever of unknown origin (8%) |
Open wounds of head, neck, and trunk (8%) |
Open wounds of head, neck, and trunk (7%) |
Other upper respiratory infections (9%) |
Other upper respiratory infections (6%) |
|
4. |
Viral infections (6%) |
Superficial injury, contusion (6%) |
Otitis media (6%) |
Fracture of upper limb (7%) |
Open wounds of extremities (5%) |
|
5. |
Acute bronchitis (5%) |
Fever of unknown origin (6%) |
Fracture of upper limb (5%) |
Open wounds of extremities (6%) |
Abdominal pain (4%) |
|
6. |
Noninfectious gastroenteritis (3%) |
Viral infections (5%) |
Open wounds of extremities (4%) |
Other injuries due to external causes (5%) |
Other injuries due to external causes (4%) |
|
7. |
Nausea and vomiting (3%) |
Other injuries due to external causes (4%) |
Other injuries due to external causes (4%) |
Open wounds of head, neck, and trunk (4%) |
Fracture of upper limb (3%) |
|
8. |
Other gastrointestinal disorders (3%) |
Noninfectious gastroenteritis (3%) |
Sprains and strains (4%) |
Abdominal pain (3%) |
Open wounds of head, neck, and trunk (3%) |
|
9. |
Other injuries due to external causes (3%) |
Asthma (3%) |
Viral infections (4%) |
Asthma (3%) |
Urinary tract infections (2%) |
|
10. |
Superficial injury, contusion (3%) |
Pneumonia (2%) |
Asthma (3%) |
Otitis media (3%) |
Headache, including migraines (2%) |
|
SOURCE: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project (HCUP), aggregate of 2002 State Emergency Department Databases from Connecticut, Georgia, Maine, Maryland, Massachusetts, Minnesota, Missouri, Nebraska, South Carolina, Tennessee, Utah, and Vermont (http://www.hcup-us.ahrq.gov). Percentages represent the proportion of discharges in each age group. Diagnostic groups listed are based on the Clinical Classifications Software (CCS) (http://www.hcup-us.ahrq.gov/tools.jsp). Data provided by AHRQ staff. |
|||||
TABLE 2-6 Ten Leading Principal Diagnoses for Hospital Admissions That Begin in the ED in Selected States, by Age Group (in years)
|
|
Less than 1 |
Ages 1–4 |
Ages 5–9 |
Ages 10–14 |
Ages 15–17 |
|
1. |
Acute bronchitis (23%) |
Pneumonia (15%) |
Asthma (14%) |
Appendicitis (13%) |
Mood disorders (12%) |
|
2. |
Pneumonia (8%) |
Asthma (15%) |
Pneumonia (9%) |
Mood disorders (8%) |
Appendicitis (7%) |
|
3. |
Other perinatal conditions (8%) |
Fluid and electrolyte disorders (10%) |
Appendicitis (7%) |
Asthma (7%) |
Fracture of lower limb (4%) |
|
4. |
Fluid and electrolyte disorders (6%) |
Acute bronchitis (6%) |
Fluid and electrolyte disorders (5%) |
Fracture of lower limb (4%) |
Intracranial injury (4%) |
|
5. |
Fever of unknown origin (5%) |
Epilepsy, convulsions (6%) |
Fracture of upper limb (4%) |
Pneumonia (3%) |
Poisoning by other medications and drugs (3%) |
|
6. |
Urinary tract infection (4%) |
Other upper respiratory infections (4%) |
Epilepsy, convulsions (4%) |
Diabetes mellitus with complications (3%) |
Crushing injury or internal injury (3%) |
|
7. |
Viral infections (4%) |
Intestinal infection (4%) |
Fracture of lower limb (3%) |
Fracture of upper limb (3%) |
Asthma (3%) |
|
8. |
Other upper respiratory infections (3%) |
Urinary tract infection (2%) |
Urinary tract infections (3%) |
Sickle cell anemia (3%) |
Diabetes mellitus with complications (3%) |
|
9. |
Asthma (3%) |
Noninfectious gastroenteritis (2%) |
Skin and subcutaneous tissue infections (2%) |
Intracranial injury (3%) |
Urinary tract infections (2%) |
|
10. |
Intestinal infection (3%) |
Skin and subcutaneous tissue infections (2%) |
Sickle cell anemia (2%) |
Abdominal pain (2%) |
Other complications of pregnancy (2%) |
|
SOURCE: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project (HCUP), aggregate of 2002 state inpatient databases from Connecticut, Georgia, Maine, Maryland, Massachusetts, Minnesota, Missouri, Nebraska, South Carolina, Tennessee, Utah, and Vermont (http://www.hcup-us.ahrq.gov). All data are the proportion of discharges in each age group. Diagnostic groups listed are based on the Clinical Classifications Software (CCS) (http://www.hcup-us.ahrq.gov/tools.jsp). Data provided by AHRQ staff. |
|||||
aged 15–17 admitted from the ED and the second most frequent diagnosis for those aged 10–14. Mood disorders encompass a wide variety of behavioral issues but generally fall into two categories: depression and bipolar (or manic-depressive) disorder (Beers and Berkow, 2005).
Certain types of illnesses, particularly asthma and diabetes, become exacerbated and result in hospital admission when children have health care needs that go unmet. Failure to obtain timely care can affect health status and functioning in the near and long terms and can influence the likelihood of seeking services at an ED. Data from the National Health Interview Survey for the mid-1990s indicate that unmet health care needs were prevalent among children. Near-poor and poor children were three times as likely to have unmet health care needs as nonpoor children, and uninsured children were three times as likely to have unmet needs as privately insured children (Newacheck et al., 2000).
Children with Mental Health Problems
Mental health disorders in children and adolescents deserve special mention because of their growing prevalence as causes for ED visits, as well as the difficulty that patients with mental illness pose to emergency care providers. It is estimated that 20 percent of U.S. children have a mental disorder with at least mild functional impairment; 5 to 9 percent of children aged 9–17 have a serious emotional disturbance (DHHS, 1999). These problems not only contribute to difficulties at home, at school, and in relationships with peers, but if untreated can lead to such consequences as failure in school, involvement in the juvenile or adult criminal justice system, and higher health care costs as adults, as well as suicide.
Based on extrapolation from National Electronic Injury Surveillance System (NEISS) data, more than 200,000 children present to the ED with mental health problems each year (Melese-d’Hospital et al., 2002), and research has shown that such ED visits are on the rise (Santucci et al., 2000; Sullivan and Rivera, 2000; Sills and Bland, 2002); at one pediatric ED, for example, mental health–related visits rose 59 percent between 1995 and 1999 (Santucci et al., 2000). Moreover, the patients involved are getting younger and younger; depression, bipolar disorder, and anxiety are now being identified in children of elementary school age (Scheck, 2006).
Studies have pointed to shortcomings in the effectiveness of the emergency care system in dealing with children with mental health problems. A mid-1990s survey of hospitals revealed that formal mental health services for children are unavailable in most EDs (U.S. Consumer Product Safety Commission, 1997). In a pilot study of pediatric mental health cases at 10 hospitals participating in the NEISS, researchers found that mental health evaluations of patients varied by presenting condition. Three-fourths of
emotionally disturbed children received an evaluation by a mental health professional, compared with 69 percent who had attempted suicide and 35 percent categorized as having problems with drug and/or alcohol use (Melese-d’Hospital et al., 2002). Results of other studies indicate that proper management in the ED of adolescents who have attempted suicide is lacking. Although the importance of follow-up psychiatric treatment has been demonstrated, psychotherapy is recommended to fewer than half of adolescent suicidal patients evaluated in the ED (Piacentini et al., 1995). Additionally, adolescents with somatic complaints are infrequently screened for depression (Porter et al., 1997).
These findings should not be surprising considering that ED providers often lack the training, skills, and resources to deal effectively with mentally ill patients. Standardized psychiatric training is not required of residents in emergency medicine and pediatric emergency medicine. Fewer than one-quarter of emergency medicine residency programs provide formal psychiatric training (Santucci et al., 2003). Surveys of nurses—even those working in designated pediatric EDs—show that pediatric psychiatric emergencies are among the conditions they feel the least comfortable and knowledgeable in managing (Fredrickson et al., 1994). ED physicians may not have the time to perform a thorough mental health evaluation, and many rely on psychiatrists, psychologists, or social workers for the purpose. When that assistance is not available, patients may not receive an evaluation at all. The ED setting also makes it difficult to care for a mentally ill patient. The lack of privacy and the noisy, high-stimulus environment may make it uncomfortable for patients to participate in a mental health evaluation (Hoyle and White, 2003).
The psychiatric resources available within EDs vary greatly among hospitals. For example, teaching hospitals use psychiatric residents to provide consultations to patients with psychiatric problems. Other hospitals use a pool of mental health professionals, including clinical nurse specialists, to provide such services, although these professionals may not be available around the clock. Still, in some hospitals, nurses from inpatient units evaluate psychiatric patients in the ED (Falsafi, 2001). Other hospitals may have no psychiatric resources available to ED staff.
Children with mental health problems represent a real challenge to emergency care providers. Some children present to the ED with highly disruptive behaviors, antagonizing health workers and showing signs of rage. This disruptive behavior can mask the underlying diagnosis of a mental illness (Scheck, 2006). Another major challenge is that specialized psychiatric resources to assess and treat these patients are limited; children in need of psychiatric services often cannot be accommodated immediately. Psychiatric pediatric patients are more likely to require admission than nonpsychiatric pediatric patients (Khan et al., 2002). In many hospitals, however, because
of the lack of available psychiatric treatment services, children spend extended lengths of time in the ED or general pediatric inpatient unit waiting for an available psychiatric treatment slot. This situation is particularly problematic in those aged 16–18, who often do not meet the age criteria for adolescent or adult treatment services. In one study, 33 percent of pediatric patients in the ED in need of psychiatric admission were admitted to a pediatric medical floor and waited 1 or more days before being transferred to a psychiatric facility (Mansbach et al., 2003). While assessing the adequacy of mental health resources is beyond the scope of the present study, it is clear that there is a crisis in the mental health system that is having a profound effect on the emergency care system and must be addressed.
Children with Special Health Care Needs
According to the MCHB, children with special health care needs are “those who have or are at increased risk of having chronic physical, developmental, behavioral, or emotional conditions and who also require health and related services of a type or amount beyond that required by children generally” (DHHS et al., 2004). Between 6 and 35 percent of U.S. children meet this definition, depending on which types of disabling conditions are included (AAP, 2002). The number of such children has been growing as medical advances have improved the quality and length of life of children with complex medical conditions. In fact, these children are the most rapidly growing subset of pediatric patients (Sacchetti et al., 2000).
Children with special health care needs have complex, often multiple and lifelong disabilities, and many are dependent upon assistive technological devices and require a specialized approach to assessment, management, and treatment (Spaite et al., 2000; Kastner, 2004). They are also relatively heavy consumers of health care services. Studies of emergency care services for such children in Utah and Los Angeles found that they were more likely than other children to be admitted to the hospital, use EMS for transfer between health care facilities, and receive prehospital treatment such as intravenous therapy (Gausche-Hill, 2000; Suruda et al., 2000). While emergency care providers are increasingly likely to encounter such children (Singh et al., 2003), providers often feel uncertain about their ability to meet these patients’ needs (Deschamp and Sneed, 1997), and many EMS agencies do not address these children in their treatment protocols (Singh et al., 2003).
Several efforts have been made by states, communities, and hospitals to develop notification programs for prehospital providers to alert them to children with special health care needs in the area. One of the first was a program called EMS Outreach, developed in 2000 at Children’s National Medical Center in Washington, D.C., and supported by the EMS-C program. Under this program, parents and health care providers complete a
one-page form with the child’s medical information. The form is then faxed to the EMS agency, where the information is entered into the 9-1-1 call center’s computers. The EMS stations closes to the child’s home also receive the information. The program was expanded to provide all such children with a vinyl index card containing their medical information so that they would have the information with them when away from home. The program also encourages prehospital providers to make home visits so they can become familiar with the children’s special needs and establish relationships with both children and parents. In its first year, EMS Outreach enrolled 450 special needs children (Smith et al., 2001).
Similar programs exist in other areas. An EMS-C demonstration grant in New Hampshire was used to develop the Special Needs Identification Project (SNIP). Resources developed through the project are now available online to other states through the EMS-C program’s clearinghouse (EMS-C Program, 2003). Certainly as electronic health records advance in the coming years, special needs identification programs are likely to advance as well.
Use of Emergency Care Services by Children
Prehospital Services
Approximately 200 million emergency calls are received by 9-1-1 call centers each year (National Emergency Number Association, 2004); that number includes calls for medical, police, and fire needs. There are no reliable data on the number of pediatric medical calls made to 9-1-1 annually. (The dispatch system is discussed in depth in the committee’s companion report, Emergency Medical Services at the Crossroads.) However, some data are available on the use of prehospital EMS by children, revealing that in general, their use of such services is relatively low compared with that of adults. The vast majority of pediatric patients under age 15 come to the ED by private vehicle or public transportation and therefore do not receive prehospital emergency care. In 2003, only 3.8 percent of pediatric ED patients under age 15 arrived by ambulance, compared with 11 percent of patients aged 24–44 and 41 percent of those over age 74 (McCaig and Burt, 2005).
Although pediatric patients account for approximately 27 percent of all ED visits, studies suggest that they represent only 5 to 10 percent of all prehospital transports (Seidel et al., 1984; Federiuk et al., 1993). One important source of variation in that percentage is the differing definitions of “child” used by various studies. National data on prehospital calls are not presently collected; therefore, our understanding of pediatric calls is based on studies of individual EMS systems. One of the largest such stud-
ies, covering four states, found that most pediatric calls were for boys (56 percent), and most occurred in the evening and daylight hours. Children were transported in 89 percent of the cases, and care was refused by the patient or parents in approximately 8 percent of cases (Joyce et al., 1996). Data from one EMS agency indicate that utilization rates of EMS vary by pediatric age group. In a study of children under age 15 who used the Kansas City, Missouri, EMS system between 1993 and 1995, researchers found that infants under age 1 had the highest rate of use (47.4 children transported per 1,000 persons), followed by those aged 1–4 (26.2), 10–14 (17.5), and 5–9 (17.3) (Murdock et al., 1999).
Approximately half of pediatric prehospital runs are for injury; the rest are for a wide range of medical problems. A 1991 analysis of 10,493 pediatric calls in four California EMS agencies found that 57 percent were for injuries. The most common injuries included head trauma (19 percent of calls), lacerations (16 percent), and contusions (14 percent). Medical calls accounted for the remaining 43 percent, which included knee pain (12 percent), seizures (8.5 percent), neck or back pain (9 percent), ingestions (7 percent), respiratory distress (5 percent), and abdominal pain (5 percent) (Seidel et al., 1991).
However, these statistics mask important differences in prehospital calls across different pediatric age groups. A study of nearly 18,000 transports of children under age 21 in Albuquerque, New Mexico, showed that the most prevalent chief complaints varied by age. Medical complaints predominated in children under 5, while the leading cause of transports among children aged 5–10 was motor vehicle crashes. Assault was a leading cause for transport among patients over age 11 (Sapien et al., 1999).
A number of small studies have investigated the appropriateness of pediatric ambulance transports. Results of these studies generally reveal that the majority of pediatric prehospital runs are not for critical cases (Hamilton et al., 2003) although in general, they are appropriate transports. Foltin and colleagues (1998) developed a tool for evaluating the appropriateness of pediatric ambulance utilization. Applying this tool to patients arriving at two New York City hospitals, they found that the majority of requests for ambulances were appropriate and that dispatchers called for the proper level of care the majority of the time (Foltin et al., 1998).
Still, many pediatric ambulance transports are unnecessary. A study of pediatric transports in Delaware found that they were unnecessary for 28 percent of patients. Of the unnecessary transports, 60 percent were covered by Medicaid. In fact, several studies have shown that children covered by Medicaid have higher rates of EMS transport than other children (Murdock et al., 1999) and higher rates of inappropriate EMS transport (Kost and Arruda, 1999). A study of pediatric ambulance transports in Cleveland that excluded patients needing immediate resuscitation or trauma care found
that 82 percent of ambulance transports for children covered by Medicaid were medically unnecessary in the judgment of pediatric emergency physicians. For all medically unnecessary transports, just over half of the caregivers involved cited having no other means of transportation as the reason (Camasso-Richardson et al., 1997). However, determining whether an ambulance transport is medically necessary is much easier retrospectively. Some parents may view ambulance transport as necessary if they lack an alternative means of transportation to an ED (Camasso-Richardson et al., 1997).
Children’s Use of the ED
Data from CDC’s National Hospital Ambulatory Medical Care Survey (NHAMCS) allow a fairly comprehensive picture of pediatric ED visits. In 2002, there were approximately 29 million pediatric ED visits for children under age 15, representing nearly 27 percent of all ED visits. Data from the National Center for Health Statistics show that the number of pediatric visits to the ED for children under age 15 has been rising since 1997 (see Figure 2-2). In fact, the number of pediatric ED visits increased by nearly 20 percent between 1997 and 2003. The majority of pediatric ED visits (92
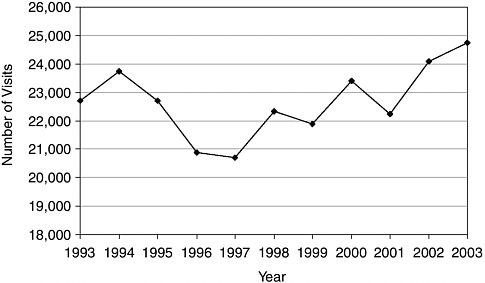
FIGURE 2-2 Number of ED visits for children under age 15 (in thousands).
SOURCE: NHAMCS, ED Summaries for 1993–2003.
percent) are to non-children’s hospitals (Gausche-Hill et al., 2004); as noted earlier, however, some general hospitals have specialized pediatric EDs.
Although the majority of pediatric ED visits are for children over age 5, infants (children under age 1) make up a disproportionately large proportion (13 percent) of all pediatric ED visits (see Figure 2-3). In fact, infants have a visit rate of 97.5 visits per 100 persons, much higher than the rate for all children under age 15 (40.8 visits per 100 persons) (McCaig and Burt, 2005). African American children have relatively high rates of ED use—62 visits per 100 children under age 15 compared with 39 visits per 100 for white children. Research on ED utilization for all ages has shown that African Americans had some of the largest increases in ED utilization between 1992 and 1997 (McCaig and Ly, 2002). Hispanic and other non-English-speaking children also use the ED at higher rates.
Nonurgent Use of the ED
Many pediatric visits to the ED are preventable or avoidable. Compared with adults, children make more visits to EDs that can be classified as ambulatory sensitive, meaning that patients do not require care within 12 hours, that immediate care is needed but could be provided in a typical primary care setting, or that immediate care is needed but could have been avoided with timely and effective primary care. Three-quarters of pediatric ED visits that occur overnight and do not result in admission are preventable or avoidable with primary care, suggesting a need for after-hours ambulatory care (Weinick et al., 2003). Perhaps not surprising, parental ED utilization
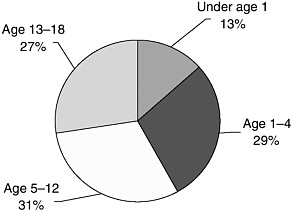
FIGURE 2-3 Percentage of ED visits for children under 18.
SOURCE: 2002 NHAMCS data, calculations by IOM staff.
is significantly associated with increased childhood utilization for both number of visits and number of nonurgent visits (Anderson et al., 2004).
The delivery of nonurgent care in the ED is of concern for three reasons. First, the primary care delivered in the ED may be of lower quality than that in other settings. The ED is designed for rapid, high-intensity responses to acute injuries and illnesses. It is fast-paced and requires intensive concentration of resources for short durations. Such an environment is ill suited to the provision of primary and preventive care (Derlet and Richards, 2000). Physicians in the ED typically do not have a relationship with patients, often lack patients’ medical records, face constant interruptions and distractions, and have no means of patient follow-up. Further, because they have low triage priority, nonurgent patients have extremely long wait times—sometimes 6 hours or more. Certainly it would be preferable for children to seek nonurgent care from a medical home.
Second, the literature is unclear as to whether providing nonurgent care in the ED is cost-effective. To some extent, EDs and trauma centers welcome the revenue generated by nonurgent pediatric visits if the hospital would otherwise serve a very low volume of emergent or urgent patients in the ED. Indeed, these revenues can be used to help cover the very large fixed overhead costs associated with maintaining the ED’s readiness to provide a full array of services on a round-the-clock basis.
On the other hand, some studies support the notion that costs for non-emergent care in the emergency setting may be substantially higher than those in a primary care setting (Fleming and Jones, 1983; White-Means and Thornton, 1995). Higher costs may be due to the frequent lack of patient records and resultant inability to construct a patient history, which necessitates a high frequency of full workups (Murphy et al., 1996). ED charges for services for minor problems have been estimated to be 2 to 5 times higher than those for a typical office visit (Kusserow, 1992; Baker and Baker, 1994), resulting in $5–7 billion in excess charges in 1993 (Baker and Baker, 1994). While studies probably overestimate the excess cost, it is nevertheless substantial. In contrast, Williams (1996) studied a sample of six hospitals in Michigan and found that average and marginal costs of ED visits were quite low, especially for those classified as nonurgent—perhaps below the cost of a typical physician visit. If hospitals build additional high-cost ED capacity as a result of the increased use of nonurgent care, however, the true cost of treating nonurgent care in the ED will be much higher than the marginal or average cost of treating such patients.
Third, nonurgent utilization may detract from the ED’s primary mission of providing emergency and lifesaving care. Regardless of their efficiency on average, EDs do not have unlimited resources. When the ED becomes saturated with patients that could be cared for in a different environment, there are fewer resources—including physicians, nurses, ancillary person-
nel, equipment, time, and space—available to respond to the population of emergent patients.
Payer Mix
The most common source of payment for ED visits is private insurance, although, as noted above, Medicaid coverage is quite prevalent among pediatric ED users (see Figure 2-4). Indeed, Medicaid represents an important source of health insurance coverage for children; fully 27 percent of all children were covered by the program in 2004 (U.S. Census Bureau, 2005). But looking at insurance status for all pediatric visits masks some important differences by age group. In fact, private coverage becomes more prevalent in higher age groups, while Medicaid coverage declines (see Figure 2-5). Research has shown that Medicaid recipients have disproportionately high rates of ED utilization, and often use the ED for nonurgent care or as their primary source of care (Newacheck, 1992; Gadomski et al., 1995; Liu et al., 1999; Sarver et al., 2002; Irvin et al., 2003). Medicaid patients (of all ages) use the ED at a rate of 81 visits per 100 persons, compared with 41.1 visits per 100 persons with no insurance and 21.5 visits per 100 persons for the privately insured (McCaig and Burt, 2005).
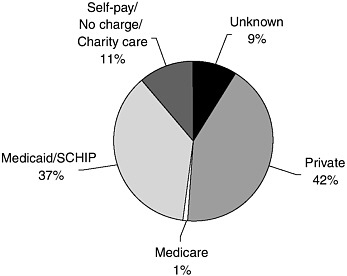
FIGURE 2-4 Pediatric ED visits by payer source.
NOTE: SCHIP = State Children’s Health Insurance Program.
SOURCE: 2002 NHAMCS data, calculations by IOM staff.
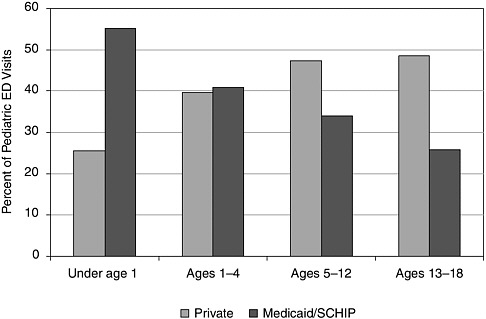
FIGURE 2-5 Percentage of pediatric ED visits covered by private insurance or Medicaid/State Children’s Health Insurance Program (SCHIP).
SOURCE: 2002 NHAMCS data, calculations by IOM staff.
There are several reasons why Medicaid enrollees have higher rates of ED utilization. A common assertion is that Medicaid enrollees have poorer access to primary care than other groups, which leads to greater use of the ED (Sharma et al., 2000). This explanation is plausible; because Medicaid reimburses providers at such low rates, it limits access to care, leaving the ED as the only source of care for some individuals. Additionally, Medicaid enrollees may have difficulty seeing primary care providers during regular office hours. According to one study, Medicaid providers who offer evening hours have patients who are less likely to use the ED (Lowe et al., 2005).
On the other hand, a study by Luo and colleagues (2003) suggests that, after controlling for confounding factors, type of insurance coverage is not associated with ED use for nonurgent visits (Luo et al., 2003). Access to primary care (Johnson and Rimsza, 2004) and continuity of care (having a strong relationship with a primary care provider) may be more important deterrents to ED utilization. In a study following 181 children, increased continuity of care with a primary care provider was associated with decreased ED utilization in the first 2 years of life (Brousseau et al., 2004). A larger study that reviewed claims data for more than 46,000 children found
that low continuity of care was associated with an increased risk of ED visits and hospitalization (Christakis et al., 2001).
Utilization in Rural Areas
Children in rural areas tend to use the ED more than their urban counterparts. According to data from the National Health Interview Survey (NHIS), 23 percent of rural children versus 20 percent of urban children had made an ED visit within the last year. Higher utilization of the ED in rural areas holds true for adults as well (Center on Aging Society, 2004). Many hypothesize that the shortage of primary care providers is a barrier to physician access for rural populations, where the physician-to-patient ratio is 1 to 3,500, clearly higher than the recommended 1 primary care physician for every 2,000 individuals.
Utilization of Services as a Result of Child Abuse
At least one study has found a link between the number of prior ED visits for injury and subsequent substantiated reports of child maltreatment (Spivey et al., 2005). A focused look at child abuse cases in the ED is needed, however, because national data do not adequately indicate the extent of the prevalence of such cases. Just over 1 percent of all pediatric ED patients are identified as having suffered child abuse; however, it has been estimated that more than 75 percent of all child abuse cases in the ED are missed (Kunen et al., 2003). In one study, researchers retrospectively identified 62 cases of child abuse in the ED. Half of the children had made at least one prior ED visit, and suspicion of abuse had been documented in only 5 cases. Those cases were reported to child protective services, but the children were not placed in protective custody. Of the 62 children identified as child abuse cases, most had made subsequent ED visits, but a history of abuse had not been documented during any of the subsequent visits for trauma (Saade et al., 2002). This study highlights the frequent missed opportunities in the ED to identify cases of abuse and intervene. In fact, abuse is often not recognized until severe injury or death occurs. A review of child abuse fatalities indicates that more than a quarter of the children involved had old fractures consistent with prior abuse and/or recent contact with health care providers (King et al., 2004).
Identification of child abuse varies by hospital type. A recent analysis of infants (children under age 1) admitted to hospitals for treatment for traumatic brain injury or femur fracture (excluding penetrating trauma or motor vehicle injury) shows that children’s hospitals diagnosed child abuse more than twice as frequently as did general hospitals (29 and 13 percent, respectively) (Trokel et al., 2006). This is a troubling finding considering
that the majority of injured children receive care in general rather than children’s hospitals.
The research on this subject indicates two failings. First, identification of child abuse is poor. Although emergency medicine physicians do receive didactic training in child abuse, a survey of residents found that many believed the training was not sufficient (Wagh and Heon, 1999). Results of one study also indicate that prehospital providers lack the knowledge necessary for recognizing, managing, and reporting cases of child abuse (Markenson et al., 2002). Second, high rates of coding errors for pediatric ED visits contribute to underestimates of child abuse. In many cases, child abuse cases identified in the ED are documented using only E-codes. Those cases would be missed in epidemiological studies that select cases using only ICD 995 abuse codes (Kunen et al., 2003).
QUALITY OF CARE
Performance measures specific to emergency care are in the initial stages of development, so formal assessments of the quality of the emergency care system are currently lacking. However, there is reason for concern about the quality of the care delivered. The emergency care system faces a number of challenges that threaten its ability to deliver quality care. Overwhelming demands on the system without the resources necessary to meet those demands contribute to a growing national crisis in emergency care. Under the current system, however, accountability for assuring access to or monitoring the quality of the system is dispersed among many providers. The result is that the system falls short of providing the type of care it should be able to provide.
Growing Pressures on the Emergency Care System
One of the greatest challenges faced by the emergency care system is overwhelming patient loads. The public’s dependence on the ED as a source of care is growing; the total number of ED visits rose by 26 percent between 1993 and 2003 (McCaig and Burt, 2005). In some EDs, nonurgent patients must wait 6 to 8 hours before being seen; nationwide, 2 percent of all patients, including pediatric patients, who come to the ED leave before ever being seen (McCaig and Burt, 2005; 2002 NHAMCS data, calculations by IOM staff).
The rising number of patient visits is only part of the problem; EDs are also experiencing great difficulty with moving seriously ill and injured patients from the ED into inpatient beds. In response to cost-cutting measures and lower reimbursement by managed care, Medicaid, and other payers, hospital inpatient bed capacity declined precipitously over the last decade.
To remain viable, some hospitals consolidated and reduced their number of inpatient beds (Brewster and Felland, 2004). Others closed important but unprofitable services, such as trauma, burn, and psychiatric care (IOM, 2003). When no vacant bed is available for an admitted ED patient, most hospitals require ED staff to provide ongoing care to the patient until one becomes available. Many patients are forced to wait hours for an inpatient bed, but some wait days (GAO, 2003). Because most EDs have a limited number of examination rooms and treatment bays, it is not uncommon for admitted patients to be kept on stretchers in ED hallways. This phenomenon, often called “boarding,” creates a logjam in the ED because these patients require ongoing attention and care, reducing the resources available to evaluate and treat incoming ED patients. EDs can quickly become overwhelmed by boarders and the crush of patients waiting for care. When patient volume becomes too high for the ED to handle, the hospital may order the ED to go “on diversion,” meaning that inbound ambulance traffic is directed to other hospitals. Diversion has become a common occurrence in many areas. In 2003, 45 percent of EDs were on diversion at some point, resulting in the diversion of an estimated 501,000 ambulance runs (Burt et al., 2006).
Diversion has a ripple effect throughout the community, impacting patients, other hospitals, and the community’s EMS system. Diversion delays lifesaving care to seriously ill and injured children and adults. By redirecting ambulances to a hospital farther away, it causes valuable time for treating patients to be lost (Neely et al., 1994). For patients who have suffered serious trauma, a heart attack, or a stroke, timely care is essential to prevent death. In these instances, extra minutes spent in transit can have dire, even fatal consequences. For patients with non-life-threatening injuries and illnesses, the extra commute time to an ED bed can cause unnecessary pain and stress. Also, when one hospital goes on EMS diversion, others often follow, either because the inflow of patients becomes too great to handle or because they wish to limit exposure to an influx of uninsured patients to the ED. The result is the health care equivalent of a “rolling blackout” as hospital after hospital closes its doors to ambulance traffic.
When hospitals are on diversion, ambulance transport teams spend more time in transit. The result is not only less accessibility for the community, but also higher levels of stress to providers who are regularly pressured to find an open hospital or care for patients in the ambulance for an extended period of time.
Boarding and ambulance diversion have been prevalent over the past several years. A number of studies have documented the problem, but perhaps most telling is a point-in-time study based on a survey sent to a random sample of hospitals. On Monday, March 12, 2001 (a typical Monday), at 7:00 PM (local time for hospitals), 11 percent of responding hospitals reported being
on diversion and 22 percent having patients boarded, awaiting transfer to an inpatient bed (Schneider et al., 2003). However, because most communities and states do not systematically monitor rates of ambulance diversion and the boarding of inpatients in hospital EDs, the extent of these problems and the magnitude of their impact on access to care are largely unknown.
Most studies of boarding and diversion do not specifically address pediatric patients, so the extent to which these problems affect such patients is also unknown. However, a Government Accountability Office (GAO) study found that ED staff have less difficulty transferring patients to pediatric beds than to adult critical care or other adult inpatient beds (GAO, 2003). Some children’s hospitals report that they do not go on diversion because there is no alternative source of care for critically injured or ill pediatric patients. However, ED crowding is at least anecdotally an important problem for many children’s hospitals. And in hospitals where adults and children are treated in the same ED, the hospital’s diversion status will affect pediatric and adult patients equally.
Another challenge to the system is that hospitals are finding it increasingly difficult to identify key specialists, such as neurosurgeons and orthopedists, who are able and willing to take call to treat emergency cases. Surgical specialists typically do not work in the ED full time, but serve in an on-call capacity in case they are needed. Surveys confirm that the availability of on-call specialists, including pediatric specialists, in many areas is rapidly eroding or is already inadequate to meet patients’ needs (AAP, 2003; ACEP, 2004; Vanlandingham et al., 2005), and that the problem is worsening (Green et al., 2005; O’Malley et al., 2005).
The role of the emergency care system as a safety net provider also takes a toll. Emergency care providers are the providers of last resort for millions of patients who are uninsured or lack adequate access to care from community providers. Hospitals on the front lines of safety net care encounter patients with intractable social problems, complications resulting from substance abuse or mental illness, and exacerbations of chronic diseases because of inadequate primary care and lack of adherence to medical instructions. Much of the service provided to these difficult patients is compensated poorly or not at all. This care places tremendous financial pressure on safety net hospitals, many of which have closed or are in danger of doing so as a result.
It is within this difficult environment that the emergency care system struggles to meet the unique needs of pediatric patients.
Pediatric Emergency Care and the Six Quality Aims
One way to assess how the current emergency care system is meeting the needs of children is to consider each of the six quality aims for care
identified by the IOM in its landmark report Crossing the Quality Chasm: A New Health System for the 21st Century: care should be safe, effective, patient-centered, timely, efficient, and equitable. Although evidence often is limited or dated, there is reason to believe that pediatric emergency care is deficient in each of the six aims.
Safe
Patient safety is often compromised in EDs because of overcrowding, the rushed and chaotic environment, frequent provider interruptions, provider fatigue due to long shifts, and limited information on patients’ medical histories (Chisholm et al., 2000; Goldberg et al., 2002; Chamberlain et al., 2004). However, it is difficult to determine the safety of emergency care services for children because data on medical errors in emergency care generally are not available. The one exception is evidence suggesting that medication errors in the ED are common for pediatric patients (Selbst et al., 2004; Marcin et al., 2005). Indeed, one study found prescribing errors in the charts of 10 percent of all patients at one pediatric ED (Kozer et al., 2002). Medication errors are especially common for children because doses must be calculated based on the patient’s weight; incorrect decimal placement frequently results in 10-fold prescribing errors (Selbst et al., 2004).
Another important threat to the safety of children during emergency care is the lack of knowledge among some providers of how treatment for children differs from that for adults. Without such knowledge, a provider can injure a child while providing care. For example, if a provider does not use special pediatric equipment or exercise proper care when intubating a child, life-threatening errors can be made. Nevertheless, physicians with limited pediatric training or experience are responsible for the majority of patient care in some EDs (Goldmann and Kaushal, 2002). In fact, in many parts of the country, the physicians who staff EDs are not residency trained in emergency medicine or pediatric emergency medicine (Moorhead et al., 2002). Unfortunately, these providers may treat children as they would an adult because of their lack of training and experience (Gausche et al., 1998; Scribano et al., 2000).
Effective
The question of whether commonly practiced emergency care interventions are effective is a surprisingly difficult one to answer for many types of interventions. Particularly in the EMS environment, there is a paucity of evidence to support the treatments that are performed, and few data are collected that could be useful in understanding the effectiveness of interventions (Callaham, 1997). Little or no evidence exists to support basic system design
features, such as tiered levels of response, intensity of medical direction, and type of EMS system (e.g., fire department–based, volunteer). The value of deploying paramedics, for example, has been questioned by a recent study (Stiell et al., 2005). A number of clinical practices currently employed, particularly in the prehospital environment (e.g., endotracheal intubation), do not have proven benefits (Gausche et al., 2000; Murray et al., 2000; Wang and Yealy, 2005).
Physician practice patterns for pediatric patients also vary widely, and examples of these variations are numerous. Substantial variations exist among physicians of different specialties—perhaps because of differences in specialty training—in the management of fever (Isaacman et al., 2001), croup (Hampers and Faries, 2002), splenic injury (Davis et al., 2005; Stylianos et al., 2006), diabetic ketoacidosis (Glaser et al., 1997), bronchiolitis (Mansbach et al., 2005), and febrile seizures (Hampers et al., 2000), as well as in resuscitation (Scribano et al., 1997) and use of sedation (Krauss and Zurakowski, 1998). In some of these cases, there are guidelines for treatment (Isaacman et al., 2001); in others, it is unclear which treatment strategy is most beneficial (Glaser et al., 2001; Mansbach et al., 2005), and outcomes are likely to vary based on the treatment provided. This variability in the management of the same conditions suggests that not all children are receiving the most effective care.
Patient-Centered
Patient-centeredness encompasses the qualities of compassion; empathy; and responsiveness to the needs, values, and preferences of patients. In the case of pediatric care, where parents are recognized as the child’s primary source of strength and support and play an integral role in the child’s health and well-being, the term “family-centered care” is often used instead (Eichner et al., 2003). In the prehospital environment, this means providers should take the time to explain the function of equipment, procedures being performed, and their rationale so family members can be better prepared to make decisions about the child’s care. In the ED, family-centered care includes creating a comfortable environment for children and their families, having child life specialists on staff, and enhancing communication between providers and families. In both environments, such care involves giving families the option of being present during procedures and resuscitation as long as doing so does not compromise provider or patient safety.
However, few EDs have written policies or guidelines that allow for the family’s presence during invasive procedures (MacLean et al., 2003), and few EMS providers are trained in managing family members or integrating their needs with those of the patient (Loyacono, 2001). Further, many EDs, particularly nonpediatric EDs, can hardly be described as family-friendly,
given long wait times to be seen and uncomfortable environments. In some EDs, adults and children wait together and are treated in the same patient care areas, which can frighten children.
Timely
People expect that patients with life-threatening problems will have prompt access to emergency care in the prehospital setting as well as in the ED. But timeliness of care is compromised in overcrowded EDs. The practices of ambulance diversion and patient boarding and their effects in delaying care were discussed above. Likewise, long ED wait times can result in protracted pain and suffering and delays in diagnosis and treatment (Derlet et al., 2001; Derlet, 2002; James et al., 2005). Unfortunately, existing studies on timeliness of care do not include analysis specific to pediatric patients.
Of particular concern are children who leave the ED without being seen. Several studies have investigated which patients leave without being seen and why. Most have concluded that patients do so because the wait was too long (Stock et al., 1994; Quinn et al., 2003), although one Canadian study found that children most often leave because they begin to feel better (Rowe et al., 2003). The majority of patients who leave without being seen have conditions of low acuity (Fernandes et al., 1994), but in some cases such patients are in need of immediate medical attention (Baker et al., 1991; Fernandes et al., 1997). In one study, two-thirds of patients who left without being seen could identify no alternative site of care that would be available to them other than the ED (Baker et al., 1991). Patients who leave without being seen are more likely than those who receive care to report pain or worsening of the seriousness of their problem (Bindman et al., 1991). Many end up returning to the ED at another time, and a small percentage subsequently require hospitalization (Sainsbury, 1990; Bindman et al., 1991).
Specific data on prehospital response times for pediatric patients based on acuity are not currently available. However, seriously ill or injured children pose a real challenge to the system’s ability to provide timely care, particularly when pediatric specialists are needed. Ambulances may have to drive to a distant hospital to access providers with pediatric expertise. But more troubling, some EMS agencies authorize ambulances to transport patients only to the nearest hospital, even if that hospital is not appropriate for the patient. In addition, geographic boundaries of an EMS catchment area may limit where ambulances may transport patients.
Timeliness also encompasses the treatment of pain, and there is some evidence indicating that children do not receive pain management in a timely manner. In one study of hospitals in Illinois, only half of children (aged 15 and younger) in severe or moderate pain were offered an analgesic. Older
children were more likely to be offered opioids than younger children, particularly those under age 1 (Probst et al., 2005).
Efficient
Efficiency refers to the system’s ability to avoid waste, including the waste of equipment, supplies, and energy (IOM, 2001). The considerable patient loads that EDs are required to treat demand efficient care delivery. As discussed earlier, many children who use prehospital and ED services might be treated elsewhere if such care were available. One study found that when Medicaid children are provided enhanced, coordinated access to primary care, utilization of the ED is lower for healthy children, while the total cost of care remains the same (Wang et al., 2005). Whether it is efficient for those patients to receive care in the ED rather than wait for treatment at a later date remains open for debate, however. Although EDs are presumed to have many inefficiencies, the economies of scale resulting from utilization of fixed capital may make it cost-effective to accommodate a certain amount of “after hours” nonurgent care in the hospital ED if doing so enables patients to be treated more quickly and allows parents to work the following day. When the opportunity costs to patients and employers for reduced time loss are factored in, the emergency system may look like a reasonably good alternative. Regardless, for the many patients who use the ED for nonurgent care because they lack access to other sources of care, restricting use of the ED would jeopardize their health.
As noted earlier, under the current system, emergency care providers lack access to patients’ medical histories, which can result in the ordering of diagnostic tests that the patient has already received (Cordell et al., 1998). Many emergency care physicians fear the legal consequences of failing to detect rare but dangerous conditions, and compensate by ordering costly diagnostic tests and treatments (Katz et al., 2005). Although some surveys indicate that defensive medicine is not a widespread problem or a major contributor to rising health care costs (Office of Technology Assessment, 1994; Pearson et al., 1995), research suggests that the phenomenon does occur and that physicians who perceive a high risk of a lawsuit are more likely to order tests and procedures that may not be needed (Lawthers et al., 1992). Defensive medicine may be especially likely to occur in emergency settings, where the prevalence of serious illness and injury is high, the public’s expectation of diagnostic accuracy is high, and the physician’s risk of making an error is increased by the limited time available to make a diagnosis and the lack of an ongoing relationship with the patient and his or her family.
Overall, it would be a considerable stretch to describe the emergency care system as efficient. The practice of boarding patients, long waits in
EDs, ambulance diversion, and long EMS patient off-load times all indicate that the system does not operate smoothly. Yet all of these issues apply to both adult and pediatric patients. There is little information on efficiency specific to pediatric emergency care. An exception is one study that looked at the efficiency of residents in a pediatric ED in terms of number of patients evaluated and treated. The study showed that efficiency varied by residents’ subspecialty and years of training (Dowd et al., 2005). Recognizing the paucity of information on the cost-effectiveness of pediatric emergency care, the EMS-C program cited the development of additional economic analyses of pediatric emergency care as an objective in its most recent 5-year plan (MCHB, 2004a).
Equitable
Disparities in health care access and outcomes have long been a problem in the United States (IOM, 2002; AHRQ, 2003). One might assume that because the emergency care system serves all individuals regardless of insurance status, age, race, or income, it is characterized by greater equity relative to the overall health care system. However, of the small number of studies that have looked at equity in emergency care and the still fewer that have examined equity in pediatric emergency care, many indicate that inequities in treatment and access exist.
As discussed above relative to effectiveness, not all patients with the same condition receive the same type of treatment, a fact that indicates a lack of equity in the receipt of care. There is some evidence of variability in treatment based on race and ethnicity for patients of all ages. For example, African Americans and Hispanics are less likely to receive pain medication for certain conditions (Todd et al., 2000), and African American patients are more likely than whites to be denied authorization for ED visits by their primary care provider (Lowe et al., 2001). Such disparities extend to children of different races and ethnicities. Studies indicate that wait times for pediatric patients vary based on race and ethnicity (James et al., 2005), that racial and ethnic disparities exist in the ED care provided to children with mild traumatic brain injury (Bazarian et al., 2003), and that African American children with orthopedic fractures covered by Medicaid are less likely to receive parenteral analgesics and sedatives than other children with similar injuries (Hostetler et al., 2002).
Although only a limited number of studies have looked at racial and ethnic disparities in emergency care, some believe the problem is greater than is currently recognized. Racial and ethnic disparities may occur in the prehospital setting through ambulance destinations, triage assessments, diagnostic testing, and disposition decisions. In the ED, disparate treatment
may include the timing and intensity of therapy, patterns of referral or prescription choices, and/or priority for hospital admission or bed decisions (Richardson et al., 2003).
Disparities in care also occur based on age. Prehospital providers are less likely to administer treatment to young children compared with adults (Gausche et al., 1998; Scribano et al., 2000). For example, one study found that paramedics are less likely to perform basic resuscitation procedures for pediatric patients than for equally critical adults (Su et al., 1997). (This issue is discussed further in Chapter 4.) Children are also less likely to receive pain medication than adults, and the youngest children, those under age 2, are less likely to receive such medication than older children (Selbst and Clark, 1990; Petrack et al., 1997; Alexander and Manno, 2003).
Naturally, geography also plays an important role in access to emergency care and pediatric specialists. Issues related to rural pediatric emergency care are explored below.
Not all studies indicate disparities in treatment, however. Two studies found that ED triage and admission decisions were made independently of racial, ethnic, or financial considerations (Kellermann and Haley, 2003; Oster and Bindman, 2003).
Rural Pediatric Emergency Care
In 2000 there were more than 15 million children below age 18 residing in rural areas, constituting 26 percent of the rural population of the United States (U.S. Census Bureau, 2000). While there is no standard definition of a rural area, the basic demographic feature of such a locale is that it is a place of low population density and small aggregate size (IOM, 2005). Children in these areas encounter significant barriers to appropriate emergency care (AAP, 2000). Friedlander and Alessandrini (2004) pointed out that rural children are classically underserved, with conditions of poverty transcending geographic considerations. Rural children are more likely than their nonrural counterparts to be poor, to lack access to primary care and appropriate referral sources, to be covered by a public insurance program, and to utilize an ED.
In 2003, more than 14 percent of people living outside of a metropolitan area lived below the poverty level, compared with 12 percent of their metropolitan counterparts (U.S. Census Bureau, 2004). According to the Kaiser Commission on Medicaid and the Uninsured, 47 percent of rural families have incomes below 200 percent of the poverty level (compared with 27 percent of nonrural families), qualifying a disproportionately large number of rural children for Medicaid benefits and emphasizing their reliance on public insurance. Fewer than half of rural children living in counties not adjacent to a county with a large city have private insurance cover-
age. Thirty percent of these children are covered by Medicaid or the State Children’s Health Insurance Program (SCHIP) (compared with 19 percent of urban/adjacent rural children), and 1 in 5 are uninsured (Kaiser Family Foundation, 2003).
Rural residence has been demonstrated to be predictive of ED use by low-income children (Polivka et al., 2000). Sharma and colleagues (2000) determined that for infants, the highest rate of ED use, 1.8 per person-year, was among rural white infants on Medicaid. The lowest rate, 0.4 visits per person-year, was among urban white infants with commercial insurance (Sharma et al., 2000).
Rural emergency care for pediatric patients is characterized by many of the same issues that affect emergency care in other areas. However, many studies have shown differences in the use of pediatric emergency care between rural and urban areas. In an examination of pediatric coroners’ cases in both rural and urban California counties, rural children were found to be less likely to use EMS provider services than their urban counterparts (66 versus 84 percent), and a significantly greater number of rural children died on the street or highway (Gausche et al., 1989). Seidel and colleagues (1991) found that trauma was a more frequent complaint in rural areas of California, responsible for 64 percent of all rural prehospital calls. A study by Svenson and colleagues (1996) found trauma in rural settings of Kentucky to be responsible for nearly 50 percent of EMS calls. Rural trauma centers have also been demonstrated to receive proportionately more victims of motor vehicle crashes (28.5 percent of patients) and “other” categories of injury (28.2 percent), to which bicycle injuries are assigned (Nakayama et al., 1992). Similar injury patterns were noted by Serleth and colleagues (1999) between 1990 and 1993, with more than half of all pediatric trauma admissions being the result of injuries related to falls, recreational activities, and motor vehicle crashes.
Despite the variations in time and setting in the above studies, each found trauma to be a leading cause of EMS activation by rural children. Yet there are deficiencies in the provision of ALS in rural areas. The use of BLS/ALS has been found to be dependent on the patient’s age and the level of provider care, with provision of ALS to younger children being less frequent than that to older patients. Failure to provide ALS occurred even though time on scene would not have been prolonged (Svenson et al., 1996). Gausche and colleagues (1989) found that only 66 percent of rural child victims of trauma received ALS interventions, 31 percent fewer than urban children in the same study (Gausche et al., 1989). Thus rural children are more likely to require EMS for traumatic injuries but less likely to obtain EMS services and appropriate life support modalities. Additionally, results of a recent study of admissions in rural EDs indicate higher nonessential admission rates at rural hospitals and by nonpediatric EM physicians, which
may reflect a lack of resources, comfort, or expertise among emergency providers for the care of pediatric patients (Derrington et al., 2005).
Rural emergency care providers and provider organizations face a number of operational challenges not encountered by those in urban or suburban areas. In rural areas, the relatively low volume of emergency calls in relation to the high overhead of maintaining a prepared staff results in very high costs per transport. To lower those costs, many rural EMS squads rely on volunteers rather than paid EMS providers, which by nature results in a less stable system. In many rural communities, younger residents are leaving while the remaining population becomes more elderly. As a result, the pool of potential volunteers is dwindling as their average age and the demands on their time increase. The closure or restructuring of many rural hospitals has further increased the demand on rural EMS agencies by creating an environment that requires long-distance, time-consuming, and high-risk interfacility transfers. Another challenge facing some rural areas is that the population can swell—double or triple—during the tourist season. Thus the EMS staffing required throughout the year varies.
Under the Balanced Budget Act of 1997, Congress established the Medicare Rural Hospital Flexibility Program. In additional to providing cost-based reimbursement to certain rural hospitals, the “Flex Program” provides states with grants to support their rural health infrastructure and foster the growth of collaborative rural health care delivery systems. In fiscal year 2003, states received approximately $22 million under the program, with the average state award being approximately $500,000. Development of EMS systems has been a growing focus of state planning efforts under the grants (Flex Monitoring Team, 2004). The committee finds this trend promising and encourages states to focus attention on pediatric needs within rural EMS systems.
REIMBURSEMENT FOR PEDIATRIC EMERGENCY CARE
The costs of providing emergency care services reflect not just the operational costs of responding to each emergency call, but also the costs associated with having personnel available around the clock. Appropriate reimbursement for pediatric emergency care services is of obvious importance. It allows emergency care organizations to increase their readiness by hiring and retaining providers with the right mix of skills and training, to offer continuing pediatric education, and to equip providers with appropriate pediatric supplies. It also allows providers to make investments that can improve the quality of care delivered, from the development of new quality initiatives to the installation of information systems.
Funding for pediatric emergency care differs from that for adult emergency care in that the payer mix is different, which has important implica-
tions for reimbursement levels. Emergency care provider organizations are highly dependent on the Medicaid and SCHIP programs for reimbursement for pediatric emergency care services. To the extent that those programs do not adequately cover the cost of services provided to Medicaid and SCHIP enrollees, providers suffer financial losses in caring for those patients. As of this writing, policy makers are facing a dilemma with regard to the Medicaid program’s growing expenditures. Among the options being considered are significant cuts in benefits coupled with increases in patient cost sharing. While the committee believes that fair payment for emergency care services under Medicaid is critical, it recognizes the political and economic realities associated with proposing increases in payment at this time. As a result, this section is intended to highlight some of the difficulties related to reimbursement for pediatric emergency care services rather than to suggest immediate changes to payment and policies.
Payer Mix
Although some emergency care providers may receive financial support through public subsidies or private donations, their primary source of income is reimbursement for services. Because reimbursement levels vary based on the insurance status of the patient, payer mix is critical to the financial health of providers.
Data from the March 2004 Current Population Survey (CPS) indicate that in 2003, 61 percent of children were covered by private insurance and 27 percent by Medicaid or other public insurance programs (for example, SCHIP or Medicare), while 12 percent were uninsured (Kaiser Family Foundation, 2004b). If all children used emergency services at the same rate, the payer source for emergency care visits would mirror the data on insurance coverage for children. However, that is not the case. There are important differences in the use of emergency services by insurance status. Table 2-7 displays information on the expected source of payment for ED visits made by children and adults in 2002.
As noted earlier, privately insured children use the ED less than publicly insured or uninsured children. Although 61 percent of children are covered by private insurance, they represent approximately 42 percent of pediatric visits to EDs. Children covered by Medicaid or other public programs tend to use the ED at disproportionately high rates. Only 27 percent of children are covered by Medicaid or other public insurance, but they account for at least 37 percent of all pediatric visits to EDs. Uninsured children tend to use the ED at rates proportionate to their numbers.
The difference in payer mix between nonelderly adult and pediatric ED visits is also of note. Children are more likely to be covered by Medicaid or SCHIP than their adult counterparts, but considerably less likely to be
TABLE 2-7 Payer Mix for ED Visits, Children and Adults, 2002
uninsured. Data on payer mix for prehospital care at the national level are unavailable, but as noted earlier, data from regional ambulance services confirm the heavy reliance of pediatric patients on Medicaid or SCHIP for health insurance coverage. However, these regional data also indicate that a large percentage of pediatric ambulance calls are for uninsured children, and therefore not likely to be reimbursed. Indeed, an examination of EMS transports by the Albuquerque, New Mexico, ambulance service (which provides 99 percent of EMS transports in that city) during 1992–1995 showed that 57 percent of transported patients under age 21 were uninsured. That study also found that payment source varied by patient age, with public insurance being overrepresented among patients younger than age 11, private insurance and lack of insurance being overrepresented among those aged 11–16, and lack of insurance being overrepresented among those aged 17–20 (Sapien et al., 1999).
Medicaid and the State Children’s Health Insurance Program
Medicaid is a federal–state health insurance entitlement program that provides coverage for low-income individuals. The program is administered by the states, and the federal government sets guidelines and matches state spending at rates of between 50 and 77 percent, depending on state per capita income (Kaiser Family Foundation, 2004a). Children typically qualify for Medicaid coverage by meeting financial criteria, which vary across states. Federal law mandates coverage of some groups below specified minimum income levels, but also allows states to expand Medicaid eligibility beyond those levels. Medicaid coverage is relatively broad, covering inpatient and outpatient services including emergency services; physician and nurse practitioner services; nursing home and home health care; laboratory and x-ray services; and early and periodic screening, diagnostic, and treatment.
In addition, states commonly cover a wide range of optional Medicaid services, including the costs of prescription drugs, durable medical equipment, and clinic services (Kaiser Family Foundation, 2004a). As of June 2003, more than 42 million individuals were enrolled in Medicaid (CMS, 2003). Children represent approximately 50 percent of Medicaid enrollees (Kaiser Family Foundation, 2004a).
SCHIP is a relatively new public insurance program, introduced in 1997. It is designed to cover “near-poor” children whose family income levels are too high for them to qualify for Medicaid yet too low for them to purchase private coverage. SCHIP operates like the Medicaid program in that it is administered by the states, and funding is matched by the federal government up to a limit. Under the SCHIP program, however, states have greater flexibility in defining eligibility requirements and benefits. Some states design their SCHIP program as essentially an expansion of their Medicaid program; in other states, SCHIP is an entirely separate health insurance program with different benefits and cost-sharing requirements. Unlike Medicaid, SCHIP is not an entitlement program; in fact, some states have a waiting list for enrollment. In the third quarter of 2004, approximately 3.5 million children were enrolled in SCHIP (CMS, 2004).
Children covered under Medicaid and SCHIP are needy in terms of their low family incomes and prevalence of health problems. Compared with privately insured children, those covered by Medicaid or SCHIP are more likely to report only fair or poor health, to have asthma, to have learning disorders, and to have medical conditions that require regular treatment with prescription drugs (Ku and Nimalendran, 2004).
States have considerable freedom to develop their own methods and standards for Medicaid reimbursement. The Omnibus Budget Reconciliation Act of 1989 requires that Medicaid payments to providers be “sufficient to enlist enough providers so that care and services are available under the plan at least to the extent that such care and services are available to the general population in the geographic area.” This provision, known as the “equal access” provision, has traditionally not been enforced by the Centers for Medicare and Medicaid Services (CMS). In fact, many states establish physician payment rates without guidance and may not review their rates for several years at a time (AAP, 2002). The result is that Medicaid reimburses care at a lower rate than other payers. Medicaid reimbursement rates are approximately 60 percent of Medicare rates and only 35 to 40 percent of private insurance rates. In a survey conducted by the AAP, more than half of responding pediatricians said that Medicaid payments failed to cover their overhead costs (AAP, 2002).
The low reimbursement rates under Medicaid are evident from the results of a 2001 AAP survey of state Medicaid offices. For three different types of ED visits, the average Medicaid rate was well below the Medicare
rate in the vast majority of states. Selected survey results are shown in Table 2-8. These results also reveal the tremendous variation in reimbursement rates across states.
Medicaid rates for emergency services are so low that hospitals tend to collect a greater portion of their charges from the uninsured than from Medicaid patients. Tsai and colleagues (2003) examined payments for ED care using 1998 data from the Medical Expenditure Panel Survey. They found that in 1998, the proportion of charges paid by the uninsured was 58 percent; the proportion paid by Medicaid was only 44 percent. Their analysis included both children and adults.
There are other important problems with Medicaid reimbursement in addition to the low rates. States also have various rules and practices under Medicaid that limit the ability of providers to collect timely payment for services provided. First, some Medicaid programs provide reimbursement for only one service per patient per day. But many children, particularly those with special needs, receive multiple services on the same day. As a result, some services go completely unreimbursed. Second, some states have rules against reimbursing providers if the beneficiary seeks service in another state. This is particularly troubling to providers near a state boarder, such as Washington, D.C., Chicago, and Kansas City. Many patients opt for care outside of their state of residence, particularly if a children’s hospital is on the other side of the border. In addition, the Medicaid payment cycle can be twice as long as that of most private insurance payers, so providers do not receive timely reimbursement. Third, some Medicaid programs do not reimburse for a variety of services that are provided to pediatric patients in the ED. An example is sedation and analgesia, which are not reimbursable under the Illinois Medicaid program. Likewise, prevention services provided in the ED are typically not reimbursed even though they have the potential
TABLE 2-8 Medicare and Medicaid Rates for ED Visits, 2001
|
ED Visit |
Medicare Rate |
Average Medicaid Rate |
Lowest Medicaid Rate |
Highest Medicaid Rate |
Number of States Where the Medicaid Rate Is Higher Than the Medicare Rate |
|
Low-complexity decision |
$30.61 |
$25.85 |
$9.00 |
$50.40 |
11 |
|
Intermediate-complexity decision |
$64.66 |
$41.68 |
$9.00 |
$97.00 |
2 |
|
High-complexity decision |
$100.62 |
$61.28 |
$9.00 |
$148.91 |
1 |
|
SOURCE: AAP, 2001b. |
|||||
to reduce future ED visits. Finally, the retrospective nature of Medicaid payment does not account for the diagnostic resources whose use may be necessary during an ED visit. In some states, for example, Medicaid may pay for treatment of a fractured ankle but not a sprained ankle; however, the only way to determine whether the ankle is fractured is with an x-ray. If the x-ray is negative, Medicaid will not pay for it or for the service provided to the patient.
Clearly, there are a number of problems associated with Medicaid payment for pediatric emergency care services. While coverage expansions through SCHIP may aid in offsetting the costs of uncompensated care, the low reimbursement rates and poor payment policies of both programs may not meet the financial needs of operating a pediatric ED.
The impact of Medicaid’s poor payment policies is felt most acutely by safety net and children’s hospitals because of their sizable dependence on Medicaid as a revenue source. Data from Children’s Memorial Hospital in Chicago indicate that a large and growing number of ED patients are covered by Medicaid (see Table 2-9). Because of Medicaid’s poor payment rates and policies, the hospital lost $1.2 million in 2004 for treating 28,000 patients covered by Medicaid. If Medicaid paid the same rates paid by Medicare, the hospital would just about break even on those ED patients. While it is true that children’s hospitals receive funds from additional sources, such as disproportionate share hospital payments and graduate medical education (GME) funding, those sources still may not cover the hospital’s operating expenses. Many children’s hospitals pursue philanthropy as a way to cover operating expenses.
Given the low payment rates under Medicaid, it should not be surprising that children—even those with private insurance coverage—have difficulty accessing pediatric specialists in the ED. If specialists expect that one-half of all patients at children’s hospital EDs will be covered by Medicaid, they may not be willing to provide care in those settings.
Medicaid payment for prehospital services is no better. Medicaid pays a fixed rate—$25 in some states—for an EMS transport, regardless of the complexity of the case or the resources utilized. Additionally, reimburse-
TABLE 2-9 Growing Dependence on Medicaid at One Children’s Hospital
|
|
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
|
Total ED Visits |
40,556 |
39,991 |
43,882 |
46,841 |
47,200 |
49,511 |
|
Medicaid ED Visits |
20,278 |
20,395 |
23,696 |
26,230 |
26,902 |
28,201 |
|
Percent Medicaid |
50% |
51% |
54% |
56% |
57% |
57% |
|
SOURCE: Data from Children’s Memorial Hospital Emergency Department. |
||||||
ment is provided only when a patient is transported. This naturally leads to perverse incentives to transport patients to the ED even if they do not require an ED visit.
Other Payment Considerations
While Medicaid concerns are primary, a number of other reimbursement issues specific to pediatric care make it difficult for emergency care providers to collect appropriate revenues for services rendered.
Only a small percentage of children (less than 1 percent) have health insurance coverage under the Medicare program (U.S. Census Bureau, 2005). Medicare is a federal program that provides health care coverage to senior citizens and individuals with disabilities. However, the way Medicare reimburses providers—using the resource based relative value scale (RBRVS)—serves as a model for other payers. The RBRVS is a way of valuating physician services based on the work, associated practice expenses, geographic location, and professional liability expenses. However, the RBRVS does not recognize the considerable effort involved in providing emergency services to children—particularly infants and young children. In fact, there are several reasons why pediatric emergency care requires greater physician time and attention than adult emergency care. First, emergency providers must respond to childrens’ fear and anxiety prior to examinations or treatment, which tends to add to the time and stress involved. Providers must also address the needs of parents, which adds an element of complexity. Second, providers must constantly adapt the examination or procedure in response to the patient’s level of cooperation or changing behavior. For example, a child may need to be sedated to allow ED staff to perform suturing, whereas suturing an adult is a relatively simple task. Third, pediatric emergencies may require follow-up with a number of different individuals and organizations, including day care facilities, schools, and parents/guardians, which results in increased expenditures of time (Committee on Coding and Nomenclature, 2004). (Certainly similar arguments could be made for other patient groups, such as the elderly, that require extra work likewise not recognized by the RBRVS.)
Like some Medicaid programs, the Medicare program does not provide payment for certain services provided in the ED. Some neonatal and pediatric critical care services, preventive care, some vascular care, immunizations, and sedation/analgesia are not recognized reimbursable pediatric services. Because the Medicare payment system serves as a model for private payers and some Medicaid programs, other payers also exclude reimbursement for those services.
In addition to being an important source of reimbursement for patient services for the elderly, Medicare is the largest source of funding for GME.
In fact, U.S. teaching hospitals receive approximately $7 billion each year to help cover the additional expenses associated with training medical residents (HRSA, 2002). However, because children’s hospitals treat children rather than many elderly Medicare recipients, they have largely been excluded from Medicare GME payments (National Association of Children’s Hospitals and Related Institutions, 2006). Congress recently addressed this imbalance through special funding for independent teaching children’s hospitals. However, children’s hospitals are arguably less able than other hospitals to provide financial support for resident training. This situation has resulted in a reluctance on the part of some children’s hospitals to have emergency medicine residents train at their facilities because those residents compete with pediatric residents and pediatric specialists for limited training dollars.
Despite the reimbursement problems associated with pediatric emergency care services, a number of hospitals have recently added pediatric EDs. Although this movement appears counterintuitive, hospitals view pediatric EDs as a way of generating revenue for the organization. Parents and caregivers generally prefer to bring their children to a pediatric ED rather than a general ED. In addition, pediatric EDs offer a marketing opportunity by bringing additional family members into contact with the hospital. One study found that an off-site pediatric urgent care clinic helped increase a hospital’s market share, enabling it to attract a large number of well-insured patients (Tennyson, 2003). Certainly these new pediatric EDs are not opening in areas where many uninsured and Medicaid children reside, however. In fact, they may be causing additional financial difficulties for children’s hospitals if they are drawing privately insured patients away from those hospitals.
REFERENCES
AAP (American Academy of Pediatrics). 1992. AAP task force on infant positioning and SIDS: Positioning and SIDS. Pediatrics 89(6 Pt. 1):1120–1126.
AAP. 2000. Committee on Pediatric Emergency Medicine. History. [Online]. Available: http:// www.aap.org/visit/copemhistory.htm [accessed January 10, 2006].
AAP. 2001a. Care of children in the emergency department: Guidelines for preparedness. Pediatrics 107(4):777–781.
AAP. 2001b. Medicaid Reimbursement Survey, 2001. Washington, DC: AAP.
AAP. 2002. Statement for the Record. Elk Grove Village, IL: AAP.
AAP. 2003. Council of Medical Specialty Societies: Workforce Questions. Washington, DC: AAP.
ACEP (American College of Emergency Physicians). 2004. Two-Thirds of Emergency Department Directors Report On-Call Specialty Coverage Problems. [Online]. Available: http://www.acep.org/1,34081,0.html [accessed September 28, 2004].
ACS (American College of Surgeons). 2004. National Trauma Data Bank Pediatric Report 2004. Chicago, IL: American College of Surgeons.
Advocates for EMS. 2004. EMSC Program. [Online]. Available: http://www.advocatesforems.org/Library/upload/EMSC_Program_Fact_Sheet.pdf [accessed August 2, 2004].
AHRQ (Agency for Healthcare Research and Quality). 2002. Children’s Health Highlights. Rockville, MD: AHRQ.
AHRQ. 2003. National Healthcare Disparities Report. Rockville, MD: DHHS.
Alexander J, Manno M. 2003. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Annals of Emergency Medicine 41(5):617–622.
Anderson M, Megan R, Zielinski S. 2004. Decreasing emergency department visits among inner-city children with asthma. Accident and Emergency Nursing 2(11):796–797.
Arrowsmith JB, Kennedy DL, Kuritsky JN, Faich GA. 1987. National patterns of aspirin use and Reye syndrome reporting, United States, 1980 to 1985. Pediatrics 79(6):858–863.
ATS (American Trauma Society). 2006. ATS and Trauma. [Online]. Available: http://www.amtrauma.org/atsandtrauma/atsandtrauma.html [accessed March 12, 2006].
Augustine J, Kellermann A, Koplan J. 2004. America’s emergency care system and severe acute respiratory syndrome: Are we ready? Annals of Emergency Medicine 43(1):23–26.
Baker DW, Stevens CD, Brook RH. 1991. Patients who leave a public hospital emergency department without being seen by a physician. Causes and consequences. Journal of the American Medical Association 266(8):1085–1090.
Baker LC, Baker LS. 1994. Excess cost of emergency department visits for nonurgent care. Health Affairs 13(5):164–171.
Bazarian JJ, Pope C, McClung J, Cheng YT, Flesher W. 2003. Ethnic and racial disparities in emergency department care for mild traumatic brain injury. Academic Emergency Medicine 10(11):1209–1217.
Beers MH, Berkow R. 2005. The Merck Manual of Diagnosis and Therapy. Whitehouse Station, NJ: Merck & Co., Inc.
Belay ED, Bresee JS, Holman RC, Khan AS, Shahriari A, Schonberger LB. 1999. Reye’s syndrome in the United States from 1981 through 1997. New England Journal of Medicine 340(18):1377–1382.
Bindman AB, Grumbach K, Keane D, Rauch L, Luce JM. 1991. Consequences of queuing for care at a public hospital emergency department. Journal of the American Medical Association 266(8):1091–1096.
Bitnun A, Allen U, Heurter H, King SM, Opavsky MA, Ford-Jones EL, Matlow A, Kitai I, Tellier R, Richardson S, Manson D, Babyn P, Read S. 2003. Children hospitalized with severe acute respiratory syndrome-related illness in Toronto. Pediatrics 112(4):e261.
Brewster LR, Felland LE. 2004. Emergency department diversions: Hospital and community strategies alleviate the crisis. Issue Brief (Center for Studying Health System Change) (78):1–4.
Brousseau DC, Meurer JR, Isenberg ML, Kuhn EM, Gorelick MH. 2004. Association between infant continuity of care and pediatric emergency department utilization. Pediatrics 113(4):738–741.
Burt CW, McCaig LF, Valverde RH. 2006. Analysis of Ambulance Transports and Diversions among U.S. Emergency Departments. Hyattsville, MD: National Center for Health Statistics.
Callaham M. 1997. Quantifying the scanty science of prehospital emergency care. Annals of Emergency Medicine 30(6):785–790.
Camasso-Richardson K, Wilde J, Petrack E. 1997. Medically unnecessary pediatric ambulance transports: A medical taxi service? Academic Emergency Medicine 4(12):1137–1141.
CDC (Centers for Disease Control and Prevention). 2004. Ten Leading Causes of Death. [Online]. Available: http://www.cdc.gov/ncipc/osp/charts.htm [accessed January 3, 2004].
CDC. 2005. Child Passenger Safety: Fact Sheet. [Online]. Available: www.cdc.gov/ncipc/factsheets/childpas.htm [accessed October 5, 2005].
Center on Aging Society. 2004. Disease Management Programs: Improving Health While Reducing Costs? Washington, DC: Center on Aging Society.
Chamberlain J, Slonim A, Joseph J. 2004. Reducing errors and promoting safety in pediatric emergency care. Ambulatory Pediatrics 4(1):55–63.
Child Trends Databank. 2004. Teen Homicide, Suicide, and Firearm Death. Washington, DC: Child Trends Databank.
Chisholm CD, Collison EK, Nelson DR, Cordell WH. 2000. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking”? Academic Emergency Medicine 7(11):1239–1243.
Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. 2001. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics 107(3):524–529.
Clarke A, Walton WW. 1979. Effect of safety packaging on aspirin ingestion by children. Pediatrics 63(5):687–693.
CMS (Centers for Medicare and Medicaid Services). 2003. Medicaid Managed Care Enrollment as of June 30, 2003. [Online]. Available: http://www.cms.hhs.gov/medicaid/managedcare/mcsten03.pdf [accessed January 24, 2004].
CMS. 2004. FY 2004 Third Quarter—Program Enrollment Last Day of Quarter by State—To-tal SCHIP. [Online]. Available: http://www.cms.hhs.gov/schip/enrollment/2004pit3qt.pdf [accessed January 24, 2004].
Committee on Coding and Nomenclature. 2004. Application of the resource-based relative value scale system to pediatrics. Pediatrics 113(5):1437–1440.
Cooper A. 2006. Organizing the community for pediatric trauma care. In: Wesson D, Cooper A, Scherer III LRT, Stylianos S, Tuggle DW, eds. Pediatric Trauma. Pathophysiology, Diagnosis, and Treatment. New York: Taylor & Francis Group.
Cordell WH, Overhage JM, Waeckerle JF. 1998. Strategies for improving information management in emergency medicine to meet clinical, research, and administrative needs. The Information Management Work Group. Annals of Emergency Medicine 31(2):172–178.
CPEM (Center for Pediatric Emergency Medicine). 2001. The Emergency Medical Services for Children Program. [Online]. Available: http://www.cpem.org/trippals/01EMSC.PDF [accessed December 14, 2004].
Davis DH, Localio AR, Stafford PW, Helfaer MA, Durbin DR. 2005. Trends in operative management of pediatric splenic injury in a regional trauma system. Pediatrics 115(1):89–94.
Derlet RW. 2002. Overcrowding in emergency departments: Increased demand and decreased capacity. Annals of Emergency Medicine 39(4):430–432.
Derlet RW, Richards J. 2000. Overcrowding in the nation’s emergency departments: Complex causes and disturbing effects. Annals of Emergency Medicine 35(1):63–68.
Derlet RW, Richards J, Kravitz R. 2001. Frequent overcrowding in U.S. emergency departments. Academic Emergency Medicine 8(2):151–155.
Derrington SF, Cole SL, Dean TD, Nasrollahzadeh F, Shontz AM, Marcin JP. 2005. Increased Nonessential Admissions in Rural Emergency Departments and by Non-Pediatric Emergency Medicine Physicians. Presented at the Pediatric Academic Societies Meeting, May 2005, Washington, DC.
Deschamp C, Sneed RC. 1997. EMS for children with special healthcare needs. Emergency Medical Services 26(11):57–61; quiz 75.
Dey A, Bloom B. 2005. Summary Health Statistics for U.S. Children: National Health Interview Survey, 2003. Hyattsville, MD: National Center for Health Statistics.
DHHS (Department of Health and Human Services). 1980. Promoting Health Preventing Disease: Objectives for the Nation. Washington, DC: U.S. Government Printing Office.
DHHS. 1990. Healthy People 2000. Washington, DC: U.S. Government Printing Office.
DHHS. 1999. Mental Health: A Report of the Surgeon General. Rockville, MD: DHHS.
DHHS. 2000. Healthy People 2010: Understanding and Improving Health (2nd edition). Washington, DC: U.S. Government Printing Office.
DHHS. 2004. Emergency Medical Services for Children. Fiscal Year 2003 Program Highlights Report. [Online]. Available: http://www.ems-c.org/Downloads/PDF/ProgramHighlights/FY03ProgramHighlights.pdf [accessed October 2004].
DHHS, HRSA, MCHB (U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau). 1995. Emergency Medical Services for Children Five Year Plan: Emergency Medical Services for Children, 1995-2000. Washington, DC: EMS-C National Resource Center.
DHHS, HRSA, MCHB. 2000. Emergency Medical Services for Children Five Year Plan: Midcourse Review. Washington, DC: EMS-C National Resource Center.
DHHS, HRSA, MCHB. 2001. Five-Year Plan: Emergency Medical Services for Children, 2001-2005. Washington, DC: EMS-C National Resource Center.
DHHS, HRSA, MCHB. 2004. The National Survey of Children with Special Health Care Needs Chartbook 2001. Washington, DC: US Department of Health and Human Services.
Dowd MD, Tarantino C, Barnett TM, Fitzmaurice L, Knapp JF. 2005. Resident efficiency in a pediatric emergency department. Academic Emergency Medicine 12(12):1240–1244.
Eichner JM, Neff JM, Hardy DR, Klein M, Percelay JM, Sigrest T, Stucky ER, Dull S, Perkins MT, Wilson JM, Corden TE, Ostric EJ, Mucha S, Johnson BH, Ahmann E, Crocker E, DiVenere N, MacKean G, Schwab WE. 2003. Family-centered care and the pediatrician’s role. Pediatrics 112(3):691–696.
EMS-C Program (Emergency Medical Services for Children Program). 2003. EMSC Product List. Vienna, VA: Emergency Medical Services for Children Clearinghouse. [Online]. Available: http://www.ems-c.org/Downloads/PDF/Products.pdf [accessed January 2006].
Falsafi N. 2001. Pediatric psychiatric emergencies. Journal of Child and Adolescent Psychiatric Nursing 14(2):81–88.
Federiuk CS, O’Brien K, Jui J, Schmidt TA. 1993. Job satisfaction of paramedics: The effects of gender and type of agency of employment. Annals of Emergency Medicine 22(4):657–662.
Fernandes CM, Daya MR, Barry S, Palmer N. 1994. Emergency department patients who leave without seeing a physician: The Toronto hospital experience. Annals of Emergency Medicine 24(6):1092–1096.
Fernandes CMB, Price A, Christenson JM. 1997. Does reduced length of stay decrease the number of emergency department patients who leave without seeing a physician? Journal of Emergency Medicine 15(3):397–399.
Fifield GC, Magnuson C, Carr WP, Deinard AS. 1984. Pediatric emergency care in a metropolitan area. Journal of Emergency Medicine 1(6):495–507.
Fildes JJE. 2005. National Trauma Data Bank Pediatric Report. Chicago, IL: ACS.
Fleming NS, Jones HC. 1983. The impact of outpatient department and emergency room use on costs in the Texas Medicaid Program. Medical Care 21(9):892–910.
Flex Monitoring Team. 2004. A Synthesis of State Flex Program Plans 2003–2004. Minneapolis, MN: University of Minnesota, University of North Carolina at Chapel Hill, University of Southern Maine.
Foltin G, Fuchs S. 1991. Advances in pediatric emergency medical service systems. Emergency Medicine Clinics of North America 9(3):459–474.
Foltin G, Pon S, Tunik M, Fierman A, Dreyer B, Cooper A, Welborne C, Treiber M. 1998. Pediatric ambulance utilization in a large American city: A systems analysis approach. Pediatric Emergency Care 14(4):453–454.
Fong NC, Kwan YW, Hui YW, Yuen LK, Yau EK, Leung CW, Chiu MC. 2004. Adolescent twin sisters with severe acute respiratory syndrome (SARS). Pediatrics 113(2):e146–e149.
Fredrickson JM, Bauer W, Arellano D, Davidson M. 1994. Emergency nurses’ perceived knowledge and comfort levels regarding pediatric patients. Journal of Emergency Nursing 20(1):13–17.
Friedlaender E, Alessandrini E. 2004. Providing optimal emergency care for medically underserved children. Clinical Pediatric Emergency Medicine 5:109–119.
Frush K, Hohenhaus S. 2004. Enhancing Pediatric Patient Safety Grant. Durham, NC: Duke University Health System.
Gadomski AM, Perkis V, Horton L, Cross S, Stanton B. 1995. Diverting managed care Medicaid patients from pediatric emergency department use. Pediatrics 95(2):170–178.
GAO (General Accountability Office). 2003. Hospital Emergency Departments: Crowded Conditions Vary among Hospitals and Communities. Report to the Ranking Minority Member, Committee on Finance, U.S. Senate. Washington, DC: GAO.
Gausche M, Seidel JS, Henderson DP, Ness B, Ward PM, Wayland BW. 1989. Violent death in the pediatric age group: Rural and urban differences. Pediatric Emergency Care 5(1):64–67.
Gausche M, Rutherford M, Lewis RL. 1995. Emergency department quality assurance/improvement practices for the pediatric patient. Annals of Emergency Medicine 25(6):804–808.
Gausche M, Tadeo R, Zane M, Lewis R. 1998. Out-of-hospital intravenous access: Unnecessary procedures and excessive cost. Academic Emergency Medicine 5(9):878–882.
Gausche M, Lewis RJ, Stratton SJ, Haynes BE, Gunter CS, Goodrich SM, Poore PD, McCollough MD, Henderson DP, Pratt FD, Seidel JS. 2000. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. Journal of the American Medical Association 283(6):783–790.
Gausche-Hill M. 2000. Pediatric continuing education for out-of-hospital providers: Is it time to mandate review of pediatric knowledge and skills? Annals of Emergency Medicine 36(1):72–74.
Gausche-Hill M, Lewis R, Gunter C, Henderson D, Haynes B, Stratton S. 2000. Design and implementation of a controlled trial of pediatric endotracheal intubation in the out-of-hospital setting. Annals of Emergency Medicine 36(4):356–365.
Gausche-Hill M, Lewis R, Schmitz C. 2004. Survey of US Emergency Departments for Pediatric Preparedness––Implementation and Evaluation of Care of Children in the Emergency Department: Guidelines for Preparedness. Emergency Medical Services for Children Partnership for Information and Communication Grant #IU93 MC 00184. Unpublished results.
Glaeser P, Linzer J, Tunik M, Henderson D, Ball J. 2000. Survey of nationally registered emergency medical services providers: Pediatric education. Annals of Emergency Medicine 36(1):33–38.
Glaser NS, Kuppermann N, Yee CK, Schwartz DL, Styne DM. 1997. Variation in the management of pediatric diabetic ketoacidosis by specialty training. Archives of Pediatrics & Adolescent Medicine 151(11):1125–1132.
Glaser NS, Barnett P, McCaslin I, Nelson D, Trainor J, Louie J, Kaufman F, Quayle K, Roback M, Malley R, Kuppermann N, Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. 2001. Risk factors for cerebral edema in children with diabetic ketoacidosis. New England Journal of Medicine 344:264–269.
Goldberg R, Kuhn G, Andrew L, Thomas H. 2002. Coping with medical mistakes and errors in judgment. Annals of Emergency Medicine 39(3):287–292.
Goldmann D, Kaushal R. 2002. Time to tackle the tough issues in patient safety. Pediatrics 110(4):823–826.
Graff KJ, Kennedy RM, Jaffe DM. 1996. Conscious sedation for pediatric orthopaedic emergencies. Pediatric Emergency Care 12(1):31–35.
Graham CJ, Stuemky J, Lera TA. 1993. Emergency medical services preparedness for pediatric emergencies. Pediatric Emergency Care 9(6):329–331.
Green L, Melnick GA, Nawathe A. 2005. On-Call Physicians at California Emergency Departments: Problems and Potential Solutions. Oakland, CA: California Healthcare Foundation.
Guidelines for pediatric equipment and supplies for basic and advanced life support ambulances. 1996. Committee on Ambulance Equipment and Supplies, National Emergency Medical Services for Children Resource Alliance. Annals of Emergency Medicine 28(6):699–701.
Haddix AC, Mallonee S, Waxweiler R, Douglas MR. 2001. Cost effectiveness analysis of a smoke alarm giveaway program in Oklahoma City, Oklahoma. Injury Prevention: Journal of the International Society for Child and Adolescent Injury Prevention 7(4):276–281.
Hamilton S, Adler M, Walker A. 2003. Pediatric calls: Lessons learned from pediatric research. JEMS: Journal of Emergency Medical Services 28(7):56–63.
Hampers LC, Faries SG. 2002. Practice variation in the emergency management of croup. Pediatrics 109(3):505–508.
Hampers LC, Trainor JL, Listernick R, Eddy JJ, Thompson DA, Sloan EP, Chrisler OP, Gatewood LM, McNulty B, Krug SE. 2000. Setting-based practice variation in the management of simple febrile seizure. Academic Emergency Medicine 7(1):21–27.
Harborview Injury Prevention and Research Center. 2006. Child-Resistant Packaging and the Poison Prevention Packaging Act. [Online]. Available: http://depts.washington.edu/hiprc/practices/topic/poisoning/packaging.html [accessed February 23, 2006].
Harris BH. 1987. Progress in Pediatric Trauma. Presentation at the meeting of the Proceedings of The National Conference on Pediatric Trauma. Boston, MA: The Kiwanis Pediatric Trauma Institute, New England Medical Center.
Hostetler MA, Auinger P, Szilagyi PG. 2002. Parenteral analgesic and sedative use among ED patients in the United States: Combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. American Journal of Emergency Medicine 20(3):139–143.
Hoyle J, White L. 2003. Treatment of pediatric and adolescent mental health emergencies in the United States: Current practices, models, barriers, and potential solutions. Prehospital Emergency Care 7(1):66–73.
HRSA (Health Resources and Services Administration). 1994. Emergency Medical Services for Children, Annual Report, FY 1993. Rockville, MD: HRSA.
HRSA. 2002. HHS Awards More Than $276 Million to Children’s Teaching Hospitals to Ensure Quality Health Care for America’s Children (Press Release). Rockville, MD: DHHS.
IOM (Institute of Medicine). 1993. Emergency Medical Services for Children. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2002. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press.
IOM. 2003. A Shared Destiny: Community Effects of Uninsurance. Washington, DC: The National Academies Press.
IOM. 2005. Quality Through Collaboration: The Future of Rural Health Care. Washington, DC: The National Academies Press.
Irvin CB, Fox JM, Smude B. 2003. Are there disparities in emergency care for uninsured, Medicaid, and privately insured patients? Academic Emergency Medicine 10(11):1271–1277.
Isaacman DJ, Kaminer K, Veligeti H, Jones M, Davis P, Mason JD. 2001. Comparative practice patterns of emergency medicine physicians and pediatric emergency medicine physicians managing fever in young children. Pediatrics 108(2):354–358.
James CA, Bourgeois FT, Shannon MW. 2005. Association of race/ethnicity with emergency department wait times. Pediatrics 115(3):e310–e315.
Johnson WG, Rimsza ME. 2004. The effects of access to pediatric care and insurance coverage on emergency department utilization. Pediatrics 113(3 Pt. 1):483–487.
Joyce S, Brown D, Nelson E. 1996. Epidemiology of pediatric EMS practice: A multistate analysis. Prehospital Disaster Medicine 11(3):180–187.
Kaiser Family Foundation. 2003. Medicaid Benefits. [Online]. Available: http://www.kff.org/medicaid/benefits/index.cfm [accessed August 20, 2004].
Kaiser Family Foundation. 2004a. The Medicaid Program at a Glance. Washington, DC: The Henry J. Kaiser Family Foundation.
Kaiser Family Foundation. 2004b. Health Coverage for Low-Income Children. Washington, DC: The Henry J. Kaiser Family Foundation.
Kaplan SL, Mason EO Jr, Wald ER, Schutze GE, Bradley JS, Tan TQ, Hoffman JA, Givner LB, Yogev R, Barson WJ. 2004. Decrease of invasive pneumococcal infections in children among 8 children’s hospitals in the United States after the introduction of the 7–valent pneumococcal conjugate vaccine. Pediatrics 113(3 Pt. 1):443–449.
Kastner TA. 2004. Managed care and children with special health care needs. Pediatrics 114(6):1693–1698.
Katz DA, Williams GC, Brown RL, Aufderheide TP, Bogner M, Rahko PS, Selker HP. 2005. Emergency physicians’ fear of malpractice in evaluating patients with possible acute cardiac ischemia. Annals of Emergency Medicine 46(6):525–533.
Kellermann AL, Haley LH. 2003. Hospital emergency departments: Where the doctor is always “in.” Medical Care 41(2):195–197.
Khan ANGA, Carmel M, Rubin DH, Suecoff S. 2002. Pediatric psychiatric illness in the emergency department: An ignored health care issue. Academic Emergency Medicine 9(5):390.
King WK, Kiesel EL, Simon HK. 2004. Child abuse fatalities: Are we missing opportunities for intervention? Academic Emergency Medicine 11(5):594-a.
Kost S, Arruda J. 1999. Appropriateness of ambulance transportation to a suburban pediatric emergency department. Prehospital Emergency Care 3(3):187–190.
Kozer E, Scolnik D, Macpherson A, Keays T, Shi K, Luk T, Koren G. 2002. Variables associated with medication errors in pediatric emergency medicine. Pediatrics 110(4):737.
Krauss B, Zurakowski D. 1998. Sedation patterns in pediatric and general community hospital emergency departments. Pediatric Emergency Care 14(2):99–103.
Krug S, Kuppermann N. 2005. Twenty years of emergency medical services for children: A cause for celebration and a call for action. Academic Emergency Medicine 12(4):345–347.
Ku L, Nimalendran S. 2004. Improving Children’s Health: A Chartbook about the Roles of Medicaid and SCHIP. Washington, DC: Center on Budget and Policy Priorities.
Kunen S, Hume P, Perret JN, Mandry CV, Patterson TR. 2003. Underdiagnosis of child abuse in emergency departments. Academic Emergency Medicine 10(5):546-a.
Kusserow RP. 1992. Use of Emergency Rooms by Medicaid Recipients. Washington, DC: DHHS.
Lawthers AG, Localio AR, Laird NM, Lipsitz S, Hebert L, Brennan TA. 1992. Physicians’ perceptions of the risk of being sued. Journal of Health Politics, Policy and Law 17(3):463–482.
Leung CW, Kwan YW, Ko PW, Chiu SS, Loung PY, Fong NC, Lee LP, Hui YW, Law HK, Wong WH, Chan KH, Peiris JS, Lim WW, Lau YL, Chiu MC. 2004. Severe acute respiratory syndrome among children. Pediatrics 113(6):e535–e543.
Liu T, Sayre MR, Carleton SC. 1999. Emergency medical care: Types, trends, and factors related to nonurgent visits. Academic Emergency Medicine 6(11):1147–1152.
Lowe RA, Chhaya S, Nasci K, Gavin LJ, Shaw K, Zwanger ML, Zeccardi JA, Dalsey WC, Abbuhl SB, Feldman H, Berlin JA. 2001. Effect of ethnicity on denial of authorization for emergency department care by managed care gatekeepers. Academic Emergency Medicine 8(3):259–266.
Lowe RA, Localio AR, Schwarz DF, Williams S, Tuton LW, Maroney S, Nicklin D, Goldfarb N, Vojta DD, Feldman HI. 2005. Association between primary care practice characteristics and emergency department use in a Medicaid managed care organization. Medical Care 43(8):792–800.
Loyacono TR. 2001. Family-centered prehospital care. Emergency Medical Services 30(6):83.
Luo X, Liu G, Frush K, Hey LA. 2003. Children’s health insurance status and emergency department utilization in the United States. Pediatrics 112(2):314.
Macias CG. 2005. Pediatric emergency medicine fellowships adopt a new application process. Pediatric Emergency Care 21(5):355–356.
MacLean S, Guzzetta C, White C, Fontaine D, Eichhorn D, Meyers T, Desy P. 2003. Family presence during cardiopulmonary resuscitation and invasive procedures: Practices of critical care and emergency nurses. Journal of Emergency Nursing 29(3):208–221.
Macpherson AK, MacArthur C. 2002. Bicycle helmet legislation: Evidence for effectiveness. Pediatric Research 52(4):472.
Mansbach JM, Wharff E, Austin SB, Ginnis K, Woods ER. 2003. Which psychiatric patients board on the medical service? Pediatrics 111(6):e693–e698.
Mansbach JM, Emond JA, Camargo CA Jr. 2005. Bronchiolitis in US emergency departments 1992 to 2000: Epidemiology and practice variation. Pediatric Emergency Care 21(4):242–247.
Marcin JP, Seifert L, Cho M, Cole SL, Romano PS. 2005. Medication Errors among Acutely Ill and Injured Children Presenting to Rural Emergency Departments. Presentation at the meeting of the Pediatric Academic Societies Meeting, Washington, DC.
Markenson D, Foltin G, Tunik M, Cooper A, Matza-Haughton H, Olson L, Treiber M. 2002. Knowledge and attitude assessment and education of prehospital personnel in child abuse and neglect: Report of a national blue ribbon panel. Prehospital Emergency Care 6(3):261–272.
MayoClinic.com. 2005. Bronchitis. [Online]. Available: http://www.MayoClinic.com [accessed April 20, 2005].
McCaig LF, Burt CW. 2005. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. Hyattsville, MD: National Center for Health Statistics.
McCaig LF, Ly N. 2002. National Hospital Ambulatory Medical Care Survey: 2000 Emergency Department Summary. Advance Data from Vital and Health Statistics; No. 326. Hyattsville, MD: National Center Health Statistics.
MCHB (Maternal and Child Health Bureau). 2004a. Emergency Medical Services for Children. Five Year Plan 2001–2005: Midcourse Review. Washington, DC: EMS-C National Resource Center.
MCHB. 2004b. Tube Tools: Rapid Sequence Intubation and Related Pediatric Airway Techniques, Version 1.0. Rockville, MD: DHHS.
MCHB. 2005a. Emergency Medical Services for Children. [Online]. Available: http://www.mchb.hrsa.gov/programs/emsc/ [accessed October 4, 2005].
MCHB. 2005b. EMSC Program. Rockville, MD: HRSA.
Melese-d’Hospital IA, Olson LM, Cook L, Skokan EG, Dean JM. 2002. Children presenting to emergency departments with mental health problems. Academic Emergency Medicine 9(5):528-a.
Middleton KR. 2005. National Center for Health Statistics Survey, “Emergency Pediatric Services and Equipment Supplement” to the National Hospital Ambulatory Medical Care Survey. Presentation at the meeting of the 2005 EMSC Annual Grantee Meeting, Washington, DC.
Middleton KR, Burt CW. 2006. Availability of Pediatric Services and Equipment in Emergency Departments: United States, 2002–03. Hyattsville, MD: National Center for Health Statistics.
Mittelstaedt EA, Simon SR. 2004. Developing a child safety seat program. Military Medicine 169(1):30–33.
Moorhead JC, Gallery ME, Hirshkorn C, Barnaby DP, Barsan WG, Conrad LC, Dalsey WC, Fried M, Herman SH, Hogan P, Mannle TE, Packard DC, Perina DG, Pollack CV Jr, Rapp MT, Rorrie CC Jr, Schafermeyer RW. 2002. A study of the workforce in emergency medicine: 1999. Annals of Emergency Medicine 40(1):3–15.
Moreland JE, Sanddal ND, Sanddal TL, Pickert CB. 1998. Pediatric equipment in ambulances. Pediatric Emergency Care 14(1):84.
Murdock TC, Knapp JF, Dowd MD, Campbell JP. 1999. Bridging the emergency medical services for children information gap. Archives of Pediatrics & Adolescent Medicine 153(3):281–285.
Murphy AW, Bury G, Plunkett PK, Gibney D, Smith M, Mullan E, Johnson Z. 1996. Randomised controlled trial of general practitioner versus usual medical care in an urban accident and emergency department: Process, outcome, and comparative cost. British Medical Journal 312(7039):1135–1142.
Murray JA, Demetriades D, Berne TV, Stratton SJ, Cryer HG, Bongard F, Fleming A. 2000. Prehospital intubation in patients with severe head injury. Journal of Trauma 49(6):1065–1070.
Nakayama DK, Copes WS, Sacco W. 1992. Differences in trauma care among pediatric and nonpediatric trauma centers. Journal of Pediatric Surgery 27(4):427–431.
NAS, NRC (National Academy of Sciences, National Research Council). 1966. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: National Academy of Sciences.
NASEMSD (National Association of State EMS Directors). 2004. Pediatric Disaster and Terrorism Preparedness. Falls Church, VA: NASEMSD.
National Association of Children’s Hospitals and Related Institutions. 2006. Education. [Online]. Available: http://www.childrenshospitals.net/Template.cfm?Section=Home&C ONTENTID=3703&TEMPLATE=/ContentManagement/ContentDisplay.cfm [accessed January 25, 2006].
National Cancer Institute. 2005. Digital vs. Film Mammography in the Digital Mammographic Imaging Screening Trial (DMIST). [Online]. Available: http://www.cancer.gov/newscenter/pressreleases/DMISTQandA/ [accessed January 10, 2006].
National Center for Complementary and Alternative Medicine. 2002. NIH Launches Large Clinical Trial on EDTA Chelation Therapy for Coronary Artery Disease. [Online]. Available: http://nccam.nih.gov/news/2002/chelation/pressrelease.htm [accessed January 10, 2006].
National Center for Health Statistics. 2004. Deaths: Final data for 2002. National Vital Statistics Reports 53(5). Hyattsville, MD: National Center for Health Statistics.
National Center for Injury Prevention and Control. 2001. Injury Fact Book 2001–2002. Atlanta, GA: CDC.
National Clearinghouse on Child Abuse and Neglect Information. 2004. Child Abuse and Neglect Fatalities: Statistics and Interventions. Washington, DC: DHHS.
National Emergency Number Association. 2004. 9-1-1 Fast Facts. Arlington, VA: National Emergency Number Association.
National Institute of Neurological Disorders and Stroke. 2006. NINDS Reye’s Syndrome Information Page. [Online]. Available: http://www.ninds.nih.gov/disorders/reyes_syndrome/reyes_syndrome.htm [accessed February 24, 2006].
National Institute on Deafness and Other Communication Disorders. 2002. Ear Infections: Facts for Parents About Otitis Media. [Online]. Available: http://www.nidcd.nih.gov/health/hearing/otitismedia.asp [accessed December 7, 2006].
National Safe Kids Campaign. 2004. Trends in Unintentional Injury Fact Sheet. Washington, DC: National Safe Kids Campaign.
Neely KW, Norton RL, Young GP. 1994. The effect of hospital resource unavailability and ambulance diversions on the EMS system. Prehospital Disaster Medicine 9(3):172–176; discussion 177.
Newacheck PW. 1992. Characteristics of children with high and low usage of physician services. Medical Care 30(1):30–42.
Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. 2000. The unmet health needs of America’s children. Pediatrics 105(4 Pt. 2):989–997.
O’Malley AS, Gerland AM, Pham HH, Berenson RA. 2005. Rising Pressure: Hospital Emergency Departments: Barometers of the Health Care System. Washington, DC: The Center for Studying Health System Change.
Office of Technology Assessment. 1989. Rural Emergency Medical Services––Special Report. Washington, DC: Office of Technology Assessment.
Office of Technology Assessment. 1994. Defensive Medicine and Medical Malpractice. Washington, DC: U.S. Government Printing Office.
Oster A, Bindman AB. 2003. Emergency department visits for ambulatory care sensitive conditions: Insights into preventable hospitalizations. Medical Care 41(2):198–207.
Pantridge JF, Geddes JS. 1967. A mobile intensive-care unit in the management of myocardial infarction. Lancet 2(7510):271–273.
Pearson SD, Goldman L, Orav EJ, Guadagnoli E, Garcia TB, Johnson PA, Lee TH. 1995. Triage decisions for emergency department patients with chest pain: Do physicians’ risk attitudes make the difference? Journal of General Internal Medicine 10(10):557–564.
PECARN (Pediatric Emergency Care Applied Research Network). 2004. About PECARN. [Online]. Available: http://www.pecarn.org/about_pecarn.htm [accessed August 2, 2004].
Peddle N, Wang C-T. 2002. Current Trends in Child Abuse Prevention, Reporting, and Fatalities. Chicago, IL: Prevent Child Abuse America.
Pena ME, Snyder BL. 1995. Pediatric emergency medicine. The history of a growing discipline. Emergency Medicine Clinics of North America 13(2):235–253.
Perez K. 1998. Emergency Medical Services for Children. Washington, DC: National Council of State Legislatures.
Petrack EM, Christopher NC, Kriwinsky J. 1997. Pain management in the emergency department: Patterns of analgesic utilization. Pediatrics 99(5):711.
Piacentini J, Rotheram-Borus MJ, Gillis JR, Graae F, Trautman P, Cantwell C, Garcia-Leeds C, Shaffer D. 1995. Demographic predictors of treatment attendance among adolescent suicide attempters. Journal of Consulting & Clinical Psychology 63(3):469–473.
Polivka BJ, Nickel JT, Salsberry PJ, Kuthy R, Shapiro N, Slack C. 2000. Hospital and emergency department use by young low-income children. Nursing Research 49(5):253–261.
Porter SC, Fein JA, Ginsburg KR. 1997. Depression screening in adolescents with somatic complaints presenting to the emergency department. Annals of Emergency Medicine 29(1):141–145.
Probst BD, Lyons E, Leonard D, Esposito TJ. 2005. Factors affecting emergency department assessment and management of pain in children. Pediatric Emergency Care 21(5):298–305.
Quinn JV, Polevoi SK, Kramer NR, Callaham ML. 2003. Factors associated with patients who leave without being seen. Academic Emergency Medicine 10(5):523-b, 524.
Ramenofsky ML. 2006. Organizing the hospital for pediatric trauma care. In: Wesson D, Cooper A, Scherer III LRT, Stylianos S, Tuggle DW, eds. Pediatric Trauma. Pathophysiology, Diagnosis, and Treatment. New York: Taylor & Francis Group.
Ramenofsky ML, Luterman A, Quindlen E, Riddick L, Curreri PW. 1984. Maximum survival in pediatric trauma: The ideal system. The Journal of Trauma 24(9):818–823.
Richardson LD, Babcock Irvin C, Tamayo-Sarver JH. 2003. Racial and ethnic disparities in the clinical practice of emergency medicine. Academic Emergency Medicine 10(11):1184–1188.
Rivara FP, Grossman DC, Cummings P. 1997. Injury prevention. Second of two parts. New England Journal of Medicine 337(9):613–618.
Rosen P. 1995. History of Emergency Medicine. New York: Josiah Macy, Jr. Foundation. Pp. 59–79.
Rosenblatt R, Law S, Rosenbaum S. 2001. Law and the American Health Care System. New York: Foundation Press.
Rowe BH, Channan P, Bullard M, Alibha A, Saunders D. 2003. Reasons why patients leave without being seen from the emergency department. Academic Emergency Medicine 10(5):513.
Saade DN, Simon HK, Greenwald M. 2002. Abused children: Missed opportunities for recognition in the ED. Academic Emergency Medicine 9(5):524.
Sacchetti A, Sacchetti C, Carraccio C, Gerardi M. 2000. The potential for errors in children with special health care needs. Academic Emergency Medicine 7(11):1330–1333.
Sainsbury S. 1990. Emergency patients who leave without being seen. Military Medicine 155(10):460–464.
Santucci KA, Sather J, Douglas M. 2000. Psychiatry-related visits to the pediatric emergency department: A growing epidemic (abstract). Pediatric Research 47(4):117A.
Santucci KA, Sather J, Baker MD. 2003. Emergency medicine training programs’ educational requirements in the management of psychiatric emergencies: Current perspective. Pediatric Emergency Care 19(3):154–156.
Sapien RE, Fullerton L, Olson LM, Broxterman KJ, Sklar DP. 1999. Disturbing trends: The epidemiology of pediatric emergency medical services use. Academic Emergency Medicine 6(3):232–238.
Sarver JH, Cydulka RK, Baker DW. 2002. Usual source of care and nonurgent emergency department use. Academic Emergency Medicine 9(9):916–923.
Scheck A. 2006, January. Children with psychiatric disorders now younger and more common in EDs. Emergency Medicine News. P. 1.
Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL. 2003. Emergency department crowding: A point in time. Annals of Emergency Medicine 42(2):167–172.
Scribano PV, Baker MD, Ludwig S. 1997. Factors influencing termination of resuscitative efforts in children: A comparison of pediatric emergency medicine and adult emergency medicine physicians. Pediatric Emergency Care 13(5):320–324.
Scribano PV, Baker MD, Holmes J, Shaw KN. 2000. Use of out-of-hospital interventions for the pediatric patient in an urban emergency medical services system. Academic Emergency Medicine 7(7):745–750.
Seidel JS. 1986a. A needs assessment of advanced life support and emergency medical services in the pediatric patient: State of the art. Circulation 74(6 Pt. 2):IV129–IV133.
Seidel JS. 1986b. Emergency medical services and the pediatric patient: Are the needs being met? II. Training and equipping emergency medical services providers for pediatric emergencies. Pediatrics 78(5):808.
Seidel JS, Hornbein M, Yoshiyama K, Kuznets D, Finklestein JZ, St Geme JW Jr. 1984. Emergency medical services and the pediatric patient: Are the needs being met? Pediatrics 73(6):769–772.
Seidel JS, Henderson DP, Ward P, Wayland BW, Ness B. 1991. Pediatric prehospital care in urban and rural areas. Pediatrics 88(4):681.
Selbst SM, Clark M. 1990. Analgesic use in the emergency department. Annals of Emergency Medicine 19(9):1010–1013.
Selbst SM, Levine S, Mull C, Bradford K, Friedman M. 2004. Preventing medical errors in pediatric emergency medicine. Pediatric Emergency Care 20(10):702–709.
Serleth HJ, Cogbill TH, Perri C, Lambert PJ, Ross AJ III, Thompson JE. 1999. Pediatric trauma management in a rural Wisconsin trauma center. Pediatric Emergency Care 15(6):393–398.
Sharma V, Simon SD, Bakewell JM, Ellerbeck EF, Fox MH, Wallace DD. 2000. Factors influencing infant visits to emergency departments. Pediatrics 106(5):1031–1039.
Shults R. 2004. Child passenger deaths involving drinking drivers––United States, 1997–2002. Morbidity and Mortality Weekly Report 53(4):77–79.
Sills MR, Bland SD. 2002. Summary statistics for pediatric psychiatric visits to US emergency departments, 1993–1999. Pediatrics 110(4):e40.
Singh T, Wright J, Adirim T. 2003. Children with special health care needs: A template for prehospital protocol development. Prehospital Emergency Care 7(3):336–351.
Smith E, Singh T, Adirim T. 2001. Outstanding outreach: A prehospital notification system makes a difference for special needs children. JEMS: Journal of Emergency Medical Services 26(5):48–55.
Spaite D, Karriker K, Seng M, Conroy C, Battaglia N, Tibbitts M, Salik R. 2000. Training paramedics: Emergency care for children with special health care needs. Prehospital Emergency Care 4(2):178–185.
Spivey M, Schnitzer P, Slusher P, Kruse R, Jaffe D. 2005. Emergency Department Injury Visits for Infants and Children. Evaluation of Frequency as an Indicator for Child Maltreatment. Presentation at the meeting of the Pediatric Academic Societies Annual Meeting, Washington, DC.
Starko KM, Ray CG, Dominguez LB, Stromberg WL, Woodall DF. 1980. Reye’s syndrome and salicylate use. Pediatrics 66(6):859–864.
Stenklyft P. 1999, March. Pediatric emergency medicine: Past, present, and future. Jacksonville Medicine Magazine. [Online]. Available: http://www.dcmsonline.org/jax-medicine/1999journals/march99/pediatricer.htm [accessed January 31, 2007].
Stiell IG, Nesbitt LP, Osmond MH, Campbell S, Gerein R, Munkley DP, Luinstra LG, Maloney JP, Wells GA, for the OPALS Study Group. 2005. OPALS Pediatric Study: What is the impact of advanced life support on out-of-hospital cardiac arrest? Academic Emergency Medicine 12(5 Suppl. 1):17-b, 18.
Stock LM, Bradley GE, Lewis RJ, Baker DW, Sipsey J, Stevens CD. 1994. Patients who leave emergency departments without being seen by a physician: Magnitude of the problem in Los Angeles County. Annals of Emergency Medicine 23(2):294–298.
Stylianos S, Egorova N, Guice KS, Arons RR, Oldham KT. 2006. Variation in treatment of pediatric spleen injury at trauma centers versus nontrauma centers: A call for dissemination of American pediatric surgical association benchmarks and guidelines. Journal of the American College of Surgeons 202(2):247–251.
Su E, Mann NC, McCall M, Hedges JR. 1997. Use of resuscitation skills by paramedics caring for critically injured children in Oregon. Prehospital Emergency Care 1(3):123–127.
Subedar N, Rathore MH. 1995. Changing epidemiology of childhood meningitis. Journal of the Florida Medical Association 82(7):467–469.
Sullivan AM, Rivera J. 2000. Profile of a comprehensive psychiatric emergency program in a New York City municipal hospital. The Psychiatric Quarterly 71(2):123–138.
Suruda A, Vernon D, Diller E, Dean J. 2000. Usage of emergency medical services by children with special health care needs. Prehospital Emergency Care 4(2):131–135.
Svenson JE, Nypaver M, Calhoun R. 1996. Pediatric prehospital care: Epidemiology of use in a predominantly rural state. Pediatric Emergency Care 12(3):173–179.
Tennyson DH. 2003. Hospital-affiliated pediatric urgent care clinics: A necessary extension for emergency departments? Health Care Management 22(3):190–202.
Todd KH, Lee T, Hoffman JR. 1994. The effect of ethnicity on physician estimates of pain severity in patients with isolated extremity trauma. Journal of the American Medical Association 271(12):925–928.
Todd KH, Deaton C, D’Adamo A, Goe L. 2000. Ethnicity and analgesic practice. Annals of Emergency Medicine 35(1):11–16.
Traffic Safety Center. 2002. The “forgotten child” is getting some attention at last. Traffic Safety Center Online Newsletter 1(2).
Trokel M, Wadimmba A, Griffith J, Sege R. 2006. Variation in the diagnosis of child abuse in severely injured infants. Pediatrics 117(3):722–728.
Tsai AC, Tamayo-Sarver JH, Cydulka RK, Baker DW. 2003. Declining payments for emergency department care, 1996–1998. Annals of Emergency Medicine 41(3):299–308.
United Nations Children’s Fund. 2001. A League Table of Child Deaths by Injury in Rich Nations. Florence, Italy: UNICEF Innocenti Research Center.
U.S. Census Bureau. 2000. Census 2000. [Online]. Available: http://www.census.gov [accessed October 2004].
U.S. Census Bureau. 2004. Current Population Survey, 2003 and 2004 Annual Social and Economic Supplements. Washington, DC: U.S. Census Bureau.
U.S. Census Bureau. 2005. Current Population Survey, 2005 Annual Social and Economic Supplement. Washington, DC: U.S. Census Bureau.
U.S. Consumer Product Safety Commission. 1997. Hospital-Based Pediatric Emergency Resources Survey. Bethesda, MD: Division of Hazard and Injury Data Systems.
U.S. Department of State. 2006. Avian Influenza Frequently Asked Questions. [Online]. Available: http://travel.state.gov/travel/tips/health/health_2747.html [accessed April 5, 2006].
Vanlandingham BD, Powe NR, Diener-West M, Marone B, Rubin H. 2005. Patient Insurance Status and Specialist On-Call Coverage in U.S. Hospital Emergency Departments: A National Study. Presented at AcademyHealth in Boston, MA.
Wagh A, Heon D. 1999. Self assessment of emergency medicine residents’ training and confidence in evaluating pediatric physical and sexual abuse. Academic Emergency Medicine 6(5):465.
Wang C, Villar ME, Mulligan DA, Hansen T. 2005. Cost and utilization analysis of a pediatric emergency department diversion project. Pediatrics 116(5):1075–1079.
Wang HE, Yealy DM. 2005. Out-of-hospital endotracheal intubation: It’s time to stop pretending that problems don’t exist. Academic Emergency Medicine 12(12):1245.
Watson W, Litovitz T, Klein-Schwartz W, Rodgers G, Youniss J, Reid N, Rouse W, Rembert R, Borys D. 2003. 2003 Annual Report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Washington, DC: American Association of Poison Control Centers.
Weinick RM, Billings J, Thorpe JM. 2003. Ambulatory care sensitive emergency department visits: A national perspective. Academic Emergency Medicine 10(5):525-b, 526.
White-Means SI, Thornton MC. 1995. What cost savings could be realized by shifting patterns of use from hospital emergency rooms to primary care sites? American Economic Review 85(2):138–142.
Williams RM. 1996. The costs of visits to emergency departments. New England Journal of Medicine 334(10):642–646.
Willinger M. 1995. SIDS prevention. Pediatric Annals 24(7):358–364.


































































