11
Colorectal Cancer and Asbestos
NATURE OF THIS CANCER TYPE
Together, cancers of the colon and rectum (ICD-9 153-154; ICD-O-3 C18.0-C20.9; see Figure 9.1) are the third-most common cancer and cause of cancer death among men and women in the United States. The American Cancer Society (Jemal et al. 2006) has projected that 148,610 new cases (106,680 colon and 41,930 rectum) and 55,170 deaths will occur in the United States in 2006. Colon and rectum cancers together account for about 10% of all cancer deaths. The incidence of cancers of the colon and rectum combined decreased by an average of 2.2% per year from 1998 to 2002, presumably in part because of increased screening and removal of adenomatous polyps that might otherwise progress to cancer. The age-standardized death rate from colorectal cancer decreased by an average of 1.8% per year from 1984 to 2002. The decreasing mortality reflects both the decrease in incidence and improvements in treatment and survival.
The risk of colon and rectum cancer increases with age; more than 90% of cases are diagnosed in people over 50 years old. Other risk factors for colon cancer are obesity (especially in men), physical inactivity, heavy consumption of alcohol and of red or processed meat, a history of inflammatory bowel disease, and a family history of colon or rectum cancer, especially in persons under 40 years old. Tobacco-smoking is an established risk factor for ademomatous polyps, the main precursor of colon cancer. Studies suggest that treatment with nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, and estrogen alone or in sequential use with progestin hormone therapy may reduce colorectal-cancer risk. However, no
medical organizations recommend treatment with NSAIDs or postmenopausal estrogen and progestin hormone replacement to prevent cancer because of potential side effects of NSAIDs and hormones. Women who take hormone-replacement therapy may be more likely to have colorectal cancer diagnosed at a more advanced stage.
The 1- and 5-year survival rates for persons with colorectal cancer are 83% and 63%, respectively. Survival continues to decline beyond 5 years to 57% at 10 years after diagnosis. When colorectal cancers are detected at an early, localized stage, the 5-year survival rate is 90%; however, only 39% of colorectal cancers are diagnosed at this stage, mostly because of low rates of screening. After the cancer has spread regionally to involve adjacent organs or lymph nodes, the 5-year survival rate drops to 67%. The 5-year survival rate for persons with distant metastases is 10%.
EPIDEMIOLOGIC EVIDENCE CONSIDERED
Results varied from study to study (for both cohort and case-control designs) in whether they were presented as colorectal or for colon and for rectum separately. In reviewing the available data on cancers of the colon and rectum in association with exposure to asbestos, the committee conducted three preliminary meta-analyses on the information presented separately for colon, for rectum, and for colorectal cancer as already combined by the original researchers. The plots and summary tables for those runs are presented in Appendix F. For the 15 cohort populations with individual results for colon and for rectum there did not appear to be any systematic difference, and their aggregate results were similar to those for the studies that had precombined their observations into a colorectal category. The results when the case-control results were considered in this fashion were so sparse that strong contrasts could not be drawn, but no major difference was apparent.
Condensing these three datasets into a single analysis would provide a better chance of amassing adequate information to reach a conclusion, and did not seem contraindicated by the screening runs. Furthermore, the legislation driving the committee’s charge specified colorectal cancer as a single endpoint. Age and sex are the primary known risk factors for rectal cancer, while colon cancer also appears more clearly associated with family history, physical inactivity, and several other factors such as body mass index and dietary and alcohol intake (Wei et al. 2004). Less ability to detect risk factors may itself be a function of limited statistical power arising from the fact that rectal cancer comprises only about 30% of tumors of the large intestine. Because these subsites are not clearly or consistently distinguished from each other on death certificates, colon and rectum cancer are frequently combined in analyses based on mortality, as was the case of a majority of
the cohort studies in this review. Taking account of all these factors, the committee decided to group separate results for colon and rectum within individual cohort studies and to discuss all the findings as colorectal.
In only two cohort studies were separate results for colon not accompanied by separate results for rectum. Only statistics on colon cancer were available for the women reported in Karjalainen et al. (1999), and subsequent tables revealed that the three colorectal cancers among all men reported by Sanden and Jarvholm (1987) were all rectal cancers in people with more than 20 years since first exposure. Otherwise, reported expectations permitted accurate combination to derive relative risks (RRs) for colorectal cancers within all the cohort populations. The 11 case-control citations were somewhat more problematic, because when colon- or rectum-specific results were given combined RRs could not be calculated from information present in the papers; the outcomes that each actually reported are indicated in the plots below.
Cohort Studies
The cohorts that presented usable information on the risk of colorectal cancer were indicated in Table 6.1. Their histories and design properties are described in Table B.1, and the details of their results concerning cancer at this site are abstracted in Table D.5. The results of both the cohort and the case-control studies are summarized in Table 11.1, and Figures 11.1 and 11.2 are plots of RRs for overall exposure and for exposure-response gradients from the cohort studies reviewed. Colorectal cancer occurred with far greater frequency than either esophageal or stomach cancer in the cohorts studied, and this enabled more statistically precise risk estimation. Thirty-two citations on cohort studies presented results on the association between asbestos exposure and colorectal cancer for a total of 41 distinct subpopulations.
The cohort studies were limited in that they were largely restricted to mortality, which may not give a complete account of occurrence of colorectal cancer. Also, data on known risks (such as family history of colorectal cancer and/or diet) were not available in any of the cohort studies; because such non-occupational risk factors are not likely to have been associated with asbestos exposure, however, they probably do not represent important confounders.
The Finnish women with asbestos-related diseases (Karjalainen et al. 1999), for whom only colon cancer was reported, had the highest RRs. The largest excesses of colorectal cancer were observed among the earliest North American insulation workers (Selikoff et al. 1979) and British male insulation workers (Berry et al. 2000). In contrast, numerous reports were consistent with no association and several were consistent with a negative asso-
TABLE 11.1 Summary of Epidemiologic Findings Regarding Cancer of the Colon or Rectum
|
Study Type |
Figure |
Comparison |
Study Populations Included |
No. Study Populations |
Summary RR (95% CI) |
Between-Study SD |
|
Cohort |
Any vs none |
All |
41 |
1.15 (1.01-1.31) |
|
|
|
|
High vs nonea |
Lower boundb |
13 |
1.24 (0.91-1.69) |
— |
|
|
|
|
|
Upper boundb |
13 |
1.38 (1.14-1.67) |
— |
|
Case- control |
Any vs none |
All |
13 |
1.16 (0.90-1.49) |
0.32 |
|
|
|
Any vs none |
EAM = 1 |
8 |
0.98 (0.75-1.29) |
.29 |
|
|
|
|
|
EAM = 2 |
5 |
2.00 (1.28-3.14) |
.00 |
|
|
High vs nonea |
EAM = 1 Lower boundb |
7 |
1.02 (0.57-1.82) |
.51 |
|
|
|
|
|
EAM = 1 Upper boundb |
7 |
1.14 (0.70-1.89) |
.45 |
|
NOTE: CI = Confidence interval; EAM = exposure-assessment method; high quality, EAM = 1; lower quality, EAM = 2; RR = relative risk; SD = standard deviation. aUsed studies that reported dose-response relationship (RR on an exposure gradient). bFor studies that reported dose-response relationship on multiple gradient metrics, the smallest “high vs none” RR was used to compute the lower bound, and the largest “high vs none” RR was used to compute the upper bound. |
||||||
ciation. Overall, the cohort studies (Figure 11.2) showed a small and marginally significant association between asbestos exposure and colorectal cancer (RR = 1.15, 95% CI 1.02-1.31).
The summary estimate derived by aggregating the highest of the reported extreme-exposure RR was 1.38 (95% CI 1.14-1.67), whereas the estimate of association from combining the lowest of the reported RR for the extreme category of an exposure gradient was 1.24 (95% CI 0.91-1.67) (Figure 11.2). Although those summary risk estimates for extreme exposures are greater than the summary for any exposure (1.15 from Figure 11.1), the difference is small.
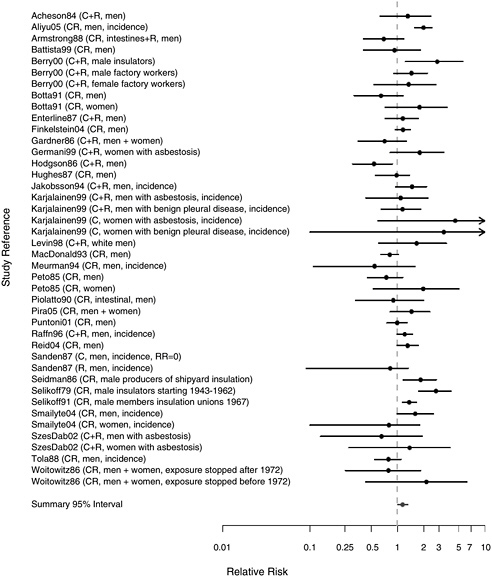
FIGURE 11.1 Cohort studies: RR of colorectal cancer in people with “any” exposure to asbestos compared with people who report none.
Case-Control Studies
The case-control studies retained for thorough evaluation after exclusion of studies that did not assess exposure to asbestos or did not meet other exclusion criteria are listed in Table 6.5 according to quality of their exposure assessment. The details of the design aspects of those studies are presented in Table C.1 and their detailed results are abstracted in Table E.5.
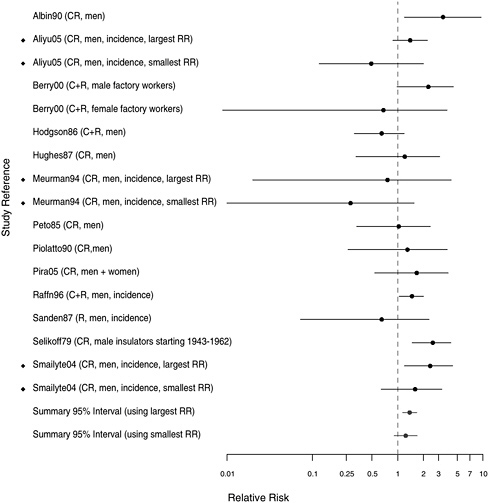
FIGURE 11.2 Cohort studies: RRs of colorectal cancer among people in most extreme exposure category compared to those with none (◆ = more than one exposure gradient reported in citation, so the plot contains both highest and lowest estimates of risk for most extreme category over all gradients).
Of the 11 citations, one (Dumas et al. 2000) reported only on rectal cancer, and five investigated only colon cancer (Fredriksson et al. 1989, Garabrant et al. 1992, Goldberg et al. 2001, Hardell 1981, Vineis et al. 1993). Separate results for colon and rectal cancers could not be readily merged into a colorectal grouping as was done for the cohorts, but the results have been considered together in this review. The findings of all 11 studies are summarized in Table 11.1 and in the plots presented in Figures 11.3-11.5, where the citation labels indicate whether the RR pertains to colon (C), rectum (R), or both (CR). The committee did not seek adjustment for confounders
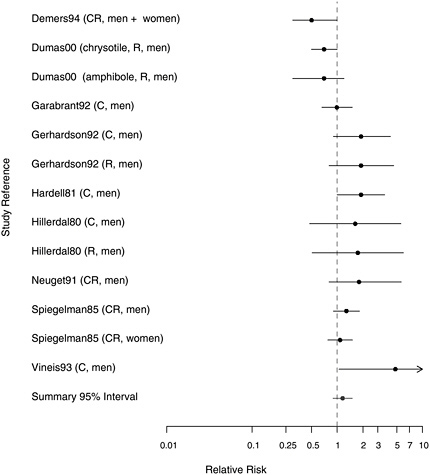
FIGURE 11.3 Case-control studies: RR of colorectal cancer in people with “any” exposure to asbestos compared with people with none.
other than sex and age for this cancer type, so a plot stratified on adjustment was not generated.
Thirteen results for any exposure were reviewed; eight point estimates exceeded 1.0, two were almost exactly 1.0, and three point estimates were less than 1.0 (Figure 11.3). When they were combined, the average estimate of association was 1.16 (95% CI 0.90-1.49).
We next considered separately high-quality and lower-quality studies (Figure 11.4). In the colorectal case-control studies with higher-quality assessment of asbestos exposure, the summary estimate of association was essentially null (95% CI 0.75-1.29); in the lower-quality studies, the summary estimate of association was significantly positive (RR = 2.00, 95% CI 1.28-3.14). That pattern suggests that lower-quality studies—those with
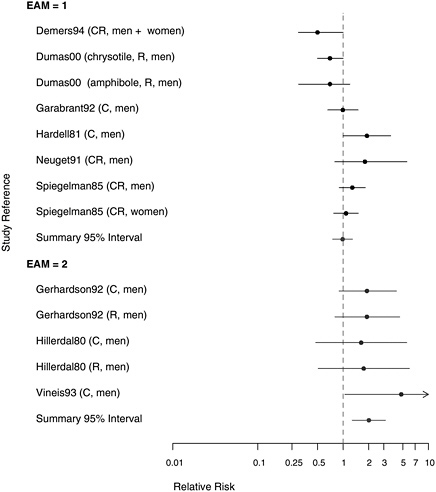
FIGURE 11.4 Case-control studies: RR of colorectal cancer in people with “any” exposure to asbestos compared with people with none, stratified on quality of exposure assessment (top, EAM = 1: higher-quality exposure assessment; bottom, EAM = 2: lower-quality exposure assessment).
less rigorous classification of exposure and typically without adjustment for confounding—were more likely to show associations between asbestos exposure and colorectal cancer.
The case-control studies evaluating gradients of exposure (Figure 11.5) did not find stronger associations between the highest exposure and colorectal cancer (RR = 1.02, 95% CI 0.57-1.82 for lowest estimates; and RR = 1.14, 95% CI 0.70-1.89 for highest estimates). That is, among groups with colorectal cancer those with high exposure did not, in aggregate, have a greater risk of cancer than those with simply any exposure.

FIGURE 11.5 Case-control studies: RRs of colorectal cancer among people in most extreme exposure category compared to those with none (◆ = more than one exposure gradient reported in citation, so the plot contains both highest and lowest estimates of risk for most extreme category over all gradients).
EVIDENCE INTEGRATION AND CONCLUSION
Evidence Considered
Thirty-two citations containing relevant information on 41 occupational cohort populations and 11 case-control studies of colorectal cancer contributed epidemiologic data. Findings related to the response to asbestos by tissues in the colon and rectum were evaluated from several well conducted chronic rodent studies, four with inhalation exposure and six with dietary administration.
Consistency
The occupational-cohort studies suggested fairly consistently, although not uniformly, that the risk of colorectal cancer was higher in exposed people than in the general population. In contrast, the case-control studies lacked consistency: estimated effects of asbestos exposure range from apparently protective to seemingly harmful, whereas the one study with the most detailed asbestos-exposure assessment and analysis (Garabrant et al. 1992) had essentially null findings.
Strength of Associations
For the case-control studies, the summary estimate of association was close to null and not statistically significant. Moreover, evidence of a dose-response relationship in the case-control studies was lacking. The overall observed risk estimate from cohort studies was modestly above 1.0 and statistically significant with some—albeit modest—evidence of a dose-response relationship.
Coherence
Colorectal tumors are most commonly adenocarcinomas that arise in polyps. Multiple risk factors are associated with colon cancer, including age, familial predisposition, obesity, physical inactivity, and inflammatory bowel disease. The potential role of asbestos fibers as a cofactor has not been investigated in epidemiologic or experimental studies.
Asbestos bodies and asbestos fibers have been identified in the colon. Ehrlich et al. (1991) recovered both from the biopsy samples from a third of a small group of asbestos workers with colon cancer, but none from the colons of patients without a history of asbestos exposure. Auerbach et al. (1980) recovered asbestos bodies from colon tissue, as did Kobayashi et al. (1987), who reported recovering them from both the large and small intestine. In patients with inflammatory bowel disease and colon tumors, it is uncertain whether fibers accumulate secondarily at sites of mucosal injury or ulceration associated with inflammation or in an expanding tumor. As is the case for finding asbestos bodies at other sites, contamination during collection or processing of tissue samples is a possibility, as discussed in Chapter 4.
One animal study (Amacher et al. 1974) showed that even a single dose of chrysotile fed to rats, if large enough, consistently caused a transient increase in DNA synthesis in the colon weeks later suggesting gastrointestinal absorption had occurred at some unspecified site, but overall animal models have failed to produce colon or colorectal cancer. Thorough exami-
nation of rats and Syrian hamsters exposed to asbestos by inhalation at levels sufficient to cause mesothelioma in both species and lung cancer in rats did not find colorectal malignancies (Hesterberg et al. 1993, 1994; McConnell 2005; McConnell et al. 1994a,b, 1999). One (HHS 1985) of six lifetime, high-dose asbestos feeding studies in rodents (HHS 1983, 1985, 1988, 1990a,b,c) did, however, produced benign adenomatous colon polyps in rats after chrysotile exposure. Benign adematous colon polyps are a precursor of the most common type of colon cancer in humans. No polyps were produced by chronic asbestos feeding in hamsters.
Conclusion
The committee judged that some aspects of the evidence were supportive of a causal association: a positive but small aggregate association with a narrow confidence band arising from the many cohort findings possible biologic plausibility suggested by the presence of asbestos bodies and fibers in the colons of asbestos workers and the experimental induction of colon polyps, albeit benign, in rats. The overall lack of consistency or of the suggestion of an association among the case-control studies (even those of the highest quality) and the absence of convincing dose-response relationships in either type of study design, however, weigh against causality.
Thus, the committee determined that the evidence is suggestive but not sufficient to infer a causal relationship between asbestos exposure and colorectal cancer.
REFERENCES
Acheson ED, Gardner MJ, Winter PD, Bennett C. 1984. Cancer in a factory using amosite asbestos. International Journal of Epidemiology 13(1): 3-10.
Albin M, Jakobsson K, Attewell R, Johansson L, Welinder H. 1990. Mortality and cancer morbidity in cohorts of asbestos cement workers and referents. British Journal of Industrial Medicine 47(9): 602-610.
Aliyu OA, Cullen MR, Barnett MJ, Balmes JR, Cartmel B, Redlich CA, Brodkin CA, Barnhart S, Rosenstock L, Israel L, Goodman GE, Thornquist MD, Omenn GS. 2005. Evidence for excess colorectal cancer incidence among asbestos-exposed men in the Beta-Carotene and Retinol Efficacy Trial. American Journal of Epidemiology 162(9): 868-878.
Amacher DE, Alarif A, Epstein SS. 1974. Effects of ingested chrysotile on DNA synthesis in the gastrointestinal tract and liver of the rat. Environmental Health Perspectives 9: 319-324.
Armstrong BK, de Klerk NH, Musk AW, Hobbs MS. 1988. Mortality in miners and millers of crocidolite in Western Australia. British Journal of Industrial Medicine 45(1): 5-13.
Auerbach O, Conston AS, Garfinkel L, Parks VR, Kaslow HD, Hammond EC. 1980. Presence of asbestos bodies in organs other than the lung. Chest 77(2): 133-137.
Battista G, Belli S, Comba P, Fiumalbi C, Grignoli M, Loi F, Orsi D, Paredes I. 1999. Mortality due to asbestos-related causes among railway carriage construction and repair workers. Occupation Medicine (London) 49(8): 536-539.
Berry G, Newhouse ML, Wagner JC. 2000. Mortality from all cancers of asbestos factory workers in east London 1933-80. Occupational and Environmental Medicine 57(11): 782-785.
Botta M, Magnani C, Terracini B, Bertolone GP, Castagneto B, Cocito V, DeGiovanni D, Paglieri P. 1991. Mortality from respiratory and digestive cancers among asbestos cement workers in Italy. Cancer Detection and Prevention 15(6): 445-447.
Demers RY, Burns PB, Swanson GM. 1994. Construction occupations, asbestos exposure, and cancer of the colon and rectum. Journal of Occupational Medicine 36(9): 1027-1031.
Dumas S, Parent ME, Siemiatycki J, Brisson J. 2000. Rectal cancer and occupational risk factors: A hypothesis-generating, exposure-based case-control study. International Journal of Cancer 87(6): 874-879.
Ehrlich A, Gordon RE, Dikman SH. 1991. Carcinoma of the colon in asbestos-exposed workers: Analysis of asbestos content in colon tissue. American Journal of Industrial Medicine 19(5): 629-636.
Enterline PE, Hartley J, Henderson V. 1987. Asbestos and cancer: A cohort followed up to death. British Journal of Industrial Medicine 44(6): 396-401.
Finkelstein MM, Verma DK. 2004. A cohort study of mortality among Ontario pipe trades workers. Occupational and Environmental Medicine 61(9): 736-742.
Fredriksson M, Bengtsson NO, Hardell L, Axelson O. 1989. Colon cancer, physical activity, and occupational exposures: A case-control study. Cancer 63(9): 1838-1842.
Garabrant DH, Peters RK, Homa DM. 1992. Asbestos and colon cancer: Lack of association in a large case-control study. American Journal of Epidemiology 135(8): 843-853.
Gardner MJ, Powell CA. 1986. Mortality of asbestos cement workers using almost exclusively chrysotile fibre. Journal of the Society of Occupational Medicine 36(4): 124-126.
Gerhardsson de Verdier M, Plato N, Steineck G, Peters JM.1992. Occupational exposures and cancer of the colon and rectum. American Journal of Industrial Medicine 22(3): 291-303.
Germani D, Belli S, Bruno C, Grignoli M, Nesti M, Pirastu R, Comba P. 1999. Cohort mortality study of women compensated for asbestosis in Italy. American Journal of Industrial Medicine 36(1): 129-134.
Goldberg MS, Parent ME, Siemiatycki J, Desy M, Nadon L, Richardson L, Lakhani R, Latreille B, Valois MF. 2001. A case-control study of the relationship between the risk of colon cancer in men and exposures to occupational agents. American Journal of Industrial Medicine 39(6): 531-546.
Hardell L. 1981. Relation of soft-tissue sarcoma, malignant lymphoma and colon cancer to phenoxy acids, chlorophenols and other agents. Scandinavian Journal of Work, Environment and Health 7(2): 119-130.
Hesterberg TW, Miller WC, McConnell EE, Chevalier J, Hadley JG, Bernstein DM, Thevenaz P, Anderson R. 1993. Chronic inhalation toxicity of size-separated glass fibers in Fischer 344 rats. Fundamental and Applied Toxicology 20(4): 464-476.
Hesterberg TW, Miller WC, Mast R, McConnell EE, Bernstein DM, Anderson R. 1994. Relationship between lung biopersistence and biological effects of man-made vitreous fibers after chronic inhalation in rats. Environmental Health Perspectives 102 (Supplement 5): 133-137.
HHS (US Department of Health and Human Services). 1983. Lifetime Carcinogenesis Studies of Amosite Asbestos (CAS NO. 12172-73-5) in Syrian Golden Hamsters (Feed Studies). NTP TR 249. Research Triangle Park, NC: National Toxicology Program.
HHS. 1985. Toxicology and Carcinogenesis Studies of Chrysotile Asbestos (CAS No. 12001-29-5) in F344/N Rats (Feed Studies). NTP TR 295. Research Triangle Park, NC: National Toxicology Program.
HHS. 1988. Toxicology and Carcinogenesis Studies of Crocidolite Asbestos (CAS No. 12001-28-4) in F344/N Rats (Feed Studies). NTP TR 280. Research Triangle Park, NC: National Toxicology Program.
HHS. 1990a. Lifetime Carcinogenesis Studies of Chrysotile Asbestos (CAS No. 12001-29-5) in Syrian Golden Hamsters (Feed Studies). NTP TR 246. Research Triangle Park, North Carolina: National Toxicology Program.
HHS. 1990b. Toxicology and Carcinogenesis Studies of Amosite Asbestos (CAS No. 12172-73-5) in F344/N Rats (Feed Studies). NTP TR 279. Research Triangle Park, NC: National Toxicology Program.
HHS. 1990c. Toxicology and Carcinogenesis Studies of Tremolite (CAS No. 14567-73-8) in F344/N Rats (Feed Studies). NTP TR 277. Research Triangle Park, NC: National Toxicology Program.Hillerdal G. 1980. Gastrointestinal carcinoma and occurrence of pleural plaques on pulmonary X-ray. Journal of Occupational Medicine 22(12): 806-809.
Hodgson J, Jones R. 1986. Mortality of asbestos workers in England and Wales 1971-1981. British Journal of Industrial Medicine 43(3): 158-164.
Hughes JM, Weill H, Hammad YY. 1987. Mortality of workers employed in two asbestos cement manufacturing plants. British Journal of Industrial Medicine 44(3): 161-174.
Jakobsson K, Albin M, Hagmar L. 1994. Asbestos, cement, and cancer in the right part of the colon. Occupational and Environmental Medicine 51(2): 95-101.
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun M. 2006. Cancer statistics, 2006. CA: A Cancer Journal for Clinicians 56: 106-130.
Karjalainen A, Pukkala E, Kauppinen T, Partanen T. 1999. Incidence of cancer among Finnish patients with asbestos-related pulmonary or pleural fibrosis. Cancer Causes and Control 10(1): 51-57.
Kobayashi H, Ming ZW, Watanabe H, Ohnishi Y. 1987. A quantitative study on the distribution of asbestos bodies in extrapulmonary organs. ACTA Pathologica Japonica 37(3): 375-383.
Levin J, McLarty J, Hurst GA, Smith A, Frank AL. 1998. Tyler asbestos workers: Mortality experience in a cohort exposed to amosite. Occupational and Environmental Medicine 55(3): 155-160.
McConnell EE. 2005 (October 27). Personal Communication to Mary Paxton for the Committee on Asbestos: Selected Health Effects. Available in IOM Public Access Files.
McConnell E, Kamstrup O, Musselman R, Hesterberg T, Chevalier J, Miller W, Thevenaz P. 1994a. Chronic inhalation study of size-separated rock and slag wool insulation fibers in Fischer 344/N rats. Inhalation Toxicology 6(6): 571-614.
McConnell E, Mast R, Hesterberg T, Chevalier J, Kotin P, Bernstein D, Thevenaz P, Glass L, Anderson R. 1994b. Chronic inhalation toxicity of a kaolin-based refactory cermaic fiber in Syrian golden hamsters. Inhalation Toxicology 6(6): 503-532.
McConnell EE, Axten C, Hesterberg TW, Chevalier J, Miller WC, Everitt J, Oberdorster G, Chase GR, Thevenaz P, Kotin P. 1999. Studies on the inhalation toxicology of two fiberglasses and amosite asbestos in the Syrian golden hamster: Part II. Results of chronic exposure. Inhalation Toxicology 11(9): 785-835.
McDonald JC, Liddell FD, Dufresne A, McDonald AD. 1993. The 1891-1920 birth cohort of Quebec chrysotile miners and millers: Mortality 1976-88. British Journal of Industrial Medicine 50(12): 1073-1081.
Meurman LO, Pukkala E, Hakama M. 1994. Incidence of cancer among anthophyllite asbestos miners in Finland. Occupational and Environmental Medicine 51(6): 421-425.
Neugut AI, Murray TI, Garbowski GC, Treat MR, Forde KA, Waye JD, Fenoglio-Preiser C. 1991. Association of asbestos exposure with colorectal adenomatous polyps and cancer. Journal of the National Cancer Institute 83(24): 1827-1828.
Peto J, Doll R, Hermon C, Binns W, Clayton R, Goffe T. 1985. Relationship of mortality to measures of environmental asbestos pollution in an asbestos textile factory. Annals of Occupational Hygiene 29(3): 305-355.
Piolatto G, Negri E, La Vecchia C, Pira E, Decarli A, Peto J. 1990. An update of cancer mortality among chrysotile asbestos miners in Balangero, northern Italy. British Journal of Industrial Medicine 47(12): 810-814.
Pira E, Pelucchi C, Buffoni L, Palmas A, Turbiglio M, Negri E, Piolatto PG, La Vecchia C. 2005. Cancer mortality in a cohort of asbestos textile workers. British Journal of Cancer 92(3): 580-586.
Puntoni R, Merlo F, Borsa L, Reggiardo G, Garrone E, Ceppi M. 2001. A historical cohort mortality study among shipyard workers in Genoa, Italy. American Journal of Industrial Medicine 40(4): 363-370.
Raffn E, Villadsen E, Lynge E. 1996. Colorectal cancer in asbestos cement workers in Denmark. American Journal of Industrial Medicine 30(3): 267-272.
Reid A, Ambrosini G, de Klerk N, Fritschi L, Musk B. 2004. Aerodigestive and gastrointestinal tract cancers and exposure to crocidolite (blue asbestos): Incidence and mortality among former crocidolite workers. International Journal of Cancer 111(5): 757-761.
Sanden A, Jarvholm B. 1987. Cancer morbidity in Swedish shipyard workers 1978-1983. International Archives of Occupational and Environmental Health 59(5): 455-462.
Seidman H, Selikoff IJ, Gelb SK. 1986. Mortality experience of amosite asbestos factory workers: Dose-response relationships 5 to 40 years after onset of short-term work exposure. American Journal of Industrial Medicine 10(5-6): 479-514.
Selikoff IJ, Seidman H. 1991. Asbestos-associated deaths among insulation workers in the United States and Canada, 1967-1987. Annals of the New York Academy of Sciences 643: 1-14.
Selikoff IJ, Hammond EC, Seidman H. 1979. Mortality experience of insulation workers in the United States and Canada, 1943-1976. Annals of the New York Academy of Sciences 330: 91-116.
Smailyte G, Kurtinaitis J, Andersen A. 2004. Cancer mortality and morbidity among Lithuanian asbestos-cement producing workers. Scandinavian Journal of Work, Environment and Health 30(1): 64-70.
Spiegelman D, Wegman DH. 1985. Occupation-related risks for colorectal cancer. Journal of the National Cancer Institute 75(5): 813-821.
Szeszenia-Dabrowska N, Urszula W, Szymczak W, Strzelecka A. 2002. Mortality study of workers compensated for asbestosis in Poland, 1970-1997. International Journal of Occupational Medicine and Environmental Health 15(3): 267-278.
Tola S, Kalliomaki PL, Pukkala E, Asp S, Korkala ML. 1988. Incidence of cancer among welders, platers, machinists, and pipe fitters in shipyards and machine shops. British Journal of Industrial Medicine 45(4): 209-218.
Vineis P, Ciccone G, Magnino A. 1993. Asbestos exposure, physical activity and colon cancer: A case-control study. Tumori 79(5): 301-303.
Wei EK, Giovannucci E, Wu K, Rosner B, Fuchs CS, Willett WC, Colditz GA. 2004. Comparison of risk factors for colon and rectal cancer. International Journal of Cancer 108(3): 433-442.
Woitowitz HJ, Lange HJ, Beierl L, Rathgeb M, Schmidt K, Ulm K, Giesen T, Woitowitz RH, Pache L, Rodelsperger K. 1986. Mortality rates in the Federal Republic of Germany following previous occupational exposure to asbestos dust. International Archives of Occupational and Environmental Health 57(3): 161-171.














