5
Older Adults and the Health Transition in Agincourt, Rural South Africa: New Understanding, Growing Complexity
Kathleen Kahn, Stephen Tollman, Margaret Thorogood, Myles Connor, Michel Garenne, Mark Collinson, and Gillian Hundt
INTRODUCTION
The population living in less developed regions of the world is growing rapidly, with the fastest growth projected for Africa. With declining mortality and fertility, the age structures of developing countries have aged. Subject to the same mortality and fertility declines, the percentage of people over age 50 will continue to rise, with large increases in the numbers of older people (Heligman, Chen, and Babkol, 1993). United Nations projections for South Africa indicate that the percentage of the population over age 60 will more than double from 6 percent in 1999 to 14 percent in 2050, estimates that are lower than those computed for less developed regions as a whole (United Nations, 1999).
While mortality levels are projected to decrease, the absolute number of deaths in the less developed regions will increase, with a shift to an older age distribution. As the population structure ages, so the age structure of deaths changes to one in which the greatest proportion of deaths is at the oldest ages. This is due to the fact that a greater proportion of the population has reached older ages as well as the lower probability of dying at younger ages. Such change in population age structure shifts the mortality profile from one dominated by the infectious diseases more common in children, toward one dominated by the noncommunicable diseases that affect older adults and the elderly. Despite the relatively young distribution of African mortality compared with other less developed regions, the number of deaths in Africa has increased more at the older ages; this reflects both
the changing age structure and the relative success of improvements in child health and reductions in child mortality.
Without HIV/AIDS, 19 percent more deaths are expected to occur during 2010-2015 compared with 1985-1990, with the entire increase occurring in the adult population (Heligman et al., 1993). However, high levels of HIV/AIDS characterize much of sub-Saharan Africa, including South Africa, and are altering the expected age distribution of these populations as a result of dramatically increasing mortality in the young and middle adult age groups (Dorrington, Bourne, Bradshaw, Laubsher, and Timaeus, 2001; Heligman et al., 1993; Joint United Nations Programme on HIV/ AIDS, 2002; Timaeus, 1998), together with decreasing fertility (Gregson, 1994; Gregson, Zaba, and Garnett, 1999).
Almost half the South African population resides in rural and semirural settings, comprising the majority of the country’s poor. The past decade has been one of momentous sociopolitical change in South Africa, with the population undergoing dramatic changes in patterns of health and disease. Yet the evidence base on which to premise interventions in support of rural health and development remains deeply inadequate. Characterizing and understanding the transitional process, let alone managing it effectively, are difficult tasks. This is apparent in the mixed results from policies to date, the concerns of leaders in the public sector, and a renewed government initiative to launch an integrated rural development strategy.
An overarching concern in the country, mirrored in many other settings, focuses on how best to apply society’s limited resources to a rapidly unfolding health and social transition in the face of escalating HIV/AIDS and continuing high levels of violence and injury. To do this, knowledge is needed about trends in rural health status and population dynamics, insight into the complex interplay between poverty-related diseases and emerging “chronic diseases of lifestyle,” understanding of the socioeconomic pressures imposed on households by severe illness and death, and evidence for medical, health, and social interventions that can enhance individual and household resilience.
Such understanding is vital to effective decision making at different levels of the health service. Understanding of changing mortality patterns is of real consequence for intervention programs, development of “essential packages” of care and the impact that can be expected, and resource allocation and human resource development. As reflected in the report of the Commission on Health Research for Development, drafted more than a decade ago, research on the problems of rural health and development remains essential to an effective societal response and may well prove the “essential link to equity in development” (Commission on Health Research for Development, 1990).
This paper is divided into three parts. First, we review the theory of
epidemiological transition and its evolution over more than 30 years. Next, we examine, as a case study, changing mortality in the Agincourt subdistrict of rural South Africa, focusing particularly on older adults and on stroke and its risk factors. We contend that the early conceptions of epidemiological transition theory are inadequate to explain the changes observed, and we locate the empirical findings in a more contemporary analysis of the health transition. Finally, we raise some implications of the transition for the provision of health care.
THE THEORY OF EPIDEMIOLOGICAL TRANSITION
The first recorded discussion of changing population patterns and their impact, espoused by Thomas Malthus, dates back more than 200 years (Caldwell, 2001; Cappuccio, 2004). Since then, ideas concerning a health transition framework have evolved to explain the changes in levels and causes of illness and death occurring in most countries (Feacham, Phillips, and Bulatao, 1992), and to attempt to predict the trajectory of future change. The limitations of the demographic transition, with its focus on change from high mortality and fertility in traditional societies to low rates in more modern societies, was recognized by Abdel Omran, who in 1971 wrote about his theory of “epidemiologic transition.” Conceptually, this broadened the scope of “mortality transition” to include changing morbidity patterns—from pandemics of infection to degenerative and manmade diseases—and the interaction of these with their socioeconomic determinants and consequences (Omran, 1971).
Omran proposed three stages through which societies move sequentially: the era of pestilence and famine, the era of receding pandemics, and the era of degenerative and manmade diseases. The first stage is characterized by exceedingly high mortality, particularly in children, due largely to infectious diseases, nutritional disorders, and complications of pregnancy and childbirth. The second stage sees declining mortality and sustained population growth, and the third stage has lower overall mortality that peaks at older ages and results from noncommunicable disease and injuries. In this stage, life expectancy is higher for women than men, in contrast to the era of pestilence and famine, which has higher male life expectancy. Omran also described three basic models of the epidemiological transition differentiated by variations in the pattern, pace, determinants, and consequences of population change: the classical or Western model, in which progressive mortality and fertility declines followed socioeconomic development (seen in most Western European societies); the accelerated model, which started later and was more rapid (experienced in Japan and Eastern Europe); and the contemporary or delayed model, which attempts to describe the unfinished transition of most developing countries. The acceler-
ated model was also determined by socioeconomic advances but enhanced by developments in medical technology, whereas the delayed model was largely driven by the spread of medical and public health interventions (Gaylin and Kates, 1997; Omran, 1971).
While regarded as having made a groundbreaking contribution to public health through concentrating on the mortality side of the demographic transition, placing health change as part of social change, leading public health practitioners to value the importance of their activities, and stimulating debate and enquiry (Caldwell, 2001; Cappuccio, 2004), Omran’s theory is not without criticism. Caldwell (2001) points out that while epidemiological transition theory emphasizes the role of social, economic, ecobiological, and environmental change, it understates the contributions of scientific discovery, medical technology, and public health interventions, such as water purification, sewage disposal, and immunization. Defining just three stages of the epidemiological transition is thought too restrictive, a limitation identified by Omran and others in the 1980s who have added a subsequent stage dealing with the reduction of age-specific death rates due to degenerative diseases (Beaglehole and Bonita, 2004; Olshansky and Ault, 1986; Omran, 1982). Their sequential relationship, moving through one stage and then the next, has been challenged, too (Beaglehole and Bonita, 2004; National Research Council, 1993). “The ephemeral nature of health trends in developed countries seriously undermines widely held notions of epidemiologic transition as a stable march of progress” (Gaylin and Kates, 1997:615).
Frenk, Bobadilla, Sepulveda, and Cervantes (1989) propose modifications to the original theory through examination of the transition in middle-income countries. They find that the eras are not necessarily sequential but may overlap, patterns of morbidity and mortality may be reversed (a so-called counter transition), change may not occur fully, and infectious and noncommunicable diseases may coexist (a protracted or prolonged transition). Epidemiological polarization is seen in places where the poorest experience the highest death rates from more pretransitional diseases, including infections and nutritional disorders. Gaylin and Kates (1997) argue that the two key limitations of epidemiological transition theory are its generalized formulation and failure to differentiate among population subgroups and its suggestion that infectious diseases can be eliminated and are replaced by degenerative diseases. The emergence of HIV/AIDS as a new infectious disease challenges the latter assumption, exacerbating mortality differentials among particular subgroups.
Although further theoretical development has been called for (Frenk, Bobadilla, Stern, Frejka, and Lozano, 1994), ongoing conceptual advances do begin to address the critique that bodies of understanding derived from demographic and epidemiological transition theory project too linear and
unidimensional a developmental path, which is inadequate to explain the transitions under way today in rural and developing settings (Beaglehole and Bonita, 2004; National Research Council, 1993). The concept of a health transition attempts to extend classical transition theory to include the social and behavioral changes that parallel and drive the changes in mortality, fertility, and patterns of illness, disability, and death. While this makes it the most appropriate framework for describing changing mortality patterns, limitations remain. It can describe differences in death rates from country to country but cannot explain these differences, its ability to predict changing patterns of disease precipitated by development is limited, it minimizes the interaction between infectious and noncommunicable diseases, and it takes insufficient account of the major social and economic changes that drove the transition (Beaglehole and Bonita, 2004).
While these transition frameworks are helpful in thinking about changing patterns of illness and death, actual information on the direction and scale of change is required, with empirical data best, for developing appropriate policy in response to the health needs of populations.
OLDER ADULTS AND THE HEALTH TRANSITION IN AGINCOURT: A CASE STUDY
The Agincourt Study Site
Geographic, Social, and Economic Characteristics of Agincourt
The Agincourt subdistrict site covers 390 sq km of the Bushbuckridge district of Mpumalanga Province, lying just south of Limpopo Province, adjacent to Mozambique’s western boundary (separated by the Kruger National Park). The area is reasonably typical of the densely settled former Bantustan areas (homelands) in South Africa’s rural northeast (about 170 persons per sq km), with some 69,000 people in 11,500 households across 21 villages that range in size from 100 to 1,100 households. Nearly one-third of the population are Mozambican immigrants, largely displaced in the early to mid-1980s during the civil war, who fled into South Africa across its eastern border and dispersed within host communities or settled on land allocated to them by local tribal authorities.
The geoecological zone is semiarid savannah, dry (annual rainfall 550-700 mm), and better suited to cattle and game farming than agricultural development. A high variability in interseasonal rainfall patterns renders the area vulnerable to drought—some 80 percent of the rain falls during summer months (Collinson et al., 2002). In addition, household plots are generally too small to support subsistence agriculture, although crops supplement the family diet (Tollman, Herbst, and Garenne, 1995). Despite
recent development activities, water shortage is a serious problem and household sanitation is generally limited to pit latrines (Dolan, Tollman, Nkuna, and Gear, 1997). The paving of gravel roads is beginning, however, and electricity is now widely available in the area, although few people can afford the service. While most children reach secondary school, few obtain any form of tertiary education (Tollman et al., 1995). Health care is based on the Agincourt Health Centre and five fixed clinics, all government facilities that provide free consultation and treatment. Referral is to three district hospitals (Mapulaneng, Matikwane, and Tintswalo) 25-60 km away. Private allopathic providers, traditional healers, and faith healers also provide services in or close to the study site.
Formal-sector employment is limited in the area. Migrant labor, involving work in the mines, in larger towns, and on nearby farms, continues to dominate, with remittances critical to local livelihoods. The permanent population is 80.5 percent of the total, the balance temporarily absent for more than 6 months in a year. The sex ratio is 93 for the whole population and 80 for the permanent population. While temporary labor migration rates of men are substantially higher than those of women, increasing numbers of women are joining the migrant labor force, a pattern that probably reflects new economic opportunities. South Africa has a system of state-supported social welfare unique in sub-Saharan Africa, which includes an old-age pension payable to women from age 60 and men from age 65.
Population Growth and Age Structure, 1992-2000
The foundation of the work in the Agincourt study site is a Health and Demographic Surveillance System (HDSS). A baseline census on the entire Agincourt population was conducted in 1992, with registration of every household and individual, including date of birth, sex, nationality, residence status, education, and relationship to household head. Since then, rigorous annual updates have been conducted, with information on all births, deaths, and in- and out-migrations collected in the population under surveillance. The update involves a household visit during which a fieldworker verifies existing information, adds new individual- or house-hold-level data, and records the demographic events that have occurred since the preceding year’s census update. Additional information is collected on all pregnancy outcomes, movements in and out of households, and deaths; maternity histories are also conducted. The result is a longitudinal database, dating back to 1992, containing empirical numerator and denominator data, used for the examination of trends in population size and structure and the calculation of rates. Details of the Agincourt HDSS approach and methods have been published elsewhere (Collinson et al., 2002).
The Agincourt population has increased in size from some 57,600 people in 1992 to close to 69,000 at the end of the decade, an increase of 8 percent despite declining fertility (Garenne, Tollman, and Kahn, 2000) and worsening mortality (Kahn, Garenne, Tollman, and Collinson, in press; Tollman, Kahn, Garenne, and Gear, 1999). Ten percent of the population is age 50 and over, a proportion similar at the beginning and the end of the decade. The proportion of elderly ages 75 to 85, however, has doubled from 1 to 2 percent of the population. This translates into a 60 percent increase in the number of elderly.
Findings
Changing Age- and Cause-Specific Mortality, 1992-2000
As part of the Agincourt HDSS, a verbal autopsy (VA) is conducted for every death recorded in the study site. This involves an interview with the closest caregiver of the deceased to elicit details on the clinical signs and symptoms of the terminal illness. Additional information is collected on lifestyle practices (alcohol, smoking, physical activity), health-seeking behavior, and occupation. Verbal autopsy review entails assessment by two medical practitioners, blind to each other, who assign a probable cause to each death. When these correspond, the diagnosis is accepted. When they differ and consensus is not achieved, a third practitioner assesses the verbal autopsy blind to the earlier findings. If this assessment is congruent with one other, it is accepted as the probable cause of death; if not, the cause is coded as “ill-defined.” Whenever possible, a main (or underlying) cause, immediate cause, and contributory factors are identified; classification is consistent with the International Classification of Diseases (ICD-10) (Kahn, Tollman, Garenne, and Gear, 1999). The Agincourt VA tool and assessment approach has been validated by comparing VA diagnoses with hospital reference diagnoses. This procedure concluded that the Agincourt VA yielded reasonable estimates of cause-of-death frequencies in all age groups and that the findings could reliably inform district health planning (Kahn et al., 1999).
Trends in Older Adult Mortality, 1992-2000
As expected, mortality rates increase with age, with those over age 75 experiencing higher mortality than those in their 50s and 60s, in both men and women. However, mortality change across the decade reveals age and gender differences (Table 5-1). During ages 75-84, male mortality remained stable while female mortality decreased. During ages 65-74, female mortality remained stable while male mortality increased. These changes were
TABLE 5-1 Change in Mortality Rates by Age and Sex, Agincourt 1992-2000
not significant. Notable, however, are trends in the 50-64 age group. Comparing the first 3 years with the final 3 years of the study period, female mortality increased significantly from 95 per 1,000 in 1992-1994 to 151 per 1,000 in 1998-2000, while male mortality decreased from 251 to 199 per 1,000. By 2000, female mortality levels had reached those of men at 182 per 1,000.
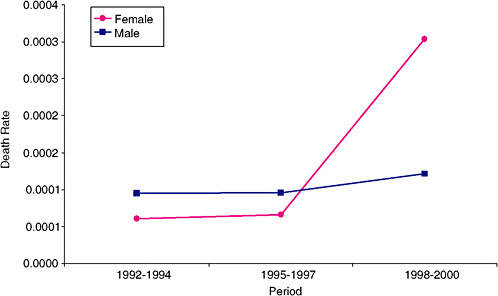
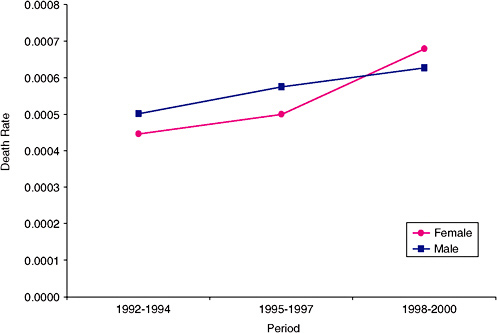
Why women appear to be losing their survival advantage in this population is a critical question. Verbal autopsy data indicate that women are bearing the brunt of emerging noncommunicable diseases: for all ages, female mortality from stroke, diabetes, and hypertension combined increased significantly over the 1992-2000 period (Figure 5-1). Female death rates from diabetes (Figure 5-2) and hypertension independently also increased significantly, exceeding male rates beginning from 1996. Divergence in the male and female trends for these conditions, as well as for stroke mortality (Figure 5-3), tested significant.
The profile of causes of death for women ages 50-64 indicates the contribution not only of cardiovascular and other noncommunicable diseases, but also of HIV/AIDS and cervical cancer to the observed mortality increase. Stroke, the top cause of death in this age group, together with diabe-
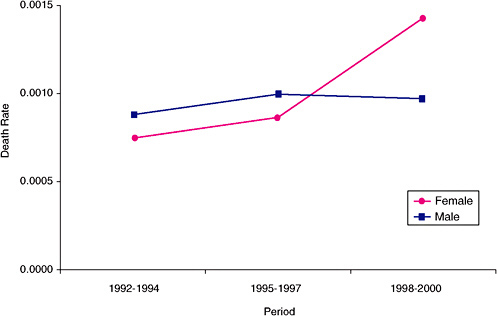
FIGURE 5-1 Death rate from noncommunicable diseases, all ages, Agincourt 1992-2000.
NOTE: Noncommunicable diseases include hypertension, diabetes, stroke, and cerebrovascular accident.
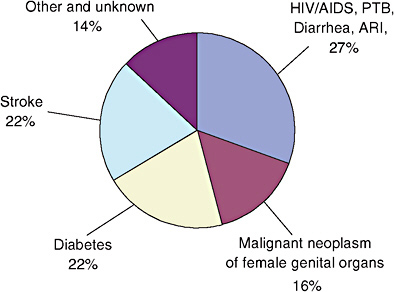
FIGURE 5-4 Causes of deaths responsible for the increase in mortality among women ages 50-64, Agincourt 1992-2000.
PTB = pulmonary tuberculosis; ARI = acute respiratory infection.
tes contributed 44 percent of the mortality increase, HIV/AIDS and related diseases a further 27 percent, and female genital malignancies (largely cancer of the cervix) 16 percent (Figure 5-4).
While the focus of this paper is on older adult mortality, it is necessary to briefly examine mortality at younger adult ages, because changes may affect the role and lifestyles of older adults, particularly women (discussed later in the chapter). In Agincourt, mortality rates are increasing dramatically in men and women ages 15-49. As in older women, a shift in gender balance is evident in the 15-29 age group, with female mortality exceeding that of men from about 1998. Increases in mortality for men and women ages 30-49 are similar.
Emerging Noncommunicable Diseases: The Case of Stroke
As populations undergo health and economic transitions, their disease patterns change, with cardiovascular disease (stroke, ischemic heart disease, and peripheral vascular disease) increasing. Hypertension is seen to increase first, followed by hemorrhagic stroke, and later peripheral vascular disease, ischemic heart disease, and ischemic stroke due to atherosclerosis (Pearson, 1999). Mortality data in Agincourt demonstrate this pattern, with stroke a top cause of death in adults ages 50-64 and age 65 and older (Kahn et al., 1999; Kahn and Tollman, 1999). However, a comprehensive picture
of the current burden requires knowledge of the prevalence, incidence, and case fatality rates of stroke. Policies and programs to improve prevention and treatment of stroke, whether at the community or health facility level, require an understanding of the risk factors as well as the lay beliefs and practices that determine health-seeking behavior.
Source of Data
The Southern Africa Stroke Prevention Initiative (SASPI) is an Agincourt-based multidisciplinary research project, including public health, epidemiology, neurology, and anthropology. The project aims to measure the current burden of stroke, to investigate the causes and social context of stroke, and to lay the groundwork for a program of intervention research. Between 2001 and 2003, the project employed multiple methods to quantify the community impact of stroke, understand the social setting of stroke, understand the nature of stroke and its risk factors in hospitalized patients and in stroke survivors in the community, and identify problems related to the prevention, diagnosis, and management of stroke (SASPI Project Team, 2003).
Stroke Prevalence and Risk Factors
A crude stroke prevalence of 290 per 100,000 people age 15 and over was found on the basis of clinical examination of all adults in the Agincourt study site who reported one-sided weakness or a history of stroke. This level is lower than that found in New Zealand, but higher than figures reported for Tanzania. A total of 66 percent of stroke survivors needed help with at least one activity of daily living, a prevalence of 200 per 100,000, which is higher than the rates previously reported for both New Zealand and Tanzania (Table 5-2) (SASPI Project Team, 2004a).
From their findings, the SASPI Project Team (2004a) suggests that Agincourt may be at an earlier stage of the health transition than New Zealand and further along than Tanzania. Alternatively, case fatality in Agincourt may be higher than in New Zealand but lower than in Tanzania. The high levels of disability could result from poor levels of care after strokes, or they could suggest more hemorrhagic than occlusive strokes. Population-based incidence studies with stroke-typing are needed to address these questions.
Risk Factors for Stroke
Little research has been done on risk factors for stroke in African populations, or on the relevance of Western population risk factors for develop-
TABLE 5-2 Comparison of Age-Standardized Rates (Segi population per 100,000) in Three Prevalence Studies
|
|
New Zealanda |
Tanzaniab |
SASPI (Agincourt) |
|
|
All Stroke Survivors |
833 |
NA |
290 |
|
|
|
Men |
991 |
154 |
281 |
|
|
Women |
706 |
114 |
315 |
|
|
Male/female ratio |
1.4 |
1.4 |
0.9 |
|
Stroke Survivors “Needing help with at least 1 activity of daily living” |
173 |
NA |
200 |
|
|
|
Men |
156 |
69 |
218 |
|
|
Women |
188 |
90 |
188 |
|
|
Male/female ratio |
0.8 |
0.8 |
1.2 |
|
NOTE: NA = not available. aBonita, Solomon, and Broad (1997). bWalker et al. (2000). SOURCE: SASPI Project Team (2004a). |
||||
ing countries. In order to develop and implement appropriate interventions, it is important to identify the risk factors for stroke prevalent in the Agincourt population. Among stroke survivors, hypertension was the main risk factor found (84 percent were hypertensive or had evidence of organ damage resulting from hypertension), suggesting that rural South Africans are in the early transition stage. Evidence of atherosclerosis and myocardial infarction, which typically appear later in the transition, was absent (SASPI Project Team, 2004a). Cigarette smoking was not a major risk factor in stroke survivors (9 percent were smokers) (SASPI Project Team, 2004b).
In the general population, risk factor patterns for cardiovascular disease appear to be consistent with those proposed for a population in early transition (Pearson, 1999; Yusuf, Reddy, Ounpuu, and Anand, 2001). A cross-sectional risk factor survey of the general Agincourt population over age 35 (Thorogood, Connor, Tollman, Lewando Hundt, and Marsh, 2005) found that over 40 percent of subjects had hypertension (blood pressure >140/90 mmHg), and that obesity (body mass index and abdominal obesity) was a significant problem in women but not in men. The relationship between body mass index and blood pressure differed between men and women, with a positive relationship found in men but not in women. Cigarette and alcohol use was uncommon in women; a high prevalence of smoking was found in men, although the amount smoked was small. Consumption of fruit and vegetables was low (less than a quarter eat fruit or
vegetables on a daily basis). About a quarter of the population had elevated blood lipids, and elevated blood glucose was rarely found (Thorogood et al., 2005).
Increasing Burden on Women
The decade of the 1990s saw steadily rising mortality in Agincourt adults up to age 65, with female mortality worsening relative to male mortality at both young (ages 20-49) and older ages (ages 50-64). Earlier transmission of HIV in women than in men is the most likely explanation at young adult ages, while data on cause of death in women over age 50 suggest that noncommunicable diseases are rising more rapidly in women, and that these may contribute to the pattern of female mortality at older ages. HIV/AIDS, while also propelling the worsening mortality in women ages 50-64, is affecting men and women similarly. Early evidence on cardiovascular risk factors indicates gender differentials in obesity, cigarette smoking, and alcohol consumption (Thorogood et al., 2005). More needs to be learned about gender differentials in risk factors, lifestyle behaviors, and genetic predisposition, if the burden on women is to be redressed through targeted health and social interventions.
The changing demography of young or prime-age adults affects older adults, particularly women, in ways that put them at great disadvantage. Increasing migration of young women to join the labor force affects their parents, who find themselves without the personal care and relief from responsibilities that are culturally expected at their stage of life. In addition, grandmothers often experience extension of their child care role to grandchildren and great-grandchildren. In the case of adult children leaving for reasons of employment, these negative impacts may be partially offset by remittances from the place of work back to the rural household. In contrast, adult children with AIDS become less able to work and consequently contribute less to household income at a time when their consumption of household resources, particularly health expenditures, increases (Gaylin and Kates, 1997). Widespread HIV/AIDS has resulted in older people left to fend for themselves, care for chronically ill and dying adult children, and raise and support grandchildren in circumstances of increasing poverty compounded by the burden of grief following the death of one or more of their children (Barnett and Whiteside, 2002).
IMPLICATIONS OF CHANGING ADULT HEALTH FOR PROVISION OF HEALTH CARE
During this early transitional stage of rural South African communities, what role does the health service currently play in hypertension control and
secondary prevention of stroke? In South Africa, free primary health care has gone some way to increasing access for the poorest sectors of society and achieving greater equity. Despite this, evidence on outreach and quality of primary care services is not encouraging (Levitt et al., 1996). Other costs, particularly transport, remain a barrier, as do restricted opening hours for working adults. In the SASPI study, few stroke survivors were on antihypertensive treatment (8 percent whereas 84 percent had evidence of hypertension), with only one person adequately controlled and only one person taking daily aspirin (SASPI Project Team, 2004b). Only a quarter of those with hypertension in the general population were on treatment (75 percent of hypertensive people were thus untreated), and half of those on treatment still had an elevated blood pressure (Thorogood et al., 2005).
Do people’s health beliefs result in inadequate utilization of Western health services, and does this partly explain the poor medical management found? In the Agincourt area, illnesses are generally understood as caused by biomedical problems (xilungu, white, Western) and by social problems (xintu, African traditional). Many conditions therefore need treatment from multiple sources. One-sided weakness is understood to be a biomedical condition (xistroku) but can also represent bewitchment or xifulana, a condition caused by humans through dysfunctional relations. Xistroku can be treated by allopathic methods, but xifulana requires intervention from churches or traditional healers. Most people access plural health care, visiting allopathic services, public clinics, and hospitals as well as private providers and also healers and prophets (Lewando Hundt, Stuttaford, and Ngoma, 2004). In fact, the majority (79 percent) of stroke survivors in Agincourt had sought allopathic care at some point after their stroke (SASPI Project Team, 2004b).
In South Africa and other developing countries, rapid demographic and epidemiological change has provided little time for health services to adjust to the needs of chronic care for older people (Bobadilla and Possas, 1993). Changing patterns pose a challenge to existing health services that are generally underresourced, inadequately skilled, and poorly organized and managed. In Agincourt, barriers to secondary prevention of stroke include cost of treatment, reluctance to use pills, difficulties with access to drugs, and lack of equipment to measure blood pressure (SASPI Project Team, 2004b), while problems with staff knowledge, attitudes, and practices have been identified in public-sector facilities providing primary care for diabetes in South Africa (Goodman, Zwarenstein, Robinson, and Levitt, 1996; Levitt et al., 1996).
There is concern that a move away from an infectious to a noncommunicable disease focus could be detrimental to poorer sectors of a population (Gwatkin and Guillot, 2000; Gwatkin, Guillot, and Heuveline, 1999), a concern relevant for rural South Africa, as disparities in child mortality by
social class have been documented in Agincourt (Hargreaves, Collinson, Kahn, Clark, and Tollman, 2004). There is clear recognition that the development and financing of health systems to meet the needs of adults and address issues of chronic care delivery must occur without compromising services for women and children (Bobadilla and Possas, 1993; Phillips, Feachem, Murray, Over, and Kjellstrom, 1993; Unwin et al., 2001). In fact, the gains in health for children achieved through communicable disease prevention and control would be undermined if efforts were not also directed to noncommunicable disease prevention and control in adults (Mosely and Gray, 1993; Reddy, 1999).
The particular challenges for rural South African health services, and probably other parts of sub-Saharan Africa in the future, are substantial. There is need to effectively prevent and control the increasing burden of noncommunicable diseases, address HIV/AIDS transmission and treatment and provide home-based care for the terminally ill, while simultaneously maintaining and improving on gains in child and maternal health. Agincourt adults and other Southern African populations are subject to extensive temporary labor migration, with consequent high mobility, making the provision of chronic, ongoing care especially challenging.
While a full account of health system limitations is beyond the scope of this paper, current understanding of the health transition in Agincourt does highlight particular areas that require strengthening. Although fiscal constraints may put achievement of all aspects beyond the short-term reach of South African health services, and certainly those of other sub-Saharan African countries, much can be achieved through better use and some reallocation of existing resources.
Three key issues are considered. While based on experience of the South African rural health care system, general principles are of relevance to other developing settings.
Building Clinical Management Capacity
Staffing of health facilities in a district should include an appropriate mix of skills at different levels of care (clinic, health center, district hospital) based on the morbidity and mortality patterns prevalent in the area. While of variable quality and accessibility, EPI (Expanded Programme on Immunisation) and nutrition programs have long been provided in many developing country settings, IMCI (Integrated Management of Childhood Illnesses) services have been introduced more recently, and VCT (HIV Voluntary Counselling and Testing) services are becoming available in some. Nurses competent to manage adult health conditions at the clinic level are now required, and the Integrated Management of Adolescent and Adult Illness (IMAI) is being developed by the World Health Organization to
support this (IMAI has a focus on acute illness as well as on chronic disease and HIV/AIDS). A “step-up” in care between different levels of the health service, such as clinic, health center, and district hospital, needs to be planned, and staff with the requisite skills employed at each level. An understanding of the evolving patterns of illness also needs to influence curriculum development for basic health worker training programs and priorities for continuing professional development. Screening programs should be introduced for conditions in which diagnosis and treatment can be sustained. Greater emphasis needs to be placed on noncommunicable disease diagnosis and management and on the detection of complications. An understanding of risk factors, including hypertension, obesity, and such lifestyle factors as smoking and alcohol consumption, as well as methods of reducing them, is needed.
Two strategies to improve the clinical care of patients are clinical protocols and patient-retained records. Clinical protocols, or structured treatment guidelines, are tools designed to promote standardized, cost-effective, high-quality treatment of particular conditions. Staff tend not to follow these guidelines if passively disseminated, however (Daniels et al., 2000; Goodman et al., 1996), and their introduction and continued use needs to be maintained by in-service training programs. Particular strategies for promoting the use of guidelines can have additional advantages; an example is inclusion of the guidelines in a structured clinical record. This can become a useful tool for audit and evaluation of the quality of care, providing opportunity for discussions regarding patient care, thereby improving both education and teamwork (Daniels et al., 2000).
A patient-retained record can also serve to improve patient care. Advantages include better compliance through an implied partnership with the health service and decreased waiting time at the clinic through elimination of queuing for clinic records (Daniels et al., 2000). This removes one disincentive for patients to return for follow-up visits. In regions with high levels of circular migration, such as much of Southern Africa, patients may attend different facilities depending on whether they are at their temporary place of work or at their permanent residence at the time of the follow-up visit. A patient-retained record ensures that full clinical, laboratory, and treatment information is available to all health providers, while clinical guidelines together with medication from an essential drugs list enable continuity of appropriate care.
Improving Access to Care
While a health service should respond to the needs and demands of its catchment population, these are not necessarily the same. Whereas needs are largely determined by the health status of a community, demand de-
pends also on the community’s perceptions of illness, which may result in excessive or inappropriately low use of services (Bobadilla and Possas, 1993). Understanding how people perceive the cause of illness is critical in understanding patterns of health care used. In settings in which people tend to access plural health care, encouraging earlier consultation and regular follow-up at Western primary care services may be an important part of developing patient literacy around noncommunicable diseases and their management.
Treatment of hypertension in sub-Saharan Africa, despite the cost and difficulties, is a priority. Yet investment in a better organized health care system is needed in order to realize the gains in adult health (Cooper, Rotimi, Kaufman, Muna, and Mensah, 1998). With regular follow-up care a critical component of chronic disease management, addressing common barriers is imperative to ensuring patient return. These include ineffective drug distribution systems, malfunctioning equipment, inadequate staff training, and poor staff attitudes.
A less rigid approach to the provision of chronic disease services will go some way to improving quality and addressing the needs of patients. Scheduling of clinic hours and patient waiting times will need attention to facilitate attendance of working adults. Clinics must be equipped with functioning blood pressure cuffs, adult weight scales, and glucometers, and a regular drug supply must be ensured to prevent patients from bypassing the primary care level or failing to attend for follow-up at all. A comprehensive approach that seeks synergy between different chronic care programs will produce benefits for each. This will be particularly the case in settings in which antiretroviral therapy is offered, as these require high-quality services, an uninterrupted drug supply, and access to laboratory facilities.
Controlling Escalating Costs
The high costs of many interventions for noncommunicable diseases are of concern in considering sustainable programs for resource-constrained health systems (Bobadilla and Possas, 1993; Burdon, 1998; Cooper et al., 1998). Interventions with low cost-effectiveness should certainly be limited, and appropriate use of allocated resources needs to be monitored. The goal for adult health programs should be early detection of common chronic conditions (those that can reasonably occur at the primary care level), thus saving resources by delaying progress to complications and advanced stages of disease that require hospitalization (Bobadilla and Possas, 1993). Improvements in quality at the primary care level, discussed above, are essential if screening, diagnostic procedures, and cost-effective ambulatory care are to be successfully devolved to this level.
CONCLUSION
Evidence from the Agincourt study site in rural South Africa, drawn from multiple sources, highlights limitations of classical epidemiological transition theory and reinforces the need for a less rigid, more flexible notion of “complex, multi-sided processes of change in particular societies” (Chen, Kleinman and Ware, 1994). Data from Agincourt demonstrate a counter transition in which mortality is increasing rather than declining as epidemiological transition theory would predict. Sequential passage through Omran’s stages—from the era of pestilence and famine, through receding pandemics, to degenerative and manmade diseases—is too linear a model and does not fit the complex interplay of social, economic, behavioral, and environmental factors that act on populations. Instead, the transition under way in rural South Africa better fits the more contemporary framework used to describe transition in other middle-income countries (Frenk et al., 1989). In Agincourt, we have a protracted or prolonged transition in which change is incomplete and different stages are spanned simultaneously. The population is experiencing coexistence of the unfinished agenda of diseases of poverty (persisting infection and malnutrition), together with emerging noncommunicable diseases and escalating HIV/AIDS (Kahn et al., 1999). The HIV/AIDS epidemic provides stark evidence that infectious diseases are not likely to be conquered and replaced with manmade and degenerative diseases. Rather, societies will have to contend with new infectious diseases concurrent with emerging noncommunicable diseases.
As shown elsewhere, noncommunicable diseases are the leading causes of death in adults (Phillips et al., 1993), with the burden falling more on women than on men in Agincourt. Evidence on stroke and cardiovascular risk factors, particularly hypertension, indicates that this population is in the early stage of health transition and is an “early adopter” community within the sub-Saharan African context (Thorogood et al., 2005). The South African experience may well anticipate that of other countries in the region.
The coexistence of communicable and noncommunicable diseases poses multiple challenges for households, policy makers, and health system planners and managers. Efforts to project the prevalence of chronic diseases for purposes of health budgeting and planning need to take into account the impact of HIV/AIDS; fewer infected people will survive to middle and older ages at which noncommunicable diseases reach their peak age-specific prevalence, resulting in lower chronic disease prevalence rates (Panz and Joffe, 1999). Developing health systems—to cater to the chronic, ongoing requirements of adult noncommunicable disease prevention and control while at the same time preserving the acute, short-term care of maternal and child health services—calls for calculated reorientation on the part of policy makers and planners. Scarce public-sector resources will have to be
creatively managed to contend with multiple and divergent health problems. A comprehensive approach should ensure that health-sector human resources and organizational and management improvements benefit both HIV/AIDS and noncommunicable disease programs.
While there are calls for further theoretical development of the health transition framework (Beaglehole and Bonita, 2004; Frenk et al., 1994), building an understanding of actual transition experience through empirical research is critical for the formulation of effective public health and social policy (Bell and Chen, 1994).
REFERENCES
Barnett, T., and Whiteside, A. (2002). AIDS in the twenty-first century: Disease and globalization. New York: Palgrave Macmillan.
Beaglehole, R., and Bonita, R. (2004). Public health at the crossroads: Achievements and prospects, second edition. Cambridge, England: Cambridge University Press.
Bell, D.E., and Chen, L.C. (1994). Responding to health transitions: From research to action. In L.C. Chen, A. Kleinman, and N.C. Ware (Eds.), Health and social change in international perspective (pp. 491-501). Cambridge, MA: Harvard University Press.
Bobadilla, J.L., and Possas, C. de A. (1993). Health policy issues in three Latin American countries: Implications of the epidemiological transition. In National Research Council, The epidemiological transition: Policy and planning implications for developing countries (pp. 145-169). Committee on Population, J.N. Gribble and S.H. Preston (Eds.). Washington, DC: National Academy Press.
Bonita, R., Solomon, N., and Broad, J.B. (1997). Prevalence of stroke and stroke-related disability: Estimates from the Auckland Stroke Studies. Stroke, 28, 1898-1902.
Burdon, J. (1998). Figure of $1,800 per life saved seems optimistic (letter). British Medical Journal, 317, 76.
Caldwell, J.C. (2001). Population health in transition. Bulletin of the World Health Organization, 79(2), 159-160.
Cappuccio, F.P. (2004). Commentary: Epidemiological transition, migration, and cardiovascular disease. International Journal of Epidemiology, 33, 387-388.
Chen, L.C., Kleinman, A., and Ware, N.C. (1994). Overview. In L.C. Chen, A. Kleinman, and N.C. Ware (Eds.), Health and social change in international perspective (p. xiv). Cambridge, MA: Harvard University Press.
Collinson, M., Mokoena, O., Mgiba, N., Kahn, K., Tollman, S., Garenne, M., Herbst, K., Malomane, E., and Shackleton, S. (2002). Agincourt DSS, South Africa. In INDEPTH network, population, and health in developing countries, volume 1. Population, health, and survival at INDEPTH sites (pp. 197-205). Ottawa, Canada: International Development Research Centre.
Commission on Health Research for Development. (1990). Health research: Essential link to equity in development. New York: Oxford University Press.
Cooper, R.S., Rotimi, C.N., Kaufman, J.S., Muna, W.F.T., and Mensah, G.A. (1998). Hypertension treatment and control in sub-Saharan Africa: The epidemiological basis for policy. British Medical Journal, 316, 614-617.
Daniels, A.R., Patel, M., Biesma, R., Otten, J., Levitt, N.S., Steyn, K., Martell, R., and Dick, J. (2000). A structured record to implement the national guidelines for diabetes and hypertension care. South African Medical Journal, 90(1), 53-56.
Dolan, C., Tollman, S., Nkuna, V., and Gear, J. (1997). The links between legal status and environmental health: A case study of Mozambican refugees and their hosts in the Mpumalanga (eastern Transvaal) Lowveld, South Africa. International Journal of Health and Human Rights, 2(2), 62-84.
Dorrington, R., Bourne, D., Bradshaw, D., Laubsher, R., and Timaeus, I.M. (2001) The impact of HIV/AIDS on adult mortality in South Africa. Report. Cape Town: South African Medical Research Council.
Feachem R.G.A., Phillips M.A., and Bulatao R.A. (1992). Introducing adult health. In R.G.A. Feacham, T. Kjellstrom, C.J.L. Murray, M. Over, and M.A. Phillips (Eds.), The health of adults in the developing world (pp. 1-22). New York: Oxford University Press.
Frenk, J., Bobadilla, J.L., Sepulveda, J., and Cervantes, M.L. (1989). Health transition in middle-income countries: New challenges for health care. Health Policy and Planning, 4(1), 29-39.
Frenk, J., Bobadilla, J-L., Stern, C., Frejka, T., and Lozano, R. (1994). Elements for a theory of the health transition. In L.C. Chen, A. Kleinman, and N.C. Ware (Eds.), Health and social change in international perspective (pp. 25-49). Cambridge, MA: Harvard University Press.
Garenne, M., Tollman, S., and Kahn, K. (2000). Premarital fertility in rural South Africa: A challenge to existing population policy. Studies in Family Planning, 31(1), 47-54.
Gaylin, D.S., and Kates, J. (1997). Refocusing the lens: Epidemiologic transition theory, mortality differentials, and the AIDS pandemic. Social Science and Medicine, 44(5), 609-621.
Goodman, G.R., Zwarenstein, M.F., Robinson, I.I., and Levitt, N.S. (1996). Staff knowledge, attitudes, and practices in public sector primary care of diabetes in Cape Town. South African Medical Journal, 87(3), 305-309.
Gregson, S. (1994). Will HIV become a major determinant of fertility in sub-Saharan Africa? Journal of Development Studies, 30(3), 650-679.
Gregson, S., Zaba, B., and Garnett, G.P. (1999). Low fertility in women with HIV and the impact of the epidemic on orphanhood and early childhood mortality in sub-Saharan Africa. AIDS, 13(Suppl A), S249-S257.
Gwatkin, D.R., and Guillot, M. (2000). The burden of disease among the global poor: Current situation, future trends, and implications for strategy. (Human Development Network. Health, Nutrition and Population). Washington, DC: The World Bank.
Gwatkin, D.R., Guillot, M., and Heuveline, P. (1999). The burden of disease among the global poor. The Lancet, 354, 586-589.
Hargreaves, J.R., Collinson, M.A., Kahn, K., Clark, C., and Tollman, S.M. (2004). Childhood mortality among Mozambican refugees and their hosts in rural South Africa. International Journal of Epidemiology, 33, 1271-1278.
Heligman, L., Chen, N., and Babkol, O. (1993). Shifts in the structure of population and deaths in less developed regions. In National Research Council, The epidemiological transition: Policy and planning implications for developing countries (pp. 9-41). Committee on Population, J.N. Gribble and S.H. Preston (Eds.). Washington, DC: National Academy Press.
Joint United Nations Programme on HIV/AIDS. (2002, July). Report on the global HIV/AIDS pandemic. Geneva, Switzerland: Author.
Kahn, K., and Tollman, S.M. (1999). Stroke in rural South Africa: Contributing to the little known about a big problem. South African Medical Journal, 89(1), 63-65.
Kahn, K., Tollman, S.M., Garenne, M., and Gear, J.S.S. (1999). Who dies from what? Determining cause of death in South Africa’s rural northeast. Tropical Medicine and International Health, 4, 433-441.
Kahn, K., Tollman, S.M., Garenne, M., and Gear, J.S.S. (2000). Validation and application of verbal autopsies in a rural area of South Africa. Tropical Medicine and International Health, 5(11), 824-831.
Kahn, K., Garenne, M., Tollman S, and Collinson, M. (in press). Mortality trends in a new South Africa (Agincourt 1992-2003): Hard to make a fresh start. Scandinavian Journal of Public Health.
Levitt, N.S., Zwarenstein, M.F., Doepfmer, S., Bawa, A.A., Katzenellenbogen, J., and Bradshaw, D. (1996). Public sector primary care of diabetics: A record review of quality of care in Cape Town. South African Medical Journal, 86(8), 1013-1017.
Lewando Hundt, G., Stuttaford, M., and Ngoma, B. (2004). The social diagnostics of stroke like symptoms: Healers, doctors and prophets in Agincourt, Limpopo Province, South Africa. Journal of Biosocial Sciences, 36, 433-443.
Mosely, W.H., and Gray, R. (1993). Childhood precursors of adult morbidity and mortality in developing countries: Implications for health programs. In National Research Council, The epidemiological transition: Policy and planning implications for developing countries (pp. 69-100). Committee on Population, J.N. Gribble and S.H. Preston (Eds.). Washington, DC: National Academy Press.
National Research Council. (1993). The epidemiological transition: Policy and planning implications for developing countries. Report of a Workshop. Committee on Population, J.N. Gribble and S.H. Preston (Eds.). Washington, DC: National Academy Press.
Olshansky, S.J, and Ault, E.B. (1986). The fourth stage of the epidemiologic transition: The age of delayed degenerative diseases. Milbank Memorial Fund Quarterly, 64, 355-391.
Omran, A.R. (1971). The epidemiologic transition. Milbank Memorial Fund Quarterly, 49(4), 509-538.
Omran, A.R. (1982). Epidemiologic transition. In J.A. Ross (Ed.), International encyclopaedia of population (pp. 172-183). London, England: Free Press.
Panz, V.R., and Joffe, B.I. (1999). Impact of HIV infection and AIDS on prevalence of type 2 diabetes in South Africa in 2010 (letter). British Medical Journal, 318, 1351-1352.
Pearson, T.A. (1999). Cardiovascular disease in developing countries: Myths, realities, and opportunities. Cardiovascular Drugs and Therapy, 13, 95-104.
Phillips, M., Feachem, R.G.A., Murray, C.J.L., Over, M., and Kjellstrom, T. (1993). Adult health: A legitimate concern for developing countries. American Journal of Public Health, 83(11), 1527-1530.
Reddy, K.S. (1999). The burden of disease among the global poor (letter). The Lancet, 354, 1477.
SASPI Project Team. (2003). Workshop of the Southern Africa stroke prevention initiative. (Report. 2-4 November). Division of Health in the Community, University of Warwick and School of Public Health, University of the Witwatersrand.
SASPI Project Team. (2004a). Prevalence of stroke survivors in rural South Africa: Results from the Southern Africa stroke prevention initiative (SASPI), Agincourt field site. Stroke, March, 627-632.
SASPI Project Team. (2004b). Secondary prevention of stroke: Results from the Southern Africa stroke prevention initiative (SASPI), Agincourt field site. Bulletin of the World Health Organization, 82(7), 503-508.
Thorogood, M., Connor, M., Tollman, S., Lewando-Hundt, G., and Marsh, J. (2005). The prevalence of cardiovascular risk factors in a rural South African population: Evidence of the impending cardiovascular epidemic from the Southern Africa stroke prevention initiative (SASPI). Unpublished manuscript, Warwick Medical School, Coventry, England.
Timaeus, I.M. (1998). Impact of the HIV epidemic on mortality in sub-Saharan Africa: Evidence from national surveys and censuses. AIDS, 12(Suppl. 1), S15-S27.
Tollman, S., Herbst, K., and Garenne, M. (1995). The Agincourt demographic and health study: Phase 1. Johannesburg, South Africa: Health Systems Development Unit, Department of Community Health, University of the Witwatersrand.
Tollman, S.M., Kahn, K., Garenne, M., and Gear, J.S.S. (1999). Reversal in mortality trends: Evidence from the Agincourt field site, South Africa, 1992-1995. AIDS, 13, 1091-1097.
United Nations, Population Division, Department of Economic and Social Affairs. (1999). Population ageing 1999. (UN Publication ST/ESA/SER.A/179). New York: Author.
Unwin, N., Setel, P., Rashid, S., Mugusi, F., Mbanya, J., Kitange, H., Hayes, L., Edwards, R., Aspray, T., and Alberti, K.G.M.M. (2001). Noncommunicable diseases in sub-Saharan Africa: Where do they feature in the health research agenda? Bulletin of the World Health Organization, 79(10), 947-953.
Walker, R.W., McLarty, D.G., Masuku, G., Kitange, H.M., Whiting, D., Moshi, A.F., Massawe, G., Amaro, R., Mhina, A., and Alberti, K.G.M.M. (2000). Age specific prevalence of impairment and disability relating to hemiplegic stroke in the Hai district of northern Tanzania. Journal of Neurology and Neurosurgery Psychiatry, 68, 749.
Yusuf, S., Reddy, S., Ounpuu, S., and Anand, S. (2001). Global burden of cardiovascular diseases Part I: General considerations, the epidemiologic transitions, risk factors, and the impact of urbanization. Circulation, 104, 2746-2753.