10
Survey Measures of Health: How Well Do Self-Reported and Observed Indicators Measure Health and Predict Mortality?
Randall Kuhn, Omar Rahman, and Jane Menken
INTRODUCTION
The costs and difficulties associated with assessing the health of a population have led to an ongoing search for indicators of health status that can be readily collected from large numbers of individuals with minimal expenditure of resources, including time, money, training, and logistics. Measuring health can be demanding in terms of interviewer time and skill, respondent comprehension, and logistic and analytic complexity. Set against the potentially higher costs and returns of physical health testing or the collection of biomarkers, there are simple self-reported and objective indicators that are relatively easy and inexpensive to collect.
If these low-cost measures are valid, they could prove beneficial in sub-Saharan Africa for assessing the overall burden of disease and the effectiveness of health systems. They could help address emerging concerns relating to adult health as processes of population aging gather pace and as HIV/ AIDS continues to affect health and mortality at all ages, both directly and through socioeconomic pathways.
Yet data to compare health indicators are rare. Rarer still is follow-up information to assess how well these measures predict subsequent mortality—the ultimate measure of poor health—in developing countries. In fact, the only developing country data set containing both multiple measures of health and prospective mortality follow-up comes from the Matlab study site in rural Bangladesh. Analysis of this data set is included in this volume for two reasons. First, measures that prove useful in one developing country context merit consideration for application in other regions. Second, Matlab
partners with community studies in sub-Saharan Africa that are part of the INDEPTH network (the International Network of field sites with continuous Demographic Evaluation of Populations and Their Health in developing countries); they provide the opportunity to replicate this study inexpensively and reasonably quickly in African contexts and in a comparative framework.
In this paper we consider five measures of health—three self-reported and two objectively observed—and address three questions:
-
How interrelated are these indicators? Can the same information on individual health be obtained with a smaller set of questions or observations, thereby reducing costs?
-
How well does each serve as a predictor of mortality? Here we assume that the poorer the health of an individual, the greater the risk of dying in a defined period (in this case, 5 years) after health is measured. The greater the predictive power, under this assumption, the better the measure is as a gauge of individual health.
-
Does the predictive power of the indices vary by age or gender? Here we ask whether, for example, self-reported poor health is related to subsequent mortality similarly across age and gender.
The study is based on health measures collected in the 1996 Matlab Health and Socioeconomic Survey (MHSS). The MHSS was carried out with funding from the U.S. National Institute on Aging as a collaboration among researchers based at the International Centre for Health and Population Research in Dhaka, Bangladesh (ICDDR,B), and at several institutions in the united States. ICDDR,B began its Health and Demographic Surveillance System (HDSS) in Matlab in the early 1960s and, for over 40 years, has visited every household at least monthly to collect accurate information on vital events. The HDSS served as the sampling frame for the MHSS (Rahman et al., 1999). Information on MHSS respondents was therefore automatically collected in the HDSS each month of the 5 years subsequent to the survey. We first consider, using MHSS data alone, the extent to which each of the health measures provides information independent of the others. Next, the combined MHSS/HDSS data are used to test how well each health indicator serves as a predictor of mortality in the follow-up period. We then rank these measures in terms of mortality predictive power and discuss the prevalence of the poor health by age and gender they reveal. Finally, we discuss two issues regarding the usefulness of these simple and inexpensive to collect measures: international comparability and comparability of the indices to more specific information on health obtainable through other means, such as biomarkers. As part of this discussion, we propose a research agenda for measuring health and evaluating health mea-
sures in sub-Saharan Africa that takes advantage of INDEPTH. INDEPTH sites, including Matlab, routinely record mortality in their Demographic Surveillance System records, and improved measurement of adult health is one of its current goals.
SIMPLE-TO-OBSERVE HEALTH INDICATORS
The indicators examined in this study are
-
self-reported health (SRH), whereby respondents are asked to classify their current health status as good, fair, or poor;
-
an index based on self-reported activities of daily living;
-
an index of self-reported major acute and chronic morbidity conditions;
-
an index of physical disability based on observed activities of daily living; and
-
current nutritional status as measured by body mass index.
Each of these indicators has been collected and studied in health surveys. While these measures are significantly related to one another, each may capture unique dimensions of ill health. They vary widely in terms of data collection time and field costs, yet none requires extensive field training or expensive or delicate equipment.
Because SRH is so easy and inexpensive to collect, there is great interest in determining its validity. Studies, primarily in more developed countries with literate populations and advanced medical systems, have demonstrated that it is a good predictor of mortality and functional ability, even after controlling for other objective health measurements (Appels, Bosma, Grabauskas, Gostautas, and Sturman, 1996; Borawski, Kinney, and Kahana, 1996; Idler and Benyamini, 1997; Idler and Kasl, 1991, 1995; Kaplan and Camacho, 1983; Mossey and Shapiro, 1982; Schoenfeld, Malmrose, Blazer, Gold, and Seeman, 1994; Sugisawa, Liang, and Liu, 1994; Wolinsky and Johnson, 1992). This predictive power may be related to its multifaceted nature, whereby SRH incorporates multiple dimensions of health (physical disability, functional or activity limitations, chronic and acute morbidity), self-assessment of severity, awareness of comorbidity, and past health trajectory (Idler and Benyamini, 1997).
SRH may not be comparable across populations (Angel and Guarnaccia, 1989; Ferraro and Kelley-Moore, 2001; Jylhä, Guralnik, Ferrucci, Jokela, and Heikkinen, 1998; Rahman, Strauss, Gertler, Ashley, and Fox, 1994; Zimmer, Natividad, Lin, and Chayovan, 2000), especially across developed and developing countries. Specifically, due to lower levels of education and formal contact with the health care system, individuals in
the developing world may have less knowledge about their own acute and chronic morbidity conditions, which may affect their subjective reports of their health. High levels of family support and lower expectations of independence of movement in developing countries may lead to a weaker relationship between physical disability or functional limitations and SRH. Efforts are under way to develop means of calibrating responses to SRH questions by giving respondents anchoring health vignettes (Salomon, Tandon, and Murray, 2004).
Inconsistent gender differences in SRH have been reported: some studies show a female disadvantage (Gijsbers van Wijk, van Vliet, Kolk, and Everaerd, 1991; Rahman et al., 1994; Zimmer et al., 2000) while others find no disadvantage (Jylhä et al., 1998; Leinonen, Heikkinen, and Jylhä, 1998; McDonough and Walters, 2001; Zimmer et al., 2000). More importantly, several studies in the developed world show gender differences in the association between SRH and mortality, with a stronger association for men (Bath, 2003; Benyamini, Blumstein, Lusky, and Modan, 2003; Deeg and Bath, 2003; Deeg and Kriegsman, 2003; Idler, 2003; Spiers, Jagger, Clarke, and Arthur, 2003). Rather than reflecting a health disadvantage for women, these studies suggest, women’s higher reports may reflect their “greater sensitivity” to health conditions.
There are relatively few studies for developing countries (Frankenberg and Jones, 2003; Rahman et al., 1994; Yu et al., 1998; Zimmer et al., 2000). In several nations in which allocation of resources is perceived to be biased in favor of men, men are less likely to report poor SRH; however, women have lower adult mortality rates. Rather than evidence of a sex difference in reporting, most studies have found that women’s higher rates of poor SRH actually reflect measurable sex differences in morbidity and disability.
In Bangladesh, women’s life expectancy only recently reached equality with men’s. Female respondents to the MHSS were 50 percent more likely to report poor SRH than men. Women also reported greater disability and morbidity on more detailed self-reports, and they were observed to have higher levels of physical dysfunction than men (Rahman and Barsky, 2003; Rahman and Liu, 2000). Rahman and Barsky found, when controls for observed disability, self-reports of disability and morbidity, and their interactions were introduced, that no sex difference in SRH remained, so that the SRH differences were not due to women’s complaining more for a given level of health as measured in other ways. Body mass index (BMI) was found to be a strong predictor of survival over a 20-year follow-up period in a study that included only women. Their BMI was measured in an ICDDR,B study in the late 1970s, and they were followed subsequently in the HDSS until they died or migrated away (Duffy and Menken, 1998; Menken, Duffy, and Kuhn, 2003). In this group, average BMI was only
18.5, and very few had a BMI greater than 25; the log-odds of survival increased linearly with BMI. No comparable information is available for men.
This analysis seeks to investigate relationships among these measures of health further, with particular emphasis on age and gender differences and to examine how well they predict mortality.
DATA AND METHODS
Setting
Matlab is a rural area about 55 km from the Dhaka, the capital of Bangladesh. ICDDR,B has long maintained a research station that sponsors the HDSS and extensive research on the health of a population of over 200,000 people. It also provides health services that supplement the government system of health care. The overwhelming majority of older individuals live with adult children (mostly sons), and alternative sources of support—financial and otherwise—outside the family are scarce. Bangladesh per capita income in 2000 was US$370/year. The predominant occupation for rural men is agriculture, with labor force participation rates remaining very high even for older men. Women are largely restricted by convention to activities in the home, with relatively little opportunity to venture outside the homestead, although these restrictions have decreased in recent years. Given the high level of poverty and the scarcity of health providers (4,671 persons/physician, 3,312 persons/hospital bed), contact with the formal health care system is thought to be relatively infrequent. National life expectancy in 2000 was 58 for both men and women; at age 50 it was approximately 30 years, again, with no significant gender differences. Approximately 10 percent of the population was over age 50 (Bangladesh Bureau of Statistics, 2002).
The 1996 Matlab Health and Socioeconomic Survey
The MHSS is a multistage, multisample household survey that collected information from 11,150 individuals age 15 and over in 4,538 households. While designed for comparability to similar nationally representative family life surveys, such as the Indonesian and Malaysian Family Life Surveys, MHSS eschewed a nationally representative sample in favor of a sample based entirely in Matlab because of the availability of the HDSS (Rahman et al., 1999). Matlab HDSS data have been used extensively in the demographic literature, and the HDSS is considered to be one of the few high-quality (i.e., complete, accurate, and up-to-date) demographic data sources in the developing world (Fauveau, 1994). In particular, age reporting is
considered to be highly accurate, a feature not found in other South Asian data sources (Menken and Phillips, 1990).
As part of a collaborative study funded by the U.S. National Institute on Aging, investigators at the Harvard School of Public Health, the University of Colorado at Boulder, ICDDR,B, and Independent University, Bangladesh, MHSS respondents were tracked through the HDSS from 1996 through 2000. The matching resulted in an event history database that identifies whether a respondent died in a particular calendar year and whether he or she was censored from the HDSS population through migration.
The technique of matching survey data to subsequent surveillance data, often employed using the Current Population Survey and death registration data in the United States, offers some advantages over a panel survey. Foremost among these is cost, since longitudinal analysis requires only matching the survey to subsequent data collected as part of an ongoing system rather than fielding a follow-up study. Furthermore, a surveillance system may date death or censoring more accurately and may be more accurate in distinguishing between these two types of exits from the sample than a periodic panel survey (which collects no information except at the survey points). Panel surveys in other developing countries typically have had attrition rates of 10 percent or more, leading to uncertainty about the cause of attrition and potential bias in assessing mortality. In addition, survey costs can rise considerably as follow-up efforts intensify (Frankenberg and Thomas, 2000). Panel surveys have the advantage of offering far more detailed data on longitudinal changes in health status, nutrition, and morbidity. However, the survey plus surveillance approach offers a crucial opportunity to study the effects of health on subsequent survival. The complementarity of these approaches is obvious. We plan a 10-year followup of the MHSS households.
Sampling
The HDSS provided the sampling frame for the MHSS (Rahman et al., 1999). The Matlab surveillance area consists of 8,640 baris or residential compounds, of which roughly one-third (31.1 percent) or 2,687 baris were randomly selected. The bari is the basic unit of social organization in rural Bangladesh and in Matlab in particular (Aziz, 1979; Rahman, 1986). Baris usually consist of a cluster of households linked in many instances in a kin network (however, about 16 percent of baris consist of only a single household and, even in multihousehold baris, kin networks may exist only for subclusters of households). Sampling baris rather than households provides a better representation of family networks, a major focus of the MHSS survey. In single-household baris, that household was selected for detailed interviews. In all other baris, two households were selected. All individuals
TABLE 10-1 Sample Exclusions
|
|
Missing |
All Indicators Present |
|
|
Individual Respondent |
|
|
|
|
|
No sampling weight |
54 |
11,096 |
|
|
No HDSS match |
165 |
10,931 |
|
Self-Reported Health Indicators |
|
|
|
|
|
SRH—general health |
0 |
10,931 |
|
|
ADL—activities of daily living |
13 |
10,918 |
|
|
Major disease |
0 |
10,918 |
|
Observed Health Indicators |
|
|
|
|
|
ADL—activities of daily living |
1,001 |
9,950 |
|
|
BMI—body mass index |
1,304 |
9,536 |
|
SOURCES: 1996 Matlab Health and Socioeconomic Survey and 1996 Health and Demographic Surveillance System. |
|||
in these households who were age 50 and over were interviewed. For those below age 50, certain criteria were followed to reduce the interviewing load vis-à-vis large households. Probability weights reflecting this multistage sampling scheme were assigned to each individual and are included in the MHSS public-use data set (Rahman et al., 1999; Rahman, Menken, Foster, and Gertler, 2001).
There were 11,150 individuals age 15 and over in the bari sample. People were eliminated from this analysis (see Table 10-1) if the individual probability weight could not be calculated (54) or the MHSS identification number was erroneous and could not be matched in the HDSS (165). Thus we begin with 10,931 respondents who could be followed in the HDSS. Individuals were dropped if information was missing on self-reported activities of daily living, the major disease index, or observed activities of daily living, or if BMI was either missing or out of range. Most nonresponses stem from the fact that there were special teams for collection of observed health indicators and for anthropometric measurement. They visited only subsets of all MHSS households. Very few respondents refused to participate. Thus for the purposes of this study, we focus on 9,536 respondents age 15 and older (4,399 men, and 5,137 women) for whom we have complete information. Rahman and Barsky (2003) found little difference between individuals who had complete information on health indicators and all respondents.
Mortality Analytic Plan
Longitudinal models of mortality subsequent to MHSS fieldwork were estimated to investigate the predictive power of the health measures. Each respondent contributed an observation for each person-year from 1996 to
2000 unless censored by death or out-migration. The logistic hazards model of mortality tested has the following form:
where µik is the risk that person i who survived to the start of follow-up year k dies in that year, Femalei is 1 if person i is female and 0 if male, Ageik is person i’s age at the start of follow-up year k, SRij is the jth of J self-reported health indicators, and OBSim is the mth of M observed health indicators for person i. The health indicators were recorded once—in the MHSS. Therefore, Age is the only time-varying variable.
Estimation of models incorporates a Huber-White correction for intracluster correlation in the distribution of the probability of mortality across observation years for a given respondent. Results presented in the tables display the relative odds associated with a variable, or the relative change in
resulting from a one-unit change in a variable.
Table 10-2 presents the number of MHSS respondents by sex and broad age group and the number of deaths recorded for each sex/age group in the
TABLE 10-2 Respondents, Deaths, Person-Years, and Death Rates
|
|
|
Respondents |
Recorded Deaths |
Percentage with Recorded Death |
Person- Years |
Percentage Dying Per Person-Year |
|
Men |
|
|
|
|
|
|
|
|
<50 |
2,861 |
26 |
0.9 |
12,697 |
0.2 |
|
|
50+ |
1,539 |
197 |
12.8 |
7,912 |
2.5 |
|
|
Total |
4,399 |
223 |
5.1 |
20,609 |
1.1 |
|
Women |
|
|
|
|
|
|
|
|
<50 |
3,765 |
18 |
0.5 |
17,136 |
0.1 |
|
|
50+ |
1,372 |
115 |
8.4 |
7,387 |
1.6 |
|
|
Total |
5,137 |
133 |
2.6 |
24,523 |
0.5 |
|
Total |
|
|
|
|
|
|
|
|
<50 |
6,626 |
44 |
0.7 |
29,833 |
0.1 |
|
|
50+ |
2,910 |
312 |
10.7 |
15,299 |
2.0 |
|
|
Total |
9,536 |
356 |
3.7 |
45,132 |
0.8 |
|
SOURCES: 1996 Matlab Health and Socioeconomic Survey; 1996-2000 Health and Demographic Surveillance System Mortality Files. |
||||||
HDSS over the subsequent 5 years. Deaths of 10.7 percent of those over age 50 in the MHSS were recorded in the HDSS within the follow-up period, compared with only 0.7 percent of those under age 50 and 3.7 percent overall. These figures, however, do not adjust for out-migration (censoring). Among those over 50 in the MHSS, only 3.2 percent out-migrated during the follow-up period, compared with 15.1 percent of those under age 50 and 11.5 percent of all respondents (not shown). Out-migrants were censored at the end of the last full year of their observation. Those who died contributed a person-year for each year in which they were alive at the start. Those for whom neither death nor out-migration was recorded in the HDSS in the follow-up period each contributed 5 person-years of observation. The number of person-years of observation in which age was under 50, over 50, and all ages at the start of the year is given in Table 10-2 along with the yearly death rates (deaths/person-years). This death rate was 0.8 percent for all ages. While there was a relatively high rate in the older group (2.0 percent), death was a quite rare event in the younger subsample (0.1 percent). For this reason, all mortality analyses were replicated using the Rare Events Logistic Regression package for STATA (King, 2004). In all cases, rare event models resulted in higher coefficient estimates and lower standard errors, so we choose to report the more conservative logistic regression results in our later tables. Table 10-2 also shows lower mortality rates for women than for men; however, as is shown later, with more precise controls for age, sex differences are not significant.
Health Indicators
The five health indicators are defined below. The self-reported and observed activities of daily living (ADL) scores and self-reported indicator of major disease were originally developed by Rahman and Barsky (2003).
SRH was assessed with the simple question “What is your current health status?” Less than 30 seconds were required to administer this question. Responses were healthy, fairly healthy, or in poor health. SRH was coded as 1 if the respondent reported he or she was in poor health, and as 0 for those who reported they were healthy or fairly healthy The latter responses were combined because we were most concerned with poor health. It is important to note, however, that a different coding scheme (i.e., poor or fair versus good health) could affect the results.
Following Merrill, Seeman, Kasl, and Berkman (1997), Rahman and Liu (2000), and Rahman and Barsky (2003), we constructed a series of measures for functional limitations in self-reported ADLs. We used self-report information on 10 ADL items, which were divided into two clusters: (I) limitations in personal care—four items—ability to (a) bathe, (b) dress, (c) get up and out of bed, and (d) use the toilet, and (II) limitations in range
of motion—six items—ability to (a) carry a 10 kg weight for 20 yards, (b) use a hand-pump to draw water, (c) stand up from a squatting position on the floor, (d) sit in a squatting position on the floor, (e) get up from a sitting position on a chair or stool without help, and (f) crouch or stoop. Collecting the entire battery of questions required about 5 minutes of interview time.
Because men and women appear to have different norms regarding personal care, in this paper we consider only the second cluster of six range-of-motion questions. Each of the six components of range of motion was scored as 0 (can easily do all the activities in the cluster) or 1 (have trouble with one or more activities in the cluster, resulting in an self-reported ADL score ranging from 0 (no limitation) to 6.
Self-reported chronic morbidity (Rahman et al., 1999), to which we refer as major disease, was assessed with a checklist of 14 sentinel conditions (anemia, arthritis, broken bones, cataracts, vision problems, asthma, other breathing difficulty, diabetes, pain or burning on urination, paralysis, tuberculosis, gastric/ulcer problems, edema, and a residual category called other conditions). For each condition, respondents were asked to report whether they had experienced it in the three months prior to the survey, and if so whether it had caused them no difficulty, some difficulty, a great deal of difficulty, or inability to carry out their day-to-day activities. Collection of the full battery of morbidity questions required about 6 minutes of interview time. Those who had experienced one or more of the sentinel conditions that had caused a great deal of difficulty/inability to carry out their day-to-day activities were scored as 1, while those who had none of the sentinel conditions or who experienced only minor chronic disease were scored as 0.
Physical disability was assessed objectively as in prior studies (Merrill et al., 1997; Rahman and Liu, 2000; Rahman and Barsky, 2003) by asking respondents to perform four timed physical tasks: maintaining side by side, semi-tandem and tandem positions (balance); walking 8 feet twice (gait); chair-rises (lower extremity movement); and shoulder rotation (upper extremity movement). Collection of these measures required about 10 minutes of data collection team time, as well as moderately higher equipment and training costs. Each task had a three-level score: 2 (unable to do the activity), 1 (had some difficulty doing the activity), and 0 (could do the activity easily), assigned by an independent observer. The four individual subscales were added to form a scale ranging in value from 0 to 8, with lower scores indicating better performance and 0 indicating the person could perform all activities easily. When this measure was dichotomized, those with scores of 3 or above were considered in poor health.
Height and weight were measured and BMI calculated as (weight in kg)/(height in meters)2. Collection of these measures required 5 minutes of
data collection team time, as well as extra costs for measurement tools and training of specific enumerators to operate scales and measuring sticks. Those with a BMI less than 16 were considered to be severely malnourished and scored as 1, while those with a BMI of 16 or above were scored as 0.
It is worth noting that for self-reported major disease, the summary measure is comprised of heterogeneous categories of symptoms and disease labels that reflect the prevailing morbid conditions in rural Bangladesh. As such they are locally specific, and cross-country comparisons using these summary measures would be difficult to interpret.
RESULTS
Figures 10-1 and 10-2 present, by age group and sex, the percentage estimated by self-reported and observed indicators respectively to be in poor health. Poor health increases with age and the rise begins early in adulthood. In this society, the slowest rise with age is in observed severe malnutrition. There are striking sex differences in poor health according to nearly
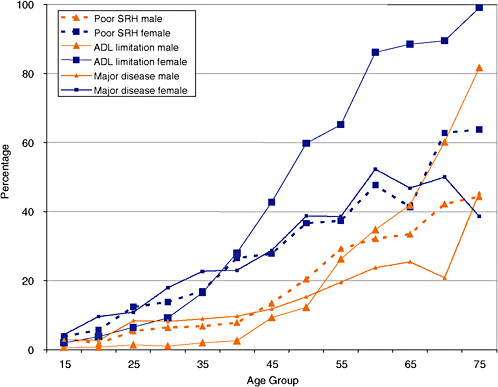
FIGURE 10-1 Self-reported health indicators, by age and sex.
SRH = self-reported health; ADL = activities of daily living.
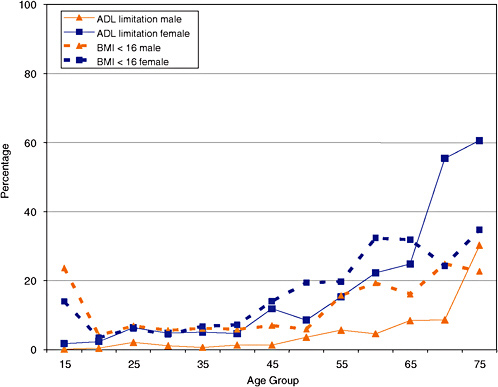
FIGURE 10-2 Observed health measures, by age and sex.
ADL = activities of daily living; BMI = body mass index.
all measures and especially at older ages. At age 40, over 20 percent of women self-reported poor health, no matter how measured, while the corresponding figures for men are about 10 percent. Until about age 40, there was little difference in the proportion severely malnourished, but after that age, women disproportionately were underweight for their height.
Extent to Which the Various Health Indicators Are Interrelated
Bivariate and multiple correlations (when each indicator is estimated from the other four) are shown in Table 10-3. Clearly, while these indicators are related, none is very closely determined by the others. These results are confirmed in a principal component analysis (not shown). In that analysis, the first component, which accounts for close to 50 percent of the variation, shows approximately equal weightings from all five indicators. Yet it is not until four factors are included that the variation accounted for reaches 89 percent. Thus, while the indicators are interrelated, each has a sizeable component unrelated to the others.
TABLE 10-3 Interrelationships Between Health Measures: 1996 Matlab Health and Socioeconomic Survey
TABLE 10-4 Subsequent Mortality by Health Status
Mortality in the Five Years Subsequent to the MHSS in Relation to the Health Indicators
Health status, as measured by each of the five indicators treated dichotomously, is substantially related to subsequent mortality (Table 10-4). Of those who self-reported poor health, 10.2 percent died versus 1.9 percent of those who self-reported good or fair health. ADL scores, whether self-reported or observed, showed greater differentials in outcome by health status, while major disease and BMI indicators differentiated risk of dying less well. Figure 10-3 works backward from survival outcome. It provides evidence that those who died, compared with those who survived the five-year follow-up period, were much more likely to have been in poor health at the time of the MHSS. Using SRH, 53 percent of those who died had said they were in poor health, compared with only 16 percent of those who survived. For reported ADL limitations, 72 percent of those who died had reported some limitation, compared with 19 percent of those who lived. For observed ADL limitations, less common overall, 31 percent of those who died had been observed to be mobility-impaired, compared with only 5 percent of those who survived. The greatest difference clearly was in the reported ADL measure.1
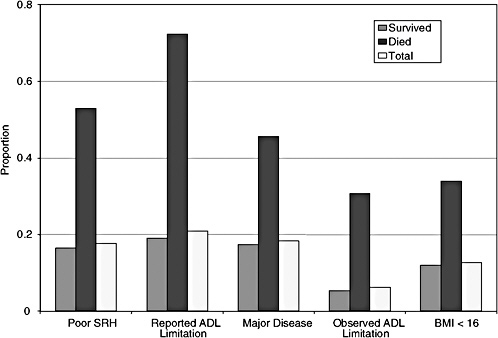
FIGURE 10-3 Health status indicators by subsequent survival. SRH = self-reported health; ADL = activities of daily living; BMI = body mass index.
Figure 10-4 demonstrates the predictive power of the ADL scores— which characterize people along a continuum rather than a simple dichotomy. The likelihood of dying over the 5-year follow-up period shows a generally monotonic increase with ADL score, whether self-reported or observed. Furthermore, the two measures appear to capture slightly different mortality trajectories. Self-reported ADL shows a greater increase in mortality as it moves from representing people who can do all tasks easily (score = 0) to those who score difficulty with only one or two. It may be that individuals recognize the level or change in level more acutely than can be picked up on the kinds of measures that went into the observed ADL score. Observed ADL scores may capture extreme levels of poor health better: respondents who scored five or more experienced a subsequent mortality risk that approached 30 percent.
Multivariate Models
We turn to multivariate models of mortality to address several questions. First, which indicator adds greatest explanatory power when age and sex are taken into account? Second, does the predictive power of these health measures differ for older and younger adults? Initial models predicting the
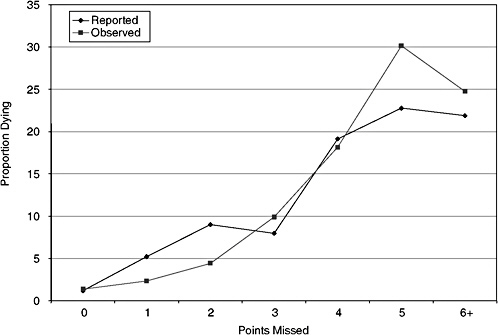
FIGURE 10-4 Proportion dying by self-reported and observed ADL scores.
odds of dying are shown in Table 10-5 for the total sample of person-years, person-years for which the individual was under 50 at the start of the year, and person-years for which the individual was 50 or over at the start. The first line reports on the model in which age is the only predictor. The pseudo-R2 is .18 for total person-years. Interestingly, age is not a significant predictor of mortality in adults under 50. Adding sex does not significantly improve the predictive power of the model, as shown in line 2. Therefore, once age-in-years is in the model, no sex difference is detected. The remaining lines show the improvement in pseudo-R2 when a single health indicator is added. For total person-years, SRH adds .01 to the pseudo-R2 and those with poor SRH have odds of dying 2.28 times the odds of those of the same age and sex who do not report poor SRH. In all three models, poor SRH is significantly associated with increased subsequent mortality. A much larger coefficient is estimated for the young subsample of person-years, in which there is a low baseline level of mortality. The yearly probability of dying for this subsample is 0.12 percent (Table 10-2). Poor SRH in the young group (OR = 5.6), when age and sex are held constant at their means, raises the probability of death from 7 to 41 in 10,000. This is a large effect, especially considering that it results from a single question. For the over-50 subsample, the effect of poor SRH is smaller but highly significant (OR =
TABLE 10-5 Logistic Regression Models of Mortality Adding Age, Sex, and One Health Measure
|
|
|
All |
Age <50 |
Age 50+ |
|||
|
Pseudo-R2 Gain |
Odds Ratioa |
Pseudo-R2 Gain |
Odds Ratioa |
Pseudo-R2 Gain |
Odds Ratioa |
||
|
Age |
0.179b |
1.09*** |
0.001b |
0.99 |
0.092b |
1.11*** |
|
|
Female |
0.001 |
0.80 |
0.001 |
0.99 |
0.001 |
0.09 |
|
|
Adding a single health indicator to model with age and sex |
|||||||
|
Self-Reported |
|
|
|
|
|
|
|
|
|
SRH |
0.012 |
2.28*** |
0.028 |
5.57* |
0.012 |
2.08*** |
|
|
ADL score |
0.024 |
0.76*** |
0.048 |
.51*** |
0.023 |
0.79*** |
|
|
Major disease |
0.006 |
1.82** |
0.028 |
5.45* |
0.006 |
1.64** |
|
Observed |
|
|
|
|
|
|
|
|
|
ADL score |
0.014 |
0.78*** |
0.001 |
1.17 |
0.020 |
0.78*** |
|
|
BMI < 16 |
0.010 |
2.28*** |
0.017 |
3.63 |
0.010 |
2.00*** |
|
Observations |
45,098 |
|
29,807 |
|
15,291 |
|
|
|
NOTE: Calculations treat all observations for an individual as a cluster and use individual sample weights. SRH = self-reported health; ADL = activities of daily living; BMI = body mass index. aThe odds ratio for female is from the model with age and sex; those for the health indicators are from models with age and sex plus that indicator as predictors. bThis figure is the pseudo-R2 for the model with age as the single predictor. * p<.05; ** p<.01; *** p<.001. |
|||||||
2.1) and the probability of death, again estimated at the means of age and sex, rises from 1 to 2 percent. While each indicator is significant in the total and age 50 and over models, only the self-reports—whether of general health or ADLs or major disease—add predictive power for younger people.
Stepwise regressions were carried out (Table 10-6) in which age and sex were entered first and then health indicators entered in the order of the magnitude of their additional predictive power. For total person-years and the over-50 subsample, observed ADLs entered first, followed by self-reported ADLs, BMI, and SRH. The index of major disease did not enter at all. For the under-50 subsample, only self-reported ADLs served to predict mortality, whereas for those over 50, all indicators except major disease increased the fit to the data.
Finally, the complete models, in which age, sex, and the four indicators that were significant in any of the Table 10-6 models are included, are shown in Table 10-7. For the total person-years and over-50 models, mortality increases significantly with age, with each additional year associated with a 6-7 percent increase in the odds of dying. Controlling for age and health, the odds of dying for a woman in the same samples are less than half (.44-.46) those of a man. The sizable advantage in mortality controlling for health that women have is substantial enough that, despite having substantially worse health on all observed and self-reported health indicators, their mortality (adjusted only for age and shown in Table 10-4) was not significantly different from men’s.
This disjunction between sex differences in health and mortality introduces the possibility that, as in other studies, women may overreport poor health and greater disability. If this were the case, the inclusion of interactions between sex and each of the significant health measures included in Table 10-7 would show significant negative interactions between health measures and the female main effect, indicating that the health measure was a worse predictor of health for women. Yet when sex−health measure interactions were entered, either individually or as a group, none approached statistical significance (models not shown, see Kuhn, Rahman, and Menken, 2004).
The absence of any significant interactions between the respondent’s sex and the predictive power of SRH measures is an extremely robust finding. The effects do not even approach significance, and these results do not change when nonsignificant interaction terms for sex and observed health measures are dropped (models not shown). Women’s adjusted risk of mortality, controlling for other factors, is much lower than men’s. Women’s low baseline mortality risks are multiplied by risks due to poor health, which are more common among women; the result is overall equality in mortality of men and women. The process is not driven by a less substantial relationship between women’s poor health and women’s survival, but by the fact
TABLE 10-6 Stepwise Logistic Regression Models of Mortality Adding Health Measures to Age and Sex
|
By Entry Order |
All |
Age <50 |
Age 50+ |
|||
|
Pseudo-R2 Gain |
Odds Ratio |
Pseudo-R2 Gain |
Odds Ratio |
Pseudo-R2 Gain |
Odds Ratio |
|
|
Observed ADL Score |
0.014 |
1.28*** |
— |
— |
0.020 |
1.29*** |
|
Reported ADL Score |
0.017 |
1.26*** |
0.048 |
1.94*** |
0.015 |
1.21*** |
|
BMI < 16 |
0.006 |
1.91*** |
— |
— |
0.006 |
1.72** |
|
SRH |
0.003 |
1.51* |
— |
— |
0.002 |
1.42* |
|
Major Disease |
— |
— |
— |
— |
— |
— |
|
Final Pseudo-R2 |
0.220 |
|
0.050 |
|
0.135 |
|
|
Observations |
45,098 |
|
29,807 |
|
15,291 |
|
|
NOTE: The gain and odds ratio come from the model in which the indicator first entered (see note to Table 10-4). SRH = self-reported health; ADL = activities of daily living; BMI = body mass index. * p<.05; ** p<.01; *** p<.001. |
||||||
TABLE 10-7 Logistic Regression Model of Mortality with Age, Sex, and Health Measures as Predictors
|
|
All |
|
Age <50 |
|
Age 50+ |
|
|
|
Odds Ratio |
S.E. |
Odds Ratio |
S.E. |
Odds Ratio |
S.E. |
||
|
Age |
1.06*** |
0.01 |
0.97 |
0.04 |
1.07*** |
0.01 |
|
|
Female |
0.44*** |
0.07 |
0.62 |
0.34 |
0.46*** |
0.08 |
|
|
Self-Reported |
|
|
|
|
|
|
|
|
|
SRH |
1.51* |
0.28 |
3.00* |
1.64 |
1.42* |
0.25 |
|
|
ADL score |
1.21*** |
0.04 |
1.83*** |
0.08 |
1.17*** |
0.04 |
|
Observed |
|
|
|
|
|
|
|
|
|
ADL score |
1.18*** |
0.04 |
1.47 |
0.60 |
1.21*** |
0.03 |
|
|
BMI < 16 |
1.81** |
0.33 |
2.46 |
1.39 |
1.65** |
0.28 |
|
Observations |
45,098 |
|
29,807 |
|
15,291 |
|
|
|
Pseudo-R2 |
0.220 |
|
0.084 |
|
0.135 |
|
|
|
NOTE: Major disease is excluded because it was not significant in any model. SRH = self-reported health; ADL = activities of daily living; BMI = body mass index. * p<.05; ** p<.01; *** p<.001. |
|||||||
that the same poor health multiplier effect is applied to a lower baseline mortality effect. This result holds in rare events logistic regression models and probit regression models, both of which also apply the very realistic assumption that mortality risks are multiplicative in nature, not additive. These models were also run using a linear probability model in order to estimate the size of interaction effects if mortality risks were indeed additive. Interactions between sex and SRH were found to be highly nonsignificant in these models as well.
Discussion
This analysis demonstrates both the multidimensional nature of the relatively simple and low-cost health measures in the MHSS and their substantial value and validity in a low-income setting such as Bangladesh. We believe this is the only study to examine subsequent mortality in relation to these multiple measures of health. Each measure is a significant predictor of subsequent mortality, particularly for elders. With the exception of major disease, each appears to capture, at least in part, a different dimension of health from the others. These findings support the notion that individuals can effectively assess their own health status even in settings of poor education and low levels of interaction with modern health systems.
Furthermore, the measures seem equally appropriate for men and women. The higher age-specific prevalence of poor health, whether reported
or observed, among women does not appear to result from their overreporting poor health compared with men. The proportional increase of mortality for those whose health was poor versus not poor, whichever the health measure used, did not differ for women and men. At the same level of health, women had lower mortality risks than men; however, these lower risks were combined with much higher rates of poor health. These differences countered one another; as a result, we found no sex differences in overall age-adjusted mortality.
Objective health measures are frequently assumed to be superior to self-reports because they minimize concerns over reporting bias and international comparability. We find, however, that they are not necessarily better predictors of mortality. The self-reported and observed measures were similar in predicting mortality at older ages, while self-reports were the only significant predictors of mortality at younger ages.
The marginal time and financial costs of collecting each measure vary substantially. Cost estimates based on the MHSS are given in Table 10-8, along with the improvement in mortality prediction found when each health measure was added to the model based on age and sex (repeated from Table 10-5). For comparison, we consider the high expected costs of drawing and analyzing a blood sample. For the second round of the MHSS, we have proposed a battery of seven biomarker analyses.2 The estimated costs are included in Table 10-8. Self-reported measures take less survey time than observational tests or drawing a blood sample and incur no additional capital costs; in addition, they can be collected by less skilled interviewers. The observed indicators cost at least 2.5 times more to collect than the self-reports. The current cost of collecting biomarkers is extremely high, but is likely to decrease in the future for two reasons. First, as collection is standardized, less expensive technology may be developed. Second, with continuing research, a small set of essential indicators is likely to be agreed upon.
These results raise questions regarding a minimal set of survey-based health measures that ensures precision and accordance with international standards. The least expensive measure, a single SRH question requiring $0.01 per respondent, adds significantly in predicting subsequent mortality for respondents of all ages. In fact, it predicts mortality better than a number of more complex health indicators.
TABLE 10-8 Cost of Health Measures and Increase in Pseudo-R2
|
|
Marginal Cost ($) |
Increase in Pseudo-R2(%) |
||||||
|
Time |
Labor |
Capital |
Total |
All |
Under 50 |
Age 50+ |
||
|
Self-Reported |
|
|
|
|
|
|
|
|
|
|
SRH |
0:20 |
0.01 |
0 |
0.01 |
1.2 |
2.8 |
1.2 |
|
|
ADLs |
4:40 |
0.12 |
0 |
0.12 |
2.4 |
4.8 |
2.3 |
|
|
Major disease |
6:00 |
0.16 |
0 |
0.16 |
0.6 |
2.8 |
0.6 |
|
Observed |
|
|
|
|
|
|
|
|
|
|
ADLs |
10:00 |
0.50 |
0.05 |
0.55 |
1.4 |
0.1 |
2.0 |
|
|
Body mass index |
5:00 |
0.30 |
0.10 |
0.40 |
1.0 |
1.7 |
1.0 |
|
|
Blood-drawn biomarkers |
20:00 |
22.00 |
38.00 |
60.00 |
− |
− |
− |
|
NOTE: Taken from Table 10-5; change when each health measure is added to model with age and sex. SRH = self-reported health; AD L = activities of daily living; BMI = body mass index. |
||||||||
The self-reported ADL index, the next least expensive indicator to collect, adds even more to the predictive power of our models. This indicator seems to work at least as well, and possibly better, than observed ADLs and anthropometric measures that are far more demanding of resources. However, as for SRH, it is important to ask whether self-reported ADLs produce results that are truly comparable across different populations and subgroups within populations. The results here indicate they are promising enough to be included in studies in other countries in order to assess their usefulness.
The detailed questions on specific conditions that went into the major disease index were far more complicated to implement than the ADL questions and the index added no explanatory power to the analysis of mortality. It may be that the questions on specific conditions are better predictors than the overall index; we plan to address this issue in further analyses of the MHSS.
The observed ADL index and BMI add significantly in predicting mortality for elders. They are not significant for those under 50. It may be that the activities that go into the MHSS ADL index are not sufficiently difficult to detect disabilities that contribute to higher short-term mortality risk in younger adults. Neither the observed ADL index nor BMI picks up the increase in poor health with age for those under 50, especially for females, that is self-reported. In contrast, SRH and the self-reported ADL index increase with age and are significant mortality predictors, perhaps because younger adults recognize change in their own abilities or differences in comparison with peers even when their disabilities do not put them in a range considered unusual by the observer. We suspect that, unless the set of tasks is changed to detect more subtle disability, observed ADL measures for younger adults should be included in survey data collection only as a baseline for longitudinal follow-up rather than as valid health indicators.
The four measures discussed here—SRH, self-reported and observed ADLs, and BMI—are strong predictors of survival over the next 5 years in the rural Bangladesh context, although the observed measures work best for elders. They are therefore good markers of general health and the effects of the health system and can be used to examine basic gender and socioeconomic differentials in that society. The high prevalence of poor health based on the self-reports, even at low ages, in Bangladesh makes these measures perhaps even more valuable than they would be in more advanced societies. More importantly, compared with complex measures such as biomarkers or disability adjusted life years, these measures can be obtained more frequently and in much larger samples for the same cost. If resources are especially constrained, it may be possible to restrict the set of measures collected further and still be able to capture levels, differentials, and trends in overall health over time.
Given the urgent need to assess health and track its trends over time in
sub-Saharan Africa, we strongly recommend including a range of health indicators in data collection—in a way that permits research on indicators in this region. Studies are needed that collect, in selected settings, simple and low-cost health indicators like those examined in this paper; expanded versions of these indicators (e.g., SRH with more categories); other objective measures (e.g., lung capacity, grip strength) that are more costly in terms of survey-team time, equipment, and training; and selected biomarkers that are far more expensive to collect and more difficult to analyze. It would also be appropriate to address issues of comparability of measures across population through techniques such as calibrating vignettes. Simultaneous collection—in a few selected studies—of all of these indicators in comparable manner will permit the kind of “head-to-head” analysis performed here for one country and for the measures included in the MHSS. This research would be most informative if carried out where it is possible to follow respondents for some period of time to observe survival outcomes.
The expected outcomes of this research include
-
Identification of measures that provide valid information on prevalence of specific conditions or diseases and those which provide information on overall health.
-
Estimates of costs and difficulties of collecting each indicator.
-
Cost-benefit analyses, which would help investigators decide on the package of indicators to be included in future data collection.
One obvious locus for this type of research is the INDEPTH network. Its Demographic Surveillance System sites offer crucial advantages. Since the sites carry out continuous longitudinal follow-up of large populations, they provide data on mortality trends prior to collection of the health measures. While few sites have been operating as long as the Matlab HDSS (which is a member of INDEPTH), a number, such as Agincourt in South Africa and Navrongo in Ghana, have been operating for at least 10 years. A set of health indicators measured in a one-time survey would contribute to the assessment of measures described in this paper. INDEPTH sites routinely collect the follow-up data needed to study relationships of health measures to subsequent mortality. In addition, if these measures were included periodically in subsequent DSS rounds, their sensitivity to trends and emerging differentials in health could be assessed.
The issue of comparability between populations could be addressed in two ways—for which DSS sites are again especially appropriate. Following the work on vignettes (see Salomon et al., 2004), calibrating vignettes could be included in at least one DSS round that includes health indicators. These vignettes could be extended to include ADLs as well as other aspects of health for which self-reports are collected. In addition, mortality prediction
across sites could be analyzed to determine if, as for men and women in Bangladesh, the increase in the odds of mortality for those in poor health as measured by a specific indicator is the same across countries.
Development of low-cost and informative health status modules could be guided by this research. They could be regularly included in DSS data collection rounds, providing valuable comparable information across sites on health levels and trends over time. These modules could also be included in standalone surveys covering larger geographic areas. Nationally representative surveys could then provide the basis for comparative studies of countries, with data from INDEPTH sites providing greater detail and longitudinal validation.
In addition to tracking changes in health over time in defined populations, DSS sites have demonstrated they are ideal settings for conducting and evaluating health and social interventions intended to improve health either directly (e.g., family planning programs, oral rehydration programs) or indirectly (education of women, micro-credit programs). They offer well-established sampling frames with regular follow-up so that program and control groups can be established and compared over time. Increasingly, programs include direct adult health interventions, such as Agincourt’s South African Stroke Prevention Initiative. Regular observation of simple health measures can provide a baseline for assessing differences between experimental and control groups, and follow-up information for assessing the long-term impact of interventions on comparable health status measures. At the same time, repeated observation of health status allows researchers in DSS sites to measure the health impact of programs not aimed directly at health, including education, family planning, and women’s status interventions. Finally, such measures facilitate analysis of the health effects of unexpected economic or political crises and other changing social or health patterns.
As societies in sub-Saharan Africa grow older and continue to absorb the consequences of the HIV/AIDS epidemic, it will grow increasingly important to assess their health and health needs on a regular basis and to evaluate the impact of intervention programs. For these reasons, further research on the promising set of simple indicators evaluated here for one developing country setting and on the more detailed and expensive measures discussed here is an essential part of a research agenda on aging in Africa.
ACKNOWLEDGMENTS
This work was supported by NIA grants R01 AG16308, R03 AG19294-01, P30 AG17248, and P01 AG11952-05 to Harvard University and the University of Colorado. The research is based on collaboration
among investigators at ICDDR,B: International Centre for Health and Population Research, Harvard University, Brown University, University of Colorado, Independent University, Bangladesh, and RAND. As always, we thank the people of Matlab, Bangladesh, for their commitment to research and participation in the Matlab Health and Socioeconomic Survey and the ICDDR,B Health and Demographic Surveillance System.
REFERENCES
Angel, R., and Guarnaccia, P. (1989). Mind body and culture: Somatization among Hispanics. Social Science and Medicine, 28, 1229-1238.
Appels, A., Bosma, H., Grabauskas, V., Gostautas, A., and Sturmans, F. (1996). Self-rated health and mortality in a Lithuanian and a Dutch population. Social Science and Medicine, 42, 681-690.
Aziz, K.M.A. (1979). Kinship in Bangladesh. Dhaka, Bangladesh: International Centre for Diarrhoeal Disease Research.
Bangladesh Bureau of Statistics. (2002, January). Statistical pocketbook of Bangladesh, 2000. Dhaka: Statistics Division, Ministry of Planning, Government of the People’s Republic of Bangladesh.
Bath, P.A. (2003). Differences between older men and women in the self-rated health-mortality relationship. Gerontologist, 43, 387-395.
Benyamini, Y., Blumstein, T., Lusky, A., and Modan, B. (2003). Gender differences in the self-rated health-mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist, 43, 396-405.
Borawski, E.A., Kinney, J.M., and Kahana, E. (1996). The meaning of older adults’ health appraisals: Congruence with health status and determinants of mortality. Journals of Gerontology Series: Psychological Sciences and Social Sciences, 51, S157-S170.
Deeg, D.J.H., and Bath, P.A. (2003). Self-rated health, gender, and mortality in older persons: Introduction to a special section. Gerontologist, 43, 369-371.
Deeg, D.J.H., and Kriegsman, D.M.W. (2003). Concepts of self-rated health: Specifying the gender difference in mortality risk. Gerontologist, 43, 376-386.
Duffy, L., and Menken, J. (1998). Health, fertility, and socioeconomic status as predictors of survival and later health of women: A 20-year prospective study in rural Bangladesh. (Working Paper No. WP-98-11). Population Program, Institute of Behavioral Science, University of Colorado at Boulder.
Fauveau, V. (1994). Matlab: Women, children and health. Dhaka, Bangladesh: International Centre for Health and Population Research.
Ferraro, K.F., and Kelley-Moore, J.A. (2001). Self-rated health and mortality among black and white adults: Examining the dynamic evaluation thesis. Journal of Gerontology Series B: Psychological Sciences and Social Sciences, 56, S195-S205.
Frankenberg, E., and Jones, N. (2003). Self-rated health and mortality: Does the relationship extend to a low-income setting? Minneapolis, MN: Population Association of America.
Frankenberg, E., and Thomas, D. (2000). The Indonesia family life survey (IFLS): Study design and results from waves 1 and 2. Santa Monica, CA: RAND.
Gijsbers van Wijk, C.M., van Vliet, K.P., Kolk, A.M., and Everaerd, W.T. (1991). Symptom sensitivity and sex differences in physical morbidity: A review of health surveys in the United States and the Netherlands. Women Health, 17, 91-124.
Idler, E.L. (2003). Discussion: Gender differences in self-rated health, in mortality, and in the relationship between the two. Gerontologist, 43, 372-375.
Idler, E.L., and Benyamini, Y. (1997). Self-rated health and mortality: A review of 20-seven community studies. Journal of Health and Social Behavior, 38, 21-37.
Idler, E.L., and Kasl, S.V. (1991). Health perceptions and survival: Do global evaluations of health status really predict mortality? Journal of Gerontology, 46, S55-S65.
Idler, E.L., and Kasl, S.V. (1995). Self-ratings of health: Do they also predict changes in functional ability? Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 50, S344-S353.
Jylhä, M., Guralnik, J.M., Ferrucci, L., Jokela, J., and Heikkinen, E. (1998). Is self-rated health comparable across cultures and genders? Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 53, S144-S152.
Kaplan, G.A., and Camacho, T. (1983). Perceived health and mortality: A nine-year follow-up of the human population laboratory cohort. American Journal of Epidemiology, 117, 292-304.
King, G. (2004). ReLogit: Rare events logistic regression for STATA (version 1.1, 10/29/99). Available: -http://gking.harvard.edu/stats.shtml [accessed March 2005].
Kuhn, R., Rahman, O., and Menken, J. (2004). Relating self-reported and objective health indicators to adult mortality in Bangladesh. Paper presented at the 2004 annual meeting, Population Association of America, Population Aging Center, Institute of Behavioral Science, University of Colorado at Boulder.
Leinonen, R., Heikkinen, E., and Jylhä, M. (1998). Self-rated health and self-assessed change in health in elderly men and women: A five-year longitudinal study. Social Science and Medicine, 46, 591-597.
McDonough, P., and Walters, V. (2001). Gender and health: Reassessing patterns and explanations. Social Science and Medicine, 52, 547-559.
Menken, J., and Phillips, J.F. (1990). Population change in a rural area of Bangladesh, 1967-87. Annals of the American Academy of Political and Social Science, 510, 87-101.
Menken, J., Duffy, L., and Kuhn, R. (2003). Childbearing and women’s survival in rural Bangladesh. Population and Development Review, 29(3), 405-426.
Merrill, S.S., Seeman, T.E., Kasl, S.V., and Berkman, L.F. (1997). Gender differences in the comparison of self-reported disability and performance measures. Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 52, M19-M26.
Mossey, J.M., and Shapiro, E. (1982). Self-rated health: A predictor of mortality among the elderly. American Journal of Public Health, 2, 800-808.
Rahman, M. (1986). Tradition, development, and the individual: A study of conflicts and supports to family planning in rural Bangladesh. Asian Population Change Series No. 1. P. Kane and L. Ruzicka (Eds.). Department of Demography, Australian National University, Canberra.
Rahman, M.O., and Barsky, A.J. (2003). Self-reported health among older Bangladeshis: How good a health indicator is it? The Gerontologist, 43, 856-863.
Rahman, M.O., and Liu, J. (2000). Gender differences in functioning for older adults in rural Bangladesh: The impact of differential reporting. Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 55, M28-M33.
Rahman, M.O., Strauss, J., Gertler, P., Ashley, D., and Fox, K. (1994). Gender differences in adult health: An international comparison. The Gerontologist, 34, 463-469.
Rahman, M.O., Menken, J., Foster, A., Peterson, C., Khan, M.N., Kuhn R., and Gertler, P. (1999). The Matlab health and socioeconomic survey: Overview and user’s guide. (DRU-2018/1). Santa Monica, CA: RAND.
Rahman, O., Menken, J., Foster, A., and Gertler, P. (2001). Matlab (Bangladesh) health and socioeconomic survey. Available: http://webapp.icpsr.umich.edu/cocoon/ICPSR-STUDY/02705.xml [accessed May 13, 2005].
Salomon, J.A., Tandon, A., and Murray, C.J.L. (2004, January). Comparability of self-rated health: Cross-sectional multicountry survey using anchoring vignettes. British Medical Journal, doi:10.1136/bmj.37963.691632.44.
Schoenfeld, D.E., Malmrose, L.C., Blazer, D.G., Gold, D.T., and Seeman, T.E. (1994). Self-rated health and mortality in the high functioning elderly: A closer look at healthy individuals. (MacArthur Field Study of Successful Aging). Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 49, M109-M115.
Spiers, N., Jagger, C., Clarke, M., and Arthur, A. (2003). Are gender differences in the relationship between self-rated health and mortality enduring? Results from three birth cohorts in Melton Mowbray, United Kingdom. Gerontologist, 43, 406-411.
Sugisawa, H., Liang, J., and Liu, X. (1994). Social networks, social support, and mortality among older people in Japan. Journal of Gerontology, 49, S3-S13.
Wolinsky, F.D., and Johnson, R.J. (1992). Perceived health status and mortality among older men and women. Journal of Gerontology, 47, S304-S312.
Yu, E.S.H., Kean, Y.M., Slymen, D.J., Liu, W.T., Zhang, M., and Katzman, R. (1998). Self-perceived health and 5-year mortality risks among the elderly in Shanghai, China. American Journal of Epidemiology, 147, 880-890.
Zimmer, Z., Natividad, J., Lin, H., and Chayovan, N. (2000). A cross-national examination of the determinants of self-assessed health. Journal of Health and Social Behavior, 41, 465-481.





























