3
Diverse Populations
The obesity epidemic is occurring among boys and girls throughout the United States, among younger children and adolescents, across all socioeconomic groups and among all racial/ethnic subpopulations. However, in several racial/ethnic groups, in low-income populations, and among recent immigrants to the United States, the rates of obesity among children and youth are alarmingly high or are increasing faster than average. The children and youth who are at the highest risk for obesity often experience other social, economic, and health disparities concurrently and do not live in environments that inherently support health-promoting behaviors. In addition, although some of the risk factors for obesity are relatively ubiquitous in settings where American children and youth spend their time (e.g., communities, schools, shopping malls, retail stores, and home), epidemiologic evidence shows that African-American, Hispanic/ Latino, American Indian/Alaska Native, and Pacific Islander populations and children experiencing poverty are more likely to live in environments with inadequate support for health-promoting behaviors. Assessing the impact of these different environments presents an enormous challenge for tracking progress against obesity in diverse populations. On the other hand, the diversity of the U.S. population and the variation in patterns of obesity-related risks also provide opportunities to expand our understanding of how trends, patterns, and risk factors manifest in certain environments and to identify the types of interventions that are likely to be effective when they are tailored specifically to build on a population’s characteristics, perspectives, and social and cultural assets.
Much remains to be learned about the role of race/ethnicity, socioeconomic status (SES), and regional disparities in childhood obesity to build an evidence base that will support the most effective strategies and promising practices. Progress in preventing childhood obesity should include an examination of efforts to define and address the contexts and mechanisms that lead to and perpetuate childhood obesity in environments with excessive risks. Several recommendations in the Health in the Balance report (IOM, 2005) emphasized the need for prominent government leadership and community collaboration to develop and promote programs and policies that will collectively encourage healthful eating patterns and physical activity behaviors, particularly for young populations at the highest risk for obesity and related chronic diseases.
Helping at-risk children and youth balance their energy intakes and their energy expenditures requires an understanding of the complex and interacting influences of the social, economic, and built environments and the adverse environmental conditions that low-income and racially/ethnically diverse populations encounter as they regularly attempt to obtain affordable foods, beverages, and meals that contribute to a healthful diet and find opportunities to engage in recreational play and physical activity (Day, 2006; Glanz et al., 2005; Goodman, 2003; Gordon-Larsen et al., 2006; IOM, 2005; Jetter and Cassady, 2005; Powell et al., 2004). A multifaceted approach to address obesity and related health considerations is relevant to children and youth overall but leads to different perspectives on the appropriate solutions for specific populations, depending on their historical and sociopolitical contexts and the timing and rate of relevant economic and lifestyle transitions (Kumanyika, 1994; Kumanyika and Golden, 1991).
Because the focus of this report is on evaluation, this chapter provides only a brief overview of the context for these issues. The reader is referred to the extensive body of research regarding the interactions among societal, cultural, genetic, and biobehavioral risk and protective factors and their implications for promoting population health (Dabelea et al., 2000; Gillman et al., 2003; Halfon and Hochstein, 2002; Halfon and Inkelas, 2003; IOM, 2001, 2003; Krieger, 1994; Krieger and Davey Smith, 2004; McEwen, 2001; NRC and IOM, 2000, 2004; Reilly et al., 2005; Rosenbloom, 2002). The chapter focuses on the key issues relevant to improving the implementation and evaluation of obesity prevention efforts involving high-risk and culturally diverse populations.
UNDERSTANDING SPECIFIC CONTEXTS
Many aspects of society have changed concomitantly with the rise in childhood obesity. A broader understanding of the potential interplay
among these societal changes and children’s biological and behavioral responses is needed. For the population subgroups most affected by obesity, the relevant adverse social and environmental factors may be concentrated or magnified. A variety of causal pathways are associated with many aspects of systemic disadvantage (e.g., poverty, substandard housing, limited educational opportunities, and low levels of social integration), which can lead to adverse health, social, and economic circumstances (Gostin and Powers, 2006). These factors have greater impacts on those with the fewest resources to buffer these influences. The subpopulations that have the highest prevalence of obesity are those considered to be socially, economically, and politically disadvantaged in other respects. Thus, although the determinants of obesity are generally of the same nature among all population groups, special considerations are needed to assess whether the pathways to progress in preventing childhood obesity in the entire population will also reach the subgroups who are the most affected. Long-term investments that support the development or adaptation and evaluation of childhood obesity prevention initiatives are needed. These initiatives also need to be adapted to various settings, contexts, and subpopulations for their dissemination if they are proven to be effective.
Obesity Prevalence
Obesity and its risk-behavior determinants (e.g., high levels of consumption of energy-dense and low-nutrient diets, physical inactivity, and sedentary behaviors) are major drivers of health disparities by race/ethnicity as they contribute to three of the disease categories responsible for the majority of excess mortality: type 2 diabetes, cardiovascular diseases (CVDs), and cancer (Wong et al., 2002). Obesity and at-risk obesity prevalence rates in American children and youth reveal significant differences by age and sex and between racial/ethnic groups (Freedman et al., 2006; Hedley et al., 2004; Ogden et al., 2006; Sherry et al., 2004). There does not appear to be a general excess risk in all age and gender groups, although the increases in obesity over the past 30 years have been especially pronounced at the upper part of the body mass index (BMI) distribution for children and youth. From 1971–1974 to 1999–2002, the prevalence of individuals in certain subgroups with BMI levels above the 99th percentile increased substantially. Additionally, African-American girls ages 6 to 17 years have experienced greater increases in obesity prevalence than white children and adolescents. These increases began in the 1970s, whereas the increases among individuals in other racial/ethnic groups were not observed until the 1980s (Freedman et al., 2006).
By tracking obesity prevalence rates in subpopulations and evaluating the progress achieved by obesity prevention interventions, it may be pos-
sible to reduce the risk of obesity in these groups and ensure that primary obesity prevention strategies are reaching the entire target population. It is also important to track increases in BMI levels and obesity prevalence because childhood obesity is associated with an increased risk of CVD and mortality in adulthood (Li et al., 2004; Srinivasan et al., 2002).
In 2003–2004, National Health and Nutrition Examination Survey (NHANES) data showed that 33.6 percent of U.S. children and adolescents were either obese (17.1 percent) or at risk of becoming obese (16.5 percent) (Ogden et al., 2006). The analysis of trends from NHANES data reveal that, when compared with non-Hispanic white cohorts, non-Hispanic black and Mexican-American children and adolescents, ages 2 to 19 years, have a greater prevalence of obesity.1 Non-Hispanic African-Americans and Mexican-American children and adolescents are also at greater risk of becoming obese (Hedley et al., 2004; Ogden et al., 2006). The prevalence rates of obesity and at risk for obesity in children and adolescents by age, sex, and racial/ethnic group for 2003 and 2004 are shown in Figure 3-1.
State-specific prevalence and trends among 2- through 4-year-old children from low-income U.S. families were examined from 1989 to 2000. The results showed significant increases in obesity among low-income children in 30 states and significant decreases in childhood underweight in 26 states (Sherry et al., 2004). Although no geographic predominance was apparent, the number of states reporting obesity prevalence rates of more than 10 percent increased from 11 in 1989 to 28 in 2000. The number of states reporting decreased rates of underweight also rose during the same time frame, as reflected by 9 states in 1989 and 23 states in 2000 that had underweight prevalence rates equal to or less than 5 percent (Sherry et al., 2004).
National obesity prevalence data are limited for American Indian/ Alaska Native and Asian/Pacific Islander children and youth. Nevertheless, an analysis of data for 9,464 American Indian children and youth, ages 5 to 18 years, compared with NHANES II data (1976 to 1980) found that 39 percent had BMIs above the 85th percentile (Jackson, 1993). Another analysis estimated the prevalence of obesity in a sample of 1,704 7-year-old children from 7 American-Indian communities across the United States to be between 27 and 30 percent for boys and girls, and the at-risk obesity prevalence was estimated at 20 to 21 percent for boys and girls (Caballero et al., 2003). In 2002 and 2003, an analysis of 11,538 American Indians, ages 5 to 17 years, attending 55 schools on 12 reservations located in the
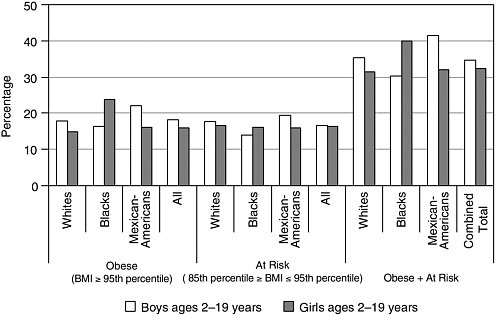
FIGURE 3-1 Percentage of U.S. children and adolescents ages 2 to 19 years who are obese or at risk for obesity by sex and race/ethnicity in 2003 to 2004.
SOURCE: Ogden et al. (2006).
Aberdeen Area of the Indian Health Service (North Dakota, South Dakota, Iowa, and Nebraska), found that both the obesity prevalence and the at-risk obesity prevalence rates exceeded the levels for all U.S. children at almost every age group. The obesity prevalence rate was 24 percent for 5-year-old American-Indian children. Nearly one half (47 percent) of 5-year-old boys and 41 percent of 5-year-old girls were at risk for obesity (Zephier et al., 2006).
There are limited data on the prevalence rates of obesity among Alaska-Native children and youth. One analysis examined the BMI levels of 1,632 students, ages 3 to 18 years, in 20 rural Alaskan communities. Results showed that nearly 50 percent were either obese (25 percent; n = 407) or at risk for obesity (24 percent; n = 392) (Dirks et al., 2006). National prevalence data for Asian/Pacific-Islander populations are not available. However, the obesity prevalence rate among a sample of low-income preschool children in Hawaii was 8.7 percent in 1997, whereas the national mean that year was 10.3 percent. However, the rate caught up to the national mean in 2002, with prevalence rates of 13.1 percent in Hawaii and 13.5 percent nationally (Baruffi et al., 2004). A cross-sectional study of 21,911 Samoan, Filipino, Hawaiian, Asian, Hispanic/Latino, African-American, and white toddlers ages 12 to 59 months participating in the Hawaii Special Supple-
mental Nutrition Program for Women, Infants, and Children (WIC) in 1997 and 1998 found a higher than expected prevalence of obesity among preschoolers ages 2 to 4 years. Samoan toddlers had the highest prevalence of obesity at 27 percent, followed by Filipinos (12.4 percent), Hawaiians (11.3 percent), Hispanics (10.1 percent), Asians (9.0 percent), whites (8.5 percent), and African Americans (7.3 percent) (Baruffi et al., 2004).
Health Effects of Childhood Obesity
Type 2 diabetes, which accounted for less than 3 percent of all cases of new-onset diabetes among children and adolescents two decades ago, today accounts for between 30 and 45 percent of new-onset cases among adolescences and young adults (ADA, 2000; Rosenbloom et al., 1999). An analysis of data from NHANES (1999–2000), representing 27 million U.S. adolescents, showed a higher prevalence of impaired fasting glucose levels (an indicator for type 2 diabetes risk) among obese adolescents (17.8 percent) that among adolescents of normal weight (7.0 percent). In addition, the data showed that the rate of impaired fasting glucose levels was most pronounced among Mexican-American adolescents (13.0 percent) compared with the rates among African-American (4.2 percent) and white adolescents (7.0 percent) (Williams et al., 2005). On the basis of an analysis of data from NHANES (1999 to 2002) with a sample of 4,370 adolescents ages 12 to 19 years, the prevalence of type 2 diabetes was substantial and was projected to affect more than 39,000 U.S. adolescents and 2.77 million adolescents with impaired fasting glucose levels. These estimates present important implications for public health because of the high level of conversion from an impaired fasting glucose level to type 2 diabetes in adults and the increased risk of CVD in individuals with type 2 diabetes (Duncan, 2006).
American-Indian/Alaska-Native, African-American, and Hispanic/Latino adolescents have a higher prevalence of type 2 diabetes than white adolescents; and this rise has occurred in parallel with the obesity epidemic among both children and adults (Gahagan et al., 2003; Oeltmann et al., 2003; Pinhas-Hamiel and Zeitler, 2005). American Indians/Alaska Natives have the highest rates of type 2 diabetes of any racial/ethnic group in the United States (National Diabetes Information Clearinghouse, 2005) and significant rates of heritability of CVD (North et al., 2003). Type 2 diabetes is a major public health crisis among American Indian/Alaska Native adolescents. From 1990 to 1998, the total number of young American Indians/Alaska Natives diagnosed with diabetes increased by 71 percent, and the prevalence increased by 46 percent (6.4 per 1,000 population to 9.3 per 1,000 population). An increase in prevalence was greater among adolescents ages 15 to 19 years and young adults (Acton et al., 2002). Between
1990 and 2001, the prevalence of type 2 diabetes increased by 106 percent among 15- to 19-year-old American-Indian youth and increased by 50 percent among American-Indian children and youth younger than 15 years of age (IHS National Diabetes Program, 2004).
Sociodemographic Profiles
Racial/Ethnic Diversity of the U.S. Population
According to the 2000 U.S. Census, approximately 30 percent of the U.S. population identified themselves as members of a racial or an ethnic minority group. The 2000 Census counted more than 36 million African Americans (12.9 percent of the population); more than 35 million Hispanics/Latinos (12.5 percent) who live in the United States and another 3.8 million who live in the Commonwealth of Puerto Rico; nearly 12 million Asians (4.2 percent); 874,000 Native Hawaiians and other Pacific Islanders; and 4.3 million people (1.5 percent of the total U.S. population) reported that they were American Indians/Alaska Natives (2.4 million or 1 percent reported only American Indian/Alaska Native as their race), of which 35.9 percent live in American Indian areas (which include reservations) or Alaska Native village areas (Hobbs and Stoops, 2002; Ogunwole, 2006). By 2050, it is projected that these groups will account for almost 50 percent of the U.S. population (MBDA, 1999). The ethnic minority population is expected to account for nearly 90 percent of the total growth in the U.S. population, from an ethnic/racial minority population of 69 million in 1995 to one of 186 million in 2050 (MBDA, 1999). Thus, the term “minority” is increasingly misleading as a descriptor for diverse racial/ ethnic groups in the aggregate, at least with respect to the proportion of the multicultural U.S. population.
Geographic Variation in Population Diversity
Each of the 50 states throughout the nation has growing childhood, youth, and adult obesity burdens that are leading to overwhelming economic, health, and social challenges that will reverberate at the federal, state, and local levels. Certain issues for high-risk populations dominate in certain states and localities where racial and ethnic minority populations are a numerical majority. Currently, this is the case in California, given the higher proportion of Hispanics/Latinos and African Americans compared with the proportion of non-Hispanic whites.
Hispanics/Latinos, who represent 20 different nationalities, are the nation’s largest and fastest-growing ethnic group as the result of ongoing immigration and natural increases in the birth rates of Hispanic/Latino
citizens (NRC, 2006a). Given current demographic trends, nearly one in five U.S. residents will be of Hispanic/Latino origin by 2025 (NRC, 2006b).2
In addition to California, it is projected that by 2025, Texas, New Mexico, Hawaii, and the District of Columbia will also have population distributions in which non-Hispanic whites will be the minority (MBDA, 1999). Collectively, these four states and the District of Columbia represent 25 percent of the entire U.S. population. From this perspective on U.S. population demographics, finding ways to meet the challenges of addressing childhood obesity in racially, ethnically, and culturally diverse contexts becomes an urgent priority.
Socioeconomic Status, Poverty, Health Disparities, and Health Outcomes
Socioeconomic Status and Poverty
Patterns of disease are best understood within the context of social determinants of health, which represent the societal conditions that affect health and that can be changed by social and health policies and programs. Three categories of social determinants that potentially affect health include social institutions (e.g., cultural and faith-based organizations, political structures, and economic systems including availability and distribution of fresh fruits and vegetables), physical surroundings (e.g., neighborhoods, worksites, towns, and cities), and social relationships (e.g., social networks and the differential treatment of subpopulations) (Anderson et al., 2003b). The implications of social determinants of health for assessing and evaluating progress in obesity prevention are discussed at the end of this chapter and in Chapter 6.
Research has shown that the SES characteristics of the neighborhood in which individuals live (e.g., average income and percent unemployment) are better predictors than individual characteristics of morbidity and mortality (Diez-Roux et al., 1997; Finkelstein et al., 2004; Jargowsky, 1997), and that poverty is the most powerful single determinant of health (Lynch et al., 1997). Poverty causes poor health through its connection with reduced access to and use of health care services (with the quality of preventive, primary, and specialty health care services for this population often
being lower), food insecurity3 and low-quality diets, and behaviors that do not support healthy lifestyles (DHHS and AHRQ, 2005; NCHS, 2005). African-American, Hispanic/Latino, and American Indian/Alaska Native households are substantially overrepresented among all U.S. households with incomes below the poverty level (DeNavas-Walt et al., 2005; NRC, 2006b; Robert and House, 2000). Moreover, children and adults in families with incomes below or near the federal poverty level4 have poorer health outcomes than those in families with higher incomes (DHHS and AHRQ, 2005; IOM, 2003).
In 2003, 11 percent of U.S. children had no health insurance (Annie E. Casey Foundation, 2006). Children in low-income families are substantially more likely than children in higher-income families to lack health care coverage (NCHS, 2005). In 2002 and 2003, uninsured children were three times more likely than their counterparts with insurance (32 percent versus 11 percent, respectively) to have not had a visit to a physician or health clinic for health care within the previous year (NCHS, 2005). Racial/ethnic minority children and youth face a number of barriers to receiving timely, appropriate, and high-quality health care services (NCHS, 2005; NRC, 2006a). Children covered by Medicaid are nearly six times more likely than children covered by private insurance to be treated for obesity. In addition, the treatment of obesity in children covered by Medicaid is more expensive (approximately $6,700/year) than the treatment of obesity for children covered by private insurance (approximately $3,700/year) (Thomson Medstat, 2006). Children with obesity experience higher rates of hospitalizations and greater use of physician services than their nonobese peers (Thomson Medstat, 2006).
The percentage of Americans living in poverty increased from 11.3 percent in 2000 to 12.5 percent in 2003. The 2004 poverty rate among children under 6 years of age was 21 percent (Annie E. Casey Foundation, 2006). In 2004, 38.2 million individuals (an estimated 11.9 percent of the total population), including 13.9 million children, lived in households with food insecurity (Nord et al., 2005). Several studies examining the relationships among food insecurity, SES, and obesity in children or youth have not been able to demonstrate a strong association or causal effect after adjustment for other factors (Hofferth and Curtin, 2005; Kaiser et al., 2002; Matheson et al., 2002; Whitaker and Orzol, 2006).
Many racial/ethnic minority subpopulations have experienced social, political, and historical contextual events that continue to have long-lasting effects on their physical health, psychosocial well-being, and economic livelihoods (Duran et al., 1998; NRC, 2006b; Williams and Collins, 1995). The challenges associated with understanding the relationship between SES and obesity risk are discussed in Box 3-1.
Immigration and Acculturation
Immigrants are the fastest-growing segment of the U.S. population. As a percentage of the total population, the foreign-born population increased
|
BOX 3-1 Challenges in Understanding the Relationship Between Socioeconomic Status and Obesity Risk Despite the substantial variation in BMI that exists as a function of both SES and race/ethnicity, uncertainties remain as to whether these rates can be attributed solely to SES, because obesity disparities are not the same across ethnic groups and they do not emerge at comparable times during childhood (Parsons et al., 1999). There is no consensus about the reasons for these disparities, although recent research provides certain insights. Variation in obesity risk by race/ethnicity and SES appears to occur early in life. An assessment of 16,000 preschool children, ages 2 to 4 years, enrolled in the Head Start Program in New York City found that 27 percent were obese and 15 percent were at risk for obesity. An estimated one in four Head Start children in that sample were found to be obese by the age of 2 years, and one in three children were obese by the age of 4 years. Although obesity was identified as a problem among all Head Start children in New York City, Hispanic/Latino and African-American preschoolers are disproportionately affected (New York City Department of Health and Mental Hygiene, 2006). Moreover, socioeconomic deprivation in childhood has been found to be both a strong predictor of obesity in adulthood for African-American adult women (James et al., 2006a) and adult hypertension in adulthood for African-American men (James et al., 2006b). Mexican-American children and youth living along the U.S.-Mexico border experience higher levels of economic disadvantages and special challenges in accessing foods that contribute to a healthful diet, regular physical activity, and health care services (Abarca and Ramachandran, 2005; Ruiz-Beltran and Kamau, 2001). Low-SES Mexican school-aged children living along the U.S. border in Tijuana, adjacent to San Diego County in California, have been found to be at increased risk of obesity and related chronic diseases, which may be related to less healthful food choices for children attending schools in low-SES neighborhoods (Villa-Caballero et al., 2006). In contrast, among Mexican children and adolescents, particularly those living in urban areas, obesity is increasing among higher SES groups (IOM, 2007). |
|
Analyses of nationally representative longitudinal data—the National Longitudinal Survey of Youth (Strauss and Knight, 1999; Strauss and Pollack, 2001) and the National Longitudinal Study of Adolescent Health (NLSAH) (Goodman, 1999)—have suggested that family SES is inversely related to obesity prevalence in children and that the effects of SES and race/ethnicity are independent of other variables. A more recent analysis of a nationally representative sample of adolescents enrolled in the NLSAH examined trends in racial/ethnic disparities for leading health indicators from Healthy People 2010 (Harris et al., 2006) across multiple domains from adolescence to young adulthood. The results revealed that the health risk increased for 15 of 20 indicators among racially/ethnically diverse adolescents. Access to health care decreased from the teen to the adult years for most U.S. racial/ethnic groups, and the disparity was particularly high for American Indians (Harris et al., 2006). Analyses of nationally representative cross-sectional data reveal additional findings that can help to provide an understanding of the relationship between SES and obesity. An examination of the 1988 to 1994 NHANES data showed that the prevalence of obesity in white adolescents was higher for those in low-income families, but there was no clear relationship between family income and obesity in individuals in other age or racial/ethnic subgroups (Ogden et al., 2003; Troiano and Flegal, 1998). A more recent analysis of trends in the association between poverty and adolescents’ obesity risk was conducted for four cross-sectional NHANES surveys conducted from 1971 to 2004 (Miech et al., 2006). Although the obesity prevalence did not differ by SES or family poverty status for teens through age 14 years, a widening disparity was observed for 15- to 17-year-olds, especially boys, girls, non-Hispanic whites, and non-Hispanic African Americans. There was a 50 percent higher risk of obesity among adolescents in poor families compared with that among adolescents in non-poor families. Possible mechanisms that contributed to the obesity risk for adolescents were physical inactivity, higher levels of consumption of sweetened beverages, and skipping breakfast (Miech et al., 2006). |
from 4.7 percent in 1970 to 11.5 percent in 2002 (Dey and Lucas, 2006). The children of immigrant families are thus among the fastest-growing and the most ethnically diverse segment of the American child population. The median age of the individuals who make up the Hispanic/Latino second generation, for example, is just over 12 years (NRC, 2006b). Significant differences in the physical health status exist among U.S.-born and foreign-born individuals. Differences in the lengths of stay of immigrants in the United States suggest that the role of acculturation on immigrant health is complex and differs for various racial/ethnic groups (Dey and Lucas, 2006; Goel et al., 2004; Gordon-Larsen et al., 2003). However, what is clear from the available evidence is that the acculturation of young and adult immigrant populations is associated with the adoption of lifestyle behaviors and social norms that promote weight gain and obesity.
An analysis of a nationally representative sample of 13,783 adolescents from the National Longitudinal Study of Adolescent Health found that
second- and third-generation adolescents of U.S. immigrant families, especially Asian-American and Hispanic/Latino adolescents born in the United States, are twice as likely to be obese than the first-generation residents (Popkin and Udry, 1998). In another study, acculturation to the United States was identified as a risk factor for obesity-related behaviors, such as increased television viewing and higher levels of consumption of energy-dense and low-nutrient foods among Asian-American and Hispanic/Latino adolescents (Unger et al., 2004).
The disparities in the rates of obesity for Hispanic/Latino adolescents have been attributed to environmental, contextual, biological, and sociocultural factors, in addition to differences in income and education (NRC, 2006a,b). The families of foreign-born immigrant youth are more likely to have both lower family incomes and mothers with lower levels of education. They are also more likely than their American-born counterparts to live in communities with higher densities of immigrants and greater linguistic isolation (Gordon-Larsen et al., 2003). Additionally, children from immigrant families have more compromised physical health than children from nonimmigrant families and use health care services less frequently (Huang et al., 2006).
The deleterious effects of acculturation among Hispanic/Latino youth suggests that this ethnic population will be increasingly burdened by the complications of obesity, and the U.S. health care system will be faced with larger numbers of Hispanics/Latinos experiencing chronic diseases and their complications (NRC, 2006a).
These trends for immigrant youth parallel the observations for immigrant adults. Among the different immigrant subgroups, the number of years of residence in the United States is associated with higher BMI levels after 10 years, and the prevalence of obesity among immigrants who have lived in the United States for at least 15 years has been found to approach that of American-born adults (Goel et al., 2004).
Health Disparities and Health Outcomes
Health disparities are commonly defined as the population-specific differences in the presence of disease, health outcomes, or access to health care among racial, ethnic, and SES groups (Chen et al., 2006; Lavizzo-Mourey et al., 2005; Yancy et al., 2005). Because of the complexity of identifying, measuring, and monitoring health status and health determinants, it is challenging to reach a consensus about the dimensions of health disparities. Complicated relationships and interactions among race, ethnicity, gender, income, education, degree of acculturation, immigrant status, and place of residence have an impact on health disparities and health outcomes (IOM, 2006). Additionally, the lack of complete and accurate data examining
health disparities among children between and within racial and ethnic groups and children living across a full spectrum of SES levels limits understanding of the relative contributions and moderators of these disparities (Chen et al., 2006).
Key influences on understanding the pathways to health include a more complete knowledge of prenatal and other vulnerable periods; predisease pathways, representing the early and long-term precursors to disease; cumulative health risks across time; gene-environment interactions; and the intergenerational transmission of behaviors (NRC, 2001). Exposure to life stressors and health status are inextricably connected. For example, the effects of adverse childhood experiences, especially during critical developmental periods in childhood, on obesity and the health risks of stress and depression are areas of ongoing research (Ackard et al., 2003).
Adverse childhood experiences are an example of a set of life contexts which are experienced early in life, yet have profound effects on health and obesity risks into adulthood, independent of SES, race, and ethnicity. The Adverse Childhood Experiences (ACE) Study explored the exposures of more than 13,000 adult enrollees in a health maintenance organization to eight categories of adverse childhood experiences (e.g., abuse). The risk for obesity increased with the number and the severity of each type of childhood abuse (Williamson et al., 2002). Although the ACE Study addressed adult health outcomes rather than childhood health outcomes, the results support the hypothesis that a variety of physical, mental health, and social problems have common roots and that negative health-related behaviors may serve as coping strategies to manage the long-term consequences of childhood stress. Difficult and stressful childhood circumstances may increase the risk for mental health problems in children, which may in turn increase the risk for behaviors that contribute to childhood obesity (Goodman and Whitaker, 2002; Lumeng et al., 2003; Williamson et al., 2002). Many of these responses decrease the ability of individuals to self-regulate both physiological and emotional responses (van der Kolk and Fisler, 1994).
An improved understanding of the complex interplay of the environmental and the biological factors that influence behaviors can be achieved only through the synthesis of the findings of many scientific disciplinary perspectives. Such a synthesis of findings will allow a greater understanding of the complex web of risk factors for childhood obesity, enhance the ability to design more effective interventions, and improve the ability to develop appropriate evaluation measures (Box 3-2). Additionally, further research is needed to clarify the vulnerable periods in childhood and adolescence with particular relevance to risks for obesity and to understand how best to apply this knowledge to preventive efforts.
|
BOX 3-2 The Life Course Approach to Health A life course approach refers to how health status at any given age or for any given birth cohort reflects both contemporary conditions and prior living circumstances, from in utero through childhood, adolescence, and adulthood. This perspective views health as the product of these life experiences—both the risks and the protective experiences and environments—and acknowledges that life experiences have a cumulative impact. This approach also recognizes that individuals have developmental trajectories that are both biological and social over time and that they are shaped by the social, economic, political, technological, and ecological contexts of societies. A life course health development framework can be used to understand and address the complex web of interacting risk factors that place individuals and populations at higher risk for health disparities, including childhood obesity. This framework shows the close interaction of risk factors that may initially appear to be unrelated but that resonate across the web of health influences at multiple levels, from the societal level to the community and individual levels. Changes in any of these risks will have long-term effects and implications for the individual into adulthood. The development of health trajectories is characterized by the following features:
SOURCES: Halfon and Hochstein (2002); Krieger (2001); Yu (2006). |
INTERVENTIONS AND POLICY LEVERS FOR HIGH-RISK POPULATIONS
Because the communities and populations that are at higher risk for childhood obesity are often those with larger numbers of ethnically diverse and lower-SES groups, it is important to take into account the collective contexts of these communities as interventions are developed or adapted. As important as the issue of obesity prevention may be, many of these communities are facing problems that have immediate consequences (e.g., unemployment, poor schools, and violence) leaving fewer resources available for obesity prevention. The barriers to the implementation of obesity
prevention programs in these contexts should be acknowledged in designing and implementing interventions. For example, communities may be less receptive to people who do not live with them and who have limited experience with the daily realities of the communities. Additionally, there may be limited response to those who identify the priorities of the community without participatory input from community members. The short-term nature of research projects and grant funding can also be an impediment to community engagement if effective programs are dismantled before a problem is sufficiently addressed or before approaches are modified and institutionalized for long-term sustainability. Further, lifestyle change interventions may be perceived as a negative judgment of a community, which may increase the level of fatalism or sense of futility about whether a problem can be addressed, as well as create conflict between communities and external program staff. Careful attention to these issues can be instrumental in overcoming barriers. Seeking community involvement early on and throughout an intervention’s development, implementation, and evaluation is particularly important.
Because many conditions and health outcomes share common underlying causes and affect individuals in the same families and communities, it will be necessary to address these problems in an integrated way as they are experienced in communities (Kumanyika, 2005). It must also be acknowledged that interventions that have worked in one community may not be effective or may need to be adapted to low-income and racially/ethnically diverse communities because of such factors as competing risks and threats, cost, an overwhelmed local infrastructure, or different cultural values and practices. An ecologic and culturally competent5 paradigm is urgently needed to address the spectrum of barriers that racial/ethnic groups and low-income children and youth face to identify the most promising practices that will reduce the prevalence of obesity and promote healthy lifestyles.
Issues Related to Progress
Despite the multiple challenges that diverse communities experience, resources and assets exist that should be used to design, implement, and evaluate childhood obesity prevention interventions. Many communities have a strong sense of their cultural roots, including a deep connection to
their families and histories of healthful traditional foods and physical activities. The translocation of cultural values onto these communities has proven to be less effective than the use of interventions that arise from community values. For example, many community interventions that promote the health of the family and community are more likely to be successful than those that promote actions intended to improve one’s own health. This cultural belief in the value of working to enhance the common good may be a leverage point for interventions, especially given the powerful effect that collective efficacy6 has on obesity risk in youth (Cohen et al., 2006). Other strengths often include a respect for elders, a network of an extended family with norms governing an individual’s place within that structure, strong spiritual values, and the integral nature of movement to music (such as dance) as a celebratory activity throughout life.
Interventions that are designed and evaluated with meaningful input from a community and that reinforce the strengths and assets of the community members are more likely to be effective and sustainable. Actively involving key stakeholders, decision makers, or sectors of a community as integral components of an intervention team at all stages, from the initial conceptualization of the intervention to monitoring and evaluation, can enhance trust between the researchers and community members (DHHS, 2001; Pyramid Communications, 2003) (Appendix G). Researchers and funders are using community-based participatory research approaches that emphasize collaboration with communities to explore and act on local concerns. This research approach allows stakeholders to identify the key problems to be studied, formulate research questions in culturally sensitive ways, and use study results to support relevant program and policy development or social change. Every obesity prevention initiative does not require using participatory research methods. However, when the results of an initiative are to be used for and by communities, members of the community should collaborate in all stages, including generating the findings and determining the ways in which the evaluation results are formulated, interpreted, and applied (Green and Mercer, 2001).
The culture and beliefs held by a community may be a powerful tool that can be used to promote health beyond an intervention. For example, in a diabetes prevention study conducted in a Pima Indian community, the biological outcomes for the lifestyle intervention group were less positive than those for the control group whose activities emphasized Pima history and culture (Narayan et al., 1998). As efforts are made to evaluate the effectiveness of obesity prevention interventions nationwide, there is a need to standardize interventions for comparison purposes. However, this must
be balanced with the adaptation of interventions to local cultures and worldviews (Yancey et al., 2006c).
A variety of opportunities exist for targeting, implementing, and evaluating policies and interventions reaching diverse populations of children and youth at the highest risk for obesity and related chronic diseases. For example, the Head Start Program delivers a range of services related to comprehensive nutrition and nutrition education to foster healthy development and school readiness in low-income preschool children ages 2 to 5 years throughout the nation. The U.S. Department of Agriculture (USDA) administers 15 federal food assistance and nutrition safety-net programs through the states to improve the nutritional well-being of low-income households with children and youth. (See Chapter 4 and Appendix D for information on the evaluation of these programs.)
Policy makers can reinforce current programs to foster food security and equity by adding a specific childhood obesity prevention component to the Head Start Program and the USDA-administered federal nutrition programs including the Food Stamp Program (FSP), the WIC program, and the school nutrition programs (Kumanyika and Grier, 2006). Other potential policy levers include Medicaid, the State Child Health Insurance Program (SCHIP) (Lurie et al., 2005), and the engagement and mobilization of faith-based communities to achieve childhood obesity prevention goals (Chapter 6).
As a means to improve existing evaluation and surveillance systems, federal and state initiatives—such as the Early and Periodic Screening, Diagnostic, and Treatment program, which provides comprehensive health care services for infants, children, and adolescents enrolled in Medicaid; the SCHIP; WIC; FSP; and the school nutrition programs—should measure the impact of the programs on obesity risk beyond outputs7 in order to further document the structural, policy, behavioral, and health outcomes that are directly linked to childhood obesity rates.
Moreover, there will need to be a creative pursuit of innovative and cost-effective interventions such as the Farmer’s Market Nutrition Program (USDA, 2006), and evaluating the effectiveness of interventions such as school health report cards in reaching low-income and uninsured children in states where children do not receive regular preventive health care services from a primary care provider.
Because fewer opportunities for physical activity are found, on average, in low-income communities and those with higher proportions of racially/ethnically diverse groups, innovative programs are needed that promote
environmental justice—efforts that address the disproportionate exposures to harmful environmental conditions by low-income and minority communities—and opportunities for physical activity for populations at high risk for obesity (Day, 2006; Powell et al., 2004). Changes in the built environment are needed in many cities and communities to enhance opportunities for physical activity; however, environmental intervention approaches are less well developed, particularly in terms of legislative policy changes (Burdette and Whitaker, 2005; Sallis and Glanz, 2006; Sloane et al., 2006; Yancey et al., 2006c; Zimring et al., 2005).
The challenges presented by neighborhood violence, inadequate pedestrian safety accommodations (e.g., high-speed traffic, few signals or stop signs), the deterioration of parks and sidewalks, and dual working parents indicate that the school and after-school settings are critical venues for reaching children and youth. Increasing the amount of time in physical education and the quality of physical education in schools is an important step (Burgeson et al., 2001) (Chapter 7). For example, physical education has been demonstrated to result in a decrease in weight gain among elementary school girls (Datar and Sturm, 2004). However, this is as far as most states have pursued measures to increase childhood physical activity from a legislative perspective and many of these efforts have been limited (TFAH, 2005) (Chapter 7).
More collective efforts that have been evaluated and proven to be effective are needed to reintroduce vigorous physical activity across the entire school day to achieve increases in energy expenditure among children and youth (Kumanyika and Grier, 2006; Yancey et al., 2005). One example of an intervention approach developed in less affluent urban and suburban schools with substantial ethnic minority populations is Take 10!® (Lloyd et al., 2005; Stewart et al., 2004), described in Box 3-3.
|
BOX 3-3 Innovative Physical Activity Promotion Programs Take 10!® Take 10!® is a classroom-based program that integrates physical activity into the curriculum of kindergarten to fifth-grade elementary school students. Ten-minute physical activity sessions are linked to math, science, social studies, and language arts lessons to substitute for sedentary, didactic learning approaches. Early studies of Take 10!® by the International Life Sciences Institute (ILSI) Center for Health Promotion have demonstrated the feasibility and utility of this approach for regularly engaging students and teachers in physical activity at a moderate to vigorous intensity range for 10 minutes and found that it can count toward the minimum 30 minutes of moderate to vigorous physical activity per day in schools recommended by the Centers for Disease Control and Prevention. Evaluation results have |
|
shown that 75 percent of teachers reported that they were able to do a Take 10!® activity at least three times per week in the first two semesters, and the program was sustained by 60 to 80 percent of the teachers for three or more times per week after 1 year (ILSI, 2006; ILSI Center for Health Promotion, 2005; Lloyd et al., 2005; Stewart et al., 2004). Physical Activity Across the Curriculum The goals of the Physical Activity Across the Curriculum (PAAC) study were to incorporate physical activity into regular academic lessons and to assist students with accumulating each week 90 to 100 minutes of physical activity that they perform during the school day, in addition to physical education (PE) and recess. The evaluation methods included direct observation of weekly physical activity by using SOFIT,a the collection of annual BMI measurements, the performance of weekly and annual surveys and annual focus groups with teachers, and the collection of measures of health risk and academic achievement at the baseline and 3 years after the intervention (Donnelly, 2005). The results of the National Institutes of Health-funded study of PAAC/Take 10!® conducted by researchers at the University of Kansas demonstrated that by the beginning of the third year of implementation, more than 70 percent of elementary school non-PE teachers had been conducting 10-minute physical activity breaks in 14 low-income intervention schools across 3 cities in which an estimated 75 percent of students qualified for free or reduced-cost lunches (ILSI Center for Health Promotion, 2005). Moving School Project The Moving School project, is another model that was developed in Germany. Moving School replaces the static sitting position, in which children in traditional schools spend the majority of their time (97 percent of lesson time) sitting, with dynamic sitting (53 percent), standing (31 percent), and walking (10 percent) during class time. The study evaluated the differences in physical activity between 22 second-grade students in a Moving School in Hannover, Germany, and 25 second-grade students in a traditional school in Flanders, Belgium. Accelerometer data revealed significantly greater levels of physical activity among the students of the Moving School than among those in the traditional school (Cardon et al., 2004). |
Examples of Progress
Ongoing and new initiatives across the country provide examples of programs and policy changes focused on improving nutrition and increasing physical activity in populations at high risk for obesity. At the Institute of Medicine (IOM) committee’s symposium focused on communities held in Atlanta, Georgia in October 2005, high school students from New York
City described their participation in the efforts of the TRUCE Fitness and Nutrition Center. The TRUCE Center endeavors to engage young people in proactive health initiatives that nurture social responsibility, promote investment in the community, and help to prevent adolescent obesity (Appendix G) (Box 3-4).
The Latino Childhood Obesity Prevention Initiative, administered through the nonprofit organization Latino Health Access, is a multiyear demonstration project that involves parents, students, teachers, principals, and other stakeholders in making changes relevant to increasing physical activity and improving nutrition in four schools in Orange County, California. The first phase of the program focused on building common ground and raising awareness of the issues through community and parent meetings, formation of an advisory group, exercise classes offered for parents, and use of assessment tools. The effectiveness of the program was evaluated through various indicators, such as the levels of parental participation,
|
BOX 3-4 Harlem Children’s Zone In New York City’s Central Harlem neighborhood an extensive community development and enrichment initiative, The Harlem Children’s Zone, offers a range of programs that have the potential to positively address childhood obesity. The TRUCE Fitness and Nutrition Center provides African-American and Hispanic/ Latino adolescents with a safe space where they can participate in educational, physical activity, and social opportunities including health promotion and nutrition education. The project has demonstrated the importance of physical activity and nutrition in maintaining wellness and preventing disease, involving young people in developing public health strategies, promoting academic excellence, and providing a safe environment with opportunities for physical activity. In response to a community-mapping exercise that documented the lack of available fresh fruits and vegetables in Harlem, the TRUCE Center initiated the Garden Mosaic Project. The Center reclaimed an abandoned city-owned lot where students worked alongside other community members to transform the space into a community garden. To demonstrate their mission of social responsibility, the harvested food is donated to a local soup kitchen that serves homeless people within their community. A key element of the intervention—intergenerational role modeling and storytelling in accordance with African-American tradition—reinforced a positive ethnic identity and self-efficacy as students worked with elderly community members in all aspects of gardening. Evaluations have primarily focused on process and outputs such as monitoring the number of children and youth involved in the program and asking the youth to keep journals to reflect on their learning experiences. SOURCES: Appendix G; Garden Mosaics (2006). |
attendance at events, and parental involvement in physical activity. The second phase of the program focused on mobilizing action. The indicators used to assess this effort included the extent of parental recruitment of other parents to participate in healthful meal preparation classes, the extent of parental participation in school board and city council meetings, and the number of parents participating in physical activity with their children. Evaluation results for Phase I and II indicate that the desired outcomes were achieved. Phase III of the project is under way and will attempt to reduce barriers to incorporating healthy dietary habits and physical activity behaviors for the schools and families (DHHS, 2006b).
American Indian and Alaska Native communities have developed a number of initiatives to address the childhood obesity epidemic (Appendix D), including the development of partnerships with nonprofit organizations, state and local governments, and the federal government. In recognition of the high rates of type 2 diabetes among individuals in native communities described earlier in this chapter, the U.S. Congress established the Special Diabetes Program for Indians (SDPI) through the Indian Health Service (IHS) in 1997 (IHS National Diabetes Program, 2004). Annual SDPI allocations are distributed as ongoing grants to 318 different IHS, tribal, and urban Indian programs in 35 states to provide diabetes prevention and treatment programs (IHS National Diabetes Program, 2004). Each site designs and carries out its own diabetes intervention depending on local priorities. A 2002 survey of programs showed that after SDPI was initiated, 75 percent (compared with 13 percent before the initiation of SDPI) have community-based healthful eating programs for American Indian children, youth, and families; 50 percent (compared with 18 percent before the initiation of SDPI) have school-based healthful eating programs for children; 83 percent (compared with 41 percent before the initiation of SDPI) routinely screen for obesity in children and youth; 60 percent (compared with 18 percent before the initiation of SDPI) currently offer weight management programs for children and youth; 71 percent (compared with 10 percent before the initiation of SDPI) have community-based physical activity programs for children, youth, and families; and 53 percent (compared with 22 percent before the initiation of SDPI) provide school-based physical activity programs. In addition, a number of programs used SDPI funds to provide fitness classes for children and youth, build or improve playgrounds, initiate walking clubs, and provide aerobics classes (IHS National Diabetes Program, 2004).
Nome is a community of approximately 3,500 people situated on the Bering Sea in northwest Alaska. More than half of the city’s population is Alaska Native, predominantly members of one of the several Eskimo groups who live in the Norton Sound Region. Summercise is a program sponsored by the Norton Sound Health Corporation; Kawerak, Inc.; the Nome Es-
kimo Community; the city of Nome; and the Nome Community Center. These sponsors work together to recruit health professionals and healthy role models from the community to provide classes for Nome children during the summer months. Class offerings include many activities drawn from the Eskimo traditions of the region, such as dances, games, and the collection and preparation of traditional subsistence foods. Children are asked to choose a health goal to work on over the summer, such as eliminating sweetened soda, candy, or chips, or being more physically active.
Another example of community action is provided by the Centers for Disease Control and Prevention’s Racial and Ethnic Approaches to Community Health (REACH) 2010 demonstration grants. REACH 2010 grants directly support 40 community coalitions throughout the United States, of which 27 (70 percent) focus on CVD or diabetes prevention and management (Jenkins et al., 2004; Levy et al., 2004; Liburd et al., 2005; Ma’at et al., 2002; Tucker et al., 2006). These coalitions include traditional public health partners (e.g., local and state health departments, community-based organizations, universities, and safety-net programs) and nontraditional partners (e.g., boards of education, faith-based organizations, and city or county urban planning and redevelopment agencies).
Cherokee Choices, a program of the Eastern Band of Cherokee Indians in North Carolina, is funded by a REACH 2010 grant. One of its main components is an obesity and diabetes risk-reduction project located at the Cherokee Elementary School. The initiative uses American Indian mentors, who provide healthful eating and physical activity interventions. They also provide emotional support, teach emotional coping skills, assist with academic tutoring, organize trips to sites of cultural significance, and use other techniques to improve the overall health and self-esteem of the children and to decrease their perceived stress. Teachers have reported a variety of positive outcomes, such as a change in the school culture, with a greater emphasis on being healthier. Participants in the mentoring program report positive connections with their mentors, fewer conflicts and improved communication with friends, greater interest in school, fewer missed school days, and greater knowledge of healthful food and beverage choices. The Walk and Talk after-school program is a component of Cherokee Choices and attendance has grown over time (Jeff Bachar, Cherokee Choices program manager, personal communication, June 7, 2006).
Many of the REACH 2010 grants target African-American communities, each of which has a substantive focus on promoting physical activity and healthful eating by using a comprehensive community-wide approach to create systems changes at various levels and with the reinforcement of change at the individual level (Ma’at et al., 2002). Although these projects are not primarily aimed at reducing childhood obesity, a number of their features differentially influence the sociocultural, economic, and physical
environments of children and youth (e.g., a focus on women as the family health and nutrition decision makers and caregivers). The programs also attempt to change the organizational practices of adults who are parents, teachers, religious leaders, and coaches and who serve other gatekeeper and decision-maker roles. The programs also pair the demand generation with the supply creation (e.g., the pairing of experiential learning, role modeling, and the provision of culturally relevant health data with healthier restaurant menu items, healthier products in food retail outlets, healthier snacks and refreshments at events and functions, and the incorporation of physical activity into meetings and events in a culturally relevant way such as low- to moderate-intensity movement to music). Project elements include the implementation of organizational wellness programs in local government offices, small businesses, and nonprofit agencies (Yancey et al., 2004, 2006a); the establishment of cardiovascular wellness centers at churches and other faith-based institutions, beauty salons, and barbershops (Ma’at et al., 2002); the organization of a coalition of black churches aimed at educating and supporting women to influence their churches to model healthy behavior change; and the hiring and training of lay health advisers to provide outreach and education in targeted neighborhoods, including the establishment of a farmers’ market to link increased access to healthful foods with economic development for local and neighborhood businesses (Liburd et al., 2005).
EVALUATION APPROACHES FOR DIVERSE POPULATIONS
Multicultural and culturally competent approaches to evaluation have only recently emerged as important considerations in evaluating social and public health policies and programs. Applying a paradigm that acknowledges the differences in how people from various backgrounds experience life and view the world will assist and enrich the evaluation of obesity prevention initiatives across and within SES groups and ethnically and culturally diverse populations (Brach and Fraserirector, 2000; Hopson, 2003).
As discussed in Chapter 2, there are a variety of perspectives on what constitutes a high-quality program or effort to prevent childhood obesity. The committee encourages programs and interventions to address several program quality dimensions, including consideration of the needs of underserved and high-risk populations, the use of relevant empirical evidence when the program is designed and implemented, the identification of similar efforts and the establishment of important cross-sectoral connections and collaborations, and consideration of the spectrum of outcomes (e.g., structural, institutional, systemic, behavioral, and health). Programs
and interventions should also be able to show how changes in short-term or intermediate outcomes relate to changes in long-term outcomes.
Interventions with evaluation components that target underserved populations and that also increase the level of engagement of these populations in communitywide approaches are urgently needed to effectively address childhood obesity in these diverse groups. Successful engagement will require the identification of the distributional equity and the differential effects of programs on underserved ethnically diverse groups and groups of various SES in order to inform “midcourse corrections” or the next generation of interventions. The capacity to reduce the obesity risk or disparities among certain subpopulations may be adopted as a selection criterion for intervention actions.
Behavioral interventions and evaluation approaches should be expanded into a variety of multicultural and resource-limited settings. The magnitude of the influence of any health promotion intervention will depend on the combination of its effectiveness, the extent and quality of its implementation, and its sustainability (Rogers, 2003). The active promulgation and the use of a variety of evidence-based programs and policies are needed to foster the societal uptake and institutionalization of obesity prevention interventions. Certain types of behavioral outcomes (e.g., tobacco use and immunization status) are easier to evaluate than other outcomes (e.g., cultural competency, social cohesion, civic engagement, and collective efficacy) (Anderson et al., 2003b, 2005).
Furthermore, it is challenging to accurately assess the intermediate outcomes of community interventions aimed at broad social determinants of health, such as community advocacy and economic and educational opportunities, that effect change across multiple intermediate and long-term outcomes because of the limitations in establishing links between upstream health promotion interventions and health outcomes (Anderson et al., 2005) (Chapter 6). The approaches taken must balance the trade-offs between initial selectivity, which improves retention and homogeneity (internal validity), and broader inclusiveness, which preserves relevance to the targeted population (external validity).
Important considerations for the design, implementation, monitoring, and evaluation of culturally competent obesity prevention interventions in diverse populations include the following:
-
Build on cultural assets (e.g., the salience of dance as a common form of physical activity among African Americans and Hispanics/ Latinos) (Beech et al., 2003; Boon and Clydesdale, 2005; Day, 2006; Robinson et al., 2003; Yancey et al., 2006c), recognize the role of cultural influence on health, and integrate culturally competent ap-
-
proaches into the delivery of health care and social services (Anderson et al., 2003a; Andrulis, 2005).
-
Address multiple health issues pertinent to a range of stakeholders in order to build momentum and community support for interventions (e.g., the Harlem Fitness Zone and the Cherokee Choices projects) and the Active Living by Design interventions (Sallis et al., 2006).
-
Recognize that the use of nonintervention control groups may not be acceptable to ethnic minority communities; rather, delayed intervention designs may be more tenable (Boon and Clydesdale, 2005).
-
Involve researchers who are knowledgeable about the racial/ethnic groups or cultures being studied or evaluated (American College of Epidemiology, 1995; Anderson et al., 2003a; Gil and Bob, 1999; Hopson, 2003; IOM, 1994; Kumanyika et al., 2005).
-
Focus attention on the process of intervening in addition to achieving outcomes. This may include particular attention to delivery channels, messengers, materials and messages, and other cultural adaptations or targeting. Subgroup analyses are critical, and, when differences are found, further examination is needed to explore why the interventions are not effective for certain subgroups (e.g., characteristics of the intervention itself or how it was implemented) (Kreuter and McClure, 2004; Yancey et al., 2006b).
Expanding Surveillance to Identify Areas With High Obesity Burdens and Related Chronic Disease
Data collection and analyses for surveillance and monitoring are core functions of governmental public health practices. However, methodological limitations to the identification and documentation of health disparities must be addressed. The public health infrastructure has the capacity to monitor aggregate racial/ethnic groups (e.g., categories defined by the U.S. Bureau of the Census). However, some individuals in racially/ethnically diverse communities may not participate in formal national data-gathering efforts because of logistical issues and concerns about how the data might be used. These challenges may result in the underrepresentation of racial/ ethnic minority populations in national surveillance systems. Representative surveillance and monitoring systems must be established to allow the monitoring of minority populations at potential health risk. The REACH 2010 Risk Factor Survey, for example, is conducted annually in African-American, Hispanic/Latino, Asian/Pacific Islander, and American Indian communities throughout the United States (CDC, 2004). Data from this survey demonstrate that residents in racial/ethnic minority communities experience greater disease risk and burden than individuals in the general population living in similar areas or states.
The continuous and expanded surveillance of health status in racial/ ethnic minority communities is an important measurement challenge for evaluators, yet it is needed to provide accurate disease prevalence estimates for evaluating culturally targeted prevention strategies for smaller geographic areas (e.g., for certain zip codes, school catchments areas, or census tracts). Expanding access to surveillance data would decrease the burden placed on community-based organizations, school districts, and other local government agencies to monitor and evaluate interventions, thereby allowing them to focus on the service delivery missions that motivate their activities (Yancey et al., 2005). The federal and state governments can expand their roles in collecting data by race/ethnicity and refining the definitions of race/ethnicity categories (Lurie et al., 2005).
Surveillance and monitoring systems may not provide the data needed for a comprehensive assessment of program quality. Community-based participatory research is one qualitative research approach to inquiry that emphasizes community partnerships and action for social change and the reduction of health disparities as an integral component of the research process (McAllister et al., 2003). Indeed, qualitative indicators require more precise definitions. Yet, effective programs and services will depend on the ability to measure and evaluate these indicators and integrate an understanding of the indicators into interventions. The ability to measure an array of indicators, both qualitative and quantitative, for a variety of diverse populations and outcomes is central to the elimination of health disparities and the prevention of childhood obesity in high-risk communities.
SUMMARY AND RECOMMENDATIONS
Quantitative assessment of progress over the past few years in preventing childhood obesity in diverse population groups is difficult. Examples are provided throughout the chapter of localized successes and innovative programs that are being implemented and evaluated across the nation. Large-scale initiatives focused on disproportionately affected groups are needed and should incorporate participatory approaches into their design, implementation, and evaluation.
Making progress toward closing the childhood obesity and health disparity gaps in high-risk racial/ethnic minority populations and diverse low-income populations will depend on several factors. These include a national commitment to substantially improve the social and built environments of high-risk communities; defining the contexts and mechanisms that lead to and perpetuate childhood obesity; and designing, implementing, and evaluating effective and culturally competent interventions, evaluation tools, and outcome measures.
Childhood obesity prevention efforts should creatively identify and build upon community assets, collective efficacy, and other leverage points where the needs of diverse populations are served, such as federal nutrition safety-net programs and shared cultural values and traditions. Attention to these factors will promote the implementation and evaluation of promising interventions that can help identify future best practices that support childhood obesity prevention efforts.
Recommendations 2 and 3 discussed in Chapter 2 explicitly propose further action focused on strengthening the implementation and the evaluation of obesity prevention interventions, policies, and initiatives relevant to culturally and ethnically diverse populations. This emphasis highlights the need to carefully consider and involve the people most affected in the policy change or intervention.
Recommendation 2: Policy makers, program planners, program implementers, and other interested stakeholders—within and across relevant sectors—should evaluate all childhood obesity prevention efforts, strengthen the evaluation capacity, and develop quality interventions that take into account diverse perspectives, that use culturally relevant approaches, and that meet the needs of diverse populations and contexts.
Recommendation 3: Government, industry, communities, and schools should expand or develop relevant surveillance and monitoring systems and, as applicable, should engage in research to examine the impact of childhood obesity prevention policies, interventions, and actions on relevant outcomes, paying particular attention to the unique needs of diverse groups and high-risk populations. Additionally, parents and caregivers should monitor changes in their family’s food, beverage, and physical activity choices and their progress toward healthier lifestyles.
REFERENCES
Abarca J, Ramachandran S. 2005. Using community indicators to assess nutrition in Arizona-Mexico border communities. Prev Chronic Dis [Online]. Available: http://www.cdc.gov/Pcd/issues/2005/jan/04_0082.htm [accessed July 23, 2006].
Ackard DM, Neumark-Sztainer D, Story M, Perry C. 2003. Overweight among adolescents: Prevalence and associations with weight-related characteristics and psychological health. Pediatrics 111(1):67–74.
Acton KJ, Burrows NR, Moore K, Querec L, Geiss LS, Engelgau MM. 2002. Trends in diabetes prevalence among American Indian and Alaska Native children, adolescents, and young adults. Am J Public Health 92(9):1485–1490.
ADA (American Diabetes Association). 2000. Type 2 diabetes in children and adolescents. Pediatrics 105(3):671–680.
American College of Epidemiology. 1995. Committee on Minority Affairs Statement of Principles on Epidemiology and Minority Populations. Ann Epidemiol 5:505–508.
Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Task Force on Community Preventive Services. 2003a. Culturally competent healthcare systems. A systematic review. Am J Prev Health 24(3 Suppl):68–79.
Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Task Force on Community Preventive Services. 2003b. The community guide’s model for linking the social environment to health. Am J Prev Med 24(3 Suppl):12–20.
Anderson LM, Brownson RC, Fullilove MT, Teutsch SM, Novick LF, Fielding J, Land GH. 2005. Evidence-based public health policy and practice: Promises and limits. Am J Prev Med 28(5 Suppl):226–230.
Andrulis DP. 2005. Moving beyond the status quo in reducing racial and ethnic disparities in children’s health. Public Health Rep 120(4):370–377.
Annie E. Casey Foundation. 2006. 2006 Kids Count Data Book. [Online]. Available: http://www.aecf.org/kidscount/sld/databook.jsp [accessed July 10, 2006].
Baruffi G, Hardy CJ, Waslien CI, Uyehara SJ, Krupitsky D. 2004. Ethnic differences in the prevalence of overweight among young children in Hawaii. J Am Diet Assoc 104(11): 1701–1707.
Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, Slawson D, Nunnally C, Rochon J, McLain-Allen B, Pree-Cary J. 2003. Child- and parent-targeted interventions: The Memphis GEMS Pilot Study. Ethnic Dis 13(1 Suppl 1):S40–S53.
Boon CS, Clydesdale FM. 2005. A review of childhood and adolescent obesity interventions. Crit Rev Food Sci Nutr 45(7–8):511–525.
Brach C, Fraserirector I. 2000. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev 57(Suppl 1):181–217.
Burdette HL, Whitaker RC. 2005. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics 116(3):657–662.
Burgeson CR, Wechsler H, Brener ND, Young JC, Spain CG. 2001. Physical education and activity: Results from the school health policy and program study 2000. J School Health 7(17):279–293.
Caballero B, Himes JH, Lohman T, Davis SM, Stevens J, Evans M, Going S, Pablo J. 2003. Body composition and overweight prevalence in 1704 schoolchildren from 7 American Indian communities. Am J Clin Nutr 78(2):308–312.
Cardon G, De Clercq D, De Bourdeaudhuij I, Breithecker D. 2004. Sitting habits in elementary schoolchildren: A traditional versus a “Moving School.” Patient Educ Couns 54(2): 133–142.
CDC (Centers for Disease Control and Prevention). 2004. REACH 2010 surveillance for health status in minority communities—United States, 2001–2002. MMWR 53(SS-6): 1–36.
Chen E, Martin AD, Matthews KA. 2006. Understanding health disparities: The role of race and socioeconomic status in children’s health. Am J Public Health 96(4):702–708.
Cohen DA, Finch BK, Bower A, Sastry N. 2006. Collective efficacy and obesity: The potential influence of social factors on health. Soc Sci Med 62(3):769–778.
Dabelea D, Hanson RL, Lindsay RS, Pettit DJ, Imperatore G, Gabir MM, Roumain J, Bennett PH, Knowler WC. 2000. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: A study of discordant sibships. Diabetes 49(12):2208–2211.
Datar A, Sturm R. 2004. Physical education in elementary school and BMI: Evidence from the Early Childhood Longitudinal Study. Am J Public Health 94(9):1501–1506.
Day K. 2006. Active living and social justice: Planning for physical activity in low-income, black, and Latino communities. J Am Planning Assoc 72(1):88–99.
DeNavas-Walt C, Proctor BD, Lee CH. 2005. Income, Poverty, and Health Insurance Coverage in the United States: 2004. Current Population Reports, P60-229. U.S. Bureau of the Census. Washington, DC: U.S. Government Printing Office. [Online]. Available: http://www.census.gov/prod/2005pubs/p60-229.pdf [accessed July 12, 2006].
Dey AN, Lucas JW. 2006. Physical and mental health characteristics of U.S.- and foreign-born adults: United States, 1998–2003. Advance Data from Vital and Health Statistics. No. 369. Hyattsville, MD: National Center for Health Statistics.
DHHS (U.S. Department of Health and Human Services). 2001. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: Office of the Surgeon General. Public Health Service.
DHHS. 2006a. 2006 Federal Poverty Guidelines. [Online]. Available: http://www.dhhs.state.nh.us/DHHS/PIO/LIBRARY/Policy-Guideline/federal-poverty-guidelines.htm [accessed May 29, 2006].
DHHS. 2006b. Best Practice Initiative: Latino Health Access Latino Childhood Obesity Prevention Initiative Demonstration Project. [Online]. Available: http://phs.os.dhhs.gov/ophs/BestPractice/LatinoObesity.htm [accessed May 29, 2006].
DHHS and AHRQ (Agency for Healthcare Research and Quality). 2005. 2005 National Healthcare Disparities Report. [Online]. Available: http://www.ahrq.gov/qual/nhdr05/nhdr05.pdf [accessed April 13, 2006].
Diez-Roux AV, Nieto FJ, Muntaner C, Tyroler HA, Comstock GW, Shahar E, Cooper LS, Watson RL, Szklo M. 1997. Neighborhood environments and coronary heart disease: A multilevel analysis. Am J Epidemiol 146(1):48–63.
Dirks LG, Ross-Tsilkowski A, Ballew C. 2006. Rural Alaska Native Pediatric Height and Weight Survey 2005. Alaska Native Tribal Health Consortium, Anchorage, AK. Indian Health Service 17th Annual Research Conference, April 24–26. Abstract.
Donnelly JE. 2005 (June 29). Physical Activity Across the Curriculum/Take 10! Presentation at the Institute of Medicine Symposium Progress in Preventing Childhood Obesity: Focus on Schools, Wichita, Kansas. Institute of Medicine Committee on Progress in Preventing Childhood Obesity.
Duncan GE. 2006. Prevalence of diabetes and impaired fasting glucose levels among U.S. adolescents. Arch Pediatr Adolesc Med 160(5):523–528.
Duran E, Duran B, Brave Heart MYH, Yellow-Horse-Davis S. 1998. Healing the American Indian soul wound. In: Danieli Y, ed. International Handbook of Multigenerational Legacies of Trauma. New York: Plenum Press.
Finkelstein EA, Khavjou OA, Mobley LR, Haney DM, Will JC. 2004. Racial/ethnic disparities in coronary heart disease risk factors among WISEWOMAN enrollees. J Women’s Health 13(5):503–518.
Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. 2006. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity 14(2):301–308.
Gahagan S, Silverstein J. American Academy of Pediatrics Committee on Native American Child Health. American Academy of Pediatrics Section on Endocrinology. 2003. Prevention and treatment of type 2 diabetes mellitus in children, with special emphasis on American Indian and Alaska Native children. American Academy of Pediatrics Committee on Native American Child Health. Pediatrics 112(4):e328.
Garden Mosaics. 2006. TRUCE Carrie McCracken Community Garden. New York, NY: Garden Mosaics. [Online]. Available: http://www.gardenmosaics.cornell.edu/pgs/data/inventoryread.aspx?garden=84 [accessed June 3, 2006].
Gil EF, Bob S. 1999. Culturally competent research: An ethical perspective. Clin Psychol Rev 19(1):45–55.
Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA. 2003. Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics 111(3):e221–e226.
Glanz K, Sallis JF, Saelens BE, Frank LD. 2005. Healthy nutrition environments: Concepts and measures. Am J Health Promot 19(5):330–333.
Goel MS, McCarthy EP, Phillips RS, Wee CC. 2004. Obesity among U.S. immigrant subgroups by duration of residence. J Am Med Assoc 292(23):2860–2867.
Goodman E. 1999. The role of socioeconomic status gradients in explaining differences in U.S. adolescents health. Am J Public Health 89(10):1522–1528.
Goodman E. 2003. Letting the “gini” out of the bottle: Social causation and the obesity epidemic. J Pediatr 142(3):228–230.
Goodman E, Whitaker RC. 2002. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 109(3):497–504.
Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. 2003. Acculturation and overweight-related behaviors among Hispanic immigrants to the U.S.: The National Longitudinal Study of Adolescent Health. Soc Sci Med 57(11):2023–2034.
Gordon-Larsen P, Nelson MC, Page P, Popkin BM. 2006. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 117(2):417– 424.
Gostin LO, Powers M. 2006. What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Aff 25(4):1053–1060.
Green LW, Mercer SL. 2001. Can public health researchers and agencies reconcile the push from funding bodies and the pull from communities? Am J Public Health 91(12):1926– 1943.
Halfon N, Hochstein M. 2002. Life course health development: An integrated framework for developing health, policy, and research. Milbank Q 80(3):433–479.
Halfon N, Inkelas M. 2003. Optimizing the health and development of children. J Am Med Assoc 290(23):3136–3138.
Harris KM, Gordon-Larsen P, Chantala K, Udry JR. 2006. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med 160(1):74–81.
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. 2004. Prevalence of overweight and obesity among U.S. children, adolescents, and adults, 1999–2002. J Am Med Assoc 291(23):2847–2850.
Hobbs F, Stoops N. 2002. Demographic Trends in the 20th Century. Census 200 Special Reports. [Online]. Available: http://www.census.gov/prod/2002pubs/censr-4.pdf [accessed July 31, 2006].
Hofferth S, Curtin S. 2005. Poverty, food programs, and childhood obesity. J Policy Anal Manage 24(4):703–726.
Hopson R. 2003. Overview of Multicultural and Culturally Competent Program Evaluation. Oakland, CA: Social Policy Research Associates. [Online]. Available: http://www.calendow.org/reference/publications/pdf/evaluations/TCE0 509-2004_Overview_of_Mu.pdf [accessed April 18, 2006].
Huang ZJ, Yu SM, Ledsky R. 2006. Health status and health service access and use among children in U.S. immigrant families. Am J Public Health 96(4):634–640.
IHS (Indian Health Service). National Diabetes Program, Department of Health and Human Services. 2004. Interim Report to Congress: Special Diabetes Program for Indians. [Online]. Available: http://www.ihs.gov/MedicalPrograms/diabetes/resources/r_rtc2004index.asp [accessed July 12, 2006].
ILSI (International Life Sciences Institute). 2006. What Is Take 10!®? [Online]. Available: http://www.take10.net/whatistake10.asp [accessed May 23, 2006].
ILSI Center for Health Promotion. 2005. A General Overview of Physical Activity and Nutrition Intervention Programs. [Online]. Available: http://chp.ilsi.org/NR/rdonlyres/1287022A-3300-426A-ACCF-C87D5CEA1348/0/SchoolHCCommtyProgramsListILSICHP041206.pdf [accessed May 31, 2006].
IOM (Institute of Medicine). 1994. Balancing the Scales of Opportunity: Ensuring Racial and Ethnic Diversity in the Health Professions. Washington DC: National Academy Press.
IOM. 2001. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington DC: National Academy Press.
IOM. 2003. The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press.
IOM. 2005. Preventing Childhood Obesity: Health in the Balance. Washington DC: The National Academies Press.
IOM. 2006. Examining the Health Disparities Research Plan of the National Institutes of Health: Unfinished Business. Washington DC: The National Academies Press.
IOM. 2007. Joint U.S.–Mexico Workshop on Preventing Obesity in Children and Youth of Mexican Origin. Washington, DC: The National Academies Press.
Jackson MY. 1993. Height, weight, and body mass index of American Indian school children, 1990–1991. J Am Diet Assoc 93(10):1136–1140.
James SA, Fowler-Brown A, Raghunathan TE, Van Hoewyk J. 2006a. Life-course socioeconomic position and obesity in African American women: The Pitt County study. Am J Public Health 96(3):554–560.
James SA, Van Hoewyk J, Belli RF, Strogatz DS, Williams DR, Raghunathan TE. 2006b. Life-course socioeconomic position and hypertension in African American men: The Pitt County study. Am J Public Health 96(5):812–817.
Jargowsky PA. 1997. Poverty and Place: Ghettos, Barrios and the American City. New York, NY: Russell Sage Foundation.
Jenkins C, McNary S, Carlson BA, King MG, Hossler CL, Magwood G, Zheng D, Hendrix K, Beck LS, Linnen F, Thomas V, Powell S, Ma’at I. 2004. Reducing disparities for African Americans with diabetes: Progress made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Public Health Rep 119(3):322–330.
Jetter KM, Cassady DL. 2005. The availability and cost of healthier food alternatives. Am J Prev Med 30(1):38–44.
Kaiser LL, Melgar-Quinonez HR, Lamp CL, Johns MC, Sutherlin JM, Harwood JO. 2002. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc 102(7):924–929.
Kreuter MW, McClure SM. 2004. The role of culture in health communication. Annu Rev Public Health 25:439–455.
Krieger N. 1994. Epidemiology and the web of causation: Has anyone seen the spider? Soc Sci Med 39(7):887–903.
Krieger N. 2001. A glossary for social epidemiology. J Epidemiol Community Health 55(10): 693–700.
Krieger N, Davey Smith G. 2004. “Bodies count” and body counts: Social epidemiology and embodying inequality. Epidemiol Rev 26(1):92–103.
Kumanyika SK. 1994. Obesity in minority populations: An epidemiologic assessment. Obes Res 2(2):166–182.
Kumanyika SK. 2005. Obesity, health disparities, and prevention paradigms: Hard questions and hard choices. Prev Chronic Dis [Online]. Available: http://www.cdc.gov/Pcd/issues/2005/oct/05_0025.htm [accessed July 23, 2006].
Kumanyika SK, Golden PM. 1991. Cross-sectional differences in health status in U.S. racial/ ethnic minority groups: Potential influence of temporal changes, disease, and lifestyle transitions. Ethn Dis 1(1):50–59.
Kumanyika SK, Grier S. 2006. Targeting interventions for ethnic minority and low-income populations. In: Paxon C, ed. Future Child 16(1):187–207.
Kumanyika SK, Gary TL, Lancaster KJ, Samuel-Hodge CD, Banks-Wallace J, Beech BM, Hughes-Halbert C, Karanja N, Odoms-Young AM, Prewitt TE, Whitt-Glover MC. 2005. Achieving healthy weight in African-American communities: Research perspectives and priorities. Obes Res 13(12):2037–2047.
Lavizzo-Mourey R, Richardson WC, Ross RK, Rowe JW. 2005. A tale of two cities. Health Aff 24(2):313–315.
Levy SR, Anderson EE, Issel LM, Willis MA, Dancy BL, Jacobson KM, Fleming SG, Copper ES, Berrios NM, Sciammarella E, Ochoa M, Hebert-Beirne J. 2004. Using multilevel, multisource needs assessment data for planning community interventions. Health Promot Pract 5(1):59–68.
Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. 2004. Childhood adiposity as a predictor of cardiac mass in adulthood: The Bogalusa Heart Study. Circulation 110(22): 3488–3492.
Liburd LC, Jack L Jr, Williams S, Tucker P. 2005. Intervening on the social determinants of cardiovascular disease and diabetes. Am J Prev Med 29(5 Suppl 1):18–24.
Lloyd LK, Cook CL, Kohl HW. 2005. A pilot study of teachers’ acceptance of a classroom-based physical activity curriculum tool: Take 10!®Texas Assoc Health Phys Educ Rec Dance J 73(3):8–11.
Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. 2003. Association between clinically meaningful behavior problems and overweight in children. Pediatrics 112(5): 1138–1145.
Lurie N, Jung M, Lavizzo-Mourey R. 2005. Disparities and quality improvement: Federal policy levers. Health Aff 24(2):354–364.
Lynch JW, Kaplan GA, Shema SJ. 1997. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med 337(26): 1889–1895.
Ma’at I, Owens M, Hughes M. 2002. Observations from the CDC. REACH 2010 coalitions: Reaching for ways to prevent cardiovascular disease and diabetes. J Womens Health 11(10):829–839.
Matheson DM, Varady J, Varady A, Killen JD. 2002. Household food security and nutritional status of Hispanic children in the fifth grade. Am J Clin Nutr 76(1):210–217.
MBDA (Minority Business Development Agency). U.S. Department of Commerce. 1999. Minority Population Growth: 1995–2050. [Online]. Available: http://www.mbda.gov/documents/mbdacolor.pdf [accessed June 16, 2006].
McAllister CL, Green BL, Terry MA, Herman V, Mulvey L. 2003. Parents, practitioners, and researchers: Community-based participatory research with early Head Start. Am J Public Health 93(10):1672–1679.
McEwen BS. 2001. From molecules to mind: Stress, individual differences, and the social environment. Ann NY Acad Sci 935:42–49.
Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. 2006. Trends in the association of poverty with overweight among U.S. adolescents, 1971–2004. J Am Med Assoc 295(20):2385–2393.
Narayan KM, Hoskin M, Kozak D, Kriska AM, Hanson RL, Pettitt DJ, Nagi DK, Bennett PH, Knowler WC. 1998. Randomized clinical trial of lifestyle interventions in Pima Indians: A pilot study. Diabet Med 15(1):66–72.
National Diabetes Information Clearinghouse. 2005. National Diabetes Statistics. [Online]. Available: http://diabetes.niddk.nih.gov/dm/pubs/statistics/index.htm [accessed July 12, 2006].
NCHS (National Center for Health Statistics). 2005. Health United States, 2005 with Chartbook on Trends in the Health of Americans. Hyattsville, MD: NCHS. [Online]. Available: http://www.cdc.gov/nchs/data/hus/hus05.pdf [accessed February 11, 2006].
New York City Department of Health and Mental Hygiene. 2006. Obesity in Early Childhood: More Than 40% of Head Start Children in NYC Are Overweight or Obese. [Online]. Available: http://www.nyc.gov/html/doh/downloads/pdf/survey/survey-2006 childobesity.pdf [accessed April 9, 2006].
Nord M, Andrews M, Carlson S. 2005. Household Food Security in the United States, 2004. Economic Research Report Number 11. Washington, DC: Economic Research Service, U.S. Department of Agriculture.
North KE, MacCluer JW, Williams JT, Welty TK, Best LG, Lee ET, Fabsitz RR, Howard BV. 2003. Evidence for distinct genetic effects on obesity and lipid-related CVD risk factors in diabetic compared to nondiabetic American Indians: The Strong Heart Family Study. Diabetes Metab Res Rev 19(2):140–147.
NRC (National Research Council). 2001. New Horizons in Health: An Integrative Approach. Washington DC: National Academy Press.
NRC. 2006a. Hispanics and the Future of America. Washington DC: The National Academies Press.
NRC. 2006b. Multiple Origins, Uncertain Destinies: Hispanics and the American Future. Washington DC: The National Academies Press.
NRC and IOM. 2000. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington DC: National Academy Press.
NRC and IOM. 2004. Children’s Health, the Nation’s Wealth. Washington, DC: The National Academies Press.
Oeltmann JE, Liese AD, Heinze HJ, Addy CL, Mayer-Davis EJ. 2003. Prevalence of diagnosed diabetes among African-American and non-Hispanic white youth, 1999. Diabetes Care 26(9):2531–2535.
Ogden CL, Carroll MD, Flegal KM. 2003. Epidemiologic trends in overweight and obesity. Endocrinol Metab Clin N Am 32(4):741–760, vii.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. 2006. Prevalence of overweight and obesity in the United States, 1999–2004. J Am Med Assoc 295(13): 1549–1555.
Ogunwole SU. 2006. We the People: American Indians and Alaska Natives in the United States. Census 2000 Special Reports. U.S. Census Bureau. [Online]. Available: http://www.census.gov/prod/2006pubs/censr-28.pdf [accessed July 31, 2006].
Parsons TJ, Power C, Logan S, Summerbell CD. 1999. Childhood predictors of adult obesity: A systematic review. Int J Obes Relat Metab Disord 23(Suppl 8):S1–S107.
Pinhas-Hamiel O, Zeitler P. 2005. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr 6(5):693–700.
Popkin BM, Udry JR. 1998. Adolescent obesity increases significantly in second and third generation U.S. immigrants: The National Longitudinal Study of Adolescent Health. J Nutr 128(4):701–706.
Powell LM, Slater S, Chaloupka FJ. 2004. The relationship between community physical activity settings and race, ethnicity and socioeconomic status. Evidence-Based Prev Med 1(2):135–144.
Pyramid Communications. 2003. Communities Helping Children Be Healthy: A Guide to Reducing Childhood Obesity in Low-income African-American, Latino and Native American Communities. [Online]. Available: http://www.rwjf.org/files/publications/HealthyChildren.pdf [accessed March 13, 2006].
Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, Steer C, Sherriff A. 2005. Early life risk factors for obesity in childhood: Cohort study. Br Med J 330(7504):1357– 1364.
Robert SA, House JS. 2000. Socioeconomic inequalities in health: Integrating individual-, community-, and societal-level theory and research. In: Abrecht GL, ed. Handbook of Social Studies in Health and Medicine. New York: Sage Publications.
Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, Pruitt LA, Powell TM, Owens AS, Thompson NS, Flint-Moore NM, Davis GJ, Emig KA, Brown RT, Rochon J, Green S, Varady A. 2003. Dance and reducing television viewing to prevent weight gain in African-American girls: The Stanford GEMS pilot study. Ethnic Dis 13(1 Suppl 1):S65–S77.
Rogers EM. 2003. Diffusion of Innovations, 5th ed. New York, NY: Free Press.
Rosenbloom AL. 2002. Fetal nutrition and insulin sensitivity: The genetic and environmental aspects of “thrift.” J Pediatr 141(4):459–462.
Rosenbloom AL, Joe JR, Young RS, Winter WE. 1999. Emerging epidemic of type 2 diabetes in youth. Diabetes Care 22(2):345–354.
Ruiz-Beltran M, Kamau JK. 2001. The socio-economic and cultural impediments to well-being along the US-Mexico border. J Community Health 26(2):123–132.
Sallis JF, Glanz K. 2006. The role of built environments in physical activity, eating, and obesity in childhood. In: Paxon C, ed. Future Child 16(1):89–108.
Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. 2006. An ecological approach to creating active living communities. Annu Rev Public Health 27:297–322.
Sherry B, Mei Z, Scanlon KS, Mokdad AH, Grummer-Strawn LM. 2004. Trends in state-specific prevalence of overweight and underweight in 2- through 4-year-old children from low-income families from 1989 through 2000. Arch Pediatr Adolesc Med 158(12): 1116–1124.
Sloane D, Nascimento L, Yancey AK, Flynn G, Lewis LB, Guinyard JJ, Diamant A, Galloway-Gilliam L, Yancey AK. 2006. Assessing resource environments to target prevention interventions in community chronic disease control. J Health Care Poor Underserved 17(2):146–159.
Srinivasan SR, Myers L, Berenson GS. 2002. Predictability of childhood adiposity and insulin for developing insulin resistance syndrome (syndrome X) in young adulthood: The Bogalusa Heart Study. Diabetes 51(1):204–209.
Stewart JA, Dennison DA, Kohl HW, Doyle A. 2004. Exercise level and energy expenditure in the Take 10!® in-class physical activity program. J School Health 74(10):397–400.
Strauss RS, Knight J. 1999. Influence of the home environment on the development of obesity in children. Pediatrics 103(6):e85.
Strauss RS, Pollack HA. 2001. Epidemic increase in childhood overweight, 1986–1998. J Am Med Assoc 286(22):2845–2848.
TFAH (Trust for America’s Health). 2005. F as in Fat: How Obesity Policies are Failing in America 2005. Washington, DC: The Trust for America’s Health. [Online]. Available: http://healthyamericans.org/reports/obesity2005/Obesity2005Report.pdf [accessed May 9, 2006].
Thomson Medstat. 2006. Childhood Obesity: Costs, Treatment Patterns, Disparities in Care, and Prevalent Medical Conditions. Research brief. [Online]. Available: http://www.medstat.com/pdfs/childhood_obesity.pdf [accessed February 2, 2006].
Troiano RP, Flegal KM. 1998. Overweight children and adolescents: Description, epidemiology, and demographics. Pediatrics 101(3):497–504.
Tucker P, Liao Y, Giles WH, Liburd L. 2006. The REACH 2010 logic model: An illustration of expected performance. Prev Chronic Dis [Online]. Available: http://www.cdc.gov/Pcd/issues/2006/jan/05_0131.htm [accessed July 23, 2006].
Unger JB, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. 2004. Acculturation, physical activity, and fast-food consumption among Asian-American and Hispanic adolescents. J Community Health 29(6):467–481.
USDA (U.S. Department of Agriculture). 2006. WIC Farmers’ Market Nutrition Program. [Online]. Available: http://www.fns.usda.gov/wic/FMNP/FMNPfaqs.htm [accessed June 13, 2006].
van der Kolk BA, Fisler RE. 1994. Childhood abuse and neglect and loss of self-regulation. Bull Menninger Clin 58(2):145–168.
Villa-Caballero L, Caballero-Solano V, Chavarria-Gamboa M, Linares-Lomeli P, Torres-Valencia E, Medina-Santillan R, Palinkas LA. 2006. Obesity and socioeconomic status in children of Tijuana. Am J Prev Med 30(3):197–203.
Whitaker RC, Orzol SM. 2006. Obesity among US urban preschool children: Relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med 160(6):578–584.
Williams DR, Collins C. 1995. U.S. socioeconomic and racial differences in health: Patterns and explanations. Annu Rev Sociol 21(1):349–386.
Williams DE, Cadwell BL, Cheng YJ, Cowie CC, Gregg EW, Geiss LS, Engelgau MM, Narayan KM, Imperatore G. 2005. Prevalence of impaired fasting glucose and its relationship with cardiovascular disease risk factors in U.S. adolescents, 1999–2000. Pediatrics 116(5):1122–1126.
Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. 2002. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord 26(8): 1075–1082.
Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. 2002. Contribution of major diseases to disparities in mortality. N Engl J Med 347(20):1585–1592.
Yancey AK, Lewis LB, Sloane DC, Guinyard JJ, Diamant AL, Nascimento LM, McCarthy WJ. 2004. Leading by example: A local health department-community collaboration to incorporate physical activity into organizational practice. J Public Health Manage Pract 10(2):116–123.
Yancey AK, Robinson RG, Ross RK, Washington R, Goodell HR, Goodwin NJ, Benjamin ER, Langie RG, Galloway JM, Carroll LN, Kong BW, Leggett CJ, Williams RA, Wong MJ, American Heart Association Advocacy Writing Group. 2005. Discovering the full spectrum of cardiovascular disease: Minority Health Summit 2003: Report of the Advocacy Writing Group. Circulation 111(10):e140–e149.
Yancey AK, Ortega AN, Kumanyika SK. 2006a. Effective recruitment and retention of minority research participants. Annu Rev Pub Health 27:1–28.
Yancey AK, Ory M, Davis SM. 2006b. Dissemination of physical activity promotion interventions in underserved populations. Am J Prev Med. 31(4S):82–91.
Yancey AK, Simon PA, McCarthy WJ, Lightstone AS, Fielding JE. 2006c. Ethnic and sex variations in overweight self-perception: Relationship to sedentariness. Obesity 14(5):1–9.
Yancy CW, Benjamin EJ, Fabunmi RP, Bonow RO. 2005. Discovering the full spectrum of cardiovascular disease: Minority Health Summit 2003: Executive summary. Circulation 111(10):1339–1349.
Yu S. 2006. The life-course approach to health. Am J Public Health 96(5):768.
Zephier E, Himes JH, Story M, Zhou X. 2006. Increasing prevalences of overweight and obesity in Northern Plains American Indian children. Arch Pediatr Adolesc Med 160(1): 34–39.
Zimring C, Joseph A, Nicoll GL, Tsepas S. 2005. Influences of building design and site design on physical activity: Research and intervention opportunities. Am J Prev Med 28(2 Suppl 2):186–193.



































