5
Pilot Tests and Assessment of Their Impact
INTRODUCTION
Moderator: Dr. Julia Rowland
This session of the workshop addresses pilot tests of survivorship care planning and efforts under way to assess their impact. Craig Earle describes the LIVESTRONG™ Survivorship Center of Excellence Network, which is supported by the Lance Armstrong Foundation. The role that the American Society of Clinical Oncology’s Quality Oncology Practice Initiative (QOPI) could potentially play to improve survivorship care is then discussed by Patricia Ganz. Martin Brown illustrates the potential for research networks to promote applied survivorship research with the success of the National Cancer Institute’s HMO Cancer Research Network in carrying out cancer-related health services research. Peter Bach then describes the Centers for Medicare and Medicaid Services’ (CMS) 2006 Oncology Demonstration Program as an effort to learn more about the status and quality of contemporary cancer care. Lastly, Craig Earle returns to present a comprehensive evaluation and research agenda for survivorship research.
LIVESTRONG™ SURVIVORSHIP CENTER OF EXCELLENCE NETWORK
Presenter: Dr. Craig Earle
The Lance Armstrong Foundation (LAF) plans to accelerate progress in addressing the complex needs of the rapidly growing number of cancer
survivors through a collaborative network established to meet the following goals:
-
Transform how survivors are perceived, treated, and served;
-
Help create a body of knowledge, understanding, and evidence;
-
Develop and deliver evidence-based treatment and care interventions;
-
Increase the quality and integration of survivorship services;
-
Strengthen linkages between survivorship services and primary cancer treatment and care;
-
Increase accessibility to services among ethnically diverse and underserved survivors;
-
Create insurance and reimbursement mechanisms to cover survivors’ care and services; and
-
Help find sources of support to sustain survivorship centers over the long term.
In establishing these goals, the LAF recognized the complexity of survivorship care, the relative lack of experience with long-term survivorship care, and the lack of training available for providers of survivorship care.
Centers of excellence have been established in five locations: (1) Memorial Sloan-Kettering Cancer Center in New York City; (2) Dana-Farber Cancer Institute in Boston; (3) Fred Hutchinson Cancer Research Center in Seattle; (4) the University of Colorado in Denver; and (5) the Jonsson Comprehensive Cancer Center at the University of California, Los Angeles. These centers will be involved in the following activities:
-
Collaborative clinical, biomedical, psychosocial, and health services research;
-
Accessible, relevant, and integrated quality care and services;
-
Development and testing of new medical, psychosocial, and behavioral interventions;
-
Dissemination and delivery of new information, interventions, and best practices to those in need; and
-
Training the next generation of health care professionals, social service providers, and researchers.
Each center of excellence will develop its own network of community-based centers, which will provide direct services locally to survivors in traditionally underserved areas. Figure 5-1 shows the interactions among the LAF, the centers of excellence, and their affiliated network of community-based centers.
The LAF invited selected cancer centers to respond to a “closed” request for proposals (RFP). The following additional four cancer programs
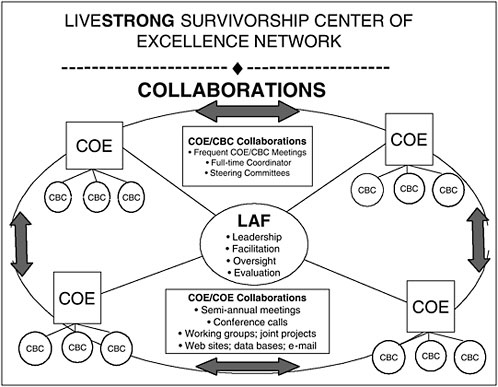
FIGURE 5-1 Interactions among participants in the Lance Armstrong Foundation Center of Excellence Network.
SOURCE: Earle, 2006.
are not officially part of the network but have received support to develop their survivorship programs:
-
Cook Children’s Medical Center in Fort Worth, Texas;
-
University of Pennsylvania in Philadelphia;
-
Nevada Cancer Institute in Las Vegas; and
-
Rainbow Babies and Children’s Hospital in Cleveland, Ohio.
The plan is to harness the expertise, experience, creativity, and productivity of the leading centers and have them share their knowledge and resources to improve the delivery of services to survivors. This collaboration is expected to accelerate the progress in cancer survivorship. The development of a standardized Survivorship Care Plan is one of the priorities of the network. The centers have a coordinated development plan under way to pilot test templates at the centers of excellence and their community-based partners. This program will serve as a large laboratory to promote quality cancer survivorship care.
Discussion
Dr. David Poplack of Texas Children’s Cancer Center asked Dr. Earle about planned initiatives in the area of education and training, pointing out that awareness of survivorship issues and care is absent from most contemporary programs. In fact, it is possible for a pediatrician to go through training and never rotate through a hematology or oncology unit. Dr. Shulman of the Dana-Farber Cancer Institute confirmed that at his institution the house staff are spending less and less time in cancer medicine and are spending almost no time in the ambulatory setting, which is where survivors are seen. There is a training system in place that will graduate a group of primary care doctors who have essentially no experience in this area.
Dr. Earle acknowledged the importance of training, adding that physicians need not become experts in oncology, but they need at least to recognize what the potential issues are when dealing with a cancer survivor and have some idea of what to do and whom to refer to. The Dana-Farber Center of Excellence is affiliated with a rural oncology practice in New Hampshire and is collaborating with an urban community health center and centers in New England that deliver pediatric cancer care. Specialists in the center will be working with community-based primary care physicians, pediatricians, and pediatric oncologists to raise awareness of survivorship issues and how to address them.
Dr. Lee Newcomer of the UnitedHealth Group asked Dr. Earle to describe how the Centers of Excellence would know if they were successful in 3 years and how they planned to measure the achievement of success. The centers have been measuring patient satisfaction and acceptance as well as knowledge gained following interactions with the clinic. Dr. Earle recognized the importance of looking at some other outcomes, such as anxiety, and those relating to the coordination of the transition out of cancer therapy. Dr. Lawrence Shulman suggested that the measure of the network’s success will be the pace of accomplishment and the creation of collaborative efforts. Ms. Mary McCabe added that, in terms of outcomes or metrics for success, the collaborators from Memorial Sloan-Kettering decided to start with two very simple but realistic aspects of the program, feasibility and acceptability. The program changes the paradigm of care and extends it to include the survivorship period. Important questions are, “Can this be done in a cancer center?” and “Is it acceptable to the patients, the physicians, the nurses, and the referring primary care providers?” A survey will be conducted of these stakeholders to assess reactions to the program. Another metric to be used is adequacy of screening among cancer survivors followed in the institution.
In response to a question about future solicitations and participation in
the LAF effort, Ms. Caroline Huffman said that a steering committee is providing guidance and that, at this point, LAF plans to keep the closed RFP model. The Centers of Excellence Network is viewed as bold and filled with tremendous possibilities, but the immediate plans are to concentrate on getting the network launched and initiating the ambitious collaborative projects.
When questioned about educational materials used in the centers of excellence clinics, Dr. Earle reported that, although they were not using the Lance Armstrong LIVESTRONG™ notebook, they are incorporating all of its elements in structured letters to patients that include the treatment plan, the treatment summary, and the survivorship care plan. Structured consultation notes are sent to the primary care providers and the oncologists involved. Mr. Richard Boyajian added that the team at the Dana-Farber Cancer Institute is involved with BlueCross and BlueShield in the development and evaluation of a transition notebook for use among breast cancer survivors.
Clinics in this network will be working toward developing and testing a single template, rather than having each of the centers developing its own. An attempt is being made to satisfy both the academic and community-based providers.
Ms. Kathy Smolinski, representing the Association of Oncology Social Work, asked whether there are staffing standards for the centers of excellence. Dr. Earle responded that there were no standards, and that each center has developed staffing levels for its own setting. The program started with limited evidence and experience at hand. A tremendous amount has been learned in the past year and a half, as the clinic has taken on this relatively new area of survivorship care. Ms. McCabe, from the Memorial Sloan-Kettering Center of Excellence, added that while each of the centers has taken an institutional approach to what might work, the barriers and the goals for each of the centers are the same. This common purpose is behind the collaboration on specific tasks, such as the care plan and adherence to screening. There are some important areas in which there is agreement, but at the same time there is a realization that one size does not fit all. Dr. Earle mentioned that the issue of acceptability of survivorship clinics among oncology physicians is a critical one. Some physicians are very threatened by the idea of a specialized survivorship clinic, worrying that they will lose their patients if such a program is available.
Dr. Patricia Ganz of the University of California, Los Angeles described the diversity represented in the five centers of excellence. Three are freestanding cancer centers, and two are state-funded university programs. All are comprehensive cancer centers, but they vary in their level of resources. The kinds of models that each center develops will reflect this diversity and that which exists in the various community-based partners. Oncology care
delivered in America varies greatly by geography and setting, and different models of excellence are likely to emerge to suit specific environments.
QUALITY ONCOLOGY PRACTICE INITIATIVE
Presenter: Dr. Patricia Ganz
Several years ago, as the American Society of Clinical Oncology (ASCO) embarked on the National Initiative on Cancer Care Quality (NICCQ), it became very apparent to the highly skilled health services researchers who were running that project how arduous it was to collect oncology data from medical chart reviews. The study involved reviews of 1,600 patients in multiple cities. Unlike other data collection efforts related to diabetes, arthritis, and heart disease, the review of oncology care was complicated by records being in multiple places, completed by different kinds of providers, and organized in a nonstandard fashion. The record abstractors felt lucky if the record included an initial consultation note that might have spelled out the planned treatment or a flow sheet that captured the course of treatment received. Often, however, a nurse abstractor had the arduous task of going through every page of the record to find out what drug doses were delivered and if a doctor followed the recommended prescription for the adjuvant therapy.
It became clear to ASCO that if the professional society was going to advance quality-of-care assessment, there needed to be a better way of getting this kind of data in a systematic way. With the publication of the Institute of Medicine (IOM) report on cancer survivorship, it became clear that survivorship care planning depends on having accurate and accessible diagnostic and treatment information.
Dr. Deborah Schrag discussed in her presentation the steps that have been taken to establish the content for the treatment summary (see Chapter 2). To test the draft template, five oncologists involved in ASCO’s QOPI volunteered to try it in their group practices. Two versions were tested in practices, most of which did not have an electronic medical record; a paper-and-pencil and a dictatable form. Both formats seemed relatively easy to use. The dictated form obtained more information because physicians may have felt obligated to go back through the chart and dictate it as they would a discharge summary. The paper version was completed more quickly than the dictated form.
Disease-specific formats are undergoing development to be tested further within the QOPI network because there are common regimens for treatment that can be prefilled, making completion of the form easier. For hematologic cancers, it may be difficult to decide when a patient needs an
end-of-treatment summary, since for many of those individuals the disease may be chronic in nature.
Based on this pilot work, it is clear that more work is needed on the treatment summary. Physicians pilot testing the form felt strongly that it needs to be brief. The form needs to synthesize succinctly what went on without summarizing the entire chart. That said, some medical oncologists have indicated that they want the information to be comprehensive and complete so that the form could meet other recordkeeping requirements. It will be critical to communicate the purpose and intent of the treatment summary so that the appropriate elements are included on the standardized template.
In terms of next steps, plans are to revise the forms and then broaden the participation into more QOPI practices. The development process will be iterative and will involve getting buy-in from all users. Physician and nurse buy-in is a prerequisite to success. Ultimately, the design of the template has to be adapted for electronic medical records. ASCO is actively pursuing development of an oncology electronic record because those that are available for primary care physicians are not well suited for oncology.
Dr. Rowland commented on the strictly medical content of the draft templates and wondered what would happen if one added a psychosocial component. Dr. Ganz responded by pointing out that the template is meant to be a conversation piece. Like the informed consent form, it is not just signing the document that is important. Transfer of information depends on the verbal communication, the other supplementary materials given to the patient, and then the reiteration of the information at every visit. Even though the form is short, the piece of paper should be associated with a very lengthy conversation, and it is something that the patient takes away. These tools can serve as a catalyst for these in-depth conversations. The written records are especially important, because patients do not always have access to their medical records and may need them in the case of natural disasters or doctors closing their practices. Having a concise synoptic statement of what went on can go a long way to facilitate the conduct of conversations.
Some doctors are better at engaging in these conversations than others. Perhaps survivors can be encouraged and activated to ask at the end of treatment “Well, how am I going to be followed now? How are you going to know if my cancer is coming back?” When these questions arise, physicians will at least have a document with the medical aspects of care spelled out. We hope it is going to be backed up in many practices with the resource information that Ms. Diane Blum described in her presentation (see Chapter 4). Physicians, as part of their posttreatment conversation should be ready to say, “By the way, I know this is a very stressful period; would you want to talk to the social worker who works with me or the
support group that I think would be helpful to you?” Setting time aside to have a conversation is what the Survivorship Care Plan template will facilitate. It is a starting point, and there is agreement that we have to get started.
Dr. Michael Fordis of Baylor College of Medicine mentioned the possibility of granting credit for continuing medical education (CME) as an incentive for using the Survivorship Care Plan template. Some CME credits are being granted to individuals who are participating in quality improvement initiatives. Maintenance of certification was mentioned as another potential incentive, but the experience nationally is that relatively few providers participate in quality programs in response to this incentive. Dr. Ganz pointed out that there is a large group of physicians who completed their training more than 10 years ago and who are now required to do something for their American Board of Internal Medicine recertification. This may provide an impetus for some to participate in the QOPI project. The initial cohort of QOPI participants was motivated by competition and an interest in peer evaluation. Once there is agreement on the treatment summary, its completion could be considered for inclusion in the QOPI quality measure set. This may occur in the next 2 to 3 years. ASCO is discussing with the National Committee for Quality Assurance (NCQA) the potential for a physician certification program in oncology, which could be based on the QOPI initiative.
Dr. Al Marcus of the AMC Cancer Research Center agreed with the need for treatment summaries and care plans as recommended in the IOM report and elsewhere. He pointed out that pilot tests are under way to assess usability and feasibility, but in the long term he thought that these care plans must be evaluated for their effects on important survivorship outcomes. Such evidence will be needed to persuade payers and others that survivorship care planning is an essential component of care.
THE HMO CANCER RESEARCH NETWORK
Presenter: Dr. Martin Brown
The Cancer Research Network (CRN) is a cooperative agreement supported by the National Cancer Institute. It consists of research organizations affiliated with 12 large nonprofit health maintenance organizations in the United States, including:
-
Six Kaiser Permanente affiliates (Southern California, Northern California, Oregon, Hawaii, Georgia, and Colorado);
-
Group Health Cooperative, Seattle, Washington;
-
Lovelace Sandia Health Clinic, Albuquerque, New Mexico;
-
Henry Ford Health System, Detroit, Michigan;
-
Health Partners, Minneapolis, Minnesota;
-
Harvard Pilgrim Health Care, Boston, Massachusetts;
-
Meyers Primary Care Institute, Worcester, Massachusetts.
The CRN is a resource for which there are potential partnerships for survivorship research. The network, originally funded in 1999, has been approved for renewal. Support will depend on peer review and the budget of the National Cancer Institute (NCI) in 2007. If all goes well, this network will be an available resource for at least 5 more years. The network is ideally suited for pilot testing a treatment summary and care plan, because the researchers in this network have access to health care systems that will provide care to 15 million individuals by 2007. There were 37,503 incident cancers in the network in 2003. CRN is especially well suited for studies of survivorship and long-term outcomes because the majority of health maintenance organization (HMO) members diagnosed with cancer remain enrolled. Five-year retentions rates were 84 percent.
Most of the health systems involved in the CRN have integrated delivery systems and are on the cutting edge of having comprehensive and integrated health information technology systems. These networks already have automated data on enrollment, utilization, laboratory, pharmacy, and hospitalizations. They are all in the third or fourth year of installing electronic medical records, and most of them are using the same vendor for the electronic medical record. An oncology module is under development and will be used across the network. All the networks are in the process of building extensive Web applications to connect the management, the providers, and the patients of these networks. All of these resources are potentially available for researchers who want to conduct intervention studies or surveillance studies. Many of the sites have established linkages to local Surveillance Epidemiology and End Results (SEER) tumor registries or maintain a local tumor registry.
There are several components of existing studies that relate to survivorship. For example, one study assessed the efficacy of prophylactic mastectomy for women at high risk for breast cancer. From that study a follow-up cohort was constructed, and those women are being questioned about their survivorship experience. Other studies are assessing psychosocial issues, late effects of treatment, and palliative and end-of-life care. The network has established a survivorship interest group, so there is interest and experience in this area. External members are welcome to join the survivorship special interest group.
The network is open to the general research community. External investigators can propose studies to the network. The network has an informatics resource that can do quick turnaround feasibility analyses to determine how many patients are available, what kind of information is
available on these patients through electronic medical records, what type of patient is not available, and types of information that would require chart review or a special survey.
A study can proceed if it is feasible, there is an interested scientific partner in the network, and funding is available. Numerous studies have been undertaken in collaboration with outside investigators. To make the CRN more accessible to outside investigators, NCI is mandating in the renewal requests for applications that additional resources go into a collaboration core, which will have dedicated resources to facilitate even quicker and better kinds of studies. NCI is considering the possibility of a funded competitive supplemental program dedicated to researchers who want to do collaborative studies. This would be something of a fast-track mechanism for getting these collaborative studies up and going.
A recent issue of the Journal of the NCI Monograph (No. 35, 2005) is exclusively devoted to the CRN. It includes a very detailed description of its structure, function, and governance and about 18 research articles, some of them related to survivorship research.
Discussion
Dr. Rowland highlighted an attractive feature of the CRN, that investigators may access family data because families are usually enrolled in the systems of care. A study can therefore include outcomes not only of the survivor, but also of the secondary survivors’ health care utilization. The CRN also allows assessments of the costs associated with interventions and with utilization. This is a unique platform to ask some of the very questions that have been raised during the workshop about the role of care plans and their potential benefits for patients and their families, payers, and society.
Dr. Tim Byers, of the University of Colorado Cancer Center, asked Dr. Brown to comment on the availability of funding to support external investigators who wish to collaborate with the CRN. Dr. Brown expects that when the new grant starts up again in March 2007, there will be substantial pilot funds in the grant. However, if an investigator wants to do a major study in collaboration with the CRN, they will have to apply for RO1 funding through the usual processes. The competitive supplemental funding mechanisms mentioned may be available in a year or two. Some other funding mechanisms might be relevant. One is a program announcement for economic studies. It does not have any funds associated with it, but these program announcements have been very useful in channeling grants to the right program directors and study sections. The applicants are advised to some degree, and they have been quite successful. Cathy Bradley has done some very interesting work on the employment experience of
cancer survivors. She has had several grants funded through this program announcement.
There is also a program announcement on the use of health claims data for health services research. This has been used primarily to fund research using the SEER-Medicare database, which is maintained by NCI, but it could also be used for analyses of other types of health claims
THE CENTERS FOR MEDICARE AND MEDICAID SERVICE’S 2006 ONCOLOGY DEMONSTRATION PROGRAM
Presenter: Dr. Peter Bach
CMS conducts demonstration projects to identify and evaluate new approaches to health services delivery and/or reimbursement. There are many examples of demonstration projects turning into programmatic initiatives. One example is Medicare Advantage, which is a system in which private plans receive a capitated payment amount for each Medicare beneficiary who chooses to receive all their care from the plan. The Medicare Part D program, which pays for prescription drugs, also began as a demonstration program. CMS is actively experimenting with different strategies, for example, paying for quality metrics or paying for efficiency, in an effort to move toward a delivery system that enhances quality and is patient centered.
An oncology demonstration program began in 2005 to evaluate the use of billing codes to gather data on cancer patient symptoms. Oncologists submitted symptom G codes in association with codes used for infusion chemotherapy administration. Under Medicare’s fee-for-service system, a doctor submits a bill on a form (called the 1500 form) and codes are filled in at the bottom of that bill signifying the patient’s diagnosis and the services delivered. For this demonstration, CMS created additional codes to capture physician assessments of pain control, nausea and vomiting, and fatigue. Physicians were paid $130 for reporting on these three symptoms in association with a chemotherapy treatment visit. By the end of the year, more than 80 percent of oncologists were submitting data on chemotherapy patients’ symptoms using these billing codes. This demonstration provided the proof of principle that the billing system could work to capture data on important patient outcomes. Mathematica has a contract to evaluate these data and summarize lessons learned from this demonstration.
The 2005 demonstration was limited to patients undergoing intravenous chemotherapy, and there was interest in broadening the scope of measurement to extend to all cancer patients along the continuum of care. In addition, there was an interest in developing longitudinal measures of efficiency, that is, getting similar or better outcomes and well-coordinated
|
BOX 5-1 Cancer Types Covered in the CMS 2006 Oncology Demonstration Project
SOURCE: Bach, 2006. |
care for less cost. Longitudinal data are also need to assess alternative payment mechanisms, such as prospective or capitated payment.
Several steps have been taken in 2006 to augment the oncology demonstration program. In 2006, the demonstration will apply to nearly all oncology patient visits, insofar as it will rely on evaluation and management codes (called E&M codes) instead of G codes. Physicians use E&M codes for doctor-patient interactions when the focus is on problems and care planning. This shift in emphasis also removed the incentive for intravenous treatments in place of alternative therapeutic choices, such as oral chemotherapy.
Under the 2006 demonstration, physicians submit claims for every E&M visit, a process that creates a longitudinal record of claims. CMS is paying $23 for each of these reports. This reimbursement level is lower per claim ($130 in 2005), but physicians can apply the E&M code to more of their patients. New measures have been incorporated into the 2006 demonstration, including disease status, visit focus, and guideline adherence for each patient, on each visit. CMS created codes for 13 cancers, representing about 85 percent of Medicare payments to hematologist oncologists and medical oncologists (Box 5-1).
CMS created a set of stratification disease status codes for each of these 13 cancer types. There is a total of 60 disease status codes with three to seven codes per cancer type.
Having measures of disease status was felt to be more valuable than having information on stage alone. A patient’s disease status can change over time. The six disease status codes for colon cancer shown in Figure 5-2 incorporate information on stage.
The colon cancer codes include five categories representing a hybrid of stage of presentation and current disease status, for example, presence of
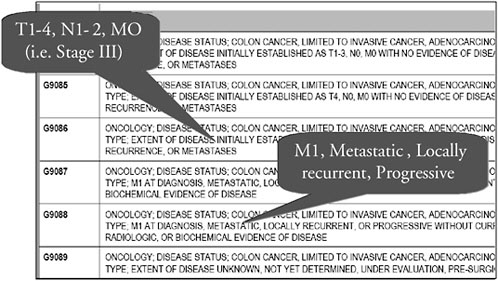
FIGURE 5-2 Colon cancer disease status codes.
SOURCE: Bach, 2006.
recurrence or metastases. In creating these categories, there was some lumping and some splitting. Code G9086, for example, is stage III colon cancer after surgery, representing an important subgroup of patients who benefit from adjuvant chemotherapy. In contrast, code G9088 represents a mix of patients, ones presenting with metastatic disease as well as ones developing local recurrences and metastatic disease after diagnosis. The sixth category, code G9089, represents the situation when extent of disease is unknown, is not yet determined, or under evaluation.
Oncology visits typically address multiple issues, and, under the demonstration, clinicians are asked to code one of the following six activities as the predominant focus of the visit:
-
Work-up, evaluation, or staging;
-
Decision making, supervising therapy, or managing toxicity;
-
Disease surveillance;
-
Expectant management;
-
Palliative therapy or end-of-life care (life prolongation not anticipated); or
-
Other.
The 2006 demonstration also asks clinicians to report on their adherence to clinical practice guidelines issued by the National Comprehensive
Cancer Network (NCCN) and the American Society of Clinical Oncology. Much of cancer care for the 13 cancer types included in the demonstration is addressed by the guidelines of these two organizations. Clinicians, in reporting whether or not they have adhered to guidelines, can use one of the following response categories:
-
Yes, treatment adherent to guidelines;
-
No, patient on institutional review board (IRB)–approved clinical trial;
-
No, treating physician disagrees with guideline recommendations;
-
No, patient prefers alternative or no treatment;
-
No, patient comorbidity or performance status precludes guideline treatment;
-
There are no guidelines relevant to patient’s condition;
-
No, another reason.
The focus of CMS on guideline adherence is based on the belief that guidelines capture the current standards for most of cancer care. Most of the guidelines are evidence based, and the extent of the evidence supporting them is well annotated. When the guidelines are not evidence based, they are at least based on a consensus of current opinion. In addition, using guidelines is advantageous because they are generally kept up-to-date. Trying to use CMS codes to keep up with changing standards of oncology care would be difficult. An alternative to asking about guideline adherence would be to measure directly the application of particular elements of care for selected patient subgroups. Sometimes, such direct measures are embedded in the guidelines. Included in the NCCN guidelines, for example, is that stage III colon cancer patients after surgery should be offered adjuvant chemotherapy.
This demonstration will help CMS learn whether asking about guideline adherence is an effective way to measure quality of care. The demonstration will allow CMS to determine when physicians disagree with guidelines, what clinical situations are not well addressed, and when patients elect alternative treatments. Answers to these questions could inform medical educators, guideline developers, cancer advocacy and education, and research policy.
More needs to be learned about how patient preferences affect treatment decisions. If the 2006 demonstration data show that patients are making choices that run counter to current guidelines, for example, refusing radiotherapy when it is recommended, there will have to be further analyses to understand what factors underlie these decisions. Does this reflect patient preference, or does it represent the fact that there are no accessible radiotherapy facilities?
Dr. Bach provided an example of how the 2006 demonstration project measures adherence to the standard of offering stage III colon cancer patients adjuvant chemotherapy after surgery. To determine the proportion of patients for whom appropriate care is provided, a rate is assembled with a numerator and a denominator. The denominator includes patients with an ICD-9 code for colon cancer as well as the disease status code indicating stage III cancer. The focus of the visit would be coded “supervising treatment.” In this case, the physician would need to report whether their treatment conformed to the relevant guideline for treatment. They could indicate that the patient’s treatment adhered to guidelines or that the patient preferred alternative or no treatment. The physician reports can be validated using claims data. CMS pays for individual chemotherapies using J codes, so in this example, these claims can be used to assess whether adjuvant chemotherapy is actually provided. A preliminary look at data from January and February 2006 indicates that adjuvant therapy is provided in about 82 percent of cases of stage III colon cancer, according to physician reports. About 6 percent of patients are refusing this therapy.
The CMS 2006 oncology demonstration will provide some needed basic information on disease status and treatment patterns. This is information that even the cancer registries cannot provide. There may be opportunities to learn more about the frequency and timing of recurrence and cancer progression. The data may also provide valuable information on the proportion of care directed at palliation. Very preliminary data from the demonstration suggest that between 1 and 2 percent of cancer visits have palliation as a primary focus.
The CMS 2006 demonstration also permits some examination of the quality of cancer care. We will be able to document the extent to which oncologists are at least self-reporting that they are following practice guidelines. It may be possible to generate feedback reports to physicians to inform them how their practices compare with peers. Ultimately, the demonstration may form the basis for publicly reported information on oncology practices. A report card format could be used to present comparative information on local oncology practices. These hypothetical applications will require much more experience and evaluations of preliminary efforts. This demonstration may also help to build the groundwork for estimating prospective costs for disease management and for providing benchmarks for measures of efficiency.
Dr. Bach asked the workshop audience to consider whether the 2006 CMS oncology demonstration represents the right approach to measurement. A strength of the demonstration, in his view, is the reliance on guideline-based standards from the oncology community. The demonstration represents a departure from other CMS efforts, for example, the physi-
cian voluntary reporting program, in which internal standards have been developed.
There are many challenges ahead. Coordinating the codes and the guidelines represents a technical challenge. Importantly, the guidelines that are used in the program must be free of conflicts of interest. Agreement among stakeholders will need to be reached to determine how assurances for conflict-free guidelines can be made.
Discussion
Dr. James Talcott began the discussion by raising a concern about basing the oncology demonstration on guidelines that are both evidence based and based on expert opinion. There is sometimes a blurring of the distinction between these two types of guidelines. When experts are convened to develop guidelines, the recommendations for care often end up reflecting how these experts happen to practice. The consensus guidelines may not be consistent with evidence. Dr. Talcott also wanted clarification on potential conflicts of interest. Are the concerns related primarily to financial conflicts of interest? There is also an embedded self-interest of experts on the guideline committees that needs to be considered. Dr. Talcott asked if CMS has thought about the dependence on consensus guidelines as part of the CMS 2006 demonstration.
Dr. Bach responded that more rigor is needed in terms of the content of the guidelines, how CMS characterizes the guidelines, and how the doctors evaluate whether or not they are following them. How to balance the use of consensus-based standards versus evidence-based ones is very important. Presumably, the guidelines will improve as they receive more scrutiny. In many areas of oncology practice, there are limited data with which to determine best practices. This reflects a shortcoming of the current knowledge base, and the CMS demonstration is likely to help drive the development of further knowledge.
Dr. Sheldon Greenfield pointed out that physicians’ adherence to guidelines is usually not based on reports from the physicians who are being evaluated. Is it possible that the CMS 2006 demonstration is bringing about changes in practice by raising physicians’ awareness of available clinical practice guidelines? Dr. Bach agreed that there may be such an effect, whereby practices are influenced by the very act of measuring their performance. This “Hawthorne” effect is likely to diminish over time. There were many hits on the NCCN guideline website following the announcement of the 2006 demonstration. CMS expects clinicians to be familiar with the guidelines. Hospitals self-report their adherence to quality measures, and audits of the validity of these reports have been largely positive but mixed.
CMS will have to conduct validation studies through analyses of administrative records and some fieldwork.
Dr. Ganz asked whether participation in the 2006 demonstration is as high as that observed in the 2005 demonstration. What is required of physicians in 2006 is much more challenging. The reporting categorization and coding scheme is more complex and time-consuming in 2006. Dr. Bach replied that while data are preliminary and from only the first few months of the demonstration, participation appears to be high, with greater than 80 percent of physicians reporting data.
In the context of developing treatment summaries and care plans, Dr. Ganz asked if in 2 to 3 years agreement is reached on content and format, whether the use of these documents could be ascertained in the CMS demonstration system. Dr. Bach indicated that it would likely be relatively easy to integrate use of care plans into the demonstration, especially if a recommendation for the use of treatment and care plans were incorporated into recognized practice guidelines. Dr. Bach pointed out that the focus of the visit coding used in the 2006 demonstration has not broken out survivorship care planning. Ideally, one would like to be able to identify this aspect of care, but the rules of E&M coding are complex, and changing them can be quite involved. It is easier to nest this sort of information into the existing codes for focus of the visit.
Dr. Byers asked whether CMS’s quality improvement organizations (QIOs) could play a role in developing and demonstrating the effectiveness of treatment and care plans. Dr. Bach agreed that the QIOs could be a vehicle for independent demonstration projects. There are many examples of pilot projects carried out in a single state QIO. For example, studies have been conducted to see if mailing people fecal occult blood testing cards improves screening rates. QIOs have a quality measurement infrastructure that allows them to conduct such studies. QIOs are guided in their activities by a nationally established scope of work. Over time, it may be possible to incorporate aspects of survivorship care into those overarching goals set for the program. Before CMS would act to incorporate treatment and planning into programmatic initiatives, there would need to be evidence on effectiveness and related costs.
Dr. Byers asked if there were ways to identify the potential misuse of certain therapies. He pointed out that CMS sometimes pays for treatment that is contraindicated according to guidelines. Trastuzumab (Herceptin), for example, is sometimes prescribed for uses for which there is no evidence that it is effective. Dr. Bach responded by stating that CMS does not have a national coverage determination on Herceptin. This means that CMS does not regulate its use at the national level. The use of Herceptin is managed by CMS contractors, the local carriers. It is within their contractual discretion to monitor the appropriateness of drugs and tests. CMS will pay for
Herceptin for its listed off-label use in compendia. If CMS makes a national coverage determination on an intervention, then payment policies can be enforced. For example, CMS will not pay for an implantable cardiac defibrillator for anyone with an ejection fraction over 35 percent.
AN EVALUATION AND RESEARCH AGENDA
Presenter: Dr. Craig Earle
The IOM asserted in its recent report that survivorship care plans have strong face validity and can reasonably be assumed to improve care unless and until evidence accumulates to the contrary. The report recommended moving forward with implementation and at the same time engaging in applied research to define optimal models of delivery and quantify effects on survivors’ health and well-being. In the IOM report there is a strong recommendation for action and also a charge going out to the research community to accumulate the evidence surrounding use of survivorship care planning. Creating survivorship care plans is time-consuming and requires work from busy clinicians. Understanding the benefit to patients as well as the costs to health systems and providers will be important factors in disseminating survivorship care planning.
Research is needed to determine how the entire Survivorship Care Plan, in addition to the following elements of it, affect outcomes:1
-
Treatment summary;
-
Description of possible clinical course (e.g., expected recovery from acute toxicities);
-
Surveillance plan for recurrence and late effects;
-
Psychosocial issues and available resources; and
-
Lifestyle recommendations.
There are research questions associated with each of these elements. Are all of these elements needed for all cancer survivors? Are psychosocial interventions as important for a stage II colon cancer as they are for a woman with advanced breast cancer? Is the transition to survivorship really a teachable moment, or is it the case that lifestyle issues would be better addressed by a primary care provider 6 months later? These are empirical questions that need to be answered.
Research outcomes that could be considered occur at both the patient level and the systems level (Table 5-1).
|
1 |
This presentation is supplemented by a commissioned background paper prepared by Dr. Earle (see Appendix D.5). |
TABLE 5-1 Research Outcomes to Be Evaluated in Survivorship Research
|
Patient-Level Outcomes |
System-Level Outcomes |
|
|
|
SOURCE: Earle, 2006. |
|
The IOM survivorship focus groups indicated that satisfaction with care would improve with survivorship care planning. Some patients have the feeling that they have been abandoned by their oncologists. While there is a perception that doctors are not doing much for them in the posttreatment period, in reality, many things are being done. Perhaps providers need to discuss with patients what follow-up steps are being taken on their behalf. Explicitly sitting down and saying, “Here is what I have been doing for you; here is what I have been checking in your blood work in advance of your visit” might improve the patient’s communication, knowledge, and satisfaction.
Evaluating how survivorship care planning affects anxiety or depression is critically important, because while such planning is likely to address these issues for most patients, it may increase anxiety or depression for others. Implementing parts of the Survivorship Care Plan may assist in identifying late effects of cancer treatment, and if interventions are available there is the possibility of relieving symptoms and improving quality of life, functional status, and survival. Implementing surveillance strategies might identify second malignancies earlier or recurrences of cancer at a time when interventions could be beneficial. Survival could be considered as an outcome of studies evaluating survivorship care plans. However, surveillance studies require very large sample sizes to detect what are likely to be very small differences, and so survival may not necessarily be the main outcome by which to judge the success or failure of survivorship care planning.
There are also systems-level outcomes that can be considered in evaluations of survivorship care planning. These include communication and coordination of care studies that could focus on potential improvements in
linkages between specialty and primary care, as well as increased involvement of primary care physicians in posttreatment care.
Practice patterns and processes and quality of care—for example, whether appropriate mammography surveillance occurs following breast cancer treatment—could be affected by survivorship care planning and should be evaluated. Efficiency is a very important measure. Better coordinated, well-planned care is probably less costly. Care planning may help to avoid duplication of follow-up tests or unnecessary tests. If patients are well informed of their potential risks for late effects or recurrence, they may not receive MRIs for headaches or other tests that are not likely to be informative. Survivorship care planning could, however, result in care that is more expensive given the time and resources that will be needed to create and then implement the plan. Care planning would also result in people receiving tests who, without care planning, would not have received recommended surveillance. That is going to add to cost, one hopes with benefit, but it will add to cost. How survivorship care planning affects resource use and costs is an important area of research.
In testing survivorship care plans, attention will have to be paid to the needs of subpopulations. Individuals with different cancers may have distinct issues to be addressed. Age, race/ethnicity, socioeconomic status, and geography could all affect the optimal format and content of a care plan. For example, the format that might work best for an adolescent or young adult cancer survivor is probably different from a format suited to an elderly person with prostate cancer or colon cancer. The health of patients affects the health of their family members and other caregivers and so it is reasonable to also look at the effects of survivorship care planning on caregivers.
There are many researchable questions around the setting and personnel required for survivorship care planning. Demonstrations are needed to evaluate whether the responsibility for care planning should rest primarily with the oncology specialist, perhaps in conjunction with a nurse practitioner, a team in a dedicated survivorship clinic, or through a shared care model between the oncology and primary care provider. The optimal care delivery model will be likely to vary according to patient preference and circumstance. Demonstrations may also be tested to evaluate methods to financially support the delivery of services.
Various formats for care plans can also be tested, for example, structured oral consultations, written paper copy, or electronic formats. How structured or flexible the format needs to be to accommodate different clinical practices also needs to be assessed. Critical is determining the minimum essential elements of the care plan. Feasibility studies will be needed to see if some parts of the care plan can be automatically generated, for example, from electronic pharmacy record systems. It may be feasible to
develop and test Web-based systems that are accessible by both patients and their care providers.
Several types of research study designs may be applied to these various questions. Qualitative research, such as focus groups and interviews, can identify potential barriers to implementation and strategies to overcome them. Observational studies, such as cross-sectional surveys of patients, may be instructive to assess knowledge, needs, and gaps in care delivery. Answers to some questions pertaining to surveillance patterns may be ascertained through medical record review or analyses of administrative data. Prospective cohort studies may also be informative. For example, a cohort study that included a baseline measurement of knowledge, anxiety, or other outcome of interest and then provided patients with all or part of the Survivorship Care Plan could help determine how that variation in plan content affects outcome.
Quasi-experimental studies, in which the experience before and after administering care planning is assessed, could be informative. There may also be some natural experiments in which comparisons could be made between clinics that, for example, implemented just the treatment summary and those that implemented both the treatment summary and the care plan.
Finally, randomized controlled trials could be conducted on aspects of patient follow-up. Such trials are expensive and logistically difficult, but they are very informative. Eva Grunfeld is an investigator who has completed several trials on alternative follow-up strategies for women with breast cancer.2 Clinical trials would provide the best evidence on how outcomes are affected by survivorship care planning. For the questions pertaining to economic resource utilization, trials may be the only mechanism to obtain good estimates. One of the challenges to conducting randomized trials will be contamination. If randomization occurs at the level of a patient, a physician who is providing care planning to some patients and not to others is probably going to improve the survivorship care planning that they do with all patients. Because the IOM and other groups have recommended survivorship care planning, there may also be ethical issues if some patients are randomized to a group that does not receive care plans.
Any trial will probably have to test different levels or intensities of care planning. In this case, large sample sizes will be necessary to detect differences between groups.
In conclusion, rigorous systematic studies are necessary in order to determine what works and what does not work in survivorship care planning. The IOM report called for increased support for research and demonstration projects. The goal is to have good evidence on which to base guidelines and standards of care and thereby improve care delivery and optimize the health of survivors.
Discussion
Dr. Raich of Denver Health Medical Center suggested that multiinstitutional, interdisciplinary collaborations will be needed to strengthen the capacity to address the many research questions raised by Dr. Earle. Dr. Earle agreed that a large collaborative venture was probably needed to address the many challenges posed by this research. He noted, however, that such collaborative networks were difficult to organize and fund. Dr. Smita Bhatia of City of Hope Comprehensive Cancer Center emphasized the need to learn from the experience of the pediatric oncology community, which has organized a team effort to create care summaries and guidelines.






















