Appendix D.1
The Cancer Treatment Plan and Summary: Re-Engineering the Culture of Documentation to Facilitate High Quality Cancer Care
Deborah Schrag, MD, MPH*
Molla Donaldson, DrPH**
Abstract:
Cancer chemotherapy is typically administered over many days, sometimes in the hospital and sometimes in office settings. It is notoriously difficult, and often impossible, to recreate cancer treatment histories from medical records. This impedes communication between and among health care systems, physicians, and patients as they traverse the spectrum of cancer care. Medical record keeping does not include preparation of synoptic overviews when patients transition from one therapy to another. For these reasons, it can be difficult for patients and physicians to assemble an accurate understanding of individual chemotherapy treatments as well as the overall trajectory of a patient’s cancer care. The availability of new and better drugs for treating cancer means that patients are living longer, receiving more treatment, and managing the consequences of these therapies. In turn, living longer means that cancer patients’ medical records become thicker and it becomes even more challenging and time-consuming to create a history from those written records. In addition, like society as a whole, cancer patients are increasingly mobile, seeking care at multiple settings and interacting with a variety of health care and allied professionals. In conjunction with the
National Coalition for Cancer Survivorship(NCCS) and other patient advocacy groups, the American Society of Clinical Oncology (ASCO), the major professional organization representing medical oncologists, is developing strategies to encourage medical oncologists to prepare synoptic documents that provide an overview of care at key transition points. The goal is two-pronged: to create a synoptic document which can not only be used by other providers to quickly recreate patient medical histories, but also to serve as a springboard for discussion with patients at key transition points. This background paper first outlines the rationale for developing cancer treatment plans and summaries as a strategy to improve the quality of cancer care and then describes progress to date towards achieving this goal.
I.
Overview
Cancer care in the 21st century is exceedingly complex. As cancer patients live longer and the range of chemotherapy treatment options expands, patients are ever more likely to receive care from multiple physicians, across diverse delivery systems, over periods of many years. Both the longer periods of survival and the multiplicity of providers make it especially challenging for oncologists to assemble all the information that is necessary to understand a patient’s cancer treatment history. It is not just that obtaining the actual physical records is problematic—although it can be—rather, the more common challenge is obtaining a coherent summation of myriad relevant events from a series of chronologically organized records. Without a summary available to them, patients who have experienced a series of complex treatments have great difficulty becoming partners in their own care after completion of curative treatment.
Cancer survivors typically receive care from both oncology and non-oncology providers and eventually transition back to the “regular” health care system, where their care is usually provided by clinicians with no special oncology training. Cancer survivors report that their providers are sometimes uncertain about what, if any, special care might be required given their cancer history.
To understand the cancer history, patients and their noncancer physicians face a choice between requesting entire oncology records (on the one hand) or a few key documents (on the other). The drawback of obtaining entire records from multiple settings is that they are time-consuming to review and inefficient to transmit and store. Furthermore, only a small fraction of the contents of those records is likely to be relevant for ongoing care. However, the drawback of asking for select key documents is that detail may be missing. Medical oncology treatment can be viewed as a story which begins with a detailed chapter (the new visit note) and unfolds over
time in a series of follow-up chapters in office notes, chemotherapy flow sheets, surgical, radiation, imaging and laboratory reports, referrals, and possibly hospital discharge summaries. What both patients and providers often need, however, is a brief summary of this story. At present, there is no standard for preparing a “treatment summary,” and it is not part of the culture of routine oncology practice.
Cancer quality-of-care research has highlighted the importance of care coordination for cancer patients. One strategy for improving coordination is to change the culture of medical records documentation so that preparation of synoptic treatment summaries becomes routine. The goal of this background paper is to: (1) describe the current practice of medical records documentation with a special focus on oncology; (2) discuss the rationale for a treatment summary; (3) address challenges for implementation and; (4) identify key components of these summaries with illustrations from sample templates developed in conjunction with the American Society of Clinical Oncology (ASCO).
This background paper focuses on the overall goal of changing the culture of medical records documentation to include treatment summaries for all patients, but highlights aspects of care that have special relevance for survivors. The “transition to survivorship” care plan is simply a special type of chemotherapy treatment summary that requires special attention to issues of long-term follow-up such as fertility, management of late- and long-term effects of cancer, and screening recommendations. The objective of ASCO and the National Coalition for Cancer Survivorship’s (NCCS) treatment plan/treatment summary initiative is to ensure that synopses of care are provided for all cancer patients, including long-term survivors. Successful implementation of this initiative will require the collaboration of multiple stakeholders.
Medical oncologists are usually the providers who coordinate care for cancer patients receiving multimodality treatment. For this reason, this background paper emphasizes preparation of treatment plans and summaries by medical oncologists. Moreover, medical oncology treatments are especially challenging to track in medical records because, in contrast to surgery and radiation, they unfold over lengthy time intervals. However, it is important to emphasize that the preparation of treatment summaries is relevant for other cancer providers and indeed, for all health care providers who deliver care to persons with complex chronic conditions.
II.
Background and Rationale: Why Cancer Treatment Summaries Are Necessary
The development of a treatment summary can help achieve three objectives related to improving the quality of cancer care:1 (1) to improve coor-
|
BOX D.1-1 Objectives of Adoption of Oncology Treatment Summaries Adoption of a treatment summary could improve three interrelated aspects of cancer care delivery:
Care Coordination is especially important because:
Communication is especially important because:
Efficiency is especially important because:
|
dination of care as patients transition among various health care providers; (2) to improve communication between patients and physicians; and (3) to improve the efficiency of cancer care delivery by streamlining documentation for clinicians and clinical support staff. Box D.1-1 describes three components of care—care coordination, communication, and efficiency—that could be improved by changing the culture of oncology practice to include treatment summaries.
The Need for Treatment Summaries—Insights from Quality of Care Research
A series of influential reports by the Institute of Medicine (IOM) called attention to systemic problems in the general health care delivery system and
recommended several strategies to improve the quality of health care.2-4 With the release in 1999 of the IOM report Ensuring Quality Cancer Care and subsequent work of the National Cancer Policy Board, it has become clear that in the United States, many cancer patients, even those with adequate health insurance, do not receive the most effective available treatments in a timely fashion.2-4 Since these reports’ publication, the quality of cancer care has remained in the national spotlight. Major efforts to measure, understand, and improve the quality of cancer care have also been undertaken. In particular, the NCI and ASCO have conducted large-scale studies to characterize the state of cancer treatment and more recently to develop “Navigator” programs to prevent patients from becoming lost in the web of a complex system.5,6 Starting in 1998, ASCO and the Susan G. Komen Foundation sponsored the National Initiative on Cancer Care Quality (NICCQ). Researchers from Harvard University and the RAND Corporation reviewed medical records and interviewed patients diagnosed with breast and colorectal cancer in five U.S. cities in order to characterize the quality of their care. 6 This study underscored how difficult and time-consuming it was for highly trained researchers to locate patient data and accurately determine the treatments patients had received in order to assess whether those patients had received appropriate adjuvant chemotherapy. Even after Institutional Review Board (IRB) approval to review these records was received, many barriers to ascertaining chemotherapy use from medical record review remained. First, patients were seen by many physicians and sometimes by more than one medical oncologist. Second, most oncologists practice alone or in small-group settings and usually have paper records. Third, even when researchers were able to access oncology records, information about chemotherapy use was not easy to abstract because of highly variable patterns of documentation. Although many oncologists use flow sheets to record their use of chemotherapy, the organization and style of these documents varies considerably. Although these records may be relatively easy for oncologists to understand, they are less comprehensible to other clinicians because they include many oncology abbreviations and details of concern only to the treating oncologist, such as the white blood cell count after each dose of therapy. Information about treatment in medical oncology charts is usually recorded in an event-by-event chronological format; as a result, researchers often had to sift through many pages of notes to obtain key information about a patient’s treatment. It was even more difficult to glean from medical records whether patients had completed prescribed courses of treatment, the reasons for treatment discontinuation, and the planned next steps. Fourth, even determining diagnosis was challenging. Although initial consultation notes usually record an initial diagnosis, records often contain incomplete information because the diagnosis may evolve as more information is obtained.
The Harvard-RAND researchers presented their work to an advisory group of ASCO members interested in quality of care, representatives from the Susan G. Komen Breast Cancer Foundation, and other advocacy groups such as the NCCS. In a discussion of “lessons” learned from this large scale observational study, the utility of a chemotherapy treatment summary was recognized as a logical and potentially effective quality improvement tool. The emerging idea of an oncology treatment summary coincided with national initiatives by the NCCS, ASCO, the Lance Armstrong Foundation, the National Cancer Institute (NCI), the American Cancer Society, and the IOM to improve the care of cancer survivors.
The need for a treatment summary was also evident in other research initiatives, including the NCI’s Cancer Care Outcomes Research and Surveillance Consortium (CanCORS),5 in research from the Cancer Research Network, an affiliation of large HMOs,5 as well as large interview studies highlighting problems with care coordination as especially prevalent in cancer.
The treatment summary was also recognized as a potentially valuable tool to address problems with communication between patients and providers. In a recent population-based study of 1,067 colorectal cancer patients from Northern California, cancer patients completed surveys modified from the Picker Institute to report on their access to care, symptom control, psychosocial support, health information, treatment-specific information, confidence in providers and coordination of care. They identified access to information, psychosocial support, and care coordination as the three most deficient aspects of their care.7 Black, Hispanic and other non-English speaking patients reported significantly more problems than white English speakers, and this was especially pronounced in the domains of communication and coordination of care. Despite health information being readily available in multiple media formats, this and other research indicates that patients are dissatisfied with communication with their physicians. This is in part because patients value having health information that is filtered by a trusted and knowledgeable source, synthesized and custom-tailored to their individual circumstances.
Coordination of Care Among Oncologists and Other Health Care Professionals
Coordination of care involves facilitating patients’ access to practitioners whose expertise may improve their health outcomes or experience. These providers must have key clinical information at hand to formulate recommendations and then function collaboratively as a team to deliver care. Some practices are multispecialty and multidisciplinary, though even in these settings coordination can be a challenge. In other cases, cancer care
involves providers who practice in different locations, health systems, and specialties. Coordination is generally improved when one provider—typically the medical oncologist, but sometimes the surgeon or the primary care physician—assumes responsibility for orchestrating and overseeing all aspects of care. This critical coordination function helps to ensure that health care providers work together to provide care. This role may extend well beyond making referrals. The coordinating physician must be actively engaged to ensure that neither essential pieces of information, nor the patient himself or herself, gets lost within the complex system. The coordinating physician must also ensure that other practitioners’ expertise is obtained to address frequently overlooked needs, such as psychosocial distress.
Not all providers involved in a patient’s care need or want the entire oncology record. A cardiologist, for example, needs to know how much doxorubicin a patient has received, and a dentist must know what precautions are needed for a patient with a MediPort in place or when there is a history of low platelets. However, synoptic treatment plans and summaries are not simply intended to make care safer and more effective for cancer patients in nononcology settings; they can also help oncologists with coordination. When communicating with other oncologists and between oncologists and their colleagues in closely related fields like surgery and radiation oncology, every oncologist has confronted the onerous task of reading through reams of office notes and flow sheets to ascertain what chemotherapy was delivered, why it was delivered, and how it was tolerated.
Communication of the Treatment Plan and Summary, and the PostTreatment Plan Between Medical Oncologists and Patients
Oncologists have complex communication responsibilities when talking with patients. They must explain the patient’s diagnosis, prognosis, and therapeutic options in a comprehensible way, and listen to and incorporate patient preferences while formulating a treatment plan. Documenting treatment plans can serve as a valuable springboard for discussion about current and future chemotherapy. That is, systematic review of the information with the patient may help him or her understand the purpose of treatment, and to structure conversations about treatment decisions. Providing patients with a copy of the treatment plan may also empower them to begin conversations with family members and other health care practitioners, as well as their oncologist. Creating documents that patients can review at a later time also addresses the widely recognized phenomenon that patients remember only a small proportion of the information provided during an office visit. A physical (or access to an electronic) record enables patients to review the key content in a more relaxed setting at a place and time when information may be more easily absorbed and shared with others.
After a course of chemotherapy is complete, the summary and plan for follow-up, including surveillance for recurrence and late effects may serve as a valuable foundation for discussion. Providing patients with a document empowers them to communicate effectively with other providers. whether or not they understand every sentence in the document. This may be especially important for non-English speaking patients
Practice Efficiency: Minimize the Administrative Burden for Administrators and Staff
Information about medical oncology treatment is not recorded in a single place or in a standardized format in health care records. As a result, when multiple oncologists are involved in a patient’s care, they typically request a patient’s entire record and thus create a workload that burdens office staff and physicians. A chemotherapy treatment plan outlining the planned regimen and a subsequent treatment summary describing how treatment was tolerated and the outcomes of care could streamline communication among oncologists and between oncologists and other key cancer-care providers, such as surgeons and radiation oncologists.
Facilitate Quality of Care Monitoring and Improvement
In order to evaluate the quality of cancer care, it is not necessary to know the number of milligrams of every treatment dose. Neither is it necessary to know the specifics of every dose delay or reduction. The inclusion of chemotherapy treatment summaries in medical charts would have greatly simplified the work of the NICCQ investigators by reducing the need to sift through pages of records that were not relevant to assessing quality.
More generally, quality of care monitoring also involves ensuring patients’ safety, both individually and as a member of a group receiving similar chemotherapeutic agents. For example, it is critical to identify harmful effects of chemotherapy drugs that emerge after these drugs have received FDA approval (sometimes called, “after market” monitoring). Treatment summaries that track and aggregate the toxicities that patients experience could greatly facilitate monitoring such unexpected effects, especially if the treatment summary is developed in electronic form with flexible reporting capability.
III.
The Culture of Medical Records Keeping by Physicians
Physicians are required to keep medical records that describe health care delivery. These records serve multiple purposes. They enable the individual physician to recall his or her thoughts and plans from one visit to the
next. Documentation also provides key information to other health care providers working with the oncologist as well as clinicians at other sites. Documentation fulfills a legal function by creating a permanent record of health care.
Although some new electronic systems are changing the status quo, medical records are almost always organized chronologically by events, such as visits. The abstraction necessary to create a synopsis is challenging, time-consuming and requires physician input. However, electronic systems can be structured to facilitate this activity by populating specific fields of key relevance such as diagnostic information; for example, site, histology and stage. When care evolves over time, these records become progressively denser and more difficult to review. It is common practice to focus on the most recent history, and for this reason key information may become buried in a thick stack of documents. Consider the challenge for an emergency room (ER) physician evaluating a dehydrated patient with longstanding metastatic breast cancer. The ER physician can easily determine what operations have been performed by searching the record for operative and pathology reports. Episodes of radiation are summarized. Hospitalizations are described with a discharge summary. However, recreating the trajectory of the cancer care history requires review of medical oncology notes to determine the drugs given and the context of treatment. Although this information is available, it is often spread across multiple visit notes, flow sheets, and treatment administration records. It can be sufficiently difficult to reconstruct a cancer history from a medical record that a physician in the ER may avoid the chart altogether and instead try to obtain this history directly from the patient. When patients are careful historians and attentive to important detail, this strategy works reasonably well. However, when patients are too ill to provide history, lack informed caregivers, or have language barriers, they may not be able to provide important information.
In addition, records include detail that may not be helpful, even to treating oncologists. A key example is documentation for the purpose of billing. In the mid-1990s, the Health Care Financing Administration (HCFA, now the Centers for Medicare and Medicaid Services or CMS) developed a detailed set of rules delineating documentation standards for billing Medicare. These rules specified the number of items in the physical exam (for example three aspects of the respiratory system) and the number of body systems that need to be included in a systems review in order to bill for complex “evaluation and management” visits. These requirements led to burgeoning detail in medical records and widespread use of templates with detailed physical exams and reviews of systems to support reimbursement. However, this information often has minimal value for either patients or providers. Physicians developed standardized templates
as workarounds to circumvent the repetitive and onerous task of documentation. Although these billing templates may provide a reasonably accurate assessment of a patient’s status at a point in time, they are notoriously poor for conveying the larger picture of a patient’s overall trajectory for a chronic disease such as cancer. Nor does this documentation provide useful information for quality reporting or practice improvement. Unlike HFCA rules for reimbursement, the purpose of the treatment plan/ treatment summary initiative is to infuse meaning into medical recordkeeping.
Some medical events are straightforward to describe because they involve a particular date or procedure. When physicians want to know which surgical treatment a cancer patient has had, they know to ask for two critical documents: the operative report and the pathology report. Although these documents do not provide a summary of postoperative complications, they set forth—in a fairly standardized format—the reason for performing the operation, the procedure planned and actually performed, and any immediate complications.
In radiation oncology, the concept of a radiation treatment summary is widely accepted. When meeting with a patient who reports prior radiation at an outside hospital, physicians know to ask for this summary document. In most circumstances, they neither need nor want more detail than is included in this summary: typically the reason for radiation, the area radiated, the treatment planned, and the treatment actually delivered. Radiation oncologists may use different templates for this summary, some providing more or less accompanying narrative detail. However, the culture of radiation oncology is that all providers prepare some version of this key document.
In contrast to radiation and surgery, which constitute discrete episodes of care, a chemotherapy regimen has less clear boundaries. A regimen may be given once or over a period of years, and the amount of information that needs to be summarized may vary significantly. In some cases, patients may be given a three-drug regimen, develop an allergy to one drug, and have a component of the initial regimen discontinued or an alternative drug substituted. Patients may embark on long-term maintenance therapy with hormones. They sometimes temporarily stop treatment to relieve symptoms, to take a needed break from medication, or to attend to personal obligations. In this fashion, the boundaries of a chemotherapy regimen may become indistinct. Nevertheless, it is possible to provide some guidelines regarding what is meant by a “chemotherapy regimen” for those who will complete treatment summaries.
Oncologists share with other clinicians the challenge of complementing the chronological longitudinal approach to recordkeeping with succinct
synopses. Treatment summaries are also recognized as important in the management of complex chronic care conditions such as mental illness with psychosis, diabetes, inflammatory bowel disease, and multiple sclerosis. Progress towards developing and implementing treatment summaries in these areas has been slower.
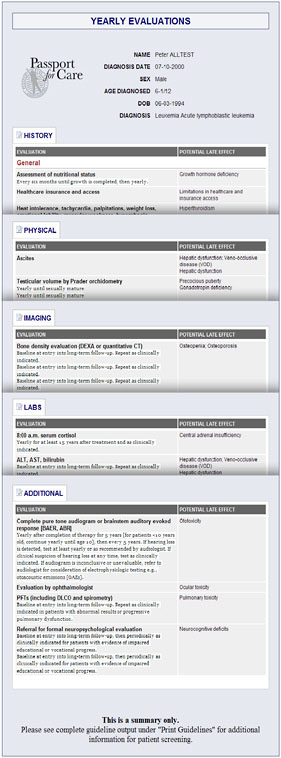
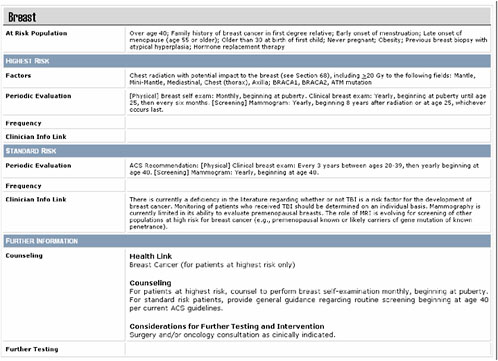
On the other hand, other health care professionals do create summary documents that provide overviews for lengthy episodes of health care that do not occur on a single date. For example, obstetricians have overviews that detail antepartum, pre-, intra- and postpartum care on a single page. These summaries are invaluable when a woman presents for a second pregnancy because the obstetrician can quickly determine a woman’s level of obstetrical risk. Similarly, pediatricians have summary documents that record a child’s immunization record, growth and development, and major childhood illnesses. These documents work well because most obstetrical and pediatric care adheres to a similar routine. Pediatric oncology offers another example. In pediatric oncology the Children’s Oncology Group (COG) has drafted a treatment summary template for survivors of childhood cancer. In comparison, there are as of yet no accepted oncology-specific prototypes for adult oncology. Several promising initiatives are underway, however, to implement the recommendation of both the President’s Cancer Panel and the IOM Committee on Cancer Survivorship. These efforts are focused on developing a care plan, treatment summary, and follow-up plan for patients finishing their primary treatment. With input from key stakeholders, ASCO has developed and has begun pilot testing a chemotherapy treatment summary. Certain cancer centers have developed their own treatment summaries (e.g., Memorial Sloan-Kettering Cancer Center, The Massey Cancer Center) and survivorship care plans (UCLA, Memorial Sloan-Kettering). These interrelated and complementary efforts have not yet converged on a single well-accepted standard. What is clear, however, is that the concept and goal is universally recognized and considered valuable by both patients and providers. The challenge is to develop consensus regarding the intended target audience for the summaries, how these documents should be structured, what they should contain, at what level of detail, and the timing for their completion. The objective of the ASCO initiative is to develop treatment plans in stages, beginning with core elements of a treatment plan and summary for other clinicians and for patients. Later stages will include cancer-specific versions, patient-oriented versions, and electronic versions that can be used as templates by electronic oncology record vendors. There is no expectation that we will arrive at a single document that will work in all circumstances. However, providing practitioners with a variety of templates that can be customized for particular practice needs and patient populations is a starting point.
IV.
What Are the Key Elements in a Chemotherapy Treatment Plan and Treatment Summary?
Chemotherapy Treatment Plan
A chemotherapy treatment plan is a one-page document. It should include:
-
Diagnosis: cancer site, histology and stage;
-
Goals of therapy, anticipated benefits;
-
Name of the regimen, the component drugs in the regimen, and the starting dosages;
-
Duration of treatment and number of planned cycles;
-
Strategy for assessing response;
-
Side effects and precautions*;
-
Assessment of risks and benefits; and alternatives.
Ideally, the document should be reviewed with the patient and his or her family member when a treatment is started. Because patients are often overwhelmed by information at the time of diagnosis and have difficulty assimilating information after receiving bad news, having a written treatment plan that could be referred to later by patients, family members, and potentially by other physicians, is a logical and sensible strategy. This is particularly relevant for non-English speakers and low-income patients, whose cancer care is often fragmented across providers or rotating trainees.
Chemotherapy Treatment Summary
A chemotherapy treatment summary is a succinct, ideally one-page document prepared at the end of a course of treatment or when a patient completes adjuvant therapy when a regimen is discontinued because of toxicity. The summary might be appended to the treatment plan. The treatment summary should include:
-
The duration of treatment or the number of treatments planned and the number actually delivered;
-
Whether any drugs were dropped from the regimen;
-
Any major toxicity and hospitalization resulting from treatment complications such as febrile neutropenia;
-
Response to treatment (based on radiographic, biochemical, or clinical criteria, or combinations of these criteria;
-
The reason treatment was discontinued;
-
Planned next steps (e.g. hospice care, an alternative regimen, expectant management, posttreatment surveillance etc.);
-
Who is responsible for performing follow-up and any other special monitoring.
Survivorship Care Plan
When cancer patients transition from active treatment to surveillance, and then from close surveillance to long-term survivorship, it is important to generate both a summary document that specifies any ongoing problems for that patient and schedules for follow-up evaluations and procedures.
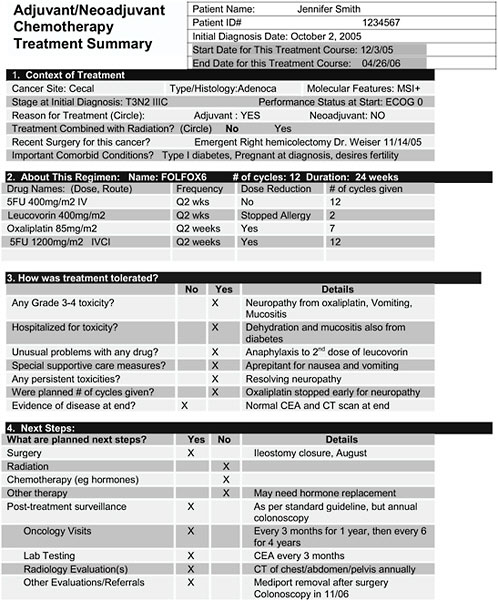
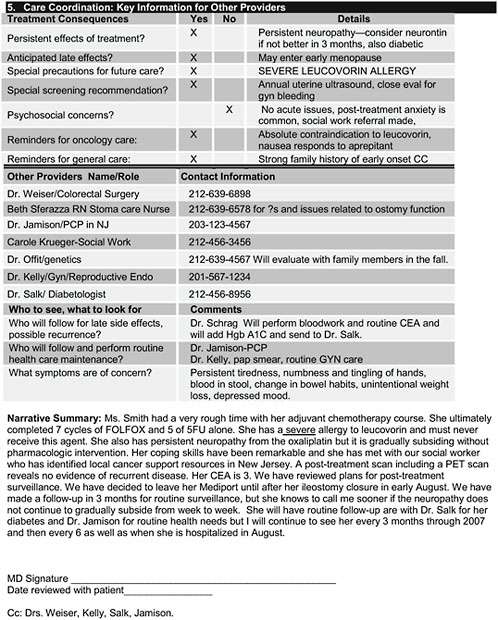
Figure D.1-1 illustrates a draft ASCO treatment summary for a patient with stage III colon cancer. It was completed at the end of adjuvant therapy. This document is synoptic; that is, it does not include all details about the care provided. Although it is intended to be shared with patients, it includes enough detail for other treating health practitioners. These documents are not meant to replicate the medical record. The treatment plan/summary should include no more detail than two sides of a sheet of paper. This is consistent with most operative reports, hospital discharge summaries, pathology reports, pediatric records of growth and immunization, and other key synopses that are well-accepted in health care. The goal of the ASCO treatment summary initiative is to obtain consensus among oncology professionals about key elements. For now, it focuses on care coordination and traditional medical issues rather than on psychological well-being or secondary prevention such as tobacco use, nutrition, or exercise, though these are nonetheless recognized as very important.
V.
Challenges for Implementation of Cancer Treatment Plans and Summaries
Changing the professional culture of medical oncology to include preparation of treatment plans and treatment summaries will be extremely challenging. Previous pilot work conducted by ASCO with volunteer physician practices indicates that although physicians think that treatment plans and summaries are important and worthwhile, the main obstacle to preparing them is limited time given their busy and demanding practices. Demonstrating that this mode of documentation can ultimately save rather than add time—particularly with development of electronic versions that are easy to
complete—will be necessary for their widespread adoption as a part of routine practice. Reimbursement for completing the summaries and liability issues are secondary concerns. Overall, a profound cultural shift will be required to change entrenched practice patterns.
Who Is the Primary Target Audience?
This section addresses some of the most frequent questions and concerns that have been raised by oncologists, primary care physicians, active patients, and survivors during the early development phases of the ASCO initiative.
The target audience for treatment plans and summaries includes both patients and health care providers; however, it is a challenge to address both audiences effectively with the same document. ASCO’s early versions of a summary (Figure D.1-1) are geared more towards health care providers than patients. Although technical, rather than lay language is used to convey material succinctly, the goal is for oncologists to use these summaries as a springboard for discussion with patients. A treatment plan/summary prepared for the patient would look somewhat different but could constitute the next phase of development.
For any version, the core elements would be consistent but the language and terminology would vary based on who the primary user will be. If it is the patient, then the summary should use Standard English and avoid medical terminology. If nononcology health care providers are the intended recipients, medical terminology without the use of oncology-specific abbreviations and jargon is appropriate. If other oncologists are the intended audience, details including regimen names and oncology-specific abbreviations are appropriate and helpful.
It is neither feasible nor practical to have separate documents geared towards distinct audiences because of the time and workload required to prepare these documents. At present, the goal is to develop a version that is relatively free of oncology-specific jargon and therefore suitable for nononcology medical providers. Ideally, preparation of these documents will trigger conversations between patients and physicians that clarify meaning and any unfamiliar terms. To some extent, the level of the detail and tone of the document should also vary based on the disease context. For example, patients with advanced metastatic cancer are cared for by oncology professionals or palliative care professionals who are familiar with cancer-related terms and abbreviations. A patient with chronic myelogenous leukemia, metastatic breast, ovarian, or prostate cancer may be followed for many years and across many sites of care. However, a primary oncologist is likely to remain involved in management. In these situations, it is reasonable to anticipate that the summary will be reviewed most frequently by other
oncologists. In contrast, when patients complete treatment for early stage disease such as adjuvant or primary therapy (and pass through the customary subsequent period of close surveillance) they will transition to a nononcologist, likely their primary care physician. In this case, the target audience will be a nononcology health care professional and the context of care should influence the detail oncologists provide.
The ASCO draft summaries are intended to be used by patients and providers of all types, but they focus primarily on use by nononcologist physicians, based on the presumption that they are the group most likely to need to know the details of prior treatment. ASCO’s rationale for this is that the primary goal of the treatment summary is to facilitate coordination of care for patients as they navigate through a complex fragmented health care system. Patients themselves should be encouraged not only to keep but also to provide a copy of their treatment summary and plan for follow up to future health care provider. Because of the documents’ more general medical language, many patients will understand their details with little difficulty. Some patients will use these summary documents as the basis of discussion.
When Should a Summary Be Prepared?
There are many situations in oncology where it makes sense to prepare a summary: for example, at the end of a course of adjuvant therapy, or at the completion of primary curative therapy. There are other situations where it is less clear. For patients with chronic diseases like low-grade lymphoma, the duration of one treatment may be many months. It is not possible to define the precise time interval of various treatments. In general, whenever there is a substantial change in treatment or a regimen is completed, a summary should be prepared. Specific time points, such as those developed by the National Comprehensive Cancer Network, can be built into guidelines.8 However, these determinations will also involve judgment on the part of individual physicians.
What Is the Right Platform—Paper or Computer?
The optimal strategy for development of treatment summaries is to integrate them as components of electronic health record systems. If these documents are three-dimensional with branching logic, drop-down menus, and checklists, they will be able to capture more important detail more succinctly and efficiently. ASCO is committed to developing electronic versions that can be downloaded, used, and modified.
However, many oncology practices still rely entirely on paper for recordkeeping and of the few oncology practices that have true electronic
medical records, many use systems that are hard to adapt. Therefore, development must proceed on several fronts simultaneously: paper versions that can be completed by pen, templates for telephone dictation, and electronic versions. Priority should be given to developing an electronic version, given its greater capabilities. Health information technology vendors are competing to develop oncology products, and achieving consensus on the core elements of summary documents will advance their timely incorporation into electronic health record systems.
Static or Living Document?
Treatment summaries will need to be updated as screening recommendations change, as recurrences that warrant additional testing arise, and as new evidence on late effects emerge. For patients with metastatic disease, an old treatment plan and summary will be superseded by a new one. For patients who have completed therapy, recommendations for screening or follow-up may change. However, because the goal is not to replace the medical record, which provides a longitudinal comprehensive record of care, even a summary that is not updated is still likely to be valuable.
Some physicians are concerned about their liability exposure: for example, if a screening recommendation changes but a form is not updated. A solution may be to date the documents and make it clear to patients that recommendations included in summaries may become outdated. Such concerns, however, should not impede the ultimate goal of having useful summaries that can be shared.
Can This Activity Be Reimbursed?
Preparation of a treatment summary and reviewing the material with a patient is considered complex coordination of care and can be submitted for payment using level four or level five codes for evaluation and management. There is no reason to expect that insurers would not reimburse providers for this service; however, it is not clear that preparation of the summary would be a reimbursed service if it did not include face-to-face interaction with the patient.
Should There Be One or Several Versions of the Treatment Plan/Summary?
Developing a template that works for all situations in oncology is a challenge. ASCO’s goal is to make sample templates freely available to encourage its membership to prepare these documents, review them with patients, and adapt and improve them. Pilot experience suggests that the information that is needed on a summary for patients with metastatic dis-
ease who transition from one treatment to the next is quite different from what is needed for patients who have completed adjuvant or primary curative therapy. For this reason, at least two templates are needed: one for patients following a course of adjuvant/neoadjuvant therapy, and one for patients with advanced disease. These synoptic documents will be most useful if they are tailored to the specific disease. If these templates are available in modifiable format, oncologists will be able to customize and adapt them to suit their own specific purposes based on the types of patients they see. ASCO can create a repository to serve as a clearinghouse for sharing these documents as different versions are developed. The goal is to create a source for open-access to nonproprietary templates that include core elements and standard vocabularies for those elements (e.g., staging). Adaptations based on extent and type of disease could build on these core elements.
How Can Implementation Be Encouraged?
Few patients currently receive a treatment plan or summary. Ensuring that all cancer patients receive these summaries will require fundamental change in how oncologists deliver care. Changing deeply embedded practice and documentation patterns, however, will not be easy. Even with its strong influence, ASCO may not be able to accomplish this without support and encouragement from other stakeholders. For adoption of treatment plans and summaries on a widespread basis, implementation will need to proceed along several fronts. Patient advocacy groups like NCCS can encourage patients to ask for these documents. Other organizations such as the American Board of Internal Medicine and the National Committee for Quality Assurance can include this aspect of oncology care in their provider evaluations. Improvements in care could be made by adopting as a standard measure of quality patients’ receipt of treatment plans and summaries and through initiatives designed to reengineer the culture of medical recordkeeping.
Electronic medical record vendors can embed treatment plan and summary templates in their systems. Payors could facilitate their adoption by explicitly reimbursing providers for the work of developing treatment plans and summaries and posttreatment planning and reviewing them with patients.
Coordinating care and communicating with patients about their treatments may be the most valued services oncologists provide and should be encouraged. Currently, oncologists are not well compensated for developing mutually agreed-upon treatment plans or posttreatment surveillance plans following completion of adjuvant therapy, for engaging in discussions
regarding whether or not to administer chemotherapy, or for implementing an end-of-life care plan.
Altering traditions and entrenched systems requires great effort. However, it is imperative to align the reimbursement system with services that can foster patient-centered high quality care. In collaboration with major health care payers, particularly the Centers for Medicare and Medicaid Services, policymakers must work to modify the current reimbursement system to ensure that providers are appropriately compensated for these essential cognitive services that are highly valued by patients rather than rewarded for spending inordinate amounts of time complying with billing rules mandating documentation of detailed physical exams and reviews of systems that do not improve care.
Can Nononcology Professionals Prepare These Summaries?
Some hospitals rely on nononcology professionals to prepare discharge summaries. This is particularly the case when these discharge summaries are focused on maximizing reimbursement. However, because the goal of this treatment planning/summary effort is to foster dialogue between oncologists and their patients, oncologists should engage directly in this process. Some aspects of the plan or summary could be completed by support staff or nurses in the hospital or oncology practice. In fully electronic environments, the formulary and pharmacy records of treatments given could populate fields in a treatment plan and treatment summary Both oncology physicians and oncology nurses can, and should, review the treatment summary with their patients. Ultimately the treatment summary is not a valuable activity if it is purely an administrative or secretarial chore.
VI.
Conclusion
Increasingly, problems relating to coordination and communication have been recognized as hampering the delivery of high quality cancer care. The goal of the treatment plan and summary is to achieve meaningful improvement in cancer care delivery and the patient experience. Changing the culture of documentation is intended to facilitate improved dialogue between patients and their health care providers. With some behavior change and restructuring of documentation requirements, it should be possible to foster better coordination and communication and more readily track cancer treatment histories in medical records. This initiative will depend upon standardized forms, ideally in electronic formats that are made freely available. As a first step, pilot work will be necessary to develop templates that work across diverse practice sites and in diverse clinical situations. The transition to survivorship for patients who have completed
curative therapy or adjuvant/neoadjuvant treatment is a logical and important starting place because of the large and increasing numbers of cancer patients who are making this transition. Patients, payors, and providers must all engage in this process. If a critical mass of providers engages in this effort, a “tipping point” will be reached such that all providers will begin to participate in this process to conform to the standards of their peers. Professional organizations like ASCO, in partnership with patient advocacy organizations, can facilitate this process by developing consensus regarding what key elements these documents should include and by ensuring that reimbursement is linked to documentation that is accessible and useful to patients and physicians. Changing the professional culture and accepted practices of documentation and aligning incentives to support this effort should promote better communication and coordination. As a result, we can achieve meaningful improvement in the quality of cancer care.
REFERENCES
1. Schrag D. Communication and coordination: the keys to quality. J Clin Oncol. Sep 20 2005;23(27):6452-6455.
2. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, D.C.: National Academy Press; 2000.
3. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press; 2001.
4. Institute of Medicine. 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities. Washington, D.C.: The National Academies Press; 2004.
5. Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. Aug 1 2004;22(15):2992-2996.
6. Malin JL, Schneider EC, Epstein AM, Adams J, Emanuel EJ, Kahn KL. Results of the National Initiative for Cancer Care Quality: how can we improve the quality of cancer care in the United States? J Clin Oncol. Feb 1 2006;24(4):626-634.
7. Ayanian JZ, Zaslavsky AM, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. Sep 20 2005;23(27):6576-6586.
8. National Comprehensive Cancer Network. National Comprehensive Cancer Network. http://www.nccn.org/. Accessed May 24, 2006.
Appendix D.2
Recommendations for Health Behavior and Wellness Following Primary Tr eatment for Cancer
Lee W. Jones, PhD*
Wendy Demark-Wahnefried, PhD, RD, LDN**
Introduction
Every 23 seconds, an American is diagnosed with cancer.1 Given advances in early detection and treatment, 64% of those diagnosed with this disease can expect to be alive in 5 years.1 These individuals will join the ever-expanding numbers of cancer survivors who now number over 10 million and constitute 3-4% of the U.S. population.2,3 While these numbers are encouraging, it is important to acknowledge that the impact of cancer is significant and associated with several long-term health and psychosocial sequelae.2-15 Indeed, cancer survivors constitute a vulnerable population who have distinct health care needs.7,16 Data clearly show that compared to general age- and race-matched populations, cancer survivors are at greater risk for developing second malignancies and other diseases, such as cardiovascular disease (CVD), diabetes, and osteoporosis.2-16 An early comparison by Brown et al.6 of over 1.2 million patient records obtained from the SEER database with those obtained from the National Center for Health Statistics found a significantly higher noncancer relative hazards ratio for cancer patients of 1.37 and concluded that “the evidence that cancer patients die of noncancer causes at a higher rate than persons in the general population is overwhelming.” Data collected over the past decade confirm these findings.2-4,8,17 These competing causes of death and comorbid conditions are believed to result from cancer treatment, genetic predisposition, and/or common lifestyle factors.2,4,13-15
Hewitt et al.10 also report that cancer survivors have almost a two-fold increase in having at least one functional limitation, and in the presence of another comorbid condition the odds ratio increases to 5.06 (95%CI 4.47-5.72). These findings have been confirmed by other studies in diverse populations of cancer survivors.18-23 From an economic perspective, an analysis by Chirikos et al.24 indicated that “the economic consequence of functional impairment exacts an enormous toll each year on cancer survivors, their families and the American economy at large” 24, findings confirmed by others.25-28
Based on these national trends, cancer survivorship is fast emerging as a public health concern and has been set as a national priority.2-5,8,13 In a recent Institute of Medicine (IOM) report entitled “From Cancer Patient to Cancer Survivor: Lost in Transition,”29 the numerous health issues of cancer survivors were summarized, and the potential benefits of lifestyle modifications were briefly reviewed. From this report, recommendations were put forth to guide health care providers, patient advocates, and other stakeholders in an effort to improve the health and well-being of this rapidly expanding and high-risk population—a population that heretofore “has been relatively neglected in terms of advocacy, education, clinical practice and research.”29 The goal of this paper is to review these recommendations in light of more recent advances, with the following topic areas addressed: (1) strength of evidence for recommendations in areas of weight management, diet, exercise, smoking cessation, as well as other areas, such as alcohol and sunscreen use, complementary and alternative therapies, management of osteoporosis, and immunizations; (2) perceived needs of cancer survivors for health information and preferred channels of delivery; and (3) resources available to providers and patients regarding healthful lifestyle practices. To this end, gaps in the IOM report were identified and in addition, an updated search of literature published within the past 2 years was performed using CancerLit, PubMed, and Medline databases and employing search terms of cancer survivor(s) or neoplasms/survivor cross-referenced with MeSH terms of lifestyle, health behavior, cardiovascular training, rehabilitation, physical fitness, physical activity, exercise, body weight, obesity, weight loss, diet, nutrition, complementary therapies, dietary supplements, tobacco, smoking cessation, alcohol drinking, sunprotective agents, osteoporosis, immunization and intervention studies. Relevant articles were then hand-searched for pertinent previously published papers.
Health Promotion Concerns for Cancer Survivors
Weight Management
Positive and negative energy balance are dual concerns in cancer popu-
lations. For some groups of survivors, such as those diagnosed with select respiratory, gastrointestinal or childhood cancers, or those living with advanced-staged disease, anorexia and cachexia may be problems that persist after primary treatment.30-32 For these survivors, continued supportive care therapies including dietary counseling and the potential use of pharmacotherapy (e.g., megestrol acetate) and/or nutritional support may be critical for recovery and may enhance the ability to eat and to maintain adequate nutritional stores30,31,33 that are important for improved functional status and well-being.34 Physical activity also may help to increase appetite, relieve constipation, and improve quality of life in these survivors.35 As noted in the IOM report,29 as critical as anorexia and cachexia are to cancer care, for the majority of cancer survivors, obesity and overweight are problems that are far more prevalent.35-37 Obesity is a well-established risk factor for cancers of the breast (postmenopausal), colon, kidney (renal cell), esophagus (adenocarcinoma), and endometrium;38,39 thus a high proportion of cancer survivors are overweight or obese at the time of diagnosis. Furthermore, increased premorbid body weight has been associated with cancer mortality for cancers of the breast, esophagus, colon and rectum, cervix, uterus, liver, gallbladder, stomach, pancreas, prostate, kidney, non-Hodgkin’s lymphoma and multiple myeloma, as well as all cancers combined.40-42 Finally, additional weight gain is common during or after treatment for various cancers, and may exacerbate risk for functional decline, comorbidity and perhaps even cancer recurrence and cancer-related death.43-45 While studies exploring the relationship of post-diagnosis weight gain and survival have been somewhat inconsistent,45-50 the most recent published study by Kroenke and colleagues,45 the largest to date (N=5,204), suggests that breast cancer survivors who increased their BMI by 0.5 to 2 units were found to have a relative risk (RR) of recurrence of 1.40 (95% CI: 1.02-1.92) and those who gained more than 2.0 BMI units had a RR of 1.53 (95% CI: 1.54-2.34); both groups also experienced significantly higher all-cause mortality. In addition, several studies have reported that increased body weight post-diagnosis negatively impacts quality of life.37,44,51 This accumulating evidence of adverse effects of obesity in cancer survivors, plus evidence indicating that obesity has negative consequences for overall health and physical function make the pursuit of weight management a priority for cancer survivors,35,37,52-55—a priority that is substantiated through viable physiologic mechanisms,55-57 as well as concern that the health issues of this population are overlaid upon the pandemic of overweight and obesity currently existing in this nation.41,58
Despite the demonstrated adverse effects of obesity in cancer survivors, only five reported studies have examined weight management in cancer populations and all were conducted among women with breast cancer. Two of these studies were performed largely on survivors who had com-
pleted active treatment, and found that individualized dietary counseling provided by a dietitian was effective in promoting weight loss.59,60 The more recent study by Djuric and colleagues60 found that counseling by a dietitian was most effective if combined with a structured Weight Watchers® program which included exercise with weight change at 12 months being +.85 ± 6.0 kg vs. −8.0 ± 5.5 kg or −9.4 ± 8.6 kg in the control versus dietitian or dietitian plus Weight Watchers® program, respectively. Multiple behavior interventions that utilize a comprehensive approach to energy balance, and that include both diet and exercise components may have the potential to be more effective than interventions relying on either component alone.61 In their evaluation of a diet and exercise intervention among early stage breast cancer patients which was begun during the time of treatment and extended throughout the year following diagnosis, Goodwin et al. found that exercise was the strongest predictor of weight loss.62,211,212 Given evidence that sarcopenic obesity (gain of adipose tissue at the expense of lean body mass) is a documented side effect of both chemotherapy and hormonal therapy,63-67 exercise, especially strength training exercise, may be of particular importance for cancer survivors since it is considered the cornerstone of treatment for this condition.68 To date, however, only one study has reported the physiologic effects of resistance training exercise in cancer survivors, a pilot study by McKenzie and Kalda69 where preliminary data suggest that arm exercises among breast cancer patients are safe and not associated with increased risk of lymphedema, but where no outcomes exist regarding body composition.69
As noted in the IOM report29 and the research of others,70 cancer survivors also may have particular problems with self-esteem and depression that may undermine the ultimate success of weight management programs. More research is needed to develop interventions that not only address the unique physiological needs of this population, but also their distinct psychological issues as well. Until more is known, guidelines established for weight management in general populations should be applied to cancer survivors, and include not only dietary and exercise components, but also behavior therapy.71 With research indicating that 70% of cancer survivors are overweight or obese, there is a definite need to develop effective weight management interventions for this needy population.52
Nutrition and Diet
Energy Restriction
As noted in the previous section, accumulating evidence suggests that weight management should be the uppermost nutritional priority for cancer
survivors. Thus, for the majority of cancer survivors who are overweight, energy-restricted diets are recommended. 35,52,54,55 Moderate energy deficits of up to 1,000 calories/day can be achieved by concomitantly increasing energy expenditure (via exercise) and reducing energy intake. Energy restriction can be achieved by reducing the energy density of the diet by substituting low-energy density foods (e.g., water-rich vegetables, fruits, cooked whole grains, soups) for foods that are higher in calories.72 This “volumetric approach” can enhance satiety and reduce feelings of hunger and deprivation that often serve to undermine energy-restricted diets. An additional strategy is limiting portion sizes of energy dense foods.73-77 Newly issued dietary guidelines for cancer survivors will emphasize energy balance and by and large endorse dietary recommendations that have been established for the primary prevention of cancer and other chronic diseases.28,35,52,78,79
Balancing Fat, Protein, and Carbohydrate Intake
Protein, carbohydrate, and fat all contribute energy (calories) in the diet, and each of these dietary constituents is available from a wide variety of foods. Making informed choices about foods that provide these macro-nutrients can ensure variety and nutrient adequacy. In general, the choice of foods and their proportions within an overall diet (dietary pattern) may be more important than absolute amounts.35,37,58 Given that cancer survivors are at high risk for other chronic diseases, the recommended amounts and type of fat, protein, and carbohydrate to reduce these disease risks also are germane.35 A 2005 study by Kroenke et al. of 2,619 breast cancer survivors participating in the Nurse’s Health study suggests that those who report a prudent diet (e.g., high proportional intakes of fruits, vegetables, whole grains, and low-fat dairy products) had significantly lower mortality from non-breast cancer causes compared to those who reported a Western-type diet (e.g., high proportional intakes of meat, refined grains, high-fat dairy products, and desserts).79
Fat
To date, 14 studies examining the relationship between fat intake and survival after the diagnosis of breast cancer have been reported, and the results are notably inconsistent.80 In prostate cancer, only one study has explored the association between fat intake and survival and found that saturated fat intake (but not total fat) was associated with worse survival.81 One recently completed study (Women’s Intervention Nutrition Study [WINS]) and one ongoing study (Women’s Healthy Eating and Living study [WHEL]), were designed to test whether a reduction in fat intake can reduce
risk for recurrence and increase overall survival in women who were diagnosed with early stage breast cancer.82,83 Preliminary results from the WINS study suggest that women assigned to the low-fat diet arm (< 15% energy from fat) exhibited a 24% reduction in risk for recurrence; with subset analyses suggesting that this effect was even greater among women with ER-disease ( i.e., 42%).82 The main results from the WHEL Study are anticipated by 2008; however to date, the low fat, high fruit and vegetable intervention has been found to significantly reduce estradiol levels.84 It should be noted that four other randomized controlled trials have been reported among cancer survivors that were aimed at determining the efficacy of individualized counseling, group classes or volunteer-led programs in reducing fat intake. All of these programs were effective in promoting dietary change, and three of the four studies resulted in significant weight loss.85-88
Some types of fat, such as monounsaturates, are associated with reduced risk for heart disease and possibly cancer, whereas others, such as saturated fats, are associated with increased risks.58,89 Some studies have suggested that omega-3 fatty acids may have specific benefits for cancer survivors.89 However, in light of a recent systematic review by MacLean et al. 90 which found little support for any protective association between omega-3 fatty acids and cancer risk, more research is required. That said, consuming foods that are rich in omega-3 fatty acids, such as fish and walnuts, should be encouraged because of the strong relationship between omega 3 intake and reduced risk for cardiovascular disease (CVD) and overall mortality.90-92 Currently, the recommended level of fat in the diet is 20-35% of energy, with saturated fat intake limited to <10% and trans fatty acids limited to <3% of total energy intake.58
Protein
To date, few studies have examined the relationship between protein intake and cancer specific outcomes in humans. One study, however, found that, increased intakes of red meat, bacon and liver were associated with recurrence among early-stage breast cancer survivors.93 Given these data, as well as strong evidence that red meat and processed meat are associated with increased primary risk for colorectal cancer, survivors are encouraged to limit their consumption of these foods.35,89 Protein intakes of roughly 0.8 g/kg of body weight are recommended with 10-35% of energy coming from protein.94
Carbohydrates
As with protein, little research has been undertaken with regard to carbohydrates (starches, sugars and fiber) and cancer survival, though fiber
has been explored extensively with regard to recurrence of precancerous lesions (e.g., colorectal adenomas),95,96 where it’s role may be influenced by gender and is still unclear. Given that glycemic control is a newly emerging area of interest in relation to cancer, more research is anticipated in this area in the next few years.97 Given a lack of definitive data, survivors are encouraged to follow dietary guidelines established for the prevention of chronic diseases that endorse intakes of carbohydrates ranging from 45-65% of total energy intake and fiber intakes of 14 g. per 1,000 kcal.58 Carbohydrates should come primarily from nutrient-dense food sources, such as vegetables, whole fruits, and whole grains—low-energy density foods that promote satiety, and weight control, while enhancing nutrient adequacy.35,58,75 Refined carbohydrates and sugars are discouraged given their relative lack of nutritional benefit and their contribution to energy intake.35,58,91
Vegetables and Fruits
Given high concentrations of various phytochemicals, anti-oxidants, and fiber, vegetables and fruits have been promoted not only among healthy populations for the prevention of cancer, but also among cancer survivors.35,75,89 In the 10 observational studies that have examined the relationship between intakes of vegetables and fruit (or nutrients indicative of those foods) and risk for cancer recurrence, the evidence has been mixed. Half of the studies have observed a significant protective effect of fruits or vegetables in general, or specific items or families of items, such as tomato sauce or cruciferae, and the other half found no associations.35 However, plasma carotenoids (a marker of vegetable and fruit intake) have been associated with greater likelihood of recurrence-free survival in one observational study.98 Results of the WHEL study, which not only promotes a low fat diet, but also daily minimum intakes of five vegetable and three fruit servings, 16 oz. of vegetable juice, and 30 g of dietary fiber should be helpful in assessing the impact of a high vegetable and fruit diet among survivors.83,99 In the meantime, cancer survivors are encouraged to consume amounts consistent with guidelines established for survivors and the U.S. Dietary Guidelines, i.e., at least five daily servings, with an ultimate goal of at least seven (for women) to nine (for men) daily servings.35,58,91
Specific Foods or Dietary Regimens
While various functional foods and dietary regimens have been identified as being potentially helpful in hindering progressive or recurrent disease among cancer survivors, to date, there is little consensus or results from randomized controlled trials, to support the use of specific foods, such
as soy or regimens, such as macrobiotic diets. Guidelines therefore call for a varied diet that is based on principles of moderation.35,89
Exercise
In recent years, several research groups have started to examine the potential effects of exercise as a supportive care intervention that may compliment existing anticancer therapies and address a multitude of concerns associated with cancer and its treatment. The Institute of Medicine report on exercise behavior for cancer survivors was primarily based on the 2004 Agency for Healthcare Research and Quality (AHRQ) evidence review.61 In the interim, four other systematic reviews have been published and summarize current evidence on exercise and adult cancer survivors.100-103 In total, these five reviews identified 16 independent research investigations that examined the role of exercise in cancer survivors following the completion of primary therapy. To summarize, most studies were conducted in breast cancer survivors with fewer studies in colorectal, non-Hodgkin’s lymphoma, or mixed cancer populations. All studies either tested the effects of endurance or mixed (endurance combined with progressive resistance training) exercise training programs prescribed at a moderate-vigorous intensity (50-75% of baseline exercise capacity), 3 or more days per week, for 10 to 60 minutes per exercise session. The length of the exercise programs lasted from 2 to 15 weeks. Major outcomes of these reports were varied and included cardiorespiratory fitness, strength, quality of life, pain, immune parameters, and depression. Overall, these reports conclude that exercise interventions following completion of primary treatment were associated with consistent and positive effects on the following outcomes: (1) vigor and vitality; (2) cardiorespiratory fitness; (3) quality of life; (4) depression; (5) anxiety; and (6) fatigue.61,101-103 Despite these positive findings, all four reviews concluded that the current putative literature provides promising preliminary evidence of the potential role of exercise in this setting and that additional large-scale, well-controlled intervention studies are required.61,101-103
In this updated review, we have examined eight additional independent studies104-111 that have been published during the past year and evaluate them against the back-drop of published reviews and reports. Similar to the studies reviewed in the IOM (AHRQ) report and the three prior systematic reviews, these recent studies continue to predominantly focus on breast cancer104-106,108,110,111 with one study each in lung109 and mixed cancer patients.107 Most studies tested the effects of a combined endurance and progressive resistance training program,104-111 two used endurance only,110,111 and one used resistance training only.105 The intervention length ranged from 2 to 12 months, and study endpoints were varied and included
cardiorespiratory fitness, quality of life indices, lymphedema, body composition, and metabolic hormone profile. Overall, the results of these eight recent studies support previous findings; significant benefits of exercise on several identified study endpoints are presented in Table D.2-1.
These findings corroborate the conclusions of the 2004 AHRQ report and the other systematic reviews suggesting that exercise is associated with a moderately positive effect on cardiorespiratory fitness and quality of life.61,101-103 Exercise also was generally associated with a small positive effect on other outcomes of interest, such as fatigue, anxiety, and depression. Importantly, no study reported any exercise-related adverse events. However, additional large-scale, well-controlled intervention studies in other cancer populations, as well as breast cancer survivors, are required that provide a comprehensive examination of safety issues.
Since the IOM report, two recent landmark studies have been reported that examined the association between physical activity and cancer recurrence and overall survival in persons diagnosed with breast112 and colon cancer.113 In the first study, Holmes and colleagues examined the association between self-reported physical activity levels and breast cancer recurrence and mortality in a cohort of 2,987 female nurses participating in the Nurses Health Study who had been diagnosed with early-stage breast cancer.112 Results indicated that women who engaged in 9 or more metabolic equivalent (MET) hours per week (equivalent to brisk walking for 1 hour, 5 days/wk) had an unadjusted absolute mortality risk reduction of 6% at 10 years compared with women who engaged in less than 3 MET hours per week (equivalent to walking at an average pace for 1 hour).112 In the second study, Meyerhardt et al.113 examined the influence of self-reported physical activity on outcome in 816 patients with colon cancer. After adjustment for medical and demographic variables, preliminary results indicated that men and women who engaged in more than 25 MET-hours of physical activity per week had a hazards ratio for disease-free survival of 0.65 (95% CI, 0.38-1.11; p for trend = 0.02) compared with patients who reported low levels of physical activity.113 These are the first reports to examine the association between exercise behavior and cancer recurrence and survival. Overall, these results significantly strengthen the evidence supporting the role of exercise for cancer survivors following the completion of primary treatment. Large-scale randomized controlled trials are now required to confirm these exciting and important findings.
Although much work remains to be done, the current literature provides sufficient evidence that exercise is a safe and well-tolerated supportive intervention that physicians can recommend to their patients following the completion of primary therapy. Clearly, as in other clinical and nonclinical populations, cancer survivors should obtain physician/oncologist clearance before embarking on any exercise intervention or program. This may be
particularly important in cancer survivors who may be at high risk for late-occurring toxicity secondary to treatment. For example, anthracycline-based chemotherapy regimens and left-sided chest radiotherapy are associated with acute and late-occurring cardiac toxicity,114-117 whereas conventional anticancer therapies are associated with several progressive disorders such as endothelial dysfunction,118 and weight gain.63,119 Either one or a combination of these disorders increases patients’ risk of CVD. Thus, appropriate CVD and cardiac screening procedures are recommended prior to the initiation of an exercise program. One additional long-term concern in breast cancer survivors initiating an exercise program is lymphedema. Although few studies have examined this question, the current evidence suggests that upper body exercise does not induce or exacerbate lymphedema.61 However, as stated in the IOM report, further research is required on this topic to formulate appropriate exercise prescriptions for women with or at risk for lymphedema;61 it is important to note that a gap in research still remains, since there have been no published studies in the interim. Until more evidence is available, current recommendations of the American Cancer Society, the Centers for Disease Control, and the American College of Sports Medicine are advised: engage in at least moderate activity for 30 minutes or more on 5 or more days per week (see Table D.2-2).35,89
Smoking Cessation
As noted in the IOM report, nearly one-third of all cancers are caused by smoking; thus, there is a high likelihood of tobacco use among survivors, especially those who have been diagnosed with smoking-related malignancies, i.e., lung, head and neck, cervix, bladder, kidney, pancreas, and myeloid leukemia.120,121 Persistent tobacco use postdiagnosis also is associated with poorer outcomes, including increased complications of treatment, progressive disease, second primaries, and increased comorbidity.122,123 Thus, while smoking cessation plays a substantial role in prevention and primary care, it is perhaps even more critical for cancer survivors to quit smoking.124 Fortunately, many survivors respond to the “teachable moment” that a cancer diagnosis provides,125 and high quit rates are noted (~50%) among survivors with smoking-related tumors.78,126 Unfortunately, many survivors are unable to remain smoke-free, with approximately one-third of smokers continuing to smoke after their cancer diagnosis.78 Recent data from the National Health Interview Survey also suggest that current smoking rates may be especially high in younger cancer survivors (ages 18-40) than in the general population,127 though subsequent controlled analyses on data with longer follow-up suggest that these differences may not be as discrepant as previously thought.128
Given evidence that combined interventions that utilize behavioral
TABLE D.2-1 Exercise Studies Following the Completion of Primary Therapy (authors in alphabetical order)
|
Authors, Year |
Site |
Sample |
Age |
Design |
Exercise Intervention |
|
Damush et al.111 |
Breast |
34 survivors an average of 3 yr post treatment |
59.6 |
Pre-Post |
Oncologist-referred self-management program to increase physical activity |
|
Lane et al.104 |
Breast |
16 dragon boat participants with no history lymphedema |
52.4 |
Pre-Post |
Resistance and endurance exercise training program with dragon boat training |
|
Ohira et al.105 |
Breast |
86 survivors an average of 2 yr post diagnosis |
Exercise (53) Control (53) |
RCT |
Progressive resistance exercise training program |
|
Pinto et al. 106 |
Breast |
86 survivors an average of 2 yr post diagnosis |
Exercise (53) Control (53) |
RCT |
Home-based physical activity intervention program |
|
Thorsen et al.107 |
Mixed |
139 lymphoma, breast, gyneco- logic, or testicu- lar survivors an average of 1 month post treatment |
Exercise (39) Control (39) |
RCT |
Home-based endurance and resistance exercise training program |
|
Cheema et al.108 |
Breast |
34 dragon-boat survivors an average of 5 yr post treatment |
57.7 |
Pre-Post |
Combined supervised resistance and endurance exercise training program |
|
Spruit et al. 109 |
Lung |
10 survivors an average of 3 months post treatment |
65.5 |
Pre-post |
Combined supervised resistance and endurance exercise training program |
|
Wilson et al. 110 |
Breast |
24 African- American survivors an average of 3 month post treatment |
55 |
Pre-post |
Theory-based community-based walking program |
|
ABBREVIATIONS: IGF-II, Insulin-like growth factor II; METs, metabolic equivalent; QOL, quality of life; RCT, randomized controlled trial; RPE, rate of perceived exertion; VO2peak, Peak Oxygen Consumption (mL.kg.min−1). |
|||||
|
Duration |
Frequency/ Intensity |
Results |
|
6 months |
3×/wk1-hr sessions for 3 weeks and telephone support |
Statistically significant ↑ in self-reported physical activity, physical fitness, perceived barriers to exercise, and QOL |
|
5 months |
3×/wk resistance (8-12 repetitions of 6 different exercises) and 3×/wk endurance (60% of maximum heart rate) exercise training. Dragon boat training 2×/wk for 90 min |
Statistically significant ↑ in upper extremity strength and volume over the course of the intervention. Changes consistent on both arms |
|
6 months |
2×/wk1-hr supervised sessions for 13 weeks followed by 2×/wk home- based sessions for 13 weeks |
Statistically significant ↑ overall QOL, upper and lower body strength, ↓ body fat and IGF-II. Changes in strength were correlated with changes in some psychosocial outcomes |
|
3 months (follow-up at 6 and 9 months) |
5×/wk for 12 weeks at 55% to 65% of maximum heart rate |
Statistically significant ↑ total and moderate physical activity minutes and physical fitness. Exercise group reported ↑ vigor and ↓ fatigue |
|
14 weeks |
Minimum of 2 sessions/wk at 60% to 70% of maximum heart rate |
Exercise had greater increase in cardiorespiratory fitness and fatigue in comparison with control group |
|
2 months |
2×/wk resistance (8-12 repetitions of 10 different exercises) and 3×/wk endurance (65% to 85% of maximum heart rate) exercise training sessions |
Statistically significant ↑ in body composition, upper and lower body strength, aerobic endurance and overall QOL |
|
2 months |
Daily cycle ergometry, treadmill walking, weight training and gymnastics at a moderate intensity |
Statistically significant ↑ in peak and endurance exercise capacity. No improvements in pulmonary function |
|
2 months (follow-up at 3 months) |
8 weekly 75 minute large and small physical activity counseling sessions |
Statistically significant ↑ in number of steps & exercise beliefs. Significant ↓ body mass index & body weight |
TABLE D.2-2 Exercise Prescription Guidelines for Cancer Survivors after Completion of Primary Treatment
|
Low Intensity (Light Effort) Endurance Exercise
|
|
Moderate Intensity (Moderate Effort) Endurance Exercise
|
|
Vigorous Intensity (Strenuous Effort) Endurance Exercise
|
|
Progressive Resistance Exercise (Weight-Bearing)
|
|
Flexibility/Stretching Exercise (Weight-Bearing)
|
|
CALCULATIONS: HRreserve = maximal heart rate (HRmax) minus resting heart rate (HRrest). Multiply HRreserve by .20 to .84 to obtain target heart rate for desired intensity of exercise. SOURCE: Adapted from Courneya208, Brown et al.,35 and Warburton et al.209,210. |
counseling along with pharmacotherapy are effective, definitive guidelines exist for providing care as it relates to smoking cessation.29 The 5-A approach endorsed by the U.S. Preventive Services Task Force provides a concrete framework for health care providers to deliver appropriate care regarding smoking cessation and is a featured element within the IOM report.29,129 Despite this extant framework, the barriers to longstanding smoking cessation success are substantial and findings from intervention trials have been mixed; the IOM report provides a solid overview of studies
conducted up until 2005 and notes the significance of smoking cessation within the survivor population and the numerous barriers that exist.29 Fortunately, the early trials of Gritz et al.130 as well as the most recent trial of Emmons et al.131 provide success stories that can guide future treatment, research, and practice. The randomized controlled trial by Emmons et al.131 tested a peer telephone counseling intervention with tailored materials against standardized self-help materials (both with optional nicotine replacement) among 796 currently smoking adult childhood cancer survivors. They found that quit rates were significantly higher in the counseling group compared to the self-help group at both the 8-month (16.8% vs. 8.5%; p < .01) and 12-month follow-up (15% vs. 9%; p < .01).131 This home-based intervention also was found to be cost-effective. This recent positive trial not only is important for its contribution to smoking cessation research, but it also paves the way more generally for future health promotion programs by testing innovative strategies that are well accepted and more readily disseminable to survivor populations who often are hard to reach. As noted in the IOM report,29 opportunities also exist for interventions that incorporate social or familial support as a key element. An ongoing trial that is currently testing the efficacy of such a family-based intervention is entitled “Family Ties” (CA92622) and results are anticipated within the next 2 years. As in areas of diet and exercise, more research is necessary to determine interventions that are optimally effective and promote permanent smoking cessation—acknowledging that continued tobacco-use may be particularly resistant in cancer survivors. It is also worth noting that smokers may represent a prime population not only for smoking cessation efforts, but also for multiple risk factor interventions, since findings of Butterfield et al.132 suggest that the majority (63%) of cancer survivors who smoke also are likely to engage in at least two to three other unhealthful lifestyle behaviors, such as sedentary behavior, high red meat consumption, and excessive alcohol use.
Other Areas (Alcohol and Sunscreen-Use, Complementary and Alternative Therapies, Osteoporosis Prevention, and Immunizations)
Alcohol Use
Alcohol, like tobacco, is an addictive substance, with the use of both being highly correlated and associated with higher risk of similar cancers, such as kidney and head and neck cancers. Given these similarities, a need for multiple behavior interventions that integrate both smoking cessation with alcohol abstinence,133,134 particularly in high-risk populations (e.g., veterans) are needed.133 To date, the only intervention undertaken that has addressed both behaviors has been in 64 adolescent cancer survivors and
from the perspective of preventing high risk behaviors rather than actively intervening in those who have longstanding addictions.135 This intervention by Hollen et al.135 was effective in modifying attitudes and behaviors short-term (1-month follow-up), but not long term (6-month follow-up).
In considering alcohol as an independent risk factor, data suggest that head and neck patients who continue to drink at least 15 servings of alcohol per week have roughly a four-fold increased risk of developing a second primary tumor compared to those who abstain.136 Morbidity due to other causes such as pulmonary and cardiovascular disease, as well as alcohol-related conditions, also is significantly higher among survivors who continue to drink.137 In contrast, current evidence does not suggest that continued alcohol-use increases risk of recurrence or all-cause mortality among breast cancer survivors, even though alcohol-use is associated with the development of mammary carcinoma.37 Differences in dose and the reduced prevalence of alcoholism within this population may explain the lack of an association. Indeed, recent analyses of the 2000 National Health Interview Survey, suggest that overall cancer survivors do not drink any more than those in the general population, though moderate-to-heavy drinking is noted more frequently among select groups, such as survivors of head, neck and lung cancers (24.1%), as well as prostate cancer (22.3%).127,128 Like smoking, however, alcohol-use diminishes significantly with age,127,128 and “risky-use” (> 2 drinks per day for men and >1 drink/day in women) is noted among only 4.1% of cancer survivors who are age 65 and older. The low prevalence of risky drinking among the majority of cancer survivors, plus established findings indicating that light-to-moderate alcohol-use is protective against CVD are taken into account in diet and physical activity recommendations established by the American Cancer Society.35,89 These recommendations parallel those purported in the U.S. Dietary Guidelines,58 and the American Heart Association,138 i.e., those who choose to drink alcohol, should do so sensibly (up to 2 drinks/day for men and up to 1 drink/day for women) and should not be taking medications or have conditions for which alcohol is contraindicated.
Complementary and Alternative Medicine:
As noted in the IOM report, the use of complementary and alternative medicine (CAM) is prevalent both in the general population and particularly among cancer survivors.29 Common categories of CAM include specific dietary or exercise regimens (e.g. the Gonzales diet, Reiki, yoga, etc), dietary and herbal supplements, acupuncture, massage and psychological or mind-body therapies (e.g. imagery, journaling, support groups). A recent paper by Hann et al.139 suggests that up to two-thirds of adult cancer
TABLE D.2-3 Patient Guidelines for Complementary and Alternative Medicine
|
survivors use some form of CAM therapy, with 69% reporting a belief that it will prevent recurrence and 25% stating that it will offer cure. A 2005 review by Monti and Yang,140 reports that CAM-use fulfills psychosocial needs that are inadequately addressed by the conventional biomedical system, and as the IOM report suggests, survivors may derive potential benefit for managing select side effects, as well as reducing pain and anxiety. Therefore physicians are encouraged to recommend select CAM therapies, such as support groups, massage, and relaxation therapy that appear safe for cancer survivors. However, given the paucity of evidence on the biological agents (e.g., chelation therapy, restrictive dietary regimens or dietary supplements), current guidelines do not endorse the use of these products or regimens.35,89,141 Instead, patients are encouraged to access reliable sources of information, such as the National Center for Complementary and Alternative Medicine (http://nccam.nih.gov) and to follow key points when considering CAM therapies (see Table D.2-3). Open dialogues with physicians and other health care providers play an integral role in this process, especially given the potential for deleterious interactions between various CAM therapies and prescribed treatments. However, as noted in the IOM review,29 patients are often reluctant to divulge such information. Thus, physicians are encouraged to initiate and maintain open communication regarding CAM.29,139-141
Sun-Protective Behaviors:
Skin cancer is the most common form of cancer in the United States.1 In 2006, it is expected that more than one million men and women will be diagnosed with one of three forms of skin cancer – basal cell carcinoma, squamous cell carcinoma, or melanoma. High levels of exposure to UV radiation increase the risk of all three types of skin cancer, and approximately 65% to 90% of melanomas are caused by UV exposure. As such, risk of skin cancer can be substantially reduced by adopting sun-protective behaviors (i.e., sunscreen-use, wearing clothing, seeking shade) that limit exposure to sunlight – the primary source of UV radiation.142
Given the central role of radiation-induced DNA damage in the etiologies of both melanoma and basal cell carcinoma, cancer survivors who have previously received locoregional radiotherapy, particularly childhood and hematopoietic cell transplantation cancer survivors, are at increased risk for certain forms of melanoma and basal cell skin cancers.143-146 In these reports, nonmelanoma cancer development occurred after a considerable latency period (10 to 20 years after radiation) suggesting that younger patients (particularly children) may have a greater inherent sensitivity to radiation.147 Given this evidence, cancer survivors, particularly those who have received radiation at a young age (i.e., childhood cancer survivors, hematopoietic cell transplant survivors) should be closely monitored for skin cancers. Physicians are encouraged to perform regular examinations during patient follow-up visits as well as recommend sun-protective behaviors demonstrated to reduce skin cancer incidence.
Despite convincing evidence that sun protective behaviors can reduce the primary incidence of benign and malignant skin lesions, only one study has attempted to increase these behaviors in cancer survivors. In this study, 200 patient-caregiver dyads were given an education-based, sun-protective intervention at 2 and 6 months following skin cancer surgery. Results indicated that both patients and caregivers reported higher sun-protective knowledge, intentions, and behavior at 1 year postsurgery.148 Although more research in cancer survivors is required, the extensive available literature documenting the benefits of these behaviors on the primary prevention of skin cancer provides sufficient evidence for physicians to recommend sun protective behaviors as part of comprehensive cancer care in these high risk patients. It is important to note, however that a controversy currently exists regarding the pros and cons of sunlight exposure in other cancers, most notably lung, prostate and colorectal cancers. The findings of Giovannuci et al.149 and others150-151 suggest that modest sunlight exposure may be protective, not only for the primary risk of cancer, but also in survival.149-151 These data call into question current guidelines and underscore the need for further research.
Osteoporosis Prevention
Osteoporosis is a common disease in healthy adults over the age of 50 years, with one in three women and one in four men being affected worldwide;152 it is a condition for which diet and physical activity play important roles. Epidemiologic findings suggest that bone density may be biomarker of cancer risk, with lower bone density being a risk factor for colorectal cancer and increased bone density being positively associated with uterine and post-menopausal breast cancer.153-157 Even though lower bone density may be protective for breast cancer in older women, clinical studies suggest that osteoporosis is still a prevalent health problem even in these survivors; data of Twiss et al.158 indicate that 80% of older breast cancer patients have t-scores less than −1 and thus have clinically confirmed osteopenia or frank osteoporosis at the time of their initial appointment.158 Thus, substantial proportions of colorectal and breast cancer patients may have suboptimal bone density at the time of diagnosis.
In addition, various cancer therapies, such as gonadotropin-releasing hormone agonists (hormone therapy), glucocorticoids, certain chemotherapeutics (e.g., methotrexate, cyclophosphamide, doxorubicin), radiation therapy, and thyroid-stimulating hormone suppressive therapy all enhance bone turnover and act to further compromise bone integrity.159,160 As such, osteo-penia, osteoporosis, and increased rates of fracture have been noted in a wide spectrum of cancer survivors, including breast, prostate, testicular, thyroid, gastric, and central nervous system cancers, as well as non-Hodgkin’s lymphoma and various hematologic malignancies.160-163
Osteoporosis is a well-documented problem not only among older adult survivors, but also among young adult survivors of childhood cancers.27,164-167 The goals of patient care are early recognition of those patients at high risk for osteoporosis and to prevent fractures in patients with documented bone deterioration. The American Society of Clinical Oncology (ASCO) has outlined a management strategy to promote bone health that includes baseline bone density assessment with continued monitoring and treatment based on bone density results.168 As reviewed by Chlebowski,159 these guidelines focus largely on pharmacologic means (e.g., pamidronate, zoledronic acid) and selective estrogen-receptor modulators (e.g., raloxifene) to improve bone density and reduce risk of fracture. Lifestyle interventions are also postulated to play an important role in addressing this issue. In healthy adults, current recommendations for osteoporosis prevention and treatment include dietary and lifestyle changes (e.g., weight-bearing exercise, consumption of adequate amounts of calcium (800-1,500 mg/day depending on age range and gender) and adequate amounts of vitamin D (400-600 iu/day), as well as reduction of ancillary risk factors found to affect intake, calcium absorption, or bone turnover, such as smoking, caffeine, alcohol,
sodium, and excessive protein consumption).169 Potential improvements on bone mineral density of lifestyle interventions are yet to be tested specifically among cancer survivors.170 To date, the only research that has been reported is a pilot study by Waltman and colleagues171 who examined the effects of a 12-month multicomponent program of progressive resistance training, alendronate, calcium, and vitamin D on preventing osteoporosis in 21 postmenopausal breast cancer survivors who had completed primary treatment. All participants experienced a significant increase in bone mineral density (BMD) of the spine and hip. Clearly, preliminary data from this study combined with the demonstrated effects of combined regimens of exercise, diet and pharmacologic agents on BMD in healthy adults provides strong suggestive evidence for future larger randomized trials to investigate the effects of multicomponent interventions that include exercise and diet on skeletal health in cancer survivors; until then the guidelines established by ASCO appear the most germane.168
Immunizations
Infections are responsible for more than half a million cancer cases worldwide each year. Of the numerous infections that have been associated with increased cancer risk, the human papillomavirus (HPV) is the most commonly recognized. The association between HPV and malignancies of the lower anogential tract, particularly the cervix, is well established.172 In the United States, comprehensive cervical cancer screening programs (the papanicolaou [pap] test) has dramatically decreased the risk of cervical cancer.172
Although the role of vaccinations in the prevention of certain forms of cancer and other diseases is an established part of clinical practice, the role of these therapies in persons who have been diagnosed with cancer remains largely unknown.173 Individuals diagnosed with cancer are often immuno-compromised as a result of treatment (e.g., chemotherapy, high-dose steroids) or the disease itself (hematologic malignancies are immunosuppressive). Thus, it appears logical that immunizations may play a beneficial role in cancer survivors who may be susceptible to bacterial, viral, and fungal infections. However, there is concern that cancer patients may be unable to provide a protective response to immunizations and, paradoxically, immunizations may even increase the risk of clinical infection.173
A recent systematic review examined the available published evidence on the role of immunizations in cancer patients who had not undergone bone marrow transplantation.173 The authors reviewed the efficacy and safety of vaccination against nine preventable diseases (i.e., haemophilus influenzae type b, hepatitis B, influenza, measles, meningococcal meningitis, poliomyelitis, 23-valent polysaccharide pneumococcus, tetanus, and
varicella) that are associated with considerable morbidity and mortality among cancer survivors. After the completion of primary treatments, the influenza vaccine response in patients with solid tumors was similar to that of healthy adults and side effects were mild. Overall, influenza vaccinations appear to be safe and well-tolerated by cancer patients both during and following primary treatments and may confer some protection against influenza-related morbidity and mortality. Fewer studies have examined the efficacy of measles vaccinations in cancer survivors because of the risks involved with vaccinating immunocompromised individuals with live vaccines. Therefore, the Centers for Disease Control and Prevention recommends that cancer patients undergoing chemotherapy should not receive measles vaccinations. In patients who have completed primary treatment, there are currently insufficient data to support measles vaccinations or vaccinations against the other preventable diseases listed. As a general rule, any patient considering vaccination should obtain physician clearance and wait at least 4 weeks after the completion of primary treatment.173
Perceived Needs for Health Promotion and Preferences for Delivery Among Cancer Survivors
Health Beliefs
Surveys conducted among cancer survivors over the past two to three decades have produced consistent findings regarding survivors’ attributions of the cause of their disease. The most frequently reported reasons (attributions) are heredity, environmental pollutants, occupation, stress, and tobacco use.174-179 These findings were confirmed in a recent population-based study by Wold et al.,180 who found attributions of cause for the following nonmodifiable and modifiable risk factors (reported as the percentage response of breast, prostate, and colorectal cancer survivors [N=670]): family history (83%); smoking (79%); environmental pollutants (69%); occupational exposures (59%); stress (56%); various dietary factors (47-51%); obesity (45%); and lack of exercise (28%). The authors concluded that public health organizations and providers need to educate survivors, as well as their healthy counterparts, on modifiable risk factors associated with the primary prevention of cancer and related morbidity.
Therefore, while most survivors attribute their cancer diagnosis to factors beyond their control (with the exception of tobacco use), relatively few credit dietary factors and obesity, and less than one-third attribute, lack of exercise. Despite these attributions, other surveys among survivor populations suggest high levels of interest in diet (54%) and exercise (51%) interventions, as well as comparable levels of interest in smoking cessation programs (60%), among adult cancer survivors who currently smoke, with
this interest in behavioral change attributed to a desire to “prevent recurrence.”181 These findings are remarkably similar in pediatric cancer survivor populations (with even higher levels of interest noted among their parents).36 Van Weert et al.182 recently reported even higher levels of interest (80%) in multiple behavior interventions. Thus, the cancer diagnosis may signal a notable “about-face” in terms of health beliefs and may be an opportune time or a “teachable moment” for undertaking health behavior change.
Behavior Change Postdiagnosis
To date, published findings exist on 30 studies that have explored persistent lifestyle practices (those that extend beyond the initial treatment year) among cancer survivors; a majority of these studies were systematically reviewed by Demark-Wahnefried et al.52 The preponderance of earlier research suggested that the practice of healthy lifestyle behaviors was higher among cancer survivors than in the population at large; however, many of these studies relied on modest-sized convenience samples and were limited in terms of length of follow-up and heterogeneity of cancer type.52 Three recent reports emanating from much larger datasets and assessing behaviors in longer-term survivors indicate that few health behavior differences exist between cancer survivors and healthy populations or noncancer controls.43,127,128
Two of these studies relied on data collected from survivors of several different cancers and who were nested within a national sample that included both cancer cases and controls, thus yielding data that are less likely to be influenced by responder bias.127,128 Analyses by Coups and Ostroff127 and Bellizzi et al.128 on health behaviors of cancer cases compared to age-and race-matched controls participating in the National Health Initiative Survey-2000 indicate that while cancer survivors are 9% (95% CI, 1.03-1.16) more likely to adhere to physical activity guidelines, for the most part their health behaviors parallel those of the general population—a population marked by inactivity, overweight or obesity, suboptimal fruit, vegetable, and fiber consumption, and high intakes of fat.58,129,130 Similar results were found in another study that exclusively tracked lifestyle behaviors in a cohort of women (N=2,321) with early-stage breast cancer.43 Thus, findings of these larger, more recent studies are in direct contrast to prior findings—differences that may be attributable to more heterogeneous samples of survivors who were followed for longer periods of time. These recent data provide us with a paradigm shift and the potential realization that although many cancer patients report healthful lifestyle changes after diagnosis, these changes may not generalize to all populations of cancer survivors or may be temporary. Given higher rates of comorbidity within
this population and evidence that diet, exercise, and tobacco use affect risk for other cancers and other chronic diseases, these recent data support a need for lifestyle interventions that target this vulnerable population, and perhaps with greater need than previously thought.2,3,5-7,11-13,16,17,21,22,27,29,45,79,129,130
When Is the Best Time to Intervene?
Few data exist as to when cancer survivors may be most receptive to health behavior interventions. An early study of 988 breast and prostate cancer survivors,181 suggests that most (57%) reported a preference for diet, exercise, and/or smoking cessation information “at diagnosis or soon thereafter” and that a significant decrease (p=.003) was noted as time elapsed from diagnosis. These results are supported by unpublished data that show response rates among elderly cancer survivors to a home-based diet and exercise intervention are 34.3% among those within 18 months of diagnosis, as compared to 13.9% among those who are 5 or more years out.183 Factors such as age and gender also may affect interest and uptake of lifestyle interventions. For example, McBride et al.184 found that interest levels for lifestyle interventions may be sustained over time among women, but not in men, since the psychological impact of disease diminishes significantly with time from diagnosis among male, but not in female survivors.
Timing of interventions also is dependent upon the targeted behavior (diet, exercise, smoking cessation, etc); the channel of delivery (clinic- or home-based), treatments received (e.g., surgery, radiation, chemotherapy), side effects (fatigue, pain, nausea, etc.), and desired outcomes (short-term symptom management or overall long-term health). Furthermore, issues such as time, transportation, child care, and patients’ willingness to undertake new lifestyle behaviors may undermine the success of health promotion efforts and require careful consideration regarding timing, content, delivery channel, and patient selection. Also important is the realization that several strategic iterations may be necessary in order to create an intervention that not only has proven efficacy, but that also is well accepted and generalizable to the patient population at large.
Preferred Channels for Delivery
As with intervention timing, there are relatively few studies that have explored preferences with regard to intervention delivery channel and even fewer that have compared the relative efficacy of different methods. In one study of 307 cancer survivors, Jones et al.185 found that 85% of cancer survivors preferred face-to-face exercise counseling for a one-session class. Other researchers have found that distance and accompanying issues of
time and transportation pose significant barriers for in-person programs, especially among older cancer survivors (61% of cancer survivors are comprised of those 65 years of age or older).181,186-188 Such barriers also are present among survivors of more rarely occurring cancers who often have to travel great distances to receive specialized care in appropriate clinical settings, i.e., childhood survivors.36 In a recent review of exercise interventions, van der Bij et al.189 leveled criticism that most health promotion interventions and programs “never reach the people who would benefit most from them.” Given the relative prevalence of cancer within the American population, as compared to more common health disorders such as CVD and diabetes, there is an enhanced need to develop interventions that, if not initially—then ultimately are disseminable to populations of cancer survivors at large. In two separate survey studies among breast and prostate cancer survivors (N=988, mean age 63 + 11 years) and childhood cancer survivors (N=209; mean age 20 + 6 years), Demark-Wahnefried and colleagues36,181 found that distance medicine-based or home-based programs were significantly favored over clinic-based venues with the proportions of survivors (breast and prostate versus childhood cancer) reporting “extremely high” to “high” levels of interest in the following delivery channels: mailed interventions (53%/59%); computer-based interventions (CD-ROM or internet) (not assessed/45-47%); and telephone counseling (23%/10%). The surprising result that mailed interventions garnered higher preference scores than computer-based formats among younger cancer survivors also is supported by the findings of Im and Chee,190 who found that cancer survivors report several barriers to computer-based programs. Also worthy to note are the recent findings of a review by Rutten et al.191 who found that cancer survivors were twice as likely to report reliance on print materials as sources of health information rather than the internet or other media sources.191 It is currently unknown whether these results are apt to change over time or whether there is a definite hardset preference for print materials over computer-based venues. Given that cancer is a disease associated with aging and that receptivity for computer-based formats is even lower in older populations, it is safe to say that although web-based programs offer future promise; full penetrance of such programs, especially among the most underserved populations of cancer survivors, is currently questionable.52
To date, the preponderance of reported health promotion efforts among cancer survivors have utilized clinic-based interventions and 11 studies have employed hybrid programs that rely on both clinic-based sessions and telephone counseling.60,99,187,192-195 Far fewer studies have tested interventions that were delivered exclusively via home-based approaches. As referred to previously, the recent successful smoking cessation trial of Emmons et al.131 which tested the efficacy of a telephone counseling and mailed
material-based intervention is a foundational effort in this arena. In another study of 86 sedentary breast cancer survivors, Pinto et al.106 found that women randomized to a 12-week telephone counseling-print material intervention, as compared to an attention control, experienced significantly greater improvements in fitness and vigor, and reduced fatigue, though no significant differences were noted in weight status or percent body fat. To date, there have been no reported findings of interventions that have been delivered exclusively through mailed or computer-based approaches, though favorable results of the Fresh Start Trial, a diet and exercise intervention delivered exclusively via series of sequentially-tailored mailed print materials, will be released at this year’s ASCO meeting. By-in-large most health promotion interventions among cancer survivors have reported favorable findings with only one study by Segal et al.196 comparing relatively efficacy between interventions delivered via clinic-based versus clinic-based plus telephone counseling formats. In their trial of 123 early stage breast cancer survivors, they found that physical functioning increased by 5.7 points in the mixed delivery group and 2.2 points in the clinic-based program, as compared a decrease of 4.1 points in the control group (p=.04), though no significant differences between groups were found in aerobic capacity.196 More research obviously is needed to determine optimal approaches, not only with regard to delivery channel, but also to such factors as timing and pairing of behavioral components.
The Role of the Oncologist in Health Promotion
A consistent and well-known factor in promoting behavior change is the recommendation of the health care provider.197-201 Currently, however only about 20% of oncology care physicians appear to offer guidance regarding healthful lifestyle change,181,202 and report barriers, such as competing treatment or health concerns, time constraints, or uncertainty regarding the delivery of appropriate health behavior messages.203-205 Creative strategies are needed to most efficiently harness the motivational power of the physician without unduly taxing resource-use. As an example, a recent randomized controlled trial (N=450) by Jones et al.206 showed that breast cancer patients who received an oncologist’s recommendation to exercise reported a mean increase of 3.4 MET hours per week, as compared to those not receiving a similar message (p=.011), furthermore, the physician’s recommendation was found to directly affect perceived behavioral control associated with behavioral change.207 Therefore, oncologists can play a key role in catalyzing behavior changes that have the potential for improving the overall long term health of their patients, and can rely on nurses and allied health personnel, as well as health behavior researchers to most efficiently and effectively promote behavior change.
Resources Available to Providers and Patients for Health Promotion
With the increasing recognition of the growing population of cancer survivors and the unique needs of this growing population, a wide range of evidence-based resources are now available. These resources not only educate oncology care providers about the unique issues facing today’s cancer survivors, but also serve to educate survivors themselves about optimal health behaviors following a cancer diagnosis and completion of primary treatments. In Table D.2-4, a list of recommended resources are provided that offer comprehensive information on cancer survivorship issues reviewed in this report. A list of specialized resources also are provided that offer more in-depth information about select areas of health promotion (e.g., exercise, healthy weight, etc.). These resources may offer information that is cancer-specific, as well as providing more general assistance.
Summary
In a recent review of the benefits of various lifestyle factors (i.e., diet, exercise, smoking cessation, alcohol abstinence and sunscreen use), Kuhn and colleagues,204 provided a rather grim assessment of the value of behavioral interventions among cancer patients. To be sure, little is known regarding the direct impact of postdiagnosis behavioral change on cancer-related progression, recurrence, or survival. In addition, there also are comparatively few data that support the role of behavior change on other health outcomes and comorbidity. Indeed, much more research is necessary, not only to determine proof of concept (i.e., that behavior change can make an impact on cancer-specific outcomes and overall health), but also to arrive at interventions that are well accepted and that reach cancer survivors who are most vulnerable. Data, however, are beginning to accumulate that show benefit. In the interim, oncology care providers can assist their patients by endorsing existing health guidelines and encouraging their patients to take active roles in pursuing general preventive health strategies.
TABLE D.2-4 Selected Resources Available to Oncology Providers and Patients Regarding Healthy Behaviors/Wellness
|
Health Behavior/Wellness |
Organization |
Contact Information |
Recommended Publication/Brochure/Website |
|
General Survivorship Issues |
American Cancer Society |
http:www.cancer.org; 1-800-ACS-2345 |
General Information, as well as specific information on diet, exercise, smoking cessation, and sunscreen use |
|
|
American Institute for Cancer Research |
http://www.aicr.org; 1-800-843-8114 |
General information, as well as specific information on diet, supplements, and exercise |
|
Cancer Information Service |
http://cis.nci.nih.gov; 1-800-4-CANCER |
General information, as well as specific information on smoking cessation |
|
|
The Centers of Disease Control |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc.gov/cancer/survivorship/ |
A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies (in conjunction with the Lance Armstrong Foundation) |
|
|
The Lance Armstrong Foundation, LIVESTRONG™ |
1-866-235-7205; http://www.livestrong.org |
LIVESTRONG™ Survivorship Notebook |
|
|
National Cancer Center Office of Cancer Survivorship |
General information, as well as links to preventive care sites |
|
Health Behavior/Wellness |
Organization |
Contact Information |
Recommended Publication/Brochure/Website |
|
|
The National Coalition for Cancer |
877-NCCS-YES (877-622-7937); NCCS, 1010 Wayne Avenue, Suite 770, Survivorship Silver Spring, MD, 20910; info@canceradvocacy.org; http://www.canceradvocacy.org/default.aspx |
Your Life After Cancer Treatment |
|
Weight Management |
American Diabetes Association |
1-800-DIABETES (1-800-342-2383); AskADA@diabetes.org; http://www.diabetes.org/weightloss-and-exercise/weightloss/portioncontrol.asp |
101 Weight Loss Tips for Preventing and Controlling Diabetes |
|
|
American Heart Association |
1-800-AHA-USA1 (1-800-242-8721); http://americanheart.org |
An Eating Plan for Healthy Americans (http://americanheart.org/presenter.jhtml?identifier=1088) |
|
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc.gov/nccdphp/dnpa/obesity/ |
Dietary Guidelines for Americans 2005 (http://www.healthierus.gov/dietaryguidelines) |
|
|
NAASO – The Obesity Society |
http://www.obesityonline.org/site/index.cfm; http://www.naaso.org/information/practicalguide.asp |
Weight assessment, and diet, and exercise information. |
|
|
National Heart Lung and Blood Institute |
http://www.nhlbi.nih.gov/health/prof/heart/index.htm#obesity |
Weight assessment and diet and exercise information. |
|
Diet |
American Dietetic Association |
1-800-877-1600; http://eatright.org |
Step Up to Nutrition and Health |
|
|
United States Department of Agriculture |
1-888-7PYRAMID (1-888-779-7264); http://mypyramid.gov |
http://mypyramid.gov/tips_resources/index.html |
|
Exercise |
American College of Sports Medicine |
(317) 637-9200; http://www.acsm.org |
Current Comments (a series of statements concerning sports medicine and exercise) http://www.acsm.org/AM/Template.cfm?Section=Current_Comments |
|
|
American Heart Association |
1-800-AHA-USA1 (1-800-242-8721); http://americanheart.org |
How Can Physical Activity Become a Way of Life? Why Should I Be Physically Active? |
|
|
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc.gov/nccdphp/dnpa/physical/ |
Trials for Health: Increasing Opportunities for Physical Activity in the Community |
|
Smoking Cessation |
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); http://www.cdc.gov/tobacco; http://www.cdc.gov/tobacco/how2quit.htm. |
You can Quit Smoking: Consumer Guide (http://www.cdc.gov/tobacco/quit/canquit.htm) |
|
|
National Cancer Institute |
1-800-QUIT-NOW (1-800-784-8669); http://www.cancer.gov. |
Clearing the Air (for all smokers) Clear Horizons (for smokers over age 50) Forever Free (for smokers who have recently quit) (all available at http://www.smokefree.gov/info.html) continued |
|
Health Behavior/Wellness |
Organization |
Contact Information |
Recommended Publication/Brochure/Website |
|
Alcohol Use |
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc.gov/alcohol/index.htm |
Several links to government agencies and nonprofit organizations that address alcohol and health |
|
|
National Institute on Alcohol Abuse and Alcoholism |
National Institute on Alcohol Abuse and Alcoholism (NIAAA), niaaaweb-r@exchange,nih.gov; http://www.niaaa.nih.gov |
Several links to national alcohol data, NIAAA-sponsored websites, newsletters, etc. |
|
Complementary and Alternative Medicine |
National Cancer Institute |
1-800-4-CANCER (1-800-422-6237); National Cancer Institute’s Cancer Information Service; http://www.cancer.gov; http://www.cancer.gov/cancertopics/treatment/cam. Also see Office ofCancer Complementary and Alternative Medicine: http://www.cancer.gov/cam/ |
Links to several specific complementary and alternative medicine topics (http://www.cancer.gov/cancertopics/treatment/cam) |
|
|
National Center for Complementary and Alternative Medicine |
1-888-644-6226; nccam.nih.gov; info@nccam.nih.gov |
Links to several specific complementary and alternative medicine topics (http://nccam.nih.gov/health/) |
|
Sun-Protective Behaviors |
American Academy of Dermatology |
866-503-SKIN (866-503-7546); http://www.aad.org |
Skin Cancer Updates (several useful links on the latest skin cancer news) http://www.aad.org/public/News/DermInfo/DInfoSkinCancerUpdates.htm |
|
|
National Cancer Institute |
1-800-4-CANCER (1-800-422-6237); National Cancer Institute’s Cancer Information Service; http://www.cancer.gov; http://www.cancer.gov/cancertopics/types/skin |
What You Need to Know About Skin Cancer http://www.cancer.gov/cancerinfo/wyntk/skin |
|
Skin Cancer Foundation |
1-800-SKIN-490 (1-800-754-6490); http://www/skincancer.org |
Links to several brochures and manuals about skin cancer; https://www.skincancer.org/catalog/index.php |
|
|
Osteoporosis Prevention |
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc.gov/nccdphp/dnpa/bonehealth |
Links to several brochures and manuals about osteoporosis; http://www.cdc.gov/nccdphp/dnpa/bonehealth/osteoporosis_month.htm |
|
|
National Osteoporosis Foundation |
202-223-2226; http://www.nof.org |
Links to several brochures and manuals about osteoporosis; http://www.nof.org |
|
Immunizations |
The Centers for Disease Control and Prevention |
1-800-CDC-INFO (1-800-232-4636); cdcinfo@cdc.gov; http://www.cdc. |
Links to several brochures and manuals about the national immunization program; http://www.cdc.gov/nip/gov/nip/ |
REFERENCES
1. Jemal A, Siegel R, Ward E, et al: Cancer statistics, 2006. CA Cancer J Clin 56:106-30, 2006
2. Jemal A, Clegg LX, Ward E, et al: Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer 101:3-27, 2004
3. Rowland J, Mariotto A, Aziz N, et al: Cancer Survivorship - United States. MMWR 53:526-529, 2004
4. Aziz NM: Cancer survivorship research: challenge and opportunity. J Nutr 132:3494S-3503S, 2002
5. Aziz NM, Rowland JH: Trends and advances in cancer survivorship research: challenge and opportunity. Semin Radiat Oncol 13:248-66, 2003
6. Brown BW, Brauner C, Minnotte MC: Noncancer deaths in white adult cancer patients. J Natl Cancer Inst 85:979-87, 1993
7. Day RW: Future need for more cancer research. J Am Diet Assoc 98:523, 1998
8. Edwards BK, Howe HL, Ries LA, et al: Annual report to the nation on the status of cancer, 1973-1999, featuring implications of age and aging on U.S. cancer burden. Cancer 94:2766-92, 2002
9. Ganz PA: Late effects of cancer and its treatment. Semin Oncol Nurs 17:241-8, 2001
10. Hewitt M, Rowland JH, Yancik R: Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci 58:82-91, 2003
11. Leigh SA: The long-term cancer survivor: a challenge for nurse practitioners. Nurse Pract Forum 9:192-6, 1998
12. Li FP, Stovall EL: Long-term survivors of cancer. Cancer Epidemiol Biomarkers Prev 7:269-70, 1998
13. Meadows AT, Varricchio C, Crosson K, et al: Research issues in cancer survivorship: report of a workshop sponsored by the Office of Cancer Survivorship, National Cancer Institute. Cancer Epidemiol Biomarkers Prev 7:1145-51, 1998
14. Schultz PN, Beck ML, Stava C, et al: Cancer survivors. Work related issues. Aaohn J 50:220-6, 2002
15. Travis LB: Therapy-associated solid tumors. Acta Oncol 41:323-33, 2002
16. Nord C, Mykletun A, Thorsen L, et al: Self-reported health and use of health care services in long-term cancer survivors. Int J Cancer 114:307-16, 2005
17. Wingo PA, Ries LA, Parker SL, et al: Long-term cancer patient survival in the United States. Cancer Epidemiol Biomarkers Prev 7:271-82, 1998
18. Ashing-Giwa K, Ganz PA, Petersen L: Quality of life of African-American and white long term breast carcinoma survivors. Cancer 85:418-26, 1999
19. Baker F, Haffer SC, Denniston M: Health-related quality of life of cancer and noncancer patients in Medicare managed care. Cancer 97:674-81, 2003
20. Bradley CJ, Neumark D, Luo Z, et al: Employment outcomes of men treated for prostate cancer. J Natl Cancer Inst 97:958-65, 2005
21. Mandelblatt JS, Edge SB, Meropol NJ, et al: Predictors of long-term outcomes in older breast cancer survivors: perceptions versus patterns of care. J Clin Oncol 21:855-63, 2003
22. Silliman RA, Prout MN, Field T, et al: Risk factors for a decline in upper body function following treatment for early stage breast cancer. Breast Cancer Res Treat 54:25-30, 1999
23. Williams ME: Identifying the older person likely to require long-term care services. J Am Geriatr Soc 35:761-6, 1987
24. Chirikos TN, Russell-Jacobs A, Jacobsen PB: Functional impairment and the economic consequences of female breast cancer. Women Health 36:1-20, 2002
25. Chang S, Long SR, Kutikova L, et al: Estimating the cost of cancer: results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. J Clin Oncol 22:3524-30, 2004
26. Ramsey SD, Berry K, Etzioni R: Lifetime cancer-attributable cost of care for long term survivors of colorectal cancer. Am J Gastroenterol 97:440-5, 2002
27. Schultz PN, Beck ML, Stava C, et al: Health profiles in 5836 long-term cancer survivors. Int J Cancer 104:488-95, 2003
28. Yabroff KR, Lawrence WF, Clauser S, et al: Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst 96:1322-30, 2004
29. Hewitt M, Greenfield S, Stovall EL: Institute of Medicine and National Research Council: From Cancer Patient to Cancer Survivors: Lost in Transition. Washington, DC, National Academies Press, 2006
30. Beckett DM: Rethinking nutritional support for persons with cancer cachexia: A call for research to evaluate the effects of nutaceuticals. Biological Research in Nursing, in press
31. Brown JK: A systematic review of the evidence on symptom management of cancer-related anorexia and cachexia. Oncol Nurs Forum 29:517-32, 2002
32. Meacham LR, Gurney JG, Mertens AC, et al: Body mass index in long-term adult survivors of childhood cancer: a report of the Childhood Cancer Survivor Study. Cancer 103:1730-9, 2005
33. Schattner MA, Willis HJ, Raykher A, et al: Long-term enteral nutrition facilitates optimization of body weight. JPEN J Parenter Enteral Nutr 29:198-203, 2005
34. Ravasco P, Monteiro-Grillo I, Vidal PM, et al: Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol 23:1431-8, 2005
35. Brown JK, Byers T, Doyle C, et al: Nutrition and physical activity during and after cancer treatment: An American Cancer Society guide for informed choices. CA Cancer J Clin, in press
36. Demark-Wahnefried W, Werner C, Clipp EC, et al: Survivors of childhood cancer and their guardians. Cancer 103:2171-80, 2005
37. Rock CL, Demark-Wahnefried W: Nutrition and survival after the diagnosis of breast cancer: a review of the evidence. J Clin Oncol 20:3302-16, 2002
38. Bergstrom A, Pisani P, Tenet V, et al: Overweight as an avoidable cause of cancer in Europe. Int J Cancer 91:421-30, 2001
39. Organization WH: International Agency for Research in Cancer Handbook of Cancer Prevention, 2002
40. Amling CL: The association between obesity and the progression of prostate and renal cell carcinoma. Urol Oncol 22:478-84, 2004
41. Calle EE, Rodriguez C, Walker-Thurmond K, et al: Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348:1625-38, 2003
42. Freedland SJ, Aronson WJ, Kane CJ, et al: Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital database study group. J Clin Oncol 22:446-53, 2004
43. Caan B, Sternfeld B, Gunderson E, et al: Life After Cancer Epidemiology (LACE) Study: a cohort of early stage breast cancer survivors (United States). Cancer Causes Control 16:545-56, 2005
44. Herman DR, Ganz PA, Petersen L, et al: Obesity and cardiovascular risk factors in younger breast cancer survivors: The Cancer and Menopause Study (CAMS). Breast Cancer Res Treat 93:13-23, 2005
45. Kroenke CH, Chen WY, Rosner B, et al: Weight, weight gain, and survival after breast cancer diagnosis. J Clin Oncol 23:1370-8, 2005
46. Camoriano JK, Loprinzi CL, Ingle JN, et al: Weight change in women treated with adjuvant therapy or observed following mastectomy for node-positive breast cancer. J Clin Oncol 8:1327-34, 1990
47. Chlebowski RT, Weiner JM, Reynolds R, et al: Long-term survival following relapse after 5-FU but not CMF adjuvant breast cancer therapy. Breast Cancer Res Treat 7:23-30, 1986
48. Goodwin PJ, Panzarella T, Boyd NF: Weight gain in women with localized breast cancer—a descriptive study. Breast Cancer Res Treat 11:59-66, 1988
49. Heasman KZ, Sutherland HJ, Campbell JA, et al: Weight gain during adjuvant chemotherapy for breast cancer. Breast Cancer Res Treat 5:195-200, 1985
50. Levine EG, Raczynski JM, Carpenter JT: Weight gain with breast cancer adjuvant treatment. Cancer 67:1954-9, 1991
51. Courneya KS, Karvinen KH, Campbell KL, et al: Associations among exercise, body weight, and quality of life in a population-based sample of endometrial cancer survivors. Gynecol Oncol 97:422-30, 2005
52. Demark-Wahnefried W, Aziz NM, Rowland JH, et al: Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol 23:5814-30, 2005
53. Houston DK, Stevens J, Cai J, et al: Role of weight history on functional limitations and disability in late adulthood: the ARIC study. Obes Res 13:1793-802, 2005
54. Chlebowski RT, Aiello E, McTiernan A: Weight loss in breast cancer patient management. J Clin Oncol 20:1128-43, 2002
55. McTiernan A: Obesity and cancer: the risks, science, and potential management strategies. Oncology (Williston Park) 19:871-81; discussion 881-2, 885-6, 2005
56. Irwin ML, McTiernan A, Bernstein L, et al: Relationship of obesity and physical activity with C-peptide, leptin, and insulin-like growth factors in breast cancer survivors. Cancer Epidemiol Biomarkers Prev 14:2881-8, 2005
57. Calle EE, Kaaks R: Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4:579-91, 2004
58. Services USDohaH: Dietary Guidelines for Americans 2005, U.S. Department of Agriculture, 2005
59. de Waard F, Ramlau R, Mulders Y, et al: A feasibility study on weight reduction in obese postmenopausal breast cancer patients. Eur J Cancer Prev 2:233-8, 1993
60. Djuric Z, DiLaura NM, Jenkins I, et al: Combining weight-loss counseling with the weight watchers plan for obese breast cancer survivors. Obes Res 10:657-65, 2002
61. Quality AfHRa: Effectiveness of Behavioral Interventions to Modify Physical Activity Behaviors in General Populations and Cancer Patients and Survivors. Rockville, MD, U.S. Department of Health and Human Services (AHRQ Publ. No. 04-E027-2), 2004, pp 107-111
62. Goodwin P, Esplen MJ, Butler K, et al: Multidisciplinary weight management in locoregional breast cancer: results of a phase II study. Breast Cancer Res Treat 48:53-64, 1998
63. Demark-Wahnefried W, Peterson BL, Winer EP, et al: Changes in weight, body composition, and factors influencing energy balance among premenopausal breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol 19:2381-9, 2001
64. Freedman RJ, Aziz N, Albanes D, et al: Weight and body composition changes during and after adjuvant chemotherapy in women with breast cancer. J Clin Endocrinol Metab 89:2248-53, 2004
65. Harvie MN, Howell A, Thatcher N, et al: Energy balance in patients with advanced NSCLC, metastatic melanoma and metastatic breast cancer receiving chemotherapy— a longitudinal study. Br J Cancer 92:673-80, 2005
66. Smith MR: Changes in body composition during hormonal therapy for prostate cancer. Clin Prostate Cancer 2:18-21, 2003
67. Warner JT, Evans WD, Webb DK, et al: Body composition of long-term survivors of acute lymphoblastic leukaemia. Med Pediatr Oncol 38:165-72, 2002
68. Heber D, Ingles S, Ashley JM, et al: Clinical detection of sarcopenic obesity by bioelectrical impedance analysis. Am J Clin Nutr 64:472S-477S, 1996
69. McKenzie DC, Kalda AL: Effect of upper extremity exercise on secondary lymphedema in breast cancer patients: a pilot study. J Clin Oncol 21:463-6, 2003
70. Jenkins I, Djuric Z, Darga L, et al: Relationship of psychiatric diagnosis and weight loss maintenance in obese breast cancer survivors. Obes Res 11:1369-75, 2003
71. Health NIo: The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, 2000
72. Rolls BJ, Drewnowski A, Ledikwe JH: Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc 105:S98-103, 2005
73. Nestle M: Increasing portion sizes in American diets: more calories, more obesity. J Am Diet Assoc 103:39-40, 2003
74. Nielsen SJ, Popkin BM: Patterns and trends in food portion sizes, 1977-1998. Jama 289:450-3, 2003
75. Rolls BJ, Roe LS, Meengs JS: Reductions in portion size and energy density of foods are additive and lead to sustained decreases in energy intake. Am J Clin Nutr 83:11-7, 2006
76. Smiciklas-Wright H, Mitchell DC, Mickle SJ, et al: Foods commonly eaten in the United States, 1989-1991 and 1994-1996: are portion sizes changing? J Am Diet Assoc 103:41-7, 2003
77. Young LR, Nestle M: The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health 92:246-9, 2002
78. Demark-Wahnefried W, Pinto BM, Gritz ER: Promoting health and physical function among cancer survivors: Potential for prevention and questions that remain. J Clin Oncol, in press
79. Kroenke CH, Fung TT, Hu FB, et al: Dietary patterns and survival after breast cancer diagnosis. J Clin Oncol 23:9295-303, 2005
80. Rock CL: Diet and breast cancer: can dietary factors influence survival? J Mammary Gland Biol Neoplasia 8:119-32, 2003
81. Meyer F, Bairati I, Shadmani R, et al: Dietary fat and prostate cancer survival. Cancer Causes Control 10:245-51, 1999
82. Chlebowski RT, Blackburn GL, Elashoff RE, et al: Dietary fat reduction in postmenopausal women with primary breast cancer: Phase III Women’s Intervention Nutrition Study (WINS). Proceedings of the American Society of Clinical Oncology 24, 2005
83. Pierce JP, Faerber S, Wright FA, et al: A randomized trial of the effect of a plant-based dietary pattern on additional breast cancer events and survival: the Women’s Healthy Eating and Living (WHEL) Study. Control Clin Trials 23:728-56, 2002
84. Rock CL, Flatt SW, Thomson CA, et al: Effects of a high-fiber, low-fat diet intervention on serum concentrations of reproductive steroid hormones in women with a history of breast cancer. J Clin Oncol 22:2379-87, 2004
85. Hebert JR, Ebbeling CB, Olendzki BC, et al: Change in women’s diet and body mass following intensive intervention for early-stage breast cancer. J Am Diet Assoc 101:421-31, 2001
86. Kristal AR, Shattuck AL, Bowen DJ, et al: Feasibility of using volunteer research staff to deliver and evaluate a low-fat dietary intervention: the American Cancer Society Breast Cancer Dietary Intervention Project. Cancer Epidemiol Biomarkers Prev 6:459-67, 1997
87. Nordevang E, Callmer E, Marmur A, et al: Dietary intervention in breast cancer patients: effects on food choice. Eur J Clin Nutr 46:387-96, 1992
88. Chlebowski RT, Rose D, Buzzard IM, et al: Adjuvant dietary fat intake reduction in postmenopausal breast cancer patient management. The Women’s Intervention Nutrition Study (WINS). Breast Cancer Res Treat 20:73-84, 1992
89. Brown JK, Byers T, Doyle C, et al: Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin 53:268-91, 2003
90. MacLean CH, Newberry SJ, Mojica WA, et al: Effects of omega-3 fatty acids on cancer risk: a systematic review. JAMA 295:403-15, 2006
91. Krauss RM, Eckel RH, Howard B, et al: Revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. J Nutr 131:132-46, 2001
92. World Health Organization: Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO EXpert Consultation. World Health Organization Technical Report Series 916, 2003
93. Hebert JR, Hurley TG, Ma Y: The effect of dietary exposures on recurrence and mortality in early stage breast cancer. Breast Cancer Res Treat 51:17-28, 1998
94. Institute of Medicine: Dietary Reference Intakes for Energy, Carbohydrates,, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. 2002
95. Asano T, McLeod RS: Dietary fibre for the prevention of colorectal adenomas and carcinomas. Cochrane Database Syst Rev:CD003430, 2002
96. Jacobs ET, Lanza E, Alberts DS, et al: Fiber, sex, and colorectal adenoma: results of a pooled analysis. Am J Clin Nutr 83:343-9, 2006
97. Krone CA, Ely JT: Controlling hyperglycemia as an adjunct to cancer therapy. Integr Cancer Ther 4:25-31, 2005
98. Rock CL, Flatt SW, Natarajan L, et al: Plasma carotenoids and recurrence-free survival in women with a history of breast cancer. J Clin Oncol 23:6631-8, 2005
99. Pierce JP, Newman VA, Flatt SW, et al: Telephone counseling intervention increases intakes of micronutrient- and phytochemical-rich vegetables, fruit and fiber in breast cancer survivors. J Nutr 134:452-8, 2004
100. Schmitz KH, Holtzman J, Courneya KS, et al: Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 14:1588-95, 2005
101. Knols R, Aaronson NK, Uebelhart D, et al: Physical exercise in cancer patients during and after medical treatment: a systematic review of randomized and controlled clinical trials. J Clin Oncol 23:3830-42, 2005
102. Conn VS, Hafdahl AR, Porock DC, et al: A meta-analysis of exercise interventions among people treated for cancer. Support Care Cancer, 2006
103. Galvao DA, Newton RU: Review of exercise intervention studies in cancer patients. J Clin Oncol 23:899-909, 2005
104. Lane K, Jespersen D, McKenzie DC: The effect of a whole body exercise programme and dragon boat training on arm volume and arm circumference in women treated for breast cancer. Eur J Cancer Care (Engl) 14:353-8, 2005
105. Ohira T, Schmitz KH, Ahmed RL, et al: Effects of weight training on quality of life in recent breast cancer survivors: the Weight Training for Breast Cancer Survivors (WTBS) study. Cancer, 2006
106. Pinto BM, Frierson GM, Rabin C, et al: Home-based physical activity intervention for breast cancer patients. J Clin Oncol 23:3577-87, 2005
107. Thorsen L, Skovlund E, Stromme SB, et al: Effectiveness of physical activity on cardiorespiratory fitness and health-related quality of life in young and middle-aged cancer patients shortly after chemotherapy. J Clin Oncol 23:2378-88, 2005
108. Cheema BS, Gaul CA: Full-body exercise training improves fitness and quality of life in survivors of breast cancer. J Strength Cond Res 20:14-21, 2006
109. Spruit MA, Janssen PP, Willemsen SC, et al: Exercise capacity before and after an 8-week multidisciplinary inpatient rehabilitation program in lung cancer patients: A pilot study. Lung Cancer 52:257-60, 2006
110. Wilson DB, Porter JS, Parker G, et al: Anthropometric changes using a walking intervention in African American breast cancer survivors: a pilot study. Prev Chronic Dis 2:A16, 2005
111. Damush TM, Perkins A, Miller K: The implementation of an oncologist referred, exercise self-management program for older breast cancer survivors. Psychooncology, 2005
112. Holmes MD, Chen WY, Feskanich D, et al: Physical activity and survival after breast cancer diagnosis. JAMA 293:2479-86, 2005
113. Meyerhardt JA, Heseltine D, Niedzwiecki D, et al: The impact of physical activity on patients with stage III colon cancer: Findings from Intergroup trial CALGB 89803. Proceedings of the American Society of Clinical Oncology, 2005
114. Henderson IC, Berry DA, Demetri GD, et al: Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol 21:976-83, 2003
115. Meinardi MT, van Veldhuisen DJ, Gietema JA, et al: Prospective evaluation of early cardiac damage induced by epirubicin-containing adjuvant chemotherapy and locoregional radiotherapy in breast cancer patients. J Clin Oncol 19:2746-53, 2001
116. Perez EA, Suman VJ, Davidson NE, et al: Effect of doxorubicin plus cyclophosphamide on left ventricular ejection fraction in patients with breast cancer in the North Central Cancer Treatment Group N9831 Intergroup Adjuvant Trial. J Clin Oncol 22:3700-4, 2004
117. Piccart MJ, Di Leo A, Beauduin M, et al: Phase III trial comparing two dose levels of epirubicin combined with cyclophosphamide with cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer. J Clin Oncol 19:3103-10, 2001
118. Beckman JA, Thakore A, Kalinowski BH, et al: Radiation therapy impairs endothelium-dependent vasodilation in humans. J Am Coll Cardiol 37:761-5, 2001
119. Demark-Wahnefried W, Winer EP, Rimer BK: Why women gain weight with adjuvant chemotherapy for breast cancer. J Clin Oncol 11:1418-29, 1993
120. Cancer IAfRo: International Agency for Research on Cancer monographs on the evaluation of the carcinogenic risk of chemicals to humans. Lyon, France, International Agency for Research on Cancer Press, 2004
121. American Cancer Society: Cancer Prevention and Early Detection, 2006
122. Gritz ER, Dresler C, Sarna L: Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Cancer Epidemiol Biomarkers Prev 14:2287-93, 2005
123. Lin K, Patel SG, Chu PY, et al: Second primary malignancy of the aerodigestive tract in patients treated for cancer of the oral cavity and larynx. Head Neck 27:1042-8, 2005
124. Gritz ER, Vidrine DJ, Lazev AB: Smoking cessation in cancer patients: Never too late to quit. In Given B, Given CW, Champion V, et al (eds): Evidence-Based Interventions in Oncology. New York, Springer Publishing Company, 2003, pp 107-140
125. McBride CM, Ostroff JS: Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control 10:325-33, 2003
126. Gritz ER, Fingeret MC, Vidrine DJ, et al: Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer 106:17-27, 2006
127. Coups EJ, Ostroff JS: A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med 40:702-11, 2005
128. Bellizzi KM, Rowland JH, Jeffery DD, et al: Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol 23:8884-93, 2005
129. Force USPST: Counseling to Prevent Tobacco Use and Tobacco-Related Disease: Recommendation Statement, 2003
130. Gritz ER, Carr CR, Rapkin D, et al: Predictors of long-term smoking cessation in head and neck cancer patients. Cancer Epidemiol Biomarkers Prev 2:261-70, 1993
131. Emmons KM, Puleo E, Park E, et al: Peer-delivered smoking counseling for childhood cancer survivors increases rate of cessation: the partnership for health study. J Clin Oncol 23:6516-23, 2005
132. Butterfield RM, Park ER, Puleo E, et al: Multiple risk behaviors among smokers in the childhood cancer survivors study cohort. Psychooncology 13:619-29, 2004
133. Lambert MT, Terrell JE, Copeland LA, et al: Cigarettes, alcohol, and depression: characterizing head and neck cancer survivors in two systems of care. Nicotine Tob Res 7:233-41, 2005
134. Pinto BM, Trunzo JJ: Health behaviors during and after a cancer diagnosis. Cancer 104:2614-23, 2005
135. Hollen PJ, Hobbie WL, Finley SM: Testing the effects of a decision-making and risk-reduction program for cancer-surviving adolescents. Oncol Nurs Forum 26:1475-86, 1999
136. Day GL, Blot WJ, Shore RE, et al: Second cancers following oral and pharyngeal cancers: role of tobacco and alcohol. J Natl Cancer Inst 86:131-7, 1994
137. Deleyiannis FW, Thomas DB, Vaughan TL, et al: Alcoholism: independent predictor of survival in patients with head and neck cancer. J Natl Cancer Inst 88:542-9, 1996
138. Association AH: American Heart Association Dietary Guidelines, 2006
139. Hann DM, Baker F, Roberts CS, et al: Use of complementary therapies among breast and prostate cancer patients during treatment: a multisite study. Integr Cancer Ther 4:294-300, 2005
140. Monti DA, Yang J: Complementary medicine in chronic cancer care. Semin Oncol 32:225-31, 2005
141. Rock E, DeMichele A: Nutritional approaches to late toxicities of adjuvant chemotherapy in breast cancer survivors. J Nutr 133:3785S-3793S, 2003
142. Saraiya M, Glanz K, Briss PA, et al: Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med 27:422-66, 2004
143. Leisenring W, Friedman DL, Flowers ME, et al: Nonmelanoma skin and mucosal cancers after hematopoietic cell transplantation. J Clin Oncol 24:1119-26, 2006
144. Euvrard S, Kanitakis J, Claudy A: Skin cancers after organ transplantation. N Engl J Med 348:1681-91, 2003
145. Bhatia S, Estrada-Batres L, Maryon T, et al: Second primary tumors in patients with cutaneous malignant melanoma. Cancer 86:2014-20, 1999
146. Baker KS, DeFor TE, Burns LJ, et al: New malignancies after blood or marrow stem-cell transplantation in children and adults: incidence and risk factors. J Clin Oncol 21:1352-8, 2003
147. Levi F, Moeckli R, Randimbison L, et al: Skin cancer in survivors of childhood and adolescent cancer. Eur J Cancer 42:656-659, 2006
148. Robinson JK, Rademaker AW: Skin cancer risk and sun protection learning by helpers of patients with nonmelanoma skin cancer. Prev Med 24:333-41, 1995
149. Giovannucci E, Liu Y, Rimm EB, et al: Prospective study of predictors of vitamin D status and cancer incidence and mortality in men. J Natl Cancer Inst 98:451-9, 2006
150. Gorham ED, Garland CF, Garland FC, et al: Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol 97:179-94, 2005
151. Zhou W, Suk R, Liu G, et al: Vitamin D is associated with improved survival in early-stage non-small cell lung cancer patients. Cancer Epidemiol Biomarkers Prev 14:2303-9, 2005
152. Foundation IO: Osteoporosis in the European Community: a call to action - an audit of policy developments since 1998. Lyon, France, International Osteoporosis Foundation, 2003
153. Nelson RL, Turyk M, Kim J, et al: Bone mineral density and the subsequent risk of cancer in the NHANES I follow-up cohort. BMC Cancer 2:22, 2002
154. Buist DS, LaCroix AZ, Barlow WE, et al: Bone mineral density and endogenous hormones and risk of breast cancer in postmenopausal women (United States). Cancer Causes Control 12:213-22, 2001
155. Newcomb PA, Trentham-Dietz A, Egan KM, et al: Fracture history and risk of breast and endometrial cancer. Am J Epidemiol 153:1071-8, 2001
156. van der Klift M, de Laet CE, Coebergh JW, et al: Bone mineral density and the risk of breast cancer: the Rotterdam Study. Bone 32:211-6, 2003
157. Zmuda JM, Cauley JA, Ljung BM, et al: Bone mass and breast cancer risk in older women: differences by stage at diagnosis. J Natl Cancer Inst 93:930-6, 2001
158. Twiss JJ, Waltman N, Ott CD, et al: Bone mineral density in postmenopausal breast cancer survivors. J Am Acad Nurse Pract 13:276-84, 2001
159. Chlebowski RT: Bone health in women with early-stage breast cancer. Clin Breast Cancer 5 Suppl:S35-40, 2005
160. Mackey JR, Joy AA: Skeletal health in postmenopausal survivors of early breast cancer. Int J Cancer 114:1010-5, 2005
161. Smith MR: Therapy Insight: osteoporosis during hormone therapy for prostate cancer. Nat Clin Pract Urol 2:608-15; quiz 628, 2005
162. Greenspan SL, Coates P, Sereika SM, et al: Bone loss after initiation of androgen deprivation therapy in patients with prostate cancer. J Clin Endocrinol Metab 90:6410-7, 2005
163. Lee H, McGovern K, Finkelstein JS, et al: Changes in bone mineral density and body composition during initial and long-term gonadotropin-releasing hormone agonist treatment for prostate carcinoma. Cancer 104:1633-7, 2005
164. Arikoski P, Voutilainen R, Kroger H: Bone mineral density in long-term survivors of childhood cancer. J Pediatr Endocrinol Metab 16 (Suppl) 2:343-53, 2003
165. Baroncelli GI, Bertelloni S, Sodini F, et al: Osteoporosis in children and adolescents: etiology and management. Paediatr Drugs 7:295-323, 2005
166. Relling MV, Yang W, Das S, et al: Pharmacogenetic risk factors for osteonecrosis of the hip among children with leukemia. J Clin Oncol 22:3930-6, 2004
167. Kelly J, Damron T, Grant W, et al: Cross-sectional study of bone mineral density in adult survivors of solid pediatric cancers. J Pediatr Hematol Oncol 27:248-53, 2005
168. Hillner BE, Ingle JN, Chlebowski RT, et al: American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21:4042-57, 2003
169. Gass M, Dawson-Hughes B: Preventing osteoporosis-related fractures: an overview. Am J Med 119:S3-S11, 2006
170. Swenson KK, Henly SJ, Shapiro AC, et al: Interventions to prevent loss of bone mineral density in women receiving chemotherapy for breast cancer. Clin J Oncol Nurs 9:177-84, 2005
171. Waltman NL, Twiss JJ, Ott CD, et al: Testing an intervention for preventing osteoporosis in postmenopausal breast cancer survivors. J Nurs Scholarsh 35:333-8, 2003
172. Frazer IH, Cox JT, Mayeaux EJ, Jr., et al: Advances in prevention of cervical cancer and other human papillomavirus-related diseases. Pediatr Infect Dis J 25:S65-81, quiz S82, 2006
173. Arrowood JR, Hayney MS: Immunization recommendations for adults with cancer. Ann Pharmacother 36:1219-29, 2002
174. Faller H, Schilling S, Otteni M, et al: [Social support and social stress in tumor patients and their partners]. Z Psychosom Med Psychoanal 41:141-57, 1995
175. Linn MW, Linn BS, Harris R: Effects of counseling for late stage cancer patients. Cancer 49:1048-55, 1982
176. Linn MW, Linn BS, Stein SR: Beliefs about causes of cancer in cancer patients. Soc Sci Med 16:835-9, 1982
177. Maskarinec G, Gotay CC, Tatsumura Y, et al: Perceived cancer causes: use of complementary and alternative therapy. Cancer Pract 9:183-90, 2001
178. Stewart DE, Cheung AM, Duff S, et al: Attributions of cause and recurrence in long-term breast cancer survivors. Psychooncology 10:179-83, 2001
179. Stewart DE, Wong F, Duff S, et al: “What doesn’t kill you makes you stronger”: an ovarian cancer survivor survey. Gynecol Oncol 83:537-42, 2001
180. Wold KS, Byers T, Crane LA, et al: What do cancer survivors believe causes cancer? (United States). Cancer Causes Control 16:115-23, 2005
181. Demark-Wahnefried W, Peterson B, McBride C, et al: Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer 88:674-84, 2000
182. van Weert E, Hoekstra-Weebers J, Grol B, et al: A multidimensional cancer rehabilitation program for cancer survivors: effectiveness on health-related quality of life. J Psychosom Res 58:485-96, 2005
183. Demark-Wahnefried W: Unpublished data. 2006
184. McBride CM, Clipp E, Peterson BL, et al: Psychological impact of diagnosis and risk reduction among cancer survivors. Psychooncology 9:418-27, 2000
185. Jones LW, Courneya KS: Exercise counseling and programming preferences of cancer survivors. Cancer Pract 10:208-15, 2002
186. Glanz K: Behavioral research contributions and needs in cancer prevention and control: dietary change. Prev Med 26:S43-55, 1997
187. Pinto BM, Friedman R, Marcus BH, et al: Effects of a computer-based, telephone-counseling system on physical activity. Am J Prev Med 23:113-20, 2002
188. Rose MA: Health promotion and risk prevention: applications for cancer survivors. Oncol Nurs Forum 16:335-40, 1989
189. van der Bij AK, Laurant MG, Wensing M: Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med 22:120-33, 2002
190. Im EO, Chee W: Issues in Internet survey research among cancer patients. Cancer Nurs 27:34-42; quiz 43-4, 2004
191. Rutten LJ, Arora NK, Bakos AD, et al: Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ Couns 57:250-61, 2005
192. Courneya KS, Friedenreich CM, Quinney HA, et al: A randomized trial of exercise and quality of life in colorectal cancer survivors. Eur J Cancer Care (Engl) 12:347-57, 2003
193. Courneya KS, Friedenreich CM, Sela RA, et al: The group psychotherapy and home-based physical exercise (group-hope) trial in cancer survivors: physical fitness and quality of life outcomes. Psychooncology 12:357-74, 2003
194. Tyc VL, Rai SN, Lensing S, et al: Intervention to reduce intentions to use tobacco among pediatric cancer survivors. J Clin Oncol 21:1366-72, 2003
195. Wilson RW, Jacobsen PB, Fields KK: Pilot study of a home-based aerobic exercise program for sedentary cancer survivors treated with hematopoietic stem cell transplantation. Bone Marrow Transplant 35:721-7, 2005
196. Segal R, Evans W, Johnson D, et al: Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol 19:657-65, 2001
197. Mandelblatt J, Kanetsky PA: Effectiveness of interventions to enhance physician screening for breast cancer. J Fam Pract 40:162-71, 1995
198. Manne S, Fasanella N, Connors J, et al: Sun protection and skin surveillance practices among relatives of patients with malignant melanoma: prevalence and predictors. Prev Med 39:36-47, 2004
199. Rauscher GH, Hawley ST, Earp JA: Baseline predictors of initiation vs. maintenance of regular mammography use among rural women. Prev Med 40:822-30, 2005
200. Rimer BK: Improving the use of cancer screening for older women. Cancer 72:1084-7, 1993
201. Taylor V, Lessler D, Mertens K, et al: Colorectal cancer screening among African Americans: the importance of physician recommendation. J Natl Med Assoc 95:806-12, 2003
202. Jones LW, Courneya KS, Peddle C, et al: Oncologists’ opinions towards recommending exercise to patients with cancer: a Canadian national survey. Support Care Cancer 13:929-37, 2005
203. Ahuja R, Weibel SB, Leone FT: Lung cancer: the oncologist’s role in smoking cessa-tion. Semin Oncol 30:94-103, 2003
204. Kuhn KG, Boesen E, Ross L, et al: Evaluation and outcome of behavioural changes in the rehabilitation of cancer patients: a review. Eur J Cancer 41:216-24, 2005
205. Yarnall KS, Pollak KI, Ostbye T, et al: Primary care: is there enough time for prevention? Am J Public Health 93:635-41, 2003
206. Jones LW, Courneya KS, Fairey AS, et al: Effects of an oncologist’s recommendation to exercise on self-reported exercise behavior in newly diagnosed breast cancer survivors: a single-blind, randomized controlled trial. Ann Behav Med 28:105-13, 2004
207. Jones LW, Courneya KS, Fairey AS, et al: Does the theory of planned behavior mediate the effects of an oncologist’s recommendation to exercise in newly diagnosed breast cancer survivors? Results from a randomized controlled trial. Health Psychol 24:189-97, 2005
208. Courneya KS: Exercise in cancer survivors: an overview of research. Med Sci Sports Exerc 35:1846-52, 2003
209. Warburton DE, Nicol CW, Bredin SS: Prescribing exercise as preventive therapy. CMAJ 174:961-74, 2006
210. Warburton DE, Nicol CW, Bredin SS: Health benefits of physical activity: the evidence. CMAJ 174:801-9, 2006
211. Demark-Wahnefried W, Kenyon A, Eberle P, et al: Preventing sarcopenic obesity among breast cancer patients who receive adjuvant chemotherapy: results of a feasibility study. Clin Exerc Physiol 4:44-9, 2002
212. Loprinzi CL, Athmann LM, Kardinal CG, et al: Randomized trial of dietician counseling to try to prevent weight gain associated with breast cancer adjuvant chemotherapy. Oncol 53:228-32, 1996
Appendix D.3
The Passport for Care Improving the Lives of Childhood Cancer Survivors: Development of a Novel Internet Resource for Managing Long-Term Health Risks
David G. Poplack, MD,* Michael Fordis, MD,** Marc E. Horowitz, MD,* Wendy Landier, RN, MSN, CPNP, CPON,+ Melissa M. Hudson, MD,++ Smita Bhatia, MD,+ Kevin C. Oeffinger, MD,# Ann C. Mertens, PhD,## and Quentin W. Smith, MS**
1.
Introduction to the Passport for Care (PFC)
The Institute of Medicine,1 the President’s Cancer Panel,2 and the Centers for Disease Control and Prevention3 have emphasized the importance of periodic evaluation and screening of cancer survivors for late effects of treatment for their cancers. The Children’s Oncology Group (COG) recently released version 2 of a set of comprehensive, evidence-based, long-term follow-up guidelines for health care providers managing childhood cancer survivors.4 While recognizing that the length and depth of the COG guidelines are important in order to provide clinically relevant, evidence-based recommendations and supporting health education materials, clinician time limitations and the effort required to identify the specific recommendations relevant to individual patients using the current paper-based
format of the guidelines have been identified as barriers to their clinical application. This report discusses the development of an online decision support tool, the PFC, which allows health care providers and childhood cancer survivors to quickly and accurately generate individualized exposure-based screening recommendations and patient educational materials according to the COG Long-Term Follow-Up Guidelines via a web-based, user-friendly interface.
The PFC includes an interface and database for recording summaries of survivor treatment exposures; a “Guidelines Generator” employing a logic layer with decision rules that link treatment exposures to periodic evaluations and screening recommendations; and back-end guideline administration and maintenance tools. When completed, the PFC will also provide the survivor ready access to individualized healthcare resources, an online survivor forum, and regular health screening information. It is designed for secure use by the childhood cancer survivor who, if they choose, can share information contained within the PFC with their physicians and other health care providers.
This background paper describes the rationale, process, and status of efforts to create this dynamic resource for survivors of childhood cancer and their health care providers. The PFC is designed to be easily modified to accommodate new and emerging findings regarding risks associated with cancer treatment exposures, and it offers a means of alerting survivors and professionals involved in their care regarding these findings.
In the ensuing pages, we provide a brief review of the current state of the knowledge regarding late effects of treatment for childhood cancer and the strategies for managing risks for late effects. We also describe the multidisciplinary collaborative effort involved in the creation, testing, refinement, and deployment of the PFC. Lastly, we provide a description of the current status of the PFC, discuss barriers and challenges to its development and implementation, and review the implications of the PFC as a potential model resource for follow-up of survivors of adult cancer and possibly other chronic diseases.
2.
The Challenge Posed by Late Effects of Treatment for Childhood Cancer
2a. The Emergence of Cancer Survivorship as a National Priority. Within the last few years cancer survivorship has been recognized as a national public health priority by: (1) the Institute of Medicine (IOM) in their 2003 report Childhood Cancer Survivorship: Improving Care and Quality of Life;1,5 (2) the Centers for Disease Control and Prevention (CDC) in its recently released A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies;3 and (3) the President’s Cancer Panel
in its 2003-2004 Annual Report, Living Beyond Cancer: Finding a New Balance.2 Several themes emerged from the recommendations and strategies of all three documents: (1) There is a need to raise awareness among survivors themselves, family members, policy makers and the public about issues surrounding survivorship, including the long-term risk for late sequelae of cancer treatment; (2) survivors and providers need to be informed of the benefits of screening and periodic examinations as evidence and guidelines emerge regarding long-term follow-up; and (3) patient navigation systems and web-based tools need to be developed, tested, and maintained to facilitate optimum follow-up care of survivors.
2b. Challenges to Implementing Recommendations for Cancer Survivors. Cancer survivorship represents a prototypical serious chronic health problem. Recovery from cancer requires transitions from specialty care to primary care, with follow-up after treatment supported by evidenced-based guidelines for care.2 Systematic follow-up studies of late effects in survivors of adult malignancies have been limited and comprehensive guidelines remain largely unavailable. However, the experience with long-term follow-up of childhood cancer survivors has provided sufficient evidence to link therapeutic exposures with potential late effects to inform guideline development. The pediatric oncology experience may provide a model for exploration of how guidelines for adult cancer follow-up care and management of other chronic conditions may be deployed and implemented.
2c. The Experience with Childhood, Adolescent, and Young Adult Cancer Care. Since the 1970’s, the majority of children and adolescents with cancers have been treated in clinical trials sponsored by the National Cancer Institute. Professionals at institutions affiliated with the COG have, historically, treated over 90% of all children with cancer in the United States.6 The affiliated institutions in the United States, Canada, Europe, and Australia, numbering 232 organizations as of May 2006,7 offer innovative diagnostic and therapeutic interventions through 150 treatment protocols designed to improve clinical and functional outcomes for children and adolescents with cancer.8
The National Cancer Institute through its Surveillance Epidemiology and End Results (SEER) program has documented the success achieved in treatments of childhood, adolescent, and young adult cancer in recent years. Over the last quarter century, 5-year survival rates for the five age groupings used in tracking have increased as follows for childhood cancers of all sites: (1) ages 0-4: from 56.8% in 1974-1976 to 78.3% in 1995-2001; (2) ages 5-9: from 55.5% in 1974-1976 to 78.6% in 1995-2001; (3) ages 10-14: from 55.1% in 1974-1976 to 79.2% in 1995-2001; and (4) ages 15-19: from 63.8%% in 1974-1976 to 79.5% in 1995-2001.9
The population of childhood cancer survivors now numbers over 270,000.1 Several reports have extrapolated from SEER data reported by Jemal and colleagues in estimating that roughly 1 in 570 individuals between 20 and 34 years of age is a long-term survivor of childhood cancer.1,10-12 Whether or not improvements in survival continue at rates suggested by some researchers and epidemiologists, there are clear indicators of success in prolonging the lives of children with cancer through more effective treatment of the acute stages of disease. As a consequence, pediatric oncologists and others who have been involved in cancer care for children have recognized the obligation to examine the late sequelae of cancer and cancer treatment and to develop strategies to screen for and manage risks effectively.
2d. The Consequences of Treatment Success. The remarkable improvements in pediatric cancer survival rates have brought with them a new set of challenges for health care providers and for national, state, and local health care systems. Childhood cancer survivors commonly experience late effects of treatment.13-24 Two-thirds or more of childhood cancer survivors are likely to experience at least one late effect,13,16-20 and in 25-40% of long-term survivors, the late effects associated with treatment for cancer are likely to be severe or life threatening.11,13-15,17,25 Late effects encompass a myriad of detrimental physical conditions providing evidence for the need for follow-up screening and early intervention These effects range from multiorgan and systems dysfunction or failure;26-62 to subsequent malignancies.21,48,63-71 In addition, chronic or subclinical changes persisting after cancer treatment may result in premature onset of common conditions associated with aging (e.g., diabetes mellitus, cardiovascular disease, hypertension, hyperlipidemia)46-48,51,53,54,56-62,72 that place the long-term survivor at higher risk for chronic illness and premature death.
Treatment for childhood cancer can also affect normal growth, leading to reduced height73-78 and increased risk for obesity.79-82 The likelihood of growth problems associated with particular cancer treatments provides evidence for the need for regular screening in such patients and timely intervention to manage risks of abnormal stature and weight. Apart from physical manifestations of disease related to prior childhood cancer treatment, there is a large body of literature related to psychosocial effects of childhood cancer and its treatment on both survivors and family members.83-103 These effects may be related to: stress and the trauma inflicted by cancer and its treatment on children and their families;104-121 deficits in cognition and learning difficulties related to treatment;92,122-130 and/or factors involving body image and self-concept in children and young adults who perceive themselves as being different from their peers.97,131-135 The heightened risk for cognitive, behavioral, and interpersonal problems related to a prior
cancer and cancer treatment experience requires vigilance on the part of care providers so that timely assessment and appropriate treatment services can be arranged, should symptoms of such problems appear.
2e. Complexity in Risk Assessment and Management. The difficulties that many health care providers experience in trying to gauge the types and levels of health risks associated with prior childhood cancer treatment were summarized succinctly by Landier and colleagues:
… health care providers encountering childhood cancer survivors must be knowledgeable about potential cancer-related adverse effects in order to prescribe appropriate monitoring and to implement therapeutic interventions should health problems arise. Unfortunately, because of the relative rarity of childhood cancer, many health care providers lack familiarity with cancer-related health risks and risk-reduction methods relevant for this population. Moreover, the heterogeneous nature of pediatric malignancies, representing numerous histological subtypes with unique epidemiology, biology, and treatment regimens, further reduce the likelihood of primary care providers attaining proficiency in managing long-term childhood cancer survivors. At most, health care providers outside of academic centers may care for no more than a handful of survivors, usually each with different cancers, treatment exposures, and health risks, making delivery of appropriate care a daunting task. Consequently, primary care providers in the community setting are often unfamiliar with cancer-related health risks and uncomfortable with supervising the care of childhood cancer survivors.136pp.150-151
2f. Survivors’ Lack of Awareness of Health Risks and Effective Risk Management Strategies. Confounding the poor understanding of childhood cancer treatment-related health risks by many health professionals is the general lack of awareness of such risks by the survivors themselves. A limited number of studies have revealed significant knowledge deficits and misperceptions in survivors’ understanding of their cancer diagnosis, treatment, and cancer-related health risks.137-141 One study of adult survivors of childhood cancer diagnosed between 1945 and 1974 concluded that certain factors (e.g., younger age at treatment, nonwhite race, less intensive treatment, lower paternal education, diagnosis in the earlier years of the study) were associated with greater knowledge deficits among survivors.137 In more recent studies, survivors demonstrated greater general knowledge about their cancer histories and associated health risks, but exhibited limited knowledge of specific treatment details, a key factor in coordinating long-term risk-based health care.138,139,141 The knowledge deficits observed in two of these studies may be confounded by cultural and ethnic variations in attitudes regarding disclosure of the diagnosis of cancer, especially to
very young children.138,139 However, persistent knowledge deficits about cancer-related health risks in older survivors limit their participation in screening and risk-reducing interventions.140
Several studies indicate that survivors perceive themselves as more vulnerable to health problems than others not treated for cancer, requiring more attention by the provider in protecting his or her health.135,142-147 However, health concerns do not consistently motivate engagement in protective behavioral practices or abstinence from risky behaviors.143,147-149
Examination of data on health service utilization from a large cohort of childhood cancer survivors confirmed that many of those who had treatments associated with higher risks failed to obtain follow-up screening as recommened.150 Absence of recommended cancer-related medical visits within a 2-year period among survivors who should be screened based on known risks associated with specific treatments—including chest/mantle radiation therapy (RT), cumulative anthracycline dose ≥300 mg/m2, bleomycin, etoposide or ifosfamide—was documented for nearly half of survivors surveyed in most cases. For those treated with chest/mantle RT, 47.9% did not report a cancer-related follow-up visit; for those treated with a ≥300 mg/m2 cumulative anthracycline dose, the percentage not experiencing a cancer-related follow-up visit was 51.7%; for bleomycin treatment the percentage was 40.8%; and for high risk therapy, including any of the three just cited and/or treatment with etoposide or ifosfamide, the percentage was 50.7%.150 The study authors concluded that, for most study participants, the likelihood of a cancer-related follow-up visit or a physical examination decreased at an age when the risks for potentially modifiable late effects from cancer were on the rise.150
3.
Health System Factors Influencing the Delivery of Effective Follow-Up Services
3a. Systems-Based Barriers to Effective Follow-Up. Financial and health care systems barriers also influence follow-up care. One issue that has received considerable attention in the professional literature since the early 1990s relates to transition from pediatric to adult care.151-164 There are well documented problems in the transition to adult care for young people with special health needs, including those previously treated for cancer. These problems include lack of needed treatment services (i.e., no place to refer young people when adult services are needed); provider unwillingness to take on young people with special needs; lack of comparability to services that had been available in the pediatric system; and lack of working knowledge among adult providers in managing the special needs of patients with conditions related to prior childhood diseases.158,159,164
Regarding procedural barriers, a major problem involves the transfer
of accurate, complete, and appropriate information from the pediatric oncology treatment setting to the adult primary care or adult oncology treatment setting. Effective follow-up of treatment-related health risks is contingent on provision of a comprehensive medical summary to professionals who will be involved in care of the younger or older adult who has a history of treatment for childhood cancer.165 The transfer of treatment risk-related information to primary health care providers has been hampered by evolving cancer therapies and late effects profiles, as well as by the long latency period needed to evaluate many health outcomes and the generally unknown risks of aging on treatment sequelae.11
The transfer is further hampered by the lack of uniform and/or compatible information technology systems and electronic record distribution systems in U.S. health care. U.S. medical practices have been slow to adopt information technologies that are increasingly important in health care environments in which patients are likely to move geographically, change health care providers either by choice or due to other factors (e.g., changes in health care provider participation in specific third-party payer plans, loss of health insurance coverage due to job changes), or otherwise alter their health care seeking behaviors. Data suggest that, over a 12- to 24-month period, between 15% and 25% of privately insured persons change their health care provider due to changes in health plans.166,167 Such changes have the potential to disrupt the transfer of essential information (e.g., disease history, health risk data, and prior treatment exposures) to health care providers who require the information in order to assist the patient in making informed decisions about his or her care.
3b. Demands on Health Care Provider Time. Another systems-related issue that impacts delivery of effective follow-up services to survivors of childhood cancer relates to demands placed on health care providers’ time. Expectations for comprehensive health screening and delivery of preventive services by health care providers continue to grow. One recent study concluded that, in order for primary care providers to satisfy all the preventive health care recommendations of the U.S. Preventive Services Task Force, 7.4 hours per working day would be devoted to preventive services—exclusive of any time spent in actual problem-based care.168 Given the extra time required in order to assess childhood cancer treatment-related risks, particularly in the absence of technology support in many settings, the potential for inadequate risk identification and management is high.
4.
Childhood Cancer Survivors: A Model for Long-Term Follow-Up for Cancer Treatment
The survivors of childhood, adolescent, and young adult cancers repre-
sent a population that offers several important advantages for study of disease- and treatment-related factors that may increase risks for health problems later in life. Characteristics of this survivor group that lend themselves to modeling for health risk management include:
-
The population is well characterized with initial exposures to treatment modalities documented by protocol;1,4
-
Greater than 90% of children with cancer in the United States are treated within institutions that are members of the National Cancer Institute (NCI)-supported COG using therapeutic approaches that conform to COG-treatment protocols.6
-
The late effects of cancer therapy have been and continue to be systematically investigated as part of the Childhood Cancer Survivor Study (CCSS), involving 20,346 childhood cancer survivors diagnosed between 1970 and 1986 and treated at 26 cancer centers in the U.S. and Canada.169 Therefore, a large population of identifiable survivors is also readily available through the CCSS and long-term survivor clinics at select COG institutions for studies.169 This population offers opportunities to test the effectiveness of interventions that can then be applied to the broader population of childhood, adolescent, and young adult cancer survivors, and ultimately extended to the total population of cancer survivors.
-
Evidence-based guidelines for long-term follow-up have been developed by COG for survivors of childhood, adolescent, and young adult cancer.4
-
The development and deployment of the PFC, an Internet-based decision support tool for both survivors and their health care providers is well underway. As recently reported, the PFC, a functional decision support system that includes automated capabilities to generate individualized screening and follow-up guidelines and resources, is entering the first phase of pilot testing in early 2007.170 Progress toward development of the PFC is reviewed in the remainder of this chapter.
5.
The Passport for Care
5a. Purpose. The PFC is an Internet-based decision support system being developed for use by patients and providers to guide long-term follow-up screening for late effects resulting from exposures for treatment of childhood cancer. The purposes of the PFC are to serve as a communication tool to bridge the transition in care from cancer treatment to long-term survivorship; to engage survivors and health care providers in an extended care relationship; and to engage and empower survivors in assuming control and direction for interventions to ensure health.
5b. Description of PFC Features. PFC features include a portable care summary of treatment exposures; individualized guidelines for care; alerts for guideline changes; individualized resources for the survivor and for the health care provider; survivor networks or virtual communities established through online forums; and opportunities to participate in survivor-related research. The PFC is being designed to contain separate online portals for survivors and health care providers; however survivors and providers will each have access to information across both portals. The survivor portal will contain information in presentation and language suitable for lay audiences. The health care provider portal will provide elements for subspecialty audiences of oncologists and for primary care providers.
The survivor will have options regarding which specific PFC components to share with various health care providers in either electronic or print formats. Also, the PFC will incorporate an audit function that will permit the survivor to review authorized access to the PFC. This latter function will enable the survivor to monitor PFC use by different providers, thereby facilitating tracking of communication among and between providers (e.g., oncologists, primary care providers, behavioral health specialists, others). Although not accessible by the survivor, the PFC will also contain tools for the guidelines developers to use to update or modify guidelines as recommended by the COG, review guidelines for standardization and consistency, and adjust guideline outputs.
In the pediatric arena, it is envisioned that the PFC will be an essential tool in reengineering the approach to care by preparing patients and/or family members for long-term survivorship. As treatment is completed, the details of the PFC are to be shared with the survivor and/or family members in preparation for participation. The discussion may be accompanied by reference to and review of specific steps that the patient and/or family member can take in monitoring for potential late effects and in intervening early if needed.
Discussion of PFC participation may serve several purposes. It provides an opportunity to communicate that a long-term follow-up plan is in place for the survivor, and it may diminish the sense of abandonment that some cancer survivors, both adults and children, describe with completion of acute treatment and discharge from care.171,172 PFC-related discussion may foster empowerment of the patient and may encourage establishment of extended partnerships with health care providers for purposes of health risk monitoring and intervention. Access to trusted and reliable resources for patient education and information may be facilitated via the PFC, laying the foundation for survivor-directed information seeking. Establishing a sense of independence and responsibility is important in building an effective health maintenance system that can be modified and updated to accom-
modate emerging risk-related research findings, as well as changing life circumstances specific to each patient.1
5c. Overview of PFC Development, Structure and Elements. The staged development of the PFC involves an iterative process informed by qualitative and quantitative research that includes focus groups and stakeholder interviews, prototype development, usability evaluation, clinic testing, and results-based improvement using an approach modified from that described by Mooney and Bligh.173 Findings from qualitative data collection indicate that survivors want information that explains their previous treatments and risks for late effects; they want the ability to control their medical information; they want and need recommendations for their follow-up care and informational resources tailored to their specific cancer history; and they require summaries that can be shared with their personal health care providers in order to ensure that the provider is aware of risks associated with prior childhood cancer treatment. It is anticipated that research that will occur during the various stages of PFC development may identify additional needs of survivors and providers that the PFC can be modified to address.
5d. The PFC: A Multi-Disciplinary Collaboration. Led by faculty at the Texas Children’s Cancer Center (TCCC) and the Center for Collaborative and Interactive Technologies at Baylor College of Medicine, the PFC has been developed in collaboration with representatives from the COG and the CCSS. The participants in the Working Group are noted in Table D.3-1. Input has also been obtained from members of a national steering committee and other stakeholders, including advocacy groups with particular interests in cancer survivorship and long-term follow-up care.
5e. The Health Care Provider Portal. The initial stage of PFC development has focused on creation of the “health care provider portal.” A description of this portal is provided below.
As shown in Figure D.3-1, the health care provider portal has the following components:
-
A summary of care including demographic data, diagnoses, and history of treatment exposures for each survivor;
-
The COG Long-term Follow-up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers stored in a database;
-
The decision rules linking treatment exposures to potential late effects and recommendations for screening and other resources;
-
Web-based and print outputs providing individualized information regarding potential late effects, risk factors, and associated screening rec-
TABLE D.3-1 PFC Working Group Members and Organizational Affiliations (presented alphabetically by surname)
|
Smita Bhatia, MD City of Hope National Medical Center, Duarte, CA Chair, COG Late Effects Committee |
Wendy Landier, RN, CPNP City of Hope National Medical Center, Duarte, CA Member, COG Nursing and Late Effects Committees |
|
Sarah Bottomley, RN, MN, CPNP Texas Children’s Cancer Center, Houston, TX |
Ann Mertens, PhD University of Minnesota, Minneapolis, MN Investigator, Childhood Cancer Survivor Study |
|
Michael Fordis, MD Center for Collaborative and Interactive Technologies Baylor College of Medicine, Houston, TX |
Kevin Oeffinger, MD Memorial Sloan-Kettering, New York, NY Member, COG Late Effects Committee |
|
Marc Horowitz, MD Texas Children’s Cancer Center Baylor College of Medicine, Houston, TX |
David Poplack, MD Texas Children’s Cancer Center Baylor College of Medicine, Houston, TX |
|
Melissa Hudson, MD St. Jude’s Children’s Research Hospital, Memphis, TN Member, COG Late Effects Committee |
|
-
ommendations (Figures D.3-2, D.3-3, and D.3-4; guidance for screening for other malignancies (Figure D.3-5); tailored survivor and health care provider education and information resources (Figure D.3-6); and evidence-based scoring of recommendations and references (Figure D.3-7); and
-
Guideline editing and reviewing tools for use by guideline developers. The latter tool set has been used to assist with standardization of the latest version of the COG Long-Term Follow-up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers (Version 2.0—March 2006).4 The PFC health care provider portal will serve as an electronic repository for the COG Long-Term Follow-Up Guidelines and as a tool to foster standardization of clinical services at the point of care.
5f. Internet-Based Deployment. Because of the distributed nature of anticipated users of the PFC, an Internet-based system was deemed most appropriate. An Internet-based approach offers the advantages of easy accessibility, interoperability, and public availability.
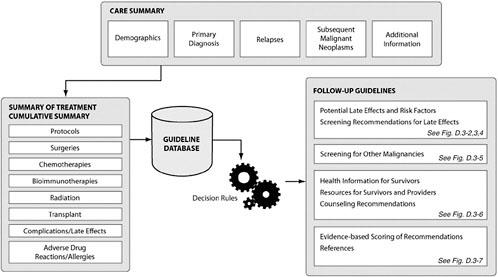
FIGURE D.3-1 The functional components of the PFC include a care summary containing demographics, primary diagnosis, relapses, subsequent malignant neoplasms, and additional information. These data are used to compile a cumulative summary of treatment. Screening recommendations and individualized resources are generated from the cumulative summary of treatment and the guideline database using a set of decision rules.
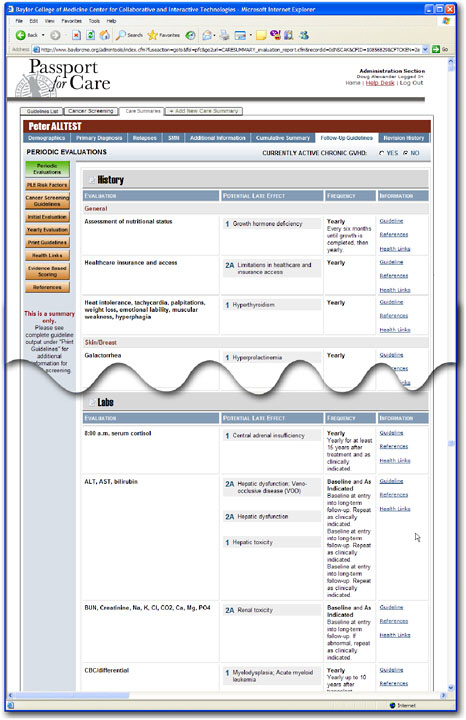
FIGURE D.3-2 Periodic history, physical, diagnostic imaging, laboratory and other evaluations are displayed with the type of evaluation that should be performed, the potential late effect that is being evaluated, the frequency of recommended evaluations and links to important additional information such as the COG Healthlink (see Figure D.3-6), pertinent references and the full guideline (see Figure D.3-7).
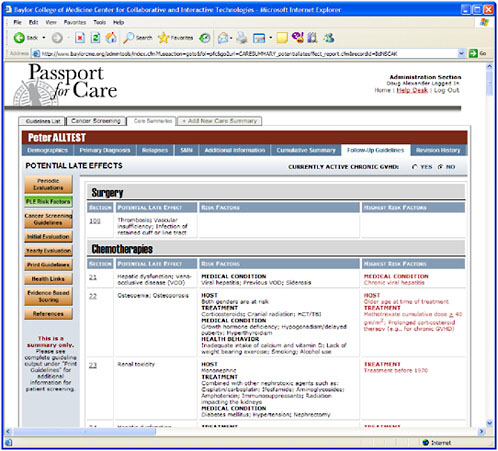
FIGURE D.3-3 This view of the guidelines allows the health care provider to view the risk factors for each of the potential late effect that the survivor is susceptible to.
5g. COG LTFU Guidelines. Comprehensive Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers have been developed by COG’s Nursing Discipline and Late Effects Committee.4,174 COG members have enthusiastically endorsed broader dissemination and use of the guidelines in helping childhood cancer survivors and other health professionals who provide care to survivors to recognize and manage health risks related to late effects of treatment. In the most recent version of the guidelines released to the public (version 2.0 issued in March 2006), potential late effects, risk factors, highest risk factors, recommended periodic evaluation and frequency, health protective counseling recommendations, considerations for further testing and interventions, and references are presented in tabular format corresponding to specific therapeutic agents.4
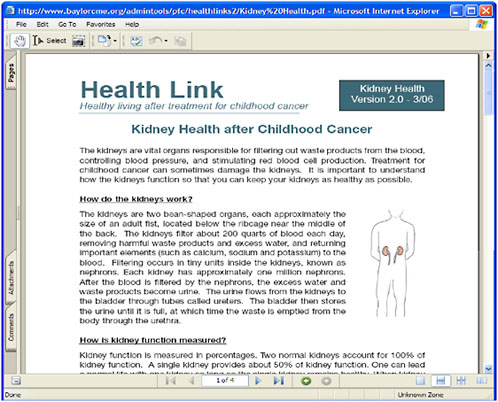
FIGURE D.3-6 The COG Healthlink information for survivors can be easily accessed by an online link to the COG website from the evaluations page (Figure D.3-2).
A summary of screening recommendations for common adult-onset cancers developing as subsequent malignancies in this population, directions regarding how to use the guidelines, a listing of references to relevant scientific literature, and a detailed topical index are included. An explanation of the levels of evidence related to each identified risk for a late effect is also presented. The scores assigned, according to a modified version of the National Comprehensive Cancer Network “Categories of Consensus,”175 relate to the strength of association of the identified late effect with the specific therapeutic exposure based on current literature.4 Each score is coupled with a recommendation for periodic health screening based on the collective clinical experience of the panel of experts who developed the guidelines. These scores enable users to judge the strength of the evidence associated with each late-effect risk and the recommendations accompanying it.
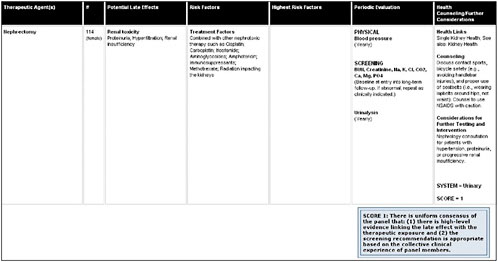
FIGURE D.3-7 The full guideline can be accessed by a link from the evaluations page (Figure D.3-2). The score of the strength of the evidence linking the potential late effect to the therapeutic exposure is presented.
However, because of the length of the guidelines and the detail contained in them, clinical utility of the paper-based version of the guidelines on a day-to-day basis in a busy clinical practice is limited. It is precisely for this reason that the PFC, with its ability to generate individualized follow-up recommendations, is anticipated to be attractive to the practicing clinician.
5h. Challenges in PFC Development and Its Adoption. PFC development has required addressing a number of challenges. A brief review of the barriers confronting PFC developers may prove informative for the broader initiatives addressing the needs of all 10 million adult cancer survivors in the United States.
(1) Impacts of Guideline Publication on Provider Behavior. Studies dating back nearly two decades have documented problems related to guideline adherence across different types of adult and childhood practice settings and disease states.176-181 Feifer and colleagues summarized barriers to effective guideline implementation at the healthcare provider level (i.e., not knowing that guidelines exist, not being familiar with and/or agreeing with content, lacking time to apply guidelines in the clinical setting); the patient level (i.e., inconsistency with health beliefs, time and financial constraints, lack of trust in the guidelines); and systems level (i.e., not having the right information in the right place at the right time, resource constraints, patient volume).181 Despite the literature suggesting poor adherence to clinical guidelines in many practice settings, there is growing recognition of the attributes of clinical guidelines that improve the likelihood of their application in clinical settings. Studies have indicated that factors that enhance the likelihood of adherence to clinical guidelines include: engaging patients as partners;182-185 using point-of-care reminders;186-189 and employing population-based management techniques.190-194 For these reasons the PFC was designed to include components that address the needs of both the survivors and their providers in a health care partnership providing resources tailored to survivor or provider needs and offering point-of-care or near point-of-care decision support individualized to the needs of the specific survivor.
(2) Guideline Development. The process of development of the comprehensive Long-term Follow-up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers has been well described and will not be reviewed here.174 However, mention must be made of the public investment from the National Cancer Institute (NCI) in the CCSS that, along with other efforts, has proven essential for identifying and link-
ing therapeutic exposures to late effects. The NCI has also supported development of the COG Long-Term Follow-Up Guidelines under the U10 CA098543 grant. Similar initiatives are needed across the spectrum of adult cancers to accelerate development of an evidence base that can provide the foundation for guideline development. In this regard it is worth noting the approach that COG has taken in guideline development.
Even in the arena of pediatric cancer treatment and follow-up, a complete evidence base for development of screening guidelines is lacking. Therefore, COG experts made use of the literature linking late effects to treatment exposures and combined the available evidence with expert consensus. In doing so, COG guideline developers recognized that there are no randomized clinical trials available on which to base recommendations for periodic screening evaluations of childhood cancer survivors.4 As a consequence, professionals involved in guideline development examined “… the strength of data from the literature linking a specific late effect with a therapeutic exposure, coupled with an assessment of the appropriateness of the screening recommendation based on the expert panel’s collective clinical experience.”4,p. 4 Each guideline was then scored using a modified version of the National Comprehensive Cancer Network “Categories of Consensus” to communicate the levels of evidence and consensus to users.175
(3) Care Summary Development. Although modifications and refinements continue to be made, an end-of-treatment summary or care summary that permits data collection that can be used for clinical and research purposes has been developed by COG committees. While it is attractive to collect more data rather than less, caution should be exercised in this regard. For example, in the case of the PFC, generation of individualized guidelines requires only a limited subset of the information contained in the complete COG Care Summary dataset. Collection and archiving of the complete dataset could require commitment of time and money that, for some clinicians, may discourage participation and use. We are exploring approaches for streamlining data collection strategies in a manner that allows for use of the more limited dataset for the PFC, however, permits collection of the larger dataset (if preferred by the provider) and expansion of data collection as evidence evolves.
(4) Accommodating Change. Accommodating change in a project such as the PFC can, in itself, pose a barrier to effective implementation. Change can occur at many levels (e.g., survivor’s treatment history, providers’ roles in working with the survivor in long-term follow-up
care, the guidelines knowledge base and emergence of new findings with regard to risks and the recommendations for follow-up evaluation). While the COG Care Summary incorporated into the PFC is not designed to be a complete medical record, a careful effort was undertaken to permit capturing changes in treatment exposures that could influence follow-up guideline recommendations. In particular, the Care Summary accommodates treatments for relapses and subsequent malignancies. Relapses and subsequent malignancies that occur during care or follow-up at a COG institution could presumably be entered into the PFC database using personnel and approaches similar to those used in creating the initial Care Summary.
Should relapses or subsequent malignancies occur in adulthood under the care of an adult oncologist, staff less familiar with the PFC would need to become involved in updating the history of treatment exposures in the PFC. Training and support mechanisms, necessary to prepare health care providers and other clinical staff who will be involved in such activities, will be incorporated into the patient portal of the PFC under development. Contemplation of such developments invites consideration of whether guideline recommendations will need to accommodate the later exposures to treatments. With respect to changes in provider roles, the patient portal of the PFC is being designed to allow for capture of information on changes in healthcare providers and contact information on former and current providers, thereby facilitating timely contact with current providers, as well as providers involved earlier in care.
As data emerge regarding indications and recommendations for follow-up, the guidelines for long-term follow-up for potential late effects are anticipated to change. With paper-based or token-based (e.g., a smart card) systems, the recommendations accompanying the treatment history may become dated, if not obsolete, presenting a significant barrier to use. In contrast, an Internet-based deployment for the PFC offers the advantages that guidelines can be conveniently modified in one location with changes populating any recommendations subsequently produced. This is accomplished using administrative tools created and deployed for use by guideline developers and maintainers.
(5) Standardization and Interoperability. Use of proprietary software and systems can produce significant barriers to data sharing and interoperability. For example, one can envision: (1) the possible requirement to aggregate or exchange data with other electronic systems, including electronic medical records (EMRs), insurance or payer databases, or other clinical decision support systems; or (2) the need to develop reports or analyses based on any number of parameters (e.g.,
diagnoses, treatment exposures, procedures). As noted in recent reviews of clinical support systems, such tasks can be greatly facilitated by use of coded data, standard vocabularies, and messaging standards (e.g., Health Level Seven [HL7]).195,196 More broadly, support is coalescing around a new vision for nationwide health information using a decentralized “network of networks” facilitated by consensus regarding shared policies and common technical standards. Connecting for Health Common Framework: Resources for Implementing Private and Secure Health Information Exchange is an initiative underwritten by the Markle Foundation that involves a wide range of stakeholders with interests in health and health care information.197 Monitoring of this initiative, which has advanced from the conceptual to the demonstration phase, will provide guidance in ensuring that the end result of efforts like the PFC are accessible to a wide range of audiences using varying hardware and software configurations to access summary data and other components of programs designed to foster effective long-term follow-up of care services.
(6) Integrating into Clinical Workflows. Technology, no matter how compelling, will remain unused if it does not serve the needs of the clinician or clinical staff, and if it does not integrate seamlessly into workflows of clinical service settings. For this reason, it is critical that stakeholders are involved in developmental efforts, providing input and feedback throughout the processes of prototype creation and iterative testing and improvement. Early stakeholder involvement ensures that the selection of technologies and applications meets provider needs and can be used within extant clinical environments. Stakeholder involvement must engage the full range of individuals who will be involved in application use and maintenance (e.g., individuals entering clinical data into the Care Summary, nurses and health care providers using the recommendations, guideline developers, and patients). Training and support procedures are also essential components of a deployment plan to ensure that integration into the clinic workflow can proceed smoothly.
(7) Protecting Patient Confidentiality and Privacy. Protecting the privacy of survivors and ensuring confidentiality is a paramount concern in designing any software application involving identifiable health information. Protection of privacy and confidentiality is also a legal requirement under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).198 Providing reliable and effective security for digital information requires a multimodal strategy involving access authorizations (e.g., passwords, user IDs, user tokens) and attribution
(e.g., audit logs), as well as application and data, transmission, network, and physical (i.e., hardware) security using various tools and strategies (e.g., data encryption, firewalls, virtual private networks [VPNs], locked rooms with key card or biometric access). Included in the technical specifications for the PFC is explicit information on strategies for ensuring that the program is secure and that the resulting program complies with federal mandates, including HIPAA requirements. In this regard, it is worth noting that the PFC has been designed with security: (1) at the browser level, involving digitally secured certificate access via a secure hypertext transfer protocol (HTTPS) connection and an encrypted identifier for each user; (2) at the application level through user authentication, log-in with user ID and password protection, verification through the database, assignment to a clinic and record set, and creation of an audit trail providing a log of who viewed specific data and when it was viewed; and (3) at the database level via encrypted storage files that are keyed at multiple levels within the encrypted application page. Deployment will also include additional network and physical security of the type described above. In addition to conforming to HIPAA requirements, further security will be assured through review and compliance with the requirements of the Baylor College of Medicine IT security and requirements of the Institutional Review Board (IRB). IRB approval will be secured prior to any personal information being gathered for storage and use via the PFC database. Informed consent will be required in order for survivors to participate in testing or later use of the PFC.
(8) Development and Maintenance Costs. While public funding is available for research and evaluation of extant tools, limited funding is available for the development of novel technological applications. Investigators interested in advancing the creation of new tools for managing chronic disease may find themselves seeking funding from private sources, including foundations, private individuals, and their own institutions. Even greater challenges may be faced by developers who, for legitimate scientific reasons, must focus initially on smaller audiences or specific subsets of larger patient populations, such as childhood cancer survivors. Public funding agencies interested in encouraging development of innovative decision-support tools for chronic disease, should consider reevaluating current requests for applications (RFAs) to accommodate the needs of pilot projects focusing on well-defined populations as long as sufficient data can be gathered to demonstrate the value of the particular innovative approaches.
(9) Other Challenges. There are other challenges to be met in designing and implementing projects like the PFC. Collaboration across disciplines is essential, and as experience with the PFC has demonstrated, engagement of clinical experts with informatics specialists at the earliest phases of guideline development can greatly accelerate the critical transition from print to electronic formats. Also, involvement of other experts in areas such as health communications, patient adherence, quality improvement, social psychology, health literacy, patient privacy and confidentiality, ethics, security, and interoperability standards may prove valuable in application development and in achievement of a successful outcome. Furthermore, resources, including funding, should be available to explore experimentally the efficacy and practicality of approaches for health care provider and patient behavioral change, including evolving continuing medical education and patient education approaches that may prove critical in improving professional and patient compliance and changes in health outcomes.
Finally, perhaps the most significant challenge to development of any tool like the PFC for any population of survivors is the assurance that the patient and guideline information will be updated and maintained in the future. Ensuring that the PFC or similar initiatives will be available to survivors throughout their lifetimes requires new models ensuring extended support. Consideration of models and strategies to provide for the longevity of the PFC are items under active discussion and exploration.
5i. PFC Testing and Roll-out. A fully operational version of the PFC is undergoing initial testing in preparation for early deployment and evaluation in the TCCC survivor clinic. Initial pilot testing will allow for assessment of the effectiveness of the automated guideline generator to determine if decision algorithms have been properly formulated and programmed, if data components are properly linked to respond effectively to risk-related queries, and if the responses to queries yield the correct information with regard to risk-based follow-up. Testing results will be used to modify and refine the PFC in preparation for subsequent testing in three additional COG clinics.
Once pilot testing has been completed, and the PFC has been revised and/or refined to ensure that it operates effectively it will be made available, in a staged manner to COG-affiliated institutions for initial field implementation. At this point, one portal will be operational—a portal for oncology health care providers for use in COG oncology clinics. Simultaneously, a second PFC portal, for survivors and primary care providers, will be developed and undergo testing and evaluation.
5j. Survivors of Adult Cancer and the PFC. It is attractive to consider applying a PFC-like approach to the care of adult survivors of cancer, however, it is important to recognize that follow-up of patients treated for cancer as adults poses unique challenges that differ from those encountered in the population of childhood cancer survivors.
Adult cancer patients are typically treated in the offices of private oncologists, rather than in academic medical centers, as are the majority of children with cancer. Furthermore, adult cancer care may reflect a greater diversity of approaches, with many patients not treated on standardized protocols. Follow-up studies of adult cancer survivors and the evidence base linking treatment exposures to potential late effects are limited. Comprehensive follow-up guidelines for survivors of most adult cancers have not been developed, and consensus regarding the development and use of an end-of-treatment summary is still evolving. It is important to note that the PFC is widely adaptable and may have far-ranging applications, including to the adult cancer survivor population, once comprehensive consensus-based guidelines for various adult cancers have been developed.
CONCLUSION
The substantial successes achieved in the treatment of childhood cancers over recent decades and the increased longevity of such patients has been accompanied by the additional need to address the late sequelae associated with cancer therapy. The Passport for Care (PFC) is a dynamic resource designed to provide survivor and provider education, resources, decision support, and health care recommendations tailored to the individual needs of the long term survivor of childhood cancer. Although the PFC targets a comparatively small population, the approach or elements of the approach is likely to be informative and/or serve as a model for applications designed to address the needs of the 10 million adult cancer survivors in the United States.
Successful development and deployment of such applications are anticipated to face a variety of challenges, including those relevant to scientific, clinical, health systems, logistical, interoperability, provider and patient adherence, security, guideline updating, long-term maintenance, and financial support issues. Strategies are available to address or begin to address a number of the potential barriers; however, significant hurdles do remain in the initial stages with respect to the provision of support to develop such model health care information tools and systems.
Finally, if such models prove successful and cost-effective in improving health outcomes, public health policy makers in partnership with other public and private stakeholders will need to develop policies and systems that can
accommodate the long-term needs for maintaining decision support tools demonstrated to improve the lives of patients with chronic disease.
REFERENCES CITED
1. National Cancer Policy Board (U.S.), Weiner SL, Simone JV, Hewitt ME. Childhood Cancer Survivorship: Improving Care and Quality Of Life. Washington, D.C.: The National Academies Press; 2003.
2. Reuben S. Living beyond cancer: finding a new balance. Bethesda, MD.: U.S. Dept. of Health and Human Services, National Institutes of Health, National Cancer Institute; 2004.
3. Centers for Disease Control and Prevention. A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies. Atlanta, GA: The Centers for Disease Control and Prevention and The Lance Armstrong Foundation; April 2004.
4. CureSearch: Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers, v 2.0. March 2006; 227. Available at: http://www.survivorshipguidelines.org/pdf/LTFUGuidelines.pdf. Accessed June 13, 2006.
5. National Cancer Policy Board (U.S.), Weiner SL, Simone JV. Childhood cancer survivorship: improving care and quality of life. Washington, D.C.: The National Academies Press; 2003.
6. American Cancer Society. Detailed guide: cancer in children. How are childhood cancers treated? Cancer reference information [January 4, 2005; http://www.cancer.org/docroot/CRI/content/CRI_2_4_4X_How_Are_Childhood_Cancers_Treated_7.asp. Accessed April 18, 2006.
7. Children’s Oncology Group. Resource Directory: COG Institutions by Country http://www.curesearch.org/resources/cog.aspx. Accessed May 30, 2006.
8. National Cancer Institute. Care for children and adolescents with cancer: Questions and Cancers National Cancer Institute FactSheet [November 10, 2005; http://www.cancer.gov/PDF/FactSheet/fs1_21.pdf. Accessed April 17, 2006.
9. Ries L, Eisner M, Kosary C, et al. SEER Cancer Statistics Review, 1975-2002. SEER Cancer Statistics Review [2005; http://seer.cancer.gov/cgi-bin/csr/1975_2002/search.pl#results. Accessed April 8, 2006.
10. Jemal A, Murray T, Ward E, et al. Cancer statistics, 2005. CA Cancer J Clin. Jan-Feb 2005;55(1):10-30.
11. Hudson MM. A model for care across the cancer continuum. Cancer. Dec 1 2005; 104(11 Suppl):2638-2642.
12. Bhatia S, Meadows AT. Long-term follow-up of childhood cancer survivors: future directions for clinical care and research. Pediatr Blood Cancer. Feb 2006;46(2):143-148.
13. Garre ML, Gandus S, Cesana B, et al. Health status of long-term survivors after cancer in childhood. Results of an uniinstitutional study in Italy. Am J Pediatr Hematol Oncol. May 1994;16(2):143-152.
14. von der Weid N, Beck D, Calfisch U, Feldges A, Wyss M, Wagner H. Standardized assessment of late effects in long-term survivors of childhood cancer in Switzerland. Results of a Swiss Pediatric Oncology Group study. Int J Pediatr Hematol Oncol. 1996;3:483-490.
15. Stevens MC, Mahler H, Parkes S. The health status of adult survivors of cancer in childhood. Eur J Cancer. Apr 1998;34(5):694-698.
16. Crom DB, Chathaway DK, Tolley EA, Mulhern RK, Hudson MM. Health status and health-related quality of life in long-term adult survivors of pediatric solid tumors. Int J Cancer Suppl. 1999;12:25-31.
17. Oeffinger KC, Eshelman DA, Tomlinson GE, Buchanan GR, Foster BM. Grading of late effects in young adult survivors of childhood cancer followed in an ambulatory adult setting. Cancer. Apr 1 2000;88(7):1687-1695.
18. von der Weid N, Swiss Pediatric Oncology Group. Late effects in long-term survivors of ALL in childhood: Experiences from the SPOG late effects study. Swiss Med Wkly. April 2001;131(13-14):180-187.
19. Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA. Sep 24 2003;290(12):1583-1592.
20. Bhatia S. Cancer survivorship—pediatric issues. Hematology (Am Soc Hematol Educ Program). 2005;Prepublication release:507-515.
21. Bassal M, Mertens AC, Taylor L, et al. Risk of selected subsequent carcinomas in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. Jan 20 2006;24(3):476-483.
22. Friedman DL, Freyer DR, Levitt GA. Models of care for survivors of childhood cancer. Pediatr Blood Cancer. Feb 2006;46(2):159-168.
23. Bottomley SJ, Kassner E. Late effects of childhood cancer therapy. J Pediatr Nurs. Apr 2003;18(2):126-133.
24. Pogany L, Barr R, Shaw A, Speechley K, Barrera M, Maunsell E. Health status in survivors of cancer in childhood and adolescence. Qual Life Res. 2006;15:143-157.
25. Lackner H, Benesch M, Schagerl S, Kerbl R, Schwinger W, Urban C. Prospective evaluation of late effects after childhood cancer therapy with a follow-up over 9 years. Eur J Pediatr. Oct 2000;159(10):750-758.
26. Shalet SM, Rosenstock JD, Beardwell CG, Pearson D, Jones PH. Thyroid dysfunction following external irradiation to the neck for Hodgkin’s disease in childhood. Clin Radiol. Sep 1977;28(5):511-515.
27. Green DM, Brecher ML, Yakar D, et al. Thyroid function in pediatric patients after neck irradiation for Hodgkin disease. Med Pediatr Oncol. 1980;8(2):127-136.
28. Kaplan MM, Garnick MB, Gelber R, et al. Risk factors for thyroid abnormalities after neck irradiation for childhood cancer. Am J Med. Feb 1983;74(2):272-280.
29. Constine LS, Donaldson SS, McDougall IR, Cox RS, Link MP, Kaplan HS. Thyroid dysfunction after radiotherapy in children with Hodgkin’s disease. Cancer. Feb 15 1984;53(4):878-883.
30. Devney RB, Sklar CA, Nesbit ME, Jr., et al. Serial thyroid function measurements in children with Hodgkin disease. J Pediatr. Aug 1984;105(2):223-227.
31. Fleming ID, Black TL, Thompson EI, Pratt C, Rao B, Hustu O. Thyroid dysfunction and neoplasia in children receiving neck irradiation for cancer. Cancer. Mar 15 1985; 55(6):1190-1194.
32. Oberfield SE, Allen JC, Pollack J, New MI, Levine LS. Long-term endocrine sequelae after treatment of medulloblastoma: prospective study of growth and thyroid function. J Pediatr. Feb 1986;108(2):219-223.
33. Katsanis E, Shapiro RS, Robison LL, et al. Thyroid dysfunction following bone marrow transplantation: long-term follow-up of 80 pediatric patients. Bone Marrow Transplant. May 1990;5(5):335-340.
34. Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP. Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med. Mar 21 1991;324(12):808-815.
35. Ogilvy-Stuart AL, Shalet SM, Gattamaneni HR. Thyroid function after treatment of brain tumors in children. J Pediatr. Nov 1991;119(5):733-737.
36. Sanders JE. Endocrine problems in children after bone marrow transplant for hematologic malignancies. The Long-term Follow-up Team. Bone Marrow Transplant. 1991;8 Suppl 1:2-4.
37. DeGroot LJ. Effects of irradiation on the thyroid gland. Endocrinol Metab Clin North Am. Sep 1993;22(3):607-615.
38. Hancock SL, Donaldson SS, Hoppe RT. Cardiac disease following treatment of Hodgkin’s disease in children and adolescents. J Clin Oncol. Jul 1993;11(7):1208-1215.
39. Ali MK, Ewer MS, Gibbs HR, Swafford J, Graff KL. Late doxorubicin-associated cardiotoxicity in children. The possible role of intercurrent viral infection. Cancer. Jul 1 1994;74(1):182-188.
40. Boulad F, Bromley M, Black P, et al. Thyroid dysfunction following bone marrow transplantation using hyperfractionated radiation. Bone Marrow Transplant. Jan 1995; 15(1):71-76.
41. Lipshultz SE, Lipsitz SR, Mone SM, et al. Female sex and drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Engl J Med. Jun 29 1995;332(26):1738-1743.
42. Fein DA, Hanlon AL, Corn BW, Curran WJ, Jr., Coia LR. The influence of lymphangiography on the development of hypothyroidism in patients irradiated for Hodgkin’s disease. Int J Radiat Oncol Biol Phys. Aug 1 1996;36(1):13-18.
43. Chin D, Sklar C, Donahue B, et al. Thyroid dysfunction as a late effect in survivors of pediatric medulloblastoma/primitive neuroectodermal tumors: a comparison of hyperfractionated versus conventional radiotherapy. Cancer. Aug 15 1997;80(4):798-804.
44. Novakovic B, Fears TR, Horowitz ME, Tucker MA, Wexler LH. Late effects of therapy in survivors of Ewing’s sarcoma family tumors. J Pediatr Hematol Oncol. May-Jun 1997;19(3):220-225.
45. Sorensen K, Levitt G, Bull C, Chessells J, Sullivan I. Anthracycline dose in childhood acute lymphoblastic leukemia: issues of early survival versus late cardiotoxicity. J Clin Oncol. Jan 1997;15(1):61-68.
46. Hudson MM, Poquette CA, Lee J, et al. Increased mortality after successful treatment for Hodgkin’s disease. J Clin Oncol. Nov 1998;16(11):3592-3600.
47. Nysom K, Holm K, Lipsitz SR, et al. Relationship between cumulative anthracycline dose and late cardiotoxicity in childhood acute lymphoblastic leukemia. J Clin Oncol. Feb 1998;16(2):545-550.
48. Green DM, Hyland A, Chung CS, Zevon MA, Hall BC. Cancer and cardiac mortality among 15-year survivors of cancer diagnosed during childhood or adolescence. J Clin Oncol. Oct 1999;17(10):3207-3215.
49. Sklar C, Whitton J, Mertens A, et al. Abnormalities of the thyroid in survivors of Hodgkin’s disease: data from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab. Sep 2000;85(9):3227-3232.
50. Sklar CA, LaQuaglia MP. The long-term complications of chemotherapy in childhood genitourinary tumors. Urol Clin North Am. Aug 2000;27(3):563-568, x.
51. Green DM, Grigoriev YA, Nan B, et al. Congestive heart failure after treatment for Wilms’ tumor: a report from the National Wilms’ Tumor Study group. J Clin Oncol. Apr 1 2001;19(7):1926-1934.
52. Kadan-Lottick N, Marshall JA, Baron AE, Krebs NF, Hambidge KM, Albano E. Normal bone mineral density after treatment for childhood acute lymphoblastic leukemia diagnosed between 1991 and 1998. J Pediatr. Jun 2001;138(6):898-904.
53. Kremer LC, van Dalen EC, Offringa M, Ottenkamp J, Voute PA. Anthracycline-induced clinical heart failure in a cohort of 607 children: long-term follow-up study. J Clin Oncol. Jan 1 2001;19(1):191-196.
54. Oeffinger KC, Buchanan GR, Eshelman DA, et al. Cardiovascular risk factors in young adult survivors of childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol. Oct 2001;23(7):424-430.
55. Sklar C, Boulad F, Small T, Kernan N. Endocrine complications of pediatric stem cell transplantation. Front Biosci. Aug 1 2001;6:G17-22.
56. Keefe DL. Anthracycline-induced cardiomyopathy. Semin Oncol. Aug 2001;28(4 Suppl 12):2-7.
57. Lipshultz SE, Lipsitz SR, Sallan SE, et al. Long-term enalapril therapy for left ventricular dysfunction in doxorubicin-treated survivors of childhood cancer. J Clin Oncol. Dec 1 2002;20(23):4517-4522.
58. Mertens AC, Yasui Y, Liu Y, et al. Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer. Dec 1 2002;95(11):2431-2441.
59. Adams MJ, Hardenbergh PH, Constine LS, Lipshultz SE. Radiation-associated cardiovascular disease. Crit Rev Oncol Hematol. Jan 2003;45(1):55-75.
60. Gurney JG, Kadan-Lottick NS, Packer RJ, et al. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer. Feb 1 2003;97(3):663-673.
61. Athanassiadou F, Kourti M, Papageorgiou T, Stamou M, Makedou A, Boufidou A. Severe hyperlipidemia in a child with acute lymphoblastic leukemia treated with L-asparaginase and prednisone. Pediatr Int. Dec 2004;46(6):743-744.
62. Huettemann E, Junker T, Chatzinikolaou KP, et al. The influence of anthracycline therapy on cardiac function during anesthesia. Anesth Analg. Apr 2004;98(4):941-947.
63. Metayer C, Lynch CF, Clarke EA, et al. Second cancers among long-term survivors of Hodgkin’s disease diagnosed in childhood and adolescence. J Clin Oncol. Jun 2000; 18(12):2435-2443.
64. Swerdlow AJ, Barber JA, Hudson GV, et al. Risk of second malignancy after Hodgkin’s disease in a collaborative British cohort: the relation to age at treatment. J Clin Oncol. Feb 2000;18(3):498-509.
65. Feig SA. Second malignant neoplasms after successful treatment of childhood cancers. Blood Cells Mol Dis. May-Jun 2001;27(3):662-666.
66. Neglia JP, Friedman DL, Yasui Y, et al. Second malignant neoplasms in five-year survivors of childhood cancer: childhood cancer survivor study. J Natl Cancer Inst. Apr 18 2001;93(8):618-629.
67. Bhatia S, Yasui Y, Robison LL, et al. High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin’s disease: report from the Late Effects Study Group. J Clin Oncol. Dec 1 2003;21(23):4386-4394.
68. Barnard DR, Woods WG. Treatment-related myelodysplastic syndrome/acute myeloid leukemia in survivors of childhood cancer—an update. Leuk Lymphoma. May 2005; 46(5):651-663.
69. Travis LB, Hill DA, Dores GM, et al. Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA. Jul 23 2003;290(4): 465-475.
70. Kenney LB, Yasui Y, Inskip PD, et al. Breast cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Intern Med. Oct 19 2004;141(8): 590-597.
71. Lew SM, Morgan JN, Psaty E, Lefton DR, Allen JC, Abbott R. Cumulative incidence of radiation-induced cavernomas in long-term survivors of medulloblastoma. J Neurosurg. Feb 2006;104(2 Suppl):103-107.
72. Kourti M, Tragiannidis A, Makedou A, Papageorgiou T, Rousso I, Athanassiadou F. Metabolic syndrome in children and adolescents with acute lymphoblastic leukemia after the completion of chemotherapy. J Pediatr Hematol Oncol. Sep 2005;27(9):499-501.
73. Probert JC, Parker BR, Kaplan HS. Growth retardation in children after megavoltage irradiation of the spine. Cancer. Sep 1973;32(3):634-639.
74. Probert JC, Parker BR. The effects of radiation therapy on bone growth. Radiology. Jan 1975;114(1):155-162.
75. Noorda EM, Somers R, van Leeuwen FE, Vulsma T, Behrendt H. Adult height and age at menarche in childhood cancer survivors. Eur J Cancer. Mar 2001;37(5):605-612.
76. Gurney JG, Ness KK, Stovall M, et al. Final height and body mass index among adult survivors of childhood brain cancer: childhood cancer survivor study. J Clin Endocrinol Metab. Oct 2003;88(10):4731-4739.
77. Brownstein CM, Mertens AC, Mitby PA, et al. Factors that affect final height and change in height standard deviation scores in survivors of childhood cancer treated with growth hormone: a report from the childhood cancer survivor study. J Clin Endocrinol Metab. Sep 2004;89(9):4422-4427.
78. Goldsby RE, Taggart DR, Ablin AR. Surviving childhood cancer: the impact on life. Paediatr Drugs. 2006;8(2):71-84.
79. Oeffinger KC, Mertens AC, Sklar CA, et al. Obesity in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol. Apr 1 2003;21(7):1359-1365.
80. Sklar CA, Mertens AC, Walter A, et al. Changes in body mass index and prevalence of overweight in survivors of childhood acute lymphoblastic leukemia: role of cranial irradiation. Med Pediatr Oncol. Aug 2000;35(2):91-95.
81. Rogers PC, Meacham LR, Oeffinger KC, Henry DW, Lange BJ. Obesity in pediatric oncology. Pediatr Blood Cancer. Dec 2005;45(7):881-891.
82. Meacham LR, Gurney JG, Mertens AC, et al. Body mass index in long-term adult survivors of childhood cancer: a report of the Childhood Cancer Survivor Study. Cancer. Apr 15 2005;103(8):1730-1739.
83. Koocher GP, O’Malley JE. The Damocles syndrome: psychosocial consequences of surviving childhood cancer. New York: McGraw-Hill; 1981.
84. Schmale AH, Morrow GR, Schmitt MH, et al. Well-being of cancer survivors. Psychosom Med. May 1983;45(2):163-169.
85. Cella DF, Tross S. Psychological adjustment to survival from Hodgkin’s disease. J Consult Clin Psychol. Oct 1986;54(5):616-622.
86. Mulhern RK, Wasserman AL, Kovnar EH, Williams JM, Ochs JJ. Serial neuropsychological studies of a child with acute lymphoblastic leukemia and subsequent glioblastoma multiforme. Neurology. Nov 1986;36(11):1534-1538.
87. Teta MJ, Del Po MC, Kasl SV, Meigs JW, Myers MH, Mulvihill JJ. Psychosocial consequences of childhood and adolescent cancer survival. J Chronic Dis. 1986; 39(9):751-759.
88. Williams JM, Ochs J, Davis KS, et al. The subacute effects of CNS prophylaxis for acute lymphoblastic leukemia on neuropsychological performance: a comparison of four protocols. Arch Clin Neuropsychol. 1986;1(2):183-192.
89. Mulhern RK, Wasserman AL, Friedman AG, Fairclough D. Social competence and behavioral adjustment of children who are long-term survivors of cancer. Pediatrics. Jan 1989;83(1):18-25.
90. Brown RT, Kaslow NJ, Hazzard AP, et al. Psychiatric and family functioning in children with leukemia and their parents. J Am Acad Child Adolesc Psychiatry. May 1992;31(3):495-502.
91. Gray RE, Doan BD, Shermer P, et al. Psychologic adaptation of survivors of childhood cancer. Cancer. Dec 1 1992;70(11):2713-2721.
92. Brown RT, Madan-Swain A. Cognitive, neuropsychological, and academic sequelae in children with leukemia. J Learn Disabil. Feb 1993;26(2):74-90.
93. Madan-Swain A, Brown RT, Sexson SB, Baldwin K, Pais R, Ragab A. Adolescent cancer survivors. Psychosocial and familial adaptation. Psychosomatics. Sep-Oct 1994; 35(5):453-459.
94. Chesler M, Zebrack B. An Updated Report on Our Studies of Long-Term Survivorship of Childhood Cancer and a Brief Review of the Psychosocial Literature Ann Arbor, MI: Center for research on Social Organization, University of Michigan; 1997.
95. Elkin TD, Phipps S, Mulhern RK, Fairclough D. Psychological functioning of adolescent and young adult survivors of pediatric malignancy. Med Pediatr Oncol. Dec 1997;29(6):582-588.
96. Kokkonen J, Vainionpaa L, Winqvist S, Lanning M. Physical and psychosocial outcome for young adults with treated malignancy. Pediatr Hematol Oncol. May-Jun 1997;14(3):223-232.
97. Pendley JS, Dahlquist LM, Dreyer Z. Body image and psychosocial adjustment in adolescent cancer survivors. J Pediatr Psychol. Feb 1997;22(1):29-43.
98. Zeltzer LK, Chen E, Weiss R, et al. Comparison of psychologic outcome in adult survivors of childhood acute lymphoblastic leukemia versus sibling controls: a cooperative Children’s Cancer Group and National Institutes of Health study. J Clin Oncol. Feb 1997;15(2):547-556.
99. Richardson RC, Nelson MB, Meeske K. Young adult survivors of childhood cancer: attending to emerging medical and psychosocial needs. J Pediatr Oncol Nurs. Jul 1999;16(3):136-144.
100. Chen E, Zeltzer LK, Craske MG, Katz ER. Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev. Jul-Aug 2000;71(4):933-947.
101. Eiser C, Hill JJ, Vance YH. Examining the psychological consequences of surviving childhood cancer: systematic review as a research method in pediatric psychology. J Pediatr Psychol. Sep 2000;25(6):449-460.
102. Manne S, Nereo N, DuHamel K, et al. Anxiety and depression in mothers of children undergoing bone marrow transplant: symptom prevalence and use of the Beck depression and Beck anxiety inventories as screening instruments. J Consult Clin Psychol. Dec 2001;69(6):1037-1047.
103. Langer T, Martus P, Ottensmeier H, Hertzberg H, Beck JD, Meier W. CNS late-effects after ALL therapy in childhood. Part III: neuropsychological performance in long-term survivors of childhood ALL: impairments of concentration, attention, and memory. Med Pediatr Oncol. May 2002;38(5):320-328.
104. Alter CL, Pelcovitz D, Axelrod A, et al. Identification of PTSD in cancer survivors. Psychosomatics. Mar-Apr 1996;37(2):137-143.
105. Butler RW, Rizzi LP, Handwerger BA. Brief report: the assessment of posttraumatic stress disorder in pediatric cancer patients and survivors. J Pediatr Psychol. Aug 1996;21(4):499-504.
106. Stuber ML, Christakis DA, Houskamp B, Kazak AE. Posttrauma symptoms in childhood leukemia survivors and their parents. Psychosomatics. May-Jun 1996;37(3):254-261.
107. Barakat LP, Kazak AE, Meadows AT, Casey R, Meeske K, Stuber ML. Families surviving childhood cancer: a comparison of posttraumatic stress symptoms with families of healthy children. J Pediatr Psychol. Dec 1997;22(6):843-859.
108. Kazak AE, Barakat LP, Meeske K, et al. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol. Feb 1997;65(1):120-129.
109. Stuber ML, Kazak AE, Meeske K, et al. Predictors of posttraumatic stress symptoms in childhood cancer survivors. Pediatrics. Dec 1997;100(6):958-964.
110. Kazak AE. Posttraumatic distress in childhood cancer survivors and their parents. Med Pediatr Oncol. 1998;Suppl 1:60-68.
111. Rourke MT, Stuber ML, Hobbie WL, Kazak AE. Posttraumatic stress disorder: understanding the psychosocial impact of surviving childhood cancer into young adulthood. J Pediatr Oncol Nurs. Jul 1999;16(3):126-135.
112. Hobbie WL, Stuber M, Meeske K, et al. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol. Dec 15 2000;18(24):4060-4066.
113. Erickson SJ, Steiner H. Trauma spectrum adaptation: somatic symptoms in long-term pediatric cancer survivors. Psychosomatics. Jul-Aug 2000;41(4):339-346.
114. Manne S, DuHamel K, Nereo N, et al. Predictors of PTSD in mothers of children undergoing bone marrow transplantation: the role of cognitive and social processes. J Pediatr Psychol. Oct-Nov 2002;27(7):607-617.
115. Alderfer MA, Labay LE, Kazak AE. Brief report: does posttraumatic stress apply to siblings of childhood cancer survivors? J Pediatr Psychol. Jun 2003;28(4):281-286.
116. Brown RT, Madan-Swain A, Lambert R. Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. J Trauma Stress. Aug 2003;16(4):309-318.
117. Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. Apr-May 2004;29(3):211-219.
118. Kazak AE, Alderfer MA, Streisand R, et al. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: a randomized clinical trial. J Fam Psychol. Sep 2004;18(3):493-504.
119. Alderfer MA, Cnaan A, Annunziato RA, Kazak AE. Patterns of posttraumatic stress symptoms in parents of childhood cancer survivors. J Fam Psychol. Sep 2005; 19(3):430-440.
120. Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol. May 2006;31(4):413-419.
121. Stoppelbein LA, Greening L, Elkin TD. Risk of Posttraumatic Stress Symptoms: A Comparison of Child Survivors of Pediatric Cancer and Parental Bereavement. J Pediatr Psychol. 2006;31(4):367-376.
122. Mulhern RK, Ochs J, Fairclough D, Wasserman AL, Davis KS, Williams JM. Intellectual and academic achievement status after CNS relapse: a retrospective analysis of 40 children treated for acute lymphoblastic leukemia. J Clin Oncol. Jun 1987;5(6):933-940.
123. Mulhern RK, Wasserman AL, Fairclough D, Ochs J. Memory function in disease-free survivors of childhood acute lymphocytic leukemia given CNS prophylaxis with or without 1,800 cGy cranial irradiation. J Clin Oncol. Feb 1988;6(2):315-320.
124. Brown RT, Madan-Swain A, Pais R, et al. Cognitive status of children treated with central nervous system prophylactic chemotherapy for acute lymphocytic leukemia. Arch Clin Neuropsychol. Nov 1992;7(6):481-497.
125. Brown RT, Sawyer MB, Antoniou G, et al. A 3-year follow-up of the intellectual and academic functioning of children receiving central nervous system prophylactic chemotherapy for leukemia. J Dev Behav Pediatr. Dec 1996;17(6):392-398.
126. Brown RT, Madan-Swain A, Walco GA, et al. Cognitive and academic late effects among children previously treated for acute lymphocytic leukemia receiving chemotherapy as CNS prophylaxis. J Pediatr Psychol. Oct 1998;23(5):333-340.
127. Kazak AE, Simms S, Barakat L, et al. Surviving cancer competently intervention program (SCCIP): a cognitive-behavioral and family therapy intervention for adolescent survivors of childhood cancer and their families. Fam Process. Summer 1999;38(2):175-191.
128. Winqvist S, Vainionpaa L, Kokkonen J, Lanning M. Cognitive functions of young adults who survived childhood cancer. Appl Neuropsychol. 2001;8(4):224-233.
129. von der Weid N, Mosimann I, Hirt A, et al. Intellectual outcome in children and adolescents with acute lymphoblastic leukaemia treated with chemotherapy alone: age- and sex-related differences. Eur J Cancer. Feb 2003;39(3):359-365.
130. Buizer AI, de Sonneville LM, van den Heuvel-Eibrink MM, Veerman AJ. Behavioral and educational limitations after chemotherapy for childhood acute lymphoblastic leukemia or Wilms tumor. Cancer. Mar 27 2006;Prepublication release.
131. Beardslee C, Neff EJ. Body related concerns of children with cancer as compared with the concerns of other children. Matern Child Nurs J. Fall 1982;11(3):121-134.
132. Neff EJ, Beardslee CI. Body knowledge and concerns of children with cancer as compared with the knowledge and concerns of other children. J Pediatr Nurs. Jun 1990; 5(3):179-189.
133. Anholt U, Fritz G, Keener M. Self-concept in survivors of childhood and adolescent cancer. J Psychosoc Oncol. 1993;11(1):1-16.
134. Madan-Swain A, Brown RT, Foster MA, et al. Identity in adolescent survivors of childhood cancer. J Pediatr Psychol. Mar 2000;25(2):105-115.
135. Zebrack BJ, Chesler M. Health-related worries, self-image, and life outlooks of long-term survivors of childhood cancer. Health Soc Work. Nov 2001;26(4):245-256.
136. Landier W, Wallace WH, Hudson MM. Long-term follow-up of pediatric cancer survivors: education, surveillance, and screening. Pediatr Blood Cancer. Feb 2006;46(2):149-158.
137. Byrne J, Lewis S, Halamek L, Connelly RR, Mulvihill JJ. Childhood cancer survivors’ knowledge of their diagnosis and treatment. Ann Intern Med. Mar 1 1989;110(5):400-403.
138. Kadan-Lottick NS, Robison LL, Gurney JG, et al. Childhood cancer survivors’ knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. Jama. Apr 10 2002;287(14):1832-1839.
139. Bashore L. Childhood and adolescent cancer survivors’ knowledge of their disease and effects of treatment. J Pediatr Oncol Nurs. Mar-Apr 2004;21(2):98-102.
140. Caprino D, Wiley TJ, Massimo L. Childhood cancer survivors in the dark. J Clin Oncol. Jul 1 2004;22(13):2748-2750.
141. Zebrack BJ, Eshelman DA, Hudson MM, et al. Health care for childhood cancer survivors: insights and perspectives from a Delphi panel of young adult survivors of childhood cancer. Cancer. Feb 15 2004;100(4):843-850.
142. Mulhern RK, Tyc VL, Phipps S, et al. Health-related behaviors of survivors of childhood cancer. Med Pediatr Oncol. Sep 1995;25(3):159-165.
143. Hudson MM, Tyc VL, Srivastava DK, et al. Multi-component behavioral intervention to promote health protective behaviors in childhood cancer survivors: the protect study. Med Pediatr Oncol. Jul 2002;39(1):2-1; discussion 2.
144. Tyc VL, Hudson MM, Hinds P. Health promotion interventions for adolescent cancer survivors. Cognitive and Behavioral Practice. 1999;6:128-136.
145. Park EB, Emmons KM, Malloy NW, Seifer E. A qualitative exploration of health perceptions and behaviors among adult survivors of childhood cancers. J Cancer Educ. Winter 2002;17(4):211-215.
146. Cox CL, McLaughlin RA, Rai SN, Steen BD, Hudson MM. Adolescent survivors: A secondary analysis of a clinical trial targeting behavior change. Pediatr Blood Cancer. Mar 15 2005.
147. Demark-Wahnefried W, Werner C, Clipp EC, et al. Survivors of childhood cancer and their guardians. Cancer. May 15 2005;103(10):2171-2180.
148. Hollen PJ, Hobbie WL, Finley SM, Hiebert SM. The relationship of resiliency to decision making and risk behaviors of cancer-surviving adolescents. J Pediatr Oncol Nurs. Sep-Oct 2001;18(5):188-204.
149. Emmons K, Li FP, Whitton J, et al. Predictors of smoking initiation and cessation among childhood cancer survivors: a report from the childhood cancer survivor study. J Clin Oncol. Mar 15 2002;20(6):1608-1616.
150. Oeffinger KC, Mertens AC, Hudson MM, et al. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. Jan-Feb 2004;2(1):61-70.
151. Schidlow DV, Fiel SB. Life beyond pediatrics. Transition of chronically ill adolescents from pediatric to adult health care systems. Med Clin North Am. Sep 1990;74(5):1113-1120.
152. Rettig P, Athreya BH. Adolescents with chronic disease. Transition to adult health care. Arthritis Care Res. Dec 1991;4(4):174-180.
153. Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. Nov 1993;14(7):570-576.
154. Rosen DS. Transition to adult health care for adolescents and young adults with cancer. Cancer. May 15 1993;71(10 Suppl):3411-3414.
155. Betz CL. Facilitating the transition of adolescents with chronic conditions from pediatric to adult health care and community settings. Issues Compr Pediatr Nurs. Apr-Jun 1998;21(2):97-115.
156. Blum RW. Introduction. Improving transition for adolescents with special health care needs from pediatric to adult-centered health care. Pediatrics. Dec 2002;110(6 Pt 2):1301-1303.
157. Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. Dec 2002;110(6 Pt 2):1322-1327.
158. Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. Dec 2002;110(6 Pt 2):1307-1314.
159. Scal P. Transition for youth with chronic conditions: primary care physicians’ approaches. Pediatrics. Dec 2002;110(6 Pt 2):1315-1321.
160. White PH. Access to health care: health insurance considerations for young adults with special health care needs/disabilities. Pediatrics. Dec 2002;110(6 Pt 2):1328-1335.
161. Merrick J, Kandel I. Adolescents with special needs and the transition from adolescent to adult health care. Int J Adolesc Med Health. Apr-Jun 2003;15(2):103.
162. Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. Oct 2003;33(4):309-311.
163. McDonagh JE. Growing up and moving on: transition from pediatric to adult care. Pediatr Transplant. Jun 2005;9(3):364-372.
164. Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics. Jun 2005;115(6):1607-1612.
165. Ginsberg JP, Hobbie WL, Carlson CA, Meadows AT. Delivering long-term follow-up care to pediatric cancer survivors: transitional care issues. Pediatr Blood Cancer. Feb 2006;46(2):169-173.
166. Cunningham PJ, Kohn L. Health plan switching: choice or circumstance? Health Aff (Millwood). May-Jun 2000;19(3):158-164.
167. Smith MA, Bartell JM. Changes in usual source of care and perceptions of health care access, quality, and use. Med Care. Oct 2004;42(10):975-984.
168. Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. Apr 2003;93(4):635-641.
169. University of Minnesota Cancer Center. Surviving childhood cancer. November 1, 2002; http://www.cancer.umn.edu/ltfu. Accessed December 1, 2004.
170. Fordis M, Horowitz M, Landier W, et al. Investigation of the feasibility of developing an online decision support tool for healthcare providers managing the long-term follow-up of survivors of childhood cancer. Paper presented at: Society of Academic Continuing Medical Education (SACME)/Research in Continuing Medical Education (RICME); April 8, 2006; Key West, FL.
171. McKinley ED. Under Toad days: surviving the uncertainty of cancer recurrence. Ann Intern Med. Sep 19 2000;133(6):479-480.
172. Grant J, Cranston A, Horsman J, et al. Health status and health-related quality of life in adolescent survivors of cancer in childhood. J Adolesc Health. May 2006; 38(5):504-510.
173. Mooney GA, Bligh JG. Computer-based learning materials for medical education: a model production. Med Educ. May 1997;31(3):197-201.
174. Landier W, Bhatia S, Eshelman DA, et al. Development of risk-based guidelines for pediatric cancer survivors: the Children’s Oncology Group Long-Term Follow-Up Guidelines from the Children’s Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. Dec 15 2004;22(24):4979-4990.
175. National Comprehensive Cancer Network. Categories of Consensus. 2006; http://www.nccn.org/professionals/physician_gls/categories_of_concensus.asp. Accessed April 19, 2006.
176. Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. Nov 9 1989;321(19):1306-1311.
177. Tunis SR, Hayward RS, Wilson MC, et al. Internists’ attitudes about clinical practice guidelines. Ann Intern Med. Jun 1 1994;120(11):956-963.
178. Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. Aug 15 1997;157(4):408-416.
179. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. Oct 20 1999;282(15):1458-1465.
180. Browman GP. Clinical practice guidelines and healthcare decisions: credibility gaps and unfulfilled promises? Nat Clin Pract Oncol. Oct 2005;2(10):480-481.
181. Feifer C, Fifield J, Ornstein S, et al. From research to daily clinical practice: what are the challenges in “translation”? Jt Comm J Qual Saf. May 2004;30(5):235-245.
182. Greenfield S, Kaplan S, Ware JE, Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. Apr 1985;102(4):520-528.
183. Greenfield S, Kaplan SH, Ware JE, Jr., Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. Sep-Oct 1988;3(5):448-457.
184. Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. Dec 15 1997;127(12):1097-1102.
185. Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. May 7 2002;136(9):641-651.
186. Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. Nov-Dec 1996;3(6):399-409.
187. Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. Oct 21 1998;280(15):1339-1346.
188. Mitchell E, Sullivan F. A descriptive feast but an evaluative famine: systematic review of published articles on primary care computing during 1980-97. BMJ. Feb 3 2001; 322(7281):279-282.
189. Gandhi TK, Sequist TD, Poon EG, et al. Primary care clinician attitudes towards electronic clinical reminders and clinical practice guidelines. AMIA Annu Symp Proc. 2003:848.
190. Evans RS, Pestotnik SL, Classen DC, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. Jan 22 1998;338(4):232-238.
191. McCulloch DK, Price MJ, Hindmarsh M, Wagner EH. A population-based approach to diabetes management in a primary care setting: early results and lessons learned. Eff Clin Pract. Aug-Sep 1998;1(1):12-22.
192. Griffin S, Kinmonth AL. Systems for routine surveillance for people with diabetes mellitus. Nurs Times. Jul 5-11 2001;97(27):44.
193. Rundall TG, Shortell SM, Wang MC, et al. As good as it gets? Chronic care management in nine leading US physician organisations. BMJ. Oct 26 2002;325(7370):958-961.
194. Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. Nov-Dec 2004;2(6):595-608.
195. Osheroff JA, Pifer EA, Teich JM, Sittig DF, Jenders RA. Improving Outcomes with Clinical Decision Support: An Implementer’s Guide. Chicago, IL: Healthcare Information and Management Systems Society; 2005.
196. Teich JM, Osheroff JA, Pifer EA, Sittig DF, Jenders RA. Clinical decision support in electronic prescribing: recommendations and an action plan: report of the joint clinical decision support workgroup. J Am Med Inform Assoc. Jul-Aug 2005;12(4):365-376.
197. Connecting For Health Steering Group. The Connecting for Health Common Framework: Overview and Principles. April, 2006; http://www.connectingforhealth.org/commonframework/docs/Overview.pdf. Accessed May 24, 2006.
198. 104th U.S. Congress. Public Law 104-91—Health Insurance Portability and Accountability Act of 1996: An Act. August 21, 1996; http://aspe.hhs.gov/admnsimp/pl104191.htm. Accessed May 24, 2006.
Appendix D.4
Regional Approaches to Cancer Survivorship Care Planning
Tim Byers, MD, MPH
Professor, University of Colorado School of Medicine
Deputy Director, University of Colorado Cancer Center
Synopsis: State-level cancer control collaboratives could help to institute a widespread adoption of cancer survivorship planning, but most of the current collaboratives will first need to better engage health care providers.
Introduction
Cancer Control as a Regional Issue
If cancer survivor plans are to constitute a standard in cancer care, many different organizations will need to collaborate to institute this new service as a medical care norm.1 Regional organizations that currently collaborate in cancer control programs could be particularly helpful to broadly institute cancer survivor planning. The purpose of this paper is to examine this potential, and to critically assess both the capabilities and weaknesses of organizations engaged in regional cancer control activities. The term “regional” could define many different types of geopolitical units. In this review, “regional” will be considered mostly as statewide or as pertaining to subregions of a state, such as an urban area with its surrounding suburbs, or a defined rural area of a state with a regional identity. The term “regional” could also refer to areas of the country that include several states, such as the Southwest or the Midwest, but most multistate regional organizations, such as Department of Health and Human Services (DHHS) regions and American Cancer Society (ACS) Divisions, have been created
principally for administrative convenience, and do not have functional collaborative programs. As most public health activity tends to be state-specific, and most cancer control programming is now at the state level, the term “regional” will mostly be used here as synonymous with “statewide.”
State-based cancer organizations have been under development as a public health strategy over the past decade by the Centers for Disease Control and Prevention (CDC).2 The CDC comprehensive cancer control strategy is to support public health departments to create state-wide collaborative organizations that join expertise from public health agencies, universities, nongovernmental voluntary cancer organizations, and health care providers. That CDC would designate state health departments as the conveners of statewide collaborative organizations derives from the historic relationship between CDC and state governments. States are the geopolitical units with primary responsibility for public health in the United States, and the historic role of CDC has been to support states in their public health efforts. CDC’s cancer control strategy via states has been to build a program of comprehensive cancer control onto their earlier investments in chronic disease prevention and control, including state tobacco control programs, cancer registries, breast and cervical cancer screening, and behavioral risk factor surveillance systems.
The Current Status of State-Based Comprehensive Cancer Control
The CDC model for state-based comprehensive cancer control is to build programs in two stages: first planning, then implementation. The planning process can take from one to several years. Planning is a collaborative process in which the state health department cancer control program staff convene work groups to examine cancer trends and risk factors, then to examine existing resources and opportunities, and finally to create consensus objectives and strategies to reduce the state’s cancer burden. At this time, 44 states have completed the cancer planning process, with publication of their state cancer plans.3 The implementation stage then follows, a prolonged period with no definable ending, in which collaboratives in the state work to develop a comprehensive cancer control program and to accomplish the goals set out in the cancer plan. As the CDC budget for cancer control is not growing as rapidly as is the number of states entering into the implementation phase, the level of funding per state for implementation has been decreasing in recent years. Thus, comprehensive cancer control across the United states is progressing in terms of the numbers of states completing plans and moving into implementation, but it is at the same time regressing from the perspective of the availability of resources to implement plans within states.
The main strength of state-based cancer programs derives from their
multiorganizational and multidisciplinary nature. State cancer coalitions (variously also called “alliances,” or “partnerships”) serve the function of communication and collaboration about various cancer control activities across many different sectors within states. These sectors include public health agencies, academic centers, nongovernmental voluntary health agencies, and health care providers. Most of the actual work of cancer control in the state cancer coalitions is conducted by the partner organizations. The purpose of the coalition is to motivate and coordinate the collective body of work done by partner organizations. Within the coalitions, most of the planning and communication occurs within work groups or task forces. The composition of these groups differs across states but usually includes disease-specific groups (e.g., breast cancer, colorectal cancer, prostate cancer, skin cancer), or groups focusing on specific issues that cut across cancer sites (e.g., surveillance, evaluation, health disparities).
There are two major weaknesses of state cancer control coalitions: insufficient funding and insufficient independence. CDC has provided funding for the development of cancer plans across states, but as states finish the planning process, there is insufficient funding to enact programs to achieve the lofty goals defined in the planning process. With the numbers of states entering into the implementation phase of comprehensive cancer control growing much more rapidly that the CDC budget for cancer control, the result has been lower budgets for states to effectively engage in implementation activities. A result, then, is that states can be proud of the glossy cancer plans on their shelves and empowered by the potentials of new partnerships formed in the planning process but can then have considerable difficulty maintaining that collaborative spirit as they try to implement lofty goals with insufficient resources.
Another weakness of state cancer programs is their lack of independence from their funding source. Comprehensive cancer programs are funded by CDC grants to state health departments, sometimes supplemented also by state monies, but in all cases the effort is managed by the state public health department. Although CDC properly envisions the role of the public health department as the convener of statewide collaboratives, and regards the strength of coalitions as coming from their multisectorial representation, the fact that cancer coalitions are convened and staffed by state public health department personnel means that coalition partners tend to regard the process as a state health department activity. As a result, many partners, especially health care providers, do not become as fully engaged as they otherwise might if the effort had a more independent identity. This problem is compounded, of course, by the problem of insufficient funding. Coalitions can often be hesitant to become fully engaged in issues that are politically sensitive, such as policy or legislative matters in which state employees (the conveners of coalitions) are disallowed from engagement
due to their government employee status. Apart from these legal conflicts, the public health department identity of cancer coalitions also tends to distance the coalitions from health care providers because of the historic gap between public health departments and health care providers. Most public health workers who convene cancer coalitions have not been trained as health care providers and are much more fluent in public health skills such as mass marketing, health education, and surveillance, than in matters pertaining to clinical cancer care. One result of the low level of provider input into state cancer programs has been the low profile of goals and strategies to meet the many needs of cancer patients in treatment, rehabilitation, and survivorship.
Cancer Survivorship Content Within State Cancer Plans
There are 44 state cancer plans (Alaska, Idaho, Illinois, Mississippi, Montana, and Oklahoma are now drafting cancer plans).3 State cancer plans are written in varying degrees of detail, and in many different formats. All plans include descriptions of cancer risk in the state and set specific targets for reducing cancer incidence and mortality as well as lowering the prevalence of cancer risk factors across the state. Nearly all plans are heavily weighted by objectives for cancer prevention and early detection. Most plans also include some mention of cancer survivorship issues by at least briefly acknowledging the importance of cancer survivorship. Many plans, for instance, simply define cancer survivorship by the National Cancer Institute (NCI) definition (“An individual is considered a cancer survivor from the time of diagnosis, through the balance of his or her life”), or state the many needs of survivors without defining specific objectives. Most plans cover pain control or end-of-life care as their principal cancer survivorship focus. The emphasis on pain control and end-of-life care are understandable as the evidence base in these areas is stronger than for most of the other issues in cancer survivorship. In fact, a recent Institute of Medicine (IOM) report that defined a set of measures for the State of Georgia (intended as a model set of quality measures for any state) included pain control and hospice utilization as the only cancer survivorship measures among 52 measures. 4 Many plans also make general reference to the need for better education of both cancer survivors and health care providers about cancer survivorship needs and support systems. Some plans specify more survivorship needs and objectives that could potentially be tied to cancer survivorship planning. Selected aspects of those more specific objectives are summarized in Table D.4-1.
Only two state plans specifically mention objectives that could be interpreted as promoting the specific idea of cancer survivorship plans (Minnesota and Oregon). In the Minnesota plan, objective #17 is to “Optimize
TABLE D.4-1 Specific Statements of Need and Objectives Related to Cancer Survivorship Support that Might Be Tied to Cancer Survivorship Plans in Selected State Cancer Plans
|
State (page in plan) |
Need |
Objective |
|
Alabama (25) |
Cancer support services are underutilized. |
Increase knowledge of cancer support services by both providers and the public. |
|
Arizona (127) |
Cancer patients need better support services. |
Promote patient navigator programs, help providers direct patients to supportive care, and monitor gaps in support services. |
|
Colorado (62-66) |
Rehabilitation after cancer treatment is lacking. |
Support the development of navigation and rehabilitation services. |
|
Connecticut (89-91) |
Cancer patients find the survivorship process confusing. |
Define “high-quality” care for cancer survivors. |
|
Iowa (46-47) |
Poor communication exists between providers and patients regarding cancer care. |
Increase communication between providers and patients about cancer care, and also educate providers about the need to take care of themselves. |
|
Indiana (47-49) |
Cancer support services are underutilized. |
Increase knowledge of cancer support services by both providers and the public. |
|
Kansas (35-37) |
Recovery and reintegration of cancer survivors into family, society and workplace is lacking. |
A business standard of excellence is proposed for return to work, and an emphasis is placed also on preventive behaviors, including nutrition, among cancer patients. |
|
Louisiana (71-74) |
Rehabilitation after cancer treatment is needed. |
Provide clearer information to both providers and patients about cancer rehab services. |
continuity of care for cancer survivors during and beyond the initial course of treatment.” That objective would be assessed by monitoring the proportion of primary care physicians who receive information about their patients’ cancer treatment and follow-up recommendations from their patients’ oncologists. Special surveys would be done to accomplish that assessment. In the Oregon plan, objective #3 is to “Increase the proportion of cancer patients who are informed and participate with their provider in their long-term follow-up care plan.” That objective would be achieved
|
State (page in plan) |
Need |
Objective |
|
Maine (61-62) |
Rehabilitation and survivorship services are needed. |
A “best practices” approach is suggested to define high-quality services statewide. |
|
Maryland (92-94) |
Need to develop survivorship awareness and services. |
Several objectives are defined for education but also one for establishing cancer survivor clinics. |
|
Minnesota (42-43) |
Continuity of care is lacking. |
Encourage oncologists to provide clear treatment summaries and care plans to primary care practitioners. |
|
Nevada (18) |
Develop a more comprehensive approach to long-term cancer survivorship. |
The Nevada Cancer Institute is developing a cancer survivorship program that can be a model, made possible by LAF. |
|
New York (30) |
Employment and insurance issues are barriers for cancer survivors. |
Employment and insurance will be addressed as statewide policy issues. |
|
Oregon (73-77) |
The transition from cancer care to survivorship is confusing. |
Increase the proportion of cancer patients who are informed and participate with their provider in their long-term follow-up plan. |
|
Texas (76-80) |
Identifies many needs in information and access. |
Increase knowledge of survivorship issues for the general public, cancer survivors, health care professionals, and policy makers. |
|
Virginia (82) |
Rehabilitation for cancer is insufficient. |
Assure that cancer rehab services become available statewide. |
using strategies that include increased communication with providers about follow-up guidelines and developing long-term follow-up plans as collaborative activities between providers and patients.
Survivorship planning is rarely pointed to in state cancer plans, probably because the idea of cancer survivorship plans is fairly new, and there is as yet little evidence basis for including it as a statewide objective. Many state cancer plans only generally acknowledge the many needs of cancer survivors, however, and many plans merely point to the general needs of
health care providers as well as patients and family members for education about cancer survivorship. The fact that detailed objectives in most of the plans are much less common than the general rhetoric about the importance of survivorship may suggest that state cancer coalition members would be quite receptive to specific measurable objectives for cancer survivorship planning.
Cancer Survivorship as a Public Health Issue
The CDC has joined in a partnership effort with the Lance Armstrong Foundation (LAF) to better develop a public health role in cancer survivorship.5 In their 2004 report entitled “A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies”, the CDC-LAF partnership defines four areas of traditional public health activity within which cancer survivorship can be relevant: (1) surveillance and applied research; (2) communication, education, and training; (3) programs, policies, and infrastructure; and (4) access to quality care and services.
Cancer surveillance might be the single most important area in which public health agencies could have an immediate impact on cancer survivorship. All states operate cancer registries. These registries were developed to monitor cancer incidence and survival. Outcomes apart from recurrence and survival have been assessed only as special studies tied to cancer registries. Over time, though, cancer registries have begun to also monitor the quality of cancer care.6 In the near future, outcomes such as fatigue, pain, confusion, satisfaction with health care, and both the need for and utilization of community support services could become routinely measured as part of cancer surveillance systems in states. Communication, education, and training are traditional public health functions that fit well into the model of cancer coalition activities. These types of activities require far fewer resources than do the provision of services. Programs, policies, and infrastructure are more problematic for state comprehensive cancer control programs, both because of insufficient funding for programs and because of insufficient independence to affect policies. Access to quality care and services is also a challenge for public-health-dominated coalitions, as public health agencies provide very little cancer care, and health care access is now determined more by insurance and entitlement programs than by public health agencies.
Other State-Based Organizations Relevant to Cancer Survivorship
Many state-based organizations are active in cancer survivorship programs. In most states, these organizations are also active members of the state cancer coalition. These include comprehensive cancer centers,
quality improvement organizations, health care professional organizations, health care provider systems, and nongovernmental cancer voluntary organizations.
Comprehensive Cancer Centers
NCI provides core support to 39 comprehensive cancer centers across the United States.7 The principal mission of these centers is to conduct cancer research. In order to be designated as a comprehensive cancer center, centers must demonstrate their expertise in cancer control research and their connection to cancer control activities in the populations they serve. NCI funding does not directly support community outreach and cancer control service programs of cancer centers, but the requirement of community outreach as a criterion for the “comprehensive” designation is a strong incentive for cancer center researchers to collaborate in community-based programs such as state cancer coalitions. NCI provides core support for cancer centers to conduct research. Most of those resources support the basic science and clinical science core laboratories needed for research, but some cancer centers also use NCI resources to support community outreach and population sciences. Academic cancer center members who conduct community-based and population-based cancer research are frequently the faculty who become engaged in state cancer coalitions. In addition, cancer researchers with special interests in a particular type of cancer are often engaged in the work group or task force for that cancer type. With the recent drop in funding levels for cancer research by NCI, there has been a tightening of budgets not only for new research, but also for core support to cancer centers. Though new initiatives in cancer survivorship such as survivor planning will likely be supported by cancer centers, and though cancer centers would be excellent settings in which to conduct demonstration projects, it is unlikely that NCI will be a major source of new funding for this as a developmental project via cancer centers in the near future.
NCI does provide major support for clinical trials, however, both via cancer centers and via community-based trial organizations. It is in the realm of clinical trials where cancer survivor plans could emerge as a service project of cancer center investigators, blending service with research. All clinical trials now include at least some assessment of quality-of-life outcome measures. This happened as a mandated policy from the cooperative trial groups supported by NCI. NCI could, as a matter of policy, also mandate that that all patients exiting the first course of treatment in clinical trials be provided a full written treatment summary and follow-up plan, essentially a cancer survivorship plan. If such a policy were not accompanied by additional resources, it would be met with some resistance from clinicians, but clinical trial systems in both cancer centers and in the com-
munities would be excellent places in which to support demonstration projects as addendums to ongoing trials.
Quality Improvement Organizations
The Center for Medicare and Medicaid Services (CMS) supports interventions to improve the quality of health care services principally through a system 53 of state and territory-based organizations called Quality Improvement Organizations (QIOs).8 It is the mission of QIOs to conduct projects within each state to improve the quality of medical services provided to Medicare beneficiaries. These projects are often done in collaboration with other states as either national or multistate projects, under a general framework of themes and goals set by CMS. Important projects have been done to improve the quality and reach of proven interventions such as adult immunizations, the clinical management of diabetes, pneumonia, heart failure, and myocardial infarction. In the area of cancer quality improvement, projects have been done to increase mammography utilization and colorectal screening, but to date no projects have been done to improve the quality of cancer survivorship. As Medicare pays for a substantial proportion of cancer care in the United States, engaging the QIOs to implement and evaluate a cancer survivorship planning project might be a very effective way to develop, evaluate, and then, eventually, to implement cancer survivor plans. A widespread national quality improvement project on cancer survivorship planning would likely need to follow a stronger set of evidence for efficacy, but a small demonstration project could be done with CMS support. The advantage of this as a CMS QIO project is that such a project would be done in settings in which successful partnerships with hospital care systems have been done before, on statewide bases, with strong evaluations.
Health Care Professional Organizations
Health care professional societies such as the American Society of Clinical Oncology (ASCO), the American College of Surgeons (ACoS), and the Oncology Nursing Society (ONS) have been leaders in the development and implementation of guidelines to improve the standard of care. These professional organizations tend to impact problems of clinical care at a national level, but there are often viable local or state-level chapters, and many of the leaders in these organizations are also active members of state cancer coalitions. ASCO has been active in setting standards for cancer care, and cancer survivorship planning could eventually be added into quality cancer care standards. ACoS certifies hospitals across the United states according to their cancer treatment quality standards, so cancer survivorship planning
could be added into other hospital-based quality standards. The ONS provides ongoing continuing education to nurses to improve the quality of nursing oncology practice, and nurses would likely play important roles in survivorship care planning and patient support. All three of these organizations, both via their national organizations and also via their local and state organizations, could be instrumental in developing and instituting cancer survivorship planning.
Health Care Systems
Health care systems and organizations are often organized with regional reach. Large HMOs, for instance, often capture a substantial proportion of patients in a region (e.g., Kaiser in the San Francisco Bay Area, or Group Health Cooperative in the Puget Sound area). Hospital systems can also have considerable influence on medical practice in an urban or rural region of a state. Health care systems such as these could therefore substantially influence practice norms in a region if they were to institute cancer survivorship plans as a matter of policy.
Nongovernmental Voluntary Organizations (NGOs)
There are many NGO cancer advocacy and support organizations across the United States that are active at regional or state levels. The ACS is now an approximately 1 billion dollar per year organization, with national local, regional, state, and local organizational features. ACS has a collaborative approach to cancer control and, in most states, is a key partner in cancer coalition activities. ACS is a provider of cancer patient support services but also is engaged in cancer control applied research, in policy formation, and in capacity development. ACS has partnered with CDC to institute state cancer control leadership development training. Teams of leaders representing the many sectors in cancer coalitions are trained together as teams to conduct both planning and programming in cancer control. Other NGO cancer voluntary organizations of importance in cancer coalitions include cancer site-specific organizations such as the Susan G. Komen Foundation and the Avon Foundation, and mission-specific organizations such as the LAF. The LAF has had mostly a national impact via successful publicity on cancer survivorship and rehabilitation tied to Lance Armstrong’s personal story, but in addition it is now creating regional impact by creating LIVESTRONG™ Centers of Excellence in cancer survivorship at selected cancer centers across the United States (now in New York, Boston, Denver, Los Angeles, and Seattle).
Table D.4-2 summarizes the critical strengths and weaknesses of se-
lected organizations in terms of their potential to impact problems of cancer survivorship such as cancer survivorship planning.
How Might Cancer Survivorship Plans Be Regionally Instituted?
Cancer survivorship planning could most quickly have regional and statewide impact if it were to be instituted as part of a state’s comprehensive cancer control program. A successful process would need to engage health care providers, however, much more than is currently the norm in cancer control programs. Following a process to add specific objectives and strategies into existing cancer plans could bring together cancer coalition partners in states who have in the past expressed only general needs for addressing the needs of cancer survivors, without specific measurable objectives. The initial objectives would likely not be statewide adoption of cancer survivorship planning, but they could be phased objectives to first implement demonstration projects, evaluate them, and then disseminate the practice. The principal function of a planning (goal setting) phase might be to engage regional partners to envision the possibilities of a set of demonstration projects in which cancer survivorship planning could be developed and implemented in different ways, and evaluated in terms of patient and provider satisfaction as well as other outcomes. Alternative ways can be assessed to develop cancer survivorship plans, to deliver them to patients, and to then navigate (or not) patients through recovery and long-term survival. Outcomes can be assessed in many domains, including cost-effectiveness. The rudimentary coverage of cancer survivorship issues by most state cancer plans is evidence for some preexisting dialogue between planners, public health-oriented professionals, and health cancer care providers. Reconvening these partners around the specific proposal to conduct demonstration projects might be welcome in many states. A critical issue, of course, will be the time and resources needed to conduct and evaluate demonstration projects of this type. Those issues are discussed in the section that follows.
Recommendations
The IOM report From Cancer Patient to Cancer Survivor: Lost in Transition makes important recommendations related to cancer survivorship planning:
-
Recommendation #1 calls for health care workers, patient advocates, and others to “… act to ensure the delivery of appropriate survivorship care.”
TABLE D.4-2 A Summary of Selected Strengths, Weaknesses, and Opportunities Faced by Various Types of Organizations in Affecting the Uptake of Cancer Survivorship Planning in Regions
-
Recommendation #2 deals specifically with survivorship planning: “Patients completing primary treatment should be provided with a comprehensive care summary and follow-up plan that is clearly and effectively explained. This Survivorship Care Plan should be written by the principal provider(s) who coordinated oncology treatment. This service should be reimbursed by third-party payors of health care.”
-
Recommendation #5 calls for CMS, NCI, and others to “… support demonstration programs to test models of coordinated, interdisciplinary survivorship care….”
-
Recommendation #6 states that “Congress should support the Centers for Disease Control and Prevention (CDC), other collaborating institutions, and the states in developing comprehensive cancer control plans that include consideration of survivorship care, and promoting the implementation, evaluation, and refinement of existing state cancer control plans.”
Based on these recommendations, and in light of the regional organizations and opportunities reviewed above, the following specific recommendations are proposed:
1. Add cancer survivorship planning into to state cancer plans. Although the cancer planning process has been long for many states, and although most state plans target specific years for outcomes (e.g., 2010, etc.), states are able to add additional objectives to their plans at any time. Planning is, of course, not the same as action, but planning can serve to bring together sectors that otherwise seldom interact. In this instance, the planning process can energize the dialogue between professionals with public health skills in population science, behavioral science, and evaluation, with health care providers who are skilled in managing patients with cancer. Suggested objectives for the implementation of demonstration projects in cancer survivorship planning could be developed by an independent source, such as the CDC-LAF partnership, or they could be developed by some lead states, and then shared with other states. The planning process need not be lengthy. The critical need to move through planning and into implementation of demonstration projects will be to identify sufficient funding to support the work. Funding could come from various sources, but NGOs and foundations tied to health care systems might be well positioned to provide support for this type of work. With the engagement of state cancer coalitions in the demonstration phase of this work, state coalitions would then be ready to move toward statewide dissemination in the next step. Ongoing needs in state cancer coalitions are to close the gap between the public health and the clinical care sectors, and to create more independence from state departments of health. Cancer survivorship planning, if
properly supported and independently funded, could serve to accomplish both of these needs.
2. Develop business models and support structures to provide widespread support for cancer survivorship planning should demonstration projects be successful. If the demonstration projects show that the survivorship care plans provided to patients do, indeed, lead to reduced confusion, improved compliance with follow-up recommendations, and improved quality of life for long-term cancer survivors, then it will be important to develop mechanisms of widespread dissemination of this type of service. The providers who partner to demonstrate and evaluate this service will likely not be representative of all providers. A business model needs to also be developed to make cancer survivorship planning become as easy and as widespread as possible, with both time efficiency and cost efficiency in mind. Eventually, it is likely that plans could be developed in partnerships between providers and businesses, using web-based methods, and with standardized methods for patient communication and evaluation. This business model could be developed even during the demonstration phase of work, as a Small Business Innovation Research (SBIR) grant from NCI.
3. Include measures of cancer survivorship in current public health surveillance systems as well as in health care systems. Cancer registries are already following patients for outcomes of recurrence and mortality, and special studies have shown that it is very feasible to also monitor quality-of-life outcomes after cancer treatment. Cancer registries could begin to systematically monitor cancer survivorship outcomes and needs such as fatigue, pain, the use of support systems, and satisfaction with care. This information would then inform statewide efforts and priorities in cancer survivorship systems. Through the support CDC provides for both comprehensive cancer control and state cancer registries, this type of outcome assessment could be supported first as special studies, then as core activities once cost-effective methods are determined. The Behavioral Risk Factor Surveillance System could also be used to monitor needs of long-term cancer survivors in each state. Either based on direct responses of cancer survivors who happen to be sampled, or (more likely) snowball sampling within families or acquaintances, the experiences and issues faced by cancer survivors in states could be systematically assessed.
Health care systems are increasingly conducting routine patient satisfaction surveys. Systematic surveys of cancer patients under care and of those who have been released from care could monitor performance of systems in meeting cancer survivors’ needs. The IOM recommendation for the State of Georgia specifically calls for surveys of pain control, but in fact many other problems could be monitored in this way, including fatigue, confusion with recommendations, adherence with recommendations, and behavioral changes, as well as satisfaction with health care services.
REFERENCES
1. IOM (Institute of Medicine) 2006. From Cancer Patient to Cancer Survivor: Lost in Transition. Hewitt M, Greenfield S, Stovall E, eds. Washington, DC, The National Academies Press.
2. IOM (Institute of Medicine) 2003. Fulfilling the Potential of Cancer Prevention and Early Detection. Curry S, Byers T, and Hewitt M, eds. Washington, DC, The National Academies Press.
3. http://www.cancercontrolplanet.cancer.gov.
4. IOM (Institute of Medicine) 2005. Assessing the Quality of Cancer Care: An Approach to Measurement in Georgia. Eden J and Simone J, eds. Washington, DC, The National Academies Press.
5. CDC (Centers for Disease Control and Prevention) and LAF (Lance Armstrong Foundation) 2004. A National Action Plan for Cancer Survivorship: Advancing Public health Strategies. Atlanta, GA: CDC.
6. McDavid K, Schymura M, Armstrong L, Santilli L, Schmidt B, Byers T, et al. Rationale and design of the Breast, Colon, and Prostate Cancer Patterns of Care Study by the National Program of Cancer Registries. Cancer Causes and Control 2004;15:1057-66.
7. http://www3.cancer.gov/cancercenters.
8. Medicare Quality Improvement Organization Program Priorities. CMS, DHHS, January, 2006. Accessed via www.MedQIC.org.
Appendix D.5
Cancer Survivorship Care Planning: An Evaluation and Research Agenda
Craig C. Earle, MD, MSc
Harvard Medical School
Center for Outcomes and Policy Research
Dana-Farber Cancer Center
Introduction
The recent Institute of Medicine (IOM) report From Cancer Patient to Cancer Survivor: Lost in Transition recommended that “survivorship care plans” be created for patients as they complete primary therapy for cancer in order to ensure clarity for all involved about patients’ diagnoses, treatment received, and plan for surveillance. The survivorship care plan should explicitly identify the providers responsible for each aspect of ongoing care and give information on resources available for psychosocial and other practical issues that may arise as a result of the prior cancer diagnosis. Creation of such a document would likely require a dedicated “off-treatment” or “transition” consultation in most cases. The IOM stated that such survivorship care plans “have strong face validity and can reasonably be assumed to improve care unless and until evidence accumulates to the contrary.” This may be true, but it was an unusual step to make such a strong recommendation in the absence of much evidence. The logistics and resources required to implement survivorship care planning are nontrivial. If evidence eventually does not support their use, a lot of time, money and effort will have been wasted. Therefore, it is incumbent on the health services research community to quickly yet rigorously evaluate each element of the survivorship care plan and the effects, both good and bad, of its implementation.
The theory implicit in this focus on optimizing the transition from cancer patient to survivor is that if treatment summaries and survivorship
care plans become part of standard practice and included in the medical record, they can facilitate communication among providers about the treatments patients have received and what the known toxicities have been, while also providing information as to the late effects they should be on the lookout for. Cancer care is often fragmented among many different specialists, and there has traditionally not been adequate communication back to primary care physicians (PCPs), for example, of such basic information as the specific diagnosis, stage, and treatment received. Moreover, the lack of clear practice guidelines for survivors creates uncertainty about what, if anything, nonspecialist providers should be doing to help follow cancer survivors. Survivorship care plans would provide clear direction about what should be done for a given patient and who should do it. Moreover, if standardized and available in electronically searchable formats, they may also assist broader efforts to monitor care patterns and evaluate the quality of care delivered.
Barriers to achieving the IOM’s vision of survivorship care planning include: reaching consensus about what information these summaries should contain; making it feasible for busy oncologists to take the time to create them carefully; changing the oncology culture so that treatment summaries become part of expected practice; and educating patients about the potential benefits of such planning in order to maximize adherence to its content. Clearly, the summary described in Table D.5-1 would be a labor-intensive undertaking. On a larger scale, there are already manpower concerns in the oncology workforce brought about by the aging population, improved cancer therapeutics, and previous policy decisions limiting the training of specialist physicians. Spending more time on survivorship means there will be fewer available person-hours to care for patients with active cancer.
This review will not address the critical role of basic science research to elucidate such things as the mechanisms of long-term and late effects, and will not get into specific questions regarding surveillance for particular cancers. Rather it will focus on the general health services research questions around evaluating the implementation of various aspects and models of survivorship care planning at the point of transition from active cancer therapy.
Evaluation of Survivorship Care Plans
It is essential that we conduct rigorous systematic studies to see what works and what does not work in survivorship care planning. Table D.5-2 outlines key elements to be considered when envisioning such studies. Most study hypotheses or research questions related to survivorship care planning would be based to some extent on the notion that an element or elements of the care plan affect(s) one or more outcomes. The essentials of
TABLE D.5-1 The Institute of Medicine Survivorship Care Plan
|
Upon discharge from cancer treatment, including treatment of recurrences, every patient should be given a record of all care received and important disease characteristics. This should include, at a minimum:
|
|
Upon discharge from cancer treatment, every patient and his/her primary health care provider should receive a written follow-up care plan incorporating available evidence-based standards of care. This should include, at a minimum:
|
|
SOURCE: IOM Report: From Cancer Patient to Cancer Survivor: Lost in Transition, Box 3-16, pp. 152-3, adapted from the President’s Cancer Panel (2004). |
TABLE D.5-2 Constructing Studies to Evaluate Survivorship Care Plans
|
Care plan element |
Outcome |
Population |
Setting |
Format of the Care Plan |
Study Design |
|
Patient-level
|
|
|
|
|
|
|||||
|
|||||
|
Systems-level
|
|||||
|
the majority of research proposals could be summarized by describing the study design, population to be studied, the setting in which the care plan would be created and disseminated, and the format of the care plan or care plan element being evaluated. A hallmark of this research is its emphasis on understanding the integration and interaction of multidisciplinary domains. Based on these considerations and what is already known about the situation in question, an appropriate study design can then be chosen.
Care Plan Elements
The survivorship care plan as described by the IOM is a comprehensive proposal that was arrived at by expert opinion. One can take it for what it is and design evaluation exercises around implementation of the entire plan, or evaluate different parts of the plan in different settings. Some studies would be designed to ask focused questions about a particular element of care planning in a specific population and setting, while others could look at the overall effect of care planning on such outcomes as communication and coordination of care. Although the IOM provided guidance on the elements of the ideal survivorship care plan, there is still much content to be developed and many ways that the same information can be presented. Moreover, resource guides need to be created for issues such as employment and insurance in which medical providers are often not expert. What is outlined below is a discussion of the elements of study design that would contribute to the evidence base to support or refute the inclusion of individual components of the IOM’s broad call to implement survivorship care planning as a standard of care in oncology practice.
Treatment Summary
While some specialists, by virtue of carrying out discrete treatments, routinely create summaries of their own therapies (e.g., operative notes or radiation completion summaries), there is usually not in common practice today an overall summary of cancer-related interventions and effects at the conclusion of primary cancer therapy. Whether the creation of such a document is beneficial is an open question, though. It would seem obvious that it would facilitate care; however, it could be that the treatment summary is superfluous for a straightforward clinical situation that is consistently managed in a very standard way. An example might be early-stage colon cancer treated with surgery alone: not much more needs to be known as even the histology is expected to be uniform and late effects uncommon. On the other hand, it can be crucial to understanding the risks faced by a patient with lymphoma who received multimodality therapy. The general utility of treatment summaries and their feasibility in terms of collation of informa-
tion and the resources required for their creation need to be determined in specific clinical situations.
Possible Clinical Course
Several elements of the survivorship care plan can be summarized as being descriptions of the possible clinical course a patient will take. This includes estimating the time frame over which acute toxicities would be expected to subside, long-term effects that would not be expected to substantially improve, and/or late effects that could occur at some time in the distant future. It would also include advice about what signs and symptoms could portend a relapse and should prompt medical attention. Such information can be useful in alerting patients and providers to things that might not otherwise be recognized as being related to the antecedent cancer. Hopefully such recognition would lead to earlier intervention that could improve outcomes. On the other hand, they could also lead to increased anxiety and overinvestigation. Consequently, the optimal way to provide such information and the effects, both good and bad, of raising this awareness needs to be considered in a research program.
Surveillance Plan
Surveillance for recurrence: Recommendations for surveillance for cancer recurrence are unique to each type of cancer, stage, disease histology, and the presence of any suspected genetic predisposition. They are generally thought to be important because of an expectation that they can affect survival. However, they are often controversial. Surveillance of the primary tumor site can in some cases detect salvageable local recurrences, for example, in anal, rectal, and breast malignancies. For disease that has spread beyond the primary site, there are some cancers, like colon cancer, renal cell carcinoma, and some sarcomas in which a small proportion of patients who recur distantly with oligometastatic disease can undergo surgery for possible cure. In many situations, however, there is not even a plausible rationale to intensely monitor asymptomatic patients in order to find incurable distant metastases, as it has not been shown in most cancers that palliative chemotherapy in asymptomatic patients is advantageous.
Surveillance research presents several methodological challenges. Randomized trials are required because nonrandomized studies are susceptible to lead-time and length-time biases. Randomized trials are logistically difficult and expensive to carry out, however, because they have to be very large to detect usually small differences in survival. Furthermore, what is tested is generally a complex strategy, and so the chosen components, frequency, and the duration of surveillance are open to challenge. Moreover, differ-
ences in overall survival outcomes may be lessened by ever improving treatment for relapsed disease. In the absence of high-quality evidence, there is in most cases little agreement about surveillance recommendations among experts.1 Consequently, further discussion of specific issues in surveillance for recurrence is beyond the scope of this manuscript.
Surveillance for late effects of treatment: Long-term effects are those that first occur during cancer treatment and persist after completion of primary therapy. An example would be scarring from surgery. Late effects, on the other hand, are toxicities that are not apparent during primary treatment but that manifest clinically some time later, such as second cancers from radiation or chemotherapy. Specific late effects vary greatly depending on the site of disease and treatment modalities involved. Surgery and radiotherapy are local treatments and so their long-term and late effects are mostly confined to the structures in and around the primary tumor, although there can also be systemic effects from removal or destruction of an endocrine gland or the spleen. On the contrary, the effects of systemic therapy are related to the specific drugs involved. The challenge when following cancer patients is to recognize potential problems related to their prior cancer treatment, but still to monitor and investigate symptoms judiciously. Cancer survivors, like the rest of us, are aging and will develop other comorbid conditions. It is important to understand whether survivorship care planning can help increase the likelihood of appropriate workup of symptoms that may portend cancer recurrence or treatment late effect while not causing overly aggressive investigation of vague unrelated symptoms.
Psychosocial Issues and Resources
The challenges of cancer survivorship go beyond physical issues. It can affect interpersonal relationships in many ways and raise concerns related to insurance, employment, and finances. The IOM report suggests that the survivorship care plan include information on these possible effects and recommends referrals for assistance where possible. It is reasonable to question how much of this need is currently going unfulfilled, and whether proactive identification of these problems is actually able to result in better resolution. For example, can we really improve their employment situation? Are the necessary services widely available, or is the recommendation for something that cannot practically be implemented in many settings? Is provision of cancer-related resources and information in the form of web addresses and telephone numbers enough? It seems likely that if we could ensure that survivors know their rights and put them in contact with available help, they will do better in these areas, but this is an empirical question.
Lifestyle Recommendations
The end of primary treatment for cancer has been called a “teachable moment.”2 This recognizes that with significant events in a patient’s life, there is a greater opportunity than at other times to have an impact on health with programs that have been shown to help change risk behaviors. As a result, a comprehensive survivorship care plan should include specific recommendations about things that survivors can do to reduce the risk of cancer recurrence (chemoprevention), second primaries (e.g., diet, exercise, stopping smoking), or of developing other unrelated diseases (e.g., immunizations) now that their cancer is cured. Collecting data on how best to operationalize this recommendation and its effect on altering behavior is important to justify expending this effort at the already overwhelming time of transitioning from cancer treatment.
Outcomes
There are several outcomes on which survivorship care planning can have an impact. Most can be assessed using existing measures, but development and validation of instruments able to capture important constructs specific to the survivor population will likely be necessary as well. The challenge in designing research is to choose end points that are going to be responsive to the effects of survivorship care planning so that improvements will be feasibly detected, yet are still important enough to be worth the effort of care planning. It would be optimal for the health services research community to converge as much as possible on a set of consistent outcome measures so that separate research groups can assess different models of care and still produce results that can be compared across studies.
Knowledge and Communication
At the patient level, several elements of the care plan are designed to increase patients’ awareness of their disease and the treatment they have received. Instruments to measure such knowledge can be developed and compared with situations in which there has and has not been a care plan implemented. Similarly, the availability of this information to practitioners is a practical measure of communication among providers. Other constructs like decisional conflict, which may be decreased when patients make decisions in the setting of enhanced knowledge about their situation, could also be evaluated.
Clarity around who will be delivering various aspects of care to cancer survivors is often missing. One study found that a third of cancer survivors were not sure which physician was in charge of their cancer follow-up.3 Some
patients are aware of this and are able to take responsibility for obtaining at least some of their necessary care. Others can be empowered if made aware of what the plan should be. There will always be a proportion of patients, however, who lack the knowledge or personality to advocate for themselves. As a result, one of the most valuable features of holding cancer providers responsible for a survivorship care plan may actually be in defining explicitly which providers will take responsibility for different aspects of a patient’s care. Assessing whether the survivor and involved providers are aware of and agree on who will take on the various roles of cancer surveillance, screening for other cancers where appropriate, and noncancer and preventive care is an important end point to consider studying.
Acceptability and Satisfaction
As different methods of implementing survivorship care plans are developed and tested, the satisfaction with and acceptability of the format of care planning needs to be assessed. For example, will patients accept an off-treatment consult with a nurse practitioner in a survivorship clinic, and are they as satisfied with this as if their oncologist had done it? Will they interact with web-based applications or do they prefer written documents? There are several instruments designed to measure satisfaction that could be adapted to be relevant to questions related to survivorship care planning.
Survival
Quantity and quality of life are generally considered to be the primary outcomes of biomedical research. Survivorship care plans could affect overall survival by improving adherence to important surveillance recommendations, ensuring optimal noncancer care, and/or by causing positive lifestyle changes. It may be worthwhile to look for this in some studies, but as described above, it may be difficult to detect what would likely be relatively small survival differences in most cases, and follow-up would have to be very long.
Quality of Life
Quality of life may be affected more directly than survival by survivorship care planning. Having specific recommendations about what to do for follow-up may decrease patient anxiety and ameliorate depressive symptoms. Early identification of late effects with appropriate intervention may decrease physical symptoms and improve functional status. On the other hand, highlighting all of the long-term or late effects that are possible may actually increase distress. Perceived health and self-esteem may be improved
for some patients while others may become overly focused on their previous cancer experience, have increased fear of recurrence, and have trouble moving on with their lives. Consequently, preferences for the health state resulting from implementation of survivorship care plans may be reflected in measurable differences in utility.
Processes and Quality of Care
While not enough is known about the efficacy of treatment summaries and survivorship care plans to establish the simple fact of their creation as indicators of quality cancer care, some of the processes embedded in the care plans do have sufficient evidence base to be evaluated as measures of quality. In this way, quality of care becomes an outcome by which different models of care can be evaluated. For example, it is widely accepted that colorectal cancer survivors should undergo regular endoscopic surveillance to detect recurrence, new primaries, and/or to remove premalignant polyps. Therefore, studies comparing different “best practice models” could be evaluated to see which one produced the most adherence to this recommendation.
Health Care Resource Utilization
On the systems level, efficiency is a very important outcome. Any form of care plan implementation is going to consume resources, especially provider time. On a larger scale, health care costs may be affected in uncertain ways. For example, formal plans could decrease patient anxiety and result in fewer interval visits to physicians. Clear information about the likely course of disease and surveillance plan may avert inappropriate workup of probably unrelated symptoms by providers who are less familiar with specific cancer situations. Alternatively, survivors may seek investigation for potential problems they have been made aware of by the survivorship care planning process and would not otherwise have pursued. Also, if successful, survivorship care plans may cause patients who currently are not receiving appropriate surveillance measures to receive them, thereby resulting in increased appropriate health care utilization and costs. Hopefully these latter interventions would also improve health outcomes, however, allowing evaluation of the cost-effectiveness of survivorship care plans. A consideration when studying the economics of this is that the analytic methodology of discounting generally makes interventions like survivorship care plans that have up-front costs but benefits that often do not accrue until many years in the future appear relatively unattractive.
Population
The next consideration when designing research is to define the population to be studied. The notion of survivorship care planning applies to all cancer survivors. However, certain elements are more important for some than for others. Patients with very early-stage cancers may not need a specific surveillance plan, as the risk of relapse is vanishingly small. Lifestyle recommendations are more important for a survivor of head and neck cancer, for example, smoking cessation, than they are for a lymphoma survivor. Psychological distress may be more likely in a patient who has undergone disfiguring surgery (mastectomy or colostomy) than one who has had little long-term effect from cancer treatment. The concerns of an adolescent or young adult cancer survivor may have little in common with those of a geriatric oncology patient. The emphasis of the survivorship care plan will have to be tailored to the situation of each survivor, and as such, studies focused on the specific concerns relevant to relatively homogeneous populations of survivors will usually be most informative.
Even a study focused on a narrowly defined clinical situation will have to consider the diversity of the survivor population, however. Investigators will need to decide whether they want to study a representative sample of all patients or to focus on the priority areas of a subgroup. For example, how does the information needs of Spanish-speaking Latino survivors differ from those of white English-speaking patients? Should surveillance recommendations be modified in the presence of significant comorbidity? Is a web-based application as helpful to elderly survivors as younger ones? How does socioeconomic status affect the importance of employment and insurance assistance? Are survivorship resources accessible to survivors in different geographic locations across the country and across the continuum of urban and rural settings? Should children and adolescents be included? The tradeoffs necessary when studying defined populations involve balancing the efficacy of a care planning intervention against effectiveness and generalizability, while also considering practical matters of ease of subject recruitment and statistical power.
Caregiver Burden
Cancer survivorship affects more than just the cancer patient. There is a growing literature on the burden of cancer treatment on caregivers, and the challenges cancer survivors face can similarly affect the health and quality of life of their loved ones. As a result, it is appropriate for investigators to design studies that inquire whether survivorship care planning could affect satisfaction and health-related quality of life outcomes for caregivers as well.
Setting
There is no single organizational model that must be adopted in order to deliver high-quality care to cancer survivors. Although the National Coalition for Cancer Survivorship (NCCS) articulated the proposal that “long-term survivors should have access to specialized follow-up clinics that focus on health promotion, disease prevention, rehabilitation, and identification of physiologic and psychological problems,” in reality, whether follow-up is provided by oncologists, PCPs, or specialized survivor clinics is not the important issue. Rather, it is by ensuring that a named provider is responsible for each aspect of follow-up that the chances of quality care occurring will be maximized. In fact, the IOM’s Committee on Health Care Quality in America affirmed that “care based on continuous healing relationships” is important. In other words, patients shouldn’t necessarily be removed from the care of their treating PCPs and oncologists in order to receive specialized survivor care. In addition, other specialists may be involved, and/or a “shared care” model of cooperation between specialists and primary care physicians in the follow-up of the cancer survivors could be attempted. The logistics of implementing formal survivorship care planning would be quite different if it was envisioned to occur in an oncologist’s office, primary care practice, or specialized survivorship clinic. Therefore, in most cases, possibly with the exception of patient-driven care planning formats discussed below, investigators will have to decide and clearly specify which model they will study.
Even within a setting there are questions to be addressed about the efficiency, acceptability, and quality of survivorship care planning when it is carried out by treating physicians, allied providers such as nurses or nurse practitioners familiar with the patient, or by providers specialized in survivorship care planning but not familiar with the individual patient, as would be encountered in a specialized survivorship clinic. Few dedicated survivorship clinics currently exist, and they are all quite different. Some only take over the mechanics of surveillance, while others focus on providing primary care, especially to disadvantaged populations. Still others take on a consultative role, looking for signs and symptoms of long-term and late effects and then making appropriate referrals, as well as assisting with the transition consultation and creating a survivorship care plan. In this way, specialized clinics could help with the workload barrier; however, patients and physicians may fear losing contact with each other and so the feasibility of such a model is a question requiring study. Consequently, the fifth recommendation of the IOM report calls for funding organizations to “support demonstration programs to test models of coordinated, interdisciplinary survivorship care in diverse communities and across systems of care.”
Care Plan Format
If survivorship care planning is currently carried out at all, it is usually in the sense of informal discussions with patients near the end of treatment about what the plan will be going forward. The IOM report suggests that that should change and provides examples but does not give a specific prescription about what form the survivorship care plan should take. Simply having a consultation in which all the elements of the plan are discussed, leaving the patient responsible to write down or remember the salient points, would probably still be a large improvement over current transition practices. However, it is expected that some form of documentation of the process that can be shared with the patient and other providers would be even more successful. A written consultation note or letter will achieve some of the aims of the IOM, but because of a lack of standardization it is quite likely to miss some of the suggested elements.
Standardization of the survivorship care plan to some extent is probably desirable. Some clinics use a combination of general and tailored information to develop a plan for patients. For example, templates can have spaces for a provider to fill in the elements of a treatment summary and surveillance plan on forms preprinted with standard lifestyle recommendations and lists of available resources. There are several examples of this sort of program in individual pediatric oncology clinics, a larger province-wide program in the Canadian province of Ontario, and the patient-centered materials developed by the Lance Armstrong Foundation. Electronic and/or handwritten versions of the templates can be available as necessary and each evaluated scientifically.
Creating even a standardized survivorship care plan is time-consuming and difficult, however. Providers could attempt to create a document as they go along during the course of care, but realistically, busy oncologists are usually stretched to their limit dealing with the acute toxicities of treatment and are unable to also work consistently on posttreatment care planning. Templates could increase feasibility if nonphysician staff such as nurses or nurse practitioners could assemble much of the data. Automated systems can be envisioned in which drugs, cumulative doses of chemotherapy, and radiation sites and fractions could be pulled from pharmacy and other administrative records and fed into the evolving treatment summary. Even with standardization and automation, however, creation of a survivorship care plan will still require significant time and resources. Advocacy organizations like the American Cancer Society and Lance Armstrong Foundation have tried to support patient-directed models by providing information on survivorship issues for common cancer types and helping survivors summarize for themselves their medical treatment and plan for follow-up care. It may be that such an approach is more realistic than a physician-based model.
Another big challenge of survivor care is the mobile patient population. A wonderful care plan can be developed, but if the patient subsequently moves to a new area, changes insurers, or even just changes doctors, the information can become practically inaccessible to his/her new providers. Because of this, an important area in need of research is the evaluation of technologies that could create care plans that are truly portable and accessible from almost anywhere. Options include “smart cards” or other media that a patient could physically carry with a large amount of electronic data in a more portable form than a paper record. Another exciting possibility is web-based applications. Patients could control access to a web-based record through standard Internet security measures (e.g., passwords, USB keys). Physicians with limited electronic resources in their practices but with Internet access could contribute to and edit information for the treatment summary and care plan over the web. In this way, a patient’s plan could have input from all relevant providers. If a provider did not have Internet access, it could still provide the information for the patient or another provider to input. If the patient does not have Internet access, the final product could be printed in a hard copy version, thereby getting around the problem of disparities in electronic resources among patients that currently exist. Such formats have been implemented in some controlled settings, but their utility as population-based interventions remains to be established.
Study Design
Qualitative Research
The evaluation of survivorship care plans can involve most types of health services research study designs. Because this is a new intervention, not actually in widespread use, there is a lot of qualitative work to be done to understand the current problems in, for example, coordination of follow-up, or what the most important barriers are to implementing survivorship care planning in practice. Focus groups or key informant interviews could be undertaken with different stakeholders (e.g., survivors, oncologists, PCPs) to explore these issues and inform the design of larger quantitative studies. Case reports can increase awareness of uncommon late effects or describe anecdotal situations in which survivors may find themselves related to work or insurance.
Observational Research
If the important questions are known, observational studies can be designed to attempt to quantify and prioritize the areas of need. Cross-sectional surveys can address current practices in the various aspects of
survivorship care planning. They can be used to identify deficiencies in patients’ knowledge of their disease and its treatment, the surveillance plan, possible late effects, and resources available to them. Surveys can also be used to document the amount of communication that has taken place between the various specialists and with PCPs. Lastly, surveys can assess satisfaction and acceptability of different models of survivorship care among diverse stakeholders.
Some aspects of care relevant to survivorship planning can be observed directly rather than relying on patient or physician report in surveys. Retrospective medical record review and examination of administrative claims data are examples of noninterventional study designs that can confirm practice patterns with respect to surveillance for recurrence and management of long-term and late effects. Studies employing such methods can provide important insight into actual care delivered.
Prospective Cohort Studies
Different settings and formats for the creation and implementation of survivorship care plans can be piloted in prospective cohort studies. Such studies would generally start with a baseline measure of the outcome of interest, say, knowledge or anxiety. The survivorship care plan would then be implemented and follow-up determinations of the change from baseline would indicate whether the program was considered a success or failure. Other cohort studies would evaluate a nonrandom mix of patients who did and did not receive various elements of a care plan, allowing assessment of outcomes for hypothesis generation.
Quasi-experimental studies, in which there are both intervention and control groups but without random allocation of subjects into these groups, can also provide evidence of the effectiveness of survivorship care plans. Such studies can take the form of before/after analyses of outcomes divided at the time of implementation of a survivorship care plan program. This type of research is susceptible to secular trends in outcome, however, which could result from increasing general awareness of cancer survivorship among patients and providers. Another quasi-experimental design could be to take advantage of a natural experiment in which some constituents of a care plan are implemented for one group of patients but not for another similar group. Comparison of outcomes between these groups could provide information about the effects of these parts of the care plan.
Randomized Controlled Trials
The most powerful study design is the randomized controlled trial. Randomization can be at the level of the patient, although this may lead to
contamination as a provider may become generally more aware of the importance of planning for survivorship and bias the study toward the null by treating control patients more like the intervention patients than they otherwise would. The problem of contamination also precludes the use of crossover designs for most questions related to survivorship care planning. Alternative designs would be to randomize providers or practices, but then there may be an imbalance in characteristics of the providers in each group, or of the patients in these practices, that could affect the outcome of the study.
Given the IOM recommendation, investigators should be aware that institutional review boards may not consider it ethical to randomize patients to having no survivorship care planning and so a “usual care” intervention, rather than a placebo, may have to be devised. This could consist of tailored information rather than a formal consultation, for example. Unfortunately, providing an intervention to the control group will bias any study toward the null and necessitate a larger sample size.
Examples of Research Questions and Study Designs
-
Question: What are the practical barriers to implementing survivorship care plans in oncology practice?
-
Study Design: Focus groups with providers from a variety of settings (e.g., private practice versus academic centers, different specialties, managed care versus fee-for-service contractors). Questions could try to elicit ideas for ways to facilitate transition consultations and creation of survivorship care plans in real world settings. Key informant interviews with medical directors and practice managers may provide insight into the feasibility of programs that depend on additional investment in information technology. Estimating the resource burden of creating a survivorship care plan could inform policy decisions about reimbursement for survivorship transition consultations.
-
-
Question: In what areas do patients currently need more information: their diagnosis, previous treatment, plan for surveillance and monitoring, possible late effects, resources available, and/or who to turn to for different problems?
-
Study Design: Cross-sectional survey of survivors of all kinds to assess their current knowledge and desire for information in order to find which elements of the proposed survivorship care plan have the greatest gaps between desired and actual knowledge, and to identify subpopulations of patients in which certain needs are particularly prevalent.
-
-
Question: Is there variation in surveillance practice?
-
Study Design: Administrative data analysis of surveillance practices for patients with stage II and III colon cancer, analyzing practice patterns and outcomes by geography, provider and patient characteristics (e.g., age, sex, race, socioeconomic status), organizational and insurance structure, and whether disparities in the quality of follow-up care exist.
-
-
Question: How much does a transition consultation for survivorship care planning increase patients’ knowledge of their previous treatment and care plan?
-
Study Design: Prospective cohort study in which there is a base-line assessment of stage I–III breast cancer survivors’ knowledge of these areas just after completion of primary therapy via an interviewer-administered survey. All subjects would then have a transition consultation and be given a written survivorship care plan. Six months later another interviewer-administered survey would assess change in knowledge from baseline.
-
-
Question: What are the effects of survivorship care planning on a survivor’s family and caregivers?
-
Study Design: Prospective cohort study in which prostate cancer caregivers’ burden is evaluated over a 2-year period and related to whether the survivor received a survivorship care plan, adjusted for other explanatory variables.
-
-
Question: Does survivorship care planning decrease anxiety and depression?
-
Study Design: Before/after study in which anxiety and depression levels are measured in a cohort of patients finishing treatment for Hodgkin’s disease in a major referral center. A transition consultation and survivorship care plan is then implemented at that institution and anxiety and depression levels are evaluated for patients completing treatment in the following year.
-
-
Question: How does receipt of different parts of the survivorship care plan affect satisfaction with the transition from active cancer treatment?
-
Study Design: Analysis of data from a natural experiment in which different practices have implemented different parts of the care plan. Patients in each practice can be surveyed to assess their levels of satisfaction and differences related to the part of the care plan they received.
-
-
Question: Are transition consultations with a specialized survivorship nurse practitioner acceptable to patients?
-
Study Design: Randomized controlled trial in which head and neck cancer patients are randomized between either having a survivorship
-
-
care plan created by a specialized nurse practitioner during a consultation in a survivorship clinic or during a routine visit with their medical oncologist near the end of primary therapy, comparing measures of satisfaction between the two groups.
-
Question: Can specific interventions targeted to lifestyle changes to decrease risk behaviors be more successful in the context of survivorship care planning.
-
Study design: Randomized controlled trial in which breast cancer patients completing adjuvant chemotherapy all receive a transition consultation and survivorship care plan, but half are invited to take part in an intensive diet and exercise intervention immediately, while the other half receive the same intervention 6 months later. Acceptance, compliance, and measures of dietary and exercise improvement would be the outcomes.
-
-
Question: Does survivorship care planning decrease unnecessary health care resource utilization?
-
Study Design: Practices are randomized between usual care: giving patients individually-tailored treatment summaries, informal discussion of surveillance plans, and standard information about available resources; and an intervention group in which the survivorship care plan explicitly lays out the plan for surveillance and which symptoms should prompt medical evaluation. Data collected will include the costs associated with creating the care plan, and enumeration of physician visits and investigations received. This study could also inform cost-effectiveness analyses should improvement in survival and/or quality of life be found to be attributable to institution of such plans.
-
-
Question: Which format of survivorship care plan is most effective at increasing communication among providers?
-
Study Design: Practices are randomized between web-based and paper versions of the survivorship care plan (with copies sent to all involved physicians). Survivors’ PCPs are later asked to answer basic questions about the survivor’s cancer and its care, using records available in their office.
-
Conclusion
Over time, as studies evaluating the effects of survivorship care planning on relevant outcomes are carried out, they would serve as the basis for secondary data analyses such as systematic overviews and technology assessments. Surveillance practices have already been the subject of several meta-analyses and decision analyses but this is only one component of care
planning. Rigorous efficacy and effectiveness data would lead to the development of evidence-based clinical practice guidelines for survivorship care planning (the IOM report’s third recommendation), thereby creating standards of care. From such standards, quality indicators related to survivorship care (promulgated in the fourth recommendation of the IOM report) could be identified and validated. This would spawn a field of inquiry related to access to care and disparities for different survivor populations. The fifth recommendation in the IOM report calls for funded demonstration programs to test models of care, and the final recommendation advocates that public as well as private agencies such as insurance plans should increase their support of survivorship research and expand mechanisms for its conduct. This last recommendation is actually the first step in all of this, however, as establishing an evidence base for the creation and implementation of survivorship care plans through the type of research outlined herein is necessary to realize the IOM’s vision in which attention to the transition from cancer survivor to cancer patient is accepted as a routine part of oncology practice.
REFERENCES
1. Johnson FE: Overview, in Johnson FE, Virgo KS (eds): Cancer Patient Follow-Up. St. Louis, Mosby, 1997, p. 4.
2. Ganz PA: A teachable moment for oncologists: cancer survivors, 10 million strong and growing! J Clin Oncol 23:5458-5460, 2005.
3. Miedema B, MacDonald I, Tatemichi S: Cancer follow-up care. Patients’ perspectives. Can Fam Physician 49:890-895, 2003.