2
Suvivorship Care Planning
IMPLEMENTING THE SURVIVORSHIP CARE PLAN
Presenter: Dr. Patricia Ganz
As the Institute of Medicine (IOM) committee finished its deliberations on recommendations for the report From Cancer Patient to Cancer Survivor: Lost in Transition, there was a perception that the benefits of implementing the Survivorship Care Plan would be so obvious that everyone would jump on the bandwagon to make it happen. This rapid adoption may occur, but some effort to facilitate implementation is likely to be necessary. Overcoming some of the challenges and barriers to implementation is critical because survivorship care planning is a sentinel project in the drive for quality cancer care.
A key message of the report is that the needs and concerns of the large and growing number of cancer survivors cannot be ignored. The report also raised awareness of cancer as a chronic condition that requires long-term monitoring for its aftereffects and sequelae. That cancer increasingly involves long-term maintenance therapy is another chronic-care feature of the disease, not too unlike diabetes. Also documented in the IOM report is the problem of poor coordination of care and, as the title of the report indicates, the fact that cancer survivors are often “lost in transition.”
Why is cancer different from other chronic diseases? Cancer is a very complex set of diseases, and treatments are often multimodal, involving a multidisciplinary team of providers. The treatments themselves are toxic
and expensive, and very often care is poorly coordinated. Cancer treatment is often provided in isolation from other care, even though cancer patients tend to be elderly, with multiple comorbidities and health care needs. Oncology professionals at the onset of treatment provide some initial communication to the primary care physician, but during treatment such contact may decline. Given the demands of cancer treatment, most patients do not have time to see their primary care physician, and consequently cancer treatment may seriously disrupt patients’ routine care and distance them from the care system to which they will have to return following their treatment.
The development of evidence-based guidelines has been impeded by the lack of research on the late effects of cancer therapy. The American Society of Clinical Oncology (ASCO) is developing guidelines for many important domains of survivorship care, but it has often had to rely on descriptive cohort studies as an evidence base. Even in the childhood cancer arena, in which survivorship issues have long been recognized, there are few studies on which to base guidelines. Support for research in this area is needed to advance understanding of cancer’s late effects.
Follow-up care plans, to the extent that they have been developed and used, do not have a standard format and have focused on surveillance for recurrence. ASCO has developed guidelines for breast and colorectal cancer that include recommendations for follow-up for recurrent disease. These guidelines, however, do not deal with other complex and multidimensional issues facing survivors. Absent from most guidelines, for example, is information on health promotion and disease prevention. As cancer survivors live longer, they will need comprehensive health care that includes preventive services to address their cancer and other chronic conditions. In the area of infertility, which is a concern of many cancer survivors, many patients have been told, “You should be happy just to be alive.” In this example, potential late effects need to be addressed during treatment planning to help ensure that individuals make informed choices and have an opportunity to lead full, normal lives to the extent possible.
Why does cancer care present such a challenge? Health services researchers engaged in cancer-related quality of care studies find that they have to request as many as three to five medical charts to examine the content of an episode of care. Cancer treatment is often prolonged and may occur in numerous outpatient and inpatient settings, some of which are specialized treatment facilities. There may be very limited communication among the treating physicians, and each of the multiple medical records may document only a portion of the treatment history. In large urban areas, patients may be operated on at one institution, have their chemotherapy at an oncologist’s office, have radiation therapy at another institution, and then see a primary care physician somewhere else. Cancer care can be very
complicated, and with no electronic records and limited communication, achieving integrated coordinated care can be very difficult.
How can one address this challenge? There are many solutions on the horizon. Integrated electronic medical records will be helpful if somebody is cared for within one system but, as previously mentioned, many patients are in and out of different care settings, often with incompatible information systems. Patient navigators can help patients with communication and coordination of care to ensure completion of the recommended treatment. Posttreatment consultation planning and counseling may also help, but issues that are salient at the end of treatment may not be fully addressed at the outset. None of these strategies is widely available for patients receiving active treatment today. Transition care planning is needed to address issues of coordination of care and quality of care throughout the care trajectory.
Why is survivorship care planning needed, and why is it so vital now? The Survivorship Care Plan is a vehicle that summarizes and communicates what transpired during cancer treatment. It is, in some respects, similar to a hospital discharge summary. Imagine someone being discharged from the hospital without a discharge summary. Whether it is a short or long hospital stay, it would be very cumbersome and time-consuming for the primary care provider responsible for postdischarge care to review the hospital chart to learn what went on during the stay and to divine the care plan for his or her patient. Providers are not reimbursed for preparing the hospital discharge summary, yet completing them is legally required. This obligation to document is inculcated into students throughout medical training. In an analogous fashion, it makes common sense for treating physicians, at the conclusion of treatment, to summarize and document the episode of cancer care.
The Survivorship Care Plan also needs to be prospective and record the known and potential late effects of cancer treatments with their expected time course. This may be very challenging because, as mentioned, there is a paucity of follow-up data for some treatments. More importantly, though, oncologists need to communicate to the survivor and to the other health care providers not only what has been done, but also what needs to be done in the future. This prospective plan is especially important in light of the mobility of the patient population, as well as the difficulty in retrieving older records. If patients were routinely given a formal document at the end of treatment that explained what went on, both in technical and lay terms, it would help them wherever they went and wherever they sought later care. This record could be updated fairly easily if there were such a foundation document.
As envisioned, the Survivorship Care Plan would also function to promote a healthy lifestyle to prevent recurrence and reduce the risk of other comorbid conditions. A summary document with a recommended follow-
up plan completed at the conclusion of treatment gives patients an opportunity to take some responsibility for their care and may help to ensure adherence to follow-up recommendations. If patients move or go to a new primary care physician, the Survivorship Care Plan becomes the blueprint for future care.
The Survivorship Care Plan described in the IOM report incorporates recommendations from other IOM reports. The IOM, in its call for quality care, has promoted the ideal of: (1) continuous healing relationships between patients and providers; (2) customization of care based on patient needs and values; (3) the patient as the source of control; (4) shared knowledge and the free flow of information; (5) use of evidence-based decision making; (6) safety as a system property; (7) the need for transparency, and, thus, communication among all involved; (8) anticipation of needs; (9) a decrease in waste; and (10) cooperation among clinicians.1 Survivorship care planning helps everyone know what needs to be done and who is going to be in charge of the various aspects of a person’s care. Such planning helps to avoid the fragmentation of the surgeon’s doing one thing, the radiation therapist’s repeating it, and the primary care physician’s not knowing if anything was done and doing it again. Having a care plan and a clear sense of assigned responsibility, with the patient or survivor as the custodian of the document, could potentially lead to substantial improvement in care efficiency.
Figure 2-1 illustrates the place of survivorship care in the cancer care trajectory. Patients may cycle out of survivorship care back into treatment again, but the focus is on patients who are being managed either with chronic or intermittent disease or who have long-term cancer-free survival and need a prospective plan of care.
The IOM report identified key elements that should be included in the Survivorship Care Plan:
-
Specific tissue diagnosis and stage;
-
Initial treatment plan and dates of treatment;
-
Toxicities during treatment;
-
Expected short- and long-term effects of therapy;
-
Late toxicity monitoring needed;
-
Surveillance for recurrence or second cancer;
-
Who will take responsibility for survivorship care;
-
Psychosocial and vocational needs; and
-
Recommended preventive behaviors/interventions.
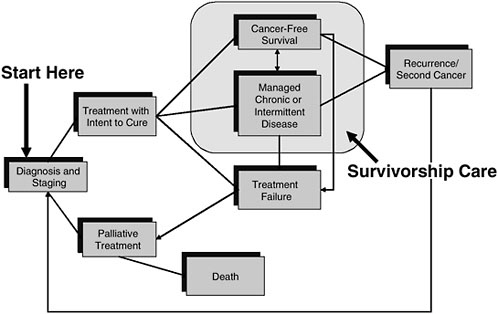
FIGURE 2-1 Cancer care trajectory.
NOTE: Palliative care is provided throughout the cancer care trajectory
SOURCE: Adapted from IOM Committee on Cancer Survivorship, 2006. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press.
Implementing such comprehensive care planning presents challenges to providers, and some may judge the IOM recommendation premature given the state of the evidence. Evidence is beginning to emerge on the value of this kind of care planning, or guided care, after patients complete their primary treatment.
Eva Grunfeld is a family physician who has conducted a number of randomized controlled trials to test whether primary care or family physicians provide the same quality care as oncologists to patients—in this case, breast cancer patients—after their initial treatment. She performed a randomized controlled trial most recently in Canada in which half of the women who were approached agreed to participate. Family physicians did as good a job as oncologists in terms of detecting recurrences, and women’s satisfaction with care and assessment of quality of life did not vary by whether they received follow-up care from their family physician or oncologist.2 A one-
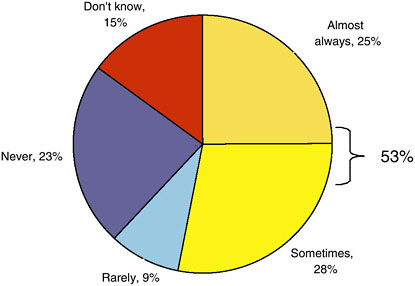
FIGURE 2-2 Primary care physicians receiving end-of-treatment summaries from oncologists.
SOURCE: Ganz presentation of information adapted from BlueCross of California, 2006.
page follow-up guideline was given to the family physician, similar to the Survivorship Care Plan under discussion, telling the physician exactly what to do, and when told, these family physicians performed as well as oncologists. This is a very nice piece of evidence to support survivorship care planning.
Dr. Ganz reported experience working with BlueCross of California to develop a course on the primary care physician’s role in the care of cancer survivors. BlueCross of California conducts regular surveys of primary care physicians, and, in anticipation of the course, a few questions about survivorship care planning were added to the survey. The survey was fielded at about the time of the IOM report’s release (November 5, 2005). The response rate was very low (5 percent), so the results should be interpreted with caution. Among the 75 respondents, only 25 percent said that they “almost always” received a detailed end-of-treatment summary from the oncologist treating their patients (Figure 2-2). An additional 28 percent said that they “sometimes” received such a summary. Therefore, about half of the primary care physicians reported either not receiving, rarely receiving, or not knowing whether they received care summaries at the end of treatment.
The primary care physicians were also asked two additional questions: “How prepared are you to monitor and manage your patients’ late health effects that may arise as a result of the therapeutic exposures used during
cancer treatment?” and “How prepared are you to handle transition-of-care issues for your patients after discharge from cancer treatment, including communication with oncology providers?” Only 33 percent of the primary care physicians felt “very prepared” for managing the late health effects, and 41 percent felt “very prepared” about the transition care (Figure 2-3).
Notably, there was an increased perceived ability to manage the late health effects and the handling of transition issues when providers had received end-of-treatment summaries from oncologists (Figure 2-4).
According to this small convenience sample of primary care physicians, confidence in managing cancer survivors’ care increased when treatment summaries were available, but oncologists are not routinely sending such summaries to them. The quality of the treatment summaries sent to these primary care physicians was probably somewhat limited, but even so, they did appear to make a difference in how competent primary care physicians felt in terms of following up their survivors. Again, the numbers were small and the physicians participating are not likely to be representative of the population of BlueCross primary care providers in California, but the findings lend some credence to the value of survivorship care plans.
An example of a Survivorship Care Plan is shown in Box 2-1. This care plan was drafted for use in IOM’s qualitative research (Chapter 3) and should be considered a work in progress. It is likely to be modified for use on
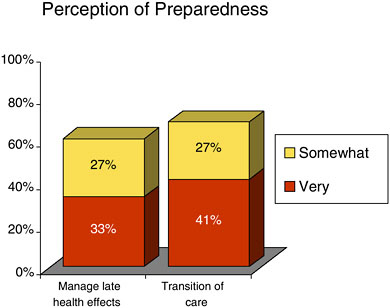
FIGURE 2-3 Primary care providers’ confidence in managing cancer patients’ late health effects.
SOURCE: Ganz presentation of information adapted from BlueCross of California, 2006.
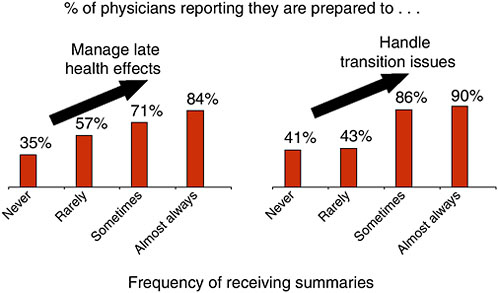
FIGURE 2-4 Relationship between confidence of the primary care physicians in managing cancer patients’ late effects and receipt of an end-of-treatment summary.
SOURCE: Ganz presentation of information adapted from BlueCross of California, 2006.
the basis of the results of the qualitative research and the experience of others who are testing these templates. The plan describes treatment and follow-up for a relatively young man with stage III colon cancer with lymph node involvement. The treatment summary portion of the plan documents the treatment he had, his surgery, the kind of staging studies that were performed, and the results of recent tumor marker tests. The summary lacks some details of treatment, but it is felt to provide appropriate general information for a primary care physician. Essential to communicate to primary care providers is information on what they need to be looking for and what management issues need to be addressed. To foster communication, the Survivorship Care Plan would be maintained in the oncologist’s medical record, sent to the primary care physician, and shared with the patient.
As described in the sample care plan, the patient has high-stage cancer with increased risk of recurrence, which puts providers on alert that this individual has to be under good surveillance. The care plan also outlines what symptoms the patient should report if he experiences them (e.g., blood in the stool, abdominal pain, changing bowel habits). In terms of necessary medical assessments, he needs to be seen every 3 to 6 months for the first 3 years after primary treatment and then every 6 months for years 4 and 5. This schedule and the specification of recommended tests and imaging studies are based on the ASCO guideline. The care plan recommends genetic counseling due to his
|
BOX 2-1 Sample Cancer Survivorship Care Plan
CANCER TREATMENT SUMMARY Colorectal Cancer Diagnosis: Date of tissue diagnosis of cancer: 7-15-05 Stage of cancer: III Lymph node involvement Pathologic findings: high grade cancer arising in a large polyp, 3 of 10 nodes positive Diagnostic tests done: dates and results Colonoscopy: 7-1-05, obstructing lesion at hepatic flexure CT scan Chest: no mets CT scan Abdomen: enlarged mass in right colon, no liver mets CT scan Pelvis; no abnormalities Pre-operative and Post-operative serum CEA levels (dates and results): 7/5/05 10; 8/15/05 3.9 Last CEA 2.0 on 3-10-06
Risk of cancer recurrence and second cancer: Patient has high-stage cancer with increased risk of recurrence. |
||||||||||||||||||||||||||||||||||
|
Patient should report these signs and symptoms if persistent: Blood in stool, abdominal pain, change in bowel habits, cough that doesn’t go away, bone pain, new lumps, nausea, vomiting, loss of appetite, weight loss, fatigue Recommended surveillance to detect recurrence/second cancer (specify frequency):
Potential late effects of treatment (e.g., cardiovascular, skeletal): Surgery: Bowel problems, such as diarrhea, fecal leakage/incontinence, constipation, bowel obstruction, hernia, pain, psychological distress Chemo/Biotherapy: fatigue, peripheral neuropathy Patient should report these signs and symptoms if persistent: Diarrhea, constipation, pain with urination, erectile dysfunction, painful intercourse, infertility, numbness or tingling in hands or feet Recommended surveillance for late effects of treatment(s): monitor for recovery of peripheral neuropathy Preventive care recommendations (e.g., osteoporosis prevention, weight management, smoking cessation, diet): This patient needs counseling about smoking cessation and weight loss. |
|
Physician(s) who will monitor recurrence/second cancer, late effects, and preventive care: Dr. Adams will monitor for late effects and preventive care recommendations. Dr. Jones will monitor CEA and do endoscopy and imaging studies at prescribed intervals.
|
||||||||||||||||||||||||||||||||||||||||||||
young age and family history. Under the section on late effects, the care plan specifies potential surgical and chemotherapy complications and, in addition, any other signs or symptoms that could be related to treatment, including sexual dysfunction and peripheral neuropathy. The care plan also addresses lifestyle issues. This particular patient was a smoker and is overweight, and so health promotion and disease prevention action items are included, along with a delineation of who should take charge of monitoring these interventions. As indicated on this care plan, the oncologist assumes responsibility for some of the cancer-related surveillance issues, while the primary care physician takes care of monitoring for late effects and prevention counseling and interventions.
What are the barriers to routine generation of treatment summary and survivorship care plans? There are some specialties, for example surgery and radiation oncology, that routinely create an operative note or radiation treatment summary note. That has not been the case in medical oncology, perhaps because as recently as the early 1970s, oncologists did not have as much to offer patients. With current treatment modalities, many more cancer patients are surviving, but the treatments have become very complex. In addition, most medical oncology care occurs in the outpatient arena.
Oncologists report that they have very busy practices, lack time, and do not get reimbursed for this type of service. This may be a perception rather than a reality, and there may be ways to overcome these impediments by designing efficient mechanisms for preparation of treatment summaries and survivorship care plans. Efficiency will be essential, given the number of cancer survivors that are cared for in oncology practices. Completing the care in real time when people are finishing their treatment should make the task less burdensome.
Another potential barrier to survivorship care planning is a lack of awareness on the part of oncologists that cancer survivors are lost in transition, that survivors want this service, and that care planning may help patients take charge of their care. Oncologists also need to appreciate that primary care physicians can be actively involved in providing follow-up care.
How can the Survivorship Care Plan be used in practice? The care plan should facilitate an end-of-treatment consultation with the patient, including a discussion of specific follow-up recommendations. Even if the patient does not want to hear everything about late effects at that point in time, the information will be available in this document. Patients face many issues at the end of treatment, and they may not be able to hear or digest all of the information in the care plan, but having the information in one place will be helpful as questions arise later. Setting out who is to be responsible for what aspects of survivorship care and who is to take responsibility for implementing the plan can lead to efficiencies in health care delivery and potential cost savings. Survivorship care plans also represent a standardized way of communicating to all involved in the patient’s care about what went on and essential next steps.
What is needed to implement the Survivorship Care Plan? Five elements are key to implementation: (1) acceptance of cancer as a chronic disease; (2) adequate reimbursement; (3) time, either time for the oncology specialist or a physician extender working collaboratively, to create and deliver care plans in a systematic way; (4) more research to expand the evidence base, so that survivorship recommendations have a solid basis; and (5) training for all health professionals in the needs of the growing number of survivors and how to act on the care plan recommendations.
THE STATUS OF TREATMENT SUMMARIES FOR ONCOLOGY CARE
Presenter: Dr. Deborah Schrag
An ASCO initiative, “Treatment Plan/Treatment Summary” that is under way is integral to survivorship care planning. The purpose of this
|
BOX 2-2 Motivations for the ASCO “Treatment Plan/Treatment Summary” Initiative
|
initiative is to standardize a format for medical oncologists to prepare a treatment plan when patients embark on a new course of therapy. This treatment plan summary would document the diagnosis, purpose of treatment, agent, schedule, anticipated toxicities, and the plan for reevaluation. The need for this summary has emerged from decades of quality-of-care research documenting how much information patients do not hear or retain during initial oncology consultations.3
The other part of the ASCO initiative is to standardize a format for medical oncologists to complete a treatment summary when patients complete a chemotherapy regimen. The purpose of this summary is to describe treatment tolerance, response, outcomes, and planned next steps. The preparation of this summary is of particular importance to patients who have completed curative or potentially curative regimens and subsequently transition all or some of their care to other providers.
The IOM cancer survivorship report and several other influential reports and initiatives have motivated this effort (Box 2-2).
The recognition of poor oncology documentation practices came into sharp focus with the National Initiative on Cancer Care Quality (NICCQ), a study that examined the quality of care for patients with breast and colon cancer diagnosed in 1998 in five U.S. cities. This study, which was supported by ASCO and the Susan G. Komen Foundation, determined that the quality of care for study patients was quite good, but that it was incredibly difficult for researchers to retrieve treatment information from medical charts to assess cancer care.
|
3 |
For more information, a background paper by Dr. Schrag, “The Cancer Treatment Plan and Summary,” is included in Appendix D.1. |
Volunteers from the ASCO membership are piloting the use of templates for treatment plans and treatment summaries. Oncologists involved in this initiative are motivated by a desire to streamline the burden of documentation and to be responsive to the advocacy community, which has identified such summaries as key to providing much-needed information to survivors and their families. A move toward “pay for performance” on the part of Medicare and other insurers is another factor driving this initiative. There is an acknowledgment that clinical audits and evaluations of performance depend on good documentation. Electronic medical record systems hold great promise for improving documentation, and vendors who are developing these systems are eager to accommodate oncologists on what they want in terms of content and format. Finally, the events surrounding recent hurricanes tragically illustrated the consequences of not having portable health records. Patients in the midst of their cancer treatment were dislocated without any documentation of their diagnosis and treatment.
Treatment Summaries
The treatment summary is responsive to evidence of problems in three important interrelated domains of quality:
-
Care coordination: physician-to-physician communication has become more difficult as more subspecialists have become involved in care. A cancer patient may have a pain doctor, two kinds of endocrinologists, and two gynecology specialists.
-
Patient-physician communication: patients’ information and psychosocial needs are not being adequately addressed, and the process of shared decision making may not be documented when multiple treatment options are available.
-
Efficiency: providing information to insurance companies and to other physicians involved in the patient’s care is time-consuming, and mechanisms are needed to streamline the burden of record review, document creation, transmittal, and flow management.
Preparation of treatment summaries can also facilitate quality improvement by aiding providers’ self-scrutiny, as is the case for Quality Oncology Practice Initiative (QOPI) participants, as well as external review for quality assurance. Public health tracking, for example for cancer registries, could also be expedited. Cancer registrars currently find it difficult to extract information from medical records.
Some physicians routinely prepare treatment summaries. Surgeons document their care through operative reports. Radiation oncologists have standardized treatment summaries. More generally, all physicians are re-
sponsible for completing a summary for patients discharged from the hospital. Pediatricians have agreed on a standard format for the pediatric health record, which is not necessarily comprehensive but does include the basic growth curve and immunization record. Obstetricians have an agreed-on standard obstetrical summary.
Medical oncologists have not yet taken this approach to documentation, perhaps because oncology care is often complex, variable, and prolonged, making it difficult to summarize. It is these very traits that make it a necessity to have good documentation of care. Other medical specialties that are involved with the management of complex chronic disease have also recognized and tried to address their documentation shortcomings. Psychiatrists must contend with chronically mentally ill individuals, who over the years may be cared for in health care, social services, or criminal justice institutions. Documentation is also problematic in the case of diabetes, renal dialysis, transplantation, and HIV/AIDS. In all of these areas, in which it is common for patients to transition between providers and care settings, a treatment summary can provide valuable information to caregivers.
In an attempt to promote the use of treatment summaries, ASCO will develop a sample template that will be:
-
Synoptic, not a comprehensive, detailed review of the medical record (and not a replacement for informed consent or flow sheets);
-
Available as “open source” and modifiable by its users (templates could be downloaded from the ASCO website);
-
Adaptable in its formatting;
-
Minimally burdensome; and
-
Multipurpose.
Treatment Plans
As a complement to the treatment summary that is prepared at the conclusion of treatment, ASCO is also working on a template for a treatment plan that would be prepared at the onset of chemotherapy and reviewed with patients. This plan would include:
-
Summary information, such as regimen name and administration plan (e.g., FOLFOX with Bevacizumab every 2 weeks as an outpatient), numbers of cycles until reevaluation, reevaluation plan (e.g., CT scan in 10 weeks);
-
Contact information for cancer care team members (e.g., patient support, medical oncologist, oncology nursing, radiation oncologist, primary care);
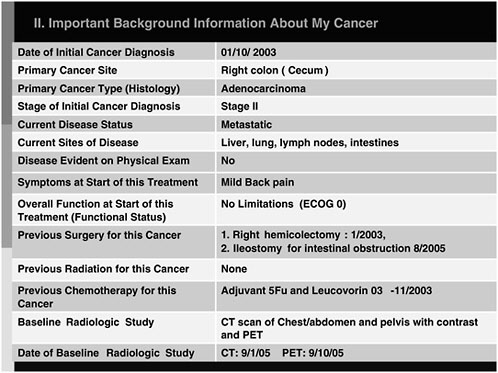
FIGURE 2-5 Example of a portion of the medical oncology treatment plan template that provides background information.
SOURCE: Schrag, 2006.
-
Disease status at the start of treatment;
-
Rationale for treatment; and
-
Basic ingredients of the regimen.
Figure 2-5 is an example of the part of the treatment plan template showing important background information.
One of the advantages of the treatment plan is that, once it is completed, it can be used repeatedly for notes and it can also be used to formulate the preamble for the treatment summary.
Status of Treatment Plans/Treatment Summaries
The ASCO group working on the design of the treatment plan and summary recognized the importance of both documents, but in discussing the concept with practicing medical oncologists, realized that it would be difficult to have both documents adopted simultaneously. The ASCO group
|
BOX 2-3 Potential Audience for Treatment Summaries
|
had to decide where to put their initial efforts and focus. Was it more important to first encourage medical oncologists to adopt treatment planning to help ensure patients’ informed decision making, or should the completion of treatment summaries be the first priority to improve the survivorship care transition? The ASCO planning group decided to initially focus on the treatment summary with the ultimate goal of having two integrated documents that would span the care trajectory.
Identifying the key audience for the care summary has implications for its design. There are many potential audiences for the care summary (Box 2-3). The ASCO designers are focusing on other “nononcology” physicians and will encourage those completing the summary to avoid overly technical oncology jargon.
Another challenge is defining the end of treatment, the time when a treatment summary needs to be prepared. The ASCO planning group developed some ground rules:
-
Do not prepare a treatment summary if a component of a regimen is discontinued;
-
Do not prepare a summary if the patient has a brief (e.g., less than 2 month) break or “holiday” from treatment (e.g., during hospitalization or a comorbid event);
-
Do prepare a summary if the patient proceeds to surgery, radiation, or a new chemotherapy regimen;
-
Completion of adjuvant/neoadjuvant treatment or of primary curative therapy is a logical time to prepare a summary; and
-
Transition to full-fledged survivorship presents another opportunity to prepare a summary.
It may not be easy to define when the treatment summary should be
|
BOX 2-4 Why Physicians Document Greater emphasis:
Less emphasis:
|
created, and practicing oncologists will have to use their judgment in determining when the summary has value. There are, however, some logical points for its creation—at the completion of adjuvant or neoadjuvant treatment regimes or completion of primary curative therapy. It is at these times that having the treatment summary dovetails with survivorship care planning. In oncology, these transitions probably account for nearly 50 percent of all chemotherapy treatment.
The incentives and disincentives that shape physicians’ documentation practices are important to understand when planning for implementation of treatment summaries. Why do physicians document, and what factors could bring about a change in the documentation culture? Some of the key motivators include medicolegal requirements, reimbursement, and a simple jog to providers’ memories during subsequent visits (Box 2-4). There is less emphasis in terms of documentation on communicating with colleagues. Oncologists generally formally communicate with colleagues through letters. Chart documenting is for nuts-and-bolts business and workaday inner office communication. Communicating with a primary care physician or a colleague is an entirely separate endeavor. There has been little emphasis on written communications with patients or creating a record for either public health reporting, research, or quality monitoring. There are some deep-seated cultural patterns in terms of how and why physicians document that need to be overcome in order to get treatment summaries into routine practice.
What are some strategies for implementation? Many have suggested that reimbursement will be key to implementation, but it is unclear if existing reimbursement codes for complex coordination of care are suffi-
cient for both the creation of the treatment summary and the end-of-treatment consultation. The level 5 code for a highly complex visit and coordination of care may suffice.
Patients are also key to implementation. There is a new Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) initiative that requires providers to wear buttons that say, “Ask me if I have washed my hands.” Advocacy organizations have promoted the idea of survivorship care plans, and as patients become informed and start asking for these documents, physicians will be in a position to meet their expectations. Adoption would rapidly occur if health care payers asked for treatment summaries and linked their receipt to reimbursement.
The various groups that are involved with quality-of-care measurement (e.g., the National Committee on Quality Assurance, the American Board of Internal Medicine) can also help drive this process. When surgeons, on whom oncologists depend for referrals, start anticipating and requesting these documents, oncologists will be motivated to change.
Working with the electronic medical record vendors will help with implementation, but evidence will be needed that creating the summary can be efficient and that this documentation will be acceptable in lieu of other forms of documentation. At the present time, because of reimbursement requirements, the medical records include many repeat reviews of systems and physical exams that do not inform other providers. This redundant information is provided to meet reimbursement requirements. ASCO’s new vision of documentation will have to replace the current system, but the dialogue with payers has not yet commenced.
At the time of the workshop, ASCO’s development strategy was being led by Dr. Molla Donaldson, the head of Quality Policy Initiatives within ASCO.4 The goal of the development strategy thus far has been to identify critical content and to get feedback from oncologists, other cancer and noncancer providers, and patients. ASCO aims to develop templates and sample formats that have flexible formatting, including a two-dimensional, fill-in-the-blank paper form that can be completed by hand, as well as a dictatable version. Eventually, the goal is to have three-dimensional versions with drop-down menus. Dissemination strategies ultimately are going to include simply making the software and downloadable forms available. Evaluations will help determine the extent and value of the use of the templates.
A prototype of the treatment summary (see end of Appendix D.1) was designed to answer very basic questions:
-
When was the treatment given and over what time period?
-
Why was this treatment given and what was the context of treatment?
-
What was the treatment? What are the basic details of the regimen?
-
How was the treatment tolerated?
-
What are the planned next steps?
-
Who will perform follow-up?
The form looks deceptively easy to complete, but according to the experience of pilot testers, it is actually somewhat time-consuming to complete.
There is some preliminary feedback from some pilot tests in select oncology practices and from National Comprehensive Cancer Network (NCCN) facilities. Every physician who has participated in the pilot testing has said that the ASCO initiative is valuable, but it has implications for maintaining the volume of patients in their practices given the time necessary to complete the forms. There are also some concerns about liability. Oncologists worry that if a plan is written down and then is not implemented, there may be legal ramifications. These are some of the issues that need to be examined further and resolved. Although this initiative remains in its very early phases, there is widespread interest and support for this endeavor from providers and patients alike. All recognize that there are considerable obstacles to implementation and that changing entrenched habits will be a challenge.
DISCUSSION
Dr. John Rainey, a medical oncologist in private practice who participated in some of the pilot testing, reported that it took about 20 minutes to complete the treatment summary template. He felt that it would have been easier to complete if a treatment plan had been available. Summarizing the treatment is time-consuming, and there is a tendency to give insufficient attention to psychosocial and long-term aspects of care. Having a treatment plan would make it relatively easy to prepare the summary in about 10 minutes at the end of treatment. The focus then could be on toxicity and the long-term plan. He indicated that it might have been better to start initially with the treatment plan and then work on the summary.
Dr. Lee Newcomer, of the UnitedHealth Group, suggested that the treatment summary and care plan have great potential to save time. When on weekend call and picking up a case, for example, an oncologist could look at one page, rather than flip through the chart, saving a good 20 minutes per case. In terms of reimbursement, Dr. Newcomer indicated that the treatment plan would likely be reimbursed as part of a new patient consultation, that the plan would definitely be considered part of that new
patient consultation. If radiation oncologists have a distinct ICD-9 code for their treatment summary, this is perhaps a model to examine. There may need to be some rethinking about how to compensate medical oncologists for the extra time involved in its preparation.
Dr. Lawrence Shulman of Dana-Farber Cancer Institute mentioned that private insurers are concerned about haphazard follow-up and the potential under- or overordering of tests. They are beginning to realize that good care can be less expensive care. In his opinion, if treatment plans and summaries are ultimately cost saving, there will be opportunities for reimbursement. Writing the summary itself may not be reimbursed, according to Dr. Ganz, but oncologists do get paid for counseling visits. If the treatment plan facilitates an additional 20 minutes of discussion with the patient, this time spent counseling could be reimbursed. She suggested that the summary could replace the often fragmentary documentation of the content of those visits.
Dr. William Kraybill, a surgeon from Roswell Park Cancer Institute, indicated that the multidisciplinary conference may provide an opportunity to create the treatment plan summary. Dr. Schrag added that radiation and surgical oncologists have developed treatment summaries, and informal discussions with representatives of these specialties suggest that medical oncology needs to develop a treatment summary for its specialty. She thought that one specialist will have to assume the responsibility of preparing the document after the multidisciplinary team meeting. The patient does not usually attend the multidisciplinary conference, so the posttreatment consultation would need to be held separately.
Dr. Betty Ferrell, a nurse and researcher from City of Hope National Medical Center, described how, over the past 25 years, there has been an interdisciplinary effort to document that cancer survivorship is more than just physiological effects, late effects, and drug treatments. She pointed out that the IOM report recognized that survivorship is also about serious psychosocial issues, including family disruption, economic concerns, and fertility. Dr. Ferrell expressed some concern that the ASCO plans for a treatment plan and summary appeared to be reducing survivorship care planning to physical issues and drugs and to also be focused on reimbursement issues. Critical at this junction is to establish what patients need and then design documents to meet those needs. Ultimately, the Survivorship Care Plan should capture psychosocial issues and be designed to be interdisciplinary in nature. It is crucial to have nursing and social work involved, in addition to medical and radiation oncologists. Survivorship care plans without an interdisciplinary focus would represent a step backward, not forward.
Dr. Michael Fordis from Bayor College of Medicine thought that, to minimize the burden of documentation, it is very important for the ASCO
planning group to define clearly the purpose of the summary documents. There appear to be different expectations and potential multiple uses. It is also important to consider the level of evidence and research that is available to support the various applications.
The oncology care and survivorship issues under discussion represent a domain in health care that is a “poster child” for why interoperability within health care is needed, according to Dr. Ross Martin of Pfizer Human Health. He added that electronic medical records and the associated communication between electronic medical records and personal health records are vital to success in this area. The multimodal delivery, the multiple domains involved in care, the long duration of care, and the high costs of care all point to the need to deliver this complex care efficiently. The American Health Information Community was formed last year, with the express purpose, according to Secretary Leavitt of the U.S. Department of Health and Human Services, to look at these “breakthrough-use” cases for how one can accelerate interoperability among and within health care through electronic medical records. Continuity of care was one of the identified breakthrough-use cases. Many of the applications will be dependent on paper first, because that is the reality of many practices. Progress must accelerate, however, to reach the next stage of development. There are many ongoing initiatives to produce electronic formats for continuity-of-care records, but the templates for treatment plans and summaries can easily be integrated into these formats.
Dr. Schrag reiterated that the goal of the ASCO initiative is to have the treatment plans and summaries available electronically with drop-down menus, so that in a limited amount of space a lot more detail can be captured, whether it is a follow-up referral to a fertility specialist or to a psychologist or a therapist. Starting with a two-dimensional paper template is necessary because the majority of medical oncology practices remain paper based. Estimates are that 30 to 40 percent of medical oncologists do not use a computer for their medical records. The goal is to proceed on multiple fronts simultaneously, at the same time reaching consensus on the documents’ audience and content. It has been a challenge to meet the range of needs that have been identified. A document that satisfies a patient is not the same as a document that will satisfy a fellow oncologist, a future oncologist, a surgeon, and a primary care physician. In trying to create documents that meet some of everyone’s needs, they may meet all of no one’s needs. Achieving a balance is a challenge.
Dr. Martin pointed out how critical it is during the early stages of development to have in mind the end optimal model, which in this case is a template with an electronic format. There is a need to accommodate existing paper processes, but it is difficult to adapt a paper process later if an electronic model is not conceived of in the beginning. Dr. Sheldon Greenfield
agreed on the importance of clarity of purpose at the outset. He raised the point Dr. Ferrell made earlier that there may have to be a different focus, a separate but equal track for patients and providers. He added that it is sometimes difficult for professional societies to champion these activities because the rank-and-file members may thwart the progressive leadership and refuse to adopt the new recommendations for documentation. The right people need to be assembled, particularly payers and quality assurance groups, such as the National Committee for Quality Assurance. They are taking the initiative on similar issues. It is important to establish the composition of the group that is needed to make decisions about the purpose and scope of the initiative.
Dr. Schrag mentioned that the practicing community of oncologists who have been consulted on the ASCO initiative acknowledge that the innovations in documentation envisioned are important. Although they are recognized as a good idea, there is resistance. She added that, as described in the book by Malcolm Gladwell, there may need to be a “tipping point,” a cultural shift to an expectation that everyone creates and uses these documents. There will have to be simultaneous effort from multiple directions, including from survivor groups. Aggressive strategies, such has having providers wear buttons that say, “Ask me if I gave you a treatment summary” would probably not be appreciated by the provider community.
Ms. Stovall described how many patients are very intimidated by their physicians and have the perception that if they asked about hand-washing they would be labeled as a bad patient. In her opinion, the JCAHO hand-washing initiative gives patients permission to ask the question. From the patient perspective, it relieves a burden and may not be such a bad thing. From the physician perspective, it may be viewed as a “stick”; however, it may be preferable to prevent an infection than to have the question asked.
In terms of the content of the treatment plan and summary, it is essential for psychosocial issues to be addressed. It must be understood that relieving the anxiety and depression that almost every person with cancer faces when he or she is diagnosed will improve the patient’s experience and make cancer care more manageable. Dr. Schrag agreed and suggested that providers will probably need to have both carrots and sticks to implement survivorship care planning.
From the perspective of primary care, Dr. Jean Kutner of the University of Colorado Health Sciences Center thought that providers of diabetes care are probably at the forefront of shared care across specialties. Oncology, when the treatment plan and summary are adopted, would be lauded as a shining example in terms of specialist to primary care communications. She felt that primary care providers would appreciate enormously having oncologists take the lead in establishing who is responsible for what elements of follow-up care and documenting succinctly the status of care and
the presence of clinical and psychosocial concerns. Having a comprehensive but short treatment summary and follow-up plan would make primary care visits more efficient.
Ms. Susan Leigh, a cancer survivorship consultant, indicated that, from an advocacy perspective, survivorship care planning must be viewed as a team effort not limited to doctors. Nurses and social workers are critical members of this team. Attention needs to be paid to how to communicate this kind of information to survivors. It involves a lot more than simply giving them a paper and talking about all the specifics of their treatment. Sharing such information can be very traumatizing and anxiety-producing. Communication research is needed to better understand how to deliver this type of information effectively and compassionately. Mr. Richard Boyajian, a nurse practitioner from Dana-Farber Cancer Institute, added that it is important to keep in mind that the treatment plan and summary should be considered a starting point from which the various disciplines—nursing, social work, and others—will be involved to address the entire array of patient needs. The focus on the needs of the patient must be maintained. Patients are entitled to the information that these documents provide.
Health care payers could be integral to the adoption of the treatment plan and summary, according to Dr. Newcomer of the UnitedHealth Group. He suggested that interest may initially be greater in the initial treatment plan because the plan could serve as a document that counselors could use to help patients address questions about coverage or find appropriate support groups. If it could be used as a precertification tool, it would generate payer interest very quickly. When payers get involved, things can happen quickly. For example, despite having a standard for colon cancer surgery established for 10 years, it has not been adhered to for half the patients in the country. This year, in less than 3 months, UnitedHealthcare told surgeons in four cities that if they could not demonstrate adherence to the standard regarding node resection, then they would not be eligible to see patients with UnitedHealthcare coverage. Change in practice occurred very quickly. Some providers dropped out, but most are adhering to the standard. This example illustrates how payers can initiate a tipping point in physician practice.
Dr. Newcomer thought that one central purpose needs to be identified for the treatment plan and summary. The plan should clarify what is anticipated and also include both medical and psychosocial aspects of care. Many oncologists will need tools to assist them in making psychosocial assessments. The development of comprehensive treatment plans will illustrate how little is known about follow-up.
For some aspects of the care plan, such as symptom management and psychosocial issues, the particular treatment that a person has may not be that important, according to Dr. Greenfield. It is important to keep in
mind that the summaries are only a starting point for sets of discussions. Dr. Peter Raich of Denver Health Medical Center added that an interdisciplinary approach is needed to develop the treatment plan and summary, and these tools need to be aimed at the patient. Perhaps two instruments are needed, one for physician communication and the other for patient communication. These documents would provide a proactive way to educate and guide patients into the survivorship phase of their treatment. This phase of care provides a teachable moment, and it should be used to help patients with lifestyle changes that will be very important as they continue in their survivorship.
Dr. Greenfield concluded that however the treatment plan and summary evolve, with perhaps two tracks, a physician track and a patient track, it would put oncology at the forefront of many other medical specialties. There have been many quality-related activities in other disciplines, but the focus is usually entirely on the medical and not on the psychosocial aspects of care. If there were a way to put the two together, it would represent a huge national step forward, and, as has been pointed out, payers may be able to use the documentation and facilitate adoption.
Dr. Donaldson congratulated Dr. Schrag for the enormous amount of work she has undertaken on the treatment plan and summary, and pointed out that, although the effort has been led within ASCO, there is an understanding that additional members of the survivorship community will have to be involved in further development. Development will move ahead to accommodate practices with and without an electronic health record, but, regardless of the platform, some agreement is needed on content. A question was raised regarding dissemination and the role of specialty societies. A group called the Cancer Quality Alliance has recently been formed, co-chaired by Ellen Stovall and Patricia Ganz, which includes representatives from insurance companies, the federal government, social work, nursing, and so on, across the board. The Cancer Quality Alliance is therefore a logical place for both development and dissemination activities relating to treatment plans and summaries.
Ms. Carol Curtiss raised the concern that the draft templates under discussion would appear to be very useful to health care providers in understanding what is happening to patients, but they may not be very useful to patients in learning to live well through diet and exercise and getting back to wellness. Not enough is known in these areas to provide very specific advice; however, she thought that it could be frightening for patients to simply receive a list of potential late effects without some guidance on what they themselves can do to maintain or improve their health.
Ms. Wendy Landier described how the Children’s Oncology Group (COG) has developed evidence-based, long-term follow-up guidelines and treatment summary forms (see Appendix F). A lesson learned over years of
development is that it is very important to establish what will be done with the summary information. The pediatric oncology community has honed the summary down to key elements that are needed to generate patient-specific guidelines. It is through the COG guidelines and not through the treatment summary that psychosocial issues are addressed. Appropriate guidelines are generated on the basis of the treatment summary that documents the patient’s treatment-related risk factors.
Dr. Loria Pollack of the Centers for Disease Control and Prevention concluded the discussion by pointing out that one of the potential uses of a treatment plan is to assist patients in treatment following a disaster. She described how there were an estimated 24,000 people diagnosed with cancer in the past year in the areas affected by Hurricane Katrina. Many of these individuals were displaced during their treatment, and when they sought care in another setting, some could not tell the oncology providers what type of cancer they had. In discussions of whether to start with plans or summaries, it would be helpful to keep these experiences in mind.


























