4
INFECTIOUS DISEASES DIAGNOSED IN US TROOPS WHO SERVED IN THE PERSIAN GULF WAR, OPERATION ENDURING FREEDOM, OR OPERATION IRAQI FREEDOM
Infectious diseases have accompanied war throughout recorded history; the clinical aspects of Operation Desert Shield (ODSh), Operation Desert Storm (ODSt), Operation Iraqi Freedom (OIF), and Operation Enduring Freedom (OEF) have been no different. Although medical and epidemiologic personnel in the US military can anticipate troops’ exposure to many pathogens and mitigate their effects, naturally-occurring pathogens infected some troops during these operations. This chapter summarizes information about the infectious diseases and pathogens identified in US troops who served or are serving in ODSh, ODSt, OIF, or OEF. That information comes from several sources, including published scientific literature, medical surveillance monthly reports published by the Army Medical Surveillance Activity, the Centers for Disease Control and Prevention (CDC), and infectious disease experts at the Department of Defense (DOD) and the Department of Veterans Affairs. In Chapter 5, the committee evaluates the published scientific literature about the possible long-term adverse health outcomes of nine of the diseases discussed in this chapter.
Thriving on the troops’ crowded and sometimes unsanitary living conditions, microbial pathogens have caused primarily diarrheal illnesses and acute upper respiratory infections during ODSt, ODSh, OEF, and OIF (Hyams et al. 2001a; Paparello et al. 1993; Richards et al. 1993a; Thornton et al. 2005; Wasserman et al. 1997). Smaller numbers of military personnel have had various insect-borne diseases, nosocomial infections, brucellosis, chickenpox, meningococcal disease, and Q fever.
Even this chapter’s comprehensive review of public documents may not capture the full burden of infectious disease on US troops who have served in southwest and south-central Asia. Military medical investigators’ primary mission is to apply their findings to maintain troops’ health and they might not always publish summary reports in medical journals. In addition, field commanders may be reluctant to report illnesses perceived as trivial (such as vomiting and diarrhea) even when an outbreak of disease interferes with military operations (Matson 2005). Finally, a new policy purveyed by the DOD restricts the publication of some kinds of medical information that enemy combatants could use to gain an advantage over US troops (Department of the Army 2005b).
DIARRHEAL DISEASE
Enteric Infections in the Gulf War
The leading cause of morbidity among American forces deployed to the Persian Gulf region was diarrheal disease (Hyams et al. 1995a). From August 1990 to May 1991, about 50% of surveyed ground troops and personnel onboard the USNS Mercy experienced at least one episode of acute diarrhea (Haberberger et al. 1994; Hyams et al. 1991). Large outbreaks of watery diarrhea began in August 1990; outbreaks of more severe, bloody diarrhea began in the following month. In addition, gastroenteritis with vomiting as a primary symptom occurred both sporadically and epidemically throughout the war.
Ground Troops
Laboratory Analysis
Hyams and colleagues collected clinical and epidemiologic data from male US troops stationed in northeastern Saudi Arabia to determine the causes and prevalence of diarrheal disease among the troops, risk factors for diarrheal disease in the field, and the effectiveness of pharmacologic treatments (Hyams et al. 1991). From 432 soldiers who sought medical care and presented with gastroenteritis, stool samples were collected and examined for numerous enteropathogens, as described below and summarized in Table 4.1. The soldiers collectively represented all branches of the military, several regions of northeastern Saudi Arabia, and a variety of living conditions. Gastroenteritis was defined as diarrhea (three or more loose or watery stools within 24 hours), abdominal cramps, vomiting, or bloody stools.
The stool specimens were cultured for various pathogens: E. coli, Salmonella, Shigella, Aeromonas, Plesiomonas, Yersinia, Vibrio spp., and Campylobacter. Bacterial enteropathogens were identified with the methods described in Manual of Clinical Biology, 4th edition (Kelly et al. 1985). The specimens were also examined for parasites with direct microscopy and for group A rotavirus with a commercial monoclonal-antibody-based immunoassay. Stool specimens and serum from subsets of patients underwent other tests for adenovirus, astrovirus, calicivirus, coronavirus-like agents, group A rotavirus, and norovirus (also known as Norwalk virus). One or more bacterial enteropathogens were identified in 49.5% of the stool cultures, representing 214 patients. Enterotoxigenic E. coli (ETEC), Shigella sonnei, or both were found in cultures from 205 of those patients. The scientists also found nontyphoid Salmonella spp., enteroinvasive E. coli, and Campylobacter. Tests for viruses yielded positive results for norovirus and rotavirus. There was no evidence of parasitic infection.
TABLE 4.1 Summary of Test Results for Enteropathogens in Stool or Serum from 432 US Military Personnel with Gastroenteritis During Operation Desert Shield
|
|
Identified |
|
|
Enteropathogen or Enterotoxin |
Yes (No. patients) |
No (No. patients) |
|
Bacteria |
|
|
|
Aeromonas |
-- |
x |
|
Campylobacter spp. |
x (2) |
x (430) |
|
Enteroinvasive E. coli |
x (3) |
x (429) |
|
Enterotoxigenic E. coli |
x (128) |
x (304) |
|
Plesiomonas |
-- |
x |
|
|
Identified |
|
|
Enteropathogen or Enterotoxin |
Yes (No. patients) |
No (No. patients) |
|
Salmonella spp. (not S. typhi) |
x (7) |
x (425) |
|
Salmonella typhi |
|
x |
|
Shigella spp. |
x (113) |
x (319) |
|
Vibrio cholerae |
-- |
x |
|
Yersinia spp. |
-- |
x |
|
Enterotoxins |
|
|
|
Circulating Clostridium perfringens enterotoxins |
-- |
x |
|
Circulating staphylococcal enterotoxins |
-- |
x |
|
Parasites |
|
|
|
Entamoeba histolytica |
-- |
x |
|
Giardia lamblia |
-- |
x |
|
Viruses |
|
|
|
Adenovirus |
-- |
x |
|
Astrovirus |
-- |
x |
|
Calicivirus |
-- |
x |
|
Coronavirus-like agents |
-- |
x |
|
Norovirusa |
x (1-9)b |
x (17) |
|
Rotavirus (group A) |
x (1) |
x (431) |
|
aStool contained particles that were morphologically similar to norovirus. bMultiple tests for viral enteropathogens were conducted on subsets of stool and serum samples, and the number of samples that tested positive for norovirus varied by test from 1 to 9 (Table 4.2). SOURCE: Adapted with permission from Hyams et al. 1991. |
||
Only 19 of the 432 soldiers in the study reported vomiting as a primary symptom. These cases were clustered temporally (in November and December) but not geographically. The testing of stool samples and paired serum samples suggested that norovirus was the principal etiologic agent in troops with vomiting (Table 4.2). Various investigators later conducted studies specifically on norovirus in the Gulf War context, as discussed below.
TABLE 4.2 Summary of Test Results for Viral Enteropathogens and Enterotoxins in Stool or Serum from Subsetsa of US Military Personnel with Gastroenteritis During Operation Desert Shield
|
|
Identified |
|
|
Enteropathogen |
Yes (No. patients) |
No (No. patients) |
|
In stool samples from 19 patients with vomiting as a primary symptom, November-December 1990 |
||
|
Enzyme immunoassay results: |
|
|
|
Adenovirus |
-- |
x |
|
Norovirus |
x (3) |
x (16) |
|
Rotavirus (group A) |
-- |
x |
|
Immune electron microscopy results (in 13 of 19 specimens): |
|
|
|
Adenovirus |
-- |
x |
|
Astrovirus |
-- |
x |
|
Calicivirus |
-- |
x |
|
Coronavirus-like agents |
-- |
x |
|
|
Identified |
|
|
Enteropathogen or Enterotoxin |
Yes (No. patients) |
No (No. patients) |
|
Norovirusb |
x (3) |
x (10) |
|
Rotavirus |
-- |
x |
|
In stool samples from 68 patients with diarrhea but no vomiting, November-December 1990 |
||
|
Enzyme immunoassay results: |
|
|
|
Adenovirus |
-- |
x |
|
Norovirus |
-- |
x |
|
Rotavirus |
-- |
x |
|
Immune electron microscopy results (in 18 of 68 specimens): |
|
|
|
Adenovirus |
-- |
x |
|
Astrovirus |
-- |
x |
|
Calicivirus |
-- |
x |
|
Coronavirus-like agents |
-- |
x |
|
Norovirusb |
x (1) |
x (17) |
|
Rotavirus |
-- |
x |
|
Paired serum samples from 11 patients with vomiting alone or vomiting and diarrhea |
||
|
Evaluated for a 4-fold or greater increase in serum antibody titer to: |
|
|
|
Adenovirus |
-- |
x |
|
Circulating Clostridium perfringens enterotoxins |
-- |
x |
|
Circulating staphylococcal enterotoxins |
-- |
x |
|
Norovirus |
x (9) |
x (2) |
|
Rotavirus (group A) |
-- |
x |
|
a'These groups of patients were part of a cohort of 432 troops. bStool contained particles that were morphologically similar to norovirus. SOURCE: Adapted from Hyams et al. 1991. |
||
Characterization of ETEC. The high prevalence of ETEC and Shigella isolates led investigators to characterize these organisms further (Table 4.3). Shigella isolates were identified by species; additional studies about the occurrence of Shigella among Gulf War troops are discussed below.
TABLE 4.3 Bacterial Enteropathogens Identified in Stool Specimens from 214a U.S. Military Personnel with Gastroenteritis
|
Enteropathogen |
No. (%)b of Patients |
|
Enterotoxigenic E. coli |
|
|
Heat-labile |
15 (3.5) |
|
Heat-stabile |
44 (10.2) |
|
Heat-labile and heat-stabile |
64 (14.8) |
|
Mixedc heat-labile and heat-stabile |
2 (0.5) |
|
Enteroinvasive E. coli |
3 (0.7) |
|
Shigella |
|
|
S. dysenteriae |
4 (0.9) |
|
S. flexneri |
12 (2.8) |
|
S. boydii |
8 (1.9) |
|
S. sonnei |
89 (20.6) |
|
Enteropathogen |
No. (%)b of Patients |
|
Salmonella (not S. typhi) |
7 (1.6) |
|
Campylobacter |
2 (0.5) |
|
a Bacterial enteropathogens were identified in 214 (49.5%) of the 432 stool samples collected. b The total percentage of isolates is higher than the percentage of patients with an identified enteropathogen because 36 patients had mixed infections. c Two patients had mixed heat-labile and heat-stabile enterotoxigenic E. coli infections, with individual colonies producing either heat-labile or heat-stable toxin alone. SOURCE: Reprinted with permission from Hyams et al. 1991. |
|
Hyams and colleagues tested E. coli-like organisms for heat-labile and heat-stabile toxin by using alkaline phosphate-conjugated oligonucleotide DNA probes and Y-1 adrenal cell and suckling-mouse assays (Hyams et al. 1991). Later, Wolf and colleagues further analyzed the Hyams et al. ETEC isolates for their toxin distribution, and other factors (Wolf et al. 1993). A given strain of ETEC may produce heat-labile enterotoxin (LT), heat-stabile enterotoxin (ST), or both. LT is nearly identical with the toxin that causes cholera. Some 85% of 132 ETEC isolates from 124 symptomatic Gulf War troops produced LT (Table 4.4).
TABLE 4.4 Toxin distribution Among 132 ETEC Isolates from 124 US Troops with Gastroenteritis during Operation Desert Storm
|
Toxin |
No. (percentage) of isolates |
|
LT and ST |
59 (45) |
|
LT |
53 (40) |
|
ST |
20 (15) |
|
SOURCE: Adapted with permission from Wolf et al. 1993. |
|
Antimicrobial susceptibility. Using the disk-diffusion method, Hyams and colleagues determined which of five antibiotics would most effectively treat the strains of ETEC and Shigella identified in the stool cultures. Up to 63% of the ETEC and up to 85% of the Shigella specimens were resistant to several of the antibiotics most accessible to clinicians in the field (Table 4.5), including trimethoprim-sulfamethoxazole, the antibiotic most frequently used to treat diarrhea during the early stages of ODSh deployment. In contrast, the scientists found, ETEC and Shigella were 100% susceptible to ciprofloxacin and norfloxacin. Hyams and colleagues reported that empiric results of antibiotic treatment for diarrheal disease in the field led military clinicians to gravitate toward ciprofloxacin and norfloxacin over time. Clinicians also reportedly administered quinolone drugs to affected critical combat troops to shorten the duration of gastroenteric symptoms.
TABLE 4.5 Antimicrobial Resistance of Enterotoxigenic E. coli and Shigella Specimens
|
|
Proportion of Resistant Specimens, % |
|
|
Antibiotic |
Enterotoxigenic E. coli (N = 125) |
Shigella (N = 113) |
|
Trimethoprim-sulfamethoxazole |
39 |
85 |
|
Tetracycline |
63 |
68 |
|
Ampicillin |
48 |
21 |
|
Ciprofloxacin |
0 |
0 |
|
Norfloxacin |
0 |
0 |
|
SOURCE: Adapted with permission from Hyams et al. 1991. |
||
Epidemiologic Analysis
To learn the prevalence of and risk factors for diarrheal disease among US troops stationed in northeastern Saudi Arabia during ODSh, Hyams and colleagues administered an epidemiologic survey to 2,022 personnel from all branches of the military in October-December 1990 (Hyams et al. 1991). After an average of 2 months in Saudi Arabia, 57% of those surveyed had suffered at least one episode of diarrhea. The symptoms of diarrheal disease had led 22% of all respondents to seek medical care, and had prevented 20% of all respondents from performing their duties. Thirty-two percent of those surveyed had experienced two or more separate episodes of diarrhea. In some units, the attack rate was 5-10% per week.
A univariate analysis of potential risk factors for the transmission of diarrheal disease during ODSh suggested an association between an episode of diarrhea and eating salad, dining in a mess hall, and drinking from a canteen. (A laboratory study of 12 heads of lettuce obtained from food-distribution facilities in September 1990 found coliform bacteria in all 12; ETEC was identified in two (Hyams et al. 1991).) No association was found between an episode of diarrhea and obtaining food from local vendors, eating in a local restaurant, or drinking bottled water. A multivariate analysis of these risk factors and an evaluation of published research on the transmission of Shigella indicated that flies and relatively poor personal hygiene probably accounted for the spread of ETEC and Shigella.
The disabling effect of repeated outbreaks of diarrheal disease in US forces during ODSh despite the best available preventive measures led Hyams and colleagues to call for the development of a vaccine to protect troops (Hyams et al. 1991). DOD is supporting development of such vaccines (Stephens and Nataro 2004).
Shigella
The presence of immunoglobulin A (IgA) and immunoglobulin G (IgG) anti-Shigella lipopolysaccharide (LPS) in predeployment serum did not offer protective immunity to infection by Shigella spp. among US ground troops who participated in the Persian Gulf War, Hyams and colleagues reported (Hyams et al. 1995b). The investigators reached that conclusion by studying a cohort of 883 combat troops and support personnel in three Marine Corps units who were flown directly to Saudi Arabia in late December 1990 and directly back to the United States in May 1991. Initially stationed in Saudi Arabia, and then relocated to Kuwait, the subjects lived in remote, rugged, desert camps. US military personnel prepared most of their food, which came from the United States except for local fresh produce. The subjects drank both locally produced bottled water and water purified by reverse-osmosis (Hyams et al. 1993).
The investigators obtained serum samples from all members of the three units who were accessible during the week before their deployment and the 2 two days after their return (827 subjects). Paired serum samples were tested for antibodies to both S. sonnei and S. flexneri. Epidemiologic questionnaires were also administered to this cohort before and after deployment.
Among the 827 subjects, 18% seroconverted during ODSh and ODSt; that underscored earlier findings that troops deployed to ODSh and ODSt faced a considerable risk of Shigella infection. The study revealed the absence of an association between seroconversion and the occurrence of diarrheal symptoms. Overall, 60% of the cohort reported one or more episodes of diarrhea, and 18% reported diarrhea with fever. In contrast, many troops who seroconverted were asymptomatic.
Because S. sonnei LPS cross-reacts with the LPS of Plesiomonas shigelloides, some of the high concentrations of serum antibodies observed in samples from the 827 marines might not have been the result of exposure to Shigella spp. To determine whether exposure to Shigella led
to persistently high antibody concentrations in some subjects and seroconversions in others, Mikhail and colleagues examined how a subset of the paired serum samples reacted to four Shigella invasion plasmids, which cross-react with just one enteroinvasive strain of E. coli (Mikhail et al. 1996). They also used ELISA to detect antibodies to S. sonnei LPS. In their report, the authors noted that antibodies to LPS and invasion plasmid antigens in serum increase and decrease within 4 months during naturally acquired Shigella infections.
Only 12 sets of serum samples were large enough to use for this experiment (six from seroconverters and six with persistently high concentrations of antibodies to S. sonnei LPS). By using Western blot, the investigators observed antibody reactions to numerous invasion plasmid antigens both before and after deployment in serum from troops with persistently high concentrations of antibodies to S. sonnei LPS, which suggest that they had been exposed to S. sonnei before deployment and were repeatedly exposed to it during deployment. In the postdeployment serum from troops who seroconverted, the scientists observed IgA and IgG recognition of additional invasion plasmid antigens and increased concentrations of antibodies to S. sonnei LPS—even in two soldiers who were asymptomatic for diarrheal illness throughout the war. The authors interpreted those results as an indication that troops who seroconverted had been exposed repeatedly to S. sonnei in the field.
Norovirus
Norovirus (NV) and Norwalk-like viruses caused both sporadic cases and outbreaks of acute gastroenteritis among ground troops and shipboard personnel throughout the Gulf War. Brief and debilitating, NV gastroenteritis usually causes acute vomiting, diarrhea, nausea, and abdominal cramps that last 1-2 days. Some people never develop symptoms even after direct challenge, but others are repeatedly susceptible to symptomatic infection. All infected people shed highly contagious NV in stools from as early as 15 hours after exposure to as late as 14 days after. Studies of NV infections among military personnel indicate that crowding is the most important risk factor for transmission (McCarthy et al. 2000).
After the Gulf War, Hyams and colleagues demonstrated the incidence of NV infection among troops deployed to Saudi Arabia and Kuwait from late December 1990 through May 1991 (Hyams et al. 1993). Using the paired serum samples from the 883-troop cohort described above, the investigators used ELISA to measure antibody activity to recombinant NV particles. The investigators defined evidence of infection as a 4-fold or greater increase in titer of anti-NV antibodies from predeployment serum to postdeployment serum.
Matching the ELISA results with the subjects’ clinical symptoms, as reported in the aforementioned postdeployment epidemiologic questionnaire, the investigators obtained the results displayed in Table 4.6. After adjusting for oversampling of subjects with vomiting, the investigators estimated that NV infected 6% of the study population. The scientists could not determine the specific sources of infection, although they enumerated the probable opportunities for person-to-person spread of NV: rapid deployment of massive numbers of soldiers, overcrowding, and rugged desert living conditions that included communal temporary latrines and bathing facilities.
To aid the development of a vaccine against NV and Norwalk-like virus for the US military, Lew and colleagues compared the published genetic sequence of NV with sequences of NV strains extracted from three stool specimens from US troops who developed gastroenteritis while deployed to Saudi Arabia for ODSh (Lew et al. 1994).
TABLE 4.6 Number of Subjects with Various Clinical Manifestations of Enteric Disease and Serologic Evidence of Norovirus Infection
|
|
No. (%) with Complaint |
No. (%) with ≥ 4-fold Increase in Norovirus Antibody (n = 32) |
|||
|
Clinical Manifestation |
Entire Cohort (n = 883) |
Subjects Tested for Norovirus Infection (n = 404) |
|||
|
Vomiting alone |
17 |
(1.9) |
17 |
(4.2) |
4 (23.5) |
|
Vomiting and diarrhea |
117 |
(13.3) |
117 |
(29.0) |
14 (12.0) |
|
Diarrhea alone |
406 |
(46.0) |
170 |
(42.1) |
11 (6.5) |
|
No vomiting or diarrhea |
343 |
(38.8) |
100 |
(24.8) |
3 (3.0) |
|
SOURCE: Reprinted with Permission from Hyams et al. 1993. |
|||||
Enteric Parasitic Infections
Enteric parasites may have infected a small percentage of troops deployed to the Persian Gulf region in 1990 and 1991 (Malone et al. 1991). Malone and colleagues studied the risk of enteric parasitic disease in a cohort of 422 marines returning from Saudi Arabia and Kuwait after 5 months of service on the front lines of ODSt. Like the marines described above, this cohort had little contact with local populations. The investigators collected stool samples from the troops within 2 days of their arrival in the United States. The specimens were analyzed for evidence of helminthic and protozoan infections according to the thimerisol (Merthiolate)-iodine-formalin concentration technique.
The only evidence of enteric parasitic infection found in the cohort was Giardia lamblia cysts in specimens from nine marines, or 2% of the subjects. Four of the nine troops had experienced an episode of diarrhea while deployed to the Middle East, and seven of the nine had previously been deployed aboard a ship that made port calls in the Mediterranean. None of the nine marines had diarrhea when their stool samples were obtained.
Oster and Sanford make passing reference to “a few” cases of amebiasis among troops deployed to the Persian Gulf War (Oster and Sanford 1992); however, the report lacks supporting epidemiologic, clinical, and microbiologic data. The committee is unaware of other reports of amebiasis among Gulf War troops.
Shipboard Military Personnel
About 46% of the 870 military personnel deployed to the Persian Gulf aboard the hospital ship USNS Mercy T-AH 19 had at least one episode of diarrhea in the period August 1990-January 1991 (Paparello et al. 1993). That finding is derived from the results of an epidemiologic survey designed to assess the prevalence and effects of diarrheal illness among shipboard personnel deployed to the Middle East during ODSh.
The USNS Mercy was a referral hospital for patients from other ships in the Persian Gulf and ground-based medical facilities during ODSh. From December 13, 1990, to January 7, 1991, investigators distributed a voluntary questionnaire to all Navy personnel aboard the ship; about 83% (N = 722) completed it (Table 4.6). The questions covered demographics; history of eating off the ship; job description; location of spaces where subjects worked, ate, and slept; and gastrointestinal symptoms. In contrast with the populations of most other studies described in this chapter, 32% of the subjects were female.
In addition to the results listed in Table 4.7, the investigators found that officers were more likely to report an episode of diarrhea and more often unable to perform routine duties due to diarrhea than enlisted personnel. One explanation, the authors speculated, is that officers tended to eat in a wide variety of local restaurants during visits to foreign ports, whereas enlisted
personnel did not. The investigators also found independent associations between lower age (range, 17 to 31 years) and an episode of diarrhea with vomiting and between female sex and an episode of diarrhea with vomiting. The authors speculated about many explanations for the latter finding: that women were more likely to report symptoms to sick call, that a greater percentage of women than men were officers, and that women worked more closely with patients and thus were more often exposed to diarrheal pathogens.
TABLE 4.7 Morbidity Due to Diarrheal Disease Among 722 US Navy Shipboard Personnel Deployed to the Persian Gulf During ODSh
|
Symptoms and Outcomes |
Fraction of Troops (N = 722), % |
|
Diarrhea |
46.3 |
|
Diarrhea and fever |
11.6 |
|
Diarrhea and vomiting |
6.2 |
|
Sick-call visit |
7.6 |
|
Inability to work |
6.0 |
|
SOURCE: Adapted with permission from Paparello et al. 1993. |
|
Most of the 8.3% of subjects who received medication responded to treatment with norfloxacin or ciprofloxacin. The investigators suspected but could not confirm an infectious etiology for most cases of diarrheal disease among the USNS Mercy’s crew on the basis of the acute onset and short duration of most cases and a frequent association with eating in foreign ports. The relatively small space for living, eating, and attending to patients aboard the USNS Mercy promoted close contact that may have facilitated the transmission and spread of enteric pathogens among the crew and between patients and crew.
Gastroenteritis in Operation Enduring Freedom and Operation Iraqi Freedom
Epidemiologic Investigations of Gastroenteritis
An epidemiologic survey of 15,459 deployed troops conducted in January-March 2004 revealed that 74.5% of military personnel had experienced at least one episode of diarrhea while serving in OEF, OIF, or both (Sanders et al. 2005a). Sanders and colleagues of the Navy’s Enteric Disease Research Program reached that finding and others through a survey designed to assess the incidence and effect of the most common illnesses and noncombat injuries among deployed US troops participating in OEF and OIF. The investigators’ findings related to diarrheal disease are discussed here, and findings pertinent to respiratory disease and leishmaniasis are presented later.
The survey posed 199 questions that covered demographics, clinical information, general health, and health-risk behaviors and attitudes. The questions were dispersed among 20 unique single-page forms, each containing 19-21 questions (some questions appeared on multiple forms). That enabled the researchers to obtain a representative distribution of responses. The investigators verified the accuracy, integrity, and internal validity of the data obtained from each form.
The troops who completed the questionnaire represented about 11% of the US military force in OEF and OIF during the study period. The study subjects either were participating in the military’s rest and recuperation (R&R) program in Doha, Qatar, or had stopped at an American
air base en route to the United States for a 2-week break after an initial tour of duty in Afghanistan or Iraq.
Analysis of the survey data revealed that self-reported symptoms of diarrheal disease were moderately severe and multiple episodes common. Gastroenteritis occurred more frequently among troops deployed to Iraq (76.8%) than to Afghanistan (54.4%). The duration and severity of symptoms were greater for troops in Iraq than in Afghanistan. Table 4.8 contains additional salient data obtained through the survey about the occurrence of diarrheal illness among US forces during OEF and OIF.
TABLE 4.8 Impact of Diarrhea Among US Military Personnel Deployed to Iraq and Afghanistan, 2003-2004
|
Characteristics of illness |
No. cases in Iraq (N, % or rangea) |
No. cases in Afghanistan (N, % or rangea) |
p |
||
|
Experienced diarrhea |
7,553 |
(76.8) |
543 |
(54.4) |
< 0.0001 |
|
Number of episodes |
5 |
(2-8) |
2 |
(2-5) |
0.0003 |
|
Duration (days) |
4 |
(1.5-4) |
1.5 |
(1.5-4) |
0.008 |
|
Maximal number loose stools per day |
5 |
(2.5-5) |
2.5 |
(2.5-5) |
< 0.0001 |
|
Reported more than six stools per day |
1,166 |
(20.8) |
55 |
(14.0) |
|
|
Illness characteristics from Iraq and Afghanistanb combined Percentage |
95% CI |
||||
|
Sought care for diarrhea |
40.2 |
38.0-42.5 |
|||
|
Number of clinic visitsc |
2.0 |
1-2 |
|||
|
Fever with diarrhea |
25.8 |
22.3-29.2 |
|||
|
Vomiting with diarrhea |
18.0 |
15.0-21.1 |
|||
|
Vomiting without diarrhea |
16.5 |
14.0-19.1 |
|||
|
Persistent diarrhea (>14 days) |
9.8 |
7.5-12.1 |
|||
|
Chronic diarrhea (>30 days) |
3.3 |
1.9-4.7 |
|||
|
Disposition |
|||||
|
Confined to quarters (bedrest) |
14.2 |
11.5-16.9 |
|||
|
Days in quartersc |
2.0 |
1-2 |
|||
|
Hospitalized |
1.8 |
0.7-2.8 |
|||
|
NOTE : CI = confidence interval. a Ranges are from the 25th percentile to the 75th percentile (the interquartile range). b No statistical differences in these characteristics were observed between sites. c Values are median and interquartile range. SOURCE: Adapted with permission from Sanders et al. 2005a. |
|||||
Sanders and colleagues note that recall and selection bias may have influenced their results. They assert that the point estimates derived probably can be generalized to the entire population of US troops deployed to Iraq and Afghanistan for OEF and OIF.
The results presented above validate the findings of an earlier, smaller study in which Sanders and colleagues found that diarrheal illness among troops deployed to OEF and OIF occurred at a high rate and frequently manifested with severe symptoms (Sanders et al. 2005b; Sanders et al. 2004). They also found that diarrheal illness appeared to interfere with military operations more during OEF and OIF than during ODSh. They reached those conclusions by analyzing data collected from an anonymous questionnaire administered to 4,348 volunteers in the period October 27, 2003-January 27, 2004.
The epidemiologic questionnaire was designed to assess the incidence of diarrheal illness and its associated symptoms, treatment, and impact on military missions. Diarrhea was defined as three or more loose or liquid stools in 24 hours or two or more loose or liquid stools associated with other gastrointestinal symptoms or fever.
The respondents, who participated voluntarily, had been deployed for a median of 8 months to Iraq and 6.7 months to Afghanistan. Most were on R&R in Doha, Qatar; others were traveling through Incirlik Air Base, Turkey, after their deployment to Iraq had ended. Although Sanders and colleagues noted several sampling biases in their study, they concluded that it was unlikely that their results overestimated rates of diarrheal illness in the overall population of troops in Iraq and Afghanistan.
Sixty-four percent of respondents stationed in Afghanistan and 77% stationed in Iraq reported one or more episodes of diarrhea during their deployment. More than half the subjects reported multiple episodes. The amount of time spent off a military compound was associated with an increased risk of developing diarrhea. The investigators concluded that time spent off a base probably represented a surrogate measure of exposure to local food and drink.
The investigators found that diarrheal illness affected military operations in OEF and OIF more than it had during ODSh. Of the survey participants, 45% experienced an episode of diarrhea severe enough to decrease job performance for a median of 3 days; 62% of subjects sought medical care for diarrheal illness at least once, and 17% were consequently confined to bed rest for a median of 2 days. For nearly one-third of troops with diarrhea, treatment included intravenous rehydration. Personnel deployed to Iraq were more likely to experience diarrheal illness, to have multiple episodes, and to have severe diarrhea (more than 10 stools per day).
Sanders and colleagues did not attempt to identify the etiologic agents of diarrheal illness in their study population. Nevertheless, they speculated that ETEC and other enteropathogenic forms of E. coli probably caused most episodes of diarrhea that respondents described as watery (Table 4.9). They also speculated that norovirus caused many cases of diarrheal disease in troops who experienced vomiting as a primary symptom.
TABLE 4.9 Demographics and Diarrheal Illness Characteristics of US Military Personnel Deployed to Iraq and Afghanistan
|
Characterizationa of Diarrhea |
Occurrence Among Troops Stationed in Iraq (N = 3915) [N (%)] |
Occurrence Among Troops Stationed in Afghanistan (N = 255) [N (%)] |
|
Watery |
2815 (72) |
149 (58) |
|
Vomiting (mainly) |
317 (8) |
6 (2) |
|
Blood in diarrhea |
128 (3) |
5 (2) |
|
Diarrhea with fever |
471 (12) |
23 (9) |
|
a These characterizations reflect absolute responses that are not mutually exclusive and may include symptoms across multiple episodes. SOURCE: Adapted with permission from Sanders et al. 2005b. |
||
Laboratory Analysis of Gastroenteritis
More than any other type of infectious disease, gastroenteritis due to norovirus1 and Shigella spp. plagued the population of 83,000 US marines deployed to Iraq in spring 2003 according to a study led by staff of a Navy preventive medicine laboratory that provided clinical
and diagnostic support (Thornton et al. 2005). Located in a city about 175 km south of Baghdad, the laboratory collected and analyzed stool samples and other clinical specimens from 30 First Marine Expeditionary Force battalion aid stations and several other medical stations in the area. Thornton and colleagues published the results of their analysis of 129 stool specimens collected from April 24 to June 1, 2003, from 33 medical stations scattered across south-central Iraq.
The authors reported that large outbreaks of nausea, vomiting, and diarrhea lasting 24-48 hours occurred in the First Marine Expeditionary Force from early April though the middle of May, suggesting a viral etiology for most cases of gastroenteritis during that period. Febrile dysentery predominated in that population beginning in the middle of May.
Numerous factors placed the troops of the First Marine Expeditionary Force at risk for gastroenteritis, the authors wrote. The primitive nature of the camps, overcrowding, and filth flies in latrines and dining facilities characterized the troops’ unsanitary living environment. Local ambient temperatures climbed to 40°C during the period of study. Some troops broke military rules to eat locally prepared food, particularly grilled chicken. Finally, a relatively small number of microorganisms are capable of causing shigellosis and norovirus gastroenteritis in humans. In an editorial commentary on Thornton’s report, Matson postulates that robustly healthy people who become dehydrated during daily activity may face a greater risk of severe outcome when infected with norovirus (Matson 2005).
The investigators used plating, biochemical identification, antigen serologic testing, fluorescent antibody antigen detection, and enzyme immunoassay to evaluate stool specimens diagnostically for enteropathogens. Specifically, they tested specimens for pathogenic E. coli, Campylobacter spp., Salmonella spp., Shigella spp., Giardia spp., and Cryptosporidium. Suspect E. coli was tested for heat-labile and heat-stabile enterotoxins; additionally, investigators plated stool with gross blood or fecal leukocytes on sorbitol-MacConkey agar to detect enterohemorrhagic E. coli. The antimicrobial susceptibility of detected bacteria was evaluated with the disk-diffusion method.
Reverse-transcriptase polymerase chain reaction (PCR) was used to detect norovirus. In addition, the authors sequenced the RNA polymerase genes of detected norovirus to distinguish strains, compare the strains with each other and with known strains, and analyze the occurrence of norovirus strains by military unit and timing.
Table 4.10 illustrates the results of the laboratory-based diagnostic evaluation. One or more enteropathogens were detected in 57 of the 129 stool samples (44%). Norovirus was detected in 23% of the specimens; the investigators found 21 norovirus strains among 30 agent-positive patients. The most frequently detected bacterial enteropathogens were Shigella sonnei and Shigella flexneri; they were isolated from a total of 20% of the specimens. The presence of fecal leukocytes in 43 of 109 stool samples (39%) indicated inflammatory diarrhea, the investigators concluded.
Most of the bacterial isolates tested by Thornton and colleagues were doxycycline-resistant (Table 4.10), and several bacterial enteropathogens identified in prior studies of military populations were observed less frequently in this study population. For those reasons, both the authors and Matson (the editorial commentator) postulated that the mandatory dose of doxycycline (100 mg/day) taken by personnel in the First Marine Expeditionary Force for antimalarial prophylaxis may also have reduced the potential impact of bacterial enteric pathogens.
Extrapolating their results to the entire First Marine Expeditionary Force, Thornton and colleagues conservatively estimated that several thousand cases of norovirus illness occurred in
April and May 2003. They also postulated that norovirus is ubiquitous in Iraq, on the basis of their observations and reported outbreaks of viral gastroenteritis among other US and allied forces in different parts of the country.
TABLE 4.10 Major Findings from 129 Stool Specimens Obtained from Marines with Gastroenteritis During Operation Iraqi Freedom and Percentage of Bacterial Isolates Resistant to Antimicrobial Agents as Determined by Disk-Diffusion Assay
|
Agent |
No. Agent-Positive Patients |
No. Units with Agent-Positive Patients |
Percentage of Drug-Resistant Isolates, by Drug |
|||||
|
Doxycycline |
Ciprofloxacin |
TMP-SMZ |
Cefoxitin |
Cefazolin |
Ceftriaxone |
|||
|
All bacteria |
35 |
26 |
86 |
14 |
86 |
14 |
14 |
3 |
|
Shigella fIexneri |
13 |
8 |
92 |
0 |
77 |
0 |
0 |
0 |
|
Shigella sonnei |
13 |
8 |
100 |
0 |
100 |
0 |
0 |
0 |
|
Campylobacter spp.a |
5 |
5 |
40 |
100 |
100 |
100 |
100 |
20 |
|
Other bacteriab |
4 |
4 |
75 |
0 |
50 |
0 |
0 |
0 |
|
Norovirus |
30 |
14 |
NA |
NA |
NA |
NA |
NA |
NA |
|
NOTE: Doxycycline, 30μg in disk; ciprofloxacin, 5 μg; TMP-SMZ (trimethoprim-sulfamethoxazole), 1.25 μg of trimethoprim; cefoxitin, 30 μg; cefazolin, 30 μg; ceftriaxone, 30 μg. NA = not applicable. a Fifty-six stool samples were tested for Campylobacter spp. b Putative enteroinvasive Escherichia coli: two cases; Salmonella arizonae: one case; Plesiomonas shigelloides: one case. SOURCE: Reprinted with permission from Thornton et al. 2005. |
||||||||
Although the study by Thornton and colleagues was relatively robust in terms of methods, Matson noted three weaknesses in its design compared with similar studies in civilian populations: incomplete standardized clinical data collection, an unknown denominator from which the numerator of laboratory samples was derived, and lack of description of clinical illness and associated morbidity (Matson 2005). The investigators themselves acknowledged the lack of a solid denominator and attack rates in their report, attributing these limitations to the difficulty of gathering public health data and specimens during maneuver warfare.
RESPIRATORY DISEASE
Mild Acute Respiratory Disease in the Gulf War
Mild acute respiratory disease was one of the two leading infectious causes of morbidity among US troops who served in the Gulf War. Some investigators estimated that it accounted for about 7-12% of first-time outpatient visits to primary-care medical personnel in combat units (Wasserman et al. 1997). Crowded living conditions—and for some troops, residence in tightly constructed, air-conditioned buildings—probably facilitated the transmission of respiratory pathogens among US forces (Hyams et al. 1995a; Richards et al. 1993a). In one study, investigators identified Streptococcus pyogenes, Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, influenza virus types A and B, and adenovirus in clinical specimens obtained from soldiers who presented with respiratory symptoms (Richards et al. 1993a).
Crowding occurred frequently during ODSh because so many troops were deployed so quickly. Hyams and colleagues explain that, on arrival in Saudi Arabia, “combat troops were crowded together in warehouses and tents at initial staging areas and then moved to isolated desert locations” (Hyams et al. 1995a). Such conditions naturally facilitated the transmission of respiratory pathogens. That was dramatically illustrated by changes in the weekly rates of respiratory disease among of the 40,000 marines deployed to northeastern Saudi Arabia. Most of them were transported to the Persian Gulf in late August or late December 1990; the percentage of marines that received outpatient treatment for respiratory disease spiked during each deployment (Figure 4.1) (Hyams et al. 1995a).
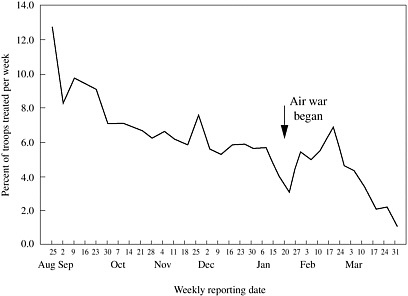
FIGURE 4.1 Weekly rates of total outpatient (sick call) visits among about 40,000 Marine Corps ground troops stationed in northeastern Saudi Arabia who participated in the US Navy’s disease surveillance system.
SOURCE: Reprinted with permission from Hyams et al. 1995a.
Ground Troops
Richards and colleagues conducted epidemiologic, clinical, and environmental studies to determine the prevalence of risk factors for and severity of acute respiratory disease among US ground troops stationed in northeastern Saudi Arabia during ODSh (Richards et al. 1993a).
From November 1990 to January 1991, a voluntary questionnaire was administered to 2,598 men in four units selected to reflect diverse living conditions, geographic locations, and branches of the military (Army and Marine Corps). The rate of participation in the survey exceeded 95%. Respondents had been stationed in Saudi Arabia for a mean of 102 days.
When asked about symptoms of respiratory disease experienced at any time during their deployment, 34.4% of the survey respondents complained of sore throat, 43.1% of a cough, and 15.4% of chronic rhinorrhea. The symptoms of respiratory disease were severe enough to
prevent 1.8% of respondents from performing their routine duties. The longer a soldier was deployed, the more likely he was to report respiratory problems. Having a history of respiratory disease (reported by 6% of respondents) or being a smoker (reported by 37% of respondents) significantly increased the likelihood of respiratory complaints.
The investigators asked survey participants where they slept—in tents, warehouses, non-air-conditioned buildings, or air-conditioned buildings—as a proxy measure of environmental exposure because troops often worked, relaxed, and slept in the same structure. Statistical analyses of the troops’ responses revealed that the risk of developing a cough or sore throat increased as exposure to the outdoors decreased. Moreover, troops who slept in air-conditioned buildings were significantly more likely to develop both a sore throat and a cough. In contrast, exposure to the outdoors increased the risk of developing chronic rhinorrhea; troops who slept in tents were at highest risk. Controlling for smoking, time spent in the war theater, and a history of respiratory disease magnified those associations.
Blood and oropharyngeal-swab specimens were obtained from 68 military personnel who presented with acute respiratory symptoms at any of five medical facilities from October 1990 to January 1991. Using immunofluorescence, latex agglutination, and standard culture techniques, investigators identified bacterial and viral pathogens in 10 of the patients’ specimens (Table 4.11).
Ground-surface samples of sand were collected from seven widely dispersed areas where US troops were stationed. No pathogenic bacterial or fungal organisms were isolated from the analyzed samples. The investigators did not collect or study airborne particles of sand.
TABLE 4.11 Pathogens Identified in Specimens from 68 Troops with Acute Respiratory Symptoms During Operation Desert Shield
|
Pathogen |
No. Patients Infected (N = 14)a |
|
Streptococcus pyogenes |
3 |
|
Neisseria meningitidis |
4 |
|
Streptococcus pneumoniae |
1 |
|
Haemophilus influenzae |
1 |
|
Mycoplasma pneumoniae |
1 |
|
Influenza virus type A |
1 |
|
Influenza virus type B |
2 |
|
Adenovirus |
1 |
|
a Etiologic agents were identified in specimens from only 14 of the 68 patients. SOURCE: Richards et al. 1993a. |
|
On the basis of the results of their epidemiologic, clinical, and environmental analyses, Richards and colleagues concluded that cases of cough and sore throat during ODSh probably had an infectious etiology, whereas environmental factors probably accounted for cases of chronic rhinorrhea. The investigators postulated that the recirculation of indoor air containing respiratory pathogens and the crowding of troops in air-conditioned buildings to escape the desert heat contributed to the high rate of mild acute respiratory disease observed during the Gulf War.
Shipboard Military Personnel
The reported risk of upper respiratory disease was lower among US ground troops than among Navy personnel who served aboard the 1,000-bed hospital ship USNS Mercy T-AH 19 during ODSh (Paparello et al. 1993). That was one conclusion of an epidemiologic study designed to assess the prevalence and impact of upper respiratory disease among shipboard personnel deployed to the Middle East during ODSh.
As described above, the USNS Mercy was a referral hospital for patients from other ships in the region and ground-based medical facilities during ODSh. From December 13, 1990-January 7, 1991, investigators distributed a voluntary questionnaire to all Navy personnel aboard the ship; about 83% (n = 722) completed it.
Among the surveyed population, 79% reported at least one upper respiratory complaint during their deployment. The respondents’ symptoms generally were mild but persistent. Cold-like symptoms with fever were reported by 27.9%, cough by 53.2%, sore throat by 49.1%, and chronic rhinorrhea by 16.6%. The severity of such symptoms prevented 7.4% of respondents from performing their duties.
No significant association existed between smoking and respiratory complaints. Female sex and a history of respiratory disease were independently associated with cold-like symptoms plus fever and inability to perform duties. Investigators could not determine the reason for the sex-based association.
Pathogens probably caused the majority of respiratory disease aboard the USNS Mercy on the basis of the nature and short duration of reported symptoms, the investigators concluded. Moreover, they postulated that the relatively small total space for living, eating, and attending to patients promoted close contact that probably facilitated the transmission and spread of respiratory pathogens among the crew and between patients and crew.
Severe Acute Respiratory Disease in the Gulf War
More than 1,800 US military personnel deployed to the Persian Gulf region developed respiratory disease severe enough to require hospitalization of a day or more (Smith et al. 2004). Among those patients, 214 were diagnosed with pneumonia (etiologic agent unspecified), 90 with acute sinusitis, 102 with chronic sinusitis, and 81 with bronchitis; 678 cases were diagnosed as asthma, and the remaining cases of respiratory disease were not identified. The committee is unaware of published literature about the details of these cases other than what appears in this chapter.
Any of more than 50 viruses, bacteria, fungi, parasites, rickettsiae, chlamydiae, and mycoplasmas can cause pneumonia (Donowitz and Mandell 2000). A smaller array of viral, bacterial, and fungal organisms can cause acute sinusitis; however, such noninfectious agents as allergens and toxins may also instigate this disease. Acute bronchitis usually has a viral etiology, although it is also associated with Bordetella pertussis, Mycoplasma pneumoniae, and Chlamydia pneumoniae (strain TWAR) (Gwaltney 2000a). The pathogenesis of chronic sinus disease is poorly understood; at least six genera of bacteria have been cultured from patients with this diagnosis (Gwaltney 2000b).
Respiratory Disease in Operation Enduring Freedom and Operation Iraqi Freedom
About 70% of military personnel deployed to Iraq and Afghanistan in 2003 and the first quarter of 2004 contracted a respiratory infection during their tour of duty, according to the
epidemiologic survey of 15,459 deployed troops described above (Sanders et al. 2005a). A cold or cough characterized nearly all self-reported cases of respiratory illness in that study (Table 4.12). A minority of subjects—2.6%—reported that they had been diagnosed with pneumonia; most of the cases were mild enough to obviate the need for hospitalization. A separate study found that more than 60 cases of pneumonia (severe and mild) occurred among US troops in Iraq from March 1, 2003 to August 20, 2003 (Anderson et al. 2005).
Nineteen deployed troops were hospitalized with acute bilateral pneumonitis with increased concentrations of eosinophils in March-August 2003 (CDC 2003a). All patients required intubation and mechanical ventilation; two ultimately died. The severity of this illness, its unknown cause, and its association with service in southwest and south-central Asia led the military to begin conducting special surveillance for severe acute pneumonia among troops deployed to OEF or OIF.
As of September 2003, laboratory evidence of infection with a pathogen had been identified in four of the 19 patients, as outlined in Table 4.13. In Chapter 6, the committee addresses idiopathic acute eosinophilic pneumonia (a syndrome whose etiology remains unknown).
TABLE 4.12 Impact of Respiratory Illness Among US Military Personnel Deployed to Iraq or Afghanistan, 2003-2004
|
|
Percentage of Troops |
95% Confidence Interval |
|
No. of respiratory infections (cough or cold) during deployment |
|
|
|
None |
30.9 |
27.6-34.4 |
|
1 |
19.1 |
16.4-22.2 |
|
2-3 |
35.6 |
32.3-39.2 |
|
>3 |
14.4 |
12.0-17.2 |
|
Sought medical care for respiratory infection |
17.0 |
14.2-19.8 |
|
Received medicine from provider for respiratory infection |
17.8 |
14.9-20.7 |
|
Self-medicated for respiratory infection |
29.3 |
26.2-32.5 |
|
Experienced allergy attack |
22.5 |
19.4-25.6 |
|
Experienced asthma attack |
3.6 |
2.2-5.0 |
|
Developed pneumonia |
2.6 |
1.4-3.8 |
|
Started or restarted smoking |
47.6 |
41.7-53.6 |
|
No. of packs per day |
|
|
|
None |
61.0 |
57.2-64.7 |
|
½ |
17.5 |
14.6-20.4 |
|
1 |
14.5 |
11.8-17.2 |
|
>1 |
7.0 |
5.1-9.0 |
|
Smoke Iraqi cigarettes |
72.2 |
66.8-77.5 |
|
SOURCE: Adapted with permission from Sanders et al. 2005a. |
||
Table 4.13 Four Cases of Severe Acute Pneumonitis with Evidence of Infectious Etiology
|
Case |
Pathogen detected |
Method of identification |
Probable or suspect infection? |
|
1 |
Streptococcus pneumoniae |
Isolated from sputum culture |
Probable |
|
2 |
S. pneumoniae |
Antigen detected in urine |
Suspect |
|
3 |
Coxiella burnettii |
Serologic evidence |
Suspect |
|
4 |
Acinetobacter baumanii |
Evidence in bronchoscopic culture |
Suspect |
|
SOURCE: CDC 2003a. |
|||
INSECT-BORNE DISEASES
Despite the endemicity of a number of insect-borne diseases in Saudi Arabia, Kuwait, and Iraq in 1990-1991, epidemiologic and laboratory surveillance for such diseases by military medical personnel identified very few cases among US troops who participated in the Gulf War (Richards et al. 1991; Richards et al. 1993b). A few dozen cases of leishmaniasis, malaria, and West Nile fever combined were diagnosed either in the field or after the war. In contrast, military medical facilities have reported more than 1050 cases of arthropod-borne disease—primarily cutaneous leishmaniasis—in troops who served in OEF and OIF. Several factors account for the difference. First, US troops serving in OEF and OIF have been present in southwest and south-central Asia year-round, including the warm seasons, when arthropods are most active. Second, many of the troops have served in or near settings where arthropods thrive, such as urban areas, areas where the infrastructure is dilapidated or destroyed, and estuaries. Finally, the Gulf War lasted only 10 months, whereas OIF and OEF are in their 4th and 5th years, respectively.
Leishmaniasis
Leishmaniasis is the umbrella term for a family of sand-fly-borne parasitic diseases that includes cutaneous leishmaniasis (CL), diffuse cutaneous leishmaniasis, mucocutaneous leishmaniasis (MCL), visceral leishmaniasis (VL, also called kala-azar), and viscerotropic leishmaniasis (VTL).
The signatures of CL are skin lesions that range in severity from small, dry, crusted areas to large, deep, mutilating ulcers. MCL is characterized by lesions that may lead to destruction of the nose, oral cavity, pharynx, and larynx. VL manifests as fever, enlargement of the liver and spleen, anemia, leukopenia, and hypergammaglobulinemia. VTL, a milder form of VL disease, may begin abruptly after infection or weeks to years later; alternatively, infected individuals may be asymptomatic. The acute syndrome is a febrile disorder that may include chronic fatigue and gastrointestinal symptoms; the chronic syndrome might consist of low-grade fever and malaise for several months.
Chapter 5 contains a detailed description of acute leishmaniasis and an analysis of its potential long-term adverse health outcomes. The following text summarizes what has been published about the cases of leishmaniasis contracted during the Gulf War, OEF, and OIF.
Leishmaniasis in the Gulf War
Clinicians at Walter Reed Army Medical Center (WRAMC) in Washington have identified 20 cases of CL and 12 cases of VTL among veterans of the Gulf War (Hyams et al. 1995a; Magill et al. 1993). Because VTL appeared to be clinically distinct from VL and had not
previously been reported in the scientific literature, it has generated a substantial amount of attention and interest.
Viscerotropic Leishmaniasis
Twelve cases of VTL were identified in male US troops who had served in at least five military units in desert or urban locations in Kuwait, Iraq, and eastern Saudi Arabia (Hyams 1999; Magill et al. 1993; Magill et al. 1994). A cluster of these patients apparently became infected near the city of Dhahran along the Persian Gulf coast of Saudi Arabia about 200 miles south of the Saudi-Kuwaiti border (Magill et al. 1993).
From November 1990 to December 1993, 11 patients presented with unexplained fever, chronic fatigue, malaise, cough, intermittent diarrhea, or abdominal pain (Magill et al. 1993). Nine also had adenopathy or mild, transient enlargement of the liver and spleen. Serologic surveys conducted among troops in the same units as the first seven patients identified another infected person who was asymptomatic. Among the first seven cases, primary symptoms presented a median of 7 months after the soldiers had arrived in the Persian Gulf and within 5 months after they had departed. The ninth case became symptomatic, and the diagnosis was made 2 years after he left Saudi Arabia (Magill et al. 1994). The last three cases were identified and diagnosed in 1993 (Hyams 1999).
Leishmanial parasites were cultured from either bone-marrow aspirates or lymph-node biopsies from all 12 patients. With Leishmania-specific indirect immunofluorescent monoclonal antibody or direct fluorescent antibody, it was possible to visualize the parasites in smears of the aspirates or tissue from nine patients (such data were unavailable on three patients). Leishmania tropica, which usually causes CL, was identified through enzyme electrophoresis as the etiologic agent in at least 10 cases; however, none of the 12 patients displayed evidence of CL by either history or physical examination. While undergoing evaluation for leishmaniasis, three patients were found to have underlying conditions: acute retroviral syndrome and HIV seroconversion, renal-cell carcinoma, and acute Epstein-Barr viral infection (CDC 1992; Magill et al. 1993; Magill et al. 1994; Oster and Sanford 1992).
The published literature contains data on the treatment of nine of the 11 symptomatic patients for VTL. One of these patients’ symptoms subsided without treatment; the other eight received parenteral sodium stibogluconate for up to 30 days. Clinicians aborted that treatment in two patients who developed severe thrombocytopenia after 8 and 18 days. The signs and symptoms of VTL resolved in five of the six patients who completed a 30-day course of sodium stibogluconate; after 10 months, the sixth patient underwent elective splenectomy to resolve his condition (CDC 1992; Magill et al. 1993; Magill et al. 1994; Oster and Sanford 1992).
Cutaneous Leishmaniasis
On the basis of the experience of allied forces stationed in Iraq and Iran during World War II, the US military anticipated that troops would be at risk for CL during the Gulf War (Hyams et al. 1995a; Martin et al. 1998). In fact, only 20 cases were recognized and diagnosed (Martin et al. 1998). The very low rate of infection has been attributed to several factors: use of insecticides and repellents; stationing of most combat troops in the open desert, as sand flies and their primary mammalian hosts (desert rodents) thrive in oases and urban areas; and deployment of the majority of ground troops during winter months, when sand flies are least active (Hyams et al. 1995a).
Few specifics about the 20 cases of CL have been published in scientific journals. Locations where patients became infected included from central Saudi Arabia, northeastern Saudi Arabia, and southern Iraq (Kreutzer et al. 1993). The first 17 cases presented with
noduloulcerative disease typical of classic CL; the diagnosis was confirmed with examination of stained smears and cultures of aspirates or of biopsy specimens from the margin of an ulcer (Ohl et al. 1993). In specimens containing enough parasites for evaluation with isoenzyme analysis, L. major was identified as the etiologic agent (Kreutzer et al. 1993; Ohl et al. 1993). It was later determined that L. major caused all 20 cases (Magill 2005). It is unclear whether or how the 20 patients were treated for CL. Most skin lesions caused by L. major do not require treatment, because they heal spontaneously without persistent disfiguration, as described in Chapter 5 (Mandell et al. 2005).
Leishmaniasis in Operation Enduring Freedom and Operation Iraqi Freedom
Published reports and public presentations indicate that more than 1,000 US troops have had a diagnosis of leishmaniasis contracted during a tour of duty in OEF or OIF.
In the anonymous epidemiologic survey of nearly 15,500 troops conducted by Sanders and colleagues and described above, 2.1% of respondents reported receiving a diagnosis of leishmaniasis in 2003 or early 2004 (Sanders et al. 2005a). Extrapolating that finding to the entire force of 140,000 personnel deployed to Iraq and Afghanistan at that time suggests that 2,940 troops may have contracted the disease.
Cutaneous Leishmaniasis in Operation Enduring Freedom and Operation Iraqi Freedom
As of May 2005, military medical personnel had diagnosed and confirmed CL in more than 1,000 military personnel who served in OEF or OIF and were deployed to Afghanistan, Kuwait, or Iraq (Magill 2005; Willard et al. 2005; Zapor and Moran 2005). Each diagnosis was confirmed with light microscopy, culture, PCR assay, or a combination of these. Isoenzyme electrophoresis of cultured parasites from 176 patients consistently revealed L. major to be the etiologic agent in cases from Iraq (CDC 2004b; Magill 2005), and L. tropica caused CL in the cases from Afghanistan (Magill 2005).
Demographic data were collected from 361 patients treated for CL with sodium stibogluconate under an investigational new drug protocol administered at WRAMC (CDC 2004b). Sodium stibogluconate is a pentavalent antimony compound marketed as Pentostam® outside the United States. Although the patients came from multiple branches of the US military, most were in the Army’s active force. It is believed that all but four of the 361 patients were infected in Iraq, particularly along the Iraqi border with Syria and Iran; two soldiers were infected in Kuwait and two in Afghanistan. Nearly 80% of the patients reported that their skin lesions first appeared in August-November 2003. Almost half first noted skin lesions characteristic of CL in September or October.
Staff at WRAMC reported successful treatment of the first 22 patients with 20 mg of sodium stibogluconate per kilogram (kg) of body weight per day by intravenous infusion for 20 days (CDC 2003b). Reversible side effects of the treatment protocol included fatigue, arthralgia, myalgia, headache, and chemical pancreatitis. In addition, a detailed report of 237 soldiers deployed from Fort Campbell, Kentucky, who acquired CL in OIF described diagnosis, clinical presentation, and response to therapy (Willard et al. 2005). It indicated that about 1% of Fort Campbell troops had a diagnosis of CL, that most were laboratory-confirmed, and that PCR was the most useful diagnostic technique. All cases responded to treatment. CL cases resulting from service in OIF are being managed with a variety of approaches, including oral fluconazole, sodium stibogluconate, cryotherapy, and ThermoMed (a device with FDA 510K clearance that delivers localized radiofrequency-generated heat directly to a lesion through a set of prongs placed onto the lesion).
US soldiers deployed to Iraq received dozens or even hundreds of insect bites beginning in April 2003 (Weina et al. 2004). DOD conducted surveillance from April to September 2003 to determine the prevalence of Leishmania-infected female phlebotomine sand flies—the vector for CL—in and near urban and periurban parts of Iraq where US soldiers have been stationed (CDC 2003b). Light traps facilitated the collection of about 65,000 of the flies, about half of them female. A fluorogenic PCR test revealed that 1.4% of the flies were infected with Leishmania spp.; the rate of infection ranged from zero in Diwaniya to 5% in An Nasiriya.
Visceral Leishmaniasis in Operation Enduring Freedom and Operation Iraqi Freedom
As of December 31, 2005, VL has been diagnosed and reported in two soldiers who were stationed in Iraq during OIF and three who participated in OEF (CDC 2004a; Magill 2005; Zapor and Moran 2005).
Case reports describing two of the three OEF soldiers affected by VL indicate that they were previously healthy men in their 30s who had served in the same Special Forces unit of the Army during distinct periods: March-September, 2003 (patient A) and May-October 2002 (patient B) (CDC 2004a). Both men presented with acute febrile illness in December 2003. On initial clinical evaluation, they displayed a few of the classic yet non-specific signs of advanced VL: fever, cachexia, enlarged liver and spleen, pancytopenia, and hypergammaglobulinemia with hypoalbuminemia. No leishmanial parasites were observed on light microscopic examination of bone-marrow and liver-biopsy specimens from patient A, nor were the parasites noted in cultured bone marrow. Genus-specific PCR analysis of the bone-marrow specimen also was negative. Clinicians then evaluated patient A for noninfectious diseases and evidence of infection by other etiologic agents. In February 2004, a combination of clinical and parasitologic criteria enabled clinicians to diagnose VL in patient A. By that time, he manifested all the classic signs of advanced VL. In addition, a re-examination of his liver-biopsy specimen with light microscopy revealed one definite and many probable Leishmania parasites. The etiologic species was not reported. After the first week of a 14-day course of treatment with liposomal amphotericin B (AmBisome®), the patient became afebrile and resumed physical training.
As in the case of patient A, light microscopic examination of a liver-biopsy specimen from patient B yielded positive results for Leishmania parasites. Genus-specific PCR analyses identified the etiologic agent as the L. donovani-infantum complex. A 15-day course of treatment with a lipid formulation of amphotericin B (Abelcet®) temporarily improved patient B’s health, but he relapsed 2 weeks later. Thirty days after completing the first treatment protocol, he began a 28-day course of sodium stibogluconate (20 mg/kg of body weight per day) administered intravenously. The clinical outcome for patient B has not been reported.
The third reported case of VL from OEF was contracted during deployment to Seeb, Oman, in October 2001-March 2002 (Halsey et al. 2004). The patient, a 37-year-old male Air Force sergeant, became ill about 9 weeks after returning to the United States. His illness manifested as fever, chills, malaise, frontal headache, significant loss of weight, and enlarged liver and spleen. A bone-marrow biopsy was smear- and culture-negative for adult Leishmania protozoa (amastigotes) but PCR-positive. In addition, the patient’s serum tested positive for Leishmania-specific immunoglobulin G in a novel enzyme-linked immunosorbent assay (ELISA). Clinicians determined the species to be L. infantum-donovani by using a second PCR assay that had species-specific primers and probes. The patient’s symptoms quickly subsided after he began therapy with liposomal amphotericin B at 3 mg/kg per day on days 1-5, 14, and 21. Four months later, he remained free of symptoms, and his liver was functioning normally.
The two soldiers deployed to Baghdad who contracted VL presented with fever, enlarged liver and spleen, cytopenia, and hypergammaglobulinemia (Weina et al. 2004). On presentation, one had been deployed for 11 months, and the other had left Iraq 7 months earlier. Examination of bone-marrow biopsies from both patients revealed Leishmania parasites. The patients tested positive for Leishmania in an rK39 serologic test; and, their serum yielded titers of 1:1,024 or greater in a Leishmania immunofluorescent antibody test. Using a PCR assay with species-specific primers, clinicians were able to determine the species—L. infantum-donovani—in one case. The treatment protocols and their outcomes were not published.
Malaria
Very few cases of malaria have been reported in US veterans of the Gulf War, OEF, and OIF. That is not surprising because in 1990-1991, malaria had been eliminated from northeastern Saudi Arabia, where most US troops were stationed, and no indigenous malaria transmission occurred in Kuwait, Bahrain, or Qatar (Hyams et al. 1995a; Oldfield et al. 1991). Malaria due to Plasmodium vivax (vivax malaria) occurred in small numbers in northern Iraq during the late 1980s to 1991 (Oldfield et al. 1991). In the wake of the Gulf War, however, Iraq experienced a serious malaria epidemic; by 2000, vivax malaria had become a serious problem in that country (Schlagenhauf 2003). Moreover, the disease is endemic in many parts of Afghanistan.
Publications during the last 15 years about the threat of vivax malaria to US and allied forces in southwest and south-central Asia sound several consistent themes: the seriousness of the disease, shortcomings of chemical and personal countermeasures, and suboptimal rates of compliance with those countermeasures among troops of many nationalities. According to a 1995 report by the Army Medical Surveillance Activity, “after operations in highly endemic areas, sporadic cases [of malaria] may be expected despite compliance with all prevention guidelines” (MSMR 1995).
Malaria in the Gulf War
Vivax malaria existed in the Euphrates River valley of Iraq in 1990 and 1991 (Young et al. 1992). Seven cases of vivax malaria were reported among US troops who crossed into southern Iraq, where coalition forces operated briefly (Hyams et al. 1995a). No information was given on complications in those troops.
Malaria in Operation Enduring Freedom and Operation Iraqi Freedom
As of May 2005, 52 cases of vivax malaria had been reported in US troops who served either exclusively in Afghanistan or in both Afghanistan and Iraq (Kilpatrick 2005). It is believed that all 52 infections were contracted in Afghanistan, although Plasmodium vivax is endemic in areas of both countries (Wallace et al. 2002). None of the patients was diagnosed with malaria prior to leaving the war theater; this is not surprising, because vivax malaria is known to incubate in human hosts and may relapse up to 5 years after initial infection (Boecken and Bronnert 2005; Johnson 2004).
Thirty-eight of the 52 reported cases of vivax malaria occurred in a 725-man Army Ranger task force deployed to eastern Afghanistan in June-September 2002. Kotwal and colleagues, the primary-care clinicians for these rangers, collected and later analyzed data from the patients during their evaluation, treatment, and followup. In addition, a retrospective anonymous survey was administered to the whole task force in July 2003 to ascertain compliance
with malarial countermeasures. Retrospective analysis led the authors to conclude that the 38 rangers became infected while working at two specific forward-operating bases during summer 2002 (Kotwal et al. 2005).
The antimalarial chemoprophylaxis prescribed for this Army Ranger task force consisted of 250-mg mefloquine tablets ingested weekly beginning 2 weeks before deployment and ending 4 weeks after deployment. To prevent the late onset of malaria, the troops also were instructed to ingest one 15-mg primaquine tablet daily for 2 weeks after deployment. In addition, it is expected that all US soldiers at risk of malaria are trained and supplied to minimize their exposure to mosquitoes by impregnating their uniforms and bed nets with permethrin, wearing the uniforms properly, using the bed nets, and frequently coating exposed skin with insect repellent that contains 33% DEET (Johnson 2004; Kotwal et al. 2005).
The first three rangers to become symptomatic had vivax malaria diagnosed in March and April 2003. Fifteen more rangers fell ill and had diagnoses in May; the remaining 20 cases came to light in June-November 2003 (Lay 2005). The attack rate for the 725-person task force was 52.4 cases per 1,000 soldiers.
P. vivax infection causes flu-like symptoms that are often severe and debilitating (Boecken and Bronnert 2005; Spudick et al. 2005). Most of the infected rangers presented with fever; many also complained of chills, headache, muscle aches, or nausea. A complete blood-cell count obtained for 31 of the patients demonstrated that most had mild to moderate anemia and thrombocytopenia. The attending physicians based their initial diagnoses on those clinical signs and symptoms. Each case was confirmed with microscopic visualization of malaria parasitemia in the patient’s red blood cells on laboratory-prepared blood smears. A median of 233 days (range, 1-399 days) elapsed between these soldiers’ return from the theater of war and confirmation of their diagnoses.
Two rangers relapsed after completing their first treatment regimen. One of those cases was complicated by life-threatening acute respiratory distress syndrome (ARDS) during the primary attack; the patient relapsed three times from June to December 2003. The multiple relapses indicated infection with primaquine-tolerant P. vivax (Spudick et al. 2005). Pulmonary complications, such as ARDS, might occur with vivax malaria more frequently than is generally recognized.
The results of the anonymous postdeployment survey reported by Kotwal and colleagues indicate that at least 72% of the 725-member task force complied poorly with most of the malarial countermeasures described above (Kotwal et al. 2005). Some 52% followed the US Army guidelines for mefloquine, 41% for primaquine, and 31% for both; 82% reportedly treated their uniforms with permethrin, but only 29% routinely applied DEET to exposed skin. Delayed presentation of vivax malaria is well described, primarily in people who fail to take primaquine as terminal prophylaxis after returning from malaria-endemic areas of the Middle East (Gasser et al. 1991).
Only 14 cases of malaria were reported in US troops in 2004, a 63% decrease from the year before (Lay 2005). All the cases were caused by P. vivax infection and were contracted in Afghanistan (Kilpatrick 2005), and they presented sporadically from February to November.
Kotwal and colleagues suggest that continuously educating field troops about the importance of countermeasures and having leaders monitor and enforce the use of chemoprophylaxis and personal protective measures might further reduce the occurrence of malaria among US forces (Kotwal et al. 2005). At the same time, they and others note several shortcomings of the countermeasures themselves (Boecken and Bronnert 2005; Kotwal et al.
2005; Spudick et al. 2005). Avoiding mosquito bites in the field is difficult and somewhat impractical. For example, nighttime patrols, use of night-vision devices, and vigilance during dusk and dawn place troops at higher risk of exposure to nocturnally active Anopheles mosquitoes, the vectors of malarial parasites, in endemic areas. Permethrin-impregnated bed nets have no utility for soldiers who are at work at night.
West Nile Fever
West Nile virus belongs to the Japanese encephalitis virus antigenic complex in the genus Flavivirus of the family Flaviviridae. Mosquitoes transmit West Nile virus, which was first isolated in 1937 from a febrile woman in the West Nile Province of Uganda. Although 80% of infected people are asymptomatic, those who develop clinical disease usually present with a nonspecific febrile illness lasting 3-6 days. Chapter 5 contains an in-depth discussion of this disease.
West Nile Fever in the Gulf War
Only one person who served in the Gulf War had a diagnosis of West Nile fever due to an infection contracted during the war (Richards et al. 1991). The patient was hospitalized with acute fever, debility, and arthralgias; these symptoms subsided without therapy after 4 days. Clinicians at the US Navy Forward Laboratory in Saudi Arabia tested the patient’s serum with ELISA for immunoglobin M (IgM) and IgG antibodies to the etiologic agents of nine viral and rickettsial diseases: Congo-Crimean hemorrhagic fever, dengue fever, hantaviral disease (Hantaan virus), Q fever, Rift Valley fever, Sindbis, sand fly fever, typhus, and West Nile fever. The serum tested IgM-positive for West Nile virus, but IgM- and IgG-negative for the other arboviruses.
A separate study designed to determine the incidence of insect-borne infections among Gulf War troops identified 30 marines who had been infected with a flavivirus before deployment to Saudi Arabia (Richards et al. 1993b). In the study, an epidemiologic questionnaire was administered and a blood sample obtained from each of 865 marines just before deployment and immediately after. The serum samples were initially screened with ELISA for Crimean-Congo hemorrhagic fever, Rift Valley fever, sand fly fever, Sindbis, West Nile fever, and rickettsiae in the typhus and spotted-fever groups. Moderately increased titers of IgG to West Nile virus in the predeployment and postdeployment serum of 30 marines led investigators to test those blood samples for antibodies to other flaviviruses (for example, St. Louis encephalitis, dengue, and yellow fever viruses). Sera from those marines were reactive to the other flaviviruses.
West Nile Fever in Operation Enduring Freedom and Operation Iraqi Freedom
As of December 2005, there were no reported cases of West Nile fever in military personnel deployed to OEF or OIF.
BRUCELLOSIS
Brucellosis is a serious zoonotic disease endemic in many parts of the world including southwest and south-central Asia (Mandell et al. 2005). The etiologic agent, Brucella spp., has numerous mammalian reservoirs; infected animal hosts shed the bacteria in their milk and urine.
Humans can contract the disease by ingesting unpasteurized dairy products, by way of infected aerosols inhaled or inoculated into the conjunctival sac of the eyes, and through direct contact between animals or their secretions and cut or abraded skin.
Among all US soldiers who participated in the Gulf War, OEF, and OIF, only one case of brucellosis has been diagnosed (Andrews 2004). An Army helicopter pilot became ill in July 2004 about a week after he completed a 5-month tour of duty in Iraq and returned to his unit in Würzburg, Germany. His initial symptoms of malaise, intermittent chills and fevers as high as 103.9°F, and profuse sweating worsened during the next 5 days despite unspecified “symptomatic treatment” and a day of hospitalization. The patient was readmitted to Würzburg Army Hospital on day 5. Antibodies to B. abortus were identified through laboratory analysis of an unspecified tissue specimen. In addition, a Brucella isolate later identified as B. melitensis was isolated from the patient’s blood. Medical personnel then diagnosed brucellosis. The case report on this patient lacks a description of the course of treatment administered, but the report notes that the patient completed a 14-day course of primaquine after redeploying (presumably to Iraq). The report also notes that the patient had taken chloroquine as malaria prophylaxis but missed his last weekly dose. Epidemiologic questioning of the patient identified only one possible source of the infection: observing the slaughter of a sheep in Iraq.
CHICKENPOX (VARICELLA)
Seventy-five US military personnel who served in ODSh or ODSt were hospitalized for chickenpox during their deployment (Smith et al. 2004). Although it is typically benign in children, chickenpox may cause a more severe disease in adults that might include pneumonitis, hepatitis, and encephalitis. Indeed, the disease kills one in 5,000 infected adults (Heymann 2004). A common complication is bacterial suprainfection, usually of the skin (Military Vaccine Agency 2005b). In 1995, the US Food and Drug Administration licensed a vaccine for this disease.
MENINGOCOCCAL DISEASE
Infectious diseases reportedly caused only one death among US troops deployed to ODSh or ODSt: a fatal case of meningococcal meningitis (Hyams et al. 2001a; Writer et al. 1996). No further information has been published about the death. The literature mentions a second, nonfatal case of meningococcal disease during ODSh or ODSt (Hyams et al. 1995a), but validating evidence is absent. The committee is unaware of other published literature on cases or outbreaks of meningococcal disease among US troops deployed to southwest and south-central Asia during the conflicts discussed in this report.
NOSOCOMIAL INFECTIONS
Gulf War
The committee is unaware of any reports of nosocomial infection among US troops deployed to the Persian Gulf region for ODSh or ODSt. About 470 military personnel who served in those operations suffered nonmortal wounds (Department of Defense 2005).
Operation Enduring Freedom and Operation Iraqi Freedom
More than 16,600 military personnel deployed to OEF and OIF have suffered nonmortal wounds (Defense Manpower Data Center 2006). Many of these troops lost limbs or parts of limbs as a result of explosions that caused traumatic or surgical amputation (Davis et al. 2005). Soil- and water-dwelling bacteria, including Acinetobacter baumanii, have colonized and infected many soldiers’ amputation sites and other blast wounds (Zapor and Moran 2005). Indeed, orthopedic war wounds have become the most common reason for infectious-disease consultations since September 2001 at WRAMC (Zapor and Moran 2005). Cultured specimens from wounds have often implicated a multiple-drug-resistant strain of A. baumanii (Zapor and Moran 2005).
A. baumanii has long been a cause of nosocomial infections. Infected battle injuries from OEF and OIF, however, have increased the rate of bloodstream infections by A. baumanii by more than 2,000% at two major US military hospitals (Table 4.14) (CDC 2004c). Moreover, some strains of A. baumanii have demonstrated resistance to all but one antimicrobial agent in the present pharmacologic arsenal—colistin, a toxic drug (CDC 2004c).
The active-duty military personnel described below, who were generally young and healthy before sustaining war wounds, usually recovered from A. baumanii infection after receiving medical treatment.
TABLE 4.14 Increase in Incidence of A. baumannii Bloodstream Infections at Two Military Hospitals, 2000-2004
|
|
No. Cases |
|
|
|
Hospital |
pre-2003 |
January 2003-August 2004 |
Percentage Increase in No. Cases |
|
Walter Reed Army Medical Center |
2 (2001-2002) |
45 |
2,150 |
|
Landstuhl Regional Medical Center |
1 (2000-2002) |
33 |
3,200 |
|
SOURCE: Scott et al. 2004. |
|||
Case Series 1:
Brooke Army Medical Center
From March 1, 2003, to May 31, 2004, Brooke Army Medical Center (BAMC), in Houston, Texas admitted 151 injured active-duty soldiers who had been deployed to OEF or OIF (Davis et al. 2005). Davis and colleagues report that all patients but one had previously been admitted to Landstuhl Regional Medical Center (LRMC) in Landstuhl, Germany; three had also been admitted to a second US Army medical facility before BAMC.
Of the tissue samples obtained from 84 of those patients, 48 (32%) tested positive for Acinetobacter calcoaceticus-baumanii complex; 30 patients (63% of those colonized) were clinically infected, and 23 met the case definition for either Acinetobacter osteomyelitis or Acinetobacter wound infection (Table 4.15). None had been diagnosed with Acinetobacter spp. before evacuation from Iraq or Afghanistan.
All but one of the 23 patients with Acinetobacter osteomyelitis or Acinetobacter wound infection received parenteral antimicrobial drug treatment selected to match the susceptibility of the infecting A. baumanii strain (Table 4.16). The primary therapeutic challenge was antimicrobial resistance. Most patients with Acinetobacter osteomyelitis underwent a 6- to 8-week course of drug therapy complemented by multiple surgical debridements of necrotic bone; one patient was treated with surgical debridement alone. Drug therapy for 10 of the osteomyelitis patients involved two antimicrobials, usually imipenem and amikacin. In contrast, patients with
Acinetobacter wound infection received just one antimicrobial, generally for 10-16 days. All patients responded to therapy. Their followup had lasted a mean of 9 months (range, 1-23 months) at the time the report was published.
TABLE 4.15 Type of Acinetobacter Infection in 23 Wounded Soldiers Admitted to BAMC, March 2003-May 2004, and Therapies Received
|
Type of Infection |
No. cases |
|
Acinetobacter osteomyelitis |
15 |
|
Acinetobacter osteomyelitis with bacteremia |
3 |
|
Acinetobacter burn infection |
2 |
|
Acinetobacter deep wound infection |
3 |
|
SOURCE: Davis et al. 2005. |
|
TABLE 4.16 Antimicrobial Drug Susceptibilities for 38 Isolates of Acinteobacter calcoaceticu-baumannii Complex Recovered from Wound or Blood Cultures
|
Antimicrobial Drug |
Percentage of Susceptible Isolates |
|
Amikacin |
48 |
|
Amoxicillin/clavulanate |
9 |
|
Ampicillin/sulbactam |
50 |
|
Cefepime |
14 |
|
Cefotetan |
3 |
|
Ceftazidime |
12 |
|
Ceftriaxone |
6 |
|
Ciprofloxacin |
11 |
|
Colistina |
100 |
|
Gentamicin |
8 |
|
Imipenem |
89 |
|
Tobramycin |
14 |
|
Trimethoprim/sulfamethoxazole |
29 |
|
a Colistin susceptibility evaluated in three multiple-drug-resistant isolates. SOURCE: Davis et al. 2005. |
|
Case Series 2:
Walter Reed Army Medical Center and Landstuhl Regional Medical Center
Scott and colleagues report the identification of A. baumannii bloodstream infections in 102 patients at five military hospitals where active-duty military personnel injured in OEF or OIF received treatment (CDC 2004c). The cases were identified from January 1, 2002, to August 31, 2004. Table 4.17 displays the number of infected patients per hospital, their age range, and the subset who that been admitted with (mostly traumatic) injuries associated with OEF or OIF. At both WRAMC and LRMC, clinicians identified a significant percentage of A. baumannii bloodstream infections associated with activities in OEF or OIF within 48 hours of admission (62% at WRAMC and 67% at LRMC). The 78 A. baumanii isolates obtained from patients at WRAMC and LRMC manifested varied levels of resistance to antimicrobial agents commonly used to treat such infections (Table 4.18).
DOD has reportedly taken a number of actions to avert a widespread outbreak of A. baumanii nosocomial infections in military medical treatment facilities that serve troops deployed to OEF and OIF. The department has developed clinical management and wound-care guidelines to help clinicians prevent and mitigate A. baumanii infections in military treatment facilities and has launched an investigation into the sources of the pathogen. It is also conducting laboratory surveillance for A. baumanii at four major military hospitals in the United States and Germany and, to the extent possible, at US military medical treatment facilities on the ground in Iraq, Kuwait, and Afghanistan (CDC 2004c). Preliminary data have reportedly linked environmental isolates of A. baumanii obtained from field hospitals to patient isolates obtained during both surveillance and clinical evaluation (Zapor and Moran 2005).
TABLE 4.17 Cases of A. baumanii Infection Identified in Five Military Hospitals, January 2002-August 2004
|
Hospital |
No. Cases |
Median Age (Range) (years) |
No. (%) Casualties Associated with OEF or OIF |
|
|
Walter Reed Army Medical Center |
45 |
30 (19-72) |
29 |
(64) |
|
Landstuhl Regional Medical Center |
33 |
39 (6-86) |
32 |
(97) |
|
Brooke Army Medical Center |
5 |
NP |
5 |
(100) |
|
National Naval Medical Center |
8 |
NP |
8 |
(100) |
|
USNS Comfort |
11 |
NP |
11 |
(100) |
|
TOTAL |
102 |
--- |
85 |
--- |
|
NOTE: NP = not published in the source article. SOURCE: Scott et al. 2004. |
||||
TABLE 4.18 Pattern of Antimicrobial Susceptibility among Strains of A. baumanii Isolated from Patients with Bloodstream Infections at WRAMC and LRMC, January 2002-August 2004
|
Antimicrobial Drug |
Percentage of Susceptible Isolates |
|
|
WRAMC (N = 45) |
LRMC (N = 33) |
|
|
Imipenem |
82 |
87 |
|
Amikacin |
48 |
80 |
|
Ampicillin/sulbactam |
35 |
8 |
|
Piperacillin/tazobactam |
27 |
0 |
|
Cefepime |
22 |
0 |
|
Ciprofloxacin |
20 |
3 |
|
NOTE: WRAMC = Walter Reed Army Medical Center, LRMC = Landstuhl Regional Medical Center. SOURCE: Scott et al. 2004. |
||
Q FEVER
Q fever is a zoonotic disease endemic in southwest and south-central Asia (Wallace et al. 2002). The clinical syndrome may be acute or chronic. The acute illness usually manifests as a nonspecific febrile illness, pneumonia (sometimes atypical pneumonia), hepatitis, or a combination of the three; occasionally, it presents as acute meningitis or encephalitis. Chronic Q fever usually presents as endocarditis, granulomatous hepatitis, or vertebral osteomyelitis. Q
fever frequently goes undiagnosed in humans; many cases are presumably subclinical or asymptomatic.
Cattle, sheep, and goats are the main reservoirs of the disease, which is caused by the bacterium Coxiella burnetii. A single organism can constitute an infectious dose. C. burnetii most frequently infects humans who inhale infected aerosolized body fluids of infected animals; the consumption of raw milk from C. burnetii-infected animals also has caused Q fever in humans.
Three cases of Q fever were reported in US troops who participated in the Gulf War (Hyams et al. 1995a), and 10 cases have been diagnosed in troops deployed to Iraq (Kilpatrick 2005).
Q Fever Contracted During the Gulf War
A case report about one of the three Gulf War troops who had a diagnosis of Q fever has been published (Ferrante and Dolan 1993). A 51-year-old man who had been involved in the ground war in ODSt presented with focal neurologic deficits suggestive of transient ischemic attacks in a crescendo pattern. Two weeks before the onset of symptoms, the patient had returned from Saudi Arabia, where he frequently worked around camels and had once driven a vehicle past a flock of sheep.
The first evaluation of the patient’s cerebrospinal fluid (CSF) yielded an abnormal profile consistent with aseptic meningitis; however the sample was culture-negative for bacteria, fungi, and mycobacteria. Clinicians obtained two more CSF samples at 10 and 14 days; serology from the last puncture yielded a positive C. burnetii IgM indirect fluorescent antibody (IFA) titer consistent with recent Q fever infection. CDC confirmed that result, and Q fever meningoencephalitis was diagnosed. It is believed that the patient contracted the disease in Saudi Arabia through exposure to infected camels or sheep.
Clinicians treated the patient with a 21-day course of oral doxycyline (100 mg twice a day). Six weeks after the first lumbar puncture, serology for C. burnetii IgM IFA titer was negative. No further neurologic sequelae occurred during 12 months of followup.
Q Fever Contracted During Operation Enduring Freedom and Operation Iraqi Freedom
Ten cases of Q fever have been diagnosed in troops serving in OIF as of December 2005. All the patients became infected in northern Iraq (Kilpatrick 2005). We summarize here a report of about eight of the 10 cases; we are unaware of reports in the public literature about the other two patients.
During an investigation of a cluster of 19 cases of severe pneumonia in US troops serving in Iraq, extensive serologic testing for possible infectious etiologies revealed that three patients had positive antibody titers for C. burnetii by immunofluorescence assay (Anderson et al. 2005). The three patients’ predeployment serum samples were negative in the same test. The results led investigators to examine whether C. burnetii accounted for other cases of pneumonia among military personnel deployed to Iraq during the same period (March 1-August 20, 2003).
Predeployment and postdeployment serum samples were available for 22 of 62 soldiers who had pneumonia diagnosed in Iraq. Serum was tested by immunofluorescence assay for phase I and phase II antibody to C. burnetii. Five of the 22 soldiers had seroconverted to C. burnetii before their postdeployment serum draws, leading the investigators to conclude that they also had contracted Q fever in the period March 1-August 20, 2003.
All eight patients in this study first sought medical care while stationed in northern Iraq. The first three patients were in northern Iraq when their symptoms of pneumonia began. The investigators postulated that humans may be at greater risk of contracting Q fever in northern Iraq owing to the larger concentrations of livestock that may exist there because the land is favorable for ruminants to graze. One of the first three patients reported drinking raw sheep’s milk, two reported tick bites within 30 days of becoming ill, and all three reported contact with dogs, cats, sheep, goats, and camels (potential reservoirs of C. burnetii).
VIRAL HEPATITIS
Clinicians diagnosed a few cases of hepatitis A and B among deployed US troops during the Gulf War, according to Hyams and colleagues (Hyams et al. 1995a); the exact number of cases is unclear. The committee is unaware of published reports about those cases. The hospitalization rates for acute hepatitis among all active-duty military personnel in 1990 and 1991 were 187 per 100,000 and 168 per 100,000 respectively (Table 4.19) (Hyams et al. 2001b). The data do not indicate how many cases were associated with participation in ODSh or ODSt.
Staff at the Armed Forces Institute of Pathology diagnosed one case of hepatitis B and 15 cases of hepatitis C among Gulf War veterans from 1992 to 1997 (Specht et al. 2000). The investigators reportedly lacked the data to determine whether the patients had contracted hepatitis before, during, or after the war.
Hepatitis A and B vaccination policies differ among the services (IOM 1996). In the past, the Army, Navy, Marine Corps, and Coast Guard administered the hepatitis A vaccine as directed by the applicable surgeon general or the commandant of the Coast Guard; the Air Force vaccinated its personnel against hepatitis A when deploying them to a high-risk area. As of 1996, all services administered the hepatitis B vaccine to personnel in high-risk occupational groups or as directed by the applicable surgeon general or the commandant of the Coast Guard. More recently, DOD policy requires that all personnel be vaccinated for hepatitis A (Department of Defense 2006a; Military Vaccine Agency 2005a) and Army policy requires that all deployed personnel be vaccinated for hepatitis B (Department of the Army 2005a).
TABLE 4.19 Age- and Sex-Adjusted Hospitalization Rates per 100,000 Personnel for Acute Hepatitis Among Active Duty U.S. Military Forces, 1990 and 1991
|
Year |
Acute Hepatitis A |
Acute Hepatitis B |
Acute Hepatitis C |
Acute Unspecified Viral Hepatitis |
Total |
|||||
|
No. |
Rate |
No. |
Rate |
No. |
Rate |
No. |
Rate |
No. |
Rate |
|
|
1990 |
113 |
3.52 |
0 |
-- |
0 |
-- |
75 |
3.08 |
187 |
6.56 |
|
1991 |
74 |
2.87 |
25 |
0.96 |
1 |
0.05 |
72 |
3.07 |
168 |
6.75 |
|
SOURCE: Adapted with permission from Hyams et al. 2001a. |
||||||||||
TUBERCULOSIS
No cases of active tuberculosis (TB) were recognized in military personnel who served in ODSt and ODSh (Hyams et al. 1995a). In many soldiers in some units, however, tuberculin skin tests (TSTs) were negative before the Gulf War and positive afterward (Oster and Sanford 1992). Among military personnel deployed to OEF and OIF, approximately 2.5 percent of those given pre- and post-deployment TSTs converted from negative to positive (Kilpatrick 2005). TST
conversion is pathognomonic of acute infection with Mycobacterium tuberculosis; thus, transmission of M. tuberculosis occurred within some military units deployed to southwest and south-central Asia. Immunocompetent individuals who become infected with M. tuberculosis face a 10 percent lifetime risk for developing active TB in the absence of prophylactic treatment. The committee discusses TB at length in Chapter 5.
DEPARTMENT OF DEFENSE MEDICAL DATABASES
On January 10, 2006, IOM submitted a request to DOD to conduct a search of the Defense Medical Surveillance System (DMSS) database (described in Rubertone and Brundage (2002)) for numbers of cases of infectious diseases coded by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The request included searching for infectious diseases diagnosed in military personnel deployed to the Gulf War, OIF, and OEF. DOD approved IOM’s request on January 20. Because the DMSS database does not contain many data pertaining to in-theater morbidity during the Gulf War, DOD recommended that an additional search be conducted with a different DOD database on Gulf War in-theater hospitalization data.
On June 2, 2006, IOM received the results of the search of the Gulf War in-theater hospitalization database. Those results are presented in Table 4.20. DOD developed the database to investigate in-theater hospitalizations during the Gulf War (Smith et al. 2004). It contains records from almost 20,000 admissions occurring in the Kuwaiti theater of operations and evacuated admissions to hospitals in Europe. The committee reviewed the search results and determined that the results would not have changed the committee’s approach to its charge or conclusions.
At the time of completion of this report, IOM had not received the results of the DMSS database search on infectious diseases diagnosed during OIF and OEF.
TABLE 4.20 Numbers of Cases of Infectious Diseases in the Gulf War In-Theater Hospitalization Database
|
ICD-9CM Category |
Disease |
No. Cases |
|
003.0 |
Salmonella gastroenteritis |
9 |
|
003.9 |
Salmonella infection, unspecified |
2 |
|
004.9 |
Shigellosis, unspecified |
3 |
|
005.0 |
Staphylococcal food poisoning |
2 |
|
005.9 |
Food poisoning, unspecified |
18 |
|
006.0 |
Acute amebic dysentery without mention of abscess |
3 |
|
006.8 |
Amebic infection of other sites |
3 |
|
006.9 |
Amebiasis, unspecified |
14 |
|
008.5 |
Bacterial enteritis, unspecified |
6 |
|
008.69 |
Other viral enteritis |
2 |
|
008.8 |
Intestinal infection due to other organism, not elsewhere classified |
86 |
|
009.0 |
Infectious colitis, enteritis, and gastroenteritis |
23 |
|
009.1 |
Colitis, enteritis, gastroenteritis, presumed infectious origin |
2 |
|
009.2 |
Infectious diarrhea |
34 |
|
009.3 |
Diarrhea of presumed infectious origin |
4 |
|
011.60 |
Tuberculous pneumonia (any form), unspecified examination |
1 |
|
011.90 |
Unspecified pulmonary tuberculosis, unspecified examination |
1 |
|
034.0 |
Streptococcal sore throat |
19 |
|
ICD-9CM Category |
Disease |
No. Cases |
|
035 |
Erysipelas |
1 |
|
038.10 |
Staphylococcal septicemia, unspecified |
1 |
|
038.9 |
Unspecified septicemia |
2 |
|
040.0 |
Gas gangrene |
1 |
|
041.10 |
Staphylococcus, unspecified, in condition classified elsewhere |
1 |
|
041.4 |
Escherichia coli infection |
1 |
|
042 |
Human immunodeficiency virus disease |
2 |
|
047.9 |
Unspecified viral meningitis |
3 |
|
048 |
Other enterovirus diseases of the central nervous system |
1 |
|
052.1 |
Varicella (hemorrhagic) pneumonitis |
1 |
|
052.7 |
Chickenpox with other specified complications |
1 |
|
052.8 |
Chickenpox with unspecified complication |
3 |
|
052.9 |
Varicella without mention of complication |
64 |
|
053.8 |
Herpes zoster with unspecified complication |
1 |
|
053.9 |
Herpes zoster without mention of complication |
11 |
|
054.10 |
Genital herpes, unspecified |
2 |
|
054.19 |
Other genital herpes |
1 |
|
054.2 |
Herpetic gingivostomatitis |
2 |
|
054.43 |
Herpes simplex disciform keratitis |
3 |
|
054.79 |
Herpes simplex with other specified complications |
1 |
|
054.9 |
Herpes simplex without mention of complication |
1 |
|
055.9 |
Measles without mention of complication |
1 |
|
057.8 |
Other specified viral exanthemata |
1 |
|
057.9 |
Viral exanthem, unspecified |
1 |
|
066.0 |
Phlebotomus fever |
5 |
|
070.10 |
Viral hepatitis A without mention of a hepatic coma, lab test confirmed |
4 |
|
070.30 |
Viral hepatitis B without coma, acute/ unspecified without hepatic delta, lab test confirmed |
6 |
|
070.9 |
Unspecified viral hepatitis without hepatic coma |
3 |
|
072.9 |
Mumps without mention of complication |
1 |
|
074.1 |
Epidemic pleurodynia |
1 |
|
075 |
Infectious mononucleosis |
27 |
|
077.8 |
Other viral conjunctivitis |
3 |
|
078.10 |
Other diseases due to viruses and chlamydiae, viral warts, unspecified |
29 |
|
078.11 |
Other diseases due to viruses and chlamydiae, condyloma acuminatum |
9 |
|
078.19 |
Other diseases due to viruses and chlamydiae, other specified viral warts |
6 |
|
079.89 |
Other specified viral infections |
5 |
|
079.98 |
Unspecified chlamydial |
1 |
|
079.99 |
Unspecified viral infections |
299 |
|
084.1 |
Vivax malaria (benign tertian) |
7 |
|
084.6 |
Malaria, unspecified |
4 |
|
085.0 |
Leishmaniasis visceral (kala-azar) |
1 |
|
085.1 |
Cutaneous leishmaniasis, urban |
1 |
|
085.9 |
Leishmaniasis, unspecified |
2 |
|
091.3 |
Secondary syphilis of skin or mucous membranes |
1 |
|
091.50 |
Syphilitic uveitis, unspecified |
1 |
|
098.0 |
Acute gonococcal infection, lower genito-urinary tract |
1 |
|
098.16 |
Acute gonococcal endometritis |
1 |
|
099.3 |
Reiter's disease |
6 |
DEPARTMENT OF DEFENSE POLICY REGARDING PREDEPLOYMENT AND POSTDEPLOYMENT SERUM COLLECTION
DOD policy specifies that “predeployment serum specimens for medical examinations will routinely be collected within one year of deployment” and that “postdeployment serum specimens for medical examinations will be collected no later than 30 days after arrival at the demobilization site, home station, or in-patient medical treatment facility” (Department of Defense 2006b). Predeployment and postdeployment serum samples are required for all deployments outside the continental United States that are longer than 30 days and to areas without fixed US medical treatment facilities (Kilpatrick 2006). The serum samples are stored indefinitely at the DOD Serum Repository.
Routine testing of the serum samples is not conducted except testing for HIV (Kilpatrick 2006). However, the serum samples have been used for research studies (for example, on Lyme disease, Helicobacter pylori infection, and leishmaniasis), and for operational studies (for example, on severe acute pneumonia cases during OIF, malaria among Marines in Liberia, and WNV).
The committee agrees with DOD’s overall policy regarding collection and use of serum specimens. However, for banked serum specimens to be most useful for determining whether infectious exposures occurred during deployment, the predeployment specimens need to be collected before travel. Current policy allows for collection of predeployment serum specimens up to a year after deployment. If specimens are not collected until after deployment, it would be difficult to ascertain whether any signs of infection found in the “predeployment” specimens are due to exposure during the current deployment or before it.
REFERENCES
Anderson AD, Smoak B, Shuping E, Ockenhouse C, Petruccelli B. 2005. Q fever and the US military. Emerging Infectious Diseases 11(8):1320-1322.
Andrews RB. 2004. Brucellosis in a soldier who recently returned from Iraq. Medical Surveillance Monthly Report 10(4):30.
Boecken GH, Bronnert J. 2005. Pathogenesis and management of a late manifestation of vivax malaria after deployment to Afghanistan: Conclusions for NATO Armed Forces Medical Services. Military Medicine 170(6):488-491.
CDC (Centers for Disease Control and Prevention). 1992. Viscerotropic leishmaniasis in persons returning from Operation Desert Storm—1990-1991. Morbidity and Mortality Weekly Report 41(8):131-134.
CDC. 2003a. Severe Acute Pneumonitis Among Deployed US Military Personnel—Southwest Asia, March—August 2003. Morbidity and Mortality Weekly Report 52(36):857-859.
CDC. 2003b. Cutaneous leishmaniasis in US military personnel—Southwest/Central Asia, 2002-2003. Morbidity and Mortality Weekly Report 52(42):1009-1012.
CDC. 2004a. Two cases of visceral leishmaniasis in US military personnel—Afghanistan, 2002-2004. Morbidity and Mortality Weekly Report 53(12):265-268.
CDC. 2004b. Update: Cutaneous leishmaniasis in US military personnel—Southwest/Central Asia, 2002-2004. Morbidity and Mortality Weekly Report 53(12):264-265.
CDC. 2004c. Acinetobacter baumannii infections among patients at military medical facilities treating injured US service members, 2002-2004. Morbidity and Mortality Weekly Report 53(45):1063-1066.
Davis KA, Moran KA, McAllister CK, Gray PJ. 2005. Multidrug-resistant Acinetobacter extremity infections in soldiers. Emerging Infectious Diseases 11(8):1218-1224.
Defense Manpower Data Center. Military Casualty Information. [Online]. Available: http://www.dior.whs.mil/mmid/casualty/castop.htm [accessed March 2006].
Department of the Army. 2005a. Medical Screening of Personnel Mobilized for Deployment or Deployed in Support of Contingency Operations (Predeployment Screening Requirements). Falls Church, VA: Office of the Surgeon General.
Department of the Army. 2005b. Release of Actionable Medical Information Policy Memorandum. Fort Sam Houston, TX: Headquarters, United States Army Medical Command.
DOD (Department of Defense). 2005. Principal Wars in Which the United States Participated US Military Personnel Serving and Casualties A. [Online]. Available: http://www.dior.whs.mil/mmid/casualty/WCPRINCIPAL.pdf [accessed March 2006].
DOD. 2006a. Individual Medical Readiness. Department of Defense Instruction. Washington, DC.
DOD. 2006b. Policy for Pre- and Post-Deployment Serum Collection. Washington, DC: Assistant Secretary of Defense.
Donowitz GR, Mandell GL. 2000. Acute pneumonia. In: Mandell GL, Bennett JE, Dolin R, Editors. Principles and Practice of Infectious Diseases. 5th ed. New York: Churchill Livingstone. Pp. 717-743.
Ferrante MA, Dolan MJ. 1993. Q fever meningoencephalitis in a soldier returning from the Persian Gulf War. Clinical Infectious Diseases 16(4):489-496.
Gasser RA Jr, Magill AJ, Oster CN, Tramont EC. 1991. The threat of infectious disease in Americans returning from Operation Desert Storm. New England Journal of Medicine 324(12):859-864.
Gwaltney JM, Jr. 2000a. Acute Bronchitis. In: Mandell GL, Bennett JE, Dolin R, Editors. Principles and Practice of Infectious Diseases. 5th ed. New York: Churchill Livingstone. Pp. 703-706.
Gwaltney JM, Jr. 2000b. Sinusitis. In: Mandell GL, Bennett JE, Dolin R, Editors. Principles and Practice of Infectious Diseases. 5th ed. New York: Churchill Livingstone. Pp. 676-686.
Haberberger RL, Scott DA, Thornton SA, Hyams KC. 1994. Diarrheal disease aboard a US Navy ship after a brief port visit to a high risk area. Military Medicine 159(6):445-448.
Halsey ES, Bryce LM, Wortmann GW, Weina PJ, Ryan JR, DeWitt CC. 2004. Visceral leishmaniasis in a soldier returning from Operation Enduring Freedom. Military Medicine 169(9):699-701.
Heymann DL. 2004. Control of Communicable Diseases Manual. Washington, DC: American Public Health Association.
Hyams KC. 1999. Gulf War Syndrome: Potential role of infectious diseases. Current Opinion in Infectious Diseases 12(5):439-443.
Hyams KC, Bourgeois AL, Merrell BR, Rozmajzl P, Escamilla J, Thornton SA, Wasserman GM, Burke A, Echeverria P, Green KY, et al. 1991. Diarrheal disease during Operation Desert Shield. New England Journal of Medicine 325(20):1423-1428.
Hyams KC, Malone JD, Kapikian AZ, Estes MK, Xi J, Bourgeois AL, Paparello S, Hawkins RE, Green KY. 1993. Norwalk virus infection among Desert Storm troops. Journal of Infectious Diseases 167(4):986-987.
Hyams KC, Hanson K, Wignall FS, Escamilla J, Oldfield EC, 3rd. 1995a. The impact of infectious diseases on the health of US troops deployed to the Persian Gulf during operations Desert Shield and Desert Storm. Clinical Infectious Diseases 20(6):1497-1504.
Hyams KC, Malone JD, Bourgeois AL, Hawkins R, Hale TL, Murphy JR. 1995b. Serum antibody to lipopolysaccharide antigens of Shigella species among US military peronnel deployed to Saudi Arabia and Kuwait during Operation Desert Storm. Clinical and Diagnostic Laboratory Immunology 2(6):700-703.
Hyams KC, Riddle J, Trump DH, Graham JT. 2001a. Endemic infectious diseases and biological warfare during the Gulf War: A decade of analysis and final concerns. American Journal of Tropical Medicine and Hygiene 65(5):664-670.
Hyams KC, Smith TC, Riddle J, Trump DH, Gray G. 2001b. Viral hepatitis in the US military: A study of hospitalization records from 1974 to 1999. Military Medicine 166(10):862-865.
IOM (Institute of Medicine). 1996. Interaction of Drugs, Biologics, and Chemicals in US Military Forces: Current and Future Issues. Washington, DC: National Academy Press.
Johnson KE. 2004. Malaria, US Army, 2003. Medical Surveillance Monthly Report 10(1):6-8.
Kelly MT, Brenner DJ, Farmer JJIII. 1985. Enterobacteriaceae. In: Lennette EH, Balows A, Hausler WJ, Jr., Shadomy HJ, Editors. Manual of Clinical Microbiology. 4th ed. Washington, DC: American Society for Microbiology. Pp. 263-277.
Kilpatrick ME. 2005. Presentation to IOM Committee on Gulf War and Health: Infectious Diseases. Washington, DC.
Kilpatrick ME. 2006. Deployment Health Support Office of the Assistant Secretary of Defense, Health Affairs. Personal Communication.
Kotwal RS, Wenzel RB, Sterling RA, Porter WD, Jordan NN, Petruccelli BP. 2005. An outbreak of malaria in US Army Rangers returning from Afghanistan. Journal of the American Medical Association 293(2):212-216.
Kreutzer RD, Grogl M, Neva FA, Fryauff DJ, Magill AJ, Aleman-Munoz MM. 1993. Identification and genetic comparison of leishmanial parasites causing viscerotropic and cutaneous disease in soldiers returning from Operation Desert Storm. American Journal of Tropical Medicine and Hygiene 49(3):357-363.
Lay JC. 2005. Malaria, US Army, 2004. Medical Surveillance Monthly Report 11(1):7-10.
Lew JF, Kapikian AZ, Jiang X, Estes MK, Green KY. 1994. Molecular characterization and expression of the capsid protein of a Norwalk-like virus recovered from a Desert Shield troop with gastroenteritis. Virology 200(1):319-325.
Magill AJ. 2005. Leishmaniasis in Veterans of Desert Storm and Iraqi Freedom. Presentation to IOM Committee on Gulf War and Health: Infectious Diseases. Washington, DC.
Magill AJ, Grogl M, Gasser RA Jr, Sun W, Oster CN. 1993. Visceral infection caused by Leishmania tropica in veterans of Operation Desert Storm. New England Journal of Medicine 328(19):1383-1387.
Magill AJ, Grogl M, Johnson SC, Gasser RA Jr. 1994. Visceral infection due to Leishmania tropica in a veteran of Operation Desert Storm who presented 2 years after leaving Saudi Arabia. Clinical Infectious Diseases 19(4):805-806.
Malone JD, Paparello S, Thornton S, Mapes T, Haberberger R, Hyams KC. 1991. Parasitic infections in troops returning from Operation Desert Storm. New England Journal of Medicine 325(20):1448-1449.
Mandell GL, Bennett JE, Dolin R. 2005. Principles and Practice of Infectious Diseases. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone.
Martin S, Gambel J, Jackson J, Aronson N, Gupta R, Rowton E, Perich M, McEvoy P, Berman J, Magill A, Hoke C. 1998. Leishmaniasis in the United States military. Military Medicine 163(12):801-807.
Matson DO. 2005. Norovirus gastroenteritis in US Marines in Iraq. Clinical Infectious Diseases 40(4):526-527.
McCarthy M, Estes MK, Hyams KC. 2000. Norwalk-like virus infection in military forces: Epidemic potential, sporadic disease, and the future direction of prevention and control efforts. Journal of Infectious Diseases 181(2 Suppl):S387-S391.
Mikhail MM, Mansour MM, Oyofo BA, Malone JD. 1996. Immune response to Shigella sonnei in US Marines. Infection and Immunity 64(9):3942-3945.
Military Vaccine Agency. 2005a. Hepatitis A Infection and Hepatitis A Vaccine. Military Vaccine (MILVAX) Agency, Office of The Army Surgeon General, US Army.
Military Vaccine Agency. 2005b. Chickenpox Vaccination Program: Questions and Answers. Military Vaccine (MILVAX) Agency, Office of The Army Surgeon General, US Army.
MSMR (Medical Surveillance Monthly Report). 1995. Malaria in active duty soldiers. Medical Surveillance Monthly Report 1(4):9.
Ohl CA, Hyams KC, Malone JD, Oldfield E 3rd. 1993. Leishmaniasis among Desert Storm veterans: A diagnostic and therapeutic dilemma. Military Medicine 158(11):726-729.
Oldfield EC 3rd, Wallace MR, Hyams KC, Yousif AA, Lewis DE, Bourgeois AL. 1991. Endemic infectious diseases of the Middle East. Reviews of Infectious Diseases 13(3 Suppl)S199-S217.
Oster CN, Sanford JP. 1992. Febrile illness in a Desert Storm veteran. Hospital Practice (Office Edition) 27(11):145-148, 151, 155-160.
Paparello SF, Garst P, Bourgeois AL, Hyams KC. 1993. Diarrheal and respiratory disease aboard the hospital ship, USNS-Mercy T-AH 19, during Operation Desert Shield. Military Medicine 158(6):392-395.
Richards AL, Hyams KC, Merrell BR, Dasch GA, Woody JN, Ksiazek TG, LeDuc JW, Watts DM. 1991. Medical aspects of Operation Desert Storm. New England Journal of Medicine 325(13):970-971.
Richards AL, Hyams KC, Watts DM, Rozmajzl PJ, Woody JN, Merrell BR. 1993a. Respiratory disease among military personnel in Saudi Arabia during Operation Desert Shield. American Journal of Public Health 83(9):1326-1329.
Richards AL, Malone JD, Sheris S, Weddle JR, Rossi CA, Ksiazek TG, LeDuc JW, Dasch GA, Hyams KC. 1993b. Arbovirus and rickettsial infections among combat troops during Operation Desert Shield/Desert Storm. Journal of Infectious Diseases 168(4):1080-1081.
Rubertone MV, Brundage JF. 2002. The Defense Medical Surveillance System and the Department of Defense serum repository: Glimpses of the future of public health surveillance. American Journal of Public Health 92(12):1900-1904.
Sanders JW, Putnam SD, Riddle MS, Tribble DR, Jobanputra NK, Jones JJ, Scott DA, Frenck RW. 2004. The epidemiology of self-reported diarrhea in operations Iraqi freedom and enduring freedom. Diagnostic Microbiology and Infectious Disease 50(2):89-93.
Sanders JW, Putnam SD, Frankart C, Frenck RW, Monteville MR, Riddle MS, Rockabrand DM, Sharp TW, Tribble DR. 2005a. Impact of illness and non-combat injury during operations iraqi freedom and enduring freedom (Afghanistan). American Journal of Tropical Medicine and Hygiene 73(4):713-719.
Sanders JW, Putnam SD, Riddle MS, Tribble DR. 2005b. Military importance of diarrhea: Lessons from the Middle East. Current Opinion in Gastroenterology 21(1):9-14.
Schlagenhauf P. 2003. Malaria in Iraq—the pitfalls of Plasmodium vivax prophylaxis. Lancet Infectious Diseases 3(8):460.
Scott P, Artis D, Uzonna J, Zaph C. 2004. The development of effector and memory T cells in cutaneous leishmaniasis: The implications for vaccine development. Immunological Reviews 201:318-338.
Smith TC. 2006. Results of IOM Requested Database Search for Infectious Disease Cases During the Gulf War. San Diego, CA: Department of Defense Center for Deployment Health Research, Naval Health Research Center.
Smith TC, Corbeil TE, Ryan MA, Heller JM, Gray GC. 2004. In-theater hospitalizations of US and allied personnel during the 1991 Gulf War. American Journal of Epidemiology 159(11):1064-1076.
Specht CS, Lewin-Smith MR, Kalasinsky VF, Peterson MR, Mullick FG. 2000. The surgical pathology and cytopathology of US Persian Gulf War military veterans: Identification of diseases endemic to the theater of operations. Archives of Pathology and Laboratory Medicine 124(9):1299-1301.
Spudick JM, Garcia LS, Graham DM, Haake DA. 2005. Diagnostic and therapeutic pitfalls associated with primaquine-tolerant Plasmodium vivax. Journal of Clinical Microbiology 43(2):978-981.
Stephens I, Nataro JP. 2004. Prevention of enteric diseases. Advances in Experimental Medicine and Biology 549:71-82.
Thornton SA, Sherman SS, Farkas T, Zhong W, Torres P, Jiang X. 2005. Gastroenteritis in US Marines during Operation Iraqi Freedom. Clinical Infectious Diseases 40(4):519-525.
Wallace MR, Hale BR, Utz GC, Olson PE, Earhart KC, Thornton SA, Hyams KC. 2002. Endemic infectious diseases of Afghanistan. Clinical Infectious Diseases 34(5 Suppl):S171-S207.
Wasserman GM, Martin BL, Hyams KC, Merrill BR, Oaks HG, McAdoo HA. 1997. A survey of outpatient visits in a United States Army forward unit during Operation Desert Shield. Military Medicine 162(6):374-379.
Weina PJ, Neafie RC, Wortmann G, Polhemus M, Aronson NE. 2004. Old world leishmaniasis: An emerging infection among deployed US military and civilian workers. Clinical Infectious Diseases 39(11):1674-1680.
Willard RJ, Jeffcoat AM, Benson PM, Walsh DS. 2005. Cutaneous leishmaniasis in soldiers from Fort Campbell, Kentucky returning from Operation Iraqi Freedom highlights diagnostic and therapeutic options. Journal of the American Academy of Dermatology 52(6):977-987.
Wolf MK, Taylor DN, Boedeker EC, Hyams KC, Maneval DR, Levine MM, Tamura K, Wilson RA , Echeverria P. 1993. Characterization of enterotoxigenic Escherichia coli isolated from US troops deployed to the Middle East. Journal of Clinical Microbiology 31(4):851-856.
Writer JV, DeFraites RF, Brundage JF. 1996. Comparative mortality among US military personnel in the Persian Gulf region and worldwide during Operations Desert Shield and Desert Storm. Journal of the American Medical Association 275(2):118-121.
Young RC Jr, Rachal RE, Huguley JW 3rd. 1992. Environmental health concerns of the Persian Gulf War. Journal of the National Medical Association 84(5):417-424.
Zapor MJ, Moran KA. 2005. Infectious diseases during wartime. Current Opinion in Infectious Diseases 18(5):395-399.








































