5
Strengthening Traditional Tobacco Control Measures
During the 1990s, substantial progress was made in laying the foundation for an effective tobacco control policy, but that progress has stalled for at least three reasons. First, it is difficult to sustain public attention on endemic problems; in particular, on the challenges of prevention and cessation. Public attention (including the priority-setting driven by public opinion) is easily diverted to the crisis of the moment, and in times of austerity, expenditures on prevention and cessation efforts always seem to be the most dispensable. These tendencies explain in part why the political commitment needed for a sustained effort is lacking. Second, the political and commercial power of the tobacco industry remains substantial, even following the disclosures of past misconduct arising out of recent state reimbursement litigation, the Master Settlement Agreement (MSA), and the U.S. Justice Department’s suit under the Racketeering Influenced and Corrupt Organization Act. Third, all the tobacco control measures described in Chapter 3 have had to be implemented in the context of a largely unregulated market in which tobacco products continue to be aggressively promoted. These promotion efforts are still at work, and it is difficult for public health programs to keep up, especially when the economy falters and public revenues fall short. The behavioral potential of aggressive prevention and cessation efforts is amply illustrated by the successes achieved in California, Massachusetts, and other states. So, too, however, is the fragility of these efforts—when the money disappeared, so did the programs.
The nation needs to muster the political will to intensify the efforts implemented so successfully during the 1990s and to build on them. These
comprehensive state programs, as well as their individual components, have been shown to be effective. Failure to sustain these efforts will cost lives. This chapter of the committee’s report outlines the core components of tobacco control as they have been implemented within the existing legal structure. It should be emphasized, however, that one of the constraints on the current legal structure is that no federal agency has regulatory jurisdiction over tobacco products. Another constraint is that the federal statute regulating the labeling and advertising of cigarettes forecloses state regulation of advertising and marketing of cigarettes “based on smoking and health.” This unfortunate circumstance, addressed in Chapter 6, preempts most state efforts to regulate the appearance, display, promotion, and placement of cigarettes in retail outlets.
Chapter 5 begins with a discussion of the effectiveness of comprehensive state programs, as well as the states’ current approaches toward funding these programs. The states’ expenditures for tobacco control are placed in the context of the revenue streams generated by tobacco excise taxes and payments received under the MSA.
The remainder of the chapter focuses on seven key substantive elements of comprehensive state programs:
-
Tobacco excise taxes
-
Smoking restrictions with broad coverage
-
Youth-access restrictions with adequate enforcement
-
Prevention programs based in schools, families, and health care systems
-
Media campaigns
-
Cessation programs
-
Grassroots community advocacy
The recommendations made throughout the chapter are meant to set forth a blueprint for strengthening and intensifying current tobacco control policies and programs, assuming that the current legal structure of tobacco control remains unchanged. The chapter closes with a projection of the likely impact of following (or not following) this blueprint on the national prevalence of tobacco use over the next 20 years.
COMPREHENSIVE STATE PROGRAMS
During the early days of tobacco use prevention, after the publication of the 1964 Surgeon General’s report (HEW 1964), many state health departments relied on the funds in their state budgets for tobacco control and treatment. Interventions tended to be targeted toward smoking cessation for individuals. By the late 1980s, however, funding for comprehensive state
tobacco control programs increased, beginning with California and then expanding to all states.
California launched the first statewide comprehensive tobacco control program in 1990, one and a half years after the passage of Proposition 99. This landmark referendum mandated an increase in state tobacco taxes and directed 20 percent of the revenues to tobacco control programs (Bal 1998; Glantz and Balbach 2000; Najera 1998). At that time, the National Cancer Institute (NCI) was already preparing to launch the seven-year national American Stop Smoking Intervention Study (ASSIST) program. In 1991, the ASSIST program funded community-level interventions to prevent tobacco use in 17 states (NCI 2005; Stillman et al. 2003).
By the mid-1990s, every state in the United States had some funding for comprehensive tobacco control, either from the ASSIST program or from the Initiatives to Mobilize for the Prevention and Control of Tobacco Use (IMPACT) program, funded by the Centers for Disease Control and Prevention (CDC). In addition, from 1994 through 2000, some states1 also received funding for tobacco control efforts from the Robert Wood Johnson Foundation’s (RWJF) SmokeLess States program (Gerlach and Larkin 2005; Tauras et al. 2005). In addition to educational and cessation programs, the funding supported statewide coalitions of individuals and organizations that pursued action strategies to strengthen tobacco control policies.
The ASSIST program promoted three types of interventions: program services, policy changes, and mass media. However, the ASSIST program guidelines stated that “efforts to achieve priority public policy objectives should take precedence over efforts to support service delivery” (NCI 2005, p.23). Mass media initiatives were intended to support those policy changes. The four ASSIST program priority policy areas were eliminating environmental tobacco smoke (ETS), increasing tobacco excise taxes, limiting tobacco advertising and promotion, and reducing youth access (NCI 2005).
Evaluation of Comprehensive State Programs
In 2005, the CDC’s Office on Smoking and Health (OSH) released a summary of the literature on evidence of the effectiveness of state tobacco control programs (Kuiper et al. 2005). Organized by major reviews and five outcome indicators (tobacco-related mortality, prevalence, consumption, cessation, and smoke-free legislation and policy), the results are generally organized by state. The evidence provided can be considered a guide to state health departments for measuring the success of their comprehensive
tobacco control programs. Of the five indicators of success, one is a health outcome—tobacco-related mortality—and three are markers that lead to improved health outcomes: decreases in smoking prevalence, decreases in consumption of tobacco products, and smoking cessation. The fifth indicator, smoke-free legislation and policy, is an intermediate outcome that alters the environment that supports tobacco use.
This review appeared six years after the publication of the CDC’s Best Practices for Comprehensive Tobacco Control Programs. Published in 1999, Best Practices had concluded that the evidence was sufficiently compelling to encourage all states to pursue comprehensive programs. This conclusion was drawn on the basis of analyses of the excise tax-funded state programs in California, Massachusetts, Oregon, and Maine, as well as the agency’s experience in providing assistance to four other states: Florida, Minnesota, Mississippi, and Texas. The 2005 review reiterates the effectiveness of these programs, while also documenting the successes of other state programs that have appeared since 1999.
Over the past decade and a half, a number of investigators have tried to assess the contribution of comprehensive state programs to policy changes and reductions in smoking (DHHS 2000; Elder et al. 1996; Siegel 2002; Stillman et al. 2003; Tauras et al. 2005; Wakefield and Chaloupka 2000; Warner 2000). By design, a comprehensive tobacco control program consists of several elements (e.g., antismoking media campaigns, counseling services, and school-based prevention initiatives), and some authors have focused on evaluating the effectiveness of individual program components. Later in this chapter, the committee refers, for instance, to several studies that have assessed the impacts of state-sponsored antismoking media campaigns on smoking prevalence and changes in smoking-related beliefs. This section reviews studies that have looked at the effects of comprehensive programs as a whole.
One study that evaluated state programs throughout the country found that a program’s intensity had a very large negative correlation with the prevalence of current smoking (r = −0.81, p < .0001) and a large positive correlation with the quit rate (r = 0.82, p < .0001) among adults 30 to 39 years of age (Jemal et al. 2003). Another study determined that states with better-funded programs have lower prevalence and consumption rates (Tauras et al. 2005). However, many states have substantially cut their tobacco control programs’ budgets in recent years.
Description of Programs
Over the course of the 1990s, several other states—including Arizona, Florida, Massachusetts, and Oregon—followed California’s lead and developed their own comprehensive tobacco control programs (Wakefield
and Chaloupka 2000). Studies reviewing the effects of each of these states’ efforts have been published, and many of these are listed in CDC’s 2005 literature summary (Kuiper et al. 2005). As the first two states in the country to implement comprehensive programs, California and Massachusetts have received a particularly large amount of attention. A specific examination of these two states’ pioneering efforts reveals that comprehensive state programs can be effective in reducing tobacco use and tobacco-related disease, especially when they are fully-funded and operational.
California
In November 1988, California voters passed Proposition 99, which increased the state tobacco tax by 25 cents per pack of cigarettes. One year later, the California Assembly passed legislation that distributed the revenue earned from the tobacco tax increase as follows: 35 percent for hospital services, 20 percent for a health education account, 10 percent for physician services, 5 percent for research, and 5 percent for environmental conservation concerns (25 percent of the funds remained unallocated). Funds from the health education and research accounts were used for the creation of a statewide tobacco control program. The California Tobacco Control Program (CTCP), the first of its kind in the country, debuted in the spring of 1990 (Bal 1998; Najera 1998; TEROC 2000).
Together, the California Department of Health Services (CDHS) and the California Department of Education (CDE), along with the University of California, support a decentralized network of local health departments (LHDs), schools, researchers, and competitive grantees that forms the core of the CTCP. The CDE’s Healthy Kids Program Office oversees the program’s school-based components, whereas the University of California administers various research activities through its Tobacco Related Disease Research Program. The Tobacco Control Section of CDHS, which receives approximately two-thirds of the available funds from the Health Education Account, coordinates the public health elements of the program. These elements include programs conducted at the local level by LHDs and community organizations; a statewide media campaign; cessation counseling services (such as the California Smokers’ Helpline); a materials clearinghouse; and four networks that seek to better integrate California’s African American, American Indian, Asian and Pacific Islander, and Hispanic populations into the state’s tobacco control efforts. California has also coordinated its efforts with other tobacco control initiatives, including the RWJF’s SmokeLess States program (CDHS 1998; State of California 2004; TEROC 2000, 2003).
Throughout the 1990s, the CTCP’s funding fluctuated dramatically. Between 1989–1990 and 1995–1996, for instance, the program experienced
a 60 percent reduction in funding (from $131.3 million to $53.4 million). In addition, although the CTCP’s budget more than doubled between 1995–1996 and 1997–1998 (from $53.4 million to $140.7 million), funding declined yet again in 1998–1999 as well as in 1999–2000 (Independent Evaluation Consortium 2002).
In its first few years, before these major budget fluctuations, the CTCP embraced a mix of policy, media, and program interventions to address a range of factors contributing to tobacco use (CDHS 1998). By 1993, however, looming budget cuts necessitated a more focused approach. Anticipating funding reductions, program administrators revised the CTCP’s structure and priorities to streamline the state’s tobacco control efforts. Administrators refocused the program’s activities into four clearly defined areas: (1) reducing exposure to secondhand smoke, (2) countering the influence of the tobacco industry, (3) reducing youth access to tobacco products, and (4) providing cessation services (CDHS 1998). Since then, however, the CTCP has suffered additional reductions in funding, including a budget cut of 30 percent ($46 million) in FY 2002. Consequently, the gap between tobacco control funding and tobacco industry spending has widened considerably, especially in comparison to the more intensive and better-funded early years of the program. By 2002, California—once the trailblazer in comprehensive tobacco control programming—had fallen to 20th in state rankings for per-capita funding for tobacco control (TEROC 2003).
Massachusetts
Massachusetts modeled much of its tobacco control program after that of the CTCP. In November 1992, Massachusetts voters passed a ballot initiative (commonly known as Question 1) that—like Proposition 99 in California four years earlier—increased the state tobacco tax by 25 cents per pack of cigarettes. Although the Massachusetts Constitution prohibits the earmarking of tax revenue (as the California legislature had done with money earned from its tobacco tax increase), the drafters of Question 1 composed language that urged—but did not mandate—the state to allocate revenue collected from the tobacco tax to a statewide tobacco control program. Following passage of the initiative, Massachusetts legislators soon allocated revenue from the tobacco tax to a newly created Health Protection Fund for the financing of a tobacco-control program (Cady 1998; Connolly and Robbins 1998; Nicholl 1998).
Administered by the Massachusetts Department of Public Health, the Massachusetts Tobacco Control Program (MTCP) began operating in October 1993 with the launch of a mass media campaign, which used a wide spectrum of media, including television, radio, newspapers, and billboards, to disseminate its antismoking message throughout the state. In the follow-
ing months, the MTCP started implementing additional tobacco control initiatives with an emphasis on three priority areas: (1) preventing youth from starting to smoke, (2) reducing smoking prevalence among adults, and (3) reducing nonsmokers’ exposure to ETS. Massachusetts, like California, embraced a localized approach to achieve these goals. Although the MTCP first managed local programs by program type, it soon restructured its operations by organizing localities into six regional networks. Representatives from local tobacco control programs, along with MTCP representatives, began meeting monthly within their respective regional networks to ensure statewide cohesion and better facilitate exchanges of information. In addition, the MTCP has funded community coalitions to organize mobilization efforts, as well as boards of health and LHDs, to enact and enforce tobacco control regulations. Statewide programming, meanwhile, has included the media campaign and the Try to Stop Resource Center, which offers the Smoker’s Quitline, a website (www.trytostop.org) for smokers seeking cessation support, and educational materials. The Center for Tobacco Prevention and Control at the University of Massachusetts Medical School performs research on tobacco use and nicotine dependence (Connolly and Robbins 1998; Hamilton et al. 2002; MDPH 2002a, 2002b).
Massachusetts has also mirrored California in coordinating its activities with other tobacco control initiatives. From 1991 through 1999, for instance, Massachusetts was 1 of 17 states in the country to participate in the NCI’s ASSIST program. Massachusetts participated in various training programs and information exchanges with its fellow ASSIST states, as well as with California and other states with tobacco control programs (Celebucki et al. 1998).
As with the CTCP, the MTCP’s early years represented its most intensive period of funding and activity. From 1994 to 1997, for example, the $7.09 per-capita spent on tobacco control in Massachusetts represented the highest investment of its kind in the country. Budgetary cuts have threatened the effectiveness of the MTCP throughout its history, however, and even in the first 3 years of its existence, the MTCP experienced a pattern of decreasing expenditures (Wakefield and Chaloupka 2000). These early reductions, however, pale in comparison with the cuts that occurred at the beginning of the 2000s. Although funds from the MSA helped increase the MTCP’s budget in FY 2000, funding levels dropped again in FY 2001. In addition, between FY 2002 and FY 2003, as the state faced acute budget shortfalls, it decreased the MTCP’s budget from $34 million to $5.5 million. These cuts resulted in a serious reduction of the MTCP’s activities, including the elimination of almost all local programming and the discontinuation of the media campaign. Since these cuts occurred, surviving elements of the program have operated at a level far below that of the previous decade (Hamilton et al. 2003; MDPH 2002a, 2006).
Description of Evaluations
From the start, both California and Massachusetts incorporated evaluation mechanisms into their tobacco control programs. California developed a multidimensional evaluation structure that comprised local program assessments, in-house surveys, and an independent review. Through the “10 percent” clause, which requires local grantees to devote 10 percent of their program budgets to evaluation, the state can review the effects of programs carried out at the local level, where most CTCP activities take place. The CDHS’s in-house data-gathering efforts, meanwhile, have included the Behavior Risk Factor Survey, the California Adult Tobacco Survey, and the California Youth Tobacco Survey. CDHS contracts with the University of California San Diego (UCSD) to operate the much larger California Tobacco Survey (CTS). UCSD conducts this survey every 3 years through interviews of individuals from randomly selected households, and reaches approximately 78,000 adults and 6,000 youth. The CTS provides CDHS with statewide smoking prevalence rate estimates (broken down into county and regional estimates) as well as data on attitudinal changes (Russell 1998).
The CTCP’s enabling legislation mandated an independent evaluation of the program. The Gallup Organization has conducted this independent review, subcontracting various elements of its evaluation to Stanford University and the University of Southern California (USC). In their reviews, Gallup and its subcontractors have examined the overall impact of the program as well as the relative effectiveness of its various components (media campaigns, local initiatives, school-based programs, etc.). Other surveys used in the evaluation of the CTCP include the CDHS’s annual survey of the rate of illegal sales of tobacco products to minors and occasional surveys targeting specific issues, such as the Field Institute poll on the number of smoke-free bars in the state. The Evaluation Task Force, with members from across the United States and Canada, advises the state on evaluation efforts (Independent Evaluation Consortium 2002; Russell 1998).
Massachusetts has used a similar multidimensional approach to evaluating the MTCP’s success in reducing tobacco use. From October 1993 through March 1994, MTCP conducted the Massachusetts Tobacco Survey, a baseline survey that collected data on tobacco use among adults and youth through randomized telephone interviews. Beginning in March 1995, MTCP began conducting the Massachusetts Adult Tobacco Survey, a monthly follow-up cross-sectional survey, to monitor changes in tobacco use and related attitudes. In addition, along with the RWJF, the MTCP funded longitudinal surveys to evaluate the program’s impact on adults and youth. Finally, like California, Massachusetts commissioned an independent assessment of its tobacco control program. In evaluating the success of the
MTCP, Abt Associates Inc. has reviewed data on smoking prevalence, quit attempts, smoking cessation, exposure to ETS, incidents of tobacco sales to minors, and changes in attitudes regarding tobacco use and tobacco-control policy (Hamilton et al. 2002). Frequent budget cuts, however, have impacted the regularity of the MTCP’s surveillance efforts, restricting the extent and consistency of program evaluation (Hamilton et al. 2002).
Findings Regarding Effects
The results of the evaluations and surveys mentioned above, along with the findings from a number of peer-reviewed studies, indicate that California and Massachusetts have made progress in their tobacco control efforts; this progress is most notable when the respective programs have been well-funded and fully-implemented. On the basis of data from the CDC’s Behavior Risk Factor Surveillance System, Figure 5-1 illustrates the successes that both states have had in reducing tobacco use in comparison with the rest of the country. Figure 5-1 shows that a 23.2 percent reduction in the prevalence of current smoking in California took place between 1990 (the first full year of the state’s tobacco control program) and 2005, whereas the reduction in the U.S. median during the same period was
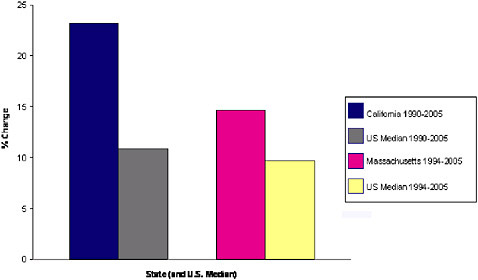
FIGURE 5-1 Percent reduction in current adult smokers in California and Massachusetts from the first year of their tobacco control programs (1990 and 1994, respectively) to 2005 (the year for which the most current data are available) compared with the percent reduction in the U.S. median for the same two time periods, based on data from the Behavior Risk Factor Surveillance System.
SOURCE: (CDC 2006a).
10.9 percent. In Massachusetts, meanwhile, a 14.6 percent reduction took place between 1994 (the first full year of the implementation of its tobacco control program) and 2005. During those same years, the U.S. median experienced a smaller reduction of 9.7 percent.
California
During the CTCP’s early years, California experienced significant declines in the prevalence rate of smoking among adults. To determine whether the declines could be attributed to the program or to alternative factors (e.g., national trends or demographic changes) Siegel and colleagues (2000) compared data for California with data for the rest of the country. They found that California’s rate of decline in adult smoking prevalence between 1990 and 1994 was 0.39 percent per year, whereas the rate of decline in the rest of the United States was only 0.05 percent per year. Restriction of the analysis to various demographic groups did not significantly affect the results. Consequently, Siegel and colleagues suggested that the greater reduction in adult smoking prevalence in California in comparison to that of the rest of the country in the early 1990s could be due to the implementation of the CTCP (Siegel et al. 2000).
It is important to note, however, that California’s adult smoking prevalence rate has remained relatively level since the mid-1990s (CDHS 2002).2 In an evaluation of the CTCP’s activities from 1989 to 1996, Pierce and colleagues (1998) divided the program’s first 7 years into two distinct periods. They found that during Period 1 (January 1989 to June 1993), adult smoking prevalence and per-capita cigarette consumption declined more than 50 percent faster than in previous years and more than 40 percent faster than in the rest of the United States. During Period 2 (July 1993 to December 1996), however, the rate of decline for both adult smoking prevalence and per-capita cigarette consumption slowed, with the prevalence declining at only 15 percent and consumption declining at only 34 percent of the Period 1 rate of decline. Furthermore, although the rate of decline in cigarette consumption remained substantially higher than the rate recorded in the rest of the United States during Period 2, California’s rate of decline in adult smoking prevalence no longer exceeded that of the rest of the United States. This slowdown coincided with decreased financing of tobacco control programs by the state (Pierce et al. 1998).
Fichtenberg and Glantz (2000), meanwhile, analyzed the CTCP’s effectiveness in relation to the rate of decline of deaths attributable to heart
disease in California. They found that between 1989 and 1992, both percapita cigarette consumption rates and the annual rate of mortality from heart disease declined significantly more in California than in the rest of the country. Reflecting the trends noted above, however, the rates of decline slowed noticeably after 1992. Consequently, Fichtenberg and Glantz concluded that the CTCP was initially effective in reducing deaths from heart disease but that cutbacks in the scale and funding of the program weakened further progress (Fichtenberg and Glantz 2000).
The last independent evaluation of the CTCP to be released by the Gallup Organization and its partners (Stanford and USC) assessed the program’s overall impact in relation to Californians’ exposure to its various elements and messages, as reported in surveys conducted in 1996–1997, 1998, and 2000. The evaluation concluded that the CTCP has had an impact on behavior, as counties with greater exposure to the program showed better outcomes than counties with less exposure, including a greater decline in adult smoking prevalence between 1996 and 2000, lower perceived access to cigarettes among 10th graders, and an increase from 1996 to 2000 in the proportion of adults with complete smoking bans in their homes (Independent Evaluation Consortium 2002).
The CTCP has also had success in reducing tobacco use among youth. A study released in 2005 associated the CTCP with reduced uptake and smoking rates among adolescents and young adults. The authors found that the rate of “ever puffing” declined by 70 percent among 12- to 13-year-olds from 1990 to 2002, by 53 percent among 14- to15-year-olds from 1992 to 2002, and by 34 percent among 16- to 17-year-olds from 1996 to 2002. The study identified similar patterns for smoking experimentation (smoking one or more cigarettes ever) and established smoking (smoking more than 100 cigarettes in a lifetime). Although the smoking prevalence among young adults (ages 18 to 24 years) remained constant in the rest of the country from 1992 to 2002, the prevalence among young adults in California decreased significantly (by 18 percent) from 1998–1999 to 2001–2002 (Pierce et al. 2005). Gilpin and colleagues found a similar behavioral trend when they compared the results of two 3-year longitudinal studies (1993–1996 and 1996–1999) that measured smoking initiation rates at the baseline among California adolescents who had never smoked. The authors identified a lower rate of initiation at follow-up in the cohort of the second study than in that of the first study (Gilpin et al. 2005).
Data published by CDHS indicate that California has continued to make progress in reducing tobacco use among youth. According to CDHS, from 2000 to 2004, the 30-day smoking prevalence rate among high school students in California decreased from 21.6 percent to 13.2 percent (CDHS 2005). Figure 5-2 shows that although the rate of decline in smoking prevalence among youth in California mirrored the rate of decline in the rest of
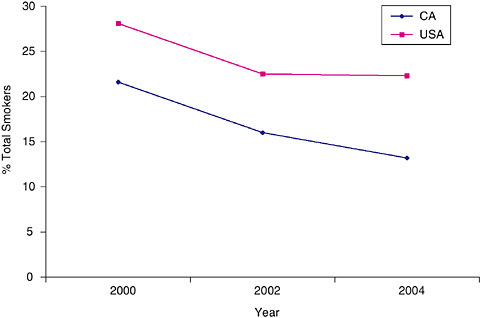
FIGURE 5-2 Thirty-day smoking prevalence among high school students (9th to 12th grades) in California and the United States between 2000 and 2004. Data for 2000 are from the National Youth Tobacco Survey, and data for 2002 and 2004 are from the California Student Tobacco Survey.
SOURCE: (CDHS 2005).
the country from 2000 to 2002, the smoking prevalence rate among youth declined at a greater rate in California than in the United States as a whole from 2002 to 2004. Figure 5-3 depicts the smoking rates among youth over the course of the 1990s in both California and the United States (excluding California). Although the rates rose in California as well as in the rest of the country in the early part of the decade, by the mid-1990s the smoking prevalence rate among youth in California began to decline, whereas the prevalence nationwide continued to increase for several more years.
Massachusetts
Like California, Massachusetts has made progress in reducing tobacco use, with both adult smoking prevalence and per-capita cigarette consumption trending downward since the implementation of the MTCP. Figure 5-1 illustrates Massachusetts’s success in reducing the prevalence of smoking among adults, showing that from 1994 to 2005 Massachusetts experienced
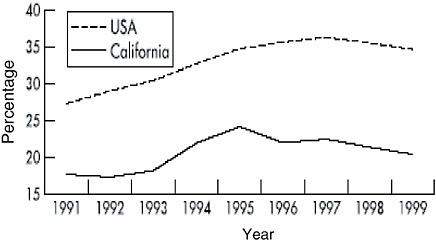
FIGURE 5-3 Smoking rates for high school seniors in California and the United States excluding California, 1991 to 1999 Monitoring the Future.
SOURCE: (Farrelly et al. 2003).
a greater percent change in the prevalence of current adult smokers than did the U.S. median.
In its last independent evaluation of the MTCP, Abt Associates Inc. similarly assessed the program by comparing state and national data. Controlling for demographic characteristics and comparing current smoking prevalence rates in Massachusetts with those in 41 states without comprehensive tobacco control programs, Abt Associates found that adult smoking prevalence rates declined more rapidly in Massachusetts than in the comparison states. According to the Abt analysis, the adjusted prevalence rate in Massachusetts declined between 1990 and 2000, from 22.7 percent to 20.5 percent (an annual rate of 0.9 percent), whereas the adjusted prevalence rate in the comparison states declined from 22.0 percent to 21.7 percent (an annual rate of 0.4 percent). Consequently, Abt Associates concluded (like Siegel and colleagues in the case of California) that the decline in the adult smoking prevalence rate in Massachusetts could be attributed to the existence of the MTCP and not to national trends or demographic changes. Abt also noted that Massachusetts experienced a drop (40 percent) in per-capita cigarette consumption from 1992 to 2001, two times greater than the drop (20 percent) experienced in the rest of the country, excluding California. Furthermore, the decline in youth smoking prevalence in Massachusetts was found to be greater than that in the rest of the United States (Hamilton et al. 2003). The results of a similar analysis that reviewed data obtained through 1999 were published in 2002 (Weintraub and Hamilton 2002).
An earlier review (the results of which were published by the CDC in 1996) sought to determine the impact of the state’s excise tax and tobacco control program on per-capita cigarette consumption and adult smoking prevalence. In doing so, the authors compared the rates in Massachusetts with those in the rest of the United States during two time periods: the 3 years leading up to the passage of Question 1 on the state ballot initiative (1990 to 1992) and the years immediately following the implementation of the excise tax and establishment of the MTCP (1993 to 1996). Although they determined that smoking prevalence rates in Massachusetts required further study, they found that per capita cigarette consumption decreased significantly from the first period to the second. During the first period, consumption in Massachusetts declined by 6.4 percent, whereas that in the rest of the country declined by 5.8 percent (except for California, where consumption declined by 11.0 percent). From 1992 to 1996, however, per-capita consumption declined by 19.7 percent in Massachusetts, 15.8 percent in California, and just 6.1 percent in the remaining states and the District of Columbia. The authors reasoned that because real cigarette prices actually fell in 1993 (because of price reductions by the tobacco industry), the excise tax alone could not account for the decline in cigarette consumption that continued through 1996. Consequently, they concluded that Massachusetts’s tobacco control program played a role alongside tax increases in reducing the rate of tobacco use in the years immediately following the passage of Question 1 (CDC 1996).
Biener and colleagues (2000a) confirmed and added to the findings of the 1996 CDC study. They found that although Massachusetts and 48 comparison states experienced similar declines (15 percent and 14 percent respectively) in per-capita cigarette consumption from 1988 to 1992, Massachusetts experienced a greater annual decline (more than 4 percent) than the comparison states (less than 1 percent annually) following the establishment of excise tax and the establishment of the MTCP. As the authors of the CDC study had already observed, the decline in Massachusetts occurred even though price reductions for cigarettes effectively negated the potential effects of the excise tax increase. The authors also determined that after 1992 Massachusetts experienced a greater rate of decline in adult smoking prevalence than did the comparison states. The prevalence of smoking declined by 0.43 percent per year in Massachusetts but by only 0.03 percent in the comparison states. On the basis of these findings, the authors concluded that tobacco control programs such as the MTCP can reduce the rates of tobacco use and the related health risks (Biener et al. 2000a).
Massachusetts’s success in reducing the rates of tobacco use among youth has fluctuated over time, however. In its last review of the MTCP, Abt Associates reported that although the prevalence of smoking among youth in Massachusetts and the United States as a whole actually grew during
the early 1990s, Massachusetts managed to reverse this trend in the second half of the decade, with the prevalence of smoking among youth falling more rapidly in Massachusetts from 1995 to 2001 (from 36 to 26 percent) than in the rest of the country (35 to 29 percent) (Hamilton et al. 2003). A separate study conducted by Soldz and colleagues (2002) identified similar trends. On the basis of data from the triennial Massachusetts Prevalence Study, Soldz and colleagues found that although the prevalence increased at both the state and national levels from 1990 to 1993, Massachusetts managed to reverse this trend in the latter half of the decade. Comparing data from the 1996 and 1999 surveys, the authors determined that over the 3-year period, the rate of cigarette use among students in grades 7 through 12 dropped from 30.7 percent to 23.7 percent. The percent decline in Massachusetts, they found, was greater than the declines seen in neighboring states and in the nation as a whole. Furthermore, the decrease in the rate of cigarette use was broad-based, occurring in numerous subsets of the youth population in Massachusetts. The prevalence rate declined among students in middle school as well as high school, boys and girls, and African Americans and whites. Soldz and colleagues concluded that the scale of this decline, especially in comparison with the smaller regional and national declines, strongly demonstrated the effectiveness of the MTCP in reducing the rate of cigarette use among Massachusetts youth (Soldz et al. 2002).
On the basis of data from the CDC’s Youth Behavior Risk Survey, Figure 5-4 illustrates the progress that Massachusetts made during the mid-to-late 1990s in reducing the rate of tobacco use among youth, reflecting the conclusions reached by the independent evaluation as well as by Soldz and colleagues (2002). Figure 5-4 also shows, however, that after these two studies were conducted, the smoking prevalence rate among youth in the state began to decline at a slower rate than that among youth in the country as a whole. This slowdown coincides with the sharp reductions made to the MTCP’s budget during the early part of the 2000s. Although, in light of 2005 data, the smoking prevalence rate among youth in Massachusetts once again compares favorably with that among youth in the United States at large, the prevalence of smoking among youth in the state has essentially stalled, indicating an end to the declines seen in the latter half of the 1990s.
Summary
The evidence presented and reviewed above shows that comprehensive state programs have achieved substantial reductions in the rates of tobacco use in both California and Massachusetts. This is particularly true of the early years of the CTCP and MTCP, when both states aggressively funded and implemented their tobacco control programs. Evaluations of Florida’s
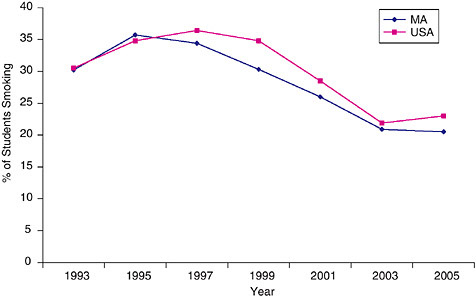
FIGURE 5-4 Comparison of the rate of current cigarette use among high school students (grades 9 to 12) in Massachusetts with the U.S. median, based on data from the Youth Risk Behavior Surveillance System.
SOURCE: (CDC 2006b).
youth-themed “truth” campaign, as well as programs in other states, such as Arizona, Oregon, and—most recently—New York, also indicate that statewide tobacco control programs can be effective in reducing the rates of tobacco use (Bauer et al. 2000; CDC 1999a; 2001; RTI International 2005; Siegel 2002; Sly et al. 2001a; Wakefield and Chaloupka 2000). In recent years, however, large budget cutbacks to many states’ tobacco control programs, including that of Massachusetts, have jeopardized continued success. To effectively reduce tobacco use, states must maintain, over time, a comprehensive and integrated tobacco control strategy.
FUNDING FOR COMPREHENSIVE STATE PROGRAMS
After the end of the ASSIST program, when the responsibility for tobacco prevention shifted from NCI to OSH at CDC, OSH implemented a Tobacco Control Program to sustain comprehensive state tobacco control programs. Under that program each state can receive approximately $1 million per year for comprehensive tobacco control efforts (CDC 2003). Suggested levels of funding per capita are included to assist states in allocating funds from various sources. However, state governments are not funding
such efforts at the levels that the CDC recommends for best practices (Tauras et al. 2005), either from general funds or from payments under the MSA (revenues received under the MSA have typically been siphoned off by state governments to support programs other than those for tobacco control). In this section, the committee summarizes state expenditures on tobacco control and the sources of revenues that are funding these programs.
State Tobacco Control Expenditures
Expenditures on tobacco control vary widely among states (Figure 5-5 [Prevention Spending Dollars per person] and Table 5-1). In FY 2005, per-capita state expenditures on tobacco control varied from more than $11 in Delaware ($11.87) and Maine ($11.14) to nothing (aside from the CDC grant) in the District of Columbia, Michigan, Missouri, New Hampshire, South Carolina, and Tennessee. The mean per-capita state expenditure was $2.76.
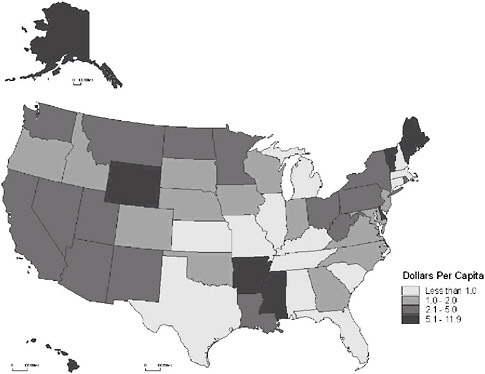
FIGURE 5-5 FY 2005 state tobacco control spending per capita (based on 2000 census data).
TABLE 5-1 Per-Capita State Tobacco Control Revenues and Expenditures, 2005
|
State |
MSA Payment Received per Capita ($) |
Net Excise Tax Revenue per Capita ($) |
Prevention Spending per Capita ($) |
|
Alabama |
22.91 |
33.63 |
0.08 |
|
Alaska |
34.71 |
77.06 |
6.70 |
|
Arizona |
19.48 |
54.99 |
4.50 |
|
Arkansas |
19.74 |
47.51 |
6.58 |
|
California |
12.01 |
30.23 |
2.18 |
|
Colorado |
20.31 |
26.74 |
1.00 |
|
Connecticut |
34.74 |
74.61 |
0.02 |
|
Delaware |
32.17 |
103.60 |
11.87 |
|
District of Columbia |
66.95 |
35.43 |
0.00 |
|
Florida |
24.48 |
27.38 |
0.06 |
|
Georgia |
19.11 |
27.66 |
1.40 |
|
Hawaii |
31.66 |
68.62 |
7.35 |
|
Idaho |
17.89 |
34.87 |
1.47 |
|
Illinois |
23.88 |
51.38 |
0.89 |
|
Indiana |
21.38 |
53.94 |
1.78 |
|
Iowa |
18.94 |
29.88 |
1.74 |
|
Kansas |
19.76 |
43.79 |
0.28 |
|
Kentucky |
27.77 |
12.35 |
0.67 |
|
Louisiana |
32.35 |
31.11 |
2.53 |
|
Maine |
38.46 |
72.09 |
11.14 |
|
Maryland |
28.56 |
50.51 |
1.79 |
|
Massachusetts |
40.54 |
65.01 |
0.60 |
|
Michigan |
27.60 |
109.67 |
0.00 |
|
Minnesota |
37.56 |
32.58 |
3.80 |
|
Mississippi |
42.54 |
15.24 |
7.03 |
|
Missouri |
25.91 |
17.74 |
0.00 |
|
Montana |
30.01 |
62.72 |
2.77 |
|
Nebraska |
22.16 |
39.14 |
1.69 |
|
Nevada |
19.45 |
64.58 |
2.20 |
|
New Hampshire |
34.31 |
75.61 |
0.00 |
|
New Jersey |
29.29 |
92.84 |
1.31 |
|
New Mexico |
20.90 |
33.04 |
2.75 |
|
New York |
21.64 |
49.32 |
2.08 |
|
North Carolina |
18.47 |
4.89 |
1.86 |
|
North Dakota |
36.32 |
28.23 |
4.83 |
|
Ohio |
28.28 |
48.86 |
4.69 |
|
Oklahoma |
19.14 |
30.37 |
1.39 |
|
Oregon |
21.38 |
63.65 |
1.02 |
|
Pennsylvania |
29.82 |
83.79 |
3.75 |
|
Rhode Island |
43.71 |
123.70 |
2.38 |
|
South Carolina |
18.29 |
6.41 |
0.00 |
|
South Dakota |
29.46 |
34.85 |
1.99 |
|
Tennessee |
27.54 |
19.70 |
0.00 |
|
Texas |
24.74 |
23.60 |
0.35 |
|
Utah |
12.70 |
24.33 |
3.22 |
On average, states spend about half of CDC’s recommended minimum level for comprehensive state tobacco control programs including the nine components specified in Best Practices for Comprehensive Tobacco Control Programs community programs to reduce tobacco use, chronic disease programs to reduce the burden of tobacco-related diseases, school programs, enforcement, statewide programs, countermarketing, cessation programs, surveillance and evaluation, and administration and management (CDC 1999c). In 1995, the CDC’s recommended range of per-capita spending for the nation as a whole was $5.85 to $15.85. The CDC identified such an expenditure range to take into account important variations among states, including overall population (and therefore the possibility of achieving economies of scale), as well as tobacco use prevalence and demographic factors.
According to the CDC, “approximate annual costs to implement all of the recommended program components have been estimated to range from $7 to $20 per capita in smaller states (population under 3 million), $6 to $17 per capita in medium-sized states (population 3 million to 7 million), and $5 to $16 per capita in larger states (population over 7 million)” (CDC 1999c). In recommending funding ranges for each state, CDC generally works within these estimates, although it should be noted that for the states with smaller populations, CDC recommends an upper estimate higher than $20 (for example, in Delaware, the District of Columbia, Montana, North Dakota, Rhode Island, South Dakota, Vermont, and Wyoming). California has the lowest lower estimate of $5.12 per capita, and Wyoming has the highest upper estimate of $30.01.
The committee reviewed the methodology that CDC uses to calculate
these estimated general ranges. The agency first identified best practices for each of the nine components of a comprehensive program and then calculated funding ranges (in millions) for each program component for each state—taking population, tobacco-use prevalence, and demographic factors into account—totaled the lower and upper estimates of each component on a state-by-state basis to find a total state program cost, and then calculated the per-capita ranges for each state. The scientific evidence that has emerged since 1999 appears to have substantiated CDC’s judgment regarding best practices in each of the relevant domains, and the committee sees no reason to question the CDC’s expert judgments regarding the likely costs of implementing these practices in various states. Accordingly, the committee has decided to use the CDC estimates as a template for its recommendations regarding state tobacco control expenditures.
Revenue Sources for State Tobacco Control Programs
What are the revenue sources of state funding for tobacco control? It might be expected that a certain percentage of revenues produced by tobacco excise taxes and the Master Settlement Agreement would be “earmarked” or set aside for tobacco control. However, few states have adopted this strategy, and there is very little correlation between the amounts generated by these two tobacco-related revenue streams and the amount expended on tobacco control.
State Tobacco Excise Taxes
States vary widely in their tobacco excise tax rates and in the amount of revenue that those taxes produce per capita (Table 5-1), ranging in FY 2005 from more than $80 per capita in Rhode Island ($124), Michigan ($110), Delaware ($104), New Jersey ($93), and Pennsylvania ($84) to less than $15 per capita in North Carolina ($5), South Carolina ($6), and Kentucky ($12). As these numbers suggest, and as Figure 5-6 shows, per-capita excise tax revenues are the highest in the Northeast and the lowest in the Southeast. The average per-capita excise tax revenue in all states was $47.80, and two-thirds of the states had revenues of at least $32 per capita.
In recent years, largely in response to state budget shortfalls, there has been a dramatic increase in the average tobacco excise tax rates and the number of states increasing their tax rates. According to Farrelly and colleagues (2003), in 2002 alone, 21 states raised their cigarette taxes, more states than in the past 5 years combined, and the average state cigarette excise tax rate increased significantly from 31 cents per pack (in 2002 dollars) in 1990 to 62 cents per pack in early 2003. These increases have exacerbated what were already substantial disparities in tobacco excise tax
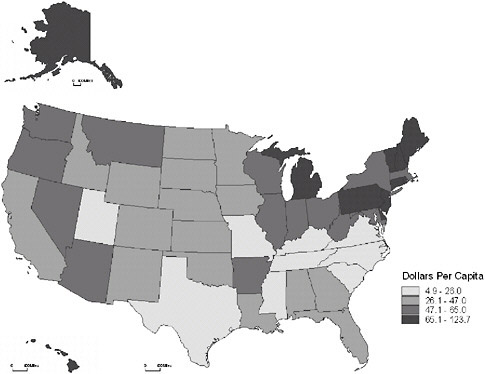
FIGURE 5-6 Per-capita tobacco excise tax revenues collected by state 2005, based on 2000 census data.
rates across the country and the attendant problems of interstate smuggling (Farrelly et al. 2003).
California was the first state to earmark a portion of its excise tax revenues for tobacco control efforts. As noted, a voter initiative, Proposition 99, increased the state tobacco tax by 25 cents per pack of cigarettes in 1988, and in 1990 the California Assembly enacted legislation distributing the revenue earned from the tobacco tax increase. The legislation directed that 20 percent of the revenues be allocated to a health education account, and funds from the health education and research accounts finance a statewide tobacco control program. Only in California, Oregon, and Utah have excise taxes served as a major designated source of funding for tobacco control.
Whether tax revenues should be earmarked for specific purposes is a controversial issue in public finance, and there is no compelling reason why tobacco control activities should be funded from any particular source of revenues (in fact, as noted above, Massachusetts was constitutionally precluded from earmarking the revenues generated by its 1992 tobacco excise tax increase to tobacco control). In addition, earmarking of a specified
proportion of revenues represents a pre-commitment to prioritize tobacco control expenditures in a way that would preclude the weighing of other priorities. However, the argument for earmarking a presumptive (but reversible) portion of tobacco excise tax revenues to tobacco control does have a common-sense persuasive force (Hamilton et al. 2005), and a decision to link tobacco excise tax revenues to tobacco control efforts represents a modest political commitment to sustain these activities.
In light of the traditional political separation between decisions about revenues (including excise tax rates) and expenditure decisions, it is perhaps unsurprising that per-capita state excise tax revenues and per-capita tobacco control expenditures are only modestly correlated (Figure 5-7).
Master Settlement Agreement Allocations
Another important element in the political economy of tobacco control is the MSA. On average in 2005, the states received $27.46 per capita from the proceeds of the MSA. Because these calculations were based on projected Medicaid expenditures for tobacco-related diseases, they varied substantially (Table 5-1), from a low of $12.01 per capita in California to a high of $66.95 in the District of Columbia (Figure 5-8).
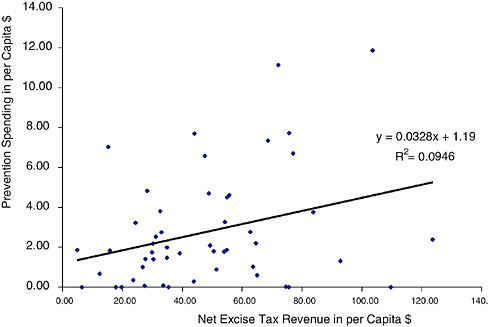
FIGURE 5-7 Correlation between per-capita tobacco control spending and per-capita excise tax revenues.
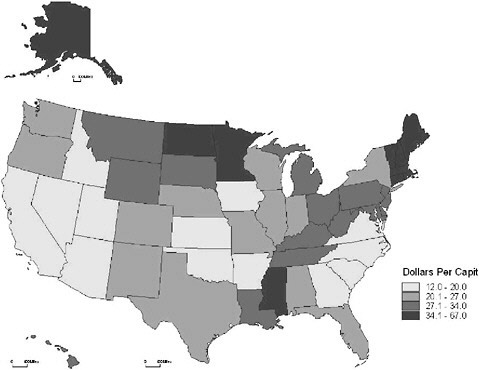
FIGURE 5-8 Per-capita payments received from the MSA, by state, in FY 2005 (based on 2000 census data).
The MSA does not stipulate how the states should spend the settlement funds. Consequently, the 46 states, the District of Columbia, and the five territories party to the MSA have developed various regulations, structures, and mechanisms for allocating settlement payments. A November 2005 report jointly issued by the American Cancer Society, the American Heart Association, the American Lung Association, and the Campaign for Tobacco-Free Kids illustrates the diverse approaches that the states have used to administer these funds over the past several years (AHA et al. 2005). Although some states regularly apply payments directly to their general budgets, others have established specific funds to which they direct their MSA allotments. Delaware law, for instance, mandates that all settlement payments be deposited into the Delaware Health Fund, which finances health-related programs, including the state’s tobacco control efforts. Kansas law, meanwhile, directs the entirety of the state’s MSA payments (after the first $70 million, which was placed into the state’s general fund) into the Kansas Endowment for Youth fund, which finances a range of youth-related programs. And Michigan and Nevada direct portions of their MSA allotments to education
scholarship funds. Just a few states, however, such as Nevada and Virginia, explicitly require portions of their settlement funds to be applied to tobacco control efforts.
Several tobacco-producing states apply large portions of their MSA payments to funds that assist citizens and businesses traditionally dependent on the tobacco industry. North Carolina law requires that 50 percent of the state’s annual MSA receipts be placed in a fund that provides assistance to tobacco-dependent communities. An additional 25 percent is allocated to a separate fund that directly aids tobacco farmers and tobacco manufacturing workers, among others. Similarly, Virginia law allocates 50 percent of the commonwealth’s MSA-derived funds to the Tobacco Indemnification and Community Revitalization Trust Fund, which provides economic assistance to tobacco growers and tobacco-dependent communities (AHA et al. 2005).
In recent years, budget shortfalls have compelled a number of states to divert MSA payments from tobacco-control–related funds and programs, such as those listed above (AHA et al. 2005). Largely to address such shortfalls, 15 states have also opted to securitize future MSA proceeds (GAO 2006). California, for instance, securitized its future settlement payments to fund its FY 2003 and FY 2004 budgets (AHA et al. 2005). In electing to securitize MSA proceeds, states receive advance income by issuing bonds backed by future MSA payments. States must pay to service the debt accrued through securitization, however; and in FY 2005 four states, including California, applied 100 percent of their MSA payments to servicing this debt (in addition, New Jersey allocated 99.9 percent of its MSA payments to debt servicing). In an April 2006 review of how states spend their MSA payments, the U.S. Government Accountability Office (GAO) calculated that servicing of securitization debt represented 24 percent of the total MSA funds allocated by states in FY 2005 (GAO 2006).
GAO also reported that between FY 2004 and FY 2005, the portion of MSA payments allocated to cover budget shortfalls decreased dramatically, from 44 to 4 percent, with states applying the largest portion of MSA-derived funds (32 percent) in FY 2005 to health-related programs (e.g., health care services, health insurance, and health research). It should be noted, however, that although the portion of funds allocated to such programs increased, the actual dollar amount decreased between FY 2004 and FY 2005, because fewer states obtained money up front through securitization. Allocations of MSA payments to tobacco control programs, meanwhile, remain extremely low, averaging just 4.7 percent of total MSA payments in FY 2005. In fact, since GAO began reviewing state allocations of MSA money, the percentage apportioned to tobacco control efforts has not exceeded 6 percent (GAO 2006). GAO does not anticipate any change in allocations to tobacco control programs for FY 2006.
Sloan and colleagues (2005) found that the mean total annual spending from settlement funds was $30.65 per capita from FY 2000 to FY 2004. Median spending was about $25 per capita. However, less than half of that money was spent on health-related activities, and very little of it was spent on tobacco control efforts. Approximately one-fourth of the state budgets reported during this period allocated no money to tobacco control. Among budgets that allocated anything to tobacco control, the usual allocation was less than $2.50 per capita (see Figure 3 in the article by Sloan and colleagues 2005). States tended to spend less on tobacco control if they had more seniors, more individuals under the age of 18 years, and higher per-capita incomes. Not surprisingly, tobacco-producing states tended to spend smaller amounts of their MSA proceeds on tobacco control (Sloan et al. 2005).
In sum, only a small proportion of MSA revenues is devoted to tobacco control, and MSA revenues are specifically earmarked for this purpose in only a handful of states. In some states, however, the modest appropriations from MSA payments have accounted for a significant proportion of tobacco-control–related expenditures. Gross and colleagues (2002), for instance, determined that even though the percentage of MSA funds directed to tobacco control was very low, “when the tobacco-control-program expenditures from all 50 states were considered in aggregate, over half of the funding was derived from settlement income” (Gross et al. 2002). This proportion is probably much lower now because so many states have used their MSA funds to shore up budget gaps.
Summary and Recommendation
In the committee’s view, states should adopt a funding strategy designed to provide stable support for the level of tobacco control funding recommended by the CDC. MSA payments are not a reliable source of funds in most states. The most sensible approach would be to allocate a suitable share of tobacco excise tax revenues to tobacco control efforts. History suggests that these taxes are not likely to be reduced once they have been increased; moreover, high excise taxes also serve the goal of reducing tobacco use (see below) while raising revenues for tobacco control efforts and other public purposes. In most states, the CDC’s recommended expenditure target (about $16 per capita for the nation as a whole) could be achieved by setting aside about one-third of the proceeds from the tax. The committee recognizes that explicit earmarking is forbidden by some state constitutions and is presumptively unacceptable in other states. However, even if formal earmarking is unacceptable, legislators responsible for public health expenditures should embrace a political strategy of linking the amount of the tobacco control budget line to a percentage of tobacco excise tax revenues.
Recommendation 1: Each state should fund state tobacco control activities at the level recommended by the CDC. A reasonable target for each state is in the range of $15 to $20 per capita, depending on the state’s population, demography, and prevalence of tobacco use. If it is constitutionally permissible, states should use a statutorily prescribed portion of their tobacco excise tax revenues to fund tobacco control programs.
EXCISE TAX
It is well established that an increase in the price of cigarettes decreases their use and that raising tobacco excise taxes is one of the most effective policies for reducing the use of tobacco. From a policy perspective, one of the unresolved questions is whether price increases act synergistically with other tobacco control interventions to decrease consumption. After a brief review of the literature on these topics, the committee addresses the proper level of excise taxation solely on the basis of tobacco control considerations and comments on the practical difficulties presented by disparate levels of state excise taxes.
Price Increases Decrease Cigarette Use
Over a period of more than three decades, economists and health policy analysts have accumulated a large body of evidence on the effect of price on cigarette consumption. The effect of price on cigarette use has also been the subject of numerous recent reviews (Chaloupka 1999, (Chaloupka and Warner 2000; Leverett et al. 2002; Pinilla 2002) and meta-analyses (Gallet and List 2003). The conclusion reached by virtually every study of every demographic group in both developed and developing countries is that an increase in cigarette price reduces the level of cigarette use. A recent cross-sectional study of 70 countries based on aggregate consumption data found a price elasticity in the range of −0.49 to −0.57 percent (Blecher and van Walbeek 2004).
Price has been found to affect virtually every measure of cigarette use, including per-capita consumption, as derived from aggregate macrolevel data, as well as smoking prevalence and the number of cigarettes smoked daily, as derived from individual microlevel data (Hu et al. 1995a). Recent studies with microlevel data have found that higher cigarette prices increase the probability that a current adult smoker will make an attempt to quit (Levy et al. 2005) and that a young adult smoker will stop smoking (Tauras 2004b). In a study of adult smokers, access to low-taxed cigarettes was found to deter cessation attempts (Hyland et al. 2005). The June 2006 National Institutes of Health (NIH) state-of-the-science panel on tobacco
use (NIH 2006b) found that an increase in the unit price of tobacco products increases the rate of tobacco use cessation and reduces the level of consumption among individuals across a wide spectrum of racial and socioeconomic groups.
Just as increases in cigarette taxes deter consumption, declines in cigarette prices have been found to increase the level of consumption. In one Canadian study, for example, tax cuts in certain provinces slowed the rate of decline of smoking by inducing more smokers to start and leading fewer smokers to quit (Hamilton et al. 1997). Another study suggested that the price decrease in Canada in the early 1990s may have contributed to an increase in the rate of smoking among youth in the province of Ontario (Waller et al. 2003). In the United States, the increase in the rate of smoking among youth in the early 1990s has been attributed to declines in cigarette prices (Gruber 2001).
Cigarette Price Increases Reduce Cigarette Use by Adolescents
Although some studies have reported mixed or negative findings, the most recently published research generally supports the finding that higher cigarette prices discourage youth from smoking (Chaloupka 1999; Chaloupka and Pacula 1998; Chapman and Richardson 1990; Ding 2003; Gruber 2001; Harris and Chan 1999; Liang et al. 2003). Increased cigarette prices have been found to deter smoking among young people when investigators controlled for peer effects (Powell et al. 2005).
Some recent research has attempted to distinguish between the effects of price on adolescent experimentation with cigarettes and the effects of price on cigarette use among established adolescent smokers. One recent study, based on microlevel data from a 1993 national youth survey, found that cigarette price affects the latter group but not the former group (Emery et al. 2001). However, another study, based on the Growing Up Today Study of 1999, found that adolescents residing in states with the highest quartile of cigarette tax rates had a lower probability of experimental smoking (Thomson et al. 2004). Still another recent study suggested that cigarette prices do affect the probability that adolescent males, but not adolescent females, will initiate smoking. Adolescent female smoking initiation was found to depend on perceptions of being overweight or the desire to lose weight (Cawley et al. 2004).
Some of the inconsistencies in past research may have resulted from inaccurate measurement of the actual prices that teenagers paid for cigarettes. One study suggested that region-specific average retail prices or tax rates may incorrectly gauge the actual prices paid by youth smokers and that perceived price is a more specific measure of the smoker’s actual out-of-pocket costs (Ross and Chaloupka 2003).
The June 2006 NIH state-of-the-science panel on tobacco use (NIH 2006b) determined that increases in excise taxes are effective in preventing tobacco use among adolescents and young adults, even though recent studies have found that increases in cigarette tax induce smokers to seek out tax-exempt cigarettes, to take advantage of coupon offers, and to avoid the impact of tax hikes in other ways (Hyland et al. 2004).
Do Cigarette Price Increases Act Synergistically with Other Antismoking Interventions?
Researchers have attempted to untangle the effects of price increases from those of other antitobacco policies, including informational campaigns and restrictions on public smoking, that are often carried out concurrently with governmental tax increases (Scollo et al. 2003; Stephens et al. 2001). Although many studies have established that cigarette price increases and other antismoking policies act independently to suppress demand, the question of a possible synergistic effect remains unanswered. Put differently, could antismoking policies raise the price elasticity of demand, or could price increases enhance the effectiveness of other antismoking interventions?
A number of studies have identified the independent effects of cigarette price increases and local restrictions on smoking at work sites or public places, in both the United States and Canada (Chaloupka 1999; Keeler et al. 1993; Stephens et al. 1997; Tauras 2004a; Yurekli and Zhang 2000). Other studies have identified the independent effects of tax increases and state or local tobacco control campaigns. Early research in this area was based on the antismoking campaigns in California and Massachusetts. Thus a study of quarterly cigarette sales data from 1980 to 1992 in California found that the antismoking campaign and cigarette taxation both contributed to the decline in the level of cigarette use (Hu et al. 1995b). Likewise, a study of the Massachusetts tobacco control campaign found declines in consumption greater than those expected from tax increases alone (CDC 1996).
Recent work on the interaction between price changes and other anti-smoking policies has extended beyond the initial experiences of California and Massachusetts. In one cross-sectional study, increases in state tobacco control funding were found to reduce smoking, even when prices are taken into account (Farrelly et al. 2003). Another study reported independent effects of cigarette price and state-level media campaigns on the probability of making a quit attempt of at least 3 months’ duration (Levy et al. 2005). The combination of antismoking programs and increased tobacco taxes reduced the level of cigarette consumption among youth more than expected as a result of price increases alone (Wakefield and Chaloupka 2000).
Some studies have noted the combined effect of price increases and other antismoking measures, but made an attempt to identify specific contribution of each strategy. Thus cigarette smoking among adults declined after New York City raised local cigarette taxes, made available cessation services, distributed nicotine patches for free, and instituted legal action to ban smoking in public places in 2002 (Frieden et al. 2005). A study in the state of Oregon, reported in Morbidity and Mortality Weekly Report, found that the combination of an excise tax increase and the state’s Tobacco Prevention and Education Program diminished the level of cigarette use (CDC 1999a).
A recent study focused on the impact of the 1998 MSA in the United States, specifically, the effect of the agreement on retail cigarette prices and aggregate cigarette consumption (Sloan et al. 2004). By 2002, the MSA was estimated to have reduced the rate of cigarette consumption by 13 percent among 18- to 20-year-olds, 5 percent among 21- to 65-year-olds, and 13 percent among those 65 years of age and older. The decline in consumption was mediated primarily through the effect of the MSA on cigarette prices, but there was evidence that MSA-associated policies, aside from increased prices, reduced consumption among younger smokers.
How High Should Tobacco Excise Taxes Be?
At the present time, state governments are the primary taxing authorities for tobacco products. During 2005, the consumption-weighted average state excise tax was 76.73 cents per pack (Capehart 2005). By contrast, the federal excise tax has been 39 cents per pack since 2002. Of an estimated total consumption of 388 billion cigarettes in 2004, only 5 billion (or 1.3 percent) were sold through federally tax-exempt outlets, including Indian reservations, military bases, and shipments to Puerto Rico (Capehart 2005).
Tax Evasion
When cigarette excise taxes are evaluated solely from a public health perspective (i.e., exclusively as an instrument for deterring consumption), the level to which the tax might justifiably be raised is limited only by concerns that higher taxes stimulate tax avoidance, such as by creating a demand for nontaxed or lower-taxed cigarette products or for other tobacco product substitutes. Broadly speaking, there are at least three avoidance strategies: (1) producing cigarettes at home, (2) ordering cigarettes to be shipped by mail or package delivery service from sellers who do not collect the tax, and (3) physically purchasing and importing cigarettes from a lower-tax jurisdiction.
The first cigarette tax evasion strategy, home production, has traditionally constituted a negligible fraction of the overall market and, until that situation changes, all that is required is basic monitoring to make sure that the market is not growing substantially. The second cigarette tax evasion strategy, interstate shipping, has become an increasing concern with the proliferation of internet sites selling untaxed cigarettes. The committee addresses this problem below and recommends legislation prohibiting both online tobacco sales and direct shipment of tobacco products to consumers.
The third cigarette tax evasion strategy, smuggling from states with low excise taxes to states with high excise taxes, has traditionally been the greatest concern due to the great variation in state-level excise taxes and the porosity of state borders with respect to commerce. Even if the price within the United States were uniform, policymakers would still have to consider the prospect of smuggling from other countries. International black markets could develop in which foreign cigarettes are smuggled into the country to avoid equalizing excise taxes, or U.S.-manufactured cigarettes could be exported and then illegally re-imported. International smuggling, however, does not appear to be a substantial concern at the present time. The committee will address the smuggling problem later in this chapter.
External Costs
Aside from the impact on consumption, other factors may be relevant to policymakers in selecting the proper level of an excise tax. One key concern is the “efficient” level of taxation that requires smokers to fully internalize the social costs of their smoking (Chaloupka and Warner 2000). From an economic perspective, the main purpose of excise taxes is to make the cigarette consumer who decides to buy cigarettes pay not only for the cigarettes themselves but also pay an amount equivalent to the costs that their smoking imposes on the rest of society. Such a “Pigouvian tax” raises the price of cigarettes to an economically efficient level by internalizing the external costs of consumption.
Computations of the external cost per pack of cigarettes, however, have hinged on exactly how the external costs of smoking are defined. As Chaloupka and Warner observed, “there is no complete consensus on precisely what consequences warrant inclusion, and even for those for which there is consensus, estimates of the magnitude of the true social externalities vary widely” (Chaloupka and Warner 2000, p. 1579). For example, some economists would regard the injury that a smoking mother confers on her children as an internal cost within the family, whereas others would count it as an external cost. Thus a study by Hay (1991) estimated that the costs
of the long-term intellectual and physical consequences of smoking-related low-birth-weight disabilities implied a tax of $4.80 per pack (Hay 1991). Although economists would generally agree that the effects of ETS outside the family should be considered an external cost, an earlier estimate of the external costs (15 cents per pack) by Manning and colleagues (1989) was later criticized because the authors did not have full information on the consequences of ETS exposure at the time (Chaloupka and Warner 2000).
Other economists have pointed out that many smokers would like to quit and regret having made the decision to become a smoker. As discussed in Chapter 2, individuals typically become smokers when they are adolescents, at a time when the costs of smoking are not fully understood or anticipated. In this sense, the adolescent did not take into account the “costs” being imposed on the older addicted smoker who now regrets his or her earlier decision. From that standpoint, many current smokers favor higher prices, and that very fact should be taken into account in analyzing the most efficient level of taxation. In general, it takes a peculiarly strong faith in consumer rationality to apply the standard Pigouvian calculus to an inherently hazardous product to which people become addicted as teenagers.
Regressivity
Whatever the most efficient level of taxation, another concern is that higher taxes may be regressive; that is, poorer people may pay more per capita than would people with higher incomes because the prevalence of smoking is considerably higher among people with lower incomes and less education than among people with higher incomes and more education (see Chapter 1). Ordinarily, there might well be a legitimate concern when a tax increases the price of a good, simply because increases in the prices of goods particularly affect those who are the least able to pay. Tobacco is not an ordinary good, however. Its consumption is (and is perceived to be) a harm to many of its consumers. To the extent that the pool of smokers includes a disproportionate number of less educated and lower-income people, a tax may well benefit them rather than harm them. To the extent that an excise tax decreases smoking initiation and helps to spur decreases in smoking, its beneficial effects may well be concentrated among the poorer members of society. For this reason, the concern about the regressivity of any tax increase seems to the committee to be somewhat overstated, even misplaced. Nevertheless, the main implication of concern regarding the regressivity of tobacco excise taxes, in the committee’s view, is that distributional concerns should be taken into account and that higher taxes should be coupled with state financing of cessation programs and services, especially for lower-income smokers.
New Measures
The states and the federal government should use tobacco excise taxes for the dual purposes of reducing consumption and funding tobacco control programs. Taking into account only tobacco control considerations, the committee believes that the ideal situation would be a uniform level of tobacco excise taxation for the entire nation at the highest feasible level. Feasibility here refers to the need to minimize cross-border smuggling and to minimize an unfair and politically unacceptable impact on current smokers, especially disadvantaged populations. A uniform tax would presumably be most efficiently administered at the federal level, although the revenues could be distributed to the states according to a mutually agreeable formula that would lead the states to refrain from exercising their own taxing authority; however, a plan under which the federal government “preempts” the field of tobacco excise taxation may be regarded as too radical at the present time.3 Another possibility would be for the federal government to coordinate a system that creates incentives for states to reduce the disparities in state excise taxes. In Chapter 6, the committee presents the outline of a plan under which the federal government would link the availability of federal subsidies for a state’s tobacco control expenditures to the amount of these tobacco control expenditures and the level of the state’s tobacco excise tax. Among other purposes, this plan is designed to use federal spending leverage to induce states with lower tobacco excise taxes to raise them, reducing the disparities in state excise taxes.
Unless and until the federal government takes on such a coordinating role, cross-state smuggling is likely to remain a serious problem. For the purposes of the policy blueprint being outlined in this chapter, the committee’s assumption is that the current legal structure of tobacco control will remain unchanged. On the basis of that assumption, the states will retain the responsibility to coordinate their own efforts. To help them do that, while increasing the overall level of tobacco excise taxation, the committee recommends the tobacco excise tax rates of the states in the top quintile become the target for the remaining states. (Currently, the lower bound rate for the top quintile is about $1.25 per pack. If states with lower rates were to move their tax rates toward those in the top quintile, the variation
in state excise tax rates—and the frequency of smuggling—would be substantially lowered.) As noted earlier, all states should earmark a statutorily prescribed portion of their excise tax revenues sufficient to fund tobacco control programs at a level recommended by the CDC.
Recommendation 2: States with excise tax rates below the level imposed by the top quintile of states should also substantially increase their own rates to reduce smuggling and tax evasion. State excise tax rates should be indexed to inflation.
The federal tobacco excise tax has traditionally served as a tool for raising revenue rather than as an instrument of tobacco control. However, for the reasons summarized above, the committee thinks that the federal tobacco excise tax rate should be increased substantially—at least on the order of $1.00 per pack—even if the federal government’s overall role in tobacco control remains a supportive one. The possibility of a more substantial federal role in tobacco control is explored in Chapter 6.
Recommendation 3: The federal government should substantially raise federal tobacco excise taxes, currently set at 39 cents a pack. Federal excise tax rates should be indexed to inflation.
SMOKING RESTRICTIONS
As noted in Chapter 3, grassroots advocacy for clean air laws was the first major achievement of contemporary tobacco control efforts. Despite continuing progress in expanding the reach of legislation restricting smoking in venues with significant public exposure, the task remains incomplete. Coverage of the existing state “smokefree indoor air” laws varies significantly. Table 5-2 summarizes the coverage of state laws as of the first quarter of 2005 (CDC 2005c). This section reviews current smoking restrictions and their effects in nonresidential indoor locations (workplaces and public accommodations), group residential locations (hospitals, nursing homes, and correctional facilities), private residences, and public outdoor areas.
Workplaces and Public Accommodations
The CDC data presented in Table 5-2 indicate that as of late 2005, most states now have some restrictions on smoking on public transportation, with 23 states banning it completely and 19 states requiring either separate ventilated areas or designated smoking areas. Similarly, 44 states have placed restrictions on smoking in government work sites. 16 of these states have enacted complete smoking bans in government workplaces.
TABLE 5-2 Scope of State Indoor Air Restrictions as of 4th Quarter, 2005
|
Location |
Banned (100% Smoke Free) |
Separate Ventilated Areas |
Designated Areas |
Any Restriction |
No Restrictions |
|
Bars |
6 |
2 |
4 |
12 |
39b |
|
Commercial day care centers |
29a |
3 |
6b |
38 |
13 |
|
Enclosed arenas |
12 |
3 |
14 |
29 |
22b |
|
Government work sites |
16 |
6 |
22b |
44 |
7 |
|
Grocery stores |
13 |
3 |
19b |
35 |
16 |
|
Home-based day care centers |
23a |
3 |
1 |
27 |
24b |
|
Hospitals |
15 |
4 |
24b |
43 |
8 |
|
Hotels and motels |
1 |
1 |
17 |
19 |
32b |
|
Malls |
10 |
4 |
5 |
19 |
32b |
|
Prisons |
4 |
2 |
3 |
9 |
42b |
|
Private work sites |
11 |
4 |
16b |
31 |
20 |
|
Public transportation |
23b |
3 |
16 |
42 |
9 |
|
Restaurants |
11 |
2 |
21b |
34 |
17 |
|
aIncludes 13 states where smoking is banned when children are on the premises for commercial day care centers and 21 states for those of home-based day care centers. bIncludes Washington, D.C. SOURCE: (CDC 2005c). |
|||||
However, 20 states still have no restrictions at all on smoking in private-sector work sites. Of course, employers are free to adopt smoking restrictions on their own, and in 1998–1999, almost 70 percent of U.S. workers reported that their workplaces had an official policy prohibiting smoking in work areas and public or common areas, up from 46.5 percent in 1993 (CDC 2005e).
Table 5-2 also shows that 38 states either have weak regulations for restaurants (limiting smoking to designated areas) or have no restrictions at all. Bars are, of course, less regulated, with 39 states having no restrictions. In recent years, however, local governments have been more inclined to adopt comprehensive workplace restrictions that include restaurants and bars. New York City and Washington, D.C., are two prominent examples. As of October 2006, 342 municipalities ban smoking in restaurants and 252 municipalities require smoke-free bars (ANRF 2006). The trend toward coverage of restaurants and bars seems largely responsive to concerns about the plight of workers whose employment choices may be limited and to the failure of the market to respond to nonsmoker preferences for smoke-free venues.
Effects of Workplace Restrictions
Smoking restrictions serve three purposes: (1) they protect nonsmokers from the health effects and the noxious odors of secondhand smoke; (2) they help smokers quit, cut down on their smoking, and avoid relapses; and (3) they reinforce a nonsmoking social norm. Clean air laws, in fact, have done more to reduce consumption than any intervention other than price increases for cigarettes.
Effects on Nonsmokers ETS, or secondhand smoke, is a known carcinogen and has been associated with a variety of adverse health effects in nonsmokers, including lung cancer and coronary disease (EPA 1992). It is estimated that 43 percent of nonsmokers have biological evidence of secondhand smoke exposure (DHHS 2006) and that 3,000 lung cancer deaths and 35,000 to 62,000 coronary heart disease deaths in nonsmokers are attributable to such exposure (CDC 2002). In fact, for every eight smokers who die from smoking, one nonsmoker dies from secondhand smoke exposure (Schoenmarklin and Tobacco Control Legal Consortium 2004). In 2002, the International Agency for Research on Cancer (IARC) estimated that involuntary smoking increases the risk of an acute coronary heart disease event by 25 to 35 percent, and that the excess risk of lung cancer due to exposure to a spouse’s secondhand smoke is approximately 20 percent for women and 30 percent for men (IARC 2002).
Involuntary smoking has been found to also have adverse effects on the respiratory system. Very strong evidence of a causal relationship exists for
chronic respiratory symptoms (IARC 2002). In addition, exposure to secondhand smoke is associated with an increased risk of sudden infant death syndrome (SIDS), asthma, bronchitis, and pneumonia in young children. The CDC considers ETS exposure to be a serious public health hazard that can be effectively prevented through effective regulation designed to reduce exposure (TIPS 2006a). Furthermore, it is estimated that secondhand smoke exposure costs the United States more than $5 billion per year in direct medical costs and approximately $4.68 billion per year in lost productivity costs, although these figures are considerably lower than estimates from just 15 years ago. This difference is attributed to reductions in both the number of people smoking and the rate of ETS exposure for nonsmokers (Behan et al. 2005).
A study of hospitality workers in New York showed that the percentage of hospitality workers exposed to ETS declined by 85 percent within the 12 months after the state’s smoke-free indoor ban took effect. During the same period, hospitality workers reported a 57 percent decline in sensory symptoms of ETS exposure, such as eye irritation, runny nose or sneezing, and sore or scratchy throat, and a 37 percent decline in upper respiratory symptoms, including wheezing, coughing, phlegm, and shortness of breath (Farrelly et al. 2005).
Effects on Consumption by Smokers Substantial evidence indicates that workplace smoking restrictions have been effective in decreasing cigarette consumption and increasing smoking cessation among active smokers. Various studies have shown that smoke-free workplace laws reduce smoking prevalence by amounts ranging from 3.8 percent to 6 percent and consumption among continuing users by 2 percent to 14 percent (Bonta, Appendix B). One 2002 study estimated that a smoke-free policy for all U.S. workplaces would decrease per capita cigarette consumption for the entire population by 4.5 percent (Fichtenberg and Glantz 2002). In addition, studies have shown that workplace smoking restrictions increase smoking cessation. Data collected during the Community Intervention Trial for Smoking Cessation, known as COMMIT, shows that those who reported a smoke-free work site between 1988 and 1993 were 25 percent more likely to attempt to quit smoking than those who were allowed to smoke at work (Glasgow et al. 1997). One study in California demonstrated that employees at smoke-free work sites are up to 38 percent more likely to quit smoking than those who work in areas with no workplace laws against smoking (Moskowitz et al. 2000).
Studies have shown that the prevalence of smoking is 4 percent higher in states without comprehensive clean indoor air laws and that the average annual consumption is 14 packs per person higher in such states (Emont et al. 1992). Overall, clean air laws may reduce smoking prevalence by
roughly 10 percent in the general population. In addition, states with stringent smoking restrictions have an average quit rate of 50 percent, whereas states without strong smoking laws have an average quit rate of 44 percent (Bonta, Appendix B).
Ireland was the first country to institute comprehensive nationwide smoke-free workplace legislation, and initial reports indicate that the ban has been a public health success and has met with substantial public approval. In fact, survey results show, somewhat counterintuitively, that 83 percent of Irish smokers reported that they felt the ban was a “good” or a “very good” thing. Not only did the law dramatically decrease ETS in workplaces, pubs, and other public places, but also 80 percent of Irish smokers who reported quitting smoking after implementation of the ban said that the law made them more likely to quit and 88 percent said that the law helped prevent relapse. In addition, 46 percent of Irish smokers who continued smoking after the ban was implemented indicated that the law made them more likely to quit, and 60 percent reported that it decreased their overall consumption (Fong et al., in press; Fong et al. 2006).
Effects on Patronage in Restaurants and Bars Opponents of smoking bans in restaurants and bars argue that these restrictions would have a deleterious effect on business and employment in the hospitality sector. Recent research has shown, however, that this has not been the experience in jurisdictions with bans on smoking in restaurants and bars. A 2004 literature review by Scollo and Lan covering 21 studies of smoke-free policies found that there was “no negative economic impact from the introduction of smoke-free policies in restaurants and bars” (Scollo and Lal 2004). The New York City Department of Health’s First Annual Independent Evaluation of New York’s Tobacco Control Program reported in 2004 that after the passage of New York’s Clean Indoor Air Act (CIAA), which banned smoking in all places of employment, including restaurants and bars, there was little change in the patronage of bars. The report also found that restaurants and industry employment, alcohol excise tax revenues, and bar licenses suffered no adverse effects (RTI International 2004). Additionally, a 2002 CDC report on a smoking ban in restaurants and bars in El Paso, Texas concluded that no statistically significant changes in restaurant and bar revenues occurred after the smoking ban took effect (CDC 2004b). Moreover, residents of areas that have instituted indoor smoking bans have indicated increasing support for such restrictions. Since the implementation of New York’s CIAA, for instance, popular support for indoor smoking bans has grown with each passing year. By the beginning of 2005, 79 percent of adults in New York State reported that they supported the CIAA (RTI International 2005).
Recommendation 4: States and localities should enact complete bans on smoking in all nonresidential indoor locations, including workplaces, malls, restaurants, and bars. States should not preempt local governments from enacting bans more restrictive than the state ban.
Hospitals and Health Care Facilities
Implementation of smoking bans in hospitals and health care facilities increased substantially during the 1980s and early 1990s, largely because of the mandate of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) that all hospitals be smoke-free. This organization, which evaluates and accredits more than 15,000 health care organizations and programs nationwide, promulgated the nonsmoking standard effective December 31, 1993. Hospitals were quick to comply with the new standard, and by the end of 1994, more than 96 percent of hospitals had done so and more than 40 percent had enacted even stricter restrictions (Fee and Brown 2004). Hospital smoking bans were originally instituted because of a concern for the health of patients and reflected an effort to capitalize on the JCAHO restrictions by emphasizing the health risks of smoking. Studies conducted since the bans went into effect have indicated that they not only protect patient health, but also reduce smoking among hospital employees (Fee and Brown 2004). Some concern has been raised about the wisdom of a ban on patient smoking in psychiatric hospitals, but research has shown that such bans have been implemented with little adverse effect (Smith et al. 1999).
Few states have enacted bans on smoking in nursing homes, although most require designated smoking areas if smoking is permitted. However, both federal and most state laws permit a total ban. According to Bergman, in 2003 about 64 percent of nursing homes did not allow smoking inside, with the remaining 36 percent limiting smoking to designated areas (Bergman 2003).
Recommendation 5: All health care facilities, including nursing homes, psychiatric hospitals, and medical units in correctional facilities, should meet or exceed JCAHO standards in banning smoking in all indoor areas.
Correctional Facilities
Despite the substantial evidence of the effectiveness of workplace smoking bans and their widespread adoption in hospitals, correctional facilities have been reluctant to take aggressive steps to eliminate smoking. Unlike JCAHO, neither the American Jail Association nor the American
Correctional Association has mandated smoke-free policies for its institutions, although both have adopted resolutions supporting such restrictions (Hammond and Emmons 2005). According to a 2002 survey, at least 38 state correctional departments had enacted some form of ban (Bonta, Appendix B), but very few of these have instituted total bans (Hammond and Emmons 2005). However, there is a discernible trend in the direction of stricter policies. On July 15, 2004, the Federal Bureau of Prisons established a nearly total ban for employees and inmates at 105 prisons. Also, in 2004, California passed a law eliminating tobacco products from prisons and youth correctional facilities (Bonta, Appendix B).
The relatively modest level of restriction on smoking in correctional facilities is somewhat surprising, given the significant implications of secondhand smoke exposure in such facilities. First, the sheer size of the population is cause for concern, as approximately 2 million inmates are incarcerated in jails and prisons at any one time (BJS 2005). Second, the problem of secondhand smoke exposure is particularly acute in correctional facilities because about 60 percent of inmates are smokers and the mandatory enclosure and poor ventilation in many prisons can create very high levels of ETS (Hammond and Emmons 2005). Partially because of these concerns, the U.S. Supreme Court ruled in 1993 that inmates do not have a constitutional right to smoke and that exposure to unreasonable levels of ETS may constitute “cruel and unusual punishment” under certain circumstances (Helling v. McKinney, 509 U.S. 25 [1993]). Indeed, studies have shown that smoke-free prison policies have been effective in dramatically reducing ETS exposure, particularly in crowded or poorly ventilated areas (Hammond and Emmons 2005). In addition, banning smoking can improve overall inmate health and may reduce health care costs in prisons. Consequently, part of the motivation for California’s recent legislation was the estimated $280 million in health care costs attributable to inmate cigarette smoking (The Monitor’s View 2005).
There are practical concerns, however, about instituting smoke-free policies. Specifically, prison administrators fear that total smoking bans may lead to an increase in inmate-staff tensions and the rise of a black market for tobacco products. This concern may be somewhat overstated, though, as a 2001 survey of the 51 U.S. prison systems that had instituted bans revealed that only 2 of these systems reported any increased violence and 20 percent reported increased inmate-staff tension following the implementation of the ban (Hammond and Emmons 2005). However, these findings may be attributable to under-enforcement of the bans that have gone into effect. Patrick and Marsh report that tobacco use inside prisons often does not cease even years after universal bans are enacted (Patrick and Marsh 2001). These factors tend to mitigate the effectiveness of bans in correctional facilities. However, in the committee’s view, the positive health
effects of protecting staff, nonsmoking inmates, and visitors from ETS justify an indoor ban as well as the costs of meaningful enforcement.
Recommendation 6: The American Correctional Association should require through its accreditation standards that all correctional facilities (prisons, jails, and juvenile detention facilities) implement bans on indoor smoking.
Multi-Unit Residential Locations
Residents of apartment buildings are exposed to ETS entering the air from common areas and neighboring units, and these exposures have led to a steady stream of litigation, especially on behalf of children and medically vulnerable adults, aiming to force landlords to adopt smoking restrictions. The housing market is slowly beginning to respond to a growing grassroots support for smoke-free multiunit housing, particularly in California. Recent polling data reveal that 82 percent of those living in apartments in California support smoking restrictions in their buildings and 69 percent favor separate nonsmoking sections (Wilcox 2005). Several California-based organizations that promote smoke-free housing have been created. Most notable among these is an organization whose website, www.smokefreeapartments.org, features more than 130 apartment owners with more than 1,400 nonsmoking units, according to the most recent estimates. In addition, in 2006 the California Apartment Association, in response to member demand, began offering information on how to create smoke-free areas. However, support for apartment smoking restrictions is not limited to California. A 2003 analysis of apartment renters in Minneapolis, Minnesota, concluded that 79 percent of nonsmokers preferred that their buildings be smoke-free (Hennrikus et al. 2003). In addition, a 2003 survey of Washington State tenants found that 67 percent were interested or very interested in smoke-free housing (Tacoma-Pierce County Health Department 2003).
Despite the growing support for smoke-free housing and the fact that there is no legal impediment to legislating such a ban, virtually no legislative action has addressed smoking in multiunit residential buildings (outside common areas). No state statutes have regulated smoking in any type of private residences. For instance, in 2004, the city of Thousand Oaks, California, took an unprecedented step by adopting a resolution that one-third of the units available in every new publicly-funded apartment building in the city be designated as nonsmoking; it was the first municipality in the country to take such a step (Smokefree Apartment House Registry 2004). Similarly, in August 2005, the housing authority in Cadillac, Michigan,
voted to ban smoking in an apartment complex for seniors, making it 1 of less than 10 public housing authorities nationwide that have instituted such bans (Older Americans Report 2005). Self-imposed restrictions by landlords and developers also appear to be rare.
Some occupants of multiunit residences have initiated litigation to require landlords to provide smoke-free housing. Victims of ETS exposure may pursue legal action against fellow tenants or landlords via common-law remedies, claims of safety and health code violations, or the federal Fair Housing Act. Common-law lawsuits have been the most common, although most are settled out of court, and very few cases have reached the appellate level (Schoenmarklin and Tobacco Control Legal Consortium 2004). Plaintiffs have occasionally been successful in raising common-law property or tort claims, although such cases are rare. Some of the more successful theories include breach of warranty of habitability, breach of the covenant of quiet enjoyment, or nuisance.
Legal experts have generally been skeptical regarding the prospects of victory in such lawsuits because a plaintiff must prove that living conditions have been made unbearable as a result of secondhand smoke (Osterwalder and Beeman 2005). There are indications that legal precedent may be changing, however, as a couple was recently evicted from their condominium in Boston, Massachusetts, after neighbors complained about excessive cigarette smoke. This was the first case of its kind in the United States, and some believe that this case may have a nationwide impact (Blumberg 2005).
Rather than direct regulation, the most sensible policy is to stimulate competition for smoke-free lease terms among condominium developers and owners of multiunit dwellings while encouraging landlords to make entire buildings smoke-free, perhaps with financial incentives.
Recommendation 7: States should enact legislation requiring leases for multiunit apartment buildings and condominium sales agreements to include the terms governing smoking in common areas and residential units. States and localities should also encourage the owners of multiunit apartment buildings and condominium developers to include nonsmoking clauses in these leases and sales agreements and to enforce them.
To encourage the development and enforcement of nonsmoking clauses in leases and sales agreements, states and localities should modify any law that is perceived by landlords and developers to preclude nonsmoking clauses or to inhibit their enforcement.
College Campuses
The recent increase in smoking among 18–24 year olds highlights the importance of implementing smoking policies on college campuses. In 2005, the American College Health Association (ACHA) encouraged colleges and universities to move toward tobacco-free campuses, while taking a step-by-step approach to their policies. The ACHA strongly urged colleges and universities to prohibit tobacco use in all public buildings on campus (including classrooms, libraries, museums, stadiums, dormitories, building entrances, and dining facilities) and within twenty feet of these buildings. In addition, the ACHA urged colleges and universities to prohibit tobacco advertising in campus-controlled venues, and to prohibit the sale of tobacco products or provision of free sampling of tobacco products on campus (ACHA 2005).
According to the American Nonsmokers’ Rights Foundation (2007), about 43 colleges and universities have adopted a completely smoke-free campus, including all indoor and outdoor spaces throughout the groups of the college or university. In a study conducted by Halperin and Rigotti (2003) of public universities’ tobacco control policies, it was found that approximately half of the universities surveyed banned smoking in all residence halls and dormitories. Half of the universities also had written policies prohibiting smoking within a certain distance of all campus building entrances. However, many colleges fall well below the recommended guidelines. Halperin and Rigotti (2003) found that only 68 percent of the universities reported that no tobacco products were sold on campus, and that of the universities that did sell tobacco products, more than two-thirds (69 percent) allowed students to use their meal cards or student accounts to purchase tobacco products. Only half of the schools surveyed had written policies in place that banned the advertisement of tobacco products on campus.
Such policies restricting or prohibiting smoking on college campuses or in residential areas have been effective. For example, a study by Wechsler and colleagues (2001) found that current smoking prevalence was significantly lower among residents of smoke-free college housing as compared with residents of unrestricted housing. Cigar use was also found to be lower among students living in smoke-free residences compared to those residing in unrestricted housing. Students living in smoke-free residences were also less likely to initiate smoking (if they had not smoked regularly before age 19) compared to those living in unrestricted dorms. Borders and colleagues (2005) found that preventive education programs on campus were associated with lower odds of smoking and that designated smoking areas were associated with higher odds of smoking.
Despite the potential effectiveness of these college smoking bans, these tobacco restrictions on college campuses have been met with ambivalence. As suggested by Loukas and colleagues (2006), college officials may need to
address the issue of changing student attitudes about smoke-free campuses as policies are instated.
Recommendation 8: Colleges and universities should ban smoking in indoor locations, including dormitories, and should consider setting a smoke-free campus as a goal. Further, colleges and universities should ban the promotion of tobacco products on campus and at all campus-sponsored events. Such policies should be monitored and evaluated by oversight committees, such as those associated with the American College Health Association.
Residences and Privately-Owned Vehicles
The proportion of Americans living in smoke-free homes is uncertain. In 1999, more than 60 percent of U.S. homes reported having a strict smoking ban (no smoking allowed at any time or in any place in the home) (Levy et al. 2004). The most pertinent question, however, is what proportion of smokers are not allowed to smoke in their own homes. In 2006, Borland and colleagues published the results of a two-wave cohort survey that examined the prevalence of smoke-free policies in the residences and vehicles of smokers. Only 27.9 percent of U.S. smokers from the second-wave cohort reported having total smoking ban in their homes, although 57.1 percent of smokers reported that they do not smoke in their cars when nonsmokers are present (Borland et al. 2006).
The aim of the U.S. Department of Health and Human Services (DHHS), as described in Healthy People 2010, is to reduce the percentage of children regularly exposed to tobacco smoke at home to 6 percent. According to baseline data used to establish this target (from the National Health Interview Survey), 20 percent of children 5 years of age and younger lived in a home in which someone smoked at least 4 days a week in 1998 (CDC 2005a; DHHS 2001; 2006). By 2004, this rate fell to 11 percent, according to the U.S. Environmental Protection Agency’s 2004 National Survey on Environmental Management of Asthma and Children’s Exposure to Environmental Tobacco Smoke (EPA 2006).
Meanwhile, according to an analysis of the 1999 National Youth Tobacco Survey, 13.4 percent of middle school students and 17.0 percent of high school students reported daily exposure to cigarette smoke while they were in a car (Farrelly et al. 2001). Exposure to ETS in vehicles is an important concern, as levels of secondhand smoke in vehicles can be particularly high, even exceeding levels in bars in which smoking is permitted. Vehicles thus represent an environment in which ETS exposure can be seriously detrimental to an individual’s health, particularly to that of a child or infant (OTRU 2006).
Persuading parents to adopt smoke-free policies in their homes and cars provides an opportunity for furthering the multiple goals of tobacco control in a morally compelling context. Clean air rules in homes and cars protect children from highly injurious toxic exposures, facilitate smoking cessation by parents and other family members who smoke, and reduce the rate of smoking initiation by teenagers, especially when clean air laws are combined with parental monitoring and authoritative messages (even by parents who smoke).
Protecting Children from ETS
Not surprisingly, the most important source of ETS exposure to young children is parental smoking (DHHS 2006; Jordaan et al. 1999). National data indicate that although the percentage of U.S. children exposed to secondhand smoke in the home declined substantially throughout the 1990s, about 25 percent of children between the ages of 3 and 11 years still live with at least one smoker (DHHS 2006; TIPS 2006b). Furthermore, young children of smoking mothers continue to be exposed to ETS at a higher level than any other group of nonsmokers (Behan et al. 2005).
Children who are regularly exposed to ETS are at greater risk for a variety of respiratory ailments, including asthma, bronchitis, and pneumonia (AAP 1986; DiFranza and Lew 1996; Etzel 1997; Gortmaker et al. 1982; Mannino et al. 1996). In addition, such children are also at risk of suffering cognitive impairments. Yolton and colleagues, for instance, estimated that more than 21.9 million children are at risk of reading deficits due to exposure to secondhand smoke. They also found that exposure to smoke is associated with deficits in math and visuospatial reasoning (Yolton et al. 2005). Exposure to ETS has also been linked to serious conditions in infants, such as low birth weight and SIDS (ANR 2005; DHHS 2006). The children of smokers also miss more days of school because of illness than the children of nonsmokers (Mannino et al. 1996). Overall, annual health care costs as a direct result of children’s passive exposure to tobacco smoke is in the range of $5 billion (Aligne and Stoddard 1997).
The demonstrable health risks of persistent smoke exposure in the home has led many courts to take parental smoking into account in custody and visitation disputes (see Pierce v. Pierce, 860 N.E.2d 1087, Ohio Ct. App. 2006). These orders typically direct smoking parents to refrain from smoking in the home when children are present and sometimes up to 48 hours before they will be present (Banzhaf 2005). Some commentators have argued that, at least under some circumstances, smoking in the home can amount to child endangerment or medical neglect warranting assertion of family court jurisdiction as a basis for mandating changes in parental behavior (Chinnock 2003). Several jurisdictions at both the local and state
levels, meanwhile, have enacted or approved legislation prohibiting smoking in vehicles in which a child is present (Belluck 2007; OTRU 2006).
Reducing Smoking
Not only do household bans benefit children by reducing the adverse health effects from secondhand smoke exposure, but they also lead to reduced smoking and increased cessation by adults as well. Farkas and colleagues have conducted two studies that demonstrate this effect. Smokers who lived under a total smoking ban were more likely to report a quit attempt in the previous year, and those who made quit attempts were less likely to relapse (Farkas et al. 2000). In fact, smoke-free homes are associated with lower rates of smoking prevalence than smoke-free workplaces (Bonta, Appendix B). Similarly, a survey of Oregonians found that a full household smoking ban resulted in a doubling of the odds of a subsequent quit attempt and that for those contemplating a quit attempt (i.e., those with an intention to quit within the next month), a full ban led to a lower relapse rate (Pizacani et al. 2004). Further evidence from a survey of high school students indicates that a more restrictive home smoking policy is associated with a greater likelihood of being in an earlier stage of smoking uptake and a lower 30-day smoking prevalence (Wakefield et al. 2000). The results of studies of households with smoking bans in Australia have been even more dramatic: the odds of quitting smoking were found to be 4.5 times greater in households with a smoking ban (Siahpush et al. 2003). This evidence suggests that the social context of smoking is an important factor for smokers and that eliminating smoking from the living environment increases the rate of smoking cessation.
Reducing Initiation
Household smoking bans also have the effect of reducing smoking among youth, as the effects of parents as role models appear to be a major factor in determining children’s future smoking behavior. Studies indicate that 12-year-old children of parents who smoke are roughly twice as likely to begin smoking between the ages of 13 and 21 years as those whose parents do not smoke. Also, in addition to less smoking by parents, stricter family monitoring and rules regarding smoking were related to a lower risk of smoking initiation (Hill et al. 2005). Farkas and colleagues found that adolescents age 15 to 17 years were 74 percent less likely to be smokers if they lived in houses with smoking restrictions (Farkas et al. 2000). Other studies have verified that strong home smoking bans are associated with lower rates of smoking uptake, prevalence, and consumption among teenagers (Wakefield et al. 2000). A panel convened in June 2006 by NIH found in its review of the scientific literature on tobacco use that clean indoor air policies and laws regulating exposure to tobacco smoke have indeed proven
effective in preventing tobacco use among adolescents and young adults (NIH 2006b). In addition, a new Canadian study has raised the possibility that not only do parents influence their children’s future smoking behavior by setting an example, but parents may also physically “prime” their children to become smokers by exposing them to nicotine. The study found that the presence of cotinine in the saliva at a young age was a significant predictor of future smoking addiction (Ubelacker 2005).
Recommendation 9: State health agencies, health care professionals, and other interested organizations should undertake strong efforts to encourage parents to make their homes and vehicles smoke free.
The committee believes that a voluntary approach to reducing parental smoking in homes and vehicles is preferable to a legal prohibition. However, the committee does support otherwise appropriate legal interventions in custody or abuse cases involving parents whose smoking endangers the health of their children.
Outdoor Spaces
Smoking in outdoor spaces is the last frontier in the progressive restriction of smoking and can be expected to be controversial. Bayer and Colgrove (2002) and Chapman (2000) doubt that these restrictions can be defended on the basis of ETS exposure by nonsmokers and therefore contend that banning outdoor smoking is unambiguously paternalistic. Moreover, such bans would be difficult to enforce with an equal hand, and their enforcement would likely create a public backlash against smoke-free policies in general (Chapman 2000). Proponents of outdoor smoking restrictions, on the other hand, argue that such measures are scientifically justifiable because the nature of the atmospheric dispersion of ETS will cause nonsmokers to be exposed to equally high or higher levels of ETS in outdoor environments than they are in indoor environments (Repace 2000). Others point out that banning outdoor smoking has additional benefits, aside from reducing exposure to ETS, including reducing the fire risk, decreasing litter, and protecting the public from nuisance (Bloch and Shopland 2000). Concerns about the offensiveness of smoking are especially pronounced in crowded locations (e.g., on crowded beaches or in parks). Furthermore, the declarative effects of enacting and enforcing these restrictions are substantial because they send a powerful message about the social disapproval of smoking, a message that will not be lost on children and adolescents.
Despite the controversial nature of restrictions in outdoor places, there is a growing movement to institute such bans in California, which has
been on the forefront of many innovations in tobacco control. Survey data indicate that a majority of Californians support a ban on smoking in outdoor public places such as parks, beaches, golf courses, and sports stadiums (Gilpin et al. 2004). In November 2003, Solana Beach, California became the first municipality in the county to ban smoking on beaches, and a number of other cities in California have since followed suit. Effective January 1, 2004, the California legislature enacted a ban on smoking within 20 feet of all entrances to government buildings and state university and community college buildings. In addition, on January 25, 2005, San Francisco adopted the most expansive “curb-to-curb” outdoor smoking ban in the state, prohibiting smoking in city parks, plazas, piers, gardens, and recreational fields (Bonta, Appendix B).
Given the competing values at stake, the committee believes that this is an issue that should be resolved at the community level.
Recommendation 10: States should not preempt local governments from restricting smoking in outdoor public spaces, such as parks and beaches.
YOUTH ACCESS
In 1992, Congress enacted the Synar Amendment, aimed at addressing the continuing illegal sales of tobacco to minors. The legislation required that all states enact and enforce youth tobacco access laws and prescribed loss of federal block grant substance abuse and treatment funding as a sanction for noncomplying states. Under regulations subsequently adopted by the DHSS, the states were required to reduce the rate of retailer violations of youth-access laws to 20 percent or less by 2003. In a complementary effort, the Food and Drug Administration (FDA) adopted a comprehensive set of youth-access regulations in 1996 that included a major compliance check program under the auspices of the FDA. As noted above, however, the U.S. Supreme Court invalidated the FDA program in 2000 on the grounds that tobacco regulation was outside the scope of the agency’s authority.
Although every state has baseline legislation prohibiting tobacco sales to minors (usually the restriction of tobacco sales to those younger than age 18 years), both the Synar Amendment and the failed FDA effort reflected the fact that in the 1990s, states and localities were not enforcing youth-access provisions with any vigor. In 1996, once the rules promulgated by the Synar Amendment came into effect, the logical inquiry was whether the legislation would exert an independent positive influence on state and local enforcement practices. In an analysis of 1997 substance abuse block grant applications from all states, DiFranza concluded that “states and DHHS are violating the statutory requirements of the Synar Amendment rendering
it ineffective” (DiFranza 1999). However, in a recent review of the experience resulting from implementation of the Synar Amendment, DiFranza and Dussault (2005) gave a more positive assessment, concluding that the Synar Amendment led to universal adoption of youth-access restrictions, that DHHS pressured some states to embrace compliance testing in lieu of retailer education alone, and that most states made considerable progress in achieving the goal of reducing retailer violation rates in random inspections to 20 percent. They reiterated, however, that some states did not implement the law aggressively and that the federal government failed to put enough pressure on these states to improve their performance (DiFranza and Dussault 2005).
Even though youth-access restrictions are taken more seriously now than they were a decade ago, there is still little evidence that increased retailer compliance has had a meaningful impact on the availability of tobacco to minors or that retailer compliance has had any independent effect in reducing the rates of youth smoking initiation or levels of cigarette consumption. In the late 1990s, a number of studies of communities that engaged in proactive enforcement were conducted. Those studies were aimed at assessing the efficacy of these efforts. Rigotti concluded that “[t]hese studies have yet to provide conclusive evidence that interventions using retailer education or law enforcement alone can change the ease with which young people obtain tobacco products” (Rigotti 2001). The June 2006 NIH state-of-the-science panel on tobacco use, however, listed youth-access restrictions as one of several effective interventions for preventing tobacco use among adolescents and young adults (NIH 2006b).
Although the available evidence does not point toward an optimal level of enforcement for youth-access restrictions, it does seem clear that a visible effort to enforce supply-side access restrictions is warranted, not necessarily because it has substantial independent value but, rather, because it is a complementary component of a comprehensive package of control initiatives. Among other reasons, meaningful enforcement is needed to demonstrate that the public commitment to reducing tobacco use in the critical early years of smoking initiation is not half-hearted (Bonnie 2001). As a previous Institute of Medicine report observed in 1994:
In the long run, the real public health benefit of a reinvigorated youth-access policy lies not in its direct effect on consumer choices but rather in its declarative effects—that is, in its capacity to symbolize and reinforce an emerging social norm that disapproves of tobacco use. Legal restrictions often have important educative effects and thereby help to shape attitudes and beliefs. They do this best when they are congruent with an emergent social norm accompanied by a strong social consensus, precisely the conditions that now exist in the context of tobacco control…. Con-
versely, overt failure to implement the youth-access restrictions actually undermines the tobacco-free norm; an unenforced restriction is probably worse than no restriction at all. Unenforced laws convey the message that the intent is not to be taken seriously and thereby undermine school and community attempts to educate youth regarding the serious health consequences of tobacco use…. The message should be strong and unequivocal that tobacco use is unhealthful and socially disapproved. Youth-access laws are an essential part of that message (IOM 1994a).
A reasonably enforced youth-access restriction is an essential element of modern tobacco control efforts, and there is, in fact, widespread agreement among tobacco control activists and public health experts regarding the provisions that should be incorporated in a model law (IOM 1994b). The principal guideposts featured in such a program are as follows:
-
Establish a minimum legal smoking age of at least 18 years
-
Require that retailers establish proof of age by checking identification
-
License tobacco retailers
-
Require periodic assessments of retailers’ compliance
-
Establish administrative or civil law penalties for illegal sales
-
Prohibit self-service displays of tobacco products
One important question is whether the regulation of youth access should be left exclusively to state control, which has been the traditional approach with the exception of the brief period when the FDA’s Tobacco Rule was in force. In the committee’s opinion, the main advantage of federal action in this area is that it provides an opportunity to establish a uniform licensing mechanism for the retail sale of tobacco products. The committee therefore endorses revival of the FDA’s Tobacco Rule, which prescribes minimum requirements for retailers to prevent sales to minors and allows the states to implement more stringent requirements (see Chapter 6).
Whether or not the FDA’s Tobacco Rule is revived, the states should take the following steps to reduce tobacco sales to minors:
Recommendation 11: All states should license retail sales outlets that sell tobacco products. Licensees should be required to (1) verify the date of birth, by means of photographic identification, of any purchaser appearing to be 25 years of age or younger; (2) place cigarettes exclusively behind the counter and sell cigarettes only in a direct face-to-face exchange; and (3) ban the use of self-service displays and vending machines. Repeat violations of laws restricting youth access should be subject to license suspension or revocation. States should not preempt local governments from licensing retail outlets that sell tobacco products.
A considerable number of states and localities currently license tobacco sales outlets. The weak enforcement of youth-access laws in many states, however, suggests that the potential deterrent threat of license suspension or revocation is not being realized. States should adopt a graduated penalty scheme whereby initial offenses are tied to fines but repeat violators face license suspension and revocation. Wherever possible, enforcement authority should reside in a public health agency.
The age verification requirement of the above recommendation follows the mandate contained in the FDA’s 1996 Tobacco Rule and should be regarded as a baseline for effective monitoring of compliance. As recommended by the IOM committee in 1994 the FDA’s 1996 Tobacco Rule set the federal minimum age requirement for the purchase of tobacco products at 18 years, but left the states free to adopt more stringent regulations, including adopting a minimum age of purchase higher than 18 years. The committee favors that approach, which would be effectuated by the proposed Family Smoking Prevention and Tobacco Control Act (discussed in Chapter 6). Although raising the minimum purchase age on a national basis would stretch the law too far from social reality, states should be permitted to experiment with a 21-year-old minimum age requirement for the purchase of tobacco products.
The remainder of the recommendation fills two gaps in the MSA. The MSA failed to adopt the behind-the-counter mandate prescribed by the FDA’s 1996 Tobacco Rule. Placing product displays behind the counter not only prevents shoplifting, largely by youths, but also tends to reduce the likelihood of spontaneous impulse purchases. Similarly, the MSA failed to address the problem of youth access to vending machines, leaving it to the states to enact restrictions. This self-service mode of access to tobacco is an open invitation to violation of the proscriptions on underage sales. In view of the unlikely prospect of adult-only venues being closely policed for potential violations, the committee’s strong recommendation would be for an outright ban on vending machine sales of cigarettes. The FDA’s 1996 Tobacco Rule endorsed limiting such machines to adult-only facilities, and the 1994 IOM report Growing Up Tobacco Free similarly endorsed a ban and cautiously qualified an absolute prohibition by stating that “less restrictive alternatives to a complete ban should be adopted only if shown to be effective” (IOM 1994a).
The committee reaffirms all of the specific recommendations pertaining to youth access recommended by the IOM in 1994, including requiring sales units to contain at least 20 cigarettes (thereby banning so-called kiddie packs or “loosies”) and making it an offense for an adult to purchase tobacco products for a minor.
RETAIL SHIPMENTS
The number of Internet tobacco retailers has increased dramatically in recent years (Ribisl, Appendix M) (Parmet and Banthin 2005), generating concerns about minors accessing tobacco products and consumers evading excise tax payments. Those concerns appear to be well founded, as research findings and anecdotal data suggest that both access by minors and avoidance of excise taxes have contributed to the popularity of Internet tobacco vendors. For example, following New York City’s increase to $1.50 in excise tax per pack of cigarettes in 2002, there was an 89 percent increase in cigarettes purchased outside of the city, 18.1 percent of which were purchased over the Internet (Ribisl, Appendix M). Evasion of state excise taxes for Internet tobacco purchases is a pervasive problem. While studies suggest that few minors are now obtaining cigarettes online, researchers believe that as states adopt more restrictive approaches to retail tobacco sales, more youth may seek to purchase cigarettes from Internet retailers (Ribisl, Appendix M).
Regulation of Internet tobacco sales has presented numerous challenges for state officials, particularly because a large number of online tobacco vendors are located either outside of the United States or on Native American tribal lands (Ribisl, Appendix M). Although the federal Jenkins Act requires Native American retailers to report Internet tobacco sales to the applicable state tax administrator to facilitate collection of excise taxes from consumers (Jenkins Act, 2005), investigation and enforcement of Jenkins Act violations have been virtually nonexistent to date (GAO 2002). However, the prospects for state enforcement have recently increased by judicial decisions recognizing states’ implied rights of action against online vendors under the Jenkins Act (Banthin 2004; Campaign for Tobacco-Free Kids 2003). In July 2005, a federal judge ordered a tribal Internet seller to provide Washington State officials with its list of customers within the state to facilitate the collection of excise taxes from those residents (Washington State Department of Revenue 2005).
The nature of Internet sales—conducted anonymously and in the privacy of the consumer’s home—has also frustrated state efforts to police online sales, as officials have no practical way of ensuring that Internet vendors accurately verify the purchasers’ ages. In fact, recent studies have revealed that most Internet tobacco vendors fail to verify their customer’s age, and those that purport to do so have largely been ineffective in obtaining age verification. One study found that only 6.3 percent of Internet vendors requested that buyers submit a copy of their photo identification before a sale, and the companies that do require age verification often fulfill the orders submitted without the requested identification (Ribisl, Appendix M). Many online vendors merely require consumers to type in a valid birth date or click on a box indicating that they are 18 years or older (Ribisl,
Appendix M). Alternatively, the website may state that by submitting an order, the customer is certifying that he or she is of legal age to purchase tobacco products (Ribisl, Appendix M). Upon surveying commonly used age verification protocols, researchers have concluded that existing approaches do little to deter minors from purchasing tobacco products online (Ribisl, Appendix M) (Parmet and Banthin 2005).
Given the inadequacy of current point-of-sale age verification for Internet transactions, many states have enacted legislation to prescribe verification requirements. In 2000, Rhode Island became the first state to impose an age-verification requirement on vendors seeking to ship tobacco products into the state (Rhode Island Public Laws. Chapter 321, Section 1. Providence, RI, 1996; Rhode Island Public Laws. Chapter 210, Section 1. Providence, RI, 2000; Parmet and Banthin 2005). Before shipping any tobacco product, retailers must obtain a copy of the customer’s government-issued identification, as well as a written attestation from the consumer certifying the accuracy and authenticity of the identification. In addition, the retailer must deliver the product to the address listed on the identification and must use a delivery service that requires the signature of the addressee or another adult (General Laws of Rhode Island, Chapter 392, Section 1. Section 11-9-13.11. Providence, RI, 2005). Since the passage of the Rhode Island law, a number of states have enacted similar legislation, requiring age verification at both the point of sale and the point of delivery of tobacco products, whereas others have imposed additional obligations for Internet retailers. For example, California’s youth-access law requires that retailers check back with consumers via a phone call to confirm the delivery of tobacco products and ensure that the consumer’s credit card statement reflects that a tobacco purchase had been made (California Business & Professions Code. Section 22963. Sacramento, CA, 2004).
In 2003, Maine imposed age-verification requirements on both retailers and delivery personnel; the law required retailers to use only carriers that deliver packages only to the actual purchaser, require the purchaser to sign for the package, and require recipients to present a valid government-issued photo identification to the delivery person as a condition of and before delivery (Maine Revised Statutes Annotated. Title 22, Sections, 1551, 1555-A et seq. Augusta, ME, 2005). This law was met with resistance by state carrier companies (Kesich 2004), and in May 2005 a federal district court enjoined enforcement of the provisions of the statute applying to carriers, and the Court of Appeals for the First Circuit affirmed a year later (N.H. Motor Transportation Association v. Rowe, 448 F.3d 66 (1st Cir. 2006). The Court of Appeals held that the provision required carriers to determine whether to impose the delivery conditions listed in the statute, thereby delaying the delivery of packages containing tobacco, as well as
other packages, and was preempted by a federal law regulating cargo carriers. Although the federal courts struck down the Maine statute’s applicability to carriers, the provisions requiring retailers to request and verify the purchaser’s age were unaffected. These restrictions are similar to those imposed by other states, suggesting that courts will continue to uphold state laws that regulate retailers’ actions but that do not impose significant requirements on carriers.
To facilitate enforcement of existing legislation regulating online tobacco transactions, state officials have forged private agreements with credit card and delivery companies to restrict Internet sales and delivery of tobacco products. In March 2005, state attorneys general and the federal Bureau of Alcohol, Tobacco, Firearms, and Explosives announced an agreement with all major credit card companies under which the companies promise to prevent their cards from being used in transactions in which Internet vendors fail to comply with age verification requirements or to register their sales with state governments (US Fed News 2005). Although the response by online tobacco companies suggests that the agreement had an initial impact on retailers (Cooper 2005; Michel 2005; Tedeschi 2005), concerns remain that tobacco vendors will circumvent the deal by accepting payments from third-party payment processing companies that will serve as intermediaries between the credit card companies and the online retailers (National Journal Group 2005).
The difficulties of enforcing age verification and tax collection requirements have led some states to prohibit Internet sales and shipments of tobacco to consumers altogether. In 2000, New York State enacted Public Health Law 1399-ll, which prohibits direct shipment of cigarettes to state residents and bans carriers from transporting such shipments (2005). Brown and Williamson challenged the constitutionality of the law, but the Second Circuit Court held that any burden on interstate commerce was significantly outweighed by the statute’s benefits, and therefore the law did not violate the Commerce Clause (Brown & Williamson Tobacco Corp. v. Pataki, 320 F.3d 200, 2d Cir. 2003). Of course, the problem of enforcement remains. In July 2005, the New York attorney general announced an agreement between the state and the DHL courier company in which the carrier agreed to stop shipping cigarettes directly to residents (Times Wire Services 2006).
State attorneys general have had considerable success in forging agreements with carriers to end the shipment of tobacco products purchased over the Internet. In November, 2005, UPS announced that it would stop delivering cigarettes bought online (UPS Reviews 2005). Federal Express maintains a policy of shipping only between licensed dealers or from a distributor to a dealer and will not ship directly to consumers (Times Wire Services 2006; Tuttle 2006). However, the U.S. Postal Service declined a request by the National Association of State Attorneys General to cease
shipping cigarettes directly to consumers (Kempner 2005), on the grounds that it was not able to inspect mail without a search warrant and that it would be impractical for postal clerks to decide which packages to accept or reject (Cooper 2005). In June 2005, after these failed negotiations with the U.S. Postal Service, Rep. John McHugh of New York introduced legislation that would forbid carriers from transporting cigarettes and other tobacco products and would impose a $100,000 fine for each violation (Ovarian Cancer Research and Information Amendments of 1993. H.R. 2810, 103rd Congress, 1993).
In the committee’s view, given the difficulty of policing Internet tobacco transactions and constitutional barriers to additional, state-imposed delivery requirements, the only practical way to effectively regulate online tobacco retailers is through legislation prohibiting both online tobacco sales and shipment of tobacco products directly to consumers. This approach is supported not only by the states’ interests in reducing sales to youth and facilitating excise tax collections, but also by the states’ more general interest in reducing the convenience of tobacco purchases and thereby reducing consumption (see discussion of the goal of transforming the retail tobacco market in Chapter 6). Statutes restricting direct shipment of alcoholic beverages provide a precedent for such legislation, as most states either explicitly prohibit direct shipment of alcoholic beverages to consumers or do so practically by requiring that all transactions for alcoholic beverages take place within the state’s licensed distribution system (see Kinney, Appendix I). Under a similar legislative scheme, shipment of tobacco products would be restricted to licensed wholesale or retail outlets, and consumers would be permitted to purchase these products only in face-to-face transactions in licensed retail settings.
Recommendation 12: All states should ban the sale and shipment of tobacco products directly to consumers through mail order or the Internet or other electronic systems. Shipments of tobacco products should be permitted only to licensed wholesale or retail outlets.
PREVENTION INTERVENTIONS
The most fully developed programs for preventing tobacco use by youth have been implemented in school settings. School-based programs will remain the mainstay of group-oriented or individually-oriented prevention activities. The committee also believes, however, that investing in programs for families and health care providers is warranted, even though the evidence base remains thin. Support for these efforts should be augmented as the evidence base develops.
School-Based Interventions
Reviews and meta-analyses of school-based prevention have produced mixed results. On the one hand, meta-analyses have established that school-based prevention programs that are interactive, that teach about social influences, and that provide opportunities to learn and practice social skills have an average effect size of 0.24, which represents a 12 percent reduction in the rate of initiation of smoking among adolescents. On the other hand, some programs purporting to be of the same nature, such as Drug Abuse Resistance Education (see the meta-analysis by Ennett et al. [1994]) and the Hutchinson project (Peterson et al. 2000) have produced no significant effects.
The NIH’s June 2006 state-of-the-science panel noted that previous research showed the short-term effectiveness of school-based interventions in preventing tobacco use among adolescents (NIH 2006b). Wiehe and colleagues (2005) conducted a meta-analysis of eight studies with individuals in 12th grade or age 18 years or older at follow-up and reported that only one program, Life Skills Training (Botvin and Eng 1982) produced significant long-term effects (Wiehe et al. 2005). Skara and Sussman (2003), meanwhile, found 25 studies with long-term follow-up, 15 of which reported effects 2 or more years after the intervention, with an average relative reduction of 11.4 percent (Skara and Sussman 2003). That review also indicated that program effects were less likely to decline if programs included extended programming or booster sessions in high school.
Findings from Prevention Programs That Are School-Based Only
The reviews cited above suggest that only those programs that included 15 or more interactive sessions in middle school, that taught about social influences, and that provided opportunities to learn and practice social skills are effective in the long term. In a review prepared for this report, Flay (Appendix D) found descriptions of three such school-based programs (the Tobacco and Alcohol Prevention Project [TAPP], Life Skills Training, and Project SHOUT [Students Helping Others Understand Tobacco]) that produced an average short-term (grade 8 or 9) relative reduction in smoking onset of 22 percent that increased to 28 percent at long-term follow-up (grades 10 to 12).
TAPP (Hansen et al. 1988) was a 15-session social-influences–oriented program developed in the early 1980s. The core components of the social influences approach have been employed in many evaluated programs and Hansen (1988) provides a good description of the theory and content of this approach. It has two main core elements: (1) resistance skills training to teach skills to resist the specific and general social pressures to smoke, and
(2) normative education to correct student misperceptions of prevalence and acceptability of use. Programs using this approach also often involve active learning or the use of the Socratic or dialectic teaching approaches, open discussion, the use of peers or older admired youth as instructors, and behavioral rehearsals to ensure that skills are learned well. TAPP included the above core elements plus inoculation against mass media messages, information about parental influences, information about the consequences of use, and the making of a public commitment not to smoke. Peer opinion leaders were used to assist teachers with program delivery.
TAPP was evaluated in two cohorts of seventh grade classes in a nonrandomized study in Los Angeles County. Only cohort 1, conducted in two moderately-sized school districts, was followed into grade 10. Health education and social studies teachers received 2 days of training prior to delivering the program. By the end of eighth grade the relative reduction (RR) in past-month smoking was 26.2 percent. By the end of grade 10 there was a 19.1 percent RR in past-month smoking and 18.3 percent RR in ever smoking. In a secondary analysis of only those students present at all waves of the study, the RR in past-month smoking was 43 percent.
This was an early study of the social influences approach, and it demonstrated that the approach can be very effective. The use of peer leaders probably enhanced what program effects would have occurred with teacher-only delivery (Klepp et al. 1986, Tobler 1992). The whole-sample result is preferred as the initial estimate of program effects because it provides a more realistic assessment of what would happen under real-world conditions; however, note that the larger effect obtained for students present throughout the study could be obtained if all schools were to implement the program faithfully.
Life Skills Training (LST) is one of the most researched school-based smoking prevention or any other kind of substance use prevention program. Developed by Gil Botvin (Botvin and Eng 1982), LST consists of 30 classroom sessions with 15 delivered in grade 7, 10 in grade 8, and 5 in grade 9 (usually the first year of high school). The program was designed to teach students a wide array of personal and social skills. These include content similar to other smoking prevention programs that focus on social influences (Glynn 1989; Hansen 1988), including learning and practicing refusal and other assertion skills, information about the short- and long-term consequences of smoking, correction of misperceptions of the prevalence of use by same-age peers, and information about the decreasing acceptability of smoking in society. Other generic program content addresses the development of communication skills and ways to develop personal relationships.
Multiple studies over 25 years have demonstrated the effectiveness of the LST program when delivered by different providers, in different kinds of schools, and for different kinds of students (Botvin 2000; Botvin and Griffin
2002). Only one study has included medium-term follow-up through high school (Botvin et al. 1995). This was a follow-up of the largest single trial, conducted in 56 suburban and rural schools serving largely (91 percent) white students in three geographical regions of New York State (Botvin et al. 1990). Schools were assigned randomly to two experimental conditions (one day or video-taped teacher training) or a control condition. Level of implementation ranged from 27 to 97 percent by teacher reports, with about 75 percent of the students receiving 60 percent or more of the intervention. Six program schools and 18 percent of the students were excluded from the analysis of program effects because of poor implementation. At the end of grade 9 the RR was a relatively small 8.9 percent (1.63 percent versus 1.48 percent) for weekly smoking, reflecting the low prevalence of weekly smoking at this age. At the end of twelfth grade, the RRs were 19.7 percent (33 percent versus 26.5 percent) and 20.4 percent (27 percent versus 22 percent) for monthly and weekly smoking, respectively. For the high-implementation group, the medium-term RRs were both 28 percent. However, the RRs for the (almost) complete sample provide the most appropriate estimate of what effects could be obtained under real-world conditions—indeed, they may still be an overestimate of the effects that might be obtained when the program developer is not involved—although larger effects might be obtained with full, high-quality, implementation.
Independent evaluations of LST have found similar or larger short-term effects. In a nonrandomized trial in Spain, where the program was delivered by teachers to grade 9 students, a 21 percent RR in average monthly smoking at the end of grade 10 reduced to 11 percent by the end of grade 12 (Fraguela et al. 2003). Independent evaluations of LST in Midwestern states found a short-term RR of 22 percent in a randomized trial in rural Iowa (Spoth et al. 2002; Trudeau et al. 2003) and short-term RRs of 43 percent in current smoking and 9 percent in ever-use in Indianapolis (Zollinger et al. 2003). Another small-scale (three schools per condition) randomized evaluation in Pennsylvania found small immediate effects for girls only, and these had decayed by the end of grade 7 and were no longer apparent by the end of grades 8–10 (Smith et al. 2004). In a nonrandomized trial of a German adaptation of the life skills approach in 106 German-speaking elementary schools in Austria, Denmark, Luxembourg, and Germany, a 10 percent RR in ever smoking and less than 1 percent RR in past-month smoking were reported (Hanewinkel and Asshauer 2004).
Project SHOUT (Eckhardt et al. 1997; Elder et al. 1993) used trained college undergraduates to teach 18 sessions to 7th and 8th graders that included information on the health consequences of smoking, celebrity endorsements on nonuse, the antecedents and social consequences of tobacco use, decision making, resistance skills advocacy (writing letters to tobacco companies, magazines, and film producers; participating in community ac-
tion projects designed to mobilize them as antitobacco activists), a public commitment to not use tobacco, and positive approaches to encouraging others to avoid tobacco or quit. A unique aspect of this program was the use of newsletters and individualized phone calls in later grades. In 9th grade, five newsletters were mailed to students and two to their parents, and each student received four phone calls from trained undergraduate counselors that were individually tailored to their tobacco use status at the end of 8th grade or the prior phone call. During 11th grade approximately half of the students received two more newsletters that focused on tobacco company tactics to recruit new smokers; information on recent city, state, or national legislation regarding tobacco; cessation advice; and information on secondhand smoke. They also received one phone call that focused on eliminating smoking in restaurants and other public places, and the rights of customers and employees in those places affected by the potential ban.
The program was evaluated in 22 schools with ethnically diverse populations in the San Diego area, some suburban and some rural. Schools were assigned randomly to program and control conditions after matching on pretest levels of tobacco use. Effects observed at the end of grade 8 (14.6 percent versus 10.8 percent, RR = 22 percent) were not statistically significant. However, by the end of grade 9 the intervention produced a relative reduction in tobacco use in the past month of 30.3 percent (19.8 percent versus 13.2 percent). By the eleventh grade, the average RR was 44.1 percent (12.6 percent versus 7 percent). For the group that did not receive the grade 11 intervention, the RR decayed to only 9.5 percent. The pattern of effects observed for this study suggests that much of the medium-term effect was due to personal attention via newsletters and phone calls in grades 9 and 11. Indeed, one has to wonder if the personal attention set up a response bias among respondents, such as those who received personalized newsletters and phone calls were motivated to tell the researchers what they wanted to hear; however, lack of a differential response rate to the surveys by condition speaks against this, at least in part. Considerable research suggests that the power of similar-age peers and the power of college-age counselors for high school students should not be underestimated. Although the cost of the intervention as studied was kept down by the use of volunteer students, it is not clear how easily this model can be disseminated. The results also strongly suggest, however, that even a brief intervention during high school was enough to actually increase the effect observed at the end of grade 9.
Results from three social influence and social competence programs with 15 or more sessions over 2–4 years, preferably with some content in high school, had significant medium-term effects (i.e., at grades 10–12): an average of a 27.6 percent (range 18.7–44.1) relative reduction in smoking. The extraordinary effects of Project SHOUT may have been due to the added content on tobacco industry activities, the teaching and encourage-
ment of advocacy skills, and the personal attention. These results need to be replicated. The medium-term effects suggest that a minimal personal contact intervention of this kind in high school could increase the effects of any other program delivered in middle school.
Findings for School Plus Community/Media Programs
The reviews cited above (plus that of Flay [2000]) also suggest that the addition of mass media or community-based components to such programs can increase their effectiveness. Flay (Flay, Appendix D) found four such programs (North Karelia, Minnesota Class of 1989, the Midwestern Prevention Project, and the Vermont mass media and school project) and they produced a 40 percent relative reduction in smoking onset in the short term that fell to 31 percent at long-term follow-ups. The maintenance of such programs might keep their effectiveness levels as high as 40 percent.
Vartiainen and colleagues (1983, 1986, 1990, 1998) tested a 10-session social influences program delivered by trained health education teachers and peer leaders in the province of North Karelia, Finland. A community-wide heart disease prevention program and mass media campaign modeled on the Stanford three-cities project (Farquhar et al. 1977) was going on throughout North Karelia at the same time. Two schools received the 10-session program from the project health educator and trained peer leaders and two schools received a 5-session version from regular teachers. Two schools from another province, where there was no prevention program, were used as controls. At the end of grade 9 the RR (average of lifetime, monthly, and weekly) was 44.6 percent (for both program conditions), which decayed to 38.7 percent by grade 11. By 3 years beyond the end of high school, the RR had decayed to 22.9 percent in the health educator condition and 37.3 percent in the teacher condition; by 10 years beyond high school, the average RR was 20 percent with the two conditions not significantly different. These results can only be interpreted as the joint effects of the school-based smoking prevention program and the community-wide heart disease prevention campaign (which had a reduction of smoking as one of its targets). Thus these results suggest effects that are larger than those of the school-based programs reviewed above. The larger effects obtained by regular teachers suggests that programs might be more effective when delivered by regular classroom teachers than when delivered by visitors to classrooms, possibly because of the ongoing relationships that teachers establish with students. However, the long-term effects were no different.
The Minnesota Class of 1989 project was another in which a school-based prevention curriculum was tested in the context of a community-wide heart disease prevention program (Perry et al. 1989). The community pro-
gram consisted of community education—including mass media—and organization activities—including screening, cessation clinics, and workplace education—designed to reduce three cardiovascular risk factors: smoking, cholesterol levels, and blood pressure (Luepker et al. 1994; Mittelmark et al. 1986). The school-based smoking prevention program (Perry et al. 1992, 1994) was based on the Minnesota Smoking Prevention Program (Arkin et al. 1981; Murray et al. 1994), one of the early social influences programs, and included material on diet and exercise as well as tobacco. Seven sessions on smoking prevention were delivered by peer leaders assisted by teachers in 7th grade. In 8th and 9th grades an additional 10 sessions concerning tobacco use were delivered by teachers. The classroom components were supplemented by the development of health councils through which students participated in other cardiovascular risk reduction projects.
The smoking prevention program was evaluated with a design in which students in all of the schools in one community received both the community-wide cardiovascular intervention and the school-based smoking prevention program, and students in all the schools in another community did not. All students in one cohort were surveyed every year from grade 6 to grade 12. As in all school-based studies, attrition occurred continuously over the 6 years, and by grade 12 only 45 percent of the original participants were surveyed. There were no differences in smoking rates at sixth grade. By the end of seventh grade, after the core smoking prevention content had been delivered, weekly smoking prevalence was about 40 percent lower in the program condition, and this effect was maintained through 12th grade, 3 years after the end of direct smoking prevention instruction and a year after the end of general community education.
Like the North Karelia project, this study demonstrates that school-plus-community programming can have substantial effects that are maintained to a large extent through the end of high school.
The Midwestern Prevention Project (also known as Project STAR, Students Taught Awareness and Resistance) tested a school-plus-community (and mass media) version of the social influences approach in eight communities in the Kansas City metropolitan area. The school-based component consisted of 10 sessions delivered by classroom teachers to 6th or 7th grade students (depending on the year of transition to middle school) and 5 sessions delivered the following year (when a parent-involvement component was also implemented). Of these schools, 8 were assigned randomly to conditions, 24 other schools elected to deliver the program and 18 others elected to wait till after the project. Mass media programming was available to all communities every year. Other community-based programming started in the third year and likewise was available in all communities. At the 2-year follow-up, the RR was 37.5 percent (Pentz et al. 1989). By grades 9–10, it was 18 percent (Johnson et al. 1990). These results are difficult to
interpret because all students were exposed to the mass media and community components. The mass media programming, in particular, would be expected to reduce the difference between groups because the control group would no longer be a real control, and it might have reduced students’ rate of onset relative to if they had not been exposed to the community program. This might explain the relatively fast decay.
The Vermont Mass Media Project tested the effectiveness of a mass media social influences smoking prevention program when delivered in the context of a school-based program. Worden and colleagues (1988) undertook a careful development process to develop television and radio spots that would discourage cigarette smoking by adolescents. They randomly assigned two communities to the program condition (mass media plus school) and two matched communities to a school-only condition. There was no true control group. In the program communities, they purchased the time for airing the spots (734 TV spots in year 1 decreasing to 348 by year 4, and 248 radio spots in year 1 increasing to 450 by year 4) and provided schools with the school-based program (four sessions in each of grades 5–8 and three sessions in each of grades 9 and 10—each student in the study cohort was exposed to 4 years of program during grades 5–8, 6–9, or 7–10) and teacher training to deliver them. Neither schools nor students were told about the media programming, and the mass media programming never mentioned the school program. Thus, as far as students were concerned, there was no linkage between the two programs.
The RRs in weekly smoking among the school plus mass media program group compared to the school-only program group were 36.6 percent (14.8 percent versus 9.1 percent) at the end of the program (grades 9–11) and 28.8 percent 2 years later at grades 10–12 (Flynn et al. 1992, 1994, 1995). Larger effects were observed for daily smoking—44 percent RR at the end of the program and 36 percent a year later. It is difficult to estimate what the effects of the school-only program might have been, and, therefore, the relative contributions of the school and mass media programming. Nevertheless, this study demonstrates that well-designed media programming can produce large effects above those of the school-only program, about 80 percent of which are maintained for at least 2 years.
Summary Regarding School-Based Prevention
Flay (Appendix D) suggested, in part on the basis of the results described above, and after making adjustments for levels of adoption and implementation, that the implementation of effective school-based programs in the nation’s schools could reduce smoking onset by age 24 by 10 percent, and that effective school-based programs combined with coordinated
complementary mass media or community programming could reduce the rate of smoking onset by age 24 by 20 percent.
Recommendation 13: School boards should require all middle schools and high schools to adopt evidence-based smoking prevention programs and implement them with fidelity. They should coordinate these in-school programs with public activities or mass media programming, or both. Such prevention programs should be conducted annually. State funding for these programs should be supplemented with funding from the U.S. Department of Education under the Safe and Drug-Free School Act or by an independent body administering funds collected from the tobacco industry through excise taxes, court orders, or litigation agreements.
Parent- or Family-Based Interventions
Extensive research shows that youths reared in homes in which parents have authoritative parenting styles characterized by warmth and involvement, clear and firm boundaries, and active monitoring are less likely to engage in health risk behaviors, including tobacco use (Andersen et al. 2004; Chassin et al. 2005; Clark et al. 1999; Cohen et al. 1994; Kerr and Stattin 2000; O’Byrne et al. 2002; Simons-Morton et al. 2004; Stattin and Kerr 2000; Steinberg et al. 1994). Research also shows that youth are more likely to smoke if their parents or others in the household smoke. Despite compelling evidence showing associations between parent smoking and adolescent smoking (Chassin et al. 1996; Fagan et al. 2005; Flay et al. 1998; Jackson and Henriksen 1997; Simons-Morton et al. 2004; Tilson et al. 2004), few adolescent tobacco interventions include a parent or family component and little research has evaluated the effects of parent- or family-based interventions. Moreover, the available intervention studies have serious methodological limitations, including the fact that they have small sample sizes that typically include parents who are already motivated, they have little likelihood of being faithfully replicated, and they assess only short-term outcomes.
Some interventions have been successful at increasing parent-child communication about the risks associated with tobacco and the reasons not to smoke. Programs have also had some success at changing attitudes toward smoking among youth and knowledge about tobacco through parental influences and communication between parents and their children. Few interventions and evaluations have been aimed at increasing parental monitoring of health risk behaviors, and even fewer studies have examined whether changes in parental behaviors and increased parent-child communication about tobacco use results in changes in actual youth smoking behaviors.
Those few studies that have been conducted, however, have shown mixed results, with most showing no positive effect of these activities on smoking initiation or cessation rates.
Part of the explanation for the relative lack of parental interventions is that research has not focused on identifying the causal mechanisms and processes by which parents influence their children’s tobacco use to produce practical applications. It is plausible that parents can directly prevent their children from smoking by monitoring and restricting their activities, restricting their access to tobacco, and discouraging or disallowing their children from associating with peers who use tobacco. Alternatively, parents might have an indirect effect on adolescent tobacco use by spending time discussing tobacco-related risks with their children and suggesting alternative activities in which their children might engage (Halpern-Felsher, Appendix G).
In the absence of more substantial evidence, the committee is reluctant to include any definitive recommendation on parental and family interventions in this blueprint, aside from recommending that increasing the proportion of smoke-free homes be included as a marker of progress in tobacco control efforts. Instead, the committee emphasizes the need for more evaluation of parent interventions and their effects on youth smoking behaviors. The committee also recommends more research on how and why parental monitoring of their children’s activities and other means of involvement in their children’s lives might influence youth behavior. Such mechanistic information will allow determination of the most proximal influences on youth behavior that can be translated into parental interventions.
Health Care-Based Interventions
In addition to providing primary health care for children, adolescents, and families, the annual health visit provides a potentially pivotal opportunity for physicians to provide clinical preventive services that can reduce children’s and adolescents’ engagement in health risk behaviors, including tobacco use. As such, a number of national guidelines concerning physicians’ provision of preventive services have been developed (e.g., Guidelines for Adolescent Preventive Services; Bright Futures; Guidelines for Health Supervision of Infants, Children, and Adolescents; Health Supervision Guidelines; The Clinician’s Handbook of Preventive Services: Put Prevention into Practice; and Guide to Clinical Preventive Services).
In general, these guidelines recommend that all children and adolescents have an annual health care visit during which all patients receive confidential preventive services, including screening, education, and counseling in a number of areas such as the biomedical, emotional, and sociobehavioral aspects of their lives (e.g., alcohol and tobacco use, sexual behavior, violence, and
safety). Furthermore, the guidelines recommend that pediatricians discuss substance use as part of routine health care during prenatal visits (Kulig 2005). The guidelines suggest that, in addition to inquiring about tobacco use in general, physicians should specifically query youth about the extent to which they use tobacco; about the settings in which they use tobacco; and whether their tobacco use has had a negative impact on their social, educational, or vocational activities (Kulig 2005). Furthermore, physicians should ask their patients about tobacco use in the home, including whether the child’s parents, siblings, or other members of the household use tobacco (Kulig 2005). Health care providers need to encourage smoke-free homes and provide guidance and assistance to parents and youth on the various means of smoking cessation, including counseling and the use of nicotine replacement products and other pharmacological treatments.
Despite these guidelines, research shows that physicians’ rates of patient screening, educating, and counseling on tobacco use during routine visits are less than optimal. Physicians cite a number of barriers to their provision of clinical preventive services such as (1) their large number of patients, resulting in constraints on the amount of time that they may spend with each patient; (2) inadequate reimbursement relative to the time and effort required to provide such services; (3) fear of alienating patients and their families; (4) insufficient education and training; (5) a lack of dissemination to physicians of research supporting positive tobacco treatment outcomes and the negative effects of the failure to intervene; and (6) a lack of information about how to access referral and treatment resources (Kulig 2005). Research also suggests that whether physicians do, in fact, screen their adolescent patients about their tobacco use may be related to their overall willingness to deliver preventive services (Ozer et al. 2004).
Recent research indicates that the rates of screening, educating, and counseling of youth about tobacco use during routine medical exams can be significantly increased through skills-based training of health care providers and the implementation of clinical administrative tools, such as reminders and charting forms. Little research has been conducted, however, on whether increased rates of screening, educating, and counseling by physicians result in reduced rates of tobacco initiation or greater rates of cessation (Halpern-Felsher, Appendix F).
In addition to primary health care visits, another time in which health care providers can be effective in screening for tobacco use and referring smoking cessation is during an emergency room (ER) visit. Smokers are disproportionately more likely to visit an ER compared with nonsmokers, accounting for 40 percent of adult patients attending ERs (Boudreaux et al. 2005; Lowenstein et al. 1995). Children and adolescents raised by caregivers who smoke are also more likely to visit an ER, especially for respiratory-related illnesses such as asthma or bronchitis. Beyond acute or
emergency care needs, ERs are increasingly used by adults as their primary source of health care (Bernstein et al. 1997; Lowenstein et al. 1995). Therefore, the ER visit provides a timely and convenient opportunity, as well as the relevant patient population, for smoking screening and cessation efforts. Bernstein and Cannata (2006) showed that smokers who visit an ER have at least some interest in quitting, and that the motivation to quit is highest among patients who believe that their purpose for the ER visit is due to a smoking-related illness.
Citing these and other statistics on tobacco use among ER patients, guidelines (e.g., a joint task force comprised of individuals from the American College of Emergency Physicians, Council of Emergency Medicine Residency Directors, Emergency Medicine Residents Association, and Emergency Nurses Association; see Bernstein et al., in press) have been developed, and recommend that emergency room health care providers screen, council, and refer patients who smoke to cessation programs, with particular emphasis placed on referring patients to the national smokers’ Quitline. Despite these recommendations, tobacco screening and referral among ER health care providers is low. While ER providers are more likely to inquire about tobacco use, they are much less likely to inquire about their patients’ desire to quit or to advise or refer smoking cessation. For example, Vokes et al. (2006) showed that only 56 percent of ER patients were screened about their smoking status, with higher rates of screening for patients who had a tobacco-related illness. While 56 percent of patients who smoke were advised to quit, only 13 percent were provided with a smoking cessation referral.
Tobacco-related preventive services in the ER setting may be met with some resistance in part because ER providers do not believe that they are the correct source for initiating smoking cessation efforts. Instead, ER providers view primary health care providers as responsible for screening, counseling, and treatment concerning tobacco use (Bernstein and Cannata 2006). ER providers also feel reluctant to provide tobacco-related intervention because of perceptions that such brief interventions are not efficacious or that they have limited time for such provision of care (Bernstein et al. 2006). Nevertheless, Schroeder and other researchers argue that smoking prevention and cessation should take place for all smokers during all ER visits, and can be accomplished in a brief, 30-second intervention in which ER providers “ask, advise, and refer” their patients, with referral being to the national Quitline (Bernstein et al. 2006; Schroeder 2006; Vokes et al. 2006).
Tobacco-related screening and intervention efforts are not limited to the physician, nor do they need to be conducted solely through direct patient-provider communication. Triage or treatment nurses, social workers, health educators, and trained peer counselors can also deliver the messages. Tobacco screening, advice, and referral can be conducted through direct communica-
tion or through computerized self-assessments, kiosks in the waiting rooms, or brochures provided throughout the ER departments (see Bernstein et al., in press, for a review). These efforts can also be extended to pediatric emergency rooms, in which screening and cessation efforts can take place directly with youths who might be smoking as well as with their caregivers. Providing the clear message about the effects of second-hand smoke on children, especially when a child presents to the ER with respiratory illness, is likely to be a powerful deterrent.
Empirical data showing the efficacy of providing tobacco screening, counseling, and referral in the ER setting is limited and an inadequate number of studies have been conducted to inform the development of ER interventions. Nonetheless, evidence is accumulating suggesting that ER visits can indeed be a source of public health interventions (e.g., injury prevention), and that this public health message can be extended to tobacco cessation as well.
Notwithstanding the absence of evaluation research, the committee is persuaded by the uniform endorsement of clinical guidelines and by the general literature on physician interventions that the increased use of preventive interventions by physicians and other primary care providers during routine, acute, and ER visits for youth and adults is a worthwhile investment. For this reason, the committee believes that physicians, dentists, and other health care providers should screen and counsel their patients about their tobacco use, not only during annual health visits, but also in any other clinical context in which health screening is being undertaken, such as in emergency rooms.
Recommendation 14: All physicians, dentists, and other health care providers should screen and educate youth about tobacco use during their annual health care visits and any other visit in which a health screening occurs. Physicians should refer youth who smoke to counseling services or smoking cessation programs available in the community. Physicians should also urge parents to keep a smoke-free home and vehicles, to discuss tobacco use with their children, to convey that they expect their children to not use tobacco, and to monitor their children’s tobacco use. Professional societies, including the American Medical Association, the American Nursing Association, the American Academy of Family Physicians, the American College of Physicians, and the American Academy of Pediatrics, should encourage physicians to adopt these practices.
MEDIA CAMPAIGNS TO PREVENT SMOKING
Media campaigns have recently been used as an important measure to reduce initiation of tobacco use. Before we review them and the evidence of effectiveness, we comment on the Fairness Doctrine campaign, one of the first and one of the most effective tobacco control interventions, which focused on adult smokers.
The Fairness Doctrine Campaign
In the early decades of television broadcasting, media outlets allotted little airtime to educating the public about the health risks of tobacco use, whereas cigarette advertisements appeared on the airwaves with great regularity (Warner 1985). In 1967, however, the Federal Communications Commission (FCC) issued a ruling that required stations airing cigarette commercials to also provide airtime for antismoking messages. The FCC based its decision on the so-called Fairness Doctrine, which required broadcasters to offer balanced coverage of controversial issues of public importance (Cummings and Clarke 1998a; Farrelly et al. 2003).
The FCC’s ruling resulted in the implementation of television’s first major antismoking campaign. Between 1967 and 1970, public service announcements (PSAs) on the health consequences of tobacco use appeared on television, often during prime time viewing hours, which was a rarity for non-revenue–producing spots (Cummings and Clarke 1998a). Advocates of antismoking media campaigns have pointed to the leveling off of cigarette sales during that time period and to television viewers’ increased knowledge of the health risks of tobacco use as evidence of the PSAs’ effectiveness (Cummings and Clarke 1998b; Farrelly et al. 2003; Warner 1979, 1985). According to Warner, between 1967 and 1970 (when the antismoking messages mandated by the Fairness Doctrine appeared on the airwaves), per-capita cigarette consumption decreased with each successive year. This represents the first 4-year decline in per-capita cigarette consumption in the 20th century (Warner 1979, 1985). In comparing the actual annual percapita cigarette consumption to predictions of what the level of consumption would have been if the antismoking initiatives of the 1960s and early 1970s had not taken place, Warner found that the antismoking PSAs that aired from 1968 to 1970 were associated with a significant decline in the level of cigarette consumption. He concluded that had the FCC not mandated anti-smoking messages, the predicted level of consumption would have been 19.5 percent greater than the actual level of consumption (Warner 1977).
By January 1971, however, federal laws banning the advertisement of cigarettes on television and radio had come into effect, and the FCC could no longer require media outlets to donate airtime for antismoking PSAs
under the Fairness Doctrine. Consequently, the number of PSAs addressing tobacco use declined drastically over the next two decades (Cummings and Clarke 1998b; Dorfman and Wallack 1993). In the end, no other large-scale national antismoking media campaign would occur for almost 30 years (Farrelly et al. 2005).
State Campaigns
During the 1990s, the antismoking media campaign emerged as a key component of many states’ tobacco control efforts. California, Florida, and Massachusetts organized some of the earliest and most prominent statewide media campaigns (Pechmann and Reibling 2000), with a number of other states following suit in the latter part of the decade. Noting the importance of these state-funded antismoking media campaigns in preventing tobacco use, in 2005 the CDC reported the estimated monthly exposure of adolescents to anti-tobacco advertisements in 37 states and the District of Columbia between 1999 and 2003. The CDC study found that exposure to the media campaigns among adolescents increased considerably between 1999 and 2002, but then dropped in 2003 when states across the country, facing serious budget crises, scaled back or eliminated their antismoking media campaigns. Noting that the lack of substantial change in youth smoking prevalence between 2002 and 2004 might have been attributable to reduced exposure to antismoking media campaigns, the CDC called on states to better ensure that adolescents are exposed to state-funded antitobacco advertisements. In its review, the CDC study highlighted the discouraging declines in expenditures in Florida and Massachusetts, and to a lesser extent California, given these three states’ early dedication to funding antismoking media campaigns (CDC 2005f).
California
California launched its media campaign in April 1990 as one part of the newly established CTCP. Californians voted in November 1998 to increase the tax on cigarette sales by 25 cents per pack, and approximately 20 percent of the revenue earned from that tax was allotted to the Health Education Account to fund the media campaign and other educational initiatives (Stevens 1998). At the time of its inception, the campaign was the largest and most expensive statewide antismoking media campaign in the United States and featured paid advertisements in a wide variety of media, including television, radio, billboards, and newspapers (Popham et al. 1993, 1994a; Stevens 1998).
During the campaign’s initial phase (April 1990 through June 1991),
CDHS spent more than $28.6 million and produced more than 50 television spots, 50 radio announcements, 20 outdoor advertisements, and 40 newspaper advertisements (Popham et al. 1994a). The campaign initially focused on achieving two main goals: (1) increasing general awareness of the dangers of secondhand smoke and (2) convincing the public that the tobacco industry had employed manipulative strategies in marketing its products (Stevens 1998). To achieve the second goal, CDHS developed advertisements holding the tobacco industry responsible for smoking-related deaths and disease. “Industry Spokesperson,” one of the first ads aired in the campaign, portrayed a group of tobacco industry executives discussing the need to recruit new smokers to replace those that had either quit or died from smoking. The advertisement closes with the cynical declaration, “We’re not in this business for our health” (Stevens 1998). Another advertisement, “Testifiers,” exposed the industry’s attempts to minimize the public’s knowledge about the health consequences of smoking. Representatives of the tobacco industry were shown giving circuitous testimony and denying the adverse health effects of smoking (Dorfman and Wallack 1993). The strategy of exposing the tobacco industry’s marketing methods has since emerged as a central theme in other state and national media campaigns (Farrelly et al. 2005).
Despite the large financial investment that the state made during the first 15 months of the media campaign, funding levels fluctuated throughout the rest of the 1990s. Per-capita annual expenditures stood at about 50 cents between 1990 and 1993, fell to about 35 cents between 1994 and 1996, and then rose to about 90 cents from 1997 to 1998 (Friend and Levy 2002). Furthermore, in the latter half of the decade, California’s media campaign lost one of its most effective tools when the state prohibited the airing of advertisements that attacked the tobacco industry. In 2001, however, a newly integrated media campaign once again featured the failings of the industry (Givel et al. 2001).
Because antismoking media campaigns generally constitute just one element of statewide comprehensive tobacco control programs, evaluating the direct effects of such campaigns can be difficult. The studies that have looked specifically at California’s media campaign, however, have indicated that it has proven somewhat effective in altering tobacco-related attitudes and behavior. In evaluating the first year of the campaign (1990–1991), Popham and colleagues (1994) collected and analyzed data from the campaign’s two main target groups, students in grades 4 through 12 and adult smokers. Although they reported some mixed results, Popham and colleagues pointed to increased levels of campaign awareness and desired changes in attitudes relating to health and smoking among youth as evidence of the campaign’s beneficial impact (Popham et al. 1994b). In a
1995 study, Hu and colleagues (1995) sought to disentangle the effects of the media campaign from the effects of other factors that may have played a role in reducing tobacco use in California in the early 1990s. Controlling for increased cigarette prices and the tobacco industry’s own advertising efforts, they found that the media campaign’s antismoking messages reduced aggregate cigarette sales (Hu et al. 1995b). In addition, upon reviewing the empirical literature on the effectiveness of state-funded media campaigns, including results from the aforementioned studies, Friend and Levy determined that the California campaign, in conjunction with other tobacco control efforts, could be associated with decreases in smoking rates. They noted, however, that the evidence indicated that California’s media campaign proved most effective during its first few years of implementation (Friend and Levy 2002).
Massachusetts
Massachusetts’s media campaign closely mirrored California’s in both its origins and scope. Like California, Massachusetts organized its media campaign within the broader framework of a comprehensive tobacco control program. In early 1993, having increased the per-pack cigarette tax by 25 cents, the state established the MTCP. The MTCP unveiled the country’s second statewide antismoking media campaign in October of that year (CDC 1996; Friend and Levy 2002; Miller 1998).
Massachusetts’s campaign focused on three main themes: (1) ETS, (2) smoking cessation, and (3) the health risks (Friend and Levy 2002). Under the tagline “It’s time we made smoking history,” the campaign featured a wide variety of stylistic approaches. Several studies have indicated that the most effective spots in Massachusetts’s campaign were those that evoked feelings of outrage, sadness, and fear (Biener 2000, 2002; Biener et al. 2000b). One series of ads portrayed real people suffering from smoking-related diseases, including Janet Sackman, a cigarette model who lost her vocal cords to cancer; Victor Crawford, a tobacco lobbyist who died from throat cancer; and Wayne McClarren, a former Marlboro Man who was shown dying from lung cancer (Biener 2000). Like California, Massachusetts also highlighted the practices of the tobacco industry. The state’s 1999 media campaign, under the slogan “Where’s the Outrage?,” presented statistics on smoking-related deaths and exposed efforts by the tobacco industry to recruit young smokers (Biener 2002).
From 1993 to 2000, MTCP spent approximately $13 million per year on antitobacco advertising (Biener et al. 2000b), representing one-third of MTCP’s total expenditures (Biener et al. 2000a). Much of that investment, however, was made in the first 3 years of the campaign (CDC 1996). The state, in fact, repeatedly cut the campaign’s budget
throughout the latter half of the 1990s (Friend and Levy 2002), and in FY 2001 effectively eliminated the campaign, as the state began to reduce the scale of the tobacco program in general (Hamilton et al. 2003).
Several researchers have sought to determine the impact of Massachusetts’s media campaign on tobacco use in the state. In a 2000 study, Siegel and Biener reported the results of a 4-year longitudinal study of a cohort of Massachusetts youth, concluding that exposure to television antismoking advertisements had a significant effect on younger adolescents. Although they could not identify a significant effect among 14- to 15-year-olds, they found that 12- to 13-year-olds who had reported exposure to antismoking advertisements at the baseline were significantly less likely to be established smokers by the time that follow-up interviews were conducted (Siegel and Biener 2000). In another 2000 study, Biener and colleagues analyzed Massachusetts adults’ level of exposure and receptivity to antismoking television advertisements. With 88 percent of the cohort reporting some exposure to the advertisements, and 56 percent reporting seeing an advertisement at least once a week, Biener and colleagues concluded that the Massachusetts media campaign had achieved a high level of penetration among adults. Finding that only 12 percent of the cohort held a negative opinion of at least one advertisement, Biener and colleagues determined that the media campaign was well received by Massachusetts adults in general. They also found that the most effective advertisements for adults who had quit smoking or who were preparing to quit were those that elicited strong negative emotions (Biener et al. 2000b). In a separate study, Biener determined that Massachusetts youth responded to antitobacco television advertisements in a manner similar to adults (Biener 2002). Finally, based on their review of the empirical literature, Friend and Levy determined that Massachusetts’s antismoking media campaign, like California’s, could be associated with decreased smoking rates, specifically in conjunction with a comprehensive tobacco control program. They concluded, however, that Massachusetts’s efforts, like California’s, were most successful in the earliest years of the media campaign (Friend and Levy 2002).
Florida
Unlike California and Massachusetts, Florida did not initiate a statewide antismoking media campaign until the end of the decade, nor did Florida fund its program with excise tax revenues (Friend and Levy 2002). Instead, the state used funds from a settlement that it reached with the tobacco industry in August 1997, which provided the state with $11.3 billion over the course of 25 years (Givel and Glantz 2000; Sly et al. 2001b).
After establishing the Florida Tobacco Pilot Program (FTPP) in early
1998, state officials immediately set out to develop and implement a large-scale antitobacco media campaign (Givel and Glantz 2000). Unique to Florida, this campaign would focus exclusively on youth (Sly et al. 2002). While performing background research, FTPP staff determined that the program’s target audience perceived traditional PSAs as preachy and severe. Consequently, FTPP incorporated efforts to work with youth representatives in developing a media campaign that would be better received by younger viewers. Industry manipulation emerged as a theme of particular resonance. At the March 1998 Teen Tobacco Summit, youth participants, angered by the tobacco industry’s marketing practices, selected “truth” as the campaign’s brand name. The state and its partners would continue to solicit youth input even after the campaign’s initiation (Givel and Glantz 2000; Zucker et al. 2000).
During the campaign’s first 10 months, 12 advertisements appeared on the airwaves statewide (Sly et al. 2001b). The campaign also included outdoor signage, print ads, and posters. T-shirts, baseball caps, and other merchandise featuring the “truth” brand complemented the advertisements. In addition, in the summer of 1998, youths, politicians, and celebrities participated in a cross-state train tour that promoted the “truth” campaign and its message (Zucker et al. 2000).
Initially, the 1997 settlement forbade Florida from attacking the industry and limited the antitobacco campaign to 2 years. In September 1998, however, Florida reached a new agreement with the tobacco industry that lifted the ban on industry attacks as well as the 2-year time limit. Subsequently, the “truth” campaign turned to exposing the industry’s manipulative tactics. To capture the attention of young and savvy viewers, the campaign produced advertisements in a range of styles, from high-tech to home video. One advertisement that appeared in the wake of the 1998 settlement renegotiation portrayed the tobacco industry as the villain in a mock film trailer. Another, “Demon Awards,” showed the tobacco industry accepting an award for the amount of deaths it has caused; fellow attendees included Hitler and Stalin (Givel and Glantz 2000; Zucker et al. 2000).
Data from Florida indicate that the “truth” campaign quickly succeeded in reducing tobacco use among youth. In their review of the literature on the effectiveness of statewide antismoking media campaigns, Farrelly and colleagues point to the results of the Florida Youth Tobacco Survey, which indicate that after the first year of the campaign, the rate of smoking among middle school and high school students dropped by 18 percent and 8 percent, respectively (Farrelly et al. 2003). The CDC declared the drop in teen smoking following the first year of the campaign to be “the largest annual reported decline observed in this nation since 1980” (CDC 1999b). Several studies, meanwhile, have established the “truth” campaign’s success in generating high levels of message and campaign awareness (Sly et al.
2001a; Zucker et al. 2000), and a 2001 study, based on longitudinal survey results, associated exposure to the media campaign with a lower likelihood of youth smoking initiation (Sly et al. 2001b). Finally, in comparing the effectiveness of Florida’s media campaign with a similar national effort (see below), Niedereppe and colleagues found that Florida teenagers were less likely than teenagers in the rest of the United States to have smoked in the previous 30 days. Moreover, that study determined that Florida teenagers had higher levels of antitobacco awareness and held less favorable opinions of the tobacco industry than their national counterparts (Niederdeppe et al. 2004).
American Legacy Foundation’s National truth®Campaign
As already described, antismoking media campaigns have, in recent years, primarily been implemented at the state level. In February 2000, however, the American Legacy Foundation (Legacy) launched the first comprehensive national antismoking media campaign in the United States since the Fairness Doctrine era (Farrelly et al. 2005).
Modeled closely after Florida’s program, Legacy’s own truth® campaign promoted a similar counterindustry message (Niederdeppe et al. 2004). In an effort to appeal to the campaign’s target audience (youth between the ages of 12 and 17 years), Legacy featured trendy teenagers in its truth® advertisements and (borrowing another element from Florida’s campaign) marketed its message as an integrated brand, complementing the television spots with promotional items, street marketing, and a website (Farrelly et al. 2002).
Unlike the directive-oriented “Just Say No” antismoking PSAs of the 1970s and 1980s, the Legacy-produced advertisements vividly delivered stark facts on industry marketing practices and the health consequences of smoking. One prominent ad from the truth® campaign, “Body Bags,” portrayed a group of youth piling bags outside the headquarters of a tobacco company. They announced through a megaphone, that the bags represented the 1,200 people killed by tobacco each day (Farrelly et al. 2002, 2005).
Between 2000 and 2002, Legacy spent approximately $100 million per year on the truth® campaign (Farrelly et al. 2005). To evaluate the effectiveness of this substantial investment, in 1999, it began sponsoring the Legacy Media Tracking Surveys, which, among other indicators, measured exposure to ETS, access to tobacco products, knowledge and attitudes regarding tobacco use, intention to quit, and awareness of the truth® campaign and its messages among 12- to 17-year-olds and 18- to 24-year-olds. Survey results showed significant increases in campaign awareness among youth, as well as growing support for campaign-sponsored messages just 10 months into the campaign (Farrelly et al. 2002). Data have also revealed
an accelerated national decline in youth smoking following the initiation of Legacy’s national truth® campaign (Farrelly et al. 2005).
Effectiveness of Media Campaigns
National or statewide media campaigns intended largely or primarily to discourage the uptake of smoking by youth appear to be, in most cases, reasonably effective in achieving their goal. This finding was reaffirmed by the NIH’s June 2006 state-of-the-science panel, which identified mass media campaigns as one of three effective approaches to reaching the general population and preventing tobacco use among adolescents and young adults (NIH 2006b).
Effect sizes, as noted in the technical appendix (Slater, Appendix N), appear to average about 6 percent relative to the preexisting rate—that is, the rate of smoking among youth in the particular population being studied falls about 6 percent. These effects appear to be reasonably consistent in studies that use a variety of different evaluation designs within regional and national field intervention contexts.
Although these effect sizes are modest and cost of achieving them is high, the reach of television and other media-based campaigns is exceptionally broad; a 6 percent relative effect size in the context of a media campaign represents a substantial number of young people, especially in a national campaign. Slater (Appendix N) suggests that the absolute prevalence of smoking among American youth is probably about 2 percent less than it would be in the absence of such campaigns and that further efforts might make that prevalence another 1 percent lower. In other words, if such media campaign efforts were to end and their effects to date were to dissipate, the prevalence of smoking in each succeeding cohort of youth might be expected to be 3 percent higher than it would be if such campaigns were to continue. This means that millions more American youth will begin smoking over the next twenty years than would otherwise be the case. It should also be noted that the effects of campaigns to discourage the uptake of smoking by youth are probably conservative, in that they do not take into account the possible effects on uptake among youth younger or older than the target age or the likely reinforcement of public support for local, regional, or national tobacco control policy efforts.
It also should be noted that most evaluations of such campaigns have taken place in contexts in which a variety of other community or regional education or control efforts are taking place. In most cases it is not possible to distinguish the extent to which the effects of media campaigns are facilitated by such efforts or, conversely, to identify the extent to which such local efforts are supported by media campaigns. (There is some empirical evidence regarding the reinforcing effects of media efforts on in-school
smoking prevention curricula; see Appendix D for information on such curricula.) Some evaluations, however, (Farrelly et al. 2005) have examined the independent effects of potential media exposure, suggesting that the effects that they find are attributable to the media campaign. Given these uncertainties, it is probably best to assume that it is preferable, whenever possible, to run such campaigns simultaneously with more comprehensive, community-based efforts.
Finally, media campaigns do have various effects, and it is entirely possible for an expensive campaign to have no effect or even effects that result in the rates of smoking moving in the wrong direction. It is essential to ensure that media interventions be research-based, with rigorous testing of the messages and periodic evaluation of their effects, and that they be independent from political pressures that might lead to efforts being driven by political agendas rather than by data (Pechmann and Slater 2005). Finally, it should be noted that it is considerably more cost-effective to purchase media time and space nationally than on a state-by-state basis.
Recommendation 15: A national, youth-oriented media campaign should be funded on an ongoing basis as a permanent component of the nation’s strategy to reduce tobacco use. State and community tobacco control programs should supplement the national media campaign with coordinated youth prevention activities. The campaign should be implemented by an established public health organization with funds provided by the federal government, public-private partnerships, or the tobacco industry (voluntarily or under litigation settlement agreements or court orders) for media development, testing, and purchases of advertising time and space.
CESSATION INTERVENTIONS
An estimated 44.5 million adults in the United States are smokers, and these individuals comprise about 20.9 percent of the adult population (CDC 2005g). If nothing is done to help them stop smoking, almost half of them will die prematurely of tobacco-related diseases. On the basis of projections of future smoking prevalence by use of current smoking trends among adults in the United States, there will be at least 33 million smokers 20 years from now, regardless of how well the next generation of young people is prevented from initiating tobacco use and becoming addicted to tobacco.
Abundant epidemiological evidence demonstrates that populations who quit smoking have improved health status and lower rates of morbidity and mortality compared with those of populations that do not quit. Increased
population smoking cessation rates will likely decrease cigarette smoking prevalence rates more quickly than an approach focusing exclusively on reducing initiation rates. Accelerating cessation among current smokers will produce immediate benefits, saving millions of lives and billions of dollars over the next decade (see work of Levy, Appendix J and Mendez, Appendix K, and later in this chapter “Projected Impact of Strengthening Measures”).
In general, the committee favors a comprehensive, coordinated system of care management for cessation treatment. Such a comprehensive system of care management has five key components: (1) motivating more smokers to make more frequent quit attempts; (2) educating smokers to use evidence-based interventions when they do try to quit; (3) reducing the extraordinarily high rates of relapse after cessation; (4) ensuring that all smokers receive continuity of care management and follow-up, including access to the best care available and full insurance reimbursement; and (5) structuring the comprehensive system of care to provide additional levels of more intensive/specialized treatment (i.e., stepped-care) for smokers that need them (i.e., those who fail to quit with lesser levels of care). Stepped-care is especially important for smokers who are hardest to reach and hardest to treat, such as those at disproportionate risk of treatment failure (e.g., underserved, low-income, uninsured smokers and those with comorbid psychiatric/substance abuse and medical disorders—see also Wallace, Appendix P). The overriding challenge is to educate and motivate more smokers to try to quit and to provide suitable access to effective cessation interventions for as many smokers as possible.
Effective Interventions Exist
A large number of randomized clinical trials and other research studies confirm the efficacy of smoking cessation interventions (Fiore et al. 2000; Hopkins et al. 2001; Task Force on Community Preventive Services 2005) (see Abrams, Appendix A). Interventions can be categorized in terms of the type of intervention, the venue, the intensity, the duration, and the cost. Interventions may be behavioral, pharmacological, or both. They can be administered by health care or other professionals, lay volunteers, or they can be self-administered. They can be guided interventions available in print media, on the telephone, via the Internet, or through purchase of over-the-counter treatments. They may be administered incidentally to other activities, such as at the workplace, during health care visits, and during educational activities. Interventions may include brief episodes of counseling or prolonged programs addressing both cessation and cessation maintenance.
In general, greater intensity of treatment (duration and number of
contacts, more modalities of intervention) improves cessation outcomes (for details see Abrams, Appendix A). At the risk of oversimplification, the committee believes that intervention intensity can be classified into three broad categories: (1) minimal, (2) moderate, and (3) maximal. Abstinence at a minimum of 6 months follow-up is related to the intensity of the intervention in a dose-response fashion. Abstinence rates range from (1) about 5–10 percent for smokers quitting on their own or using self-help materials; (2) 10–20 percent for brief, moderate intensity interventions; (3) 20 percent to over 30 percent for maximally intensive individual or combined pharmacological and behavioral interventions (Fiore et al. 2000).
Along with behavioral therapy, pharmacotherapy is an important adjunct to smoking cessation treatments. Currently marketed pharmacotherapies include nicotine replacement products (gums, patches, nasal sprays, inhalers, and lozenges), bupropion, and other recent agents such as Varenicline—a novel α4β2 nicotinic receptor partial agonist pharmacotherapy. In clinical trials, existing pharmacotherapies can improve cessation rates by 1.2 to 2.5 times, on average, compared with those achieved with a placebo (Fiore et al. 2000). Combined behavioral and pharmacological treatment can triple to quadruple cessation rates but these results are not as consistent across studies. The limitations of the pharmacotherapies are that their effectiveness is moderate (achieving cessation rates of 10 to 20 percent, depending on the population of smokers and whether concomitant behavioral therapies are used) and the fact that many dependent smokers have already tried these therapies and failed to quit smoking when they have used them. Most studies of re-treatment with the same medication find that cessation rates are very low.
Thus it is imperative that new medications and other new psychosocial treatments or modes of delivery be developed to aid smoking cessation. Such medications might be more effective than existing medications, which is particularly important for highly nicotine-dependent smokers. Even if new medications are not more effective than the currently available medications, new medications would provide an alternative to current medications and would encourage more smokers who failed cessation in the past to consider making another quit attempt using the new medication. In addition to medications, helping smokers who have repeatedly failed to quit may require more intensive and specialized treatments such as a stepped-care approach (for details see Abrams et al. 1996, 2003). Services might also include a comprehensive system of care management that enables smokers to obtain better continuity of care and follow-up. Smokers with higher levels of nicotine dependence and those with comorbid psychiatric/substance abuse disorders might especially benefit from new pharmacotherapy and a new systems of care management (for details see Abrams, Appendix A and Wallace, Appendix P).
In moving from clinical trials to large-scale community dissemination research, intervention strategies generally shift from treating highly motivated volunteers to reaching out to a more diverse, less-motivated population of smokers. In this community-wide effort, interventions with different types, modes, methods, and channels of delivery are used to reach defined subpopulations on the basis of geography, demography (e.g., age, gender, race, ethnicity, or impoverishment), clinical status (e.g., the presence of a psychiatric comorbidity or pregnancy), health plan, insurance status, or other group status (e.g., youth smokers in secondary schools). Each high-prevalence group represents special challenges to community-based tobacco control efforts. Interventions that are translated from clinical to community settings reveal considerable variability in outcome effectiveness and effect sizes are therefore more difficult to calculate with confidence.
The Limitations of Cessation Programs
Although cessation programs have much to offer, they also have limitations and shortcomings. Less than 50 percent of the 44.5 million current smokers make a quit attempt each year. Of those that try to quit, over 70 percent do so on their own without use of evidence-based programs, and, of those, over 90 percent will relapse. Most programs are evaluated for a maximum of only 6 to 12 months, and efficacy beyond that point may not be well understood; long-term relapse rates have also been documented. Furthermore, randomized trials of interventions are often conducted with smokers who are motivated to quit and who are free of many impediments to program participation; such trials possibly yield higher cessation rates than would occur in general community settings (for details see Abrams, Appendix A).
Less intensive, less costly, and less specialized programs, however, can reach more smokers, with the most intensive interventions being reserved for those that require them. (Abrams et al. 1996, 2003; Orleans 1993). For example, a two-tiered intervention based on intensity and cost might consist of (1) standard care, such as brief behavioral therapy and over-the-counter nicotine replacement therapy; and (2) intensive specialized care, such as the use of multiple clinical sessions and prescription medications, and treatment delivery by addiction specialists. Smokers who either fail standard care or have comorbid complications can be placed on more advanced specialized care. An explicit clinical trial of stepped-care has not yet been published, but many delivery systems implicitly use some form of stepped-care in their intervention programs, in addition to the minimal levels of care recommended by U.S. Public Health Service Guidelines (Fiore et al. 2000).
The Challenge: Increasing Rates of Smoking Cessation at the Population Level
Despite the presence of many successful interventions, the impact of smoking cessation efforts on reducing population smoking prevalence is currently small and falls far short of its potential. The NIH’s June 2006 state-of-the-science panel on tobacco use summarized this challenge as follows: “Most adult smokers want to quit, and effective interventions exist. However, only a small proportion of tobacco users receive intervention. This gap represents a major national quality-of-care problem” (NIH 2006b, p. 11). Interventions are underused for a variety of reasons pertaining to the individual consumer (a lack of knowledge of or demand for cessation programs) as well as to systems and organizational barriers, such as the failure to provide accessible, comprehensive, convenient, continuous, and affordable treatments. Achieving higher cessation rates can be attained by increasing the demand for and use of existing evidence-based cessation interventions by (1) reaching more smokers with cessation messages—including education about the quitting process—as well as the availability and the safety of smoking cessation modalities and products for tobacco use cessation, such as nicotine replacement therapies; (2) motivating more quit attempts among people who now make none, and more frequent quit attempts among those who now try by providing meaningful incentives to quit; (3) increasing the use of evidence-based interventions when smokers are attempting to quit; (4) providing continuity of care, tailored and targeted interventions, and a stepped-care model for those with smoking histories and other individual susceptibility characteristics (e.g., comorbidity) who need more intensive and specialized treatments; and (5) providing adequate and aligned financial, political, and policy initiatives to fully integrate all the effective components into a comprehensive, multilevel system of care, commensurate with the need to address the nation’s largest preventable cause of disease and death.
Currently, the demand among smokers for cessation programs and services remains modest, despite the desire of most smokers to quit (NIH 2006b) and the increasingly restrictive environmental and normative social climate against smoking. A multifaceted approach to increasing the demand for smoking cessation programs can include increasing restrictions on smoking, mass media campaigns, financial incentives, and efforts to create a strong consumer-driven demand for attractive smoking cessation products and services. These same strategies were identified by the NIH’s state-of-the-science panel as effective methods of increasing the use of cessation interventions (NIH 2006b).
Data addressing the demand for cessation services among smokers are available. For example, Zhu and colleagues (2000) reported that 78 per-
cent of smokers believed that they were just as likely to quit on their own as with assistance, but smokers who believed that cessation assistance was effective were twice as likely to intend to quit or make a quit attempt and more than three times as likely to use intervention assistance when quitting (Zhu et al. 2000). Hammond and colleagues (2004) surveyed smokers’ perceived effectiveness of cessation methods and found that the great majority of respondents said they wanted additional information on where to get help quitting (87 percent), how to quit (86 percent), the benefits of quitting (85 percent), and toll-free quitlines (70 percent), and that they wanted access to a website that would provide more information about cessation (68 percent). Respondents had inadequate awareness of the availability and utility of clinical cessation intervention methods, such as counseling (Hammond et al. 2004). Yong and colleagues (2005) reported that older smokers (those older than age 60 years) perceived themselves to be less vulnerable to harm (self-exempting beliefs), less concerned about the health effects of smoking, less confident about being able to quit (self-efficacy), and less willing to try to quit. However, respondents’ knowledge of cigarette prices, health providers’ advice, inexpensive medications, and health risk information was associated with a greater intent to quit and more quit attempts (Yong et al. 2005).
Although the best mix of smoking cessation strategies remains unclear, the overarching objective is readily apparent: In order to enhance program use and population cessation rates, smokers must know that safe, effective, and accessible cessation programs—including medications—are available. It is important to point out that from an population perspective, overall impact is a product of “reach × efficacy” (Abrams et al. 1996). Thus reaching a larger number of smokers with a somewhat less effective intervention can produce a greater number of people who quit than reaching a small number of people with a more effective intervention. Getting more smokers to use even a minimal intensity cessation program generally doubles the likelihood of success and therefore makes an important contribution to the overall impact on population smoking prevalence rates.
Recommendation 16: State tobacco control agencies should work with health care partners to increase the demand for effective cessation programs and activities through mass media and other general and targeted public education programs.
Disseminating Cessation Programs
Well-performed studies on the ability to disseminate smoking cessation programs to the community provide reasonable and reliable data as a
basis for projecting the impact, on a populationwide basis, of the efficient implementation of the best available practices. An important example is the use of quitlines, which can increase smoking abstinence by as much as 30 to 50 percent over the rate achieved under control conditions (Fiore et al. 2000). On the basis of the growing body of evidence from smoking cessation program dissemination research trials and the extensive deliberations of an expert panel, Fiore and colleagues recommended funding a national telephone quitline as a means of reaching more smokers, achieving an additional 5 million quitters per year, and saving 3 million lives over the next two decades (Fiore et al. 2004).
Quitlines have proven to be an effective smoking cessation intervention. Recognizing their value in helping individuals to stop smoking and acknowledging recommendations for a more robust, countrywide quitline, DHHS established a national quitline network in 2004. The network increased funding to states with existing quitlines, offered grants for the creation of quitlines in states that did not yet provide the service, and made available smoking cessation counselors in states without quitlines (DHHS 2004).
Given the demonstrated success of smoking quitlines and the ease by which most Americans can now access them, the national quitline network is an important cessation tool that should be maintained with adequate funding. Other emerging technologies are also beginning to show promise such as the use of tailored evidence-based cessation programs delivered on a 24/7/365 basis via the internet, either alone or in combination with quitlines, or brief primary care interventions in physician’s offices (for details see Abrams Appendix A).
Recommendation 17: Congress should ensure that stable funding is continuously provided to the national quitline network.
The quitline is a highly useful intervention because advertising the availability of the quitline helps to stimulate demand and accessing it provides a low-cost service for facilitating cessation. What other steps should be taken to stimulate awareness of and demand for cessation technologies? Would a large-scale social marketing campaign be cost-effective? Unfortunately, important gaps in knowledge on how to expand cessation awareness and demand remain, particularly for some large and important smoking populations, such as youth. Some evidence indicates that mediated communication efforts can be effective in facilitating smoking cessation (Snyder et al. 2004), but expanding the use of cessation technologies will require improved communication, education, and marketing.
At present, the evidence on how best to combine media interventions, other social marketing techniques, and innovative strategies for dissemi-
nating cessation technologies is inconclusive. Without such evidence it is premature to endorse a major national media and social marketing effort intended to accelerate smoking cessation rates. The immediate goal should be to identify successful combined strategies, with the intent of implementing them on a national scale with public funding, with resources provided by public-private partnerships, or with funds provided under court orders or litigation settlements with tobacco companies.
Recommendation 18: The Secretary of the U.S. Department of Health and Human Services, through the National Cancer Institute, the Centers for Disease Control and Prevention, and other relevant federal health agencies, should fund a program of developmental research and demonstration projects combining media techniques, other social marketing methods, and innovative approaches to disseminating smoking cessation technologies.
If such projects show success, future efforts should be national in scope and should be implemented by a public health organization with no ties to the tobacco industry and with funds provided by the federal government, public-private partnerships, or the tobacco industry (whether voluntarily or under litigation settlement agreements or court orders) for media development, testing, and purchases of advertising time and space. Regional, state, or local funding should be provided to supplement the national campaign with coordinated cessation activities.
Delivering Cessation Services
Targeting populations with a high smoking prevalence at the community level is part of any important tobacco control program (for a discussion on these populations, see Wallace, Appendix P). However, for the general delivery of cessation services within the health care system, the adoption of an integrated, multilevel, systems approach is needed to maximize the potential for carrying out all the components of effective cessation programs in an organized, evidence-based manner. It is important to align clinical policies and delivery system structures to support and finance tobacco cessation as a chronic, refractory, addictive condition and to approach it as one might approach the chronic management of hypertension, diabetes, or asthma. Such an approach would ensure continuous engagement with smokers and provide coordinated, tailored interventions before, during, and after they quit smoking. Smokers must be supported in their cessation efforts at every level of the infrastructure of health care delivery systems through the use of aligned policies, financial incentives, and full reimbursement for the costs that they incur in their cessation efforts.
Ideally, health care delivery systems, such as managed care organizations and mental health clinics, not only should foster comprehensive smoking cessation management but also should track the type and extent of care delivered within that system over time as a matter of quality assurance. For example, a managed health care organization may have a policy that requires all providers in all settings (e.g., emergency rooms, primary care, and specialty care settings) to screen for smokers and to develop, document, and implement an individualized treatment plan for each smoking member of the health plan. Surveillance and measurement of key performance and quality indicators will improve accountability, fidelity, and adherence to best practices. Such activities are already in place in quality assurance programs, such as those promoted by the National Committee for Quality Assurance.
Recommendation 19: Public and private health care systems should organize and provide access to comprehensive smoking cessation programs by using a variety of successful cessation methods and a staged disease management model (i.e. stepped care), and should specify the successful delivery of these programs as one criterion for quality assurance within those systems.
All health care delivery organizations should have in place a comprehensive care management system for smoking cessation that includes continuity of care, appropriate tracking systems and quality indicators and properly aligned structural and financial incentives to support providers’ and smokers’ efforts to treat their condition in much the same manner as other chronic conditions like diabetes. They should also target populations with high rates of comorbidity and high smoking prevalences.
Reimbursement for Smoking Cessation Services
Evidence suggests that institutions investing in comprehensive smoking cessation programs or services (e.g., health care facilities and worksites) will receive a substantial return on their investment within 2 to 3 years (AHIP 2004). Warner and colleagues (2004) simulated the financial impact and cost effectiveness of a smoking cessation program in a hypothetical managed care organization (MCO) using data from three large MCOs (Warner et al. 2004). Quitters gained an average of 7.1 years of life, with a direct coverage cost of $3,417 for each year of life saved. The net cost to the MCO was $0.41 per patient per month. With the costs of health care expenditures for smokers and productivity losses from smoking estimated to be more than $167 billion per year (CDC 2005d) the expected savings from the implementation of effective cessation programs could be substantial.
In recent years, there has been significant improvement in private, federal, and state insurance coverage for some components of the evidence-based treatments recommended in the U.S. Public Health Service clinical guidelines (Fiore et al. 2000; Task Force on Community Preventive Services 2001). For example, Medicare announced that as of March 2005 it will cover up to two cessation attempts per year, and that each attempt may include four counseling sessions, for a total of eight sessions per year. Pharmacotherapy for smoking cessation is also covered by the new Medicare prescription drug benefit. The NIH’s state-of-the-science panel on tobacco use found “strong evidence” supporting the effectiveness of reducing out-of-pocket costs and reimbursing providers for cessation services (NIH 2006b). However, in the United States overall, insurance coverage remains spotty, and covered cessation treatment programs typically invest only in the minimum recommended level of coverage. A 2002 national survey of MCOs found that 30 percent had no written policy on coverage for tobacco cessation services and 42 percent provided no coverage for behavioral interventions (McPhillips-Tangum et al. 2004). In 1998, only half of the 5 million Medicaid recipients nationwide who were current smokers were eligible for any type of smoking cessation treatment benefit (Schauffler et al. 2001).
States purchase health insurance for more than 5 million employees and retirees. In a survey of state employee insurance plans conducted in 2002 and 2003, only 6 of 45 states required smoking cessation coverage that was fully consistent with the U.S. Public Health Service guidelines for all employees (Fiore et al. 2000). To capture the demonstrable benefits of cessation programs, various public and private health insurance programs available in the United States should provide reimbursement for a broad range of effective smoking cessation interventions.
In sum, insurance and benefit coverage for smoking cessation programs remains an important problem. Identifying funds for these programs is always a challenge, but two important sources of additional revenues for cessation services that have been used in some venues are tobacco excise taxes and court-ordered litigation settlements from tobacco companies.
Recommendation 20: All insurance, managed care, and employee benefit plans, including Medicaid and Medicare, should cover reimbursement for effective smoking cessation programs as a lifetime benefit.
For a smoker, it is long journey from starting to smoke and enjoying smoking to wanting to stop and successfully stopping. For much of that journey the smoker is not actively attempting to quit. Thus there are many opportunities to enhance cessation success rates at many points along the smoker’s journey. Opportunities range from becoming more aware of the
risks of smoking and the benefits of cessation to learning about the tools available for cessation, understanding the process of cessation and what to expect, becoming motivated to make frequent and serious quit attempts, not becoming discouraged by relapse, and eventually quitting for good. There is substantial room to improve the overall cessation outcome rate at every step of the way during this journey. This extraordinary opportunity can only be fully realized by strengthening and developing policies that support a comprehensive smoking cessation care management system that addresses each and every step in the journey from current smoker to lifetime ex-smoker.
COMMUNITY MOBILIZATION
Community coalitions played a central role in the acceleration of successful tobacco control efforts from 1988 to 2000. The scientific literature bearing on the effects of coalition activity is reviewed by Sparks in Appendix O and the following discussion is drawn from the information presented.
The most important functions of these community coalitions were that they mobilized organized grassroots support for tobacco control activities, gave a voice to the community in policymaking, and held governments and businesses accountable for their decisions. Mobilizing communities for advocacy has become a mainstream public health tool over the past generation. One area in which success has been documented is alcohol policy, specifically, in relation to drunk driving and underage drinking (IOM/NRC 2004). Ironically, one of the ingredients of success in the alcohol policy domain has been participation in local coalitions by some segments of the alcohol industry. This experience poses a stark contrast to the efforts of the tobacco industry to terminate community action in the smoking domain, in which the tobacco industry uses the false claim that community action and advocacy amount to “lobbying,” which is often limited by federal and state laws. The value at stake in these disputes with the tobacco industry is not only public health but also local self-determination.
From the beginning, public policy advocacy was an integral part of comprehensive state tobacco control programs because they emphasized population-level changes, including changes in legislation and public policy. For example, the ASSIST program promoted three types of interventions (program services, policy, and mass media) and the guidelines stated that “efforts to achieve priority public policy objectives should take precedence over efforts to support service delivery” (NCI 2005, p. 23). Mass media initiatives were intended to support those policy changes, which meant that media advocacy that engaged the news media in support of prevention policies was the focus of media initiatives, whereas social marketing
played a secondary role. The four ASSIST program priority policy areas were eliminating ETS, raising tobacco taxes, limiting tobacco advertising and promotion, and reducing youth access.
The CDC identifies governmental and voluntary policies that promote clean indoor air and restrict access to tobacco products as well as other policy objectives as best practices, citing the successes of the California, Massachusetts, and Oregon community coalitions in achieving policy and program objectives (CDC 1999c). Statewide programs that promote media advocacy and countermarketing campaigns are also cited among the best practices, based on the CDC’s review of core documents from the California and Massachusetts campaigns.
There have been few efforts to analyze the contributions of the state tobacco control coalitions to comprehensive state programs, and it has been especially difficult to measure the impacts of their advocacy initiatives. Most investigators who have evaluated state programs observe that state coalitions have played a key role in the achievement of policy changes that reduce tobacco consumption; yet, those investigators have also commented on the difficulty of measuring the extent to which coalition activities at the state or local level were responsible for either policy change or health outcomes. One reason that the link between community action and reductions in tobacco use is difficult to document is that public health methodology for measuring complex community and population-based social and policy changes is not as well developed as it is for measuring individual and small group changes (Sparks, Appendix O). However, evidence from the domain of alcohol policy convincingly demonstrates the effects of mobilizing community coalitions, both on the enactment of new policies to reduce underage drinking and alcohol-impaired driving and on the actual changes in the prevalence of consumption as well as the targeted alcohol problems (IOM/NRC 2004).
Even without quantitative studies of the efficacy of policy advocacy, most people in the tobacco control community assume that without citizen advocacy, it is doubtful that the changes in tobacco taxes, smoke-free workplace laws, restrictions on smoking in public accommodations, and restrictions on sales to youth would have occurred. This assumption is reasonable because decision makers do not decide to strengthen tobacco control policies unless an active citizenry demands such change. In this sense, tobacco control policies are the end point of coalition advocacy initiatives, and their effectiveness can be measured by counting the hundreds, possibly thousands, of local and state tobacco control policies adopted during the 1990s (Gerlach and Larkin 2005). The Surgeon General’s report, Reducing Tobacco Use, called the emergence of statewide coalitions the most important advance in comprehensive programs and concluded that comprehensive state programs, such as those in California and Massachu-
setts, provide evidence that such programs reduce smoking (Public Health Service 2000).
Tobacco Industry Reaction to Successful Public Policy Advocacy
The tobacco industry immediately recognized the potential power of an advocacy strategy by state coalitions when such coalitions began to be formed. The industry attacked the ASSIST program from its inception (NCI 2005; Trochim et al. 2003; White and Bero 2004) to reduce the threat of citizen action. Analysis of internal documents from members of the tobacco industry indicates that the tobacco industry deliberately pursued a campaign to equate citizen advocacy efforts with lobbying and to limit those activities (NCI 2005; White and Bero 2004). Congress eventually prohibited anyone receiving federal funds from lobbying state and local governments (Federal Acquisition Streamlining Act of 1994 Pub. L. No. 103-355, 108 Stat. 3243). The tobacco industry used the Freedom of Information Act to divert state health department resources and threatened lawsuits against state health departments and individual state employees for violating the lobbying restriction (NCI 2005). The MSA also prohibits the American Legacy Foundation from engaging in any political activities or lobbying. The industry’s position equates advocacy with lobbying and cites Internal Revenue Service regulations that forbid public agencies from using public money for lobbying (White and Bero 2004).
In reaction to the tobacco industry’s position, federal agencies and many state health departments have severely limited advocacy activities that were—and that still are—perfectly legal. Lobbying, a well-understood term in various legal contexts, such as in the statutes governing tax-exempt foundations, refers to direct communication to a legislator on specific legislation or grassroots communication to the members of the general public urging them to take action on specific legislation (Gerlach and Larkin 2005; IOM 1988; Wallack et al. 1993). As the term is used in public health, however, “advocacy” refers to a much broader concept and set of activities, such as organized social action aiming to create a shift in public opinion and to mobilize resources and forces to support an issue, policy, or constituency (Wallack et al. 1993), or the process of educating policymakers and members of the community about certain health-related issues and the measures that can be taken to address them (Gerlach and Larkin 2005).
Gerlach and Larkin point out that as early as the first year of the SmokeLess States program, the RWJF’s support of the Coalition for Tobacco-Free Colorado was challenged as lobbying by the tobacco industry (Gerlach and Larkin 2005). In response, the RWJF was careful to make a distinction between lobbying, (which the SmokeLess States program would not fund) and advocacy (which it would). Coalitions were free to use their
own funds for such activities; indeed, the Foundation encouraged and finally insisted that coalitions find such funds. Both the RWJF and the NCI ASSIST program held training workshops for state coalitions on policy advocacy. As the report on the ASSIST program from NCI makes clear policy advocacy and lobbying are not the same thing (NCI 2005, p. 352).
The tobacco industry’s strong opposition to public health advocacy is a good indication of how important advocacy initiatives should be in any blueprint for future tobacco control efforts. The industry attacks have weakened federal and state willingness to fund advocacy programs. The potential for future gains is thus endangered if state health departments, foundations, and community organizations become hesitant to openly acknowledge how critical citizen advocacy is to successful policy change.
States and local communities should not be barred from using federal funds for tobacco control advocacy efforts at the state or local levels, as long as such activities do not involve lobbying (i.e., contacting legislators about a specific bill or urging constituents to do so). Advocating policies that would promote the public health and education of the public or legislators about the effects of adopting new policies (or of failing to do so) does not constitute lobbying. The CDC should encourage citizen participation in the democratic process and should clarify the distinction between legitimate citizen advocacy and restricted lobbying.
Maintaining Momentum
Recent evidence of the impact of advocacy by mobilized communities lies in the continuing adoption of smoke-free cities and towns across the United States. As of October 2006, 519 municipalities have enacted local smoke-free laws, including some localities that have banned smoking in restaurants and bars (ANRF 2006). Smoke-free movements’ success has also accelerated at the state level; 19 states and Washington, D.C., have now enacted smoke-free state laws, many of which include workplaces, restaurants, and bars (Table 5-3). Even as funding for coalitions has become less secure, these policy successes continue to occur with a momentum that was unanticipated in the late 1990s. The success of smoke-free policies in the past 5 years shows the importance of continued federal and state support for community-level strategies for tobacco control efforts as well as the need for broad demonstration programs.
The evidence reviewed above indicates that the comprehensive approach used in the 1990s, including policy advocacy, has resulted in many policy changes for tobacco control efforts that, in turn, have had an effect on the prevalence of tobacco use. There are two main reasons to continue such a comprehensive approach and a focus on policy advocacy. The first, which is specific to tobacco control, is that, if all state and local policies for
TABLE 5-3 Summary of Smoke Free State Laws
|
State |
Enactment Date |
Provisions (Effective Date) |
|
California |
July 1994 |
Restaurants (01/01/95) and bars (01/01/98) |
|
Utah |
1994, March 2006 |
Workplaces (05/01/06), restaurants (01/01/95), and bars (01/07/09) |
|
South Dakota |
February 2002 |
Workplaces (07/01/02) |
|
Delaware |
May 2002 |
Workplaces, restaurants, and bars (11/27/02) |
|
Florida |
November 2002 |
Workplaces and restaurants (07/01/03) |
|
New York |
March 2003 |
Workplaces, restaurants, and bars (07/24/03) |
|
Connecticut |
May 2003 |
Restaurants (10/01/03) and bars (04/01/04) |
|
Maine |
June 2003 |
Restaurants and bars (01/01/04) |
|
Idaho |
April 2004 |
Restaurants (07/01/04) |
|
Massachusetts |
June 2004 |
Workplaces, restaurants, and bars (07/05/04) |
|
Rhode Island |
April 2005 |
Workplaces and restaurants (03/10/05), bars (03/31/05) |
|
North Dakota |
June 2005 |
Workplaces (08/01/05) |
|
Vermont |
June 2005 |
Restaurants and bars (09/01/05) |
|
Montana |
April 2005 |
Workplaces and restaurants (10/01/05), bars (09/01/09) |
|
Washington |
November 2005 |
Workplaces, restaurants, and bars (12/08/05) |
|
New Jersey |
January 2006 |
Workplaces, restaurants, and bars (04/15/06) |
|
District of Columbia |
January 2006 |
Workplaces (04/03/06), restaurants and bars (01/01/07) |
|
Colorado |
March 2006 |
Restaurants and bars (07/01/06) |
|
Louisiana |
June 2006 |
Workplaces and restaurants (01/01/07) |
|
Hawaii |
July 2006 |
Workplaces, restaurants, and bars (11/16/06) |
|
NOTE: Workplaces includes both public and private nonhospitality workplaces, including, but not limited to, offices, factories, and retail stores. Restaurants includes any attached bar in the restaurant. Bars include freestanding bars without separately ventilated rooms. SOURCE: See http://www.no-smoke.org/pdf/SummaryUSPopList.pdf. |
||
tobacco control are counted, policy advocacy has had its greatest effect in altering the normative environment supporting tobacco use. Even though formal evaluation data for a meta-analysis may be scant, state health departments have broadened the scope of their tobacco control activities. Accordingly, state officials can document changes in social norms that support tobacco-free environments and public support for tobacco control efforts, and they can also list changes in public policy that limit tobacco use. A cadre of public health advocates was trained intensively through the ASSIST, IMPACT, and SmokeLess States program coalition initiatives. Not only should this cadre be maintained, but funding and resources also should be available so that these advocates may provide training for the next generation of tobacco control workers in the 50 states and the other territories in the United States. The momentum of public advocacy should not be lost.
The second, and even more crucial, reason to continue to support a comprehensive approach is that continuing to implement and evaluate comprehensive social and environmental interventions is essential to the continued development of effective public health promotion efforts. Understanding of how to implement such interventions, as well as how to develop methods for evaluating the effectiveness of such interventions, cannot advance if the federal government, state governments, and national nonprofit foundations do not take the lead in advancing the public’s health through such initiatives. Involvement in broad initiatives is critical to the training of future public health professionals who need practice in population-based solutions to public health problems. Such initiatives, with their national focus, are so costly, however, that they require federal coordination and support. As an example of the kind of advances that the field needs, OSH’s recent release of Key Outcome Indicators for Evaluating Comprehensive Tobacco Control Programs (CDC 2005b) illustrates how program evaluation of complex initiatives can be enhanced. The OSH tobacco control program requires that states receiving funds for tobacco control efforts develop action plans based on logic models, in which community mobilization and policy and regulatory actions lead to defined short-, intermediate-, and long-term outcomes for tobacco control efforts. Detailed outcome indicators then make it possible to measure success quantitatively.
Recommendation 21: While sustaining their own valuable tobacco control activities, state tobacco control programs, CDC, philanthropic foundations, and voluntary organizations should continue to support the efforts of community coalitions promoting, disseminating, and advocating for tobacco use prevention and cessation, smoke-free environments, and other policies and programs for reducing tobacco use.
SPECIAL POPULATIONS WITH HIGHER RATES OF CIGARETTE SMOKING
As Chapter 1 illustrates, tobacco use and tobacco-related diseases impact segments of society differentially. Prevention and cessation problems need to be attentive to the special circumstances and outreach needs of these subgroups. For example, Native-American and Alaska Native adults are more likely to smoke than white, Asian-American, or Hispanic-American adults.4 Not surprisingly, members of subgroups with a high smoking prevalence are more likely to experience tobacco-related morbidity and mortality such as from heart disease or lung cancer, thereby contributing significantly to health disparities. Although African Americans have a similar smoking prevalence to whites, African Americans are more susceptible to developing and dying from lung cancer and are less likely to quit smoking than white smokers. At least one study shows that Hispanic-American smokers are less likely than white smokers to receive cessation advice from health care providers (Levinson et al. 2004).
Attention should also be given to the special circumstances and needs of recent immigrants from countries where smoking is socially acceptable. For example, smoking rates among Southeast Asian adults, Korean men in particular, have been shown to be significantly higher (34–43 percent) than in the U.S. male population (Kandula et al. 2004; Ma et al. 2004). For new immigrant populations and populations for whom English is a second language, access to culturally competent and linguistically appropriate interventions could be a key requirement for engaging them in prevention and cessation programs (Baezconde-Garbanati and Garbanati 2000; Orleans and Fishman 2000). Research into the design and impact of culturally sensitive intervention programs, however, is limited. Such research should be further developed to enhance the evidence base on how to best address the needs of an increasingly diverse population (NIH 2006a).
Other populations at increased risk for tobacco use are described by Wallace in Appendix P. These groups include individuals with psychiatric disorders and a history of substance abuse, among others. Typical approaches to smoking cessation in populations with comorbidities and risk behaviors can help individuals to stop smoking, but long-term abstinence has been shown to be more difficult to achieve. Research is also needed on how best to design smoking cessation intervention and their effectiveness in the treatment of individuals with co-occurring conditions.
Wallace (Appendix P) also notes, that “the themes of poverty, lower socioeconomic status and health and social disparities pervade many of the high risk groups for tobacco use” (Wallace, Appendix P). The rate of smok-
ing among adults who are below the poverty level is about 32.9 percent (CDC 2004a). Persons with low socioeconomic status may have less access to health care that might be needed to address smoking-related morbidities. While data on the prevalence of smoking among homeless individuals is difficult to obtain, reports from international studies indicate that prevalence rates can range from 75 to 85 percent (Folsom and Jeste 2002). Identifying and eliminating disparities in tobacco use and related morbidity and mortality is an important part of the CDC’s goal for ensuring success in tobacco control programs, leading many state programs to include a stated emphasis on disparities in their strategic plans. State- and locally-supported prevention and treatment programs need to assess the proportion of their population who fall into these categories and to consider modifying prevention and treatment programs to ensure that they reach these populations effectively.
Military personnel are another population at high risk of tobacco use. Following a significant decline in cigarette smoking from 51 percent in 1980 to 30 percent in 1998, cigarette smoking rates have begun to increase (Hamlett-Berry 2004). More recently, a 2005 Department of Defense Survey of Health-Related Behaviors Among Active Duty Military Personnel found that about one third of military personnel reported smoking in the past month across all branches of service (Bray et al. 2006). The prevalence of smoking in the past month was highest (38.2 percent) among army personnel. Veterans who have separated from active duty also show higher smoking rates than those found in the general civilian population. Reporting data from a 1999 health survey of veterans who received care from the Veterans Health Administration, (Miller et al. 2001) found the prevalence of smoking to be 33 percent compared to 23 percent in the adult civilian population. Military service has been suggested by some researchers as a risk factor for smoking (Klevens et al. 1995). Veterans could benefit from cessation services from the Veterans Administration or from state and locally provided treatment programs. Active duty military personnel could also benefit from prevention and cessation services from the Department of Defense.
Recommendation 22: Tobacco control programs should consider populations disproportionately affected by tobacco addiction and tobacco-related morbidity and mortality when designing and implementing prevention and treatment programs. Particular attention should be paid to ensuring that health communications and other materials are culturally-appropriate and that special outreach efforts target all high-risk populations. Standard prevention or treatment programs that are modified to reach high-risk populations should be evaluated for effectiveness.
PROJECTED IMPACT OF STRENGTHENING EXISTING TOBACCO CONTROL MEASURES
This chapter has outlined a blueprint for how the country can strengthen and intensify current tobacco control policies and programs, assuming that the current legal structure of tobacco control efforts remains unchanged. What would be the impact on national tobacco use prevalence of following, or not following, this blueprint, relative to prevalence based on the baseline projections outlined at the end of Part I of the committee’s report?
Table 5-4 (from Table 3 of Levy, Appendix J) shows that the SimSmoke model projects considerable potential benefit if the policies outlined in this chapter are pursued aggressively. Specifically, the policies modeled by the SimSmoke model are as follows:
-
Tax increases of $1 and $2 per pack
-
Nationwide implementation of clean air laws for all work sites (including bars)
-
Comprehensive media campaigns targeting youth and adults and funded at the levels recommended by the CDC (i.e., beyond the levels that have been used in the past) to prevent initiation and to increase quit attempts, heighten consumer demand for proven cessation programs and to increase smoker’s health literacy about the value of using evidence-based treatments when trying to quit
-
Comprehensive cessation policies (full coverage of pharmacotherapy and behavioral therapy, training and coverage for tobacco brief interventions, multisession quit lines, internet interventions, and free nicotine replacement therapy)
-
Universal implementation of school-based prevention sufficient to
TABLE 5-4 Projected Adult Smoking Prevalence Through 2025 Under Status Quo and Best-Case Policy Scenarios
|
Policy Scenario |
2005 |
2010 |
2015 |
2020 |
2025 |
|
Status quo |
20.6% |
19.3% |
18.1% |
16.9% |
15.5% |
|
$1.00 tax increase |
20.6% |
18.4% |
17.1% |
15.9% |
14.5% |
|
$2.00 tax increase |
20.6% |
17.8% |
16.4% |
15.1% |
13.7% |
|
Clean air laws |
20.6% |
18.6% |
17.4% |
16.3% |
14.9% |
|
Media campaign |
20.6% |
18.1% |
16.9% |
15.8% |
14.4% |
|
Cessation treatment |
20.6% |
18.2% |
16.7% |
15.3% |
13.8% |
|
Education programs |
20.6% |
19.2% |
17.6% |
16.1% |
14.6% |
|
Youth-access policies |
20.6% |
19.1% |
17.6% |
16.2% |
14.7% |
|
All policies with $1.00 tax |
20.6% |
15.5% |
13.4% |
11.8% |
10.2% |
|
All policies with $2.00 tax |
20.6% |
14.9% |
12.9% |
11.2% |
9.7% |
-
cut the rate of smoking initiation by 10 percent
-
Heavy enforcement of youth-access laws, accompanied by publicity and high penalties
-
All of these things being done together with $1- or $2-per-pack tax increases
Empirical data concerning interactions among multiple policy interventions implemented simultaneously are sparse. The SimSmoke model makes the reasonable but still untested assumption that “when more than one policy is in effect, the percentage reductions are multiplicatively applied,” implying that “the relative effect is independent of other policies but the absolute effect is smaller when another policy is in effect” (Levy, Appendix J). For example, if two policies that would each reduce a model flow by 10 percent are both implemented together, they reduce that flow by 19 percent since (1–10 percent) × (1–10 percent) = 81 percent, which is a 19 percent reduction. Hence the results of an estimated “all-policies” analysis are less certain than those of an analysis of individual policies.
The individual policies, particularly the cessation interventions and tax increases, could have a substantial effect on tobacco use prevalence over time. Indeed, collectively they are projected to meet the Healthy People 2010 smoking prevalence target of 12 percent in about 2020, with a 10 percent prevalence reached in 2025. The potential impact of full implementation of the blueprint presented in this chapter is depicted in Figure 5-9, which compares the SimSmoke model projections under the best-case conditions with the status-quo and worst-case projections presented in Chapter 3.
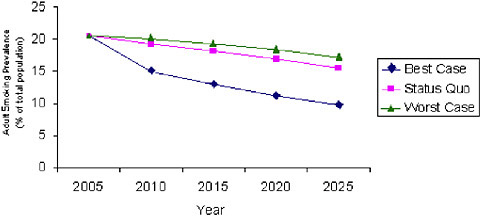
FIGURE 5-9 Comparison of SimSmoke model estimates of adult smoking prevalence, 2005 to 2025, under the best-case, status-quo, and worst-case scenarios.
Overall, however, the committee finds these model projections only modestly encouraging. On the positive side, the actions outlined in this chapter seem to be powerful and effective. Implementing this set of recommendations fully might allow the important goal of a 10 percent smoking prevalence to be achieved, albeit 15 years later than envisioned in Healthy People 2010. On the other hand, removing any single one of the comprehensive policy’s components would prevent the modeled prevalence from hitting the 10 percent target in 2025. Hence, the success of these strategies is, in some sense, fragile, requiring absolute commitment to full implementation. Given the recent retrenchment in tobacco control efforts described in Chapter 3, one might worry whether that level of commitment can be achieved and sustained. Nevertheless, any major initiatives undertaken to reduce tobacco use, including those outlined in the blueprint described in this chapter, should be carefully evaluated both for their levels and integrity of delivery and for their effectiveness.
It is not literally true that the only way that the 10 percent smoking prevalence target can be reached in 2025 is by implementing this particular combination of actions. Any set of actions, whether they are produced by policy interventions or by exogenous events, that sufficiently reduces initiation or increases the rate of smoking cessation would enable the country to meet that 10 percent target. This point is illustrated in Figure 5-10, which was created by running the System Dynamics Model in reverse to determine the break-even changes in initiation and cessation that are needed to achieve
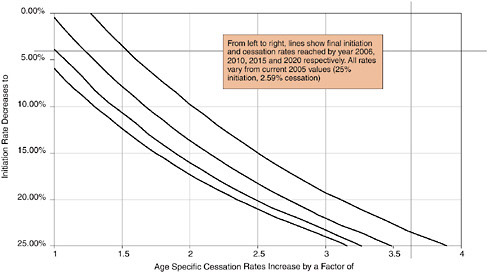
FIGURE 5-10 Combination of initiation and cessation rates required to reach a smoking prevalence of 10 percent by 2025.
a smoking prevalence of 10 percent by 2025. The figure shows four different break-even lines, each corresponding to different rates of change. The line farthest to the left shows the initiation and cessation that would be required if those changes took place more or less instantly. The line farthest to the right shows the changes that would be needed if such changes were phased in between now and 2020.
Figure 5-10 presents a lot of information into one display, so it is worth pausing to explain exactly how to read it. Note that the line farthest to the right essentially crosses the point (2, 10 percent) corresponding to a doubling in the cessation rate (horizontal axis) and a 10 percent rate of initiation (vertical axis). That means that if, between now and 2020 (2020 is used because this is the fourth line from the left), initiation rates fell from the current rates of 25 percent down to 10 percent, and cessation rates doubled over the same time period, then by 2025 those changes would be enough to drive the smoking prevalence to 10 percent by 2025. Any combination of changes to the lower left of that line would not be enough. Any combination of changes to the upper right, if effective by 2020, would be enough to drive the smoking prevalence below 10 percent by 2025.
Reductions in initiation and increases in cessation are complements, or alternative ways to reach the target (hence the lines slope from upper left to lower right). The general impression that the committee takes away from this chart is that the 10 percent smoking prevalence in 2025 target is attainable, but it will require rather potent actions sustained over a long period of time.
One way to achieve the goal would be full implementation of the actions described in this chapter. However, these proposals have been selected within two substantial constraints: they are known to be effective, and they can be implemented within the existing legal structure of tobacco control.
Chapter 6 describes proposals that relax these two constraints. The ideas presented go beyond implementation of the tried and trusted methods that have been subject to extensive experimentation and peer review. Rather, they are policy strategies that hold great potential but that are relatively untried and that therefore have been relatively unexamined empirically. One overall lesson that can be taken from the modeling exercises is this: if the country is serious about attaining 10 percent smoking prevalence by 2025, then unless the country has great confidence that the plan outlined in this chapter will be rapidly, faithfully, and continuously implemented in its entirety, other approaches should be considered.
Realistically, the committee is doubtful that the prevalence of smoking among adults will drop significantly below 15 percent, or that the rate of smoking initiation will permanently fall below 15 percent if the basic legal structure of the tobacco market, and the tobacco control community’s responses to that market, remain unchanged. Although achieving these levels
would be a major improvement, they are not satisfactory from a public health standpoint, simply because of the large numbers of premature deaths and other serious harmful consequences that would inevitably follow. The steps outlined in this chapter are surely necessary in the short run, but we should be prepared to do more over the long run.
REFERENCES
AAP (American Academy of Pediatrics). 1986. Involuntary smoking: a hazard to children. Pediatrics 77:755-757.
Abrams DB, Niaura R, Brown RA, Emmons KM, Goldstein MG, Monti PM. 2003. The Tobacco Dependence Treatment Handbook: A Guide to Best Practices. New York: The Guilford Press.
Abrams DB, Orleans CT, Niaura RS, Goldstein MG, Prochaska JO, Velcer W. 1996. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: a combined stepped-care and matching model. Annals of Behavioral Medicine 18(4):290-303.
ACHA (American College Health Association). 2005. Position Statement on Tobacco on College and University Campuses. Web Page. Available at: http://www.acha.org/info_resources/tobacco_statement.pdf; accessed June 12, 2007.
AHA (American Heart Association), American Cancer Society, Campaign for Tobacco-Free Kids, and American Lung Association. 2005. A Broken Promise to Our Children: The 1998 State Tobacco Settlement Seven Years Later. Web Page. Available at: http://www.tobaccofreekids.org/reports/settlements/2006/fullreport.pdf; accessed May 30, 2006.
AHIP (America’s Health Insurance Plans). 2004. Making the Business Case for Smoking Cessation. Web Page. Available at: http://www.businesscaseroi.org/roi/default.aspx; accessed July 26, 2006.
Aligne CA, Stoddard JJ. 1997. Tobacco and children: an economic evaluation of the medical effects of parental smoking. Archives of Pediatric and Adolescent Medicine 151(7):648-653.
Andersen MR, Leroux BG, Bricker JB, Rajan KB, Peterson AV Jr. 2004. Antismoking parenting practices are associated with reduced rates of adolescent smoking. Archives of Pediatric and Adolescent Medicine 158(4):348-352.
ANR (Americans for Nonsmokers’ Rights). 2005. Health Effects of Secondhand Smoke on Children. Web Page. Available at: http://www.no-smoke.org/document.php?id=212; accessed July 11, 2006.
ANRF (American Nonsmokers’ Rights Foundation). 2006. Municipalities with Local 100% Smokefree Laws. Web Page. Available at: http://www.no-smoke.org/pdf/100ordlisttabs.pdf; accessed August 11, 2006.
ANRF. 2007. Colleges and Universities with Smokefree Air Policies. Web Page. Available at: http://www.no-smoke.org/pdf/smokefreecollegesuniversities.pdf; accessed June 12, 2007.
Arkin RM, Roemhild HF, Johnson CA, Luepker RV, Murray DM. 1981. The Minnesota smoking prevention program: a seventh-grade health curriculum supplement. Journal of School Health 51(9):611-616.
Baezconde-Garbanati L, Garbanati JA. 2000. Tailoring tobacco control messages for Hispanic populations. Tobacco Control 9(Suppl I):i51.
Bal DG. 1998. Designing an effective statewide tobacco control program—California. Cancer 83(12 Suppl Robert):2717-2721.
Banthin C. 2004. Cheap smokes: state and federal responses to tobacco tax evasion over the internet. Health Matrix 14:325-356.
Banzhaf JF. 2005. 17th State Bans Smoking in Home to Protect Children. Web Page. Available at: http://www.no-smoking.org/august05/08-05-05-1.html; accessed July 14, 2006.
Bauer UE, Johnson TM, Hopkins RS, Brooks RG. 2000. Changes in youth cigarette use and intentions following implementation of a tobacco control program: findings from the Florida Youth Tobacco Survey, 1998–2000. Journal of the American Medical Assocation 284(6):723-728.
Bayer R, Colgrove J. 2002. Science, politics, and ideology in the campaign against environmental tobacco smoke. American Journal of Public Health 92(6):949-954.
Behan DF, Eriksen MP, Lin Y. 2005. Economic Effects of Environmental Tobacco Smoke. Schaumburg, IL: Society of Actuaries.
Belluck P. 2007, January 19. Maine city bans smoking in cars with children. The New York Times.
Bergman J. 2003. Smoking Policies in Long-Term Care and Residential Facilities Serving Older Persons. Web Page. Available at: www.tcsg.org/powerpoint7/index.htm; accessed February 23, 2005.
Bernstein E, Bernstein J, Levenson S. 1997. Project ASSERT: an ED-based intervention to increase access to primary care, preventative services, and the substance abuse treatment system. Annals of Emergency Medicine 30(2):181-189.
Bernstein SL, Boudreaux ED, Cydulka RK, Rhodes KV, Lettman NA, Almeida SL, McCullough LB, Mizouni S, Kellermann AL. 2006. Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations. Annals Emergency Medicine 48(4):e417-e426.
Bernstein SL, Cannata M. 2006. Nicotine dependence, motivation to quit, and diagnosis in emergency department patients who smoke. Addictive Behavior 31(2):288-297.
Biener L. 2000. Adult and youth response to the Massachusetts anti-tobacco television campaign. Journal of Public Health Management and Pracicet 6(3):40-44.
Biener L. 2002. Anti-tobacco advertisements by Massachusetts and Philip Morris: what teenagers think. Tobacco Control 11 (Suppl 2):ii43-ii46.
Biener L, Harris JE, Hamilton W. 2000a. Impact of the Massachusetts tobacco control programme: population based trend analysis. British Medical Journal 321(7257):351-354.
Biener L, McCallum-Keeler G, Nyman AL. 2000b. Adults’ response to Massachusetts anti-tobacco television advertisements: impact of viewer and advertisement characteristics. Tobacco Control 9(4):401-417.
BJS (Bureau of Justice Statistics). 2005. Summary Findings: Prisons. Web Page. Available at: http://www.ojp.usdoj.gov/bjs/prisons.htm; accessed May 11, 2007.
Blecher EH, van Walbeek CP. 2004. An international analysis of cigarette affordability. Tobacco Control 13(4):339-346.
Bloch M, Shopland DR. 2000. Outdoor smoking bans: more than meets the eye. Tobacco Control 9(1):99.
Blumberg DL. 2005, June 22. Even home isn’t haven for smokers. Christian Science Monitor. P. 16.
Bonnie RJ. 2001. Tobacco and public health policy: A youth centered approach. Slovic PE, Ed. Smoking: Risk, Perception, and Policy. Thousand Oaks, CA: Sage Publications.
Borders TF, K Tom Xu, Bacchi D, Cohen L, SoRelle-Miner D. 2005. College campus smoking policies and programs and students’ smoking behaviors. BioMed Center Public Health 5(74).
Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. 2006. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control 15(Suppl 3):iii42-iii50.
Botvin GJ. 2000. Preventing drug abuse in schools: social and competence enhancement approaches targeting individual-level etiologic factors. Addictive Behavior 25(6):887-897.
Botvin GJ, Baker E, Dusenbury L, Botvin EM, Diaz T. 1995. Long-term follow-up results of a randomized drug abuse prevention trial in a white middle-class population. Journal of the American Medical Association 273(14):1106-1112.
Botvin GJ, Baker E, Dusenbury L, Tortu S, Botvin EM. 1990. Preventing adolescent drug abuse through a multimodal cognitive-behavioral approach: results of a 3-year study. Journal of Consultng and Clinical Psychology 58(4):437-446.
Botvin GJ, Eng A. 1982. The efficacy of a multicomponent approach to the prevention of cigarette smoking. Preventative Medicine 11(2):199-211.
Botvin GJ, Griffin KW. 2002. Life skills training as a primary prevention approach for adolescent drug abuse and other problem behaviors. The International Journal of Emergency Mental Health 4(1):41-47.
Boudreaux ED, Kim S, Hohrmann JL, Clark S, Camargo CA. 2005. Interest in smoking cessation among emergency department patients. Health Psychology 24(2):220-224.
Bray RM, Hourani LL, Rae Olmsted KL, Witt M, Brown JM, Pemberton MR, Marsden ME, Marriott, Scheffler, Vandermaas-Peeler R, Weimer B, Calvin S, Bradshaw M, Close K, Hayden D. 2006. 2005 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel. Washington, DC: Department of Defense/RTI International.
Cady B. 1998. History of successful ballot initiatives—Massachusetts. Cancer 83(12 Suppl Robert):2685-2689.
Campaign for Tobacco-Free Kids. 2003. State of Washington V. Dirtcheapcig.Com, Inc. Web Page. Available at: http://tobaccofreekids.org/reports/internet/WARuling.pdf; accessed May 29, 2007.
Capehart T. 2005. Tobacco Outlook: Leaf Production Plummets with End of Program. Washington, DC: Economic Research Service, U.S. Department of Agriculture.
Cawley J, Markowitz S, Tauras J. 2004. Lighting up and slimming down: the effects of body weight and cigarette prices on adolescent smoking initiation. Journal of Health Economics 23(2):293-311.
CDC (Centers for Disease Control and Prevention). 1996. Cigarette smoking before and after an excise tax increase and an antismoking campaign—Massachusetts, 1990–1996. MMWR (Morbidity and Mortality Weekly Report) 45(44):966-970.
CDC. 1999a. Decline in cigarette consumption following implementation of a comprehensive tobacco prevention and education program—Oregon, 1996–1998. MMWR (Morbidity and Mortality Weekly Report) 48(7):140-143.
CDC. 1999b. Ten great public health achievements—United States, 1900–1999. MMWR (Morbidity and Mortality Weekly Report) 48(12):241-243.
CDC. 1999c. Best Practices for Comprehensive Tobacco Control Programs—August 1999. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
CDC. 2001. Tobacco use among adults—Arizona, 1996 and 1999. MMWR (Morbidity and Mortality Weekly Report) 50(20):402-406.
CDC. 2002. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States, 1995–1999. MMWR (Morbidity and Mortality Weekly Report) 51(14):300-303.
CDC. 2003. Chronic Disease. Grants and Funding: Consolidating and Streamlining Program Announcements. Web Page. Available at: http://www.cdc.gov/nccdphp/grants_funding/consolidating.htm; accessed August 15, 2006.
CDC. 2004a. Prevalence of cigarette use among 14 racial/ethnic populations—United States, 1999–2001. MMWR (Morbidity and Mortality Weekly Report) 53(3):49-52.
CDC. 2004b. Impact of a smoking ban on restaurant and bar revenues—El Paso, Texas, 2002. MMWR (Morbidity and Mortality Weekly Report) 53(7):150-152.
CDC. 2005a. CDC Wonder: DATA 2010 … The Healthy People 2010 Database. Web Page. Available at: http://wonder.cdc.gov/data2010/focus.htm; accessed July 10, 2006.
CDC. 2005b. Key Outcome Indicators for Evaluating Comprehensive Tobacco Control Programs. Atlanta, GA.
CDC. 2005c. State Tobacco Activities Tracking and Evaluation (STATE) Stystem. Web Page. Available at: http://apps.nccd.cdc.gov/statesystem/; accessed June 8, 2007.
CDC. 2005d. Annual smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 1997–2001. MMWR (Morbidity and Mortality Weekly Report) 54(25):625-628.
CDC. 2005e. State smoking restrictions for private-sector worksites, restaurants, and bars— United States, 1998 and 2004. MMWR (Morbidity and Mortality Weekly Report) 54(26):649-653.
CDC. 2005f. Estimated exposure of adolescents to state-funded anti-tobacco television advertisements—37 states and the District of Columbia, 1999–2003. MMWR (Morbidity and Mortality Weekly Report) 54(42):1077-1080.
CDC. 2005g. Cigarette smoking among adults—United States, 2004. MMWR (Morbidity and Mortality Weekly Report) 54(44):1121-1124.
CDC. 2006a. Behavioral Risk Factor Surveillance System. Web Page. Available at: http://www.cdc.gov/brfss/; accessed July 19, 2006.
CDC. 2006b. YRBSS: Youth Risk Behavior Surveillance System. Web Page. Available at: http://www.cdc.gov/HealthyYouth/yrbs/index.htm; accessed July 19, 2006.
CDHS (California Department of Health Services). 1998. A Model for Change: The California Experience in Tobacco Control. Sacramento, CA: California Department of Health Services.
CDHS. 2002. California Tobacco Control Update. Web Page. Available at: http://www.dhs.ca.gov/tobacco/documents/pubs/TCSupdate.pdf; accessed February 1, 2006.
CDHS. 2005. Prevalence: Youth Smoking. Sacramento, CA.
Celebucki C, Biener L, Koh HK. 1998. Evaluation: methods and strategy for evaluation—Massachusetts. Cancer 83(12 Suppl Robert):2760-2765.
Chaloupka FJ. 1999. Macro-social influences: the effects of prices and tobacco-control policies on the demand for tobacco products. Nicotine and Tobacco Research 1(Suppl 1):105-109 .
Chaloupka FJ, Pacula RL. 1998. An Examination of Gender and Race Differences in Youth Smoking Responsiveness to Price and Tobacco Control Policies, Working Paper 6541. Web Page. Available at: http://www.impacteen.org/fjc/PublishedPapers/w6541.pdf; accessed June 8, 2007.
Chaloupka FJ, Warner KE. 2000. The Economics of Smoking. Handbook of Health Economics. Vol. 1B. Pp. 1541-1612.
Chapman S. 2000. Banning smoking outdoors is seldom ethically justifiable. Tobacco Control 9(1):95-97.
Chapman S, Richardson J. 1990. Tobacco excise and declining tobacco consumption: the case of Papua New Guinea. American Journal of Public Health 80(5):537-540.
Chassin L, Presson CC, Rose JS, Sherman SJ. 1996. The natural history of cigarette smoking from adolescence to adulthood: demographic predictors of continuity and change. Health Psychology 15(6):478-484.
Chassin L, Presson CC, Rose J, Sherman SJ, Davis MJ, Gonzalez JL. 2005. Parenting style and smoking-specific parenting practices as predictors of adolescent smoking onset. Journal of Pediatric Psychology 30(4):333-344.
Chinnock WF. 2003. No smoking around children: the family courts’ mandatory duty to restrain parents and other persons from smoking around children. Arizona Law Review 453.
Clark PI, Scarisbrick-Hauser A, Gautam SP, Wirk SJ. 1999. Anti-tobacco socialization in homes of African-American and white parents, and smoking and nonsmoking parents. Journal of Adolescent Health 24(5):329-339.
Cohen DA, Richardson J, LaBree L. 1994. Parenting behaviors and the onset of smoking and alcohol use: a longitudinal study. Pediatrics 94(3):368-375.
Connolly G, Robbins H. 1998. Designing an effective statewide tobacco control program— Massachusetts. Cancer 83(12 Suppl Robert):2722-2727.
Cooper M. 2005, June 9. Bill would ban delivery of cigarettes in mail. The New York Times. B. p. 4.
Cummings KM, Clarke H. 1998a. The Use of Counter-Advertising as a Tobacco Use Deterrent. Web Page. Available at: http://www.advocacy.org/publications/mtc/counterads.htm; accessed September 12, 2005.
Cummings KM, Clarke H. 1998b. Health Science Analysis Project—Policy Analysis No. 8. Washington, DC: Advocacy Institute.
DHHS (U.S. Department of Health and Human Services). 2000. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services.
DHHS. 2001. Healthy People 2010, Volume II: 27 Tobacco Use. Web Page. Available at: http://www.healthypeople.gov/Document/HTML/Volume2/27Tobacco.htm#_Toc489766224; accessed July 20, 2006.
DHHS. 2004. HHS Announces National Smoking Cessation Quitline Network. Web Page. Available at: http://www.hhs.gov/news/press/2004pres/20040203.html; accessed July 17, 2006.
DHHS. 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
DiFranza JR. 1999. Are the federal and state governments complying with the Synar Amendment? Archives of Pediatric and Adolescent Medicine 153(10):1089-1097.
DiFranza JR, Dussault GF. 2005. The federal initiative to halt the sale of tobacco to children— the Synar Amendment, 1992-2000: lessons learned. Tobacco Control 14(2):93-98.
DiFranza JR, Lew RA. 1996. Morbidity and mortality in children associated with the use of tobacco products by other people. Pediatrics 97(4):560-568.
Ding A. 2003. Youth are more sensitive to price changes in cigarettes than adults. Yale Journal of Biological Medicine 76(3):115-124.
Dorfman L, Wallack L. 1993. Advertising health: the case for counter-ads. Public Health Reports 108(6):716-726.
Eckhardt L, Woodruff SI, Elder JP. 1997. Related effectiveness of continued, lapsed, and delayed smoking prevention intervention in senior high school students. American Journal of Health Promotion 11(6):418-421.
Elder JP, Edwards CC, Conway TL, Kenney E, Johnson CA, Bennett ED. 1996. Independent evaluation of the California Tobacco Education Program. Public Health Reports 111(4):353-358.
Elder JP, Wildey M, de Moor C, Sallis JF Jr, Eckhardt L, Edwards C, Erickson A, Golbeck A, Hovell M, Johnston D, et al. 1993. The long-term prevention of tobacco use among junior high school students: classroom and telephone interventions.[see comment]. American Journal of Public Health 83(9):1239-1244.
Emery S, White MM, Pierce JP. 2001. Does cigarette price influence adolescent experimentation? Journal of Health Economics 20(2):261-270.
Emont S, Choi W, Novotny T, Giovino G. 1992. Clean indoor air legislation, taxation, and smoking behaviour in the United States: an ecological analysis. Tobacco Control 2:13-17.
Ennett ST, Tobler NS, Ringwalt CL, Flewelling RL. 1994. How effective is drug abuse resistance education? A meta-analysis of Project DARE outcome evaluations. American Journal of Public Health 84(9):1394-1401.
EPA (Environmental Protection Agency). 1992. Respiratory Health Effects of Passive Smoking: Lung Cancer and Other Disorders. Washington, DC: Office of Health and Environmental Assessment, Office of Research and Development, U.S. Environmental Protection Agency.
EPA. 2006. Health Effects of Exposure to Secondhand Smoke. Web Page. Available at: http://www.epa.gov/smokefree/healtheffects.html; accessed July 7, 2006.
Etzel RA. 1997. Active and passive smoking: hazards for children. Central European Journal of Public Health 5(2):54-56.
Fagan P, Brook JS, Rubenstone E, Zhang C. 2005. Parental occupation, education, and smoking as predictors of offspring tobacco use in adulthood: a longitudinal study. Addictive Behavior 30(3):517-529.
Farkas AJ, Gilpin EA, White MM, Pierce JP. 2000. Association between household and workplace smoking restrictions and adolescent smoking. Journal of the American Medical Association 284(6):717-722.
Farquhar JW, Maccoby N, Wood PD, Alexander JK, Breitrose H, Brown BW Jr, Haskell WL, McAlister AL, Meyer AJ, Nash JD, Stern MP. 1977. Community education for cardiovascular health. Lancet 1(8023):1192-1195.
Farrelly MC, Chen J, Thomas KY, Healton CJ. 2001. Legacy First Look Report 6: Youth Exposure to Environmental Tobacco Smoke. Washington, DC: American Legacy Foundation.
Farrelly MC, Davis KC, Haviland ML, Messeri P, Healton CG. 2005. Evidence of a dose—response relationship between “truth” antismoking ads and youth smoking prevalence. American Journal of Public Health 95(3):425-431.
Farrelly MC, Healton CG, Davis KC, Messeri P, Hersey JC, Haviland ML. 2002. Getting to the truth: evaluating national tobacco countermarketing campaigns.[erratum appears in American Journal of Public Health 2003 May;93(5):703]. American Journal of Public Health 92(6):901-907.
Farrelly MC, Niederdeppe J, Yarsevich J. 2003. Youth tobacco prevention mass media campaigns: past, present, and future directions. Tobacco Control 12(Suppl 1):i35-i47.
Farrelly MC, Nonnemaker JM, Chou R, Hyland A, Peterson KK, Bauer UE. 2005. Changes in hospitality workers’ exposure to secondhand smoke following the implementation of New York’s smoke-free law. Tobacco Control 14(4):236-241.
Farrelly MC, Pechacek TF, Chaloupka FJ. 2003. The impact of tobacco control program expenditures on aggregate cigarette sales: 1981-2000. Journal of Health Economics 22(5):843-859.
Fee E, Brown TM. 2004. Hospital smoking bans and their impact. American Journal of Public Health 94(2):185.
Fichtenberg CM, Glantz SA. 2000. Association of the California Tobacco Control Program with declines in cigarette consumption and mortality from heart disease. New England Journal of Medicine 343(24):1772-1777.
Fichtenberg CM, Glantz SA. 2002. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ 325(7357):188.
Fiore MC, Bailey WC, Cohen SJ. 2000. Treating Tobacco Use and Dependence (Clinical Practice Guideline). Rockville, MD: U.S. Department of Health Human Services. Public Health Service.
Fiore MC, Croyle RT, Curry SJ, Cutler CM, Davis RM, Gordon C, Healton C, Koh HK, Orleans CT, Richling D, Satcher D, Seffrin J, Williams C, Williams LN, Keller PA, Baker TB. 2004. Preventing 3 million premature deaths and helping 5 million smokers quit: a national action plan for tobacco cessation. American Journal of Public Health 94(2):205-310.
Flay BR. 2000. Approaches to substance use prevention utilizing school curriculum plus social environment change. Addictive Behavior 25(6):861-885.
Flay BR, Hu FB, Richardson J. 1998. Psychosocial predictors of different stages of cigarette smoking among high school students. Preventive Medicine 27(5 Pt 3):9-18.
Flynn BS, Worden JK, Secker-Walker RH, Badger GJ, Geller BM. 1995. Cigarette smoking prevention effects of mass media and school interventions targeted to gender and age groups. Journal of Health Education 26(2):S45-S51.
Flynn BS, Worden JK, Secker-Walker RH, Badger GJ, Geller BM, Costanza MC. 1992. Prevention of cigarette smoking through mass media intervention and school programs. American Journal of Public Health 82(6):827-834.
Flynn BS, Worden JK, Secker-Walker RH, Pirie PL, Badger GJ, Carpenter JH, Geller BM. 1994. Mass media and school interventions for cigarette smoking prevention: effects 2 years after completion. American Journal of Public Health. 84(7):1148-1150.
Folsom D, Jeste DV. 2002. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatrica Scandinavica 105(6):404-413 .
Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeill A, Anderson S, Cummings KM, Allwright S, Mulcahy M, Howell F, Clancy L, Thompson ME, Connolly G, Driezen P. 2006. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tobacco Controll 15(Suppl 3):iii51-iii58.
Fraguela J, Martin A, Trinanes E. 2003. Drug-abuse prevention in the school: four-year follow-up of a programme. Psychology in Spain 7(1):29-38.
Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. 2005. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. American Journal of Public Health 95(6):1016-1023.
Friend K, Levy DT. 2002. Reductions in smoking prevalence and cigarette consumption associated with mass-media campaigns. [Review] [63 refs]. Health Education Research. 17(1):85-98.
Gallet CA, List JA. 2003. Cigarette demand: a meta-analysis of elasticities. Health Economics 12(10):821-835.
GAO (General Accounting Office). 2002. Internet Cigarette Sales: Giving ATF Investigative Authority May Improve Reporting and Enforcement. Washington, DC: GAO.
GAO. 2006. Tobacco Settlement: States’ Allocations of Fiscal Year 2005 and Expected Fiscal Year 2006 Payments. Washington, DC: GAO.
Gerlach KK, Larkin MA. 2005. To Improve Health and Health Care, Vol. VIII. San Francisco, CA: Jossey-Bass.
Gilpin EA, Lee L, Pierce JP. 2005. How have smoking risk factors changed with recent declines in California adolescent smoking? Addiction 100(1):117-125.
Gilpin E, Lee L, Pierce JP, Tang H, Lloyd J. 2004. Support for protection from second hand smoke: California 2002. Tobacco Control 13(1):96.
Givel M, Glantz S. 2000. Failure to defend a successful state tobacco control program: policy lessons from Florida. American Journal of Public Health 90(5).
Givel S, Dearlove J, Glantz S. 2001. Tobacco Policy Making in California 1999-2001: Stalled and Adrift. San Francisco, CA: Center for Tobacco Research and Education (University of California).
Glantz S, Balbach E. 2000. Tobacco War: Inside the California Battles. Berkeley: University of California Press.
Glasgow RE, Cummings KM, Hyland A. 1997. Relationship of worksite smoking policy to changes in employee tobacco use: findings from COMMIT. Community Intervention Trial for Smoking Cessation. Tobacco Control 6(Suppl 2):S44-S48.
Glynn TJ. 1989. Essential elements of school-based smoking prevention programs. Journal of School Health 59(5):181-188.
Gortmaker SL, Walker DK, Jacobs FH, Ruch-Ross H. 1982. Parental smoking and the risk of childhood asthma. American Journal of Public Health 72(6):574-579.
Gross CP, Soffer B, Bach PB, Rajkumar R, Forman HP. 2002. State expenditures for tobacco-control programs and the tobacco settlement. New England Journal of Medicine 347(14):1080-1086.
Gruber J. 2001. Tobacco at the crossroads: the past and future of smoking regulation in the United States. The Journal of Economic Perspectives 15(2):193-212.
Halperin AC, Rigotti NA, Rothstein WG, Rajapaksa S. 2003. US public universities’ compliance with recommended tobacco-control policies. Journal of American College Health 51(5):181.
Hamilton VH, Levinton C, St-Pierre Y, Grimard F. 1997. The effect of tobacco tax cuts on cigarette smoking in Canada. Canadian Medical Association Journal 156(2):187-191.
Hamilton W, Norton G, Weintraub J. 2002. Independent Evaluation of the Massachusetts Tobacco Control Program, 7th Annual Report—January 1994 to June 2000. Cambridge, MA: Abt Associates Inc.
Hamilton WL, Biener L, Rodger CN. 2005. Who supports tobacco excise taxes? Factors associated with towns’ and individuals’ support in Massachusetts. Journal of Public Health Management and Practice 11(4):333-340.
Hamilton WL, Rodger CN, Chen X, Njobe TK, Kling R, Norton G. 2003. Independent Evaluation of the Massachusetts Tobacco Control Program. Eighth Annual Report: January 1994–June 2001. Cambridge, MA: Abt Associates Inc.
Hamlett-Berry K. 2004. Smoking cessation policy in the VA health care system: Where have we been and where are we going? In: Isaccs S, ed. VA in the Vanguard: Building on Sucess in Smoking Cessation: Proceedings of a Conference Held September 21, 2004 in San Francisco, California. Washington, DC: Department of Veterans Affairs. Pp. 7-40.
Hammond D, McDonald PW, Fong GT, Borland R. 2004. Do smokers know how to quit? Knowledge and perceived effectiveness of cessation assistance as predictors of cessation behaviour. Addiction 99(8):1042-1048.
Hammond SK, Emmons KM. 2005. Inmate exposure to secondhand smoke in correctional facilities and the impact of smoking restrictions. Journal of Exposure Analysis and Environmental Epidemiology 15(3):205-211.
Hanewinkel R, Asshauer M. 2004. Fifteen-month follow-up results of a school-based life-skills approach to smoking prevention. Health Education Research 19(2):125-137.
Hansen W. 1988. Theory and Implementation of the Social Influence Model of Primary Prevention. Prevention Research Findings: 1988. OSAP Prevention Monograph-3. Washington, DC: Office of Substance Abuse Prevention (U.S. HHS).
Hansen WB, Malotte CK, Fielding JE. 1988. Evaluation of a tobacco and alcohol abuse prevention curriculum for adolescents. Health Education Quarterly 15(1):93-114.
Harris JE, Chan SW. 1999. The continuum-of-addiction: cigarette smoking in relation to price among Americans aged 15-29. Health Economics 8(1):81-86.
Hay JW. 1991. The Harm They Do to Others: A Primer on the External Costs of Drug Abuse. Searching for Alternatives: Drug Control Policy in the United States. Stanford, CA: Hoover Institution Press. Pp. 200-225.
Hennrikus D, Pentel PR, Sandell SD. 2003. Preferences and practices among renters regarding smoking restrictions in apartment buildings. Tobacco Control 12(2):189-194.
HEW (Department of Health, Education, and Welfare). 1964. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: U.S. Department of Health, Education, and Welfare; Public Health Service.
Hill KG, Hawkins JD, Catalano RF, Abbott RD, Guo J. 2005. Family influences on the risk of daily smoking initiation. J Adolesc Health 37(3):202-210.
Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande-Kulis VG, Fielding JE, Alao MO, McKenna JW, Sharp DJ, Harris JR, Woollery TA, Harris KW. 2001. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine 20(2 Suppl):16-66.
Hu TW, Ren QF, Keeler TE, Bartlett J. 1995a. The demand for cigarettes in California and behavioural risk factors. Health Economics 4(1):7-14.
Hu TW, Sung HY, Keeler TE. 1995b. The state antismoking campaign and the industry response: the effects of advertising on cigarette consumption in California. American Economic Review 85(2):85-90.
Hyland A, Higbee C, Li Q, Bauer JE, Giovino GA, Alford T, Cummings KM. 2005. Access to low-taxed cigarettes deters smoking cessation attempts. American Journal of Public Health 95(6):994-995.
Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. 2004. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine and Tobacco Research 6(Suppl 3):S363-S369.
IARC (International Agency for Research on Cancer). 2002. Volume 83 Tobacco Smoke and Involuntary Smoking. Web Page. Available at: http://monographs.iarc.fr/ENG/Monographs/vol83/volume83.pdf; accessed June 8, 2007.
Independent Evaluation Consortium. 2002. Final Report. Independent Evaluation of the California Tobacco Control Prevention and Education Program: Waves 1, 2, and 3 (1996–2000). Rockville, MD: The Gallup Organization.
IOM (Institute of Medicine). 1988. The Future of Public Health. Washington, DC: National Academy Press.
IOM. 1994a. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youth. Washington, DC: National Academy Press.
IOM. 1994b. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youth. Washington, DC: National Academy Press.
IOM/NRC (National Research Council). 2004. Reducing Underage Drinking: A Collective Responsibility. Washington, DC: The National Academies Press.
Jackson C, Henriksen L. 1997. Do as I say: parent smoking, antismoking socialization, and smoking onset among children. Addictive Behavior 22(1):107-114.
Jemal A, Cokkinides VE, Shafey O, Thun MJ. 2003. Lung cancer trends in young adults: an early indicator of progress in tobacco control (United States). Cancer Causes Control 14(6):579-585.
Johnson CA, Pentz MA, Weber MD, Dwyer JH, Baer N, MacKinnon DP, Hansen WB, Flay BR. 1990. Relative effectiveness of comprehensive community programming for drug abuse prevention with high-risk and low-risk adolescents. Journal of Consulting and Clinical Psychology 58(4):447-456.
Jordaan ER, Ehrlich RI, Potter P. 1999. Environmental tobacco smoke exposure in children: household and community determinants. Archives of Environmental Health 54(5):319-327.
Kandula NR, Kersey M, Lurie N. 2004. Assuring the health of immigrants: what the leading health indicators tell us. Annual Review of Public Health 25:357-376.
Keeler TE, Hu TW, Barnett PG, Manning WG. 1993. Taxation, regulation, and addiction: a demand function for cigarettes based on time-series evidence. Journal of Health Economics 12(1):1-18.
Kempner M. 2005, June 6. UPS reviews cigarette shipments. The Atlanta Journal-Constitution. Business.
Kerr M, Stattin H. 2000. What parents know, how they know it, and several forms of adolescent adjustment: further support for a reinterpretation of monitoring. Developmental Psychology 36(3):366-380.
Kesich GD. 2004, November 18. UPS, others sue over Maine tobacco law; the suit challenges the rewuirement that delivery driver verify age, identity of tobacco recipients. Portland Press Herald. Local & State.
Klepp KI, Halper A, Perry CL. 1986. The efficacy of peer leaders in drug abuse prevention. Journal of School Health 56(9):407-411.
Klevens RM, Giovino GA, Peddicord JP, Nelson DE, Mowery P, Grummer-Strawn L. 1995. The Association Between Veteran Status and Cigarette-Smoking Behaviors. American Journal of Preventive Medicine 11(4):245-250.
Kuiper N, Nelson D, Schooley M. 2005. Evidence of Effectiveness: A Summary of State Tobacco Control Program Evaluation Literature. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Kulig JW. 2005. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics 115(3):816-821.
Leverett M, Ashe M, Gerard S, Jenson J, Woollery T. 2002. Tobacco use: the impact of prices. Journal of Law, Medicine and Ethics 30(3 Suppl):88-95.
Levinson A, Pérez-Stable E, Espinoza P, Flores E, Byers TE. 2004. Latinos report less use of pharmaceutical aids when trying to quit smoking. American Journal of Prevtive Medicine 26(2):105-111.
Levy DT, Romano E, Mumford E. 2005. The relationship of smoking cessation to sociodemographic characteristics, smoking intensity, and tobacco control policies. Nicotine & Tobacco Research 7(3):387-396.
Levy DT, Romano E, Mumford EA. 2004. Recent trends in home and work smoking bans. Tobacco Control 13(3):258-263.
Liang L, Chaloupka F, Nichter M, Clayton R. 2003. Prices, policies and youth smoking, May 2001. Addiction 98(Suppl 1):105-122.
Loukas A, Garcia M, Gottlieb NH. 2006. Texas college students’ opinions of no-smoking policies, secondhand smoke, and smoking in public places. Journal of American College Health 1(55):27-32.
Lowenstein S, Tomlinson D, Koziol-McLain J, Prochazka A. 1995. Smoking habits of emergency department patients: an opportunity for disease prevention. Academic Emergency Medicine 2:165-171.
Luepker RV, Murray DM, Jacobs DR Jr, Mittelmark MB, Bracht N, Carlaw R, Crow R, Elmer P, Finnegan J, Folsom AR, et al. 1994. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. American Journal of Public Health 84(9):1383-1393.
Ma GX, Tan Y, Toubbeh JI, Su X, Shive SE, Lan Y. 2004. Acculturation and smoking behavior in Asian-American populations. Health Education Research 19(6):615-625.
Manning WG, Keeler EB, Newhouse JP, Sloss EM, Wasserman J. 1989. The taxes of sin: do smokers and drinkers pay their way? Journal of the American Medical Assocation 261(11):1604-1609.
Mannino DM, Siegel M, Husten C, Rose D, Etzel R. 1996. Environmental tobacco smoke exposure and health effects in children: results from the 1991 National Health Interview Survey. Tobacco Control 5(1):13-18.
McPhillips-Tangum C, Bocchino C, Carreon R, Erceg C, Rehm B. 2004. Addressing tobacco in managed care: results of the 2002 survey. Preventing Chronic Disease 1(4): 1-11.
MDPH (Massachusetts Department of Public Health). 2002a. MTCP Background. Web Page. Available at: http://www.mass.gov/dph/mtcp/background/background.htm; accessed June 23, 2006.
MDPH. 2002b. MTCP Statewide Services. Web Page. Available at: http://www.mass.gov/dph/mtcp/programs/statewide.htm; accessed July 20, 2006.
MDPH. 2006, June 22. Massachusetts Tobacco Control Program Accomplishments. Web Page. Available at: http://www.mass.gov/dph/mtcp/reports/accomplishments.pdf; accessed June 22, 2006.
Michel L. 2005, April 4. Internet cigarette sales take hit. Buffalo News. News.
Miller A. 1998. Designing an effective counteradvertising campaign—Massachusetts. Cancer 83(12 Suppl Robert):2742-2745.
Miller DR, Kalman D, Ren XS, Lee AF, Niu Z, Kazis LE. 2001. Health Behaviors of Veterans in the VHA: Tobacco Use. Washington, DC: U.S. Department of Veterans Affairs Veterans Health Administration Office of Quality and Performance and VHA Health Assessment Project Center for Health Quality, Outcomes, and Economic Research.
Mittelmark MB, Luepker RV, Jacobs DR, Bracht NF, Carlaw RW, Crow RS, Finnegan J, Grimm RH, Jeffery RW, Kline FG, et al. 1986. Community-wide prevention of cardiovascular disease: education strategies of the Minnesota Heart Health Program. Preventive Medicine 15(1):1-17.
The Monitor’s View. 2005, July 7. Snuffing out tobacco in prisons. Christian Science Monitor. P. 8.
Moskowitz JM, Lin Z, Hudes ES. 2000. The impact of workplace smoking ordinances in California on smoking cessation. American Journal of Public Health 90(5):757-761.
Murray DM, Hannan PJ, Jacobs DR, McGovern PJ, Schmid L, Baker WL, Gray C. 1994. Assessing intervention effects in the Minnesota Heart Health Program. American Journal of Epidemiology 139(1):91-103.
Najera AP. 1998. History of successful ballot initiatives—California. Cancer 83(12 Suppl Robert):2680-2684.
National Journal Group. 2005, June 20. Efforts to regulate internet tobacco sales may be revived. National Journal’s Congress Daily.
NCI (National Cancer Institute). 2005. ASSIST: shaping the future of tobacco prevention and control. NCI. Tobacco Control Monograph Series. Vol. 8, No. NIH Publication Number 05-5645. Bethesda, MD: National Institutes of Health.
Nicholl J. 1998. Tobacco tax initiatives to prevent tobacco use: a study of eight statewide campaigns. Cancer 83(12 Suppl Robert):2666-2679.
Niederdeppe J, Farrelly MC, Haviland ML. 2004. Confirming “truth”: more evidence of a successful tobacco countermarketing campaign in Florida. American Journal of Public Health 94(2):255-257.
NIH (National Institutes of Health). 2006a. Final Statement: National Institutes of Health State-of-the-Science Conference Statement, Tobacco Use: Prevention, Cessation, and Control. Web Page. Available at: http://consensus.nih.gov/2006/TobaccoStatementFinal090506.pdf; accessed January 18, 2007a.
NIH. 2006b. National Institutes of Health State-of-the-Science Conference Statement. Web Page. Available at: http://consensus.nih.gov/2006/2006TobaccoSOS029html.htm; accessed July 26, 2006.
O’Byrne KK, Haddock CK, Poston WS. 2002. Parenting style and adolescent smoking. Journal of Adolescent Health 30(6):418-425.
Older Americans Report. 2005, August 5. City’s housing authority bans smoking in senior apartments. Older Americans Report.
Orleans CT. 1993. Treating Nicotine Dependence in Medical Settings: A Stepped-Care Model. Orleans CT, Slade J, Editors. Nicotine Addiciton: Principles and Management. New York: Oxford University Press. Pp. 145-161.
Orleans CT, Fishman J. 2000. Tailored communications for smoking cessation. Tobacco Control 9(Suppl I):i49.
Osterwalder J, Beeman DE. 2005, April 13. Fresh air: officials to consider tougher rules; no vacancy for smokers; smoke-free housing debate forces leaders to pit personal rights vs. health concerns. The Press Enterprise. A. p. 1.
OTRU (Ontario Tobacco Research Unit). 2006. The Smoke-Free Ontario Act: Extend Protection to Children in Vehicles. Web Page. Available at: http://www.otru.org/pdf/updates/update_aug2006.pdf; accessed January 19, 2007.
Ozer EM, Adams SH, Gardner LR, Mailloux DE, Wibbelsman CJ, Irwin CE Jr. 2004. Provider self-efficacy and the screening of adolescents for risky health behaviors. Journal of Adolescent Health 35(2):101-107.
Parmet WE, Banthin C. 2005. Public health protection and the commerce clause: controlling tobacco in the Internet Age. New Mexico Law Review 35:81-122.
Patrick S, Marsh R. 2001. Current tobacco policies in U.S. adult male prisons. The Social Science Journal 38:27-37.
Pechmann C, Reibling ET. 2000. Planning an effective anti-smoking mass media campaign targeting adolescents. Journal of Public Health Management and Practice 6(3):80-94.
Pechmann C, Slater MD. 2005. Social Marketing Messages That May Motivate Irresponsible Behavior. Ratneshwar S. Inside Consumption: Consumer Motives, Goals, and Desires. New York: Routledge.
Pentz MA, MacKinnon DP, Dwyer JH, Wang EY, Hansen WB, Flay BR, Johnson CA. 1989. Longitudinal effects of the midwestern prevention project on regular and experimental smoking in adolescents. Preventive Medicine 18(2):304-321.
Perry C, Kelder S, Klepp K. 1994. Community-wide cardiovascular disease prevention in young people. European Journal of Public Health 4:188-194.
Perry CL, Kelder K-I, Siller C. 1989. Community-wide strategies for cardiovascular health: the Minnesota heart health program youth program. Health Education Research 4: 87-101.
Perry CL, Kelder SH, Murray DM, Klepp KI. 1992. Communitywide smoking prevention: long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. American Journal of Public Health 82(9):1210-1216.
Peterson AV Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. 2000. Hutchinson Smoking Prevention Project: long-term randomized trial in school-based tobacco use prevention—results on smoking. Journal of the National Cancer Institute 92(24):1979-1991.
Pierce J, Gilpin E, Emery S, Farkas A, Zhu S, Choi W, Berry C, Distefan J, White M, Soroko S, Navarro A. 1998. Tobacco Control in California: Who’s Winning the War? An Evaluation of the Tobacco Control Program, 1989–1996. La Jolla, CA: University of California, San Diego.
Pierce JP, White MM, Gilpin EA. 2005. Adolescent smoking decline during California’s tobacco control programme. Tobacco Control 14(3):207-212.
Pinilla J. 2002. [Tobacco taxes, prices and demand for tobacco products: a comparative analysis]. Gaceta Sanitaria 16(5):425-435.
Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. 2004. A prospective study of household smoking bans and subsequent cessation related behaviour: the role of stage of change. Tobacco Control 13(1):23-28.
Popham WJ, Potter LD, Bal DG, Johnson MD, Duerr JM, Quinn V. 1993. Do anti-smoking media campaigns help smokers quit?. Public Health Report. 108(4):510-513.
Popham WJ, Potter LD, Hetrick MA, Muthen LK, Duerr JM, Johnson MD. 1994a. Effectiveness of the California 1990-1991 Tobacco Education Media Campaign. American Journal of Preventive Medicine 10(6):319-326.
Popham WJ, Potter LD, Hetrick MA, Muthen LK, Duerr JM, Johnson MD. 1994b. Effectiveness of the California 1990–1991 tobacco education media campaign. American Journal of Preventive Medicine 10(6):319-326.
Powell LM, Tauras JA, Ross H. 2005. The importance of peer effects, cigarette prices and tobacco control policies for youth smoking behavior. Journal of Health Economics 24(5):950-968.
Public Health Service. 2000. Reducing Tobacco Use: A Report of the Surgeon General. Public Health Service Pub.
Repace J. 2000. Banning outdoor smoking is scientifically justifiable. Tobacco Control 9(1):98.
Rigotti N. 2001. Chapter 6—reducing the supply of tobacco to youths. Regulating Tobacco. New York: Oxford University Press. Pp. 143-175.
Ross H, Chaloupka FJ. 2003. The effect of cigarette prices on youth smoking. Health Economics 12(3):217-230.
RTI International. 2004. First Annual Independent Evaluation of New York’s Tobacco Control Program. Research Triangle Park, NC: RTI International.
RTI International. 2005. Second Annual Independent Evaluation of New York’s Tobacco Control Program. Research Triangle Park, NC: RTI International.
Russell CM. 1998. Evaluation: methods and strategy for evaluation—California. Cancer 83(12 Suppl Robert):2755-2759.
Schauffler HH, Barker DC, Orleans CT. 2001. Medicaid coverage for tobacco-dependence treatments. Health Affairs (Millwood) 20(1):298-303.
Schoenmarklin S, Tobacco Control Legal Consortium. 2004. Infiltration of Secondhand Smoke into Condominiums, Apartments and Other Multi-Unit Dwellings. St. Paul, MN: Tobacco Control Legal Consortium.
Schroeder SA. 2006. Should emergency physicians help smokers quit? Annals of Emergency Medicine 48(4):415-416.
Scollo M, and Lal A. 2004. Summary of Studies Assessing the Economic Effects of SmokeFree Policies in the Hospitality Industry. Web Page. Available at: http://www.vctc.org.au/tc-res/Hospitalitysummary.pdf; accessed February 23, 2005.
Scollo M, Younie S, Wakefield M, Freeman J, Icasiano F. 2003. Impact of tobacco tax reforms on tobacco prices and tobacco use in Australia. Tobacco Control 12(Suppl 2): ii59-ii66.
Siahpush M, Borland R, Scollo M. 2003. Factors associated with smoking cessation in a national sample of Australians. Nicotine and Tobacco Research 5(4):597-602.
Siegel M. 2002. The effectiveness of state-level tobacco control interventions: a review of program implementation and behavioral outcomes. Annual Review of Public Health 23:45-71.
Siegel M, Biener L. 2000. The impact of an antismoking media campaign on progression to established smoking: results of a longitudinal youth study. American Journal of Public Health 90(3):380-386.
Siegel M, Mowery PD, Pechacek TP, Strauss WJ, Schooley MW, Merritt RK, Novotny TE, Giovino GA, Eriksen MP. 2000. Trends in adult cigarette smoking in California compared with the rest of the United States, 1978–1994. American Journal of Public Health 90(3):372-379.
Simons-Morton B, Chen R, Abroms L, Haynie DL. 2004. Latent growth curve analyses of peer and parent influences on smoking progression among early adolescents. Health Psychology 23(6):612-621.
Skara S, Sussman S. 2003. A review of 25 long-term adolescent tobacco and other drug use prevention program evaluations. Preventive Medicine 37(5):451-474.
Sloan FA, Carlisle ES, Rattliff JR, Trogdon J. 2005. Determinants of states’ allocations of the master settlement agreement payments. Journal of Health and Political Policy Law 30(4):643-86.
Sloan FA, Mathews CA, Trogdon JG. 2004. Impacts of the Master Settlement Agreement on the tobacco industry. Tobacco Control 13(4):356-361.
Sly DF, Heald GR, Ray S. 2001a. The Florida “truth” anti-tobacco media evaluation: design, first year results, and implications for planning future state media evaluations.[see comment]. Tobacco Control 10(1):9-15.
Sly DF, Hopkins RS, Trapido E, Ray S. 2001b. Influence of a counteradvertising media campaign on initiation of smoking: the Florida “truth” campaign. American Journal of Public Health 91(2):233-238.
Sly DF, Trapido E, Ray S. 2002. Evidence of the dose effects of an antitobacco counteradvertising campaign. Preventive Medicine. 35(5):511-518.
Smith CM, Pristach CA, Cartagena M. 1999. Obligatory cessation of smoking by psychiatric inpatients. Psychiatric Service. 50(1):91-94.
Smith E, Swisher J, Vicary J, et al. 2004. Evaluation of life skills training and infused-life skills training in a rural setting: outcomes at two years. Journal of Alcohol and Drug Education 48(1):51-70.
Smokefree Apartment House Registry. 2004. News Release: City Creates Non-Smoking Sections in New Affordable Housing. Web Page. Available at: http://www.smokefreeapartments.org/T.O.%20News%20Release.pdf; accessed July 14, 2006.
Snyder LB, Hamilton MA, Mitchell EW, Kiwanuka-Tondo J, Fleming-Milici F, Proctor D. 2004. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. Journal of Health Communication 9(Suppl 1):71-96.
Soldz S, Clark TW, Stewart E, Celebucki C, Klein Walker D. 2002. Decreased youth tobacco use in Massachusetts 1996 to 1999: evidence of tobacco control effectiveness. Tobacco Control 11(Suppl 2):ii14-ii19.
Spoth RL, Redmond C, Trudeau L, Shin C. 2002. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychology of Addictive Behavior 16(2):129-134.
State of California. 2004. Proposition 99 and the Legislative Mandate for the California Tobacco Control Program. Web Page. Available at: http://www.dhs.ca.gov/tobacco/html/about.htm; accessed May 22, 2006.
Stattin H, Kerr M. 2000. Parental monitoring: a reinterpretation. Childhood Development 71(4):1072-1085.
Steinberg L, Fletcher A, Darling N. 1994. Parental monitoring and peer influences on adolescent substance use. Pediatrics 93(6 Pt 2):1060-1064.
Stephens T, Pederson LL, Koval JJ, Kim C. 1997. The relationship of cigarette prices and nosmoking bylaws to the prevalence of smoking in Canada. American Journal of Public Health 87(9):1519-1521.
Stephens T, Pederson LL, Koval JJ, Macnab J. 2001. Comprehensive tobacco control policies and the smoking behaviour of Canadian adults. Tobacco Control 10(4):317-322.
Stevens C. 1998. Designing an effective counteradvertising campaign—California. Cancer 83(12 Suppl Robert):2736-2741.
Stillman FA, Hartman AM, Graubard BI, Gilpin EA, Murray DM, Gibson JT. 2003. Evaluation of the American Stop Smoking Intervention Study (ASSIST): a report of outcomes. Journal of the National Cancer Institute 95(22):1681-1691.
Tacoma-Pierce County Health Department. 2003. Fresh Air Everywhere. Web Page. Available at: http://www.tpchd.org/files/library/fb76d4134077b3c4.pdf; accessed July 11, 2006.
Task Force on Community Preventive Services. 2001. Recommendations regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine 20(2 Suppl):10-15.
Task Force on Community Preventive Services. 2005. The Guide to Community Preventive Services (Community Guide): What Works to Promote Health? Oxford, England: Oxford University Press.
Tauras JA. 2004a. Public policy and smoking cessation among young adults in the United States. Health Policy 68(3):321-332.
Tauras JA. 2004b. Public policy and smoking cessation among young adults in the United States. Health Policy 68(3):321-332.
Tauras JA, Chaloupka FJ, Farrelly MC, Giovino GA, Wakefield M, Johnston LD, O’Malley PM, Kloska DD, Pechacek TF. 2005. State tobacco control spending and youth smoking. American Journal of Public Health 95(2):338-344.
Tedeschi B. 2005, April 4. Now That Credit Card Companies Won’t Handle Online Tobacco Sales, Many Merchants Are Calling It Quits. The New York Times. C. p. 5.
TEROC (Tobacco Education and Research Oversight Committee). 2000. Toward a Tobacco-Free California: Strategies for the 21st Century, 2000-2003. Web Page. Available at: http://www.dhs.ca.gov/tobacco/documents/pubs/TEROCReport99.pdf; accessed February 1, 2006.
TEROC. 2003. Toward a Tobacco-Free California, 2003-2005: The Myth of Victory. Web Page. Available at: http://www.dhs.ca.gov/tobacco/documents/pubs/TobaccoMasterPlan2003.pdf; accessed February 1, 2006.
Thomson CC, Fisher LB, Winickoff JP, Colditz GA, Camargo CA Jr, King C 3rd, Frazier AL. 2004. State tobacco excise taxes and adolescent smoking behaviors in the United States. Journal of Public Health Management and Practice 10(6):490-496.
Tilson EC, McBride CM, Lipkus IM, Catalano RF. 2004. Testing the interaction between parent-child relationship factors and parent smoking to predict youth smoking. Journal of Adolescent Health 35(3):182-189.
Times Wire Services. 2006, July 6. DHL to Restrict Cigarette Shipments. Los Angeles Times. Business. P. 3.
TIPS (Tobacco Information and Prevention Source). 2006a. Exposure to Environmental Tobacco Smoke and Nicotine Levels—Fact Sheet. Web Page. Available at: http://www.cdc.gov/tobacco/research_data/environmental/factsheet_ets.htm; accessed July 14, 2006.
TIPS. 2006b. Secondhand Smoke: Fact Sheet. Web Page. Available at: http://www.cdc.gov/tobacco/factsheets/secondhand_smoke_factsheet.htm; accessed July 10, 2006.
Tobler NS. 1992. Drug prevention programs can work: research findings. Journal of Addictive Disorders 11(3 ):1-28.
Trochim WM, Stillman FA, Clark PI, Schmitt CL. 2003. Development of a model of the tobacco industry’s interference with tobacco control programmes. Tobacco Control 12(2):140-147.
Trudeau L, Spoth R, Lillehoj C, Redmond C, Wickrama KA. 2003. Effects of a preventive intervention on adolescent substance use initiation, expectancies, and refusal intentions. Prevention Science 4(2):109-122.
Tuttle R. 2006, July 6. DHL Agrees to Stop Shipping Cigarettes Sold Via Internet. Newsday.
Ubelacker S. 2005, August 15. Kids’ exposure to second-hand smoke may lead to smoking as teens: study. Canadian Press NewsWire. Web page. Available at: http://www.nexis.com; accessed July 11, 2006.
UPS reviews cigarette shipments. 2005. Atlanta Journal Constitution. July 6, D3.
U.S. Fed News. 2005, March 17. Attorneys General, ATF Announce Joint Initiative with Credit Card Companies to Prevent Illegal Cigarette Sales Over Internet. U.S. Fed News.
Vartiainen E, Fallonen U, McAlister AL, Puska P. 1990. Eight-year follow-up results of an adolescent smoking prevention program: the North Karelia Youth Project. American Journal of Public Health 80(1):78-79.
Vartiainen E, Paavola M, McAlister A, Puska P. 1998. Fifteen-year follow-up of smoking prevention effects in the North Karelia youth project. American Journal of Public Health 88(1):81-85.
Vartiainen E, Pallonen U, McAlister A, Koskela K, Puska P. 1983. Effect of two years of educational intervention on adolescent smoking (the North Karelia Youth Project). Bulletin of the World Health Organization 61(3):529-532.
Vartiainen E, Pallonen U, McAlister A, Koskela K, Puska P. 1986. Four-year follow-up results of the smoking prevention program in the North Karelia Youth Project. Preventive Medicine 15(6):692-698.
Vokes NI, Bailey JM, Rhodes KV. 2006. “Should I give you my smoking lecture now or later?” Characterizing emergency physician smoking discussions and cessation counseling. Annals of Emergency Medicine 48(4):406-414, 414-417.
Wakefield M, Chaloupka F. 2000. Effectiveness of comprehensive tobacco control programmes in reducing teenage smoking in the USA. Tobacco Control 9(2):177-186.
Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, Ruel EE. 2000. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ 321(7257):333-337.
Wallack L, Dorfman L, Jernigan D, Mekani T. 1993. Media Advocacy and Public Health. Newbury Park, CA: Sage Publications.
Waller BJ, Cohen JE, Ferrence R, Bull S, Adlaf EM. 2003. The early 1990s cigarette price decrease and trends in youth smoking in Ontario. Canadian Journal of Public Health 94(1):31-35.
Warner KE. 1977. The effects of the anti-smoking campaign on cigarette consumption. American Journal of Public Health 67(7):645-650.
Warner K. 2000. The deed for, and value of, a multi-level approach to disease prevention: the case of tobacco control. IOM. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academy Press. Pp. 417-449.
Warner KE. 1979. Clearing the airwaves: the cigarette ad ban revisited. Policy Analysis 5:435-450.
Warner KE. 1985. Cigarette advertising and media coverage of smoking and health. New England Journal of Medicine 312(6):384-388.
Warner KE, Mendez D, Smith DG. 2004. The financial implications of coverage of smoking cessation treatment by managed care organizations. Inquiry 41(1):57-69.
Washington State Department of Revenue. 2005. Major Tribal Internet Cigarette Seller Agrees to Provider Customer Lists. Web Page. Available at: http://dor.wa.gov/Docs/Pubs/News/2005/NR_Smokesignals_settles.pdf; accessed July 11, 2006.
Wechsler H, Kelley K, Seibring M, Kuo M, Rigotti NA. 2001. College smoking policies and smoking cessation programs: results of a survey of college health center directors. Journal of American College Health 49(5):205-213.
Weintraub JM, Hamilton WL. 2002. Trends in prevalence of current smoking, Massachusetts and states without tobacco control programmes, 1990 to 1999. Tobacco Control 11(Suppl 2):ii8-ii13.
White J, Bero LA. 2004. Public health under attack: the American Stop Smoking Intervention Study (ASSIST) and the tobacco industry. American Journal of Public Health 94(2):240-250.
Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP. 2005. A systematic review of school-based smoking prevention trials with long-term follow-up. Journal of Adolescent Health 36(3):162-169.
Wilcox GJ. 2005, April 14. Apartment smoking bans may widen. Daily News.
Worden JK, Flynn BS, Geller BM, Chen M, Shelton LG, Secker-Walker RH, Solomon DS, Solomon LJ, Couchey S, Costanza MC. 1988. Development of a smoking prevention mass media program using diagnostic and formative research. Preventive Medicine. 17(5):531-558.
Yolton K, Dietrich K, Auinger P, Lanphear BP, Hornung R. 2005. Exposure to environmental tobacco smoke and cognitive abilities among U.S. children and adolescents. Environmental Health Perspectives 113(1):98-103.
Yong HH, Borland R, Siahpush M. 2005. Quitting-related beliefs, intentions, and motivations of older smokers in four countries: findings from the International Tobacco Control Policy Evaluation Survey. Addictive Behavior 30(4):777-788.
Yurekli AA, Zhang P. 2000. The impact of clean indoor-air laws and cigarette smuggling on demand for cigarettes: an empirical model. Health Economics 9(2):159-170.
Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. 2000. Smoking cessation with and without assistance: a population-based analysis. American Journal of Preventive Medicine 18(4):305-311.
Zollinger TW, Saywell RM Jr, Muegge CM, Wooldridge JS, Cummings SF, Caine VA. 2003. Impact of the life skills training curriculum on middle school students tobacco use in Marion County, Indiana, 1997–2000. Journal of School Health 73(9):338-346.
Zucker D, Hopkins RS, Sly DF, Urich J, Kershaw JM, Solari S. 2000. Florida’s “truth” campaign: a counter-marketing, anti-tobacco media campaign. Journal of Public Health Management and Practice 6(3):1-6.


















































































































