C
Preventing Obesity in Mexican–American Children and Adolescents
Frederick Trowbridge, Trowbridge & Associates, Inc., Atlanta, Georgia
Fernando Mendoza, Stanford University School of Medicine Palo Alto, California
INTRODUCTION
Childhood obesity has become a worldwide concern because of its epidemic proportions and its growing link to type 2 diabetes and other chronic health conditions. Over the past two decades, there has been an increase in childhood and adolescent obesity to an unprecedented level. During the 1960s–1970s, the prevalence of obesity in children and adolescents in the United States was relatively stable at about 4–7 percent. However, during the 1980s the obesity prevalence doubled, with 11 percent of children and adolescents having body mass index (BMI) levels over the 95th percentile by the early 1990s (CDC, 2005b). In the latest National Health and Nutrition Examination Survey (NHANES) 2003–2004 (Ogden et al., 2006), childhood and adolescent obesity prevalence increased to 17 percent, which is triple the rate in NHANES I (1971–1974) and NHANES II (1976–1980) (Hedley et al., 2004). This dramatic increase in prevalence has driven childhood and adolescent obesity to a prominent position in the clinical and research arenas of child health. Moreover, as the links between obesity and its co-morbidities (e.g., type 2 diabetes, asthma, hypertension, sleep apnea, skeletal-muscular disorders, self-esteem and mental health disorders, and other chronic illnesses) have become more evident, the awareness of the long-term health effects of child and adolescent obesity has raised concerns at all levels of child health policy.
Addressing the problem of obesity in Mexican–American children and adolescents will require consideration of the unique historical and demo-
graphic characteristics of Mexican Americans. Since the 1500s Mexican Americans have lived in what is now the southwestern United States and have maintained a continuing interchange of culture with Mexico. Today, Mexicans continue to immigrate to locations across the United States, and to maintain their cultural ties. Currently, one in five children in the United States lives in an immigrant family; they are either first- or second-generation children of immigrant parents (NRC/IOM, 1998). The country of origin for the largest proportion of these children is Mexico. In 2000, 39 percent of children in families new to the United States were Mexican—no other country contributes more than 4 percent (Hernandez, 2004).
The substantial and ongoing interchange of people and culture between the United States and Mexico makes it clear that addressing childhood obesity in the Mexican–American community requires an approach that recognizes the common social, cultural, economic, and possibly genetic factors that contribute to childhood obesity in both Mexican–American and Mexican children and adolescents. At the same time, the influence of the substantially different social, cultural, and economic environment in which Mexican–Americans living in the United States find themselves, must also be taken into account. This paper reviews the prevalence and trends in obesity in Mexican–American children and youth and considers the multiple factors that may contribute to this growing health problem. The paper then provides an overview of current intervention strategies and programs and proposes actions that may offer the greatest potential for success in preventing and controlling the obesity epidemic.
EXTENT AND CONSEQUENCES OF OBESITY IN MEXICAN– AMERICAN CHILDREN AND YOUTH
Data from national surveys clearly demonstrate a high and increasing prevalence of childhood obesity in the United States (Ogden et al., 2002, 2006; Hedley et al., 2004). Obesity is particularly prevalent among Mexican–American children and youth. Moreover, Mexican–American children have a high prevalence of abdominal obesity, which may put them at elevated risk for type 2 diabetes and cardiovascular disease (CVD). High rates of obesity also may indicate that Mexican–American children and adolescents are more exposed to the negative impacts of obesity on their social and emotional health. Finally, since many Mexican–American children and youth depend on publicly funded health care programs such as Medicaid, the high prevalence of obesity will place increasing demands on health care providers serving Hispanic populations and thus will have significant implications for the funding needs of these programs.
Measurement of Obesity in Children and Youth
Body Mass Index (BMI)
BMI is recommended widely as an appropriate measure of obesity in children older than 2 years of age (Daniels et al., 1997; Pietrobelli et al., 1998). This indicator is calculated easily from simple measurements of height and weight and is associated closely with indicators of cardiovascular disease (CVD) risk (Katzmarzyk et al., 2004). In addition, analysis of BMI data is facilitated by the availability of gender-specific reference data developed by the CDC for determining BMI-for-age percentiles (Kuczmarski et al., 2002). Reference curves based on an international data set derived from large, nationally representative surveys of child growth from six countries also are available (Cole et al., 2000). These reference curves are designed to merge smoothly with the BMI values for adults defining overweight as having a BMI between 25 to 29.9 kg/m2 and obese as having a BMI equal to or greater than 30 kg/m2. For consistency between the IOM report and this paper, obesity in children and youth is defined as having a BMI equal to or greater than age- and gender-specific 95th percentile of the BMI charts developed by the Centers for Disease Control and Prevention (CDC) in 2000. Being at-risk for obesity is defined as having a BMI between the age- and gender-specific 85th and 95th percentiles of the CDC BMI charts (IOM, 2005).
However, BMI also has recognized limitations as an obesity indicator. The relationship of BMI to body fat in children varies in relation to age, maturational stage, gender, race, and fat distribution, so that a given BMI will not reflect an equivalent level of body fat for all individuals (Daniels et al., 1997). Despite these limitations, BMI remains a useful and practical indicator for clinical assessment and for characterizing obesity prevalence in population-based studies.
Waist Circumference
Waist circumference is a more specific indicator of abdominal fat, and it appears to perform at least as well as BMI in identifying children with a clustering of CVD risk factors (Katzmarzyk et al., 2004). Among the 4–17-year-old children and youth who were sampled in the NHANES III (1988– 1994), waist-to-height ratio actually performed better than BMI in identifying those with elevated CVD risk factors (Kahn et al., 2005). A 10-year cohort study beginning when children were 9 and 10 years old found that waist circumference and triglyceride level were significant predictors of the metabolic syndrome1 at ages 18 to 19 years. In this study, BMI was not a
significant predictor once waist circumference was included in the multivariate model (Morrison et al., 2005). The importance of abdominal obesity as a risk factor for CVD in adults was highlighted in a recent study that found that having an elevated waist-to-hip ratio was associated more strongly with myocardial infarction than having an elevated BMI (Yusuf et al., 2005). The population-attributable risk of myocardial infarction for the top two quintiles of waist-to-hip ratio was 24.3 percent versus only 7.7 percent for the top two quintiles of BMI.
Descriptive data showing percentile distributions of waist circumference have been developed for 2–8-year-old African–American, European– American, and Mexican–American children based on data from NHANES III (Fernandez et al., 2004). In the same NHANES III data set, the waist circumference-to-height ratio did not vary significantly in relation to sex or age group, making it feasible to use a single set of cutoffs for classifying children of both sexes and all ages from 4 to 17 years (Kahn et al., 2005). The strong association of increased waist circumference with CVD risk factors and the availability of reference data support the use of waist circumference indicators, in addition to BMI, as valid and practical tools for assessing obesity and associated CVD risk in children and adolescents. However, additional research is needed to confirm the risks associated with abdominal obesity in different age, gender, and ethnic groups (especially Mexican and Mexican–American children and youth) and the usefulness of waist circumference as an indicator, alone or in combination with BMI, in identifying abdominal obesity in these different groups of children and adolescents.
Obesity Prevalence and Trends
Prevalence
Since the late 1970s, there has been a dramatic increase in the prevalence of obesity among children and youth across all racial and ethnic groups in the United States. Data from national surveys indicate that the prevalence of obesity has more than doubled for children ages 2–5 years and adolescents ages 12–19 years, and obesity rates have more than tripled for children ages 6–11 years (Ogden et al., 2002). Prevalence estimates based on the National Longitudinal Survey of Youth data from 1986–1998 in children ages 4–12 years provide a similar picture of the increasing prevalence of obesity (Strauss and Pollack, 2001).
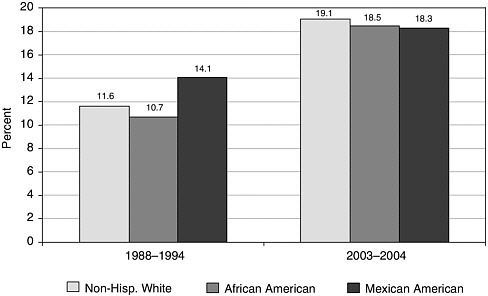
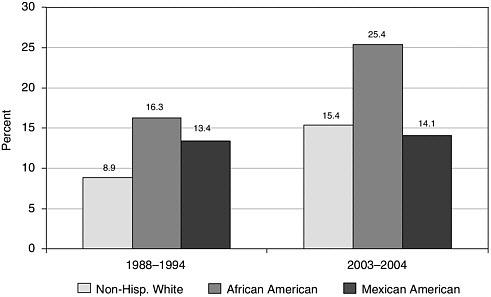
An elevated prevalence of obesity is particularly evident for Mexican– American boys. In NHANES 2003–2004 (Ogden et al., 2006), Mexican– American boys ages 2–5 and 6–11 years had a higher prevalence of obesity than boys of any other race or ethnic group, while obesity prevalence for male adolescents was similar to other ethnic groups. (Figure C-1). In the 2003–2004 NHANES, Mexican–American girls ages 2–5 and 6–11 years had a prevalence of obesity that was less than that of African–American girls but greater than that of non-Hispanic White girls, while obesity prevalence for female Mexican–American adolescents was similar to non-Hispanic Whites (Figure C-2). Figure C-3 displays more data on obesity prevalence detailed by age group, gender, and ethnicity (Ogden et al., 2006). Additional research is needed to assess the underlying attitudes and diet and physical activity practices that may trigger these age, gender, and ethnic group differences.
It is of interest to compare the prevalence of obesity in Mexican– American children and adolescents with their counterparts in Mexico. Data from the Mexican National Nutrition Survey (1999) (Rivera et al., 2001) and the Mexican National Health Survey (2000) (Olaiz et al., 2003) were analyzed using the same CDC reference criteria to define obesity (López Ridaura et al., 2006; del Rio-Navarro et al., 2004; Kuczmarski et al., 2002). Overall, results indicated that, except for the preschool age group, Mexican children had a lower prevalence of obesity than ethnically similar children in the United States surveyed in 1999–2000 (Ogden et al., 2006). Obesity prevalence in 2–5-year-old Mexican children was similar to their
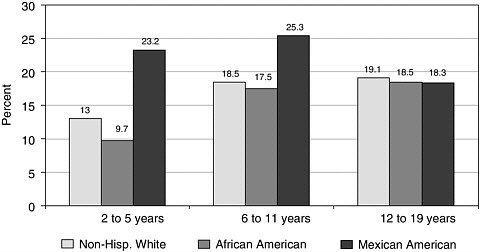
FIGURE C-1 Obesity prevalence in boys, NHANES 2003–2004.
SOURCE: Ogden et al. (2006).
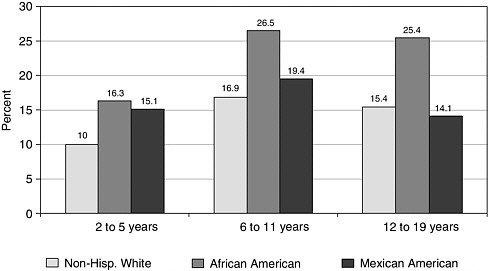
FIGURE C-2 Obesity prevalence in girls, NHANES 2003–2004.
SOURCE: Ogden et al. (2006).
Mexican–American counterparts. However, older Mexican children and adolescents had an obesity prevalence that was only half or one-third of the prevalence seen in Mexican–American children and adolescents (Table C-1 and Figure C-4).
These results in children and adolescents from ethnically similar backgrounds suggest that environmental factors in the United States exert a significant influence on the growth and weight status of Mexican–American children and youth.
Abdominal Obesity Prevalence
Abdominal obesity appears to be a particular concern for Mexican adults, children, and youth. Data from the Mexican National Health Survey conducted in 2000 indicate a high prevalence of abdominal obesity in Mexican adults based on waist circumference measurements, with a reported prevalence of 46.3 percent in men (waist circumference ≥ 94 cm) and 81.4 percent in women (waist circumference ≥ 80 cm) (Sanchez-Castillo et al., 2005). Abdominal obesity was elevated even in women of normal weight, with co-morbidities relating better to waist circumference than to BMI. Moreover, the high prevalence of abdominal obesity in Mexican men and women was associated with a prevalence of diabetes and hypertension similar to or exceeding levels observed in the non-Hispanic White population in NHANES III (1988–1994).
TABLE C-1 Prevalence of Obesity in Non-Hispanic White, Mexican–American, and Mexican Children: 1999–2000
|
Age/ Gender Group |
NHANES 1999–2000 Non-Hispanic White |
NHANES 1999–2000a Mexican American |
Mexican National Nutrition Surveyb 1999 |
Mexican National Health Surveyc 2000 |
|
Boys |
|
|
|
|
|
2–5 |
6.9 |
13.1 |
11.1 |
|
|
6–11 |
11.9 |
26.7 |
9.1 |
|
|
12–17 |
11.8 |
27.2 |
|
10.6 |
|
Girls |
|
|
|
|
|
2–5 |
10.5 |
8.7 |
9.7 |
|
|
6–11 |
11.6 |
19.8 |
8.5 |
|
|
12–17 |
11.0 |
19.3 |
|
9.3 |
|
NOTE: Obesity is defined as greater than 95th percentile of BMI (Kuczmarski et al., 2002). aOgden et al. (2002). bRivera et al. (2002). cdel Rio-Navarro et al. (2004). Data represent average prevalence values for children 12 to 17 years. |
||||
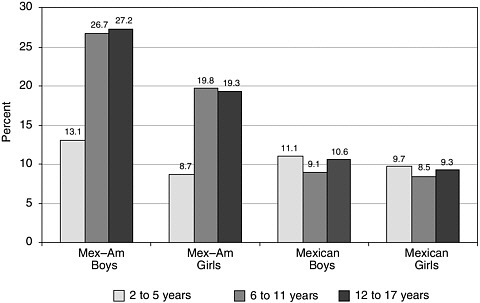
FIGURE C-4 Prevalence of obesity in Mexican–American and Mexican children, 1999–2000.
SOURCE: Rivera et al. (2002) and del Rio-Navarro et al. (2004).
These observations of increased abdominal obesity in Mexican adults parallel the finding of increased abdominal girth in Mexican–American children and youth. In the NHANES III survey, 13.9 percent of Mexican– American children were classified as having a waist circumference-to-height ratio category that exceeded their BMI category, whereas only 7 percent of non-Hispanic Blacks and 9.48 percent of the overall sample were so classified (Kahn et al., 2005). A separate analysis of NHANES III data found that the smoothed 90th percentile of waist circumference for Mexican– American boys was consistently higher than that observed for either African–American boys or European–American boys. The 90th percentile for Mexican–American girls also was consistently higher than that of European–American girls at all ages and greater than that of African– American girls up to 9 years of age. Analysis of waist circumference data from the 1999–2000 NHANES survey also found a consistent pattern of higher mean waist circumference values for Mexican–American children (Ford et al., 2004) (Figure C-5).
These findings of increased waist circumference suggest that Mexican– American children and youth, and particularly Mexican–American boys at all ages, may be at an increased risk of co-morbidities associated with abdominal obesity, including type 2 diabetes.
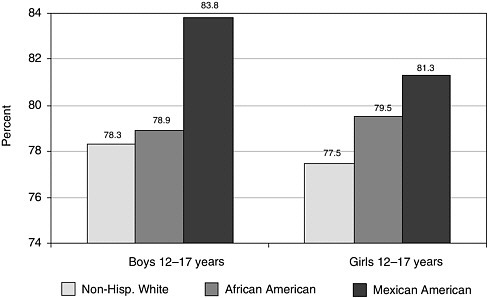
FIGURE C-5 Waist circumference (cm) of boys and girls 12–17 years old, by ethnic group.
SOURCE: NHANES 1999–2000; Ford et al. (2004).
Historical and Current Obesity Trends
Obesity among Mexican–American children is not a new finding. A review of growth studies on Mexican–American children and youth during 1920–1980 (based primarily on immigrant and low-income Mexican Americans) showed a high prevalence of short stature and low weight that was indicative of undernutrition (Malina et al., 1986). However, by the 1970s and early 1980s, regional studies in this review indicated a higher-than-expected level of obesity among Mexican–American children and youth. This increased level of obesity was associated with a shorter stature as compared with non-Hispanic Whites, resulting in a short, plump physique.
Data from NHANES I (1971–1974) demonstrated that differences in BMI between Mexican–American and non-Hispanic children and youth were related significantly to socioeconomic status (SES) (Mendoza and Castillo, 1986). Mexican–American children who had a lower SES had BMIs higher than their non-Hispanic counterparts, but this finding disappeared as SES increased. A combined analysis of NHANES I (1971–1974) and NHANES II (1976–1978) also found that stature was associated directly with SES and that poor children and youth were shorter (Martorell et al., 1988b). Overall, Mexican–American children and youth in this study
were shown to have a short, plump physique, and the data suggested they also had increased upper body fat (Martorell et al., 1988a). Height comparisons between Mexican–American children and non-Hispanic White children showed differences related to SES, although a similar association was not seen for Mexican–American adolescents. These observations suggest that short stature in lower SES Mexican–American children was likely to be related to less adequate nutrition early in life or even during the prenatal period. Since an SES effect was not seen in adolescents it may be that other factors, possibly genetic, are more influential after puberty.
Data analysis from the Hispanic Health and Nutrition Examination Survey (HHANES) (1982–1984) indicated that Mexican–American children showed a higher-than-expected proportion of children above the 90th percentile for BMI between ages 6–11 years—with several year-groups showing twice the expected level—although adolescents showed more variability in the prevalence of obesity (Martorell et al., 1989). Further analyses of the HHANES showed that obesity was associated with increased centralized upper body adiposity and was not a result of having a different body proportion as compared with non-Hispanic Whites (Kaplowitz et al., 1989; Martorell et al., 1988a). In summary, data from HHANES confirmed findings from early studies, indicating that Mexican–American children had increased levels of obesity.
The upward trend in obesity prevalence in Mexican–American children has continued in recent years. Between NHANES III (1988–1994) and NHANES (2003–2004), the prevalence of obesity in adolescent Mexican– American boys ages 12–19 years increased by 4.2 percent (Figure C-6). Among girls, the largest increases were noted in non-Hispanic White and African–American adolescents, although obesity also increased in Mexican–American girls (Figure C-7) (NCHS, 2004; Ogden et al., 2006). It is interesting to note that reported obesity prevalence in male Mexican– American adolescents 12–19 years old decreased from 27.2 percent in 1999– 2000 to 18.3 percent in 2003–2004, and in female adolescents from 19.3 percent in 1999–2000 to 14.1 percent in 2003–2004 (Ogden et al., 2006). The authors note that subgroup estimates by sex, age, and race/ethnicity are less precise than overall estimates due to smaller sample sizes, so that these prevalence estimates must be interpreted with caution.
It is interesting to note that as obesity prevalence has increased over the last several decades, the linear growth of Mexican–American children and adolescents has shown relatively little change. Linear growth improved from the 1960s to 1980s when HHANES was conducted, suggesting that Mexican–American children and youth had not previously been achieving their full height potential (Martorell et al., 1989). Analysis of more recent data indicates that although weight-for-age and BMI percentiles of Mexican–American children increased between HHANES (1982–
1984) and NHANES III (1988–1994), stature-for-age percentiles were largely unchanged (Ryan et al., 1999). Moreover, median height-for-age values for Mexican–American children in NHANES III closely paralleled the median of the CDC reference population and thus indicated that Mexican–American children were achieving linear growth similar to the general U.S. population up to early adolescence.
At approximately 13 to 14 years of age, however, the median stature of Mexican–American girls and boy falls to about the 25th percentile of the CDC reference. The reasons for the falloff in linear growth in adolescents are not well defined but might be related to genetic influences such as an earlier onset of puberty. In any case, the pattern of increased weight-for-age in the interval from HHANES to NHANES III, coupled with little change in stature-for-age, has resulted in a higher ratio of weight to height and is reflected in the increased prevalence of elevated BMI values in Mexican– American children and youth. Further research is needed to better understand the underlying causes of this pattern of linear and weight growth as well as the relationship it may have to the development of obesity. It also would be of interest to compare the pattern of weight and stature growth in Mexican–American children and adolescents with the pattern observed in their counterparts in Mexico.
Data from the National Longitudinal Survey of Youth also demonstrate the upward trend in childhood obesity and indicate a more rapid increase among Hispanic and African–American youth when compared to their European–American counterparts (Strauss and Pollack, 2001). Between 1986 and 1998, the annual rate of increase in obesity prevalence in children ages 4–12 years has been estimated at 4.3 percent and 5.8 percent for Hispanic and African–American youth, respectively, when compared to 3.2 percent for European–American youth. Obesity increased more rapidly among children in southern states (6.2 percent per year) when compared with children in northeastern, central, and western states (3.6 percent, 1.8 percent, and 2.2 percent, respectively) (Strauss and Pollack, 2001). This regional difference in prevalence may be related partly to the high prevalence of Hispanics residing in the southern United States.
Trends in waist circumference in children and adolescents also have been observed. In the interval between NHANES III (1988–1994) and NHANES (1999–2000), waist circumference increased significantly among 12–17-year-old adolescents (Ford et al., 2004). The largest increase in this age group was observed among Mexican–American boys, whose mean waist circumference measurements increased by 5.8 cm (from 78 cm to 83.8 cm)— an increase that was larger than that seen in African–American (5.2 cm) or White non-Hispanic boys (0.5 cm). The mean waist circumference of Mexican–American adolescent girls increased by 5 cm (from 76.3 cm to 81.3 cm)—an increase that was greater than that observed for African– American girls (2.9 cm) or European–American girls (3 cm) of the same age
group. These findings indicate a significant increase in abdominal obesity among Mexican–American adolescents.
Overall, these data indicate that childhood obesity, and perhaps abdominal obesity in particular, represents a long-term and increasing problem among Mexican–American children and adolescents.
Health and Economic Impacts of Obesity
Impact on Physical Health
The relationship between obesity and chronic disease risk in adults has been observed and documented widely. Obesity increases the risk of many conditions including hypertension, CVD, stroke, type 2 diabetes, and certain types of cancer. Since obese children and youth are more likely to be overweight or obese as adults, there is a direct link between childhood obesity and long-term chronic disease risk. Concerns about childhood-onset obesity are supported by documented associations between childhood obesity and increased CVD risk and mortality in adulthood (Srinivasan et al., 2002; Li et al., 2004). Lifetime risk of developing type 2 diabetes for children born in the United States in 2000 has been estimated at 30 percent for boys and 40 percent for girls, with a higher level of risk for ethnic minorities (Narayan, 2003). Although childhood-onset obesity accounts for only 25 percent of adult obesity cases, obesity that is present before a child is 8 years of age and persists into adulthood is associated with severe obesity— defined as a BMI greater than 40 kg/m2—in adulthood as compared with a BMI of 35 for adult-onset obesity (Freedman et al., 2001). Between 1990 and 2000, severe obesity (which is associated with more serious health complications) more than doubled, increasing from 0.78 percent to 2.2 percent in U.S. adults (Freedman et al., 2002).
Longitudinal data in 5–17-year-old European–American and African– American children indicate that obese children had a significantly increased risk for elevated low-density lipoprotein cholesterol, systolic and diastolic blood pressure, and fasting insulin. Fifty percent of the children with two or more of these risk factors were identified by using obesity (defined as a BMI equal to or greater than the 95th percentile) as a screening tool (Freedman et al., 1999). More recent studies in 126 obese Hispanic children ages 8–13 years found that 90 percent of these children had at least one feature of the metabolic syndrome and 30 percent had three or more risk factors and were diagnosed with the metabolic syndrome (Cruz et al., 2004). Furthermore, a recent analysis of NHANES (1999–2000) found that 12–19-year-old Mexican–American adolescents had a higher prevalence (13 percent) of impaired fasting glucose than either non-Hispanic Black (4.2 percent) or non-Hispanic White adolescents (7 percent) (Williams et al., 2005).
As noted previously, increased waist circumference or waist-to-height ratio have been shown to be as effective, or even more effective than BMI, in identifying children with multiple CVD risk factors (Katzmarzyk et al., 2004; Kahn et al., 2005). For this reason, the increasing abdominal obesity observed in Mexican–American youth indicates that they may be at particular risk for CVD in adulthood.
The association of obesity with the risk of developing type 2 diabetes in childhood and adolescence is a particularly serious concern. Children and adolescents who develop type 2 diabetes may experience the micro- and macrovascular complications of this disease at younger ages than individuals who develop diabetes in adulthood (Hannon et al., 2005). An increasing incidence of type 2 diabetes was documented in a longitudinal study from 1982–1994 that showed a 10-fold increase—from 0.7 cases per 100,000 per year in 1982 to 7.2 cases per 100,000 per year in 1994—in incidence among 10–19-year-old adolescents (Pinhas-Hamiel et al., 1996).
An analysis of data from NHANES III (1988–1994) and NHANES (1999–2002) showed a higher prevalence of diabetes and impaired glucose tolerance (a pre-diabetic condition) among Mexican–American adults compared with non-Hispanic Whites, which is consistent with data showing that Mexican–American adults are 1.7 times more likely to have diabetes than non-Hispanic White adults (CDC, 2003, 2005a). Similarly, higher rates of type 2 diabetes are being observed in Mexican–American children and adolescents. As an example, a survey of six high schools in Ventura County, California, identified 28 diabetic adolescents—75 percent more than expected (Neufeld et al., 1998). Correlations were found between the Hispanic enrollment in each school and the number of diabetic adolescents as well as between the obesity rates and adolescents with type 2 diabetes and impaired glucose tolerance.
Sleep apnea is another morbidity related to obesity. It has been suggested that Mexican Americans may have a higher prevalence of sleep apnea than other Hispanic subgroups (Strohl and Redline, 1996). Unfortunately, the available data for the prevalence of obstructive sleep apnea among Mexican–American children and adolescents are very limited (R. Pelayo, Stanford University Sleep Center, personal communication, 2005), even though clinical experience in obesity centers suggests that this is a prominent and growing problem (L. Hammer, Stanford University Medical Center, personal communication, 2005).
Asthma is another morbidity associated with childhood obesity. This condition has been reported to occur at a similar rate among Mexican– American children and adolescents surveyed in HHANES and NHANES III when compared with non-Hispanic Whites (NCR/IOM, 1998, 1999). An analysis by generational status of Mexican–American children and adolescents recorded a lower maternal-reported prevalence of asthma among first-
and second-generation children when compared with third and later generations (NRC/IOM, 1998). Although these data are self-reported and rely on having access to physicians, the trend of increasing asthma with each generation mirrors the pattern for childhood and adolescent obesity. An evaluation of the prevalence of asthma among Mexican–American children and youth in NHANES III showed an odds ratio of 2.1 (1.4, 2.9) for children with a BMI greater than the 85th percentile (Agredano et al., 2004).
Other physical conditions associated with obesity are abnormal serum lipids, hyperinsulinemia or glucose intolerance, and hypertension. These conditions form the basis for Syndrome X (also called the metabolic syndrome). A sample of 52 non-Hispanic White mother–child pairs were compared with 92 Mexican–American mother–child pairs to assess the risk for abnormal lipid profiles, hyperinsulinemia, hypertension, and obesity (Reaven et al., 1998). The findings of this study showed higher levels of obesity and hyperinsulinemia in Mexican–American children and adults compared with non-Hispanic White children and adults and therefore indicated that the Mexican Americans had an increased risk for CVD. Subsequent recommendations for avoiding increased rates of Syndrome X in Mexican American populations included early dietary intervention and exercise modification (Reaven et al., 1998).
Impact on Social and Emotional Health
In addition to the effects of obesity on physical health status and long-term chronic disease risk, obesity in childhood and adolescence can affect social and emotional well-being. As early as 5 years of age, higher weight status in girls was found to be associated with decreased body self-esteem and a perception of decreased cognitive abilities (Davidson and Birch, 2001). The same study found that independent of the girls’ actual weight status a higher level of parental concern about child obesity was associated with a lower perception of physical and cognitive abilities by the daughters.
Another study among kindergartners and first-graders found that obesity was associated with lower academic performance in unadjusted data; however, after social and economic variables (e.g., race and ethnicity as well as mothers’ education levels) were considered, the association was no longer significant (Datar and Magnabosco, 2004). These findings suggest that obesity is a marker but not a causal factor in children’s academic performance. However, this study points out that obesity is observed more easily by other students compared with SES characteristics, and its significant association (unadjusted) with lower academic performance can contribute to the stigma of obesity, even in the early years of elementary school. Mexican–American children may experience a double burden of stigmati-
zation because of the combined effects of stigmas associated with both obesity and ethnic origin.
Obese children are often subject to teasing from their normal-weight peers. The degree of teasing has been associated with higher weight concerns, more loneliness, poorer self-perception of physical appearance, higher preference for sedentary and isolated activities, and lower preference for physical or social activities (Hayden-Wade et al., 2005). Obesity also can affect self-perceived quality of life. A study of 106 children and adolescents ages 5–18 years (60 percent of the youth were Mexican) who were referred to a children’s hospital for evaluation of obesity found that the self-reported quality of life score of the obese children and youth was significantly lower than that of their normal-weight peers and was similar to the score reported by children diagnosed with cancer (Schwimmer et al., 2003). Another study of body image and adolescent mental health found that Hispanic girls were more depressed and had lower self-esteem than other racial and ethnic groups even after controlling for body image. This study concluded that Hispanic adolescents may be at increased risk for mental health problems (Siegel et al., 1999).
Mexican–American children and adolescents have had a long battle with obesity and continue to lead the nation with regard to the proportion of their population who are either obese or at high risk for becoming obese. In addition, they are exhibiting the co-morbidities associated with obesity. Mexican–American adults are demonstrating the poor health outcomes associated with obesity, including increased levels of diabetes and CVD. It is important to remember that today’s adults were children and adolescents in the 1970s and 1980s when Mexican Americans were first recognized to be at a greater risk for obesity. Consequently, if Mexican–American adults currently have some of the highest rates of diabetes in the country, what will this population look like when the current group of children become adults?
Impact on Health Care Costs
Studies of health care expenditures in the United States have documented the high cost and sharp upward trend in expenditures attributable to obesity. Econometric models indicate that the annual cost of obesity-related health care is approximately $75 billion (expressed in 2003 dollars) and that approximately half of these expenditures are financed by public funds through Medicare and Medicaid programs (Finkelstein et al., 2004). Overall, per capita health care costs have been rising rapidly, from an estimated $2,188 per capita in 1987 to $3,298 per capita in 2001 (expressed in 2001 dollars). Approximately 27 percent of this increase, or $301 per capita, can be attributed to obesity-related health care costs (Thorpe et al., 2004).
Hospital discharge data indicate that the economic burden of obesity-related illness is also increasing among children and youth in the United States. From 1979 to 1999 discharges with a diagnosis of diabetes nearly doubled, obesity and gallbladder diseases tripled, and sleep apnea discharges increased fivefold (Wang and Dietz, 2002). The same study also documented a greater than threefold increase in obesity-associated hospital costs, from $35 million during 1979–1981 to $127 million during 1997–1999.
These studies did not identify specifically health care costs associated with increasing obesity in Mexican–American children and youth. However, since many Mexican–American families depend on publicly funded programs (such as Medicaid) for health care, and since many may be underinsured or uninsured, the high prevalence and rapid increase in obesity among Mexican Americans inevitably will place increasing demands on these health care providers and have important implications for the funding needs of these programs (Flores et al., 1998; Burgos et al., 2005).
To date no study has calculated the economic impact of obesity in Mexican–American children and youth. However, an analysis of the economic impact of obesity has been conducted for the state of California, where approximately 35 percent of the population is Mexican American, 50 percent of the infants born are Hispanic and primarily Mexican American, and a large immigrant (mainly Mexican) population exists. This analysis assessed the economic cost attributable to physical inactivity, being overweight, and obesity with respect to medical costs, workers compensation, and loss productivity. The results showed a $21.7 billion loss—$10.2 billion in medical care, $338 million in workers compensation, and $11.2 billion in loss productivity. The following annual costs were determined: physical inactivity, $13.3 billion; obesity, $6.4 billon; and being overweight, $2 billion. An increase to $28 billion by 2005 subsequently was forecast unless aggressive actions were taken (Chenoweth, 2005).
These data from California provide insight into the enormous economic costs associated with obesity. When these costs are projected to the national level in the United States and Mexico, the overall impact on health care costs is staggering. Moreover, the outlook is that these costs will continue to increase unless ways are found to prevent and control the adult and childhood obesity epidemic.
FACTORS INFLUENCING OBESITY IN MEXICAN–AMERICAN CHILDREN AND YOUTH
Energy Balance
Obesity is the end result of an energy imbalance, in which overall caloric intake exceeds caloric expenditure. The high and increasing levels of
obesity in Mexican–American children and youth would suggest strongly that their energy intake exceeds their energy expenditure and that the imbalance has increased over time. This excess of energy intake over expenditure could be the result of changing dietary patterns favoring an increased intake of higher caloric foods, decreased energy expenditure through limited physical activity, or some combination of both effects.
A number of contextual factors also may influence energy balance. Cultural perceptions of children’s ideal body physique by parents may influence child feeding patterns, favoring a robust physique early in life and thereby increasing a child’s risk of obesity. Another potential contextual influence on energy balance is the generational status of the child’s family, in other words, whether the child’s family is the first or second or even a later generation living in the United States. Changes in energy balance in first-generation families may be affected by changes in types and quantity of food available after the families immigrate into the United States as well as by the process of acculturation in dietary preferences. Transition from traditional Mexican diets to American diets likewise may affect second and later generation families as succeeding generations become more acculturated. The insecure employment settings and the environment of poverty in which many Mexican Americans live also may have effects on energy balance by influencing dietary choices, physical activity opportunities, and access to health care.
Finally, it is possible that maternal factors, such as pre-pregnancy obesity, and genetic factors may influence obesity risk. A discussion on the potential impact of these factors on energy balance and obesity risk follows.
Dietary Patterns and Obesity Risk
Data from national surveys indicate an overall increase in daily caloric intake, by approximately 150–200 calories, of American adults from 1971 to 2000 (CDC, 2004). The same trend appears to exist with regard to children—a recent IOM report found that “total calorie intake appears to have increased substantially over the past 25 years for preschool children and adolescent boys and girls, with more modest changes for children ages 6–11 years” (IOM, 2006). However, differences in caloric intake in relation to ethnicity were not defined.
Is the increased prevalence of obesity in Mexican–American children and youth related to the quality of their diets? Large scale dietary intake data to address this question were first provided in the HHANES. An analysis of food frequency demonstrated that Mexican–American children and youth reported eating from the recommended four food groups only 70 percent and 55 percent of the time, respectively (Murphy et al., 1990). Further analysis of these data by foreign-born as well as U.S.-born Mexican
Americans demonstrates that foreign-born Mexican Americans reported eating fruits and vegetables more frequently and eating fewer sugars (NRC/ IOM, 1999). Similar findings were seen in NHANES III in adolescents. Those adolescents living in less acculturated homes had less fat, protein, and energy in their diets and more folate (Mazur et al., 2003). Intakes of these nutrients increased with acculturation.
In a study of a nationally representative sample of children, dietary recall on two separate days was used to determine the frequency of fastfood intake. Hispanic children were the least likely to eat fast food as compared with non-Hispanic Whites and African Americans (Bowman et al., 2004). However, once gender, SES, and geographic region were controlled, Hispanic youth were similar in fast-food intake to non-Hispanic Whites. In a U.S. Department of Agriculture study, the diets of children and adolescents were examined using data from NHANES (1999–2000) and a healthy eating index, which measured 10 nutritional components, including the intake of recommended fruits and vegetables and of fat (Basiotis, 2004). This study showed that Mexican Americans overall have a better dietary intake profile than non-Hispanic Whites or Blacks. Furthermore, those born in Mexico had better intake profiles than those born in the United States.
Overall, dietary intake studies suggest that less acculturated children and adults have nutritionally better food intakes with respect to fruits and vegetables, however, as acculturation increases so does fat intake. Therefore, maintaining a traditional diet seems to be an important factor in preventing obesity in Mexican–American children and their families.
Physical Activity and Sedentary Behaviors
Physical activity is the second part of the obesity equation. Data from NHANES III on physical activity and television watching (Andersen et al., 1998) showed that Mexican–American boys and girls reported less physical activity (defined as engaging in three bouts of vigorous activity per week) than non-Hispanic White boys (80.2 percent versus 87.9 percent) and girls (72.6 percent versus 77.1 percent). Mexican-American boys and girls also reported watching more television than non-Hispanic Whites—33.3 percent versus 24.3 percent for boys and 28.3 percent versus 15.6 percent for girls watched more than four hours per day. Watching television is a sedentary activity and occupies time that might otherwise be devoted to more active pursuits. In addition, children are exposed to extensive advertising for high-calorie and low-nutrient foods and beverages (IOM, 2006). More research is needed to better define the television-watching habits of Hispanic and Latino children and youth and to determine how the content of Spanish- and English-language programming impacts their physical activity and dietary behaviors.
Data from the 2002 Youth Media Campaign Longitudinal Survey—a national survey on physical activity—showed that Mexican–American youth are significantly less likely to participate in organized sports than non-Hispanic Whites (25.9 percent versus 46.6 percent) and are somewhat less likely to report (within a seven-day period) participation in free-time play activity (74.6 percent versus 79.3 percent) (Duke et al., 2003). This survey also examined barriers to physical activity and found that Hispanic parents more frequently reported barriers related to transportation issues, a lack of appropriate facilities, expense, a lack of parent time, and a lack of neighborhood safety. However, neighborhood safety was the only barrier that was significantly increased for Hispanic parents when compared with the African–American and non-Hispanic White parents (41.2 percent versus 13.3 percent and 8.5 percent, respectively).
Other data on Hispanic adolescents show similar findings. The California Health Interview Survey 2003 found less regular physical activity among Hispanic (primarily Mexican American) than non-Hispanic White adolescents. Moreover, twice the percentage of Hispanic teens reported no physical activity when compared with non-Hispanic Whites (9.5 percent versus 4.1 percent) (Babey et al., 2005). Only 70 percent of Hispanic teens were in schools that required physical education. In those schools, Hispanic adolescents reported doing regular physical activity significantly more often than Hispanic adolescents in schools where physical education was not required (70.2 percent versus 58.6 percent). Overall, these studies suggest that Mexican–American children and youth are less engaged in regular physical activity than their non-Hispanic counterparts. Barriers to physical activity include the perception of unsafe neighborhoods, the cost (in dollars and time) of sport activities, and the lack of local recreational opportunities such as parks and open spaces. The latter is significant since soccer was reported as the most preferred sport of Hispanic teens in the 2002 Youth Media Campaign Longitudinal Survey.
Culturally Based Perceptions that Influence Obesity
The perception of desirable body physique and what is considered “normal weight” can influence obesity risk by affecting dietary and physical activity behaviors. These perceptions have cultural overlays from current experience (e.g., from the fashion industry) and past experiences such as familial experiences with malnutrition or recurrent illness. These issues need to be explored with Mexican Americans, because they come from a complex cultural milieu involving both Mexican and American influences. Moreover, with a large proportion of immigrants recently arrived from Mexico and the majority of Mexican Americans maintaining some ties to the Latino culture, perceptions of normal weight for Mexican–American
children, youth, and parents may be quite different from those of non-Hispanics.
Maynard et al. (2003) examined the NHANES III data to explore maternal perceptions of their children’s weight status. Although only 65 percent of mothers identified their children as overweight when they had a BMI greater than the 95th percentile, there was no difference in this ability between Mexican–American and non-Hispanic White mothers (Maynard et al., 2003). However, using the same survey, Klaudt et al. (2002) found that Mexican–American mothers who rated their children as being at the correct weight or at a low weight had children with a higher BMI compared with non-Hispanic White mothers. This finding raises the possiblity that Mexican–American mothers believe that a more rotund physique is normal. Even though the child might not be obese by BMI standards, if the mother’s perception is that a “plump” child is healthy, then this perception will need to be addressed so that interventions to control obesity can be successful. Consequently, future research should seek to uncover a better understanding of what Mexican–American mothers consider to be good parenting practices with regard to diet and physical activity.
A more complete understanding of cultural perceptions regarding child rearing may need to involve educating not only the parents but also the entire extended family and community. Familism—the importance of family and culture—is a fundamental factor in Mexican–American families. Romero et al. (2004) hypothesized that this would be strongest in less-educated, Spanish-speaking, and poor families. Instead, the greater levels of familism were seen in those with more education, higher income, and bilingual or English-speaking families. Although this study involved a large, mobile immigrant population, it suggests that even with acculturation, Mexican Americans still retain a strong family orientation. As such, lifestyle changes for Mexican–American children probably will be achieved best by supporting changes at the family and community levels.
Generational Status
Analyses of the HHANES data found that differences in height and weight among immigrant and U.S.-born Mexican–American children were primarily the result of parental SES, and that birthplace did not contribute significantly to either weight or height (NRC/IOM, 1999). Mexican– American children, whether U.S.- or non-U.S. born, had relatively normal weights during childhood compared to their heights. However, during adolescence there was more variability in weights between adolescent boys and girls, particularly with first-generation boys who demonstrated the lowest weights. In HHANES, 12–18-year-old adolescents showed increasing obesity in later generations. However, being foreign born did not dem-
onstrate any difference in BMI for Mexican–American adolescents once age, gender, and SES were controlled (NRC/IOM, 1999). In another study that used data from the National Longitudinal Study of Adolescent Health, Hispanic adolescents born in the United States were twice as likely to be obese than those born outside of the country (Popkin and Udry, 1998). Mexican Americans were the largest Hispanic group in the sample and had the highest percentage (32 percent) over the 85th percentile (considered to be at-risk for obesity). Thus, these studies suggest that U.S.-born Mexican–American youth are more obese than those born in Mexico. This finding is consistent with recent data from the National Health Interview Survey indicating significantly higher rates of obesity and hypertension among U.S.-born Hispanic adults when compared with Hispanic immigrants residing in the United States for less than five years (CDC, 2006).
Acculturation
Acculturation is the process of changing cultural customs, attitudes, perceptions, and behaviors. The time frame of the acculturation process varies from individual to individual and is driven by the living environment and other social pressures for acculturation, such as schools, friends, media, and work. Measures of acculturation usually assess changes in language usage, food preferences, leisure preferences, and social networks. The process of acculturation also can involve changes in perceptions and models of health and well-being that can have a major impact on an individual’s health behaviors and assessments of health risk. Even though generational and immigrant status are linked closely to the acculturation process, they are not the same. For that reason, the effects of acculturation on Hispanic obesity need to be explored further.
In a study of immigrant Hispanic adults sampled from the National Health Interview Survey 1998, those who were in the United States for 15 years or longer had a greater likelihood of having a BMI of 30 or greater (Kaplan et al., 2004). Among Hispanics who had been in the United States fewer than 5 years, 9.4 percent had a BMI greater than 30; among those who had been in the United States for more than 15 years, 24.2 percent had a BMI greater than 30. In this study, Mexican Americans were more than 50 percent of the sample and had the highest proportion of obese adults.
In a study conducted in Washington State, Mexican immigrants were found to consume fewer fruits and vegetables as they became more acculturated (Neuhouser et al., 2004). Using data from NHANES III, Dixon et al. (2000) examined the differences in dietary intakes of adult Mexican– American men and women and found that those who were less acculturated took in less fat and more fiber and vitamins. Although these studies focused primarily on adults, they suggest that as immigrants become more accultur-
ated, their diets change and obesity increases from one generation to the next. Since Mexican–American children and youth comprise such a large proportion of those living in immigrant families, the processes involved in acculturation may be major factors in the increasing prevalence of obesity.
Workforce Participation and the Environment of Poverty
Mexican Americans, who comprise two-thirds of all U.S. Hispanics, continue to be one of the poorest and youngest groups of Americans, with 37 percent of the populations under 18 years of age. The U.S. Census reports that 21.9 percent of Hispanic families live in poverty. In addition, even though Mexican Americans have a workforce participation equal to that of non-Hispanic Whites, they have the highest rate of being uninsured (BLS, 2004; DeNavas-Walt et al., 2005). Both parents typically are working to support their families, a situation that makes child care a major issue. This is particularly true for immigrant families who have higher rates of poverty (Burgos et al., 2005). In addition, with low levels of education, Mexican–American parents tend to have lower paying jobs that are less likely to provide insurance. Their jobs often have less security and typically less union protection, particularly for farm workers before their unionization. Thus, although Mexican Americans have high workforce participation, they continue to live in poverty without health insurance and with limited upward mobility. These realities will impact efforts to prevent obesity by limiting the availability of money to buy healthy food, live in safe areas, and have health insurance to receive preventive and therapeutic medical care.
Though many live in poverty, Mexican Americans are a heterogeneous population in many different ways: economically, culturally, educationally, and even regionally. The status of Mexican Americans currently is undergoing a dramatic change, which can be seen in states like California where Mexican Americans now hold leadership positions in government. This diversity in the population, from the poorest to the most powerful, needs to be considered in developing a strategic plan to improve the problem of obesity in this community while maintaining a focus on those most at risk and least able to help themselves.
Maternal and Genetic Effects on Obesity Risk
Recent studies have suggested that maternal factors such as prepregnancy obesity may influence subsequent obesity risk for children, especially if born to a Hispanic mother (Whitaker, 2004; Salsberry and Reagan, 2005). Genetic factors that may influence energy usage through variable metabolic rates and the degree of fat storage are also potentially
important. Preliminary studies in American–Pima Indian populations have shown genotypes in which metabolic rates that are lower by as much as 150 Kcal/d, such that the unburned calories may increase the risk of obesity (Kovacs et al., 2005). The study’s investigators were unable to show a direct association with obesity; however, further research may demonstrate a genetic risk for this population that would have significant implications for Mexican Americans who may share the same genotype. Thus, it is possible that Mexican and Mexican–American children with a high proportion of indigenous ancestry may have a greater tendency toward obesity.
CURRENT POLICIES AND PROGRAMS
Various intervention activities have been developed to address child obesity, including media-based health promotion, school-based interventions, community-level activities, health care and family counseling, and research and monitoring. Information on current intervention programs is available from a variety of sources (Action for Healthy Kids, 2005; International Life Sciences Institute, 2005; Shaping America’s Youth, 2004). The majority of these interventions have addressed English-speaking audiences, but some programs and materials have been developed in Spanish.
Many current programs have been evaluated to assess their impact on obesity, and the results indicate that the programs have at least short-term reductions in obesity prevalence or improvements in obesity-related dietary and physical activity behaviors. However, these evaluations often are limited methodologically. For example, a recent review of school-based interventions by the Task Force on Community Preventive Services concluded that there was insufficient evidence to determine the effectiveness on children and adolescents of interventions in school settings (CDC, 2005c). Another recent report by the Preventative Services Task Force also cautioned that “interventions to treat overweight adolescents in clinical settings have not been shown to have clinically significant benefits and are not widely available” (Whitlock et al., 2005).
A wide variety of intervention activities that hold promise for successful outcomes are underway although their long-term effectiveness is still to be demonstrated. A number of these interventions have been adapted for use with Spanish-speaking children and families. As noted in the IOM report Preventing Childhood Obesity: Health in the Balance, it would be detrimental to wait for conclusive evidence before moving forward with interventions that, based on available evidence, are most likely to provide positive results (IOM, 2005).
This section provides an overview of current intervention activities in the media, schools, communities, and health care settings, as well as related research and monitoring activities. Primary attention is paid to policies and
programs that are focused on or relevant to obesity prevention in Mexican– American or other Hispanic children and youth.
Media-Based Health Promotion
The widespread access of Mexican–American families to Spanish media offers promising opportunities to provide health promotion information through media channels. The great majority of Mexican–American families have daily access to television, and radio continues to be a prominent media source for Latinos (Kissam et al., 2003). Access to the Internet is increasing rapidly. Studies by the Pew Internet and American Life Project found that half of all adult Hispanics who speak English had used the Internet and that 78 percent of those with Internet access are online at least 3–5 times a week (Spooner and Rainie, 2001). Although Mexican Americans have substantial media access, the quality of health information disseminated over these channels varies considerably in quality and consistency. Broadie et al. (1999) found that even though Latinos sought out information from the general media, they did not trust the media for health information and felt that media sources did not cover the health issues most relevant to minority communities.
Television viewing by Mexican–American children and youth may be particularly important as both a causal factor in obesity and as a potential source of intervention. A recent IOM report, Food Marketing to Children and Youth: Threat or Opportunity, found that children are being exposed to extensive advertising for high-calorie, low-nutrient foods but very limited advertising for more healthful foods and beverages (IOM, 2006). Information on the media exposure of “tweens” and “teens” is available, but there does not appear to be a current content analysis of food and beverage advertisements directed at Hispanic and Latino children and youth despite a high level of expenditure on Hispanic media and advertising (Roberts et al., 2005; Endicott et.al., 2005).
Efforts are underway, however, to improve both the quantity and quality of health information content, although their effectiveness still needs to be evaluated (Velez-Subervi, 1999). Descriptions of some of the more prominent Spanish-language media-based activities initiated by both government and privately sponsored organizations follow. Additional Spanish-language media activities are summarized in tabular form.
Government-Sponsored Media Interventions
Government agencies in the United States and Mexico have initiated media-based interventions to promote healthy eating and physical activity. Some of these programs are briefly described below. Table C-2 summarizes
TABLE C-2 Government-Sponsored Media Interventions
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
VERB |
“Tweens” (9–13 years) |
|
Contact: |
|
Eat Smart, Play Hard |
6–18 years |
|
Contact: http://www.fns.usda.gov/eatsmartplayhard/Collection/sp-collect_tools.html |
information about these programs and provides information about several additional, government-sponsored media intervention activities.
VERB
The VERB campaign was developed by the Centers for Disease Control and Prevention (CDC) as a five-year social marketing campaign for “tweens,” children of ages 9–13 years. The campaign is based on formative research that assessed youths’ attitudes and practices relating to physical activity. Longitudinal evaluation of the campaign’s impact demonstrated
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Todo en Sobrepeso y Obesidad |
Older teens and adults |
|
Developed by Mexican Government Contact: |
|
BAM |
9–13 years |
|
Contact: |
|
Powerful Bones, Powerful Girls |
Tweens and teenage girls |
|
Contact: |
|
Small Steps/Kids |
Primary school age |
|
Contact: |
positive effects. Surveys conducted at baseline and at one year after the launch of the campaign found that 74 percent of the children surveyed were aware of the VERB campaign. Levels of self-reported, free-time physical activity increased among various subgroups of children aware of the campaign when compared with levels in children who were unaware of VERB (Huhman et al., 2005). Ongoing evaluation of the VERB campaign will provide valuable information on the potential effectiveness of Web-based health promotion. Though the VERB website for “tweens” does not have Spanish-language content, its images, games, and activities are designed to be appealing to all ethnic groups. VERB has health promotion information
in Spanish on the CDC website, with links to a wide variety of health information.
Eat Smart, Play Hard
The U.S. Department of Agriculture (USDA) has also launched a national nutrition education and promotion campaign called Eat Smart, Play Hard, which was targeted at preschool and school-age children and their caregivers. The campaign uses multiple communication vehicles, approaches, and channels, including print materials and the Internet. In addition to English-language content, the campaign’s website displays Spanish-language educational materials designed for use by children and adolescents in schools and community programs.
Todo en Sobrepeso y Obesidad
The Mexican government, in collaboration with professional societies and industry partners, has developed a health information website: Todo En Sobrepeso y Obesidad. The site provides information on obesity and related cardiovascular risks for patients, health professionals, and families. Because it originates in Mexico, the content is culturally and linguistically adapted for use by Mexican Americans. A related site, Todo en Diabetes, provides information specifically for patients, professionals, and families concerned about or caring for persons with diabetes.
Privately-Sponsored Media Interventions
A variety of media-based interventions also have been privately sponsored. Some of the more prominent programs that provide Spanish-language content follow. These programs also are summarized in Table C-3, along with several additional privately supported media interventions.
Salud es Vida … Enterate!
Television and radio broadcasters have potential to reach a great number of Hispanics with health information. A prominent example is the health education initiative of Univision Communications Inc., Salud es Vida … Enterate!, which was launched in 2003. This health promotion effort provides informational messages and programming—including public service announcements (PSAs), vignettes, news, and dedicated health programs featuring nationally recognized Hispanic celebrities and medical experts—on radio and television. To complement this effort, Univision.com has developed a comprehensive Spanish-language website that provides information
TABLE C-3 Privately Sponsored Media Interventions
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Salud es Vida … Enterate!! |
Parents and Older teens |
|
Contact: Univision Communications Inc. http://www.univision.com/content/channel.jhtml?chid=2&schid=8241 |
|
Coalition for Healthy Children |
Children, teens, and parents |
|
Contact: |
|
Kidnetic |
Primary school kids and teens |
|
Contact: |
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Shaping America’s Youth |
All ages |
|
Contact: |
on a wide range of health issues and advice on healthful nutrition and physical activities. The campaign is not directed at children or adolescents, but the messages do reach Hispanic parents who are seeking information about nutrition, physical activity, and being overweight as those topics relate to caring for their children. Partners with Univision in this initiative include the Kaiser Family Foundation, the Ad Council, the American Diabetes Association and many other health, community, and medical organizations.
Coalition for Healthy Children: Combating Childhood Obesity
Another initiative to enhance health information for children and youth is the Coalition for Healthy Children, a public–private collaboration designed to use the collective strengths of marketers, the media, nonprofits, foundations, and government agencies to address the obesity crisis. With support from the Robert Wood Johnson Foundation and in cooperation with the Advertising Council, the coalition aims to provide consistent, research-based messages targeted at parents and children. The coalition’s strategy is to have each of its members incorporate these common messages into their communications activities, including advertising, packaging, websites, grassroots programs, and marketing events. Program impact will be assessed through an ongoing tracking study. Although no specific plans have been developed for translating these or other messages into Spanish, coalition members could address this need and share their efforts with others.
School-Based Interventions
A wide variety of school-based intervention programs have been developed but few are designed specifically for Hispanic children. However, Spanish-language teaching materials are available from a number of sources, and many programs and policies that promote physical activity and provide
for healthful food choices in schools can benefit all children, including Mexican Americans.
Implementing school-based obesity interventions can present a number of challenges (GAO, 2005). Changes in school curriculum to include more nutrition education or increased physical activity opportunities must be integrated into and contend with other academic priorities. Physical activity programs may be less controversial since changes in school food or vending policies must deal with the added costs of providing more healthful meals and possible lost income from vending contracts. School administrators cite a lack of program models and clear guidelines but at the same time want flexibility to adapt interventions to meet their local needs and resources.
Despite these challenges, many school-based interventions have been initiated (Food and Nutrition Service, 2005). Several intervention programs, including Bienestar and CATCH, have been undertaken and evaluated in schools with a high proportion of Mexican–American children. These intervention programs have combined nutrition education and have increased opportunities for physical activity with policy changes with regard to vending and the nutritional quality of school meals. These programs provide examples of promising strategies for school-based intervention that have been successful in schools with a high proportion of Mexican–American children. A complementary strategy, described below, is the development of school wellness policies as required by recent federal legislation. Finally, Table 4-3 lists resources for obtaining Spanish-language educational materials for classroom instruction and for sharing with parents, although the effectiveness of these materials has not been evaluated.
Bienestar
Developed in San Antonio, Texas, Bienestar is a bilingual, nutrition and physical activity promotion program designed specifically for use in elementary schools with a high proportion of Hispanic children. The intervention is based on social cognitive theory that recognizes the need to change the social systems that influence children’s behaviors. In line with this theoretical construct, the intervention consists of programs targeting parents, school health classes, cafeterias, and after-school programs.
The impact of the intervention on obesity and diabetes risk factors was evaluated, and the results were reported in a recent study in San Antonio, Texas (Trevino et al., 2005). This randomized, controlled trial found that after adjusting for covariates the mean fasting capillary glucose levels decreased in the intervention schools and increased in control schools. Fitness scores increased significantly in intervention children and decreased in control children. However, no significant difference was found in the percentage of body fat. Even though longer follow-up will be needed to determine
long-term benefits, these results indicate the potential success of a multicomponent, bilingual intervention to modify risk factors for diabetes.
CATCH
The Coordinated Approach to Child Health (CATCH) program in El Paso, Texas, implemented a school-based intervention to increase moderate to vigorous physical activity and to improve the nutritional content of school meals. Evaluation in 24 schools with a high proportion of Mexican–American children found that, for most intervention schools, the intervention was associated with significantly increased moderate to vigorous physical activity and decreased fat in school meals. However, some schools did not meet fat content goals, and no schools met the vigorous physical activity goals (Heath and Coleman, 2002). Other follow-up studies in a cohort of children from ethnically diverse backgrounds in California, Louisiana, Minnesota, and Texas have shown that behavioral changes associated with the CATCH intervention were maintained for three years without further intervention. Although not specific to any single ethnic group, these findings suggest that behavioral changes initiated during the elementary school years may persist into early adolescence (Nader et al., 1999).
Wellness Policy Development
An important policy development stemming from the Child Nutrition and WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) Reauthorization Act of 2004 requires all school districts with a federally-funded school meals program to develop and implement wellness policies that address nutrition and physical activity by the start of the 2006– 2007 school year. This new requirement for a defined wellness policy presents a significant opportunity for advancing school-based nutrition and physical activity promotion. School administrators, teachers, and parents should be encouraged to use the opportunity to review current policies and identify changes that can improve the healthfulness of the school environment and contribute to obesity prevention.
A number of resources are available to assist schools in developing wellness policies. The National Alliance for Nutrition and Activity has developed a set of model policies for use by local school districts. Resources to aid schools in formulating wellness policies include CDC’s School Health Index, USDA’s Changing the Scene guidelines, and wellness policy development tools trainings from Action for Healthy Kids (Table C-4). Support for developing and implementing school wellness policies should be a high priority.
TABLE C-4 School-Based Interventions and Teaching Materials
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Bienestar |
Grades 3–5 |
|
Contact: Social and Health Research Center |
|
CATCH (Coordinated Approach to Child Health) |
Intervene grades K–5 Follow-up grades 6–8 |
Environmental Change Goals:
|
Contact: |
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
School Wellness Policy Development |
School staff and parents |
|
Contact: http://www.schoolwellnesspolicies.org/ http://apps.nccd.cdc.gov/shi/default.aspx |
|
My Pyramid for Kids |
Grades K–5 |
|
Contact: |
|
MiPirámide |
Children and teens |
|
|
|
What’s to Eat |
Parents and older children |
|
Contact: |
|
Learning Zone Express |
Grades K–12 |
|
Contact: |
Community-Based Interventions
Many community level interventions have been initiated to promote physical activity and nutrition improvement in children, adolescents, and adults. Examples of programs that specifically address the needs of Hispanic children and youth are described in the following sections as are more general programs that assist the community as a whole in implementing obesity prevention strategies. The programs cited are summarized in Table C-5.
Government-Sponsored Interventions
Diviértase y Sea Activo
Diviértase y Sea Activo (Have Fun and Be Active) is the title of a physical activity program funded by the Contra Costa Children and Families Commission of Contra Costa County, California. A video, available in Spanish and English, encourages families to choose a healthy, active lifestyle by showing images of families participating in variety of physical activities. A related activity also provided by the Commission is the scheduling of community health promotion fairs for Hispanic families; the fairs are advertised to the community as Diviértase y Manténgase Saludable Talleres (Have Fun and Be Healthy Workshops). At these events families learn to prepare healthy snacks, play games, and participate in fun physical activities. This program provides an interesting model in which activities potentially contributing to obesity prevention can be integrated into a larger framework of community efforts to promote child health.
California Latino 5-a-Day
California’s Latino 5-a-Day program promotes fruit and vegetable consumption among Spanish-speaking adults. The intervention is designed to reach Latinos in their homes, where they shop, where they eat, and where they gather with other community members. Evaluation of the program’s impact by telephone interviews found a significant increase in fruit and vegetable consumption and increased awareness of the 5-a-Day message among Spanish-speakers in the target area of the campaign. Although the program does not directly address children and adolescents, the campaign may have an impact by modifying parent’s attitudes and food purchase behaviors. California also has developed a Children’s 5-a-Day Power Play Campaign targeted to 9–11-year-old children. Even though the program is not presented in Spanish, it is designed to appeal to English-speaking Latino children.
TABLE C-5 Government-Sponsored Interventions
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Diviértase y Sea Activo |
1–5 years |
|
Contact for purchase of the video: http://www.abridgeclub.com/Videos_&_DVD.htm#Have%20Fun%20&%20Be%20Active Brochure for health fair: http://www.cchealth.org/espanol/pdf/wic_funshops_esp_2005_10.pdf |
|
California Latino 5-a-Day Children’s 5-a-Day Power Play |
|
|
Contact: http://www.dhs.ca.gov/ps/cdic/cpns/lat5aday/lat_research.htm |
|
Food Stamp Program |
|
|
Contact: http://www.sfgate.com/cgi-bin/article.cgi?file=/chronicle/archive/2004/10/01/BAGG691K4B1.DTL |
Food Stamp Program
Participation in the food stamp program can assist low-income families in buying nutritious foods that may be less likely to contribute to obesity. Eligibility for food stamps is based on income, and all children born in the United States are entitled to the benefits. However, a survey by the Alameda County Community Food Bank estimated that 1.7 million Californians, many of them Latino, are eligible for food stamps but do not participate in the program. These findings suggest that an educational campaign to expand awareness of and participation in the food stamp program by Mexican Americans could help improve access to healthful foods and would be a valuable component of an overall obesity prevention strategy.
Private and Community-Sponsored Interventions
Many promising community-based programs have been initiated by private and non-profit organizations that are concerned with the health and welfare of children. Examples of such programs are described in the following sections and summarized in Table C-6.
CANFit
The California Adolescent Nutrition and Fitness (CANFit) Program is designed to help communities build the capacity to improve the nutrition and physical activity status of low-income ethnic youth who are 10–14 years old. CANFit has launched health promotion campaigns specifically addressing the Hispanic community. For example, the Adelante con Leche Semi-descremada 1 percent campaign, implemented in Los Angeles in 1999–2000, was designed to motivate Latino youth and their families to switch from drinking whole or two-percent milk, to drinking one-percent or fat-free milk. Based on sales report data, the Adelante campaign resulted in a 200-percent increase in one-percent milk sales (see Table C-6 for reference).
Latino Health Access
Latino Health Access is a community-based health promotion program that uses community health promoters who are recruited to work in the communities where they live. The promotores are skilled at educating and serving as role models for their peers. The Children and Youth Initiative, a program of Latino Health Access in California, is a school and community based intervention that is designed specifically for assisting children who
TABLE C-6 Private and Community-Sponsored Interventions
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
CANFit (California Adolescent Nutrition and Fitness program) |
10–14 years |
|
Contact: |
|
Latino Health Access |
Children and youth |
|
Contact: |
|
Kraft Salsa, Sabor y Salud |
Latino families |
|
Contact: |
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Latino Nutrition Coalition |
Latino families |
|
Contact: http://www.latinonutrition.org/ http://oldwayspt.org/index.php?area=latino_nutrition_coalition |
live in high-risk environments to adopt nutrition, physical activity, and other positive behaviors that promote good health.
Salsa, Sabor y Salud
Kraft has partnered with the National Latino Children’s Institute to develop Salsa, Sabor y Salud (Food, Fun, and Fitness), an eight-session healthy-lifestyle course for Latino families. The program supports Hispanic families in adopting healthy lifestyles that will reduce the risk of obesity and related health problems. Launched in 2003, Salsa, Sabor y Salud has reached nearly 10,000 adults and children through 50 community organizations in six states.
Latino Nutrition Coalition
The Latino Nutrition Coalition is a consortium of industry leaders, scientists, and chefs in cooperation with the Oldways Preservation Trust to promote better Latino health through traditional foods and lifestyles. The Coalition will focus on practical programs of education and promotion in grocery stores, schools, health clinics, and restaurants. Initiatives that will include community fiestas and festivals are planned in five or six cities.
Health Care Interventions
Mexican Americans and other Hispanics face a number of barriers in accessing health care, including language barriers, cultural differences, poverty, lack of health insurance, and transportation difficulties. These chal-
lenges complicate the provision of healthcare interventions to prevent and manage obesity in Mexican–American children. Evaluation of interventions in the health care setting has encountered methodological limitations. In 2002 the U.S. Preventive Services Task Force concluded that “the evidence is insufficient to recommend for or against behavioral counseling in primary care settings to promote physical activity,” noting that there were no completed trials with children or adolescents that compared counseling with usual care practices (USPSTF, 2002). In 2003 another task force report concluded that “the evidence is insufficient to recommend for or against routine behavioral counseling to promote a healthy diet in unselected patients in primary care settings,” noting that “no controlled trials of routine behavioral dietary counseling for children or adolescents in the primary care setting were identified” (USPSTF, 2003). As noted previously, a recent task force report cautioned that “interventions to treat overweight adolescents in clinical settings have not been shown to have clinically significant benefits and are not widely available.” Although much more needs to be done to provide a more adequate research base, both government-sponsored and privately supported efforts are underway to address obesity in clinical settings. Examples of health care interventions that address Hispanic populations are highlighted in the following sections and are summarized in Table 4-6.
Government-Supported Health Care Interventions
Vida Saludable, Corazon Contento
The Vida Saludable, Corazon Contento guide is translated and adapted from the WISEWOMAN CVD prevention program for underserved and underinsured women ages 40 to 64 years. Funded by CDC, this program offers guidance to health care providers on screening for CVD risk factors, lifestyle counseling to improve diet and physical activity, and clinical referral and follow-up services. The program involves a three-session intervention that emphasizes readiness for change, goal-setting, individual tailoring, self-monitoring, and social support. Counseling is facilitated by bilingual community health workers. Although not designed to reach children and adolescents directly, the information and support provided to Spanish-speaking women potentially can assist in promoting healthy dietary and physical activity practices within their families. California currently is planning to pilot test the guide in five sites.
WIC Program
The WIC program serves 8 million women, infants, and children—almost half of the United States’ infants and a quarter of 1–5 year olds. In 2002, for the first time, Hispanics made up the largest group of WIC participants (38.1 percent) (Table C-7). In states with a high proportion of Latinos, the great majority of WIC participants are Latino. For example, in California, 70 percent of WIC participants are Latino. This high level of participation makes the WIC program a major point of contact for Latinos with health care professionals and an important potential source of counseling with regard to a healthful diet and physical activity. At the same time, the limitations of the WIC program are clear: the program provides only limited health counseling on an infrequent basis. Such minimal exposure and follow-up is unlikely to be adequate to substantially affect behaviors.
Privately Sponsored Healthcare Interventions
The Kidshape family lifestyle intervention is designed to promote healthful dietary and physical activity behaviors in 6–14-year-old overweight children and their parents. This clinical intervention has been implemented in various locations in southern California. The program is now being implemented in both English and Spanish in a clinic in northern California (Contra Costa County) as part of a larger community-based effort to prevent and treat childhood obesity in a population with a high proportion of Mexican Americans. The eight-week program is family oriented and requires that both parents and children attend all of the weekly sessions. It is reported that 87 percent of children lose weight and 80 percent maintain weight loss 1.5–2.5 years after finishing the program, but the Kidshape website does not provide the supporting data (Table C-7). While clearly needing evaluation, the Kidshape program is an example of the type of family-based clinical intervention that seems most promising.
Research and Monitoring
Research and monitoring activities are a critical part of the overall strategy to prevent child obesity. As noted above, there are intrinsic challenges in conducting evaluations of school-based and community intervention programs. Continuing and expanded research is needed to define best practices and demonstrate effectiveness. Ongoing monitoring of weight status and behavioral trends also is needed to gauge long-term progress in obesity prevention.
TABLE C-7 Government-Supported and Privately Sponsored Health Care Interventions
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Vida Saludable, Corazon Contento |
Women 40–64 years |
|
Contact: http://www.hpdp.unc.edu/wisewoman/vida.htm http://wwwtest.cdc.gov/wisewoman/project_locations/california.htm |
|
WIC Program |
Birth to 5 years |
|
Contact: http://www.fns.usda.gov/oane/MENU/Published/WIC/FILES/PC2002.htm |
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Kidshape |
6–14 years and parents |
|
Contact: http://www.cchealth.org/espanol/detalles_sobre_kidshape.html |
National-Level Survey and Monitoring Activities
At the national level in the United States, the ongoing Health and Nutrition Examination surveys, Behavioral Risk Factor Surveillance surveys, and Youth Risk Behavior surveys provide essential information on obesity prevalence and behavioral trends. However, data from these sources may not be specific or detailed enough to characterize and monitor the attitudes and behaviors of children and youth with regard to dietary and physical activity behaviors. To address this need, CDC has developed the Youth Media Campaign Longitudinal Survey (YMCLS), an annual national telephone survey of young people ages 9–13 years and their parents. The YMCLS is designed to measure the physical activity–related beliefs, attitudes, and behaviors of youth and their parents and to monitor youth exposure to the VERB social marketing campaign. Survey results provide information on the VERB campaign’s impact and guide the campaign’s evolution.
The surveys also provide a valuable research base that can aid in the design of other obesity prevention efforts. More specifically, focused interviews with Hispanic teens and parents documented a variety of cultural attitudes that may affect the adoption of healthful physical activity behaviors (Table C-8). For example, Hispanic youth are encouraged to put family needs above their own, and activity for personal benefit may be discouraged. Household chores and baby-sitting younger siblings after school while parents work were identified as barriers, especially for girls. Physical activ-
TABLE C-8 Research and Monitoring Activities
|
Program |
Target Group |
Program Description |
Evaluation and Contact Information |
|
Youth Media Campaign Longitudinal Survey |
9–13 years |
|
Contact: http://www.cdc.gov/youthcampaign/research/PDF/4.4.10-HisLatExSummaryRes.pdf |
|
Children’s Healthy Eating and Exercise Practices Survey |
9–11 years |
|
Contact: http://www.dhs.ca.gov/ps/cdic/cpns/research/calcheeps2003.html |
|
Teen Eating, Exercise, and Nutrition Survey |
12–17 years |
|
Contact: http://www.dhs.ca.gov/ps/cdic/cpns/research/calteens2000.html |
|
High School Fast Food Survey |
|
|
Contact: |
|
California Health Interview Survey |
1–18 years |
|
Contact: |
ity was considered as merely playing and a distraction, and no connection was seen between physical activity and health benefits. Parents were reluctant to involve their kids in programs that didn’t seem culturally relevant or that were not sanctioned by cultural authority figures they trust. These data indicate the very useful information obtainable by telephone surveys and supplemental interviews with Hispanic respondents.
State-Level Survey Activities
National data from the sources described previously often are inadequate to assess the status of state populations or specific subgroups that may vary substantially from overall national trends. State- and population-specific surveys frequently are needed to sufficiently assess obesity prevalence and the attitudes and behaviors related to obesity risk. Several California state-level surveillance and monitoring programs that may serve as useful examples are summarized in Table C-8. In particular, the California Health Interview Survey (CHIS)—conducted in English, Spanish, Chinese, Korean, and Vietnamese— is perhaps the nation’s most culturally inclusive survey. The CHIS has been used to report on several factors relating to childhood obesity, including dietary intakes, physical activity, and environmental issues contributing to obesity.
Online Formative Research
For Mexican–American parents and youth, having access to the Internet offers the potential to do online research that can reach thousands of respondents. Data provided online are already in electronic form and are ready to be tabulated and analyzed statistically. Respondents provide demographic information such as age, gender, place of residence, income, and education level for use in interpreting the information. Longitudinal followup is feasible via e-mail to assess response to an intervention. Research and monitoring using the Internet should be explored as a promising option for future development and evaluation of obesity prevention efforts.
THEORETICAL FRAMEWORK FOR INTERVENTION
Although interventions to treat obesity in children and adolescents who are already overweight can be successful, the process often requires intensive and sustained intervention, and long-term success is not assured. Moreover, Mexican–American children have limited access to health care and costs, and language and other barriers can be significant. These realities underscore the conclusion of the IOM report Preventing Obesity: Health in the Balance that the strategy to address childhood obesity must be to focus on primary prevention (IOM, 2005).
A recent series of meetings coordinated by the Berkeley Media Studies Group looked at ways to accelerate the development of effective policies to foster healthier nutrition and eating environments. The “acceleration” meetings reviewed the experience of other public health prevention efforts such as those addressing tobacco, alcohol, firearms, and traffic safety. The summary of these meetings suggested that based on the experience of these other public health efforts the path of least resistance for obesity prevention would be to focus on individual behavior change (Dorfman et al., 2005). This strategy puts the onus of responsibility on individuals to adopt healthful nutrition and physical activity habits. However, individual behavior change is unlikely to be successful unless positive behavioral changes are supported by the media, school, community, and health care environments in which individuals live.
The discussions at the acceleration meetings led to the conclusion that prevention efforts must shift focus from behavior to policy changes that affect the environments where behaviors take place. Although policy changes are more likely to meet more resistance than interventions that focus on individual behavior change, a policy change strategy offers the best opportunity to achieve effective and sustained prevention.
Behavioral Theory
The theoretical framework described in the IOM report Preventing Obesity: Health in the Balance used an ecological systems theory model that depicts the behavioral settings and leverage points that influence food intake and energy expenditure (IOM, 2005). The child or adolescent is seen as being at the center of concentric rings of influence from family, school, community, industry, and government, and the larger culture and society. Leverage points that influence behavior include the food system, opportunities for physical activity or sedentary behavior, and information regarding the health implications of dietary behaviors and physical activity. Behavioral choices within this ecological system also are seen as affected by social norms and values.
Another behavioral theory that has been used in conceptualizing strategies for obesity prevention is social learning theory. This theory emphasizes the importance of observing and modeling the behaviors, attitudes, and emotional reactions of others. In this model, developed principally by Bandura, most human behavior is learned through observation and modeling. The social learning theory model, later renamed by Bandura as social cognitive theory, was used in developing the multicomponent, school-based Bienestar intervention (Bandura, 1986; Trevino et al., 1998). According to this model, social systems in the individual’s environment, in addition to internal standards and self-evaluation, mediate the relationship between the
individual’s knowledge and his or her consequent behaviors. Because of the importance of social systems in the individual’s environment, the Bienestar program designed components that affected the child’s environment in the classroom, cafeteria, after-school, and home settings. Another intervention focusing on increasing fruit and vegetable consumption also used social learning theory by emphasizing changes in the home environment and parental support to achieve positive behavioral changes in 10–12-year-old children (Gribble et al., 2003).
The ecological systems model and the social cognitive theory model both appear to be valid constructs for the development of obesity prevention interventions, since both recognize the importance of environmental factors in influencing behaviors. However, an issue to be considered in using either model is whether Mexican–American families have the same level of empowerment as non-Hispanic families to make changes in schools and community environments. Mexican Americans may be more fatalistic about health or about their ability to make changes. Given these concerns, it is unclear that there currently exists a best practice model for obesity prevention in Mexican–American children. Further research is needed to clarify the kinds of intervention strategies that will work best in Hispanic communities.
Evidence-Based Approach
The IOM report describes the need for an evidence-based approach to the development of obesity prevention interventions by using multiple sources of evidence, including randomized controlled trials (if available), quasi-experimental, and observational studies. It is critical to systematically evaluate the effectiveness of intervention efforts, while at the same time to recognize the practical realities and the fiscal and socio-political environments in which programs are implemented. Because of these constraints, research has evaluated only a limited number of interventions relevant to obesity prevention in Mexican–American children. Additional research is needed to define best practice models in media, school, community, and health care settings. Attention should be focused on the development and testing of community empowerment models and on interventions that draw on and incorporate values and beliefs stemming from Mexican culture, music, art, and literature.
RECOMMENDATIONS FOR ACTION
Overall goals for obesity prevention in Mexican–American children parallel those for all children and youth as expressed in IOM’s Preventing Obesity, Health in the Balance. In the long term, the overriding goals are to
achieve a reduction in the incidence and prevalence of obesity; improve dietary patterns to be consistent with dietary guidelines; meet physical activity guidelines; and achieve physical, psychological, and cognitive growth and development goals. However, more specific intermediate goals and recommendations that address the specific needs of Mexican–American children and youth must be defined.
Achieving policy, environmental, and behavioral goals for obesity prevention for Mexican–American children and youth will require interventions at many levels, including television, print, and electronic media; schools; communities; and health care settings. To be successful, these efforts must be supported by ongoing research and monitoring and by effective advocacy.
Some key issues to be addressed include the following: (a) the need for comprehensive, multifaceted interventions that can address dietary and physical activity behaviors; (b) greater insight into the feasibility of scaling up interventions to programs in large populations groups; and (c) an increased understanding of ways to sustain interventions after initial start-up funds are no longer available. Outlined below are a variety of potential actions that might be recommended and prioritized based on the discussions in the workshop.
Media-Based Interventions
Media-based interventions are appealing because of their potential to reach large target audiences and for their low cost. Given the high level of access that Mexican–American families have to television and radio as well as the growing access they have to the Internet, especially by older children and youth, these media channels are an increasingly important means of providing information and motivation for healthy lifestyle choices. Another appealing feature of media-based interventions is the ability of electronic content to be shared internationally, in particular between Mexico and the Mexican–American populations in the United States. At the same time, food and beverage advertising through the same media can promote consumption of high-calorie and low-nutrient food and beverages and can negatively influence dietary and physical activity behaviors, thus increasing the risk of obesity. Specific actions that support expanding the potential and reducing the negative impact of media-based messages are cited in the following list.
Health Information in Television, Radio, and Print Media
-
Establish policies and guidelines that define appropriate marketing of foods and beverages to children and youth in general and specifically to Mexican–American children and youth.
-
Increase the number of new industry products and advertising messages that promote energy balance at a healthy weight and are targeted to Mexican–American consumers.
Internet-Based Health Promotion Resources
-
Develop culturally appropriate Web content that specifically targets Mexican–American children, youth, and parents.
-
Develop Web content in Spanish, or adapt it from existing English language websites, to provide accurate and appealing health information and to offer tips and guidance in choosing healthy lifestyles.
School-Based Interventions
School environments provide an important influence on children’s behaviors and can foster healthful nutrition and physical activity or negatively influence these behaviors. Many of the interventions currently being implemented and evaluated are carried out in the school setting. Some key strategies for fostering health-promoting school environments include the following:
-
Provide training for and support development of school wellness policies that promote healthful school nutrition and physical activity environments.
-
Implement school food service and vending policies that encourage healthful dietary choices.
-
Support the development and dissemination of language and culturally appropriate health education materials for Mexican–American children and youth.
-
Support research to develop and evaluate school-based interventions that are sustainable and effective in promoting increased participation in healthful physical activity.
Community-Based Interventions
Community-based youth programs and policies that create environments where children, youth, and families can share physical activity are critical components of an obesity prevention strategy.
-
Support expansion of community-based youth programs that serve Mexican–American children and youth.
-
In neighborhoods with a high proportion of Hispanic families, support policies such as the expansion of park facilities, sidewalks, and bike paths that encourage safe physical activity.
-
Provide training opportunities and materials to youth program staff to enhance their effectiveness.
-
Give recognition for achievements in developing successful community-based programs that serve Mexican–American populations.
-
Improve access to and affordability of fruits and vegetables for low-income Mexican–American populations.
-
Encourage participation by Mexican–American families in federal food assistance programs that increase access to healthful foods.
-
Implement policies that promote neighborhood safety, improved air quality, public transportation, and design conducive to healthy activity.
Health Care Interventions
Although many Mexican–American families lack adequate access, health care providers remain an important and trusted source of information and guidance. The impact of health care in motivating positive nutrition and physical activity behaviors can be enhanced by the following actions:
-
Develop guidelines outlining best practices for health care providers to assist in counseling Mexican–American youth and families regarding healthful dietary and physical activity habits. Anticipatory guidance by health care providers should begin early and include information on maternal nutrition, breastfeeding, infant nutrition, and healthful diet and physical activity for children, youth, and families.
-
Provide health promotion materials and information that is adapted to Hispanic language and culture.
-
Encourage the development and evaluation of training courses and materials for health care professionals in the assessment and behavioral management of child obesity, particularly when caring for Mexican– American children and adolescents.
-
Encourage collaboration between medical, public health, and school services to provide consistent and thus reinforcing health promotion messages and support for populations of Mexican–American children who are at high risk for childhood obesity, independent of insurance status or ability to pay.
Research and Monitoring
Expanded research and evaluation efforts are needed to provide the scientific underpinnings for obesity prevention efforts. Priority areas for research and opportunities for Mexico–U.S. collaborations are outlined below.
-
Establish policies to support behavioral research that can assess the impact of television, radio, Internet, and print media messages on eating habits and physical activity in Mexican–American children and youth.
-
Conduct research on the use of the Internet by Hispanic families and children, especially when they are seeking health-related information. Segment by age, gender, income, education, and location.
-
Conduct research on the effectiveness of Web-based health promotion directed at Mexican–American children and youth.
-
Support research on the effectiveness of school-based interventions for obesity prevention, particularly relating to the impact on Mexican– American children and youth.
-
Conduct research on the availability, use, and effectiveness of community-based health promotion activities for improving dietary choices and physical activity in Hispanic, especially Mexican–American, children and youth.
-
Support research to better understand the attitudes and perceptions of Mexican Americans about the health consequences of obesity and the link between obesity and dietary and physical activity habits.
-
Support continued monitoring of obesity prevalence and related risk factors at the national level, particularly in high-risk populations such as Mexican Americans.
-
Support and expand state and local surveys that provide insight into obesity status, attitudes, and dietary and physical activity behaviors, especially in populations at increased risk.
-
Facilitate interdisciplinary research between medicine, public health, architecture, planning, food production economics, and communication to explore the ecological model of childhood obesity, particularly relying on scholars from ethnic study centers.
Mexico–U.S. Collaboration
Achievement of goals for intervention, monitoring, and research of child and adolescent obesity will be assisted greatly by establishing a framework in which Mexican and United States’ researchers, public health professionals, and policy makers can readily exchange ideas and information and can collaborate in future research and intervention efforts. Below are some specific steps that might be considered to foster such collaboration.
-
Establish an ongoing mechanism for binational coordination to facilitate periodic meetings, e-mail newsletters, and other means of communication between Mexican and U.S. intervention program directors and researchers to exchange information on obesity prevention activities and research findings and to foster collaboration.
-
Establish a Mexico–United States scientific exchange program that provides opportunities for researchers in obesity prevention to share ideas and undertake joint research.
-
Identify specific intervention strategies that could be implemented and evaluated in both countries, such as
-
Use of a standardized health report card for tracking weight status and risk factors for obesity in children and youth,
-
Use of waist circumference as a screening tool to identify children and youth at risk,
-
Use of Internet-based resources (such as “todoenobesidad”) to provide health information and guidance, and
-
Effectiveness of multicomponent school-based interventions to reduce behavioral and physiological risk factors, such as the Bienestar program.
-
-
Develop a common framework for evaluating intervention effectiveness and provide opportunities, such as joint workshops, to review and learn from the experiences in each country.
-
Provide awards that recognize significant research and programmatic accomplishments in obesity prevention relating to Mexican and Mexican– American children and youth.
-
Provide training grants and fellowship support to encourage young researchers to enter the field of obesity prevention.
-
Establish a Mexico–U.S. practice exchange that provides opportunities for public health, community organizations, advocates, policy makers, and others to share best practices, models, tools, and other information.
-
Share and disseminate information on success stories in obesity prevention in both countries.
Advocacy
Learning from the experiences of other public health efforts, it is clear that success in obesity prevention will depend on the fostering of effective advocacy at many levels. As outlined in the Accelerating Policy on Nutrition report, the success of advocacy efforts will depend especially on accomplishing the following key objectives (Dorfman et al., 2005):
-
Establish clear policy goals.
-
Foster opportunities for dialog with a wide range of stakeholders to develop a common framework and terminology for describing the nature of the problem and the most effective means to achieve obesity prevention and to promote health.
-
Seek political opportunities to advance the policy goals.
-
Mobilize resources and invest in building infrastructure for advocacy, conducting research, and cultivating leadership.
REFERENCES
Action for Healthy Kids. 2005. Events, Programs, and Reports. [Online]. Available: http://www.actionforhealthykids.org [accessed April 15, 2006].
Agredano Y, Schetzina K, Mendoza F. 2004. Are immigrant Mexican–American children at greater risk for asthma? Pediatric Research 1326.
Andersen R, Crespo C, Bartlett S, Cheskin L, Pratt M. 1998. Relationship of physical activity and television watching with body weight and level of fatness among children. Journal of the American Medical Association 279(12):938–942.
Babey S, Diamant A, Brown R, Hastert T. 2005. California Adolescents Increasingly Inactive. Los Angeles, CA: UCLA Center for Health Policy Research.
Bandura A. 1977. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall.
Bandura A. 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall.
Basiotis P, Carlson A, Gerrior S, Juan W, Lino M. 2004. The Healthy Eating Index, 1999– 2000: Charting dietary patterns of Americans. Family Economics and Nutrition Review 16(1):39–48.
BLS (Bureau of Labor Statistics). 2004. Comparison of Labor Force Participation Rates and the Age of Composition of Hispanic and White non-Hispanic Men. Employment Projections. Washington, DC: U.S. Department of Labor.
Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. 2004. Effect of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics 113(1):112–118.
Broadie M, Kjellson N, Hoff T, Parker M. 1999. Perception of Latinos, African Americans, and Whites on media as a health information source. Howard Journal of Communication 10(3):147–167.
Burgos A, Schetzina K, Dixon B, Mendoza F. 2005. Importance of generational status in examining access to and utilization of health care services by Mexican–American children. Pediatrics 115(3):e322–e330.
CDC (Centers for Disease Control and Prevention). 2003. Prevalence of diabetes and impaired fasting glucose in adults—United States 1999–2000. Morbidity and Mortality Weekly Report 52(35):833–837.
CDC. 2004. Trends in intake of energy and macronutrients—United States, 1971–2000. Morbidity and Mortality Weekly Report 53(4):80–82.
CDC. 2005a. National Diabetes Fact Sheet. [Online]. Available: http://www.diabetes.org/uedocuments/NationalDiabetesFactSheetRev.pdf [accessed November 10, 2006].
CDC. 2005b. Prevalence of Overweight Among Children and Adolescents: United States 1999– 2002. [Online]. Available: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overwght99.htm. [accessed November 10, 2006].
CDC. 2005c. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: A report on recommendations of the Task Force on Community Preventive Services. Morbidity and Mortality Weekly Report 54(10):1–12. [Online]. Available: http://www.cdc.gov/MMWR/preview/mmwrhtml/rr5410a1.htm [accessed November 10, 2006].
CDC. 2006. Physical and Mental Health Characteristics of U.S. and Foreign-Born Adults: United States, 1998–2003. Advance Data from vital and health statistics No. 369. Hyattsville, MD: National Center for Health Statistics.
Chenoweth D. 2005. The Economic Cost of Physical Inactivity, Obesity, and Overweight in California Adults: Health Care, Workers Compensation, and Loss Productivity. New Bern, NC: Chenoweth and Associates, Inc.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. 2000. Establishing a standard definition for child overweight and obesity worldwide: International Survey. British Medical Journal 320(7244):1240–1243.
Cruz ML, Weigensberg MJ, Huang TT, Ball G, Shaibi GQ, Goran MI. 2004. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. Journal of Clinical Endocrinology and Metabolism 89(1):108–113.
Daniels SR, Khoury PR, Morrison JA. 1997. The utility of body mass index as a measure of body fatness in children and adolescents: Differences by race and gender. Pediatrics 99(6):804–807.
Datar A, Magnabosco JL. 2004. Childhood overweight and academic performance: National study of kindergartners and first-graders. Obesity Research 12(1):58–68.
Davidson KK, Birch LL. 2001. Weight status, parental reaction and self-concept in five-year-old girls. Pediatrics 107(1):46–53.
del Rio-Navarro BE, Velazquez-Monroy O, Sanchez-Castillo CP, Lara-Esqueda A, Berber A, Fanghanel G, Violante R, Tapia-Conyer R, James W. 2004. The high prevalence of overweight and obesity in Mexican children. Obesity Research 12(2):215–223.
DeNavas-Walt C, Proctor B, Lee C. 2005. Income, Poverty, and Health Insurance Coverage in the United States: 2004. U.S. Census Bureau. Washington, DC: U.S. Department of Commerce.
Dixon LB, Sundquist J, Winkleby M. 2000. Differences in energy, nutrient, and food intakes in a U.S. sample of Mexican American women and men: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Epidemiology 152(6):548–557.
Dorfman L, Wilbur P, Lingas EO, Woodruff K, Wallack L. 2005 Accelerating Policy on Nutrition: Lessons from Tobacco, Alcohol, Firearms, and Traffic Safety. Final report from a series of meetings conducted by the Berkeley Media Studies Group. Oakland, CA: Public Health Institute.
Duke J, Huhman M, Heitzler C. 2003. Physical activity levels among children aged 9–13 years—United States 2002. Morbidity and Mortality Weekly Report 52(33):785–788.
Endicott RC, Brown K, MacDonald S, Schumann M, Ryan M, Sierra J, Wentz L. 2005. Hispanic Pact Pack. Advertising Age (Supplement). Pp. 1–51. [Online]. Available: http://www.adage.com/images/random/hispfactpack05.pdf.
Fernandez JR, Redden DT, Pietrobelli A, Allison DB. 2004. Waist circumference percentiles in nationally representative samples of African American, European American, and Mexican American children and adolescents. Journal of Pediatrics 145(4):439–444.
Finkelstein EA, Fiebelkorn IC, Wang G. 2004. State-level estimates of annual medical expenditures attributable to obesity. Obesity Research 12(1):18–24.
Flores G, Abreu M, Olivar MA, Kastner B. 1998. Access barriers to health care for Latino children. Archives of Pediatrics and Adolescent Medicine 152(11):1119–1125.
Food and Nutrition Service. 2005. Making It Happen! School Nutrition Success Stories. Alexandria, VA: U.S. Department of Health and Human Services, U.S. Department of Agriculture, and U.S. Department of Education.
Ford ES, Mokdad AH, Ajani UA. 2004. Trends in risk factors for cardiovascular disease among children and adolescents in the United States. Pediatrics 114(6):1534–1544.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. 1999. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 103(6):1175–1182.
Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. 2001. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics 108(3):712–718.
Freedman DS, Khan LK, Serdula MK, Galuska DA, Dietz WH. 2002. Trends and correlates of class 3 obesity in the United States from 1990 through 2000. Journal of the American Medical Association 288(14):1758–1761.
GAO (U.S. Government Accountability Office). 2005. Childhood Obesity: Most Experts Identified Physical Activity and the Use of Best Practices as Key to Successful Programs. GAO-06-127R. Washington, DC: GAO.
Gribble LS, Falciglia G, Davis AM, Couch SC. 2003. A curriculum based on social learning theory emphasizing fruit exposure and positive parent child-feeding strategies: A pilot study. Journal of the American Dietetic Association 103(1):100–103.
Hammer L. 2005. Personal communication. Stanford, CA: Medical Director, Center for Health Weight.
Hannon TS, Rao G, Arslanian SA. 2005. Childhood obesity and type 2 diabetes mellitus. Pediatrics 116(2):473–480.
Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, Wilfley DE. 2005. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research 13(8):1381–1392.
Heath EM, Coleman KJ. 2002. Evaluation of the institutionalization of the Coordinated Approach to Child Health (CATCH) in a U.S./Mexico border community. Health Education and Behavior 29(4):444–460.
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Flegal KM. 2004. Prevalence of overweight and obesity among U.S. children, adolescents, and adults. Journal of the American Medical Association 91(23):2847–2850.
Hernandez D. 2004. Children of immigrant families: Demographic changes and the life circumstances of immigrant families. The Future of Children 14(2):17–47.
Huhman M, Potter LD, Wong FL, Banspach SW, Duke JC, Heitzler CD. 2005. Effects of a mass media campaign to increase physical activity among children: Year-1 results of the VERB campaign. Pediatrics 116(2):e277–e284.
International Life Sciences Institute. 2005. ILSI CHP Nutrition and Physical Activity Program List. [Online]. Available: http://chp.ilsi.org/Publications/CHPPhysicalActivityProgramList.htm [accessed April 15, 2006].
IOM (Institute of Medicine). 2005. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press.
IOM. 2006. Food Marketing to Children and Youth: Threat or Opportunity? Washington, DC: The National Academies Press.
Kahn HS, Imperatore G, Cheng YJ. 2005. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. Journal of Pediatrics 146(4):482–488.
Kaplan MS, Huguet N, Newsom JT, McFarland BH. 2004. The association between length of residence and obesity among Hispanic immigrants. American Journal of Preventive Medicine 27(4):323–326.
Kaplowitz H, Martorell R, Mendoza F. 1989. Fatness and fat distribution in Mexican American children and youth from the Hispanic Health and Nutrition Examination Survey. American Journal of Human Biology 1:631–648.
Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, Berenson GS. 2004. Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics 114:e198–e205.
Kissam E, Intili J, Garcia A. 2003. Spanish-Language community radio as a resource for health promotion campaigns targeted to farmworkers and recent immigrants. Californian Journal of Health Promotion 1(2):183–197.
Klaudt M, Schetzina K, Mendoza F, Robinson T. 2002. Racial/Ethnic Differences in Maternal Perception of Children’s Weight. Ambulatory Pediatric Association, Region IX and X, February 2002 Annual Meeting. Carmel, CA.
Kovacs P, Ma L, Hanson RL, Franks P, Stumvoll M, Bogardus C, Baier LJ. 2005. Genetic variation in UCP 2 (uncoupling protein 2) is associated with energy metabolism in Pima Indians. Diabetologia 48(11):2292–2295.
Kuczmarski RJ, Ogden CL, Guo SS. 2002. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Statistics 11:246.
Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. 2004. Childhood adiposity as a predictor of cardiac mass in adulthood: The Bogalusa Heart Study. Circulation 110(22):3488–3492.
López R, Barquera S, Hernandez Prado B, Rivera JR. 2006. Preventing Obesity in Mexican Children and Adolescents. U.S.–Mexico Workshop on Prevention of Childhood Obesity. Washington, DC: Institute of Medicine.
Malina R, Martorell R, Mendoza F. 1986. Growth status of Mexican American children and youth: Historical trends and contemporary issues. American Journal of Physical Anthropology 29(S7):45–79.
Martorell R, Mendoza FS, Castillo RO, Pawson IG, Budge CC. 1987. Short and plump physique of Mexican American children. American Journal of Physical Anthropology 73:475–478.
Martorell R, Malina RM, Castillo RO, Mendoza FS, Pawson IG. 1988a. Body proportions in three ethnic groups: Children and youths 2–17 years in NHANES II and HHANES. Human Biology 60(2):205–222.
Martorell R, Mendoza F, Castillo R. 1988b. Poverty and stature in children. In: Linear Growth Retardation in Less Developed Countries. Waterlow JC. Ed. New York: Raven Press 14:57–73.
Martorell R, Mendoza F, Castillo R. 1989. Genetic and environmental determinants of growth in Mexican Americans. Pediatrics 84(5):864–871.
Maynard MG, Blanck H, Serdula M. 2003. Maternal perception of weight status of children. Pediatrics 111:1226–1231.
Mazur RE, Marquis GS, Jensen HH. 2003. Diet and food insufficiency among Hispanic youth: Acculturation and socioeconomic factors in the third National Health and Nutrition Examination Survey. American Journal of Clinical Nutrition 78:1120–1127.
Mendoza F, Castillo R. 1986. Growth abnormalities in Mexican–American children in the United States: The NHANES I Study. Nutrition Research 6:1247–1257.
Morrison JA, Friedman LA, Harlan WR, Harlan LC, Barton BA, Schreiber GB, Klein DJ. 2005. Development of the metabolic syndrome in black and white adolescent girls: A longitudinal assessment. Pediatrics 116(5):1178–1182.
Murphy S, Castillo R, Martorell R, Mendoza F. 1990. An evaluaiton of the food group intakes by Mexican American children. Journal of the American Dietetic Association 90(3): 388–393.
Nader MD, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, Webber LS, Elder JP, Montgomery D, Feldman HA, Wu M, Johnson C, Parcel GS, Luepker RV. 1999. Three-year maintenance of improved diet and physical activity. Archives of Pediatrics and Adolescent Medicine 153(7):695–704.
Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. 2003. Lifetime risk for diabetes mellitus in the United States. Journal of the American Medical Association 290(14):1884–1890.
NCHS (National Center for Health Statistics). 2004. Health, United States, 2004, with Chartbook on Trends in the Health of Americans. Hyattsville, MD: NCHS.
Neufeld ND, Raffel LJ, Landon C, Chen YD, Vadheim C. 1998. Early presentation of type 2 diabetes in Mexican American youth. Diabetes Care 21(1):80–86.
Neuhouser ML, Thompson B, Coronado GD, Solomon CC. 2004. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. Journal of the American Dietetic Association 104(1):51–57.
NRC/IOM (National Research Council/Institute of Medicine). 1998. From Generation to Generation: The Health and Well-Being of Children in Immigrant Families. Washington, DC: National Academy Press.
NRC/IOM. 1999. Children of Immigrants: Health, Adjustment, and Public Assistance. Washington, DC: National Academy Press. Pp. 187–243.
Ogden CL, Flegal KM, Carroll MD, Johnson CL. 2002. Prevalence and trends in overweight among United States children and adolescents, 1999–2000. Journal of the American Medical Association 288(14):1728–1732.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. 2006. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association 288295(13):1549–1555.
Olaiz G, Rojas R, Barquera S, Shamah T, Aguilar C, Cravioto P, López P, Hernández M, Tapia R, Sepúlveda J. 2003. Encuesta Nacional de Salud 2000. Tomo 2. La salud de los adultos. Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública.
Pelayo R. 2005. Personal communication. Palo Alto, CA: Stanford Sleep Center.
Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. 1998. Body mass index as a measure of adiposity among children and adolescents: A validation study. Journal of Pediatrics 132(2):204–210.
Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. 1996. Increased incidence of non-insulin dependent diabetes mellitus among adolescents. Journal of Pediatrics 128:608–615.
Popkin B, Udry JR. 1998. Adolescent obesity increases significantly in second and third generation U.S. immigrants: The national longitudinal study of adolescent health. Journal of Nutrition 128:701–706.
Reaven P, Nader PR, Berry C, Hoy T. 1998. Cardiovascular disease insulin risk in Mexican– American and Anglo-American children and mothers. Pediatrics 101(4):1–7.
Rivera J, Shamah Levy T, Villalpando Hernández S, González de Cossío T, Hernández Prado B, Sepúlveda J. 2001. Encuesta Nacional de Nutrición 1999. Estado nutricio de niños y mujeres en México. Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública.
Rivera JA, Barquera S, Campirano F, Campos I, Safdie M, Tovar V. 2002. Epidemiological and nutritional transition in Mexico: Rapid increase of non-communicable chronic diseases and obesity. Public Health Nutrition 5(1A):113–122.
Roberts DF, Foehr UG, Rideout V. 2005. Generation M: Media in the Lives of 8–18 Year Olds. KFF. [Online]. Available: http://www.kff.org/entmedia/upload/Generation-M-Media-in-the-Lives-of-8-18-Year-olds-Report.pdf [accessed April 15, 2006].
Romero A, Robinson T, Haydel K, Mendoza F, Killen J. 2004. Association among familism, language preference, and education in Mexican American mothers and their children. Journal of Developmental and Behavioral Pediatrics 25(1):34–40.
Ryan AS, Roche AF, Kuczmarski RJ. 1999. Weight, stature, and body mass index data for Mexican Americans from the third national health and nutrition examination survey. American Journal of Human Biology 11:673–686.
Salsberry PJ, Reagan PB. 2005. Dynamics of early childhood overweight. Pediatrics 116(6):1329.
Sanchez-Castillo CP, Lara JJ, Villa AR, Aguirre J, Escobar M, Gutierrez H, Chavez A, James WP. 2005. Unusually high prevalence rates of obesity in four Mexican rural communities. Public Health Nutrition 8(1):53–60.
Schwimmer JB, Burwinkle TM, Varni J. 2003. Health-related quality of life of severely obese children and adolescents. Journal of the American Medical Association 289(14):1813– 1819.
Shaping America’s Youth. 2004. Shaping America’s Youth. [Online]. Available: http://www.shapingamericasyouth.org/Programs.aspx?page=search [accessed April 15, 2006].
Siegel JM, Yancey AK, Aneshensel CS, Schuler R. 1999. Body image, perceived pubertal timing and adolescent mental health. Journal of Adolescent Health 25(2):155–165.
Spooner T, Rainie L. 2001. Hispanics and the Internet. Pew Internet and American Life Project. [Online]. Available: http://www.pewinternet.org/PPF/r/38/report_display.asp [accessed April 15, 2006].
Srinivasan SR, Myers L, Berenson GS. 2002. Predictability of childhood adiposity and insulin for developing Insulin Resistance Syndrome (Syndrome X) in young adulthood: The Bogalusa Heart Study. Diabetes 51:204–209.
Strauss RS, Pollack HA. 2001. Epidemic increase in childhood overweight, 1986–1998. Journal of the American Medical Association 286(22):2845.
Strohl KP, Redline S. 1996. Recongition of obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine 154:279–289.
Thorpe KE, Florence CS, Howard DH, Joski P. 2004. The impact of obesity on rising medical spending. Health Affairs. Web Exclusive. October 20:W4-480 to W4-486.
Trevino RP, Hernandez A, Hale DE, Garcia OA, Mobley C. 2005. Impact of the Bienestar school-based diabetes mellitus prevention program on fasting capillary glucose levels: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine 158(9): 911–917.
Trevino RP, Pugh JA, Hernandez AE, Menchaca VD, Ramirez RR, Mendoza M. 1998. Bienestar: A diabetes risk-factor prevention program. Journal of School Health 68(2): 62–67.
USPSTF (U.S. Preventive Service Task Force). 2002. Physical Activity Counseling. [Online]. Available: http://www.ahrq.gov/clinic/uspstf/uspsphys.htm [accessed April 15, 2006].
USPSTF. 2003. Healthy Diet Counseling. [Online]. Available: http://www.ahrq.gov/clinic/uspstf/uspsdiet.htm [accessed April 15, 2006].
Velez-Subervi F. 1999. Spanish-language television coverage of health news. Howard Journal of Communications 10(3):207–228.
Wang G, Dietz WH. 2002. Economic burden of obesity in youths aged 6–17 years. Pediatrics 109(5):e81–e87.
Whitaker RC. 2004. Predicting preschooler obesity at birth: The role of maternal obesity in early pregnancy. Pediatrics 114(1):e29.
Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. 2005. Screening and interventions for childhood overweight: A summary of evidence for the U.S. Preventive Services Task Force. Pediatrics 116(1):e125–e144.
Williams DE, Cadwell BL, Cheng YJ, Cowie CC, Gregg EW, Geiss LS, Engelgau MM, Narayan KM, Imperatore G. 2005. Prevalence of impaired fasting glucose and its relationship with cardiovascular disease risk factors in U.S. adolescents, 1999–2000. Pediatrics 116(5):1122–1126.
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L, Tanomsup S, Wangai P Jr, Razak F, Sharma AM, Anand SS, INTERHEART Study Investigators. 2005. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet 366(9497):1640– 1649.