B
Preventing Obesity in Mexican Children and Adolescents
Ruy López Ridaura, Research Center for Population Health: Chronic Disease Division, Instituto Nacional de Salud Pública (National Institute of Health, INSP)
Simón Barquera, Research Center for Nutrition and Health, INSP
Bernardo Hernández Prado, Research Center for Population Health: Reproductive Health Division, INSP
Juan Rivera, Research Center for Nutrition and Health, INSP
INTRODUCTION
Mexico is among many countries that have experienced a rapid increase over the past two decades in the proportion of children and adolescents with excessive weight. In the decade between the First (1988) and Second (1999) National Nutrition Surveys, there was an increase in the prevalence of Mexican children ages 2–4 years who were either obese or at risk for obesity,1 rising from 21.9 percent to 28.7 percent. This is the only age group in children for which national trend data are available. For older Mexican children, the lack of national trend data limits the evaluation of obesity trends during that decade. However, data from the Second National Nutrition Survey show equally alarming evidence of a growing obesity epidemic in children and youth. Based on the age- and gender-specific body mass index (BMI) charts developed by the Centers for Disease Control and Prevention (CDC) in 2000 (Kuczmarski et al., 2000), 21.1 percent of Mexican children ages 6–11 years have a BMI equal to or greater than the 85th percentile and are considered to be obese (8.8 percent) or at risk for obesity (12.3 percent). Among girls ages 12–19 years, 22.3 percent have a BMI
equal to or greater than the 85th percentile and are either obese (5.7 percent) or at risk for obesity (16.6 percent).
These data reflect an evolving obesity epidemic, representing an enormous burden for the public health and health care systems in Mexico. The association between childhood obesity and many health risks, in both children and adults, has been consistently found. The major public health impact is the association of childhood obesity with chronic disease risks in adulthood, especially overweight and obesity, type 2 diabetes, hypertension, asthma, hyperlipidemia, cardiovascular diseases (CVD), and certain cancers. Excessive weight at younger ages has also been associated with adverse psychosocial outcomes such as low self-esteem, depression, anxiety, and impaired cognitive function, especially in adolescents, although findings have not always been consistent (Swallen et al., 2005). However, research is currently not available to demonstrate this association in Mexican children and youth.
Nutrition-related chronic diseases represent a serious public health problem for the Mexican population. According to the Organization for Economic Cooperation and Development (OECD) 2005 Health Report, one quarter (24.2 percent) of the Mexican adult population is classified as obese (OECD, 2005). Data from the most recent National Health Survey (2000) showed that nearly 8 percent of all Mexican adults over 20 years of age have type 2 diabetes and approximately 30 percent have hypertension (Olaiz et al., 2003). Moreover, type 2 diabetes and CVD are the leading causes of death in the adult Mexican population, and some small studies suggest an increasing incidence of type 2 diabetes and glucose intolerance at younger ages (Cruz et al., 2004; Rodríguez-Moran et al., 2004).
Although there has not been a comprehensive evaluation of the economic impact of obesity in Mexico, a recent analysis estimated an attributable cost of diabetes for the public health sector of approximately $317 million U.S. dollars for the year 2005, almost equally distributed between direct and indirect costs (Arredondo and Zuñiga, 2004). The increasing incidence of obesity at younger ages and the scarce public resources in the country will considerably aggravate these economic projections.
As in many developing countries, the Mexican population is in the process of an epidemiologic transition and is experiencing a double disease burden. Child mortality rates and the incidence of infectious diseases have decreased. However, statistics show a significant increase in obesity and related chronic diseases such as diabetes, hypertension, and CVD in adults. High rates of malnutrition and related problems are still observed, especially among sub-populations of Mexican children. This paradoxical situation is the result of multiple factors, partly attributed to the uneven development among different segments of the population and increased socioeconomic inequalities (Uauy et al., 2001). A closely related phenom-
enon that the Mexican population has experienced over the past few decades is a nutritional transition, that is a shift in the overall structure of dietary patterns and a reduction in energy expenditure. This transition is affecting most of the population, and has been proposed that it is the main driving force of the obesity epidemic and related chronic conditions in developing countries (Popkin, 2001).
Given the concern over the growing prevalence of obesity and its impact, the U.S. Congress directed the CDC in 2002 to request that the Institute of Medicine (IOM) develop an action plan targeted to prevent obesity in U.S. children and youth. The IOM convened a multidisciplinary committee to develop a prevention-focused action plan. In 2004, the committee released the report Preventing Childhood Obesity: Health in the Balance (IOM, 2005), which proposed a set of recommendations for a variety of sectors and stakeholders that, when implemented together, would catalyze synergistic actions to effectively prevent the large majority of children and youth in the United States from becoming obese and facilitate the adoption of healthier lifestyles. By making childhood obesity a national priority, this set of recommendations calls on coordinated actions among the government, industry, media, community organizations, schools, and families that together will develop a broad-based public health strategy needed to effectively halt and decrease this growing epidemic (IOM, 2005).
Are these recommendations applicable to Mexican–American and Mexican children and youth? Are these recommendations applicable to the particular public health challenges faced by Mexico? Is there any benefit to developing a common binational obesity prevention agenda or strategy? These are the main questions that stimulated the IOM to sponsor a joint U.S.–Mexico workshop—in collaboration with the National Institute of Public Health in Mexico (INSP) and supported by Kaiser Permanente—that will focus on exploring a binational approach to obesity prevention and the adaptation of the IOM report recommendations to Mexican children and youth living in the United States and in Mexico. The purpose of this paper is to review the factors that contribute to obesity in Mexican children and adolescents, provide an overview of current programs addressing this problem, and propose a set of actions that may offer the greatest potential for success in preventing and controlling the epidemic. A companion paper, authored by U.S. colleagues, will address obesity trends and determinants in Mexican–American children and youth (Trowbridge and Mendoza, 2007) and provide a complementary view to the issues presented in this paper.
Based on an ecologic perspective, several components and their degrees of influence are context specific. For instance, the acceptance and understanding of “healthy behavior” recommendations are linked closely to cultural values that could be specific for each ethnic group. Also, given that
most of the recommendations imply actions at different normative levels, there are substantial differences in the legal, economic, and political contexts that need to be considered carefully in the use of the IOM report model to develop recommendations for Mexican children and youth living on both sides of the U.S.–Mexico border.
Approaching obesity prevention among Mexican children and youth as a binational problem could have many advantages. Given the strong link between the population in Mexico and the one that has migrated to the United States, common cultural perceptions and values can be explored as a combined effort to design culturally acceptable recommendations and to define research priorities. Moreover, the permanent relationship, including remittances and transfer of commodities between U.S. migrant workers and their families, might allow the development of coordinated strategies that could impact not only the population living at the border (characterized by a high mobilization across countries) but also the population living in the remote areas (especially the rural areas) of Mexico, where most migrants trace their family roots. Finally, the obesity burden, on one hand, and the evidence of effective programs in the United States, on the other, can potentially improve advocacy efforts in Mexico and vice versa. Therefore, if coordination between countries can be fostered, progress toward effective preventive interventions will be accelerated with benefits and impacts on both sides of the U.S.–Mexico border.
DEFINING THE PROBLEM
Definition and Measurement of Obesity
BMI, which is calculated by dividing weight in kilograms by height in squared meters (kg/m2), is a useful indirect measurement of body fat and unhealthy weight in children ages 2 years and older and adults. It is often used as a screening tool to identify individuals who are obese and those at risk for obesity because the measurements of height and weight are easily obtained compared with skinfold thickness measurements and other complex procedures that require more training and standardization. BMI is one of the best indicators of body fat, which is proposed as the cause component of the health consequences associated with obesity (Mei et al., 2002). Indeed, BMI has been associated consistently with several risk factors, even among children and adolescents. Preliminary results of the association between BMI and chronic disease risk factors among Mexican adolescents based on the National Health Survey (2000) are consistent with analyses from other countries in which CVD risk factors show a dose–response relationship with BMI categories, whereby the normal-weight category shows the lowest risk profile and the obesity category shows the highest risk pro-
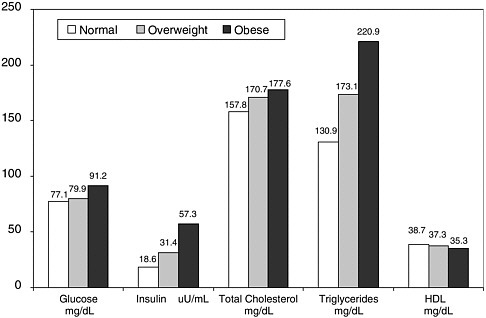
FIGURE B-1 BMI categories and their association to CVD risk factors in children and adolescents ages 10–19 years, from the Mexican Health Survey (2000).
SOURCE: Villalpando et al. (in press).
file (Villalpando et al., in press) (Figure B-1). BMI has certain disadvantages. It has been suggested that other indicators, such as waist circumference, waist-to-hip ratio, or skinfold thickness measurements, could have a stronger association with metabolic abnormalities. However, these measurements are not usually obtained for children and youth in health clinics and school systems as readily as weight and height, and are usually not known by parents; thus, BMI is the measurement most commonly used.
Although there may be a need to develop ethnic-specific definitions for overweight and obesity, the cut-off points used to define overweight (a BMI between 25 and 29.9 kg/m2) and obesity (a BMI equal to or greater that 30 kg/m2) for adults are widely accepted. However, given that BMI changes with children’s growth and development, it is more appropriate to use age-and gender-specific BMI charts to define obesity and at risk for obesity in children and adolescents. For consistency with the IOM report Preventing Childhood Obesity: Health in the Balance (IOM, 2005) and with the companion paper examining the factors contributing to obesity in Mexican– American children and youth, this paper uses the CDC BMI charts established in 2000 to define obesity and being at-risk for obesity for children
and adolescents between the ages of 2–19 years. According to this reference, children and adolescents with a BMI equal to or greater than the 95th percentile are considered obese, and those with a BMI between the 85th and 95th percentiles are considered to be at risk for obesity (IOM, 2005; Kuczmarski et al., 2000). In the absence of a reference population or cut-off points specific for the Mexican population, the authors conclude that the CDC BMI charts are the best available for children and adolescents 2–19 years. In the future, the recently released WHO Child Growth Standards, developed using data collected by the World Health Organization (WHO) Multicentre Growth Reference Study that provide new guidelines for assessing obesity in children ages 0–5 years (WHO, 2006a) could also be used for that age range.
Obesity Prevalence and Trends in Children and Youth in Mexico
The only national survey that included anthropometric measurements of school-aged children was the Second National Nutrition Survey (Rivera et al., 2001), conducted by the National Institute of Public Health of Mexico between October 1998 and March 1999. The Third National Nutrition Survey 2006 is currently in progress and will provide further data on obesity trends in children, youth, and adults throughout the entire country.
The results of the Second National Nutrition Survey were based on a national probabilistic sample of 17,944 households. The sampling methodology and response rates are described in detail elsewhere (Resano-Pérez et al., 2003). The resulting sample is representative at the national level of urban (≥ 2,500 people) and rural (< 2,500 people) sites and of four geographic regions: north (the wealthiest region), south (the poorest region), Mexico City [a large urban center with the greatest socioeconomic status (SES) contrasts], and central (including states that are generally between the north and the south with respect to SES). The study population included children younger than 5 years of age (n = 8,011), school-aged children ages 5–11 years (n = 11,415), and women ages 12–49 years (n = 18,311). The sample represented about 10.6 million children 4 years of age or younger and 15.6 million children ages 5–11 years. In addition to these age ranges, which were employed in the First and Second Mexican National Nutrition Survey and are used in previous publications, for consistency with the IOM report (IOM, 2005) and the companion paper on Mexican–American children, we computed prevalences for the following age ranges (Table B-1): 0–23 months, 2–5 years, 6–11 years, and 12–19 years. However, some of the results presented in this document use the age ranges employed by the National Nutrition Surveys because we obtained them from published material.
The national prevalence of children at risk for obesity and obese by age, geographic region, and sociodemographic characteristics derived from the National Nutrition Survey 1999 are illustrated in Table B-1. In infants younger than 2 years, the national prevalence of children at risk for obesity [defined as the percent > +2 SD of the WHO/National Center for Health Statistics (NCHS)/CDC reference population] is 5.84 percent. For children ages 2–5 years, the prevalence of obesity (BMI ≥ 95th percentile of the age-and gender-specific CDC BMI charts) was 10.4 percent, and the prevalence of children at risk for obesity (BMI between the 85th and 95th percentile of the CDC BMI charts) was 17.1 percent for a total of 27.5 percent of children in this age category who are either at risk or obese. Both groups present higher prevalence in the north compared with the other regions, and for 2– 5-year-olds, the prevalence was higher in urban versus rural areas and in high versus low SES strata.
The only age category for which there are available data from two national surveys (1988 and 1999), allowing for an evaluation of obesity trends, is children younger than 5 years of age. Figure B-2 shows the trend in the proportion of children ages 2–4 years that were over the 85th percentile of the reference population. An increase was evident at the national level (31 percent, from 21.9 percent to 28.7 percent) and in each of the four regions represented in the survey; this increase was especially notable in the north (with the highest SES), which showed an estimated increase over 50 percent (from 20.8 percent to 31.8 percent) in the prevalence of obesity or at risk for obesity (> 85th percentile) over the 11-year period. This increment was mainly driven by the proportion of children who were at risk for obesity rather than the obesity category.
Among Mexican children ages 6–11 years, 8.8 percent were classified as obese (> 95th percentile) and 12.3 percent were classified as at risk for obesity (> 85th percentile) at the national level. The magnitude of the regional prevalence followed the children’s SES status. The highest prevalence of obesity was found in the north (12.7 percent), followed by Mexico City (11.4 percent), the central region (8.8 percent), and the south (5.5 percent). The prevalence was higher in those living in urban (11 percent) versus rural areas (3.4 percent), in children whose mothers had a higher level of formal education (e.g., more than high school = 13.2 percent, high school = 11.8 percent, primary school = 7.5 percent, without formal education = 4.8 percent), and in the non-indigenous population (9.4 percent versus 3.4 percent). The prevalence of children at risk of obesity was higher than for the obesity category following the same pattern. The relatively larger prevalence of unhealthy weight in wealthier subpopulations is in contrast with the very small differences in prevalence of unhealthy weight found among the same subpopulations for adult women (Rivera et al., 2002).
TABLE B-1 Prevalence of Children at Risk for Obesity and Obese by Age and Selected Geographic and SocioDemographic Characteristics
|
|
0–23 months |
2–5 years |
6–11 years |
12–19 years |
|||
|
Age category |
Wt-for-ht (WHO) |
Age- and gender-specific BMI charts (Kuczmarski et al., 2000) |
|||||
|
Indicator |
|
At Risk |
Obese |
At Risk |
Obese |
At Risk |
Obese |
|
Cut-off points |
> +2 SD |
85–95 |
> 95 |
85–95 |
> 95 |
85–95 |
> 95 |
|
National |
5.84 |
17.1 |
10.4 |
12.3 |
8.8 |
16.6 |
5.7 |
|
Region |
|
|
|
|
|
|
|
|
North |
7.1 |
19.5 |
12 |
15.5 |
12.7 |
18.3 |
10.1 |
|
Center |
4.6 |
17.7 |
9 |
11.6 |
8.8 |
17.4 |
7 |
|
Mexico City |
5.7 |
13.6 |
9.7 |
15.5 |
11.4 |
20.7 |
3.8 |
|
South |
6.3 |
16.7 |
11.3 |
9.6 |
5.5 |
13.4 |
3.2 |
|
Location |
|
|
|
|
|
|
|
|
Rural |
5.6 |
17.1 |
10.8 |
8.6 |
3.4 |
12.8 |
4.2 |
|
Urban |
6.4 |
17.2 |
9.8 |
13.9 |
11 |
18.2 |
6.3 |
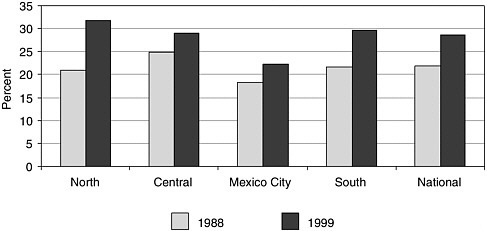
FIGURE B-2 Prevalence of risk of obesity or at risk for obesity by region and year of survey (children ages 2–4 years).
SOURCE: Rivera et al. (2001).
Undernutrition and Catch-Up Growth in Children and Youth in Mexico
The coexistence of under- and overnutrition is a characteristic of the Mexican population, particularly among children and young women. Along with the high prevalence of unhealthy weight in children, the prevalence of stunting ,2 anemia, and micronutrient deficiencies remain public health concerns. Stunting continues to be an important public health problem in children younger than 5 years of age while wasting3 is no longer a widespread problem, decreasing from a national prevalence of 6 percent in 1988 to a prevalence of 2 percent in 1999. At the national level, stunting occurred in almost one of every five children younger than 5 years of age (17.7 percent) while wasting occurred in only 2 percent. The mean height-for-age z-score in this age group was −0.8 ± 1.3 while the mean weight-for-height z-score was +0.2 ± 1.1. Stunting occurs predominantly during the first two years of life. The prevalence increases almost threefold between the first and the second years of life (from about 8 percent to 22 percent) and remains at about 20 percent up to 4 years of age. From 5–11 years, the percent of
stunting in children was 16.1 percent, which is mainly the result of stunting during early childhood. The long-term effects of stunting on height are evident in the adult population. On average, Mexican adult women are short (e.g., the mean height of women 12–49 years of age is 152.9 cm).
Anemia and micronutrient deficiencies are widespread in most age groups (Villalpando et al., 2003a, b, c). More than one in every four children younger than 5 years (27.2 percent) are anemic, and between one-quarter to one-half have one or more micronutrient deficiencies. The prevalence of iron, zinc, and vitamin A deficiencies are at approximately 52 percent, 33 percent, and 27 percent, respectively. Additionally, more than 25 percent of children have serum ascorbic acid concentrations indicative of low dietary intake of vitamin C. Some micronutrient deficiencies occur predominantly at younger ages. Anemia rates peak in the second year of life, when almost half of all children are affected, but decrease to about 17 percent prevalence at 4 years of age. Iron deficiency affects about two-thirds of all children between 1 and 2 years of age and less than 50 percent between 3 and 4 years of age.
The prevalence of anemia in children ages 5–11 years was 19.5 percent; it was slightly higher in rural (21.9 percent) than urban (18.3 percent) areas, higher in indigenous (24 percent) than non-indigenous (18 percent) children, and much lower in Mexico City (11 percent) than in other regions (18 percent to 24 percent). The micronutrient with the highest deficiency prevalence was iron (36 percent), followed by vitamin C (30 percent), vitamin A and zinc (about 20 percent), and folic acid (about 10 percent). Urban areas had a much lower prevalence of iron and zinc deficiencies (38.2 percent and 18.2 percent, respectively) than rural areas (48.3 percent and 40 percent, respectively) (Rivera and Sepúlveda-Amor, 2003).
As mentioned earlier, stunting is a public health problem in Mexico, but the prevalence of wasting is within expected values for a healthy population. Results from the Second National Nutrition Survey (Rivera et al., 2001) show that the mean height-for-age z-score is −0.4 from 0–11 months, drops to −1.1 at 12–23 months, and remains at around −1.0 up to 59 months of age. The prevalence of stunting is 8.5 percent from 0–11 months of age, rises sharply to 21.8 percent at 12–23 months, and remains at about that level until 4 years of age. These data indicate that stunting occurs from birth to 23 months of age and that there is no substantial catch-up growth from 23 to 59 months. At the end of the preschool period, the height of children is about 1 SD below the mean value of the reference population, and about 20 percent of children have heights in the lower extreme (< –2 SD) of the reference distribution. In contrast, the mean weight-for-height z-score remains between +0.1 and +0.3 from birth to 59 months of age, indicating that weight relative to height is slightly above the value expected
given the height of the population. Moreover, wasting remains below 3.5 percent from birth to 59 months.
For older children important catch-up growth is not observed either, especially in low socioeconomic conditions. Data from the Second National Nutrition Survey 1999 showed that children ages 2–9 years from the upper 25 percent of the SES index have higher values of height-for-age relative to the rest of the population (average differences 3.8 cm in girls and 4.1 cm in boys) but are still shorter than the WHO/NCHS/CDC reference (average differences 1.6 cm in girls and 1.8 cm in boys) (Figures B-3 and B-4) (Monterrubio-Flores, 2006). Thus, whereas the prevalence of stunting for 5–11-year-old children is about 16 percent, the prevalence of BMI > 85th percentile of the 2000 CDC BMI charts in this age category ranges from 19 percent to 35 percent (average = 25.7 percent) in boys and from 21 percent to 43 percent (average = 28.6 percent) in girls (Rivera et al., 2001). This contrast indicates that even though linear catch-up growth is not achieved, weight relative to height, i.e., BMI, is high.
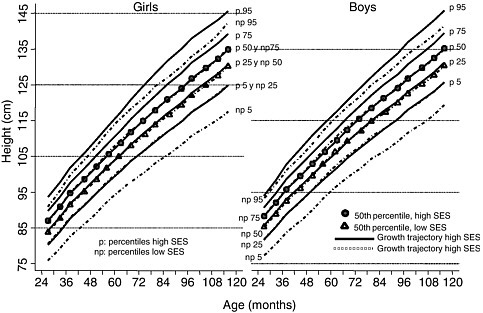
FIGURE B-3 Height-for-age calculated percentiles for Mexican children ages 2–9 years old, according to socioeconomic status (SES).
NOTES: Calculated percentiles are based on the entire Mexican population. SES is classified by the SES index distribution using the 75th percentile as the cutoff point— high is > 75 percent and low is < 75 percent.
SOURCE: Monterrubio-Flores (2006).
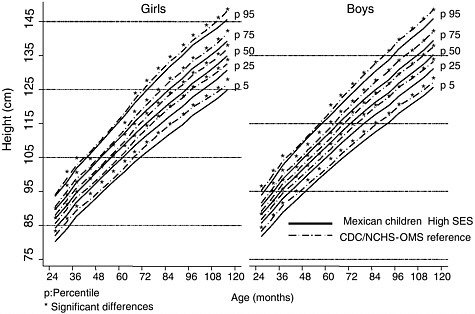
FIGURE B-4 Height-for-age calculated percentiles for Mexican children ages 2–9 years from the upper quartile of socioeconomic status (SES) distribution versus the CDC/NCHS-OMS reference population.
NOTES: Calculated percentiles are based on the entire Mexican population. SES is classified by the SES index distribution using the 75th percentile as the cutoff point: high is > 75 percent and low is < 75 percent.
SOURCE: Monterrubio-Flores (2006).
The aforementioned data show that childhood obesity represents a growing problem in Mexican society, a problem that will add an additional burden to a health care system already preoccupied and overwhelmed by public health issues related to poverty and underdevelopment. When comparing prevalence of under- and overnutrition in the populations of the United States and Mexico, two important differences emerge. First, the Mexican data clearly reflect a dual burden—the problem of undernutrition (especially stunting) and micronutrient deficiencies are unsolved and therefore require ongoing public health strategies and monitoring systems for addressing the problem. In contrast, these problems are not widespread in the American population and thus are not public health priorities. Second, the prevalence of childhood obesity in Mexico is higher among wealthier groups, whereas in the United States, the populations at greatest risk for
obesity are ethnic minorities (e.g., African Americans, Hispanic Americans, American Indians) and lower SES families. Interestingly, this latter difference does not occur in the Mexican adult population, in which obesity is much more homogeneous among SES groups. This difference in the distribution of obesity among SES groups between children and adults may be related to low SES households providing environments that are more prone to encourage infections and malnutrition, especially among young children. These differences should be considered when formulating recommendations to prevent obesity in children and adolescents in Mexicans living in Mexico and those living in the United States.
FACTORS INFLUENCING CHILDHOOD AND ADOLESCENT OBESITY
In order to define a set of recommendations for preventing obesity among Mexican children and youth, the relative contribution of different determinants driving the problem must be examined. Although several scientific observations have built strong evidence on the biological and socioeconomic determinants of obesity, the relative contribution of these factors is context specific. This section contains an analysis and description, based on the best available evidence, of the relative weight of potential determinants in the Mexican context.
Using an ecologic framework to understand the determinants of obesity, it is clear that several factors at different levels interact to explain energy imbalance, which is the direct cause of obesity. The next section reviews the relative contribution of the two main factors related to energy balance—energy intake versus energy expenditure—and explores the social and cultural factors influencing them in the Mexican context. The authors use available evidence to describe how the environment has changed for Mexican children and youth over the last few decades toward an “obesogenic” environment, understood as an environment that may promote obesity and encourage the expression of an individual’s predisposition to gain weight.
Energy Balance and Individual Factors
Obesity can be viewed as a problem of a positive energy balance—in other words, an excess energy intake relative to a given energy expenditure sustained over time. Even a minor energy imbalance over time can result in the accumulation of excess body fat. During childhood and adolescence, adequate balance should be kept in order to allow normal growth. When energy intake exceeds expenditures, including the requirement for normal growth and development, then body fat accumulates and the risk of obesity
increases. Dietary intake represents the energy intake side of the energy balance equation, while energy expenditure has several components—resting metabolic rate, adaptive thermogenesis, the thermogenic effect of food, and physical activity (Horton, 1983).
In addition to energy intake, other factors, including genetics, can explain the variability between populations in linear growth. However, there is consensus that the variability in linear growth across regions is due more to social, demographic, and economic factors than to genetics, at least among preschool children (Habicht et al., 1974). In an international comparison using the WHO global database on child growth and a database of national factors, Frongillo et al. (1997) concluded that most national variability of stunting and wasting among preschool children was explained by national factors and geographic region where higher energy availability, female literacy, and gross product were the most important associated factors. The genetic contribution to linear growth after puberty remains unknown.
In the last few decades, extensive research has focused on the search for a genetic component in the etiology of obesity, and consequently some evidence on the role of genes in the obesity etiology has been documented (Snyder et al., 2004; Chagnon et al., 2000; Oksanen et al., 1997; Rosenbaum and Leibel, 1998). According to the “thrifty genotype” hypothesis, originally proposed in the sixties by James Neel (1962), Indian ancestry could be a genetic risk factor for metabolic syndrome features, including obesity; the hypothesis could partially explain the individual predisposition observed in highly admixed populations such as Mexicans. An analysis among Mexican Americans in San Antonio, Texas, showed that diabetes risk augments as the Native-American admixture increases estimated from skin color measurements (Gardner et al., 1984). Recently, the use of ancestral indicator markers has been proposed as an alternative methodology to evaluate this hypothesis and for genetic mapping purposes, although its effectiveness remains to be proven (Fernandez and Shiver, 2004). However, for the moment there has not been a gene or even a unique genomic region associated consistently with obesity risk. More importantly, the fact that the observed worldwide trends in obesity cannot be explained by modification on the genetic pool of populations suggests a minor role of the genetic component in the current obesity epidemic. Moreover, as a non-modifiable factor, the contribution of genetic factors in designing effective obesity preventive strategies may have a minor role when compared to environmental and behavioral factors.
Another proposed factor that may increase individual susceptibility to obesity and related chronic diseases such as CVD and diabetes, other than genetic susceptibility, is malnutrition in early life, especially low birth weight (LBW) and stunting before the age of 3 years (Caballero, 2001). The in-
creasing prevalence of noncommunicable chronic diseases affecting more people at younger ages in developing countries than in the developed world (WHO, 2006b) may suggest an extra vulnerability of populations in epidemiologic transition, such as the Mexican people. If nutritional insults in early life confer this extra vulnerability, then the results of combating undernutrition in early life (gestation and the first 2–3 years of life) will have double benefits—adequate nutritional policies will affect not only the undernutrition-related problem but also the increasing epidemic of chronic diseases.
After observing an association of LBW and low height at 1 year of age with hypertension and other CVD, Barker (1992) proposed the fetal origin of disease hypothesis, later known as thrifty phenotype hypothesis, as an alternative to the thrifty genotype hypothesis previously described (Hales and Barker, 2001). This hypothesis (called “programming hypothesis”) suggests that poor fetal or early life nutrition causes an adaptation process that increases the capacity to store energy, and thus may program future propensity to obesity, diabetes, and CVD. Since then, several studies (mainly in developed countries) have tried to test this hypothesis with inconclusive results. The association between LBW or short stature during early life and the risk for diabetes and hypertension has been observed in several populations (Simmons, 2005). However, other studies have failed to observe the same association (Stern et al., 2000; Lucas et al., 1999). The size of the effect and its relative impact of the programming hypothesis on the high prevalence of these diseases in developing countries remain controversial.
In terms of the risk of developing obesity in adulthood, the impact of fetal or postnatal growth retardation remains unclear. Large cohort studies such as the Nurses’ Health Study have shown a J-shape in the association of birth weight and adult obesity, with both LBW as well as high birth weight showing an increased risk relative to normal birth weight (5.6–7 pounds, equivalent to 2.5–3.8 kg) (Rich-Edwards et al., 1999). The impact of postnatal growth retardation on the risk of obesity is less clear. For instance, the study—which because of its natural design has been recognized as quasi-experimental—of records on the Dutch famine during World War II has shown that the prevalence of adult obesity was higher among those exposed to famine during the first two trimesters of pregnancy than among those exposed during the last trimester and early infancy. This last group had an even lower prevalence of obesity than those who were not exposed to the famine (Stein et al., 1995).
One of the reasons for the inconsistency of the results may be the fact that the majority of these studies have been performed in developed countries, where there is a low prevalence of undernutrition and therefore the effect could be low. On the other hand, the majority of these studies have shown that LBW and stunting are not risk factors per se. The increased risk
may be expressed only among subjects who move from a scarcity to an abundance of energy intake. Studies characterized by their nutritional transition with clear modifications in dietary patterns and lifestyle are needed from developing countries to support or reject this hypothesis. However, analysis of a Guatemalan population showed that fetal programming might have a minor role at least for CVD risk among adults (Stein et al., 2002.)
Although the programming hypothesis is still controversial, while new evidence from developing countries arises the potential contribution of LBW and short stature during the first years of life in the definition of preventive strategies should be considered, especially in Mexico where stunting remains as a prevalent problem. In contrast to the genetic component information, the basis of programming theory could be modified in just one generation if researchers succeed in controlling undernutrition during early life. This implies investing in nutrition promotion programs in early life as a potential strategy for obesity prevention.
Levels of Physical Activity and Inactivity
Although there is limited information on levels and trends of time dedicated to physical activity and inactivity in Mexican children and youth, the available information indicates a tendency to sedentary lifestyles. In a study conducted on children and youth ages 9–16 years in low- and middle-income schools in the Mexico City area, they devoted an average of 4.1 hours/day to total video viewing (representing total leisure screen time except computer use) and only 1.8 hours/day to moderate or vigorous physical activity. Boys reported more television viewing and time spent in physical activity than girls (Figure B-5) (Hernandez et al., 1999).
Another study conducted using a similar methodology with youth and young adults ages 11–24 years in the state of Morelos, Mexico, found results that also suggest a sedentary lifestyle. In this case, adolescent boys and young men reported significantly more time dedicated to moderate and vigorous physical activities than girls and young women. Boys spent more time playing videogames [3.2 (SD 2.4) hours daily], than watching television [2.7 (SD 1.9) hours daily], while adolescent girls and young women spent 2.6 (SD 2.5) hours daily using VCR or videogames and 2.8 (SD 1.9) hours daily watching television. Significant differences in the mean daily screen time—defined as total hours per day watching television, videogames, or VCR—were observed by age, type of community, SES, and medical insurance in both adolescent boys and girls and young adult men and women. Adolescent girls who reported that they were dieting to lose weight had significantly less screen time exposure than girls who wanted to gain weight. Mean screen time significantly increased with the level of urbanization of the community, and, in girls and young women, screen time increased with
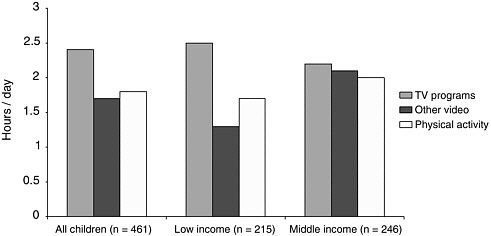
FIGURE B-5 Mean time dedicated to video viewing and physical activity, Mexico City children and youth ages 9–16 years, 1999.
SOURCE: Hernandez et al. (1999).
increasing SES (p < 0.01) (Lajous M; personal communication; August 2004; Cancun, Mexico). A study using data from the Second National Nutrition Survey (1999) found that adolescent girls and women ages 12–49 years dedicated an average of 45 minutes/day to physically active sports and 3.64 hours/day to television viewing. Thirty-four percent of the adolescent girls and young women ages 12–20 years old reported that they practiced sports regularly, and they had higher odds of practicing sports than women ages 31–49 years old (Hernandez et al., 2003).
The association between television viewing and obesity (as measured by BMI levels) has been documented (Gortmaker et al., 1996; Robinson, 2001). This association also was found in Mexico in the studies mentioned previously. In the study conducted with children in Mexico City, after adjustments for other covariates such as parental obesity, SES, age, and gender, children who spent more than 3.1 hours/day viewing television programs were 1.69 times more likely to be obese or at risk for obesity than children who viewed television programs less than 1 hour/day. On the other hand, children who engaged in physical activity less than 1 hour/day were 1.6 times more likely to be obese or at risk for obesity than children who engaged in physical activity more than 2.5 hours/day. When analyzing the associations between television program viewing, physical activity, and being obese or at risk for obesity, similar associations were found (Table B-2) (Hernandez et al., 1999). There were related findings in the study conducted with youth in the state of Morelos in which a BMI of 0.13 kg/m2 higher (95 percent CI 0.04, 0.23) was found in adolescent boys who spent
TABLE B-2 Adjusted Odds Ratios for Children Ages 9–16 Years at Risk for Obesity and Obese by Television Program Viewing and Physical Activity Level, Mexico City, 1999
more than 5 hours/day viewing television compared with adolescents who viewed television less than 2 hours/day ((Lajous M; personal communication; August 2004; Cancun, Mexico).
Eating Pattern Trends: Nutritional Transition
As stated previously, Mexico is experiencing a nutritional transition with a clear shift over the past decades to higher intakes of fat, refined carbohydrates and processed foods, and lower intakes of whole grains, vegetables, and dietary fiber that represent traditional diets (Popkin, 2001; Rivera et al., 2004a). The transition is closely related to the process of urbanization and the migration from rural areas into the cities but also is affecting the rural areas to a lesser extent. The relationship among the nutritional transition, urbanization, and poverty is complex and manifests differently in various countries. Studies have shown that the nutritional transition was observed mainly among the higher SES groups living in rural areas and among low SES groups in urban areas, suggesting that lower-income populations, principally in urbanized environments, could be affected by the two extremes of the nutritional spectrum (Seidell, 2000). In Mexico, the nutritional transition, as assessed by changes in dietary fat intakes and BMI values in adults, has been observed in all regions regardless of their level of development, in urban and rural areas, and in all socioeconomic groups. In contrast, as presented previously, high BMIs in children are more prevalent in the more developed regions and urban areas. However, evidence suggests that children living in low-income neighborhoods and attending public schools in Tijuana along the Mexican side of the U.S.–Mexican border are
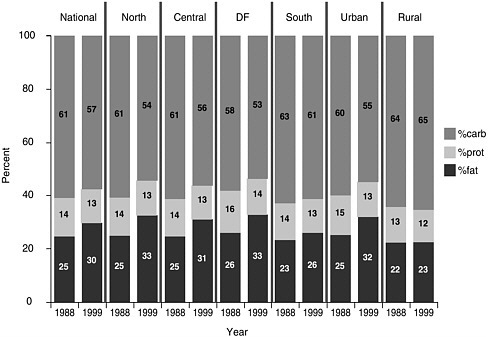
FIGURE B-6 Relative contribution of macronutrients to total energy intake from 1988 to 1999.
SOURCE: Barquera et al. (in press).
experiencing a nutrition transition with respect to an increased risk of obesity and related chronic disease (Villa-Caballero et al., 2005).
The strongest evidence of this transition comes from the contrast between adults’ self-reported dietary intakes from the 1988 and 1999 National Nutritional Surveys. During this 11-year period, the percentage of energy intake from fat among Mexicans increased from 23.5 percent to 30.3 percent (Figure B-6). This increment was observed across all regions of the country, including the poorest region (south), which increased from 22.1–26.9 percent during the same time period (Rivera et al., 2004a). However, this increment was not observed in rural areas, where the percentage of energy intake from fat remained stable at 22–23 percent. Unfortunately, there is a lack of information about changes in the type of fats (e.g., saturated, trans fat, and unsaturated fat) in the Mexican diet, especially for children and youth.
In this same analysis, the mean percentage of energy intake from carbohydrates decreased slightly from 59.7 percent to 57.5 percent. However, the lack of information on the type of carbohydrate (especially in the 1988 survey) limits the possibility to analyze intakes of refined versus complex
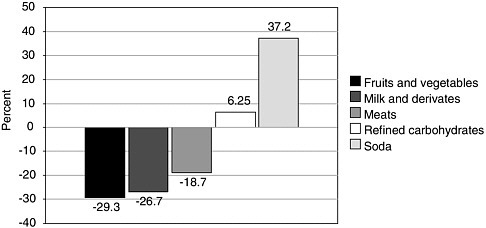
FIGURE B-7 Changes in mean food purchases in 1996 (relative to 1994) by food group.
SOURCE: Rivera et al. (2004a).
carbohydrates. A secondary analysis using data from National Income and Expenditure Surveys collected by the Instituto Nacional de Estadística, Geografía e Informática (INEGI) from 1984 to 1998 showed that consumer purchases of refined carbohydrates and sweetened sodas increased by 6.3 percent and 37.2 percent from 1984 to 1998, respectively, whereas the amount of fruit and vegetables purchased dropped by almost 30 percent during the same period (Figure B-7) (Rivera et al., 2004). This observation suggests that complex carbohydrate intake has declined. Whether or not the modification of relative prices of these food commodities during this period played an influential role in the consumer purchases is an area that requires further research.
In the Second National Nutrition Survey 1999, dietary intake for school-aged children was evaluated using a 24-hour dietary recall. Foods were ranked according to their contribution to the total amount of food intake (in grams). Four food groups represented nearly 50 percent of their total amount of food consumed. The main contributors to children’s diets were milk and dairy products (185.5 g), tortilla and maize products (156.4 g), and sugar and sugar-sweetened beverages (135.3 g). Only 8 percent of the children had fruits and vegetable intakes greater than 400 g/day, which represents the current recommended intake (WCRF, 1997), while 56 percent had intakes less than 100 g/day (Figure B-8) (Ramirez CI and Rivera JA; personal communication; February 2006). The median energy intake in preschool children was 949 calories and 1,377 in school-aged children. Pro-
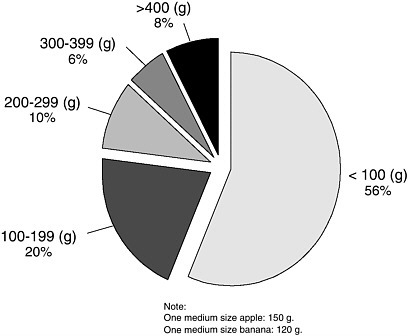
FIGURE B-8 Distribution of school children according to fruit and vegetable consumption based on the Second National Nutrition Survey, 1999.
SOURCE: Barquera et al. (2003).
tein intake in both groups was well above adequate levels at 150 percent of estimated requirements. Children living in the northern and Mexico City regions had the highest fat intake and the lowest fiber intake. Children living in the southern region, indigenous children, and those in the lowest SES group had higher fiber and carbohydrate intakes and the lowest fat intake (Barquera et al., 2003).
A study conducted using data from the Second National Nutrition Survey 1999 classified foods consumed by children ages 1–4 years as either centrally processed or not processed. Centrally processed foods are defined as those involving any kind of industrial process, whether they are foods that had been consumed without industrial process before (e.g., milk or bread) or foods that were developed by industry (e.g., sweetened soda and packaged snack foods). Centrally processed foods made an important contribution to the total energy and nutrient intakes at the national level and in sub-populations. For example, the contribution to total energy intake was 46 percent; protein intake was 39 percent; total fat intake was 56 percent; and saturated fat intake was 69 percent. These findings underscore the im-
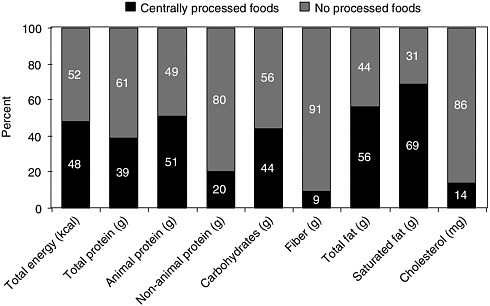
FIGURE B-9 Contribution of centrally processed foods to total energy and nutrient intakes in children younger than 5 years old.
SOURCE: González-Castell et al. (2003).
portance of the food and beverage industry in the diets of preschool children and demonstrate the need for involving food and beverage companies in efforts to prevent and control childhood obesity (González-Castell et al., 2003) (Figures B-9 and B-10).
Factors that Influence Energy Intake and Energy Expenditure
Family and Sociocultural Factors
Family and cultural values are strong determinants of both eating patterns and physical activity levels (Patrick and Nicklas, 2005). Although direct evidence was not available on the role of family and cultural values as determinants of childhood obesity in Mexico, there is anecdotal evidence suggesting that chubby children are perceived to be healthy children, especially among the poorest and rural sub-populations, in Mexican society. Researchers are unaware of any empirical evidence supporting this widespread cultural belief or its origin. It has been suggested that recent and concurrent undernutrition in the same communities or even in the same families, reinforce the ideas that heavier children are healthier. In a small
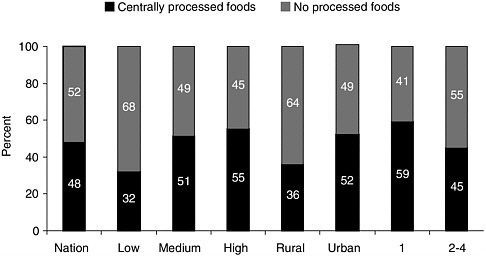
FIGURE B-10 Contribution of centrally processed foods to total energy intake of population subgroups (nationwide, low socioeconomic status (SES), medium SES, high SES, rural, urban) in children younger than 5 years old and 1 or 2-4 years old.
SOURCE: González-Castell et al. (2003).
study in Xalapa, Veracruz, half of all parents of obese children did not identify their own children as having any weight problem (Brewis, 2003). This parental perception suggests either a level of denial or a normalization of obesity that reinforces children to be heavier than the accepted healthy range. These beliefs, combined with other cultural values such as feeding a child as an act of love and caring, or that acquiring and using consumer goods that decrease physical activity such as television, video games, and cars are identified as markers of higher SES within communities, need to be counterbalanced with community-based interventions that empower parents and key community members to promote healthier lifestyles. This is an area where both observational and experimental research are greatly needed.
Self-reported energy intake can vary considerably between non-obese and obese subjects. Based on data from the Second National Nutrition Survey 1999, researchers estimated energy under-reporting in Mexican women ages 18–49 years using a 24-hour dietary recall questionnaire. Researchers found that the prevalence of energy under-reporting in non-obese women was approximately one-third (33.66 percent) and more than half (53.73 percent) in obese women. The adjusted prevalence ratio for under-reporting was 1.51 times higher in obese compared with non-obese women (95 percent CI 1.35, 1.69). The researchers concluded that obese Mexican women tend to under-report energy consumption more than their non-obese coun-
terparts. The differential under-reporting in Mexico between obese and non-obese women suggests that there is a perception of the association between diet and excess weight, which may be a positive sign of increasing awareness of the epidemic (Campirano et al., 2003). However, experimental studies in children and adolescents have shown that mean daily caloric intakes may be under-reported by as much as 17 to 33 percent of energy expenditure and that under-reporting tends to increase with age (Bandini et al., 2003; Champagne et al., 1998). Similar methodological challenges exist for conducting research on children’s physical activity levels (IOM, 2005).
Another factor that may influence dietary patterns and physical activity is the change in family structure experienced in Mexico during the last two to three decades. The following additional issues also may influence dietary and physical activity patterns: the increase of women’s roles in the labor force, increasing rates of divorce and single parenthood, increasing numbers of families with key members in the United States, and decreasing household size. For example, reduced time available for food selection and for cooking can encourage the use of more energy-dense processed food and therefore can influence the quality of the diet. Also, reduced time of parents at home coupled with increasing levels of insecurity in the streets may encourage television viewing and sedentary lifestyles. However, empirical evidence of these possible effects in Mexico is lacking.
Environmental Factors: Transition Toward an Obesogenic Environment
Opportunities for physical activity. Information about access and use of television and the Internet indicates that Mexico is moving toward a more sedentary environment. The number of television stations operating in the country has increased from 115 in 1980 to 658 in 2004 (Secretaría de Comunicaciones y Transportes, 2005). Not surprisingly, by 2000 85 percent of the households in Mexico had access to a television set, and this proportion reached 97 percent in Mexico City. Even in the states with a high poverty level, such as Chiapas or Oaxaca, more than 56 percent of the households had a television set (INEGI, 2000). Mexico has a higher number of television sets per capita than most Latin American countries, although the number is still lower than that in the United States (Figure B-11). However, exposure to television in Mexico can be underestimated because Mexican households are larger than those in the United States. Restricted television (television systems that charge for access) also is becoming more popular, increasing from 1,250,000 subscriptions in 1995 to 2,660,000 in 2003 (COFETEL, 2005).
In addition to the explosive growth of the television industry in Mexico, the Internet also is becoming more popular. The number of Internet users grew from 94,000 in 1995 to 16,492,454 in 2005 (INEGI, 2005a). Most
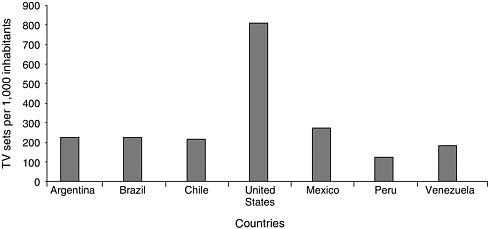
FIGURE B-11 Number of television sets per 1,000 inhabitants, selected countries, 1997.
SOURCE: COFETEL (2005).
importantly, Internet use is concentrated in youth and adolescents, as shown in Figure B-12, rising from 2.43 percent to 7.73 percent between 2001 and 2005 for children ages 6–11 years and from 14.41 percent to 34.16 percent between the same years in adolescents ages 12–17 years. Finally, it is estimated that more than 22.8 million Mexicans—13.1 percent of 6- to 11-year-old children and 28.1 percent of 12- to 17-year-old adolescents—use computers (INEGI, 2005b).
Another indicator suggesting that the Mexican population is moving toward an obesogenic environment with reduced options to engage in physical activity is the growth in the number of motorized vehicles. Although the population of Mexico has increased 17 percent from 1990 to 2000, the number of motor vehicles registered increased by 38 percent during the same period of time, representing nearly 11 million automobiles in 2000 and 13.5 million automobiles in 2002 (INEGI, 2005b).
Trends in access to unhealthy and healthy foods. Over the past few decades, Mexicans have experienced an increased availability and access to less healthful foods and beverages (e.g., high energy–dense, low nutrient– dense, and low-fiber foods and high-calorie low-nutrient beverages). This is especially true for Mexicans living in urban areas. This increased access to these types of foods and beverages is yet another fact indicating the country is shifting toward an obesogenic environment.
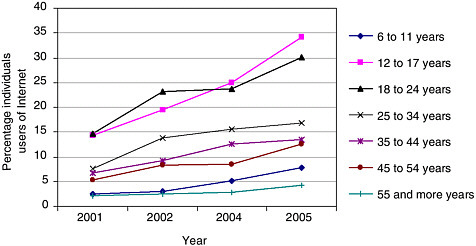
FIGURE B-12 Percentage of Mexicans who are Internet users by age group, 2001– 2005.
SOURCE: INEGI (2005b).
Transnational corporations representing the fast food restaurant or quick serve restaurant industry have expanded substantially over all the major and middle-size cities across Mexico. The first Mexican franchise of McDonald’s Corporation opened in 1985 in one of the wealthiest neighborhoods of Mexico City. According to the company’s website, there are currently 320 franchises nationwide located not only in wealthy areas but also in middle- and low-income neighborhoods (McDonald’s Corporation, 2006). A very similar phenomenon has happened with other restaurant companies such ALSEA, which operates Domino’s Pizza and Burger King in Mexico. According to a company report (ALSEA, 2005), over 15 years, the quick serve restaurant company has established 529 Domino’s Pizza sites in 123 cities and promoted sales of more than 37 million pizzas in 2004. Indeed, hamburgers and pizza are the major types of fast food restaurants representing 30 percent and 37 percent, respectively, of the entire fast food market in Mexico. The success of these companies relies on the acceptance of their products by Mexicans. Given the huge consumer demand, the meals are affordable for a large proportion of the population (Hawkes, 2002).
Another form of energy-dense foods that are widely available is Mexican street foods that are sold informally on the streets in cities as well as in schools. Although data are limited about the numbers of sites, varieties, prices, and nutrient-content of the Mexican street foods, this industry appears to be rooted in Mexican culinary culture and its growth has paralleled the population growth in urban areas. An important feature of this industry
is the modification of traditional Mexican food that usually was not fried and contained tomato, hot pepper, and other vegetables. However, current street foods sold are high energy–dense as a result of widespread use of vegetable oil for frying, increasing the use of cream and cheese, and reducing the use of vegetables. Therefore, this “Mexican fast food,” which is not centrally processed, is an important source of total energy in the Mexican diet, including children and youth.
As with the fast food restaurant industry, the high consumption of sweetened beverages, particularly carbonated soft drinks, in Mexico is linked to large-scale marketing activities across multiple media platforms (e.g., print, radio, broadcast and cable television, Internet, outdoor signage). Indeed, according to a WHO report that reviewed marketing activities of global soft drink and fast food companies in emerging markets, Mexico was identified as the world’s leading per-capita consumer of Coca-Cola. In 1998, Mexicans consumed more than 400 milliliters per day of sweetened carbonated soft drinks. By volume of sales, Mexico is the Coca-Cola Company’s second largest market after the United States (Hawkes et al., 2002).
Another important source of energy in the Mexican diet is the high intake of oil. The use of oils with a high trans fatty acid content has increased considerably in both the fast food industry and in baked and fried foods and snacks produced by industry. Also, high fructose corn syrup has been replacing the sugar cane as a sweetener in soft drink production, although some evidence exists about its potential impact on weight gain (Bray et al., 2004), this is still a topic of much debate. The association of certain types of fats or sweeteners to obesity remains unknown and needs further research.
Advertising and marketing trends. In 2004, food advertising was ranked fourth and beverage advertising was ranked sixth in 20 categories for the amount spent on advertising to Mexicans through television, radio, and print media totaling US $1.064 billion and US $565 million, respectively. Television advertising is the primary venue for food and beverage advertising to the Mexican population (WARC, 2005). There were limited data publicly available to the authors documenting the growing trend of companies’ promotion of high energy–dense and low nutrient–dense foods and sweetened beverages, sedentary activities, and entertainment to Mexican children and youth. There are data showing that fast food restaurant and beverage companies engage in philanthropic activities and sponsorship of sporting events as ways to market to Mexican youth (Hawkes, 2002). The Global Kids Study, conducted in 1996 and 1998 by Just Kid Inc., Nickelodeon, and Research International, provides information about the brand and consumer environment, attitudes, beliefs, and consumption behaviors
of a cohort of 400 children, ages 7–12 years, and their mothers who were surveyed in each of six countries. The purpose of the marketing research was to provide Nickelodeon with a strategic planning tool to support the entertainment company’s international business initiatives targeting children and youth in countries such as Mexico. The cities where the study was conducted in Mexico include Mexico City, Guadalajara, and Monterey. An interview and questionnaire were used to gather detailed marketing research data about the children and their families. The findings showed that international global brands, such as Coca-Cola, McDonald’s, Pizza Hut, and Kentucky Fried Chicken, are well recognized by Mexican children based on their brand awareness and preferences (Friend and Stapylton-Smith, 1999). There are presently no publicly available data documenting Mexican children’s and youths’ discretionary income, particularly among higher SES groups, which they may use to purchase foods and beverages without parental guidance, especially away from home settings such as fast food restaurants, shopping malls, and schools.
Consumers ages 18 years and younger are subject to special protection under Mexican law. However, there is currently no single governmental authority or body of law governing products or advertising to Mexican children and youth. The three government institutions primarily responsible for the regulation of children’s advertising in Mexico are the Attorney General for Consumer Protection, Ministry of the Interior, and the Ministry of Health (Arochi et al., 2004). The non-governmental self-regulatory organization in Mexico is the National Council for Advertising (Consejo Nacional de la Publicidad) (Friedman and Dickler, 2003). There are clear guidelines and laws restricting the promotion of alcohol and tobacco products to Mexican children. According to Article 16 of the Communications Council Code of Ethics, advertisers must not “undermine parental authority, judgment, or preferences” and “children should not be encouraged to urge other persons to purchase a product, especially their parents.” Companies are also encouraged to avoid taking advantage of children’s credulity or lack of experience. While television and radio advertising should not exceed 18 percent of the total time of transmission to Mexicans, special regulations for children’s advertising have not yet been developed in Mexico. Furthermore, there are currently no guidelines or regulations for the promotion of high-calorie and low-nutrient foods and beverages to young consumers (Arochi et al., 2004).
However, Mexico is one of the many countries that endorsed the WHO Global Strategy on Diet, Physical Activity, and Health at the 57th World Health Assembly in 2004 (WHO, 2004). The Global Strategy provides member states with a range of policy options to address less healthful dietary practices and physical inactivity, including provisions for marketing, advertising, sponsorship, and promotion to support international public
health goals. These provisions recommended that “food and beverage advertisements should not exploit children’s inexperience or credulity,” should discourage messages that promote less healthful dietary practices, and encourage positive healthful messages (WHO, 2004).
School environments. Unhealthy weight in children, particularly in school-age children, results from an environment that enhances the intake of high energy–dense foods and restricts the opportunities for regular physical activity. Children spend a substantial amount of time at school. Therefore, the school environment is an important influence on their physical activity behaviors and dietary patterns.
The Ministry of Education implements a physical education program in elementary schools nationwide (Secretaría de Educación Pública, 1994) that envisions two physical education sessions, each lasting about 30–50 minutes per week, as a means to promote a healthy lifestyle. The program also aims to promote a healthy diet through elementary-level educational materials that include units related to hygiene and nutrition and the promotion of healthful lifestyles.
The physical education component of the program is structured according to the different skills and development characteristics attributable to each age group. The program is designed to promote five different types of skills. Stimulation of motor perception; conditional physical skills; basic sports skills building; physical education for health; and social interaction. The plan includes a section that suggests several activities and one more that recommends methods for evaluating the plan’s performance. Nevertheless, the program is not implemented as designed according to existing policies.
Researchers conducted a search for publications on the school environment and its relationship to childhood obesity in Mexican schools but was not able to find published articles on this topic. However, formative research was obtained from a project that was recently initiated in 12 public schools in Mexico City; the project aims to change the core elements in the school environment that promote obesity (Rivera J, National Institute of Public Health; personal communication; March 2006). The first phase of the project undertook an assessment of the school environment. Preliminary data from children in 4th and 5th grades in 12 schools representing over 1700 students showed that children, are exposed to an unhealthy environment in several ways. Children are exposed to high energy–dense foods (e.g., high-fat and high-sugar snacks and foods such as candy, ice cream, pizza, pork skin chips with cream, tacos, and other traditional Mexican fried foods) and to large portion sizes. In addition, children eat several times at school (they have as much as six feeding opportunities during the four hours at school). The availability of fresh fruits and vegetables is very lim-
ited, and most often the available fruits are served with cream. The preparation and handling of foods sold in schools are under uncertain sanitary conditions that increases the food safety risks for the children. Additionally, most of the schools lack free drinking water from fountains. In the few schools where potable water fountains are available, they are not well maintained and are not used for drinking water.
Physical activity is low. The school-break period is the time designed to eat lunch, and there is limited time left for active play or physical activity. During this time children are not allowed to run due to safety concerns, because all grades have recess at the same time and older children running or playing could harm younger children. In addition, there is limited space available for physical activity in many of the schools surveyed. In general, the school facilities and sports equipment do not facilitate adequate physical education classes and children spend on average less than 40 minutes of Physical Education (PE) per week, about 40 percent of the time established by norms (100 minutes per week). Moreover, PE classes are not active enough; children spend only nine minutes per week on moderate to vigorous physical activity.
These results are similar to findings from a small pilot study in 10 schools in Mexico City. In this sample, approximately half of the schools in the pilot study did not have appropriate areas for the physical education classes; the average space available was 290 m2 for approximately 330 students. Moreover, teachers showed little motivation to promote physical activity, and the physical education classes were not well structured. Approximately 30 percent of children did not participate in physical education classes, and moderate to vigorous physical activity was achieved for approximately 10 minutes by those participating in the physical education classes. In 80 percent of the schools the average length of the physical education class is 50 minutes a day, and the remaining 20 percent of the schools divide the class length by age groups (30 minutes for children younger than 10 years of age and 50 minutes for older children) two times per week. Only 20 percent of the schools organize and promote extracurricular sporting events such as soccer and athletics tournaments. One of the major limitations of extracurricular physical activity programs is that many schools have several shifts (e.g., morning and evening) at the same facility, so that extracurricular physical activity programs are not possible. The following issues were identified as potentially important in terms of their influence on behavior and dietary intake at school:
-
Lack of drinking water from water fountains or other public supplies at schools in seven of the eight schools surveyed, which may promote the intake of sweetened beverages.
-
Lack of bottled water and the widespread availability of sweetened beverages in concession stands that have similar prices; therefore, there may be a reduced incentive for the children to drink water during the school day.
-
Lack of regulations for foods and beverages sold either at concession stands on the school grounds or at retail establishments located near schools.
-
The federally funded and mandatory school breakfast program provides energy-dense and centrally processed foods at very affordable prices.
-
Widespread availability of high energy–dense foods and sweetened beverages within and around the school environment.
-
Low availability of vegetables and fruits within and around the school environment.
Although this formative research is not representative of public schools throughout Mexico, or even the schools in Mexico City, it provides a qualitative assessment of the school environment that may be useful to identify the elements within the environment that promote obesity and opportunities for positively intervening to promote a healthier school environment.
Other environmental factors. These factors are important determinants of an environment favoring a positive energy balance in most of the Mexican population. However, there are many other factors that are likely to influence children and youth and can be considered components of an obesogenic environment. However, there is limited research on these factors upon which to design evidence-based strategies for effectively preventing obesity in Mexican children and youth.
The exponential growth of mega cities in Mexico, with a lack of environmental design planning to facilitate physical activity, are likely to have an important impact on the availability and access to physical activity facilities, especially in poor and new neighborhoods in the suburbs of these cities. Data regarding availability and use of physical activity facilities are clearly needed to evaluate and potentially modify this factor. Another issue potentially contributing to reduced physical activity are safety concerns and poor air quality in Mexican cities, especially in Mexico City, which has been identified as one of the cities worldwide with the highest level of air pollution (Villarreal-Calderón et al., 2002).
Finally, with regard to energy intake, it is likely that a change in agricultural and food production policies favoring large-scale production, marketing supports for commercial producers, and developing a more competitive agricultural sector for export markets (Zahniser et al., 2005) could modify the price and access of certain foods but not necessarily the most healthful choices. Many of these policies adhere to international trade agreements such as North American Free Trade Agreement (NAFTA) (Zahniser et al., 2005); thus the impact and consequences they may have on the di-
etary patterns of the Mexican population has not been fully explored. Further research in this area is needed.
CURRENT POLICIES AND PROGRAMS
Despite the strong evidence of an increasing obesity epidemic among children and adolescents in Mexico, its impact on the awareness of the population at different levels has been limited. Within the last few years, perhaps as a consequence of published research and dissemination of the Second National Nutritional Survey 1999 results, the obesity epidemic has reached the media, especially print- and web-based media. Among the scientific community, obesity, particularly in children, is currently a topic that has generated a great deal of attention in terms of funding and human resources, with support for several ongoing research projects. However, there is still an enormous need for raising awareness at the individual, family, and community levels, as well as within the government sector at all levels. Probably because of the recent and still current problem of undernutrition as one of the main public health problems among children, the complete understanding of the double burden of undernutrition and obesity from the government and policymakers is needed to elevate childhood obesity as a national priority.
As a consequence of the low awareness within the government sector, there are a limited number of programs, mostly on a small scale, and information about these programs is not readily available. The next section describes selected programs and policies that are related to the obesity problem.
Government Policies on Food Labeling, Media Control, and Dietary Guidelines
Mexico has a set of policies, norms, and guidelines for food labeling and media control of advertising food products. However, there are many inconsistencies during the implementation of these policies, and many of them have not been periodically reviewed or modified in response to the increasing public health problem of obesity. There has not been any evaluation on consumer understanding and the impact of the information provided on food labels. Regarding the media control, as noted earlier, television advertising is the primary venue for food and beverage advertising to the Mexican population (WARC, 2005). However, there is a lack of data on the effects of advertising on Mexican children’s preferences, purchase requests, and influence on household purchases of food and beverage products. Limited evidence indicates that there may be a rise in television advertising of processed foods and beverages high in sugar or fat, or both, and
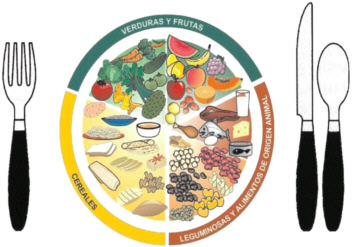
FIGURE B-13 El Plato del Bien Comer. Dietary guidelines.
SOURCE: Norma Oficial Mexicana (2005).
with healthy nutrition claims without specific policies guiding the health claims or types of advertising reaching young children.
For several years a group of nutrition experts has been working on developing dietary guidelines for Mexico. After a long process that led to consensus-based guidelines, they are soon to be officially published for the Mexican population. The guidelines are based on a plate model rather than a food guide pyramid (Figure B-13) and present food groups and advice on ways that consumers can combine them. Since these are consensus-based guidelines, this educational tool can be used as the basis for developing an effective communication strategy aimed at improving dietary practices in Mexico.
Social Programs
Oportunidades
The pillar of the Mexican social assistance strategy is the conditional cash transfer program, Oportunidades. The objective of the program is to break the intergenerational cycle of poverty though the development of human capital. At present, the program reaches more than five million families (about 25 million people) living in extreme poverty.
Oportunidades provides families with a monetary transfer intended for food purchase, a fortified food supplement for all children from 6 to 23
months of age, children aged 2 to 4 years with low weight for age, and for pregnant and lactating women; and educational scholarships conditioned on regular attendance in school, the size of which is grade and gender dependent. All benefits are conditioned on the use of regular preventative health services, the content of which changes over the life-course and regular attendance of the female head of household (to whom the monetary transfer is also given) to a series of health and nutrition education workshops. The program also provides curative health care (SEDESOL, 2006).
A number of positive impacts of the Oportunidades program on nutritional status of the population have been reported. In both urban (Neufeld et al., 2006) and rural Mexico (Rivera et al., 2004b) participation is the program resulted in an increase of approximately 1 cm in linear growth of children who were in the program from a very young age (< 6 mo) compared to children of similar age not in the program. A positive impact on the prevalence of anemia has also been reported among children less than 2 years of age (Rivera et al., 2004; Neufeld et al., 2005). However, there is concern that participation in the program may promote undesirable excess weight gain. Increased weight gain with improved socioeconomic status and higher income has been documented in a number of settings around the world (Uauy et al., 2001; Du et al., 2004). The extra resources provided to the family may be used to purchase more high energy–dense foods and sweetened beverages. The fortified food supplement for women and children provide approximately 1.4 and 2.15 kcal/g, respectively. In this population where the diet does not appear to have an energy deficit, regular consumption of the supplement in addition to the usual home diet without substitution of a similar quantity of energy may result in excess weight gain. Regular consumption is clearly desirable due to its high micronutrient content, approximately 100 percent of the Recommended Dietary Intake (IOM, 2001) of iron, zinc, and a number of other micronutrients known to be deficient in the diets of Mexican children and women during pregnancy and lactation (Rivera et al., 2003) . Consumption of the supplement has been shown to result in considerable improvements in the dietary intake of micronutrients and there is some indication of improvements in mineral status of women and children (Neufeld et al., 2006). On the other hand, the health and nutrition workshops and increased exposure to preventative health care services may lead to improved dietary and lifestyle choices among beneficiaries with a resultant decrease in the prevalence and/or severity of obesity.
The prevalence of obesity in adults who were eventually enrolled in the program (before program benefits were received) was over 20 percent (Fernald et al., 2004). In women living in urban Mexico, program participation was associated with a greater increase in body mass index over a two-year follow-up period compared to non-participants, particularly among those who had high body mass index at the start of the follow-up
(Neufeld et al., 2006). There was an increase of 1.5 percent in the prevalence of obesity in adolescents involved in the program when compared to adolescents who did not participate (Gutiérrez et al., 2005). Among preschool children, there is no evidence that participation in the program is associated with obesity, although there was a tendency towards higher BMI among the children who were enrolled in the program before 6 months of age, compared to non-beneficiaries (Neufeld et al., 2006).
The Oportunidades program with its system of co-responsibilities and its broad coverage is a promising vehicle through which to launch obesity prevention. Two studies are currently underway as part of the program evaluation activities to further clarify the impact of the program on weight gain among women and children and to strengthen the health education component of the program in reference to obesity prevention. The first is a large randomized controlled trial implemented within the context of the program. The main objective of the study is to determine whether regular consumption of the fortified food supplement is associated with increased weight gain among children and women during pregnancy and increased weight retention post partum compared to two other supplements with identical micronutrient content but without additional energy. The second study uses qualitative research methods to gain an understanding of the perceived determinants of overweight and obesity in the population and barriers to change in behaviors associated with excess weight gain. The results of both studies will be presented to decision makers within the program with specific recommendations of how to strengthen obesity prevention among program beneficiaries.
Health-Sector Programs
Preven-IMSS
The National Institute for Social Security (IMSS) provides health services to approximately 50 percent of the Mexican population. As part of the organization’s process of health improvement services, they recently designed and implemented an integrated health programs strategy known as Preven-IMSS. This strategy is focused on a portfolio of preventive actions aimed at improving the health status of their target population and marks the first time that IMSS has launched a large-scale prevention program. Starting in 2002, actions were organized by age group and vulnerable populations: children (younger than 10 years of age), adolescents (ages 10– 19 years), women (ages 20–59 years), men (ages 20–59 years), and older adults (older than 60 years of age). All the programs include major food and nutrition, physical activity, and health education components (Gutiérrez-Trujillo, 2005).
The main preventive actions for children are focused on health promotion, nutrition education, disease control and prevention, early identification of diseases, oral health, vaccination, and miscellaneous actions (e.g., personal hygiene, breastfeeding promotion, and fever control). For adolescents, the program’s preventive actions are focused on physical activity promotion; accident prevention; violence and addiction prevention; oral health; sexual health and education; nutrition education; obesity detection and control; parasite treatment; vaccination; use of preservatives; human immunodeficiency virus and sexually transmitted diseases prevention; visual, auditory, and postural defects; and reproductive health. There are also components for adults.
For each preventive action, there is a set of designed activities and objectives personalized for each age group. As part of the promotion strategy, this program has a nationally distributed magazine (sold at newspaper shops) that features health care information related to these actions. In addition, television advertisements focus on healthy lifestyles, nutrition, obesity prevention, and promoting the magazine to the general public. Until now, this program has not been evaluated fully; however, a recent internal baseline survey was designed and implemented to assess the coverage of the main components and to evaluate intermediate program outcomes such as prevalence of anemia, frequency of physical activity, undernutrition, overweight, and obesity. This survey found an inadequate register of the nutritional status in the diverse population groups and of the health promotion activities. It is expected that one-year follow-up surveys will monitor selected outcomes of this integrated health program (Gutiérrez-Trujillo, 2005).
Ministry of Health Programs for Noncommunicable Chronic Diseases
The Ministry of Health of Mexico has several programs that consider prevention as a relevant component (Ministry of Health, 2006). These programs are not integrated health or nutrition programs but programs focused primarily on the most relevant public health problems, such as obesity, diabetes mellitus, high blood pressure, and cancer. Each of these diseases has a program that includes general management and preventive recommendations that must be followed by the government health service providers. However, most (if not all) of these programs, focus attention on promoting behavioral changes and early detection in adults, especially young adults over the age of 20 years. Obesity prevention during childhood and adolescence has been given much less consideration; rather, the predominant problems of concern for this group are related to food security (undernutrition and micronutrients deficiencies).
The following are some recently implemented actions for increasing the awareness and actions related to obesity prevention in children and youth in the public sector:
-
Implementation of regional or state-level programs; evaluation by the state (public) health sector needs to be conducted.
-
Creation of obesity clinics in public pediatric hospitals addressing the clinical care and management of obese children and research focuses on the consequences of obesity.
-
Development of an official memo outlining a future nationwide communication campaign for obesity prevention that in addition to addressing food production, media regulation, and food labeling, is intended to promote healthier lifestyles with special attention to children and adolescents.
-
Addition of obesity prevention among children and adolescents as one of the five priorities for research funding in the last request for proposals by CONACYT, the federal agency that provides oversight for research funding.
Moreover, recent efforts by the private sector have been implemented but must still be evaluated.
GOALS AND RECOMMENDATIONS
In accordance with the recommendations in the IOM report, Preventing Childhood Obesity: Health in the Balance (IOM, 2005), the final goals for obesity prevention among childhood and youth should be to stop the current trend in rising obesity incidence and prevalence and related chronic diseases and ultimately reduce the proportion of children and youth with an unhealthy weight. This ultimate goal necessarily should include increasing the proportion of children and adolescents meeting a healthful diet and appropriate amounts of regular physical activity and following a healthy growth trajectory. In the process of achieving these goals, it is important to define intermediate outcomes that will be needed to evaluate progress of a multi-faceted obesity prevention strategy. Based on the information described in previous sections, the authors propose a series of goals and recommendations for action for a multilevel and nationwide obesity prevention strategy among children and adolescents. An objective of the U.S.–Mexico binational meeting will be to broadly discuss this list of recommendations among key persons from each sector (e.g., academia, government, industry, schools, communities) to reach consensus on the next steps needed to initiate this multilevel strategy. A list of possible intermediate outcomes and goals for discussion during the binational meeting include:
-
Increased quantity and quality of physical activity at schools in both planned physical education time and recreational time such as recess.
-
Increased and improved facilities for recreational activities in communities, especially suburban areas.
-
Increased advertising and marketing messages in preferably broadcast, cable, and satellite television, but also in other media such as radio, the Internet, and cell phones, aimed at children, youth, and their parents that promote healthy lifestyles, including healthful diets and regular physical activity.
-
Decreased number of media advertising or marketing campaigns promoting high-calorie and low-nutrient food and beverage products targeted at children and adolescents that increase the risk of positive energy balance (such as refined sugars and saturated and trans fats).
-
Decreased proportion of children and youth who have more than two hours of leisure screen time (including television and video watching) per day.
-
Increased proportion of children and youth consuming more than five portions of fruits and vegetables per day.
As stated in the IOM recommendations, in order to achieve these types of intermediate outcomes, a multilevel strategy clearly is needed. However, in contrast to the U.S. context, Mexican society at large (e.g., government, industry, community leaders, schools, families) is far behind on some fundamental aspects needed to build support for this strategy. Three main issues that should be covered as priority steps in developing an effective obesity prevention strategy are:
-
creating awareness among decision makers (including all branches of federal and state powers) as well as among the general public;
-
regulating and enforcing laws;
-
empowering communities so that they can achieve the necessary changes in different environments (e.g., school, community, industry) that, as described in previous sections, are contributing to a net positive energy balance among Mexicans in general, and specifically children and youth.
Priority recommendations for action specifically related to the Mexican context are listed below. The recommendations can be viewed as preliminary and will be modified through discussion with different stakeholders.
Government Level
-
Underpin the idea of childhood obesity prevention as an urgent national priority, with strong participation and leadership of government at all levels in several actions including:
-
Regulations and implementation of media and food, beverage, and restaurant industry policies;
-
Support and funding of obesity prevention programs at federal and state levels with planned evaluations of their health impact;
-
Support and funding of surveillance and monitoring efforts and wide dissemination of their findings not only at the national level, such as the National Nutrition Surveys, but also at the state and county levels;
-
Planning of urban development with an appropriate access and promotion of facilities for recreational activities;
-
Initiation of a widespread nationwide media campaign across print, electronic (e.g., radio, television), and wireless and Internet-based media (e.g., cell phones) to increase awareness of the obesity problem in the population;
-
Expand the training of professionals to design, implement, and evaluate strategies for effectively responding to the obesity epidemic.
-
Review current regulations for food labeling (NOM 051-SECOFI and NOM-086-SSA1-1994), evaluate the impact and consumers’ understanding of food labeling, and make necessary modifications required to support obesity prevention goals.
-
Review current government regulations and guidelines on the use of health claims on food products, especially nutrition-related health claims.
-
Develop incentives or regulations for advertising and marketing to children and youth, especially for food and beverage products high in total calories and in particular for those with a high content of refined carbohydrates, added sugars, and fat.
-
Seek mechanisms such as incentives or regulations to improve the enforcement of policies related to media and the food, beverage, and restaurant industries, including food labeling.
-
Create an advisory committee that, together with the Federal Commission for the Protection from Sanitary Risk (COFEPRIS), will develop and evaluate policies for food labeling, marketing, media control, and dietary guidelines. This committee should include experts from different public and private institutions, as well as industry representatives and consumers. Priority steps should focus on the following areas:
-
Modify food labeling, focusing on the need of acceptance and understanding for the majority of the population. Limited evidence suggests that most of the information contained on food labels is difficult for consumers to understand. Develop communication strategies that are clear and understandable by the general public.
-
Reduce, at minimum, the content of health claims in media-based marketing, especially for those foods that promote “healthy” choices that do not meet basic nutritional guidelines.
-
-
-
Conduct research on advertising and marketing targeted at Mexican children and youth focused on high-calorie, low-nutrient food and beverage products, and limit or eliminate practices that promote these types of products.
-
In collaboration with industry, conduct research on the types and amount of fat that is used and needed in products.
-
Set a limit on the recommended use of dietary fats and oils, particularly saturated fat and trans fats, by the food, beverage, and restaurant industry and fast food available through informal establishments.
-
Regulate media marketing for food products with high content of refined carbohydrates and fat in regards to type of information, and advertising locations. For example, the possibility of setting strict limits in children’s environments, such as schools, parks, and entertainment centers, should be researched and discussed.
-
-
Evaluate the use of policy instruments such as international trade, subsidies, and taxes for encouraging or discouraging the production and consumption of certain foods to encourage the availability and access to healthful foods such as fruits and vegetables during all seasons and to reduce the consumption of less healthful foods and beverages.
-
Promote the consumption of fruits and vegetables and other familiar healthful foods and beverages through diverse media.
-
Promote a diverse media campaign supporting the consumption of water as a substitute for sweetened beverages (including carbonated soft drinks).
School Level
-
Revise the school breakfast program to ensure healthful food and meal options.
-
Regulate the foods and beverages offered to children and youth in and around the school environment.
-
Promote the enforcement of minimally established time that children and youth participate in physical education in both private and public schools, as well as physical education programs that achieve the recommended amounts of moderate to vigorous physical activity.
-
Encourage the organization of local and regional events to promote sports practice in schools.
-
Define minimal spaces at schools to ensure regular physical activity during physical education time and during recess.
-
Revise and improve school curricula to include obesity prevention and healthy lifestyle promotion.
Community Level
-
Stimulate community organization and community members’ empowerment to request and influence the modification of norms and environments aimed at achieving healthy lifestyles.
-
Explore the spectrum of available organizations to identify the best strategies for increasing community empowerment and awareness, especially among parents, of the obesity epidemic. Potential community organizations include parents’ societies, religious groups, and non-governmental organizations.
In conclusion, Mexico is on the course of an epidemiologic and nutritional transition toward more sedentary lifestyles and obesogenic environments. The present trajectory is moving toward an increasing burden of obesity in children and youth with serious predictable health and economic burdens to the entire population and Mexican society. These risks must be addressed immediately with multi-level interventions undertaken by a variety of stakeholders in government, schools, and communities targeting children and youth in many settings. The response to the growing obesity epidemic in Mexico will require many years and perhaps decades to implement and to evaluate the effectiveness of the results. The joint U.S.–Mexico workshop, for which this and the companion paper from the U.S. context served as background for discussion, should delineate the initial steps of the strategy required to tackle this urgent public health problem.
REFERENCES
Alsea. 2004. Annual Report. [Online.] Available: http://www.alsea.com.mx [accessed May 5, 2006].
Arredondo A, Zuñiga A. 2004. Economic consequences of epidemiologic changes in diabetes in middle-income countries: The Mexican case. Diabetes Care 27(1):104–109.
Arochi R, Tessmann KH, Galindo O. 2004. Advertising to children in Mexico. Young Consumers 6(4):82–85.
Bandini LG, Must A, Cyr H, Anderson SE, Spadano JL, Dietz WH. 2003. Longitudinal changes in the accuracy of reported energy intake in girls 10–15 years of age. American Journal of Clinical Nutrition 78(3):480–484.
Barker DJ. 1992. Fetal growth and adult disease. British Journal of Obstetrics and Gynaecology 99(4):275–276.
Barquera S, Rivera-Dommarco J, Safdie M, Flores-Aldana M, Campos-Nonato I, Campirano F. 2003. Energy and nutrient intake in pre-school and school-age Mexican children: National Nutrition Survey 1999. Salud Pública de México 45(4):540–550.
Barquera S, Hotz C , Rivera J, Tolentino L, Espinoza J, Campos I, Shamah T. In press. Food consumption, food expenditure, anthropometric status, and nutrition-related diseases in Mexico. In: Kennedy et al., eds. Double-Burden of Malnutrition in Developing Countries. Rome, Italy: Food and Agricultural Organization. Pp. 161–204.
Bray GA, Nielsen SJ, Popkin BM. 2004. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. American Journal of Clinical Nutrition 79:537–543.
Brewis A. 2003. Biocultural aspects of obesity in young Mexican school children. American Journal of Human Biology 15:446–460.
Caballero B. 2001. Early nutrition and risk of disease in the adult. Public Health Nutrition 4(6a):1335–1336.
Campirano F, Barquera S, Haas J, Téllez-Rojo M, Rivera-Dommarco J. 2003. Estimación del sub-reporte de energía en mujeres mexicanas obesas y no obesas. In: Barquera S, ed. Aspectos de Alimentación y Nutrición en México. Cuernavaca, México: Instituto Nacional de Salud Pública. Pp. 24–33.
Chagnon VC, Wilmore JH, Borecki IB. 2000. Association between the leptin receptor gene and adiposity in middle-aged Caucasian males from the heritage family study. Journal of Clinical Endocrinology and Metabolism 85:29–34.
Champagne CM, Baker NB, DeLany JP, Harsha DW, Bray GA. 1998. Assessment of energy intake underreporting by doubly labeled water and observations on reported nutrient intakes in children. Journal of the American Dietetic Association 98(4):426–433.
COFETEL (Comisión Federal de Telecomunicaciones). 2005. Dirección General de Tarifas e Integración Estadística. [Online]. Available: http://www.inegi.gob.mx [accessed November 11, 2005].
Cruz M, Torres M, Aguilar-Herrera B, Perez-Johnston R, Guzman-Juarez N, Aranda M, Kumate J. 2004. Type 2 diabetes mellitus in children—an increasing health problem in Mexico. Journal of Pediatric Endocrinology and Metabolism 17(2):183–190.
Du S, Mroz TA, Zhai F, Popkin BM. 2004. Rapid income growth adversely affects diet quality in China—particularly for the poor. Social Science and Medicine 59(7):1505–1515.
Fernald LC, Gutiérrez JP, Neufeld LM, Olaiz G, Bertozzi SM, Mietus-Snyder M, Gertler PJ. 2004. High prevalence of obesity among the poor in Mexico. Journal of the American Medical Association 291(21):2544-2545.
Fernandez JR, Shiver MD. 2004. Using genetic admixture to study the biology of obesity traits and to map genes in admixed populations. Nutrition Review 62(7):S69–S74.
Friedman AE, Dickler H. 2003. International Advertising Clearance. Amsterdam, Netherlands: Global Advertising Lawyers Alliance.
Friend B, Stapylton-Smith M. 1999. Through the Eyes of Children. Presentation at the ESOMAR Marketing in Latin America Conference. Santiago, Chile. April 1999.
Frongillo EA, de Onis M, Hanson KM. 1997. Socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting of children. Journal of Nutrition 127(12):2302–2309.
Gardner LI, Stern MP, Haffner SM, Gaskill SP, Hazuda HP, Relethford JH, Eifler CW. 1984. Prevalence of diabetes in Mexican Americans: Relationship to percent of gene pool derived from native American sources. Diabetes 33(1):86–92.
González-Castell D, Rivera-Dommarco J, González-Cossío T, Barquera-Cervera S. 2003. Contribución de los alimentos industrializados en la ingestión de energía, macronutrimentos y fibra en niños mexicanos de 1 a 4 años. M.S. Thesis. Cuernavaca, Morelos, México: Escuela de Salud Pública de México, Instituto Nacional de Salud Pública.
Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. 1996. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Archives of Pediatrics and Adolescent Medicine 150(4):356–362.
Gutiérrez-Trujillo G. 2005. Cobertura de los programas integrados de salud (PREVENIMSS): Promoción de la salud, nutrición, salud reproductiva, prevención, detección y control de
enfermedades. In: Martínez-Salgado et al., eds. Las Múltiples Facetas de la Investigación en Salud. Instituto Mexicano del Seguro Social. Pp. 91–114.
Gutiérrez JP, Gertler P, Hernández Avila M, Bertozzi S. 2005. Impacto de Oportunidades en los comportamientos de riesgo de los adolescentes y en sus consecuencias inmediatas. Resultados de corto plazo en zonas urbanas y de mediano plazo en zonas rurales. In: Hernández Prado B, Hernández Avila M., eds. Evaluación Externa de Impacto del Programa Oportunidades 2004. Vol II. Cuernavaca, México: Instituto Nacional de Salud Pública Pp. 77–120.
Habicht JP, Martorell R, Yarbrough C, Malina RE, Klein RE. 1974. Height and weight standards for preschool children. How relevant are ethnic differences in growth potential? Lancet 1(7858):611–614.
Hales CN, Barker DJ. 2001. The thrifty genotype hypothesis. British Medical Bulletin 60: 5–20.
Hawkes C. 2002. Marketing activities of global soft drink and fast food companies in emerging markets: A review. In: Globalization, Diets, and Non-Communicable Diseases. Geneva, Switzerland: World Health Organization.
Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. 1999. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico City. International Journal of Obesity 23:845–854.
Hernández B, de Haene J, Barquera S, Monterrubio E, Rivera J, Shamah T, Sepúlveda J, Haas J, Campirano F. 2003. Factores asociados con la actividad física en mujeres mexicanas en edad reproductiva. Rev Panam Salud Pública/Pan American Journal of Public Health 14(4):235–245.
Horton ES. 1983. Introduction: An overview of the assessment and regulation of energy balance in humans. American Journal of Clinical Nutrition 38(6):972–977.
INEGI (Instituto Nacional de Estadística, Geografía e Informática). 2000. Estados Unidos Mexicanos. XII Censo General de Población y Vivienda 2000. Base de Datos de la Muestra Censal, Cuestionario Ampliado, México. [Online]. Available: http://www.inegi.gob.mx [accessed November 11, 2005].
INEGI. 2005a. Encuesta Nacional sobre Disponibilidad y Uso de Tecnología de la Información y Comunicaciones en los Hogares. [Online]. Available: http://www.inegi.gob.mx [accessed November 11, 2005].
INEGI. 2005b. Estadísticas de Transportes. [Online]. Available: http://www.inegi.gob.mx [accessed November 11, 2005].
IOM (Institute of Medicine). 2001. Dietary Reference Intakes. Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press.
IOM. 2005. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. 2000. CDC growth charts. Advanced Data 314:1–27.
Lucas A, Fewtrell MS, Cole TJ. 1999. Fetal origins of adult disease—the hypothesis revisited. British Medical Journal 319:245–249.
McDonald’s Corporation. 2006. McDonald’s 20 Años Conmigo. [Online]. Available: http://www.mc20.com.mx [accessed May 5, 2006].
Mei Z, Grummer-Strawn L, Pietrobelli A, Goulding A, Goran M, Dietz W. 2002. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. American Journal of Clinical Nutrition 75:978–985.
Ministry of Health. 2006. Secretaria de Salud. [Online]. Available: http://www.salud.gob.mx [accessed May 7, 2006].
Monterrubio-Flores EA. 2006. Curvas percentilares de talla edad de niños mexicanos de 2 a 9 años con características sociodemográficas asociadas a un buen crecimiento: Datos de la ENN II. M.S. Thesis. Escuela de Salud Publica de México. Instituto Nacional de Salud Pública, Cuernavaca, Morelos, México.
Neel JV. 1962. Diabetes mellitus: A “thrifty” genotype rendered detrimental by “progress”? American Journal of Human Genetics 14:353–362.
Neufeld L, García-Guerra A, Leroy F, Flores López ML, Fernández Gaxiola AC, Rivera-Dommarco JA. 2005. Impacto del Programa Oportunidades en Nutrición y Alimentación en Zonas Urbanas de México. [Online]. Available: http://evaloportunidades.insp.mx/441c7c1a3d30adf64e0e724174a9d527/impacto/2005/insp_2005_nutricion.pdf [accessed November 10, 2006].
Neufeld LM, Dominguez-Islas C, García-Guerra A, García-Feregrino R, Rivera-Dommarco J. 2006. Increase in body mass index over a two year period in women from urban Mexico. Experimental Biology Meeting, San Francisco, April 1–5. Experimental Biology 2006 Meeting Program. Abstract 638.7. P. 988.
Neufeld L, Sotres-Alvarez D, García-Feregrino R, García-Guerra A, Tolentino-Mayo L, Fernald L, Rivera-Donmarco J. 2005. Estudio comparativo sobre el estado nutricional y la adquisición de lenguaje entre niños de localidades urbanas con y sin Oportunidades. In: Hernández B, Hernández-Ávila M, eds. Evaluación Externa de Impacto del Programa Oportunidades 2004, Tomo III. Alimentación. México, D.F. Pp. 89–115.
Norma Oficial Mexicana. 2005. NOM-043-SSA2-2005, Servicios básicos de salud. Promoción y educación para la salud en materia alimentaria. Criterios para brindar orientación.
OECD (Organisation for Economic Co-operation and Development). 2005. OECD Health Data 2005. How Does Mexico Compare? [Online]. Available: http://www.oecd.org/dataoecd/16/2/34970198.pdf [accessed January 15, 2006].
Oksanen L, Ohman M, Heiman M. 1997. Markers for the gene ob and serum leptin levels in human morbid obesity. Human Genetics 99:559–564.
Olaiz G, Rojas R, Barquera S, Shamah T, Aguilar C, Cravioto P, Lopez P, Hernández M, Tapia R, Sepúlveda J. 2003. La Salud de los Adultos. In: Sepúlveda, J, Ed. Encuesta Nacional de Salud 2000, Tomo II. Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública.
Patrick H, Nicklas TA. 2005. A review of family and social determinants of children’s eating patterns and diet quality. Journal of the American College of Nutrition 24(2):83–92.
Popkin BM. 2001. The nutrition transition and obesity in the developing world. Journal of Nutrition 131:871S–873S.
Resano-Pérez E, Méndez-Ramírez I, Shamah-Levy T, Rivera JA, Sepúlveda J. 2003. Methods of the 1999 National Nutrition Survey. Salud Pública de México 45 (4S):s558–s564.
Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Gillman MW, Hennekens CH, Speizer FE, Manson JE. 1999. Birthweight and the risk for type 2 diabetes mellitus in adult women. Annals of Internal Medicine 130(4):278–284.
Rivera JA, Shamah-Levy T, Villalpando-Hernández S, González de Cossio T, Hernández-Prado B, Sepúlveda J. 2001. Encuesta Nacional de Nutrición 1999. Estado Nutricional en Niños y Mujeres en México. Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública.
Rivera JA, Barquera S, Campirano F, Campos I, Safdie M, Tovar V. 2002. Epidemiological and nutritional transition in Mexico: Rapid increase of non-communicable chronic diseases and obesity. Public Health Nutrition 5(1A):113–122.
Rivera JA, Sepúlveda-Amor J. 2003. Conclusions from the Mexican National Nutrition Survey 1999: Translating results into nutrition policy. Salud Pública de México 45 (S4):S565– S575.
Rivera JA, Barquera S, González-Cossio T, Olaiz G, Sepúlveda J. 2004a. Nutrition transition in Mexico and in other Latin American countries. Nutrition Review 62(7):S149–S157.
Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. 2004b. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: A randomized effectiveness study. Journal of the American Medical Association 291(21):2563–2570.
Robinson TN. 2001. Television viewing and childhood obesity. Pediatric Clinics of North America 48(4):1017–1025.
Rodríguez-Moran M, Salazar-Vazquez B, Violante R, Guerrero-Romero F. 2004. Metabolic syndrome among children and adolescents aged 10–18 years. Diabetes Care 27(10):2516– 2517.
Rosenbaum M, Leibel R. 1998. The physiology of body weight regulation. Relevance to the etiology of obesity in children. Pediatrics 101:525–539.
Secretaría de Comunicaciones y Transportes, Dirección General de Sistemas de Radio y Televisión. 2005. [Online]. Available: http://www.inegi.gob.mx [accessed November 11, 2005].
Secretaría de Educación Pública. 1994. Educación física. In: Fernández Editores SA de CV eds. Educación Básica Primaria, Plan y Programas de Estudio. México. D.F.: Pp. 149–162.
SEDESOL (Secretaría de Desarrollo Social). 2006. Oportunidades, reglas de operación 2006 Mexico DF, Secretaria de desarrollo social: Programa Oportunidades.
Seidell JC. 2000. Obesity, insulin resistance, and diabetes—A worldwide epidemic. British Journal of Nutrition 83:S5–S8.
Simmons R. 2005. Perinatal programming of obesity. Experimental Gerontology 40:863–866.
Snyder EE, Brandon W, Perusse L, Chagnon S, Weinagel J, Rankinen T, Bouchard C. 2004. The human obesity gene map: The 2003 update. Obesity Research 12(3):369–439.
Stein AD, Ravelli AC, Lumey LH. 1995. Famine, third-trimester pregnancy weight gain, and intrauterine growth: The Dutch Famine Birth Cohort Study. Human Biology 67(1): 135–150.
Stein AD, Conlisk A, Torin B, Schroeder DG, Grajeda R, Martorell R. 2002. Cardiovascular disease risk factors are related to adult adiposity but not birth weight in young Guatemalan adults. Journal of Nutrition 132(8):2208–2214.
Stern MP, Bartley M, Duggirala R, Bradshaw B. 2000. Birth weight and the Metabolic Syndrome: Thrifty phenotype or thrifty genotype? Diabetes Metabolism Research and Reviews 16:88–93.
Swallen KC, Reither EN, Haas SA, Meier AM. 2005. Overweight, obesity, and health-related quality of life among adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics 115(2):340–347.
Trowbridge R, Mendoza F. 2007. Preventing obesity in Mexican–American children and youth. In: Institute of Medicine (IOM). Joint U.S.–Mexico Workshop on Preventing Obesity in Children and Youth of Mexican Origin. Washington, DC: The National Academies Press.
Uauy R, Albala C, Kain J. 2001. Obesity trends in Latin America: Transiting from under- to overweight. Journal of Nutrition 131:893S–899S.
Villa-Caballero L, Caballero-Solano V, Chavarria-Gamboa M, Linares-Lomeli P, Torres-Valencia E, Medina-Santillan R, Palinkas LA. 2005. American Journal of Preventive Medicine 30(3):197–203.
Villalpando S, García-Guerra A, Ramírez-Silvia CI, Mejía-Rodríguez F, Matute G, Shamah T, Rivera JA. 2003a. Iron, zinc and iodine status in Mexican children under 12 years and women 12–49 years of age: A probabilistic national survey. Salud Pública de México 45 (4S):S520–S529.
Villalpando S, Montalvo-Velarde I, Zambrano N, García-Guerra A, Ramírez-Silva CI, Shamah T, Rivera JA. 2003b. Vitamins A and C and folate status in Mexican children under 12 years and women 12–49 years: A probabilistic national survey. Salud Pública de México 45(4S):S508–S519.
Villalpando S, Shamah-Levy T, Ramírez-Silva CI, Mejía-Rodríguez F, Rivera JA. 2003c. Prevalence of anemia in children 1 to 12 years of age: Results from a nation-wide probabilistic survey in Mexico. Salud Publica de Mexico 45(4S):S490–S498.
Villalpando S, Carrión C, Barquera S. In press. The body mass index is associated with hyperglycemia and alterations of some components of the metabolic syndrome in Mexican adolescents aged 10–19 years. Salud Pública de México.
Villareal-Calderón A, Acuna H, Villareal-Calderon J, Garduno M, Henriquez-Roldan CF, Calderon-Garciduenas L, Valencia Salazar G. 2002. Assessment of physical education time and alter-school outdoor time in elementary and middle school students in south Mexico city: The dilemma between physical fitness and the adverse health effects of outdoor pollutant exposure. Archives of Environmental Health 57(5):451.
WHO (World Health Organization). 2004. Global Strategy on Diet, Physical Activity, and Health. Report No. WHA57.17. [Online]. Available: http://www.who.int/gb/ebwha/pdf_files/WHA57/A57_R17-en.pdf [accessed May 7, 2006].
WHO (World Health Organization). 2006a. The WHO Child Growth Standards. [Online]. Available: http://www.who.int/childgrowth/en [accessed May 5, 2006].
WHO. 2006b. Preventing Chronic Diseases: A Vital Investment. World Health Organization: Geneva, Switzerland. [Online]. Available: http://www.who.int/chp/chronic_disease_report/full_report.pdf [accessed May 5, 2006].
WARC (World Advertising Research Center). 2005. The Americas Marketing Pocket Book 2005. Oxfordshire, UK: WARC.
WCRF (World Cancer Research Fund). 1997. Food, Nutrition, and the Prevention of Cancer: A Global Perspective. Washingtron, DC: American Institute for Cancer Research.
Zahniser S, Young E, Wainio J. 2005. Recent Agricultural Policy Reforms in North America. Economic Research Service, U.S. Department of Agriculture WRS-05-03. [Online]. Available: http://www.ers.usda.gov/publications/WRS0503/wrs0503.pdf [accessed May 8, 2006].















































