2
Sustainable Healthcare Facilities
In 2004 the healthcare industry in the United States constituted 16 percent of the country’s gross domestic product. Today, the United States is experiencing one of the largest healthcare facility building booms since the Hospital Survey and Construction Act, commonly referred to as the Hill-Burton Act, was passed in 1946 (Public Law 79-725). New technologies and new competitive pressures affect health care as more people are moving to the suburbs and older city hospitals are becoming obsolete. Hospital design transformation requires looking for new ways to improve healthcare quality and recognizing the relationship between medical services, environment, and diseases. Visionary thinking, connecting sustainability to health, and pollution prevention are important for the future of the healthcare industry.
The first session of the workshop is summarized in this chapter and includes presentations by Craig Zimring, Robin Guenther, and Knut Bergsland. This portion of the workshop explored the agendas involved in green health care and provided examples of sustainable healthcare facilities and the methods and tools employed in their design and operation. The information provided is drawn from the insights and experience of the presenters, and some of the current standards and best practices being implemented in green healthcare institutions today.
GREEN BUILDING AND HEALTH AGENDAS: POINTS OF CONVERGENCE
Because modern healthcare facilities are large consumers of resources, they provide an opportunity to make changes or reduce the consumption of these resources. Despite financial pressures, they are dedicated to helping people and can be models for other institutions, said Craig Zimring of the Georgia Institute of Technology. According to Zimring, there are two agendas for green health care: the green agenda and the design-as-quality-support (DQS) agenda. The
green agenda is a multilevel analysis of socioeconomic health impacts at multiple scales, ranging from a building’s occupants to society as a whole. The DQS agenda converges with the green agenda but differs, according to Zimring, in some important ways. Similar to the green agenda, the DQS agenda advances social and economic goals, but it focuses on using design to improve quality and safety outcomes, such as error and infection reduction, staff turnover, length of stay, and patient and family satisfaction. In this agenda, design is viewed as a tool that can affect healthcare outcomes for patients, staff, and the institution as a whole.
Relationship Between the Two Agendas
The green agenda is based on the notion of a virtuous cycle explained Zimring. Designing, constructing, and managing a hospital in accordance with principles of sustainable development can benefit the local community, the economy, and the environment. It can improve public health as well as reduce the demand for health services.
In contrast, the DQS agenda approaches construction from a slightly different perspective. Similar to evidence-based medicine, in which healthcare decisions can be made based on the best evidence about the outcome of those decisions, evidence-based design decisions are based on the best predictions about their outcome, asserted Zimring. Evidence-based design is the conscientious, explicit, and judicious use of current best evidence in making design decisions that advance an organization’s goals. DQS involves a process in which one understands the evidence, makes hypotheses, tests the outcomes, and works back into decision making.
Part of the DQS agenda is based on two Institute of Medicine (IOM) reports: To Err Is Human: Building a Safer Health System (IOM 2000) and Crossing the Quality Chasm: A New Health System for the 21st Century (IOM 1999). In To Err Is Human, the IOM extrapolated that as many as 98,000 people die each year from preventable medical errors. Furthermore, there are approximately 2 million hospital-acquired infections in the United States, and as many as 88,000 people die from those infections (CDC, 2000). Zimring observed that even at the lower end of these numbers, more people in the United States die from hospital-acquired preventable adverse events than from other leading causes of death, such as AIDS, breast cancer, and motor vehicle accidents (IOM, 2000).
One of the reasons why these safety problems occur is that the most experienced caregivers in hospitals—nurses—have a very high turnover rate, noted Zimring. Concern about safety, quality, and nursing turnover has contributed to a “quality revolution” and the belief that healthcare institutions can make a dramatic improvement in healthcare quality and safety through better information and strategic action. This initiative is led by such organizations as the Institute for Healthcare Improvement, the Center for Health Design, and others.
Role of the Physical Environment in Green Building and Health
Zimring observed that there is a large and growing body of evidence demonstrating the role of the physical environment in achieving healthcare quality and safety. For example, a recent meta-analysis of more than 600 primarily peer-reviewed studies found associations between the physical environment and patient and staff outcomes in four areas: reduced staff stress and fatigue and increased effectiveness in delivering care; improved patient safety; reduced patient stress and improved health outcomes; and improved overall healthcare quality (Ulrich et al., 2004). For example, access to views and natural light in healthcare facilities can have important stress-reducing effects, as well as reduce pain and the length of stay at the hospital (Ulrich, 1991). In their meta-analysis review, the authors observe that hospitals are complex systems in which it is difficult to isolate the impacts of individual factors and suggest that design-based evidence parallels evidence-based medicine for improving health care. Zimring recommended additional research in the area of evidence-based design to understand how hospital design affects health.
In conclusion, he described the green agenda as encompassing ecological health on multiple scales. It credits environmental initiatives, such as reduced resource use, and it aims for improved patient outcomes. The green agenda does not guarantee that recycled floor surfaces or less outgassing of chemicals from products will result in better care or more rapid recovery, cautioned Zimring. In reinventing hospitals and transforming their design, design is a tool to improve quality, safety, and experience.
HIGH-PERFORMANCE HEALING ENVIRONMENTS
As construction technology advanced during the past century, the design of hospitals changed from daylit, naturally ventilated, pavilion-style buildings to high-rise buildings with mechanically conditioned air, said Robin Guenther of Guenther 5 Architects. Bellevue Hospital in New York City is a prime example of this change. It was built on a site near nature, overlooking the East River, before the expertise was available to build high-rise buildings or provide mechanical ventilation. At that time, hospitals needed access to clean air and fresh water to heal people. The facility has continued to expand and based on blueprint calculations, Guenther reported that Bellevue Hospital now has 60,000 square feet of floor space, an acre and a half footprint, and less than 10 percent of the building has a window.
Because projections for construction in the healthcare sector are for approximately 100 million square feet per year, Guenther suggested that architects need to identify new models for healthcare facilities. Today’s healthcare facilities are buildings that are low in thermal mass—they heat up too quickly and cool down too rapidly—and are heavily dependent on artificial systems, such as lighting,
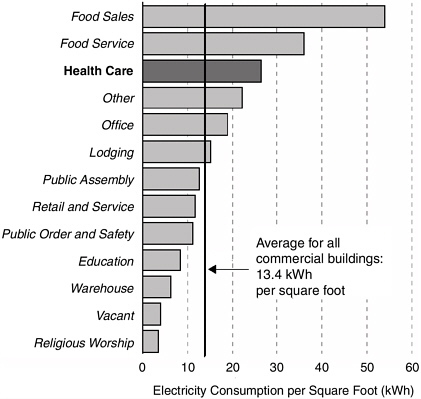
FIGURE 2-1 Healthcare facilities annually consume nearly twice the energy of an average commercial building.
SOURCE: Energy Information Administration, 1995 Commercial Buildings Energy Consumption Survey.
ventilation, and interior environments. Healthcare facilities consume nearly twice the annual energy of an average commercial office building (Figure 2-1).*
Even with healthcare expenditures constituting roughly 16 percent of the GDP, healthcare facilities are unable to keep up with demand and upgrade older facilities. Many of the structures built in the United States during the Hill-Burton Act era, particularly urban medical centers, are challenged by real estate and capital issues and are in need of replacement, said Guenther.
Leadership in Energy and Environmental Design
In the past two decades, the link between buildings and health has received considerable attention. Many media reports have highlighted the problem of indoor air toxins in sealed buildings. The October 2003 issue of Metropolis magazine was entitled “Architects Pollute,” and placed a large share of the responsibility for contributing to global warming on the shoulders of architects. An article within the issue asserted that architects and the construction industry are responsible for half of America’s energy consumption and half of its green-house gas emissions produced by burning coal, gasoline, and other fossil fuels (Hawthorne, 2003).
Americans’ growing concern that buildings do impact their health has influenced the federal government’s decision to support green building. In its report The Federal Commitment to Green Building: Experiences and Expectations, green buildings are defined as “the practice of (1) increasing the efficiency with which buildings and their sites use energy, water, and materials, and (2) reducing building impacts on human health and the environment through better siting, design, construction, operation, maintenance, and removal—the complete building life cycle” (OFEE, 2003).
The U.S. Green Building Council developed Leadership in Energy and Environmental Design (LEED) as “a nationally accepted benchmark for the design, construction, and operation of high performance green buildings. The LEED rating system is the current best practice standard for the building sector. LEED gives building owners and operators the tools they need to have an immediate and measurable impact on their buildings’ performance. LEED promotes a whole-building approach to sustainability by recognizing performance in five key areas of human and environmental health: sustainable site development, water savings, energy efficiency, materials selection, and indoor environmental quality” (U.S. Green Building Council, 2006).
Initially, LEED was created as a tool for the for-profit sector, which needed motivation to use emerging green building technologies, and was based on the premise that the nonprofit sector would embrace green building technologies as a component of their mission. LEED certification is given to the top 25 percent of green-performing buildings in the United States. With levels that include Certified, Silver, Gold, and Platinum, certification is achieved based on a third-party checklist of strategies for building, design, and construction. Of the approximately 1,800 registered projects in the LEED system in 2004, only 2 percent of these projects were in the healthcare industry (Kozlowski, 2004).
Examples of LEED Construction in Health Care
A few noteworthy LEED projects in health care include Emory University’s Winship Cancer Institute in Atlanta, Georgia; the Dell Children’s Medical Center
in Austin, Texas; Boulder Community Foothills Hospital in Boulder, Colorado; and the Patrick H. Dollard Health Center in Harris, New York.
Emory University’s Winship Cancer Institute is a research and clinical facility for cancer patients that formally received certification in the U.S. Green Building Council’s LEED program in 2005. Input from patients influenced the design of the Infusion Center, which has more intimate clusters of space for four patients each and hip-high walls that personalize the space for family members while maintaining visibility for good nursing care. The building design seeks to create an atmosphere of life, health, and the ultimate hope for a cure.
Dell Children’s Medical Center in Austin, Texas, is a LEED-registered project that is pursuing certification at the Platinum level. A redevelopment located at the old Austin Municipal Airport, it is pursuing green strategies across the board; most notably, the integration of a combined heat and power facility that doubles the efficiency of electricity generation by utilizing waste heat for thermal energy. It is scheduled for occupancy in late 2007.
Boulder Community Foothills Hospital is a replacement women’s and children’s hospital. It is a green-field hospital built on previously undeveloped, degraded wetlands that were home to a large prairie dog colony. The hospital returned 32 restored acres of the 49-acre site to the community as permanent open space. The city of Boulder then built the hospital sustainably as a way to gain community support for development of the site, explained Guenther. The hospital architects focused on local and regional low-emitting materials, reduction of water use through xeriscaping (landscaping that does not require supplemental irrigation), low-flow fixtures, and energy reduction.
Another sustainable healthcare facility is the Patrick H. Dollard Discovery Health Center in upstate New York. It is a residential facility for developmentally disabled children and adults, and the medical staff has a keen interest in the impact of the environment on developmental disabilities. The Dollard Health Center construction strategies included high-reflectance roofing, reliance on local and regional recycled-content low-emitting materials, and elimination of polyvinyl chloride in finish materials and plumbing. By using ground source heat pumps, energy demand was reduced by 42 percent and onsite fossil fuel combustion was eliminated. In addition, the facility opted to purchase green power, said Guenther.
Green Guide for Health Care
First released in 2003, The Green Guide for Health Care filled a need in the marketplace for green building tools specifically for health care. According to its website, The Green Guide for Health Care is “the healthcare sector’s first quantifiable sustainable design toolkit integrating enhanced environmental and health principles and practices into the planning, design, construction, operations and maintenance of their facilities. This guide provides the healthcare sector
with a voluntary, self-certifying metric toolkit of best practices that designers, owners, and operators can use to guide and evaluate their progress toward high performance healing environments” (GGHC, 2006). The document has an explicit health-based focus. Before this connection, healthcare administrators often dismissed green building as having no relevance to health, viewing it as purely about saving the environment, noted Guenther. In 2002, the American Society for Healthcare Engineering (ASHE) developed the Green Healthcare Construction Guidance Statement, which articulated the need to protect health on three scales: building occupants, the surrounding local community, and the global community and resources (ASHE, 2002).
The core structure and content of The Green Guide for Health Care is based on existing tools, such as LEED, transferred and modified for health care. The document encourages best practices without certification and regulatory thresholds, and it bridges design and construction with operational considerations. The Green Guide for Health Care is a web-based, downloadable, free, open-source tool. In January 2006, the website registrants numbered approximately 6,800, with diverse geographic distribution; about 10 percent of the registrants are from outside the United States. With more than 60 projects actively based in the pilot program, a critical mass of healthcare projects are engaging in this work, noted Guenther.
The healthcare industry is beginning to recognize the relationship among medical services, the environment, and diseases. The first step was taken in 1998 when the American Hospital Association signed a voluntary memorandum of understanding with the U.S. Environmental Protection Agency pledging reductions in solid waste; avoidance of persistent, bioaccumulative, and toxic compounds; and virtual elimination of the use of mercury by 2005 (AHA, 1998).
Guenther concluded by noting the responsibility of the healthcare industry to build and operate sustainable buildings, if for no other reason than for the health of the building’s occupants. The healthcare industry has the opportunity to be a model for health-based, sustainable approaches to construction, food service, active living, and waste management. It should lead creative thinking and draw inspiration from such visionaries as the early environmentalist David L. Lawrence. As mayor of Pittsburgh, Lawrence implemented a dedicated urban renewal plan connecting sustainable buildings to health and pollution prevention. Kaiser Permanente is another visionary in health care; the company’s leadership in the industry is further discussed in Chapter 6.
BUILDING GREEN AND INTEGRATING NATURE: RIKSHOSPITALET UNIVERSITY HOSPITAL IN OSLO
Building green requires a big picture approach. At its core, planning and building green hospitals require that little harm be done to the macro- and micro-environments, noted Knut Bergsland of SINTEF Health Research. This approach
should be taken throughout the life cycle of the building and should include all support systems during its useful life. Healthcare facilities need to find the most important indicators for green hospital building. To establish a culture for green building, commitment must come from the top down, noted Bergsland. Without this leadership, it will be difficult to establish environmental values in hospitals.
The crucial, priority elements in hospital buildings are those that are
Access to nature is important to wellbeing. It is a deep-rooted human need that may even transcend cultural barriers.
—Knut Bergsland
most beneficial to health and require the least effort and use of resources. For example, access to nature is important to well-being. It is a deep-rooted human need that may even transcend cultural barriers, noted Bergsland. The importance of nature as a stress-reducing factor is long established (Ulrich, 1991). Thus, planning for maximum daylight and integrating nature into hospital design by as many means as possible are the right things to do in both the patient and work environments, asserted Bergsland.
Success Story of Green Hospital Building in Norway
Norway is a small country on the outskirts of Europe with 4.6 million inhabitants (approximately the population of Colorado) and a population density similar to that of Maine. Norway’s per capita gross domestic product is similar to that of the United States at approximately $48,000 (CIA, 2007), and 10 percent of it is spent on health care (Johnsen, 2006). According to Bergsland, the healthcare system in Norway is driven by the same forces as in most other Western countries—demographic change, new information and technologies, and demands for efficiency. Health care in Norway is delivered through a national system based on equal access to and distribution of services as the main principle. The Norwegian healthcare system is 90 percent public and tax based. Hospitals are owned by the state and run as trusts, inpatients do not pay for their stay, and physicians are employed by the hospital.
Rikshospitalet University hospital in Oslo has 1.5 million square feet of floor space and is located next to woodlands with views of the city and the Oslo fjord, noted Bergsland. It is a tertiary teaching hospital providing world-class medical services, such as transplant surgery. The hospital covers all clinical specialties except for geriatrics and psychiatry; it has 585 beds, excluding intensive-care beds. The hospital has 4,000 full-time-equivalent staff members, 35,000 inpatients, 20,000 day patients, and 160,000 outpatients per year. Between 2000 and 2004, inpatient activity in the Rikshospitalet increased by 22 percent, and outpatient activity increased by 66 percent (Bergsland, 2005).
The Rikshospitalet site—on cultivated land next to the existing medical fac-
ulty—was selected by the Norwegian Parliament over protests from environmental activists. The Rikshospitalet counters the notion that hospitals should be built on a flat site, noted Bergsland. Because the site is sloping and saucer shaped, it effectively hides the substantial building structure; big volumes can be hidden in the bottom of the saucer and make the hospital appear as a 3- to 4-story building, while it actually is 6 to 7 stories high. The hospital sits on 87 acres of land, the footprint for the entire construction is 430,560 square feet, and the main building is 322,920 square feet, noted Bergsland.
The architects’ vision for the physical environment of the hospital was a village-like horizontal layout with daylight in all spaces. The architects sought to reduce anxiety and build dignity for both patients and personnel, using natural materials whenever possible (Figure 2-2). The hospital planning process started in 1990 and involved 800 people, more than 15 percent of the total workforce, including medical staff. Because of the village concept, the hospital is seen as a town rather than a building: it has a main street, a square, and a landmark tower.
The main street facilitates way finding because intersections are unique, not identical, as they tend to be in most modern hospitals. The Rikshospitalet’s curving main street is a device for patients to draw a mental picture of the route to their destination. The curvature hides the length of the corridor—280 meters long—and the traffic hierarchy minimizes the need for signage. The art and nature at the intersections help people remember their location and aid recognition. Recognition facilitates the trip, and the shortest distance to one’s destination is not a straight line, but the most beautiful route.
The main street is also a place of positive distractions; for example, concerts are held on the street at least once a month. Art is an integrated part of the building; 0.9 percent of the total building budget was earmarked for art in the hospital. Art may have similar effects on stress reduction as nature, noted Bergsland. The main plaza of the hospital faces south, creating sunny spots along the perimeter. Norway is a cold country with a low sun, and the extra light is welcome.
Integrating nature was part of the hospital design; there is a walking trail next to the site, with a creek running between the trail and the hospital (Figure 2-3). Some patients use the woods next to the hospital as part of their therapy, said Bergsland. Natural stone was used in the main street, the floors, and street furniture; wood was used in benches, chairs, reception desks, and the cafeteria. Great care was taken to preserve existing trees. Views to the outside from the main street open up to green spaces and courtyards, and there are places for contemplation. This feature also illustrates that Rikshospitalet is a friendly, non-frightening building. It is very distinct from the big clinical machines that are commonly seen, noted Bergsland.
The main entrance of the central plaza is a tower that creates the first impression of the hospital. According to Bergsland, the first impression of a building plays a disproportionate role in the conception of what comes after, such as com-

FIGURE 2-2 The village structure of the main street at Rikshospitalet aids recognition and facilitates way finding. Integrated art serves as a stress reducer. Natural daylight creates space efficiency and evokes a positive response from patients and staff.
SOURCE: Rikshospitalet Information Department, unpublished (2005). Reprinted with permission.
FIGURE 2-3 This hospital’s architects focused on designing a humanizing environment, not minimizing the footprint. The main street is the backbone of the hospital and encourages informal meeting between staff. Walkways connect patient units with treatment facilities.
SOURCE: Rikshospitalet Information Department, unpublished (2005). Reprinted with permission.
munication with a doctor. The staff cafeteria is located next to the main entrance, which facilitates informal meetings among staff members. Walkways on three levels connect the patient units with treatment facilities across the main street. Inpatients are taken to treatment across the street in their beds.
The hospital is accessible by public transportation. Oslo city authorities extended an existing rail track when the hospital was planned, and today connections to central Oslo run every eight minutes. For those who drive to the hospital, the parking structure is a 4-minute walk to the main entrance. Bicycle parking is located outside the hospital, under the main plaza.
Energy Use in the Rikshospitalet
In terms of energy use, the Rikshospitalet is not an exemplar project, noted Bergsland. It uses more energy per square meter than most other Norwegian
hospitals. Increased clinical demand has resulted in a need for extra capacity and ventilation, and some system limits have been passed. However, the glassed roof brings Norwegian winter light into the main street of the hospital, and the extra energy that is required to keep the street at 17°C in the winter is more than outweighed by the positive effect on staff morale, said Bergsland. The hospital tries to be environmentally conscious about its energy use, and, despite a 20-percent increase in clinical services in 3 years, it reduced its energy use by 10 percent (Bergsland, 2005).
The positive feedback from the people who are using the building more or less corroborates the concept that the architects suggested, said Bergsland. A preliminary study on the effects of hospital design on patient attitudes, activity patterns, productivity, and staff morale at the Rikshospitalet was performed in 2004. The results showed that people liked the building because it was interesting and nonfrightening, and they thought the main street was perfect for interaction (Bergsland, 2005). Among other positive factors cited was daylight in working and patient spaces and good functional proximities between related departments. Also, the art made staff feel proud of their environment.
Patients ranked the Rikshospitalet highly. Furthermore, productivity measures increased, and absenteeism and turnover rates decreased. The average sick leave in Norwegian hospitals is approximately 8 percent. After moving to the new building, the Rikshospitalet personnel’s sick leave rate declined from 8 to 6 percent (Bergsland, 2005).
The building concept may have played a role in achieving patient and staff satisfaction, said Bergsland, but is difficult to determine the role of design on activity, productivity, or medical outcomes. Such factors as the Hawthorne effect,† moving into new premises, organizational changes, and staffing levels may influence outcomes to a degree that is difficult to establish.












