|
6 PEPFAR’s Care Category Summary of Key Findings
|
|
Recommendation Discussed in This Chapter Recommendation 6-1: The U.S. Global AIDS Coordinator should continue to promote and support a community-based, family-centered model of care in order to enhance and coordinate supportive care services for people living with HIV/AIDS, with special emphasis on orphans, other vulnerable children, and people requiring end-of-life care. This model should include integration as appropriate with prevention and treatment programs and linkages with other public-sector and nongovernmental organization services within and outside of the health sector, such as primary health care, nutrition support, education, social work, and the work of agencies facilitating income generation. |
6
PEPFAR’s Care Category
CATEGORY, TARGET, AND RESULTS
The Care Category
The President’s Emergency Plan for AIDS Relief (PEPFAR) defines care as “palliative care” (see Box 6-1); care for children orphaned or made vulnerable due to HIV/AIDS (discussed in Chapter 7) is explicitly included in the definition (OGAC, 2004). The Office of the U.S. Global AIDS Coordinator (OGAC) provided further clarification of operational definitions and strategies for care in Final Draft HIV/AIDS Palliative Care Guidance #1: An Overview of Comprehensive HIV/AIDS Care Services in the President’s Emergency Plan for AIDS Relief (OGAC, 2005c), issued in final form in February 2006.
In the United States, the term “palliative care” denotes end-of-life or hospice care provided by trained health professionals and volunteers in the last 6 months of a person’s life. The definition adopted by PEPFAR is broader and based on that of the World Health Organization (WHO). According to WHO, palliative care is “an holistic approach to improve the quality of life of patients with incurable disease and their families through the prevention and relief of suffering by means of early identification and careful assessment and treatment of pain and other problems, physical, psychosocial and spiritual” (WHO, 2004c, p. 7). PEPFAR defines palliative care as encompassing five domains: clinical, psychological, spiritual, social, and preventive care for HIV-infected people. The PEPFAR definition
|
BOX 6-1 PEPFAR’s Definition of Palliative Care PEPFAR defines palliative care as: … patient and family-centered care [which] optimizes the quality of life of adults and children living with HIV though the active anticipation, prevention, and treatment of pain, symptoms and suffering from the onset of HIV diagnosis through death. It also provides the routine monitoring that is essential to determine the optimal time to initiate ART, but continues during and after the initiation of treatment. [It] includes and goes beyond medical management of infections, neurological, or oncological complications of HIV/AIDS to comprehensively address symptoms and suffering throughout the continuum of HIV disease. Routine, confidential counseling and testing is an essential component of palliative care to identify those who need or will need palliative care, family members who could also be infected and in need of care, and family members and partners not infected and in need of prevention. SOURCE: OGAC, 2006d, p. 3. |
is consistent with the WHO standard with several exceptions, the most significant of which are in the domain of clinical care. WHO includes both antiretroviral therapy (ART) and services to prevent mother-to-child transmission of HIV in the clinical care domain. By contrast, OGAC includes in that domain only routine follow-up to determine the best timing for initiation of ART, placing ART itself in PEPFAR’s treatment category, and includes services to prevent mother-to-child transmission in the prevention category. In addition, pain management and prevention/management of opportunistic infections are funded under PEPFAR’s care category, but are placed operationally under the treatment category. The Committee was unable to determine whether this creates challenges to ensuring that these services are a consistent part of home-based care and programs. OGAC also supports voluntary counseling and testing activities with funds from the care category, but the Leadership Act places these activities in the prevention category (OGAC, 2004). One last difference is what WHO describes as the domains of “socioeconomic care” and “human rights and legal support.” It appears that PEPFAR combines these activities into one domain that it calls “social care.” Table 6-1 shows a comparison of the WHO and PEPFAR definitions of comprehensive care; the types of providers for the services listed are shown in parentheses if they are identified.
PEPFAR divides care services into three budgeting and reporting subcategories: (1) routine care for HIV/AIDS and care for tuberculosis (TB),
(2) voluntary counseling and testing, and (3) care-related training. These services can be provided in a variety of settings, including individual homes and community facilities, such as day care centers, outpatient clinics, health centers, workplace facilities, hospice centers, and university/hospital-based centers. The Leadership Act mandates that 15 percent of all funds allocated to the focus countries be designated for palliative care services (OGAC, 2004). Funding for the care category (including funds for services to orphans and other vulnerable children) as a percentage of all resources allocated for prevention, treatment, care, and other program support activities has remained steady (see Chapter 3).
Target
Unlike the prevention and treatment categories, the care category was not assigned a specific target in the Leadership Act. The 5-year target of care for 10 million people, including orphans and other vulnerable children, was identified in the PEPFAR strategy (OGAC, 2004). Note that although millions of people have received counseling and testing services, which are seen as the point of entry for care and treatment services, OGAC is counting these people toward neither the target of 10 million people receiving care nor any other PEPFAR target.
Like the treatment target, the care target is a count of people receiving services and does not provide information about the quality or impact of those services. With the data currently available, it is not possible to determine whether the care services PEPFAR is supporting are of sufficient and equal quality, duration, and type; offered by knowledgeable and skilled providers who receive adequate and appropriate supervision at all levels (a question that applies especially to in-home volunteers and community health workers); or meet the needs of those being served. It is also difficult to determine how people served have been counted toward the care target as the definition of a person served has changed over the life of PEPFAR to become more rigorous and to be more consistent with global norms.
Results
As shown in Table 6-2, the number of people OGAC reported as having received routine care services has steadily increased each year. By fiscal year 2005, the number of people receiving routine care more than doubled. In fiscal year 2006, however, there was a decline in the number of people who received TB treatment as part of their care services, compared to the previous fiscal year. Through September 30, 2006, PEPFAR had cumulatively supported voluntary counseling and testing for nearly 19 million men, women, and children (OGAC, 2007a). Of equal significance for the
TABLE 6-1 Comparison of WHO and PEPFAR Definitions of Comprehensive Care for Adults and Children Affected by HIV/AIDS
|
Domain |
WHO |
PEPFAR |
|
Clinical Care (accessible to everyone regardless of age and gender) |
(Medical and nursing staff)
|
(Physicians, clinical officers, nurses, midwives, traditional healers, community health workers, volunteers)
|
|
Psychological Support (patient and family support to assist in disclosure) |
|
|
|
Socioeconomic Support (material support, economic security, food security to meet daily living needs) |
|
Equivalent activities are in the “social care” domain (WHO’s “human rights and legal support” domain—see below) |
|
Domain |
WHO |
PEPFAR |
|
Human Rights and Legal Support (available in health facilities, communities, and in the workplace to promote equal access to care) |
|
(PEPFAR calls this domain “social care”)
|
|
Spiritual Care (culturally appropriate and sensitive to individual and community religious beliefs and practices) |
Equivalent activities are in the “psychological support” domain |
|
|
Prevention for HIV-infected Individuals |
Not a separate category, but addressed by services and activities in several domains |
|
|
SOURCE: OGAC, 2006f; WHO, 2004c. |
||
TABLE 6-2 PEPFAR Care Results by Fiscal Year, 2004–2006
|
Category |
Fiscal Year 2004 |
Fiscal Year 2005 |
Fiscal Year 2006 |
|
Total people receiving VCT servicesa |
1,791,900 |
4,653,200 |
6,426,500 |
|
Routine care for HIV/AIDS (2004–2005)b |
455,800 |
1,397,200 |
Not applicable |
|
Routine care for HIV/AIDS (2006)b |
Not applicable |
Not applicable |
2,464,000 |
|
TB treatment and care |
241,100 |
369,000 |
301,600 |
|
Total people receiving care |
696,900 |
1,766,200 |
2,765,600 |
|
Training—routine/TB care |
36,700 |
86,000 |
93,900 |
|
Training—VCT |
14,100 |
22,200 |
33,500 |
|
Total people receiving care-related training |
50,800 |
108,200 |
127,400 |
|
Service outlets—VCT |
2,100 |
4,200 |
6,466 |
|
Service outlets—routine/TB care |
5,400 |
6,800 |
8,019 |
|
NOTE: Figures shown do not include services to orphans and vulnerable children. VCT = voluntary counseling and testing in settings not providing services to prevent mother-to-child transmission of HIV. aThe total number of people receiving VCT services are neither counted towards the number of people receiving care nor included in the total number of people receiving care services in this table, but people who were counseled and tested and found positive would presumably be referred to and receive care services. bIn 2004 and 2005, prophylaxis and treatment were excluded from routine care. In 2006, tuberculosis (TB) prophylaxis was included in the routine care indicator, and treatment of TB and HIV remained separate. SOURCE: OGAC, 2005a, 2006b, 2007a, 2007b. |
|||
inclusion of voluntary counseling and testing in the care domain is that the Leadership Act places these services in the prevention category, although OGAC supports them with funds allocated for care (OGAC, 2004). The number of people receiving care-related training has also increased each year, with a cumulative total of more than 286, 000 people being trained. The service outlets for voluntary counseling and testing more than tripled from 2004 to 2006 and the outlets for routine and TB care have increased by more than 1,000 from year to year.
BACKGROUND: MODELS OF CARE
PEPFAR’s Network Model
PEPFAR’s network model (OGAC, 2004) comprises central medical facilities, district-level hospitals, and local health clinics, supplemented by
private, often faith-based facilities to rapidly scale up existing palliative care services for adults, orphans, and other vulnerable children (see Chapter 2). In accordance with national health and HIV/AIDS strategies, PEPFAR intends to build long-term sustainability and capacity by strengthening network-wide linkages among central facilities, international and private donors, community-based services, and home-based programs. The aim is to deliver quality services to intended recipients while following uniform protocols for HIV/AIDS treatment and care and for referrals among the programs. The ultimate goal of the network model is to ensure that technical support and products flow from the center to care facilities at the periphery to expand coverage, especially to rural and underserved areas. In the model’s description, well-functioning, adequately staffed facilities with sufficient physical infrastructure and research capabilities at the core are linked with a referral network of smaller regional hospitals and district facilities down to the community level, which features satellite clinics, mobile units, and community-based services. Facilities and staff within the network identify and refer patients needing more complex care to the more advanced central facilities. Information systems would have regular feedback loops linking facilities at all levels of the network, providing solid data to health providers and policy makers for use in decision making.
This model is mainly a medical one, with much of the emphasis being placed on free-standing clinical facilities that offer medical or health services, but not necessarily social or psychological services. The lack of attention to the latter services, whether formal or informal (such as support groups), is of concern to the Committee. OGAC has stated that implementation of the model will strengthen and utilize linkages among the levels of support, but has not articulated how this will occur. Not all facilities in a community provide the same levels and types of care (OGAC, 2004, 2005b, 2006b). Moreover, supervision of care providers is essential in all settings, particularly in home-based care, which over time has required an escalating level of skill (Foster et al., 2005). As early as the PEPFAR strategy document, PEPFAR began to articulate the approach of training and using community health workers to deliver essential supplies, including medications, to people in need in their communities (OGAC, 2004). Their training, along with that of nurses, was to include routine care, symptom management, and monitoring for treatment adherence. According to the strategy, home-based care programs have provided support to large numbers of people and because of their cost-effectiveness were to play a significant role in service delivery as part of the program’s community-based approach. Yet the strategy also acknowledges that the capacity of these programs is currently limited beyond provision of the minimum standards of palliative care.
PEPFAR’s intent to begin rapid scale-up of care services was founded on the use of existing services and providers. However, the strategy
acknowledges that many of the health and social service systems in the focus countries need strengthening and in some cases are practically nonexistent. In addition, weak health systems could exacerbate the effects of stigma and discrimination for people accessing care (OGAC, 2004).
PEPFAR has worked with many faith-based and community-based organizations that have historically been “first responders” not only to HIV/AIDS, but also to other health and social conditions (GHC, 2005). The chronicity of HIV/AIDS taxes fragile systems of care more than any other condition. However, PEPFAR is partnering with these organizations, other donors, and the government sector to build on and strengthen national strategies, organizations, and programs to provide care and essential supplies to those in need. To this end, PEPFAR has provided technical assistance to governmental and nongovernmental organizations and training to personnel, while also expecting the Country Teams to support programs in their Country Operational Plans that are aligned with the national plans and strategies of the host governments. At the same time, PEPFAR has faced challenges in finding and funding local and central service contractors that can provide comprehensive care services. This challenge is compounded by contractors that specialize in particular services and pursue niche funding for their activities. This situation could lead to the funding of multiple contractors to roll out the essential services, and present challenges to the integration of services within the care category and between care and prevention and treatment services. PEPFAR has also attempted to build or strengthen care capacity by providing technical assistance to organizations and training to personnel for not only the provision of services, but also for advocacy for reform of human resources policy and development and expansion of access to and use of pain-relieving medications (OGAC, 2005a, 2006b).
Community-Based, Family-Centered Care
According to OGAC’s palliative care guidance, community-based care is “provided in a variety of community settings, including free-standing outpatient clinics, day care centers, school- or university-based clinics, community health centers, workplace clinics, or stand-alone hospices. These delivery sites provide a wide range of interventions, including primary care, management of acute and chronic medical conditions, and supportive care” (OGAC, 2006d, p. 6). OGAC has also stated its expectation that community-based programs supported by PEPFAR establish linkages with inpatient facilities to facilitate referrals, as described in the network model. OGAC provides the example of a linkage model for community-based care consisting of “links with an orphan and other vulnerable children program, a palliative care provider, a food assistance program, a voluntary family
planning program, and ART programs within the home and or community” to demonstrate how a patient can be referred to various programs to access comprehensive care at the community level (OGAC, 2006d, p. 7).
Comprehensive care does not simply denote the scope of services a program attempts to provide to intended recipients, although a wide range of support services is essential for care to be comprehensive. It is also necessary to identify specific types of services a person will need over the course of the illness, the linkages and referrals necessary to meet complex service needs, whether services are readily accessible in communities, and quality services provided by all professional and volunteer providers. Timeliness, affordability, availability, access, and cultural appropriateness are critical elements of comprehensive services (Ro et al., 2003; WHO, 2004a).
Family-centered care focuses on priorities defined by the family through its active participation and identification of problems that compromise its functioning and well-being. Family-centered care is based on a core set of values, beliefs, and principles that include compassion, timeliness of services, flexibility (one size does not fit all, especially in the context of providing core services), cultural competence, and individualization. Other characteristics of family-centered care are team planning, development, and support; a focus on outcomes; planning driven by needs; and a community-based setting (FSPC, 2004). OGAC’s guidance documents and the Committee’s observations during its country visits provide evidence that PEPFAR is incorporating the core principles of family-based care into its community-based approach. For example, the program is increasingly focusing on secondary preventive care services; income generation and economic stability for households; services aimed at helping people be as healthy as possible for as long as possible, with the added goal of keeping families intact; and increased flexibility in individual and community service planning, driven by the needs of the diverse communities within and across the focus countries.
As described in Chapter 2, interventions at the community level involving the active engagement and participation of the community have the greatest likelihood of success. A community-based, family-centered model of HIV/AIDS care extends from HIV diagnosis to care for orphans and other survivors. It recognizes the importance of the community context and family resources in the care of people living with HIV/AIDS. Community-based, family-centered care conceptualizes the continuum of care needs and creates and supports services to meet these needs at appropriate times. The goal is to support those living with and affected by HIV/AIDS in living as well as possible for as long as possible, which includes delaying the need for treatment through the use of preventive care services, initiating appropriate services when indicated, and maximizing the quality of life for all affected by the disease. Services may also be required at some point to support end-
of-life care that focuses on appropriate pain management, dignity, grief counseling, and security for those left behind (OGAC, 2006d).
Care Planning
Care planning is initiated upon receipt of an HIV-positive test result or diagnosis of an AIDS-defining opportunistic infection, as well as identification of the stage or severity of illness to determine the immediate level of services needed. Stage of illness is often assessed by CD4 count or symptoms.
Figure 6-1 provides examples of the types of services that may be needed at the various stages of illness (based here on CD4 count). Such a continuum could also be envisioned from a different perspective with different eligibility criteria, and additional social, economic, and psychological needs for children, a family unit, a family member who is HIV-negative, a woman, or an elderly grandmother who is a caregiver. The continuum could similarly be envisioned according to the impact of each stage of disease on an entire family’s needs as well as the individual’s. The emphasis of services might be different, might have different starting and end points, and might be based on varying durations of need. For example, for a person who is HIV-negative and belongs to the same family as one who is HIV-positive, the continuum would emphasize primary and secondary prevention and other services needed to remain HIV-negative, including access to health care, food, housing, and potable water, with the eventual need for bereavement care. Moreover, individuals who are HIV-negative could be directly affected by the services offered to a family member who is HIV-positive. For example, a child who is HIV-negative could be the focus of succession planning, guardianship decisions, and memory book making. If an elderly grandmother is HIV-negative, she could be the one who assumes responsibility for the care of orphans and other vulnerable children.
There are challenges involved in planning, implementing, and evaluating family-centered care. Perhaps the first of these is to develop and support a culturally sensitive concept of community-based, family-centered care in which community groups are actively involved in the process of formulating and selecting services and service providers. The community is best able to profile its strengths and its contributions so as to identify the support needed to strengthen its response to the epidemic. WHO’s studies on palliative care in Africa found that the most successful community initiatives for palliative care and support have been developed and implemented by communities themselves. For this reason, WHO strongly urges that “health sector actions should be community-centered, engaging communities and people living with HIV/AIDS as full and equal partners in the provision of palliative care and other responses to the epidemic. Communities, families,
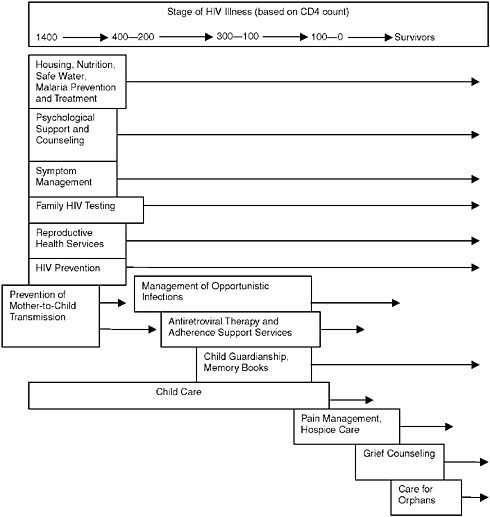
FIGURE 6-1 Stages of illness and appropriate HIV/AIDS care services.
and caregivers should be strengthened and supported in order to increase their capacity to participate in that partnership” (WHO, 2004c, p. 11). At the same time, however, long-term sustainability may be enhanced if resources support this model of care.
REVIEW OF PROGRESS TO DATE
This section reviews progress to date in the subcategories of routine care for HIV and tuberculosis, voluntary counseling and testing, and care-related training, as well as in the transition to sustainability.
Routine Care for HIV and Tuberculosis
Home-Based Care for HIV/AIDS
Home-based care can be provided by a variety of providers with varying levels of clinical and nursing care skills. Much of home-based care, by necessity, focuses on the family affected by HIV/AIDS—not only because the entire household has needs resulting from a family member having the illness, but also because the family is the primary source of support and care for sick and dying family members (WHO, 2004c; Donahue, 2005). Given the increasing demands for care as the epidemic continues to grow, PEPFAR is relying on home-based programs—which are relatively available and affordable—to provide the majority of palliative care to those in need (OGAC, 2004). Global human workforce shortages, particularly acute in Africa, exacerbate the limited availability of skilled clinicians to provide home-based care; thus the majority of this burden falls to family members, particularly women and girls. (These issues are discussed later in the chapter.)
Preventive Care for People Living with HIV/AIDS
Critical elements of a family-based preventive care package include family counseling and testing, cotrimoxazole, a safe water vessel, bed nets, TB prophylaxis, multivitamins, and home-based ART and TB care (Mermin, 2005; Yengi, 2005). As discussed below, PEPFAR supports these critical elements in its secondary preventive care service package.
In April 2006, OGAC released two sets of guidance for secondary preventive care services for both adults and children aged 0–14 born to mothers who are HIV-positive. This guidance was produced under the leadership of several of OGAC’s technical working groups—the Palliative Care Technical Working Group, the Food and Nutrition Technical Working Group, and the Orphans and Vulnerable Children Technical Working Group. PEPFAR’s second annual report to Congress acknowledged the difficulty of determining or assessing the quality of care services. These guidance documents represent an attempt to address this problem by encouraging the implementation of standardized preventive care services in palliative care programs (OGAC, 2006b).
Preventive care services have reduced mortality and morbidity not only for those living with HIV/AIDS, but also for their family members and children. Parental death associated with HIV/AIDS has been found to triple the risk of death of HIV-negative children in the home, while cotrimoxazole prophylaxis has been shown to decrease mortality for children younger than age 10 if their parent/caregiver is HIV-positive. Moreover, no
association has been found between prophylaxis and increased antimicrobial resistance among diarrheal pathogens infecting family members. For US$4 per year, clean water and storage in the home can reduce diarrheal days and episodes. Moreover, bed nets that cost about US$5 can prevent malaria and its complications and reduce malarial prevalence among children who are HIV-negative (nets have seldom been tested for beneficial use with adults who are HIV-positive) (Mermin, 2005; Yengi, 2005). Malaria is an opportunistic infection of particular concern in developing countries. Abu-Raddad and colleagues (2006), for example, found that transient and repeated increases in viral load resulting from recurrent coinfection with malaria may play an important contributory role in the spread of HIV in sub-Saharan Africa.
OGAC has acknowledged the unlikelihood that packages of care services can be standardized for all situations and countries, given variations in setting and in the capacity of partners who are implementing programs (OGAC, 2006f). In accordance with the principle of one national action framework, as well as alignment with international standards, OGAC has specifically acknowledged that “prioritization and selection of components of a preventive care package must be performed locally, and should be consistent with national guidelines and those sponsored by the World Organization operative within the country” (OGAC, 2006f, p. 3). OGAC’s guidance documents clarify specific preventive care services PEPFAR will fund directly, as well as their expectations for linking preventive care interventions to other key health care services, such as routine medical care and voluntary family planning (see the discussion of integration of services later in the chapter). Directly funded services for both adults and children (unless otherwise specified) include the following (OGAC, 2006f):
-
Technical assistance for developing guidelines and training for the use and provision of cotrimoxazole for prophylaxis of Pneumocystis pneumonia and diarrhea.
-
Effective TB interventions for people living with HIV/AIDS including skin tests, treatment of latent TB infection for adults who are HIV-positive and exposed/infected children, screening for active TB, and referral and linkage to TB diagnostic and treatment centers.
-
Services related to safe drinking water and personal hygiene, including provision of supplies to treat and store water, soap, and instructions for hand washing.
-
Provision of insecticide-treated nets (via linkages with the President’s Malaria Initiative and the Global Fund for the Treatment of AIDS, Tuberculosis and Malaria).
-
Nutrition services and micronutrient supplementation, including daily supplements for people living with HIV/AIDS—especially pregnant
-
women, lactating women, and children, as indicated by dietary assessments—as well as nutrition counseling linked to clinic- and home-based care.
-
Services and counseling to prevent transmission of HIV to others, including technical assistance for developing national policies and training for the implementation of prevention programs; ongoing counseling for people living with HIV/AIDS related to behavior change; and provision of condoms and referrals to other preventive services, such as family planning and clinics for the diagnosis and treatment of sexually transmitted infections.
-
HIV counseling and testing of family members and other contacts, including sero-discordant couples, sex partners of people who are HIV-positive, and referrals to care and prevention services for those who are identified as HIV-positive.
Management of Opportunistic Infections
HIV/AIDS weakens a person’s immune system and its ability to fight disease. As a result, many people who are HIV-positive develop bacterial, mycobacterial, fungal, protozoan, and viral infections, as well as neurological conditions, malignancies, and other conditions and complications (e.g., mood and anxiety disorders, wasting syndrome) as they progress through the continuum of the disease (AVERT, 2006). Many of these conditions are called “opportunistic infections” because they take advantage of the opportunity offered by a weakened immune system (the example of malaria was noted above). People with healthy immune systems may contract the same diseases, but people living with HIV/AIDS have a more difficult time recovering from them. One of the goals of clinical HIV care is to quickly assess and manage opportunistic infections to keep patients as healthy as possible for as long as possible. Highly active antiretroviral therapy (HAART) can reduce the amount of HIV in the body and restore immune functioning. In resourced-constrained settings where access to HAART may be limited, however, and in some cases even where HAART is available, diagnosis and treatment of opportunistic infections remains essential to improve health. Prevention of opportunistic infections is, of course, optimum, and in some cases may be achieved by avoiding pathogens that may be found in water sources, uncooked food, domestic animals, and human excrement. While PEPFAR usually addresses medical management and prophylaxis of opportunistic infections in its treatment category, it also addresses prophylaxis through activities under its secondary preventive care package related to safe drinking water, personal hygiene, and training in and use of cotrimoxazole.
Tuberculosis Treatment and Prophylaxis
The global incidence of TB continues to rise, and rates of the disease are growing exponentially in Africa because of the HIV/AIDS epidemic. Given that 50–80 percent of TB patients in sub-Saharan Africa are HIV-positive (OGAC, 2006e), TB clinics are seen as important entry points for identifying candidates for both TB treatment and initiation of ART. In some countries, nurses and lower-level workers are able to provide voluntary counseling and testing for HIV/AIDS for TB patients, but in others they are prohibited from doing so by legislative or policy restrictions. While the uptake of these services is high in some focus countries, fewer than 10 percent of TB patients know their HIV status (OGAC, 2006e). Additional challenges are in adequate diagnostic capability in resource-poor settings; prohibitive patient fees associated with some diagnostics; the difficulty of diagnosing children; the complexity of managing coinfected patients on ART (especially pregnant women); limited or no access to care and treatment because of weak referral systems; costs to patients of services from multiple sites; the dissonance between centrally provided HIV/AIDS services and TB services delivered at the primary care level; nonstandardized TB screening; and limited use of or nonexistent standard surveillance and reporting systems for comorbidities and exposure (OGAC, 2006e). Innovative approaches for addressing these challenges include co-locating services in the same facility, especially in TB clinics and during directly observed therapy in HIV clinics; using mobile units in rural areas; and using community and home-based services to jointly supervise ART and TB treatment. Limited data are available about the consistent provision of routine testing for people exposed to and being treated for TB; as well as about the frequency and success of co-located testing and TB services in PEPFAR-supported programs. The United States and WHO have worked together to formulate strategies for joint TB/HIV activities at the international, national, and subnational levels, but WHO’s new algorithms for accelerating diagnosis of sputum smear–negative TB are presenting their own challenges (OGAC, 2006e).
Voluntary Counseling and Testing
Definition
WHO defines voluntary counseling and testing as a confidential dialogue between a client and a care provider aimed at enabling the client to cope with stress and to make personal decisions related to HIV/AIDS (Rehle et al., 2000). According to international standards, dedicated programs for
counseling and testing for diagnostic purposes are a critical component of a comprehensive approach to HIV/AIDS care and support (WHO, 2004c).
Voluntary counseling and testing can be offered in a variety of settings—static settings such as clinics and hospitals, or alternative settings such as the home and mobile vans that travel throughout communities. Sessions at PEPFAR’s third annual meeting in Durban, South Africa, revealed that the uptake of mobile voluntary counseling and testing is high—much higher compared with static sites. Other data presented at the meeting showed that the availability of routine and diagnostic voluntary counseling and testing in clinical settings leads to high uptake—as high as 97 percent in some hospitals—with 55 percent of patients tested being HIV-positive (OGAC, 2006d). Moreover, many programs are offering couples counseling and testing (OGAC, 2006d), although limited data exist on the uptake of these services. Voluntary counseling and testing has several components, including group or individual pretest education, individual pretest counseling, and individual post-test counseling. In pretest education, a health educator can provide basic information about HIV/AIDS and safer sex and reinforcement messages about behavior change, as well as answer questions and recognize the need for individual counseling and referral. Pretest counseling can be used to clarify information from pretest educational sessions and provide all the information a person needs to give informed consent for the actual testing. Post-test counseling focuses on providing positive, negative, or inconclusive test results to the individual. Counselors are trained to expect a range of emotional responses regardless of the test result; to be prepared to make referrals for prevention, treatment, and care services; to provide risk reduction information and disease education; to provide information on and support for serostatus disclosure; and to be prepared to provide several counseling sessions to the individual if needed (WHO, 2004b). During the Committee’s country visits, interest was expressed at the country level in moving toward conducting more group pretest education in hopes of making pretest counseling sessions more efficient, which in turn could help increase the number of people who can be tested. Such group pretest education would not replace individual pretest counseling.
Although funded under the care category, voluntary counseling and testing also plays an important role in prevention and treatment. It can be used for case finding for care, prevention, and treatment services. In prevention, for example, estimating HIV prevalence and targeting prevention messages to people who are both HIV-negative and HIV-positive based on serologic and behavioral surveys are critical activities. In treatment, voluntary counseling and testing is helpful for identifying those eligible for ART. In care, voluntary counseling and testing can be used to identify those in need of palliative care, particularly those not eligible for ART or for whom ART is not available. There may be additional objectives for voluntary
counseling and testing, such as supporting surveillance, promoting behavior change, enabling public education, and functioning as a gateway to facilitate referrals to treatment and care services (Rehle et al., 2000). To date, the number of people tested exceeds the numbers who have received care services (OGAC, 2005a, 2006b).
Testing of Infants
PEPFAR is using various methods to identify HIV-exposed or infected children who are in need of services, including pediatric treatment. To advance testing and diagnosis of infants (6 weeks and older) who are HIV-exposed and HIV-positive, PEPFAR is collaborating with some of its implementing partners to pilot and develop the use of dried blood spot testing with polymerase chain reaction testing in several focus countries (OGAC, 2006b; Kaiser Family Foundation, 2006). Previously and with a different testing method, infants were tested at 18 months when they could already be at an advanced stage of the disease. In 2006, one PEPFAR focus country that successfully conducted pilot dried blood spot testing programs in 11 clinics and 1 referral hospital received $54 million from PEPFAR to support the continuation of the testing program (Kaiser Family Foundation, 2006). Results of the country’s PEPFAR-supported pilot studies presented at the 16th International AIDS Conference indicate that dried blood spot testing is not only diagnostically specific and sensitive, but also cost-effective because of the simplicity of the supplies and skills needed to perform the procedure: a finger prick (versus phlebotomy) provides enough of a blood sample, the samples (which do not need refrigeration) are dried on a paper card, and they are sent by courier envelope to the nearest testing facility. Given this simplicity, the investigators estimated that a technician could perform 13,000 such tests annually (Gass et al., 2006). The success of this testing method thus has important implications for the scaling up of infant testing and treatment. PEPFAR has supported the adoption of national policies to incorporate dried blood spot testing to improve diagnosis of HIV in infants in 10 of the focus countries (OGAC, 2007a).
Ethical issues are associated with HIV testing for infants, as well as older children and adolescents. Of concern is disclosing positive test results of infants and younger children, which indicate the positive serostatus of their biological mothers, who may not yet have been tested or consented to testing. The major issue of access to children and adolescents to be tested is compounded by other issues, including how to determine at what age obtaining informed consent is appropriate, how to know when a child or adolescent can understand the information provided and discussed in the counseling session well enough to give informed consent, what potential
consequences disclosing test results can have, and whether it is appropriate to disclose results to the child or adolescent (HIV Insite, 2006).
Capacity Issues for Counseling and Testing
OGAC has reported that a growing number of best practices for sustainability and scaling up of quality counseling and testing have been identified to assist Country Teams and implementing partners (OGAC, 2006b). PEPFAR is increasing its support to countries in their efforts to integrate counseling and testing into routine care as a means of scaling up testing efforts, especially in programs for pregnant women, clinics that treat TB and sexually transmitted infections, hospitals, and other clinical settings (OGAC, 2006b). PEPFAR is also supporting what it describes as local initiatives to scale up counseling and testing—among them, home-based testing that can test all family members, testing programs for partners or couples, mobile testing, and hotlines linking callers to test sites. PEPFAR has increased its support for the use of rapid tests by encouraging country teams to include such testing in their national plans.
Care-Related Training
The majority of care-related training has been in-service training or retraining for existing health workers, including community health workers (OGAC, 2006b). It is difficult to determine the ratio of in-service to preservice training supported by PEPFAR, as well as whether the training being provided is exponentially increasing the number of skilled or lay workers and paid or unpaid health workers, because information is generally unavailable on the categories of workers involved (nurses, clinical officers, physicians, community health workers, home health workers, and familial caregivers), the type of remuneration, whether the workers are being newly trained or retrained, and whether the same workers are being retrained. There is also little information available about the content of the training curriculum; whether people are completely, partially, or serially trained in knowledge and skill development to provide comprehensive care in home-based settings; and whether those trained receive backup and ongoing supervision from trained health workers, such as nurses.
Preservice support includes curriculum development by incorporating HIV/AIDS care into nursing school curricula, and in some cases a limited number of scholarships and postgraduate fellowships (OGAC, 2006c). Preservice support for highly skilled health workers is expensive and takes several years to produce a newly trained professional. The demand for care in both community and home-based programs necessitates an examination of the contributions made by all donors to human capacity development.
While PEPFAR acknowledges that the ultimate solution to workforce issues rests with the host country, and while PEPFAR may be contributing its fair share to support preservice training, the ratio of in-service to preservice support may need to be re-examined as the program continues.
PEPFAR is relying on the community health worker model of care for a variety of reasons, but primarily because its use can rapidly scale up the immediate pool of people available to provide services. As the term implies, the workers are community members who work in community settings and serve as a liaison between those who need health services and those who provide the services. Community workers often provide basic health services while promoting the key principles of primary health care—equity, multisectoral collaboration, and the use of appropriate technology (JLI, 2004). The goal of the community health worker model is to promote health among those populations and groups who have traditionally lacked access to adequate health and social services, usually due to lack of both financial and human resources. These communities are usually unable to maintain a health program of their own (Ro et al., 2003; UNICEF and WHO, 2006). In the majority of these programs, the communities are not responsible for the initiation and implementation of the program. Their role is mainly participating in some aspects of development (if they are involved in early program planning), implementation, and maintenance of programs (UNICEF and WHO, 2006). Though there are concerns about the reliance on volunteers to scale up care services, as well as some hard-learned consequences when utilizing this model, this model has successfully demonstrated the effectiveness of community health workers in helping underserved individuals access health services in appropriate ways (Ro et al., 2003). In Ethiopia alone, PEPFAR has supported the national strategy of training more than 30,000 community health workers to be placed throughout 15 regions, serving 5,000 people per area (Dybul, 2006; OGAC, 2006c).
Policy reforms supported by PEPFAR—including task shifting and altering the scope of practice for some highly skilled health workers to prioritize and increase the time they can spend providing more complex clinical care—reinforce the use of the community health worker model. Other salient policy reform activities include advocacy for eliminating mandatory retirement for skilled health workers, especially nurses, who are being re-employed to provide clinical services (OGAC, 2006c). Task shifting permits less specialized but trained health workers to assume some of the tasks of those who are more specialized. Examples of task shifting specifically related to care activities include using community health workers to offer counseling and testing services so that nurses can provide other, more complex clinical services. In some focus countries, laws have been changed to allow specially trained nurses or clinical medical officers to prescribe ARVs and medications for management of opportunistic infections,
and some community health workers to administer pain-relieving medications, cotrimoxazole prophylaxis, and other treatments for opportunistic infections to enable widespread distribution of services in community and home-based programs. Other community health workers are trained to provide nursing care; deliver refills of medications for ART and treatment of TB and opportunistic infections to patients’ homes; monitor adherence to these medications; provide condom education; engage in health promotion; provide compassionate end-of-life care; and offer peer support to meet the psychosocial needs of people living with HIV/AIDS, orphans, and other vulnerable children (OGAC, 2006c). PEPFAR also uses formal partnerships among ministries of health, organizations for people living with HIV/AIDS, and community-based organizations to enable people living with HIV/AIDS to be trained as community health workers who can provide adherence support and prevention services.
Transition from Emergency Aid to Sustainability
During its initial roll-out, PEPFAR utilized established providers that were either already providing similar services or had historically been involved in medical or social health services and held the trust of many people in the communities in which they operated. This translated into a heavy reliance on international nongovernmental organizations, including community- and faith-based organizations (OGAC, 2005a, 2006b). Over its years of operation, PEPFAR has engaged in many activities aimed at building the capacity of communities to plan, implement, and monitor care services. These activities have included providing small grants for local organizations to provide services; strengthening referral systems for social service needs; and supporting the development and operation of networks for people living with HIV/AIDS to be involved in not only the provision of care, but also the development of long-term sustainable programs (OGAC, 2005a, 2006b).
ISSUES AND OPPORTUNITIES FOR IMPROVEMENT
The Committee identified issues and opportunities for improvement in PEPFAR’s care category in the following areas: home-based care programs, addressing the psychosocial and spiritual needs of people affected by HIV/AIDS, reliance of volunteers, pain management, addressing the needs of women and girls, voluntary counseling and testing, and integration of services. However, limited data are available about the consistent provision of voluntary counseling and testing as part of home-based services in PEPFAR-supported programs.
Home-Based Care Programs
In addition to coping with the physical and emotional demands of caregiving, according to OGAC, all home-based caregivers also need to learn skills necessary to recognize symptoms of advancing disease or opportunistic infections; to determine whether patients need more advanced care and know how to access the needed services from wherever they may be available; to administer medications; to employ universal precautions to minimize risk exposure for the entire household; to be able to arrange or provide transportation and child care to the extent available; to communicate with the patient and other caregivers, both formal and informal; and to provide emotional support for those who are ill. OGAC recognizes that many home-based care services and programs lack a number of these critical aspects of care (OGAC, 2006d). Therefore, OGAC’s palliative care guidance specifically acknowledges that the introduction of comprehensive care into home-based programs requires training and education of medical providers (nurses, clinical officers and physicians, including pediatric nurses and physicians), and community care providers (see Box 6-2).
|
BOX 6-2 Training Specifications for Introducing Comprehensive Care into PEPFAR Home-Based Programs
SOURCE: OGAC, 2006d. |
The Country Operational Plans and PEPFAR’s strategic documents, guidance, and annual reports do not provide adequately detailed information on the extent to which PEPFAR is conducting this training and building this capacity at the home and community levels. Concern has been raised in particular, however, about the training received by community health workers. Although there are no international or national certifications for community health workers (OGAC, 2006c), the Committee is concerned about the variability of their training in both quality and length, as well as about the levels of ongoing supervision these workers receive, especially if they are providing the services PEPFAR has identified as critical to the provision of comprehensive care in community- and home-based settings. During country visits, the Committee heard from program implementers about a lack of timely and comprehensive programmatic guidance for family-based care services, which has resulted in delays in program planning, implementation, and evaluation, as well as great variability in the type, quantity, and quality of care services throughout the focus countries. On the African continent in particular, the Joint Learning Initiative has reported that community health workers have taken on more specialized roles in the areas of malaria control, reproductive health, and nutrition and have increased their coverage of a range of services over the last three decades; they have also assumed broader roles as change agents and community advocates. The Joint Learning Initiative has also suggested that historical constraints on the effectiveness of the community health worker model have included lack of attention to primary care and a lack of government support (JLI, 2004). PEPFAR could address some of these issues by building on the recommendations of WHO and the Joint Learning Initiative, which include improving the design, management, monitoring, and evaluation of community health worker programs, with greater emphasis on support, supervision, and community participation and ownership (JLI, 2004).
Addressing the Psychosocial and Spiritual Needs of People Affected by HIV/AIDS
Despite treatment for HIV/AIDS, the burden of pain persists, and people with HIV/AIDS continue to have psychological and spiritual needs. PEPFAR has identified resources necessary to meet these needs in providing care (OGAC, 2004). During the Committee’s country visits, however, these services appeared to be the least visible and in need of greater emphasis.
Complications of advanced disease can include neurological sequelae that can result in cognitive, affective, and motor dysfunctions that occur in up to 90 percent of people who are HIV-positive (Kalichman, 1995). Makoae and colleagues (2005) have documented the number and complexity of symptoms experienced by people in sub-Saharan Africa who are
HIV-positive, from initial diagnosis through late-stage illness. According to Holzemer (2002), the available evidence indicates that the term “asymptomatic” as used by the medical community is an unsatisfactory description of the experience of living with symptoms early in the course of HIV infection.
Emotional and spiritual needs include those arising from environmental, physical, and social stressors, as well as grief and bereavement; culturally appropriate treatment of existing or new mood and anxiety disorders; treatment of other mental disorders, including substance abuse and addiction; and the need to deal with issues related to meaning of life, control, and self-esteem. Several studies have documented the challenges faced by people living with HIV infection as they attempt to manage common symptoms, including peripheral neuropathy (Nicholas et al., 2007), fatigue (Corless et al., 2002), depression (Eller et al., 2005), and anxiety (Kemppainen et al., 2006).
Social sequelae can include having to deal with fears of contagion, sickness, and death, as well as with stigma and discrimination, and the need to develop coping strategies (Kalichman, 1995). Harding and colleagues (2005) report that despite treatment, there is the recognition that the burden of pain continues and people with HIV continue to have psychological and spiritual needs, though community burden in providing home care and psychological needs are under explored (Harding et al., 2005). Coleman et al. (2006) describes how prayer is often used as a symptom management strategy for people living with HIV in an ethnically diverse sample.
Reliance on Volunteers
An important issue related to care is the heavy reliance on volunteers to provide home-based care. Many of these are women, young girls, and elderly grandmothers who are “default volunteers” by virtue of their cultural roles and status as familial caregivers. In Africa, women are typically responsible for health care; produce 70 percent of the food consumed; and are more likely to use their incomes to meet children’s needs, including schooling. Children are likely, in the short term, to replace the labor of a women who dies (Donahue, 2005), and are often as vulnerable and in as much need of assistance as the people for whom they are caring. The phenomenon of these women and girls, and countless thousands more, who are helping those in greater need has been described as “the poor helping the destitute” (Donahue, 2005, p. 38). Anecdotal evidence suggests that they may be unable to continue in these roles for long for a variety of reasons, including burnout, lack of resources for support, increasing needs for care, failing health, and aging.
Because of their critical importance to community- and home-based
care, the sustained use of volunteers for the provision of care is a worthy subject for targeted evaluation. Harding and colleagues (2005) found that the reliance of African palliative care services on volunteers to provide community and home-based care has been largely successful for palliative care, but that community capacity and the resources and clinical supervision necessary to sustain quality care are lacking. They note that it is not yet clear how much trained professional input is needed for supervision of lay workers and patients, what the community’s maximum capacity for care is, and what level of skills can be expected from lay workers providing palliative care. Further exploration of these issues is critical to the sustainability of community and home-based services.
Some PEPFAR-supported partners who were operating prior to the program’s initiation described to the Committee retention and assistance strategies for volunteers, which to some degree mirror PEPFAR’s retention strategies for highly skilled health workers. These strategies include providing transportation to places where care services are offered, reimbursing volunteers’ health expenses, providing ART for those in need, and offering psychosocial support. These strategies are not widespread, however, and not all organizations have the resources to adopt them. Some suggest that all volunteers be paid with some form of remuneration, but the effects this might have on the management and sustainability of community and country programs are unknown. Regardless of what strategies are adopted, it would be sensitive of PEPFAR to strike an appropriate balance with the cultural beliefs and customs of familial caregiving for ill and dying family members.
Pain Management
Issues related to pain management include government policies related to the availability of opioids in many types of care settings, professional practice standards that specify who is legally allowed to administer pain medications, and concerns about the illegal redirection of medications made available for pain management (OGAC, 2006d) As previously mentioned, management of pain symptoms is included in PEPFAR’s care category, but is operationalized in the treatment category (OGAC, 2004).
Seminal research conducted by WHO (2004c) and Harding and Higginson (2005) examined palliative care and pain management in sub-Saharan Africa in the hopes of illuminating issues and practices that could reduce “the historical inadequacy of pain and symptom control in HIV/AIDS home based-care, which has been called ‘home-based neglect’” (Harding and Higginson, 2005, p. 1973). Harding reports that there continues to be misperceptions that ART obviates the need for palliative care; whereas better integration of palliative care in HAART programs is needed (Harding
and Higginson, 2004, 2005). Additional research by Harding and colleagues (2005) found significant limitations in and a pressing need for the expansion of current HIV/AIDS palliative and end-of-life care. According to the authors, among the five key strategies needed, “pain control remains a primary challenge [that must be addressed] and requires development of pain medication regulation, procurement and distribution polices, and education of health professionals, community workers, and affected people in their purpose and use” (Harding et al., 2005, p. 5). Since traditional healers are often the first point at which help is sought by both cancer and HIV patients, it is suggested that alliances be forged between traditional healers and palliative care providers; the authors note that educational programs for traditional healers have been associated with improved support for patients with HIV (Harding and Higginson, 2004, 2005). PEPFAR is supporting initiatives to build alliances between traditional healers and other health professionals, but the extent of these partnerships throughout the focus countries is unknown.
OGAC has provided specific guidance on pain management for children. According to this guidance, pain management for children should follow the principles of the WHO analgesic ladder, but special attention should be paid to nonverbal symptoms associated with pain and its intensity, since children often are not able to describe pain adequately to permit appropriate treatment (OGAC, 2006g).
During PEPFAR’s third annual meeting in Durban, it was noted that many patients and providers report that pain is undertreated in the majority of patients surveyed, and the African Palliative Care Association, a major south-to-south twinning partner, has reported that opioids are unavailable to the majority of providers—in some cases, even mild analgesics are unavailable for adequate pain management (OGAC, 2006e). The Palliative Care Technical Working Group’s fiscal year 2006 plan identified intentions to “gather and disseminate information on simplified tools to ascertain severity of symptoms and pain related to HIV disease in resource poor settings and encourage support for the development of template curricula for pain/symptom management” (OGAC, 2006g, p. 19). The plan also indicated intentions to participate in a number of national and international symposia to learn more about the latest innovations in palliative care, including the 7th Clinical Team and Conference and Scientific Symposium of the National Hospice and Palliative Care Organization in April 2006 (OGAC, 2006g).
Harding and Higginson (2005, p. 1975) note that “palliative care worldwide has been evolving to address integrated management of patients through the course of the disease.” They suggest that funders may wish to consider opportunities to improve patient management.
Addressing the Needs of Women and Girls
PEPFAR has expressed a commitment to increasing gender equity in all of its interventions in partnership with both national governments and the civil sector (OGAC, 2005a, 2006b). Women and girls have a number of needs to be met in any concerted and effective response to HIV/AIDS. Many advocates emphasize the urgency of focusing on inheritance and property rights for women and girls since increased financial independence would not only reduce their vulnerability to HIV exposure, but also improve their ability to serve successfully as head-of-households after the death of their male spouses/partners, fathers, and adult children (ICRW, 2005; UNAIDS and UNICEF, 2004; UNICEF, 2006).
Of particular importance given the emphasis of family-centered care is that many women, young girls, and elderly grandmothers may need services while simultaneously serving as primary caregivers for other ill and dying family members. Interventions are necessary to reduce their vulnerability to HIV infection, as well as to enhance their ability to shoulder the long-lasting, caregiving burden. It may be unreasonable to expect women and girls to manage the physical and emotional demands of end-of-life care without skilled assistance. Moreover, women and girls, as well as other caregivers, frequently rely on their community network for assistance, which makes strong, effective, and comprehensive community-based care a necessity.
Restoration of fertility for women on ART is a growing phenomenon with some programs reporting that up to 90 percent of the pregnancies among HIV-positive women are unplanned pregnancies and 81 percent of those unplanned pregnancies are among the women receiving ART. It is essential to address linkages among HIV/AIDS treatment and care, reproductive health, and family planning services (OGAC, 2006e). Strategies are needed to support women in voluntary family planning and reproductive health, which requires integration with prevention of mother-to-child transmission of HIV, voluntary counseling and testing in family planning settings, access to ART and other necessary medications, and care in community-and home-based settings. As part of its commitment to addressing the needs of women and girls, PEPFAR has articulated opportunities for developing such linkages. While PEPFAR funds for contraception are restricted to the purchase of condoms, linkages to existing family planning and reproductive health programs are encouraged (OGAC, 2006h). Reproductive health covers a broad range of women’s health issues, including the detection and treatment of sexually transmitted infections and support for the desire of a woman or couple who are HIV-positive or a sero-discordant couple to have children safely (Fleischman, 2006). In addition, integration with treatment programs and training of ART providers to meet the reproductive health needs of their clients may be critical in addressing family planning needs since 61 percent of those receiving ART are women (OGAC, 2005a,
2006h). Conversely, if programs are not implemented with sensitivity to these issues, both women and men may drop out of care and treatment.
PEPFAR’s 5-year strategy includes a clear commitment to addressing gender issues and reducing the vulnerability of women and girls to HIV/AIDS (OGAC, 2004). However, program results for voluntary counseling and testing is the only category that is currently required to be disaggregated by gender. Much of the gender focus in counseling and testing for diagnostic purposes is in initiatives to prevent mother-to-child transmission. By the end of fiscal year 2006, OGAC reports that cumulatively 70 percent of those receiving counseling and testing services supported by the U.S. government in prevention of mother-to-child and all other settings were women (OGAC, 2007a).
Voluntary Counseling and Testing
The past 2 years has seen increasing interest in moving toward a model of counseling and testing that makes the HIV test a routine part of medical care. In 2004, both the United Nations Programme on HIV/AIDS (UNAIDS) and WHO recommended that “health care providers routinely offer HIV testing to all patients seen in clinical and community-based health service settings where HIV is prevalent and antiretroviral therapy is available (WHO, 2006, p. 11). Such provider-initiated testing also gives the patient the opportunity to refuse the test or “opt out.” While OGAC has stated that PEPFAR will promote and support routine or opt-out testing in appropriate settings, particularly for prevention of mother-to-child transmission (OGAC, 2006b), human rights advocates have raised concern as to whether people are truly able to provide informed consent and not be coerced to undergo testing. This concern appears to stem from questions about whether patients are ready for disclosure of their status and whether stigma, discrimination, and even violence against women may result from undergoing the test and receiving the results (HIV Insite, 2006). Questions also arise about how and whether expanded programs can provide the right amount of information during counseling sessions when human resources are stretched and whether marginalized populations would become more vulnerable to human rights abuses if testing became routine. Other ethical issues, raised above with respect to children and adolescents, include discerning when people are the appropriate age to give consent, when they can understand the information provided and discussed in the counseling session well enough to give informed consent, and given the potential consequences, whether it is appropriate to disclose results to the person being tested.
OGAC has reported several key barriers to counseling and testing, including a lack of routine availability of the services in health care settings, stigma and discrimination, shortages of laboratory personnel, long
distances of patients from testing sites, inadequate access to providers, and lack of availability of rapid tests (OGAC, 2006b). At PEPFAR’s third annual meeting, several challenges related to scaling up counseling and testing services were identified, including shortages of test kits; lengthy pretest counseling sessions; referrals for care, support, and treatment for difficult-to-reach populations; logistical complications associated with the increased demand for mobile services; and lack of consensus on age of consent for HIV testing and how to communicate HIV test results to children (OGAC, 2006d). OGAC reported that 30–40 million counseling and testing sessions are needed to meet their treatment target of 2 million people. PEFAR efforts to scale-up and integrate counseling and testing services include linking counseling and testing to other HIV services, improving access to these services for the general population, and home-based testing and door-to-door counseling to reach families and sero-discordant couples (OGAC, 2007a).
During its country visits, the Committee heard reports of problems similar to those raised at the annual meeting. Receipt of test results, for example, is critical to effecting behavior change and initiating care. Yet long waits for test results were often cited as the reason people did not return for their results; the use of rapid tests reduced the numbers of people who were tested but remained ignorant of their status. Limited availability of test kits makes it difficult to respond to the demand for testing, while many test kits are past their expiration date. In its second annual report to Congress, OGAC described its intent to provide an uninterrupted supply of high-quality rapid test kits through the supply chain management system.
OGAC has reported that it is contributing to improved quality of counseling and testing services by supporting improved training and greater numbers of counselors, with an emphasis on including information on prevention during counseling sessions (OGAC, 2006b). The quality and impact of those trained to provide counseling and testing and the functioning of testing sites are difficult to determine, however, since OGAC has provided little information in this regard other than numbers. According to OGAC’s guidance, counseling and testing are to be provided according to national and international standards. However, there are few descriptions of the training providers receive, about their ongoing supervision, or about follow-up for those who have received a positive test result and have been referred to care and treatment programs.
Integration of Services
Through its disease-specific focus, PEPFAR allows for a concentrated response to all aspects of HIV/AIDS and to an individual’s needs throughout the continuum of the illness. At the same time, the program makes choices about eligibility for services because of its limited resources and the
magnitude of the needs of those affected by the disease. These unavoidable limitations make it essential that PEPFAR’s activities be integrated with and maximize opportunities for referrals to other programs and agencies, including the focus countries’ larger health systems. PEPFAR refers to such linkages as “wrap-arounds” and believes its funds can be used to leverage other resources to meet the needs of those affected by HIV/AIDS.
Wrap-around services benefit not only people living with HIV/AIDS, but also family and household members and others in the community. Some of these programs are funded by the U.S. government and some by other donors. Examples are the President’s Malaria Initiative; the Global Fund to Fight AIDS, Tuberculosis and Malaria; the United Nations Children’s Fund (UNICEF); other bilateral and multilateral family planning programs; and food security programs such as the United Nations World Food Program and Food for Peace (OGAC, 2006d). Wrap-around initiatives address such needs as promotion of gender equity; prevention of opportunistic and parasitic infections (e.g., malaria); strengthening of households’ capacity to generate income; strengthening of non-HIV-specific health programs, such as those focused on family planning, child health and immunization, food security and nutrition; substance abuse treatment; and provision of clean water and improved sanitation in communities (OGAC, 2006d). Wrap-arounds were added as an area of emphasis for fiscal year 2006 in OGAC guidance documents.
Beyond providing an opportunity for comprehensive services, integration allows for joint problem solving, reduced workload for staff, savings and better targeting of resources, continued improvement of skills for service providers, improved coordination, and the ability to coordinate in the development of annual plans (Peng, 2006). Integration can also facilitate enhanced monitoring and evaluation to improve program planning and make it possible to gauge the quality of services provided.
PEPFAR provides a wide range of services in its prevention, treatment, and care categories, but many of these services have been fragmented by budgetary allocations. This fragmentation, coupled with poor linkages and inconsistent/incomplete referrals internally and to external providers for services not supported by PEPFAR, creates missed opportunities for integration along the continuum of care and raises concern about whether patients who are receiving such fragmented services are being well served. PEPFAR guidance emphasizes comprehensive and integrated services at the community level, but much of the program’s planning is being done by partners at the national rather than the local level. For example, PEPFAR has provided technical assistance at the national level for building sustainable palliative care systems. Through this work, a common set of home-based care services is being identified. However, program planning, implementation, and evaluation have been delayed by a lack of comprehensive programmatic guidance
for family-based care services. PEPFAR, working with its partners, needs to plan strategically to implement comprehensive services and build capacity at the community level.
In the care category, PEPFAR’s program guidance is inconsistent in terms of integration of services, as evidenced by the exclusion of the services of traditional healers from what are identified as key areas of training for the provision of comprehensive care through home-based programs. At the same time, PEPFAR does have training programs targeting the development of partnerships with traditional healers to address issues related to adherence to ART and discussion of the effectiveness of ART with patients (OGAC, 2005d, 2006a). In addition, the Committee believes further work is needed to incorporate in PEPFAR’s training curricula and programmatic guidance cross-cutting issues and services such as nutrition and adherence to ART and other medications. Moreover, integration of palliative and preventive care guidance would have positive benefits in supporting overall wellness before and during ART. Other benefits could include impeding the synergism recently reported between malaria and high rates of transmission of HIV. Given the known concomitant effects of malaria and HIV, intensification of scaling-up efforts of PEPFAR’s secondary preventive care services and improving their linkages to services for comorbid infections is necessary. Doing so could contribute to efforts to keep people healthier longer, regardless of whether they are eligible for ART. Such linkages may be imperiled, however, if funding for these other key health care services lags far behind the enormous increases in funding for HIV/AIDS services from multiple sources.
Recommendation 6-1: The U.S. Global AIDS Coordinator should continue to promote and support a community-based, family-centered model of care in order to enhance and coordinate supportive care services for people living with HIV/AIDS, with special emphasis on orphans, vulnerable children, and people requiring end-of-life care. This model should include integration as appropriate with prevention and treatment programs and linkages with other public-sector and nongovernmental organization services within and outside of the health sector, such as primary health care, nutrition support, education, social work, and the work of agencies facilitating income generation.
CONCLUSION
As discussed at PEPFAR’s third annual meeting in Durban, South Africa (OGAC, 2006e), challenges to PEPFAR’s care services include the limited attention care has received as a result of confusion about what PEPFAR means by palliative care, as well as budgetary constraints; implementation
issues related to preventive care, such as the cost and replenishment of consumables; the integration of palliative care with other services; concern about the ability of programs to meet the increased demand for services resulting from voluntary counseling and testing; questions about how to measure the quality of services and define who can be counted as receiving care; expansion of care services to primary health centers; and the difficulty of ensuring adequate and appropriate commodities, such as medications for pain and management of opportunistic infections, especially TB (OGAC, 2006e).
OGAC’s continued inclusion of global care-related guidance in PEPFAR-supported programs underscores its commitment to harmonization and collaboration with other global stakeholders. As the evidence base grows and communities learn more about how best to deal with the epidemic, these practices need to be scaled up and tailored to the needs of other communities. If international standards indicate that insecticide-treated bed nets are effective and should be provided to members of all households to decrease exposure to opportunistic infections such as malaria, for example, PEPFAR-supported preventive care services need to be linked with wrap-around programs that will support such interventions. If specific pharmaceuticals are recommended to treat opportunistic infections such as TB and malaria, establishing linkages with regional and national program managers with responsibility for supply chain management to ensure their timely availability will be necessary. More widespread and consistent inclusion of international guidance may contribute to improved integration of services within service categories, as well as across the continuum of services.
PEPFAR-supported care programs need to support and promote community-based, family-centered care. Although this is part of the program’s approach to care delivery, all program implementers could benefit from improved articulation of these expectations. Consensus guidance that is well articulated will facilitate the development of clear standards for the provision and quality of community-based services for families that will contribute to a sustainable response to the epidemic. The Committee is cognizant that its recommendation to this end could have the unintended consequence of increasing the caregiving burden of women and girls; therefore, careful attention to the need for concomitant interventions to ameliorate this effect is essential.
PEPFAR’s success in achieving its 5-year target of providing care to 10 million people, as well as in providing care services thereafter, is contingent upon how it defines what it means to have received care services. A simple numerical count is inadequate because an evaluator or program manager cannot know just what services a person has received beyond “care” or whether the count provides an accurate number of people receiving specific types of services or the number of times a person has been served.
In addition, the Committee believes OGAC recognizes that PEPFAR faces challenges in measuring the quality of services rendered by providers of varying levels of skills. Issuance of PEPFAR’s preventive care package was a step toward defining quality care by standardizing basic preventive care services, and efforts to train service providers according to national and international standards where they exist contribute to standardization of care, but challenges remain in the way quality of care services is measured.
Finally, the Committee believes it is critical for OGAC to improve integration of services both within service categories and across the continuum of illness regardless of budget constraints. Successful integration can facilitate the provision of comprehensive services from the facility to the household and community levels, and ensure that everyone living with and affected by HIV/AIDS will be able to access services that are culturally appropriate, affordable, and timely.
REFERENCES
Abu-Raddad, L. J., P. Patnaik, and J. Kublin. 2006. Dual infection with HIV and malaria fuels the spread of both diseases in sub-Saharan Africa. Science 314:1603–1606.
AVERT. 2006. HIV-related opportunistic infections: Prevention and treatment. http://www.avert.org/aidscare.htm (accessed October 31, 2006).
Coleman, C. L., L. S. Eller, K. M. Nokes, E. Bunch, N. Reynolds, I. Corless, P. Dole, J. K. Kemppainen, D. Wantland, K. Kirksey, L. Seficik, P. Nicholas, J. J. Hamilton, Y.-F. Tsai, and W. L. Holzemer. 2006. Prayers as a complimentary health strategy for managing HIV related symptoms among an ethnically diverse sample. Holistic Nursing Practice 20(2):65–72.
Corless, I. G., E. H. Bunch, J. K. Kemppainen, W. L. Holzemer, K. M. Nokes, L. S. Eller, C. J. Portillo, E. Butensky, P. K. Nicholas, C. A. Bain, S. Davis, K. M. Kirksey, and F.-Y. Chou. 2002. Self-care for fatigue in HIV disease. Oncology Nursing Forum 29(5):E60–E69).
Donahue, J. 2005. Strengthening households and communities: The key to reducing the economic impacts of HIV/AIDS on children and families. In A generation at risk: The global impact of HIV/AIDS on orphans and vulnerable children. Edited by G. Foster, C. Levine, and J. Williamson. New York: Cambridge University Press. Pp. 37–65.
Dybul, M. 2006 (July 13). The President’s Emergency Plan for AIDS Relief: Looking back and looking forward. Remarks as prepared to Center for Strategic and International Studies. http://www.pepfar.gov (accessed January 3, 2007).
Eller, L. S., I. B. Corless, E. H. Bunch, J. K. Kemppainen, W. L. Holzemer, K. Nokes, C. J. Portillo, and P. Nicholas. 2005. Self-care strategies for depression in persons with HIV disease. Journal of Advanced Nursing 51(12):119–130.
Fleischman, J. 2006. Integrating reproductive health and HIV/AIDS programs: Strategic opportunities for PEPFAR. Washington, DC: Center for International and Strategic Studies.
Foster, G., C. Levine, and J. Williamson. 2005. A generation at risk: The global impact of HIV/AIDS on orphans and vulnerable children. New York: Cambridge University Press.
FSPC (Family Strengthening Policy Center). 2004. Policy brief: Introduction to family strengthening. Washington, DC: National Human Services Assembly.
Gass, R. N, C. Luo, N. Ngongo, S. Crowley, G. Tene, G. Sherman, and A. Harries. 2006. Scaling up pediatric HIV care and treatment in resource-constrained settings. Presentation at the XVI International AIDS Conference, Toronto, Canada.
GHC (Global Health Council). 2005. Faith in action: Examining the role of faith-based organizations in addressing HIV/AIDS. Washington, DC: GHC.
Harding, R., and I. Higginson. 2004. Palliative care in sub-Saharan Africa: An appraisal. London: King’s College London, University of London.
Harding, R., and I. Higginson. 2005. Palliative care in sub-Saharan Africa. Lancet 365:1971–1977.
Harding, R., D. Karus, P. Easterbrook, V. H. Raveis, I. J. Higginson, and K. Marconi. 2005. Does palliative care improve outcomes for patients with HIV/AIDS? A systematic review of the evidence. Sexually Transmitted Infections 81:5.
HIV Insite. 2006 (July 27). Routine or opt-out counselling and testing: Findings from the 2006 PEPFAR meeting. http://hivinsite.ucsf.edu/InSite?page=pa-hatip-71/ (accessed October 31, 2006).
Holzemer, W. L. 2002. HIV and AIDS: The symptom experience: What cell counts and viral loads won’t tell you? American Journal of Nursing 102(4):48–52.
ICRW (International Center for Research on Women). 2005. Towards achieving gender equality and empowering women. Washington, DC: ICRW.
JLI (The Joint Learning Initiative on Human Resources for Health and Development). 2004. Human resources for health: Overcoming the crisis. Boston, MA: Harvard University.
Kaiser Family Foundation. 2006 (October 27). Daily HIV/AIDS report: Botswana launches infant HIV testing program. http://www.kaisertnetwork.org (accessed October 27, 2006).
Kalichman, S. 1995. Understanding AIDS: A guide for mental health professionals. Washington, DC: American Psychological Association.
Kemppainen, J. K., L. S. Eller, E. Bunch, M. J. Hamilton, P. Dole, W. Holzemer, K. Kirksey, P. K. Nicholas, I. B. Corless, C. Coleman, K. M. Nokes, N. Reynolds, L. Sefcik, D. Wantland, and Y.-F. Tsai. 2006. Strategies for self-management of HIV-related anxiety. AIDS Care 18(6):597–607.
Makoae, L. N., N. M. Seboni, K. Molosiwa, M. Moleko, S. Human, N. A. Sukati, and W. L. Holzemer. 2005. The symptom experience of people living with HIV/AIDS in Southern Africa. Journal of the Association of Nurses in AIDS Care 16(3):22–32.
Mermin, J. 2005 (May 26). Community and home-based preventive care and ART. Presentation at the PEPFAR Second Annual Field Meeting, Addis Ababa, Ethiopia.
Nicholas, P., J. K. Kemppainen, G. E. Canaval, I. B. Corless, E. F. Sefcik, K. M. Nokes, C. A. Bain, K. Kirksey, L. S. Eller, P. Dole, J. J. Hamilton, C. L. Coleman, W. L. Holzemer, N. Reynolds, C. J. Portillo, E. H. Bunch, D. J. Wantland, J. Voss, R. Phillips, Y.-F. Tsai, M. R. Mendez, T. Lindgren, S. M. Davis, and D. M. Gallagher. 2007. Symptom management and self-care for peripheral neuropathy in HIV/AIDS. AIDS Care 19(2):179–189.
OGAC (Office of the U.S. Global AIDS Coordinator). 2004. The President’s Emergency Plan for AIDS Relief: U.S. five-year global HIV/AIDS strategy. Washington, DC: OGAC.
OGAC. 2005a. PEPFAR first annual report to Congress. Washington, DC: OGAC.
OGAC. 2005b. The President’s Emergency Plan for AIDS Relief: Indicators, reporting requirements, and guidelines for focus countries (revised for FY2006 reporting). Washington, DC: OGAC.
OGAC. 2005c. Final draft HIV/AIDS palliative care guidance #1: An overview of comprehensive HIV/AIDS care services in the President’s Emergency Plan for AIDS Relief. Washington, DC: OGAC.
OGAC. 2005d. FY2005 Country Operational Plans. Washington, DC: OGAC.
OGAC. 2006a. FY2006 Country Operational Plans. Washington, DC: OGAC.
OGAC. 2006b. PEPFAR second annual report to Congress. Washington, DC: OGAC.
OGAC. 2006c. PEPFAR report on work force capacity and HIV/AIDS. Washington, DC: OGAC.
OGAC. 2006d. HIV/AIDS palliative care guidance #1: An overview of comprehensive HIV/AIDS care services in the President’s Emergency Plan for AIDS Relief. Washington, DC: OGAC.
OGAC. 2006e (June 12–15). Building on successes: Ensuring long-term solutions. Annotated version of rapporteur presentations at the President’s Emergency Plan for AIDS Relief 2006 HIV/AIDS Implementers’ Meeting, Durban, South Africa.
OGAC. 2006f. Adult preventive care guidance. Washington, DC: OGAC.
OGAC. 2006g. Palliative care technical working group plan. Washington, DC: OGAC.
OGAC. 2006h. Responding to the needs of women and girls: Reproductive health and HIV/AIDS linkages (PowerPoint Presentation). Washington, DC: OGAC.
OGAC. 2007a. PEPFAR third annual report to Congress. Washington, DC: OGAC.
OGAC. 2007b. Office of the Global AIDS Coordinator’s Suggested Factual Changes to the PEPFAR Implementation: Progress and Promise Report. Email communication to IOM staff on March 29, 2007.
Peng, V. 2006 (June 2). Challenge of integrated supervision of vertical health programs in Cambodia. Presentation by USAID/URC Project for Health-Systems Strengthening, Phnom Penh, Cambodia.
Rehle, T., T. Saidel, S. Mills, and R. Magnani (eds.). 2000. Evaluating programs for HIV/AIDS prevention and care in developing countries: A handbook for program managers and decision makers. Arlington, VA: Family Health International.
Ro, M., H. Treadwell, and M. Northridge. 2003. Community health workers and community voices: Promoting good health. Battle Creek, MI: W. K. Kellogg Foundation.
UNAIDS (Joint United Nations Programme on HIV/AIDS) and UNICEF (United Nations Children’s Fund). 2004. The framework for the protection, care and support of orphans and vulnerable children living in a world with HIV and AIDS. Geneva, Switzerland: UNAIDS.
UNICEF. 2006. Africa’s orphaned and vulnerable generations: Children affected by AIDS. New York: UNICEF.
UNICEF and WHO (World Health Organization). 2006. Management of sick children by community health programme workers: Intervention models and programme examples. New York: UNICEF.
WHO (World Health Organization). 2004a. Emergency scale-up of antiretroviral therapy in resource-limited settings: Technical and operational recommendations to achieve 3 by 5. Geneva, Switzerland: WHO.
WHO. 2004b. Guide to monitoring and evaluating HIV/AIDS care and support. Geneva, Switzerland: WHO.
WHO. 2004c. A community health approach to palliative care for HIV/AIDS and cancer patients in sub-Saharan Africa. Geneva, Switzerland: WHO.
WHO. 2006. Scaling up HIV/AIDS prevention, treatment and care: A report on WHO support to countries in implementing the “3 by 5” initiatives 2004–2005. Geneva, Switzerland: WHO.
Yengi, W. 2005. Expanding HIV care and treatment in the southern Highlands of Tanzania: Support of ART through home-based care outreach. Presentation at the PEPFAR Second Annual Field Meeting, Addis Ababa, Ethiopia.




































