4
A Model for Delivering Psychosocial Health Services
CHAPTER SUMMARY
Many different providers of health services—some in oncology, some delivering health care for other complex health conditions—recognize that psychosocial problems can have both direct and indirect effects on health and have developed interventions to address them. Some of these interventions are derived from theoretical or conceptual frameworks; some are based on research findings; and some have undergone empirical testing. The best have all three characteristics. When viewed together, these interventions evidence common elements that point to a model for the effective delivery of psychosocial health services. The components of this model include (1) identifying patients with psychosocial health needs that are likely to affect their health or health care, and developing with patients appropriate plans for (2) linking patients to appropriate psychosocial health services, (3) supporting patients in managing their illness, (4) coordinating psychosocial with biomedical health care, and (5) following up on care delivery to monitor the effectiveness of services and determine whether any changes are needed. Effective patient–provider communication is central to all of these components.
EFFECTIVE DELIVERY OF PSYCHOSOCIAL HEALTH CARE
The committee conducted a search1 to identify empirically validated models of the effective delivery of psychosocial health services. This search
|
1 |
This search involved reviewing peer-reviewed literature, seeking recommendations from experts in the delivery of cancer and other complex health care (experts contacted are listed in Appendix B), and investigating models otherwise identified by the committee. |
yielded a number of models tested and found to be effective in delivering these services and improving health. These models are described in Annex 4-1 at the end of this chapter and are listed in Table 4-1, which highlights components common to many or all of them: (1) identifying patients with psychosocial health needs that are likely to affect their ability to receive health care and manage their illness, and developing with patients appropriate plans for (2) linking patients to appropriate psychosocial health services, (3) supporting them in managing their illness, (4) coordinating psychosocial with biomedical health care, and (5) following up on care delivery to monitor the effectiveness of services and determine whether any changes are needed. Table 4-1 also includes practice guidelines, produced through systematic reviews of evidence, that identify approaches for the effective delivery of psychosocial health services, along with the consensus-based guidelines for Distress Management developed by the National Comprehensive Cancer Network (NCCN)—an alliance of 21 leading U.S. cancer centers. The various ways in which these programs carry out some of these functions also are listed in the table and elaborated on in the text that follows.
Evidence derived from the models listed in Table 4-1 (summarized in Annex 4-1) strongly suggests that a combination of activities rather than any single activity by itself (e.g., screening, case management, illness self-management) is needed to deliver appropriate psychosocial health care effectively to individuals with complex health conditions. This conclusion also is supported by the findings of several systematic reviews of psychosocial care. For example, not surprisingly, screening by itself is less effective than screening with follow-up. The U.S. Preventive Services Task Force, for instance, recommends screening for depression in adults in clinical practices only when practices have systems in place to ensure effective follow-up treatment and ongoing monitoring. This recommendation reflects research finding that only small benefits result from screening by itself, but larger benefits when screening is accompanied by effective follow-up (U.S. Preventive Services Task Force, 2002). Consistent with this finding, a review of studies of interventions to improve the management of depression in primary care settings found that those with the most multidimensional approaches (such as case management combined with clinician education and structured links to connect primary and specialty medical care) were most likely to achieve desired outcomes (Gilbody et al., 2003). Another systematic review of randomized controlled trials designed to improve the use of needed health and social services after hospital discharge found that interventions emphasizing follow-up on the results of a needs assessment showed more positive results than needs assessment alone (Richards and Coast, 2003).
In this chapter, the committee recommends a unifying model for plan-
TABLE 4-1 Models for Delivering Psychosocial Health Services and Their Common Components
|
Model |
Common Componentsa |
|||||
|
Identification of Patients with Psychosocial Health Needs |
Care Planning to Address Those Needs |
Mechanisms to Link Patients to Psychosocial Health Services |
Support for Illness Self-Management |
Mechanisms for Coordinating Psychosocial and Biomedical Care |
Follow-up on Care Delivery |
|
|
Building Health Systems for People with Chronic Illnesses (Palmer and Somers, 2005) |
Risk and eligibility screening |
Yes |
Care managementb |
Yes |
Multidisciplinary team care |
Outcome measurement |
|
Needs assessment |
|
|
|
Pooled funding |
|
|
|
Chronic Care Model (ICIC, 2007) |
No |
Yes |
Linkage to community resources |
Yes |
Clinical information systems |
Use of information systems to accomplish this |
|
|
|
|
|
Team care |
|
|
|
|
|
Case management for complex cases |
|
|
Planned or structured follow-up visits |
|
|
Clinical Practice Guidelines for Distress Management (NCCN, 2007a) |
Screening for distress |
Yes |
Social work and referral services |
No |
Coordination of oncology team |
Yes |
|
Needs assessment |
|
|
|
|
|
|
|
Model |
Common Componentsa |
|||||
|
Identification of Patients with Psychosocial Health Needs |
Care Planning to Address Those Needs |
Mechanisms to Link Patients to Psychosocial Health Services |
Support for Illness Self-Management |
Mechanisms for Coordinating Psychosocial and Biomedical Care |
Follow-up on Care Delivery |
|
|
Clinical Practice Guidelines for the Psychosocial Care of Adults with Cancer (National Breast Cancer Centre and National Cancer Control Initiative, 2003) |
Screening for anxiety/depression |
No |
Development of referral pathways and networks |
No |
Multidisciplinary team care |
Yes |
|
Coordinator of care designated by patient |
Coordinator of care designated by patient |
|||||
|
Collaborative Care of Depression in Primary Care (Katon, 2003) |
Use of standardized screening and diagnostic tools for depression |
Yes |
Structured, formal arrangement for psychiatric consultation |
Yes |
Case conferences |
Surveillance of medication use and patient outcomes |
|
Mental health specialists located within primary care sites |
||||||
|
Improving Supportive and Palliative Care for Adults with Cancer (NICE, 2004) |
Needs assessment |
Yes |
Yes |
Identified as part of rehabilitation services |
Multiple strategies including, e.g., multidisciplinary teams, information systems, patient-held records |
Yes |
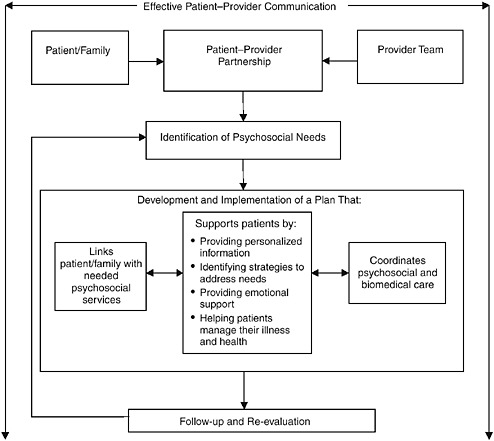
FIGURE 4-1 Model for the delivery of psychosocial health services.
ning and delivering psychosocial health care for patients with cancer. This model is based on the evidence yielded by the models listed in Table 4-1, evidence suggesting added value from multiple components of effective care delivery, and evidence (presented below) supporting the contributions of many of these individual components to the effective provision of psychosocial health care. The committee’s model, illustrated in Figure 4-1, integrates the five common components identified above. Although these components individually are in some cases supported by research findings, in other cases there may not be strong evidence of their effectiveness as stand-alone interventions. Nonetheless, the committee recommends their inclusion based on their presence in the reviewed models and with the understanding that
a lack of research findings is not necessarily synonymous with ineffectiveness.2 We also note that effective patient–provider communication is central to the success of all five components of the model. The model is described in detail below.
A UNIFYING MODEL FOR CARE DELIVERY
Effective Patient–Provider Communication
At the heart of the committee’s model is a well-functioning patient–provider partnership, characterized, in large part, by effective communication. Communicating effectively means that patients are able to receive and understand information about their illness and health care, and clearly express their needs for assistance and the values and personal resources that will shape the health care system’s response to these needs. Patients should be comfortable with asking questions of all their care providers and equally comfortable with responding to questions posed to them. They should be competent and at ease as a member of their own health care team, which will make decisions about the best strategy for addressing their illness. Patients with language barriers, cognitive deficits, or other impediments to communication should receive assistance in overcoming these barriers to effective communication.
In many instances, members of the patient’s family also are involved in this communication. In pediatric cases, a family member may be the primary communicator and participant in planning care; with adults, some patients may also have limited capacity to communicate. Even when adult patients are able to communicate, as discussed in Chapters 1 and 2, family members are key caregivers, especially for older adults. Treatment planning and planning for managing the effects of illness requires communication with the patient’s caregivers as well as with the patient. When patients do not have the capacity to participate actively themselves, there needs to be an explicit substitute who is legally and psychologically able to act as the patient’s advocate.
Care providers similarly should possess the communication skills necessary to be effective clinicians and supportive partners in care—a hallmark of high-quality health care (IOM, 2001) and health care professionals (IOM, 2003). These communication skills include establishing a good interpersonal relationship with the patient (Arora, 2003). Key aspects of
|
2 |
For example, an intervention may be so obviously helpful (e.g., providing transportation to help those without means to get to their appointments to do so) that it (rightly) has not been a priority for research (see Chapter 3), or a research design may not have been sufficient to detect the outcome of interest. |
effective patient–clinician communication identified in the National Cancer Institute (NCI) report Patient-Centered Communication in Cancer Care include (1) fostering healing relationships, (2) exchanging information, (3) responding to emotions, (4) managing uncertainty, (5) making decisions, and (6) enabling patient self management (Epstein and Street, 2007). As described in Chapter 1, however, these attributes are not commonly found in cancer care today.
Current Patient–Provider Communication
Most patients, including those with cancer, say they want more information from their physicians (Guadagnoli and Ward, 1998; Wong et al., 2000; Gaston and Mitchell, 2005; Kahán et al., 2006; Kiesler and Auerbach, 2006). Patients report being dissatisfied with the limited information they receive and when they receive it. Clinicians often have a limited understanding of patients’ information needs, knowledge, and concerns. As a result, they fail to provide the type or amount of information patients need and communicate in language that patients often do not understand (Kerr et al., 2003a,b; Kahán et al., 2006; Epstein and Street, 2007). Clinicians’ delivery of bad news is particularly problematic. Conversely, patients do not always disclose relevant information about their symptoms or concerns (Epstein and Street, 2007).
Further, the majority of patients (ranging in studies from 60 to 90 percent) say that they prefer either an active or shared/collaborative role in decisions made during office visits (Mazur and Hickman, 1997; Guadagnoli and Ward, 1998; Dowsett et al., 2000; Wong et al., 2000; Gattellari et al., 2001; Bruera et al., 2002; Davison et al., 2002, 2003; Keating et al., 2002; Davison and Goldenberg, 2003; Janz et al., 2004; Gaston and Mitchell, 2005; Katz et al., 2005; Mazur et al., 2005; Ramfelt et al., 2005; Siminoff et al., 2005; Flynn et al., 2006; Hack, 2006). However, studies show that physicians substantially underestimate patients’ desire for an active or shared role in their care (Bruera et al., 2002; Janz et al., 2004; Kahán et al., 2006).
Some physicians, particularly female and primary care physicians, have a more participatory or collaborative style with patients (Kaplan et al., 1996; Cooper-Patrick et al., 1999; Roter et al., 2002; Street et al., 2003). Lower levels of participatory decision making among physicians have been associated with several patient characteristics, including age, education, and minority status (Kaplan et al., 1996; Cooper-Patrick et al., 1999; Adams et al., 2001; Xu et al., 2004), although these patient characteristics do not account for the majority of the variation in conversational behavior among either physicians or patients during office visits (Kaplan et al., 1995; Benbassat et al., 1998). There is evidence that physicians and
patients mutually influence each other’s conversational behavior (Robinson and Roter, 1999; Del Piccolo et al., 2002; Street et al., 2003, 2005; Butow et al., 2004; Janz et al., 2004; Maly et al., 2004; Gordon et al., 2005; Kindler et al., 2005; Adler, 2007) and that physicians may take their cues in part from patients, who typically exhibit relatively passive behavior during office visits (Gordon et al., 2005, 2006a,b; Street and Gordon, 2006). Such passivity characterizes even physicians when they become patients. The average patient asks five or fewer questions during a 15-minute office visit, and many ask no questions (Brown et al., 1999, 2001; Sleath et al., 1999; Cegala et al., 2000; Butow et al., 2002; Bruera et al., 2003; Kindler et al., 2005). Among the most passive patients are those above age 60, those with more severe illness or multiple comorbid conditions (including psychological distress), those who are less well educated, and males (Butow et al., 2002; Sleath and Rubin, 2003; Street et al., 2003; Maliski et al., 2004; Gaston and Mitchell, 2005; Flynn et al., 2006; Gordon et al., 2006b; Siminoff et al., 2006a). Minorities also have been noted to be more passive in physician–patient interactions (Gordon et al., 2005; Street et al., 2005; Siminoff et al., 2006a; Gordon et al., 2006b). Moreover, a systematic review of randomized controlled trials and uncontrolled studies of interventions designed to improve the provision of information and encourage participation in decision making by patients with advanced cancer found that although almost all patients expressed a desire for full information, only about two-thirds wished to participate actively in decision making about their care (Gaston and Mitchell, 2005).
Correspondence between patients’ preferred role in decision making and their actual role during office visits with physicians, although intuitively compelling, has relatively little empirical support as a factor affecting patient outcomes and quality of care. However, such correspondence has been linked with reduced anxiety (Gattellari et al., 2001; Kahán et al., 2006) and depression (Schofield and Butow, 2003), satisfaction with treatment choices (Keating et al., 2002), and more appropriate treatment choices (Siminoff et al., 2006b). The NCI report Patient-Centered Communication in Cancer Care articulates a comprehensive research agenda for better understanding and intervening to improve patient–provider communication (Epstein and Street, 2007).
The Importance of Communication
There is reason to be concerned about findings of poor communication and lack of patient involvement. A substantial body of evidence indicates that effective physician–patient communication is positively related to patients’ health outcomes (Kaplan et al., 1989; Stewart, 1995; Piccolo et al., 2000; Heisler et al., 2002; Engel and Kerr, 2003; Kerr et al., 2003a,b;
Schofield and Butow, 2003; Maliski et al., 2004). Patients of physicians who involve them in treatment decisions during office visits have better health outcomes than those of physicians who do not (Kaplan et al., 1995; Adams et al., 2001; Gattellari et al., 2001; Hack et al., 2006). Physicians’ participatory decision-making style also is positively related to the quality and outcomes of patient care generally (Guadagnoli and Ward, 1998), including continuity of care (Kaplan et al., 1996), health outcomes (Adams et al., 2001; van Roosmalen et al., 2004), decreased psychological distress (Zachariae et al., 2003), trust in the physician (Berrios-Rivera et al., 2006; Gordon et al., 2006a,b), more preventive health services (Woods et al., 2006), better communication with physicians (Thind and Maly, 2006), and satisfaction with care (Kaplan et al., 1996; Adams et al., 2001). Similar benefits are found specifically in cancer care (Arora, 2003).
Interventions to Improve Communication
Many clinicians have identified a need for stronger communication skills for themselves, their patients, and families. Interventions to improve physician–patient communication have targeted either physicians or patients; few have targeted both simultaneously (Epstein and Street, 2007).
Training physicians to negotiate with patients has been found to increase patient involvement in treatment decisions (Timmermans et al., 2006). A substantial literature also documents the effects of interventions aimed at improving patients’ participation in their care (Epstein and Street, 2007). Such interventions include those aimed at improving patients’ participation in multiple decisions over multiple visits with physicians (e.g., question asking, decision elicitation, and negotiation skills), enhancing the presentation of options, tailoring risk information, and providing testimonials describing outcomes of treatment to help patients participate in single or discrete decisions and improve information seeking (question asking).
The means used to deliver these interventions also vary widely. “Coached care” for chronic disease makes use of patient medical records, guidelines for clinical care management reviewed with patients before office visits, and coaching in using information to participate effectively with physicians. This approach has been linked with improved physiological and functional patient outcomes and increased patient participation in physician–patient communication among patients with chronic disease (Greenfield et al., 1988; Kaplan et al., 1989; Rost et al., 1991; Keeley et al., 2004). Decision aids to assist patients in choosing among treatment options have been shown to decrease decisional conflict, increase satisfaction with treatment decisions (Whelan et al., 2004), and decrease adjuvant therapy for low-risk patients with breast cancer (Peele et al., 2005; Siminoff et al., 2006b).
An extensive literature documents the beneficial effects of interactive videos presenting treatment options, tailored risk information, and patient
testimonials describing outcomes of treatment. Benefits include improved functional outcomes, increased confidence in treatment, and increased satisfaction with decision making (Flood et al., 1996; Liao et al., 1996; Barry et al., 1997). Following similar interventions, others have noted changes in patients’ treatment choices, favoring less invasive treatment (Mazur and Merz, 1996). O’Connor and colleagues (1995) note that these types of decision aids, compared with usual care, yield improvements in patients’ knowledge of their disease and its treatment, more realistic expectations, less decisional conflict, more active participation in office visits, and less indecision about options. No effect on patient anxiety was observed. Videos with or without supporting materials have been shown to enhance patients’ understanding of treatment options (Onel et al., 1998) and physician–patient communication during office visits (Frosch et al., 2001; Brown et al., 2004a). In a review of small media interventions, counseling and small-group education sessions, or a combination of these approaches, Briss and colleagues (2004) found that while such interventions increased patients’ knowledge about their disease and the accuracy of their risk perceptions, whether such interventions lead to increased patient participation in treatment decisions has been less well studied.
Other interventions to improve patient participation in care, such as the use of question-prompt sheets, audiotaping of visits, or more basic decision aids, have been linked with greater patient involvement in treatment decisions (Butow et al., 1994; Guadagnoli and Ward, 1998; Cegala et al., 2000; Maly et al., 2004; Gaston and Mitchell, 2005).
Conclusions
Despite strong evidence for the importance of effective patient–provider communication and patients’ participation in decision making in achieving better health care outcomes, such communication is not yet the norm. As described above and in Chapter 1, physician–patient communication is generally inadequate, and patients are poorly prepared for communicating effectively (whether this involves simple information-seeking skills or more active involvement in treatment decisions). Physicians, too, are poorly prepared to elicit patients’ information needs and preferences for involvement in their care. There is a need for more creative and intensive interventions to enhance patient–physician communication and support patient decision making, targeting in particular those most at risk (e.g., older adults, those of lower socioeconomic status, and those with comorbid conditions including psychosocial distress and decreased cognition). Many approaches are being tested to meet this need. These approaches require more rigorous evaluation, especially in less well-organized health care settings.
NCI’s state-of-the-science report on patient-centered communication in cancer care (Epstein and Street, 2007) can inform clinical practice, as well
as research. This report finds that most skill-building interventions targeting clinicians consist of formal training as part of medical education or continuing education programs (e.g., a 3-day course on communication skills) to increase clinician knowledge and improve communication behaviors. Very little research has focused on changing clinical practices and health care systems. With respect to clinician education and training programs, the report finds that the most effective communication skill-building programs are those that are carried out over a long period of time, use multiple teaching methods, allow for practice, provide timely feedback, and allow clinicians to work in groups with skilled facilitators. The report also finds that because clinicians develop routines for interacting with patients early in their careers, communication training should occur early in professional education. Clinicians should seek out such opportunities for communication training as part of their continuing education activities. Training is available from such sources as the Institute for Healthcare Communication (http://www. healthcarecomm.org/index.php) to improve knowledge, skills, and clinical practice in communication with patients.
With respect to improved patient communication, use of tools to support communication and formal strategies to teach communication techniques to patients have been found effective in improving communication with clinicians. These tools and techniques include encouraging patients to write down their questions and concerns prior to meeting with clinicians; providing written “prompts” to patients that serve as reminders of key questions or issues; and providing information and decision aids about the illness, treatment, and health through booklets, videos, coaching sessions, and use of diaries (Epstein and Street, 2007). Patient advocacy organizations can play an important role in strengthening the patient side of the patient–provider partnership through the provision of such tools and training. An example is the Cancer Survival Toolbox (available free of charge), which teaches people with cancer how to obtain information, make decisions, solve problems, and generally communicate more effectively with health care providers (Walsh-Burke et al., 1999; NCCS, 2007).
Identifying Patients with Psychosocial Health Needs
Identifying psychosocial health needs is the essential precursor to meeting those needs. This can occur in several ways: (1) patients may volunteer information about these needs in their discussions with health care providers; (2) providers may ask about psychosocial health needs during structured or unstructured clinical conversations with the patient; (3) providers may screen patients using validated instruments; and (4) providers may perform an in-depth psychosocial assessment of patients after or independently of screening. These approaches vary considerably in their reliability and their sensitivity in uncovering patients’ needs.
Relying on patients to volunteer information or on providers to elicit it in the course of standard care both are unlikely to be adequate. A study of the ability of medical oncologists and nurses in the United States to recognize on their own the psychosocial problems of their oncology patients found that these providers frequently failed to detect depression at all and when they did, greatly underestimated its seriousness (Passik et al., 1998; McDonald et al., 1999). This finding parallels data on the low rate of detection of depression in primary care settings when depression screening tools are not used. And while there is evidence for the effectiveness of structured clinical interviews in detecting some psychosocial needs (e.g., for treatment of depression), this approach is criticized for the amount of time it takes and the requirement for specialized (costly) personnel to conduct the interviews (Trask, 2004). Patients’ reluctance to volunteer information about their need for psychosocial services (Arora, 2003) can also impede the detection of problems.
In contrast, several screening tools and in-depth needs assessment instruments have been found to be effective in reliably identifying individuals with psychosocial health needs. Screening involves the administration of a test or process to individuals who are not known to have or do not necessarily perceive that they have or are at risk of having a particular condition or need. It is used to identify those who are likely to have a condition of interest and should benefit from its detection and treatment. A screening instrument yields a yes or no answer as to whether an individual is at high risk. A positive screen should be followed by a more in-depth needs assessment. In some practices, needs assessment may be performed without a preceding screen.
Screening
Many screening instruments are brief and can be self-administered by the patient—sometimes in the waiting room before a visit with the clinician. Instruments range from the low-tech, requiring only paper and pencil, to the high-tech, using a computer-based touch screen; some of the latter instruments automatically compare responses with those given previously and generate an automatic report to the clinician. The success of many practices in using such screening tools counters generalizations that patients are unwilling to discuss psychosocial concerns. Still, as discussed below, too few clinicians employ these reliable methods routinely to identify patients with psychosocial health needs.
Current practice Screening for psychosocial health needs using validated instruments is not routinely practiced in oncology. In a national survey3 of
1,000 randomly selected members of the American Society of Clinical Oncology, 14 percent of respondents reported screening for psychosocial distress using a standardized tool. A third reported that they did not routinely screen for distress. Of the 65 percent that did routinely screen, 78 percent did so using some combination of asking direct questions (61 percent), such as “How are you coping?”, “Are you depressed?”, or “How do you feel?”; observing patients’ moods (57 percent); taking their history (53 percent); talking to family members (44 percent); or other methods. Similarly, of 15 organizations responding to a survey of 18 member institutions of NCCN, only 8 reported that they routinely screened for distress in at least some of their patients. Of these 8, 3 screened as part of a patient interview, 2 used a self-report measure, and 3 used both. Only 3 routinely screened all of their patients; the majority screened only certain groups of patients, such as those undergoing bone marrow transplantation or those with breast cancer (Jacobsen and Ransom, 2007).
Reasons given by individual oncologists for not screening include a lack of time, a perception of limited referral resources, a belief that patients are unwilling or resistant to discussing distress, and uncertainty about identifying and treating distress.4 Reasons given by member institutions of NCCN for not screening include screening not considered necessary or worthwhile (one institution), not enough resources to address those identified by a screener as needing care (one institution), and insufficient resources to both screen and address identified needs (one institution). The other institutions reported that they were currently in the process of pilot testing procedures for routine screening for distress (Jacobsen and Ransom, 2007).
The above concerns may not be justified. The experiences of those who have developed or now use screening tools show that screening need not take much time and that patients are willing to communicate their distress. Further, research shows that physicians’, nurses’, and other personnel’s individual assessments of the levels of stress experienced by patients or their family members are less accurate than a standardized instrument (Hegel et al., 2006). Although there remain some unresolved issues in screening that could be addressed by further research (see Chapter 8), the research and implementation examples reviewed below and in Chapter 5 demonstrate that screening can be both an effective and a feasible mechanism for identifying individuals with psychosocial health needs. The variation among existing validated screening instruments can facilitate the inclusion of screening in routine clinical practice by accommodating the differing interests and resources of various clinical sites. Patient Care Monitor (PCM), for example, is automated and part of a comprehensive patient assessment, care, and education system. Other instruments, such as the
Distress Thermometer, require nothing more than paper and pencil. Most are administered by patients themselves. Although some must be purchased commercially and require a licensing agreement and fee, others are available at no cost.
Screening tools In addition to having strong predictive value,5 effective screening tools should be brief and feasible for routine use in various clinical settings. Such tools are available for screening patient populations and identifying individuals with some types of psychosocial health care needs. For example, a number of screening tools for detecting mental health problems, such as anxiety, depression, adjustment disorders, or post-traumatic stress disorder (PTSD) or post-traumatic stress syndrome (PTSS), have been tested with cancer survivors in different oncology settings and found to meet these criteria. The Brief Symptom Inventory (BSI)©-18, for example, measures depression, anxiety, and overall psychological distress level in approximately 4 minutes (Derogatis, 2006). Its reliability, validity, sensitivity, and specificity have been documented in tests involving more than 1,500 cancer patients with more than 35 different cancer diagnoses (Zabora et al., 2001), as well as adult survivors of childhood cancer (Recklitis et al., 2006). The Hospital Anxiety and Depression Scale (HADS) also is useful in screening individuals with cancer or other illnesses for psychological distress because its 14-item, self-report questionnaire omits measures of fatigue, pain, or other somatic expressions of psychological distress that could instead be symptoms of physical illness and confound the interpretation of screening results (Zigmond and Snaith, 1983). Other useful psychological screening tools include, for example, the Brief Zung Self-Rating Depression Scale; Rotterdam Symptom Checklist; Beck Depression Inventory-Short Form (Trask, 2004); PTSD Checklist-Civilian Version (Andrykowski et al., 1998); Patient Health Questionnaire (PHQ), SF (Short Form)-8; 4-item Primary Care PTSD Screen (Hegel et al., 2006); and PHQ-9 (Lowe et al., 2004).
However, in addition to unresolved questions about the appropriate use and interpretation of the results obtained with these psychological screening tools (Trask, 2004; Mitchell and Coyne, 2007), their varying foci necessitate either administering multiple tools—infeasible for most clinical
settings6—or choosing among them. No guidance exists with respect to which tools should be used for the different types of patients seen in various clinical settings. Moreover, these tools do not screen for the broader array of psychosocial health needs. If, for example, an individual has inadequate social support or financial resources but perceives this situation as the norm or does not experience clinically significant anxiety or depression, these screening instruments may not identify this individual as having psychosocial health needs. In a small study of distress in 50 candidates for bone marrow transplantation, patient reports of distress were found to be accounted for only in part by depression and/or anxiety, suggesting that patients’ experiences of distress “were not adequately captured by simple measures of anxiety and depression (the HADS)” and that the “patient definition of distress is qualitatively different from symptoms of anxiety and depression” (Trask et al., 2002:923). Other studies also have observed variable results from the use of different screening instruments (Hegel et al., 2006).
Thus, there is a need for psychosocial screening instruments that can accurately and efficiently detect a comprehensive range of health-related psychosocial problems—including difficulties with logistical or material needs (e.g., transportation or insurance), inadequate social supports, behavioral risk factors, and emotional problems such as anxiety or depression. Although few in number, instruments that can be used to screen for a broader array of psychosocial needs exist. These instruments vary somewhat in their content and approach, which may reflect their different purposes and conceptual bases (as well as the absence of a shared understanding of health-related psychosocial stress and psychosocial health services, as discussed in Appendix B). Although additional testing of these instruments would be beneficial, the validity, reliability, and feasibility of some are sufficiently established that many oncology practices now routinely screen all of their patients for psychosocial health needs using such instruments as those described below.
The Distress Thermometer uses a visual analogue scale displayed on a picture of a thermometer to screen for any type of psychological distress. Individuals are instructed to circle the number (from zero [no distress] to 10 [extreme distress]) that best describes how much distress they have experienced over the past week (NCCN, 2006). The single-item, paper-and-pencil Distress Thermometer is self-administered in less than a minute. Testing
in individuals with different types of cancer at multiple cancer centers has shown that a rating of 4 or higher correlates with significant distress and that the instrument affords good sensitivity and specificity (Jacobsen et al., 2005). Testing has also revealed concordance with the HADS and BSI (Roth et al., 1998; Trask et al., 2002; Akizuki et al., 2003; Hoffman et al., 2004; Jacobsen et al., 2005). In guidelines issued by NCCN, a 35-item Problem List provided on the same page as the thermometer asks patients to identify separately the types of problems they have (e.g., financial, emotional, work-related, spiritual, family, physical symptoms) (NCCN, 2006). This tool can help identify psychosocial problems that are not linked to psychological distress, as well as those that are. The Problem List does not ask about behaviors such as smoking, alcohol or drug use, exercise, or diet or about cognitive problems that could interfere with illness self-management. The Distress Thermometer is available at no cost from NCCN. No data are available on the extent of its use overall, although three member cancer centers of NCCN report using it (Jacobsen and Ransom, 2007).
The Patient Care Monitor (PCM) 2.0 is an automated, 86-item screening tool that reviews psychological status, problems in role functioning, and overall quality of life, as well as physical symptoms and functioning. Designed to screen for patient problems frequently encountered by practicing oncologists, it is completed by the patient using a computer-based tablet and pen prior to each visit with the clinician. The questionnaire takes an average of 11 minutes to complete. Once completed, it is sent automatically via secure wireless connection to a central server at the practice site; responses are compared with those given previously; and the results are printed out for review by the clinician prior to the visit with the patient. Scores for distress and despair/depression are automatically generated and included in the PCM report. Measures of the instrument’s validity and reliability for use with adults have been favorable in testing among multiple convenience samples of patients in one large oncology practice (Fortner et al., 2003; Schwartzberg et al., 2007). PCM has not undergone tests of its sensitivity and specificity; however, a threshold for follow-up assessment has been established using normalized T scores derived from a normative database created from data submitted by licensed users. At present, a score of 65 is more than 1 standard deviation beyond the mean and represents the top 5 percent for either distress or despair/depression. Patients with scores of 65 or higher are strongly recommended to receive further assessment. PCM is a component of the PACE (Patient Assessment, Care, and Education) product, commercially available from the Supportive Care Network, and has a Spanish version. As of January 2007, it was in use by more than 110 oncology practices in the United States.
The Psychosocial Assessment Tool©(PAT) 2.0 was developed for use with families of children newly diagnosed with cancer to assess the patient’s
level of risk for psychosocial health problems during treatment. Risk factors for which it screens pertain to family structure and resources, social support, children’s knowledge of their disease, school attendance, children’s emotional and behavioral concerns, marital/family problems, family beliefs, and other family stressors (Kazak et al., 2001). PAT differs from the Distress Thermometer and PCM in that it was developed for children and for one-time use, although the developers report interest in its periodic use.7
The first version of PAT was pilot tested with 107 families and found to be feasible for routine use as a self-report instrument completed by families (Kazak et al., 2001). The 2.0 version includes modifications to improve clarity, ease of use, and content and can be completed in approximately 10 minutes. In subsequent testing, total scores on PAT 2.0 were significantly correlated in the predicted direction with parents’ acute distress, anxiety, and conflict and children’s behavioral symptoms, as well as with lower family cohesion. Favorable construct, criterion-related, and convergent validity were found as compared with established tools for measuring children’s behavior, parents’ anxiety and acute stress, and family functioning, as well as with physician- and nurse-completed versions of PAT. Results of tests of internal consistency and test–retest reliability have also been favorable. Cut-off scores for identifying varying levels of need have been determined a priori on the basis of research on the original PAT. As of January 2007, PAT 2.0 was recommended only for research purposes, although its developers believe that upon publication of the most recent research findings, there will be interest in its clinical use and that it is suitable for such use.8
Psychosocial Screen for Cancer (PSSCAN) is a 21-item tool that measures perceived social support (instrumental, emotional, network size), desired social support, anxiety, depression, and quality of life. Developed by the British Columbia Cancer Agency (BCCA) of Canada, it has performed well on psychometric tests and tests of reliability and validity in three samples totaling almost 2,000 patients. PSSCAN is in clinical use in a few Canadian cancer centers, although BCCA is committed to its use by all new patients. It also is being used in Ireland and in some U.S. facilities. BCCA has formulated norms for a healthy population (based on a sample size of 800; manuscript in preparation) and has developed software for the tool’s use on touch-screen computers. This software has been pilot tested with cancer patients and is ready for large-scale use. The questionnaire can be completed in less than 10 minutes by all patients (except those who do not read English or have severe problems with eye or motor control). The
software also autoscores all items on completion and prints a one-page summary of scored data for immediate staff use and incorporation into patient charts. Raw data are automatically deposited into an Excel data file for later processing with standard statistical packages. PSSCAN is available at no cost (Linden et al., 2005).9
Other screening tools also exist and have been subjected to or are in various stages of testing. Some of these are simple checklists to identify psychosocial health needs (Pruyn et al., 2004). Although there are reports on pilot tests of the feasibility of these checklists, they have not undergone further testing for their validity, reliability, or predictive value as screens. However, a review of six studies of the use of checklists to identify psychosocial health needs in cancer care found that use of these screening tools positively influenced health care providers to pay attention to psychosocial health needs, talk with their patients about these needs, and make referrals to providers of psychosocial health services (Kruijver et al., 2006).
Assessment
In the absence of a common definition of needs assessment and descriptions of how it relates to screening,10 in this report psychosocial needs assessment is defined as the identification and examination of the psychological, behavioral, and social problems of patients that interfere with their ability to participate fully in their health care and manage their illness and its consequences. Needs assessment contrasts with screening in that the latter is a brief process for identifying the risk for having psychosocial health needs, while needs assessment is a more in-depth evaluation that confirms the presence of such needs and describes their nature. Needs assessment thus requires more time than screening.
Full understanding of each individual’s psychosocial problems and resulting needs is frequently cited as an essential precursor to ensuring that cancer patients receive the necessary psychosocial health services (NICE,
2004), to providing good-quality health care overall, and to improving health-related quality of life (Wen and Gustafson, 2004). The United Kingdom’s National Institute for Clinical Evidence recommends, for example, that “assessment and discussion of patients’ needs for physical, psychological, social, spiritual, and financial support should be undertaken at key points (such as at diagnosis; at commencement, during, and at the end of treatment; at relapse; and when death is approaching)” (NICE, 2004:7). Needs assessments are theorized to facilitate communication between patients and providers about issues that are not otherwise raised (Wen and Gustafson, 2004).
A systematic review of randomized trials (Gilbody et al., 2002) and one cancer-specific randomized pilot project (Boyes et al., 2006) addressing needs assessment used by itself or with minimal follow-up (such as feedback of results to clinicians) found little support for the effectiveness of the process in improving psychosocial functioning. When combined with follow-up care planning and implementation of those plans, however, needs assessment was found to be effective in improving access to needed services in a systematic review of randomized controlled trials evaluating the effectiveness of interventions in improving access to services after hospital discharge11 (Richards and Coast, 2003). In another systematic review and meta-analysis, systematic assessment of medical, functional, psychosocial, and environmental domains and follow-up implementation of an intervention plan were found to be effective in preventing functional decline in older adults (Stuck et al., 2002). Needs assessment was also identified as one essential ingredient in reduced hospital admissions or medical costs in a qualitative analysis of effective care coordination programs for Medicare (Chen et al., 2000). These findings are consistent with that of the committee that a combination of activities, rather than a single activity by itself (in this case, needs assessment), is needed for the effective delivery of appropriate psychosocial health care.
A systematic search by Wen and Gustafson (2004) for needs assessment instruments for patients with cancer revealed 17 patient and 7 family instruments (generally self-report) for which information was available on their reliability, validity, burden, and psychometric properties (see Table 4-2). These instruments varied greatly in the needs addressed,12 the domains
covered, and the items included in similarly named domains (see Table 4-3). Reviewers also found a lack of evidence for the instruments’ sensitivity to change over time, failure to examine their required reading levels, and failure to address the period after initial treatment for cancer. Despite these deficiencies and the need for further research (see Chapter 8), results of the two systematic reviews that examined the use of needs assessment instruments when processes for follow-up on identified needs were implemented, as well as the reasonableness of needs assessment as a means of identifying individuals who need psychosocial health services, argue for the usefulness of the process as a prelude to the planning and provision of such services. This conclusion also is supported by the models for delivering psychosocial health services contained in Table 4-1.
Planning Care to Address Identified Needs
Once psychosocial health needs have been identified, a plan should be developed that will assist the patient in managing his or her illness and maintaining the highest possible level of functioning and well-being. Nearly all of the models for delivering psychosocial health services reviewed by the committee (Table 4-1) identify care planning as a component of the intervention. This inclusion of planning may originate from (1) the long-standing practice of developing treatment or care plans as a part of routine medical, nursing, and other health care; (2) the logic of developing a plan for action before action is taken; and/or (3) the identification of care planning in some research as an essential to improving health care. Although care planning in itself has not been the subject of much health services research, some research identifies it as one ingredient in effective interventions to improve health care outcomes in adults with chronic illnesses (Chen et al., 2000; Stuck et al., 2002). Written plans developed jointly with the patient and containing clear goals are characteristic of care coordination initiatives that achieve reductions in hospital care and medical costs (Chen et al., 2000). Moreover, research has shown that people vary in their expression of the need for psychosocial support and in the types of support they prefer.
For these reasons, the committee believes that planning for the delivery of psychosocial health services is a logical step in meeting the need for such services. Advance planning is likely to facilitate the identification and implementation of interventions best suited to each patient’s individual situation and to conserve resources not useful to the patient. Such planning for psychosocial health services should address mechanisms needed to effectively (1) link the patient with the needed services, (2) support the patient in managing his or her illness and its consequences, and (3) coordinate psychosocial and biomedical health care.
TABLE 4-2 Comparison of Needs Assessment Instruments (Wen and Gustafson, 2004)
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
Patient General |
||||
|
CARES (Cancer Rehabilitation Evaluation System) |
Find how cancer affects psychosocial, physical and behaviors |
93–132 items; 6 domains: physical, psychological, medical interaction, marital, sexual, miscellaneous |
Five-point scale plus “do you want help (yes/no)?” |
Competency-based model of coping |
|
Patient completes |
||||
|
CARES-SF (Cancer Rehabilitation Evaluation System-Short Form) |
Shortens the CARES for use with clinical trials |
38–57 items; 5 domains: physical, psychological, medical interaction, marital, sexual |
Five-point scale plus “do you want help (yes/no)?” |
|
|
Patient completes |
|
|||
|
CPNS (Cancer Patient Need Survey) |
Measures the importance of needs and the degree to which their needs are met |
51 items; 5 domains: coping, help, information, work, and cancer shock |
“Importance”: seven-point Likert scale; “how well met”: seven-point Likert scale |
|
|
Patient completes |
|
|||
|
CPNQ (Cancer Patient Need Questionnaire) |
Assesses unmet needs of people with cancer |
71 items; 5 domains: psychological needs, health info, ADLs, patient care/support, interpersonal communication |
Five-point scale: “what is your level of need for help?” |
|
|
Patient completes |
|
|||
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Patient General |
|||||
|
Literature; Interviews with patients and family; Expert review |
Correlated with SCL-90, KPS, DAS; Good agreement with interviewers. |
Domains α ranged from .88–.92 |
Subscales: r=.84–.95 87% agreement n=71, time=1 week |
|
Time: 10–45 min; Reading level N/A; Acceptability: most found it easy to use |
|
Selected from the CARES by experts |
Correlated well with CARES, FLIC, KPS, DAS; Large sample sizes |
Domains α ranged from .60–.84 |
Dimensions: r=.69–.92 81%–86% agreement n=120, time=10 days |
Find physical, psychosocial change with time Correlated with FLIC @ 1, 7, 14 mo post-diagnosis |
Time N/A; Reading level N/A; Acceptable N/A |
|
Interviews with nurses, patients, and caregivers using Objective Content Test and Q-sort method |
|
Overall: 0.91 Importance: .83–.93 How well met: .79–.95 Domain: α=.88–.92 |
|
|
Time: 2–45 min; Reading level N/A; Acceptability: reported no problems when used |
|
Literature; Interviews; Expert review; Pilot test |
Discriminant validity: able to distinguish patients with different disease stages |
Domains α ranged from .78–.90 |
Intercorrelation all significant kappa >.4 n=124, time=10–14 days |
|
Time: 20 min; Reading level: 4th or 5th grade; Acceptability: 25% non-completion rate |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
SCNS (Supportive Care Needs Survey) |
Assesses impact of cancer on lives of cancer patients |
61 items; 5 domains: psychological needs, health information, physical/daily living needs, patient care and support, and sexuality |
Five-point scale: “what is your level of need for help?” |
Factor analysis |
|
Patient completes |
||||
|
HCS-PF (Home Care Study-Patient Form) |
Assesses attitudes of terminally and chronically ill patients toward medical care |
33 items; 2 domains Satisfaction with: care availability, care continuity, MD availability, MD competence, MD personality, MD communication, general satisfaction Preference: home care, decision-making |
Agreement with five-point Likert scale |
|
|
Interview; patient may be able to complete |
|
|||
|
NEQ (Need Evaluation Questionnaire) |
Assess needs of hospitalized cancer patients in clinical setting |
23 items; 3 domains: helps diagnosis/prognosis, exam/treatment, communication and relations |
Agreement with yes/no statement |
Factor analysis |
|
Patient completes |
||||
|
PNAT (Patient Needs Assessment Tool) |
Screen cancer patients for physical and psychological functioning problems |
16 items; 3 domains: physical, psychological, and social |
Five-item impairment scale for each area within domain |
|
|
Part of clinician interview |
|
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Based on CPNQ; Expert review; Pilot test |
|
Domain α ranged from .87–.97 |
|
|
Time: 20 min; Reading level: 5th grade; Acceptability: patients found it understandable, 35% non-completion |
|
Based on scales by Zyranski and Ware; Pilot test |
Poor discriminant validity |
Domains α ranged from 0.10–0.75 |
|
|
Time: N/A; Reading level: N/A; Acceptability: N/A |
|
Interviews; Pilot tests |
|
Domains: α ranged from .69–.81 |
Cohen’s kappa ranged from .54–.94 |
|
Time: 5 min; Reading level N/A; Acceptability: 63% of patients OK; 24% incomplete; 3% missing data |
|
|
Time=1week |
|
|||
|
Literature; Clinical experience |
Physical domain correlates with KPS; Psychological with GAIS, BSI MPAS, BDI Social with ISEL |
Domains: α ranged from .85–.94 |
Interrater reliability: Friedman: .87, .76, .73; Spearman rank order: .59–.98 |
|
Time: 20–30 min.; Training level: low; Acceptablity: N/A |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
PNI (Psychosocial Needs Inventory) |
Measure the unmet psychosocial needs of cancer patients and their caregivers |
48 items; 7 domains: related to health professionals, information needs, related to support networks, identify needs, emotional and spiritual, practical and childcare need |
Five-point “Importance” scale Five-point “Satisfaction” scale |
|
|
Patient and caregiver complete |
|
|||
|
PCNA (Prostate Cancer Needs Assessment) |
Measures the importance and unmet needs of men with prostate cancer |
135 items; 3 domains: information, support, and care delivery |
Ten-point “Importance” scale Ten-point “Extent Need Met” scale |
|
|
Patient completes |
|
|||
|
PINQ (Patient Information Need Questionnaire) |
Measures the information need among cancer patients for the improvement of clinical practice and research |
17 items; 2 domains: disease-oriented and information about access to help and solution |
Four-point scale |
Factor analysis; Similar structure was found across Hodgkins; breast cancer patients and over time |
|
Patient completes |
||||
|
DINA (The Derdiarian Informational Needs Assessment) |
Measures the informational needs of cancer patients |
144 items; 4 domains: disease, personal, family, and social relationship |
Check the need present and rate importance on 10-point scale |
Theory of information seeking; Needs and hierarchy of needs |
|
Interview |
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Literature; Interviews; Focus group |
Discriminant validity: detected the differences among needs at four critical movements of cancer trajectory |
α >.7 for each of the first six domains |
|
|
Time: N/A; Read level: N/A; Acceptability: 59% non-response rate and the characteristic of the non-respondents was examined |
|
Literature; Interviews using Critical Incident Technique and Nominal Group; Expert review |
Correlated with overall satisfaction-with-care |
Agreement on classification by three researchers working independently |
R=.97 Time=2 weeks |
|
Time: 43 min; Reading level: 7th grade; Acceptability: 11% non-completion |
|
Literature; Interviews |
Correlated with RSC, State-Anxiety Inventory and MMPI D-scale |
Domains: α ranged from .88–.92; Inter-item correlation >0.2 |
|
Detected the changing needs of patients at three time points before and after first treatment |
Time: N/A; Reading level: N/A; Acceptability: reasons to refuse: not wanting to be reminded of their illness, feeling too old, etc. |
|
Expert review |
|
Domain: α exceeded 0.9 for all domains |
80%–100% agreement found using McNemar test time=15–20 min. |
Detected difference between control group and experimental group |
Time: N/A; reading level N/A; Acceptability: N/A |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
INM (Information Needs Measure) |
Assess the priority of informational needs of cancer patients |
9 information categories |
Control preference scale; ranking of informational resources; prioritization of information needs |
Based on the theoretical framework of Derdiarian |
|
Patient completes |
||||
|
TINQ-BC (Toronto Informational Needs Questionnaire-Breast Cancer) |
Identify information needed by women with recent breast cancer diagnosis to deal with illness |
51 items; 5 domains: diagnosis, tests, treatments, physical, psychosocial |
Five-point “Importance” scale |
|
|
Patient completes |
|
|||
|
Stage Specific |
||||
|
PACA (Palliative Care Assessment) |
Assess effectiveness of hospital’s palliative care program |
12 items; 3 domains: symptom control, insight, and future placement |
Four-point scale, except five-point scale for insight |
|
|
Professional completes |
|
|||
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Literature; Based on works by Derdiarian; Expert review |
|
Kendall zeta: .95–.99 Kendall coefficient of agreement: .20–.35 |
|
|
Time: N/A; Reading level: N/A; Acceptability: N/A |
|
Literature; Nurse opinions |
Correlated with the information scale of HOS |
Overall α=.97; Domains α ranged from .73–.93; Correlation of subscales to total scale: .38–.88 |
|
|
Time: 20 min; Reading level: N/A; Acceptability: OK |
|
Stage Specific |
|||||
|
Interviews of patients |
Symptom scores correlated with McCorkle symptom distress scale |
|
Kappa ranged from .44–1 |
Sensitivity to detected statistically significant intervention effects |
Time: few min.; Training level: N/A; Acceptability: N/A |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
STAS (Support Team Assessment Schedule) |
Assess quality of palliative care of multidisciplinary cancer support teams |
17 items; 8 domains: pain/symptom control, insight, psychosocial, family needs, home services, planning affairs, support of other professionals, communication |
Five-point Likert scale |
|
|
Professional completes |
|
|||
|
NEST (The Needs Near the End-of-Life Care Screening Tool) |
Measure experiences of end-of-life patients and possibly assess impact of interventions |
135 items; 8 domains: patient-MD relations, social connection, caregiving need, psychological distress, spirituality, personal acceptance, have purpose, clinician communication |
Five-point Likert scale |
Frame for a good death; Factor analysis; Measurement invariance across sociodemographic strata; Item response theory on the short version |
|
Interview; patient completes if possible |
||||
|
Caregiver |
||||
|
FAMCARE |
Measure family satisfaction with advanced cancer care |
20 items; 4 domains: information giving, care availability, physical care, pain control, and 2 other items |
Five-point Likert “Satisfaction scale” |
|
|
Family completes |
|
|||
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Literature; Clinical experience |
Correlated with patient and family score, Karnofsky score, Spitzer QOL index. Support team scores correlate with patient and family scores |
|
Interrater reliability: 90% agreement except predictability |
Detected improvement in palliative care |
Time: 2 min. for existing patients, 5 min. new patients; Training level: N/A; Acceptability: N/A |
|
|
Evaluated 2 palliative care support teams |
||||
|
Literature; Interviews and focus groups; Symptom items from other scales; Pilot tests; Expert review |
|
Domains: α ranged from 0.63–0.85 at baseline and 0.64–0.89 at follow up |
|
|
Time: N/A; Reading level N/A; Acceptability: 69.2% patients found interview helpful |
|
Caregiver |
|||||
|
Interviews; Family ranking of items; Q-sort |
Correlated with McCusker and with overall satisfaction with care questions |
Overall α: 0.93; Domains: α ranged from .61–.88 |
R=.92 n=23, time <23 hrs |
|
Time: 22 min; Reading level: N/A; Acceptability: N/A |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
FIN (Family Inventory of Needs) |
Measure needs of cancer patient’s family and extent needs are met |
20 items, 1 domain |
Ten-point “importance” scale and met/unmet check |
Fulfillment theory; factor analysis |
|
Family completes |
||||
|
FIN-H (Family Inventory of Needs-Husbands) |
Measure information needs of husbands of women with breast cancer |
30 items; 5 domains: surgical care needs, communication with MD, family relations, diagnosis/treatment specifics, husband’s involvement |
Five-point “Importance” subscale and three-point “Need Met” subscale |
Factor analysis |
|
Husband completes |
||||
|
HCNS (Home Caregiver Need Survey) |
Measures the importance and satisfaction of the needs of caregivers |
90 items; 6 domains: information, household, patient care, personal, spiritual, and psychological |
Seven-point “Importance” subscale and seven-point “Satisfaction” subscale |
Lackey-Wingate model |
|
Caregiver completes |
||||
|
HCS-CF (Home Care Study-Caretaker Form) |
Assess attitude of terminally and chronically ill caretakers toward medical care of their patients |
42 items; 2 domains: Satisfaction with care: availability, continuity, MD availability, MD competence, MD personality, MD communication, general satisfaction Preference for: home care, decision making |
Agreement with five-point Likert scale |
|
|
Interview; patient may be able to complete |
|
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Literature; Items from original Critical Care Family Needs Inventory; Family review |
Correlated with FAMCARE |
Overall α for “importance” scale: 0.83 |
|
|
Time: “short”; Reading level: N/A; Acceptability: N/A |
|
Based on FIN Pilot test |
|
Overall α ranged from .90–.93; 73%–87% of items: item-total correlation 0.4–0.7 |
Importance subscale: r=0.82, Need Met subscale: r=.79 time: <24 hrs |
|
Time: 16–30 min; Reading level: N/A; Acceptability: 12 husbands refused to complete |
|
Statements from patients and home caregivers; Expert evaluation; Pilot test |
Psychological, patient care, personal and household Domains correlated with KPSS |
Overall α: 0.93, 0.98; Domains: α ranged from .85–.97 |
|
Detected changing caregiver needs at 3 time points |
Time: 30 min; Reading: 5th grade level; Acceptability: caregivers OK |
|
Based on scales by Zyranski and Ware; Pilot test |
Good discriminant validity |
Domains: α ranged from .50–.85 |
|
|
Time: N/A; Reading level: N/A; Acceptability: N/A |
|
Instrument |
Purpose and Administration |
Items and Domains |
Question Format |
Conceptual and Measurement Model |
|
NSS (Need Satisfaction Scale) |
Assess the intensity and satisfaction of the needs of bereaved families |
9 items |
Five-point “Felt need” subscale and five-point “Met need” subscale |
|
|
Family completes |
|
|||
|
Relative |
||||
|
ISNQ (Information and Support Needs Questionnaire) |
Assess information and support needs of women who have primary relative with breast cancer |
29 items; 2 domains: information and support |
Four-point “Importance” subscale and Four-point “Need Met” subscale |
|
|
Self-complete |
|
|||
|
NOTE: This table is from “Needs Assessment for Cancer Patients and Their Families.” Kuang-Yi Wen and David H. Gustafson, Health and Quality of Life Outcomes, 2004, © 2004 Wen and Gustafson; licensee BioMed Central Ltd. The electronic version of it is an Open Access article: verbatim copying and redistribution of the article are permitted in all media for any purpose, provided this notice is preserved along with the article’s original URL: http://www.hqlo.com/content//pdf/1477-7525-2-11.pdf. |
||||
|
Validity |
Reliability |
Responsiveness |
Burden |
||
|
Content Validity |
Construct Validity |
Internal Consistency |
Reproducibility |
||
|
Literature; Expert review |
Unmet needs correlated with overall satisfaction with care |
Overall α: 0.84; “Felt need” subscale: 0.74; “Met need” subscale: 0.84 |
|
|
Time: 15 min; Reading level: N/A; Acceptability: N/A |
|
Relative |
|||||
|
Literature; Interviews |
|
Domains: α ranged from .92–.95 |
|
|
Time: 37 min; Reading level: “middle” class; Acceptability: “several” reported it didn’t apply |
TABLE 4-3 Comparison of Domain Item Distribution Across Needs Assessment Instruments (Wen and Gustafson, 2004)
|
PINQ |
DINA |
INM |
TINQ-BC |
PACA |
STAS |
NEST |
FAM CARE |
FIN |
FIN-H |
HCNS |
HCS-CF |
NSS |
ISNQ |
|
17 |
144 |
9 |
51 |
10 |
17 |
|
20 |
20 |
30 |
89 |
42 |
20 |
29 |
|
|
|
|
|
1 |
1 |
|
3 |
|
|
|
5 |
|
|
|
|
|
|
|
7 |
1 |
|
|
|
|
|
|
|
|
|
|
|
|
11 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5 |
|
|
• |
|
|
|
30 |
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
• |
|
|
|
6 |
|
|
|
|
|
|
|
|
1 |
1 |
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
• |
1 |
|
|
|
• |
|
|
|
11 |
|
20 |
|
|
|
|
|
|
|
|
• |
|
|
6 |
|
|
|
|
|
|
• |
2 |
3 |
|
2 |
|
|
|
|
|
|
|
|
|
|
• |
|
|
|
|
• |
|
|
6 |
|
|
|
|
|
|
|
|
|
|
3 |
• |
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
6 |
|
|
14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
18 |
|
9 |
• |
1 |
9 |
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
12 |
|
|
|
|
|
|
|
|
1 |
|
|
|
|
5 |
|
7 |
|
|
|
|
|
|
|
|
|
• |
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
8 |
|
|
|
|
|
|
|
|
|
• |
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
6 |
|
|
16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
9 |
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
20 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
11 |
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
1 |
|
|
|
|
|
|
|
|
|
Open Access article: verbatim copying and redistribution of the article are permitted in all media for any purpose, provided this notice is preserved along with the article’s original URL: http://www.hqlo.com/content//pdf/1477-7525-2-11.pdf. |
|||||||||||||
Linking Patients to Psychosocial Health Services
Several mechanisms used to link patients with psychosocial health services delivered by health and human service providers have empirical support, although the strength of this support varies. These mechanisms include structured referral arrangements and formal agreements with external providers, case management, and collocation and clinical integration of services. Use of care/system navigators is also being studied for its effectiveness in linking patients with needed services.
Structured Referral
Although referral to other organizational or individual providers is a common mechanism for linking individuals with psychosocial health services (see the models in Table 4-1, examples in Chapter 5, and services delivered by referred organizations in Tables 3-2 and 3-3 in Chapter 3), there has been little study of the general effectiveness of such referrals. Most studies of referral have addressed referrals between physicians. These and one Australian study of referrals of cancer patients to psychosocial services indicate high rates of failure to connect individuals to the referred providers, frequent failure of the referred individuals to accept the referred services, and failure to track the outcomes of referrals (Bickell and Young, 2001; Curry et al., 2002; Grimshaw et al., 2006). These findings are consistent with the low ranking accorded referral by others studying practices aimed at achieving care coordination (Friedmann et al., 2000) and the finding of low success of referral by itself in linking cancer patients to needed psychosocial health services in one study of health maintenance organizations (HMOs) (Eakin and Strycker, 2001). And oncology nurses participating in focus groups pertaining to the implementation of survivorship care plans stated that they do not typically have formalized mechanisms for making referrals to social work services (IOM, 2007). On the other hand, the high utilization of services provided by such organizations as the American Cancer Society (which do not themselves provide medical services and thus depend in part on referrals for their clients) indicates that referrals can successfully link patients to needed services.
The few studies of how to make referrals more effective in linking patients with needed services have addressed referrals from primary to specialty care. The results of these studies indicate that using structured referral forms and educating referrers are most likely to improve the referral process (Grimshaw et al., 2006). Having formal agreements in place with those to whom referrals are made can also help (Friedmann et al., 2000). Tracking or following up on the actual receipt of referred services in cancer care is also recommended (Bickell and Young, 2001; Curry et al., 2002).
Referring patients to external providers is likely to continue to be a
primary mechanism for linking patients with needed psychosocial health services because it requires fewer organizational and physical plant resources than offering all psychosocial services on site. To conserve both psychosocial health services and the personnel and resources needed to make referrals, however, it is important for providers to implement approaches for doing so efficiently and effectively. This is an area that would benefit from further study.
Case Management13
Case management consists of a variety of activities necessary to coordinate some or all of the health-related care needed by patients (Zwarenstein et al., 2004). Although these activities often vary with the severity of the illness, the needs of the individual, and the specific model of case management employed (Gilbody et al., 2003; Marshall et al., 2004), case management services that address psychosocial health needs typically include assessment of the patient’s need for supportive services; individual care planning, referral, and connection of the patient with other necessary services and supports; ongoing monitoring of the patient’s care plan; advocacy and education; and monitoring of the patient’s symptoms. These activities can be performed by an appointed individual or a group.
A review by the Cochrane Collaboration of the effectiveness of case management across various diseases and health conditions is under way; as of this writing, results are not yet available.14 However, a qualitative review conducted for the Medicare program of coordinated care programs most effective in reducing hospital admission, total medical costs, or both across a variety of diagnoses identified case management as one of two effective interventions (Chen et al., 2000). Disease-specific systematic reviews and randomized controlled studies of case management in chronic conditions other than cancer, such as HIV/AIDS (Handford et al., 2006), mental illnesses (Ziguras et al., 2000, 2002), and diabetes (Norris et al., 2002), generally have shown that a variety of forms of case management have positive impacts on health outcomes. A meta-analysis of 37 randomized controlled trials of collaborative care for the treatment of depression in primary care found that case management is a key determinant of effective treatment of depression (Gilbody et al., 2006b). However, there have
been few experimental studies of case management in cancer care, and their results vary widely.
McCorkle and colleagues (2000) studied the effect of case management by advanced practice nurses on older postsurgical patients with solid tumors. The intervention consisted of home visits and telephone calls over a 4-week period that involved assessment, information sharing, and skills training for patients and family caregivers. The nurse-managed patients experienced better 2-year survival rates, confined to the group with laterstage disease (67 vs. 40 percent 2-year survival). Another randomized trial examined the effect of nurse case management on women with breast cancer. The results suggest that case management by an oncology nurse for the 12 months following diagnosis increased the likelihood that patients participated in decision making and received evidence-based treatment (Goodwin et al., 2003). Results of other randomized trials in England and Australia, however, suggest that much remains to be learned about the effectiveness of the various activities of nurse case managers in cancer care (McLachlan et al., 2001). One study of the effects of a nurse coordinator intervention with terminally ill cancer patients found no significant differences in symptoms, psychiatric morbidity, or care satisfaction between nurse-managed and control patients and families (Addington-Hall et al., 1992). In an analysis of the health care utilization and cost impacts of the nurse coordinator intervention, however, Raftery and colleagues (1996) found significant reductions in use of hospital and home care with care management. The Australian investigators studied 450 Cancer Institute outpatients with multiple cancers and stages of disease. All patients completed a baseline computerized assessment that included informational, psychosocial, and physical needs; functioning, symptoms, and quality of life; and depressive symptoms. For patients in the intervention group, a nurse coordinator reviewed the assessment results and formulated an individualized care plan in accordance with preset psychosocial guidelines. In addition, a summary of the assessment was made available to the physician seeing the patient that day. The nurses linked patients with needed services, monitored patients and families for changing needs, and attempted to coordinate the activities of the clinical team in support of the management plan. Although counseling was frequently recommended, fewer than 30 percent of patients accepted this recommendation. No significant improvements in satisfaction of needs, psychosocial functioning, or quality of life were found.
In summary, case management has demonstrated effectiveness in the care of high-risk patients with major chronic illnesses, but its role in cancer care remains uncertain. Despite this uncertainty, a number of health plans have implemented case management activities for patients with cancer (AHIP, 2007). Case management directed at increasing adherence to evidence-based treatment (Goodwin et al., 2003) and increasing the
self-management skills of patients and family caregivers (McCorkle et al., 2000) may well be effective.
On-site Collocation and Clinical Integration of Services
Multiple studies of mental health care have found that same-site delivery of mental health and primary care is effective in linking patients to the collocated services (Druss et al., 2001; Samet et al., 2001) and can improve treatment outcomes (Unutzer et al., 2001; Weisner et al., 2001). In a 1995 study of a nationally representative sample of outpatient drug use treatment units, same-site delivery of services was more effective than formal arrangements with external providers, referral agreements, or case management in ensuring that patients would utilize necessary services (a first step in collaborative care) (Friedmann et al., 2000).
Integrating psychosocial health care into medical care settings facilitates patient follow-through on referrals, allows for face-to-face verbal communication in addition to or as an alternative to communicating in writing, and allows for informal sharing of the views of different disciplines and easy exchange of expertise (Pincus, 2003). Studies of care collaboration also have shown that physical proximity of would-be collaborators facilitates collaboration (IOM, 2004).
The opportunities for face-to-face communication provided by collocated services are important because multiple studies have identified effective communication between providers as a key feature of care collaboration (Baggs and Schmitt, 1988; Shortell et al., 1994; Schmitt, 2001). “Effective” communication is described as frequent and timely (Shortell et al., 1994; Gittell et al., 2000),15 and is characterized by discussion with contributions by all parties, active listening, openness, a willingness to consider other ideas and ask for opinions, questioning (Baggs and Schmitt, 1997; Shortell et al., 1994), and the free flow of information among participants. This type of communication is less easily achieved through electronic, mail, and telephone communications. Nonetheless, when physical collocation and integration of services is not feasible, other strategies for linking patients with needed services (e.g., through formal referral arrangements or use of case managers) can be used.
Care/System Navigators
Use of care/system navigators, as well as individual patient advocates, is similar to case management and may also help link patients to needed psychosocial services. Such programs in cancer care were developed initially
to help low-income patients participate in screening for the detection of cancer and aid those with suspicious screening findings in gaining access to diagnostic and treatment services. Initially, patient navigators tended to be local community residents without professional credentials, but more recently some have proposed that nurses, social workers, and other health workers play a navigator role. This variation in the background of the navigator relates to differences in role expectations. While all navigator programs focus on helping patients overcome barriers to receiving effective services, some also include patient education and patient advocacy roles (Dohan and Schrag, 2005).
Evidence to date for the effectiveness of patient navigator programs is confined largely to their effectiveness in getting patients screened for the detection of cancer. One of the few randomized trials of this type of patient navigation (Jandorf et al., 2005) found that patient navigators increased the prevalence of screening for colorectal cancer. Results of other quasi- and nonexperimental evaluations suggest that such programs increase screening rates and may modestly increase the proportion of patients detected with early-stage disease (Dohan and Schrag, 2005). Some qualitative evidence suggests that navigators help patients overcome barriers, both logistical (e.g., transportation) and attitudinal, although their role in helping patients once diagnosed has received little study. However, a recent randomized trial evaluating the impact of a patient navigation program on follow-through with diagnosis among women with abnormal mammograms found that the intervention significantly increased the percentage of women achieving diagnostic resolution (Ell et al., 2007).
In summary, patient navigator programs appear to help low-income patients participate in cancer screening and perhaps diagnosis. Whether such programs can also be effective in linking a diverse patient population to appropriate psychosocial services and how they differ from case management functions described above remains uncertain, however. The American Cancer Society (ACS) and NCI have both launched major initiatives to implement and evaluate patient navigator programs. The ACS program involves placing trained ACS staff in strategically selected health care facilities with oncology treatment services to provide adult cancer patients and families with personalized and reliable information about the disease, referral to ACS resources, and timely follow-up. NCI has launched a Patient Navigation Research Program to address unequal access to standard oncology care by developing interventions designed to reduce the time to delivery of standard cancer services, cancer diagnosis, and treatment after an abnormal finding. Patient navigators in this program will assist patients and their families throughout the period of care by, for example, arranging various forms of financial support, scheduling transportation to appointments, and organizing child care during appointments. ACS is working
with NCI on an evaluation of these patient navigator programs.16 NCI’s Community Cancer Centers Pilot Program includes patient navigators as one facet of these new centers (NCI, undated).
Supporting Patients in Managing Their Illness
Illness self-management is defined as an individual’s “ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition” (Barlow et al., 2002:178). Effective approaches for providing this support are reviewed in Chapter 3. Given the diverse physical, psychological, and social challenges posed by cancer, its treatment, and its sequelae, providing patients and their caregivers with knowledge, skills, abilities, and support in managing the psychosocial and biomedical dimensions of their illness and health is critical to effective health care and health outcomes for these patients.
Coordinating Psychosocial and Biomedical Health Care
A 2007 systematic review of systematic reviews of the effectiveness of care coordination, conducted by the Agency for Healthcare Research and Quality (AHRQ) (McDonald et al., 2007), found more than 40 definitions of care coordination and related terminology and 20 different coordination interventions.17 The report provides the following working definition of care coordination:
Care coordination is the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services. Organizing care involves the marshalling of personnel and other resources needed to carry out all required patient care activities, and is often managed by the exchange of information among participants responsible for different aspects of care. (McDonald et al., 2007:v)
The AHRQ review found that the most common care coordination mechanisms addressed in the literature are multidisciplinary team care, case management, and disease management (the last of which is defined variably or not at all). The review found the strongest evidence for the effectiveness
of coordination using a variety of strategies for individuals with congestive heart failure, diabetes, severe mental illness, a recent stroke, or depression, although the reviewers noted that it was not possible to identify the key component(s) of the care coordination interventions that were responsible for their effectiveness. Significantly, the review found that when systematic reviews addressed “other clinical areas such as rheumatoid arthritis, pain management, asthma, and cancer [emphasis added], there is insufficient evidence to draw firm conclusions” (McDonald et al., 2007:7). Nonetheless, until research provides better direction with respect to coordination within the context of cancer care, clinicians caring for these patients and their families will need to implement mechanisms for coordinating care based on the findings of care coordination studies for other diseases and for populations with varied conditions and on the limited studies addressing care coordination in cancer.
Cancer care typically requires multiple professional caregivers to provide accurate diagnosis and staging, surgical treatment, adjuvant or definitive chemotherapy and/or radiotherapy, and ongoing management of comorbid problems, as well as psychosocial support. The multiple handoffs involved in typical cancer care generate opportunities for confusion, redundancy, breakdowns in communication, and medical errors. Patients and families, with variable help from their clinicians, must often take the initiative to ensure that relevant information is shared across providers and that care is coordinated. The psychosocial problems described earlier, as well as the complexities of oncology care, can make it difficult if not impossible for patients and caregivers to carry out this role. This difficulty is exacerbated by the fact that care coordination as a psychosocial intervention must fulfill a dual function: coordination of psychosocial health services with biomedical services, and coordination of biomedical care provided by multiple clinicians.
Consistent with the findings of the AHRQ evidence review, both types of care coordination are likely to be achievable in various ways, including the activities described in the preceding section that are effective in linking patients to needed psychosocial health services, such as case management and collocated, clinically integrated services. A study of the efforts of hospitals and cancer centers to coordinate the care of patients with breast cancer also found the use of regularly scheduled multidisciplinary meetings and patient support personnel, such as patient educators and care navigators (Bickell and Young, 2001). In a randomized controlled trial of the integration of medical care with mental health services, same-site location, common charting, enhanced channels of communication (including joint meetings and e-mail), and in-person contact were found to facilitate the development of common goals and the sharing of information between medical and mental health providers (Druss et al., 2001). Other coordination
mechanisms likely to impact psychosocial care and outcomes include the use of guidelines and protocols that incorporate attention to psychosocial issues; patient support, such as educational, navigation, or case management interventions, to assist patients in having their needs met; and use of information systems to help ensure that providers and patients have the information they need when they need it to facilitate care (Bickell and Young, 2001).
Consistent with these findings, Ouwens and colleagues’ (2005) analysis of systematic reviews of programs for the chronically ill identified program components associated with positive effects on patient-reported outcomes, such as patients’ functional health status, satisfaction with care, and hospitalization. These components included, among others, structured clinical follow-up, often supported by case management; multidisciplinary team care facilitated by regular communication and multidisciplinary care plans in accordance with evidence-based protocols or guidelines; and feedback, reminders, and education for health professionals.
The use of multidisciplinary teams has been found to be effective in reducing mortality and hospitalizations for individuals with heart failure (McAlister et al., 2004). Such teams have been promoted by the British National Health Service and are widely implemented in the United Kingdom. In a comprehensive assessment of the literature and the U.K. experience with multidisciplinary teams in cancer care, however, Fleissig and colleagues (2006:935) conclude that “research showing the effectiveness of MDT [multidisciplinary teams] working is scarce.” Houssami and Sainsbury’s (2006) review of the literature on multidisciplinary approaches for patients with breast cancer found 15 studies, none of which was experimental. While there was some suggestion of better survival, this was attributed to characteristics of the hospital and surgeons (especially patient volume) rather than to the functioning of teams. Psychosocial outcomes were not included in this review.
In addition to the low-tech approach of having on-site nursing staff or other personnel provide care coordination, the high-tech approach of using shared patient records can be used to coordinate patient care. Electronic health records (EHRs) are an important mechanism for sharing patient information among collaborating providers and have been highlighted as one of the essential components of the developing National Health Information Infrastructure (NHII). Although sharing of patient information maintained in paper-based records can take place, the electronic capture and storage of patient information is a more thorough and efficient mechanism for timely access to needed information by the many providers serving a patient. EHRs allow (1) the longitudinal collection of electronic information pertaining to an individual’s health and health care, (2) immediate electronic access—by authorized users only—to person- and population-level
information, (3) provision of knowledge and decision support to enhance the quality of patient care, and (4) support for efficient health care delivery (IOM, 2003). Given these advantages, NCI is requiring organizations participating in its Community Cancer Centers Program to be able to build information technology capability, including electronic patient records (Niederhuber, 2006). Indeed, although still a minority, hospitals and ambulatory practices are increasingly investing in EHRs; however, these investments typically are being made by larger facilities, creating what is referred to as the “adoption gap” between large and small organizations (Brailer and Terasawa, 2003).
Whereas EHRs function to serve the information needs of health care professionals, personal health records (PHRs) generally focus on the collection of information to help individual patients better manage their health care. Early forms of PHRs differed in size, format, and content and were paper-based, relying on manual collection of information from patients and clinicians. Patients’ or caregivers’ actual use of these PHRs varied depending on their intended use and perceived value. Although patient-reported levels of satisfaction with PHRs were consistently high (83–93 percent) in several studies involving patients with cancer and diabetes and women with children (Drury et al., 1996; Davis and Bridgford, 2001; Lecouturier et al., 2002; Hampshire et al., 2004), rates of actual use ranged from 37 to 97 percent (Drury et al., 1996, 2000; Davis and Bridgford, 2001; Williams et al., 2001; Lecouturier et al., 2002; Hampshire et al., 2004; Walton et al., 2006). Providers’ level of satisfaction with using information from PHRs also varied (Drury et al., 2000; Davis and Bridgford, 2001; Williams et al., 2001; Lecouturier et al., 2002, Hampshire et al., 2004), and the few studies examining improvements in clinical status as a result of the use of PHRs found no significant differences (Drury et al., 2000; Williams et al., 2001).
Electronic versions of PHRs are becoming increasingly available as a feature offered by national health plans. These PHRs generally contain medical and pharmacy claims information and medical information libraries, and have areas for patients to record laboratory results and various health status findings (e.g., blood pressure, weight, height for children) and to collect health risk appraisal information. The committee could find no studies of the effectiveness of electronic PHRs. Research is needed to learn more about their potential value in linking cancer patients to psychosocial health services; informing their medical care; and perhaps most important, supporting them in managing their illness.
Consistent with the wide variation in the care coordination mechanisms reviewed above, the AHRQ review of care coordination concluded that the effectiveness of care coordination mechanisms will most likely depend upon appropriately matching the type(s) of care coordination mechanism(s) used with the needs of patients, although “more conceptual, empirical, and
experimental research is required to explore this hypothesis” (McDonald et al., 2007:vi). In the interim, clinical practices should adopt approaches to care coordination that best address the needs of their patient population and fit their organizational and work design characteristics.
Following Up on Care Delivery
Patient follow-up is present in all of the models listed in Table 4-1 and has been cited in several reviews identifying effective interventions for improving health care processes and outcomes (Chen et al., 2000; Stuck et al., 2002). Follow-up can take place in a variety of ways, including telephone calls to patients to monitor their status (Brown et al., 2004b; Gilbody et al., 2006b; Kornblith et al., 2006), home visits by care managers or other personnel, as part of a scheduled outpatient visit, or through Internet or web-based technology.
Follow-up involves two discrete activities. First is the determination of which services, if any, the patient used, any problems encountered, and satisfaction with services provided. Second is rescreening and assessment to identify new or unmet needs that are then addressed.
A RECOMMENDED STANDARD FOR CARE
From the evidence presented above, the committee concludes that enough is now known to support the adoption of a standard of care for the delivery of psychosocial health services in cancer care. The committee recommends the following:
Recommendation: The standard of care. All parties establishing or using standards for the quality of cancer care should adopt the following as a standard:
All cancer care should ensure the provision of appropriate psychosocial health services by
-
facilitating effective communication between patients and care providers;18
-
identifying each patient’s psychosocial health needs;
-
designing and implementing a plan that
-
links the patient with needed psychosocial services,
-
coordinates biomedical and psychosocial care,
-
-
-
engages and supports patients in managing their illness and health; and
-
-
systematically following up on, reevaluating, and adjusting plans.
Multiple organizations could significantly influence adherence to this standard of care. NCI, as the nation’s leader in cancer care, could include requirements for addressing psychosocial health needs in all of its protocols; standards for designating clinical or comprehensive cancer centers; and other programs, such as its Quality of Cancer Care Initiative. NCI also could work with other organizations in the public and private sectors to incorporate psychosocial health care into existing cancer care initiatives, such as the Centers for Disease Control and Prevention’s National Comprehensive Cancer Control Program and the Veterans Health Administration’s National Cancer Strategy. Private-sector leaders in cancer care could do the same. For example, standards-setting organizations such as NCCN and the American College of Surgeons’ Commission on Cancer could incorporate the committee’s recommended standard and its components into their own standards. Funders of leading initiatives to improve the quality of cancer care also could incorporate this standard into their programs.
Because individual clinical practices vary by their setting and patient population as well as by available resources in their practice and local community, how individual health care practices implement the standard of care and the level at which it is done will likely vary. Nevertheless, it is possible for all providers to meet this standard in some way. Examples of how some cancer care providers are doing so today and suggestions as to how others could do so, even with limited resources, are described in the next chapter. What organizations implementing this standard today have in common is attention to how care is delivered at their practice settings and a willingness to redesign care processes when needed—characteristics that require strong leadership, well known as a critical factor in the success of any major change initiative or quality improvement effort (Burns, 1978; Bodenheimer et al., 2004; National Institute of Standards and Technology, 2007).
ANNEX 4-1
EMPIRICALLY VALIDATED MODELS OF AND CLINICAL PRACTICE GUIDELINES FOR THE EFFECTIVE DELIVERY OF PSYCHOSOCIAL HEALTH SERVICES
Building Health Systems for People with Chronic Illnesses
Building Health Systems for People with Chronic Illnesses was a national initiative, funded by The Robert Wood Johnson Foundation from 1993 to 2002, aimed at improving the delivery of biomedical, mental health, and social support services for people with disabilities and chronic conditions requiring long-term care.19 A qualitative analysis of the five programs most successful in integrating the delivery of all three types of care identified the following as key elements in achieving such outcomes as improved health, reduced use of the emergency room and hospital inpatient and residential mental health care, and reduced or contained costs: (1) screening, needs assessment, and care planning; (2) consumer participation, decision support, and self-determination in care planning; and (3) mechanisms for linking biomedical and psychosocial health services, such as use of interdisciplinary teams and case management (Palmer and Somers, 2005).
Chronic Care Model
The Chronic Care Model is intended to improve the health outcomes of people with chronic illness by creating informed, activated patients who can interact effectively with prepared, proactive health care teams (Bodenheimer et al., 2002). To this end, the model prescribes six key actions for health care organizations serving individuals with chronic illness: (1) supporting patients in learning about and managing their illnesses (illness self-management); (2) helping patients use community resources to manage their health; (3) redesigning patient care by, for example, redefining roles of care team members, offering case management services for complex cases, and providing regular follow-up of all patients; (4) using clinical information systems to support individual patient care planning and coordination of care and to otherwise facilitate efficient and effective care;
(5) using decision support (for patients as well as clinicians) to promote evidence-based care; and (6) creating overarching organizational mechanisms to promote safe, high-quality care (ICIC, 2007). These elements were developed from the findings of a review of the published literature on promising strategies for management of chronic illness. They were refined as a result of input from a large panel of national experts, and subsequently tested nationally across various health care settings through The Robert Wood Johnson Foundation’s Improving Chronic Illness Care program.
Components of the Chronic Care Model have been associated with improved health outcomes in a number of studies (Bodenheimer et al., 2002). In conjunction with the Robert Wood Johnson program, the American Association of Medical Colleges launched an Academic Chronic Care Collaborative (ACCC) to improve care of persons with chronic conditions who receive their care in academic health systems and to ensure that clinical education occurs in an exemplary environment. Teams from 22 academic settings extensively redesigned their care strategies using the Chronic Care Model for persons with diabetes, asthma, and chronic obstructive pulmonary disease and achieved improvements in patient care and outcomes (AAMC, 2006). A RAND Corporation evaluation of the implementation of the Chronic Care Model in four quality improvement collaboratives sponsored by the Institute for Healthcare Improvement also found that implementation of the model for patients with diabetes, congestive heart failure, and asthma improved health care, as well as some dimensions of patients’ illness self-management and health.20 RAND’s before-and-after study included 2,032 intervention patients and 1,837 control patients at 30 participating organizations. Improvements were seen in measures of technical quality of care, such as blood glucose control and use of appropriate heart disease medications. Improved patient outcomes included reductions in emergency room visits and hospital admissions for those with congestive heart failure, improvements in health-related quality of life for patients with asthma, and reductions in risk factors for heart disease (blood pressure, cholesterol, blood glucose levels) for individuals with diabetes.21
Clinical Practice Guidelines for Distress Management
The National Comprehensive Cancer Network (NCCN), an alliance of 21 leading cancer centers in the United States, offers a number of resources for improving health care provided to individuals with cancer (NCCN, 2007b). These resources include clinical practice guidelines, one set of
which addresses the management of distress (NCCN, 2007a). NCCN’s consensus-based distress guidelines call for (1) screening of all patients at their initial visit, at appropriate intervals, and as clinically indicated to determine the level and nature of distress; (2) further evaluation, triage, and referral of patients with significant distress to appropriate resources for care; and (3) education of patients and their families about distress and its management (NCCN, 2006).
Clinical Practice Guidelines for the Psychosocial Care of Adults with Cancer
Australia’s Clinical Practice Guidelines for the Psychosocial Care of Adults with Cancer were developed from a systematic review of research evidence. Although most of the guidelines address how to care for individual symptoms, such as anxiety, or practical problems, such as financial or work-related concerns, the guidelines also recommend certain cross-cutting activities to be carried out in treatment settings. These activities include providing patients with information to support their decision making, screening all patients for clinically significant anxiety and depression, ensuring continuity of care through the designation of a person responsible for care coordination, and developing referral pathways and networks (National Breast Cancer Centre and National Cancer Control Initiative, 2003).
Improving Supportive and Palliative Care for Adults with Cancer
The National Institute for Clinical Excellence (NICE) in the United Kingdom has promulgated guidance on improving supportive and palliative care for adults with cancer. The specific model of care delivery put forth in this guidance is difficult to generalize to the United States because it is based on an infrastructure for cancer care specific to the United Kingdom, such as designated Cancer Networks22 for specific geographic areas charged with delivering components of a comprehensive National Cancer Plan. However, NICE’s guidance recommends the performance of certain generic activities as part of its model for delivering supportive and palliative services, including assessment of patients’ psychological, social, spiritual, and financial support needs alongside an assessment of physical needs; promotion of continuity and coordination of care through such mechanisms as multidisciplinary teams and interprofessional communication strategies; systems to support patients and their caregivers in participating in care; provision of
patient information; and explicit partnerships between various agencies to ensure access to and receipt of needed services (NICE, 2004).
Models for Treating Depression in Primary Care
An estimated 5–9 percent of patients in primary care settings meet criteria for having major depression (Pignone et al., 2002), and many people with depression are treated in primary care as opposed to mental health settings (Kessler et al., 2005). In addition to its direct effects on health and well-being, depression affects the utilization of and adherence to treatment for general medical conditions (discussed in Chapter 2). Although treatment of depression does not encompass all psychosocial health services, problems encountered in providing high-quality mental health care for depression in primary care settings are similar to problems encountered in detecting and managing the broader array of psychosocial health problems seen in oncology settings. Both situations involve an attempt to provide for specialty services in an environment not intended primarily for the delivery of those services. Models for ensuring care for depression in primary care settings have been developed and tested through research and a number of major initiatives. These models can inform strategies for delivering the broader array of psychosocial health services.
Collaborative Care Model
Although the term “collaborative care” is used to refer to a variety of types of interventions, one model of collaborative care developed by Katon and colleagues that has been tested in randomized controlled trials consists of a systematic approach to the structured involvement of mental health specialists in primary care. This approach employs (1) a negotiated definition of the clinical problem in terms that both patient and physician understand; (2) joint development of a care plan with goals, targets, and implementation strategies; (3) provision of support for self-management training and cognitive and behavioral change; and (4) active sustained follow-up using visits, phone calls, e-mail, and web-based monitoring and decision-support systems (Katon, 2003). In an initial randomized controlled trial of this intervention (supplemented by increased frequency of primary care visits in the first 6 weeks of treatment and scheduled visits with psychiatrists) involving 199 patients with depression seen at a primary care clinic over a 12-month period, intervention patients with major depression (but not those with minor depression) showed significantly greater improvement in symptoms than patients who received usual care (Katon et al., 1995). These findings were repeated in successive trials (Katon et al., 1996, 1999).
In a pilot study, collaborative care also has been found effective in treating low-income Latinas with cancer (Dwight-Johnson et al., 2005).
Three Component Model (3CM™) of the MacArthur Initiatve on Depression and Primary Care
Based on a review of research findings, the John D. and Catherine T. MacArthur Foundation Initiative on Depression and Primary Care developed a Three Component Model (3CM™) in which the primary care clincian, a care manager, and a mental health specialist collaborate with the patient and with each other in providing care. Primary care processes also are reengineered to promote illness self-management, quantitative monitoring of the response to care, and modification of treatment as needed. Care processes include screening and assessment using standardized tools to identify the target population (patients with depression), patient education and engagement in shared decision making, use of a designated case manager to provide telephone support for the depressed patient and periodic feedback to the clinician on the patient’s response to treatment, and formal linkages with mental health specialists (Anonymous, 2004, 2006). A randomized controlled trial of this model in three medical groups and two health plans in the United States involving 60 affiliated primary care practices and 405 patients demonstrated significantly reduced symptoms of depression and increased remission rates compared with usual treatment (Dietrich et al., 2004). 3CM™ has been recommended as an approach for ensuring comprehensive survivorship care to cancer patients through “shared care” collaborations between specialist and primary care clinicians (Oeffinger and McCabe, 2006).
Project IMPACT Collaborative Care Model
Another model of care for delivering psychosocial health services was developed by a national panel of experts for the Improving Mood—Promoting Access to Collaborative Treatment for Late-Life Depression (IMPACT) project. This model consists of systematic assessment to determine a diagnosis; collaboration among patients and primary care and specialty providers to define the problem, develop a therapeutic alliance, and formulate a personalized treatment plan; follow-up and monitoring of treatment outcomes by a case manager; and use of protocols for the involvement of consultation or greater involvement in care by specialists. In a randomized controlled trial of the IMPACT project at 18 primary care clinics associated with eight health care organizations in five states with ethnically and socioeconomically diverse patients, patients with depression
treated according to the IMPACT model, compared with those receiving usual care, were significantly more likely to receive treatment for their depression at all follow-up periods; report greater satisfaction with their care; have significantly lower scores for depression; have a higher rate of complete remission of depression; experience less health-related impairment in work, family, and social functioning; and report better overall quality of life (Unutzer et al., 2001, 2002).
Partners in Care
Partners in Care was a quality improvement intervention for depression care conducted from 1995 to 2000 in 46 primary care clinics within six diverse, nonacademic managed care plans in the western, midwestern, and eastern United States. The study included two programs: one directed at improving depression care using medications and the other at resources to support psychotherapy. Along with quality improvement techniques for changing care delivery (e.g., education of clinical staff in evidence-based depression care), both programs included (1) proactive case detection and clinical assessment; (2) activation of patients to promote knowledge about their condition and motivation to follow treatment regimens; (3) care planning and case management; (4) formal mechanisms for ongoing, effective collaboration between primary care providers and mental health specialists; and (5) follow-up. The two programs proved to be about equally successful. A group-level, randomized controlled trial of the quality improvement interventions found increased rates of appropriate care, decreased symptoms of probable mental illness, and increased health-related quality of life in the intervention group compared with the group receiving usual care (Wells et al., 2000, 2004; RAND Corporation, 2007).
Promoting Excellence in End-of-Life Care Program
Between 1998 and 2004, The Robert Wood Johnson Foundation funded 22 demonstration projects aimed at developing innovative models for delivering palliative care to people with progressive, life-threatening conditions. Projects in the Promoting Excellence in End-of-Life Care Program varied greatly with respect to their target populations (e.g., pediatric patients, persons with serious mental illness, prison inmates, military veterans, renal dialysis patients, Native Americans, Native Alaskans, African Americans, and inner-city medically underserved populations), geographic areas and settings in which they were located (urban, rural, and frontier settings; integrated health systems; hospitals; outpatient clinics; cancer centers; nursing homes; renal dialysis clinics; inner-city public health and safety net systems; and prisons), and the ways in which the delivery of palliative care was organized.
Because each project conducted its own evaluation using different methods and metrics, it was not possible to report outcomes of the program as a whole. However, a qualitative review found that despite their differences, all projects had certain key processes in common: comprehensive assessment of physical, psychosocial, and spiritual domains; interdisciplinary care; care planning; regular communication among providers, patients, and families; care management to achieve coordinated care; ongoing monitoring; and patient and family education. The review also concluded that the projects in the aggregate demonstrated that by individualizing patient and family assessment, effectively employing existing resources, and aligning services with specific patient and family needs, it was possible to improve the quality of care in ways that were financially feasible and acceptable to patients/families, health care providers, and payers (Byock et al., 2006).
REFERENCES
AAMC (Association of American Medical Colleges). 2006. Academic chronic care collaborative congress. Seattle, WA. http://www.aamc.org/patientcare/iicc/congress.htm (accessed January 22, 2007).
Adams, R. J., B. J. Smith, and R. E. Ruffin. 2001. Impact of physician participatory style in asthma outcomes and patient satisfaction. Annals of Allergy, Asthma and Immunology 86(3):269–271.
Addington-Hall, J. M., L. D. MacDonald, H. R. Anderson, J. Chamberlain, P. Freeling, J. M. Bland, and J. Raftery. 1992. Randomised controlled trial of effects of coordinating care for terminally ill cancer patients. British Medical Journal 305(6865):1317–1322.
Adler, H. M. 2007. Toward a biopsychosocial understanding of the patient–physician relationship: An emerging dialogue. Journal of General Internal Medicine 22(2):280–285.
AHIP (America’s Health Insurance Plans). 2007. Innovations in chronic care. http://www.ahipresearch.org/PDFs/Innovations_InCC_07.pdf (accessed April 3, 2007).
Akizuki, N., T. Akechi, T. Nakanishi, E. Yoshikawa, M. Okamura, T. Nakano, Y. Murakami, and Y. Uchitomi. 2003. Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 97(10):2605–2613.
Andrykowski, M. A., M. J. Cordova, J. L. Studts, and T. W. Miller. 1998. Posttraumatic stress disorder after treatment for breast cancer: Prevalence of diagnosis and use of the PTSD Checklist-Civilian version (PCL-C) as a screening instrument. Journal of Consulting and Clinical Psychology 66(3):586–590.
Anonymous. 2004. Depression management tool kit. The MacArthur initiative on depression and primary care at Dartmouth and Duke June 7, 2004. http://www.depression-primary care.org/imges/pdf/macarthur_toolkit.pdf (accessed June 7, 2004).
Anonymous. 2006. MacArthur initiative on depression and primary care. http://www.depression-primarycare.org/about/background/ (accessed January 18, 2007).
Arora, N. K. 2003. Interacting with cancer patients: The significance of physicians’ communication behavior. Social Science and Medicine 57(5):791–806.
Asadi-Lari, M., and D. Gray. 2005. Health needs assessment tools: Progress and potential. International Journal of Technology Assessment in Health Care 21(3):288–297.
Baggs, J., and M. Schmitt. 1988. Collaboration between nurses and physicians. IMAGE: Journal of Nursing Scholarship 20(3):145–149.
Baggs, J., and M. Schmitt. 1997. Nurses’ and resident physicians’ perceptions of the process of collaboration in an MICU. Research in Nursing and Health 20(1):71–80.
Barlow, J., C. Wright, J. Sheasby, A. Turner, and J. Hainsworth. 2002. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling 48(2):177–187.
Barry, M. J., D. C. Cherkin, Y. Chang, F. J. Fowler, and S. Skates. 1997. A randomized trial of a multimedia shared decision-making program for men facing a treatment decision for benign prostatic hyperplasia. Disease Management and Clinical Outcomes 1(1):5–14.
Benbassat, J., D. Pilpel, and M. Tidhar. 1998. Patients’ preferences for participation in clinical decision making: A review of published surveys. Behavioral Medicine 24(2):81–88.
Berrios-Rivera, J. P., R. L. Street Jr., M. G. Garcia Popa-Lisseanu, M. A. Kallen, M. N. Richardson, N. M. Janssen, D. M. Marcus, J. D. Reveille, N. B. Warner, and M. E. Suarez-Almazor. 2006. Trust in physicians and elements of the medical interaction in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis and Rheumatism 55(3):385–393.
Bickell, N. A., and G. J. Young. 2001. Coordination of care for early-stage breast cancer patients. Journal of General Internal Medicine 16(11):737–742.
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness. Journal of the American Medical Association 288(14):1775–1779.
Bodenheimer, T., M. C. Wang, T. G. Rundall, S. M. Shortell, R. R. Gillies, N. Oswald, L. Casalino, and J. C. Robinson. 2004. What are the facilitators and barriers in physician organizations’ use of care management processes? Joint Commission Journal on Quality and Safety 30(9):505–514.
Boyes, A., S. Newell, A. Girgis, P. McElduff, and R. Sanson-Fisher. 2006. Does routine assessment and real-time feedback improve cancer patients’ psychosocial well-being? European Journal of Cancer Care 15(2):163–171.
Brailer, D. J., and E. Terasawa. 2003. Use and adoption of computer-based patient records in the United States. Presentation to IOM Committee on Data Standards for Patient Safety on January 23, 2003. http://www.iom.edu/file.asp?id=10988 (accessed October 17, 2004).
Briss, P., B. Rimer, B. Reilley, R. C. Coates, N. C. Lee, P. Mullen, P. Corso, A. B. Hutchinson, R. Hiatt, J. Kerner, P. George, C. White, N. Gandhi, M. Saraiya, R. Breslow, G. Isham, S. M. Teutsch, A. R. Hinman, R. Lawrence, and Task Force on Community Preventive Services. 2004. Promoting informed decisions about cancer screening in communities and healthcare systems. American Journal of Preventive Medicine 26(1):67–80.
Brown, R., P. Butow, M. J. Boyer, and M. H. Tattersall. 1999. Promoting patient participation in the cancer consultation: Evaluation of a prompt sheet and coaching in question-asking. British Journal of Cancer 80(1/2):242–248.
Brown, R., P. Butow, S. Dunn, and M. H. Tattersall. 2001. Promoting patient participation and shortening cancer consultations: A randomised trial. British Journal of Cancer 85(9):1273–1279.
Brown, R. F., P. N. Butow, M. A. Sharrock, M. Henman, F. Boyle, D. Goldstein, and M. H. Tattersall. 2004a. Education and role modelling for clinical decisions with female cancer patients. Health Expectations 7(4):303–316.
Brown, R., J. Schore, N. Archibald, A. Chen, D. Peikes, K. Sautter, B. Lavin, S. Aliotta, and T. Ensor. 2004b. Coordinating care for Medicare beneficiaries: Early experiences of 15 demonstration programs, their patients, and providers. Princeton, NJ: Mathematica Policy Research, Inc.
Bruera, E., J. S. Wiley, J. L. Palmer, and M. Rosales. 2002. Treatment decisions for breast carcinoma. Patient preferences and physician perceptions. American Cancer Society 94(7):2076–2080.
Bruera, E., C. Sweeney, J. Willey, J. L. Palmer, S. Tolley, M. Rosales, and C. Ripamonti. 2003. Breast cancer patient perception of the helpfulness of a prompt sheet versus a general information sheet during outpatient consultation: A randomized, controlled trial. Journal of Pain and Symptom Management 25(5):412–419.
Burns, J. 1978. Leadership. New York: Harper and Row.
Butow, P. N., S. M. Dunn, M. H. Tattersall, and Q. J. Jones. 1994. Patient participation in the cancer consultation: Evaluation of a question prompt sheet. Annals of Oncology 5(3):199–204.
Butow, P. N., R. Brown, S. Cogar, M. H. Tattersall, and S. M. Dunn. 2002. Oncologists’ reactions to cancer patients’ verbal cues. Psycho-Oncology 11(1):47–58.
Butow, P. N., R. Devine, M. Boyer, S. Pendlebury, M. Jackson, and M. H. Tattersall. 2004. Cancer consultation preparation package: Changing patients but not physicians is not enough. Journal of Clinical Oncology 22(21):4401–4409.
Byock, I., J. S. Twohig, M. Merriman, and K. Collins. 2006. Promoting excellence in end-of-life care: A report on innovative models of palliative care. Journal of Palliative Medicine 9(1):137–151.
Cegala, D. J., L. McClure, T. M. Marinelli, and D. M. Post. 2000. The effects of communication skills training on patients’ participation during medical interviews. Patient and Education Counseling 41(2):209–222.
Chen, A., R. Brown, N. Archibald, S. Aliotta, and P. D. Fox. 2000. Best practices in coordinated care. Princeton, NJ: Mathematica Policy Research.
Cooper-Patrick, L., J. Gallo, J. J. Gonzales, H. T. Vu, N. R. Powe, C. Nelson, and D. E. Ford. 1999. Race, gender, and partnership in the patient–physician relationship. Journal of the American Medical Association 282(6):583–589.
Curry, C., T. Cossich, J. P. Matthews, J. Beresford, and S. A. McLachlan. 2002. Uptake of psychosocial referrals in an outpatient cancer setting: Improving service accessibility via the referral process. Supportive Care in Cancer 10(7):549–555.
Davis, T. M. E., and A. Bridgford. 2001. A comprehensive patient-held record for diabetes. Part two: Large-scale assessment of the Diabetes Databank by patients and health care workers. Practical Diabetes International 18(9):311–314.
Davison, B. J., and S. L. Goldenberg. 2003. Decisional regret and quality of life after participating in medical decision-making for early-stage prostate cancer. BJU International 91(1):14–17.
Davison, B. J., M. E. Gleave, S. L. Goldenberg, L. F. Degner, D. Hoffart, and J. Berkowitz. 2002. Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nursing 25(1):42–49.
Davison, B. J., P. A. Parker, and S. L. Goldenberg. 2003. Patients’ preferences for communicating a prostate cancer diagnosis and participating in medical decision-making. BJU International 93(1):47–51.
Del Piccolo, L., M. Mazzi, A. Saltini, and C. Zimmermann. 2002. Inter and intra individual variations in physicians’ verbal behaviour during primary care consultation. Social Science & Medicine 55(10):1871–1885.
Derogatis, L. R. 2006. BSI © 18 (brief symptom inventory 18). Pearson Education, Inc. http://www.pearsonassessments.com/tests/bsi18.htm#quickfacts (accessed January 3, 2007).
Dietrich, A. J., T. E. Oxman, J. W. W. Jr., H. C. Schulberg, M. L. Bruce, P. W. Lee, S. Barry, P. J. Raue, J. J. Lefever, M. Heo, K. Rost, K. Kroenke, M. Gerrity, and P. A. Nutting. 2004. Re-engineering systems for the treatment of depression in primary care: Cluster randomized controlled trial. British Medical Journal 329(7466):602.
Dohan, D., and D. Schrag. 2005. Using navigators to improve care of underserved patients: Current practices and approaches. Cancer 104(4):848–855.
Dowsett, S. M., J. L. Saul, P. N. Butow, S. M. Dunn, M. J. Boyer, R. Findlow, and J. Dunsmore. 2000. Communication styles in the cancer consultation: Preferences for a patient-centered approach. Psycho-Oncology 9(2):147–156.
Drury, M., J. Harcourt, and M. Minton. 1996. The acceptability of patients with cancer holding their own shared-care record. Psycho-Oncology 5(2):119–125.
Drury, M., P. Yudkin, J. Harcourt, R. Fitzpatrick, L. Jones, C. Alcock, and M. Minton. 2000. Patients with cancer holding their own records: A randomised controlled trial. British Journal of General Practice 50(451):105–110.
Druss, B., R. Rohrbaugh, C. Levinson, and R. Rosenheck. 2001. Integrated medical care for patients with serious psychiatric illness: A randomized trial. Archives of General Psychiatry 58(9):861–868.
Dwight-Johnson, M., K. Ell, and P. Lee. 2005. Can collaborative care address the needs of low-income Latinas with comorbid depression and cancer? Results from a randomized pilot study. Psychosomatics 46(3):224–232.
Eakin, E. G., and L. A. Strycker. 2001. Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: Patient and provider perspectives. Psycho-Oncology 10(2):103–113.
Ell, K., B. Vourlekis, P. J. Lee, and B. Xie. 2007. Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Preventive Medicine 44(1):26–33.
Engel, J., and J. Kerr. 2003. Predictors of quality of life of breast cancer patients. Taylor & Francis Health Sciences 42(7):710–718.
Epstein, R. M., and R. L. Street. 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. NIH Publ. No. 07-6225. Bethesda, MD: National Cancer Institute.
Fleissig, A., V. Jenkins, S. Catt, and L. Fallowfield. 2006. Multidisciplinary teams in cancer care: Are they effective in the UK? Lancet Oncology 7(11):935–943.
Flood, A. B., J. E. Wennberg, R. F. Nease, F. J. Fowler, J. Ding, and L. M. Hynes. 1996. The importance of patient preference in the decision to screen for prostate cancer. Prostate Patient Outcomes Research Team. Journal of General Internal Medicine 11(6):342–349.
Flynn, K. E., M. A. Smith, and D. Vanness. 2006. A typology of preferences for participation in healthcare decision making. Social Science and Medicine 63(5):1158–1169.
Fortner, B., T. Okon, L. Schwartzberg, K. Tauer, and A. C. Houts. 2003. The cancer care monitor: Psychometric content evaluation and pilot testing of a computer administered system for symptom screening and quality of life in adult cancer patients. Journal of Pain and Symptom Management 26(6):1077–1092.
Friedmann, P., T. D’Aunno, L. Jin, and J. Alexander. 2000. Medical and psychosocial services in drug abuse treatment: Do stronger linkages promote client utilization? HSR: Health Services Research 35(2):443–465.
Frosch, D. L., R. M. Kaplan, and V. Felitti. 2001. The evaluation of two methods to facilitate shared decision making for men considering the prostate-specific antigen test. Journal of General Internal Medicine 16(6):391–398.
Gaston, C. M., and G. Mitchell. 2005. Information giving and decision-making in patients with advanced cancer: A systematic review. Social Science and Medicine 61(10):2252–2264.
Gattellari, M., P. N. Butow, and M. H. Tattersall. 2001. Sharing decisions in cancer care. Social Science and Medicine 52(12):1865–1878.
Gilbody, S. M., A. O. House, and T. Sheldon. 2002. Routine administration of Health Related Quality of Life (HRQoL) and needs assessment instruments to improve psychological outcome—a systematic review. Psychological Medicine 32(8):1345–1356.
Gilbody, S. M., P. Whitty, J. Grimshaw, and R. Thomas. 2003. Educational and organizational interventions to improve the management of depression in primary care: A systematic review. Journal of the American Medical Association 289(23):3145–3151.
Gilbody, S. M., A. O. House, and T. A. Sheldon. 2006a. Outcome measures and needs assessment tools for schizophrenia and related disorders. The Cochrane Library 1.
Gilbody, S. M., P. Bower, J. Fletcher, D. Richards, and A. J. Sutton. 2006b. Collaborative care for depression: A cumulative meta-analysis and review of longer term outcomes. Archives of Internal Medicine 166(21):2314–2321.
Gittell, J., K. Fairfield, B. Bierbaum, W. Head, R. Jackson, M. Kelly, R. Laskin, S. Lipson, J. Siliski, T. Thornhill, and J. Zuckerman. 2000. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay. Medical Care 38(8):807–819.
Goodwin, J. S., S. Satish, E. T. Anderson, A. B. Nattinger, and J. L. Freeman. 2003. Effect of nurse case management on the treatment of older women with breast cancer. Journal of the American Geriatrics Society 51(9):1252–1259.
Gordon, H., R. L. Street, P. A. Kelly, J. Souchek, and N. P. Wray. 2005. Physician–patient communication following invasive procedures: An analysis of post-angiogram consultations. Social Science and Medicine 61(5):1015–1025.
Gordon, H., R. L. Street, B. F. Sharf, P. A. Kelly, and J. Souchek. 2006a. Racial differences in trust and lung cancer patients’ perceptions of physician communication. Journal of Clinical Oncology 24(6):904–909.
Gordon, H., R. L. Street, B. F. Sharf, and J. Souchek. 2006b. Racial differences in doctors’ information-giving and patients’ participation. American Cancer Society 107(6): 1313–1320.
Greenfield, S., S. Kaplan, J. E. Ware Jr., E. Yano, and H. Frank. 1988. Patients’ participation in medical care: Effects on blood sugar control and quality of life in diabetes. Journal of General Internal Medicine 3(5):448–457.
Grimshaw, J., R. Winkeins, L. Shirran, C. Cunningham, A. Mayhew, R. Thomas, and C. Fraser. 2006. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database of Systematic Reviews (4).
Guadagnoli, E., and P. Ward. 1998. Patient participation in decision-making. Social Science and Medicine 47(3):329–339.
Hack, T. F., L. F. Degner, P. Watson, and L. Sinha. 2006. Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psycho-Oncology 15(1):9–19.
Hampshire, A. J., M. E. Blair, N. S. Crown, A. J. Avery, and E. I. Williams. 2004. Variation in how mothers, health visitors and general practitioners use the personal child health record. Child: Care, Health & Development 30(4):307–316.
Handford, C. D., A. M. Tynan, J. M. Rackal, R. H. Glazier. 2006. Setting and organization of care for persons living with HIV/AIDS. Cochrane Database of Systematic Reviews (3):CD004348.
Hegel, M. T., C. P. Moore, E. D. Collins, S. Kearing, K. L. Gillock, R. L. Riggs, K. F. Clay, and T. A. Ahles. 2006. Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107(12):2924–2931.
Heisler, M., R. R. Bouknight, R. A. Hayward, D. M. Smith, and E. A. Kerr. 2002. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. Journal of General Internal Medicine 17(4):243–252.
Hoffman, B. M., M. A. Zevon, M. C. D’Arrigo, and T. B. Cecchini. 2004. Screening for distress in cancer patients: The NCCN rapid-screening measure. Psycho-Oncology 13(11): 792–799.
Houssami, N., and R. Sainsbury. 2006. Breast cancer: Multidisciplinary care and clinical outcomes. European Journal of Cancer 42:2480–2491.
ICIC (Improving Chronic Illness Care). 2007. Improving chronic illness care. http://www.improvingchroniccare.org/index.html (accessed January 12, 2007).
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2003. Health professions education: A bridge to quality. A. Greiner and E. Knebel, eds. Washington, DC: The National Academies Press.
IOM. 2004. Keeping patients safe: Transforming the work environment of nurses. A. E. K. Page, ed. Washington, DC: The National Academies Press.
IOM. 2007. Implementing cancer survivorship care planning. Washington, DC: The National Academies Press.
Jacobsen, P. B., and S. Ransom. 2007. Implementation of NCCN distress management guidelines by member institutions. Journal of the National Comprehensive Cancer Network 5(1):93–103.
Jacobsen, P. B., K. A. Donovan, P. C. Trask, S. B. Fleishman, J. Zabora, F. Baker, and J. C. Holland. 2005. Screening for psychologic distress in ambulatory cancer patients. Cancer 103(7):1494–1502.
Jandorf, L., Y. Gutierrez, J. Lopez, J. Christie, and S. H. Itzkowitz. 2005. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. Journal of Urban Health 82(2):216–224.
Janz, N. K., P. A. Wren, L. A. Copeland, J. C. Lowery, S. L. Goldfarb, and E. G. Wilkins. 2004. Patient–physician concordance: Preferences, perceptions, and factors influencing the breast cancer surgical decision. Journal of Clinical Oncology 22(15):3091–3098.
Kahán, Z., K. Varga, R. Dudás, T. Nyári, and L. Thurzó. 2006. Collaborative/active participation per se does not decrease anxiety in breast cancer. Pathology Oncology Research 12(2):93–101.
Kaplan, S., S. Greenfield, and J. Ware. 1989. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care 27(3 Supplement):S110–S127.
Kaplan, S. H., B. Gandek, S. Greenfield, W. Rogers, and J. E. Ware Jr. 1995. Patient and visit characteristics related to physician’s participatory decision-making style: Results from the Medical Outcomes Study. Medical Care 33(12):1176–1187.
Kaplan, S., S. Greenfield, B. Gandek, W. H. Rogers, and J. E. Ware. 1996. Characteristics of physicians with participatory decision making styles. Annals of Internal Medicine 124(5):497–504.
Katon, W. J. 2003. The Institute of Medicine “Chasm” report: Implications for depression collaborative care models. General Hospital Psychiatry 25(4):222–229.
Katon, W. J., M. V. Korff, E. Lin, E. Walker, G. E. Simon, T. Bush, P. Robinson, and J. Russo. 1995. Collaborative management to achieve treatment guidelines: Impact on depression in primary care. Journal of the American Medical Association 273(13):1026–1031.
Katon, W. J., P. Robinson, M. V. Korff, E. Lin, T. Bush, E. Ludman, G. Simon, and G. Walker. 1996. A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry 53(10):924–932.
Katon, W. J., M. V. Korff, E. Lin, G. Simon, E. Walker, J. Unutzer, T. Bush, J. Russo, and E. Ludman. 1999. Stepped collaborative care for primary care patients with persistent symptoms of depression. Archives of General Psychiatry 56(12):1109–1115.
Katz, S. J., P. M. Lantz, N. K. Janz, A. Fagerlin, K. Schwartz, L. Liu, D. Deapen, B. Salem, I. Lakhani, and M. Morrow. 2005. Patient involvement in surgery treatment decisions for breast cancer. Journal of Clinical Oncology 23(24):5526–5533.
Kazak, A. E., A. Prusak, M. McSherry, S. Simms, D. Beele, M. Rourke, M. Alderfer, and B. Lange. 2001. The Psychosocial Assessment Tool (PAT)©: Pilot data on a brief screening instrument for identifying high risk families in pediatric oncology. Families, Systems and Health 19(3):303–317.
Keating, N., E. Guadagnoli, M. B. Landrum, C. Borbas, and J. C. Weeks. 2002. Treatment decision making in early-stage breast cancer: Should surgeons match patients’ desired level of involvement? Journal of Clinical Oncology 20(6):1473–1479.
Keeley, R.D., J. L. Smith, P. A. Nutting, L. Miriam Dickinson, W. Perry Dickinson, and K. M. Rost. 2004. Does a depression intervention result in improved outcomes for patients presenting with physical symptoms? Journal of General Internal Medicine 19(6): 615–623.
Kerr, J., J. Engel, A. Schlesinger-Raab, H. Sauer, and D. Hölzel. 2003a. Communication, quality of life and age: Results of a 5-year prospective study in breast cancer patients. Annals of Oncology 14(3):421–427.
Kerr, J., J. Engel, A. Schlesinger-Raab, H. Sauer, and D. Hölzel. 2003b. Doctor–patient communication: Results of a four-year prospective study in rectal cancer patients. Diseases of the Colon and Rectum 46(88):1038–1046.
Kessler, R. C., O. Demler, R. G. Frank, M. Olfson, H. A. Pincus, E. E. Walters, P. Wang, K. B. Wells, and A. M. Zaslavsky. 2005. Prevalence and treatment of mental disorders, 1990 to 2003. The New England Journal of Medicine 352(24):2515–2523.
Kiesler, D. J., and S. M. Auerbach. 2006. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: Evidence, models and interventions. Patient Education and Counseling 61(3):319–341.
Kindler, C., L. Szirt, D. Sommer, R. Hausler, and W. Langewitz. 2005. A quantitative analysis of anaesthetist–patient communication during the pre-operative visit. Anaesthesia 60(1):53–59.
Kornblith, A., J. Dowell, and I. Herndon. 2006. Telephone monitoring of distress in patients aged 65 years or older with advanced stage cancer: A cancer and leukemia group b study. Cancer 107(11):2706–2714.
Kruijver, I. P. M., B. Garssen, A. P. Visser, and A. J. Kuiper. 2006. Signalising psychosocial problems in cancer care: The structural use of a short psychosocial checklist during medical or nursing visits. Patient Education and Counseling 62(2):163–177.
Lecouturier, J., L. Crack, K. Mannix, R. H. Hall, S. Bond. 2002. Evaluation of a patient-held record for patients with cancer. European Journal of Cancer Care 11(2):114–121.
Liao, L., J. G. Jollis, E. R. DeLong, E. D. Peterson, K. G. Morris, and D. B. Mark. 1996. Impact of an interactive video on decision making of patients with ischemic heart disease. Journal of General Internal Medicine 11(6):373–376.
Linden, W., D. Yi, M. C. Barroetavena, R. MacKenzie, and R. Doll. 2005. Development and validation of a psychosocial screening instrument for cancer. Health and Quality of Life Outcomes 3:54.
Lowe, B., J. Unutzer, C. M. Callahan, A. J. Perkins, and K. Kroenke. 2004. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Medical Care 42(12):1194–1201.
Maliski, S. L., L. Kwan, T. Krupski, A. Fink, J. R. Orecklin, and M. S. Litwin. 2004. Confidence in the ability to communicate with physicians among low-income patients with prostate cancer. Urology 64(2):329–334.
Maly, R. C., B. Leake, and R. A. Silliman. 2004. Breast cancer treatment in older women: Impact of the patient-physician interaction. Journal of the American Geriatrics Society 52(7):1138–1145.
Marshall, M., A. Gray, A. Lockwood, and R. Green. 2004. Case management for people with severe mental disorders (Cochrane Review, Issue 4). Chichester, UK: John Wiley and Sons, Ltd.
Mazur, D. J., and D. H. Hickam. 1997. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. Journal of General Internal Medicine 12(2):114–117.
Mazur, D. J., and J. F. Merz. 1996. How older patients’ treatment preferences are influenced by disclosures about therapeutic uncertainty: Surgery versus expectant management for localized prostate cancer. Journal of the American Geriatric Society 44(8):934–937.
Mazur, D. J., D. H. Hickam, and M. D. Mazur. 2005. The role of doctor’s opinion in shared decision making: What does shared decision making really mean when considering invasive medical procedures? Health Expectations 8(2):97–102.
McAlister, F. A., S. Stewart, S. Ferrua, and J. V. McMurray. 2004. Multidisciplinary strategies for the management of heart failure patients at high risk for admission. A systematic review of randomized trials. Journal of the American College of Cardiology 44(4):810–819.
McCorkle, R., N. Strumpf, I. Nuamah, D. C. Adler, M. E. Cooley, C. Jepson, E. J. Lusk, and M. Torosian. 2000. A specialized home care intervention improves survival among older post-surgical cancer patients. Journal of the American Geriatrics Society 48(12):1707–1713.
McDonald, K., V. Sundaram, D. Bravata, R. Lewis, N. Lin, S. Kraft, M. McKinnon, H. Paguntalan, and D. Owens. 2007. Care coordination. AHRQ Publication No. 04(07)-0051-7, Vol. 7. In Closing the quality gap: A critical analysis of quality improvement strategies. Edited by K. G. Shojania, K. M. McDonald, R. M. Wachter, and D. K. Owens. Rockville, MD: Agency for Healthcare Research and Quality. http://www.ahrq.gov/downloads/pub/evidence/pdf/caregap/caregap.pdf (accessed August 17, 2007).
McDonald, M. V., S. D. Passik, W. Dugan, B. Rosenfeld, D. E. Theobald, and S. Edgerton. 1999. Nurses’ recognition of depression in their patients with cancer. Oncology Nursing Forum 26(3):593–599.
McLachlan, S. A., A. Allenby, J. Matthews, A. Wirth, D. Kissane, M. Bishop, J. Beresford, and J. Zalcberg. 2001. Randomized trial of coordinated psychosocial interventions based on patient self-assessments versus standard care to improve the psychosocial functioning of patients with cancer. Journal of Clinical Oncology 19(21):4117–4125.
Mitchell, A., and J. Coyne. 2007. Do ultra-short screening instruments accurately detect depression in primary care? A pooled analysis and meta-analysis of 22 studies. British Journal of General Practice 57(535):144–151.
National Breast Cancer Centre and National Cancer Control Initiative. 2003. Clinical practice guidelines for the psychosocial care of adults with cancer. Camperdown, NSN, Australia: National Health and Medical Research Council.
National Institute of Standards and Technology. 2007. Baldrige National Quality Program: Health care criteria for performance excellence. Gaithersburg, MD: United States Department of Commerce.
NCCN (National Comprehensive Care Network). 2006. Distress management. In NCCN clinical practice guidelines in oncology. http://www.nccn.org/professionals/physician_gls/PDF/distress.pdf (accessed August 10, 2006).
NCCN. 2007a. Distress management (V.I.2007), 08-10-06. http://www.nccn.org/professionals/physician_gls/PDF/distress.pdf (accessed January 17, 2007).
NCCN. 2007b. National Comprehensive Cancer Network. http://www.nccn.org/default.asp (accessed November 16, 2007).
NCCS (National Coalition for Cancer Survivorship). 2007. Cancer survival toolbox®. http://www.cancersurvivaltoolbox.org (accessed March 23, 2007).
NCI (National Cancer Institute). undated. NCI community cancer centers program—frequently asked questions. http://ncccp.cancer.gov/Media/FactSheet.htm (accessed August 27, 2007).
NICE (National Institute for Clinical Evidence). 2004. Guidance on cancer services: Improving supportive and palliative care for adults with cancer: The manual. http://ww.nice.org.uk/page.aspx?0=csgspfullguideline (accessed July 12, 2006).
Niederhuber, J. E. 2006. NCCCP increases patient access to quality cancer care. NCI Cancer Bulletin 3(43).
Norris, S. L., P. J. Nichols, C. J. Caspersen, R. E. Glasgow, M. M. Engelgau, L. Jack, G. Isham, S. R. Snyder, V. G. Carande-Kulis, S. Garfield, P. Briss, and D. McCulloch. 2002. The effectiveness of disease and case management for people with diabetes. A systematic review. American Journal of Preventive Medicine 22(Supplement 4):15–38.
O’Connor, A. M., H. A. Llewellyn-Thomas, and E. R. Drake. 1995. An annotated bibliography of research on shared decision making. Toronto, Ontario: National Cancer Institute of Canada.
Oeffinger, K. C., and M. S. McCabe. 2006. Models for delivering survivorship care. Journal of Clinical Oncology 24(32):5117–5124.
Onel, E., C. Hamond, J. H. Wasson, B. B. Berlin, M. G. Ely, V. P. Laudone, A. E. Tarantino, and P. C. Albertsen. 1998. Assessment of the feasibility and impact of shared decision making in prostate cancer. Urology 51(1):63–66.
Ouwens, M., H. Wollersheim, R. Hermens, M. Hulscher, and R. Grol. 2005. Integrated care programmes for chronically ill patients: A review of systematic reviews. International Journal for Quality in Health Care 17(2):141–146.
Palmer, L., and S. Somers. 2005. Integrating long-term care: Lessons from building health systems for people with chronic illnesses. A national program of The Robert Wood Johnson Foundation. Center for Health Care Strategies, Inc. http://www.chcs.org/usr_doc/CHCSBHSFINAL.pdf (accessed January 24, 2007).
Passik, S., W. Dugan, M. McDonald, and B. Rosenfeld. 1998. Oncologists’ recognition of depression in their patients with cancer. Journal of Clinical Oncology 16(4):1594–1600.
Peele, P. B., L. A. Siminoff, Y. Xu, and P. M. Ravdin. 2005. Decreased use of adjuvant breast cancer therapy in a randomized controlled trial of a decision aid with individualized risk information. Medical Decision Making 25(3):301–307.
Piccolo, L. D., A. Saltini, C. Zimmermann, and G. Dunn. 2000. Differences in verbal behaviors of patients with and without emotional distress during primary care consultations. Psychological Medicine 30(3):629–643.
Pignone, M. P., B. N. Gaynes, J. L. Rushton, C. M. Burchell, C. T. Orleans, C. D. Mulrow, and K. N. Lohr. 2002. Screening for depression in adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine 136(10):765–776.
Pincus, H. A. 2003. The future of behavioral health and primary care: Drowning in the mainstream or left on the bank? Psychosomatics 44(1):1–11.
Pruyn, J. F. A., H. A. G. Heule-Dieleman, P. P. Knegt, F. R. Mosterd, M. A. G. van Hest, H. A. M. Sinnige, A. T. H. Pruyn, and M. F. de Boer. 2004. On the enhancement of efficiency in care for cancer patients in outpatient clinics: An instrument to accelerate psychosocial screening and referral. Patient Education & Counseling 53(2):135–140.
Raftery, J., J. Addington-Hall, L. MacDonald, H. Anderson, J. Bland, J. Chamberlain, and P. Freeling. 1996. A randomized controlled trial of the cost-effectiveness of a district coordinating service for terminally ill cancer patients. Palliative Medicine 10(2):151–161.
Ramfelt, E., K. Lutzen, and G. Nordström. 2005. Treatment decision-making in a group of patients with colo-rectal cancer before surgery and a one-year follow-up. European Journal of Cancer Care 14(4):327–335.
RAND Corporation. 2007. Overview of the partners in care study. http://www.rand.org/health/projects/pic/overview.html (accessed February 26, 2007).
Recklitis, C. J., S. K. Parsons, M.-C. Shih, A. Mertens, and L. Robinson. 2006. Factor structure of the brief symptom inventory—18 in adult survivors of childhood cancer: Results from the childhood cancer survivor study. Psychological Assessment 18(1):22–32.
Richards, S., and J. Coast. 2003. Interventions to improve access to health and social care after discharge from hospital: A systematic review. Journal of Health Services and Research Policy 8(3):171–179.
Robinson, J. W., and D. L. Roter. 1999. Psychosocial problem disclosure by primary care patients. Social Science and Medicine 48(10):1353–1362.
Rost, K. M., K. S. Flavin, K. Cole, and J. B. McGill. 1991. Change in metabolic control and functional status after hospitalization impact of patient activation intervention in diabetic patients. Diabetes Care 14(10):881–889.
Roter, D., J. Hall, and Y. Aoki. 2002. Physician gender effects in medical communication. Journal of the American Medical Association 288(6):756–764.
Roth, A. J., A. B. Kornblith, L. Batel-Copel, E. Peabody, H. I. Scher, and J. C. Holland. 1998. Rapid screening for psychologic distress in men with prostate carcinoma: A pilot study. Cancer 82(10):1904–1908.
Samet, J. H., P. Friedmann, and R. Saitz. 2001. Benefits of linking primary medical care and substance abuse services: Patient, provider, and societal perspectives. Archives of Internal Medicine 161(1):85–91.
Schmitt, M. 2001. Collaboration improves the quality of care: Methodological challenges and evidence from U.S. health care research. Journal of Interprofessional Care 15(1):47–66.
Schofield, P., and P. N. Butow. 2003. Psychological responses of patients receiving a diagnosis of cancer. Annals of Oncology 14(1):48–56.
Schwartzberg, L., B. Fortner, and A. Houts. 2007. Use of technology to enhance doctor–patient interactions. American Society of Clinical Oncology Education Book. Alexandria, VA: American Society of Clinical Oncology. Pp. 686–791.
Shortell, S., J. Zimmerman, D. Rousseau, R. Gillies, D. Wagner, E. Draper, W. Knaus, and J. Duffy. 1994. The performance of intensive care units: Does good management make a difference? Medical Care 32(5):508–525.
Siminoff, L. A., J. H. Rose, A. Zhang, and S. J. Zyzanski. 2005. Measuring discord in treatment decision-making; progress toward development of a cancer communications and decision-making assessment tool. Psycho-Oncology 15(6):528–540.
Siminoff, L. A., G. C. Graham, and N. H. Gordon. 2006a. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Education and Counseling 62(3):355–360.
Siminoff, L. A., N. H. Gordon, P. Silverman, T. Budd, and P. M. Ravdin. 2006b. A decision aid to assist in adjuvant therapy choices for breast cancer. Psycho-Oncology 15(11):1001–1013.
Sleath, B., and R. Rubin. 2003. The influence of Hispanic ethnicity on patients’ expression of complaints about and problems with adherence to antidepressant therapy. Clinical Therapeutics 25(6):1739–1749.
Sleath, B., D. Roter, B. Chewning, and B. Svarstad. 1999. Asking questions about medication: Analysis of physician–patient interactions and physician perceptions. Medical Care 37(11):1169–1173.
Stewart, M. 1995. Effective physician–patient communication and health outcomes: A review. Canadian Medical Association 152(9):1423–1433.
Street, R. L. Jr., and H. S. Gordon. 2006. The clinical context and patient participation in post-diagnostic consultations. Patient Education and Counseling 64(1–3):217–224.
Street, R. L. Jr., E. Krupat, R. A. Bell, R. L. Kravitz, and P. Haidet. 2003. Beliefs about control in the physician–patient relationship. Effect on communication in medical encounters. Journal of General Internal Medicine 18(8):609–616.
Street, R. L. Jr., H. S. Gordon, M. M. Ward, E. Krupat, and R. L. Kravitz. 2005. Patient participation in medical consultations. Why some patients are more involved than others. Medical Care 43(10):960–969.
Stuck, A. E., M. Egger, A. Hammer, C. E. Minder, and J. C. Beck. 2002. Home visits to prevent nursing home admission and functional decline in elderly people: Systematic review and meta-regression analysis. Journal of the American Medical Association 287(8):1022–1028.
Thind, A., and R. Maly. 2006. The surgeon–patient interaction in older women with breast cancer: What are the determinants of a helpful discussion? Annals of Surgical Oncology 13(6):778–793.
Thompson, C., and M. Briggs. 2000. Support for carers of people with Alzheimer’s type dementia. Cochrane Database of Systematic Reviews (2):CD000454.
Timmermans, L., R. W. van der Maazen, K. P. van Spaendonck, J. W. Leer, and F. W. Kraaimaat. 2006. Enhancing patient participation by training radiation oncologists. Patient Education and Counseling 63(1–2):55–63.
Trask, P. C. 2004. Assessment of depression in cancer patients. Journal of the National Cancer Institute Monographs 2004(32):80–92.
Trask, P. C., A. Paterson, M. Riba, B. Brines, K. Griffith, P. Parker, J. Weick, P. Steele, K. Kyro, and J. Ferrara. 2002. Assessment of psychological distress in prospective bone marrow transplant patients. Bone Marrow Transplantation 29(11):917–925.
Unutzer, J., W. Katon, J. W. Williams, C. M. Callahan, L. Harpole, E. M. Hunkeler, M. Hoffing, P. Arean, M. T. Hegel, M. Schoenbaum, S. M. Oishi, and C. A. Langston. 2001. Improving primary care for depression in late life. Medical Care 39(8):785–799.
Unutzer, J., W. Katon, C. M. Callahan, J. W. Williams, E. Hunkeler, L. Harpole, M. Hoffing, R. D. D. Penna, P. H. Noel, E. H. B. Lin, P. A. Arean, M. T. Hegel, L. Tang, T. R. Belin, S. Oishi, and C. Langston. 2002. Collaborative care management of late-life depression in the primary care setting. Journal of the American Medical Association 288(22):2836–2845.
U.S. Preventive Services Task Force. 2002. Screening for depression. http://www.ahrq.gov/clinic/uspstf/uspsdepr.htm (accessed February 21, 2007).
van Roosmalen, M. S., P. F. Stalmeier, L. C. Verhoef, J. E. Hoekstra-Weebers, J. C. Oosterwijk, N. Hoogerbrugge, U. Moog, and W. A. van Daal. 2004. Randomized trial of a shared decision-making intervention consisting of trade-offs and individualized treatment information for BRCA1/2 mutation carriers. Journal of Clinical Oncology 22(16): 3293–3301.
Walsh-Burke, K., and C. Marcusen. 1999. Self-advocacy training for cancer survivors. The Cancer Survival Toolbox. Cancer Practice 7(6):297–301.
Walton, S., H. Bedford, and C. Dezateux. 2006. Use of personal child health records in the UK: Findings from the millennium cohort study. British Medical Journal 332(7536): 269–270.
Weisner, C., J. Mertens, S. Parthasarathy, C. Moore, and Y. Lu. 2001. Integrating primary medical care with addiction treatment: A randomized controlled trial. Journal of the American Medical Association 286(14):1715–1723.
Wells, K. B., C. Sherbourne, M. Schoenbaum, N. Duan, L. Meredith, J. Unutzer, J. Miranda, M. Carney, and L. Rubenstein. 2000. Impact of disseminating quality improvement programs for depression in managed primary care: A randomized controlled trial. Journal of the American Medical Association 283(12):212–220.
Wells, K., C. Sherbourne, M. Schoenbaum, S. Ettner, N. Duan, J. Miranda, J. Unutzer, and L. V. Rubenstein. 2004. Five-year impact of quality improvement for depression: Results of a group-level randomized controlled trial. Archives of General Psychiatry 61(4):378–386.
Wen, K.-Y., and D. H. Gustafson. 2004. Needs assessment for cancer patients and their families. Health and Quality of Life Outcomes 2:11.
Whelan, T., M. Levine, A. Willan, A. Gafni, K. Sanders, D. Mirsky, S. Chambers, M. A. O’Brien, S. Reid, and S. Dubois. 2004. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery. A randomized trial. Journal of the American Medical Association 292(4):435–441.
Williams, J. G., W. Y. Cheung, N. Chetwynd, D. R. Cohen, S. El-Sharkawi, I. Finlay, B. Lervy, M. Longo, and K. Malinovszky. 2001. Pragmatic randomised trial to evaluate the use of patient held records for the continuing care of patients with cancer. Quality in Health Care 10(3):159–165.
Wong, F., D. Stewart, J. Dancey, M. Meana, M. P. McAndrews, T. Bunston, and A. M. Cheung. 2000. Men with prostate cancer: Influence of psychological factors on information needs and decision-making. Journal of Psychosomatic Research 49(1):13–19.
Woods, V. D., S. B. Montgomery, R. P. Herring, R. W. Gardner, and D. Stokols. 2006. Social ecological predictors of prostate-specific antigen blood test and digital rectal examination in black American men. Journal of the National Medical Association 98(4):492–504.
Xu, K., T. F. Borders, and A. A. Arif. 2004. Ethnic differences in parents’ perception of participatory decision-making style of their children’s physicians. Medical Care 42(4):328–335.
Zabora, J., K. BrintzenhofeSzoc, P. Jacobsen, B. Curbow, S. Piantadosi, C. Hooker, A. Owens, and L. Derogatis. 2001. A new psychosocial screening instrument for use with cancer patients. Psychosomatics 42(3):241–246.
Zachariae, R., C. Pederson, A. B. Jensen, E. Ehrnrooth, P. B. Rossen, and H. von der Maase. 2003. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. British Journal of Cancer 88(5):658–665.
Zigmond, A., and R. Snaith. 1983. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 67(6):361–370.
Ziguras, S. J., and G. W. Stuart. 2000. A meta-analysis of the effectiveness of mental health case management over 20 years. Psychiatric Services 51(11):1410–1421.
Ziguras, S. J., G. W. Stuart, and A. C. Jackson. 2002. Assessing the evidence on case management. British Journal of Psychiatry 181(1):17–21.
Zwarenstein, M., B. Stephenson, and L. Johnston. 2004. Case management: Effects on professional practice and health care outcomes: Protocol. Cochrane Database of Systematic Reviews (1).


































































