2
Engaging Complex Systems Through Engineering Concepts
INTRODUCTION
Along with the increasing interest and concern for the problems surrounding health care in the United States has come an increasing awareness of the implications of the healthcare system’s complexity. In seeking to engage engineering sciences for insight and strategies for healthcare improvement, it was important to frame the workshop presentations and discussions with a common foundation in and understanding of engineering concepts. The engineering disciplines presented as possible opportunity areas for improving healthcare delivery and management included systems engineering, industrial engineering, operations research, human factors engineering, financial engineering, and risk analysis.
William B. Rouse, executive director of The Tennenbaum Institute at Georgia Institute of Technology, described the fundamental perspectives by which systems engineering approaches complex problems. With a particular focus on the nature of prediction, control, and design, Rouse presented a model that shed light on the roots of spiraling healthcare costs and then suggested some likely effects of alternative approaches to controlling costs. Offering a list of standard options from the systems engineering toolbox that might be applied to build processes for controlling costs, as well as some new options described in a Commonwealth Fund report (Schoen et al., 2008), Rouse provided practical insights into how engineers might approach a representative set of issues in health care.
Richard C. Larson, Mitsui Professor of Engineering Systems and Civil and Environmental Engineering and director of the Center for Engineering
Systems Fundamentals at the Massachusetts Institute of Technology, introduced some principles of operations research (OR), a systems-oriented approach that draws on the principles of the scientific method to help frame, formulate, and solve difficult problems involving people and technology. Larson offered examples of the application of OR to health care, including work that used sophisticated optimization modeling and computational techniques to advance cancer therapeutics. He said that the techniques of OR have much to offer to the reengineering of systems and processes in health care. He further suggested that the applications of OR and engineering systems with the greatest potential to transform health care have not yet been identified and that further attention is needed to determine opportunities for future progress.
Discussing the engineering of systems design tools, James M. Tien, distinguished professor and dean of the College of Engineering at the University of Miami, observed that health care is a complex, integrated collection of human-centered activities that is increasingly dependent on information technology and knowledge. In particular, he explained, health care is a service system. By definition a service system combines three essential components—people, processes, and products—and Tien suggested that managing services means, in effect, managing an integrated and adaptive set of people, processes, and products. He outlined an alternative systems management view of services, discussing the increasing complexity of systems; the increasing need for real-time, adaptive decision making within these systems; and the reality that modern systems are becoming increasingly more human centered. One result is that products and services are becoming both more complex and more personalized or customized. Tien suggested that the methodologies he discussed can be applied to help improve basic services in health care.
Essential methodologies of systems engineering were also the focus of a paper by Harold W. Sorenson, professor of mechanical and aerospace engineering in the Jacobs School of Engineering at the University of California, San Diego. Sorenson discussed the principles of an “integrated perspective” for managing complex systems. He outlined the questions that typically apply in engineering complex enterprises, and he described typical approaches that a systems engineer might use to articulate the nature of a problem and to design an appropriate architecture to address it. He provided an overview of how systems engineers think about managing complexity, developing solutions, and assessing those solutions. For health care, Sorenson suggested, such an approach could allow a rapid enhancement of capabilities, the development of better working relationships among stakeholders, and the identification of new and more effective ways to deliver patient care—with the potential to lead ultimately to significant changes in healthcare culture, practice, and delivery.
CAN WE AFFORD TECHNOLOGICAL INNOVATION IN HEALTH CARE?
William B. Rouse, Ph.D., The Tennenbaum Institute, Georgia Institute of Technology
The enormous cost of U.S. health care is often cited as a key national challenge (CBO, 2008). Health care is consuming an increasingly large portion of the nation’s gross domestic product (GDP). At the same time, there are concerns that the quality of health care in the United States lags behind that of other countries (IOM, 2000, 2001). It is clear that substantial improvements in the delivery of healthcare value are needed, and, it is argued, these improvements should be achievable through value-based competition (Porter and Teisberg, 2006). Of course, it should be kept in mind that our healthcare system did not become the way it is overnight (Stevens et al., 2006).
A recent report published by the Congressional Budget Office (CBO) attributes 50 percent of the cost growth in health care over the past four decades to technological innovation (CBO, 2008). Science and engineering research has yielded a steady stream of innovations for detection, diagnosis, and treatment, whose use in many cases has grown by 10 to 15 percent per year. Compounding such growth over 40 years results in a very large level of use. In many domains, such as personal electronics or cellular telephones, such growth would be seen as an enormous success. However, the third-party payers of most healthcare bills see this growth as a threat to the viability of the healthcare system.
This paper approaches this threat as an engineering problem rather than as a problem of medical science. First, it outlines the engineering approach and contrasts that approach with science. It then explores the CBO’s conclusions a bit more deeply. It proposes three models for controlling the costs of health care so that the growth of these costs tracks the growth in GDP, providing insight into the magnitude of the efficiency gains needed to accomplish this goal. The paper concludes with a discussion of possible ways to achieve these gains.
Engineering Approach
Determination of the best way to control healthcare costs should be approached as an engineering problem rather than as a medical science problem. The potential of engineering to enhance health care has, of late, received increasing attention (NAE/IOM, 2005). This potential can be understood in terms of the following levels of understanding of any phenomenon:
- Describe past observations.
- Classify past observations.
- Predict future observations.
- Control future observations.
- Design future observations.
Science progresses from describing and classifying past observations to predicting future observations. If these predictions turn out to be accurate, science concludes that the theory or model employed has credence. If not, the theory or model needs revision. The goal is to create valid knowledge.
Engineering builds on scientific knowledge, particularly in using models to predict. However, engineers usually are not content just to predict. They also want to control the state of the system of interest or, if they can, to design or redesign the system to facilitate better control. In some cases, this penchant for design and control has enormous societal implications (McPhee, 1990).
Predict
Taken simplistically, there are two basic approaches to prediction. One is extrapolation. Equations are fit to data collected under particular conditions. These equations are then used to project the outcomes for similar conditions. Statistical models, such as those used in medicine for randomized controlled trials (RCTs), are examples of equation fitting. To the extent that the conditions of the trials adequately reflect the eventual conditions of use, we can be reasonably confident that similar outcomes will be attained when a treatment moves from trials to clinical use.
RCTs work well, although slowly and expensively, when there are large populations that can be observed under controllable conditions. However, this approach cannot be employed for the study of large-scale systems such as health care. There simply are not enough healthcare systems to achieve statistical significance in a study of the large, systemic changes likely to be needed to control costs and enhance quality to the extent outlined earlier.
Engineering approaches to solving large-scale problems typically rely on models as a basis for prediction. These models are formulated from “first principles” drawn from a range of scientific domains. These principles, usually stated as fairly simple mathematical relationships, become elements of much larger mathematical and computational models that are used to predict the outcomes of different approaches to the design and control of complex systems. Engineering approaches are illustrated later in this paper.
Control
Engineering the control of a system involves measurement, feedback, and compensation to achieve system objectives. Measurement is used to ascertain the state of the system. This, of course, requires defining system state variables, their units of measure, and how such measurements can be made. Feedback involves comparing predicted and actual system states in order to correct errors. Such feedback results in a “control loop.” Compensation concerns adding dynamic elements to the control loop in order to counteract delays and lags in system response.
Design
Engineering design involves problem analysis, solution synthesis, production of an artifact that embodies the solution, and then sustainment of the system in its use. Analysis involves understanding input–output relationships, including uncertainties, and then creating models, as discussed above. Synthesis is a matter of designing input–output relationships to achieve system objectives. Production involves the various actions—fabrication, construction, programming, and so forth—necessary to create systems that embody the desired relationships. Finally, sustainment concerns creating mechanisms that ensure that system objectives will be met in the future.
Summary
Engineering approaches to prediction, control, and design have much to offer health care with respect to making systemic improvements by decreasing costs and increasing quality. The remainder of this paper provides an illustration of how engineering might help in meeting the challenges faced by health care.
Healthcare Illustration
As discussed earlier, the past four decades have seen enormous increases in healthcare costs. Specifically, real healthcare costs tripled as a percentage of GDP in the period from 1965 to 2005, with half of this growth due to technological innovation (CBO, 2008). The magnitude of these increases has led some to conclude that the healthcare system is “running on empty” (Peterson, 2005). There appears to be virtually unanimous agreement that the system must change significantly.
Figure 2-1 summarizes the overall phenomenon discussed in the CBO report. Technological inventions become market innovations as they increase in effectiveness and the associated risks decrease. The result is in-
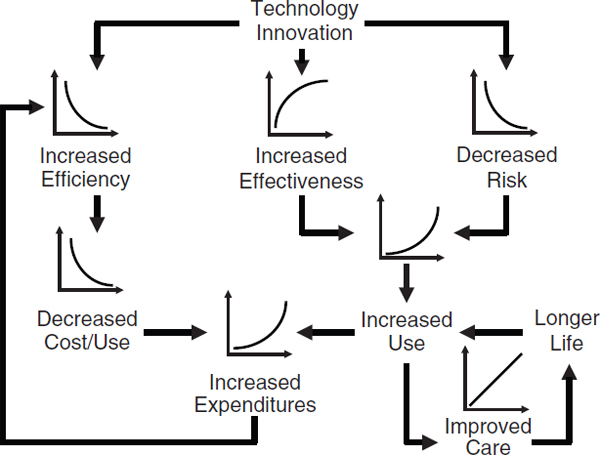
FIGURE 2-1 The dynamics of escalating healthcare costs.
creased use, which in turn leads to increased expenditures. In parallel, increased efficiency through production learning (discussed further below) leads to decreased cost per use, although not enough to keep pace with the product’s growing use in health care. Finally, increased use yields improved care, which leads to longer lives and increased chances of again employing the technology of interest.
The concern in this illustrative example is how to control the phenomenon depicted in Figure 2-1. In typical engineering fashion, we approach this control problem with a series of models, beginning with a very simple model and then elaborating as the limits of each model become clear.
Model 1: Growth
The first model considers what efficiencies are needed to counteract the growth in Figure 2-1. We start with a simple equation:
(1) Cost (1 − α) Use (1 + β) = Total (1 + δ),
where α is the annual rate of cost reduction, β is the annual rate of usage growth, and δ is the annual allowable total growth. A bit of algebra shows that the annual rate of cost reduction required is given by the following:
(2) α = (β − δ)/(β + 1).
Table 2-1 shows the cost reductions needed for five of the technologies discussed in the CBO report, assuming zero allowable growth. These are rather significant decreases. However, these decreases are more instructive than definitive because of the simplicity of the model. In particular, the model is quite limited in that it provides no mechanism for achieving cost reductions and does not differentiate between the various elements of the healthcare delivery process. Thus we need to elaborate on model 1.
Model 2: Learning
The second model considers production learning, a well-understood concept in industrial engineering (Hancock and Bayha, 1992). Quite simply, as one produces more of an item, one gets better at it, and unit costs decrease. In some industries, such as the semiconductor industry, these decreases are a primary source of profit margins. Many manufacturing industries employ production learning curves to predict costs and hence profits. The basic learning equation is given by
(3) Cost (t = T) = Cost (t = 0) No. Uses (t = T)-Rate.
This learning phenomenon is usually discussed in terms of “percent curves.” For example, a 70 percent curve means that after each doubling of the number of units produced, unit costs drop to 70 percent of what they were after the previous doubling. Table 2-2 provides a few examples of the rates required in equation (3) to achieve different percent curves.
TABLE 2-1 Cost Reductions Needed to Accommodate Growth
|
|
||
| Treatment | Annual Rate of Usage Growth (%) | Minimum Annual Rate of Cost Reduction (%) |
|
|
||
| Angiography | 10 | 9 |
| Angioplasty | 15 | 13 |
| Dialysis | 12 | 11 |
| Hip replacement | 10 | 9 |
| Knee replacement | 11 | 10 |
|
|
||
TABLE 2-2 Production Learning Parameters
|
|
|
| Percentage Cost Per Use for Each Doubling of Uses | Rate for Learning Model |
|
|
|
| 70 | 0.515 |
| 80 | 0.322 |
| 90 | 0.152 |
|
|
|
Most learning curves fall in the 70 to 90 percent range. This range reflects the experiences of many industries, including producers of airplanes, automobiles, and electronics. Curves below 70 percent are rare. As the results given below will show, controlling healthcare costs may require achieving significantly below 70 percent—a significant challenge.
Figure 2-2 shows learning curves for the three learning rates in Table 2-2, assuming a 10 percent annual rate of growth in usage. Note that the initial conditions were 100 uses at $100 per use, yielding an initial total expenditure of $10,000. Figure 2-3 shows the growth of total expenditures, again assuming a 10 percent annual growth in usage.
Table 2-3 shows the overall results for annual growth rates of 5 and 10 percent, assuming a 70 percent learning curve. Unit costs have dropped significantly, but the growth in usage has overwhelmed these efficiencies. Overall, this model exhibits impressive cost reductions from production learning, but it does not indicate where or how this learning happens. Furthermore, the model does not reflect the process whereby health care is delivered.
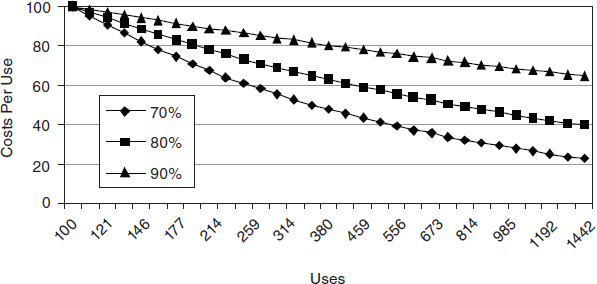
FIGURE 2-2 Learning curves for the three learning rates from Table 2-2.
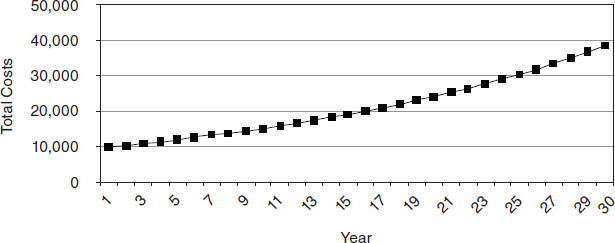
FIGURE 2-3 Expenditure growth at 10 percent annual growth in use.
TABLE 2-3 Impacts of Production Learning
|
|
|||
| Rate (%) | Results at 30 Years | ||
|
|
|||
| No. of Uses | Cost/Use ($) | Total Expenditures ($) | |
|
|
|||
| 5 | 412 | 48 | 19,874 |
| 10 | 1,586 | 24 | 38,256 |
|
|
|||
Model 3: Process
The third model explicitly considers the process by which healthcare service is provided. As shown in Figure 2-4, this process includes multiple stages and differentiates labor from technology. A rich experience base allows us to define the learning rates for technology. For present purposes we, somewhat optimistically, set the technology learning rate at 70 percent. The question then is, What labor learning rate is needed to control the growth in costs to an acceptable level? This model is given by the following equations:
(4) Cost (t) = Cost of Labor (t) + Cost of Technology (t),
(5) CTOT (t) = CPUL (t) NU (t) + CPUT (t) NU (t),
(6) CPUL (t) = CPUL (1) NU (t)-RateL,
(7) CPUT (t) = CPUT (1) NU (t)-RateT, and
(8) NU (t) = NU(1) (1 + β)t-1.
where CTOT, CPUL, and CPUT denote total costs, labor cost per unit, and technology cost per unit, respectively, while NU denotes number of units.
Figure 2-5 shows the efficiency required to control increases in health-
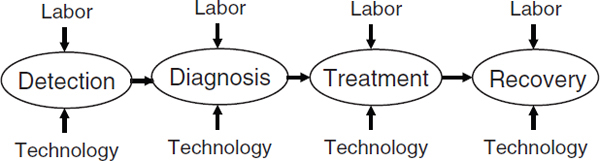
FIGURE 2-4 Service delivery process model.
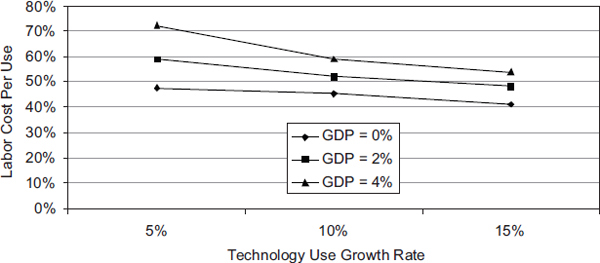
FIGURE 2-5 Required efficiency (% cost per use per doubling) for healthcare costs to track gross domestic product (GDP).
care costs to the point that they track increases in the GDP. The best case is for 4 percent GDP growth and 5 percent usage growth, which requires a learning curve of greater than 70 percent for labor. This magnitude of learning is imaginable. The worst case is for 0 percent GDP growth and 15 percent usage growth, which would require a learning curve of greater than 40 percent. This level of learning has never been achieved in any domain.
Implications
The implications of the results of these three models are quite clear. To limit the growth in total healthcare spending to the growth in GDP, some combination of the following three things is needed:
- Limit the growth of technology use.
- Limit the cost of technology use.
- Decrease the cost of labor associated with technology use.
Overall, the savings due to learning are the key to affordability. Achieving these savings will, however, be a significant challenge since learning rates of less than 70 percent are difficult to achieve.
Sources of Learning
In industries in which production learning curves have long been used, the sources of learning include labor efficiency, changes in personnel mix, standardization, specialization, method improvements, better use of equipment, changes in the resource mix, product and service redesign, and shared best practices. The Commonwealth Fund recently published recommendations for “bending the curve” (Schoen et al., 2008). Based on extensive economic analyses, the following are recommended as ways to reduce healthcare costs:
• Producing and using better information
− Promoting health information technology
− Center for medical effectiveness and healthcare decision making
− Patient shared decision making
• Promoting health and disease prevention
− Public health: reducing tobacco use
− Public health: reducing obesity
− Positive incentives for health
• Aligning incentives with quality and efficiency
− Hospital pay-for-performance
− Episode-of-care payment
− Strengthening of primary care and care coordination
− Limit on federal tax exemptions for premium contributions
• Correcting price signals in the healthcare market
− Resetting of benchmark rates for Medicare advantage plans
− Competitive bidding
− Negotiated prescription drug prices
− All-payer provider payment methods and rates
− Limit on payment rate updates in high-cost areas
The report Bending the Curve provides projections of the savings that could be realized by adopting these recommendations (Schoen et al., 2008).
Conclusions
This paper has illustrated an engineering approach to addressing the complex problem of escalating healthcare costs. Ironically, it has done so in the context of an engineering phenomenon, namely, the successful technology innovation that has led to growing markets and increased revenues. The problem in health care is that increasing revenues to innovators translate into increasing costs to payers. Such growth is viewed more favorably when individuals pay rather than when third parties pay.
It may be possible to devise market-based mechanisms to control the growth in demand. De facto rationing is also likely, although we do not like to talk about the use of this mechanism. The other primary mechanism, which was the main focus of this paper, is increasing system efficiency to lower supply costs and hence prices. Such efficiency is needed to ensure the affordability of technology innovations. Although the required improvements are substantial, the estimates of their magnitude provided here offer some guidance concerning how aggressive efficiency initiatives need to be.
In searching for efficiencies of this magnitude, it will be important to focus on the whole system (Rouse, 2008). Consider the architecture of healthcare delivery shown in Figure 2-6. The efficiencies that can be gained
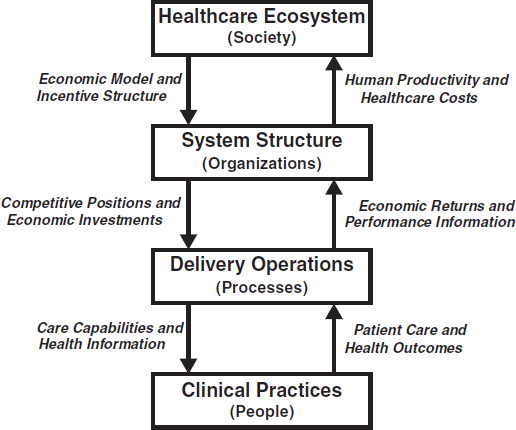
FIGURE 2-6 The architecture of healthcare delivery.
at the lowest level (clinical practices) are limited by the nature of the next level (delivery operations). For example, functionally organized practices are much less efficient than delivery that is organized around processes.
Similarly, the efficiencies that can be gained in operations are limited by the level above (system structure). Functional operations are driven by organizations structured around specialties, such as radiology. In addition, efficiencies in the system structure are limited by the healthcare ecosystem in which organizations operate. The experiences of other countries provide ample evidence of this.
The fee-for-service model central to U.S. health care ensures that provider income is linked to activities rather than to outcomes. The focus on disease and restoration of health rather than on wellness and productivity ensures that healthcare expenditures will be viewed as costs rather than investments. Recasting of “the problem” in terms of outcomes characterized by wellness and productivity may enable the identification and pursuit of efficiencies that cannot be imagined within our current frame of reference.
OPERATIONS RESEARCH FOR THE OPERATING ROOM AND MUCH MORE!
Richard C. Larson, Ph.D., Massachusetts Institute of Technology
The intent of this paper is to introduce the principles of OR to professionals in the healthcare community, with the goal of demystifying the OR approach by giving examples of its use in health care and elsewhere. As originally defined by OR cofounder Philip M. Morse, OR uses all aspects of the scientific method to help frame, formulate, and solve difficult operations problems involving people and technology. OR is a strong “systems-oriented” approach for use in developing learning healthcare systems.
Morse, a physicist at Massachusetts Institute of Technology (MIT), was the founder of OR in the United States in the late 1930s and early 1940s. Other physicists founded OR in Great Britain. According to the seminal book Methods of Operations Research, OR is an applied science that uses all known scientific techniques as tools to solve a specific problem (Morse and Kimball, 1951). It uses mathematics but is not a branch of mathematics, although the dominant mode in the OR field has become more mathematical. One of the ways in which OR can be most valuable is by offering an alternative and more insightful definition of the problem at hand.
At MIT I am at the junction of traditional OR and an emergent field called engineering systems. The way engineering systems are approached at MIT is to look at complex systems problems and put them in a box, framing them in such a way that it is possible to include all of their complexities—complexities that typically include issues from traditional en-
gineering as well as management issues and issues from the social sciences. To the extent feasible, the full complexity that exists at the intersection of those three disciplines is embraced. The healthcare system, however it is defined, has many such problems. From an OR perspective, what kinds of interventions are required?
Going back to Morse’s definition, OR requires multidisciplinary teams, not teams representing just one area or specialty. It also requires the development of an intimate knowledge of the operations in question, as well as a willingness and ability to invent new models and methods. Finally, we cannot simply pontificate from ivied buildings—we must get our boots on the ground.
OR of the 1940s and 1950s, in effect, evolved into the engineering systems of today. Those systems can bring many relevant applications to bear on health care. A special issue of OR’s flagship journal, Operations Research, was recently devoted entirely to such considerations. Similarly, a recent book, Operations Research in Healthcare: Handbook of Methods and Applications (Brandeau et al., 2004), has some 40 or 50 chapters devoted to different applications of OR in the healthcare sector.
There are many success stories that may not be widely known outside of the OR field, but these are success stories within the broader definition of the healthcare system. For example, Ed Kaplan, who happens to be a member of both the National Academy of Engineering and the Institute of Medicine, won the Edelman Prize in 1992 for his New Haven Health Department Study on clean-needle exchange (Kaplan and Heimer, 1992). As is now widely known, heroin addicts often share needles; if anyone in a group of addicts has an HIV infection, the probability of infecting the others is rather high. Kaplan applied fundamental OR probabilistic modeling techniques—some actually developed from the study of wildlife—to this problem. The equations were not elaborate, but the lateral thinking was very impressive. Kaplan’s results predicted a substantial reduction in the HIV/AIDS progression that occurred through the use of dirty needles if the government sponsored clean-needle exchanges. The city of New Haven adopted the approach, and studies suggest that the program reduced HIV/ AIDS incidence by 33 percent. This is an example of OR on the ground. Kaplan went into the field, talked with people who were involved in the system at all levels, and then applied some basic mathematical modeling techniques.
More recently, Marco Zaider from Memorial Sloan-Kettering Cancer Center and Eva K. Lee from the Georgia Institute of Technology School of Industrial and Systems Engineering and Health Systems Institute used OR to advance cancer therapeutics. Their team devised sophisticated optimization modeling and computational techniques to implement an intraoperative 3-dimensional treatment planning system for brachytherapy (the
placement of radioactive “seeds” inside a cancerous tumor) that offers a much safer and more reliable treatment. The system eliminates preoperation simulation and postimplant imaging, leading to savings of an estimated $459 million per year on the treatment of prostate cancer alone. Quality of life is improved through the use of treatment plans that deliver less radiation to healthy structures, which results in a drastic reduction (45 to 60 percent) in complications. This was a major application of OR at Georgia Tech, which also is well known for applying OR optimization techniques to airline crew and flight scheduling. More recently still, Kaplan and his colleague Larry Wein have received national acclaim for their OR-based ideas, presented in papers and in congressional testimony, on how best to respond to bioterrorism and its associated health risks.
The city of Stockholm was a 2008 finalist for the Edelman Prize for the project “Operations Research Improves Quality and Efficiency in Social Care and Home Help.” The program led to an annual savings of €20 million to €30 million ($30 million to $45 million) and improvement in the quality of home care provided to patients.
The Larson research group at MIT has used OR to assess a low-probability/high-consequence event: the possibility of a return of pandemic influenza of the magnitude of that seen in 1918 to 1919. The so-called Spanish flu, this pandemic had its genesis in Kansas and eventually killed roughly 50 million people worldwide (although the precise death count will never be known). Depending on how Bayesian one is, the probability of such a recurrence in any given year may be anywhere from 1 to 5 percent. If we are not prepared for such a pandemic worldwide, it has the potential to kill more people than a full nuclear exchange between two nuclear powers. There will be no way to cordon off boundaries. If such a pandemic strikes anywhere in the world, it will reach the United States with high probability. So it is a possibility well worth studying.
Basically, as with any respiratory infectious disease, the Spanish flu spread from person to person through face-to-face contact or by people touching contaminated objects. Today, states have responsibility for influenza prevention, with each state expected to prepare its own pandemic influenza plan. These plans were read and discussed at MIT, with 12 states being represented. One need only imagine 50 Hurricane Katrinas all happening at the same time, with each state left to cope on its own and with no expectation of federal aid. The goal of the Larson research group is to apply OR thinking, lateral thinking, and some creative thinking to determine the best ways to apply nonpharmaceutical interventions (NPIs) should an influenza pandemic occur. There is strong evidence that NPIs can greatly reduce the probability of infection should such a pandemic strike. Possible NPIs include various forms of social distancing, such as closing schools, which could be government mandated; personal choice, such as deciding to
telecommute or altering one’s shopping patterns; and hygienic behavioral changes, which can be something as simple, but important, as intensive hand washing.
Another object of study—again using probability models of OR—is one of the most popular and fundamental parameters in epidemiology: R0, which is defined as the mean number of new infections generated by a typical newly infected person in a fully susceptible population. If R0 is something like 2, for instance, a person who becomes infected with the disease will, before being isolated from the rest of the population, infect two more people on average. These two will cause the infection of four people, who will cause the infection of eight, and so on, doubling each generation. If the R0 is greater than 1, the number of infections will increase exponentially; if the R0 is less then 1, there will be a geometric decay in the number of infections.
The problem is that many in the medical community treat R0 as a constant of nature. They will say in a paper: consider an infectious respiratory disease where R0 equals 2.6003724, and we will work from there. Recent evidence suggests strongly that R0 can be decomposed into behavioral components, as is suggested in the following equation:
R0 = pλ.
That is, R0 equals p times λ, where λ is the frequency of daily contacts, and p is the probability of transmitting the infection, given contact. Seen this way, it is clear that the transmission parameter can be changed. Recent research has indicated that about 15 percent of the population has 4 or fewer face-to-face contacts per day. Another 15 percent of the population has 100 or more face-to-face contacts per day. Most of us have a value of λ that is between these extremes. The other parameter, p, represents the probability of giving the infection to someone—say, if I am infected and I shake your hand, what is the probability of giving it to you? Both λ and p are somewhat controllable by us, by our family members, and by our coworkers, and therefore we can influence R0. This was done in 2003 when severe acute respiratory syndrome struck Hong Kong and elsewhere, as members of the population drastically changed their behaviors.
There are many roads forward. Paul O’Neill’s article in OR/MS Today, “Why the U.S. Healthcare System Is So Sick and What OR Can Do To Cure It” (O’Neill, 2007), should be required reading for us all. Although additional research concerning how OR can improve the healthcare system is available, more is needed. Most notably, studies that connect OR and the social sciences (e.g., understanding how physicians and patients view uncertainty in healthcare delivery) could greatly expand the applicability of OR to healthcare improvement. Every day physicians and healthcare pro-
viders must make decisions based on many confounding factors. Doing so requires the calculation of conditional probabilities, something that is very difficult for most of us, not just physicians. Most people, including physicians, appear not to understand probability and risk as well as they should. A nice short read on the subject can be found in the book Complications: A Surgeon’s Notes on an Imperfect Science (Gawande, 2002).
Going forward, it is likely that the most transformative applications of OR and engineering systems to health care have not yet been identified, but we do need feet on the ground, and we cannot pontificate from our offices. One of the key issues can be summed up this way: Imagine that you or a loved one is in a hospital receiving treatment. In the spirit of Harry Truman, you might ask, “Where does the buck stop?” That is, who is in charge? What single individual assumes responsibility? Too often, decisions appear to be the responsibility of a committee, with the result that important decisions fall between the cracks.
ON DESIGNING AN INTEGRATED AND ADAPTIVE HEALTHCARE SYSTEM
Introduction
Health care can be considered a service system. In general, services are carried out with knowledge-intensive agents or components that work together as providers and consumers to create or coproduce value. Indeed, anyone performing the engineering design of a healthcare system must recognize that the system is a complex integration of human-centered activities that is increasingly dependent on information technology and knowledge. Like any service system, health care can be considered a combination or recombination of three essential components: people (characterized by behaviors, values, knowledge, etc.), processes (characterized by collaboration, customization, etc.), and products (characterized by software, hardware, infrastructures, etc.). Thus, a healthcare system is an integrated and adaptive set of people, processes, and products. It is, in essence, a system of systems whose objectives are to enhance its efficiency (leading to greater interdependency) and increase its effectiveness (leading to improved health). Integration occurs over the physical, temporal, organizational, and functional dimensions, while adaptation occurs over the monitoring, feedback, cybernetics, and learning dimensions. In sum, service systems such as health care are indeed complex, especially because of the uncertainties associated
with their human-centered aspects. Moreover, the system complexities can be dealt with only through methods that enhance system integration and adaptation. The purpose of this paper, then, is to highlight the critical importance of integration and adaptation when designing, operating, or refining a complex service system such as health care.
On Services
Before discussing a healthcare service system as an integrated system, an adaptive system, and a complex system, it is helpful to start by defining services and discussing their uniqueness, especially in contrast to goods. Some concluding insights are provided later.
As detailed by Tien and Berg (1995, 2003, 2006, 2007), the importance of the services sector cannot be overstated. This sector employs a large and growing percentage of workers in the industrialized nations. As reflected in Table 2-4, the services sector in the United States includes a number of large industries and accounts for 82.1 percent of total jobs, while the other 4 economic sectors (manufacturing, agriculture, construction, and mining), which together can be considered the physical “goods” sector, employ the remaining 17.9 percent. Health care, which employs 10.8 percent of the U.S. workforce, is, of course, one of the largest industries
TABLE 2-4 U.S. Employment, by Industry/Sector, 2006
|
|
||
| Industries | Employment (M) | Percentage |
|
|
||
| Trade, transportation, and utilities | 26.1 | 19.0 |
| Professional and business | 17.2 | 12.6 |
| Health care | 14.8 | 10.8 |
| Leisure and hospitality | 13.0 | 9.5 |
| Education | 13.0 | 9.5 |
| Government (except education) | 11.7 | 8.5 |
| Finance, insurance, and real estate | 8.3 | 6.1 |
| Information and telecommunication | 3.1 | 2.2 |
| Other | 5.4 | 3.9 |
| Services Sector | 112.6 | 82.1 |
| Manufacturing | 14.3 | 10.3 |
| Construction | 7.5 | 5.5 |
| Agriculture | 2.2 | 1.6 |
| Mining | 0.7 | 0.5 |
| Goods Sector | 24.7 | 17.9 |
| Total | 137.3 | 100.0 |
|
|
||
| SOURCE: Bureau of Labor Statistics, 2006. | ||
in the services sector. Yet, as Tien and Berg (2006) point out, engineering research and education do not reflect this distribution, as the majority of research is still manufacturing or hardware oriented, and degree programs are still offered mainly in those traditional disciplines that were established in the early 1900s. On the other hand, medical research and education are somewhat more sensitive to the services need of health care; for example, evidence-based protocols are becoming more prevalent in the practice of medicine. Nevertheless, Hipel and colleagues (2007) maintain that services research and education deserve more attention and support now that the computer chip, information technology, the Internet, and the “flattening of the world” (Friedman, 2005) have all combined to make services—and services innovation—the new engine for global economic growth.
What constitutes the services sector? It can be considered “to include all economic activities whose output is not a physical product or construction, is generally consumed at the time it is produced and provides added value in forms (such as convenience, amusement, timeliness, comfort or health) that are essentially intangible” (Quinn et al., 1987). Implicit in this definition is the recognition that services production and delivery are so integrated that they can be considered a single, combined stage in the services value chain, whereas the goods sector has a value chain that includes supplier, manufacturer, assembler, retailer, and customer. Alternatively, services can be viewed as knowledge-intensive agents or components that work together as providers and consumers to create or coproduce value (Maglio et al., 2006).
Unfortunately, the U.S. healthcare system is a good example of a people-intensive service system that is in disarray. It is the most expensive healthcare system in the world, yet it is among the least effective of any developed country; a minority of the population receives excellent care, while an equal minority receives inadequate care (NAE/IOM, 2005). This situation is not due to a lack of well-trained health professionals or to a lack of innovative technologies; rather, it exists because the U.S. healthcare system consists of a fragmented group of mainly small, independent providers driven by insurance companies focused on costs. Clearly it is, at best, a nonsystem (Rouse, 2008). The natural conclusion to draw is that an integrated and adaptive healthcare system must be designed and implemented, one that will involve the participation and support of a large number of stakeholders (consumers, doctors, hospitals, insurance companies, and so on). For example, patients will need to take increased responsibility for their own health care in terms of access to and use of validated information.
The remainder of this section focuses on three overarching influences. First, the emergence of electronic services is totally dependent on information technology; examples include financial services, banking, airline reservation systems, and consumer goods marketing. As discussed by Tien and Berg (2003) and detailed in Table 2-5, e-service enterprises interact or “co-
produce” with their customers in a digital medium (including e-mail and the Internet), as contrasted with the physical environment within which traditional or bricks-and-mortar service enterprises interact with their customers. Similarly, in contrast to traditional services delivered by low-wage earners, e-services typically employ high-wage earners and are more demanding in their requirements for self-service, transaction speed, and computation. With regard to data input that can be processed to produce information that, in turn, can be used to help make informed service decisions, it should be noted that both sets of services rely on multiple data sources; however, traditional services typically require homogeneous (mainly quantitative) data input, while e-services increasingly require nonhomogeneous (i.e., both quantitative and qualitative) data input. Paradoxically, the traditional service enterprises have been driven by data, although data availability and accuracy have been limited (especially before the pervasive use of the Universal Product Code and the more recent deployment of radio frequency location and identification [RFLID] tags). Likewise, the emerging e-service enterprises have been driven by information (i.e., processed data), although information availability and accuracy have been limited as a result of the current data rich, information poor (DRIP) conundrum (Tien, 2003).
Consequently, while traditional services—such as traditional manu-
TABLE 2-5 Comparison of Traditional and Electronic Services
|
|
||
| Service Enterprises | ||
|
|
||
| Issue | Traditional | Electronic |
|
|
||
| Coproduction medium | Physical | Electronic |
| Labor requirement | High | Low |
| Wage level | Low | High |
| Self-service requirement | Low | High |
| Transaction speed | Low | High |
| requirement | ||
| Computation requirement | Medium | High |
| Data sources | Multiple homogeneous | Multiple nonhomogeneous |
| Driver | Data driven | Information driven |
| Data availability/accuracy | Poor | Rich |
| Information | Poor | Poor |
| availability/accuracy | ||
| Economic consideration | Economies of scale | Economies of expertise |
| Service objective | Standardized | Personalized |
| Service focus | Mass production | Mass customization |
| Decision time frame | Predetermined | Real time |
|
|
||
facturing—are based on economies of scale and a standardized approach, e-services—such as electronic manufacturing—emphasize economies of expertise or knowledge and an adaptive approach. Another critical distinction between traditional and electronic services is that although all services require decisions to be made, decisions made in traditional services are typically based on predetermined decision rules, while e-services require real-time, adaptive decision making. It is for this reason that Tien (2003) advanced a decision informatics paradigm, one that relies on both information and decision technologies from a real-time perspective. High-speed Internet access, low-cost computing, wireless networks, electronic sensors, and ever-smarter software are the tools necessary for building a global services economy. Thus e-commerce, a sophisticated and integrated service system, combines product selection (i.e., selection of goods or services), order taking, payment processing, order fulfillment, and delivery scheduling into a seamless system, all provided by distinct service providers; in this regard, an electronic service system can be considered to be a system of different systems.
The second influence on services is their relationship to manufacturing. The interdependencies, similarities, and complementarities of services and manufacturing are significant. Indeed, many recent innovations in manufacturing are relevant to the service industries. Concepts and processes can, for the most part, be recast in terms that are relevant to services. These concepts and processes include cycle time, total quality management, quality circles, six-sigma design for assembly, design for manufacturability, design for recycling, small-batch production, concurrent engineering, just-in-time manufacturing, rapid prototyping, flexible manufacturing, agile manufacturing, distributed manufacturing, and environmentally sound manufacturing. Thus, many of the engineering and management concepts and processes employed in manufacturing can also be used to deal with problems and issues arising in the services sector.
Nonetheless, there are considerable differences between goods and services. Tien and Berg (2003) provide a comparison of the two sectors. The goods sector requires material as input, is physical in nature, involves the customer at the design stage, and employs mainly quantitative measures to assess its performance. By contrast, the services sector requires information as input, is virtual in nature, involves the customer at both the production and delivery stages, and employs mainly qualitative measures to assess its performance. Of course, even when there are similarities, it is critical that the coproducing nature of services be taken into consideration. For example, physical parameters, statistics of production, and quality can be quantified more precisely in the case of manufacturing; because a services operation depends on an interaction between the recipient and the process
TABLE 2-6 Services Vs. Manufactured Goods
|
|
||
| Focus | Services | Goods |
|
|
||
| Production | Coproduced | Preproduced |
| Variability | Heterogeneous | Identical |
| Physicality | Intangible | Tangible |
| Product | Perishable | “Inventoryable” |
| Objective | Personalizable | Reliable |
| Satisfaction | Expectation related | Utility related |
| Life cycle | Reusable | Recyclable |
| OVERALL | CHIPPER | PITIRUR |
|
|
||
of producing and delivering, the characterization is necessarily more subjective and different.
A more insightful approach to understanding and advancing services research is to consider explicitly the differences between services and manufactured goods. As shown in Table 2-6, services are, by definition, coproduced, they are quite variable or heterogeneous in their production and delivery, they are physically intangible and perishable if not consumed either as they are being produced or by a certain time (e.g., before a flight’s departure), they are focused on being “personalizable,” they are expectation related in terms of customer satisfaction, and they are reusable in their entirety. On the other hand, manufactured goods are preproduced, quite identical or standardized in their production and use, physically tangible, “inventoryable” if not consumed, focused on being reliable, utility related in terms of customer satisfaction, and recyclable with regard to their parts. In mnemonic terms and referring to Table 2-6, services can be considered to be “chipper,” while manufactured goods are a “pitirur.”
Although the comparison of services and manufacturing highlights some obvious methodological differences, it is interesting to note that, while physical manufactured assets depreciate with use and time, virtual service assets are generally reusable and may in fact increase in value with repeated use and over time. The latter assets are predominantly processes and associated human resources that build on the skill and knowledge base accumulated through repeated interactions with the service receiver, who is involved in the coproduction of the service. Thus, for example, a surgeon should improve over time, especially if the same type of surgery is repeated. Indeed, clinical productivity increases for the average physician from the dawn of a career to almost the end of a career, with a slight slowing toward the end. Likewise, while most U.S. physicians practice at a financial loss during the first few years of their career, they progressively improve their financial standing.
In services, automation-driven software algorithms have transformed
human resource−laden, coproducing service systems into algorithm-laden, self-producing services. Thus, extensive manpower would be required to coproduce the services manually if automation were not available. Although automation has certainly improved productivity and decreased costs for some services (e.g., telecommunications and Internet commerce), it has not yet had a similar effect on other labor-intensive services, such as health care. With new multimedia and broadband technologies, however, some hospitals are personalizing their treatment of patients, including by sharing patients’ electronic records. As a result, patients can take increased responsibility for their own health care.
A third critical influence on services is the computation-driven move toward mass customization. Customization implies meeting the needs of a customer market that is partitioned into an appropriate number of segments, each with similar needs (e.g., Amazon.com targets its marketing of a new book to an entire market segment if several members of the segment act to acquire the book). Mass customization implies meeting the needs of a segmented customer market, with each segment being a single individual (e.g., a tailor who laser scans an individual’s upper torso and then delivers a uniquely fitted jacket). Real-time mass customization implies meeting the needs of an individualized customer market on a real-time basis (e.g., a tailor who laser scans an individual’s upper torso and then delivers a uniquely fitted jacket within a reasonable period, while the individual is waiting).
It is interesting to note that, with regard to customization and relative to the late 1700s, the United States is in some respects going “back to the future”; that is, advanced technologies are not only empowering the individual but also allowing for individualized or customized goods and services. For example, e-education reflects a return to individual-centered learning (Tien, 2000), much like the home schooling of a previous century. Moreover, when mass customization occurs, it is difficult to say whether a service or a good is being delivered; that is, a uniquely fitted jacket can be considered to be a coproduced service/good or “servgood.” The implication of real-time mass customization, then, is that the resultant coproduced servgood must be carried out locally, although the intelligence underpinning the coproduction could be residing at a distant server and delivered like a utility. Thus, while most manufacturing jobs have already been relocated overseas (with only 10.3 percent of all U.S. employees still involved in manufacturing), and while service jobs (82.1 percent of all U.S. jobs) are beginning to be relocated overseas, real-time mass customization should help stem if not reverse the job outflow trend. In this regard, real-time mass customization should be viewed as a matter of national priority.
Clearly, health care needs to transition from being a traditional (although high-wage) to an electronic-based service industry, relying on digital media for such activities as real-time access to patient data. (Some digitally
based medical approaches need further assessment and improvement. Although robotic surgery is quite helpful in the repair of small nerves and blood vessels, for example, its overall efficacy is still under debate. Nevertheless, as robotic surgery is further refined, it will undoubtedly become a standard technique.) Additionally, health care must adopt some of the methods that have made manufacturing efficient (e.g., reduced cycle time and improved quality) while focusing on service effectiveness (e.g., maintaining a high standard of coproduction and meeting consumer expectations). Most important, health care must be adaptive and customize treatments to the needs of patients, with treatments ranging from evidence-based protocols to servgood or personalized therapies.
On Integration
As indicated earlier, a service system such as health care is actually an integration or combination of three essential components—people, processes, and products. The people in a service system can be grouped into those demanding services (consumers, users, patients, buyers, organizations, etc.) and those supplying the services (suppliers, providers, clinicians, servers, sellers, organizations, etc.). Similarly, processes can be procedural (standardized, evolving, decision focused, network oriented, etc.) or algorithmic (data mining, decision modeling, systems engineering, etc.) in structure, or sometimes both. And products can be physical (facilities, sensors, information technologies, etc.) or virtual (e-commerce, simulations, e-collaboration, etc.) in form.
Given the coproducing nature of services, it is obvious that people make up the most critical element of a service system. In turn, because people are so unpredictable in their values, behaviors, attitudes, expectations, and knowledge, they invariably increase the complexity of a service system. Moreover, the multistakeholder—and related multiobjective—nature of such systems serves only to intensify the complexity level and may ultimately result in the system’s being indefinable, if not unmanageable. Human performance, social networks, and interpersonal interactions combine to further aggravate the situation. People-oriented, decision-focused methods are considered in a later section.
Processes that underpin system integration include standards, procedures, protocols, and algorithms. By combining or integrating service processes, one could, for example, enhance a “one-stop shopping” approach, a highly desirable situation for the consumer or customer. Integration of financial services has resulted in giant banks (e.g., Citigroup), integration of home-building goods and services has resulted in super stores (e.g., Home Depot), and integration of software services has resulted in complex software packages (e.g., Microsoft Office). Integration also enhances
system efficiency, if not effectiveness. For example, the RFLID tag—a computer chip with a transmitter—serves to integrate the supply chain.
Service-related products can be grouped into two categories. First are those physical products or goods (e.g., cars, aircraft, satellites, computers) that, as indicated earlier, enable the delivery of effective and high-quality services (e.g., road travel, air travel, global positioning, electronic services). Second are more virtual products or services, including e-commerce.
More important, and as detailed in Table 2-7, service system integration can occur over many different dimensions, including physical, temporal, organizational, and functional. Physical integration can be defined by the degree of systems collocation in the natural (e.g., closed, open, hybrid), constructed (e.g., goods, structures, systems), or virtual (e.g., services, simulation, e-commerce) environment. An urban center’s infrastructures (e.g., emergency services, health services, financial services) are examples
TABLE 2-7 System Integration: Dimensions
|
|
|||
| Dimension | Definition | Characteristics | Elements |
|
|
|||
|
Physical |
Degree of systems collocation |
Natural |
Closed; open; hybrid |
|
Constructed |
Goods; structures; systems |
||
|
Virtual |
Services; simulation; e-commerce |
||
|
Temporal |
Degree of systems cotiming |
Strategic |
Analytical; procedural; political |
|
Tactical |
Simulation; distribution; allocation |
||
|
Operational |
Cognition; visualization; expectation |
||
|
Organizational |
Degree of systems comanagement |
Resources |
People; processes; products |
|
Economics |
Supply; demand; revenue |
||
|
Management |
Centralized; decentralized; distributed |
||
|
Functional |
Degree of systems cofunctioning |
Input |
Location; allocation; reallocation |
|
Process |
Informatics; feedback; control |
||
|
Output |
Efficiency; effectiveness |
||
|
|
|||
of a constructed environment. Over time, and with advances in information technology and in response to the need for improved efficiency and effectiveness, these infrastructures have become increasingly automated and interlinked, or interdependent. In fact, because the information technology revolution has changed the way business is transacted, the government is operated, and national defense is conducted, President George W. Bush (2001) singled it out as the most critical infrastructure to protect following the terrorist attacks of September 11. Thus, while the United States is considered a superpower because of its military strength and economic prowess, nontraditional attacks on its interdependent and cyber-underpinned infrastructures could significantly harm both the nation’s military power and its economy. Clearly, infrastructures, especially the information infrastructure, are among the nation’s weakest links; they are vulnerable to various attacks, from willful acts of sabotage to invasions of privacy. Recent technological advances toward imbuing infrastructures with “intelligence” make it increasingly feasible to address the safety and security issues, allowing for the continuous monitoring and real-time control of critical infrastructures.
Temporal integration can be defined by the degree of systems cotiming from a strategic (e.g., analytical, procedural, political), tactical (e.g., simulation, distribution, allocation), and operational (e.g., cognition, visualization, expectation) perspective. Expectation, for example, is a critical temporal issue in the delivery of services. More specifically, because services are to a large extent subject to customer satisfaction and because—as Tien and Cahn (1981) postulated and validated—“satisfaction is a function of expectation,” service performance or satisfaction can be enhanced through the effective management of expectation. With respect to health care, however, it may be difficult, if not impossible, to manage a patient’s expectation under certain emergency or competitive situations.
Organizational integration can be defined as the degree of systems comanagement of resources (e.g., people, processes, products), economics (e.g., supply, demand, revenue), and management (e.g., centralized, decentralized, distributed). With regard to management integration, Tien and colleagues (2004) provide a consistent approach to considering the management of both goods and services—first by defining a value chain and then by showing how it can be partitioned into supply and demand chains, which in turn can be appropriately managed. Of course, the key purpose of the management of supply and demand chains is to smooth out the peaks and valleys commonly seen in many supply and demand patterns. Moreover, real-time mass customization occurs when supply and demand chains are simultaneously managed. The shift in focus from mass production to mass customization (whereby a service is produced and delivered in response to a customer’s stated or imputed needs) is intended to provide
superior value to customers by meeting their unique needs. It is in this area of customization—where customer involvement is not only at the goods design stage but also at the manufacturing or coproduction stage—that services and manufacturing are merging in concept (Tien and Berg, 2006), resulting in the above-mentioned servgood.
Functional integration can be defined as the degree of systems cofunctioning with respect to input (e.g., location, allocation, reallocation), process (e.g., informatics, feedback, control), and output (e.g., efficiency, effectiveness). From an output perspective, for example, it is obvious that a system should act to enhance efficiency and effectiveness, the twin pillars of productivity. However, it should be noted that manufactured goods are primarily a result of an efficient supply chain, while services are primarily a result of an effective demand chain.
Again, health care—as a service system—must be integrated with regard to people, processes, and products, as well as over the physical, temporal, organizational, and functional dimensions. Designing an efficient and effective healthcare system will not be easy; socialistic systems like Sweden’s cost too much, while capitalistic systems like those in the United States both have high cost and are unfair. New design approaches are required. The information technology revolution has permitted the analysis element of system design to be carried out largely by computers; it allows a simulated and collaborative redesign process to occur until a satisfactory design that meets specified performance (e.g., morbidity, mortality, cost) criteria is achieved. The resulting integrated healthcare system will be a comprehensive, interoperable system of systems.
On Adaptation
Because a service system is, by definition, a coproducing system, it must be adaptive. Adaptation is a uniquely human characteristic, based on a combination of three essential components: decision making, decision informatics, and human interface. (Indeed, designing a healthcare system is essentially an exercise in making decisions or choices about the system’s characteristics or attributes.) Figure 2-7 provides a framework for decision making. To begin, it is helpful to clarify the difference between data and information, especially from a decision-making perspective. Data represent basic transactions captured during operations, while information represents processed data (e.g., derivations, groupings, patterns). Clearly, except for simple operational decisions, decision making at the tactical or higher levels requires, at a minimum, appropriate information or processed data. Figure 2-7 also identifies knowledge as processed information (together with experiences, beliefs, values, cultures, etc.) and wisdom as processed knowledge (together with insights, theories, etc.). Thus, strategic decisions
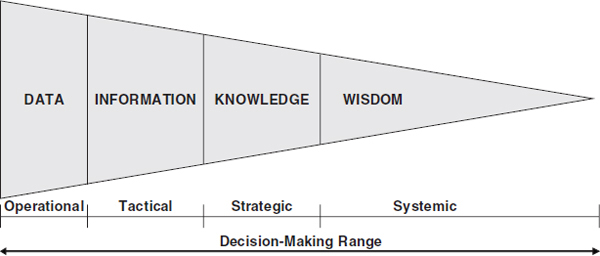
FIGURE 2-7 System adaptation: decision-making framework.
can be made with knowledge, while systemic decisions can be made with wisdom. Unfortunately, for the most part the literature does not distinguish between data and information. Economists claim that because of the astounding growth in information—really, data—technology, the United States and other developed countries are now part of a global “knowledge economy.” Although electronic data technology has transformed large-scale information systems from being the “glue” that holds the various units of an organization together to being the strategic asset that provides the organization with its competitive advantage, the United States is far from having reached the level of a knowledge economy. In terms of a continuum of data, information, knowledge, and wisdom, the United States—as well as other advanced economies—is, at best, at the beginning of a DRIP conundrum, as identified earlier.
The fact remains that data—both quantitative and qualitative—need to be fused and analyzed effectively and efficiently to provide the information needed for informed or intelligent decision making with regard to the design, production, and delivery of goods and services, including health care. As depicted in Figure 2-8, the nature of the necessary real-time decision (regarding the production or delivery of a service) determines, where appropriate and from a systems engineering perspective, the data to be collected (possibly, from multiple, nonhomogeneous sources) and the real-time fusion and analysis to be undertaken to obtain the needed information for input to the modeling effort. The modeling effort, in turn, provides the knowledge needed to identify and support the required decision in a timely manner. Clearly, methods must be developed that can fuse and analyze a steady stream of nonhomogeneous (i.e., quantitative and qualitative) data, and this is especially true for health care, where quantitative data
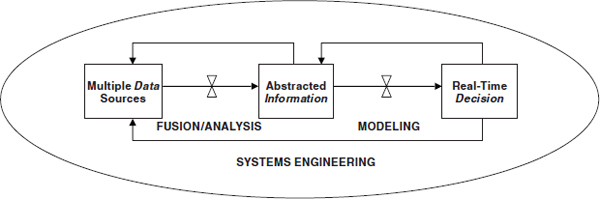
FIGURE 2-8 System adaptation: a decision informatics paradigm.
from monitoring devices must be complemented with patients’ qualitative assessments before clinicians can recommend appropriate treatment. The feedback loops in Figure 2-8 are within the context of systems engineering; they serve to refine the analysis and modeling steps.
Continuing with the decision informatics paradigm in Figure 2-8, it should be noted that decision modeling includes the information-based modeling and analysis of alternative decision scenarios. They include OR, decision science, computer science, and industrial engineering. At present, decision-modeling methods suffer from two shortcomings. First, most of the available methods—especially optimization—are applicable only in a steady-state environment, whereas in the real world all systems are in transition. (Note that steady state, like average, is an analytical concept that allows for a tractable, if not always manageable, analysis.) Second, most of the available methods are unable to cope with changing circumstances. We need methods that are adaptive so decisions can be made in real time, as is required in most healthcare situations. Thus, non-steady-state and adaptive decision methods are required. More important, real-time decision modeling requires more than simply speeding up the models and solution algorithms; like real-time data fusion and analysis, it also requires additional research and development.
The systems engineering methods implicit in Figure 2-8 concern the integration of people, processes, and products from a systems perspective; they include electrical engineering, human−machine systems, system performance, and system biology. Again, the real-time nature of coproducing services—especially human-centered services that are computationally intensive and intelligence oriented—requires a real-time systems engineering approach. Ethnography, a branch of anthropology that can help identify a consumer’s unmet needs, is being used to identify breakthrough products and service innovations. Another critical aspect of systems engineering is system performance, which provides an essential framework for assessing
the decisions made in terms of such issues as satisfaction, convenience, privacy, security, equity, quality, productivity, safety, and reliability. Similarly, undertaking systems engineering within a real-time environment will require additional thought and research.
The human interface is another essential element of an adaptive service system; it is actually a critical tool in systems engineering. Such interfaces include the interactions between and among humans and software agents, machines, subsystems, and systems of systems. The discipline of human factors deals with many of these interactions. However, another critical interface arises from the interaction of humans with data and information. In developing appropriate human–information interfaces, one must pay careful attention to a number of factors. First, human–information interfaces are a part of any decision support model; they determine the manner in which the model output or information is provided to the decision maker. Cognition represents the point of interface between the human and the information presented. The presentation must enhance the cognitive process of mental visualization and must be capable of creating images from complex multidimensional data, including structured and unstructured text documents, measurements, images, and video. Second, constructing and communicating a mental image common to a team of, say, clinicians and nurses could facilitate collaboration and could lead to more effective decision making at all levels, from operational to tactical to strategic. Nevertheless, cognitive facilitation is especially necessary in operational settings that are under high stress. Third, cognitive modeling and decision making must combine machine learning technology with a priori knowledge in a probabilistic data-mining framework to develop models of, say, a nurse’s tasks, goals, and objectives. These user-behavior models must be designed to adapt to an individual decision maker in order to promote better understanding of the needs and actions of the individual, including adversarial behaviors and intents.
More important and as detailed in Table 2-8, service system adaptation can occur in the monitoring, feedback, cybernetics, and learning dimensions. Monitoring adaptation can be defined by the degree of sensed actions with regard to data collection (e.g., sensors, agents, swarms), data analysis (e.g., structuring, processing, mining), and information abstraction (e.g., derivations, groupings, patterns). Data are acquired by sensors, which can be in the form of humans, robotic networks, aerial images, radio frequency signals, and other measures and signatures. When working with patients, for example, sensors that monitor the patients’ vital signs are essential, as are verbal inputs from the patients themselves. More recently, data warehouses have been proliferating, and data mining techniques have been gaining popularity. However, regardless of how large a data warehouse is and how sophisticated a data mining technique is, problems can occur if
TABLE 2-8 System Adaptation: Dimensions
|
|
|||
| Dimension | Definition | Characteristics | Elements |
|
|
|||
|
Monitoring |
Degree of sensed actions |
Data collection |
Sensors; agents; swarms |
|
Data analysis |
Structuring; processing; mining |
||
|
Information abstraction |
Derivations; groupings; patterns |
||
|
Feedback |
Degree of expected actions |
Standardized |
Prestructured; preplanned |
|
Procedural |
Policies; standard operating procedures |
||
|
Algorithmic |
Optimized; Bayesian |
||
|
Cybernetic |
Degree of reactive actions |
Deterministic |
Known states; deterministic actions |
|
Dynamic |
Known state distributions; dynamic actions |
||
|
Adaptive |
Unknown states; adaptive actions |
||
|
Learning |
Degree of unstructured actions |
Cognition |
Recognition based; behavioral |
|
Evidence |
Information based; genetic |
||
|
Improvisation |
Experience based; evolutionary |
||
|
|
|||
the data do not possess the desirable attributes of measurability, availability, consistency, validity, reliability, stability, accuracy, independence, robustness, and completeness.
Moreover, in most situations, data alone are useless unless access to and analysis of the data occur in real time. When developing real-time, adaptive data processors, one must consider several critical issues. First, as shown in Figure 2-8, these data processors must be able to combine (i.e., fuse and analyze) streaming data from sensors and other appropriate input from knowledge bases (including output from tactical and strategic databases) in order to generate information that can serve as input to operational decision support models or provide the basis for making informed decisions. Second, as also shown in Figure 2-8, the types of data collected and the ways in which the data are processed must depend on what decision is to
be made; these dependencies highlight the difficulty of developing effective and adaptive data processors or data miners. Furthermore, once a decision has been made, it may constrain subsequent decisions, which in turn may change future data requirements and information needs. Third, inasmuch as the data processors must function in real time and be able to adapt to an ongoing stream of data, genetic algorithms, which have equations that can mutate repeatedly in an evolutionary manner until a solution emerges that best fits the observed data, are becoming the tools of choice in this area.
Feedback adaptation can be defined by the degree of expected actions based on standardized (e.g., prestructured, preplanned), procedural (e.g., policies, standard operating procedures), and algorithmic (e.g., optimized, Bayesian) approaches. In general, different models underpin these approaches. As an example, Kaplan and colleagues (2002) developed a set of complex models to demonstrate that the best prevention approach to a smallpox attack would be to undertake immediate and widespread vaccination. Unfortunately, models, including simulations, that deal with multiple systems are still relatively immature and require additional research and development. Such system of systems models are quite complex and require a multidisciplinary approach.
Cybernetic adaptation can be defined by the degree of reactive actions that can be deterministic (i.e., known states, deterministic actions), dynamic (e.g., known state distributions, dynamic actions), or adaptive (e.g., unknown states, adaptive actions). Cybernetics is derived from the Greek word “kybernetics,” which refers to a steersman or governor. Within a system, cybernetics is concerned with feedback (through evaluation of performance relative to stated objectives) and control (through communication, self-regulation, adaptation, optimization, and management). Thus, cybernetic adaptation refers to actions that are undertaken based on an assessment of the feedback signals, with the corrective steps taken to modify the system so as to achieve the desired system objectives. A system is defined by state variables that are known in a deterministic manner (resulting in deterministic feedback or cybernetic actions), that are known in a probabilistic or distributional manner (resulting in dynamic feedback or cybernetic actions), or that are unknown (resulting in adaptive feedback or cybernetic actions). For example, autopilots—which are programmed to deal with deterministic and dynamic situations—can, for the most part, take off, fly, and land a plane, yet two human pilots are usually in the plane as well in case an unknown state occurs and the adaptive judgment of a human is required. Clearly, a trained human—such as a clinician or surgeon—remains the most adaptive controller, although machines are becoming more “intelligent” through adaptive learning algorithms.
System control is perhaps the most critical challenge facing system of systems designers. Because of the difficulty, if not impossibility, of devel-
oping a comprehensive solid-on-solid (SoS) model, either analytically or through simulation, SoS control remains an open problem and is, of course, uniquely challenging for each application domain. Moreover, real-time control of interdependent systems—which is required in nearly all application domains—poses an especially difficult problem. The cooperative control of an SoS assumes that it can be characterized by a set of interconnected systems or agents with a common goal. Classical techniques of control design, optimization, and estimation could be used to create parallel architectures for, as an example, coordinating numerous sensors. However, many issues that involve real-time cooperative control have not been addressed, even in non-SoS structures. For example, one issue concerns the control of an SoS in the presence of communication delays to and among the SoS subsystems.
Finally, learning adaptation can be defined by the degree of unstructured actions based on cognition (e.g., recognition based, behavioral), evidence (e.g., information based, genetic), and improvisation (e.g., experience based, evolutionary). Learning adaptation is mainly about real-time decision making at the operational level. In such a situation and as indicated earlier, the issue is not simply how to speed up steady-state models and their solution algorithms; indeed, steady-state models become irrelevant in real-time environments. Instead, learning adaptation concerns reasoning under both uncertainty and severe time constraints. In developing operational decision support models, one must recognize several critical issues. First, in addition to defining what data to collect and how they should be fused and analyzed, decisions will drive what kind of models or simulations are needed. These operational models are, in turn, based on abstracted information and output from tactical and strategic decision support models. The models must capture changing behaviors and conditions and be responsive within the changing environment, usually through the use of Bayesian networks. Second, most adaptive models are closely aligned with evolutionary models, also known as genetic algorithms, so they function in a manner similar to biological evolution or natural selection. In recent years, computationally intensive evolutionary algorithms have been used to develop sophisticated, real-time pricing schemes to minimize traffic congestion (Sussman, 2008), to enhance autonomous operations in unmanned aircraft, and to determine sniper locations in modern warfare (e.g., in Iraq). Third, computational improvisation is another operational modeling approach that can be employed when one cannot predict and plan for every possible contingency. (Indeed, much of what happened on September 11 was improvised, based on the ingenuity of the responders.) Improvisation involves learning by reexamining and reorganizing past knowledge in time to meet the requirements of an unexpected situation; it may be conceptualized as a search-and-assembly problem that is influenced by such factors
as the time available for planning, the prevailing risk, and the constraints imposed by prior decisions (Mendonca and Wallace, 2004).
Again, health care as a service system must be adaptive with regard to decision making, decision informatics, and human interfaces, as well as with regard to the monitoring, feedback, cybernetics, and learning dimensions. At all levels of healthcare decision making, a spectrum of possible methods can be used, ranging from adaptive—instead of randomized—medical trials to autonomous control and from virtual-touch tools to genetic algorithms, all of which are able to cope with imprecision, uncertainties, and partial truth (Zadeh, 1996). Moreover, the methods can be used to process information, take changing conditions into account, and learn from the environment; thus, they are adaptive and, to a large extent, responsive to a data stream of real-time input. In a fully integrated and adaptive system of systems, each system must be able to communicate and interact with the entire SoS, with no compatibility issues.
On Complexities
Service systems are indeed complex, requiring both integrative and adaptive approaches to deal with their complexity. There are a number of ways to characterize the complexity of a system (Rouse, 2007), especially a service system. Table 2-9 lists seven system stages that characterize the complexity of a healthcare service system and for which integrative and adaptive methods are required to mitigate, if not handle, the complexity.
The first stage, the system’s purpose, is difficult to define given the many stakeholders (patients, clinicians, insurers, etc.) involved, the multiple objectives (wellness care, emergency care, acute care, etc.) of each stakeholder, and the overarching business model (revenues, expenditures, endowments, etc.). Combining these divergent viewpoints into a consistent and viable purpose is an almost impossible task. The second stage, the system’s boundary, is, at best, ill defined and shifting; the spatial (offices, clinics, hospitals, etc.), temporal (schedules, activities, resources, etc.), and interdependent (infrastructures, supply chains, demand chains, etc.) relationships are difficult to determine. Third, the system’s design must be robust (to ensure reliability, quality, integrity, etc.), efficient (to minimize cost, inventory, waste, etc.), and effective (to maximize usefulness, satisfaction, pervasiveness, etc.). Fourth, the system’s development must be based on models (gedanken experiments, simulations, networks, etc.), scalability (multiscale, multilevel, multitemporal, etc.), and sustainability (over time, space, culture, etc.). Fifth, the system’s deployment must be with minimal risk (measured by morbidity, comorbidity, mortality, etc.), uncertainty (unexpected attitudes, behaviors, performances, etc.), and unintended consequences (delays, bad side effects, deteriorating vital signs, etc.). Sixth, the system’s operation
TABLE 2-9 Complex Service Systems: Healthcare Considerations
|
|
|||
| System Stages | Healthcare System Considerations | Critical Methods | |
|
|
|||
| Integrative | Adaptive | ||
|
|
|||
| 1. Purpose | Stakeholders; triaging; business model | ✓ | ✓ |
| 2. Boundary | Spatial; temporal; interdependent | ✓ | ✓ |
| 3. Design | Robust; efficient; effective | ✓ | ✓ |
| 4. Development | Models; scalability; sustainability | ✓ | ✓ |
| 5. Deployment | Risk; uncertainty; unintended consequences | ✓ | ✓ |
| 6. Operation | Flexible; safe; secure | ✓ | ✓ |
| 7. Life cycle | Predictable; controllable; evolutionary | ✓ | ✓ |
|
|
|||
must be flexible (agile, transparent, redundant, etc.), safe (with minimal natural accidents, human failures, unforeseen disruptions, etc.), and secure (with minimal system viruses, system crashes, privacy intrusions, etc.). Seventh, the system’s life cycle must be predictable (with regard to inputs, processes, outcomes, etc.), controllable (with appropriate sensors, feedback, cybernetics, etc.), and evolutionary (with learning capabilities, timely recoveries, intelligent growth, etc.).
Although Table 2-10 shows only a simple two-by-two, supply-vs.-demand matrix (Tien et al., 2004), it provides important insight into supply chain management (SCM, which can occur when demand is fixed and supply is flexible and therefore manageable), demand chain management (DCM, which can occur when supply is fixed and demand is flexible and therefore manageable), and real-time customized management (RTCM, which can occur when both demand and supply are flexible, thereby allowing for real-time mass customization).
Table 2-10 identifies example SCM, DCM, and RTCM methods. The literature offers abundant SCM findings (especially concerning manufacturing), only recently has focused on DCM methods (especially with regard to revenue management), and is devoid of RTCM considerations, except for a recent contribution by Yasar (2005). Yasar combines two SCM methods (capacity rationing and capacity extending) and two DCM methods (demand bumping and demand recapturing) to deal with the real-time customized management of, as examples, either a goods problem concerned with the rationing of equipment to produce classes of goods or a services
TABLE 2-10 Complex Service Systems: Integration/Adaptation Research
|
|
||
| Demand | ||
|
|
||
| Supply | Fixed | Flexible |
|
|
||
| Fixed | Unable to Manage | Demand Chain Management |
|
|
||
| Price established (at point where fixed demand matches fixed supply) | Product revenue management | |
| Dynamic pricing | ||
| Target marketing | ||
| Expectation management | ||
| Auctions | ||
| Flexible | Supply Chain Management | Real-Time Customized Management |
|
|
||
| Inventory control | Customized bundling | |
| Production scheduling | Customized revenue management | |
| Distribution planning | Customized pricing | |
| Capacity revenue management | Customized modularization | |
| Reverse auctions | Customized coproduction systems | |
|
|
||
problem concerned with the rationing of consultants to coproduce classes of services. More important, Yasar shows that the combined, simultaneous real-time management of the two SCM and two DCM methods yields a significantly more profitable outcome than the tandem application of these two sets of methods. Moreover, real-time management requires a more sophisticated solution approach than the traditional steady-state approach.
It is in this fourth, RTCM quadrant of Table 2-10 that system integration (as reflected in the SCM methods) and system adaptation (as reflected in the DCM methods) are combined and dealt with simultaneously. Thus, a combined integration/adaptation research effort is synonymous with an RTCM activity, which can occur when both demand and supply are flexible and thereby allow for real-time mass customization. This fourth quadrant also highlights the complexity involved in designing a service system that is at once both integrated and adaptive. Clearly, health care is an example of such a complex system.
On Insights
A number of insights can be gleaned from an integrated and adaptive view of healthcare services. First, electronic medical records are the glue that should keep the healthcare system integrated and adaptive. Unfortunately, most medical records—including patient data, drug prescriptions, laboratory diagnostics, clinician reports, and body scans—are still in manual folders and as a consequence are difficult to access, fuse, and analyze.
Recently Microsoft and Google launched, respectively, HealthVault and Health for use by consumers to store and manage their personal medical data online. Although patients have a legal right to obtain their medical records from doctors, hospitals, and testing laboratories, doing so is a tedious and overwhelming process because the records are usually not in electronic form. Nevertheless, sharing such electronic records with new medical providers and third-party services will make it easier to coordinate care, spot adverse drug interactions, allow for medication reminders, and track vital signs. At the same time, however, personal data residing on Microsoft or Google servers raise significant privacy concerns. At present, the Health Insurance Portability and Accountability Act (HIPAA) only requires doctors, hospitals, and third-party payers not to release information without a patient’s consent. Of course, HIPAA requirements could be broadened, and new rules could be enacted that would give consumers stronger protection and legal recourse if their records were leaked or improperly shared for purposes other than those intended.
Second, because real-time healthcare decisions must be made in an accelerated and coproduced manner, the human service provider (e.g., clinician) will increasingly become a bottleneck; he or she must be supported by a smart robot or software agent. For example, anyone could make use of a smart alter ego or agent that could analyze, and perhaps fuse, all existing and incoming e-mails, phone calls, Web pages, news clips, drug prescriptions, and stock quotes and then assign each item a priority based on the individual’s preferences and observed behaviors. Such a smart agent should be able to analyze a text message, judge the sender–recipient relationships by examining an organizational chart, and recall the urgency of the recipient’s responses to previous messages from the same sender. The agent might add information gathered by watching the user via a video camera or by scrutinizing his or her calendar. Most likely, such a smart agent would be based on a Bayesian statistical model—capable of evaluating hundreds of user-related factors linked by probabilities, causes, and effects in a vast web of contingent outcomes—that could infer the likelihood that a given decision on the software’s part would lead to the user’s desired outcome. The ultimate goal is to judge when the user can safely be interrupted, with what kind of message, and via which device. In time, smart agents representing both providers and consumers will be the service coproducers; they will employ decision informatics techniques to accomplish their tasks. It should be noted that such smart agents may never be appropriate for certain situations, especially, for example, when nuanced patient behavior is critical or when a catastrophic surgical consequence is a possibility. Obviously, these situations require direct patient–doctor interaction or coproduction, perhaps assisted by smart agents that can help in the identification of alternative diagnoses and treatments.
Third, perhaps the best example of an integrated and adaptive service system is the evolving Web 2.0. It is built, centered on, and run by users. In other words, it is a social network for the integration—including collaboration and communication—of activities (eBay, Amazon.com, Wikipedia, Twitter, MySpace, Friendster, LinkedIn, Plaxo, Facebook, etc.), entertainment (Ning, Bebo, Second Life, World of Warcraft, etc.), and searches (Google, Yahoo, MSN.com, etc.). Unfortunately, the integrated Web, while a somewhat successful e-commerce platform, is unable to interpret, manipulate, or make sense of its content. On the other hand, with the encoding of Web pages in a semantic Web format, the evolving Web will make it possible for the above-mentioned smart or decision informatics−supported agents to undertake semantic analysis of user intent and Web content, to understand and filter their meaning, and to respond adaptively in light of user needs. The semantic Web, then, would be an ideal complex service system for which integration and adaptation would constitute the basis for its functionality. Several obstacles must be overcome before full functionality is reached, however. For example, semantic standards or ontologies—such as the Web Ontology Language—must be established to maintain compatible and interoperable formats; healthcare and financial services companies are now developing their own ontologies. Indeed, a healthcare SoS also needs a common ontology to allow new system components to be integrated appropriately into the SoS without a major effort so as to achieve higher capabilities and performance than would be possible with the components as stand-alone systems. Of course, the healthcare ontology must be transdisciplinary—beyond a single discipline—in scope.
Fourth, modern systems of systems are becoming increasingly more human centered, if not human focused, with products and services becoming more personalized or customized. Certainly coproduction of services implies the existence of a human customer, if not a human service provider. The implication is profound: a multidisciplinary approach must be employed for, say, health care, and it must include techniques from the social sciences (sociology, psychology, and philosophy) and management (organization, economics, and finance). As a consequence, researchers must expand their systems (i.e., holistic oriented), human (i.e., decision oriented), and cybernetic (i.e., adaptive oriented) methods to include and be integrated with those techniques that are beyond science and engineering. For example, higher patient satisfaction can be achieved not only by improving service quality, but also by lowering patient expectations. In essence, as stated by Hipel and colleagues (2007), systems, human, and cybernetics is an integrative, adaptive, and multidisciplinary approach to creative problem solving that takes into account stakeholders’ value systems and satisfies important societal, environmental, economic, and other criteria to enhance the decision-making process in designing, implementing, operating, and
maintaining a system or SoS so as to meet societal needs in a fair, ethical, and sustainable manner throughout the system’s life cycle.
Fifth, although this paper has focused primarily on designing an integrated and adaptive healthcare system (by employing a systems engineering approach), it should be noted that a number of other engineering approaches can be applied to health care and related biological issues. Grossman (2008) identifies several disruptive engineering innovations that could change the way health care is organized, paid for, and delivered, including precision diagnostics and therapies (i.e., evidence-based medicine), advances in information and communication technologies (i.e., personal health records), and new business models (i.e., overcoming the cottage-industry structure and the dysfunctional reimbursement and regulatory framework). Indeed, as identified in Table 2-11, every engineering discipline or technology has some potential applications to biology; a number of such “technobiology” examples—developed by applying technology-based techniques to biological problems—are cited and briefly described in the table. These examples highlight the technological focus. On the other hand, “biotechnology” is about applying biology-based techniques to technological problems; such techniques include neural networks, genetic algorithms, and systems biology.
Sixth, perhaps the most critical U.S. healthcare issue is the universal access of patients to health care. Payers—particularly private insurance companies—have nearly eliminated access of at-risk individuals to healthcare providers by not allowing these individuals to enroll in their insurance programs. (At the extreme, only very healthy and relatively young individuals are able to purchase private insurance.) Thus, a huge access problem is created for the uninsured, whose solution is to go to the emergency room, where treatment must be provided at no cost, when the illness is already severe and costly to treat. A vicious subsidization cycle ensues in which individual insurance premiums skyrocket, mainly to pay for the care of individuals who are at risk and unable to obtain insurance or who cannot afford an insurance premium. The application of systems engineering—a technobiology approach—to the U.S. healthcare system is required to equilibrate the insurance imbalance and make the system efficient and effective.
Seventh, a final insight concerns the customization or personalization of medical treatment through advances in genetics, proteomics, and metabolomics. Most common illnesses will eventually be preventable; the challenge is to know which prevention effort will be most effective for a given individual. Using markers of risk (e.g., gene variants, blood levels of a protein moiety) may allow for the targeting or personalization of preventive measures in a highly cost-effective way. In this way, humans can be sheltered from chronic illnesses and remain fully functional until an advanced age,
TABLE 2-11 Technobiology Examples
|
|
||
| Discipline | Examples | Scope |
|
|
||
|
Biomedical |
1. PillCam |
1. Can capture 50,000 images of possible gastrointestinal diseases |
|
2. Nerve stimulation |
2. Neurostimulator to treat migraine headaches, chronic back and leg pain, etc. |
|
|
3. Induced hypothermia |
3. Lowering of body temperature to 91.5 degrees to achieve faster healing and to stem harmful chemical reactions that occur when flow of oxygen is restored following cardiac arrest |
|
|
Chemical |
1. Tissues |
1. Regenerative medicine: engineering stem cells to create skin, muscle, bone, cartilage, fat, blood vessel, nerve, heart, liver, bladder, kidney, etc. |
|
2. Diagnostic |
2. Test that identifies gene variations that can predict Lou Gehrig’s disease, Parkinson’s, Alzheimer’s, etc. |
|
|
3. Microcyn |
3. Electronically charged, super1-oxidized, water-based solution that attacks proteins in infectious agents of a wound, reducing need for antibiotics |
|
|
Electrical |
1. Bioimaging: VCT XT (low dose) computed tomography |
1. A 70 percent lower-radiation, 3-dimensional, high-resolution image that can be manipulated |
|
2. Robotic |
2. Automated assistance in surgery, walking, moving, etc. |
|
|
3. Bioinformatics |
3. Large-scale analysis of data for biological purposes, including drug discovery, patient treatment, etc. |
|
|
Environmental |
1. Sunshine vitamin |
1. Sunlight spurs body’s production of vitamin D, which may reduce instances of cancer, autoimmune disease, high blood pressure, heart disease, and diabetes |
|
2. Hearing pill |
2. Naturally occurring substance called N-acetylcysteine helps prevent hearing loss due to loud noise by helping the body promote reduced conformation of glutathione |
|
|
|
||
| Discipline | Examples | Scope |
|
|
||
|
Industrial |
1. Evidence-based protocols, including false discovery rate |
1. Data mining and analysis of past treatments can point to effective protocols, including minimization of false positives linking diseases and DNA genes |
|
2. Adaptive clinical trials |
2. Design and success criteria adjusted as clinical results are obtained |
|
|
3. E-care |
3. Integrated digital records |
|
|
4. Concierge care |
4. VIP/premium services |
|
|
5. Preventive care |
5. Biomarkers/diagnostic tools allow for predictive care |
|
|
6. Personalized care |
6. Genomics-based adaptive, customized care |
|
|
Material |
1. Nanoparticle medicine |
1. Focuses cancer treatment by targeting special nanoparticles that attach to cancerous cells |
|
2. Drug delivery |
2. New drug delivery material with timed release |
|
|
Mechanical |
1. Haptics |
1. Sensing and manipulation of objects and environments through touch |
|
2. Exoskeleton |
2. An external anatomical feature that supports and protects a person’s body |
|
|
3. Prosthetic |
3. An orthopedic device that can help a mobility-impaired individual |
|
|
4. Artificial disk |
4. Replaces damaged or diseased neck disks, resulting in less pain, less swelling, and fewer complications |
|
|
5. Asthma mitigation |
5. Alair System employs radio-frequency energy to warm the airway and keep muscles from constricting in asthma patients |
|
|
|
||
beyond which survival is genetically limited. Thus, health care is indeed a service, one that can be personalized and that can enhance the quality—and length—of an individual’s life.
ENGAGING COMPLEX SYSTEMS THROUGH ENGINEERING CONCEPTS: A METHODOLOGY FOR ENGINEERING COMPLEX SYSTEMS
Harold W. Sorenson, Ph.D., Jacobs School of Engineering, University of California, San Diego
Introduction
This paper is intended to give senior healthcare leaders examples from other business sectors of problems and emerging approaches to finding solutions that may be applicable to health care and may make it possible to realize the goal of developing a learning healthcare system. In general terms, these approaches have been developed to allow complex enterprises to respond better to the challenges of globally distributed operations in a highly dynamic, event-driven environment.
The ubiquitous presence of the World Wide Web has created an environment in which entities are bonded through the exchange of information. The businesses and national security organizations that have been able to operate successfully in this information-bonded environment have demonstrated outcomes and advantages that are evident to everyone. An integrated perspective that merges the views of the business and engineering communities is increasingly recognized as one of the cornerstones of a successful approach to dealing with enterprise complexity. The result can be new and more effective ways to deliver health care through the rapid fielding of enhanced capabilities based on a close working relationship among all stakeholders, including healthcare administrators and practitioners, enterprise architects, and enterprise systems engineers. Consequently, the culture, practice, and delivery of patient care can change in fundamentally important ways.
Working from a perspective focused on feedback control systems and their fundamental importance in a wide variety of engineering applications, this paper reviews principles of control and their importance in the synthesis of complex enterprise systems. As with any engineering system development, consideration of the devices that must be controlled dominates the design. For example, the control of room temperature results from measuring temperature and comparing it with the desired setting. The controller regulates the operation of the heater to achieve the desired condition. An engineering model combining the environment and the heaters is fundamental to the design of the control system and its ability to maintain temperature and comfort. As the following discussion argues, the emerging methodology for engineering complex systems has conceptual similarities,
but it involves people and organizations as well as technology, which presents a much more challenging problem.
Context for the Discussion
The issues motivating this workshop’s discussions can be thought of in terms of an emerging paradigm that has seen increasing use in the commercial and business worlds and, to some extent, within the Department of Defense. Looking carefully at these motivating issues, we see that if we look at health care as a complex adaptive system, we can approach it with a variety of improvement strategies that many companies are currently using to help them compete in their marketplace.
Reordering and abbreviating the issues that motivate the overall workshop discussion, we can derive a related list of eight issues that motivate the discussion in this paper:
- Focus on the patient for learning healthcare systems.
- Improve value and eliminate capability deficiencies.
- Apply complex adaptive systems theory to health care.
- Make extensive data more widely available and useful.
- Enable knowledge to be an enterprise asset.
- Apply system and process developments to health care.
- Recognize the dynamics of the healthcare environment.
- Change culture, practice, and delivery.
The goal of this paper is to explore these issues, identify potential approaches, and discuss possible strategies for their engagement. In this context, focusing on the patient is exactly the right place to start for a learning healthcare system. The methodology discussed starts there, with patients as the key stakeholders. Overall, the approaches discussed are driven by the need to improve value or eliminate deficiencies in capabilities; this becomes a focus driven by the stakeholder community, which says, in essence, this is what we want to be able to do better.
One central consideration for health care is the need to make data more widely available and useful. As with many types of organizations, health care suffers from a prevalence of stovepipes, silos, and other organizational conventions that prevent data from being widely accessible to the broader community. By transforming data and information into knowledge, enterprises gain an asset that can be used to address current deficiencies in healthcare delivery directly and to allow more benefits to be delivered to the patient. In summary, knowledge must become an enterprise asset. This paper examines an emerging methodology for system and process development and suggests that such development has utility in the healthcare
environment. If this methodology is successfully applied, the changes that result can have the effect of altering the culture of healthcare delivery, with concomitant changes in the practice and delivery of care.
General Approach
When we approach the problem of engineering complex enterprise systems, we typically start by asking a series of interrelated questions. How do we think about the problem? How do we manage the complexity? How do we approach the problem’s solution? How do we develop the problem’s solution? How do we assess the proposed solution? What is the effect of the development? Each of these questions is discussed briefly in the sections that follow, with a particular emphasis on the first three.
How Do We Think About the Problem?
Any enterprise, whether a healthcare or business or defense enterprise, involves a large number of people with a variety of responsibilities and jobs. To carry out these responsibilities and jobs, these stakeholders work using prescribed processes to accomplish desired functions and outcomes. And in performing this work, they use a variety of information and data. In most enterprises, the reality is that any given user is familiar with only a limited number of processes and data sources. Too often this implies that the function being performed has more limited utility than would be the case if the workers’ knowledge of processes and data were broader and more encompassing. Because of the stovepipe or silo characteristics embedded in virtually every organization, a given user in an enterprise is unfamiliar with all the other useful components of the system and has no way to learn them in a natural way.
How do we bring order to such a system? How do we manage this environment in such a way that the users can actually use the data, the processes, and the functions that exist elsewhere in the enterprise? In much of his writing, Russell Ackoff (a seminal thinker in systems science at the Wharton School) emphasizes the need to break away from reductionist thinking in managing complex enterprises. He goes to the heart of the question in his book On Purposeful Systems, written with Frederick Edmund Emery (Ackoff and Emery, 1972), when he writes, “To manage a system effectively, you might focus on the interactions of the parts rather than their behavior taken separately.” Indeed, the issue is all about interactions, interfaces, and the way information is shared and distributed.
A long-time collaborator with Ackoff, Jamshid Gharajedaghi, outlines the basics of systems thinking in his book Systems Thinking: Managing Chaos and Complexity (Gharajedaghi, 1999). Such thinking starts, he
suggests, with an operational definition of a “systems methodology” that involves three interdependent variables: structure, function, and process. Those variables, together with the environment, define the whole. For present purposes, we can think of structure as defining the components and their relationships and constraints—synonymous with input, means, and effects. Similarly, function defines the outcome, which is synonymous with output, and process defines the sequence of activities required to produce the outcome—how the function is performed. A core assumption is that the development process is necessarily iterative.
As a quick example of the interdependency of function, structure, and process, consider the heart. The function of a heart is to pump. It circulates blood. Its structure can be defined in terms of its chambers, valves, and arteries. The process is basically defined in terms of alternating cycles of contraction and expansion. The environment is the body in which the heart operates. The body in turn operates in a larger environment, which certainly affects the functioning of the heart. Clearly, the variables are interdependent and cannot be separated in considering the heart as a system.
Figure 2-9 provides background on the evolution of systems thinking. A product of the competitive world in which we live, systems thinking began with the ideas of Henry Ford regarding mass production. His model posited that people and parts are interchangeable, a way of thinking that
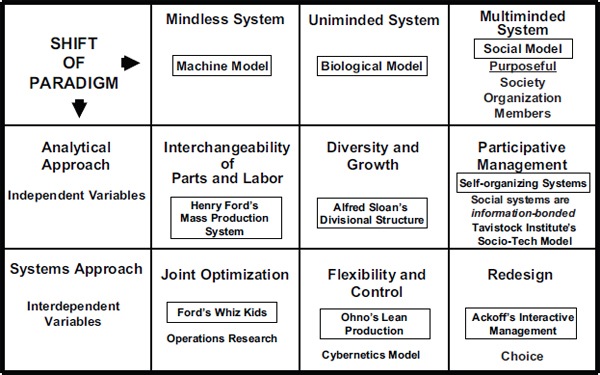
FIGURE 2-9 Evolution of systems thinking.
led to people and parts being treated as independent variables. The analytical result was to look at each part by itself. As people first experimented with mass production, they learned that the factors they regarded as being independent actually were not, but rather were interdependent. This interdependence led to a systems approach, which can be said to be the roots of operations research. The analytical problem became a search for optimal solutions that would enable an organization to do things better. An oft-cited example of the acceptance of the OR approach is the scenario involving the “whiz kids” at Ford Motor Company around 1960.
Ford started with the motto that one could have any color Ford one wanted as long as it was black. As mass production gained in popularity, it became apparent that everybody could institute mass production techniques; as a result, the first adapters of mass production, such as Ford, would lose their competitive edge. Alfred Sloan started General Motors (GM) with the idea that diversity would lead to growth. Buyers of GM products could get cars with different colors and in different varieties. To manage the resulting interdependencies, Sloan introduced a reductionist approach that was reflected in the divisional structures of the company. Organizational structures were broken down and reduced to the point where the company considered marketing to be separate from human resources, which was separate from sales, and so forth. That led to the divisional structure that is still taught in management schools today. This is much more of a biological model than Ford’s mass production model. It is a biological model because there is a brain (i.e., the chief executive officer) in charge who tells his or her arms (i.e., the divisional structure) what to do. The divisions implemented the strategy from the corporate office to develop diverse products and to stimulate corporate growth and profit.
This business model evolved to another stage with the concept of lean production, developed by Ohno at Toyota. Lean production is based on a cybernetics model in which one measures the production process and feeds that information back into decisions about inventory and production to gain efficiencies and reduce costs. This is essentially the state of the practice in most organizational theory today.
The past decade, however, thanks in large part to the power of the Web, has seen the rise of participative management. The person in charge no longer has the sole word. Based on personal experience working at high levels in companies, I can say that collaboration and participation provide the essential mechanisms to manage large, complex enterprises effectively. Top-down direction is increasingly complemented by bottom-up involvement in the decision-making process. A fundamental characteristic of this new, productive environment is its social nature. The power of these social networks is a primary source of the complex adaptive systems we are starting to recognize and address.
Social systems are information bonded, in contrast to the systems of the past, which were energy bonded. Consider the car. It has an engine, and when the car is started, the gas in the engine explodes, and the energy from that explosion is transferred through the camshaft to the driveshaft, to the axle, and to the wheels. Everything is connected by various forms of energy transfer. Most electric power grid systems operate the same way, with the electrical energy being transferred in ways that allow us to do what we want. Energy-bonded systems are created by well-known systems engineering processes that are based on well-developed requirements. In essence, it is the statement of requirements that separates project management from corporate management. In the case of a technology, its usefulness is the primary developmental concern, but enterprise systems must be concerned with organizational interactions and with the people involved in them. Learning healthcare systems can be described as being information bonded and operating through social networks.
The social model basically says that if one is purposeful and seeks to reach some kind of enterprise objective, one should take a holistic view that includes society, the organization, and, finally, the various members of that society or organization who may be involved in what one is trying to do. This holistic set of concerns leads to a totally different approach from the traditional systems engineering, which is reductionist in nature. Now, instead of analyzing things, one designs, one tries out, one builds, one fields, and one learns. The development proceeds in an iterative fashion, with new capabilities appearing on a time scale of days or a few weeks. Collaboration among stakeholders and managers becomes the necessary development interaction style. Often no single person is in charge in the sense of having tight control over the development plan. Flexibility and adaptation are central to the process and the participative management style.
To make an important point, let me introduce a little engineering jargon. Entropy is the measure of randomness in the universe. According to the Second Law of Thermodynamics, total entropy in a closed system increases over time. However, open-living systems display an opposite tendency; they move toward order, thus generating negative entropy. Emergent behaviors are a result. The Internet is a good example. Think of all the behaviors that have emerged from the use of the Internet. I am sure the creators of the Internet had no idea of the sorts of behaviors that would arise and garner so much interest, such as the information-sharing power of Google, the online auctions of eBay, and communication sites such as MySpace. These emergent behaviors are the key to understanding the potential for changing the culture, practice, and delivery of health care.
How Do We Manage the Complexity?
Data and information must be at the heart of any discussion of information-bonded systems. Consequently, the methodology being described here starts with a consideration of the mechanisms for making data and information available across an enterprise in ways that are effectively transparent to the system user. In this approach, sources and generators of data and information publish to a registry that is used to make potential users aware of the existence of the data and information and that has pointers defining how the data are found and retrieved. The users, generally, subscribe to the types of data and information they are interested in accessing. The mechanism for accomplishing this publish/subscribe operation is referred to as a service registry. The registry is important because it guarantees that data will not be warehoused. Ownership and responsibility for the data remain with those who generate them, and once the registry has been established, the methodology says that information is retrieved, processed, integrated, and managed to achieve a purpose. If new information is generated, it is registered for future users of the results. The pointers are provided so that subscribers can quickly get the information needed to solve a problem or answer a question. Alternatively, Web standards allow the discovery of information that supplements the subscriber information that is registered. For example, Google provides a search engine people use regularly in their daily lives. Standards that have already been developed for the Web are fundamental to the development of the mechanisms used to define interfaces and govern the exchange of data and information. The processes for dealing with data and information form the basis of the methodology.
Enterprises must adapt and respond in a timely and effective manner to a variety of planned and unplanned events. To deal with this ever-present situation, it is important that there be a seamless interoperation of disparate organizational entities, often in unplanned and complex ways. The rapidly changing environment has led to a search for solution invariants that might provide stability for the creation and evolution of the system that supports information interoperation (referred to here as the enterprise knowledge system [EKS]). The current approach for managing enterprise complexity, which is continuing to evolve and mature, is based on three interdependent variables: structure, function, and process. The structure, which we refer to as an architecture, provides a blueprint for evolving the EKS. It defines the components or actions of the system and their functional interconnections. The architecture is also used to capture the constraints on the system (e.g., quality of service, security and privacy rules, regulatory constraints such as HIPAA). The structural description does not involve detail on the implementation of the components, communications, or constraints. Instead, it
should be developed relatively quickly and should provide a documented basis for the implementation and evolution of the EKS itself. As with the design of a building, the architecture provides a reference that changes less often than the implementation and permits a framework within which processes and functions are allowed to change to accomplish the objectives of the business.
How Do We Approach the Problem’s Solution?
Deriving and defining the architecture is the key step of the development process for complex, adaptive systems. Fundamental to the design process is the concept of separation of concerns. Generally, the first step in separating concerns is to assume that the architecture is defined as consisting of layers or tiers. Each layer communicates with its adjoining layer through well-defined interfaces. An activity in one layer cannot interact directly with any internal feature of any other layer. This structure allows changes to be made within a layer without disturbing other layers as long as the interface descriptions remain unchanged (i.e., concerns are separated). A fundamentally important layer is the presentation layer. Users interact with the system using a portal, sometimes referred to as the human–system interface. For our architecture construct, users, through the portal, have access to the service registry and the elements of the system they are interested in using. Users can ask questions and, essentially, tell the system what they are trying to do. Everyone should be familiar with the function of a portal through Web interactions. For example, the AOL browser serves as a portal to the global community and its services.
Behind the registry is an infrastructure that allows the complexity of the networked system, such as the Web, to be hidden and transparent to the user. Through this common information infrastructure (CII), information that addresses the needs of a user is routed to appropriate functions, applications, processes, and services. An architectural style that is gaining wide acceptance is service-oriented architecture (SOA). In this style, the CII is generally referred to as the enterprise service bus.
A very simple model of architecture has users who can access the system through various kinds of hardware devices and communities of interest that are defined through having a common interest or mission that requires a variety of business applications or services. Underpinning this architecture is the CII. In this simple model of an enterprise architecture, it is important to recognize that a network simplifies the system connections of many users and their applications. A set of N users can communicate directly with one another without being connected in a point-to-point fashion. The latter mode of communication would generate an enormously complicated requirement because the number of point-to-point connections for N users
is proportional to the square of the number of users. With a networked system, the number of connections is simply N. Each user connects to the network, and the network accomplishes the point-to-point connectivity.
Returning to the SOA, the term service denotes a broad set of useful artifacts that enable users to accomplish their tasks. A service can be an application that may be useful for people across the enterprise, it can be data sources or databases that have widespread utility, or it can be computational tools that support implementations invisible to the user. In essence, a service is a reusable artifact that simplifies the development and implementation of, and facilitates the introduction of, new processes and functions that broaden the existing system capability. The SOA model is based on the differing needs and roles of service consumers and providers. The consumers interact with the system through a presentation layer. The business processes must be precisely defined and are used to derive essential services. The composition of the services produces the desired process. Required services are located via the service registry, wherever they may be located physically. The registry is used to inform the service provider of the request for the service, and the enterprise service bus executes and allows the execution of the desired business process.
In summary, one starts by asking, “What are we going to do in our business?” In the present case we might ask, “How are we going to deliver health care?” One then defines the processes that describe a healthcare function. From these processes and from the actors using the system, services are defined and added to the service registry. As described, the architecture of the system is layered, and an emphasis in the system development is on the interfaces between layers. One can change a business process without changing the service or presentation layer except in the details of that process. The value of managing the complexity of the EKS through the use of layered, or N-tiered, architectures then starts to make sense.
How Do We Develop the Problem’s Solution?
Having defined a framework for managing the complexity, it is logical to ask, “How do we develop the problem solution?” First, one identifies a function or mission that is to be provided by the healthcare delivery system. Then one identifies the people, or actors, who should be involved in using, describing, architecting, and implementing the desired capability. This group of people constitutes a community of interest, and the members are referred to as stakeholders. The future users of the system are requested to answer the question, “As an actor, how am I going to use this system?” The answers are called use cases, which become the basis for discussions between the architect and the users as the architecture is developed. The architect guides the discussion but must always be sensitive to the needs of
the user community. For the healthcare delivery community, the use cases should focus on the needs of and the services desired by and delivered to each patient. They are key actors for this system development.
The manner in which the architect translates the use case information into the structure of the desired system is not addressed here, but the architecture must provide guidance to the engineers who implement the system. The architect implements governance procedures that enable the implementation to be measured against the requirements of the architecture. A key part of the governance process is continuing interaction among the stakeholders, architects, and implementers. This interaction drives the iterative development of the system and must serve to put in place useful capabilities, often in small increments, on a frequent basis. The implementation approach is referred to as agile development. Practice has revealed a desirable phenomenon that often emerges from providing new capabilities in small, easily understood increments. Because the users can live with and use the capability, a fan club develops that facilitates the adoption of the capability across a broader community. This is one example of a desirable emergent behavior that can appear when one is working within a highly complex environment. These behaviors are observed to change cultures in a natural manner that comes from bottom-up participation, not from the top down.
How Do We Assess the Proposed Solution?
Early in this paper, I mentioned the importance of feedback control and its great utility in virtually all systems and their useful operation. There has been no discussion of the role of feedback control in this methodology, but there was an implicit reference in the previous paragraph. In essence, it is through various types of feedback that we address the question, “How do we assess the proposed solution?”
The development of complex systems such as healthcare delivery advances because of feedback and communication among all the participants. The architect serves as the feedback controller during the development of the architecture. Because the systems being developed are inherently complex, it is often difficult for the architect to determine whether the logic and behaviors dictated by the architecture will achieve the goals of the stakeholders. Systems of the type discussed here are event driven. Using theory and methods drawn from discrete-event dynamic systems, the architect can develop models of the capability being developed that can be used to assess the adequacy of the logical architecture and the behavior of the processes implemented by the architecture. These architectural models do not involve the actual implementation of any capabilities. They can be applied before time and resources are expended to actually build the system. In fact, they are useful in saving later development costs and delays in
situations where fundamental problems are discovered late in the process. Finally, the architect serves as the controller in the governance policies that are imposed on the implementers. As useful capabilities are presented to the user community, the architect again assesses the reactions of the users to identify desirable modifications, additions, and improvements.
As a capability moves into daily use, however, the architect must have planned for the possibility of behaviors arising either from events outside the community of interest or from unplanned events occurring within the system that can adversely affect the system’s usefulness. To anticipate the effects of complex events on the desired system, the architect must introduce mechanisms for measuring the internal message traffic. Sometimes referred to as business activity monitoring, these measurements are used to provide feedback that allows the earlier identification, recognition, and correction of anomalous behaviors. Thus, feedback control becomes essential in the long-term operation and performance of the system.
What Is the Effect of the Development?
In closing, we consider the question, “What is the effect of the development?” This paper has asserted that it is possible to build an environment that will lead to the rapid fielding of enhanced and new capabilities. This result can be achieved only through close working relationships among all stakeholders, including patients, healthcare administrators and practitioners, and enterprise architects and engineers. Not only can there be planned developments that provide more effective ways of delivering health care, but unexpected and useful emergent behaviors can appear. As a result, the culture, practice, and delivery of patient care will change fundamentally in important and beneficial ways. This change will be driven from the bottom up by the participants while being guided by the leadership of the healthcare community.
REFERENCES
Ackoff, R., and F. E. Emery. 1972. On purposeful systems. Chicago, IL: Aldine-Atherton.
Brandeau, M. L., F. Sainfort, and W. Pierskalla (Eds.). 2004. Operations research and health care. A handbook of methods and applications. New York: Springer.
Bush, G. W. 2001 (October 16). Executive order on critical infrastructure protection. Washington, DC: The White House.
CBO (Congressional Business Office). 2008. Technological change and the growth of health care spending. Pub. No. 2764. Washington, DC: CBO.
Friedman, T. L. 2005. The world is flat: A brief history of the twenty-first century. New York: Farrar, Strauss & Giroux.
Gawande, A. 2002. Complications: A surgeon’s notes on an imperfect science. New York: Metropolitan Books.
Gharajedaghi, J. 1999. Systems thinking managing chaos and complexity: A platform for designing business architecture. Boston, MA: Butterworth–Heinemann.
Grossman, J. H. 2008. Disruptive innovation in health care: Challenges for engineering. The Bridge 38(1):10–16.
Hancock, W. M., and F. H. Bayha. 1992. The learning curve. In G. Salvendy (Ed.), Handbook of industrial engineering, 2nd ed. (pp. 1685-1698). New York: Wiley.
Hipel, K. W., M. M. Jamshidi, J. M. Tien, and C. C. White. 2007. The future of systems, man and cybernetics: Application domains and research methods. IEEE Transactions on Systems, Man, and Cybernetics Part C 30(2):213–218.
IOM (Institute of Medicine). 2000. To err is human: Building a safer health system. Washington, DC: National Academy Press.
_____. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
Kaplan, E. H., and R. J. Heimer. 1992. HIV prevalence among intravenous drug users: Model-based estimates from New Haven’s legal needle exchange. Acquired Immune Deficiency Syndrome 5(2):163–169.
Kaplan, E. H., D. L. Craft, and L. M. Wein. 2002. Emergency response to a smallpox attack: The case for mass vaccination. Proceedings of the National Academy of Sciences 99(16):10935–10940.
Maglio, P., S. Srinivasan, J. Kreulen, and J. Spohrer. 2006. Service systems, service scientists, SSME, and innovation. Communications of the Association for Computing Machinery 49(7):81–85.
McPhee, J. 1990. The control of nature. New York: Farrar, Straus and Giroux.
Mendonca, D., and W. A. Wallace. 2004. Studying organizationally-situated improvisation in response to extreme events. International Journal of Mass Emergencies and Disasters 22(2):5–29.
Morse, P. M., and G. E. Kimball. 1951. Methods of Operations Research. Cambridge: Technology Press of Massachusetts Institute of Technology.
NAE (National Academy of Engineering)/IOM. 2005. Building a better delivery system: A new engineering/health care partnership. Washington, DC: The National Academies Press.
O’Neill, P. 2007. Why the U.S. healthcare system is so sick and what OR can do to cure it. OR/MS Today 34(6). www.lionhrtpub.com/orms/orms-12-07/frhealthcare.html (accessed May 28, 2010).
Peterson, P. G. 2005. Running on empty. New York: Picador.
Porter, M. E., and E. O. Teisberg. 2006. Redefining health care: Creating value-based competition on results. Boston, MA: Harvard Business School Press.
Quinn, J. B., J. J. Baruch, and P. C. Paquette. 1987. Technology in services. Scientific American 257(6):50–58.
Rouse, W. B. 2007. Complex engineered, organizational and natural systems. Wiley Inter- Science Online: Systems Engineering 10(3):260–271.
_____. 2008. Health care as a complex adaptive system: Implications for design and management. The Bridge 38(1):17–25.
Schoen, C., S. Guterman, A. Shih, J. Lau, S. Kasimow, A. Gauthier, and K. Davis. 2008. Bending the curve: Options for achieving savings and improving value in U.S. health spending. New York: The Commonwealth Fund.
Stevens, R. A., C. E. Rosenberg, and L. R. Burns. (Eds.) 2006. History and health policy in the United States. New Brunswick, NJ: Rutgers University Press.
Sussman, J. M. 2008. Intelligent transportation systems in a real-time, customer-oriented society. The Bridge 38(2):13–19.
Tien, J. M. 2000. Individual-centered education: An any one, any time, any where approach to engineering education. IEEE Transactions on Systems, Man, and Cybernetics Part C: Special Issue on Systems Engineering Education 30(2):213–218.
_____. 2003. Towards a decision informatics paradigm: A real-time, information-based approach to decision making. IEEE Transactions on Systems, Man, and Cybernetics, Special Issue, Part C 33(1):102–113.
Tien, J. M., and D. Berg. 1995. Systems engineering in the growing service economy. IEEE Transactions on Systems, Man, and Cybernetics Part C 25(5):321–326.
_____. 2003. A case for service systems engineering. Journal of Systems Science and Systems Engineering 12(1):13–38.
_____. 2006. On services research and education. Journal of Systems Science and Systems Engineering 15(3):257–283.
_____. 2007. A calculus for services innovation. Journal of Systems Science and Systems Engineering 16(2):129–165.
Tien, J. M., and M. F. Cahn. 1981. An evaluation of the Wilmington Management of Demand Program. Washington, DC: National Institute of Justice.
Tien, J. M., A. Krishnamurthy, and A. Yasar. 2004. Towards real-time customized management of supply and demand chains. Journal of Systems Science and Systems Engineering 13(3):257–278.
Yasar, A. 2005. Real-time and simultaneous management of supply and demand chains. Ph.D. thesis. Troy, NY: Rensselaer Polytechnic Institute.
Zadeh, L. A. 1996. The evolution of systems analysis and control: A personal perspective. IEEE Control Systems Magazine 16(3):95–98.






















































