1
Engineering a Learning Healthcare System
INTRODUCTION
As the roles and complexities of provider profiles, patient care processes, and diagnostic and treatment options grow—often in an independent and disintegrated fashion—gaps in efforts concerning patient safety, clinical outcomes, reimbursement policy, medical education, and other aspects of the functioning of the healthcare system continue to widen. Defining the future state of American health care will require a clear vision on the part of the healthcare community.
The Engineering a Learning Healthcare System: A Look at the Future workshop drew together participants from healthcare and engineering disciplines to identify challenges in health care, including effectiveness, safety, and efficiency, that might benefit from a systems engineering perspective. With the baseline assumption that reform efforts must extend beyond finance to remedy the growing complexities in health care. Participants evaluated aspects of healthcare culture and practice through examples and lessons from within and outside the healthcare sector. Workshop attendees considered approaches to taking a new look at the organization, structure, function, and delivery of services in health care while maintaining a patient-centered focus.
Presentations and discussions touched on elements from prior workshops, including Clinical Data as a Public Good and the Learning Healthcare System, in an effort to synthesize topics and take advantages of various synergies. The Engineering a Learning Healthcare System: A Look at the
Future workshop addressed multiple components central to the work of the Roundtable on Value & Science-Driven Health Care:
- Facilitate collaborative healthcare choices of each patient and provider.
- Ensure innovation, quality, safety, and value in health care.
- Foster the transformation of the American healthcare system into a learning health system that generates and applies evidence naturally.
- Emphasize prevention and health promotion as means to increase value.
- Instill principles of accountability, care coordination, expectation setting, incentive alignment, and patient-centered focus.
This chapter contains a brief summary of the workshop’s three keynote addresses followed by individually authored pieces based on those presentations. The three keynote talks were a commentary by Brent C. James on “Learning Opportunities for Health Care,” W. Dale Compton’s discussion of “Teaching Opportunities from Engineering,” and Donald M. Berwick’s presentation, “Observations on Initiating Systems Change in Health Care.”
Engineering a Learning Healthcare System: A Look at the Future
The first two keynote addresses together outlined the landscape of issues the workshop was designed to address and framed many of the most important questions that workshop participants would explore. The third keynote address, delivered near the end of the workshop, added further depth to the intellectual framework of the workshop and contributed additional specific suggestions for moving forward in engineering a learning healthcare system.
Reflecting the fact that the workshop was sponsored by the Institute of Medicine (IOM) Roundtable on Value & Science-Driven Health Care in cooperation with the National Academy of Engineering (NAE), the program opened with two talks that addressed, respectively, issues in health care and opportunities for addressing those issues from the realm of engineering.
The first presentation, “Learning Opportunities for Health Care” was by Brent C. James, executive director of the Institute for Health Care Delivery Research and vice president of medical research and continuing medical education at Intermountain Healthcare. Based in Salt Lake City, Intermountain Healthcare is an integrated healthcare system of hospitals, clinics, a large physician group, and a health maintenance organization/ preferred provider organization insurance plan covering more than 450,000
people. James is known internationally for his work in clinical quality improvement, patient safety, and the infrastructure that underlies successful improvement efforts, such as culture change, data systems, payment methods, and management roles.
James began by discussing the historical evolution of the modern structure of healthcare delivery. He outlined five areas where care delivery currently falls short of its theoretic potential, touched briefly on the reasons for that failure, and then reflected on emerging solutions, emerging frameworks, and challenges that create a context for work on improving health care.
The five areas of health system failure noted by James were (1) the well-documented, significant variation in practices; (2) high rates of inappropriate care; (3) unacceptable rates of preventable patient injury and death; (4) a striking inability to “do what we know works”; and (5) large amounts of waste and spiraling prices, which limit access. James suggested that we may be on the verge of a head-on collision of two factors: first, the guild nature of medicine, in which physicians, nurses, and other health professionals act as stand-alone experts, and second, what James characterized as “clinical uncertainty.” The latter term refers to the era of unprecedented complexity that characterizes health care today, an era marked by a lack of valid clinical knowledge and evidence regarding the best treatments and exponentially increasing new medical knowledge, in tandem with a continued reliance on subjective judgment and the innate limitations of the expert mind when making complex decisions.
James proposed four specific areas for attention in the effort to alleviate these shortfalls: (1) addressing clinical complexity, (2) developing a more robust capacity of knowledge management in a learning system, (3) improving systems for care delivery via a team approach instead of through independent experts, and (4) designing health care as a coordinated system. In particular, he called on engineering professionals to share their knowledge and expertise with healthcare professionals in order to address these issues collaboratively.
W. Dale Compton complemented James’ healthcare expertise by offering the engineering perspective. Compton, the Lillian M. Gilbreth Distinguished Professor (Emeritus) of Industrial Engineering at Purdue University, brings extensive experience in engineering research from work in academia and the private sector and has served since 2000 as Home Secretary for the NAE. He offered a variety of suggestions on how engineering can help health care transition from where it is today to the point where it might realize its full potential as a learning healthcare system.
Compton explored some of the most pressing, overarching issues, including creating change within large organizations, healthcare transformations, and integrating learning into systems change. Focusing on a case
study of the Ford Motor Company, Compton outlined several principles of continuous improvement that he believes could benefit health care. Organizing a comprehensive understanding of health care’s disparate parts from a systems point of view will be a critically important step. It will also be vital to have adequate data—and the capacity to mine that data for knowledge—as well as to engage participation by staff at all levels of an organization.
Communication is another key factor. Although communication has many dimensions that vary among organizations, Compton asserted that engineers and healthcare professionals have considerable work to do in creating a common understanding of problems and opportunities. A cadre consisting of both engineering and medical professionals is needed to tackle some of health care’s more intractable problems, working in the near term on problem solving and in the longer term on more fundamental systems design.
Later in the workshop, a keynote address from Donald M. Berwick explored in greater depth the issues that health care faces and the ways in which solutions might be engineered. Then president and chief executive officer (CEO) of the Institute for Healthcare Improvement, Berwick was also a professor of pediatrics and healthcare policy at the Harvard Medical School and professor of health policy and management at the Harvard School of Public Health. Berwick posited that there is enormous potential benefit to health care in deepening system knowledge and basing action on that knowledge. He warned, however, that real value in healthcare reform will come only if people are willing to confront the status quo, whether in technique, culture, training, or economics. The core challenge, he suggested, is that health care needs to clarify its aims, and leadership is needed to make that happen.
The heart of Berwick’s presentation discussed seven issues: (1) the need to emphasize interdependence in the healthcare system; (2) the need to make the redesign of processes more visible; (3) the need to recognize the importance and value of dynamic learning and local adaptation as scientific learning processes; (4) the question of waste, which health care must confront with knowledge and action; (5) the need for a sufficient platform for robust multidisciplinary research and development at the intersection of health care and engineering; (6) the need to enrich professional education and development in health care—for example, with more attention to teamwork and systems thinking; and (7) the reform of health care in a way that would result in a radically different, integrated systems design of the fundamental healthcare infrastructure.
Following are the full presentations of the keynote addresses that set the stage and tone for the discussions that took place throughout the remainder of the workshop.
LEARNING OPPORTUNITIES FOR HEALTH CARE
The healing professions have always been central to human society. Humanity’s earliest written records refer to clinical practice. For example, the Code of Hammurabi, written almost 1,800 years BCE, addresses the legal implications of medical treatment. Artifacts from Stone Age cultures indicate the presence and importance of healers and the healing professions in preliterate times.
Until relatively recently, the healing role was limited to two basic elements: when approached by a patient suffering a health problem, a healer could give unique insight into what was happening—that is, he could explain the present; and, drawing on experience with similar cases from the past, the healer could predict the patient’s potential health future. But for most of human history, healers had little to offer in the way of effective treatment. Any “healing” that occurred was mainly of a spiritual nature—a shoulder to lean on, a listening ear, and (2) compassion and understanding that could help a patient reach balance, acceptance, and closure. While no one made careful measurements of the health outcomes of early medical care at a population level, educated observers routinely opined that if one were seriously ill and sought the attentions of a typical physician, chances of survival actually declined. For many centuries, the most common approaches to treatment centered on a humoral theory of disease, which held that the human body was made up of four basic humors: black bile, yellow bile, white phlegm, and red blood. Disease was thought to arise from imbalances in the humors. Health could be restored by bringing the humors back into balance, usually by removing some of the red humor. As late as 1900, the most common physician-prescribed treatment in the United States was bloodletting. The second most common therapy was the administration of purgatives, producing chemically induced vomiting and diarrhea. Hospitals were where poor people went to die (Porter, 1997; Rosenberg, 1987; Starr, 1984).
Around the turn of the 19th century, medical practice underwent a massive transformation. Between the 1860s, during the American Civil War, and about 1910, clinical leaders introduced four important changes (Porter, 1997; Rosenberg, 1987; Starr, 1984).
First, they adopted the scientific method as the foundation for “how we know what we know” within the allopathic healing professions. Driven by the scientific method, a germ-based theory of disease rapidly replaced competing frameworks and their related treatments, such as the humoral theory. Over time, this approach greatly improved the professions’ under-
standing of the human organism in health and disease. It also produced literally thousands of effective treatments and fundamentally changed the medical model: where before physicians could explain the present and predict the future, medical science gave them the ability to “change a patient’s future.”1
Second, clinical leaders created the modern model of clinical education. The transformation of medical education started with a report of the American Medical Association published in 1902. That report led Andrew Carnegie to commission Abner Flexner, a high school teacher, to conduct a more detailed evaluation. Flexner found that the average course of study to become a licensed physician took about 4 months. (Apparently, little effort was needed to understand the humoral theory of disease, bloodletting, and purgatives.) That training usually took place exclusively in a classroom setting, with no exposure to patients or patient care. Flexner’s report, published in 1910, led to the closing of more than half of all so-called “medical schools” in the United States. A new 2-year curriculum, centered in hospitals at the patient bedside, emerged.
Third, the leaders tightened the process of professional licensing. Previously, laws regarding professional licensure had served primarily to protect the guild of medicine from external competition. Those laws took on new meaning when they rested on the foundation of medical science and effective clinical education. Clinical leaders refined the licensing laws, produced a new definition of medical professionalism, and used the resulting tools to hold the profession as a whole uniformly accountable to a much higher level of demonstrated knowledge, skills, and ethical conduct.
Finally, clinical leaders created a new organizational structure for care delivery. In 1895 physicians planning the new Johns Hopkins University Hospital divided management of the facility from the practice of medicine. A new class of health facility administrators managed staffing, supplies, and the physical plant, freeing physicians to focus exclusively on patients’ clinical diagnoses and treatment.
Collectively, these changes led to dramatic gains in human health measured at a population level. A child born in the United States in 1900 had a life expectancy of 49 years. A child born 100 years later, in 2000, could expect almost 77 years of life (Cutler et al., 2006) (Figure 1-1). The years from 1900 to 1960 might be called the Public Health Era. Essentially all of the life expectancy gains achieved over those six decades came from sanitation, safe food, clean water, vaccination, and immunization. For example, the cholera epidemics that killed thousands at a time during the
![]()
1 The phrase comes from Dr. James Reinertsen through a personal communication. He describes the role of the physician as (1) explain the present, (2) predict the future, and (3) change a patient’s health future.
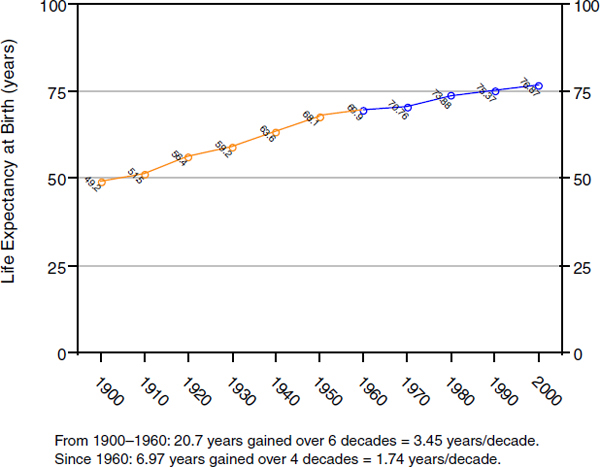
FIGURE 1-1 Increases in life expectancy at birth within the United States, by decade, 1900 through 2000.
latter half of the 19th century disappeared almost completely following the introduction of easily accessible clean drinking water. Typhus fever, one of the most common killers in human history, was virtually eliminated through improvements in living conditions that reduced the infestations of fleas that spread the disease. Deaths from smallpox, a true scourge, ceased with the introduction of effective vaccination programs. In 1900, somewhere between one-fifth and one-third of all children died before reaching the age of 5 years, victims of common pediatric infectious diseases—diphtheria, pertussis, measles, mumps, and polio (CDC, 1999). Widespread childhood immunization makes such deaths very rare today. During the Public Health Era, life expectancy at birth increased by an average of 3.45 years with each passing decade (as calculated by the author from the data presented in Figure 1-1).
Life expectancy gains due to advances in public health plateaued in the decade following the end of World War II. As these public health−related gains attenuated, however, a new source of health improvements emerged. For the first time in human history, physicians and nurses began to have
treatment tools that could change a patient’s future. Starting midcentury, disease treatment began to have a major impact on how long and how well people lived as measured at the population level. For example, since 1960 age-adjusted mortality from ischemic cardiac disease (the number one killer in modern first-world nations) has decreased by 56 percent (from 307.4 to 134.6 age-adjusted deaths/100,000 people), and since 1950 age-adjusted mortality from stroke (the number three killer in industrialized nations) has decreased by 70 percent (from 88.8 to 26.5 age-adjusted deaths/100,000 people) (CDC, 1999; Cutler et al., 2006; National Center for Health Statistics, 2000). This is remarkable progress, particularly when considered in the context of the entirety of human history. The evidence is clear: modern health professionals now routinely offer treatments that would have appeared miraculous to any previous generation.
Aim Defines the System
Given these achievements, it is worth reflecting on what is known about the factors most important in determining a person’s total health—that is, how long and how well one lives. In an analysis of the actual causes of death in the United States, roughly 40 percent of total health was found to be determined by individual behavioral choices (McGinnis and Foege, 1993). The top three behavior-based challenges to health are tobacco use, obesity, and consumption of alcohol and other recreational drugs. For example, alcohol consumption is associated with about 65 percent of fatal violent crimes, 70 percent of all domestic abuse, and 60 percent of all fatal non−motor vehicle accidents (Doonon, 1998). Other behaviorally related health issues include sexually transmitted diseases, including AIDS; pregnancies among unwed teens; and suicide, accidents, and violence, particularly among young men (McGinnis et al., 2002). Healthy behaviors are closely linked with educational level, which in turn is associated with income level and health insurance coverage.2
One’s genetic inheritance determines another 30 percent of total health. Some scientific progress has been made in understanding linkages between genes and disease, but the field is still relatively new. Some estimate that we are still 20 to 30 years away from being able to broadly offer treatments to counter genetic determinants of health.
Another 20 percent of total health relates to environmental and public health factors. These factors include clean air, safe water, and the control of epidemic infectious disease through immunization and sanitation.
![]()
2 These four elements usually appear in combination and are very difficult to separate: (1) low levels of education are directly associated with (2) unhealthy behaviors, (3) low income levels, and (4) lack of health insurance.
Only 5 to 10 percent of total health—an estimated 3.5 to 7 years of lifespan—derives from the health care delivery system.
In 1977 Aaron Wildavsky published a classic essay in which he defined “the Great Equation” as the belief that “health equals health care” and that “health care means access to care.” He cited statistics to show that the Great Equation is fundamentally false (Wildavsky, 1977). Such findings underscore the importance of understanding the returns achieved from our current national investment in health care.
In 2006, the United States spent about $7,100 per person on health care. For a typical family of four, healthcare expenditures far exceed the costs of owning a home. (Total national health care expenditures for a family of four totaled about $2,375 per month in 2005, while the median family home cost only $1,040 [KFF, 2006].) U.S. expenditures are high compared with those of other Organisation for Economic Co-operation and Development (OECD) countries (Peterson and Burton, 2007; Reinhardt et al., 2002). Sweden, for example, has the reputation of having the finest socialized medicine system in the world. Despite that country’s spending less than half of what the United States spends on health per capita, the average Swede lives about 3 years longer than the average U.S. citizen. Likewise, although infant mortality rates have decreased very significantly worldwide over recent decades, the United States has rates roughly twice as high as those reported in Sweden.3 Wildavsky’s argument raises serious questions about whether differences in overall health at a national level can be traced back to a country’s spending on health care. But even if U.S. health outcomes were equivalent to those of other developed nations, the United States still spends twice as much per person as most other modern nations. What do we get for all that extra money? Dr. W. Edwards Deming, the father of modern quality theory, regularly noted that “[a]im defines the system.” Relative to health spending, what are the aims of healthcare delivery? The current national healthcare debate implicitly assumes, without examination, that the primary aim of healthcare delivery is “total health”—how long and how well we live. There are, however, two additional possible aims.
When carefully asked, most U.S. citizens say they value their relationship with a trusted medical counselor very highly. They appear to judge their health outcomes according to their opinion of that relationship, suggesting that to patients, the clinician−patient relationship may be even more
![]()
3 Although these figures are often thought to represent a direct reflection of the quality of each nation’s healthcare delivery system, it is important to note that the Swedish advantage disappears when risk adjustments are made for the infant mortality rate for gestational age. Each country defines preterm birth differently at a functional level, with implications for whether the infant is treated as a stillbirth or is placed in newborn ICU, with massive amounts of money invested in his/her care.
important than health outcomes. “High touch” care denotes the idea of caring, not just curing. Emeril Szilagyi captured the essence of high touch care quite accurately in his 1965 essay “In Defense of the Art of Medicine”:
A man stricken with disease today is assaulted by the same fears and finds himself searching for the same helping hand as his ancestors did five or ten thousand years ago. He has been told about the clever tools of modern medicine and somewhat vaguely, he expects that by-and-by he will profit by them, but in his hour of trial his desperate want is for someone who is personally committed to him, who has taken up his cause, and who is willing to go to trouble for him. (Szilagyi, 1965)4
High touch care leads to patient satisfaction with the healthcare delivery system. Effective primary care networks, in which people have easy access to a clinical counselor, facilitate this kind of care. Compared with other countries, the United States performs poorly in providing easy access to high touch care (Schoen et al., 2007).
Another possible aim of health care delivery is rapid response, or “rescue care.” Jonsen defined the Rule of Rescue as “the imperative people feel to rescue identifiable individuals facing suffering or death” (McKie and Richardson, 2003). For the Rule of Rescue to apply, there needs to be an emotional link. There must be a name and a face so that the sufferer becomes a human being rather than a statistic (McKie and Richardson, 2003). Some commentators have pointed out that this view of care reflects a “Do something! She’s dying!” reaction. They note that the interventions applied do not have to be effective—that humans feel an overwhelming need to try to help, regardless of the chance for a positive result. For example, about a year ago, six miners were underground when a coal mine in central Utah collapsed (the Crandall Mine disaster). Their plight gripped the state of Utah and the nation, as the news media shared pictures of the six men, their life stories, and interviews with their distraught friends and families. Those six men probably died in the initial collapse, but tens of millions of dollars was spent and three would-be rescuers died on the chance that the six might be alive. Other examples of the Rule of Rescue are easy to find. Indeed, the response is so powerful that in many cases, the “victim” need not be human; we respond in similar fashion to heartrending stories of animals in distress.
When examined through the lens of rapid-response rescue care, the U.S. healthcare system is the best in the world. For example, mortality rates following major trauma in the United States are about half those seen in Europe. Mortality following a heart attack in the United States is roughly
![]()
4 Of particular interest, Szilagyi defined the “art of medicine” as the knowledge and skills to optimize the clinician−patient relationship.
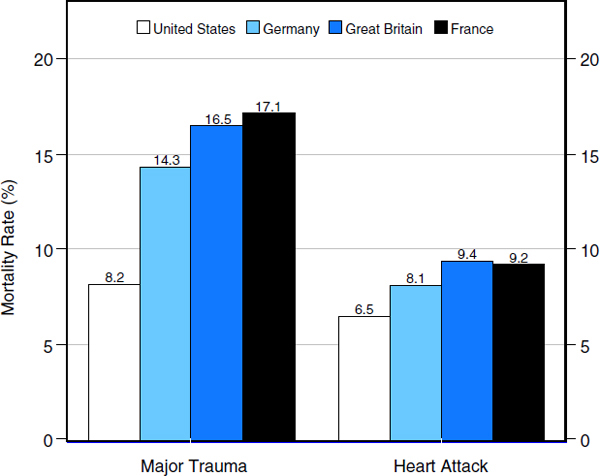
FIGURE 1-2 System performance by nation for two major examples of rescue care.
SOURCE: Based on data from OECD (2006).
a third lower than the European rates (Figure 1-2). Mortality rates for very small (less than 1,500-gram) preterm neonates in the United States are about half those observed in other developed nations (OECD, 2006). Renal dialysis rates are five times higher in the United States than in Sweden and almost twice as high as in the closest European country (Germany). Similar differences exist for other classes of high-technology, specialty-based rescue care, such as cancer treatment (Coleman et al., 2008; Verdecchia et al., 2007).
Many other countries’ healthcare systems outperform the U.S. system from the perspective of total health and patient satisfaction. This advantage appears to be attributable to healthier behaviors, better public health, and easily accessible primary care. Conversely, the U.S. healthcare system performs significantly better for patients suffering from severe illness or injury, both of which require easy access to technology and subspecialists. Yet despite the massive investment it requires, rescue care is not strongly asso-
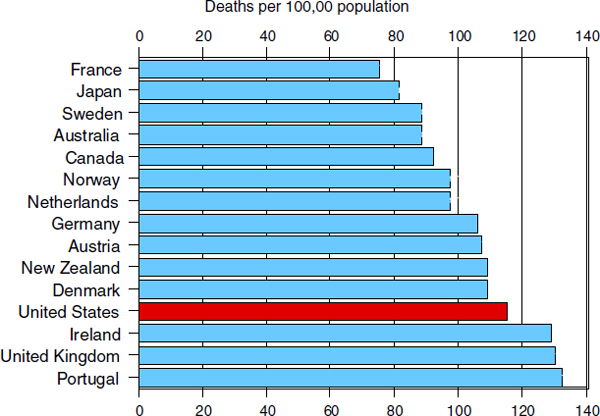
FIGURE 1-3 Mortality amenable to health care among OECD nations.
SOURCE: Based on data from OECD, 2006.
ciated with better total health at a population level. Health promotion and disease prevention, implemented through effective primary care networks, appear to have a greater effect on how long and how well populations live. Figure 1-3 compares OECD nations in terms of mortality amenable to health care. The United States fares poorly. A more recent update of the same study places the United States dead last among 19 high-income democracies on the same measure (Nolte and McKee, 2003).
Americans place a high value on rescue care and are willing to pay for it. But rescue is just one of three possible aims of health care delivery, suggesting that there are immediate opportunities to improve the quality of health care delivered in the United States.
Opportunities for Improvement
Over the last 40 years, a broad range of health services investigations have found that current U.S. health care delivery falls short of its theoretical potential. The shortcomings represent significant opportunities for improvement. They fall into five broad categories.
First, care varies widely by geographic location (i.e., care received in
one community is often very different from that received in another). The differences are so large that even with full access to care (health insurance), it would be impossible for all Americans to receive high-quality care. More than 40,000 articles documenting or discussing variations in care delivery have been published in peer-reviewed journals over the last 40 years. These well-documented, massive variations in practice are an important entry point for understanding how best to improve the quality of care received by all Americans.
Second, some investigators have suggested that geographic variation in quality of care might arise from inappropriate care, with a treatment’s innate risk to the patient outweighing any potential clinical benefit. An evaluation of a series of major treatments performed in U.S. hospitals found that 2 to 32 percent of those treatments were clinically inappropriate. For professions that hold as their primary tenet “First, do no harm,” these findings are deeply troubling. However, inappropriate care does not explain geographic variation. On average, communities with high rates of utilization show about the same proportion of inappropriate care as low-utilization communities (Chassin et al., 1998).
Third, a landmark IOM report estimated that between 44,000 and 98,000 people die each year from preventable injuries sustained as part of care delivery in U.S. hospitals (IOM, 2000). That makes American hospitals somewhere between the fourth and sixth most common cause of preventable death in the United States.
Fourth, the U.S. healthcare system is characterized by a striking inability to execute. For example, McGlynn and colleagues identified a series of treatments with strong evidence for effectiveness. The resulting list of treatments was noncontroversial; there was strong professional consensus that the treatments should routinely be provided to patients. However, such care was actually provided just 55 percent of the time (McGlynn et al., 2003). Undertreatment exists side by side with overtreatment (the second category discussed above). U.S. healthcare delivery misses by wide margins on both sides of the target of effective, beneficial care, which probably explains why inappropriate care does not account for geographic variation in care.
Fifth, by some estimates more than 45 percent of all resource expenditures in hospitals is quality-associated waste, such as recovering from preventable errors, building unusable products, providing unnecessary treatments, and simple inefficiencies (Anderson, 1991; James et al., 2006). These costs and the spiraling prices they produce limit patient access to care. They contribute to the fact that 46.6 million Americans currently lack health insurance.
Most studies documenting shortcomings in healthcare delivery have examined the U.S. healthcare system. However, similar studies in each of the above categories have been conducted in other nations, which appear
to suffer from the same failings. These findings suggest that the failure of care delivery to achieve its theoretical potential arises from a deeper set of causes than simply national health policy.
Collision Between the Craft of Medicine and Clinical Uncertainty
The same body of research that documents the ways in which healthcare delivery falls short of its theoretical potential also points to a likely cause: a head-on collision of two factors inherent in current approaches to health care.
The first factor is practice based on the craft of medicine—the idea that physicians, nurses, and other health professionals should act as standalone experts who draw on a massive personal knowledge base gained from formal education and practice experience and who honor an ethical trust that places a patient’s healthcare needs above any other end. From that foundation, each professional starts largely with raw material, then crafts a unique diagnostic and therapeutic experience customized to the needs of the individual patients who seek care or consultation. The healing professions hold that this approach guarantees the best possible result for each patient.
The second factor is what Eddy (1984) calls “clinical uncertainty.” It is a direct product of the professions’ decision to adopt the scientific method at the turn of the 19th century. Since then, clinical science has greatly increased understanding of the human organism in health and disease and has generated literally thousands of ways clinicians can intervene to change a patient’s future. This explosion of medical knowledge has had a secondary effect: Eddy argues that “the complexity of modern medicine exceeds the capacity of the (expert) human mind.” Clinical uncertainty includes four principal elements that, operating within the framework of craft-style practice, produce the opportunities for improvement catalogued in the previous section.
The first of these elements is a lack of valid clinical knowledge about best treatment across a range of competing options. For most conditions, modern healthcare delivery offers a range of possible treatments. A series of investigations led to the idea that clinicians have Level I, II, or III evidence (Lawrence and Mickalide, 1987) that identifies the best treatment for a particular patient in a specific circumstance only about 10 to 20 percent of the time (Ferguson, 1991; IOM, 1985; Williamson et al., 1979).5 In 80 to 90 percent of cases, practicing clinicians can have legitimate differences of
![]()
5 Level 1 is the randomized controlled trial, Level 2 is observational design, and Level 3 is expert consensus from a group of respected authorities using formal methods.
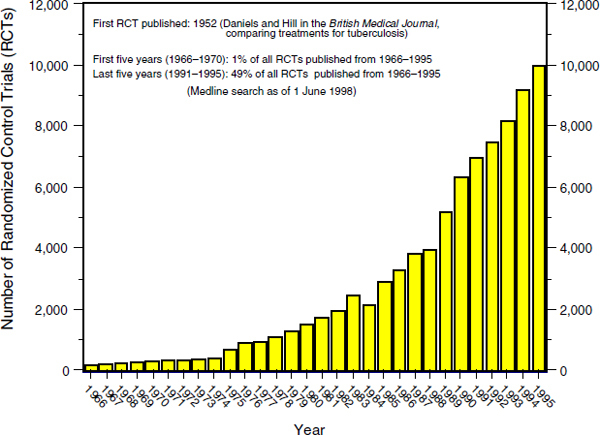
FIGURE 1-4 Rate of generation of Level 1 evidence, 1966 through 1995.
SOURCE: Chassin, 1998.
opinion about what is best, differences that are reflected in wide variation in actual practice.
The second element is the rate of increase in new biomedical knowledge. Figure 1-4 shows the number of randomized controlled trials (RCTs) published in the peer-reviewed medical literature each year from 1966 to 1995 (Chassin, 1998). Not only is medical knowledge increasing dramatically, but it appears that the rate of increase itself is increasing. The last year the National Library of Medicine relied primarily on manual abstraction to add new computer-searchable entries to its Medline archive of biomedical research was 2004. During that year, Medline grew by more than 11,000 references per week, representing about 40 percent of all articles published worldwide in peer-reviewed biomedical and clinical journals (National Library of Medicine, 2006). In other words, more than 27,000 articles are published each week in peer-reviewed biomedical and clinical journals. Shaneyfelt (2001) addresses the topic more directly. He reports that within 3 to 4 years of initial board certification, both generalist and subspecialist internists (cognitive physicians) begin to show “substantive declines in general medical knowledge.” He estimates that to maintain current knowledge, a general internist would need to read about 20 articles a day, 365 days a
year (Shaneyfelt, 2001). It is not that physicians’ knowledge decreases over time; rather, the rates of continued learning possible in a busy clinical practice cannot keep pace with the generation of new knowledge. Williamson and colleagues demonstrate that it can take almost 20 years for a major new scientific finding to achieve geographically widespread adoption and links that variation to the inability of physicians in practice to stay current (Williamson et al., 1979). Variation in the deployment of new medical knowledge results directly in variation in clinical practice.
The third element is continued reliance on subjective recall as a foundation for clinical decision making. The expert mind reaches conclusions by breaking a problem down into subproblems, pattern matching within each subproblem, and then summarizing results back into a synthetic whole. In the case of problems that require primarily pattern matching, the expert mind performs significantly better than other competing approaches (Groopman, 2007). However, current clinical practice relies increasingly on rate estimation rather than pattern matching. For example, once a physician reaches an accurate diagnosis, the next step is offering the patient accurate information about the likely outcomes—probabilities, in the form of rates—arising from each treatment choice. The same literature that documents the expert mind’s dominant performance on problems that require pattern matching also shows that the expert mind fails abysmally when asked to summarize information accurately across groups over time (rate estimation). Eddy (1992) reports that when different groups of expert physicians were asked to estimate complication rates based on subjective recall (“in my experience”), the groups typically gave responses that covered almost the full range of possible answers, and no group showed a detectable pattern of response. Eddy notes that, on any such issue, one could find a physician who honestly believed in—and was willing to testify in court to—any desired value ranging from close to 0 to almost 100 percent. Other investigators have asked practicing clinicians to estimate subjectively rates for their own performance in circumstances where measured rates were available but unknown to the physicians, and have found that respondents typically underestimated their own rates by about 20 to 50 percent (e.g., Lomas et al., 1989).
The final element is limitations in the number of factors the expert mind can consider when making a clinical decision. In a seminal article, Miller (1956) estimates that the expert mind can consider only five to nine factors when making a complex decision. Subsequent investigations have empirically demonstrated similar results. For example, Morris and colleagues (1994) were able to document significant variation in ventilator settings from morning to evening rounds in individual patients directly managed in an ICU by the same intensivist physician. They estimate that an intensivist needed to assess as many as 40 important physiological factors to make a
treatment decision. Even after compartmentalizing the problem (breaking it into subcomponent parts, such as respiratory rate, tidal volume, and oxygen concentration), expert physicians appeared to be selecting a small subset of six to eight factors each time they saw a patient. By their own assessment, it appeared that the factor selection process was subconscious and random (Morris et al., 1994).
The vast majority of care delivery practices require that expert clinicians consider more than nine factors when making a clinical decision. Variation in how physicians subconsciously select and prioritize factors could directly contribute to geographic variation in care delivery patterns overall.
Early Solutions, Emerging Frameworks, and Refined Challenges
When the inherent complexity of modern medicine and the limitations of the human mind collide with the craft of medicine, the result is wide variation, high rates of inappropriate care, unacceptable rates of care associated with injury and death, a striking inability to apply well-established proven therapies consistently and broadly, and huge amounts of waste. However, some proven solutions have emerged. At Intermountain Healthcare, our primary vehicle is called Shared Baselines. We first identify a high-priority clinical process (in terms of health risk to each patient and volume of patients affected). We then organize a team consisting of all the health professionals associated with that specific process of care, including physicians, nurses, pharmacists, therapists, technicians, and even administrators. The team develops an evidence-based best-practice guideline. This guideline is then blended into the clinical work flow, embedded in staffing, training, supplies, physical layout, educational materials, and measurement/information flow. A physician need not remember, but can simply follow the default path to implement evidence-based best practice.
The shared-baseline approach then moves one step further. We have compelling internal evidence that it is functionally impossible, outside of a very narrow range of circumstances, to write a practice guideline that perfectly fits any patient. The people who come to us for care have had different exposures to potential toxins and pathogens in the environment. More important, they are genetically different. That means they will exhibit different responses to pathogens, different expressions of disease, and different responses to treatment. They also bring different expectations and values and have different personal resources. We therefore do not just allow, or even suggest, but rather demand that each physician adapt our shared-baseline, evidence-based best-practice guideline to the needs of each individual patient. The physician must judge what should vary and how. We use the shared baseline to track that variance. A physician will undergo just as much scrutiny for complying with a shared baseline too
often, compared with his or her peers, as for complying too infrequently. In either circumstance, when physicians differ significantly from their peers working in the same practice environment, either they have something to teach or something to learn. A shared-baseline protocol is the opposite of “cookbook medicine.” It is, rather, a measurement tool designed to drive peer-based learning. Over time, variation arising from professionals disappears, while variation arising from patients is retained.
Intermountain Healthcare currently has more than 50 shared-baseline protocols operating under measurement. Roughly 5 to 15 percent of a protocol’s content is routinely adjusted to meet the needs of a particular patient. This approach is an example of a promising method for managing complexity. Within Lean (a recent sub-branch of quality theory), it is called mass customization. Mass customization is a tool for managing complexity. It allows a physician to focus on a handful of critical factors for each individual patient because the rest of the care delivery process is reliable through standardization and measurement.
Shared baselines have produced dramatic improvement in many care processes in Intermountain. Figure 1-5 illustrates one such instance, involving door-to-balloon inflation times for patients suffering acute myocardial infarction. Figure 1-6 shows reductions in mortality rates associated with the better execution resulting from the shared-baseline approach.
Shared baselines produce another important advantage. Beyond measurement and feedback of variation data in a peer-driven learning network, they establish a framework that directly supports the generation of scientifically valid knowledge from routine care. A shared baseline standardizes routine care. It can function like the control arm of an RCT. In fact, Intermountain has used shared-baseline protocols in just that way. We build them initially as care management tools to guarantee the best possible patient outcome at the lowest necessary cost. With consistent practice, error rates fall (better execution), costs fall, and a team can apply the scientific method to improve systematically. Technically, Intermountain is a community-based care delivery system. However, our shared-baseline protocols have led to a surge in publication of clinical results in peer-reviewed journals that rivals the publication rates of many academic medical centers. Within a typical academic setting, fewer than 5 percent of patients ever contribute to new medical science (i.e., enter some sort of trial); within an Intermountain shared baseline, that number approaches 100 percent.
Conclusion
Over the past century, modern medicine has evolved into a system that routinely performs miracles. In a very real sense, that same progress has moved us beyond our original roots. As the science has grown, the prob-
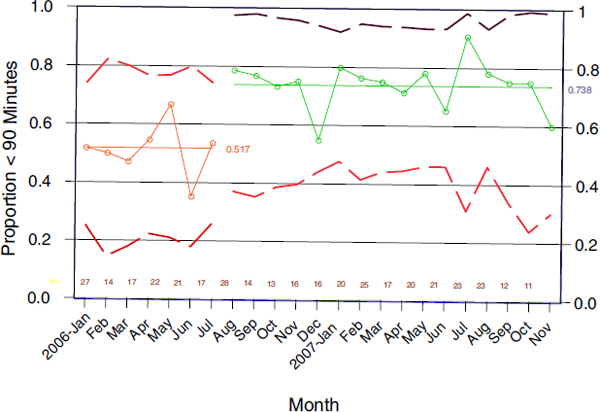
FIGURE 1-5 Proportion of all ST-segment elevated myocardial infarction patients with emergency room door to coronary angioplasty first balloon inflation time of less than 90 minutes, all Intermountain Healthcare facilities (21 hospitals), 2006 through 2007.
lem has shifted. While pattern matching is still important, an increasing portion of good clinical execution relies on assessing results across groups over time. The craft-of-medicine approach to care delivery that produced so many important results cannot address the complexity that defines modern medicine.
Engineering professionals have sought to understand and manage complex systems in many sectors and disciplines. Medical professionals could benefit from the counsel and shared learning of our engineering colleagues. As we shift from a craft-based to a profession-based practice, the idea of care delivered by a team—an organized system of care delivery, as opposed to a loose conglomeration of poorly coordinated parts—presents a number of challenges. How might engineering concepts such as system analysis, design, and control provide insight into some of the key issues facing optimal care delivery? Where can we find the best leverage for rapid, effective change? How might we better address clinical complexity? How do we build knowledge management into a learning system that lives at the heart
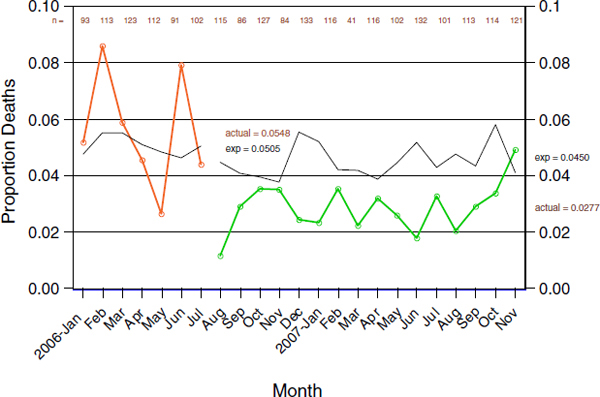
FIGURE 1-6 Mortality rates following ST-segment elevated myocardial infarction, all Intermountain Healthcare facilities (21 hospitals), 2006 through 2007.
of routine care delivery? In sum, how can we design health care as a coordinated system of production as we enter a new century?
TEACHING OPPORTUNITIES FROM ENGINEERING: LEARNING BY EXAMPLE
W. Dale Compton, Ph.D., Purdue University
Change is difficult for large organizations, but the successful ones find ways of overcoming the challenges. This paper focuses on some of the successful approaches used by organizations and suggests that the healthcare delivery system might consider undertaking similar attempts to better serve its customers.
Any large organization faces many challenges, some organizational and others related to human behavior. Setting common objectives for a new organization is one such challenge. Ensuring the fairness of performance evaluations of individuals and groups in a changed organization is another. There are also issues concerning the fairness of the reward system. These challenges are common and contribute significantly to the silos that frequently exist in large organizations. On the human behavior side, there is a
natural resistance to change. Enlisting a diverse and perhaps geographically dispersed workforce to pursue common goals can be very difficult as well. How do organizations generally go about combating such challenges? They use various tools, they move people about, they establish cross-departmental committees, and they reorganize—even when doing so is not necessary—all in an effort to get people in different areas to work together, think along common lines, and commit to cooperation. Numerous examples demonstrate that these approaches generally do not work very well.
How can a large, diffuse, diverse organization learn to do things differently in order to go in a different direction? “Large,” “diffuse,” and “diverse” are emphasized because they are terms that describe the healthcare delivery system. As we think about a learning healthcare system, we must first recognize that this system has two distinct parts: the clinical part, which encompasses biologically targeted intervention processes, and the delivery part, which consists of the processes intended to support the clinical part. With this second part—the organization and structure of the delivery system—engineering can be of assistance. From an engineering perspective, we might begin by asking the following questions: What are the system objectives? What determines performance? What changes are needed or wanted? What are important points of controlling this system?
Fortunately, the overall objectives of the healthcare system are well accepted. The system must be safe, effective, timely, patient centered, efficient, and equitable. It is interesting to note that this list usually does not include cost, even though cost affects and is affected by each of these objectives and is becoming an increasingly important issue in health care.
In thinking about the steps that might prove pertinent to changing the healthcare delivery system, it is helpful to draw on experience from another industry. Although there are many differences between the operation of a large, diverse, global manufacturing company and the healthcare enterprise, some of the experiences of the former may be useful. The comparison offered here is with a member of an industry in which success is determined by the acceptance of one’s products in a very competitive environment. Although there are multiple participants in the healthcare industry and although competition in that industry is less obvious and more difficult to quantify, it can be thought of as a consumer industry.
So allow me to describe a few experiences concerning how a large company faced the issue of quality in the 1970s. I joined Ford Motor Company in 1970. The first meeting of all corporate management that I attended dealt with quality. There was a great deal of consensus during that meeting. Everyone agreed that our product quality was poor, and everyone agreed that something had to be done about this situation. The meeting ended, and everyone went back to work and continued doing the same thing they had done before, with the result that product quality remained poor. Why?
There were no real incentives. After all, our principal competitor was just across town, and they had the same problems with product quality as Ford. So why change? Besides, everyone thought that quality cost money, and no one wanted to be the first to acknowledge having extra money.
Then, however, a crisis occurred. There was an oil embargo, and vehicle fuel efficiency became very important to the public. Big, gas-guzzling cars became unpopular. The public discovered that Japanese manufacturers offered smaller vehicles with better fuel economy and flocked to buy them. Then those customers discovered that the Japanese cars also had high quality. That was the beginning of the Japanese entry into the automotive market of the United States.
Although some commentators tried to explain the success of the Japanese as the result of their having better technology, this was not what made the Japanese cars so attractive. Rather, the Japanese products had better fuel economy because they were smaller and lighter in weight. They exhibited better quality because the Japanese had put in place procedures that kept their manufacturing processes under control. Although the Japanese had the right products for the market at the time, we must remember that when the Japanese first tried to enter the U.S. market after World War II, they were quite unsuccessful because they had poor product design and poor quality. They learned what was needed and, with the help of some key consultants, came back a few years later with superior products.
Chrysler’s dire financial circumstances at the time are well known, but Ford’s financial situation is less so. On one occasion, Ford was within a couple of days of running out of money. It was a grim situation. The Ford system had to change to survive. Quality had to be improved. But how?
First, it was recognized that in the short term, errors in the assembly of the vehicles could be eliminated so that customers would receive products with fewer problems, and the company would experience lower warranty costs. Members of Ford’s upper management, from the CEO down, were committed to this goal and served as salespersons for the need for change. The union management was brought into the process of explaining why things needed to change and how to begin. The unions agreed with the strategy and participated actively with management in enlisting everyone in the effort.
One plant was chosen to determine how to make the necessary changes. The progress achieved in that plant in a short period of time surprised everyone. Quality improved almost immediately. Now came the task of disseminating the knowledge learned there to the entire organization. Workers from the first plant were used to teach workers in other plants. People with experience in the tasks on the line taught others how to do things better. They were the most credible teachers. For the company, quality became
what was known as “Job One,” the most important timing issue in the launch of a new product.
While the manufacturing system was being changed dramatically, project engineers put in place a process to improve the design of the next major Ford product. No longer would a design by the engineers simply be passed on to the manufacturing people, who would often return it to the engineers within a few weeks, saying it could not be manufactured with either the facilities in place or those planned. This process cost time and money, and ultimately led to a misunderstanding between the two groups—an example of the perils of the silo system.
Ford introduced the concept of simultaneous engineering to reduce the silo mentality among the design engineers, the development engineers, the sales force, and the so-called “parts activities” that handled warranty problems. Cooperation across boundaries became the operating mode. This new approach led to the creation of one of the most successful Ford products—the first Ford Taurus.
Of course, there are obvious differences between Ford and the healthcare system. At Ford, there was a clear management hierarchy that could set objectives. There was a single objective, quality. It was an objective that everyone could understand and support. Everyone in the Ford system could see why the objective was needed, how they could contribute, and how they would benefit. All involved came to understand that improving quality was not simply something they would work on for a while and then return to the old ways as soon as a couple of senior managers retired.
The Ford organization also recognized that it was necessary to adopt another important Japanese concept—continuous improvement. Of the many aspects of continuous improvement, four are particularly relevant to this discussion.
First, how does one tell if improvements are occurring? To begin, one must have data. Ford had large amounts of data. Its task was to create an organization that recognized the importance of letting individuals on the assembly line use those data without having to get permission from a supervisor to try new ways of doing business. Continuous improvement can work only if employees at all levels are informed, trusted, and empowered. One important result of recognition of this idea was the introduction of some key engineering tools, such as statistical process control, whereby workers control and regularly document performance against operating objectives.
The healthcare industry faces a problem that much of our industry did not face: there are large amounts of data on the clinical side of the system but not on the delivery side. As an example, I have talked with a number of representatives of ambulatory clinics and hospitals about improving patient flow in their facilities. If one can improve patient flow, one can then improve scheduling of resources and people. To accomplish good patient
flow, one needs data on the arrival rate of patients at every station, that is, at every point where they stop. One needs to know the average time they spend at each station and the paths they follow. These data are normally gathered by having someone with a notepad and a stopwatch follow patients around. That is fine, but there is no assurance that these data will be representative of another time in that facility or another facility. As a result, few facilities have these data. It is not that the data cannot be collected, but the collection costs money and time. Yet without these data, it is difficult to use the engineering tools that can determine optimal flow.
A second aspect of continuous improvement focuses on participation by all involved. To quote from a recent publication, Adapting Process-Improvement Techniques in an Academic Medical Center, by Paul Levy, president and CEO of Beth Israel Deaconess Medical Center in Boston,
Here is an example of ventilator-associated pneumonia (VAP), a problem relevant to anyone who has been or will be in an intensive care unit (ICU) or who will have a loved one in an ICU. A patient on a ventilator who contracts pneumonia has a 30 percent chance of dying, a pretty high rate of mortality. The good thing is that we know how to prevent many of these cases by taking five well-documented steps…. [I]n the months since the ICUs began working on reducing cases of VAP, performance of the five-step bundle, and the oral care, have risen to 100 percent.
Note that the change was not a response to an order from CMS [Centers for Medicare & Medicaid Services]…. Neither the insurance companies nor patients nor even the hospital administrator insisted that these things be done. In fact it was academic physicians who read journals and other publications from around the world who instigated the changes. After several of them had read the recent literature about preventing VAP, they decided that they would change the way that ICUs cared for patients.
But—and here’s the key—they then had to organize the 200 people who work in the ICUs. Respiratory therapists, nurses, doctors all had to be trained to change the ‘industrial’ process, with no increase in staff and with basically no increase in resources. The doctors went to work and made it happen.
Many of the changes were not very complex…. I watched the results of the changes and started posting them before they reached the 90 percent rate. At that point, the head of the group sent an e-mail to his colleagues that read something like this: ‘As you may have heard, Mr. Levy has a blog on which he is now posting our success rates with ventilator-associated pneumonia prevention. Perhaps we should take this as an additional emphasis to do even better, because people out there are watching. (Levy, 2008)
The organization of the system is also a very important aspect of allowing these changes to take place. For a complex system to be manageable, the
people who design it must recognize the interactions that take place among its parts, and the design must be informed by how the actions of each element of the system affect the performance of the other elements. Seeking to optimize each of the elements by itself does not guarantee the optimization of the whole. (It can be shown mathematically that this is the case except under very limited circumstances.) One must understand the details of the interactions of the various elements.
Failure to recognize this reality is not unique to any one industry. In the manufacturing industry, we often talk about profit centers, the assumption being that the company is divided into elements and each is allowed to work to optimize its own profits, with the expectation that the total profit of the company will be optimized. Where this notion becomes patently spurious is when one part of the company makes and sells products to another part of the company. Large amounts of time and effort are spent trying to arrive at the proper “transfer price” between the two parts of the company when in fact the outcome does not matter to the company as a whole. The lesson is that the silos must be broken down. This applies to all corporate objectives, not just profit.
The third aspect of continuous improvement is communication. Both engineers and healthcare professionals must work hard to create a common understanding of problems and opportunities. It is impossible to achieve continuous improvement if people are not communicating. The report Building a Better Delivery System (NAE/IOM, 2005), produced by a committee that the late Jerry Grossman and I co-chaired, was well over a year late being published not because of disagreements among committee members, but because we had to rewrite the report several times in an effort to ensure that both engineers and healthcare professionals would—or could—read it. The language was important. I saw similar communication difficulties at Purdue when we launched the Regenstrief Center for Healthcare Engineering. Engineers and healthcare professionals do not have a common language. Simply put, most healthcare professionals do not know what questions to ask and what to do with the answers they receive, and similarly, most engineers do not understand the constraints within which healthcare professionals work. The only experience most engineers have had with health care is being patients.
The final aspect of continuous improvement is related to the first aspect of needing good data. Not only are such data needed, but the data need to be collected, distributed, and analyzed, and this requires information technology systems. The healthcare delivery system does not yet have the sort of comprehensive information technology system it needs. Some relevant bills were recently considered in Congress. The Health Care Information Enterprise Integration Initiative—H.R. 2406—would “authorize [National Institute of Standards and Technology] to increase its effort in support
of the integration of the healthcare information enterprise in the United States.” A second bill, the 10,000 People Trained by 2010 Act, would authorize the National Science Foundation “to award grants to institutions of higher education to develop and offer education and training programs.” The former bill would allocate $3.5 million to $3.8 million per year over 4 years for health informatics and an additional $9 million to $9.6 million per year over 4 years to establish multidisciplinary centers for informatics research on healthcare information. Although the first bill was never voted on, and the second passed in the House but was not voted on by the Senate, they represent a promising start.
In the long term, it will be necessary to create a cadre of both engineering and medical professionals who can work together. They must understand each other and be able to tackle collectively some of the difficult problems facing the healthcare industry. In particular, the NAE/IOM report Building a Better Delivery System recommends the creation of centers that would bring together members of the medical and engineering professions in a multidisciplinary environment where joint research would prosper, where the development of new tools would be undertaken, where the existing and new tools would be demonstrated to healthcare providers, where new joint educational tools could be created, and where assistance in implementing these tools could be provided to the healthcare community. The report calls for the establishment of 30 to 50 of these centers at a cost of about $3.5 million each (NAE/IOM, 2005). The total investment would be $100 million to $150 million per year—a modest investment compared with the approximately $500 billion currently being wasted.
A long-term refocusing of some of the educational aspects of both professions will be necessary, as well as help with problem solving in the near term. Multidisciplinary research does not mean that one discipline works on a problem while another watches or simply consents to having the first one around; there is some possibility of falling into this trap. Medical professionals are becoming more open to letting engineers into their practices, but they appear to be involved less frequent in joining the engineers in actually conducting research.
All interested parties should become actively involved in encouraging members of Congress and other officials to see the importance of investing not only in the short-term but also in long-term activities that can improve the system. Collaboration is needed to help people understand what healthcare professionals and engineers can accomplish together in the proper environment.
For a large, diverse, diffuse system to learn and change requires the involvement of all people at all levels, starting with a committed CEO. It is also necessary to have a common understanding of where the system is going, what is needed, and the tools that are available to assist in those
changes, along with a recognition of the importance of creating an environment that fosters continuous improvement. The tools that engineers possess need to be brought to bear to help improve the care delivery process, and more powerful tools need to be developed. Finally, the successes achieved by individual teams need to be demonstrated to others.
It will not be easy for the healthcare delivery system to learn and change. Change can be accomplished, individually and collectively, by applying knowledge learned in other industries. Clearly a crisis is imminent in the form of safety failures, the knowledge–practice gap, waste and inefficiency, and so forth. In the short term, the tools that can be used to implement immediate changes must be identified. For the long term, it will be necessary to develop convincing arguments that research and development must receive greater funding if a stable system is to be created.
Ford learned. It changed. It survived, and it prospered. Then it went on to forget some of the important lessons it had learned. The latter must not happen to health care. Leaders in the field have a responsibility to make change occur, as well as the wherewithal to collectively make it happen; this opportunity must not be allowed to stagnate or slip away.
OBSERVATIONS ON INITIATING SYSTEMS CHANGE IN HEALTH CARE: CHALLENGES TO OVERCOME
The potential benefit to the healthcare system of deepening system knowledge and of action based on that knowledge is enormous. The result would be equivalent to the sea change seen in health care with the entry of statistical rigor and formal experimental design in the evaluation of healthcare practices in the mid-20th century, led by pioneers such as Fred Mosteller, Tom Chalmers, Archie Cochrane, Ian Chalmers, and David Sacket. These courageous intellectual leaders changed the collective thinking about evidence, to the enormous benefit of patients. The wedding of fields that is being explored at this meeting has the same potential, and it may require equal courage. The potential for the IOM and the NAE to work together as intellectual leaders is extraordinary. Few other agents of change could carry us through the transitional barriers that this intellectual expertise is encountering.
The major challenges to instituting systems thinking in health care lie with the status quo—in technique, culture, training, and economics. It will not be possible to realize the benefits of such thinking without confronting some of those challenges, the same sort of challenges that intellectual transi-
tions in any field encounter. The core notion behind this change in perspective is, “Every system is perfectly designed to achieve the results it gets.” Therefore, the key to better performance in most complex environments is to redesign systems. Just as any car has a top speed, health care of any particular design has a characteristic safety level. The car has a top speed as a property of the car; in health care, similarly, elements such as error rates, costs, and defects are properties of the system as currently designed. That is a scientific premise: that system designs explain system performance. Some commonly espoused views fail to acknowledge performance as a characteristic of a system. These are “black box” views—unscientific views—of how things get better. Even though some of these views are today quite hegemonic in public discourse, especially the reliance on incentives to produce change, there are reasons to be skeptical of them.
A reliance on incentives, on motivation, on encouraging effort, and on markets is widespread in popular theories of healthcare change today. However, the healthcare problem is mainly one of improper designs, not an imperfect market. The great scholar of quality, W. Edwards Deming, used to say that trying harder is the worst plan. Nonetheless, most of the current dominant theories of public policy aimed at making health care perform better are “try harder plans,” and consequently they are likely to fail.
Market mechanisms are particularly worrisome when applied at the level of individuals. The majority of the healthcare workforce is trying quite hard now—and mostly doing its best. The advice offered by Donald Norman in his book on human factors The Design of Everyday Things is, “Honor thy user” (Norman, 1988). The worst thing to do when human factors are at play is to blame the human for the factors. In pursuit of excellence, someone who understands human factors works instead to construct dikes around the frailties of human beings in order to have systems perform better than human beings do and much closer to what those humans really wish they could accomplish. There is little point in trying to mold individual behavior to achieve excellence through effort. Rather, the ownership of improvement lies squarely on the shoulders of leaders of systems rather than those of individuals within the workforce.
This paper examines seven challenges. One challenge that is not included in this list because it is so basic is the challenge of setting aims. Deming used to say that without an aim, there is no system. A variation on this saying with a more positive tone is, “Aim creates a system.” One of the serious barriers to wedding engineering, sciences, and health care lies outside these fields; it is the absence of aim. A country that cannot make a clear decision that its health care will be safe, or efficient, or effective, or patient centered, or timely, or equitable will not achieve those aims. This is not a technical problem. It is a political problem, a problem of leadership.
Without aim there is no system, and without it all of our explorations of systems thinking will be fruitless.
Beyond the need to set aims, at least seven challenges to the wedding of medicine and systems knowledge can be identified. The first is the difficulty of getting people to emphasize interdependence in their thinking. Romantic views of professionalism emphasize personal responsibility, hierarchy, specialization, independence, and professional autonomy. Such views are evident everywhere in health care. Take, for example, architecture. In hospitals there are “doctors’ conference rooms” and “nurses’ conference rooms” and even “patient bathrooms” and “staff bathrooms.” There are discipline-specific spaces. The fragmentation is also evident in training: schools are separate, and the experiences offered to young people to develop their self-images are separate. Separateness, not interdependence, is emphasized in the preparation of professionals.
The separateness is further evident in the framings of professional ethics. Each discipline has its own statement of its ethics, and this statement is nowhere unified with another. There is no common, shared description of the ethical center of health care that applies to everybody, from a physician to a radiology technician to a manager. Physicians have the Hippocratic oath, nurses take pledges, and therapists take pledges, but they do not take the same pledges together.
Fragmentation is evident in the lack of financial compensation for coordinating mechanisms. It is a habit of payment systems to pay for interactions but not for coordination, as evidenced by the institutional boundaries that exist. I am engaged in a great debate right now in one of the committees on which I serve concerning whether hospitals’ mortality rates should include deaths that occur beyond the hospital walls. Is it fair to characterize a hospital mortality rate within 30 days of discharge? Hospitals are saying, “No, we are not responsible for what happens once a patient has left our building.” That attitude represents fragmentation and a failure to understand, let alone embrace, interdependence.
Failure is evident in chronic care hand-offs, and it is embedded in the language used. The word “discharge,” for example, is a peculiar one. It implies that there is an “admission” and then a “discharge,” as if the patient were a type of effluent. The word suggests the patient is no longer a responsibility, and it is a symptom of a lack of sensitivity to interdependence. Proper systems in health care will place interdependence and its management at the top of the hierarchy of professional concerns. That is not the current culture.
The second challenge is the need to increase the visibility of care processes, from the viewpoint of patients. Paul Batalden once said that health care lacks catwalks. It is extremely difficult to see processes of care. It is not easy to “hover” above the work, to see the workflow, because of the way
space and time are divided. When processes are seen, they are not always seen accurately because they are seen from the supply side, not the patient side. The work is described as it is performed, not as patients and their loved ones experience it. The immediate effect is very toxic—patients are expected to adjust to processes instead of having processes molded to their needs, even at the level of the individual. This is a vicious cycle: the more that patients are forced into processes that do not fit them as individuals, the more their expectations will be construed as unreasonable and their capacities seen as constrained.
Possibilities derive only from the redesign of processes, not from the reinforcement of current processes. The first step is to make the processes visible from the viewpoint of the people served. I have recently been studying, to my enormous benefit, with Amory Lovins, founder of the Rocky Mountain Institute and one of the world’s leading scholars in the fields of energy and the environment. In 1976 Lovins proposed a focus on what he called end use efficiency as the hallmark of proper energy design and policy. A concern with end use efficiency is exactly what is needed in health care, as opposed to centralized efficiency, which is not going to meet the needs of patients.
Currently, there are few mechanisms for the coordination and commitment necessary to make processes visible. Taichi Ohno, the creative genius behind the Toyota Production System, offered an important observation. He wrote, “When waste is at a minimum, every customer can be seen as an individual.” Not being focused on process, the healthcare system operates with exactly the opposite premise, assuming that trying to meet the needs of the individual drives costs up. It does not. Rather, when done properly, it drives costs down.
The third challenge is the need to recognize the importance of nonlinearities and the value of dynamic learning and of local adaptation as scientific learning progresses. The nonlinear nature of system dynamics in health care, as in any nonlinear system, weakens the learning power of many formal and classical methods of evaluation and inquiry. Some formal methods of inquiry tend to be insensitive to contacts, mechanisms, and recurring and meaningful stratification. Those methods also weaken the contribution of local knowledge because they are trying to protect against bias.
Health care today lacks habits and norms of inquiry that capitalize on processes and knowledge growth in a nonlinear context. That is actually the side effect of a major intellectual achievement in health care: the establishment of a hierarchy of scientific evidence as a basis for evaluating clinical practices. That hierarchy places RCTs at the top—where they surely belong when considered relative to other forms of inquiry. However, RCTs usually do not belong at the top of the hierarchy of learning processes when nonlinear complex systems are involved. Most sound learning in complex
systems occurs in local and individual settings. Currently, there are no powerful ways to harvest the knowledge accumulating through innovation in local settings in health care.
There is a chasm between, on the one hand, pragmatic engineering sciences (which are very sensitive to nonlinearities) and local learning and system improvement methods and, on the other hand, the current hegemonic hierarchies of evaluation of clinical procedures. Journals have not opened their review processes and pages to the former kind of knowledge. The RCT continues to be placed at the pinnacle of methodologies even in those settings where it simply cannot provide the information needed. I recently received an extremely discouraging e-mail from a very discouraged leader of improvement, a quite senior physician at a major medical center, who forwarded to me the instruction that he had received from his chief of medicine ordering that “no further Plan-Do-Study-Act cycles will be permitted in this department.” The chasm between formal trials and local improvement is enormous, and the cost to knowledge growth is very high.
The fourth challenge has to do with attention to waste—knowledge of and action on waste in health care. One early benefit of proper system views is knowledge concerning waste, including the degree of waste and its different forms. Waste is often the manifestation of system failure and illiteracy. In the nonsystemic view, being mired in that waste can even feel productive. What might otherwise be seen as waste feels like necessary activity. One who attacks waste, even if the attempt is to avoid suboptimization, can appear to be ill-motivated and sinister. For example, the following can feel extremely risky and assaultive in a fragmented system: (1) using someone else’s laboratory findings instead of repeating them, (2) eliminating inventories that buffer against poor flow, (3) automating processes, and (4) using capital fully. It is wasteful when the neurosurgery operating room is never touched by the orthopods and when the orthopods never allow the neurosurgeons to use their room. From the viewpoint of waste, this is poor management of capital, yet many would regard such “ring fencing” as absolutely necessary to achieving excellence in the current system.
The forms of waste in health care are just as vast as they are in other industries: rework, scrap, inventory, queues, motion, unused space and equipment, idle capital, excess information, records of no value, loss of ideas, and, most of all, demotivating of the workforce through insult and indignity. The economics of health care today are in some sense founded on waste. Waste means jobs; it means profit; it means income; it means familiar habit and comfort. Surely, waste levels exceed 30 percent in the healthcare industry; that is 30 percent of the $2.6 trillion spent. In fact, waste may exceed 60 percent, but that would be more difficult to prove. Indeed, if formal value chain analysis were used, the figure might prove to be even higher. Despite the opportunity, it should be noted that there is no formal
research agenda in health care in the nation that is intended to discover and identify waste in its myriad forms.
The fifth challenge is the missing platform for multidisciplinary research and development in the intersection of systems sciences and health care. My career benefited enormously from leaders at Harvard—Howard Hiatt the first among them—who built a platform for the intersection of quantitative analysis methods and healthcare delivery. That platform was the foundation of my own career. With Hiatt and others, I studied a variety of sciences not usually associated with health care, and that study was made easier because there was a platform that linked one part of my brain, performing quantitative analysis, to the other part of my brain, learning to be a doctor. The intersections for the collaborative efforts being explored at this workshop are insufficient. That is, the most valuable potential forms of collaborative research and development among engineering sciences, system sciences, and health care are not yet dignified.
Of interest, the barrier is dyadic. It is symptomatic of the history of the distance between the fields that engineers feel unwelcome, unfamiliar, and intimidated in the healthcare setting. They become silent, as all people tend to do when they are awed in the cathedral of health care. Healthcare leaders tend not to be aware of the engineering disciplines or to be suspicious of their applicability. Although this wall is being broken down slowly, much remains to be done. Bridge building here will be expensive and it will take time, but it will pay off. The recent examples of, say, Steven Spears’ work in health care or Eugene Litvak’s work are already paying off handsomely in settings where the participants are wise enough to seek these experts’ counsel.
As the IOM and others forge these intersections (I love the idea of a master of sciences and engineering degree in health systems), the days when industrial engineers were very common in healthcare settings should be remembered. Somehow that situation never grew into the truly fertile interaction it might have become. The question of what stalled it should be addressed. The idea of more physician-engineers is intriguing. There are physician-information technologists, physician-bioscientists, and molecular biologists who are physicians; now there need to be more engineers who are physicians, people like Kate Sylvester, who is a leader of such syntheses in the United Kingdom.
The sixth challenge has to do with the implications of systems thinking for professional development. Today there are no requirements for physicians and nurses for training in safety science and safety practices. Medical schools are just starting to incorporate these subjects into their curriculums. No physician is emerging from training today who has not heard of Osler or Watson and Crick or the Krebs Cycle, yet thousands of physicians graduate every year who have never heard of James Reason or W. Edwards Deming or Karl Weick—or even Robert Brooke or Jack Wennberg, who are
right here within the field. Nor have most of the teachers heard of these luminaries, which is probably the reason the students do not hear about them. The preparation of professionals today dismisses systems sciences through its silence. Moreover, the siloing of professional preparation itself deemphasizes the role of interdependency. I trained for 9 years in medicine before I was a fully qualified physician. In that training, I spent not a single day of study self-consciously with students of nursing, even though we would then spend our professional lives together locked in interdependency.
The seventh challenge is the greatest in some sense: institutional redesign, or the institutional rearrangements, will be needed if systems sciences are to be fully exploited. If process literacy, process knowledge, and investment in process redesign were increased, the institutions created to preserve the current fragments would become visibly inadequate, and the spaces between them would appear larger and larger. The waste incurred through fragmentation would be obvious. Systems knowledge inevitably leads to the desire for integrated design. It is not at all clear that upon emerging from that exploration, there would be a need for hospitals or offices or insurers or professions in anything close to their current forms.
Some caution against this kind of grandiose thinking about redesign, but it may be that the science would lead there, that system redesign—not political or financing rearrangement—would be the true manifestation of what should be called healthcare reform. It would be care reform, not financing reform or insurance reform or coverage reform, and yet little, if any, of that kind of change is being discussed in the current political debate.
It is doubtful that the political or social will to go there yet exists. If it did, the issues being faced in health care, such as financing, coverage, and costs, would melt away, or at least begin to do so. Furthermore, hospitals would look profoundly different. Indeed, a measure of whether health care had become truly system-minded would be whether hospitals, at last, would seek to be empty, not full. Instead, virtually every hospital board of trustees is holding virtually every executive in virtually every hospital in America accountable for making sure that occupancy levels are trending up, not down. This tells us that “success” has been defined incorrectly from the viewpoint of the true social need for health and gives some idea of the level of institutional rearrangement that would be needed if a truly rational system design were chosen.
The discussion encouraged by this workshop, about a merging of engineering, sciences, and health care, does make sense. It makes a great deal more sense than the status quo. Systems thinking and knowledge are manifest already in many areas of human endeavor other than health care, and someday they will be seen as too promising to continue to be ignored by the healthcare enterprise.
REFERENCES
CDC (Centers for Disease Control and Prevention). 1999a. Decline in deaths from heart disease and stroke—United States, 1900-1999. JAMA 282(8):724–726.
CDC. 1999b. Vaccines dramatically reduced disease in the 20th century. Morbidity and Mortality Weekly Report 48(12):21.
Chassin, M. R. 1998. Is health care ready for six sigma quality? Milbank Quarterly 76(4):565–591.
Coleman, M. P., M. Quaresma, F. Berrino, J. M. Lutz, R. De Angelis, R. Capocaccia, P. Baili, B. Rachet, G. Gatta, T. Hakulinen, A. Micheli, M. Sant, H. K. Weir, J. M. Elwood, H. Tsukuma, S. Koifman, G. A. Silva, S. Francisci, M. Santaquilani, A. Verdecchia, H. H. Storm, J. L. Young, and the CONCORD Working Group. 2008. Cancer survival in 5 continents: A world-wide population-based study (CONCORD). Lancet Oncology 9(8):730–756.
Cutler, D. M., A. B. Rosen, and S. Vijan. 2006. The value of medical spending in the United States, 1960–2000. New England Journal of Medicine 355(9):920–927.
Doonon, M. 1998. Issue brief: Will alcohol be the next tobacco? Boston: The Massachusetts Health Policy Forum.
Eddy, D. M. 1984. Variations in physician practice: The role of uncertainty. Health Affairs 3:74.
Eddy, D. M. 1992. A manual for assessing health practices and designing practice policies: The explicit approach. Philadelphia, PA: The American College of Physicians.
Ferguson, J. H. 1991. Forward. Research on the delivery of medical care using hospital firms. Proceedings of a workshop, April 30 and May 1, 1990, Bethesda, MD. Medical Care 29(7 Suppl.):JS1–JS2.
Groopman, J. 2007. How doctors think. Boston, MA: Houghton Mifflin.
IOM (Institute of Medicine). 1985. Assessing medical technologies. Washington, DC: National Academy Press.
IOM. 2000. To err is human: Building a safer health system. Washington, DC: National Academy Press.
KFF (Kaiser Family Foundation). 2006. Wall Street Journal (February 22). (2005 data.)
Lawrence, R. S., and A. D. Mickalide. 1987. Preventive services in clinical practice: Designing the periodic health examination. JAMA 257:2205–2207.
Levy, P. 2008. Adapting process-improvement techniques in an academic medical center. The Bridge 38(1):6–9.
Lomas, J., G. M. Anderson, K. Domnick-Pierre, E. Vayda, M. W. Enkin, and W. J. Hannah. 1989. Do practice guidelines guide practice? New England Journal of Medicine 321:1306–1311.
McGinnis, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. JAMA 270(18):2207–2212.
McGinnis, J. M., P. Williams-Russo, and J. R. Knickman. 2002. The case for more active policy attention to health promotion. Health Affairs 21(2):78–93.
McGlynn, E. A., S. M. Asch, J. Adams, J. Keesey, J. Hicks, A. DeCristofaro, and E. A. Kerr. 2003. The quality of health care delivered to adults in the United States. New England Journal of Medicine 348(26):2635–2645.
McKie, J., and J. Richardson. 2003. The rule of rescue. Social Science & Medicine 56(12):2407–2419.
Miller, G. A. 1956. The magic number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review 63(2):81–97.
Morris, A. H., C. J. Wallace, R. L. Menlove, T. P. Clemmer, J. F. Orme, L. K. Weaver, N. C. Dean, F. Thomas, T. D. East, N. L. Pace, M. R. Suchyta, E. Beck, M. Bombino, D. F. Sittig, S. Böhm, B. Hoffmann, H. Becks, S. Butler, J. Pearl, and B. Rasmusson. 1994. Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine 149:295–305.
NAE (National Academy of Engineering)/IOM. 2005. Building a better delivery system. Washington, DC: The National Academies Press.
National Center for Health Statistics. 2000. Health, United States, 2000 with adolescent health chartbook. DHHS Publication No. (PHS) 2000-1232-1. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, p. 7.
National Library of Medicine. 2006. Fact sheet MEDLINE. http://www.nlm.nih.gov/pubs/factsheets/medline.html (accessed April 22, 2010).
Nolte, E., and M. McKee. 2003. Measuring the health of nations: Analysis of mortality amenable to health care. British Medical Journal 327(7424):1129–1133.
Norman, D. 1988. The design of everyday things. New York: Currency Doubleday. OECD (Organisation for Economic Co-operation and Development). 2006. OECD health data—OECD website. http://www.oecd.org/dataoecd/29/52/36960035.pdf (accessed June 22, 2010).
Peterson, C. L., and R. Burton. 2007. U.S. healthcare spending: Comparison with other OECD countries. Congressional Research Service Report for Congress, September 17, order code RL34715.
Porter, R. 1997. The greatest benefit to mankind: A medical history of humanity. New York: W. W. Norton.
Reinhardt, U. W., P. S. Hussey, and G. F. Anderson. 2002. Cross-national comparisons of health systems using OECD data, 1999. Health Affairs 21(3):169–181.
Rosenberg, C. E. 1987. The care of strangers: The rise of the American hospital system. New York: Basic Books.
Schoen, C., R. Osborn, M. M. Doty, M. Bishop, J. Peugh, and N. Murukutla. 2007. Toward higher-performance health systems: Adults health care experiences in 7 countries, 2007. Health Affairs 26(6):w717–w734.
Shaneyfelt, T. M. 2001. Building bridges to quality. JAMA 286(20):2600–2601.
Starr, P. 1984. The social transformation of American medicine. New York: Basic Books (The Perseus Books Group).
Szilagyi, D. E. 1965. In defense of the art of medicine. Archives of Surgery 91:707–711.
Verdecchia, A., S. Francisci, H. Brenner, G. Gatta, A. Micheli, L. Mangone, I. Kunkler, and the EUROCARE-4 Working Group. 2007. Recent cancer survival in Europe: A 2000–02 period analysis of EUROCARE-4 data. Lancet Oncology 8(9):784–796.
Wildavsky, A. 1977. Doing better and feeling worse: The political pathology of health policy. In J. H. Knowles, ed., Doing better and feeling worse: Health in the United States (pp. 105–123). New York: W. W. Norton & Co.
Williamson, J., P. Goldschmidt, and I. Jillson. 1979. Medical practice information demonstration project: Final report. Office of the Assistant Secretary of Health, DHEW, Contract #282–77–0068GS. Baltimore, MD: Policy Research Inc.
This page intentionally left blank.




































