4
Determinants of Gestational Weight Gain
The total amount of weight gain during pregnancy is determined by many factors. Aside from physiological factors (discussed in Chapter 2); psychological, behavioral, family, social, cultural, and environmental factors can also have an impact on gestational weight gain (GWG). Understanding these factors as determinants of GWG is an important component of revising weight gain guidelines for women during pregnancy. Several conceptual models guided the committee’s consideration of determinants of GWG. The ecological perspective recognizes that health behavior such as GWG is influenced at multiple levels. Brofenbrenner (1979) identified multiple levels of environmental influence on health behavior in general:
-
The microsystem—face-to-face interactions in specific settings, such as family, school, or a peer group;
-
The mesosystem (a system of microsystems)—the interrelations among the various settings in which the individual is involved, such as that between the family and the workplace;
-
The exosystem—the larger social system in which the individual is embedded, such as the extended family or community; and
-
The macrosystem—cultural values and beliefs, such as cultural beliefs about GWG.
Other models that recognize the multiple determinants of health behavior or outcome include the health field model, which identifies multiple domains including the physical and social environments that exert influ-
ences on health behavior and outcome, and the epidemiological model, which describes a triad of epidemiologic factors to model the complex and interrelated factors contributing to the increasing rate of obesity in the United States and other countries. One of the triad components describes an “obesogenic” environment as “the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations” (Swinburn and Egger, 2002). This obesogenic environment includes physical, economic, policy, and sociocultural factors that can influence eating and physical activity behaviors.
Collectively, these models place emphasis on how the health of individuals is influenced by not only physiological functioning and genetic predisposition, but by a complex interplay of these biological determinants with social and familial relationships, environmental influences, and broader social and economic contexts over the life course. They further suggest that intervention efforts to change health behavior or outcome, such as GWG, should address not only “downstream” individual-level phenomena (e.g., physiologic pathways to disease, individual and lifestyle factors) and “mainstream” factors (e.g., population-based interventions), but also “upstream,” societal-level phenomena (e.g., public policies) (IOM, 2000).
Another model, the life-course perspective (Kuh and Ben-Shlomo, 1997), perceives life not in disconnected stages, but as an integrated continuum; it recognizes that each stage of life is influenced by the life stages that precede it, and it, in turn, influences the life stages that follow (see Chapter 6 for detailed discussion).
Some of the most significant determinants of GWG at multiple levels (social/institutional, environmental, neighborhood/community, interpersonal/family, and individual levels) occur across the life course (Figure 4-1). The following discussion begins with a review of the evidence for a direct relationship between a given determinant (identified in Figure 1-1) and GWG. Where data are lacking, rationale are provided for why the committee thinks that it is potentially an important determinant that merits further research. The committee’s review of evidence (tabulated in Appendix D) included both epidemiologic and clinical studies. Inasmuch as this research discipline is focused largely on observational studies the committee recognized the need for proof of causality for determinants and outcomes significantly associated with GWG.
SOCIETAL/INSTITUTIONAL DETERMINANTS
The committee evaluated the evidence of the impact of four societal/institutional determinants on GWG: media, culture and acculturation, health services (e.g., the type of advice that pregnant women receive about GWG), and policy. The committee recognized that understanding how these factors impact GWG, for example how cultural norms and beliefs may
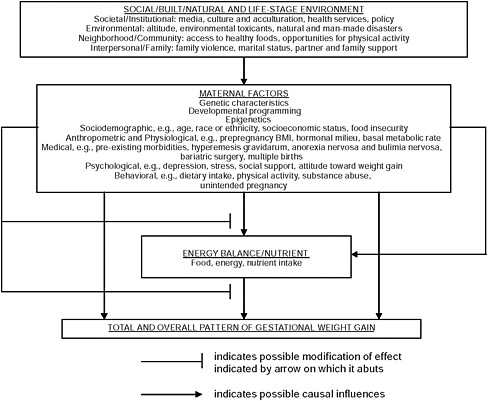
FIGURE 4-1 Schematic summary of determinants associated with GWG.
impact a woman’s eating habits during pregnancy, is necessary for developing effective weight gain recommendations. Although the committee noted some plausible associations between each of these factors and GWG, the evidence is inconclusive and the contributions of these factors to GWG (and subsequent outcomes) unclear.
Media
The committee was unable to identify studies that specifically examined the media’s influence on GWG. From a life-course perspective, however, it is plausible that the media may exert influence on GWG by shaping eating and exercise habits that become established long before pregnancy. Several previous reports have documented the influence of advertising and marketing on children’s food, beverage, and sedentary-pursuit choices in ways that can adversely affect energy balance (Kunkel, 2001; IOM, 2006). In an extensive systematic literature review, Hastings et al. (2003) concluded that food advertisements promote food purchase requests by children to parents, have an impact on children’s product and brand preferences, and
affect consumption behavior. Other studies have shown that the media can promote sedentary behaviors, such as television watching, that may adversely affect energy balance (Gortmaker et al., 1996, 1999; Robinson, 1999; IOM, 2005; Epstein et al., 2008). Poor eating habits and sedentary behaviors shaped during childhood and adolescence may be carried into young adulthood and continued into pregnancy, with the potential to affect GWG indirectly. Moreover, by influencing energy balance over the long run these habits and behaviors may also have an impact on prepregnancy body mass index (BMI) as well as other biological determinants of GWG.
Not all media influences are negative. Media can be used to convey consumer information and public health messages, such as those regarding youth smoking, and seat belt and child car seat use. However, social marketing programs that use the media to promote physical activity or healthy diet in adults, whether as part of a mass media-focused effort or a broader multi-component campaign, tend to produce mixed results. The most successful social marketing programs have had higher funding, have been better sustained, and were shaped by formative research (IOM, 2006).
Culture and Acculturation
Although it is plausible that cultural norms and beliefs may influence dietary behavior and physical activities, thereby affecting energy balance and GWG, the committee was unable to identify studies that examined specifically the effects of culture and acculturation factors on GWG. For example, it is widely believed by women of all ages, ethnic groups, and income and education levels that the consumption of certain foods marks a child before birth, which may then lead to certain food preferences and avoidances (IOM, 1992; King, 2000). As another example, most women know that low GWG will produce a small infant, which will be delivered more easily than a larger one. In some cultures this knowledge may encourage women to “eat down” in late pregnancy in order to avoid a difficult birth (King, 2000).
Acculturation, the process in which members of one cultural group adopt the beliefs and behaviors of another, is often associated with adoption of unhealthy behaviors, including food choices. Using nativity or duration of residence in the United States as a proxy for acculturation, several studies have found greater rates of overweight and obesity among children and nonpregnant adults who are more acculturated, compared to their less acculturated counterparts (Lizarzaburu and Palinkas, 2002; Hubert et al., 2005; Hernandez-Valero et al., 2007; Fuentes-Afflick and Hessol, 2008). For example, in a population-based study of 462 mothers in California, Schaffer et al. (1998) found that in the 3 months before pregnancy, foreign-born Latinas had the lowest contribution of fat to total energy intake and the highest dietary intake of carbohydrate, cholesterol, fiber, grain products,
protein foods, folate, vitamin C, iron, and zinc, compared to the dietary intake of white non-Latinas and U.S.-born Latinas. Other researchers have also documented increased risk for adverse birth outcomes, including preterm birth and low birth weight, among U.S.-born women compared to foreign-born women of the same ethnic origin (Ventura and Taffel, 1985; Scribner and Dwyer, 1989; Cabral et al., 1990; Kleinman et al., 1991; Rumbaut and Weeks, 1996; Singh and Yu, 1996; Fuentes-Afflick and Lurie, 1997; Jones and Bond, 1999; Callister and Birkhead, 2002; Baker and Hellerstedt, 2006). However, most of these studies do not report GWG, and so the contribution of GWG to adverse outcomes is unknown.
Health Services
Although many researchers have studied the impact of GWG advice on actual weight gains and although the U.S. Public Health Service Expert Panel on the Content of Prenatal Care recommended that pregnant women receive advice on gaining an appropriate amount of weight during pregnancy, the influence of weight gain advice on GWG has not been conclusively demonstrated (HHS, 1989). Several intervention studies have been conducted using nutrition advice alone (Orstead et al., 1985; Bruce and Tchabo, 1989) or such advice linked with home visits by nutritionists and supplemental food (Rush, 1981; Bruce and Tchabo, 1989), a nurse home visitation program (Olds et al., 1986), and the provision of prenatal care through multidisciplinary rather than traditional clinics (Morris et al., 1993). In three of the studies (Rush, 1981; Olds et al., 1986; Morris et al., 1993) the differences in mean GWG between intervention and control groups were not statistically significant. In two other studies (Orstead et al., 1985; Bruce and Tchabo, 1989) intervention groups gained significantly more weight than the control groups; however, the findings may be limited by gestational age bias. Additionally, most of these studies reported only mean GWG with no comparisons among different categories of pregravid BMI, further limiting interpretation of the findings. Brown et al. (1992) developed a prenatal weight gain intervention program based on social marketing methods; while circumstances arose that hampered full evaluation of the program, preliminary evidence suggests that GWG and birth weight of African Americans in the intervention group did not differ significantly from those of whites, while both weight gain and birth weight were significantly lower in African Americans than in whites in the control group.
Hickey (2000) identified several potential problems with the validity of previous studies on prenatal weight gain advice and actual GWG. These include, in addition to differences in pregravid nutritional status and BMI, issues such as self-selection bias, recall bias, differences in time during gestation when nutrition advice was given, variation in content and frequency of advice, the pairing of advice with other food or nonfood interventions,
individual and social characteristics of the provider as contrasted with those of the pregnant woman, and racial/ethnic and socioeconomic disparities in weight gain advice.
Policy
For the purpose of this report, policy is defined broadly to include principles, guidelines, or plans adopted by an organization to guide decisions, actions, and other matters. An example of how policy can influence GWG is the weight gain recommendations from the report, Nutrition During Pregnancy (IOM, 1990) and subsequent endorsement of the report’s recommendations and guidelines by obstetric organizations in the United States and many other countries.
In some cases, it is not clear what type of advice is being provided. For example, in a 2005 cross-sectional survey mailed to 1,806 practicing members of the American College of Obstetricians and Gynecologists (ACOG), more than 85 percent of the 900 respondents reported counseling their patients about GWG often or most of the time (ACOG, 2005). The survey did not, however, assess the respondents’ knowledge of the IOM (1990) guidelines or the content of counseling (Power et al., 2006).
The few studies that have examined the advice given for GWG, however, have shown that women often receive inconsistent or erroneous advice. In a survey of approximately 2,300 women, Cogswell et al. (1999) reported that, of the 1,643 women who recalled weight gain advice, 14 percent reported being advised to gain less than the recommended levels, and 22 percent were advised to gain more and that provider advice to gain either below or above the recommended levels was associated with actual weight gain below the recommendations, respectively (both associations had an adjusted odds ratio of 3.6). So about one-third of women in this study reported receiving no advice or inappropriate advice from health professionals regarding GWG, and they followed that advice. Added to that, 27 percent of women reported receiving no advice about GWG. Altogether nearly two-thirds (63 percent) of women in this study reported receiving either inappropriate advice or no advice at all. Only 39 percent recalled receiving advice that fell within the IOM (1990) guidelines.
In a more recent study, Stotland et al. (2005) found that 79 percent of the nearly 1,200 women reported a target GWG (i.e., how much weight women think they should gain during pregnancy) that fell within the IOM (1990) guidelines. The authors speculated that their figures were higher than those reported in Cogswell et al. (1999). Still, Stotland et al. (2005) found that one-third (33 percent) of women received no advice from health professionals regarding GWG, and less than half (49 percent) reported receiving advice within guidelines.
Another example of policy influencing GWG is the Special Supplemental Food Program for Women, Infants, and Children (WIC). Rush et al. (1988) conducted a national evaluation of WIC programs and found that a reversal of low weight gain in early pregnancy and greater total weight gain during pregnancy occurred among women who enrolled in WIC compared with controls. They also found greater intake of protein, iron, calcium, vitamin C, and energy among WIC participants. However, subsequent evaluations (Joyce et al., 2008) have challenged these earlier findings and found more limited associations between WIC participation and GWG. Nonetheless, it is possible that policy that increases food access would have an impact on dietary pattern and GWG.
Policy that does not directly affect pregnant women can also have an effect on GWG. Examples include policy recommendations to restrict food and beverage advertising and marketing to young children, to develop and implement nutritional standards for all competitive foods and beverages sold or served in schools, or to promote physical activity in schools (IOM, 2007). These policies can influence the development of children’s eating and exercise habits, which will be important later in life.
ENVIRONMENTAL DETERMINANTS
The committee examined three potential environmental determinants of GWG: exposure to high altitude, exposure to environmental toxicants, and exposure to a natural or human-caused disaster.
Altitude
Evidence that altitude effects GWG is inconsistent. Jensen and Moore (1997) examined the effect of high altitude on GWG and birth weight using Colorado birth certificates and found no significant difference in GWG among women residing at 3,000 to 5,000 feet; 5,000 to 7,000 feet; 7,000 to 9,000 feet; and 9,000 to 11,000 feet; they did find, however, that mean birth weight, decreased with increasing altitude, a trend that was independent of GWG and not interactive with gestational age, parity, maternal smoking, pregnancy-induced hypertension, and other factors associated with birth weight (Jensen and Moore, 1997).
Environmental Toxicants
The committee was unable to identify studies that examined specifically the effects of exposures to environmental toxicants on GWG. There is some evidence linking environmental contaminants such as organophosphate and organochlorine compounds to fetal growth, but the evidence is
inconsistent (Dar et al., 1992; Wolff et al., 2007). Additional research may better define the relationships among environmental exposures, GWG, and fetal growth.
Natural and Man-made Disasters
The committee was unable to identify studies that examined specifically the effects of natural or man-made disasters on GWG. However, it is plausible that disasters can affect GWG indirectly by influencing resource availability (including food supply), health care access, and stress levels (Callaghan et al., 2007). Several studies have documented the impact of disasters on pregnancy outcomes such as preterm birth (Weissman et al., 1989; Cordero, 1993; Glynn et al., 2001; Lederman et al., 2004) and fetal growth restriction (Eskenazi et al., 2007; Landrigan et al., 2008); however, it remains unclear whether these adverse outcomes were caused by low GWG.
NEIGHBORHOOD/COMMUNITY DETERMINANTS
The committee considered two potential neighborhood/community determinants of GWG: access to healthy foods and opportunities for physical activity.
Access to Healthy Foods
Evidence for a direct influence of neighborhood or community factors, such as access to healthy foods, on GWG is lacking. However, because appropriate nutrient intake and weight gain during pregnancy requires a safe and adequate food supply, it is likely that women who live in areas where residents have poor accessibility to foods may be at increased risk for inadequate or inappropriate GWG and associated poor pregnancy outcomes. (See Chapter 2 for trends in dietary practices and Appendix B for supplemental information.) The committee identified only two relevant studies. Laraia et al. (2004) investigated associations between the distance of a supermarket from home and diet quality of pregnant women, measured by a Diet Quality Index (DQI). They found that women who lived more than 4 miles from a supermarket had a two-fold greater risk of falling into the lowest DQI quartile compared to women who lived ≤ 2 miles from a supermarket, but the authors also did not report on GWG. More recently, in a study of urban retail food markets and birth weight outcomes in upstate New York, Lane et al. (2008) found that pregnant women who lived in proximity to urban retail corner markets without fresh produce, dairy, and other healthy foods had significantly more low birth weight infants compared to women who had access to supermarkets where healthy foods
were available. These findings were independent of income level; however, the study did not report on GWG.
Opportunities for Physical Activity
Although a growing body of evidence has demonstrated the role of the built environment for populations at high risk for obesity (see Chapter 2 for trends in physical activity), only one study was identified that examined the relationship between neighborhood contexts and GWG. Laraia et al. (2007) conducted a study of neighborhood factors associated with physical activity and weight gain during pregnancy. They found that social spaces, defined as the presence of parks, sidewalks, and porches as well as the presence of people, including nonresidential visitors, was associated with decreased odds for inadequate or excessive GWG. The social spaces scale was also associated with decreased odds of living greater than 3 miles from a supermarket. These findings suggest that neighborhood environments can influence GWG by providing access to healthy foods and opportunities for physical activities.
INTERPERSONAL/FAMILY DETERMINANTS
The committee considered three types of interpersonal/family factors and their potential impact on GWG: family violence, marital status, and partner and family support.
Family Violence
Several studies examined GWG in the context of family violence (Parker et al., 1994; McFarlane et al., 1996; Siega-Riz and Hobel, 1997; Moraes et al., 2006). In a clinic sample of 4,791 Hispanic women in Los Angeles, Siega-Riz and Hobel (1997) found that physical abuse was associated with a greater than threefold risk for inadequate GWG among obese and overweight women. Moraes et al. (2006) found in a study of 394 pregnant women in Brazil that those with the highest physical abuse score gained, on average, 3 to 4 kg less than women unexposed to intimate partner violence. Boy and Salihu (2004) conducted a systematic review and found that abused pregnant women had less GWG than non-abused women. These studies suggest an association between intimate partner violence and insufficient GWG.
Marital Status
Several studies have examined the relationship between marital status and GWG. Using 1992 U.S. national data, Kleinman et al. (1991) and
Ventura (1994), found that unmarried mothers were more likely than married mothers to gain less than 7.3 kg during pregnancy. Olsen and Strawderman (2003) found in a cohort of 622 healthy adult women that 38 percent of married women had gained above the IOM (1990) guidelines, compared to 42 percent of women who were separated or divorced, and 48 percent of single women. They also found that 21 percent of married women had gained below the IOM (1990) guidelines, compared to 23 percent for single women and 29 percent for women who were separated or divorced. Thus married women were more likely to gain within the IOM (1990) recommended weight gain range than single or separated/divorced women.
Partner and Family Support
The committee identified only two studies pertaining to the relationship between partner support and GWG. In the first, Dipietro et al. (2003) examined the influences of partner support on attitudes or behaviors toward GWG. In a cross-sectional study of 130 women with low-risk pregnancies, they found that partner support was associated with negative pregnancy body image, but not with attitudes or behaviors toward GWG. Siega-Riz and Hobel (1997) evaluated a clinic sample of 4,791 Hispanic women in Los Angeles and found that receiving financial support from the infant’s father was significantly associated with decreased risk of poor GWG for overweight and obese women, but not for underweight or normal weight women.
Again, the committee only identified two studies pertaining to the influence of family support on GWG. In a sample of 99 pregnant adolescents, Stevens-Simon et al. (1993b) found that attitudes toward GWG were directly related to their perceived family support; negative weight gain attitudes were most common among heavier adolescents, depressed adolescents, and adolescents who did not perceive their families as supportive. In a study of 46 pregnant Mexican American adolescents, Gutierrez (1999) reported that the most powerful factors contributing to good food practices during pregnancy were maternal concern about the well-being of the infant, role of motherhood, and family support system; the investigators did not report on the contribution of family support to either GWG attitude or actual GWG.
MATERNAL FACTORS
The following discussion summarizes the committee’s review of the evidence on several different types of maternal factors and their potential impact on GWG. This evidence includes sociodemographic factors, such
as age and race/ethnicity; physiological factors, some of which are also discussed in depth elsewhere in this report, and genetic factors known to impact GWG and those that may impact GWG because of their known influence on birth weight; and developmental and epigenetic programming in the mother, which may influence how a woman responds later in life.
Sociodemographic Factors
Gestational Weight Gain in Adolescents
Adolescent pregnancy has been associated with increased risk of preterm delivery, low birth weight, SGA births, and increased risk of neonatal mortality, although reported risk associations vary (Chen et al., 2007). To reduce these risks, the IOM (1990) report recommended that pregnant adolescents gain weight within the ranges for adult women unless they were under 16 years of age or less than 2 years post-menarche. In either of these cases, adolescents were encouraged to gain at the upper limits of the GWG guidelines for their prepregnancy BMI category.
The youngest adolescents as well as somewhat older adolescents who conceive soon after menarche may still be growing themselves (Scholl and Hediger, 1993). Even girls who become pregnant for a second time during adolescence may still be growing. Scholl et al. (1990) showed that adolescents who were still growing during a first pregnancy delivered infants whose birth weight did not differ from those who were not growing. This was not true among adolescents who were still growing during a second pregnancy; their infants were significantly lighter at birth than those who were not growing themselves. The possibility of a competition for nutrients between the still-growing adolescent gravida and her fetus has been advanced as an argument for recommending relatively higher gains for at least some pregnant adolescents. What has been found instead is that still-growing adolescents are not mobilizing their fat gain during pregnancy to enhance fetal growth but, rather, are supporting the continued development of their own fat stores (Scholl et al., 1994).
In a retrospective review of natality data from 2000, Howie et al. (2003) reported an increased likelihood for excessive GWG among adolescents compared to older women. Other authors have corroborated that younger adolescents have a higher GWG compared to older adolescents and adults, but whether the infant benefits from this greater weight gain is not yet clear (Hediger et al., 1990; Scholl et al., 1990; Stevens-Simon et al., 1993a). This is in part because—as is also the case for adult women—increases in GWG not only reduce the risk of delivering a low birth weight infant but also increase the risk of delivering a macrosomic infant (Scholl
et al., 1988). Nielsen et al. (2006) showed that birth weight outcomes improved in all prepregnancy BMI groups when GWG increased from below to within the lower half of the weight gain recommended by the IOM (1990) in a cohort of 815 pregnant African American adolescents. Further gains were not beneficial, particularly for infants of adolescents with a high prepregnancy BMI.
The possibility that adolescents who gained at the upper end of the range for their BMI category might have an excess risk of postpartum weight retention or the later development of obesity was not considered in formulating the 1990 guidelines, but has long been recognized as a possible downside of recommending relatively high weight gains for them (McAnarney and Stevens-Simon, 1993). Adolescents who have given birth are heavier (Gigante et al., 2005) with more adipose tissue (Gunderson et al., 2009) than adolescents who have not. Gestational weight gain was a significant predictor of increase in BMI 6 and 9 years post delivery in all prepregnancy BMI categories among the 330 primiparous black adolescents studied by Groth (2008). In addition, those who gained above the IOM (1990) guidelines were more likely to have become obese by 9 years post delivery than those who gained within the guidelines.
In summary, the relationship of GWG to fetal and birth outcomes, postpartum weight retention, and risk for future overweight/obesity appears to be generally similar to that for adult women. However, information on these subjects is more limited for pregnancy among adolescents, particularly younger adolescents, than it is for adult women. Data generated since the IOM (1990) report, particularly related to the risk of developing postpartum weight retention and obesity in adult women who had been pregnant as young adolescents, support the recommendation that “until more is known, adolescents less than two years post-menarche should be advised to stay within the IOM-recommended BMI-specific weight range without either restricting weight or encouraging weight gain at the upper end of the range” (Suitor, 1997).
Gestational Weight Gain in Older Women
Increased maternal age is significantly associated with risk for adverse pregnancy outcomes, including stillbirth (Fretts, 2005; Reddy et al., 2006), low birth weight, preterm birth, and small-for-gestational age (SGA) birth (Cnattingius et al., 1992; Delpisheh et al., 2008). In addition to poor outcomes, pregnancy in older women is also associated with increased risk for pregnancy complications, e.g., hypertension, diabetes, placenta previa, and placental abruption (Joseph et al., 2005).
In a study of obese and non-obese women who were pregnant, Gross et al. (1980) found that a greater proportion of obese subjects were older
and of higher parity than non-obese subjects. The obese subjects also had higher rates of chronic hypertension, diabetes, and inadequate GWG. Prysak et al. (1995), in a retrospective comparison of pregnancy characteristics between older (≥ 35 years old) and younger (25-29 years old) nulliparous women, found that the older women had significantly lower mean GWG than the younger women. In addition, obesity was significantly greater in the older compared to the younger women.
Endres et al. (1987) evaluated nutrient intake, prepregnancy weight, and GWG in pregnant women enrolled in the WIC program who were over 35 years of age versus adolescents aged 15-18 years. The investigators calculated prepregnancy BMI for both groups and found more than 50 percent of the older women were identified as obese prior to pregnancy. The study found no significant difference in total nutrient intake between the groups (neither met the Recommended Dietary Allowances [RDAs]), but the younger women had higher mean energy intakes (p = 0.006) and greater cumulative GWG in the third trimester (9.5 kg versus 7.6 kg) than the older women. In sum, several studies reported higher prepregnancy BMI and lower GWG among older women, compared to their younger counterparts. The contributions of GWG to birth outcomes, postpartum weight retention, and subsequent overweight/obesity among older women remain unclear.
Table 4-1 summarizes reports from the past three decades on GWG by age and racial/ethnic group.
Race or Ethnicity
Few studies have examined racial/ethnic differences in GWG, and even fewer studies have considered the influence of the many possible determinants of GWG among different racial/ethnic groups or alternatively, adjusted for race/ethnicity in their analyses. Caulfield et al. (1996), for example, found that among 2,617 black and 1,253 white women delivering at a university hospital during 1987-1989 only 28.2 and 32.5 percent of black and white women, respectively, gained within the ranges recommended by IOM (1990).
Black women are at increased risk for gaining less weight than recommended, when controlled for maternal prepregnancy BMI, height, parity, education, smoking, hypertension, duration of pregnancy, and fetal sex. Chu et al. (2009) assessed the amount of GWG among 52,988 underweight, normal weight, overweight, and obese U.S. women who delivered a singleton, full-term infant in 2004-2005 using Pregnancy Risk Assessment Monitoring System (PRAMS) data (2004-2005). They found that black women were significantly more likely than white women to gain less than 15 pounds, but less likely than white women to gain more than 34 pounds.
TABLE 4-1 Effect of Chronological Maternal Age on GWG
|
Reference |
Age (yrs) |
Racial/Ethnic Group |
Number in Sample |
Weight Gain (kg) |
Coefficient of Variation, % |
|
Ancri et al. (1977) |
12-17 |
Caucasian (one black woman) |
26 |
13.4 |
26 |
|
|
18-19 |
|
22 |
12.4 |
31 |
|
|
20-24 |
|
24 |
11.1 |
17 |
|
|
25-32 |
|
26 |
10.7 |
18 |
|
Frisancho et al. (1983) |
12-13 |
Latin American |
28 |
9.0 |
18 |
|
|
14 |
|
104 |
9.8 |
22 |
|
|
15 |
|
296 |
9.9 |
26 |
|
|
16 |
|
565 |
9.7 |
25 |
|
|
17 |
|
229 |
10.0 |
26 |
|
|
18-25 |
|
46 |
9.7 |
16 |
|
Horon et al. (1983) |
< 16 |
Black, White |
422 |
12.5 |
NRa |
|
|
20-24 |
|
422 |
12.5 |
NR |
|
Loris et al. (1985) |
13-15.9 |
Mixed group |
18 |
17.2 |
23 |
|
|
16-17.9 |
|
84 |
17.1 |
40 |
|
|
18-19.9 |
|
25 |
17.3 |
54 |
|
Meserole et al. (1984) |
13-15 |
Mixed group |
24 |
14.5 |
32 |
|
|
16-17 |
|
25 |
17.9 |
35 |
|
Endres et al. (1985) |
15-18 |
Mixed group |
46 |
12.0 |
NR |
|
|
19-30 |
|
198 |
11.0 |
NR |
|
Muscati et al. (1988) |
14-17 |
NR |
90 |
16.5 |
36 |
|
|
18-19 |
|
135 |
15.1 |
36 |
|
|
20-35 |
|
461 |
13.8 |
39 |
|
Scholl et al. (1988) |
16.9 ± 1.3b |
Black, White, Hispanic |
696 |
14.7 |
39 |
|
Haiek and Lederman (1989) |
< 16 |
Black Americans, Black |
90 |
14.6 |
NR |
|
|
19-30 |
Latin Americans, White Non-Latin Americans, White Latin Americans |
90 |
16.9 |
NR |
|
Hediger et al. (1990) |
≤ 18 |
Puerto Rican |
304 |
13.7 |
± 5.6b |
|
|
|
Black |
501 |
13.8 |
± 5.7b |
|
|
|
White |
514 |
15.9 |
± 5.7b |
|
Stevens-Simon et al. (1993a) |
< 16 |
N/A |
52 |
14.9 |
± 5.9b |
|
|
16-19 |
|
89 |
13.9 |
± 6.0b |
|
Prysak et al. (1995) |
25-29 |
White or other |
1,054 |
15.0 |
± 4.9b |
|
|
≥ 35 |
|
890 |
14.2 |
± 5.4b |
|
Gutierrez (1999) |
13-18 |
Mexican American |
46 |
14.5 |
± 4.5 |
|
Nielsen et al. (2006) |
< 17 |
African American |
776 |
14.5 |
± 6.9 |
|
aNR = Not reported. bStandard deviation. SOURCE: Modified from IOM, 1990. |
|||||
In their review of birth records of 913,320 singleton births in New York City from 1995 to 2003, Stein (information contributed to the committee in consultation with Stein [see Appendix G, Part III]) found that Asian and non-Hispanic black women were more likely to gain 0 to 9 kg, whereas Hispanic and non-Hispanic white women were more likely to gain 20+ kg during pregnancy. Table 4-2 presents GWG among women of different race and ethnicity in this study population.
Taken together, the limited data on the influence of race/ethnicity on GWG is suggestive of inadequate GWG among some racial/ethnic groups. However, the paucity of data on a national level and the lack of observational studies based on prepregnancy BMI preclude drawing any conclusions about the influence of race/ethnicity on GWG (see Chapter 2 and Figure 2-6 for trends in GWG for racial/ethnic groups by prepregnancy BMI).
Socioeconomic Status
The committee also found few studies that have reported GWG by socioeconomic status (SES), and even fewer that considered the influence of the many possible determinants of GWG among different SES groups; or alternatively, adjusted for SES in their analyses (see Appendix D). Using 2004-2005 PRAMS data, Chu et al. (2009) found that women with less than 12 years of education were more likely to gain less than 15 pounds, and less likely to gain more than 34 pounds, compared to women with more than 12 years of education (Table 4-3).
TABLE 4-2 Bivariate Association Between Gestational Weight Gain and Race or Ethnicity Among Singleton Births, New York City, 1995-2003, N = 913,290
|
Maternal race or ethnicity |
Gestational Weight Gain |
|||
|
0-9 kg N = 234,764 N (percent) |
10-14 kg N = 333,968 N (percent) |
15-19 kg N = 223,366 N (percent) |
20+ kg N = 121,192 N (percent) |
|
|
Non-Hispanic white |
56,817 (20.3) |
112,814 (40.4) |
75,274 (26.9) |
34,517 (12.3) |
|
Non-Hispanic black |
69,294 (29.2) |
77,868 (32.8) |
54,412 (22.9) |
35,899 (15.1) |
|
Hispanic |
78,528 (26.9) |
99,705 (34.1) |
70,694 (24.2) |
43,513 (14.9) |
|
Asian |
29,086 (29.0) |
42,137 (41.9) |
22,251 (22.1) |
6,964 (6.9) |
|
Other |
1,069 (30.1) |
1,444 (40.7) |
735 (20.7) |
299 (8.4) |
|
SOURCE: Information contributed to the committee in consultation with C. Stein (see Appendix G, Part III). |
||||
TABLE 4-3 Gestational Weight Gain (pounds) by Selected Characteristics Among Women Delivering Full-term, Singleton Births (underweight women excluded), PRAMS, 2004-2005
|
Characteristic |
≤ 14 (n = 8,091)a |
15-24 (n = 9,970)a |
25-34 (n = 14,545)a |
35-44 (n = 10,311)a |
≥ 45 (n = 7,112)a |
|||||
|
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
|
|
Age, yr (n)a |
||||||||||
|
14-19 (5,249) |
15.4 |
0.8 |
16.9 |
0.8 |
25.7 |
0.9 |
20.4 |
0.9 |
21.7 |
0.9 |
|
20-24 (12,477) |
15.3 |
0.5 |
19.3 |
0.5 |
26.7 |
0.6 |
20.3 |
0.5 |
18.4 |
0.5 |
|
25-29 (13,483) |
15.8 |
0.5 |
18.6 |
0.5 |
28.5 |
0.6 |
22.2 |
0.5 |
15.0 |
0.5 |
|
30-34 (11,169) |
15.1 |
0.5 |
18.6 |
0.5 |
30.8 |
0.6 |
22.1 |
0.6 |
13.4 |
0.5 |
|
≥ 35 (7,651) |
15.9 |
0.6 |
19.8 |
0.7 |
32.2 |
0.8 |
20.8 |
0.7 |
11.2 |
0.6 |
|
Race/ethnicity |
||||||||||
|
White (27,393) |
13.3 |
0.3 |
17.4 |
0.3 |
30.0 |
0.4 |
22.7 |
0.4 |
16.6 |
0.3 |
|
Black (7,790) |
21.7 |
0.7 |
21.1 |
0.6 |
23.9 |
0.7 |
18.2 |
0.6 |
15.1 |
0.6 |
|
Hispanic (7,428) |
17.3 |
0.7 |
21.2 |
0.7 |
29.3 |
0.8 |
20.1 |
0.7 |
12.1 |
0.6 |
|
Other (7,221) |
16.4 |
0.8 |
19.9 |
0.9 |
30.6 |
1.1 |
19.8 |
0.9 |
13.5 |
0.8 |
|
Education, y (n) |
||||||||||
|
< 12 (8,154) |
19.6 |
0.7 |
21.1 |
0.7 |
25.7 |
0.8 |
18.0 |
0.7 |
15.7 |
0.7 |
|
12 (15,550) |
17.3 |
0.5 |
19.4 |
0.5 |
26.0 |
0.5 |
19.9 |
0.5 |
17.4 |
0.5 |
|
> 12 (25,667) |
12.7 |
0.3 |
17.8 |
0.3 |
31.7 |
0.4 |
23.3 |
0.4 |
14.5 |
0.3 |
|
Parity (n) |
||||||||||
|
0 (20,782) |
11.5 |
0.3 |
15.9 |
0.4 |
28.3 |
0.5 |
24.3 |
0.4 |
20.1 |
0.4 |
|
1-2 (23,911) |
16.8 |
0.4 |
20.5 |
0.4 |
29.8 |
0.4 |
20.3 |
0.4 |
12.7 |
0.3 |
|
≥ 3 (5,100) |
23.2 |
0.9 |
22.9 |
0.9 |
28.3 |
0.9 |
14.8 |
0.7 |
10.8 |
0.7 |
|
Total (50,029) |
15.5 |
0.2 |
18.8 |
0.3 |
28.9 |
0.3 |
21.4 |
0.3 |
15.5 |
0.2 |
|
NOTE: χ2 test used for difference in gestational weight gain by maternal age, race/ethnicity, educational level, and parity were all statistically significant (p < .001) aBased on unweighted data. bBased on weighted data. SOURCE: Reprinted from Chu S. Y., W. M. Callaghan, C. L. Bish and D. D’Angelo. Gestational weight gain by body mass index among U.S. women delivering live births, 2004-2005: fueling future obesity. American Journal of Obstetrics and Gynecology. Copyright (2009), with permission from Elsevier. |
||||||||||
Food Insecurity
Food insecurity is closely tied to socioeconomic status and is therefore discussed here even though it is arguably a modifiable factor. Several studies have identified a relationship between food insecurity, defined as “whenever the availability of nutritionally adequate and safe food or the ability to acquire acceptable foods in socially acceptable ways is limited or uncertain” (Anderson, 1990). These studies have shown a higher prevalence of overweight and obesity among women living in food-insecure households compared to women living in food secure households (Frongillo et al., 1997; Olson, 1999; Townsend et al., 2001; Adams et al., 2003; Basiotis and Lino, 2003; CDC, 2003; Crawford et al., 2004). The mechanisms mediating this association are not well understood. Reports in the literature addressing eating patterns support the idea that food deprivation can result in overeating (Olson and Strawderman, 2008). Polivy (1996) found that food restriction or deprivation, whether voluntary or involuntary, results in a variety of changes including the preoccupation with food and eating. It has also been suggested that food-insecure households tend to purchase caloriedense foods that are often high in fats and added sugars as an adaptative response to food insecurity (Drewnowski and Darmon, 2005). Corroborating this causal link, Wilde and Peterman (2006) examined the relationship between food insecurity and change in self-reported weight over 12 months in a national sample of nonpregnant women. They found that women in households that were marginally food secure were significantly more likely to gain 4.54 kg (10 pounds) or more in a year compared to women in food-secure households. In contrast, Jones and Frongillo (2007) found that although food insecurity without hunger was associated with risk for overweight/obesity, it was not associated with subsequent weight gain in women of all racial/ethnic groups.
Although food insecurity and obesity have been shown to be positively associated in women, little is known about the direction of causality between food insecurity and obesity. In a cohort of 622 healthy adult women from rural areas followed from early pregnancy until 2 years postpartum, Olson and Strawderman (2008) found that food insecurity in early pregnancy was not associated with increased risk of obesity at 2 years postpartum, suggesting that the causal direction of the relationship between food insecurity and obesity likely goes from obesity to food insecurity. Moreover, they found that women who were both obese and food insecure in early pregnancy were at greatest risk of major gestational and postpartum weight gain, suggesting that food insecurity may play a role in GWG (trends in food insecurity are shown in Chapter 2).
Genetic Characteristics
The role of DNA sequence variation in the regulation of body weight is being investigated in many laboratories worldwide, but few investigators are focusing their attention on the genetics of weight gain during pregnancy. The committee was unable to identify studies dealing with the heritability of GWG. The only evidence on the genetic basis of GWG comes from a small number of reports focusing on the contribution of single nucleotide polymorphisms (SNPs) in specific genes. At present no study has considered the important issue of nutrition or physical activity interactions with genes on GWG.
Most of the SNP studies have focused on the effect of the Trp64Arg allelic substitution in the beta 3 adrenergic receptor gene (ADRβ3) on weight gain during pregnancy (Festa et al., 1999; Yanagisawa et al., 1999; Alevizaki et al., 2000; Tsai et al., 2004; Fallucca et al., 2006). Festa et al. (1999) showed that Austrian mothers who were homozygous for the 64Arg allele gained more weight from baseline to gestational weeks 20 to 31 than heterozygotes. Among pregnant women with type 2 diabetes, Yanagisawa et al. (1999) showed that 12.2 percent of those homozygous and 19.2 percent of those heterozygous for the Trp allele and 28.6 percent homozygous for the Arg allele gained more than 5 units in BMI during pregnancy. In contrast, in a study from Greece, Alevizaki et al. (2000) found no differences among the ADRβ3 genotypes for the rate of weight gain (g/day), calculated from the difference between the prepregnancy reported body weight and the weight measured between weeks 28 and 36 of gestation. Similarly, Tsai et al. (2004) found no differences in weight gain at 24 to 31 weeks of gestation among genotypes in a Taiwanese population. In the largest study to date, involving 627 pregnant women from Italy, Fallucca et al. (2006) found no effect of the ADRβ3 polymorphism on GWG. In the same study, a marker in the insulin receptor substrate 1 (IRS-1) gene was also not associated with GWG.
Tok et al. (2006) examined the Pro12Ala polymorphism in the peroxisome proliferator-activated receptor gamma 2 (PPARδ2) in pregnant Turkish women. Among 62 women who had gestational diabetes mellitus (GDM), those with the Pro12Ala polymorphism gained more weight during pregnancy. Among 100 nondiabetic pregnant women, 294 women homozygous for the T allele with uncomplicated, singleton pregnancies who had term deliveries ranging from 37 to 40 weeks gained significantly more weight (17.4 ± 0.9 kg) than those with the C allele (15.1 ± 0.4 kg). However, the sample included women from various ethnic ancestries, which may have affected the results in an undetermined manner.
From this small body of data, it is impossible to come to any clear conclusion about a role for specific genes and alleles in GWG. None of the studies has been based on sufficiently large sample sizes to ensure that
adequate statistical power was available to identify the effects of alleles or genotypes with a small effect size.
Genetics and Birth Weight
Gestational weight gain is associated with the weight of the infant at birth even though there may not always be a cause and effect relationship and despite the fact that reverse causation often cannot be excluded. In this context, it is useful to consider the role that genetic factors may play in the variation of birth weight. In particular, it is important to understand the potential role of risk alleles at specific genes on risk for SGA and large-for-gestational age (LGA).
The topic of the heritability of birth weight has been addressed for more than 50 years in the scientific literature. The evidence up to the late 1970s was reviewed (Robson, 1978) in a three-volume treatise on human growth. The conclusion was that the fetal genotype played a small role on birth weight, probably of the order of 10 percent, while the maternal genotype accounted for about 24 percent of the total variance. These estimates were derived from data on full siblings, half-siblings, first cousins, mother-child, father-child, and monozygotic and dizygotic twins.
The most compelling data for a role of paternal birth weight on weight of the offspring at birth also comes from a Norwegian study. A total of 67,795 father-mother-firstborn child trios were used to plot the birth weight of infants against paternal birth weight by classes of maternal birth weight (Magnus et al., 2001). The regression of a child’s birth weight on the father’s birth weight was 0.137 while that on the mother’s birth weight reached 0.252. The effect of paternal birth weight was about the same within each category of maternal birth weight, with no significant interaction effects between parental birth weight levels.
More recent twin studies have consistently generated slightly higher significant genetic components for birth weight—in the range of 20 percent to 40 percent (Vlietinck et al., 1989; Whitfield et al., 2001; Dubois et al., 2007). In a Norwegian study involving mother-father-single birth trios (up to a maximum of three singleton births per mother-father pair) from 101,748 families, Lunde et al. (2007) estimated that the fetal genetic component of birth weight was 31 percent, after adjusting for birth order, sex, and generation. The heritability estimates for birth length and gestational age were 31 and 11 percent, respectively. Given the ample statistical power of the latter study, the committee concluded that 31 percent represents the most valid and reliable heritability estimate to date of the contribution of the fetal genes to birth weight (Beaty, 2007). The latter is concordant with the 25 percent value reported in another large Norwegian study of trios composed of mother-father-firstborn child (Magnus et al., 2001).
Importantly, variation in birth weight is influenced by a number of other factors in addition to the genetic makeup of the newborn. Several studies have identified maternal genotype as another important factor. For example, in the large Norwegian study cited above, maternal genetic factors accounted for 22 percent of the variation in birth weight (Lunde et al., 2007).
In another study of 6,811 white singletons and their natural parents, Griffiths et al. (2007) evaluated the effect of parental height and weight on offspring length and weight at birth and observed that the effects of parental height on birth weight were similar for both. However, the influence of the mother’s weight on the infant’s birth weight was stronger than that of the father. Finally, in a report on parental role on the familial aggregation of SGA in 256 infants, Jaquet et al. (2005) found that both parents contributed almost equally to the risk. Specifically, the risk of SGA for an infant at birth was 4.7 times greater for mothers and 3.5 times for fathers who were themselves SGA, compared to those who were appropriate-for-gestational age (AGA). When both parents had been SGA the risk of an SGA infant was 16 times higher.
Evidence for a role of specific genes with a focus on their implications for diabetes on birth weight is limited (McCarthy and Hattersley, 2008). Glucokinase encoded by the GCK gene is an enzyme that phosphorylates glucose to glucose-6-phosphate in the pancreas, where it serves as a glucose sensor and is the rate limiting step in glucose metabolism. A defect in the pancreatic glucose-sensing mechanisms of the fetus could potentially reduce weight at birth and have profound effects on the regulation of glucose and insulin later in life. Mutations altering highly conserved amino acids in GCK were genotyped in 58 offspring and their mothers from the UK (Hattersley et al., 1998). When a mutation was present in the fetus but not carried by the mother, weight at birth was diminished by more than 500 g. A concordant observation was that in 19 pairs of siblings discordant for a GCK mutation, the infant with the mutation weighed about 500 g less at birth than the other sibling (see Figure 4-2). When a mutation was absent in the fetus but present in the mother, mean birth weight was higher by about 600 g. When the mutation was present in both mother and fetus, body weight at birth was normal. The low and high birth weights associated with a number of GCK missense mutations are thought to reflect variation in fetal insulin secretion resulting from the GCK fetal genotype and indirectly from the fetal response to maternal hyperglycemia (Hattersley et al., 1998). This may represent an explanation for some of the fetal programming cases in which there is an association between low birth weight and later insulin resistance and type 2 diabetes.
In a short report of four cases from Italy exhibiting different GCK mutations, three had substantially lower than average birth weight (Prisco et al., 2000). One recent study focused on the effect of the adenosine (A)
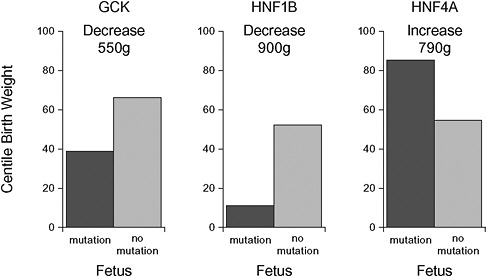
FIGURE 4-2 The impact on birth weight of a fetus inheriting three common maturity-onset diabetes in the young (MODY) gene mutations. Birth weight is presented in centile birth weight with the fetus inheriting the mutation in black and the fetus without the mutation in gray.
SOURCE: Modified from McCarthy and Hattersley, 2008. Copyright © 2008 American Diabetes Association from Diabetes®, 57: 2889-2898. Modified with permission from The American Diabetes Association.
allele (single nucleotide polymorphism [SNP] at position − 30) at the GCK gene on birth weight (Weedon et al., 2005). Using data from 2,689 mother-child pairs, the A allele in the mother was associated with a 64 g increase in the offspring birth weight. There was no effect of the offspring GCK genotype at this particular mutation on birth weight.
Hepatocyte nuclear factor 1 beta (HNF1β) is a transcription factor, encoded by the HNF1β gene, critical for the development of the pancreas. Birth weight was studied in 21 patients with HNF1β mutations (Edghill et al., 2006). Weight at birth was low in all cases, with a median weight of 2.7 kg. In 13 of these patients born to unaffected mothers, 69 percent were SGA at birth, with a median percentile weight of 3 (Figure 4-2).
Another transcription factor, hepatocyte nuclear factor 4 alpha (HNF4α) is involved in the regulation of pancreatic insulin secretion. The HNF4α gene is responsible for maturity-onset diabetes in the young (MODY-1) and accounts for about 4 percent of all MODY cases (McCarthy and Hattersley, 2008). Mutations in HNF4α also associate with type 2 diabetes. Weight at birth was studied in 108 infants from families with HNF4α mutations (Pearson et al., 2007). Birth weight was increased by 790 g in HNF4α
mutation carriers compared to nonmutated family members (Figure 4-2). Fifty-four percent of mutation carriers were macrosomic, compared with 13 percent for nonmutation family members.
In another candidate gene study, a common SNP in the fat mass and obesity associated gene (FTO) was investigated for its relationship to weight at birth in 234 full-term, healthy newborns (Lopez-Bermejo et al., 2008). An allelic variant known to influence body weight and fat mass in children and adults was not associated with birth weight, but an association became evident after about 2 weeks postnatally.
Another line of evidence for a role of genes on birth weight, and thus perhaps on GWG, comes from scanning the whole genome. Three studies have dealt with genome-wide linkages using panels of highly polymorphic markers and birth weight. The first was based on 269 Pima Indians from 92 families and 503 autosomal microsatellite markers (Lindsay et al., 2002). A quantitative trait locus (QTL) was identified on chromosome 11 (logarithmic odds [LOD] for an imprinted locus = 3.4), suggesting that a paternally imprinted gene at map position 88 cM was influencing birth weight in this population (Lindsay et al., 2002). Subsequently, a QTL on chromosome 6q was shown to be linked to birth weight in Mexican Americans from the San Antonio Family Birth Weight Study (LOD = 3.7) and partially replicated in a European American population (LOD = 2.3) (Arya et al., 2006). The latest study using this approach was also on Hispanic newborns from Texas (Cai et al., 2007). Birth weight was available from birth certificates for 629 children from 319 families. Birth weight was highly heritable in this population, and a QTL was identified on 10q22 with a LOD score of 2.6.
Based on this body of data, the committee drew the preliminary conclusions that:
-
there is a fetal genotype effect on weight at birth (about 30 percent of the adjusted variance);
-
both parents’ genes influence birth weight with a stronger effect for maternal genes;
-
specific allelic variants have been associated with weight at birth;
-
mutations in GCK and HNF1β are associated with low birth weight;
-
mutations in HNF4α are associated with high birth weight; and
-
a few quantitative trait loci on chromosomes 6, 10, and 11 have been uncovered from genome-wide linkage scans.
However, the high-risk alleles identified thus far have not been studied for their potential contributions to GWG with or without control for the weight of the infant. The issue of the contribution of specific genes and variants to human variation in birth weight would greatly benefit from
a number of genome-wide association studies with comprehensive panels of markers, particularly in cohorts with large sample size and substantial numbers of small- and large-for-gestational age infants. It will also be critical in the future to design studies that will make it possible to define the maternal and fetal alleles at key genes that associate with increased risk for GWG outside recommended ranges in the context of maternal dietary and physical activity habits.
Developmental Programming
In addition to genetics, a multitude of other maternal factors could potentially influence GWG. Early developmental programming is one of them. Developmental, or in utero, programming refers to physiological, metabolic, or behavioral adaptation resulting from exposure or lack thereof to hormones, nutrients, stress, and other agents at critical periods during embryonic or fetal development. These exposures and experiences may encode the functions of organs or systems that become manifest as elevated or diminished risk for disease later in life (Barker, 1998; Seckl, 1998).
The following example illustrates how developmental programming may influence maternal GWG. It has been suggested that developmental programming could influence the ability to respond to and cope with repeated exposure to stress. If this is shown to be the case, it could explain why some women may be at greater risk for excessive GWG. More specifically, animals and humans subjected to chronic and repeated stress exhibit elevated basal glucocorticoid levels and exaggerated hypothalamic-pituitary-adrenal (HPA) response to natural or experimental stressors (Sapolsky, 1995). Epidemiologic evidence suggests there may be a relationship between elevated glucocorticoid levels and physiologic changes associated with metabolic syndrome, including increased adiposity (Pasquali et al., 2006; Barat et al., 2007); and hyperactivity of the HPA axis has been hypothesized to play a role in development of abdominal obesity and insulin resistance (Bjorntorp, 1993, 1996; Bjorntorp and Rosmond, 2000). A potential mechanism for HPA hyperactivity is through diminished feedback inhibition of pituitary activity resulting from down-regulation of glucocorticoid receptors in the brain (Vicennati and Pasquali, 2000). Over time HPA hyperactivity and excess glucocorticoid secretion can lead to both hyperinsulinemia and insulin resistance with subsequent increased risk of type 2 diabetes (Vicennati and Pasquali, 2000). These observations suggest that GWG could be influenced by not only factors during pregnancy but also by in utero developmental events that happened to the mother herself during development that may predispose her to HPA dysregulation.
Even though the evidence for a role of developmental programming during fetal life on the risk of obesity and late-onset metabolic diseases is
growing, the committee was unable to identify studies that directly examined the influences of programming on GWG in the mother. Consequences of high GWG to the child that may be related to developmental programming are discussed in Chapter 6.
Epigenetics
Some types of developmental programming may be mediated through epigenetic events—that is, chemical modifications to the DNA and histone proteins that influence gene expression and manifest as phenotypic differences potentially mimicking those associated with DNA sequence variants. Epigenetic events begin accruing early after fertilization. Some occur at the embryonic stage in key tissues, often resulting in silencing (or switching off) of genes particularly when they occur in their promoter regions (Sinclair et al., 2007; Waterland et al., 2008). Epigenetic events are typically stable over time and can be triggered by signals in the cellular environment. For example, there is already compelling evidence to suggest that nutritional factors can entrain DNA methylation and modifications in histone proteins (Waterland and Jirtle, 2003). Such events are known to lead to the cytosine residue (in CpG islands) and histone (H3 and H4) methylation, acetylation, or other chemical modifications. When these events occur during fetal life, they provide a mechanism, although it is not the only one, by which programming of the developing organism beyond the blueprint specified in the genomic DNA may occur.
It is important to recognize that epigenetic events are not limited to the early developmental time period and can occur throughout life. For example, Fraga et al. (2005) reported that the pattern of DNA (i.e., the most common type of epigenetic event and one that typically results in gene silencing) methylation in monozygotic twins diverges more as they become older, reinforcing the view that considerable phenotypic differences can arise among individuals with the same genotype. Such phenotypic variations in physiology and behavior have been observed before in inbred rodent strains but with no satisfactory explanations for why.
Future progress in a scientific understanding of the role of developmental programming in determining GWG will require that attention be paid not only to the role of DNA sequence variation on GWG but also to the potential influence of early programming and epigenetic events and their lasting impact on pregnant women.
Anthropometric and Physiological Factors
Almost all of the evidence identified by the committee on the effect of maternal physiology on GWG is related to at least one of three physiologi-
cal factors: (1) prepregnancy BMI, (2) changes in the hormonal milieu that impact the maternal metabolic response during pregnancy, and (3) changes in basal metabolic rate (BMR) and energy expenditure (EE) during pregnancy. The following discussion summarizes this evidence. The BMI studies are, to some extent, an expansion of Chapter 2 on trends in BMI since publication of the IOM (1990) report; and the studies on hormonal milieu, BMR, and EE are, to some extent, an extension of the Chapter 3 discussion on endocrine and metabolic changes that occur during pregnancy.
Pregravid BMI
Based on epidemiological studies (e.g., those described in Chapter 2), GWG is generally inversely proportional to maternal BMI. For example, in a report of over 2.3 million deliveries in Germany from 1995-2000, Voigt et al. (2007) reported that overall, relatively short and heavy women had lower GWGs than tall and thin women. In the United States, Chu et al. (2009) used the PRAMS data from 2004-2005 to assess the amount of GWG among 52,988 underweight, normal weight, overweight, and obese U.S. women delivering full-term singleton infants (Table 4-4). They found that, overall, GWG decreased with increasing BMI. When they stratified by BMI, they found that obese women gained less weight during pregnancy than normal or overweight women; yet about one-fourth of obese women still gained 35 pounds or more. In a multivariable regression model, maternal prepregnancy obesity was the strongest predictor of low GWG (obesity correlated with lowest GWG), followed by higher parity, African American or Hispanic racial identity, and higher maternal age.
Although pregravid BMI can predict GWG there are also metabolic changes in pregnancy, i.e., basal metabolic rate (BMR), total energy expenditure (TEE), and hormonal changes that are independent of BMI that can influence GWG.
Insulin, Leptin, and Hormonal Milieu, Basal Metabolic Rate
The metabolic response to pregnancy varies widely among women. Prentice et al. (1989) reported on longitudinal changes from pre-conception through 36 weeks’ gestation in eight healthy well-nourished women. The mean GWG at 38 weeks’ gestation was 14.4 ± 4.1 kg. Lean body mass increased linearly to a mean of 6.7 ± 1.6 kg by 36 weeks’ gestation. Measured BMR varied from 8.6 to 35.4 percent above pregravid BMR, although some obese subjects showed significant decreases in BMR up to 24 weeks’ gestation (r = 0.84). In pregnant women, the relative cost of exercise for 120 minutes was approximately 10 percent of TEE. The authors concluded, from finding a small range for energy savings from either minor physical
TABLE 4-4 Gestational Weight Gain (pounds) by Prepregnancy BMI Among Mothers Delivering Full-term, Singleton Births, PRAMS, 2004-2005
|
BMI Group |
≤ 14 (n = 8,442)a |
15-24 (n = 10,583)a |
25-34 (n = 15,477)a |
35-44 (n = 10,942)a |
≥ 45 (n = 7,544)a |
|||||
|
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
Percentb |
SEb |
|
|
Underweight (BMI, < 18.5 kg/m2) |
10.5 |
0.9 |
17.7 |
1.1 |
34.4 |
1.5 |
23.2 |
1.3 |
14.2 |
1.0 |
|
Normal (BMI, 18.5-24.9 kg/m2) |
10.4 |
0.3 |
16.1 |
0.3 |
31.8 |
0.4 |
24.7 |
0.4 |
17.1 |
0.3 |
|
Overweight (BMI, 25.0-29.9 kg/m2) |
15.7 |
0.5 |
20.3 |
0.5 |
27.5 |
0.6 |
20.5 |
0.5 |
16.1 |
0.5 |
|
Obese (BMI, ≥ 30.0 kg/m2) |
29.8 |
0.7 |
24.4 |
0.6 |
22.1 |
0.6 |
13.1 |
0.5 |
10.7 |
0.5 |
|
Total |
15.3 |
0.2 |
18.7 |
0.3 |
29.1 |
0.3 |
21.4 |
0.3 |
15.5 |
0.2 |
|
NOTE: χ2 test for the difference in gestational weight gain by body mass index (BMI) group was statistically significant (p < .001). aBased on unweighted data. bBased on weighted data; percentages were age adjusted. SOURCE: Reprinted from Chu S. Y., W. M. Callaghan, C. L. Bish and D. D’Angelo. Gestational weight gain by body mass index among U.S. women delivering live births, 2004-2005: fueling future obesity. American Journal of Obstetrics and Gynecology. Copyright (2009), with permission from Elsevier. |
||||||||||
activity or thermogenesis along with high variability in BMR during pregnancy, that offering prescriptive energy intake recommendations would be impractical because it is impossible to know how an individual woman’s metabolism will respond.
Durnin (1991) reported on longitudinal changes in energy expenditure during pregnancy among Scottish and Dutch women. Among this cohort, an increase in BMR was not seen until 16 weeks’ gestation and was followed by a mean increase of 400 kcal/day over pregravid BMI. The total energy cost of pregnancy was estimated at 69,000 kcal. Adjusting for dietary energy intake (~22,000 kcal) the authors estimated that decreased physical activity or increased efficiency of work accounted for an additional savings of ~47,000 kcal. Similarly Forsum et al. (1985) found an increase in BMR throughout gestation in a study of Swedish women.
Lawrence et al. (1985) studied how women in a developing country responded to increasing food intake during pregnancy. Pregnant women in the Gambia who followed their normal dietary pattern experienced energy sparing of 11,000 kcal with no increase in BMR above pregravid BMI until 30 weeks’ gestation. Further, the women showed a mean GWG of 6 kg with no increase in adipose tissue mass. When their baseline diet was supplemented with 723 kcal/day in additional food, BMR increased by approximately 1,000 kcal over pregravid BMI. Women whose diets were supplemented with additional food had a mean 8 kg increase in GWG and a 2 kg increase in fat mass. Food supplementation had no effect, however, on the energy cost of activity and did not result in increased birth weight when physical work was decreased.
Goldberg et al. (1993) used the doubly labeled water method (International Dietary Energy Consulting Group, 1990) to assess BMR, energy intake, and body composition in 12 affluent women at pre-conception and at 6-week intervals from 6 through 36 weeks’ gestation. Estimated changes in BMR, TEE, and fat deposition were 112 ± 104 MJ, 243 ± 279 MJ, and 132 ± 127 MJ, respectively. The mean total energy cost of pregnancy calculated from BMR, TEE, and energy deposited as fat was 418 ± 348 MJ. The women’s self-reported energy intake however was only 208 ± 272 MJ, a significant underestimate of the calculated additional energy cost of pregnancy. Again, the variability in the individual biological response shown in this study supports the impracticality of prescriptive recommendations for energy intake during pregnancy.
A similar prospective study by Butte et al. (2004) of measured energy expenditure in women by prepregnant BMI showed that women in the highest BMI group accumulated greater fat mass (8.4 kg) compared to those in the low BMI group (5.3 kg). The increase in fat mass accounted for most of the variance in total weight gain among BMI groups. In both the low and high BMI groups mean TEE decreased in the second trimester but in-
creased in the third trimester. When adjusted for fat-free mass (FFM), TEE decreased in all BMI groups toward the end of gestation. Using multiple regression analysis, the change in TEE throughout the course of gestation was related to prepregnancy BMI and percent body fat as well as weight gain and increase in FFM. These variables accounted for 33 percent of the variance in 24-hour TEE, primarily from change in BMR. Physical activity accounted for very little net increase in TEE and actually decreased in all groups with advancing gestation.
Hormonal Milieu
As discussed in Chapter 3, there is wide variation in maternal metabolic response to pregnancy. Maternal pregravid insulin sensitivity may vary up to two- to three-fold, depending on factors such as obesity, level of fitness, and genetic make-up. Over the course of pregnancy a 40-60 percent decrease in insulin sensitivity occurs, depending on pregravid metabolic status (Catalano et al., 1993, 1999). For example, a 50 percent decrease in insulin sensitivity in both a thin athletic woman and an obese sedentary woman with type 2 diabetes may represent a two-fold or greater quantitative change in insulin sensitivity between them by the end of gestation. In the last 12 weeks of pregnancy, when fetal weight increases on the average from 1.0 kg to 3.5 kg, decreased insulin sensitivity increases the availability of energy to support fetal growth (Hytten and Chamberlain, 1991).
Although these changes in insulin sensitivity occur over a matter of months, compared to years in nonpregnant individuals, the same physiological associations detected in some large epidemiological studies among nonpregnant individuals may exist during pregnancy as well. For example, Swinburn et al. (1991), in a 3.5-year longitudinal study, showed that Pima Indians who were insulin resistant (measured using the euglycemic clamp technique) gained less weight than individuals who were insulin sensitive (3.1 versus 7.6 kg, p = 0.0001). The percent change in weight per year was correlated with glucose utilization (r = 0.34, p = 0.0001). The same could be true of obese vs. non-obese women. In fact, there is some preliminary data showing that, at least in early pregnancy, changes in maternal BMR and fat accretion are inversely related to the changes in insulin sensitivity in a small number of subjects (Catalano et al., 1998). Whether increased energy intake in obese insulin-resistant women during pregnancy has a greater effect on maternal and fetal fat accretion than in non-obese women remains to be determined.
Cytokines
Although there are no direct mechanistic effects relating leptin and adiponectin to GWG, both adipocytokines have been correlated with various
components of maternal metabolism and may exert an indirect effect on GWG through their effects on maternal insulin sensitivity.
Leptin is produced in relatively large quantities by the placenta and is transferred primarily into the maternal circulation (Hauguel-de Mouzon et al., 2006), with maternal leptin concentrations increasing by 12 weeks’ gestation and having a significant positive correlation with both maternal body fat and BMR in both early and late gestation (Highman et al., 1998). Kirwan et al. (2002) used a stepwise regression analysis to show that, over the course of pregnancy, leptin also makes a significant contribution to changes in insulin sensitivity that occur during gestation. There may also be a relationship between circulating leptin and increased maternal fat oxidation (Okereke et al., 2004).
Adiponectin is a unique circulating cytokine that has a positive correlation with insulin sensitivity and negative correlation with adiposity (Cnop et al., 2003). In contrast to leptin and other cytokines, adiponectin is made exclusively in the maternal and fetal compartments, and not in the placenta (Pinar et al., 2008). There is no transfer of leptin from mother to fetus or vice versa. Lower adiponectin concentrations have been reported in women with previous GDM (Winzer et al., 2004), and leptin was shown to decrease over the course of pregnancy in women with GDM compared to women with normal glucose tolerance (Retnarkaran et al., 2004; Williams et al., 2004).
In summary both leptin and adiponectin are correlated with various components of maternal metabolism such as energy expenditure and adiposity. However, there are no direct mechanistic effects relating to the changes in maternal weight gain described in human pregnancy. Indirectly these cytokines through their effects on maternal insulin sensitivity may represent markers of other mechanisms effecting gestational weight changes.
Medical Factors
Pre-Existing Morbidities
The committee considered several maternal medical factors known to be related to pregnancy outcome that could have an impact on GWG: pre-existing chronic disease or other morbidities; hyperemesis gravidarium; anorexia nervosa and bulimia nervosa; bariatric surgery; and twins and higher order pregnancies. The committee was unable to identify studies that directly examined pre-existing morbidities as determinants of GWG. However, in general the pre-conceptional health status of a woman is important for optimal pregnancy outcome. This is particularly true for chronic diseases such as inflammatory bowel disease and systemic lupus erythematosus. In women with inflammatory bowel disease, and in particular Crohn’s disease, the level of disease activity during pregnancy is related to
disease activity at conception. Fonager et al. (1998) reported a decrease in birth weight and increased preterm delivery in women with active Crohn’s disease at conception. Similarly in women with lupus complicating pregnancy, pregnancy outcomes are improved if lupus has been quiescent for at least 6 months before conception (Cunningham et al., 2005).
Hyperemesis Gravidarum
Although as many as 70-85 percent of pregnant women will have nausea and occasional vomiting in pregnancy (Jewell and Young, 2003), this often resolves by the second trimester. There are usually no long-term sequelae, and treatment is mostly symptomatic including avoidance of certain foods and eating small frequent meals. However, approximately 0.5-2.0 percent of pregnant women will develop hyperemesis gravidarum (ACOG, 2004). The most commonly cited criteria for hyperemesis gravidarum include: persistent vomiting unrelated to other medical conditions, ketonuria, and weight loss of 5 percent or greater of prepregnancy weight at < 16 weeks’ gestation (Goodwin et al., 1992). Other associated findings include dehydration, ketonuria, and electrolyte imbalance. The underlying etiology of this disorder is not known with certainty, but rapid increases in circulating human chorionic gonadotropin (HCG) and estrogen in early pregnancy have been associated with the condition (Furneaux et al., 2001; Goodwin, 2002).
In mild cases of nausea and vomiting there appears to be no adverse effect on maternal weight gain or pregnancy outcome. However, among women with hyperemesis gravidarum there is evidence of decreased GWG and a higher risk of low birth weight. Gross et al. (1989) reported on 64 women with a diagnosis of hyperemesis gravidarum. When compared to women with a similar diagnosis but who lost < 5 percent of their prepregnancy weight, women who lost > 5 percent of their prepregnancy body weight had lower total GWG (9.6 ± 2.4 versus 13.7 ± 3.2 kg, p < 0.05), compromised, fetal growth (i.e., smaller percent weight for gestational age; 38 percentile versus 72 percentile, p < 0.025), and increased growth restriction (30 percent versus 6 percent, p < 0.01). In a more recent study, Vilming and Nesheim (2000) and Bailit (2005) likewise reported that women with hyperemesis gravidarum had overall lower GWG and birth weight in comparison with a control group. Evidence for long-term outcomes on infant growth was not found.
Anorexia Nervosa and Bulimia Nervosa
Anorexia nervosa and bulimia nervosa are frequently encountered in young women of reproductive age. Both disorders are characterized by a
dysfunctional perception of body weight and shape (Wisner et al., 2007), and both may affect GWG. Anorexia, which is defined as body weight less than 85 percent of expected weight for age and height, occurs in between 0.5-1.0 percent of women of reproductive age. Bulimia is defined as weight at the minimally normal range but where the individual employs binge eating and subsequent compensatory methods such as self-induced vomiting, laxative, or diuretic medications to avoid appropriate weight gain. Bulimia occurs in 1-3 percent of young women.
In a Danish register-based follow-up study, Sollid et al. (2004) compared 302 women with eating disorders before pregnancy and who were delivered of 504 children with 900 control subjects who were delivered of 1,552 children. They reported an almost two-fold increased risk of preterm delivery (less than 37 weeks) and SGA (birth weight < 10th percentile) in women with eating disorders. Unfortunately the investigators were not able to obtain any information on prepregnancy BMI or GWG. In a smaller study from Sweden, Kouba et al. (2005) reported that among 49 women with previously diagnosed eating disorders 22 percent had a relapse of their eating disorder in pregnancy. Compared to a control group, the women with either a past or current eating disorder were at significantly increased risk of hyperemesis, and delivered children with significantly lower birth weight and head circumference as compared with a control group. Although there were no significant differences in GWG between the groups, the anorectic women (n = 24) gained less weight than women with previous history of eating disorders (10.4 ± 3.9 versus 12.1 ± 2.6 kg, p < 0.05). The authors speculated that one of the potential causes for the decreased fetal growth in the women with a history of eating disorders include their inability to achieve the recommended weight gain of 11.5-16.0 kg during pregnancy. There was no significant difference in intake of folate, protein, or total caloric intake between the two groups. Finally, in a cohort of 35,929 pregnant Norwegian women, 35 women reported broad anorexia nervosa, 304 bulimia nervosa, 1,812 binge eating disorder, and 36 eating disorder not otherwise specified (EDNOS)-purging type in the 6 months before or during pregnancy (Bulik et al., 2008). Prepregnancy BMI was lower in anorexia, and higher in binge eating disorder than the referent group, and anorexia, bulimia, and binge eating disordered mothers reported greater GWG.
Bariatric Surgery
As discussed in Chapter 2, the prevalence of obesity in the U.S. population has been steadily increasing since 1990. This has been paralleled by a recent increase in the number of bariatric surgeries performed as treatment for obesity. The reported total number of bariatric surgical procedures performed in the United States increased from approximately 13,365 in
1998 to approximately 72,177 in 2002 (Santry et al., 2005; Davis et al., 2006). Most of the procedures during this time were performed on women; 81 percent in 1998 and 84 percent in 2002. As a result of this trend, the American College of Obstetricians and Gynecologists (ACOG) published a Committee Opinion on Obesity and Pregnancy addressing the issue of bariatric surgery and pregnancy (ACOG, 2005), recommending that obese women who have undergone bariatric surgery receive the following counseling before and during pregnancy:
-
Patients with adjustable gastric banding should be advised that they are at risk of becoming pregnant unexpectedly after weight loss following surgery.
-
All patients are advised to delay pregnancy for 12-18 months after surgery to avoid pregnancy during the rapid weight loss phase.
-
Women with gastric banding should be monitored by their general surgeons during pregnancy because adjustments of the band may be necessary.
-
Patients should be evaluated for nutritional deficiencies, including iron, B12, folate, vitamin D, and calcium, and supplemented with vitamins as necessary.
With respect to GWG, the committee identified three studies that reported a decrease in weight gain during a subsequent pregnancy in women who had bariatric surgery (Skull et al., 2004; Dixon et al., 2005; Ducarme et al., 2007). Gurewitsch et al. (1996) reported that nutritional complications such as folate and B12 deficiencies are also associated with pregnancy following bariatric surgery.
However, the committee did not identify any prospective randomized trials of pregnancy outcome in obese women treated by bariatric surgery. The only published reports are those that utilize the patient as her own control, i.e., a pregnancy outcome before bariatric surgery and a subsequent pregnancy outcome after having a bariatric procedure (Marceau et al., 2004; Skull et al., 2004; Dixon et al., 2005) or retrospective case-controlled studies (Ducarme et al., 2007). Skull et al. (2004), Dixon et al. (2005), and Ducarme et al. (2007) all reported a decreased incidence of GDM and hypertensive disorders among women who had undergone bariatric surgery prior to pregnancy. Marceau et al. (2004) and Ducarme et al. (2007) also reported a decreased risk of macrosomia in women following bariatric surgery; however, neither Dixon et al. (2005) nor Skull et al. (2005) reported a decrease in macrosomia. So the effects of bariatric surgery on risk for macrosomia, as well as on birth weight, are inconclusive. Care must be taken in the interpretation of these studies because of their retrospective nature and use of various definitions of outcome measures.
Twins and Higher Order Pregnancy
As discussed in Chapter 3, the presence of multiple fetuses in a pregnancy has an influence on total GWG. In comparison to a singleton birth the additional components of the products of a twin gestation (fetus, placenta, and amniotic fluid) account for up to two additional kilograms in GWG (see discussion in Chapter 3). The effects of GWG on maternal and child health outcomes for multiple births are discussed in Chapters 5 and 6, respectively.
Psychological Factors
The committee evaluated whether several weight-related psychological factors—depression, stress, social support, and attitudes toward weight gain—might be determinants of GWG. The following discussion summarizes the committee’s review of the evidence. Based on its review, the committee found that depression, or depressive symptoms, are associated with both low and high GWG (i.e., lower or higher than the recommended ranges) but that the evidence on whether and how the other psychological factors impact GWG is inconclusive. The discussion on depression extends the Chapter 2 summary of trends since 1990 in depression during pregnancy.
Depression
The committee identified three studies showing a positive association between depression, or depressive symptoms, and low GWG. Bodnar et al. (2009) followed a sample of 242 mostly well-educated white women through pregnancy and assessed clinical depression through structured interviews at 20, 30, and 36 weeks’ gestation. The study found that all women with GWG below the ranges recommended by the IOM (1990) had an elevated prevalence of major depression, regardless of their pregravid BMI. Hickey et al. (1995) conducted a prospective study of depressive symptoms at 24-26 weeks and inadequate GWG in a large cohort of low-income, non-obese black and white women and found that among white women, individuals in the highest quartile of depressive symptom score were three times as likely as women in the lowest quartile to have weight gain below the ranges recommended by IOM (1990). The investigators did not find any association between depression and low weight gain in black women (Hickey et al., 1995). Finally, in a cohort of over 4,000 Hispanic women, Siega-Riz and Hobel (1997) found that self-reported feelings of depression during the pregnancy were negatively associated with GWG.
The committee identified two studies showing a positive association between depressive symptoms and either high GWG and/or excess fat de-
posits. Webb et al. (2009) found that pregnant women who gained in excess of the ranges recommended by IOM (1990) were more likely to have high depressive symptoms than women who met the weight gain recommendations. Casanueva et al. (2000) conducted a case-control study to test for associations between maternal depressive symptoms and fat deposition among Mexican pregnant adolescents. They used body weight and anthropometric measures of skinfold thickness to determine fat deposition beginning at 20 weeks gestation through 4 weeks postpartum. The results of this study indicated an association between depressive symptoms and excessive fat deposition in Mexican adolescents. In cross-sectional studies, high depressive symptoms have been associated with negative attitudes about GWG (Stevens-Simon et al., 1993b; Dipietro et al., 2003). Women who are concerned before and during pregnancy about their weight gain have higher depressive scores in the week following delivery (Abraham et al., 2001).
Not all studies have shown a positive association between depression and either high or low GWG. For example, Cameron et al. (1996) studied a biracial sample of 132 women in mid-gestation and found a positive association between GWG and depression score for white women with high self-esteem, a negative correlation with depression score and third-trimester weight among white women with low self-esteem, and no association between depression score and GWG among black women. Walker and Kim (2002) analyzed data from a longitudinal study of postpartum weight patterns in low-income women and found that depressive symptoms were not significantly associated with GWG. Collectively, however, the majority of studies indicate that low and high GWG may be a marker of depression during pregnancy. Trends in depression among women of child-bearing age are shown in Chapter 2.
Stress
The committee found a lack of consistent evidence in support of a relationship between stress and GWG. The impact, however, of psychosocial factors such as stress on GWG and postpartum weight retention may be underestimated as a result of the limitations in measurement and data analysis; most of the available evidence is observational, and estimates of the impact of stress are confounded by the different kinds of effects that can occur depending on how an individual responds.
Picone et al. (1982) examined the influence of psychological stress as a factor in GWG and pregnancy outcome in a controlled prospective study of a group of 60 women utilizing an urban prenatal clinic. Psychological stress was assessed using a social readjustment rating scale from the Holmes-Rahe life events questionnaire. The investigators found a correlation between higher stress scores and lower GWG, independent of nutrient or caloric
intake. The finding suggests that stress did not affect food intake in these subjects, rather it impacted the utilization of calories and nutrients from the foods consumed to support pregnancy.
Based on the published regression models, either crude or adjusted, there does not appear to be a robust association between the appraisals of stress, sufficiency of coping resources, and adequacy of GWG. However, when evaluating the risk ratio differences observed between women who gained either inadequate or excessive weight, the committee found that the women who gained inadequate weight tended to have a stronger, albeit modest, link to perceived stress. Brawarsky et al. (2005) found a similar pattern: women who reported high stress during pregnancy tended to gain weight below amounts recommended. Likewise, Orr et al. (1996) reported higher stress in relation to insufficient GWG.
Social Support
Evidence for a role of social support as a determinant of GWG is mixed and inconclusive. In a prospective study of 806 low-income, non-obese pregnant women, Hickey et al. (1995) found that the levels of social support did not predict low GWG for either black or white women. Casanueva et al. (1994) reported on the impact of psychological support, given to a group of adolescents during pregnancy, on GWG and found that adolescents who received additional psychological support by a psychotherapy team gained, on average, 2.8 kg more than adolescents who did not receive support. More recently, Olson and Strawderman (2003) found the effect of social support on GWG varied significantly by BMI group. Underweight, normal weight, and obese women who had low social support gained significantly more weight gain than their counterparts with average or high social support. However, obese women who had low social support gained significantly less weight relative to obese women with average or high social support.
Attitudes Toward Weight Gain or Weight Loss
Several studies have examined the relationship between maternal attitude toward weight gain during pregnancy and actual GWG. Palmer et al. (1985) developed an 18-item scale measuring pregnant women’s attitude toward their own weight gain and found among 29 white, middle-class women that positive attitude was significantly associated with higher actual weight gain. Stevens-Simon et al. (1993) conducted a study of 99 pregnant adolescents and found that weight gain was significantly related to 4 of 18 scale items but not the total attitude scale score. However, Copper et al. (1995) studied 1,000 black and white low-income women and found that
the attitude score was not significantly related to GWG. The investigators also reported that maternal attitude toward weight gain was influenced by prepregnancy BMI, with thin women tending to have positive attitudes and obese women negative attitudes about GWG. Taken together, the evidence is inconclusive regarding the influence of maternal attitude on actual GWG.
For the majority of women, weight loss during pregnancy is discouraged. However, a small percentage (8.1) of women reported in the Behavioral Risk Factor Surveillance Survey (BRFSS) that they attempted to lose weight during pregnancy (CDC, 1989, 1991). Another survey of women who reported being pregnant and also trying to lose weight indicated that prevalence of weight loss behavior during pregnancy occurred among those who reported drinking and smoking (12.7 percent), women in the first trimester of pregnancy (9.4 percent), those who were diabetic (9 percent), and those with very high BMIs (6.9 percent) (Cogswell et al., 1996). Cohen and Kim (2009) reviewed aggregated multiple year data between 1996 and 2003 from the BRFSS (1989) and found weight-loss attempts during pregnancy were more frequent among women over 34 years of age (6.2 percent) and Hispanic women (13.1 percent). Carmichael et al. (2003) reported in a population-based case-control study of 538 cased and 539 control infants that restricted food intake or fad dieting by the mother during the first trimester of pregnancy was associated with significant risk for neural tube defect among both food restrictors (OR = 2.1, 95% CI: 1.1-4.1) and dieters (OR = 5.8, 95% CI: 1.7-10) compared to controls. Interestingly, no significant increased risk for neural tube defect was detected for dieting behaviors during the 3 months prior to conception.
Behavioral Factors
The committee considered several behavioral factors likely to have an impact on GWG: dietary intake and physical activity (i.e., the two primary components of energy balance, with dietary intake approximating energy expenditure); substance abuse (including cigarette smoking, alcohol use, and drug use); and unintended pregnancy.
Dietary Intake
Numerous clinical trials have examined the effects of either caloric supplementation or restriction on GWG. In a systematic review of 10 trials, Kramer and Kakuma (2003) found that balanced energy/protein supplementation was associated with modest increases in GWG. In contrast two trials reviewed in Kramer and Kakuma (2003) among women who were obese (Campbell, 1983) or had high GWG (Campbell and MacGillivray,
1975) showed that energy/protein restriction was associated with a significant reduction in weekly maternal weight gain (weighted mean difference of 255 [95% CI: −436.56 to −73.0] g/week).
Several observational studies have also examined the relationship between prepregnancy BMI, caloric intake, and GWG. Bergmann et al. (1997) analyzed data in 156 healthy German women and reported that, while neither maternal BMI nor energy intake was related to birth weight, both were related to “net weight gain.” The authors defined maternal weight gain as the weight gain of the mother from the end of the third trimester minus the measured weight in the first trimester, excluding the weight of the fetus and placenta. Women in the high-BMI group (defined as > 24) had an overall lower net weight gain (4.2 kg), compared to women in the normal-BMI group (6.2 kg) and low-BMI group (5.9 kg). However, the lower weight gain was confined to the multigravid women, with primigravid women actually having a greater net weight gain. These associations did not appreciably change when adjusted for energy intake, which did not vary during the course of pregnancy.
In another study, Olson and Strawderman (2003) used a proxy measure for energy intake by questioning 622 healthy pregnant women about changes in the amount of food eaten prior to and during pregnancy. They found that consuming either “much more” or “much less” food during rather than prior to pregnancy was associated with greater (3.67 pounds; p < 0.001) and less (−3.16 pounds; p < 0.05) GWG, respectively, compared to maintaining similar levels of food intake during and prior to pregnancy. Women who ate “much more” during rather than before their pregnancy had an adjusted odds ratio of 2.35 for excessive GWG. Lagiou et al. (2004) found that increased GWG by the end of the second trimester of pregnancy was associated, in a clinic sample of 224 pregnant women, with higher total energy intake and a higher proportion of protein and lipids of animal origin (and lower proportion of carbohydrates).
Finally, analyses from the Pregnancy, Infection, and Nutrition Study (Deierlein et al., 2008) showed that compared to women consuming diets within the lowest quartile for energy density (defined as the number of calories/g of food consumed) during the second trimester, women consuming diets with energy density values in the third and highest quartiles gained a significant excess of over 1 kg in total GWG.
Beyond general food intake, several studies have also examined the effect of GWG on consumption of different types of food as well as macronutrient and micronutrient intake. Stevens-Simon and McAnarney (1992) showed that adolescents who consumed fewer than three snacks a day had slower weight gains during pregnancy. Olson and Strawderman (2003) found that women who consumed three or more servings of fruits and vegetables per day gained 1.81 pounds less than those who consumed
fewer servings during pregnancy. More recently, Olafsdottir et al. (2006) found that the percentage of energy intake from various macronutrients is an important predictor of weight gain but only among overweight women and late in pregnancy. The investigators analyzed the relationship between dietary factors and GWG in 495 healthy Icelandic women using food frequency questionnaires; they defined optimal weight gain as 12-18 kg in normal weight women and 7-12 kg in overweight women. Eleven percent of overweight women had inadequate weight gain compared to only 2 percent of normal weight women; in contrast, 14 percent of overweight women gained > 18 kg, and 20 percent of normal weight women gained > 18 kg. The investigators found that, compared with women gaining suboptimal weight, the diet of overweight women gaining excessive weight had higher energy percentage from fat and lower energy percentage from carbohydrates. They also found that consumption of dairy products and sweets in late pregnancy was associated with a decreased risk of inadequate gain and an increased risk of excessive gain during pregnancy.
The committee identified two studies that examined the effects of caloric intake on GWG in relationship to glycemic load. In a small randomized clinical trial of a low-glycemic versus a high-glycemic diet, Clapp (2002) found that the women on the low-glycemic diet gained less weight during pregnancy (22.9 compared with 40.9 pounds). The investigators speculated on several potential mechanisms that might explain the difference, including changes in: daily digestible energy requirements (i.e., metabolic efficiency), substrate utilization (glucose oxidation versus lipid oxidation), and insulin resistance and sensitivity. Deierlein et al. (2008) reported that white women with glycemic load increases were more sensitive to increased weight gain during pregnancy; the same was not true for black women.
Altogether while several studies have demonstrated a relationship between energy intake and GWG and some studies have shown that dietary intake of certain types of foods may also influence GWG, the evidence base is not substantial enough to draw any conclusions.
Physical Activity
ACOG took the position in 2002 that, in the absence of either medical or obstetric complications, 30 minutes or more of moderate exercise a day on most, if not all, days was recommended for pregnant women (ACOG, 2002). The ACOG report emphasized that participation in a wide range of recreational activities appears to be safe for pregnant women. Participation in activities with a high potential for trauma to the woman or fetus, however, should be avoided.
Published reviews on exercise and pregnancy concluded that the balance of evidence suggests a benefit of exercise during pregnancy, especially for
maternal outcomes (Morris and Johnson, 2005; Gavard and Artal, 2008). Moderate exercise during a low-risk pregnancy was found to be safe for both the mother and fetus and to improve overall maternal fitness and well-being as well as maternal and fetal outcomes (Morris and Johnson, 2005).
The report of the Physical Activity Guidelines Advisory Committee (HHS, 2008) concluded that:
-
Moderate-intensity leisure time physical activity is not associated with an increased risk of low birth weight, preterm delivery, or early pregnancy loss; and
-
Participation in vigorous activities has been associated with small reductions in birth weight compared to less active women (Leet and Flick, 2003; Hegaard et al., 2007) but not with gestational age at birth or birth weight (Evenson et al., 2002; Duncombe et al., 2006).
Gavard and Artal (2008) concurred with the latter findings. However, Kramer and McDonald (2006) in their Cochrane Review concluded that the evidence was insufficient to evaluate the risks or benefits of exercise in pregnant women for infant outcomes.
Several studies have examined the effects of regular physical activity on GWG (Abrams et al., 2000; Siega-Riz et al., 2004). Based on theoretical energy calculation alone, it appears that regular physical activity has the potential to prevent excessive GWG. The main issue then becomes whether it can be shown to work in practice. A number of observational studies but few randomized controlled trials have been reported on this topic. A small number of reports have addressed the issue of the prevalence of physical activity behavior in pregnant women. A cross-sectional survey of pregnant women found that about 48 percent reported some exercise participation during pregnancy (Hinton and Olson, 2001). The most common activities were walking, swimming, and aerobics. In general, the proportion of exercising pregnant women declines across trimesters of pregnancy. In one study of 388 pregnant women, 41 percent were active before pregnancy (Ohlin and Rossner, 1994). By the third trimester, only 14 percent of the women continued to participate in aerobic exercise.
Two meta-analyses and several reviews have concluded that the level of physical activity in pregnant women did not have an influence on GWG (Lokey et al., 1991; Sternfeld et al., 1995; Stevenson, 1997; Kramer and Kakuma, 2003; Morris and Johnson, 2005). However, the meta-analyses did not take into account a number of key factors, including the most critical one: the level of physical activity-related energy expenditure. If the energy cost of the exercise program is very low, it should not be surprising that its influences on GWG cannot be shown.
Some observational studies suggest that maintaining an active lifestyle or adding physical activity to the normal daily schedule of the pregnant woman may attenuate GWG. Clapp and Little (1995) compared exercising women who became pregnant and who continued to exercise at least three times per week to a group of women who stopped exercising once they became pregnant. The rate of GWG and of subcutaneous fat accretion (determined by skinfold thickness) was similar between the two groups during the first and second trimesters but the exercising women gained significantly less body weight and skinfold thickness during the third trimester. On average, the pregnant women who continued to exercise gained about 3 kg less. These observations were from a Norwegian study of 467 pregnant women who answered a questionnaire on physical activity level in week 36 of their pregnancy (Haakstad et al., 2007). Women who exercised regularly had significantly lower weight gain than inactive women in the third trimester only.
In a study of 96 obese women with GDM self-enrolled in either a diet (n = 57) or an exercise plus diet (n = 39) program during the last 2 months of pregnancy, the mean weight gain per week was less in the exercise plus diet group (0.1 ± 0.4 kg versus 0.3 ± 0.4 kg) (Artal et al., 2007). The exercise session consisted of walking on the treadmill or cycling in a semi-recumbent position once a week followed by unsupervised exercise at home for the remaining 6 days. The exercise plus diet group exercised for 153 ± 91 minutes per week. Complications, infant birth weight, and the proportion of cesarean deliveries were comparable between the two groups.
Based on the limited available evidence, the Physical Activity Guidelines Advisory Committee concluded that “unless there are medical reasons to the contrary, a pregnant woman can begin or continue a regular physical activity program throughout gestation, adjusting the frequency, intensity, and time as her condition warrants” (HHS, 2008). The committee added that “in the absence of data, it is reasonable for women during pregnancy and the postpartum period to follow the moderate-intensity recommendations set for adults unless specific medical concerns warrant a reduction in activity.” It is commonly recognized, however, that adequately powered, randomized, controlled intervention studies on the potential benefits and risks of regular physical activity at various dose levels in pregnant women are needed.
Physical activity, such as work, spontaneous activity, fidgeting, and personal chores as well as exercise account for a widely variable fraction of TEE. In some, this may reach only about 15 percent of daily energy expenditure while in others it may be as high as 50 percent (Hill et al., 2004). Most recently, Lof et al. (2008) assessed the effects of maternal physical
activity level (PAL) and BMI on GWG in 223 healthy Swedish women. Pregravid PAL was related to decreased weight gain in the third trimester, about 0.10 kg/week less in the high-PAL than in the low- or medium-PAL groups. Maternal BMI was inversely associated with weight gain in the second trimester but there was a positive association between maternal BMI and GWG in the third trimester. However, maternal smoking, parity, education, age, and pregravid PAL explained only 4 percent of the variance in maternal weight gain, and PAL was not related to birth weight.
In sum, several studies have demonstrated an inverse relationship between the level of physical activity and GWG. Based on energetic fundamentals alone, maintaining a reasonable level of exercise-related energy expenditure during pregnancy should moderate GWG. Energy requirements based on PAL are provided in Appendix B.
Substance Abuse
Cigarette smoking Taken together, early studies examining associations between decreasing GWG and amount of reported smoking show inconclusive results. Rush (1974) found a strong relationship between amount of smoking and decreasing GWG (p < 0.01), while Garn et al. (1979) found no association between smoking and nonsmoking mothers and GWG. Several investigators examined whether smoking had a negative effect on caloric intake as a causative factor for higher incidence of SGA in smoking mothers. Haworth et al. (1980) found that women who smoked during pregnancy actually had higher mean caloric intakes with no difference in GWG; but a greater number of low birth weight infants than nonsmokers. Similarly, Papoz et al. (1982) found higher mean caloric intake and lower birth weight in women who smoked during pregnancy. More recently, Furuno et al. (2004) found no significant difference in mean GWG between smoking and nonsmoking mothers but did find a slightly increased (1.3-fold) risk for low GWG among smokers.
Although there is limited evidence that cigarette smoking may be inversely associated with GWG there is a preponderance of evidence that supports an independent effect of smoking on birth weight (Muscati et al., 1988; Wolff et al., 1993; Adriananse et al., 1996). Secker-Walker and Vacek (2003) examined the effect of smoking on birth weight independent of GWG and found that gains in infant birth weight among mothers who stopped smoking during pregnancy were not related to GWG, but rather to the independent effect of smoking on birth weight.
Alcohol use Little information is available about effects of alcohol consumption on GWG. Wells et al. (2006) assessed biological, psychological,
and behavioral characteristics to determine associations with inadequate or excessive GWG. This analysis found no significant association between smoking and drinking and GWG outside the IOM (1990) guidelines. Little et al. (1986) found no difference in GWG between infrequent (< 7.5 g/day), occasional (7.5-15 g/day), and regular (≥ 15g/day) alcohol consumers during pregnancy. In a study of determinants of GWG in poor black adolescent mothers, Stevens-Simon and McAnarney (1992) found that alcohol use was more frequent among mothers who experienced rapid GWG. Alcohol, however, is a potent teratogen, and its effects on pregnancy outcome are independent of GWG (Hanson et al., 1978; Little et al., 1986; Jacobsen et al., 1994; Bagheri et al., 1998). Thus, any impact of alcohol consumption on GWG is of little relevance compared to its teratogenic effects.
Drug use Amphetamines are anorectic drugs, and their use during pregnancy would be expected to result in low GWG. Smith et al. (2006) assessed a cohort of 1,618 pregnant women that included 84 methamphetamine users. Analysis of GWG in the methamphetamine-exposed group showed that those who used the drug in the first two trimesters but ceased use by the third trimester gained significantly more weight than either women who used throughout pregnancy or non-exposed women, suggesting the anorexic effects of methamphetamine are limited to continuous use, and there may be a rebound in weight gain if the mother stops use. Nevertheless, this study found exposure to methamphetamines increased the incidence of SGA births 3.5 times over the non-exposed group. Graham et al. (1992) conducted a prospective study with 30 women who were social users of cocaine during the first trimester of pregnancy. No significant differences were found between the drug users and non-users for GWG, delivery complications, birth weight, and other adverse outcomes. Chronic use of cocaine, however, has been shown to be associated with adverse maternal and fetal consequences (Wagner et al., 1998; Ogunyemi and Hernandez-Loera, 2004).
Unintended Pregnancy
Evidence for an effect of unintended pregnancy on GWG appears to be conflicting. Hickey et al. (1997) found that mistimed or unplanned pregnancy was associated with an increased risk for insufficient GWG among black but not among white women. In a study by Siega-Riz and Hobel (1997), planned pregnancy was associated with a marginally statistically significant decreased risk for insufficient GWG, but only among the low and normal weight subjects in a Hispanic cohort. Using data from the National Longitudinal Survey of Labor Market Experiences of Youth, Marsiglio
and Mott (1988) found in a cohort of 6,015 primiparous women that not desiring a pregnancy was not a significant predictor of very low prenatal weight gain. Several large population-based surveys have not found an association between GWG and planned pregnancy (Kost et al., 1998; Wells et al., 2006).
VULNERABLE POPULATIONS
Seasonal Migrant Workers
The actual number of migrant farm workers currently in the United States in not known, but estimates are that at least 3-5 million migrant and seasonal workers come to the United States each year (CDC, 1997). Further, approximately 16 percent of migrant workers are women. Data about GWG among migrant women in four states was obtained through the Pregnancy Nutrition Surveillance System (PNSS). Analysis of the data collected showed that about 52 percent of migrant women gained less than the range recommended by the IOM (1990) compared to 32 percent of non-migrant women. Mean weight gain was also lower for migrant women (22.9 pounds) compared to nonmigrant women (29.7 pounds). However, even though migrant women had lower GWG than nonmigrant women, the prevalence for adverse birth outcomes (low birth weight, very low birth weight, preterm birth, and small-for-gestational age) was similar for both groups (CDC, 1997). Similarly, Reed et al. (2005) found that migrant women had higher rates of pregnancy-related risk factors but lower rates of adverse birth outcomes compared to nonmigrant women.
Military
The committee was unable to identify studies that specifically examined GWG among women in military service. Several studies found women in active-duty experience greater stress but less job control, as well as higher rates of depression, compared to a parity-matched control group of dependent military wives (Magann and Nolan, 1991; O’Boyle et al., 2005), but it is unclear how these factors might influence GWG. One study surveyed pregnant women with deployed partners (Haas and Pazdernik, 2006). Women whose partners were deployed showed a greater tendency to deliver a large infant and reported more stress and changed eating habits, compared to women whose partners were not deployed; however, the results were not statistically significant. No difference was seen in the gestational age at delivery, percentage with vaginal delivery, average number of children at home, self-reported stress, or reported GWG.
Women Incarcerated During Pregnancy
The U.S. Department of Justice estimates that women offenders account for about 16 percent of the total corrections population (Bureau of Justice Statistics, 1999). Recent estimates show that the number of women under the jurisdiction of state or federal prison authorities increased 1.2 percent from year-end 2007, reaching 115,779 (available online at http://www.ojp.usdoj.gov/bjs/prisons.htm [accessed April 13, 2009]). Of women who are incarcerated, most are of child-bearing age and approximately 6 percent are pregnant (Bureau of Justice Statistics, 1994; Safyer and Richmond, 1995).
While there are no studies that have examined the direct effect of incarceration on GWG per se, several studies (Martin et al., 1997a, 1997b; Bell et al., 2004) have examined its effect on birth weight. Martin et al. (1997a) found that a higher number of pregnancy days spent incarcerated was found to be associated with higher infant birth weight. Furthermore, Martin et al. (1997b) also found that infant birth weights among women incarcerated during pregnancy were not significantly different from women never incarcerated; however, infant birth weights were significantly worse among women incarcerated at a time other than during pregnancy than among never-incarcerated women and women incarcerated during pregnancy, suggesting certain aspects of the prison environment, such as shelters and regular meals, may be protective particularly for high-risk pregnant women.
FINDINGS AND RECOMMENDATIONS
Findings
-
There is a lack of evidence on societal/institutional (media, culture/acculturation, health services, policy), environmental (altitude, exposures to environmental toxicants, disasters), and neighborhood determinants (access to healthy foods, opportunities for physical activities) of GWG.
-
Few of the studies reviewed considered the influence of the many possible determinants of GWG among women of different racial/ethnic and socioeconomic groups, or alternatively, adjusted for race/ethnicity or SES in their analyses.
-
There is insufficient evidence to evaluate the influences of psychological factors such as depression, stress, social support, or attitude toward GWG on actual GWG.
-
There remains a lack of information to relate dietary intake or physical activity to GWG even though they are primary determinants of weight gain in nonpregnant individuals.
-
-
Married women are more likely to have appropriate GWG than unmarried women. Intimate partner violence is associated with insufficient GWG. There is a paucity of studies examining the influence of partner/family support on GWG.
-
GWG is generally higher among adolescents and lower among women > 35 years of age, although the relationship of GWG among these groups to birth outcomes, postpartum weight retention, and subsequent risk for overweight/obesity remains unclear.
-
There is a lack of evidence on GWG among vulnerable populations, specifically, seasonal migrant workers, women in military service, and women incarcerated during pregnancy.
-
The IOM (1990) GWG guidelines appear to influence what women believe to be appropriate weight gain during pregnancy, though their influence on actual GWG is less clear in part because many health professionals are providing no or inappropriate advice about weight gain during pregnancy.
-
There is growing evidence suggesting that specific fetal and maternal genes and alleles can influence GWG, though both parental genotypes appear to affect birth weight. The effect of developmental programming and epigenetic events on GWG is strongly suspected, but direct evidence is still lacking. Leptin and adiponectin may represent markers of insulin sensitivity or other mechanisms affecting gestational weight changes.
Research Recommendation
Research Recommendation 4-1: The committee recommends that the National Institutes of Health and other relevant agencies should provide support to researchers to conduct studies in large and diverse populations of women to understand how dietary intake, physical activity, dieting practices, food insecurity and, more broadly, the social, cultural, and environmental context affect GWG.
Areas for Additional Investigation
The committee identified the following areas for further investigation to support its research recommendations. The research community should conduct studies on:
-
Social, cultural, and environmental contexts of GWG. Findings from these studies should help to guide the development of implementation strategies for GWG recommendations;
-
Health care providers’ knowledge, attitude, and behavior with respect to GWG recommendations. These studies should identify
-
facilitators and barriers to adoption of GWG recommendations by health care providers in their clinical practice;
-
Partner and family influences on GWG;
-
Influences of genetic factors, epigenetic events, and developmental programming on GWG;
-
How GWG affects birth outcomes, postpartum weight retention, and overweight and obesity in later life among adolescents and older women. Findings from these studies should be used to reevaluate the appropriateness of GWG recommendations for these women;
-
Determining whether maternal biomarkers such as leptin, adiponectin, and other markers of insulin sensitivity can be used to enhance clinical prediction of adverse birth outcomes and guide further interventions for women with GWG outside the recommended ranges. Data on relevant biomarkers should be made available through databases such as the Federal Human Nutrition Research and Information Management (HNRIM) System Database; and
-
Influences of psychological factors, such as depression, stress, social support, and attitude toward GWG on actual GWG.
The Department of Health and Human Services or other appropriate federal agencies should:
-
Track racial/ethnic and socioeconomic disparities in GWG and that the research community should conduct studies on how GWG affects birth outcomes, postpartum weight retention, and overweight and obesity in later life among women of different racial/ethnic and socioeconomic groups;
-
Collect nationally representative data on dietary intake, physical activity, and food insecurity among prepregnant, pregnant, and postpartum women, and report these data by prepregnancy body mass index (including all classes of obesity), age, racial/ethnic group, and socioeconomic status; and
-
Collect data on GWG among vulnerable populations.
REFERENCES
Abraham S., A. Taylor and J. Conti. 2001. Postnatal depression, eating, exercise, and vomiting before and during pregnancy. International Journal of Eating Disorders 29(4): 482-487.
Abrams B., S. L. Altman and K. E. Pickett. 2000. Pregnancy weight gain: still controversial. American Journal of Clinical Nutrition 71(5 Suppl): 1233S-1241S.
ACOG (American College of Obstetricians and Gynecologists). 2002. ACOG committee opinion. Exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. International Journal of Gynaecology and Obstetrics 77(1): 79-81.
ACOG. 2004. Nausea and vomiting of pregnancy. Practice Bulletin No. 52 103: 803-814.
ACOG. 2005. Committee opinion number 315, September 2005. Obesity in pregnancy. Obstetrics and Gynecology 106(3): 671-675.
Adams E. J., L. Grummer-Strawn and G. Chavez. 2003. Food insecurity is associated with increased risk of obesity in California women. Journal of Nutrition 133(4): 1070-1074.
Adriaanse H. P., J. A. Knottnerus, L. R. Delgado, H. H. Cox and G. G. Essed. 1996. Smoking in Dutch pregnant women and birth weight. Patient Education and Counseling 28(1): 25-30.
Alevizaki M., L. Thalassinou, S. I. Grigorakis, G. Philippou, K. Lili, A. Souvatzoglou and E. Anastasiou. 2000. Study of the Trp64Arg polymorphism of the beta3-adrenergic receptor in Greek women with gestational diabetes. Diabetes Care 23(8): 1079-1083.
Ancri G., E. H. Morse and R. P. Clarke. 1977. Comparison of the nutritional status of pregnant adolescents with adult pregnant women. III. Maternal protein and calorie intake and weight gain in relation to size of infant at birth. American Journal of Clinical Nutrition 30(4): 568-572.
Anderson S. A.1990. Core indicators of nutritional state for difficult-to-sample populations. Journal of Nutrition 120(Suppl 22): 1555-1600.
Artal R., R. B. Catanzaro, J. A. Gavard, D. J. Mostello and J. C. Friganza. 2007. A lifestyle intervention of weight-gain restriction: diet and exercise in obese women with gestational diabetes mellitus. Applied Physiology, Nutrition, and Metabolism 32(3): 596-601.
Arya R., E. Demerath, C. P. Jenkinson, H. H. Goring, S. Puppala, V. Farook, S. Fowler, J. Schneider, R. Granato, R. G. Resendez, T. D. Dyer, S. A. Cole, L. Almasy, A. G. Comuzzie, R. M. Siervogel, B. Bradshaw, R. A. DeFronzo, J. MacCluer, M. P. Stern, B. Towne, J. Blangero and R. Duggirala. 2006. A quantitative trait locus (QTL) on chromosome 6q influences birth weight in two independent family studies. Human Molecular Genetics 15(10): 1569-1579.
Bagheri M. M., L. Burd, J. T. Martsolf and M. G. Klug. 1998. Fetal alcohol syndrome: maternal and neonatal characteristics. Journal of Perinatal Medicine 26(4): 263-269.
Bailit J. L. 2005. Hyperemesis gravidarium: Epidemiologic findings from a large cohort. American Journal of Obstetrics and Gynecology 193(3 Pt 1): 811-814.
Baker A. N. and W. L. Hellerstedt. 2006. Residential racial concentration and birth outcomes by nativity: do neighbors matter? Journal of the National Medical Association 98(2): 172-180.
Barat P., M. Gayard-Cros, R. Andrew, J. B. Corcuff, B. Jouret, N. Barthe, P. Perez, C. Germain, M. Tauber, B. R. Walker, P. Mormede and M. Duclos. 2007. Truncal distribution of fat mass, metabolic profile and hypothalamic-pituitary adrenal axis activity in prepubertal obese children. Journal of Pediatrics150(5): 535-539.
Barker D. J.1998. In utero programming of chronic disease. Clinical Science (London) 95(2): 115-128.
Basiotis P. P. and M. Lino. 2003. Food insufficiency and prevalence of overweight among adult women. Family Economics & Nutrition Review 15(2): 55-57.
Beaty T. H.2007. Invited commentary: two studies of genetic control of birth weight where large data sets were available. American Journal of Epidemiology 165(7): 753-755.
Bell J. F., F. J. Zimmerman, M. L. Cawthon, C. E. Huebner, D. H. Ward and C. A. Schroeder. 2004. Jail incarceration and birth outcomes. Journal of Urban Health 81(4): 630-644.
Bergmann M. M., E. W. Flagg, H. L. Miracle-McMahill and H. Boeing. 1997. Energy intake and net weight gain in pregnant women according to body mass index (BMI) status. International Journal of Obesity and Related Metabolic Disorders 21(11): 1010-1017.
Bjorntorp P. 1993. Visceral obesity: a “civilization syndrome.” Obesity Research 1(3): 206-222.
Bjorntorp P. 1996. The origins and consequences of obesity. Diabetes. Ciba Foundation Symposium 201: 68-80; discussion 80-69, 188-193.
Bjorntorp P. and R. Rosmond. 2000. The metabolic syndrome—a neuroendocrine disorder? British Journal of Nutrition 83(Suppl 1): S49-S57.
Bodnar L. M., K. L. Wisner, E. Moses-Kolko, D. K. Sit and B. H. Hanusa. 2009. Prepregnancy body mass index, gestational weight gain and the likelihood of major depression during pregnancy. Journal of Clinical Psychiatry. Epub ahead of print.
Boy A. and H. M. Salihu. 2004. Intimate partner violence and birth outcomes: a systematic review. International Journal of Fertility and Women’s Medicine 49(4): 159-164.
Brawarsky P., N. E. Stotland, R. A. Jackson, E. Fuentes-Afflick, G. J. Escobar, N. Rubashkin and J. S. Haas. 2005. Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. International Journal of Gynaecology and Obstetrics 91(2): 125-131.
Brofenbrenner U. 1979. The ecology of human development: experiments by nature and design. Cambridge, MA: Harvard University Press.
Brown J. E., T. M. Tharp and C. McKay. 1992. Development of a prenatal weight gain intervention program using social marketing methods. Journal of Nutrition Education 24: 21-28.
Bruce L. and J. G. Tchabo. 1989. Nutrition intervention program in a prenatal clinic. Obstetrics and Gynecology 74(3 Pt 1): 310-312.
Bulik C. M., A. Von Holle, A. M. Siega-Riz, L. Torgersen, K. K. Lie, R. M. Hamer, C. K. Berg, P. Sullivan and T. Reichborn-Kjennerud. 2008. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa). International Journal of Eating Disorders 42(1): 9-18.
Bureau of Justice Statistics. 1994. Women in Prison. Washington, DC: Government Printing Office.
Bureau of Justice Statistics. 1999. Women Offenders. Washington, DC: Government Printing Office.
Butte N. F., W. W. Wong, M. S. Treuth, K. J. Ellis and E. O’Brian Smith. 2004. Energy requirements during pregnancy based on total energy expenditure and energy deposition. American Journal of Clinical Nutrition 79(6): 1078-1087.
Cabral H., L. E. Fried, S. Levenson, H. Amaro and B. Zuckerman. 1990. Foreign-born and US-born black women: differences in health behaviors and birth outcomes. American Journal of Public Health 80(1): 70-72.
Cai G., S. A. Cole, K. Haack, N. F. Butte and A. G. Comuzzie. 2007. Bivariate linkage confirms genetic contribution to fetal origins of childhood growth and cardiovascular disease risk in Hispanic children. Human Genetics 121(6): 737-744.
Callaghan W. M., S. A. Rasmussen, D. J. Jamieson, S. J. Ventura, S. L. Farr, P. D. Sutton, T. J. Mathews, B. E. Hamilton, K. R. Shealy, D. Brantley and S. F. Posner. 2007. Health concerns of women and infants in times of natural disasters: lessons learned from Hurricane Katrina. Maternal and Child Health Journal 11(4): 307-311.
Callister L. C. and A. Birkhead. 2002. Acculturation and perinatal outcomes in Mexican immigrant childbearing women: an integrative review. Journal of Perinatal and Neonatal Nursing 16(3): 22-38.
Cameron R. P., C. M. Grabill, S. E. Hobfoll, J. H. Crowther, C. Ritter and J. Lavin. 1996. Weight, self-esteem, ethnicity, and depressive symptomatology during pregnancy among inner-city women. Health Psychology 15(4): 293-297.
Campbell D.1983. Dietary restriction in obesity and its effect on neonatal outcome. In Nutrition in Pregnancy. Proceedings of 10th Study Group of the RCOG. Campbell DM and G. MDG. London: RCOG; pp. 85-98.
Campbell D. M. and I. MacGillivray. 1975. The effect of a low calorie diet or a thiazide diuretic on the incidence of pre-eclampsia and on birth weight. British Journal of Obstetrics and Gynaecology 82(7): 572-577.
Carmichael S. L., G. M. Shaw, D. M. Schaffer, C. Laurent and S. Selvin. 2003. Dieting behaviors and risk of neural tube defects. American Journal of Epidemiology 158(12): 1127-1131.
Casanueva E., D. Legarreta, M. Diaz-Barriga, Y. Soberanis, T. Cardenas, A. Iturriaga, T. Lartigue and J. Vives. 1994. Weight gain during pregnancy in adolescents: evaluation of a non-nutritional intervention. Revista de Investigacion Clinica 46(2): 157-161.
Casanueva E., J. Labastida, C. Sanz and F. Morales-Carmona. 2000. Depression and body fat deposition in Mexican pregnant adolescents. Archives of Medical Research 31(1): 48-52.
Catalano P. M., E. D. Tyzbir, R. R. Wolfe, J. Calles, N. M. Roman, S. B. Amini and E. A. Sims. 1993. Carbohydrate metabolism during pregnancy in control subjects and women with gestational diabetes. American Journal of Physiology 264(1 Pt 1): E60-E67.
Catalano P. M., N. M. Roman-Drago, S. B. Amini and E. A. Sims. 1998. Longitudinal changes in body composition and energy balance in lean women with normal and abnormal glucose tolerance during pregnancy. American Journal of Obstetrics and Gynecology 179(1): 156-165.
Catalano P. M., L. Huston, S. B. Amini and S. C. Kalhan. 1999. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. American Journal of Obstetrics and Gynecology 180(4): 903-916.
Caulfield L. E., F. R. Witter and R. J. Stoltzfus. 1996. Determinants of gestational weight gain outside the recommended ranges among black and white women. Obstetrics and Gynecology 87(5 Pt 1): 760-766.
CDC (Centers for Disease Control and Prevention). 1989. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
CDC. 1991. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
CDC. 1997. Pregnancy-related behaviors among migrant farm workers—four states, 1989-1993. Morbidity and Mortality Weekly Report 46(13): 283-286.
CDC. 2003. Self-reported concern about food security associated with obesity—Washington, 1995-1999. Morbidity and Mortality Weekly Report 52(35): 840-842.
Chen X. K., S. W. Wen, N. Fleming, K. Demissie, G. G. Rhoads and M. Walker. 2007. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. International Journal of Epidemiology 36(2): 368-373.
Chu S. Y., W. M. Callaghan, C. L. Bish and D. D’Angelo. 2009. Gestational weight gain by body mass index among US women delivering live births, 2004-2005: fueling future obesity. American Journal of Obstetrics and Gynecology 200(3): 271 e271-e277.
Clapp J. F., III. 2002. Maternal carbohydrate intake and pregnancy outcome. Proceedings of the Nutrition Society 61(1): 45-50.
Clapp J. F., III and K. D. Little. 1995. Effect of recreational exercise on pregnancy weight gain and subcutaneous fat deposition. Medicine and Science in Sports and Exercise 27(2): 170-177.
Cnattingius S., M. R. Forman, H. W. Berendes and L. Isotalo. 1992. Delayed childbearing and risk of adverse perinatal outcome. A population-based study. Journal of the American Medical Association 268(7): 886-890.
Cnop M., P. J. Havel, K. M. Utzschneider, D. B. Carr, M. K. Sinha, E. J. Boyko, B. M. Retzlaff, R. H. Knopp, J. D. Brunzell and S. E. Kahn. 2003. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia 46(4): 459-469.
Cogswell M. E., M. K. Serdula, A. H. Mokdad and D. F. Williamson. 1996. Attempted weight loss during pregnancy. International Journal of Obesity and Related Metabolic Disorders 20(4): 373-375.
Cogswell M. E., K. S. Scanlon, S. B. Fein and L. A. Schieve. 1999. Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstetrics and Gynecology 94(4): 616-622.
Cohen J. H. and H. Kim. 2009. Sociodemographic and health characteristics associated with attempting weight loss during pregnancy. Preventing Chronic Disease 6(1): A07.
Copper R. L., M. B. DuBard, R. L. Goldenberg and A. I. Oweis. 1995. The relationship of maternal attitude toward weight gain to weight gain during pregnancy and low birth weight. Obstetrics and Gynecology 85(4): 590-595.
Cordero J. F. 1993. The epidemiology of disasters and adverse reproductive outcomes: lessons learned. Environmental Health Perspectives 101(Suppl 2): 131-136.
Crawford P. B., M. S. Townsend and D. L. Metz. 2004. How can Californians be overweight and hungry? California Agriculture 58(1): 12-17.
Cunningham F. G., J. C. Hauth, K. J. Leveno, L. Gilstrap III, S. L. Bloom and K. D. Wenstrom, Eds. 2005. Williams Obstetrics 22nd Ed. New York: McGraw-Hill Medical Publishing Division.
Dar E., M. S. Kanarek, H. A. Anderson and W. C. Sonzogni. 1992. Fish consumption and reproductive outcomes in Green Bay, Wisconsin. Environmental Research 59(1): 189-201.
Davis M. M., K. Slish, C. Chao and M. D. Cabana. 2006. National trends in bariatric surgery, 1996-2002. Archives of Surgery 141(1): 71-74; discussion 75.
Deierlein A. L., A. M. Siega-Riz and A. Herring. 2008. Dietary energy density but not glycemic load is associated with gestational weight gain. American Journal of Clinical Nutrition 88(3): 693-699.
Delpisheh A., L. Brabin, E. Attia and B. J. Brabin. 2008. Pregnancy late in life: a hospital-based study of birth outcomes. Journal of Women’s Health (Larchmt) 17(6): 965-970.
Dipietro J. A., S. Millet, K. A. Costigan, E. Gurewitsch and L. E. Caulfield. 2003. Psychosocial influences on weight gain attitudes and behaviors during pregnancy. Journal of the American Dietetic Association 103(10): 1314-1319.
Dishy V., S. Gupta, R. Landau, H. G. Xie, R. B. Kim, R. M. Smiley, D. W. Byrne, A. J. Wood and C. M. Stein. 2003. G-protein beta (3) subunit 825 C/T polymorphism is associated with weight gain during pregnancy. Pharmacogenetics 13(4): 241-242.
Dixon J. B., M. E. Dixon and P. E. O’Brien. 2005. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstetrics and Gynecology 106(5 Pt 1): 965-972.
Drewnowski A. and N. Darmon. 2005. Food choices and diet costs: an economic analysis. Journal of Nutrition 135(4): 900-904.
Dubois L., M. Girard, A. Girard, R. Tremblay, M. Boivin and D. Perusse. 2007. Genetic and environmental influences on body size in early childhood: a twin birth-cohort study. Twin Research and Human Genetics 10(3): 479-485.
Ducarme G., A. Revaux, A. Rodrigues, F. Aissaoui, I. Pharisien and M. Uzan. 2007. Obstetric outcome following laparoscopic adjustable gastric banding. International Journal of Gynaecology and Obstetrics 98(3): 244-247.
Duncombe D., H. Skouteris, E. H. Wertheim, L. Kelly, V. Fraser and S. J. Paxton. 2006. Vigorous exercise and birth outcomes in a sample of recreational exercisers: a prospective study across pregnancy. Australian and New Zealand Journal of Obstetrics and Gynaecology 46(4): 288-292.
Durnin J. V. 1991. Energy requirements of pregnancy. Diabetes 40(Suppl 2): 152-156.
Edghill E. L., C. Bingham, A. S. Slingerland, J. A. Minton, C. Noordam, S. Ellard and A. T. Hattersley. 2006. Hepatocyte nuclear factor-1 beta mutations cause neonatal diabetes and intrauterine growth retardation: support for a critical role of HNF-1beta in human pancreatic development. Diabetic Medicine 23(12): 1301-1306.
Endres J. M., K. Poell-Odenwald, M. Sawicki and P. Welch. 1985. Dietary assessment of pregnant adolescents participating in a supplemental-food program. Journal of Reproductive Medicine 30(1): 10-17.
Endres J., S. Dunning, S. W. Poon, P. Welch and H. Duncan. 1987. Older pregnant women and adolescents: nutrition data after enrollment in WIC. Journal of the American Dietetic Association 87(8): 1011-1016, 1019.
Epstein L. H., J. N. Roemmich, J. L. Robinson, R. A. Paluch, D. D. Winiewicz, J. H. Fuerch and T. N. Robinson. 2008. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Archives of Pediatrics and Adolescent Medicine 162(3): 239-245.
Eskenazi B., A. R. Marks, R. Catalano, T. Bruckner and P. G. Toniolo. 2007. Low birthweight in New York City and upstate New York following the events of September 11th. Human Reproduction 22(11): 3013-3020.
Evenson K. R., A. M. Siega-Riz, D. A. Savitz, J. A. Leiferman and J. M. Thorp, Jr. 2002. Vigorous leisure activity and pregnancy outcome. Epidemiology 13(6): 653-659.
Fallucca F., M. G. Dalfra, E. Sciullo, M. Masin, A. M. Buongiorno, A. Napoli, D. Fedele and A. Lapolla. 2006. Polymorphisms of insulin receptor substrate 1 and beta3-adrenergic receptor genes in gestational diabetes and normal pregnancy. Metabolism 55(11): 1451-1456.
Festa A., W. Krugluger, N. Shnawa, P. Hopmeier, S. M. Haffner and G. Schernthaner. 1999. Trp64Arg polymorphism of the beta3-adrenergic receptor gene in pregnancy: association with mild gestational diabetes mellitus. Journal of Clinical Endocrinology and Metabolism 84(5): 1695-1699.
Fonager K., H. T. Sorensen, J. Olsen, J. F. Dahlerup and S. N. Rasmussen. 1998. Pregnancy outcome for women with Crohn’s disease: a follow-up study based on linkage between national registries. American Journal of Gastroenterology 93(12): 2426-2430.
Forsum E., A. Sadurskis and J. Wager. 1985. Energy maintenance cost during pregnancy in healthy Swedish women. Lancet 1(8420): 107-108.
Fraga M. F., E. Ballestar, M. F. Paz, S. Ropero, F. Setien, M. L. Ballestar, D. Heine-Suner, J. C. Cigudosa, M. Urioste, J. Benitez, M. Boix-Chornet, A. Sanchez-Aguilera, C. Ling, E. Carlsson, P. Poulsen, A. Vaag, Z. Stephan, T. D. Spector, Y. Z. Wu, C. Plass and M. Esteller. 2005. Epigenetic differences arise during the lifetime of monozygotic twins. Proceedings of the National Academy of Sciences of the United States of America 102(30): 10604-10609.
Fretts R. C. 2005. Etiology and prevention of stillbirth. American Journal of Obstetrics and Gynecology 193(6): 1923-1935.
Frisancho A. R., J. Matos and P. Flegel. 1983. Maternal nutritional status and adolescent pregnancy outcome. American Journal of Clinical Nutrition 38(5): 739-746.
Frongillo E. A., Jr., B. S. Rauschenbach, C. M. Olson, A. Kendall and A. G. Colmenares. 1997. Questionnaire-based measures are valid for the identification of rural households with hunger and food insecurity. Journal of Nutrition 127(5): 699-705.
Fuentes-Afflick E. and N. A. Hessol. 2008. Acculturation and body mass among Latina women. Journal of Women’s Health (Larchmt) 17(1): 67-73.
Fuentes-Afflick E. and P. Lurie. 1997. Low birth weight and Latino ethnicity. Examining the epidemiologic paradox. Archives of Pediatrics and Adolescent Medicine 151(7): 665-674.
Furneaux E. C., A. J. Langley-Evans and S. C. Langley-Evans. 2001. Nausea and vomiting of pregnancy: endocrine basis and contribution to pregnancy outcome. Obstetrical and Gynecological Survey 56(12): 775-782.
Furuno J. P., L. Gallicchio and M. Sexton. 2004. Cigarette smoking and low maternal weight gain in Medicaid-eligible pregnant women. Journal of Women’s Health (Larchmt) 13(7): 770-777.
Garn S. M., K. Hoff and K. D. McCabe. 1979. Is there nutritional mediation of the “smoking effect” on the fetus. American Journal of Clinical Nutrition 32(6): 1181-1184.
Gavard J. A. and R. Artal. 2008. Effect of exercise on pregnancy outcome. Clinical Obstetrics and Gynecology 51(2): 467-480.
Gigante D. P., K. M. Rasmussen and C. G. Victora. 2005. Pregnancy increases BMI in adolescents of a population-based birth cohort. Journal of Nutrition 135(1): 74-80.
Glynn L. M., P. D. Wadhwa, C. Dunkel-Schetter, A. Chicz-Demet and C. A. Sandman. 2001. When stress happens matters: effects of earthquake timing on stress responsivity in pregnancy. American Journal of Obstetrics and Gynecology 184(4): 637-642.
Goldberg G. R., A. M. Prentice, W. A. Coward, H. L. Davies, P. R. Murgatroyd, C. Wensing, A. E. Black, M. Harding and M. Sawyer. 1993. Longitudinal assessment of energy expenditure in pregnancy by the doubly labeled water method. American Journal of Clinical Nutrition 57(4): 494-505.
Goodwin T. M. 2002. Nausea and vomiting of pregnancy: an obstetric syndrome. American Journal of Obstetrics and Gynecology 186(5 Suppl Understanding): S184-S189.
Goodwin T. M., M. Montoro and J. H. Mestman. 1992. Transient hyperthyroidism and hyperemesis gravidarum: clinical aspects. American Journal of Obstetrics and Gynecology 167(3): 648-652.
Gortmaker S. L., A. Must, A. M. Sobol, K. Peterson, G. A. Colditz and W. H. Dietz. 1996. Television viewing as a cause of increasing obesity among children in the United States, 1986-1990. Archives of Pediatrics and Adolescent Medicine 150(4): 356-362.
Gortmaker S. L., K. Peterson, J. Wiecha, A. M. Sobol, S. Dixit, M. K. Fox and N. Laird. 1999. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Archives of Pediatrics and Adolescent Medicine 153(4): 409-418.
Graham K., A. Feigenbaum, A. Pastuszak, I. Nulman, R. Weksberg, T. Einarson, S. Goldberg, S. Ashby and G. Koren. 1992. Pregnancy outcome and infant development following gestational cocaine use by social cocaine users in Toronto, Canada. Clinical and Investigative Medicine. Medicine Clinique et Experimentale 15(4): 384-394.
Griffiths L. J., C. Dezateux and T. J. Cole. 2007. Differential parental weight and height contributions to offspring birthweight and weight gain in infancy. International Journal of Epidemiology 36(1): 104-107.
Gross S., C. Librach and A. Cecutti. 1989. Maternal weight loss associated with hyperemesis gravidarum: a predictor of fetal outcome. American Journal of Obstetrics and Gynecology 160(4): 906-909.
Gross T., R. J. Sokol and K. C. King. 1980. Obesity in pregnancy: risks and outcome. Obstetrics and Gynecology 56(4): 446-450.
Groth S. W. 2008. The long-term impact of adolescent gestational weight gain. Research in Nursing and Health 31(2): 108-118.
Gunderson E. P., R. Striegel-Moore, G. Schreiber, M. Hudes, F. Biro, S. Daniels and P. B. Crawford. 2009. Longitudinal study of growth and adiposity in parous compared with nulligravid adolescents. Archives of Pediatrics and Adolescent Medicine 163(4): 349-356.
Gurewitsch E. D., M. Smith-Levitin and J. Mack. 1996. Pregnancy following gastric bypass surgery for morbid obesity. Obstetrics and Gynecology 88(4 Pt 2): 658-661.
Gutierrez Y. M. 1999. Cultural factors affecting diet and pregnancy outcome of Mexican American adolescents. Journal of Adolescent Health 25(3): 227-237.
Haakstad L. A., N. Voldner, T. Henriksen and K. Bo. 2007. Physical activity level and weight gain in a cohort of pregnant Norwegian women. Acta Obstetricia et Gynecologica Scandinavica 86(5): 559-564.
Haas D. M. and L. A. Pazdernik. 2006. A cross-sectional survey of stressors for postpartum women during wartime in a military medical facility. Military Medicine 171(10): 1020-1023.
Haiek L. and S. A. Lederman. 1989. The relationship between maternal weight for height and term birth weight in teens and adult women. Journal of Adolescent Health Care 10(1): 16-22.
Hanson J. W., A. P. Streissguth and D. W. Smith. 1978. The effects of moderate alcohol consumption during pregnancy on fetal growth and morphogenesis. Journal of Pediatrics 92(3): 457-460.
Hastings G., M. Stead, L. McDermot, A. Forsyth, A. MacKintosh, M. Rayner, C. Godfrey, M. Caraher and K. Angus. 2003. Review of Research on the Effects of Food Promotion to Children. Glasgow, UK: Centre for Social Marketing.
Hattersley A. T., F. Beards, E. Ballantyne, M. Appleton, R. Harvey and S. Ellard. 1998. Mutations in the glucokinase gene of the fetus result in reduced birth weight. Nature Genetics 19(3): 268-270.
Hauguel-de Mouzon S., J. Lepercq and P. Catalano. 2006. The known and unknown of leptin in pregnancy. American Journal of Obstetrics and Gynecology 194(6): 1537-1545.
Haworth J. C., J. J. Ellestad-Sayed, J. King and L. A. Dilling. 1980. Relation of maternal cigarette smoking, obesity, and energy consumption to infant size. American Journal of Obstetrics and Gynecology 138(8): 1185-1189.
Hediger M. L., T. O. Scholl, I. G. Ances, D. H. Belsky and R. W. Salmon. 1990. Rate and amount of weight gain during adolescent pregnancy: associations with maternal weight-for-height and birth weight. American Journal of Clinical Nutrition 52(5): 793-799.
Hegaard H. K., B. K. Pedersen, B. B. Nielsen and P. Damm. 2007. Leisure time physical activity during pregnancy and impact on gestational diabetes mellitus, pre-eclampsia, preterm delivery and birth weight: a review. Acta Obstetricia et Gynecologica Scandinavica 86(11): 1290-1296.
Hernandez-Valero M. A., A. V. Wilkinson, M. R. Forman, C. J. Etzel, Y. Cao, C. H. Barcenas, S. S. Strom, M. R. Spitz and M. L. Bondy. 2007. Maternal BMI and country of birth as indicators of childhood obesity in children of Mexican origin. Obesity (Silver Spring) 15(10): 2512-2519.
HHS (U.S. Department of Health and Human Services). 1989. Caring for Our Future: The Content of Prenatal Care. A Report of the Public Health Service Expert Panel on the Content of Prenatal Care. Washington, DC: U.S. Public Health Service.
HHS. 2008. Physical Activity Guidelines Advisory Committee Report. Washington, DC: Author.
Hickey C. A. 2000. Sociocultural and behavioral influences on weight gain during pregnancy. American Journal of Clinical Nutrition 71(5 Suppl): 1364S-1370S.
Hickey C. A., S. P. Cliver, R. L. Goldenberg, S. F. McNeal and H. J. Hoffman. 1995. Relationship of psychosocial status to low prenatal weight gain among nonobese black and white women delivering at term. Obstetrics and Gynecology 86(2): 177-183.
Hickey C. A., S. P. Cliver, R. L. Goldenberg, S. F. McNeal and H. J. Hoffman. 1997. Low prenatal weight gain among low-income women: what are the risk factors? Birth 24(2): 102-108.
Highman T. J., J. E. Friedman, L. P. Huston, W. W. Wong and P. M. Catalano. 1998. Longitudinal changes in maternal serum leptin concentrations, body composition, and resting metabolic rate in pregnancy. American Journal of Obstetrics and Gynecology 178(5): 1010-1015.
Hill J. O., W. H. Saris and J. A. Levine. 2004. Energy Expenditure in Physical Activity. In Handbook of Obesity: Etiology and Pathophysiology, 2nd Ed. G. A. Bray and C. Bouchard. New York: Marcel Dekker Inc.
Hinton P. S. and C. M. Olson. 2001. Predictors of pregnancy-associated change in physical activity in a rural white population. Maternal and Child Health Journal 5(1): 7-14.
Horon I. L., D. M. Strobino and H. M. MacDonald. 1983. Birth weights among infants born to adolescent and young adult women. American Journal of Obstetrics and Gynecology 146(4): 444-449.
Howie L. D., J. D. Parker and K. C. Schoendorf. 2003. Excessive maternal weight gain patterns in adolescents. Journal of the American Dietetic Association 103(12): 1653-1657.
Hubert H. B., J. Snider and M. A. Winkleby. 2005. Health status, health behaviors, and acculturation factors associated with overweight and obesity in Latinos from a community and agricultural labor camp survey. Preventive Medicine 40(6): 642-651.
Hytten F. and G. Chamberlain. 1991. Clinical Physiology in Obstetrics. Oxford: Blackwell Scientific Publications.
International Dietary Energy Consulting Group. 1990. The Doubly-Labeled Water Method for Measuring Energy Expenditure: Technical Recommendations for Use in Humans. Vienna: NAHRES-4 International Atomic Energy Agency.
IOM (Institute of Medicine). 1990. Nutrition During Pregnancy. Washington, DC: National Academy Press.
IOM. 1992. Nutrition During Pregnancy and Lactation: An Implementation Guide. Washington, DC: National Academy Press.
IOM. 2000. Promoting Health: Intervention Strategies from Social and Behavioral Sciences. Washington, DC: National Academy Press.
IOM. 2005. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press.
IOM. 2006. Food Marketing to Children and Youth. Washington, DC: The National Academies Press.
IOM. 2007. Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth. Washington, DC: The National Academies Press.
Jacobson J. L., S. W. Jacobson, R. J. Sokol, S. S. Martier, J. W. Ager and S. Shankaran. 1994. Effects of alcohol use, smoking, and illicit drug use on fetal growth in black infants. Journal of Pediatrics 124(5 Pt 1): 757-764.
Jaquet D., S. Swaminathan, G. R. Alexander, P. Czernichow, D. Collin, H. M. Salihu, R. S. Kirby and C. Levy-Marchal. 2005. Significant paternal contribution to the risk of small for gestational age. British Journal of Obstetrics and Gynaecology 112(2): 153-159.
Jensen G. M. and L. G. Moore. 1997. The effect of high altitude and other risk factors on birthweight: independent or interactive effects? American Journal of Public Health 87(6): 1003-1007.
Jewell D. and G. Young. 2003. Interventions for Nausea and Vomiting in Early Pregnancy. Chichester, UK: John Wiley & Sons, Ltd.
Jones M. E. and M. L. Bond. 1999. Predictors of birth outcome among Hispanic immigrant women. Journal of Nursing Care Quality 14(1): 56-62.
Jones S. J. and E. A. Frongillo. 2007. Food insecurity and subsequent weight gain in women. Public Health Nutrition 10(2): 145-151.
Joseph K. S., A. C. Allen, L. Dodds, L. A. Turner, H. Scott and R. Liston. 2005. The perinatal effects of delayed childbearing. Obstetrics and Gynecology 105(6): 1410-1418.
Joyce T., A. Racine and C. Yunzal-Butler. 2008. Reassessing the WIC effect: evidence from the Pregnancy Nutrition Surveillance System. Journal of Policy Analysis and Management 27(2): 277-303.
King J. C. 2000. Physiology of pregnancy and nutrient metabolism. American Journal of Clinical Nutrition 71(5 Suppl): 1218S-1225S.
Kirwan J. P., S. Hauguel-De Mouzon, J. Lepercq, J. C. Challier, L. Huston-Presley, J. E. Friedman, S. C. Kalhan and P. M. Catalano. 2002. TNF-alpha is a predictor of insulin resistance in human pregnancy. Diabetes 51(7): 2207-2213.
Kleinman J. C., L. A. Fingerhut and K. Prager. 1991. Differences in infant mortality by race, nativity status, and other maternal characteristics. American Journal of Diseases of Children 145(2): 194-199.
Kost K., D. J. Landry and J. E. Darroch. 1998. The effects of pregnancy planning status on birth outcomes and infant care. Family Planning Perspectives 30(5): 223-230.
Kouba S., T. Hallstrom, C. Lindholm and A. L. Hirschberg. 2005. Pregnancy and neonatal outcomes in women with eating disorders. Obstetrics and Gynecology 105(2): 255-260.
Kramer M. S. and R. Kakuma. 2003. Energy and protein intake in pregnancy. Cochrane Database of Systematic Reviews (4): CD000032.
Kramer M. S. and S. W. McDonald. 2006. Aerobic exercise for women during pregnancy. Cochrane Database of Systematic Reviews (3): CD000180.
Kuh D. and Y. Ben-Shlomo. 1997. A Life Course Approach to Chronic Disease Epidemiology: Tracing the Origins of Ill-health from Early to Adult Life. Oxford: Oxford University Press.
Kunkel K. 2001. Children and Television Advertising. In Handbook of Children and the Media. D. Singer and J. Singer. Thousand Oaks, CA: Sage Publishing.
Lagiou P., R. M. Tamimi, L. A. Mucci, H. O. Adami, C. C. Hsieh and D. Trichopoulos. 2004. Diet during pregnancy in relation to maternal weight gain and birth size. European Journal of Clinical Nutrition 58(2): 231-237.
Landrigan P. J., J. Forman, M. Galvez, B. Newman, S. M. Engel and C. Chemtob. 2008. Impact of September 11 World Trade Center disaster on children and pregnant women. Mount Sinai Journal of Medicine 75(2): 129-134.
Lane S. D., R. H. Keefe, R. Rubinstein, B. A. Levandowski, N. Webster, D. A. Cibula, A. K. Boahene, O. Dele-Michael, D. Carter, T. Jones, M. Wojtowycz and J. Brill. 2008. Structural violence, urban retail food markets, and low birth weight. Health & Place 14(3): 415-423.
Laraia B. A., A. M. Siega-Riz, J. S. Kaufman and S. J. Jones. 2004. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Preventive Medicine 39(5): 869-875.
Laraia B., L. Messer, K. Evenson and J. S. Kaufman. 2007. Neighborhood factors associated with physical activity and adequacy of weight gain during pregnancy. Journal of Urban Health 84(6): 793-806.
Lawrence M., J. Singh, F. Lawrence and R. G. Whitehead. 1985. The energy cost of common daily activities in African women: increased expenditure in pregnancy? American Journal of Clinical Nutrition 42(5): 753-763.
Lederman S. A., V. Rauh, L. Weiss, J. L. Stein, L. A. Hoepner, M. Becker and F. P. Perera. 2004. The effects of the World Trade Center event on birth outcomes among term deliveries at three lower Manhattan hospitals. Environmental Health Perspectives 112(17): 1772-1778.
Leet T. and L. Flick. 2003. Effect of exercise on birthweight. Clinical Obstetrics and Gynecology 46(2): 423-431.
Lindsay R. S., S. Kobes, W. C. Knowler and R. L. Hanson. 2002. Genome-wide linkage analysis assessing parent-of-origin effects in the inheritance of birth weight. Human Genetics 110(5): 503-509.
Little R. E., R. L. Asker, P. D. Sampson and J. H. Renwick. 1986. Fetal growth and moderate drinking in early pregnancy. American Journal of Epidemiology 123(2): 270-278.
Lizarzaburu J. L. and L. A. Palinkas. 2002. Immigration, acculturation, and risk factors for obesity and cardiovascular disease: a comparison between Latinos of Peruvian descent in Peru and in the United States. Ethnicity and Disease 12(3): 342-352.
Lof M., L. Hilakivi-Clarke, S. Sandin and E. Weiderpass. 2008. Effects of pre-pregnancy physical activity and maternal BMI on gestational weight gain and birth weight. Acta Obstetricia et Gynecologica Scandinavica 87(5): 524-530.
Lokey E. A., Z. V. Tran, C. L. Wells, B. C. Myers and A. C. Tran. 1991. Effects of physical exercise on pregnancy outcomes: a meta-analytic review. Medicine and Science in Sports and Exercise 23(11): 1234-1239.
Lopez-Bermejo A., C. J. Petry, M. Diaz, G. Sebastiani, F. de Zegher, D. B. Dunger and L. Ibanez. 2008. The association between the FTO gene and fat mass in humans develops by the postnatal age of two weeks. Journal of Clinical Endocrinology and Metabolism 93(4): 1501-1505.
Loris P., K. G. Dewey and K. Poirier-Brode. 1985. Weight gain and dietary intake of pregnant teenagers. Journal of the American Dietetic Association 85(10): 1296-1305.
Lunde A., K. K. Melve, H. K. Gjessing, R. Skjaerven and L. M. Irgens. 2007. Genetic and environmental influences on birth weight, birth length, head circumference, and gestational age by use of population-based parent-offspring data. American Journal of Epidemiology 165(7): 734-741.
Magann E. F. and T. E. Nolan. 1991. Pregnancy outcome in an active-duty population. Obstetrics and Gynecology 78(3 Pt 1): 391-393.
Magnus P., H. K. Gjessing, A. Skrondal and R. Skjaerven. 2001. Paternal contribution to birth weight. Journal of Epidemiology and Community Health 55(12): 873-877.
Marceau P., D. Kaufman, S. Biron, F. S. Hould, S. Lebel, S. Marceau and J. G. Kral. 2004. Outcome of pregnancies after biliopancreatic diversion. Obesity Surgery 14(3): 318-324.
Marsiglio W. and F. L. Mott. 1988. Does wanting to become pregnant with a first child affect subsequent maternal behaviors and infant birth weight? Journal of Marriage and the Family 50(4): 1023-1036.
Martin S. L., H. Kim, L. L. Kupper, R. E. Meyer and M. Hays. 1997a. Is incarceration during pregnancy associated with infant birthweight? American Journal of Public Health 87(9): 1526-1531.
Martin S. L., R. H. Rieger, L. L. Kupper, R. E. Meyer and B. F. Qaqish. 1997b. The effect of incarceration during pregnancy on birth outcomes. Public Health Reports 112(4): 340-346.
McAnarney E. R. and C. Stevens-Simon. 1993. First, do no harm. Low birth weight and adolescent obesity. American Journal of Diseases of Children 147(9): 983-985.
McCarthy M. I. and A. T. Hattersley. 2008. Learning from molecular genetics: novel insights arising from the definition of genes for monogenic and type 2 diabetes. Diabetes 57(11): 2889-2898.
McFarlane J., B. Parker and K. Soeken. 1996. Abuse during pregnancy: associations with maternal health and infant birth weight. Nursing Research 45(1): 37-42.
Meserole L. P., B. S. Worthington-Roberts, J. M. Rees and L. S. Wright. 1984. Prenatal weight gain and postpartum weight loss patterns in adolescents. Journal of Adolescent Health Care 5(1): 21-27.
Moraes C. L., A. R. Amorim and M. E. Reichenheim. 2006. Gestational weight gain differentials in the presence of intimate partner violence. International Journal of Gynaecology and Obstetrics 95(3): 254-260.
Morris D. L., A. B. Berenson, J. Lawson and C. M. Wiemann. 1993. Comparison of adolescent pregnancy outcomes by prenatal care source. Journal of Reproductive Medicine 38(5): 375-380.
Morris S. N. and N. R. Johnson. 2005. Exercise during pregnancy: a critical appraisal of the literature. Journal of Reproductive Medicine 50(3): 181-188.
Muscati S., M. Mackey and B. Newsome. 1988. The influence of smoking and stress on prenatal weight gain and infant birth weight of teenage mothers. Journal of Nutrition Education 20: 299-302.
Nielsen J. N., K.O. O’Brien, F. R. Witter, S. C. Chang, J. Mancini, M. S. Nathanson and L. E. Caulfield. 2006. High gestational weight gain does not improve birth weight in a cohort of African American adolescents. American Journal of Clinical Nutrition 84(1): 183-189.
O’Boyle A. L., E. F. Magann, R. E. Ricks, Jr., M. Doyle and J. C. Morrison. 2005. Depression screening in the pregnant soldier wellness program. Southern Medical Journal 98(4): 416-418.
Ogunyemi D. and G. E. Hernandez-Loera. 2004. The impact of antenatal cocaine use on maternal characteristics and neonatal outcomes. Journal of Maternal-Fetal & Neonatal Medicine 15(4): 253-259.
Ohlin A. and S. Rossner. 1994. Trends in eating patterns, physical activity and sociodemographic factors in relation to postpartum body weight development. British Journal of Nutrition 71(4): 457-470.
Okereke N. C., L. Huston-Presley, S. B. Amini, S. Kalhan and P. M. Catalano. 2004. Longitudinal changes in energy expenditure and body composition in obese women with normal and impaired glucose tolerance. American Journal of Physiology Endocrinology and Metabolism 287(3): E472-E479.
Olafsdottir A. S., G. V. Skuladottir, I. Thorsdottir, A. Hauksson and L. Steingrimsdottir. 2006. Maternal diet in early and late pregnancy in relation to weight gain. International Journal of Obesity (London) 30(3): 492-499.
Olds D. L., C. R. Henderson, Jr., R. Tatelbaum and R. Chamberlin. 1986. Improving the delivery of prenatal care and outcomes of pregnancy: a randomized trial of nurse home visitation. Pediatrics 77(1): 16-28.
Olson C. M. 1999. Nutrition and health outcomes associated with food insecurity and hunger. Journal of Nutrition 129(2S Suppl): 521S-524S.
Olson C. M. and M. S. Strawderman. 2003. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. Journal of the American Dietetic Association 103(1): 48-54.
Olson C. M. and M. S. Strawderman. 2008. The relationship between food insecurity and obesity in rural childbearing women. Journal of Rural Health 24(1): 60-66.
Orr S. T., S. A. James, C. A. Miller, B. Barakat, N. Daikoku, M. Pupkin, K. Engstrom and G. Huggins. 1996. Psychosocial stressors and low birthweight in an urban population. American Journal of Preventive Medicine 12(6): 459-466.
Orstead C., D. Arrington, S. K. Kamath, R. Olson and M. B. Kohrs. 1985. Efficacy of prenatal nutrition counseling: weight gain, infant birth weight, and cost-effectiveness. Journal of the American Dietetic Association 85(1): 40-45.
Palmer J. L., G. E. Jennings and L. Massey. 1985. Development of an assessment form: attitude toward weight gain during pregnancy. Journal of the American Dietetic Association 85(8): 946-949.
Papoz L., E. Eschwege, G. Pequignot, J. Barrat and D. Schwartz. 1982. Maternal smoking and birth weight in relation to dietary habits. American Journal of Obstetrics and Gynecology 142(7): 870-876.
Parker B., J. McFarlane and K. Soeken. 1994. Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstetrics and Gynecology 84(3): 323-328.
Pasquali R., V. Vicennati, M. Cacciari and U. Pagotto. 2006. The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Annals of the New York Academy of Sciences 1083: 111-128.
Pearson E. R., S. F. Boj, A. M. Steele, T. Barrett, K. Stals, J. P. Shield, S. Ellard, J. Ferrer and A. T. Hattersley. 2007. Macrosomia and hyperinsulinaemic hypoglycaemia in patients with heterozygous mutations in the HNF4A gene. Public Library of Science Medicine 4(4): e118.
Picone T. A., L. H. Allen, M. M. Schramm and P. N. Olsen. 1982. Pregnancy outcome in North American women. I. Effects of diet, cigarette smoking, and psychological stress on maternal weight gain. American Journal of Clinical Nutrition 36(6): 1205-1213.
Pinar H., S. Basu, K. Hotmire, L. Laffineuse, L. Presley, M. Carpenter, P. M. Catalano and S. Hauguel-de Mouzon. 2008. High molecular mass multimer complexes and vascular expression contribute to high adiponectin in the fetus. Journal of Clinical Endocrinology and Metabolism 93(7): 2885-2890.
Polivy J. 1996. Psychological consequences of food restriction. Journal of the American Dietetic Association 96(6): 589-592; quiz 593-594.
Power M. L., M. E. Cogswell and J. Schulkin. 2006. Obesity prevention and treatment practices of U.S. obstetrician-gynecologists. Obstetrics and Gynecology 108(4): 961-968.
Prentice A. M., G. R. Goldberg, H. L. Davies, P. R. Murgatroyd and W. Scott. 1989. Energy-sparing adaptations in human pregnancy assessed by whole-body calorimetry. British Journal of Nutrition 62(1): 5-22.
Prisco F., D. Iafusco, A. Franzese, N. Sulli and F. Barbetti. 2000. MODY 2 presenting as neonatal hyperglycaemia: a need to reshape the definition of “neonatal diabetes”? Diabetologia 43(10): 1331-1332.
Prysak M., R. P. Lorenz and A. Kisly. 1995. Pregnancy outcome in nulliparous women 35 years and older. Obstetrics and Gynecology 85(1): 65-70.
Reddy U. M., C. W. Ko and M. Willinger. 2006. Maternal age and the risk of stillbirth throughout pregnancy in the United States. American Journal of Obstetrics and Gynecology 195(3): 764-770.
Reed M. M., J. M. Westfall, C. Bublitz, C. Battaglia and A. Fickenscher. 2005. Birth outcomes in Colorado’s undocumented immigrant population. BMC Public Health 5: 100.
Retnakaran R., A. J. Hanley, N. Raif, P. W. Connelly, M. Sermer and B. Zinman. 2004. Reduced adiponectin concentration in women with gestational diabetes: a potential factor in progression to type 2 diabetes. Diabetes Care 27(3): 799-800.
Robinson T. N. 1999. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. Journal of the American Medical Association 282(16): 1561-1567.
Robson E. 1978. The Genetics of Birth Weight. In Human Growth, Volume 1 Principles and Prenatal Growth. F. Falkner and J. Tanner. London: Baillière Tindall; pp. 285-297.
Rumbaut R. G. and J. R. Weeks. 1996. Unraveling a public health enigma: why do immigrants experience superior perinatal health outcomes? Research in the Sociology of Health Care 13: 335-388.
Rush D. 1974. Examination of the relationship between birthweight, cigarette smoking during pregnancy and maternal weight gain. Journal of Obstetrics and Gynaecology of the British Commonwealth 81(10): 746-752.
Rush D. 1981. Nutritional services during pregnancy and birthweight: a retrospective matched pair analysis. Canadian Medical Association Journal 125(6): 567-576.
Rush D., D. G. Horvitz, W. B. Seaver, J. Leighton, N. L. Sloan, S. S. Johnson, R. A. Kulka, J. W. Devore, M. Holt, J. T. Lynch and et al. 1988. The National WIC Evaluation: evaluation of the Special Supplemental Food Program for Women, Infants, and Children. IV. Study methodology and sample characteristics in the longitudinal study of pregnant women, the study of children, and the food expenditures study. American Journal of Clinical Nutrition 48(2 Suppl): 429-438.
Safyer S. M. and L. Richmond. 1995. Pregnancy behind bars. Seminars in Perinatology 19(4): 314-322.
Santry H. P., D. L. Gillen and D. S. Lauderdale. 2005. Trends in bariatric surgical procedures. Journal of the American Medical Association 294(15): 1909-1917.
Sapolsky R. M.1995. Social subordinance as a marker of hypercortisolism. Some unexpected subtleties. Annals of the New York Academy of Sciences 771: 626-639.
Schaffer D. M., E. M. Velie, G. M. Shaw and K. P. Todoroff. 1998. Energy and nutrient intakes and health practices of Latinas and white non-Latinas in the 3 months before pregnancy. Journal of the American Dietetic Association 98(8): 876-884.
Scholl T. O. and M. L. Hediger. 1993. A review of the epidemiology of nutrition and adolescent pregnancy: maternal growth during pregnancy and its effect on the fetus. Journal of the American College of Nutrition 12(2): 101-107.
Scholl T. O., R. W. Salmon, L. K. Miller, P. Vasilenko, 3rd, C. H. Furey and M. Christine. 1988. Weight gain during adolescent pregnancy. Associated maternal characteristics and effects on birth weight. Journal of Adolescent Health Care 9(4): 286-290.
Scholl T. O., M. L. Hediger, I. G. Ances, D. H. Belsky and R. W. Salmon. 1990. Weight gain during pregnancy in adolescence: predictive ability of early weight gain. Obstetrics and Gynecology 75(6): 948-953.
Scholl T. O., M. L. Hediger, J. I. Schall, C. S. Khoo and R. L. Fischer. 1994. Maternal growth during pregnancy and the competition for nutrients. American Journal of Clinical Nutrition 60(2): 183-188.
Scribner R. and J. H. Dwyer. 1989. Acculturation and low birthweight among Latinos in the Hispanic HANES. American Journal of Public Health 79(9): 1263-1267.
Secker-Walker R. H. and P. M. Vacek. 2003. Relationships between cigarette smoking during pregnancy, gestational age, maternal weight gain, and infant birthweight. Addictive Behaviors 28(1): 55-66.
Seckl J. R. 1998. Physiologic programming of the fetus. Clinics in Perinatology 25(4): 939-962, vii.
Siega-Riz A. M. and C. J. Hobel. 1997. Predictors of poor maternal weight gain from baseline anthropometric, psychosocial, and demographic information in a Hispanic population. Journal of the American Dietetic Association 97(11): 1264-1268.
Siega-Riz A. M., K. R. Evenson and N. Dole. 2004. Pregnancy-related weight gain—a link to obesity? Nutrition Reviews 62(7 Pt 2): S105-S111.
Sinclair K. D., R. G. Lea, W. D. Rees and L. E. Young. 2007. The developmental origins of health and disease: current theories and epigenetic mechanisms. Society of Reproduction and Fertility Supplement 64: 425-443.
Singh G. K. and S. M. Yu. 1996. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. American Journal of Public Health 86(6): 837-843.
Skull A. J., G. H. Slater, J. E. Duncombe and G. A. Fielding. 2004. Laparoscopic adjustable banding in pregnancy: safety, patient tolerance and effect on obesity-related pregnancy outcomes. Obesity Surgery 14(2): 230-235.
Smith L. M., L. L. LaGasse, C. Derauf, P. Grant, R. Shah, A. Arria, M. Huestis, W. Haning, A. Strauss, S. Della Grotta, J. Liu and B. M. Lester. 2006. The infant development, environment, and lifestyle study: effects of prenatal methamphetamine exposure, polydrug exposure, and poverty on intrauterine growth. Pediatrics 118(3): 1149-1156.
Sollid C. P., K. Wisborg, J. Hjort and N. J. Secher. 2004. Eating disorder that was diagnosed before pregnancy and pregnancy outcome. American Journal of Obstetrics and Gynecology 190(1): 206-210.
Sternfeld B., C. P. Quesenberry, Jr., B. Eskenazi and L. A. Newman. 1995. Exercise during pregnancy and pregnancy outcome. Medicine and Science in Sports and Exercise 27(5): 634-640.
Stevenson L. 1997. Exercise in pregnancy. Part 1: Update on pathophysiology. Canadian Family Physician 43: 97-104.
Stevens-Simon C. and E. R. McAnarney. 1992. Determinants of weight gain in pregnant adolescents. Journal of the American Dietetic Association 92(11): 1348-1351.
Stevens-Simon C., E. R. McAnarney and K. J. Roghmann. 1993a. Adolescent gestational weight gain and birth weight. Pediatrics 92(6): 805-809.
Stevens-Simon C., I. Nakashima and D. Andrews. 1993b. Weight gain attitudes among pregnant adolescents. Journal of Adolescent Health 14(5): 369-372.
Stotland N. E., J. S. Haas, P. Brawarsky, R. A. Jackson, E. Fuentes-Afflick and G. J. Escobar. 2005. Body mass index, provider advice, and target gestational weight gain. Obstetrics and Gynecology 105(3): 633-638.
Suitor C. W. 1997. Maternal Weight Gain: A Report of an Expert Work Group. Arlington, VA: National Center for Education in Maternal and Child Health.
Swinburn B. and G. Egger. 2002. Preventive strategies against weight gain and obesity. Obesity Reviews 3(4): 289-301.
Swinburn B. A., B. L. Nyomba, M. F. Saad, F. Zurlo, I. Raz, W. C. Knowler, S. Lillioja, C. Bogardus and E. Ravussin. 1991. Insulin resistance associated with lower rates of weight gain in Pima Indians. Journal of Clinical Investigation 88(1): 168-173.
Tok E. C., D. Ertunc, O. Bilgin, E. M. Erdal, M. Kaplanoglu and S. Dilek. 2006. PPAR-gamma2 Pro12Ala polymorphism is associated with weight gain in women with gestational diabetes mellitus. European Journal of Obstetrics, Gynecology, and Reproductive Biology 129(1): 25-30.
Townsend M. S., J. Peerson, B. Love, C. Achterberg and S. P. Murphy. 2001. Food insecurity is positively related to overweight in women. Journal of Nutrition 131(6): 1738-1745.
Tsai P. J., S. C. Ho, L. P. Tsai, Y. H. Lee, S. P. Hsu, S. P. Yang, C. H. Chu and C. H. Yu. 2004. Lack of relationship between beta3-adrenergic receptor gene polymorphism and gestational diabetes mellitus in a Taiwanese population. Metabolism 53(9): 1136-1139.
Ventura S. J. 1994. Recent trends in teenage childbearing in the United States. Statistical Bulletin/Metropolitan Insurance Companies 75(4): 10-17.
Ventura S. J. and S. M. Taffel. 1985. Childbearing characteristics of U.S.- and foreign-born Hispanic mothers. Public Health Reports 100(6): 647-652.
Vicennati V. and R. Pasquali. 2000. Abnormalities of the hypothalamic-pituitary-adrenal axis in nondepressed women with abdominal obesity and relations with insulin resistance: evidence for a central and a peripheral alteration. Journal of Clinical Endocrinology and Metabolism 85(11): 4093-4098.
Vilming B. and B. I. Nesheim. 2000. Hyperemesis gravidarum in a contemporary population in Oslo. Acta Obstetricia et Gynecologica Scandinavica 79(8): 640-643.
Vlietinck R., R. Derom, M. C. Neale, H. Maes, H. van Loon, C. Derom and M. Thiery. 1989. Genetic and environmental variation in the birth weight of twins. Behavior Genetics 19(1): 151-161.
Voigt M., S. Straube, P. Schmidt, S. Pildner von Steinburg and K. T. Schneider. 2007. [Standard values for the weight gain in pregnancy according to maternal height and weight]. Zeitschrift fur Geburtshilfe und Neonatologie 211(5): 191-203.
Wagner C. L., L. D. Katikaneni, T. H. Cox and R. M. Ryan. 1998. The impact of prenatal drug exposure on the neonate. Obstetrics and Gynecology Clinics of North America 25(1): 169-194.
Walker L. O. and M. Kim. 2002. Psychosocial thriving during late pregnancy: relationship to ethnicity, gestational weight gain, and birth weight. Journal of Obstetric, Gynecologic, and Neonatal Nursing 31(3): 263-274.
Waterland R. A. and R. L. Jirtle. 2003. Transposable elements: targets for early nutritional effects on epigenetic gene regulation. Molecular and Cellular Biology 23(15): 5293-5300.
Waterland R. A., M. Travisano, K. G. Tahiliani, M. T. Rached and S. Mirza. 2008. Methyl donor supplementation prevents transgenerational amplification of obesity. International Journal of Obesity (London) 32(9): 1373-1379.
Webb J. B., A. M. Siega-Riz and N. Dole. 2009. Psychosocial determinants of adequacy of gestational weight gain. Obesity (Silver Spring) 17(2): 300-309.
Weedon M. N., T. M. Frayling, B. Shields, B. Knight, T. Turner, B. S. Metcalf, L. Voss, T. J. Wilkin, A. McCarthy, Y. Ben-Shlomo, G. Davey Smith, S. Ring, R. Jones, J. Golding, L. Byberg, V. Mann, T. Axelsson, A. C. Syvanen, D. Leon and A. T. Hattersley. 2005. Genetic regulation of birth weight and fasting glucose by a common polymorphism in the islet cell promoter of the glucokinase gene. Diabetes 54(2): 576-581.
Weissman A., E. Siegler, R. Neiger, P. Jakobi and E. Z. Zimmer. 1989. The influence of increased seismic activity on pregnancy outcome. European Journal of Obstetrics, Gynecology, and Reproductive Biology 31(3): 233-236.
Wells C. S., R. Schwalberg, G. Noonan and V. Gabor. 2006. Factors influencing inadequate and excessive weight gain in pregnancy: Colorado, 2000-2002. Maternal and Child Health Journal 10(1): 55-62.
Whitfield J. B., S. A. Treloar, G. Zhu and N. G. Martin. 2001. Genetic and non-genetic factors affecting birth-weight and adult body mass index. Twin Research 4(5): 365-370.
Wilde P. E. and J. N. Peterman. 2006. Individual weight change is associated with household food security status. Journal of Nutrition 136(5): 1395-1400.
Williams M. A., C. Qiu, M. Muy-Rivera, S. Vadachkoria, T. Song and D. A. Luthy. 2004. Plasma adiponectin concentrations in early pregnancy and subsequent risk of gestational diabetes mellitus. Journal of Clinical Endocrinology and Metabolism 89(5): 2306-2311.
Winzer C., O. Wagner, A. Festa, B. Schneider, M. Roden, D. Bancher-Todesca, G. Pacini, T. Funahashi and A. Kautzky-Willer. 2004. Plasma adiponectin, insulin sensitivity, and subclinical inflammation in women with prior gestational diabetes mellitus. Diabetes Care 27(7): 1721-1727.
Wisner K., D. Sit and S. Reynolds. 2007. Psychiatric Disorders. In Obstetrics Normal and Problems Pregnancies 5th Ed. S. Gabbe, J. Niebyl and J. Simpson. Philadelphia, PA: Churchill Livingstone; pp. 1249-1279.
Wolff C. B., M. Portis and H. Wolff. 1993. Birth weight and smoking practices during pregnancy among Mexican-American women. Health Care for Women International 14(3): 271-279.
Wolff M. S., S. Engel, G. Berkowitz, S. Teitelbaum, J. Siskind, D. B. Barr and J. Wetmur. 2007. Prenatal pesticide and PCB exposures and birth outcomes. Pediatric Research 61(2): 243-250.
Yanagisawa K., N. Iwasaki, M. Sanaka, S. Minei, M. Kanamori, Y. Omori and Y. Iwamoto. 1999. Polymorphism of the beta3-adrenergic receptor gene and weight gain in pregnant diabetic women. Diabetes Research and Clinical Practice 44(1): 41-47.
Websites:






























































