6
Consequences of Gestational Weight Gain for the Child
The emphasis of the report Nutrition During Pregnancy (IOM, 1990) was on the short-term consequences of gestational weight gain (GWG). Not only was there a lack of data on long-term outcomes, but also the research community was only just beginning to understand the importance of the intrauterine environment for long-term child health. Since then, the literature on the topic has expanded, and more information is now available on neonatal as well as long-term consequences of both inadequate and excessive GWG during pregnancy. The discussions in this chapter review the current evidence and strive to quantify, wherever possible, potential causal relationships between GWG and childhood outcomes.
Only by knowing the magnitude of causal relationships can one say with certainty that recommending a certain amount of GWG will result in altered frequency of adverse child health outcomes. Observational studies are often susceptible to mixing effects of confounding factors with the predictor of real interest, in this case GWG. Although reverse causality is less of a problem in cohort than in cross-sectional studies, confounding remains a concern in any observational study. It is possible that associations of GWG with outcomes do not result from GWG itself, but rather to underlying factors that influence both weight gain and the outcomes (e.g., maternal diet composition or physical activity level). In particular, it is important to determine whether these relationships are independent of prepregnancy body mass index (BMI) or if they differ by prepregnancy BMI. Only with large, well-designed, and carefully controlled randomized studies can causal relationships be inferred with a high degree of confidence. Limited experi-
mental data from randomized controlled trials in humans, however, impedes efforts to determine how much of any observed association is causal. In the following discussions, inferences regarding causality were made using the best data available in consideration of plausible biologic mechanisms, susceptibility to confounding and other aspects of the study methodology, and patterns of results.
GENERAL CONCEPTS
Causal Concepts
When considering potential causal relationships between GWG and the various child outcomes reviewed, the committee relied on the same conceptual model that it utilized when evaluating the determinants of GWG (see Figure 6-1). This model fits well with two paradigms that offer useful conceptual frameworks for considering long-term effects on the offspring. The first—the “life course approach to chronic disease”—invokes two axes (Kuh and Ben-Shlomo, 2004): time, with temporal factors acting in the pre-conceptional through the prenatal period, into infancy, childhood, and beyond to determine risk of chronic disease; and hierarchy, with hierarchical
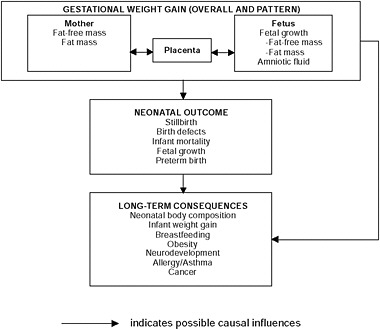
FIGURE 6-1 Schematic summary of neonatal, infant, and child consequences of GWG.
factors ranging from the social/built/natural environment (macro) through behavior, physiology, and genetics (micro) (see Chapter 4) and interacting with each other over the life course, with different determinants being more or less important at different life stages. The other paradigm—the “developmental origins of health and disease” paradigm—focuses primarily on the prenatal and early postnatal periods, because they are the periods of most rapid somatic growth and organ development (Gillman, 2005; Sinclair et al., 2007; Hanson and Gluckman, 2008). Both of these frameworks invoke the concept of programming, which refers to perturbations or events that occur at early, plastic, and perhaps critical phases of development and can have long-lasting, sometimes irreversible, health consequences. The period of plasticity may vary for different organs and systems (Gluckman and Hanson, 2006a, 2006b). The model used by the committee predicts that adult risk factors can only partially modify the trajectories of health and disease patterns established in earlier life (Barker et al., 2002; Ben-Shlomo and Kuh, 2002; McMillen and Robinson, 2005; Sullivan et al., 2008).
Potential Mechanisms Linking Gestational Weight Gain to Long-Term Offspring Health
The existence of plausible biological mechanisms is one criterion for establishing causal relationships between GWG and child health outcomes based on observational data. The following discussion focuses primarily on potential mechanisms linking GWG to offspring obesity and its consequences. Gestational weight gain is clearly about weight, so it is appropriate to address weight-related outcomes. Also most of the emerging evidence on long-term outcomes is based on these endpoints. The epidemiologic evidence for effects of GWG on other important child health outcomes are addressed later this chapter.
Developmental Programming
Developmental programming, including the possible role of epigenetics, as a potential determinant of GWG, is discussed in Chapter 4. In this chapter, the role of developmental programming as a mechanism for some of the effects of GWG on postnatal outcomes is discussed. Many animal models have demonstrated that altering the environment in utero can have lifelong consequences. Perturbations of the maternal diet during pregnancy (typically by severe energy or protein restriction; administration of hormones such as glucocorticoids; mechanical means, such as ligation of the uterine artery; or induction of anemia or hypoxia) have postnatal consequences on a number of metabolic and behavioral traits. Effects are inducible in rodents and other mammals, including non-human primates. Inasmuch as humans
differ from other animal species in duration of pregnancy, placentation, and other important factors, the importance of the findings from animal studies lies not in the specific interventions but rather in the general principle that altering the supply of nutrients, hormones, and oxygen to the growing embryo and fetus or exposing them to stressors and toxicants can have long-term effects. Much of this animal research has focused on obesity-related outcomes such as adiposity, fat distribution, sarcopenia, insulin sensitivity, glucose intolerance, and blood pressure. These are related to the leading causes of morbidity—and ultimately, mortality—in the United States. The ways in which GWG could influence obesity-related child health outcomes through developmental programming is discussed below (in Childhood Obesity and Its Consequences).
Until recently, most of the research in animal models concentrated on the long-term effects of interventions that cause offspring to be born small, typically small-for-gestational age (SGA), rather than early. Such work has been a good companion to a series of epidemiologic observations made within the past two decades that lower birth weight, apparently resulting from both reduced fetal growth and reduced length of gestation, is associated with higher risks of central obesity, insulin resistance, the metabolic syndrome, type 2 diabetes, hypertension, and coronary heart disease later in life. These associations are potentiated by rapid weight gain in childhood (Bhargava et al., 2004; Barker et al., 2005).
It is important to note, however, that in recent years researchers have recognized that higher birth weight is also associated with later obesity and its consequences. Greater GWG is associated with increased weight at birth (reviewed in the Fetal Growth section of this chapter) based on either the absolute amount of GWG and indicators of excessive gain (based on total GWG relative to the recommendations for gain within a given prepregnancy BMI category). Excessive GWG appears to be rising over time (see Chapter 2), highlighting questions about the long-term adverse effects of higher weight gains in pregnancy. Animal experiments that involve “over-nutrition” of the mother during pregnancy are discussed briefly below.
In addition, it is critical to recognize that effects of GWG, or indeed any factor that alters the in utero environment, may have long-term effects on the offspring without any alterations of fetal growth or length of gestation. Thus the most important epidemiologic evidence for long-term effects of GWG does not depend on birth weight, gestational age, or birth weight for gestational age as exposures or outcomes, but rather provides data on the direct associations of GWG with various health outcomes in the offspring. With this in mind, the committee considered “fetal growth” outcomes, including SGA and large-for-gestational age (LGA), and preterm birth as short-term outcomes. These measures have demonstrable and substantial associations with neonatal morbidity and mortality. Other short-term out-
comes include stillbirth and birth defects. In contrast, neonatal body composition is included in the discussion of long-term outcomes because of the hypothesis (still unproven, however) that relative amounts of adiposity and lean mass—and their physiologic consequences—in fetal and neonatal life are important in setting long-term cardio-metabolic trajectories.
It also bears noting that this report focuses primarily on GWG, rather than prepregnancy BMI. Nevertheless, because the two factors are closely linked, one must account for confounding and effect modification by BMI in addressing offspring effects of GWG. Also it is possible that factors in infancy or childhood (e.g., growth in stature, adiposity, and infant feeding) could mediate effects of GWG on long-term child health.
Childhood Obesity and Its Consequences
The following discussion focuses primarily on mechanisms linking GWG to childhood obesity and its consequences, although similar mechanisms likely underlie associations of GWG with fetal growth. One issue that hampers inferences regarding fetal growth is that fetal growth is usually characterized by (gestational-age-specific) weight at birth, with less consideration of trajectory from the time of conception to delivery of weight, body length, or body composition (see Chapters 3 and 4 for a review of existing studies that address these issues). In contrast to the prenatal period, serial measurements of length/height and weight are common during childhood but data on body composition are relatively scarce.
Insulin resistance and glucose intolerance during pregnancy may mediate effects of GWG on long-term child outcomes. Weight gain in pregnancy is partly a gain in adiposity, which is accompanied by a state of relative insulin resistance starting in mid-pregnancy, among other metabolic alterations (Reece et al., 1994; Williams, 2003; Catalano et al., 2006; King, 2006; Hwang et al., 2007) (also see Chapter 3). This is an adaptive response, as it allows more efficient transfer of fuels across the placenta to the growing fetus (King, 2006). In overweight and obese pregnant women, these changes are magnified; insulin resistance is more severe than in normal weight women, substantially raising the risk of impaired glucose tolerance and frank gestational diabetes mellitus.
This increased risk of impaired glucose tolerance has consequences for the fetus since glucose freely crosses the placenta; specifically, in pregnant women who have hyperglycemia, the fetus also experiences hyperglycemia. In a hypothesized sequence that Freinkel et al. (1986) termed “fuel-mediated teratogenesis,” fetal hyperglycemia causes fetal hyperinsulinemia, which in turn causes increased adiposity in the fetus. This increase is manifest as larger size at birth, which translates into higher rates of LGA and lower rates of SGA newborns (see discussion below and in Chapter 3).
Presumably through developmental programming mechanisms, increased fetal adiposity also results in increased adiposity in the growing child. Other fuels besides glucose may also be involved. For example, increased fetal production of anabolic hormones and growth factors, in combination with the increased levels of glucose, lipids, and amino acids that are typical of GDM, can cause fetal macrosomia (birth weight > 4,500 g) and increase the risk for neonatal complications (Catalano et al., 2003). Crowther et al. (2005) and Pirc et al. (2007) showed that diet and insulin therapy along with blood glucose monitoring in pregnant women with mild GDM could lower plasma insulin and leptin (but not glucose) concentrations in cord blood, decreasing the risk of macrosomia by more than 50 percent (Crowther et al., 2005).
This same impaired physiologic milieu may also increase the risk for long-term complications, particularly obesity and its metabolic sequelae. Observational studies suggest that this may be the case. For example, among 5- to 7-year-old children in two American health plans, Hillier et al. (2007) showed that risk of high weight for age was lower among those whose mothers had been treated for GDM than those who had not been treated; the weight status of the “treated” offspring was similar to those whose mothers had normal glucose tolerance. However, long-term child follow-up studies and relevant randomized trials are necessary to conclusively determine if treatment of GDM or impaired glucose intolerance during pregnancy can reduce adiposity and related physiology.
Most of the evidence in support of the Freinkel hypothesis comes from animal experiments, such as those of van Assche and colleagues (1979), and more recently Plagemann and colleagues (1998). By pharmacologically induced GDM in rats, both groups of researchers observed fetal hyperglycemia and hyperinsulinemia, as hypothesized, as well as changes in the hypothalamus that give rise to hyperphagia, overweight, and impaired glucose tolerance in maturing offspring. Another way to induce offspring metabolic derangement in rats is through overfeeding the pregnant dam. For example, Samuelsson et al. (2008) reported that maternal diet-induced obesity resulted in increased adult adiposity and evidence of cardiovascular and metabolic dysfunction in the offspring (which was not present in the offspring of lean dams). Earlier work by Dorner et al. (1988) and Diaz and Taylor (1998) showed that a period of overfeeding or GDM in the pregnant dam during a developmentally sensitive period in gestation not only could change the metabolic phenotype of the immediate offspring, but also that the induced metabolic phenotype persisted for two succeeding generations. In their review of animal studies, Aerts and Van Assche (2003) demonstrate that these intergenerational physiologic effects are maternally transmitted, most likely through epigenetic processes. Seemingly paradoxically, in ani-
mal experiments it is also possible to produce offspring that have insulin resistance, features of the metabolic syndrome, and diabetes, including GDM, by reducing energy or macronutrient intake of the mother during pregnancy. This situation can also result in intergenerational amplification of obesity and its consequences. For example, in rats, Benyshek et al. (2006) were able to alter glucose metabolism in the grand-offspring by restricting protein during pregnancy and lactation.
In summary, animal experiments show that offspring obesity and related metabolic sequelae can be induced experimentally, either through pharmacological induction of GDM or through either over- or underfeeding pregnant dams as well as through mechanical means like uterine artery ligation. Epigenetic modifications likely explain many of these phenomena (Simmons, 2007). A human counterpart to the animal experimental work is epidemiologic studies showing that higher birth weight is related to later obesity and type 2 diabetes while lower birth weight is associated with central obesity, the metabolic syndrome, and indeed, type 2 diabetes as well (Gillman, 2005). In other words, a U-shape relationship exists between birth weight and obesity-related health outcomes.
The extent to which these observations on metabolic dysfunction and offspring obesity have relevance for GWG guidelines is still unclear. Few animal studies directly assess the influence of GWG on short- or long-term offspring outcomes. Animal experimentalists typically do not measure weight gain during pregnancy, and it is not clear whether appropriate animal models exist to study GWG and offspring obesity-related outcomes. Neither is it clear that models of either diet-induced obesity or GDM are instructive for assessing effects of GWG.
Likewise, human population studies that rely on birth weight or its components, duration of gestation, and size at birth as predictors of later outcomes (e.g., Hofman et al., 2004; Hovi et al., 2007) also do not directly assess GWG. Further, intervention studies to treat GDM do not in themselves provide evidence for making recommendations for appropriate GWG. Only randomized trials that alter weight gain during pregnancy can address that goal directly. In a randomized controlled trial of reduced weight gain among obese pregnant women, Wolff and colleagues (2008) reported that reduced weight gain led to reduced insulin and leptin concentrations but that glucose values were hardly altered. Mean weight gain in the intervention group was 6.6 kg (± 5.5 kg) vs. 13.3 kg (± 7.5 kg) in the control group a mean difference of 6.7 kg (95% CI: 2.6-10.8, p = 0.002). Although the study was small, with only 50 participants, the results nonetheless raise the possibility that moderating GWG may reduce the risk of GDM and, in turn, childhood obesity, but larger and longer-term studies are needed to address this question directly.
EFFECTS ON NEONATAL MORBIDITY AND MORTALITY
There is a substantial literature on prepregnancy BMI and neonatal morbidity and mortality; maternal prepregnancy BMI is strongly associated with infant mortality and a number of other clinically important outcomes, including stillbirth and preterm birth (Figure 6-2). The literature on GWG in relation to these outcomes remains more limited, with the exception of its influence on fetal growth (Cedergren, 2006; Kiel et al., 2007).
The following discussion summarizes the committee’s evaluation of evidence on associations between GWG and a range of neonatal morbidity and mortality outcomes. Given that GWG, which is lower on average for heavier women, differs in relation to prepregnancy BMI, studies that examine GWG without stratifying by prepregnancy BMI are subject
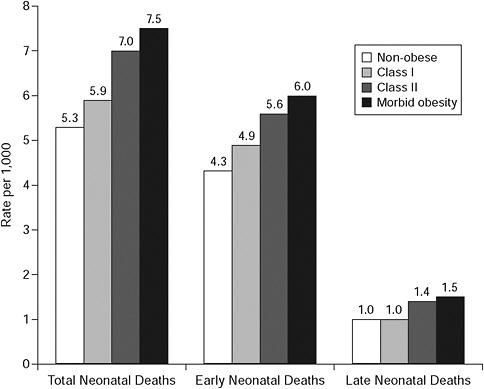
FIGURE 6-2 Rate of neonatal, early, and late neonatal death by obesity subclass.
SOURCE: Salihu et al., 2008. Obesity and extreme obesity: new insights into the black-white disparity in neonatal mortality. Obstetrics and Gynecology 111(6): 1410-1416. Reprinted with permission.
to confounding. These component relationships (prepregnancy BMI and GWG; and prepregnancy BMI and health outcome) are sufficiently strong that studies of GWG and neonatal outcomes that fail to account for pre-pregnancy BMI are of limited value in addressing the independent effects of GWG.
Stillbirth
Inadequate and excessive GWG have the potential to affect fetal viability in later pregnancy, specifically risk of stillbirth (defined as pregnancy loss after 20 weeks’ gestation). Naeye (1979) and NCHS (1986) showed that women with both low prepregnancy BMI and low GWG tended to have elevated risk of fetal or perinatal mortality (a combination of stillbirth and neonatal mortality) and that women with both elevated prepregnancy BMI and excessive GWG experienced increased risk of the same adverse outcomes.
Many studies on the potential association between GWG and stillbirths have been limited by confounding factors. For example, an analysis from the California Child Health and Development Studies of the School of Public Health, University of California, Berkeley (Tavris and Read, 1982) found a strong inverse association between total GWG and fetal death, but the association was found to be an artifact of using cumulative weight gain as the predictor; so it reflected the fact that duration of gestation for stillbirths was notably shorter than gestational duration of live births, not that lower GWG predicted fetal death. When the analysis was restricted to births of greater then 35 weeks’ gestation, there was no association.
A case-control study of stillbirths in Sweden reported a strong positive association between prepregnancy BMI and stillbirth, with odds ratios approaching 3.0 for obese women, but the authors reported no effect of GWG measured in either early or late pregnancy among term births (Stephansson et al., 2001). Although the large size of the study (649 cases and 690 controls) and the authors’ consideration of an array of covariates are notable, the results for total GWG were not presented in the publication.
In summary, the research on GWG and stillbirth remains quite limited in quantity and quality. In addition to considering prepregnancy BMI, there is a need to avoid the error of comparing total GWG in pregnancies resulting in stillbirths with those resulting in live births because of the time in pregnancy when stillbirth is likely to occur. Although early studies suggested adverse effects of low GWG among women with low prepregnancy BMI and also of high GWG among women with elevated prepregnancy BMI, more detailed studies have not been done to corroborate or refute this pattern. Recent, better studies largely do not support an association between GWG and stillbirth.
Birth Defects
The authoring committee of the IOM (1990) report did not identify any studies on the association between GWG and birth defects. Since the etiologic period for congenital defects is so early in pregnancy, GWG is not likely to be causally relevant. Although the literature on prepregnancy BMI and congenital defects now suggests an increased risk of birth defects with increasing BMI (Watkins et al., 2003; Anderson et al., 2005; Villamor et al., 2008), only one study has directly addressed GWG in relation to birth defects. Shaw (2001) reported that infants born to mothers who gained less than either 5 or 10 kg during pregnancy were at increased risk of neural tube defects. An additional report indicated that dieting to lose weight during pregnancy was associated with an increased risk of neural tube defects (Carmichael et al., 2003). It seems more likely that an association of GWG and birth defects would result from reverse causality (abnormal fetal development affecting weight gain) rather than a direct causal effect of GWG on risk of birth defects.
Infant Mortality
Infant mortality is obviously of great clinical and public health importance and is often used as a summary indicator of a population’s reproductive health status. In fact, concern with fetal growth and preterm birth as health outcomes stems largely from the known relationships between those outcomes and infant mortality (as well as morbidity); studies that directly address mortality can be helpful in interpreting the patterns seen with those other, intermediate outcomes such as preterm birth or growth restriction. However, very limited research assessing GWG and infant mortality exists. In the IOM (1990) report, only one study on perinatal mortality was examined (NCHS, 1986). Since then, there has been only one additional study. As part of the National Maternal and Infant Health Survey (NMIHS), Chen et al. (2009) examined maternal prepregnancy BMI and GWG among 4,265 infant deaths and 7,293 controls. Among underweight and normal-weight women, low GWG was associated with a marked increase in infant mortality, with relative risks on the order of 3-4 compared to those with the highest GWG; the effects were more modest among overweight and obese women, with both lower and higher GWG associated with about two-fold increases in the risk of infant mortality. In all cases, the patterns were stronger for neonatal deaths (in the first 30 days of life) than for post-neonatal deaths (those occurring after 1 month but before the completion of 1 year). In the lowest weight gain group, the relative risks for neonatal death were 3.6 among underweight women, 3.1 among normal weight women, 2.0 among overweight women, and 1.2 among obese women,
showing a diminishing effect of low GWG with increasing BMI. In the highest GWG group, the relative risks for neonatal mortality for underweight, normal weight, overweight, and obese women were 1.0, 1.2, 1.4, and 1.8, respectively, showing the exact opposite tendency—excessive GWG was more strongly associated with neonatal death with increasing prepregnancy BMI. Maternal age at delivery did not affect neonatal mortality. After adjusting for gestational age at delivery, no association was found between teenage pregnancy and neonatal mortality. The same general pattern was seen for postneonatal deaths but was less pronounced (see Table 6-1).
More studies of infant mortality are needed, but the evidence from Chen et al. (2009) warrants serious consideration not only because of the
TABLE 6-1 Maternal Prepregnancy BMI and Gestational Weight Gain of Infant Deaths and Controls (1988 National Maternal and Infant Health
|
Survey [NMIHS]) Maternal Prepregnancy BMI (kg/m2) |
Total Weight Gain During Pregnancya (kg) |
Neonatal Death ORb (95% CI) |
Postneonatal Death ORb (95% CI) |
Infant Death ORb (95% CI) |
|
< 18.5 |
< 6.0 |
3.55 (1.92-6.54) |
2.96 (1.42-6.15) |
3.26 (1.86-5.72) |
|
|
6.0-11.6 |
1.35 (0.88-2.06) |
1.34 (0.83-2.14) |
1.34 (0.93-1.92) |
|
|
12.0-17.6c |
1.00 |
1.00 |
1.00 |
|
|
≥ 18.0 |
0.99 (0.63-1.54) |
0.55 (0.32-0.95) |
0.79 (0.53-1.17) |
|
18.5-24.9 |
< 6.0 |
3.07 (2.45-3.85) |
1.96 (1.51-2.55) |
2.58 (2.12-3.14) |
|
|
6.0-11.6 |
1.41 (1.19-1.68) |
1.12 (0.92-1.36) |
1.29 (1.11-1.49) |
|
|
12.0-17.6c |
1.00 |
1.00 |
1.00 |
|
|
≥ 18.0 |
1.15 (0.96-1.37) |
0.94 (0.77-1.15) |
1.06 (0.91-1.23) |
|
25-29.9 |
< 6.0 |
1.98 (1.34-2.92) |
0.81 (0.51-1.29) |
1.42 (1.02-1.99) |
|
|
6.0-11.6 |
1.20 (0.85-1.68) |
0.64 (0.43-0.95) |
0.94 (0.71-1.25) |
|
|
12.0-17.6c |
1.00 |
1.00 |
1.00 |
|
|
≥ 18.0 |
1.41 (1.00-2.00) |
0.87 (0.58-1.31) |
1.16 (0.87-1.56) |
|
≥ 30 |
< 6.0 |
1.19 (0.69-2.06) |
0.81 (0.40-1.62) |
1.04 (0.64-1.70) |
|
|
6.0-11.6 |
0.67 (0.39-1.17) |
0.91 (0.47-1.78) |
0.78 (0.48-1.26) |
|
|
12.0-17.6c |
1.00 |
1.00 |
1.00 |
|
|
≥ 18.0 |
1.78 (0.96-3.33) |
1.29 (0.58-2.84) |
1.61 (0.92-2.81) |
|
NOTE: Midpoint and range values for outcomes (neonatal death, postnatal death, infant death) are derived using a separate reference group for each BMI category. aWeight gain during pregnancy projected to 40 weeks’ gestation. bAdjusted for race, maternal age at pregnancy, maternal education, maternal smoking during pregnancy, child’s sex, live birth order, and plurality. cReferent group for comparisons within BMI stratum. SOURCE: Modified from Chen et al., 2009. |
||||
importance of the outcome but also because of the implications for the more voluminous literature on fetal growth and preterm birth. Although this study did not link GWG to those intermediate outcomes or intermediate outcomes to mortality, the strength of the patterns and their parallels with studies of fetal growth add credibility to the presumption that a causal chain from GWG to adverse birth outcomes to death is operative. Based on a limited volume of research, but one well-done study, the committee considered the evidence for a link to infant mortality to be moderate.
Fetal Growth
The relationship of GWG to fetal growth was considered in some detail in the IOM (1990) report. The association was deemed worthy of lengthy consideration because, as noted in IOM (1990) and by others, smaller size at birth is associated with increased fetal and infant mortality, cerebral palsy, hypoglycemia, hypocalcemia, polycythemia and birth asphyxia, persistent deficits in size, and persistent deficits in neurocognitive performance (Pryor et al., 1995; Goldenberg et al., 1998). Adverse health outcomes associated with small size at birth tend to follow a dose-response relationship with elevated relative risks at the lowest weights. Large size causes delivery complications, including shoulder dystocia and other forms of birth injury, as well as cesarean delivery, maternal death, and fistulae (IOM, 1990). Birth weight is a function of both duration of gestation and rate of fetal growth, so that studies using birth weight alone as a health outcome are less informative than those that distinguish between these processes. In order to isolate fetal growth rate from duration of gestation, studies often use SGA and LGA instead of birth weight as measures of fetal growth rather than birth weight. SGA and LGA are indicators that compare an infant’s weight to the distribution of birth weight of all infants born in the same week of gestation. Most commonly, infants in the lowest and highest 10th percentiles of birth weight for gestational age are classified as SGA and LGA, respectively, although some researchers use the more extreme values of the 5th percentile or two standard deviations or more below or above the mean. Some researchers use percentile cutoff points that are specific to gender, race/ethnicity, and/or parity in addition to week of gestation, although there is some controversy about the use of racial/ethnic-specific norms, in particular because their biological meaning is in doubt. Even though black infants in the United States have a markedly different weight distribution than non-black infants (of varying race/ethnicity), with deviation from group-specific norms being very informative for predicting mortality, separate group-specific norms could be interpreted as acceptance of differences in birth outcome by race/ethnicity as absolute. Such differences are not
immutable, however, because health disparities are strongly influenced by social and behavioral factors.
At the time of the IOM (1990) report, the evidence for an effect of GWG on fetal growth was viewed as “quite convincing.” Increased GWG was related to increased birth weight, and the report noted that the strength of that relationship varied as a function of prepregnancy BMI. The lower the prepregnancy BMI, the stronger the association between increased GWG and increased birth weight. Among obese women, the association between increased GWG and increased birth weight was questionable. The patterns of influence of GWG on fetal growth were evident both for mean birth weight and for the tails of the birth-weight-by-gestational-age distribution, which are usually referred to as intrauterine growth restriction (IUGR) and macrosomia, respectively. IUGR is generally applied to births that are designated as having a lower weight than would have been attained had the pregnancy been a “normal” one. Obviously the definition of “normal” or “expected” is problematic because it is not known what would have happened had conditions been different—only what did happen. Thus results may not be comparable across studies when different indices are used. Macrosomia is variably defined as > 90th percentile of birth weight for gestational age or > 4,000 g.
In addition, observational studies have consistently linked inadequate GWG, especially in underweight and normal weight women, with increased risk for SGA, and excessive weight gain, especially in overweight and obese women, with increased risk of LGA and its sequelae. A series of early randomized trials of dietary supplements, carefully reviewed by Susser (1991), provide evidence causally linking improved nutrition to GWG and to fetal growth but only for women who were near starvation. The evidence provides very little support for the argument that increased energy or protein intake during pregnancy enhances fetal growth in general; for other groups of pregnant women (i.e., women who were not near starvation), there was no benefit and some indication of possible harm from ingesting supplements with high protein concentrations. In contrast, results from a Cochrane systematic review suggested that supplementation consistently reduced risk of SGA, although this does not necessarily mean that such benefits were mediated by GWG (Kramer and Kakuma, 2003). Another set of recent randomized trials have focused directly on the impact of limiting GWG to determine whether this results in short-term metabolic effects or improved clinical outcomes. Polley et al. (2002) randomized normal weight and overweight women (~30 in each class and arm of the trial) to assess the impact of a multifaceted program designed to maintain GWG within recommended guidelines. The intervention yielded benefits in preventing excessive GWG only among normal weight women. Women whose GWG was moderated
had infants that weighed 93 g less on average than controls. Fewer of the treated number developed GDM or had cesarean deliveries.
In summary, the issue of whether the association between GWG and fetal growth is causal cannot be answered with certainty based on the available evidence. Observational data provide replicated indications of a strong association between lower GWG and increased risk of SGA, especially in underweight and normal weight women, and between higher GWG and increased risk of LGA, particularly among overweight and obese women. There are several possible explanations for these reported associations between GWG and fetal growth: GWG is causally related to fetal growth, both GWG and fetal growth are independently affected by maternal diet and/or physical activity, or both GWG and fetal growth have shared genetic or other intrinsic biological determinants. If either of the two non-causal explanations is correct, then manipulating GWG will not affect fetal growth directly. However, if the same behavioral changes that produce a more optimal GWG also happen to result in a more optimal fetal growth, then fetal growth would be affected. The available randomized trials are either only indirectly applicable (because they are from less-relevant populations and time periods or involved only a particular form of supplement, e.g., protein) or are too small to provide strong evidence of causality. In the absence of clear evidence on the causal pathway and in an effort to ensure that the newly recommended guidelines are protective of the health of the fetus and infant, the committee presumed that the relationship between GWG and fetal growth was causal.
AHRQ Review of Studies on the Association Between GWG and Birth Weight
The Agency for Healthcare Research and Quality (AHRQ) evidence-based review on outcomes related to GWG (Viswanathan et al., 2008) identified 25 studies of variable quality that examined GWG and birth weight as a continuous measure. Every one of those studies demonstrated an association between higher GWG and higher infant birth weight. Although there was substantial variability in magnitude of effect across studies, in general birth weight differed by about 300 g between the lowest and highest GWG categories. Among the stronger studies, the AHRQ review found that for each 1 kg increase in GWG, birth weight rose 16.7-22.6 g. The fewer studies that considered weight gain by trimester tended to show a smaller increase in birth weight per unit increase in GWG in the third than in the first or second trimesters.
A smaller but still sizable number of studies (13) examined the relationship of GWG to risk of low birth weight (LBW, defined as < 2,500 g). These studies showed that risk of LBW diminishes as GWG increases, particularly
as total gain exceeds 25-30 pounds. Although the magnitude of association varied substantially across studies, in general the highest GWG category had roughly half the risk of an LBW infant compared to the lowest GWG category. At the other end of the birth weight spectrum, 12 studies considered infant macrosomia (defined as birth weight > 4,000 or > 4,500 g). Recognizing the variability in definitions of macrosomia and GWG categories, the committee found that the studies showed a consistent trend for increased risk of macrosomia with increasing GWG. Relative risks were 2-3 for macrosomia in the highest compared to the lowest GWG category.
These results consistently indicate that the relationship of GWG to birth weight applies across the full range of weights and is not limited to the low or high end of the distribution. However, because birth weight is a combination of fetal growth and duration of gestation, studies that separate these two components are more informative.
AHRQ Studies on the Association Between GWG and Weight for Gestational Age
The AHRQ review (Viswanathan et al., 2008) identified 15 studies of SGA that did not stratify by prepregnancy BMI; the studies showed a consistent pattern of diminishing risk of SGA with increasing GWG. It is difficult to provide quantitative estimates of the magnitude of this effect given variable study methods and results, but as for LBW, relative risks were on the order of 2-3 across extreme GWG categories. The six studies that stratified by prepregnancy BMI similarly found that lower GWG was associated with increased risk of SGA births. While methods and results were again variable, the studies did not strongly suggest that prepregnancy BMI modified the relationship between lower GWG and SGA, in contrast to the interpretation in the IOM (1990) report.
In the 10 studies in which GWG and LGA were considered, there was reasonably consistent support for a positive association. For each 1 kg increment in GWG, the relative risk of LGA increased by approximately a factor of 1.1, and comparing the highest to lowest categories of GWG yielded relative risks on the order of 2. The studies that stratified by pre-pregnancy BMI did not show notable differences in the GWG-LGA association across BMI categories, with only a modest tendency towards a stronger association between higher GWG and LGA among women with lower prepregnancy BMI.
Other Studies on the Association Between GWG and Fetal Growth
Subsequent to the AHRQ review (Viswanathan et al., 2008), four additional studies addressing GWG and birth weight had been published.
First, Lof et al. (2008), whose focus was on the role of physical activity in relation to GWG and pregnancy outcome, noted that GWG during weeks 12-33 (unadjusted for prepregnancy BMI) was modestly correlated with increased birth weight (r = 0.13; p = 0.05) and more strongly correlated with birth weight than GWG during either weeks 12-25 or 25-33 alone. Second, Segal et al. (2008) found similar results in a study of obesity and family history of diabetes in relation to pregnancy outcome; controlling for prepregnancy BMI, they reported an adjusted correlation coefficient of 0.19 (p = 0.09) between weight gain before the oral glucose tolerance test and birth weight.
Third, utilizing data from the Danish National Birth Cohort, Nohr et al. (2008) conducted the most informative and detailed analysis to date on the independent effects of prepregnancy BMI and GWG. Analyzing data from over 60,000 births, the authors evaluated the relationship between GWG and both SGA and LGA, as well as the interaction between prepregnancy BMI and GWG in relation to birth weight. They reported statistically significant but generally modest indications of an interaction between prepregnancy BMI and GWG, with the exception of a stronger association of low GWG with SGA among underweight women.
Subsequent analyses of this data (information contributed to the committee in consultation with Nohr) revealed that the relative risk of SGA associated with lower (< 10 kg) versus medium (10-15 kg) GWG among underweight women was 2.1, while it was 1.7 for normal weight women, 1.6 for overweight women, and 1.3 for obese women. The increased risk of LGA associated with very high GWG (≥ 20 kg) vs. medium GWG (10-15 kg) was 3.7 for underweight women, 2.6 for normal weight women, 2.0 for overweight women, and 1.8 for obese women, again suggesting that the effect of lower GWG on risk of SGA is dampened with increasing prepregnancy BMI. This large, carefully done study is important not only because it quantifies the magnitude of effect of GWG on birth weight, but also because it is consistent with the large body of previous evidence demonstrating an overall shift of fewer SGA and more LGA births (and higher mean birth weight) with increasing GWG (see Appendix G, Part I).
Fourth, utilizing data from the Pregnancy Risk Assessment Monitoring System (PRAMS), Dietz et al. (2009) estimated associations between GWG and delivery of an SGA infant using three definitions of SGA: > two standard deviations below the mean birth weight for gestational age, a customized measure, < 10th percentile of expected birth weight for gestational age, and < 10th percentile of birth weight for gestational age using a population-based reference (i.e., information derived from about 104,980 singleton term births in 2000-2005 from 29 states participating in PRAMS). The magnitudes of association between GWG and SGA are striking, with more than a 10-fold gradient in risk from lowest to highest weight gain
categories for underweight women, and a 3- to 4-fold gradient in risk for women in the other BMI categories (see Table 6-2). Risk of LGA births or births > 4,500 g yielded clear and similar findings; with increasing weight gain, there was a markedly increased risk of LGA births, present among all BMI groups, but most pronounced on a relative scale among the women with the lowest BMI.
Summary of the Evidence on an Association Between GWG and Fetal Growth
In summary, the evidence that GWG is related to birth weight for gestational age based on observational studies is quite strong and the magnitude of that association is large, with relative risks of SGA with low GWG on the order of 2-3. It appears that the entire birth weight distribution is shifted upward with increased GWG, reducing the risk of SGA and increasing the risk of LGA as the mean birth weight rises. The evidence that this pattern is enhanced among women with low prepregnancy BMI is moderately strong as well.
It is not yet clear, however, whether the associations between GWG and birth weight for gestational age is impacted by factors other than prepregnancy BMI. The IOM (1990) report suggested consideration of a different relationship between GWG and fetal growth among young mothers, but studies conducted since then have failed to provide any additional support for the differential effects by maternal age group. Research on the potentially differential effects of GWG on fetal growth according to ethnic-
TABLE 6-2 Adjusted Odds Ratios for Association of Total GWG with SGA Stratified by Prepregnancy BMI
ity, smoking status, or other maternal attributes has been sparse, and the few studies summarized in the AHRQ review inconsistent. In addition to prepregnancy BMI, the only other factor that appears to impact the association between GWG and birth weight for gestational age is time during pregnancy that GWG occurs, with modest support for a stronger effect of GWG that occurs during the first or second trimester than during the third trimester GWG (Viswanathan et al., 2008).
Preterm Birth
Preterm birth (< 37 weeks’ completed gestation) is a critical indicator of developmental maturity, with the risk of death and morbidity a direct function of the degree of prematurity. Specifically, births occurring at the margins, that is during 33-36 weeks’ gestation, are at modestly increased risk of health problems; births that occur < 33 weeks’ gestation are rarer events but at much greater risk. Morbidity risks associated with preterm birth include acute respiratory, central nervous system, and gastrointestinal disorders, long-term deficits in neurobehavioral development (IOM, 2007), and possibly adverse cardiometabolic outcomes (Hofman et al., 2004; Hovi et al., 2007). Although an early delivery may be the only alternative to intrauterine death in some instances, regardless of whether it is caused by natural processes or induced by clinical intervention (an increasingly common “cause” of preterm birth), the high and growing frequency of preterm birth in the United States makes this a critical endpoint to consider in relation to GWG.
At the time of the IOM (1990) report, the volume and quality of literature on preterm birth was quite limited. Several studies suggested that low GWG was associated with increased risk of preterm birth, but much of that may have resulted from the simple error of failing to recognize that the shortened period of pregnancy (i.e., preterm birth) limits the duration of time over which weight can be gained. Comparing total GWG between preterm and term births is meaningless since preterm birth, by definition, involves a shorter period of gestation, thereby truncating the opportunity for weight gain compared to term births.
Data generated on behalf of this committee (information contributed to the committee in consultation with: Herring [see Appendix G, Part II] and Stein [see Appendix G, Part III]) provided some of the first information on GWG and preterm birth to consider prepregnancy BMI, which is predictive of both preterm birth (higher risk with lower BMI) and GWG (higher GWG with lower BMI). The results of that effort suggested a modest U-shaped relationship between rate of net weight gain (the only proper measure to compare pregnancies of varying duration) and risk of preterm birth.
The AHRQ review (Viswanathan et al., 2008) included 12 studies on the relationship between rate of GWG and preterm birth. The studies show
a consistently increased risk of preterm birth among women in both the lowest and highest GWG categories. It is difficult to summarize the quantitative impact because the studies used varying definitions of high and low rates of weight gain and different analytic methods to characterize the relationship with preterm birth. In those studies that provided relative risks comparing higher and lower GWG to the middle range, the relative risks were on the order of 1.5-2.5 for both the higher and lower GWG groups, with greater consistency for the influence of lower GWG on preterm birth.
Effect modification by prepregnancy BMI (Siega-Riz et al., 1996; Spinillo et al., 1998; Schieve et al., 1999; Dietz et al., 2006; Nohr et al., 2007) was examined in 5 of these 12 studies. The authors of these studies consistently reported a stronger effect of a lower rate of GWG on preterm delivery among underweight women. As prepregnancy BMI increased, the magnitude of increased risk associated with a lower rate of GWG diminished. There was some evidence that the increased risk of preterm birth associated with a higher rate of GWG was greater with increasing BMI, so that the optimal GWG shifted downward with higher prepregnancy BMI. Four of the five studies that applied the IOM (1990) guidelines to define adequacy of GWG reported increased risk of preterm birth associated with inadequate GWG among underweight and normal weight women.
Several studies considered the clinical presentation of preterm birth (Siega-Riz et al., 1996; Spinillo et al., 1998; Nohr et al., 2007), and several studies considered severity of prematurity (Dietz et al., 2006; Stotland et al., 2006) in their analyses. Though limited in quantity, the results of these studies do not provide a clear suggestion that the association between GWG and preterm birth differs by clinical presentation or severity. More recently, Rudra et al. (2008) considered preterm birth subtypes in relation to prepregnancy BMI and GWG. They reported that greater GWG during gestational weeks 18-22 was weakly associated with lower risk of spontaneous preterm birth and higher risk of medically indicated preterm birth, with some variation in these patterns in relation to prepregnancy BMI.
Biological Plausibility
Although the pathogenesis of spontaneous preterm delivery has not been clearly elucidated, researchers have postulated at least five possible primary pathogenic mechanisms (IOM, 2007):
-
Activation of the maternal or fetal hypothalamic-pituitary-adrenal (HPA) axis.
-
Amniochorionic-decidual or systemic inflammation.
-
Uteroplacental thrombosis and intrauterine vascular lesions.
-
Pathologic distention of the myometrium.
-
Cervical insufficiency.
The committee found no studies that directly link GWG to activation of the maternal or fetal HPA axis. However, several animal studies have linked periconceptional undernutrition to accelerated maturation of fetal HPA axis resulting in preterm delivery (Bloomfield et al., 2003, 2004; Kumarasamy et al., 2005).
Again, the committee also found no studies directly linking GWG to amniochorionic-decidual or systemic inflammation. However, it is plausible that maternal undernutrition may increase the risk of preterm delivery by suppressing immune functions or increasing oxidative stress. Macro- or micronutrient deficiencies are known to adversely affect maternal immune functions. For example, iron-deficiency anemia can alter the proliferation of T- and B-cells, reduce the killing activity of phagocytes and neutrophils, and lower bactericidal and natural killer cell activity, thereby increasing maternal susceptibility to infections (Allen, 2001). Furthermore, protein and/or micronutrient deficiencies may impair cellular antioxidant capacities because proteins provide the amino acids needed for synthesis of antioxidant defense enzymes, such as glutathione and albumin (reactive oxygen species scavengers); and many micronutrients themselves are antioxidants. Increases in reactive oxygen species, such as oxidized low-density lipoprotein and F2-isoprostanes (lipid peroxidation products), may contribute to cellular toxicity, inflammation, vasoconstriction, platelet aggregation, vascular apoptosis, and endothelial cell dysfunction (Luo et al., 2006), which may also activate the pathway to preterm delivery involving uteroplacental thrombosis and intrauterine vascular lesions.
Summary of the Evidence on an Association Between GWG and Preterm Birth
In summary, there is strong evidence for a U-shaped association between lower GWG and preterm birth among normal weight and under-weight women, and moderate evidence for an association of higher GWG and preterm birth. The magnitude of the association is fairly strong, with relative risks on the order of two, but difficult to summarize because of variability in the definitions of higher and lower rates of weight gain. There is no empirical basis for suggesting modifiers of this relationship other than prepregnancy BMI, for which the data are clear in showing that associations of low GWG with preterm birth are stronger among underweight women.
The committee was unable to infer a causal relationship between GWG and preterm delivery based on available evidence. Although there are intriguing data linking macro- and/or micronutrient deficiencies to accelerated maturation of fetal HPA axis and altered immune functions and/or increased oxidative stress, suggesting that a direct causal relationship is biologically plausibility, important questions regarding timing, threshold, content, and interactions remain unanswered. These uncertainties about a
direct causal relationship between GWG and preterm delivery guided the committee’s approach to decision analysis in Chapter 7, which weighed the trade-offs of GWG with and without taking into account preterm delivery as an outcome.
LONG-TERM CONSEQUENCES
The IOM (1990) report recommendations for GWG focused largely on avoiding inadequate GWG and the short-term consequences of low fetal growth and prematurity (see Chapter 1). Since that time, the emergence of epidemic obesity in the U.S. population has raised the possibility that excessive weight gain may also be harmful. A small number of recent studies have addressed the relationship between GWG and adiposity at birth, markers of childhood obesity and cardiometabolic sequelae of childhood obesity. The following discussion summarizes the committee’s review of the evidence for associations between GWG and neonatal body composition, infant weight gain, breastfeeding initiation, and other long-term outcomes.
Neonatal Body Composition
As previously explained (see Fetal Growth section in this chapter), GWG is directly associated with fetal growth as measured by birth weight for gestational age. For long-term adiposity-related outcomes, however, it is important to measure not only weight (and length) at birth but also body composition. As mentioned in the chapter introduction, it has been hypothesized that relative amounts of adiposity and lean mass in fetal and neonatal life are important in setting long-term cardio-metabolic trajectories. Catalano and colleagues performed a series of studies examining the relationships between various maternal characteristics and neonatal body composition as measured by total body electrical conductivity (a method no longer in use). One set of studies compared infants who were born at term to overweight/obese women (pregravid BMI > 25 kg/m2; n = 76) with those born to lean/average weight women (n = 144) (Sewell et al., 2006). As expected, weight gain was higher among lean/average (mean 15.2 kg) than overweight/obese (13.8 kg) women. Among the overweight/obese women, stepwise regression analyses that included pregravid weight as a covariate revealed that the higher the GWG, the more the newborn fat mass. The authors did not report a correlation among the lean women, presumably because the associated p-value exceeded 0.05. In another study, which combined data from diabetic and nondiabetic pregnant women (total n = 415), GWG was directly associated with both lean and fat mass at birth (Catalano and Ehrenberg, 2006). The latter results are consistent with those of Udal et al. (1978), who found a direct association between GWG and the sum of 8 neonatal skinfold measurements among 109 nondiabetic mothers
delivering term infants, an association that was independent of prepregnancy weight, gestational age, smoking, and family history of diabetes.
Although these findings raise the possibility that higher GWG may lead to long-lasting adiposity in the offspring, more definitive evidence would come from studies addressing the relationship between GWG and body composition from birth onwards in populations from developed countries.
Infant Weight Gain
Rapid weight gain during infancy is associated with obesity later in life (Baird et al., 2005; Monteiro and Victoria, 2005; Gillman, 2008). It is unclear whether this association is a greater issue among infants who are born SGA (Ong and Loos, 2006; Taveras et al., 2009). Because of this association, infant weight gain may serve as a surrogate, or intermediate marker, of later adiposity. However, although intermediate markers are often more feasibly obtained than ultimate health outcomes, they are rarely perfect surrogates and are sometimes misleading. As a result, one should view any associations of GWG with surrogate outcomes—even in randomized trials—with caution. Also, this line of reasoning would be strengthened by serial measures of body composition, not just weight (with or without length) from birth onward.
The committee identified only one study that addressed the relationship between GWG and infant weight gain, and even then it was not the primary goal of the study: Ong et al. (2000) conducted a prospective study of 848 term infants born in the United Kingdom who had weight measured at birth and at 2 and 5 years of age. The 30.7 percent of children who gained more than 0.67 weight standard deviations in the first 2 years of life had more adiposity at age 5 than the other children, but they also had been lighter, shorter, and thinner at birth; the mothers of these children were no more likely than the mothers of children who gained less weight to have had a higher prepregnancy BMI or to have gained more weight during pregnancy.
Breastfeeding Initiation and Maintenance
Breastfeeding Outcomes
Breastfeeding is an important outcome to study not only because it may be associated with reduced offspring obesity, and therefore may serve as an intermediate marker such as infant weight gain, but also because it predicts other health outcomes such as reduced otitis media, gastrointestinal illness, and better cognition. Although observational studies (see Chapter 5) have documented a relationship between excessive weight gain during pregnancy
and poor breastfeeding outcomes, the committee identified no studies that addressed the relationship between GWG and lactation-related offspring outcomes.
Long-Term Effects on Obesity
Despite the importance of this issue, high-quality studies associating GWG with obesity and obesity-related health outcomes in childhood are only just beginning to be published. The AHRQ review (Viswanathan et al., 2008) identified only one cohort study that examined childhood obesity in relation to GWG according to the IOM (1990) guidelines. Oken et al. (2007) analyzed data from Project Viva, a prospective study of predominantly non-low-income pregnant women and their children in Massachusetts (see Table 6-3). Among the sample of 1,044 mothers included in this analysis, 51 percent gained excessive, 35 percent adequate, and 14 percent inadequate weight during pregnancy. Compared with inadequate GWG and after controlling for key covariates, adequate and excessive gains were associated with odds ratios of 3.77 (95% CI: 1.38, 10.27) and 4.35 (1.69, 11.24), respectively, for obesity at 3 years of age (BMI > 95th percentile vs. < 50th percentile). In addition, by analyzing total weight gain in 5-kg increments, the authors found higher BMI z-scores, higher sums of triceps and subscapular skinfold thicknesses, and higher systolic blood pressure in children born to women who had higher total GWG.
The AHRQ review (Viswanathan et al., 2008) identified three other studies that assessed total GWG and childhood adiposity. Because one of these studies (Ong et al., 2000) also examined weight gain from birth to 2 years as an outcome, the committee included its results in the discussion above. In another study, (Sowan and Stember, 2000) in a fully adjusted model of adiposity outcomes through 14 months of age, each 5-pound increment in total weight gain was associated with an odds ratio of 0.8 for obesity (defined as BMI > 84th percentile within the study population) (n = 630). Inferences about an association between GWG and obesity from the Sowan and Stember (2000) study are uncertain, however, for several reasons. In a third study, Li et al. (2007) empirically derived three weight-gain trajectories through childhood and found that GWG was a predictor of the “early-onset” trajectory (which was defined as “children with an early-onset of overweight that persisted throughout childhood”); adjusting for maternal BMI and other factors, the authors found that total weight gain of at least 45 pounds (versus 25-35 pounds) was associated with a relative risk of 1.7 for being in the early-onset rather than in the normal trajectory class.
Since the publication of the AHRQ review (Viswanathan et al., 2008), three additional studies have shown positive associations between GWG and offspring obesity. First, Wrotniak et al. (2008) studied approximately
TABLE 6-3 Published Studies (N > 1,000) Relating Total GWG to Child Obesity
|
|
Moreira et al., 2007 |
Oken et al., 2007 |
Oken et al., 2008 |
Wrotniak et al., 2008 |
|
Age at Outcome (y) |
6-12 |
3 |
9-14 |
7 |
|
N |
4,845 |
1,044 |
11,994 |
10,226 |
|
Birth Years |
1990-1997 |
1999-2002 |
1982-1987 |
1959-1966 |
|
GWG Exposure |
< 9 kg 9-13.5 |
per 5 kg |
per 5 lb |
per 1 kg |
|
|
13.6-15.9 16+ |
A/E vs. I |
I/E vs. A |
I/E vs. A |
|
Child BMI Outcome |
OR for overweight (IOTF) |
OR for ≥ 95th vs. < 50th |
OR for ≥ 95th vs. < 85th |
OR for ≥ 95th vs. < 95th |
|
Outcome Prevalence |
~19.5% |
9.0% |
6.5% |
5.7% |
|
Overall Results |
1.0 (ref) |
1.66 (1.31-2.12) |
1.09 (1.06-1.13) |
1.03 (1.02, 1.05) |
|
|
1.12 (0.91-1.37) |
[1.44 (1.17-1.79) for BMI 95th vs. < 85th]a |
|
|
|
|
1.20 (0.90-1.60) |
|
|
|
|
|
1.27 (1.01-1.67) |
|
|
|
|
|
|
A 3.77 (1.38-10.3) |
I 0.91 (0.74-1.13) |
I 0.88 (0.68, 1.14) |
|
E 4.35 (1.69, 11.2) |
E 1.42 (1.19-1.70) |
E 1.48 (1.06, 2.06) |
||
|
Approximate OR per 5 kg (11 lb) |
1.14 (ninth root of 1.27 raised to the fifth power)b |
1.44 |
1.21 (1.09 raised to the power 2.2) |
1.16 (1.03 raised to the fifth power) |
10,000 7-year-old term-born offspring of participants in the 1950s-1960s Collaborative Perinatal Project (see Table 6-3). Not surprisingly, mean maternal BMI (21.9 kg/m2), total weight gain (9.5 kg), birth weight (3.23 kg), and the proportions of women with excessive gain (11 percent) and children with obesity (defined as BMI > 95th percentile—5.7 percent) were lower than in current cohorts. Both total weight gain and excessive weight gain were associated with child obesity. For example, compared with adequate gain, excessive gain was associated with an adjusted odds ratio of 1.48 (95% CI: 1.06, 2.06) for BMI ≥ 95th versus < 95th percentile). The association appeared stronger for women who entered pregnancy underweight (BMI < 19.8 kg/m2) than for heavier mothers.
Second, Moreira et al. (2007) found that total GWG was directly associated with childhood overweight as defined by the International Obesity Task Force standards (Cole et al., 2000) (see Table 6-3). Among overweight women, gains ≥ 16 kg were associated with an adjusted odds ratio for childhood overweight of 1.27 when compared with weight gains < 9 kg (95% CI: 1.01-1.61).
Third, among nearly 12,000 participants in the Growing Up Today Study, after adjusting for maternal BMI and other covariates, Oken et al. (2008) found a strong, nearly linear association between total GWG and obesity (BMI > 95th versus < 85th percentile) at 9-14 years of age (see Figure 6-3 and Table 6-3). Overall, each 5-pound increment in GWG was associated with an odds ratio of 1.09 (95% CI: 1.06-1.13) for obesity. Expressing GWG in terms of recommended weight-gain ranges (IOM, 1990), the authors found that in comparison with adequate weight gain, the odds ratio for excessive gain was 1.42 (95% CI: 1.19-1.70). Inadequate gain was not clearly associated with lower risk of obesity. The authors did not find that maternal BMI modified associations of GWG with adolescent obesity; although, if anything, the association was weaker among underweight mothers, in contrast to the findings of Wrotniak et al. (2008).
A handful of other studies have not demonstrated associations between GWG and offspring adiposity-related measures. Some of these were suggestive but small (Gale et al., 2007), while others were sufficiently large but either did not focus on GWG as a main study exposure or did not adequately control for confounders (Fisch et al., 1975; Maffeis, 1994; Whitaker, 2004).
Summary of the Evidence on an Association Between GWG and Childhood Obesity
In summary, the evidence to date is suggestive but not conclusive that GWG outside the ranges recommended by IOM (1990) is associated with higher offspring BMI. Evidence that the association is effected by maternal
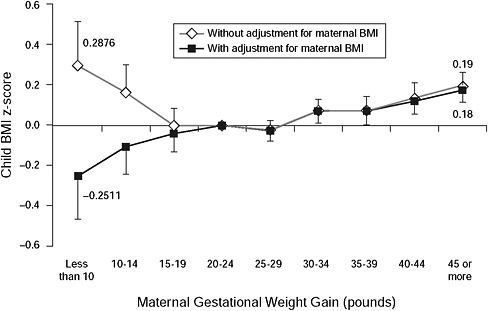
FIGURE 6-3 Associations of maternal gestational weight gain with child BMI z-score at ages 9-14 years, with and without adjustment for maternal prepregnancy BMI. All estimates are adjusted for maternal age, race/ethnicity, marital status, household income, paternal education, child sex, gestation length, age, and Tanner stage at outcome assessment.
SOURCE: Oken et al., 2008. Maternal gestational weight gain and offspring weight in adolescence. Obstetrics and Gynecology 112(5): 999-1006. Reprinted with permission.
BMI is scant, and there is no evidence on whether the timing of weight gain during pregnancy impacts offspring BMI. Most of the studies rely on BMI as the only outcome, in contrast to direct measures of adiposity and cardio-metabolic status, which would strengthen the evidence base. Only one study to date has reported on blood pressure as an outcome (Oken et al., 2007), although another recent report suggests that higher weight gain is associated with an increase in left ventricular mass from birth to 6 months (Geelhoed et al., 2008).
Nevertheless, as discussed in the chapter opening, even strong observational studies that have valid exposure and outcome measures, large sample sizes, and appropriate control for confounding cannot fully address the question of causality. Randomized controlled trials that are designed to modify GWG and include follow-up of the children would provide the most compelling evidence for or against intensive clinical or public health efforts to curb excessive weight gain.
Other Outcomes
The following discussion summarizes the committee’s evaluation of the evidence on a range of other, non-weight-related long-term offspring outcomes, including neurodevelopmental outcomes, allergies/asthma, and cancer.
Neurodevelopment
Alterations in fuel metabolism during pregnancy resulting from intended or unintended weight loss, fasting, or poorly controlled diabetes can cause ketonemia and/or ketonuria, which in turn can have consequences for the neurocognitive development of the infant (see Chapter 3). The committee reviewed the evidence for long-term neurodevelopmental consequences of ketonemia/ketonuria in pregnancy (see Appendix G). As a result of the association between lower GWG and SGA (see discussion in the Fetal Growth section of this chapter), one indirect way to evaluate the impact of GWG on neurodevelopment is by assessing associations of term and preterm SGA with neurodevelopmental outcomes.
Long-term neurodevelopment in term SGA The committee was able to identify only observational prospective studies and review articles evaluating long-term neurodevelopmental outcomes in term SGA infants. With the exception of one study conducted in China, all were conducted in industrialized nations including the United States (Goldenberg et al., 1996; Nelson et al., 1997). Of 18 studies identified, 6 examined neurodevelopmental outcomes during infancy/childhood (Watt and Strongman, 1985; Nelson et al., 1997; Sommerfelt et al., 2000; Hollo et al., 2002; Geva et al., 2006; Wiles et al., 2006), 9 during adolescence (Westwood et al., 1983; Paz et al., 1995, 2001; Pryor et al., 1995; Goldenberg et al., 1996; Strauss, 2000; O’Keefe et al., 2003; Indredavik et al., 2004; Peng et al., 2005; Kulseng et al., 2006) and 2 during adulthood (Viggedal et al., 2004; Wiles et al., 2005). Results have been mixed.
A study from a Finnish cohort found that SGA children performed worse at school than gestational age-matched controls at 10 years of age (Hollo et al., 2002). Another cohort of children in Norway found a slightly lower mean intelligence quotient (IQ) at 5 years of age associated with SGA; however, parental factors were more strongly related with IQ than SGA (Sommerfelt et al., 2000). Nelson et al. (1997) found that SGA was not associated with either the Bayley Mental Development Index (MDI) and Fagan Test of Infant Intelligence score at 1 year of age; in contrast, they found that SGA was associated with a lower Bayley Psychomotor Development Index (PDI) among black males but not among females or white male
and female infants. Watt and Strongman (1985) documented that SGA was inversely associated with MDI developmental scores at 4 months, whereas Goldenberg et al. (1996) found an inverse relationship between SGA and IQ at 5.5 years of age. Wiles et al. (2006) did not find a relationship between low birth weight and behavioral problems at 6.8 years of age.
Effect size analysis was assessed for cognitive outcome measures. Of the 18 studies reviewed, 12 reported cognitive scores by SGA status. Of these, 2 reported lower Bayley scores (Watt and Strongman, 1985; Nelson et al., 1997) and 10 reported lower IQ measures (Westwood et al., 1983; Paz et al., 1995, 2001; Pryor et al., 1995; Goldenberg et al., 1996; Sommerfelt et al., 2000; Hollo et al., 2002; Viggedal et al., 2004; Peng et al., 2005; Kulseng et al., 2006) associated with term-SGA status, although these differences were not always statistically significant. Among infants, the Bayley score difference associated with SGA ranged from 4-7 points (Watt and Strongman, 1985; Nelson et al., 1997). Among children (Goldenberg et al., 1996; Sommerfelt et al., 2000; Hollo et al., 2002), IQ differentials were 4-5 points. Among adolescents (Westwood et al., 1983; Paz et al., 1995, 2001; Pryor et al., 1995; Peng et al., 2005; Kulseng et al., 2006) the corresponding range was 2-12 points. The upper range limit was derived from a study conducted in China that did not control for socioeconomic and other potential confounding factors (Peng et al., 2005). The only study among adults that reported IQ documented a relatively large 19-point IQ differential (based on scores’ median instead of average) associated with term-SGA infants. However, it also failed to account for confounding factors (Viggedal et al., 2004). Overall, these 18 studies consistently reported small cognitive differentials associated with being born at term and SGA. The meaning of these small differentials is unclear, as in all studies average scores among individuals born SGA fell within the normal IQ range.
Associations between SGA and long-term neurodevelopmental outcomes among term newborns were inconsistent, especially among adolescents. Among studies that supported this association, major methodological shortcomings (which included substantial attrition, lack of standard definitions of SGA across studies, not properly accounting for key confounders [such as socioeconomic status and parental cognitive functioning, as well as asphyxia at birth], and lack of testing for effect modification by environmental factors) limit their interpretation. As a whole, the studies were not designed to identify the influence of SGA, independent of socioeconomic factors, on lower IQs. The committee’s evaluation of the evidence concurs with previous reviews (Grantham-McGregor, 1995; Goldenberg et al., 1998) that SGA is associated with minimal neurologic dysfunction (e.g., poor school performance) and is not associated with major handicaps, such as cerebral palsy, unless accompanied by asphyxia at birth.
Long-term neurodevelopment in preterm SGA In preterm SGA infants, the majority of longitudinal studies reviewed by the committee focused on extremely premature (Feldman and Eidelman, 2006; Kono et al., 2007; Paavonen et al., 2007; Leonard et al., 2008) or very low birth weight (VLBW) (Litt et al., 1995; Hack, 1998; Brandt et al., 2003; Kilbride et al., 2004; Litt et al., 2005; Feldman and Eidelman, 2006; Hille et al., 2007; Paavonen et al., 2007; Strang-Karlsson et al., 2008a, 2008b) infants. Among 14 studies in children, 11 found that SGA was associated with cognitive and/or neurodevelopment impairments, although this relationship may be modified by degree of postnatal catch-up growth and maternal-child interactions (Casey et al., 2006; Feldman and Eidelman, 2006). In general, the effect size was proportional to the severity of prematurity (Calame et al., 1983; Feldman and Eidelman, 2006; Kono et al., 2007). The two studies conducted among adolescents found an association of VLBW with IQ (Hille et al., 2007) and breathing-related sleep disorders (Paavonen et al., 2007). Among adults, VLBW was associated with emotional instability (Strang-Karlsson et al., 2008b) and SGA with lower head circumference among individuals who did not fully catch up in their head circumference growth during their first 12 months of life.
Effect size was again assessed for cognitive measures. Of 19 studies reviewed, 13 reported cognitive scores by SGA status; of these, 1 reported a lower Bayley score (Feldman and Eidelman, 2006) and 12 reported lower IQ measures (Escalona, 1982; Calame et al., 1983; Silva et al., 1984; Holwerda-Kuipers, 1987; Litt et al., 1995; McCarton et al., 1996; Hutton et al., 1997; Kilbride et al., 2004; Litt et al., 2005; Casey et al., 2006; Hille et al., 2007; Kono et al., 2007) associated with preterm SGA status, although these differences were not always statistically significant. Among 2-year-old children, one study found an 8-point difference in the Bayley Mental Development Index score (Feldman and Eidelman, 2006). In contrast, a study conducted among 3.5-year-old children found no differences in IQ scores associated with preterm SGA (Escalona, 1982). Among the rest of studies with children (Calame et al., 1983; Silva et al., 1984; Holwerda-Kuipers, 1987; Litt et al., 1995; McCarton et al., 1996; Hutton et al., 1997; Kilbride et al., 2004; Litt et al., 2005; Casey et al., 2006; Kono et al., 2007), IQ differentials were 2-11 points. The only study among adults that reported IQ, documented a 2-point differential associated with VLBW. Overall, the cognitive differentials appear to be relatively stronger among individuals born SGA preterm (mean ± std. dev: 6.5 ± 3.8 IQ points, n = 11 studies) than among those born SGA term (5.3 ± 3.0, n = 9 studies IQ points). However, as with term SGA, the meaning of these still relatively small differentials is unclear because in the vast majority of studies the average scores for individuals born preterm SGA fell within the normal IQ range.
The overwhelming majority of studies reviewed support an association between preterm SGA and lower neurodevelopment in the longer term. Consistent with the studies on term SGA, many of the studies on preterm SGA did not properly control for key perinatal (e.g., asphyxia), socioeconomic, parental, and home environment confounders (e.g., maternal-child interactions). In addition, although some studies included term births as reference groups (Calame et al., 1983; Silva et al., 1984; Holwerda-Kuipers, 1987; Litt et al., 1995, 2005; Hack et al., 1998; Brandt et al., 2003; Kilbride et al., 2004; Paavonen et al., 2007; Leonard et al., 2008; Strang-Karlsson et al., 2008a, 2008b), others used preterm subgroups as comparison groups (McCarton et al., 1996; Hutton et al., 1997; Casey et al., 2006; Kono et al., 2007). Because of these study design limitations, the effect size or the proportion of the variance in neurodevelopmental outcomes that can be attributed to being born premature per se or to the combination of prematurity and SGA still needs to be determined.
In summary, as was the case with infant mortality, one must link GWG to being born preterm or small- or large-for-gestational age and, from there, to neurodevelopmental outcomes. This sequence is biologically plausible and it is possible that it is causal, but the evidence to establish causality is not available.
Apgar score The Apgar score (see Glossary in Appendix A) assessments are usually conducted 1 and 5 minutes after birth, and scores can range from 0 to 10. However, Apgar scores in term infants, even at 5 minutes, have important limitations, as they are not adequate predictors of longer term morbidity and mortality and do not correlate well with neurological outcomes (ACOG, 2006) although very low scores (0-3) associated with low birth weight do predict neonatal mortality. The AHRQ review (Viswanthan et al., 2008) identified five studies examining the influence of GWG on a newborn’s Apgar score (Stevens-Simon and McAnarney, 1992; Nixon et al., 1998; Cedergren et al., 2006, Stotland et al., 2006; Wataba et al., 2006). Taken together, these studies provide only modest evidence that excessive GWG is associated with low Apgar score, and one study suggested that low GWG in nulliparous women also predicts low Apgar score.
Childhood cognition No published studies directly examine the link between GWG and neurocognitive development in infants and children. However, as discussed in Chapter 3, weight loss or failure to gain during pregnancy due to dietary caloric insufficiency may possibly induce maternal hormonal and metabolic responses, which may, in turn, have subsequent consequences for the intellectual development of the child. Because of the obligatory weight gain in maternal tissues (uterus, breast, blood) and the fetal-placental unit, a weight gain less than ~7.5-8.5 kg would likely result
in mobilization of maternal adipose tissue and possibly lean body mass. Although the gestational metabolic milieu or offspring outcomes of pregnant women who experience weight loss have not yet been addressed in the scientific literature, there have been several studies on associations between ketonemia or ketonuria, which can occur among pregnant women subjected to short-term fasting (see Chapter 3), and cognition in offspring. Some, but not all, of these studies have found an association between biomarkers of maternal metabolic fuel alterations and child intellectual development (Stehbens et al., 1977; Rizzo et al., 1991; Silverman et al., 1991). In contrast, Persson and Gentz (1984) and Naeye and Chez (1981) did not find any association of maternal acetonuria, weight loss, or low GWG with either psychomotor development or IQ in children (see Chapter 3).
In summary, although no studies specifically address the impact of very low GWG or weight loss on child intellectual development, some evidence suggests that biomarkers of short-term negative energy balance during pregnancy may be related to the child’s intellectual development. These associations may be limited to women with diabetes during pregnancy.
Allergy/Asthma
Inasmuch as GWG has been associated with risk of preterm birth, it is plausible that GWG may also be a risk factor for childhood asthma since prematurity itself is a risk factor for childhood asthma—often as a result of suboptimal lung function and resulting neonatal respiratory morbidity (Dombkowski et al., 2008). For example, in a case-control study of 262 African American 4- to 9-year-old children receiving care at a hospital-based clinic, Oliveti et al. (1996) used maternal GWG (as determined from the mother’s self-report of prepregnancy weight and maternal weight measured at the time of delivery) and child medical records to examine pre- and perinatal risk factors for asthma (as defined either by physician diagnosis or wheezing or coughing that required asthma medication).
Multivariate logistic regression analyses showed that odds of prevalent asthma were 3.42 (95% CI: 1.72-6.79) times higher among women who gained less (versus more) than 20 total pounds during pregnancy. However, the authors neither adjusted for prepregnancy BMI nor examined the BMI-GWG interaction. Among children with asthma, 24.6 percent were born preterm compared to 13.7 percent of controls.
Another way that GWG could lead to the propensity for asthma in offspring is through alteration of the developing fetal immune system. For example, Willwerth et al. (2006) found that both inadequate and excessive GWG were associated with increased cord blood mononuclear cell proliferative responses to stimulation (OR = 2.3 and 2.6, respectively), compared
to controls with adequate GWG. In that study, maternal smoking (OR = 18) was the major determinant of the response.
Cancer
Whether associations exist between GWG, birth weight, and risk for childhood cancers is not clear; however, there are a few studies that have examined the possibility.
Childhood leukemia Two lines of evidence link GWG to cancer: First, a recent meta-analysis (Hjalgrim et al., 2003) estimated that the odds for acute lymphoblastic childhood leukemia (ALL) were higher (OR = 1.26, 95% CI: 1.17-1.37) for infants with birth weight over 4,000 g compared to those under 4,000 g. Although not statistically significant, results were of similar magnitude for acute myelogenous leukemia (AML). McLaughlin et al. (2006) examined the association between pregnancy outcomes and leukemia cases registered in the state of New York and diagnosed before 10 years of age. The authors obtained information on prepregnancy weight (BMI not generally available) and GWG from birth certificates. Using multivariate regression analyses, the researchers found that total GWG greater than 14 kg conferred an increased risk for ALL (OR = 1.31, 95% CI: 1.07, 1.60). Maternal prepregnancy weight did not affect the impact of GWG on ALL; nor was there any association between GWG and AML. The authors speculated that higher GWG could result in higher fetal exposure to insulin-like growth factor I (IGF-I), which in turn may increase the risk of childhood ALL. Based on these results and because of the established relationship between higher GWG and macrosomia (see discussion in Fetal Growth section in this chapter), it is plausible that GWG may be related to childhood leukemia.
Breast cancer Almost two decades ago, Trichopoulos (1990) hypothesized that breast cancer originates from alterations in the prenatal endocrine milieu, in particular higher estrogen levels. Although longitudinal studies needed for definitively testing this hypothesis have yet to be conducted, observational studies showing direct associations between birth weight and breast cancer provide some support for an association (Michels et al., 1996; Vatten et al., 2002; Ahlgren et al., 2007). Therefore, the committee deemed it of interest to examine determinants of hormone levels in the maternal-placental-fetal unit. In a sample of 270 white women from Boston, Lagiou et al. (2006) examined the association between GWG and maternal sex hormones at 16 and 27 weeks of gestation. After adjusting for prepregnancy BMI and other covariates the authors did not detect any associations between GWG and maternal estradiol, estriol, or prolactin
levels, providing some support to the estrogen hypothesis; however, higher GWG was associated with lower levels of maternal progesterone and of sex hormone-binding globulin (−0.7 percent [95% CI: −1.5, 0.0] at 16 weeks and −1.2 percent [95% CI: −2.0, −0.4] at 27 weeks, respectively, for every 1-kg increment in GWG.
In addition, one study directly addressed the association of GWG with incident breast cancer. Analyzing data from the Finnish Cancer Registry, Kinnunen et al. (2004) found that offspring of mothers in the upper tertile of GWG (> 15 kg) had a 1.62-fold higher breast cancer risk than mothers who gained within the recommended range (11-15 kg) after adjusting for parity; mother’s age at menarche, at first birth, and at index pregnancy; and prepregnancy BMI. Together these findings provide some support for the hypothesis that excessive weight gain in pregnancy could lead to elevated breast cancer risk in the offspring.
Attention deficit hyperactivity disorder Because the human brain develops rapidly during both gestation and the early postnatal period, it is possible that maternal body fat reserves and GWG can influence fetal central nervous pathways in a manner that ultimately results in long-term behavioral disorders such as attention deficit hyperactivity disorder (ADHD). Only one study was able to identify associations between either early pregnancy BMI or GWG and ADHD (Rodriguez et al., 2008). Within three cohorts of 7- to 12-year-old Scandinavian children, teachers used standard questionnaires to rate the children’s inattention and hyperactivity symptoms; about 8.5 percent of children were classified as having ADHD symptoms. A large majority of the mothers (86.4 percent) had a normal prepregnancy BMI and adequate GWG (mean gestational age = 39.6 ± 1.6 weeks, mean birth weight = 3.6 ± 0.5 kg). Multivariate linear regression analyses showed that among women with a high prepregnancy BMI, GWG (measured weekly and in 100-g increments) was associated with increased odds of child ADHD (OR = 1.24, 95% CI: 1.07-1.44). Among lean women, those who experienced weight loss during pregnancy also had higher odds of having a child that would later develop ADHD compared to their counterparts who did not lose weight during gestation (OR: 1.52, 95% CI: 1.07-2.15). The mechanisms for these effects are unknown, although the authors speculated on the possibility of neurotoxin transfer from maternal adipose tissue to the developing fetal brain.
CONCLUDING REMARKS
Assessing the impact of GWG on child outcomes requires both a short-and long-term outlook. Strong observational evidence links GWG directly with fetal growth, so that higher weight gain predicts LGA and lower
weight gain predicts SGA. Both LGA and SGA are themselves markers of neonatal morbidity. The literature on preterm birth is more ambiguous because of a less-extensive body of epidemiologic evidence, a nonlinear (U-shape) relationship between GWG and preterm birth that is modest in magnitude, and uncertainty about biologic mechanisms. Even when GWG is measured in a way that takes into account the shortened duration of pregnancy associated with GWG with preterm births, results are subject to some uncertainty. The U-shaped association of GWG with preterm birth is harder to interpret than the monotonic dose-response gradient with birth weight for gestational age, postpartum weight retention, and childhood obesity and may reflect distinct causal processes on the low and the high end of GWG.
Among the most important long-term child outcomes are obesity and its sequelae, chiefly cardio-metabolic consequences and neurodevelopmental disorders. Observational evidence is growing that GWG predicts childhood adiposity after adjusting for prepregnancy BMI and other key factors, although some older studies do not show this association. The evidence for neurodevelopmental outcomes is dependent on inferences from intermediate endpoints of fetal size and duration of gestation.
The need for randomized trials is especially important because, to date, there is no appropriate animal experimental model for GWG, thus making it difficult to meet one of the criteria—biological plausibility—that epidemiologists often use to support causal inference. Nevertheless, as reviewed in this chapter, pathways involving insulin resistance and fetal hyperglycemia may underlie associations of GWG with both fetal growth and subsequent obesity in the offspring. At the other end of the spectrum, reduced GWG is associated with lower fetal growth and preterm birth, which themselves are associated with later central obesity, insulin resistance, and metabolic syndrome. Very little current evidence, however, suggests that inadequate or low GWG predicts obesity-related outcomes in children.
FINDINGS AND RECOMMENDATIONS
Findings
-
Causal inferences relating GWG to childhood outcomes are tenuous as a result of the paucity of experimental studies.
-
Epidemiologic support for an association between gestational weight gain and stillbirth is weak; there are few methodologically sound studies.
-
Many epidemiologic studies are consistent in showing a linear, direct relationship between GWG and birth weight for gestational age. Thus, lower GWG predicts SGA, and higher GWG predicts
-
LGA. Despite a limited number of randomized controlled trials, biological plausibility from animal models is strong. Relative risks for GWG and SGA appear to be higher among women with lower prepregnancy BMI.
-
The evidence for a relationship between GWG and preterm birth, or between GWG and gestational age at birth is weaker than evidence for an association between GWG and fetal growth, and biological plausibility is weak. Most studies show associations between lower GWG and preterm birth among underweight, and to a lesser extent, normal weight women. Higher GWG among all BMI categories may also be associated with preterm birth. Evidence is insufficient on associations with spontaneous vs. induced preterm birth.
-
A small number of studies show that GWG is directly associated with fat mass in the newborn period. Insufficient evidence is available on associations between GWG and adiposity in infancy.
-
A small number of relatively large and recent epidemiologic studies show that higher GWG is associated with childhood obesity as measured by BMI. Although biological plausibility is strong, evidence is insufficient to address effect modification by maternal BMI. Only one study has examined blood pressure as an outcome (finding associations in the same direction as BMI), and none has evaluated fat mass or other cardio-metabolic consequences of adiposity.
-
Lower GWG may be associated with risk of childhood asthma, chiefly through complications of preterm birth, although evidence is limited.
-
Higher GWG may be associated with ALL, breast cancer, and ADHD, but the evidence is largely indirect and limited in quantity.
-
Concern exists that metabolic consequences of weight loss during pregnancy may be associated with poorer childhood neurodevelopmental outcomes. Data are limited but raise the possibility that ketonemia among diabetic women could lead to suboptimal neurologic development.
Recommendation for Research
Research Recommendation 6-1: The committee recommends that the National Institutes of Health and other relevant agencies should provide support to researchers to conduct observational and experimental studies to assess the impact of variation in GWG on a range of child outcomes, including duration of gestation and weight and body com-
position at birth, and neurodevelopment, obesity and related outcomes, and asthma later in childhood.
Areas for Additional Investigation
The committee identified the following areas for further investigation to support its research recommendations. The research community should conduct studies on the following topics:
-
Child outcomes related to GWG to provide support for causal inference. Randomized trials and a combination of observational epidemiology and animal models may be more attainable benchmarks to enhance certainty regarding causal links between GWG and infant outcomes.
-
Statistical models that follow sound theoretical frameworks and clearly distinguish among confounding, mediating, and moderating (effect modifying) variables. Statistical models based on path analysis such as structural equation modeling may be able to improve interpretation of complex data.
-
Preventing excessive weight gain with all of the attributes listed above for observational studies. Even relatively small studies that can evaluate intermediate endpoints, if not the clinically important outcomes, would make a significant contribution.
Furthermore, future research on GWG and child outcomes should:
-
not assume linear relationships between GWG and offspring obesity, but should look for U- or J-shaped associations as well;
-
determine whether the pattern of maternal weight gain affects short- or long-term child outcomes, e.g., whether weight gain earlier in pregnancy is more harmful than later gain; and
-
determine whether critical or sensitive periods of adiposity accretion exist in pregnant women and, if so, when weight gain is an adequate measure to capture those periods.
REFERENCES
ACOG (American College of Obstetricians and Gynecologists). 2006. ACOG Committee Opinion. Number 333, May 2006 (replaces Number 174, July 1996): The Apgar score. Obstetrics and Gynecology 107(5): 1209-1212.
Aerts L. and F. A. Van Assche. 2003. Intra-uterine transmission of disease. Placenta 24(10): 905-911.
Ahlgren M., J. Wohlfahrt, L. W. Olsen, T. I. Sorensen and M. Melbye. 2007. Birth weight and risk of cancer. Cancer 110(2): 412-419.
Allen L. H. 2001. Biological mechanisms that might underlie iron’s effects on fetal growth and preterm birth. Journal of Nutrition 131(2S-2): 581S-589S.
Anderson J. L., D. K. Waller, M. A. Canfield, G. M. Shaw, M. L. Watkins and M. M. Werler. 2005. Maternal obesity, gestational diabetes, and central nervous system birth defects. Epidemiology 16(1): 87-92.
Baird J., D. Fisher, P. Lucas, J. Kleijnen, H. Roberts and C. Law. 2005. Being big or growing fast: systematic review of size and growth in infancy and later obesity. British Medical Journal 331(7522): 929.
Barker D. J., J. G. Eriksson, T. Forsen and C. Osmond. 2002. Fetal origins of adult disease: strength of effects and biological basis. International Journal of Epidemiology 31(6): 1235-1239.
Barker D. J., C. Osmond, T. J. Forsen, E. Kajantie and J. G. Eriksson. 2005. Trajectories of growth among children who have coronary events as adults. New England Journal of Medicine 353(17): 1802-1809.
Ben-Shlomo Y. and D. Kuh. 2002. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology 31(2): 285-293.
Benyshek D. C., C. S. Johnston and J. F. Martin. 2006. Glucose metabolism is altered in the adequately-nourished grand-offspring (F3 generation) of rats malnourished during gestation and perinatal life. Diabetologia 49(5): 1117-1119.
Bhargava S. K., H. S. Sachdev, C. H. Fall, C. Osmond, R. Lakshmy, D. J. Barker, S. K. Biswas, S. Ramji, D. Prabhakaran and K. S. Reddy. 2004. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. New England Journal of Medicine 350(9): 865-875.
Bloomfield F. H., M. H. Oliver, P. Hawkins, M. Campbell, D. J. Phillips, P. D. Gluckman, J. R. Challis and J. E. Harding. 2003. A periconceptional nutritional origin for noninfectious preterm birth. Science 300(5619): 606.
Bloomfield F. H., M. H. Oliver, P. Hawkins, A. C. Holloway, M. Campbell, P. D. Gluckman, J. E. Harding and J. R. Challis. 2004. Periconceptional undernutrition in sheep accelerates maturation of the fetal hypothalamic-pituitary-adrenal axis in late gestation. Endocrinology 145(9): 4278-4285.
Brandt I., E. J. Sticker and M. J. Lentze. 2003. Catch-up growth of head circumference of very low birth weight, small for gestational age preterm infants and mental development to adulthood. Journal of Pediatrics 142(5): 463-468.
Calame A., S. Ducret, L. Jaunin and B. Plancherel. 1983. High risk appropriate for gestational age (AGA) and small for gestational age (SGA) preterm infants. Neurological handicap and developmental abnormalities at five years of age. Helvetica Paediatrica Acta 38(1): 39-50.
Carmichael S. L., G. M. Shaw, D. M. Schaffer, C. Laurent and S. Selvin. 2003. Dieting behaviors and risk of neural tube defects. American Journal of Epidemiology 158(12): 1127-1131.
Casey P. H., L. Whiteside-Mansell, K. Barrett, R. H. Bradley and R. Gargus. 2006. Impact of prenatal and/or postnatal growth problems in low birth weight preterm infants on school-age outcomes: an 8-year longitudinal evaluation. Pediatrics 118(3): 1078-1086.
Catalano P. M. and H. M. Ehrenberg. 2006. The short- and long-term implications of maternal obesity on the mother and her offspring. British Journal of Obstetrics and Gynaecology 113(10): 1126-1133.
Catalano P. M., M. Hoegh, J. Minium, L. Huston-Presley, S. Bernard, S. Kalhan and S. Hauguel-De Mouzon. 2006. Adiponectin in human pregnancy: implications for regulation of glucose and lipid metabolism. Diabetologia 49(7): 1677-1685.
Cedergren M. 2006. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. International Journal of Gynaecology and Obstetrics 93(3): 269-274.
Chen A., S. A. Feresu, C. Fernandez and W. J. Rogan. 2009. Maternal obesity and the risk of infant death in the United States. Epidemiology 20(1): 74-81.
Churchill J. A., H. W. Berendes and J. Nemore. 1969. Neuropsychological deficits in children of diabetic mothers. A report from the Collaborative Study of Cerebral Palsy. American Journal of Obstetrics and Gynecology 105(2): 257-268.
Cole T. J., M. C. Bellizzi, K. M. Flegal and W. H. Dietz. 2000. Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal 320(7244): 1240-1243.
Crowther C. A., J. E. Hiller, J. R. Moss, A. J. McPhee, W. S. Jeffries and J. S. Robinson. 2005. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. New England Journal of Medicine 352(24): 2477-2486.
Diaz J. and E. M. Taylor. 1998. Abnormally high nourishment during sensitive periods results in body weight changes across generations. Obesity Research 6(5): 368-374.
Dietz P. M., W. M. Callaghan, M. E. Cogswell, B. Morrow, C. Ferre and L. A. Schieve. 2006. Combined effects of prepregnancy body mass index and weight gain during pregnancy on the risk of preterm delivery. Epidemiology 17(2): 170-177.
Dietz P., W. Callaghan, R. Smith, A. Sharma. 2009. Associations of low pregnancy weight gain with three measures of small for gestational age infants. American Journal of Obstetrics and Gynecology 201: 53.e1-53.e7.
Dombkowski K. J., S. W. Leung and J. G. Gurney. 2008. Prematurity as a predictor of childhood asthma among low-income children. Annals of Epidemiology 18(4): 290-297.
Dorner G., A. Plagemann, J. Ruckert, F. Gotz, W. Rohde, F. Stahl, U. Kurschner, J. Gottschalk, A. Mohnike and E. Steindel. 1988. Teratogenetic maternofoetal transmission and prevention of diabetes susceptibility. Experimental and Clinical Endocrinology 91(3): 247-258.
Escalona S. K. 1982. Babies at double hazard: early development of infants at biologic and social risk. Pediatrics 70(5): 670-676.
Feldman R. and A. I. Eidelman. 2006. Neonatal state organization, neuromaturation, mother-infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics 118(3): e869-e878.
Fisch R. O., M. K. Bilek and R. Ulstrom. 1975. Obesity and leanness at birth and their relationship to body habitus in later childhood. Pediatrics 56(4): 521-528.
Freinkel N., D. L. Cockroft, N. J. Lewis, L. Gorman, S. Akazawa, L. S. Phillips and G. E. Shambaugh, 3rd. 1986. The 1986 McCollum award lecture. Fuel-mediated teratogenesis during early organogenesis: the effects of increased concentrations of glucose, ketones, or somatomedin inhibitor during rat embryo culture. American Journal of Clinical Nutrition 44(6): 986-995.
Gale C. R., M. K. Javaid, S. M. Robinson, C. M. Law, K. M. Godfrey and C. Cooper. 2007. Maternal size in pregnancy and body composition in children. Journal of Clinical Endocrinology and Metabolism 92(10): 3904-3911.
Geelhoed J. J., L. Van Osch-Gevers, B. O. Verburg, E. A. Steegers, A. Hofman, W. Helbing, J. C. Witteman and V. W. Jaddoe. 2008. Maternal anthropometrics in pregnancy are associated with left ventricular mass in infancy. The generation R study. Pediatric Research 63(1): 62-66.
Geva R., R. Eshel, Y. Leitner, A. F. Valevski and S. Harel. 2006. Neuropsychological outcome of children with intrauterine growth restriction: a 9-year prospective study. Pediatrics 118(1): 91-100.
Gillman M. W. 2005. Developmental origins of health and disease. New England Journal of Medicine 353(17): 1848-1850.
Gillman M. W. 2008. The first months of life: a critical period for development of obesity. American Journal of Clinical Nutrition 87(6): 1587-1589.
Gluckman P. D. and M. A. Hanson. 2006a. Changing times: the evolution of puberty. Molecular and Cellular Endocrinology 254-255: 26-31.
Gluckman P. D. and M. A. Hanson. 2006b. Evolution, development and timing of puberty. Trends in Endocrinology and Metabolism 17(1): 7-12.
Goldenberg R. L., M. B. DuBard, S. P. Cliver, K. G. Nelson, K. Blankson, S. L. Ramey and A. Herman. 1996. Pregnancy outcome and intelligence at age five years. American Journal of Obstetrics and Gynecology 175(6): 1511-1515.
Goldenberg R. L., H. J. Hoffman and S. P. Cliver. 1998. Neurodevelopmental outcome of small-for-gestational-age infants. European Journal of Clinical Nutrition 52(Suppl 1): S54-S58.
Grantham-McGregor S. 1995. A review of studies of the effect of severe malnutrition on mental development. Journal of Nutrition 125(8 Suppl): 2233S-2238S.
Hack M. 1998. Effects of intrauterine growth retardation on mental performance and behavior, outcomes during adolescence and adulthood. European Journal of Clinical Nutrition 52(Suppl 1): S65-S70; discussion S70-S71.
Hanson M. A. and P. D. Gluckman. 2008. Developmental origins of health and disease: new insights. Basic & Clinical Pharmacology & Toxicology 102(2): 90-93.
Hille E. T., N. Weisglas-Kuperus, J. B. van Goudoever, G. W. Jacobusse, M. H. Ens-Dokkum, L. de Groot, J. M. Wit, W. B. Geven, J. H. Kok, M. J. de Kleine, L. A. Kollee, A. L. Mulder, H. L. van Straaten, L. S. de Vries, M. M. van Weissenbruch and S. P. Verloove-Vanhorick. 2007. Functional outcomes and participation in young adulthood for very preterm and very low birth weight infants: the Dutch Project on Preterm and Small for Gestational Age Infants at 19 years of age. Pediatrics 120(3): e587-e595.
Hillier T. A., K. L. Pedula, M. M. Schmidt, J. A. Mullen, M. A. Charles and D. J. Pettitt. 2007. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care 30(9): 2287-2292.
Hjalgrim L. L., T. Westergaard, K. Rostgaard, K. Schmiegelow, M. Melbye, H. Hjalgrim and E. A. Engels. 2003. Birth weight as a risk factor for childhood leukemia: a meta-analysis of 18 epidemiologic studies. American Journal of Epidemiology 158(8): 724-735.
Hofman P. L., F. Regan, W. E. Jackson, C. Jefferies, D. B. Knight, E. M. Robinson and W. S. Cutfield. 2004. Premature birth and later insulin resistance. New England Journal of Medicine 351(21): 2179-2186.
Hollo O., P. Rautava, T. Korhonen, H. Helenius, P. Kero and M. Sillanpaa. 2002. Academic achievement of small-for-gestational-age children at age 10 years. Archives of Pediatrics and Adolescent Medicine 156(2): 179-187.
Holwerda-Kuipers J. 1987. The cognitive development of low-birthweight children. Journal of Child Psychology and Psychiatry and Allied Disciplines 28(2): 321-328.
Hovi P., S. Andersson, J. G. Eriksson, A. L. Jarvenpaa, S. Strang-Karlsson, O. Makitie and E. Kajantie. 2007. Glucose regulation in young adults with very low birth weight. New England Journal of Medicine 356(20): 2053-2063.
Hutton J. L., P. O. Pharoah, R. W. Cooke and R. C. Stevenson. 1997. Differential effects of preterm birth and small gestational age on cognitive and motor development. Archives of Disease in Childhood. Fetal and Neonatal Edition 76(2): F75-F81.
Hwang H. S., J. Y. Kwon, M. A. Kim, Y. W. Park and Y. H. Kim. 2007. Maternal serum highly sensitive C-reactive protein in normal pregnancy and pre-eclampsia. International Journal of Gynaecology and Obstetrics 98(2): 105-109.
Indredavik M. S., T. Vik, S. Heyerdahl, S. Kulseng, P. Fayers and A. M. Brubakk. 2004. Psychiatric symptoms and disorders in adolescents with low birth weight. Archives of Disease in Childhood. Fetal and Neonatal Edition 89(5): F445-F450.
IOM (Institute of Medicine). 1990. Nutrition During Pregnancy. Washington, DC: National Academy Press.
IOM. 2007. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: The National Academies Press.
Kiel D. W., E. A. Dodson, R. Artal, T. K. Boehmer and T. L. Leet. 2007. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstetrics and Gynecology 110(4): 752-758.
Kilbride H. W., K. Thorstad and D. K. Daily. 2004. Preschool outcome of less than 801-gram preterm infants compared with full-term siblings. Pediatrics 113(4): 742-747.
King J. C. 2006. Maternal obesity, metabolism, and pregnancy outcomes. Annual Review of Nutrition 26: 271-291.
Kinnunen T. I., R. Luoto, M. Gissler, E. Hemminki and L. Hilakivi-Clarke. 2004. Pregnancy weight gain and breast cancer risk. BMC Women’s Health 4(1): 7.
Kono Y., J. Mishina, T. Takamura, H. Hara, I. Sakuma, S. Kusuda and H. Nishida. 2007. Impact of being small-for-gestational age on survival and long-term outcome of extremely premature infants born at 23-27 weeks’ gestation. Journal of Perinatal Medicine 35(5): 447-454.
Kramer M. S. and R. Kakuma. 2003. Energy and protein intake in pregnancy. Cochrane Database of Systematic Reviews (4): CD000032.
Kuh D. and Y. Ben-Shlomo. 2004. A Life Course Approach to Chronic Disease Epidemiology: Tracing the Origins of Ill-Health from Early to Adult Life. London: Oxford University Press.
Kulseng S., A. Jennekens-Schinkel, P. Naess, P. Romundstad, M. Indredavik, T. Vik and A. M. Brubakk. 2006. Very-low-birthweight and term small-for-gestational-age adolescents: attention revisited. Acta Paediatrica 95(2): 224-230.
Kumarasamy V., M. D. Mitchell, F. H. Bloomfield, M. H. Oliver, M. E. Campbell, J. R. Challis and J. E. Harding. 2005. Effects of periconceptional undernutrition on the initiation of parturition in sheep. American Journal of Physiology Regulatory Integrative and Comparative Physiology 288(1): R67-R72.
Lagiou P., A. Lagiou, E. Samoli, C. C. Hsieh, H. O. Adami and D. Trichopoulos. 2006. Diet during pregnancy and levels of maternal pregnancy hormones in relation to the risk of breast cancer in the offspring. European Journal of Cancer Prevention 15(1): 20-26.
Leonard H., N. Nassar, J. Bourke, E. Blair, S. Mulroy, N. de Klerk and C. Bower. 2008. Relation between intrauterine growth and subsequent intellectual disability in a ten-year population cohort of children in Western Australia. American Journal of Epidemiology 167(1): 103-111.
Li C., M. I. Goran, H. Kaur, N. Nollen and J. S. Ahluwalia. 2007. Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring) 15(3): 760-771.
Litt J., H. G. Taylor, N. Klein and M. Hack. 2005. Learning disabilities in children with very low birthweight: prevalence, neuropsychological correlates, and educational interventions. Journal of Learning Disabilities 38(2): 130-141.
Litt R., A. Joseph and R. Gale. 1995. Six year neurodevelopmental follow-up of very low birthweight children. Israel Journal of Medical Sciences 31(5): 303-308.
Lof M., L. Hilakivi-Clarke, S. Sandin and E. Weiderpass. 2008. Effects of pre-pregnancy physical activity and maternal BMI on gestational weight gain and birth weight. Acta Obstetricia et Gynecologica Scandinavica 87(5): 524-530.
Luo Z. C., W. D. Fraser, P. Julien, C. L. Deal, F. Audibert, G. N. Smith, X. Xiong and M. Walker. 2006. Tracing the origins of “fetal origins” of adult diseases: programming by oxidative stress? Medical Hypotheses 66(1): 38-44.
Maffeis C., R. Micciolo, A. Must, M. Zaffanello and L. Pinelli. 1994. Parental and perinatal factors associated with childhood obesity in north-east Italy. International Journal of Obesity and Related Metabolic Disorders 18(5): 301-305.
McCarton C. M., I. F. Wallace, M. Divon and H. G. Vaughan, Jr.1996. Cognitive and neurologic development of the premature, small for gestational age infant through age 6: comparison by birth weight and gestational age. Pediatrics 98(6 Pt 1): 1167-1178.
McLaughlin C. C., M. S. Baptiste, M. J. Schymura, P. C. Nasca and M. S. Zdeb. 2006. Birth weight, maternal weight and childhood leukaemia. British Journal of Cancer 94(11): 1738-1744.
McMillen I. C. and J. S. Robinson. 2005. Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiological Reviews 85(2): 571-633.
Michels K. B., D. Trichopoulos, J. M. Robins, B. A. Rosner, J. E. Manson, D. J. Hunter, G. A. Colditz, S. E. Hankinson, F. E. Speizer and W. C. Willett. 1996. Birthweight as a risk factor for breast cancer. Lancet 348(9041): 1542-1546.
Monteiro P. O. and C. G. Victora. 2005. Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obesity Reviews 6(2): 143-154.
Moreira P., C. Padez, I. Mourao-Carvalhal and V. Rosado. 2007. Maternal weight gain during pregnancy and overweight in Portuguese children. International Journal of Obesity (London) 31(4): 608-614.
Naeye R. L.1979. Weight gain and the outcome of pregnancy. American Journal of Obstetrics and Gynecology 135(1): 3-9.
Naeye R. L. and R. A. Chez. 1981. Effects of maternal acetonuria and low pregnancy weight gain on children’s psychomotor development. American Journal of Obstetrics and Gynecology 139(2): 189-193.
NCHS (National Center for Health Statistics). 1986. Maternal weight gain and the outcome of pregnancy, United States, 1980. Vital Health and Statistics. Series 21, No. 44. DHHS Pub. No. (PHS) 86-1922. Public Health Service. Washington, DC: Government Printing Office.
Nelson K. G., R. L. Goldenberg, H. J. Hoffman and S. P. Cliver. 1997. Growth and development during the first year in a cohort of low income term-born American children. Acta Obstetricia et Gynecologica Scandinavica. Supplement 165: 87-92.
Nixon S. A., M. D. Avery and K. Savik. 1998. Outcomes of macrosomic infants in a nurse-midwifery service. Journal of Nurse-Midwifery 43(4): 280-286.
Nohr E. A., B. H. Bech, M. Vaeth, K. M. Rasmussen, T. B. Henriksen and J. Olsen. 2007. Obesity, gestational weight gain and preterm birth: a study within the Danish National Birth Cohort. Paediatric and Perinatal Epidemiology 21(1): 5-14.
Nohr E. A., M. Vaeth, J. L. Baker, T. Sorensen, J. Olsen and K. M. Rasmussen. 2008. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. American Journal of Clinical Nutrition 87(6): 1750-1759.
O’Keeffe M. J., M. O’Callaghan, G. M. Williams, J. M. Najman and W. Bor. 2003. Learning, cognitive, and attentional problems in adolescents born small for gestational age. Pediatrics 112(2): 301-307.
Oken E., E. M. Taveras, K. P. Kleinman, J. W. Rich-Edwards and M. W. Gillman. 2007. Gestational weight gain and child adiposity at age 3 years. American Journal of Obstetrics and Gynecology 196(4): 322e321-e328.
Oken E., S. L. Rifas-Shiman, A. E. Field, A. L. Frazier and M. W. Gillman. 2008. Maternal gestational weight gain and offspring weight in adolescence. Obstetrics and Gynecology 112(5): 999-1006.
Oliveti J. F., C. M. Kercsmar and S. Redline. 1996. Pre- and perinatal risk factors for asthma in inner city African-American children. American Journal of Epidemiology 143(6): 570-577.
Ong K. K. and R. J. Loos. 2006. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatrica 95(8): 904-908.
Ong K. K., M. L. Ahmed, P. M. Emmett, M. A. Preece and D. B. Dunger. 2000. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. British Medical Journal 320(7240): 967-971.
Paavonen E. J., S. Strang-Karlsson, K. Raikkonen, K. Heinonen, A. K. Pesonen, P. Hovi, S. Andersson, A. L. Jarvenpaa, J. G. Eriksson and E. Kajantie. 2007. Very low birth weight increases risk for sleep-disordered breathing in young adulthood: the Helsinki Study of Very Low Birth Weight Adults. Pediatrics 120(4): 778-784.
Paz I., R. Gale, A. Laor, Y. L. Danon, D. K. Stevenson and D. S. Seidman. 1995. The cognitive outcome of full-term small for gestational age infants at late adolescence. Obstetrics and Gynecology 85(3): 452-456.
Paz I., A. Laor, R. Gale, S. Harlap, D. K. Stevenson and D. S. Seidman. 2001. Term infants with fetal growth restriction are not at increased risk for low intelligence scores at age 17 years. Journal of Pediatrics 138(1): 87-91.
Peng Y., B. Huang, F. Biro, L. Feng, Z. Guo and G. Slap. 2005. Outcome of low birthweight in China: a 16-year longitudinal study. Acta Paediatrica 94(7): 843-849.
Persson B. and J. Gentz. 1984. Follow-up of children of insulin-dependent and gestational diabetic mothers. Neuropsychological outcome. Acta Paediatrica Scandinavica 73(3): 349-358.
Pirc L. K., J. A. Owens, C. A. Crowther, K. Willson, M. J. De Blasio and J. S. Robinson. 2007. Mild gestational diabetes in pregnancy and the adipoinsular axis in babies born to mothers in the ACHOIS randomised controlled trial. BMC Pediatrics 7: 18.
Plagemann A., T. Harder, R. Lindner, K. Melchior, A. Rake, F. Rittel, W. Rohde and G. Dorner. 1998. Alterations of hypothalamic catecholamines in the newborn offspring of gestational diabetic mother rats. Brain Research. Developmental Brain Research 109(2): 201-209.
Polley B. A., R. R. Wing and C. J. Sims. 2002. Randomized controlled trial to prevent excessive weight gain in pregnant women. International Journal of Obstetrics and Related Metabolic Disorders 26(11): 1494-1502.
Pryor J., P. A. Silva and M. Brooke. 1995. Growth, development and behaviour in adolescents born small-for-gestational-age. Journal of Paediatrics and Child Health 31(5): 403-407.
Reece E. A., C. Homko and A. Wiznitzer. 1994. Metabolic changes in diabetic and nondiabetic subjects during pregnancy. Obstetrical and Gynecological Survey 49(1): 64-71.
Rizzo T., B. E. Metzger, W. J. Burns and K. Burns. 1991. Correlations between antepartum maternal metabolism and child intelligence. New England Journal of Medicine 325(13): 911-916.
Rodriguez A., J. Miettunen, T. B. Henriksen, J. Olsen, C. Obel, A. Taanila, H. Ebeling, K. M. Linnet, I. Moilanen and M. R. Jarvelin. 2008. Maternal adiposity prior to pregnancy is associated with ADHD symptoms in offspring: evidence from three prospective pregnancy cohorts. International Journal of Obesity (London) 32(3): 550-557.
Rudra C. B., I. O. Frederick and M. A. Williams. 2008. Pre-pregnancy body mass index and weight gain during pregnancy in relation to preterm delivery subtypes. Acta Obstetricia et Gynecologica Scandinavica 87(5): 510-517.
Salihu H. M., A. P. Alio, R. E. Wilson, P. P. Sharma, R. S. Kirby and G. R. Alexander. 2008. Obesity and extreme obesity: new insights into the black-white disparity in neonatal mortality. Obstetrics and Gynecology 111(6): 1410-1416.
Samuelsson A. M., P. A. Matthews, M. Argenton, M. R. Christie, J. M. McConnell, E. H. Jansen, A. H. Piersma, S. E. Ozanne, D. F. Twinn, C. Remacle, A. Rowlerson, L. Poston and P. D. Taylor. 2008. Diet-induced obesity in female mice leads to offspring hyperphagia, adiposity, hypertension, and insulin resistance: a novel murine model of developmental programming. Hypertension 51(2): 383-392.
Schieve L. A., M. E. Cogswell and K. S. Scanlon. 1999. Maternal weight gain and preterm delivery: differential effects by body mass index. Epidemiology 10(2): 141-147.
Segal P., J. K. Hamilton, M. Sermer, P. W. Connelly, A. J. Hanley, B. Zinman and R. Retnakaran. 2008. Maternal obesity and familial history of diabetes have opposing effects on infant birth weight in women with mild glucose intolerance in pregnancy. Journal of Maternal-Fetal & Neonatal Medicine 21(1): 73-79.
Sewell M. F., L. Huston-Presley, D. M. Super and P. Catalano. 2006. Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. American Journal of Obstetrics and Gynecology 195(4): 1100-1103.
Shaw G. M., K. Todoroff, S. L. Carmichael, D. M. Schaffer and S. Selvin. 2001. Lowered weight gain during pregnancy and risk of neural tube defects among offspring. International Journal of Epidemiology 30(1): 60-65.
Siega-Riz A. M., L. S. Adair and C. J. Hobel. 1996. Maternal underweight status and inadequate rate of weight gain during the third trimester of pregnancy increases the risk of preterm delivery. Journal of Nutrition 126(1): 146-153.
Silva P. A., R. McGee and S. Williams. 1984. A longitudinal study of the intelligence and behavior of preterm and small for gestational age children. Journal of Developmental and Behavioral Pediatrics 5(1): 1-5.
Silverman B. L., T. Rizzo, O. C. Green, N. H. Cho, R. J. Winter, E. S. Ogata, G. E. Richards and B. E. Metzger. 1991. Long-term prospective evaluation of offspring of diabetic mothers. Diabetes 40(Suppl 2): 121-125.
Simmons R. A.2007. Developmental origins of diabetes: the role of epigenetic mechanisms. Current Opinion in Endocrinology, Diabetes, and Obesity 14(1): 13-16.
Sinclair K. D., R. G. Lea, W. D. Rees and L. E. Young. 2007. The developmental origins of health and disease: current theories and epigenetic mechanisms. Society of Reproduction and Fertility Supplement 64: 425-443.
Sommerfelt K., H. W. Andersson, K. Sonnander, G. Ahlsten, B. Ellertsen, T. Markestad, G. Jacobsen, H. J. Hoffman and L. Bakketeig. 2000. Cognitive development of term small for gestational age children at five years of age. Archives of Disease in Childhood 83(1): 25-30.
Sowan N. A. and M. L. Stember. 2000. Parental risk factors for infant obesity. MCN; American Journal of Maternal Child Nursing 25(5): 234-240; quiz 241.
Spinillo A., E. Capuzzo, G. Piazzi, A. Ferrari, V. Morales and M. Di Mario. 1998. Risk for spontaneous preterm delivery by combined body mass index and gestational weight gain patterns. Acta Obstetricia et Gynecologica Scandinavica 77(1): 32-36.
Stehbens J. A., G. L. Baker and M. Kitchell. 1977. Outcome at ages 1, 3, and 5 years of children born to diabetic women. American Journal of Obstetrics and Gynecology 127(4): 408-413.
Stephansson O., P. W. Dickman, A. Johansson and S. Cnattingius. 2001. Maternal weight, pregnancy weight gain, and the risk of antepartum stillbirth. American Journal of Obstetrics and Gynecology 184(3): 463-469.
Stotland N. E., Y. W. Cheng, L. M. Hopkins and A. B. Caughey. 2006. Gestational weight gain and adverse neonatal outcome among term infants. Obstetrics and Gynecology 108(3 Pt 1): 635-643.
Strang-Karlsson S., K. Raikkonen, E. Kajantie, S. Andersson, P. Hovi, K. Heinonen, A. K. Pesonen, A. L. Jarvenpaa, J. G. Eriksson and E. J. Paavonen. 2008a. Sleep quality in young adults with very low birth weight—the Helsinki study of very low birth weight adults. Journal of Pediatric Psychology 33(4): 387-395.
Strang-Karlsson S., K. Raikkonen, A. K. Pesonen, E. Kajantie, E. J. Paavonen, J. Lahti, P. Hovi, K. Heinonen, A. L. Jarvenpaa, J. G. Eriksson and S. Andersson. 2008b. Very low birth weight and behavioral symptoms of attention deficit hyperactivity disorder in young adulthood: the Helsinki study of very-low-birth-weight adults. American Journal of Psychiatry 165(10): 1345-1353.
Strauss R. S. 2000. Adult functional outcome of those born small for gestational age: twenty-six-year follow-up of the 1970 British Birth Cohort. Journal of the American Medical Association 283(5): 625-632.
Sullivan M. C., K. Hawes, S. B. Winchester and R. J. Miller. 2008. Developmental origins theory from prematurity to adult disease. Journal of Obstetric, Gynecologic, and Neonatal Nursing 37(2): 158-164.
Susser M.1991. Maternal weight gain, infant birth weight, and diet: causal sequences. American Journal of Clinical Nutrition 53(6): 1384-1396.
Taveras E. M., S. L. Rifas-Shiman, M. B. Belfort, K. P. Kleinman, E. Oken and M. W. Gillman. 2009. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics 123(4): 1177-1183.
Tavris D. R. and J. A. Read. 1982. Effect of maternal weight gain on fetal, infant, and childhood death and on cognitive development. Obstetrics and Gynecology 60(6): 689-694.
Trichopoulos D. 1990. Hypothesis: does breast cancer originate in utero? Lancet 335(8695): 939-940.
Udal J. N., G. G. Harrison, Y. Vaucher, P. D. Walson and G. Morrow, 3rd.1978. Interaction of maternal and neonatal obesity. Pediatrics 62(1): 17-21.
Van Assche F. A., L. Aerts and W. Gepts. 1979. Morphological changes in the endocrine pancreas in pregnant rats with experimental diabetes. Journal of Endocrinology 80(2): 175-179.
Vatten L. J., B. O. Maehle, T. I. Lund Nilsen, S. Tretli, C. C. Hsieh, D. Trichopoulos and S. O. Stuver. 2002. Birth weight as a predictor of breast cancer: a case-control study in Norway. British Journal of Cancer 86(1): 89-91.
Viggedal G., E. Lundalv, G. Carlsson and I. Kjellmer. 2004. Neuropsychological follow-up into young adulthood of term infants born small for gestational age. Medical Science Monitor 10(1): CR8-CR16.
Villamor E., P. Sparen and S. Cnattingius. 2008. Risk of oral clefts in relation to prepregnancy weight change and interpregnancy interval. American Journal of Epidemiology 167(11): 1305-1311.
Viswanathan M., A. M. Siega-Riz, M.-K. Moos, A. Deierlein, S. Mumford, J. Knaack, P. Thieda, L. J. Lux and K. N. Lohr. 2008. Outcomes of Maternal Weight Gain, Evidence Report/Technology Assessment No. 168. (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under contract No. 290-02-0016.) AHRQ Publication No. 08-E-09. Rockville, MD: Agency for Healthcare Research and Quality.
Wataba K., T. Mizutani, K. Wasada, M. Morine, T. Sugiyama and N. Suehara. 2006. Impact of prepregnant body mass index and maternal weight gain on the risk of pregnancy complications in Japanese women. Acta Obstetricia et Gynecologica Scandinavica 85(3): 269-276.
Watkins M. L., S. A. Rasmussen, M. A. Honein, L. D. Botto and C. A. Moore. 2003. Maternal obesity and risk for birth defects. Pediatrics 111(5 Pt 2): 1152-1158.
Watt J. and K. T. Strongman. 1985. Mother-infant interactions at 2 and 3 months in preterm, small-for-gestational-age, and full-term infants; their relationship with cognitive development at 4 months. Early Human Development 11(3-4): 231-246.
Westwood M., M. S. Kramer, D. Munz, J. M. Lovett and G. V. Watters. 1983. Growth and development of full-term nonasphyxiated small-for-gestational-age newborns: follow-up through adolescence. Pediatrics 71(3): 376-382.
Whitaker R. C. 2004. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 114(1): e29-e36.
Wiles N. J., T. J. Peters, D. A. Leon and G. Lewis. 2005. Birth weight and psychological distress at age 45-51 years: results from the Aberdeen Children of the 1950s cohort study. British Journal of Psychiatry 187: 21-28.
Wiles N. J., T. J. Peters, J. Heron, D. Gunnell, A. Emond and G. Lewis. 2006. Fetal growth and childhood behavioral problems: results from the ALSPAC cohort. American Journal of Epidemiology 163(9): 829-837.
Williams D. 2003. Pregnancy: a stress test for life. Current Opinion in Obstetrics and Gynecology 15(6): 465-471.
Willwerth B. M., B. Schaub, K. G. Tantisira, D. R. Gold, L. J. Palmer, A. A. Litonjua, D. L. Perkins, C. Schroeter, F. K. Gibbons, M. W. Gillman, S. T. Weiss and P. W. Finn. 2006. Prenatal, perinatal, and heritable influences on cord blood immune responses. Annals of Allergy, Asthma, and Immunology 96(3): 445-453.
Wolff S., J. Legarth, K. Vangsgaard, S. Toubro and A. Astrup. 2008. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. International Journal of Obesity (London) 32(3): 495-501.
Wrotniak B. H., J. Shults, S. Butts and N. Stettler. 2008. Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. American Journal of Clinical Nutrition 87(6): 1818-1824.














































