1
Introduction
Secondhand smoke, also known as environmental tobacco smoke, is a complex mixture of gases and particles and includes smoke from burning cigarettes, cigars, and pipe tobacco (sidestream smoke) and exhaled mainstream smoke (Cal EPA, 2005a; HHS, 2005). According to the National Toxicology Program, sidestream smoke and mainstream smoke contain “at least 250 chemicals known to be toxic or carcinogenic” (HHS, 2005). Exposure to secondhand smoke results in heart disease, lung cancer, and other diseases in nonsmoking adults (Cal EPA, 2005a; HHS, 2005). Although much research has focused on the carcinogenic properties of smoke, this report focuses on its cardiovascular effects.
In 1972, the U.S. Office of the Surgeon General released its first statement on the public-health hazard to people suffering from coronary heart disease posed by secondhand smoke in The Health Consequences of Smoking (HHS, 1972). In 1986, it emphasized the need for further examination of the relationship between “involuntary smoking” and cardiovascular disease in The Health Consequences of Involuntary Smoking (HHS, 1986). Most recently, in The Health Consequences of Involuntary Exposure to Tobacco Smoke (HHS, 2006), it concluded that exposure to secondhand smoke could have immediate adverse effects on the cardiovascular system in adults and that it causes coronary heart disease.
Smoking cessation has been associated with reduced risk of coronary heart disease. The speed and magnitude of risk reduction after smoking cessation, however, have been debated (Critchley and Capewell, 2003; Dobson et al., 1991; Doll and Peto, 1976; Gordon et al., 1974; Negri et al., 1994). Some studies found that risk could decline to that of a lifelong nonsmoker
(Dobson et al., 1991; Gordon et al., 1974; Lightwood and Glantz, 1997), and others have suggested that some residual excess risk remains (Negri et al., 1994; Teo et al., 2006). Studies have reported a range of latency periods for such risk reduction, with the shortest being 2 or 3 years (Gordon et al., 1974). In addition, the 1990 report The Health Benefits of Smoking Cessation: A Report of the Surgeon General (HHS, 1990) and the National Cancer Institute’s Monograph 8: Changes in Cigarette-Related Disease Risks and Their Implications for Prevention and Control (NCI, 1997) discussed the cardiovascular benefits of smoking cessation. On the basis of a systematic review of 20 cohort studies, Critchley and Capewell (2003) estimated that there was a 36% reduction in mortality in patients with coronary heart disease who quit smoking compared with those who continued smoking. Their data provide evidence that limitation of secondhand-smoke exposure should reduce risk of mortality from coronary heart disease substantially.
The high prevalence of secondhand smoke and consequently the increased risk of coronary heart disease in the U.S. general population have important implications for public health. According to the Third National Health and Nutrition Examination Survey (NHANES III), about 43% of nonsmoking children and 37% of nonsmoking adults are exposed to secondhand smoke in the United States (Pirkle et al., 1996). The California Environmental Protection Agency has estimated that 46,000 (range, 22,700–69,600) excess cardiac deaths in the United States each year are attributable to secondhand-smoke exposure at home and in the workplace (Cal EPA, 2005b). Thus, home and workplace exposure can potentially produce a substantial burden of avoidable deaths from coronary heart disease. Similarly, Lightwood et al. (2009) recently estimated that at the 1999 to 2004 levels, passive smoking leads to 21,800 to 75,100 deaths from coronary heart disease and 38,100 to 128,900 myocardial infarctions annually.
Progress has been made recently in reducing involuntary exposure to secondhand smoke in workplaces, restaurants, and other public places in the United States and abroad. According to the surgeon general’s 2006 report (HHS, 2006), the percentage of U.S. nonsmokers 4 years old and older who are exposed to secondhand smoke decreased from 88% in 1988–1991 to 43% in 2001–2002, improving on the Healthy People 2010 target of 45% (HHS, 2000). Despite the improvement, some 126 million nonsmokers living in the United States in 2000 were still being exposed to secondhand smoke. Data reviewed in the surgeon general’s 2006 report indicate that smoke-free policies are the most economical and effective way to reduce secondhand-smoke exposure (HHS, 2006); the effect of legislation to ban smoking in public places and workplaces on cardiovascular health of nonsmoking adults, however, remains a question.
CHARGE TO THE COMMITTEE
The Centers for Disease Control and Prevention (CDC) asked the Institute of Medicine (IOM) to convene an expert committee to assess the state of the science on the relationship between secondhand-smoke exposure and acute coronary events. This report addresses that charge. Specifically, the committee reviewed available scientific literature on secondhand-smoke exposure (including short-term exposure) and acute coronary events, with emphasis on evidence of causality and on knowledge gaps that future research should address. To accomplish its task, the committee was asked to address a series of specific questions, which are presented in Box 1-1.
COMMITTEE’S APPROACH TO ITS CHARGE
Inherent in that charge is the evaluation for the following three sets of relationships:
-
the association between secondhand smoke exposure and cardiovascular disease, focusing on coronary heart disease and not stroke (Question 1);
-
the association between secondhand smoke exposure and acute coronary events (Questions 2, 3, and 5); and
-
the association between smoking bans and acute coronary events (Questions 4, 5, 6, 7, and 8).
In response to CDC’s request, IOM convened an 11-member committee to assess the state of the science on the relationship between secondhand-smoke exposure and acute coronary events. The committee included experts in secondhand-smoke exposure, the pharmacology and pathophysiology of secondhand smoke, clinical cardiology, epidemiology (including cardiovascular epidemiology), and statistics. The committee met three times, including two open information-gathering sessions at which the members heard from stakeholders and researchers. The appendix presents the agendas of the public meetings.
The committee also conducted an extensive literature search and reviewed relevant publications. To ensure that it was aware of all relevant studies, the committee searched medical-literature databases from 1997 to the present with keywords that included tobacco smoke pollution, secondhand smoke, passive smoking, smoke-free, smoking bans, and smoking ordinance. The databases searched include EMBASE, MedLine, CRISP, ClinicalTrials.gov, the New York Academy of Sciences GreyLit, NACCHO, and WorldCat. Databases were searched for seasonal changes and long-term trends in acute coronary events before and after smoking-ban legislation,
|
BOX 1-1 Specific Questions to the Committee The Centers for Disease Control and Prevention requested that the IOM convenean expert committee to assess the state of the science on the relationship between secondhand smoke exposure and acute coronary events. Specifically, the committee was to review available scientific literature on secondhand smoke exposure (including short-term exposure) and acute coronary events, and produce a report characterizing the state of the science on the topic, with emphasis on the evidence for causality and knowledge gaps that future research should address. In conducting its work the committee was to address the following questions:
|
for exposure data, and for data on pathophysiologic effects of secondhand smoke that could underlie any acute coronary events that might be seen. The literature searches identified thousands of publications relevant to secondhand-smoke pathophysiology and health effects and relevant to smoking bans, from which the committee identified studies to be discussed in this report.
The committee focused on the pathophysiologic, exposure, and epidemiologic studies that it thought most pertinent to its charge, including studies that looked at the cardiotoxic components of secondhand smoke (such as particulate matter). The committee evaluated in great detail 11 publications that specifically assessed the effect of smoking bans on the incidence of acute coronary events (see Chapter 5). Those publications looked at the effects of eight smoking bans in different locations: three publications on overlapping regions of Italy after implementation of a national smoking ban (Barone-Adesi et al., 2006; Cesaroni et al., 2008; Vasselli et al., 2008);
|
two publications on the effects of a smoking ban in Pueblo, Colorado—one with 18 months of data (Bartecchi et al., 2006) and one with 3 years of data (CDC, 2009); and one publication each on the effects of smoking bans in Helena, Montana (Sargent et al., 2004), Monroe County, Indiana (Seo and Torabi, 2007), Bowling Green, Ohio (Khuder et al., 2007), New York state (Juster et al., 2007), Saskatoon, Canada (Lemstra et al., 2008), and Scotland (Pell et al., 2008). Those 11 publications, which are observational studies examining changes in heart-attack rates following the implementation of a smoking ban, are not designed to answer questions regarding all three of the associations discussed previously. Most of the studies do not measure individual exposures to secondhand smoke or the smoking status of individuals. Those studies, therefore, are designed to evaluate the association between smoking bans and heart attacks, not the effects of secondhand smoke exposure. The publications on the smoking bans in Monroe County, Indiana (Seo and Torabi, 2007), and Scotland (Pell et al., 2008),
however, have data on smoking status and have conducted analyses only in nonsmokers. Those two studies, therefore, are designed to assess the association between secondhand smoke exposure and heart attacks.
For the purpose of addressing its charge, the committee defined secondhand smoke as a complex mixture that is made up of gases and particles and includes smoke from burning cigarettes, cigars, and pipe tobacco (sidestream smoke) and exhaled mainstream smoke. This includes aged smoke that lingers after smoking ceases. In consultation with CDC, the committee interpreted the charge to focus on coronary heart disease, not stroke, and mainly on the association of secondhand smoke with acute coronary events. Most of the 11 key publications, and the present report, examined in this report defined acute coronary events as acute myocardial infarction, including both “ST elevation myocardial infarction” (STEMI) and “non-ST elevation myocardial infarction” (NSTEMI). Other studies included unstable angina (new-onset, accelerating, and rest angina) and sudden cardiac death. The American Heart Association (AHA) defines sudden cardiac death as death resulting from an abrupt loss of heart function (AHA, 2009). Acute coronary syndrome is an umbrella term used to describe any group of clinical symptoms compatible with acute myocardial ischemia, which includes those cardiac events (AHA, 2009). The codes associated with acute coronary syndrome in the ninth revision of International Classification of Diseases include 410.xx for acute myocardial infarction and 411.xx for other acute and sub-acute forms of ischemic heart disease. Chronic cardiovascular disease (chronic CVD) refers to diseases that involve the cardiovascular system, including the heart and circulation, and are longer- term conditions relative to an acute event, such as a heart attack. Chronic CVD increases the risk of a cardiovascular event.
The committee differentiates between smoking bans and smoking restrictions and between smokers and nonsmokers. The definitions that the committee uses in this report for those and other terms are presented in Box 1-2.
In response to specific questions in the committee’s charge (see Box 1-1), the committee also reviewed the scientific evidence and current scientific consensus on the association between secondhand-smoke exposure and cardiovascular disease in general (Question 1) and the evidence related to the biologic plausibility of a causal association between secondhand-smoke exposure and acute coronary events (Question 2). Data on cardiovascular disease and data on acute coronary events are presented in Chapter 2. Because secondhand smoke and air pollution contain many of the same constituents (such as particulate matter), the committee also discussed the association between exposure to some constituents of air pollution and acute coronary
|
BOX 1-2 Definitions Smoker: A person that smokes tobacco products. Nonsmoker: A person that does not smoke tobacco products. Secondhand smoke: A complex mixture that is made up of gases and particles and includes smoke from burning cigarettes, cigars, and pipe tobacco (sidestream smoke) and exhaled mainstream smoke. This includes aged smoke that lingers after smoking ceases. Acute coronary event: Acute myocardial infarction, including both “ST elevation myocardial infarction” (STEMI) and “non-ST elevation myocardial infarction” (NSTEMI). Smoking ban: A legal mandate that prohibits use of lit tobacco products in designated public or private places (such as office buildings). Smoking restriction: A legal mandate that limits the use of lit tobacco products to specified areas in designated public or private places (such as office buildings). |
events. The committee presents information on air pollutants in this report relevant to the biologic plausibility of associations between secondhand smoke and cardiovascular disease, but it did not conduct an extensive literature review on the topic of air-pollutant health effects.
SOURCES OF UNCERTAINTY IN KEY STUDIES
As discussed above, 11 publications report studies of the effect of smoking bans on the incidence of acute coronary events. The design of those studies created challenges to their interpretation and uncertainties in their conclusions. Those challenges include: the lack of a closed study population, the need to disentangle the effects of the smoking ban itself from other concurrent activities that could affect smoking behaviors, exposure assessment, the time between cessation of exposure and changes in disease rates, the use of less-than-perfect control groups, the question of the biologic plausibility of the effect, the necessarily nonexperimental nature of the
studies, the need to clarify hypotheses and variability in statistical analyses.1 The challenges are discussed in detail in later chapters in this report; they are summarized briefly below.
Ideally, when evaluating an effect in a population that population would be closed, that is, it does not change with time (for example, in a clinical trial). The studies that examined the effect of smoking bans were inevitably not closed populations; people were free to move back and forth between areas with and without bans. The committee discusses the potential impact of that migration on the results of the studies in Chapter 7, but generally it would be expected to attenuate the estimated effects of smoking bans in studies unless smokers were selectively moving out of areas with bans and into areas without bans.
In examining the effect of any population intervention, ideally there is a defined time at which the intervention is implemented so that the reduction in adverse outcomes attributable to the intervention can be estimated, and that other interventions that could affect the outcome being studied can be accounted for. In this case, the intervention—the implementation of a smoking ban—does not necessarily occur at a precise time given that voluntary bans or other smoking restrictions may already be in place for a subset of the study population when the ban is imposed. Moreover, bans may vary in scope, enforcement may differ among areas and vary over time, and a smoking ban is often (but not necessarily) accompanied by other interventions, such as smoking-cessation and education efforts (see Figure 1-1). When the committee draws conclusions regarding the effects of smoking bans, therefore, it cannot completely distinguish the effects of bans from the effects of policies and activities that are occurring concurrently. At a minimum, the process leading to adoption of a ban is likely to generate awareness about smoking-related risks. These issues surrounding smoking bans are discussed further in Chapter 7, which also discusses how they might have affected the 11 key publications.
Three issues are important in assessing exposure. First, although two of the 11 studies have information on smoking statues, the other studies do not have the data available to determine the smoking status of people who have acute coronary events. Smokers might quit or decrease their smoking in anticipation of or after a ban is implemented (IOM, 2007). If a study does not look only at nonsmokers or does not determine the smoking status of people who have acute coronary events, it cannot separate decreases in acute coronary events in nonsmokers that are due to lowering of secondhand-smoke exposure from decreases that are due to smoking
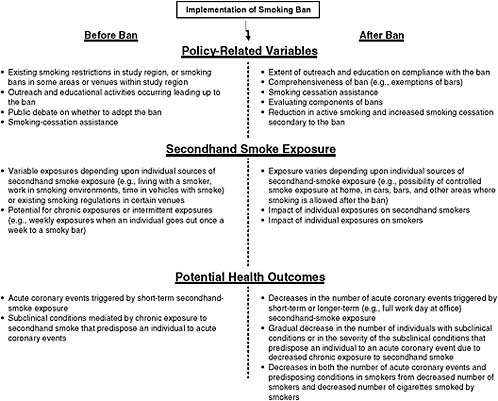
FIGURE 1-1 Factors that can affect the impact of smoking bans on cardiovascular outcomes. A number of policy-related variables can differ among locations and affect the impact of a smoking ban. The concentration of secondhand smoke can also differ among locations both before and after a ban is implemented. Outcome-related factors can differ and affect study results.
cessation.2 Second, not all the key publications quantified the extent to which the smoking bans resulted in a decrease in secondhand-smoke exposure. Third, partial smoking bans were in place in some areas before the bans examined in the studies and would have decreased secondhand-smoke exposure prior to the implementation of the law. Exposure issues related to secondhand smoke are discussed in detail in Chapter 2, and the specific exposure measurements used in the key studies are discussed in Chapter 6. Another concern is the assessment of exposure to secondhand smoke itself. There is a hierarchy of exposure-assessment methods, and most of the studies use different methods; although some of the studies are strong in assessment (for example, using measurements of secondhand smoke before and after the implementation of a ban), others are not as rigorous. Exposure assessment in general is discussed in Chapter 2 and assessment in the individual studies in Chapter 6. The issue of exposure is further complicated by the potential effects of acute versus chronic exposures. As seen in Figure 1-1, in the key studies examining smoking bans secondhand-smoke exposure could be chronic or intermittent prior to a smoking ban being implemented. After a smoking ban, chronic or intermittent exposures could still occur but possibly to a lesser extent because of the ban (see Chapter 2 for a discussion of the effect of a ban on secondhand smoke exposures). Similarly, in cohort and case–control studies the exposures could be chronic or intermittent. Because the duration, frequency and magnitude of the exposures are not analyzed in many of those studies, most of the conclusions of the committee are made for exposure in general, assuming some recurrent level of recurrent secondhand-smoke exposure. Acute, chronic, and intermittent exposures have been evaluated in experimental studies, which can provide information on the duration of exposure required to produce an effect. Those studies address the pathophysiology of any cardiovascular effects and the timeframes associated with any effects.
The issue of the interval between implementation of a smoking ban and a change in the rate of acute coronary events is included in the charge to the committee (Question 5) and is relevant to the committee’s judgment as to the biologic plausibility of a relationship between exposure to secondhand smoke and acute coronary events. That period is difficult to define under circumstances in which the precise date of initiation of an intervention is not known and can vary within an area, depending on compliance and enforcement. The time period is relevant to the mechanisms by which secondhand smoke could cause acute coronary events. The committee also examined time between exposure to particulate matter and cardiovascular
effects because particulate matter is a component of secondhand smoke. This issue is discussed in Chapter 2 and, with regard to the key studies, in Chapter 7.
The key studies used two types of controls. With one type, a study compared acute cardiovascular events in a given population before and during a smoking ban. (One study also investigated what happened when a ban was lifted.) Such a study cannot evaluate the effects of other changes over time (when, in all the areas involved, both rates of smoking and rates of acute cardiovascular disease were generally going down). Other studies instead (or in addition) selected as a control population people in an area that did not implement a ban. A study of that design can to some extent control for larger trends (secular trends), but inevitably such comparison populations could differ from study populations in several ways that might be related to both the likelihood of exposure to secondhand smoke and the incidence of acute cardiovascular events, and this would add uncertainty to the results of the study. Issues related to controls are discussed in Chapter 7.
An important aspect of the committee’s charge to weigh the evidence of a causal association between secondhand-smoke exposure and acute coronary events is the biologic plausibility of the association. Evidence related to biologic plausibility comes from experimental studies of humans and other animals. Because air pollution has many of the same constituents as secondhand smoke, the committee also reviewed evidence of a relationship between air pollution and acute coronary events. That information is discussed in Chapter 3.
The key studies discussed in this report are necessarily nonexperimental; they are observational or surveillance studies that looked at the effect of a smoking ban on hospital outcomes, out-of-hospital deaths, or both. Nonexperimental design can result in decreased information on the individual level, including information on exposure and in some instances smoking status. The results of population-based smoking-ban studies can be part of the evidence of a causal relationship between secondhand smoke and acute coronary events.
Other considerations in the determination of causality historically have included temporality, strength of the association, dose–response relationship, identified biologic mechanism, specificity, coherence with existing theory and knowledge, experimental evidence, and alternate explanations. Population-based studies can provide some evidence related to most of those, but they cannot yield experimental evidence and cannot rule out all alternative explanations. The epidemiologic studies under consideration are not randomized controlled studies, so they are subject to several potential sources of bias and confounding that need to be taken into account in weighing the validity of their results. Each of the studies has strengths, limitations, and weaknesses, including standard epidemiologic limitations
related to time-trend studies, comparison groups, control of confounding factors, lack of individual biologic measurements, and information on concurrent efforts.
Another important aspect to consider is the hypothesis tested in a study. A study could try to test several hypotheses related to secondhand-smoke exposure; each hypothesis might be best answered with a different study design, and each would be related to different questions being asked of this committee. A cohort study could test the hypothesis that long-term exposure to secondhand smoke increases the risk of coronary events, a “natural experimental” study could test the hypothesis that a long-term reduction in secondhand-smoke exposure leads to a reduced incidence of events, and an observational case-crossover study with detailed examination of the temporal relationships between exposure and episodes and detailed exposure assessment (a study similar, for example, to time-series studies of air pollution that looked at the relationship between exposures and acute coronary events) could be used to test the hypothesis that secondhand-smoke exposure triggers acute coronary events in people who are at risk. Each type of study answers different questions that are integrated into the charge to this committee.
Additional problems in using population-based studies like these when trying to infer causality include the inability to assess the pathophysiology of a relationship between secondhand-smoke exposure and acute cardiac events, difficulty in assessing dose–response relationships, and difficulty in determining the strength of a relationship in the absence of subgroup analyses of smokers, nonsmokers, and people with greater or smaller magnitudes of other risk factors. Experimental data provide information on the pathophysiology and on dose–response relationships.
Most of the studies assume a linear trend variable (month) to quantify secular trends in the rate of acute coronary events, and some of these (Juster et al., 2007; Khuder et al., 2007) fit a linear-regression model that yields an estimated age- and sex-adjusted rate of an adverse outcome. The committee discusses those approaches and other aspects related to the statistical analysis in Chapter 7.
ORGANIZATION OF THIS REPORT
This remainder of this report is organized into seven chapters and one appendix. Chapter 2 summarizes the data on exposure to secondhand smoke, including its constituents, its measurement, and typical exposure to it in the absence and presence of smoking bans. Chapter 3 presents studies of pathophysiologic responses to secondhand-smoke exposure that could be related to cardiovascular effects. It summarizes information from cellular, animal, and human experimental studies, and presents conclusions
and recommendations based on the surgeon general’s 2006 report and other research. Epidemiologic studies that looked at the association between secondhand-smoke exposure and cardiovascular disease and acute coronary events, other than studies related to smoking bans, are discussed in Chapter 4. Chapter 5 contains background on the history and context of smoking bans around the world. Chapter 6 describes the 11 key studies that examined acute coronary events in relation to smoking bans, focusing on data sources, study design, the choice of end points, and possible confounders. The information from those key studies as well as the pathophysiologic data and other epidemiologic studies discussed in Chapter 4 are then synthesized in Chapter 7. In Chapter 8, the committee summarizes its conclusions about the association between secondhand-smoke exposure and cardiovascular disease, secondhand-smoke exposure and acute coronary events, and smoking bans and acute coronary events, discussing the weight of evidence for the associations. In that chapter the committee also presents its responses to the specific questions outlined in Box 1-1. The appendix presents agendas of the public meetings held by the committee.
REFERENCES
AHA (American Heart Association). 2009. (Accessed April 6, 2009, from http://www.americanheart.org/presenter.jhtml?identifier=4741).
Barone-Adesi, F., L. Vizzini, F. Merletti, and L. Richiardi. 2006. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. European Heart Journal 27(20):2468-2472.
Bartecchi, C., R. N. Alsever, C. Nevin-Woods, W. M. Thomas, R. O. Estacio, B. B. Bartelson, and M. J. Krantz. 2006. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation 114(14):1490-1496.
Cal EPA (California Environmental Protection Agency). 2005a. Proposed identification of environmental tobacco smoke as a toxic air contaminant. Part A: Exposure assessment. Sacramento, CA: California Environmental Protection Agency.
———. 2005b. Proposed identification of environmental tobacco smoke as a toxic air contaminant. Part B: Health effects. Sacramento, CA: California Environmental Protection Agency.
CDC (Centers for Disease Control and Prevention). 2009. Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance—city of Pueblo, Colorado, 2002–2006. MMWR—Morbidity & Mortality Weekly Report 57(51):1373-1377.
Cesaroni, G., F. Forastiere, N. Agabiti, P. Valente, P. Zuccaro, and C. A. Perucci. 2008. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation 117(9):1183-1188.
Critchley, J. A., and S. Capewell. 2003. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: A systematic review. JAMA 290(1):86-97.
Dobson, A. J., H. M. Alexander, R. F. Heller, and D. M. Lloyd. 1991. How soon after quitting smoking does risk of heart attack decline? Journal of Clinical Epidemiology 44(11):1247-1253.
Doll, R., and R. Peto. 1976. Mortality in relation to smoking: 20 years’ observations on male British doctors. British Medical Journal 2(6051):1525-1536.
Gordon, T., W. B. Kannel, D. McGee, and T. R. Dawber. 1974. Death and coronary attacks in men after giving up cigarette smoking. A report from the Framingham Study. Lancet 2(7893):1345-1348.
HHS (U.S. Department of Health and Human Services). 1972. The health consequences of smoking. Rockville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
———. 1986. The health consequences of involuntary smoking: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
———. 1990. The health benefits of smoking cessation: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
———. 2000. Healthy people 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: U.S. Government Printing Office.
———. 2005. Report on carcinogens. 11th ed. U.S. Department of Health and Human Services, Public Health Service, National Toxicology Program.
———. 2006. The health consequences of involuntary exposure to tobacco smoke: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
IOM (Institute of Medicine). 2007. Ending the tobacco problem: A blueprint for the nation. Washington, DC: The National Academies Press.
Juster, H. R., B. R. Loomis, T. M. Hinman, M. C. Farrelly, A. Hyland, U. E. Bauer, and G. S. Birkhead. 2007. Declines in hospital admissions for acute myocardial infarction in New York state after implementation of a comprehensive smoking ban. American Journal of Public Health 97(11):2035-2039.
Khuder, S. A., S. Milz, T. Jordan, J. Price, K. Silvestri, and P. Butler. 2007. The impact of a smoking ban on hospital admissions for coronary heart disease. Preventive Medicine 45(1):3-8.
Lemstra, M., C. Neudorf, and J. Opondo. 2008. Implications of a public smoking ban. Canadian Journal of Public Health 99(1):62-65.
Lightwood, J. M., and S. A. Glantz. 1997. Short-term economic and health benefits of smoking cessation: Myocardial infarction and stroke. Circulation 96(4):1089-1096.
Lightwood, J. M., P. G. Coxson, K. Bibbins-Domingo, L. W. Williams, and L. Goldman. 2009. Coronary heart disease attributable to passive smoking: CHD policy model. American Journal of Preven¡tive Medicine 36(1):13-20.
NCI (National Cancer Institute). 1997. Monograph 8: Changes in cigarette-related disease risks and their implications for prevention and control. Bethesda, MD: National Institutes of Health.
Negri, E., C. La Vecchia, B. D’Avanzo, A. Nobili, and R. G. La Malfa. 1994. Acute myocardial infarction: Association with time since stopping smoking in Italy. GISSI-EFRIM investigators. Gruppo Italiano per lo Studio della Sopravvivenza nell’infarto. Epidemiologia dei Fattori di Rischio dell’Infarto Miocardico. Journal of Epidemiology and Community Health 48(2):129-133.
Pell, J. P., S. Haw, S. Cobbe, D. E. Newby, A. C. H. Pell, C. Fischbacher, A. McConnachie, S. Pringle, D. Murdoch, F. Dunn, K. Oldroyd, P. Macintyre, B. O’Rourke, and W. Borland. 2008. Smoke-free legislation and hospitalizations for acute coronary syndrome. New England Journal of Medicine 359(5):482-491.
Pirkle, J. L., K. M. Flegal, J. T. Bernert, D. J. Brody, R. A. Etzel, and K. R. Maurer. 1996. Exposure of the US population to environmental tobacco smoke: The third National Health and Nutrition Examination Survey, 1988 to 1991. JAMA 275(16):1233-1240.
Sargent, R. P., R. M. Shepard, and S. A. Glantz. 2004. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: Before and after study. BMJ 328(7446):977-980.
Seo, D.-C., and M. R. Torabi. 2007. Reduced admissions for acute myocardial infarction associated with a public smoking ban: Matched controlled study. Journal of Drug Education 37(3):217-226.
Teo, K. K., S. Ounpuu, S. Hawken, M. R. Pandey, V. Valentin, D. Hunt, R. Diaz, W. Rashed, R. Freeman, L. Jiang, X. Zhang, S. Yusuf, and I. S. Investigators. 2006. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: A case-control study. Lancet 368(9536):647-658.
Vasselli, S., P. Papini, D. Gaelone, L. Spizzichino, E. De Campora, R. Gnavi, C. Saitto, N. Binkin, and G. Laurendi. 2008. Reduction incidence of myocardial infarction associated with a national legislative ban on smoking. Minerva Cardioangiologica 56(2):197-203.
















