7
Synthesis of Key Studies Examining the Effect of Smoking Bans on Acute Coronary Events
In this chapter, the committee synthesizes the information yielded by the key studies and discusses the overall weight of evidence from them, their uncertainties, the extent to which the uncertainties affect interpretation of their results, and the conclusions that can be drawn from them.
LIMITATIONS AND SOURCES OF UNCERTAINTY IN KEY STUDIES
Some elements of design and uncertainty in the key studies pose challenges in the interpretation of the studies that are relevant to the effect of smoking bans on acute coronary events: the inherently nonexperimental design of the studies, the hypotheses tested in the studies, the lack of closed study populations, the use of less-than-perfect comparison groups, the need to disentangle the effects of a smoking ban itself from concurrent activities that could affect smoking behavior, exposure assessment, outcome, the time from cessation of exposure to secondhand smoke to changes in disease rates, the biologic plausibility of an effect, analytic issues, and the potential for publication bias. Those are all discussed in this section. When reviewing the key studies, the committee kept in mind the characteristics that would make an ideal study to evaluate the effect of an intervention, a smoking ban, on an outcome, acute coronary events. This was a useful framework but a caveat is needed. The committee looked at the study designs and analyses with the advantage of hindsight; such hindsight is helpful in considering how to design a more rigorous evaluation but does not imply that the study authors should have or could have designed an observational study that addressed all of those elements nor that all of those
elements would have been under the control of the researchers. Those characteristics are summarized in Table 7-1. The table includes a description of the characteristics of studies and some of the ideals and challenges related to them. Researchers must weigh the benefits of those ideals across all the characteristics because a study that meets all the ideals typically will not be feasible to conduct. For example, it would be difficult to conduct a study with a large sample that requires autopsies for all cases. Furthermore, journals often have page limitations that preclude the publication of detailed analyses, such as sensitivity analyses, which ideally would be included in studies like those discussed here.
Although the 11 studies discussed here are observational studies and have limitations inherent to observational studies, it is important that the studies took advantage of natural experiments to directly evaluate the effects of an intervention (a smoking ban and concomitant activities) on a health outcome of interest (acute coronary events). As discussed in Assessing the Health Impact of Air Quality Regulations: Concepts and Methods
TABLE 7-1 Characteristics and Challenges in Study Designa
|
Characteristics |
Ideal |
Research Challenges to Consider |
|
Study population |
|
When using “natural” intervention, such as smoking ban, it is difficult to control many aspects of population
|
|
Characteristics |
Ideal |
Research Challenges to Consider |
|
Smoking-ban intervention |
|
|
|
Exposure assessment |
|
|
|
Outcome |
|
|
|
Time between implementation and effect |
|
|
for Accountability Research (HEI Accountability Working Group, 2003) in the context of air-pollution regulations, studies of interventions constitute a definitive approach to determining whether regulations have health benefits. French and Heagerty (2008) also discuss the advantages and limitations of longitudinal data for assessing the impact of policy changes.
Nonexperimental Design
The key studies discussed in this report are of necessity nonexperimental; they are observational or surveillance studies that looked at the effects of a smoking ban on hospital outcomes. Such studies do not typically have a great deal of information on the individual level, including exposures and in some instances smoking status. The results of ecologic smoking-ban studies can, however, support identification of associations and findings of causality (Rubin, 2008).
Hypothesis
The majority of the key studies reviewed in this chapter were natural experiments in that there was an intervention (a smoking ban) that would lead to a reduction in secondhand-smoke exposure (with either direct evidence from a given ban or indirect evidence from bans in other locales that exposure decreased). The studies took advantage of the intervention to test the hypothesis that a reduction in secondhand-smoke exposure leads to a reduced incidence of acute coronary events. Because of a lack of information on smoking status, most of the studies did not directly address the question of whether a decrease in secondhand smoke decreases the risk of coronary events, but as discussed above, the data do indicate that secondhand-smoke exposure decreased after implementation of the bans studied; therefore, even the studies that did not have information on smoking status provide supportive evidence of the effects of secondhand smoke.
As discussed previously, only two studies (Pell et al., 2008; Seo and Torabi, 2007) had information on the smoking status of cases; therefore, only those two directly addressed the question of the effect of secondhand-smoke exposure on nonsmokers rather than the question of the effect of a smoking ban. In both of these studies a decrease in coronary events was observed among nonsmokers after implementation of the smoking ban.
It is important to consider the hypothesis tested in a study when interpreting a study. A number of different hypotheses related to secondhand-smoke exposure could be tested in a study; each would be best evaluated with a different study design, and each would be related to different questions that were asked of this committee. A cohort study could test the hypothesis that long-term exposure to secondhand smoke increases the risk of
coronary events. A natural experiment (or quasiexperimental design) could be used to test the hypothesis that a long-term reduction in secondhand-smoke exposure leads to a reduced incidence of events, and a case-crossover design with a detailed examination of the temporal relationships between exposure and incidence of events would be ideal to test the hypothesis that secondhand-smoke exposure triggers acute coronary events in at-risk people (personal communication, J. Kaufman, University of Seattle, Washington, January 30, 2009). Each type of study would answer different questions that are in the charge to this committee.
Study Populations
The key studies reviewed by the committee look at different populations, or portions of populations, have different information available, and have different sample sizes, some of which are small. The differences in the populations limit the ability to quantitatively compare the changes in risk across the studies and, in some cases, limit the confidence in those studies. The studies, however, are retrospective in nature (with the exception of Scotland) and the populations are designated on the basis of the smoking ban coverage and availability of data.
The population should be large enough to minimize problems of non-uniformity over short periods, and the baseline exposure to secondhand smoke should be large enough for the study to have the power to detect changes of public-health relevance. In addition, information on the population, such as smoking status and other risk factors for acute coronary events or cardiovascular disease that could be confounders in the study, should be available.
Ideally, the study population will have been under active surveillance or enrolled in a prospective cohort study, so that the data collected before and after implementation of the ban will be directly comparable; and the population will be closed, that is, it will not change over the period of study. Inevitably, the studies that examined the effect of smoking bans were not closed populations; people were free to immigrate to or emigrate from the region studied and to move back and forth between areas with and without bans. The extent of migration in the communities studied most likely varied from study to study. However, as mentioned in Chapter 1, migration would be expected to decrease the effects of smoking bans on acute coronary events in studies unless smokers were selectively moving out of areas with bans and into areas without bans. Although none of the studies discussed the potential for migration extensively, there is no reason to believe that most of the locations would have a large amount of migration of smokers at the time of the ban and over the relatively short period of observation. One exception might be some geographic areas in New York state that are
next to other states. For example, smokers in the New York City area might have lived, worked, or socialized in New Jersey (where a comprehensive statewide smoking ban was not put into effect until April 15, 2006) so that they could smoke. Other areas of the state that are farther from state borders (that is, farther from states that might not have had a smoking ban), however, have been much less likely to be affected by such migration. Similarly, people in locations that are more isolated (such as Helena, Montana, or Pueblo, Colorado) or in which bans are widely implemented (such as the entire country of Italy or Scotland) are less likely to have moved because of smoking bans. Thus, although migration in the populations studied is possible, the committee does not believe that migration biased the results of the studies substantially.
Comparison Groups
The key studies used two types of controls. Some compared acute cardiovascular events in a given population before and during smoking bans (internal control group). Such a study cannot evaluate the effects of other changes over time, and this is a concern especially because in many of the areas under study both rates of smoking and rates of acute cardiovascular disease were going down. There was an exception; one study was able to assess what happened when a ban was lifted.
Other studies, instead or in addition, selected a comparison or control population (external control group) from an area that did not implement a ban, but otherwise was similar to the population where the intervention occurred. Such a study can to some extent control for larger trends (secular trends), but the comparison populations could differ from study populations in several ways that might be relevant to the risk of exposure to secondhand smoke and to the incidence of acute cardiovascular events. This would be observed in the pre-ban comparison and would add uncertainty to the results.
A before–after comparison is useful if data on individuals are collected. If, instead, grouped population data are used in a before–after comparison, one would need to be assured that there is little mobility. Moreover, if there are other communitywide changes related to tobacco, such as a concurrent antitobacco advertising campaign, a before–after design will be less able to assess the effect of the ban independently of the other changes; a comparison with an external comparison group (not subject to a ban) may be of value so that concurrent changes can be accounted for. However, the fact that multiple studies that used internal or external control groups have found associations between smoking bans and a decrease in acute MI provides stronger evidence that the association is real and not an artifact related to the control population used.
Smoking Bans
In the 11 key reports reviewed by the committee, the effects of the interventions and the effects of events that occurred concurrently with them cannot be separately identified. Some of the studies attempted to quantify or catalog other activities that took place at the time of a smoking ban, but because the relative effects of the different activities on smoking behavior and exposures are unknown and because the activities were not independent, the committee could not attribute changes in the incidence of acute myocardial infarction (MI) to a particular aspect of a ban. The committee’s conclusions are therefore based on whatever changes occurred at the time of the smoking bans and not on legislation itself.
The bans themselves were of varied scope (for example, they covered different types of sites or venues), enforcement of bans has varied, and other interventions often occurred concurrently, such as smoking-cessation and education efforts. As can be seen in Table 6-1, however, most of the bans covered workplaces, including private offices, restaurants, and bars. That could have an effect on the changes in secondhand-smoke exposure in that people could spend about 8 hours or more each day at work compared with typically many fewer hours in restaurants or bars.
In the studies reviewed in Chapter 6 there is an attempt to define clearly the specific time at which an intervention occurred. As discussed in Chapter 5, however, smoking bans typically do not occur in a vacuum, so the results of the studies need to be interpreted in the context of all activities that occurred before, after, and at the time of a legislated ban—such as public debate on the law, educational campaigns, voluntary bans in households, and increased support for smoking cessation—and not just in terms of the regulation that was implemented. For example, voluntary bans or other smoking restrictions might precede a legislated ban. The fact that other activities occurred at the same time need not weaken a study, but it can limit the conclusions that can be drawn with respect to what caused observed effects. That is, decreases in adverse health effects that occur with the implementation of a ban cannot necessarily be attributed to the specific legislation; other activities, such as voluntary bans in households or outreach programs, could underlie the effects.
Exposure Assessment
To address its charge, the committee must consider the effects of smoking bans and the effects of decreases in secondhand-smoke exposure. To do that, the committee assessed the studies to determine whether changes related to the bans are a result of changes in secondhand-smoke exposure. Ideally, in assessing the impact of a change in exposure to secondhand
smoke, the size of the change in exposure would be measured to determine whether there is a dose–response relationship. Most of the key intervention studies raise two issues with regard to exposure assessment: a lack of information on the smoking status of the people with reported cases of acute MI and a lack of information on changes in secondhand-smoke exposure.
After a smoking ban is implemented, many smokers quit or decrease the number of cigarettes they smoke, and in the absence of data on smoking status it is difficult to separate a decrease in the number of cases of acute MI due to decreased exposure of nonsmokers to secondhand smoke from a decrease in the number of cases of acute MI due to decreased smoking by smokers. Two of the publications have information on the smoking status of people who had acute MI and analyzed the effects on nonsmokers. Seo and Torabi (2007) limited their study to acute MI patients who were nonsmokers, so observed decreases in acute MI are due to decreases in secondhand-smoke exposure. Pell et al. (2008) measured serum cotinine in nonsmokers, so they could draw conclusions about changes in secondhand-smoke exposure at the time of implementation of the ban rather than having to study the effect of the implementation of a smoking ban itself.
The relationship between smoking bans and decreases in air concentrations of secondhand smoke depends on the concentration of secondhand smoke in the air before the ban, the extent of the ban, and how well the ban is enforced and complied with. None of the key publications, however, contains information on the duration or pattern of exposure of individuals to secondhand smoke. That is, there is no information on how long or how often individuals were exposed before or after implementation of the smoking bans. For example, it is not known whether individuals were exposed to high concentrations sporadically for short periods or to low concentrations more consistently or both. Without that information, the committee could not determine whether acute exposures were triggering acute coronary events, chronic exposures were causing continuing damage that eventually resulted in acute coronary events, or a combination of chronic damage and acute exposure led to acute coronary events.
Although many of the key publications do not contain air-monitoring or biomarker data to assess the changes in secondhand smoke after ban implementation, other publications on the implementation of smoking bans, either in the regions examined in the key studies or in other regions, show that secondhand smoke decreases after implementation of a ban (see Chapter 2), and the committee concluded that generally the implementation of a smoking ban is associated with decreased air concentrations of secondhand smoke. Secondhand smoke reductions in the venues covered by the bans typically ranged from 50 to 90%. In addition, Pell et al. (2008) did measure serum cotinine in all acute MI cases reported and found that exposures decreased after implementation of a smoking ban.
There is information on compliance and enforcement of the eight smoking bans examined in the 11 key studies. Available data indicate compliance or a decrease in markers of secondhand smoke after the implementation of smoking bans in general but not for the specific study populations in the key publications in Italy (Gallus et al., 2006; Gorini et al., 2005; Valente et al., 2007), New York state (CDC, 2004, 2007; RTI International, 2004), and Scotland (Haw and Gruer, 2007; Menzies et al., 2006; Pell et al., 2008; Semple et al., 2007a, 2007b). Although no data on air sampling could be found for Helena, Montana; Pueblo, Colorado; and Saskatoon, Canada, data indicated a high degree of compliance with the smoking bans in those locations (Bartecchi et al., 2006; Lemstra et al., 2008; Sargent et al., 2004). There is no information on compliance, enforcement, or air monitoring for secondhand-smoke markers in Monroe County, Indiana. In contrast, air monitoring in Bowling Green, Ohio (Akbar-Khanzadeh et al., 2004) indicated that the magnitude of the decrease in secondhand-smoke markers in air was related to characteristics of the smoking restrictions. The concentration of secondhand-smoke–related compounds was lower in nonsmoking restaurants than in restaurants that permitted smoking in separate rooms.
On the basis of those data, the committee concludes that, with the exception of some establishments in Bowling Green, Ohio, the smoking bans evaluated in the key studies appear to have resulted in a large decrease in potential exposure to secondhand smoke. Decreases in acute MIs were seen in the two studies that evaluated effects only in nonsmokers (Pell et al., 2008; Seo and Torabi, 2007). Given those two facts, decreases in secondhand-smoke exposure likely contribute to the decreases in acute MIs after implementation of smoking bans seen in the studies that looked at the overall population (smokers and nonsmokers). The portion of the decrease in acute MIs that can be attributed specifically to changes in secondhand-smoke concentration, however, cannot be determined on the basis of the available data.
Outcomes
The key studies varied on the outcomes they examined. Some assessed changes in morbidity, others mortality, and others both. Morbidity and mortality from acute coronary events should be used as outcomes in considering the effect of a smoking ban. For mortality, ideally there would be autopsy confirmation of all deaths that might be due to acute coronary events; however, the larger the study, the less feasible that is. Short of that, medical records and other information could be reviewed independently to confirm the cause of death (not only for those coded as acute coronary events but for those not so coded but possibly acute coronary events nonetheless). For morbidity, there should be independent clinical confirmation,
through review of medical charts and perhaps other information, that cases meet standardized criteria, such as those recommended by the World Health Organization (WHO) or others that take into consideration electrocardiography, biomarkers of cardiac damage, and pain. It is necessary, in the case of both mortality and morbidity, that International Classification of Diseases (ICD) guidelines be followed rigorously in identifying underlying causes of death and morbidity as opposed to merely abstracting the bottom line on the hospital discharge or the death certificate.
Surveillance studies rely heavily on the use of a standardized system for classification of diseases, ICD, issued by WHO. Most countries use that system in connection with hospitalizations as well as deaths. The United States, uniquely, uses a modification of the system, the ICD-Clinical Modification (ICD-CM), to classify diagnostic information from medical records and for medical reimbursement. ICD-CM is more detailed, using an additional (fifth) coding digit. The ICD system is revised about every 10 years, and both ICD-9 and ICD-10 were in use in some countries in the key studies under review.1
Regardless of whether ICD-9 or ICD-10 is used, physicians and others typically list all causes of death and list the underlying cause of death last on the death certificate.2 Regardless of the ICD code, that is often done incorrectly; coders using death certificates for gathering statistics are directed in the ICD rules to select the listed underlying cause of death only if it could have given rise to all the other conditions listed as among the causes of death. Otherwise, they are to determine a logical sequence of events that could have led to death and select the underlying cause of the sequence, disregarding “ill-defined conditions.” In that respect, a change between ICD-9 and ICD-10 is of potential relevance to this review: in ICD-10, for the first time, the diagnosis “cardiac arrest, unspecified,” I46.9, is regarded as ill-defined. In addition, what was a single code for acute MI in ICD-9 (410) is expanded in ICD-10 to six codes (I21.0–I21.4 and I21.9) that specify the site of MI. According to an analysis by the National Center for Health Statistics, the switch from ICD-9 to ICD-10 resulted in small but significant decreases in coding of cause of death as heart diseases in
general and acute MI in particular in the United States (Anderson et al., 2001); reporting of deaths as due to acute MI decreased by 10% in England and Wales (Griffiths et al., 2004) and decreased by 0.6% in Spain (Cirera Suarez et al., 2006).
Classification of deaths as acute coronary events on death certificates, regardless of whether ICD-9 or ICD-10 is used, poses general methodologic issues. On the one hand, a number of investigators have found that the numbers of such diagnoses are quite consistent over time (Goldacre et al., 2003; Mahonen et al., 1997; Pajunen et al., 2005). On the other hand, it was found in Finland that there was considerable variation among geographic areas and levels of care (for example, in local versus central hospitals) (Mahonen et al., 1997). Of more concern is the overall accuracy of physician-based determinations of cause of death in the absence of autopsies and the very low rate of autopsies performed, particularly in the United States (Kircher et al., 1985). Specifically, for deaths from acute MI, a hospital-based autopsy case series identified substantial discrepancies (48% were missed) between autopsy-proven diagnoses and death certificates (Ravakhah, 2006). A study in Australia also identified high rates of missed cases of acute coronary events in the absence of autopsy (Nashelsky and Lawrence, 2003). In considering the effect of such misdiagnoses in the 11 key studies, however, differences in accuracy over time or between locations (for example, between the study county and a comparison county) would be of most concern.
The diagnosis of acute coronary events at hospital discharge can also be problematic. The switch from ICD-9 to ICD-10 changed how repeated hospitalizations are coded, that is, whether a person who was admitted to the hospital with a diagnosis of an acute coronary event multiple times during the course of a study would be counted multiple times in the study. Counting multiple admissions for the same person’s acute coronary events as though the admissions were of different persons might bias findings. ICD-9 classifies the diagnosis according to the first or later visit for treatment of a particular MI on the basis of the site of the MI (for example, ICD-9 410.12 is the code for acute MI; other anterior wall; subsequent episode of care). ICD-10 uses the term subsequent to refer to an MI within 4 weeks of a previous one regardless of the site.
In general, multiple studies have demonstrated that there are inaccuracies in the diagnosis of acute coronary events in medical records. A recent ecologic study in Texas found that only 401 of 496 cases of “definite myocardial infarction” met diagnostic criteria3 for acute MI developed by the
Cardiovascular Community Surveillance Program (CCSP) (Pladevall et al., 1996).
To complicate the issue, there have been other changes in diagnostic criteria for acute coronary events over the past decade. Serial measures of biomarkers of cardiac damage have been incorporated into the revised 2003 case definition from the American Heart Association (AHA) and a number of international associations (Luepker et al., 2003). Assays that measure serum concentrations of two isoforms of cardiac troponin, cardiac troponin I (cTnI) and cardiac troponin T (cTnT), are now used in the case definition of acute coronary events.4 Those assays are the most specific clinically available markers of acute coronary events. In relation to the key studies reviewed by the committee that only changes in diagnostic criteria that occurred during the timeframe of the study would affect the results of the study, and would only be relevant to studies that compared the same region before and after a smoking ban. All the key studies compare acute MIs before and after the ban, and the timeframes of all but two of the key studies (Barone-Adesi et al., 2006; Pell et al., 2008) include 2003, the time at which the case definition changed. Three of the studies include comparison populations (Lemstra et al., 2008; Pell et al., 2008; Sargent et al., 2004), and analyses with the comparison population would not be affected by the change in diagnostic criteria. It should be noted that a recent study showed that, compared with the earlier 1994 WHO MONICA (Multinational Monitoring of Trends and Determinants in Cardiovascular Disease) definition, the 2003 AHA case definition would increase the diagnosis of acute coronary events substantially (by 62–84%) if serum troponin were measured with sensitive assays (Kavsak et al., 2006). The changes in the criteria for an acute MI would be expected to increase reporting of acute MIs in later years, making a decrease in events after the smoking ban more difficult to detect. Despite that potential difficulty in detecting the decrease, the studies that looked at acute MI over time observed significant decreases (Bartecchi et al., 2006; CDC, 2009; Cesaroni et al., 2008; Juster et al., 2007; Khuder et al., 2007; Vasselli et al., 2008).
Time to Effect
The issue of the interval between an intervention (implementation of a smoking ban) and a change in the rate of acute coronary events is one of the questions included in the charge to the committee (Question 5) and is
relevant to the committee’s judgment as to the plausibility of a relationship between exposure to secondhand smoke and acute coronary events. The 11 publications differ in the followup time for acute MI. The shortest followup period is 2 months, in one of the Italian reports that demonstrated risk reductions after implementation of a ban (Vasselli et al., 2008). Other studies have looked at up to 6 months after a ban (Barone-Adesi et al., 2006; Sargent et al., 2004), between 6 months and 1 year (Cesaroni et al., 2008; Lemstra et al., 2008; Pell et al., 2008), and from more than 1 to 3 years (Bartecchi et al., 2006; CDC, 2009; Juster et al., 2007; Khuder et al., 2007; Seo and Torabi, 2007). Table 7-2 presents the periods examined in the publications and the risk reductions associated with them. As can be seen from that table, a small decrease in acute MIs—6.4% from the previous year and an estimated 13.1% from what was expected on the basis of linear regression (relative risk, 0.87; 95% confidence interval [CI], 0.84–0.93)—occurred as early as 2 months after implementation in Italy (Vasselli et al., 2008). According to Table 7-2, although there are many
TABLE 7-2 Followup Periods of Studies (listed from shortest to longest followup)
|
Publication (Region) |
Followup Perioda |
Decrease in Admission Rates |
|
Vasselli et al., 2008 (Four regions in Italy)b |
0–2 months |
6.4% decrease from 2004 to 2005 13.1% decrease (estimated) from expected based on linear regression (RR, 0.87; 95% CI, 0.84–0.93) |
|
Sargent et al., 2004 (Helena, Montana) |
0–6 months |
40% decrease in average monthly admissions (from 40 to 24; 95% CI, decrease of 0.3−131.7%) |
|
Barone-Adesi, 2006 (Piedmont region, Italy)b |
0–5 months |
11% decrease in those under 60 years old (RR, 0.89; 95% CI, 0.81–0.98) in February–June 2004 |
|
Pell et al., 2008 (Scotland) |
0–10 months |
17% decrease (95% CI, 16–18%) after implementation of smoking ban |
|
Cesaroni et al., 2008 (Rome, Italy)b |
0–12 monthsc |
11% decrease in 35- to 64-year-olds (RR, 0.89; 95% CI, 0.85–0.93); 8% decrease in 65- to 74-year-olds (RR, 0.92; 95% CI, 0.88–0.97) |
|
Publication (Region) |
Followup Perioda |
Decrease in Admission Rates |
|
Lemstra et al., 2008 (Saskatoon, Canada) |
0–12 months |
13% decrease (rate ratio, 0.87; 95% CI, 0.84–0.90) |
|
Khuder et al., 2007 (Bowling Green, Ohio)d |
9–21 months |
39% decrease in annual admission rates (95% CI, 33–45%) in 2002 (includes 2 months without ordinance)e |
|
Bartecchi et al., 2006 (Pueblo, Colorado) |
0–18 months |
27% decrease in hospitalizations (acute MIs/100,000 person-years) (RR, 0.73; 95% CI, 0.63–0.85) |
|
Seo and Torabi, 2007 (Monroe County, Indiana) |
0–22 months |
70% decrease in 2-year admissions (from 17 to 5 cases; decrease of 12 cases, 95% CI, 2.81–21.19) |
|
Juster et al., 2007 (New York state) |
5–17 monthsf |
8% (estimated) fewer admissions in 2004 than expected with just local smoking bans implemented; 19% (estimated) fewer admissions in 2004 than expected if prior smoking bans had not been in effect |
|
CDC, 2009 (Pueblo, Colorado)g |
18–36 months |
41% decrease (RR, 0.59; 95% CI, 0.49–0.70) |
|
Khuder et al., 2007 (Bowling Green, Ohio)d |
34–39 months |
47% decrease in admission rates (95% CI, 41–55%) |
|
Abbreviations: CI, confidence interval; MI, myocardial infarction; RR, relative risk. a Period for which data were analyzed. Implementation of ban is at month zero. All periods are expressed in months. For some regions the ban was implemented for a part of a month. In those cases the exact dates of the study are footnoted. b The four regions analyzed by Vasselli et al. (2008)—Piedmont, Friuli–Venezia–Giulia, Latium, Campania—contain areas analyzed by Barone-Adesi et al. (2006) and Cesaroni et al. (2008). c Smoking ban was not implemented until January 10, 2005, so followup period is actually 10 days less than 1 year. d Khuder et al. (2007) reported results at two times. Data were not analyzed for first 6 months after ban was implemented, to allow time for enforcement and compliance. e Significant decrease in trend (parameter representing change in series level, ω = −1.69; p = 0.04) in monthly series rate starting 7 months after full implementation and enforcement (November 2002). f Smoking ban was implemented July 24, 2003, so the followup period is actually from 5 months and 7 days to 17 months and 6 days. g Same study population as Bartecchi et al. (2006). |
||
uncertainties in and variability among the different studies, the decreases in general appear to be larger with longer followup periods. The committee did not conduct any analyses to assess whether there are differences with different periods. However, data presented to the committee by Dr. Stanton Glantz demonstrated a relationship between study length and magnitude of risk reduction (personal communication, Stanton Glantz, University of California, San Francisco School of Medicine, January 30, 2009).5
The time between an intervention and its effect is difficult to determine when there is no precise date of the intervention. As discussed previously for smoking bans, many activities occur before and around the time of implementation of legislation. Those activities could result in changes in smoking behaviors before the ban was implemented, blurring the timing of the intervention (for example, whether the intervention occurs when the legislation is implemented or whether the intervention occurs when a public discussion about a ban begins). Improved compliance with the ban over time or use of a phase-in period could also delay the effective date of the full intervention, further blurring its timing.
Some of the studies indicate that an effect was seen as early as within 2 months of the implementation of a smoking ban (Vasselli et al., 2008). The majority of the studies show effects within months of implementation. However, given the blurred timing of the interventions and the numerous differences among the studies—such as in the characteristics of the smoking bans, in the implementation of smoking restrictions or bans before implementation of the bans under study, and in background rates of smoking and acute MIs—the key intervention studies do not provide strong evidence on which to establish a more precise time between an intervention and a decrease in risk of acute MI.
Plausibility
As the key studies showing reductions in acute MIs after implementation of smoking bans were published, some skepticism was expressed as to the believability or likelihood of the effects, whether a detectable change in heart attacks could possibly be associated with banning smoking in public places and offices, and whether the magnitude of the effect could be as high as seen in some of the studies. The committee considered two aspects of plausibility: the biologic plausibility of the effect and the plausibility of the magnitude of the effect.
Biologic Plausibility of an Effect
The committee reviewed the pathophysiologic data on secondhand smoke and its components to evaluate whether there are biologic modes of action by which secondhand smoke could have cardiovascular events and, in particular, whether the absence of exposure to secondhand smoke could be associated with a decrease in acute MIs. Chapter 3 reviews the effects of secondhand smoke and its components on the cardiovascular system. Experimental studies have been conducted in humans, in animals, and in cell preparations to look at end points that are related to cardiovascular disease. Experimental studies of secondhand smoke and some of its components, including particulate matter (PM), demonstrate that they exert substantial cardiovascular toxicity. The toxicologic effects include endothelial dysfunction, increased thrombosis, inflammation, and adversely affected plaque stability; all these phenomena are on the pathway to acute MI. The pathophysiologic results are consistent with the results of the key ecologic studies, especially the two studies that looked at effects in nonsmokers, which show the rate of acute MI decreasing with a decrease in secondhand-smoke exposure; however, the ecologic studies do not (and cannot) address timeframes of less than 1 month. The data support a role of secondhand smoke as a potential causative agent in acute coronary events, that is, they constitute evidence that it is biologically plausible for secondhand smoke to be a causative agent in cardiovascular disease and acute coronary events.
Plausibility of Magnitude of an Effect
When considering the plausibility of the magnitude of the effect, the committee looked at the effects seen in the studies that examined the effects of secondhand smoke and the implementation of smoking bans compared with studies that examined the effects of smoking, and with studies that examined the effects of PM in air pollution.
Comparison with Data on Smokers. One aspect of the plausibility of an effect of secondhand smoke that is often questioned is the size of the effect relative to the size of the effect of smoking, especially in light of the fact that smokers also inhale secondhand smoke. The epidemiologic studies reviewed in this report show a decrease of about 6–47% in the risk of acute MI after implementation of a smoking ban (Barone-Adesi et al., 2006; Bartecchi et al., 2006; CDC, 2009; Cesaroni et al., 2008; Juster et al., 2007; Khuder et al., 2007; Lemstra et al., 2008; Pell et al., 2008; Sargent et al., 2004; Seo and Torabi, 2007; Vasselli et al., 2008); an increase in the odds ratio (OR) of 1.24 (95% CI, 1.17–1.32) to 1.62 (95% CI, 1.45–1.81) for secondhand-smoke exposure for 1–7 hours/week and at least 22 hours/week, respec-
tively, in the INTERHEART case–control study (Teo et al., 2006); and a nonsignificant OR of 1.19 (95% CI, 0.78–1.82) for the highest tertile of lifetime cumulative exposure compared with the lowest tertile of lifetime cumulative exposure (Stranges et al., 2006). It should be noted, however, that cumulative lifetime exposure may not be the appropriate exposure metric for the relationship between secondhand-smoke exposure and acute MI. In fact, the observed reduction in acute MI within a year of smoking bans indicates that recent exposure is more relevant. Such an interpretation is supported by the pathophysiologic responses to a 30-minute exposure to secondhand smoke (see Chapter 3). In the INTERHEART study (Teo et al., 2006), the OR for secondhand-smoke exposure (1.24–1.62, depending on the magnitude of exposure) can be compared to an overall OR for smoking of 2.95 (95% CI, 2.77–3.14). In that study, the OR for smoking ranged from 1.63 (95% CI, 1.45–1.82) for smoking one to nine cigarettes per day to 4.59 (95% CI, 4.21–5.00) for smoking 20 or more cigarettes per day. Regression analysis indicates that the risk of developing acute MI increases by 1.056 (95% CI, 1.05–1.06) for every additional cigarette smoked per day (Teo et al., 2006). Therefore, the increase in risk of acute MI associated with secondhand-smoke exposure in the case–control studies and the decrease in risk of acute MI seen after implementation of smoking bans are about the same or smaller than those seen with a low level of current smoking and substantially smaller than those seen with current heavy smoking. In looking at smoking cessation and the decrease in risks, the INTERHEART study showed that the risk of acute MI in those who quit smoking 1–3 years earlier decreased to 1.87 (95% CI, 1.55–2.24) and continued to decrease with time; some risk remained, however, even years after cessation smoking (Teo et al., 2006).
Comparison with Data on Particulate Matter in Air Pollution. PM is a major component of secondhand smoke (see Chapter 2). The composition of PM, including particle size, can affect its toxicity and is different between secondhand smoke and air pollution and between air pollution from different sources (Dockery, 2009). Both secondhand smoke and air pollution contain fine and ultrafine PM, so the committee conducted some analyses to compare the effects seen in the key studies with those seen in response to the PM in air pollution. Although the two types of PM differ in some characteristics, the committee concluded that there were enough similarities between the PM2.5 (PM with an aerodynamic diameter of less than 2.5 μm) in secondhand smoke and that in ambient air pollution to warrant comparison of the magnitudes of the effects of the two. This is not done to estimate the number of people who would have cardiovascular effects because of the PM in secondhand smoke but rather serves as a “reality
check” on the numbers that were seen in the key epidemiologic studies related to smoking bans.
The committee developed several scenarios of exposure to PM2.5 concentrations that represent lower or higher exposures to secondhand smoke and estimated the increased risk of and attributable number of hospital admissions for heart failure and cardiovascular disease in a portion of the U.S. population on the basis of the scenarios (see Tables 7-3, 7-4, and 7-5). The estimates used data from Medicare, and so reflect effects only on those ages 65 years or older, are only for a subset of counties in the United States, and are based solely on the cardiovascular effects of PM. Therefore, the estimates do not represent the potential public-health impact of secondhand smoke but are provided to put the decreases in hospital admissions seen in the key studies that evaluated the effect of smoking bans in the context of the health effects of one of the constituents of secondhand smoke.
For each scenario, the committee calculated, on the basis of published data, the daily average concentration of ambient PM2.5. One main source of the exposure data was the 16 Cities Study, in which about 100 people in each of 16 U.S. metropolitan areas wore two personal samplers (one at work for about 8 hours and one when “away from work,” typically at home) that measured several components of secondhand smoke, including respirable particles (measured in that study as PM3.5).6 From the home samples in that study, there were 935 personal samples from people who reported that no one smoked in their homes and the measured nicotine concentrations were under 0.1 μg/m3; they were exposed to respirable particles at an average of 18 µg/m3. There were 372 samples from people who reported that they lived with smokers; they were exposed to an average of PM3.5 at 44 µg /m3. Those values agree well with PM measurements made in randomly selected homes in New York state, where average “respirable suspended particle” concentrations were 15 µg/m3 and 44 µg/m3 in non-smoking and smoking homes, respectively (Leaderer and Hammond, 1991). There were 768 samples from workers who reported that smoking was not allowed in their workplaces and the measured nicotine concentrations were under 0.1 µg/m3. They were exposed to PM3.5 at an average of 16 µg/m3. The 355 workers who reported that smoking was allowed in their workplaces and who had observed someone smoking on the day of the sampling
were exposed to PM3.5 at an average of 50 µg/m3. The PM concentrations used for the various venues were as follows:
TABLE 7-3 Estimates of Increased Risk of Cardiovascular Disease and Annual Reduction in Hospital Admissions for Cardiovascular Disease with Changes in Particulate-Matter Exposuresa
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Cardiovascular Diseasec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
Nonsmoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
16.3 (33) |
1.15 (0.73, 1.56) |
10,470 (6,622, 14,185) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
64.0 (81) |
4.54 (2.88, 6.14) |
41,942 (26,362, 57,170) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
3.0 (20) |
0.21 (0.13, 0.28) |
1,897 (1,202, 2,566) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (93) |
5.40 (3.42, 7.30) |
50,021 (31,389, 68,286) |
|
Smoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
27.6 (45) |
1.96 (1.24, 2.65) |
17,843 (11,269, 24,210) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
75.3 (92) |
5.35 (3.39, 7.23) |
49,570 (31,109, 67,665) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
14.3 (31) |
1.01 (0.64, 1.37) |
9,201 (5,821, 12,464) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
87.5 (105) |
6.21 (3.94, 8.40) |
57,828 (36,233, 79,060) |
|
Nonsmoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
14.5 (50) |
1.03 (0.65, 1.39) |
9,336 (5,906, 12,647) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
59.0 (94) |
4.19 (2.66, 5.66) |
38,596 (24,275, 52,576) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
0.7 (36) |
0.05 (0.03, 0.06) |
427 (271, 578) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
64.7 (100) |
4.59 (2.91, 6.21) |
42,389 (26,640, 57,784) |
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Cardiovascular Diseasec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
Smoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 µg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
25.8 (61) |
1.83 (1.16, 2.48) |
16,701 (10,549, 22,655) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
70.3 (105) |
4.99 (3.17, 6.75) |
46,197 (29,012, 63,021) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
12.0 (47) |
0.85 (0.54, 1.15) |
7,720 (4,885, 10,454) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (111) |
5.40 (3.42, 7.30) |
50,021 (31,389, 68,286) |
|
a Committee calculated changes in particulate-matter exposures for different exposure scenarios and estimated corresponding changes in risk of cardiovascular-disease admissions due to those changes and corresponding reductions in annual hospital admissions in 204 largest urban counties on basis of hospital admissions data from U.S. Medicare database. b Daily exposure to particulate matter in addition to the reference concentration. c Increased risk calculated by using relative-risk estimate of 0.71 (95% CI, 0.45–0.96; Lag = 0) per 10-µg/m3 increase in PM2.5. Increased risk estimate is based on data from Peng et al. (2008). d Changes in number of hospital admissions is based on Medicare data from 204 largest urban counties, which has a total of 11.5 million Medicare enrollees. |
|||
pubs and bars,7 400 µg/m3 (Akbar-Khanzadeh et al., 2004; CDC, 2004; Ellingsen et al., 2006; Lofroth and Lazaridis, 1986; Semple et al., 2007b; Valente et al., 2007); restaurants,8 200 µg/m3 (Alpert et al., 2007; Ellingsen et al., 2006; Valente et al., 2007); bowling alleys, 60 µg/m3 (CDC, 2004); pool halls and video-game arcades, 150 µg/m3 (CDC, 2004); bingo parlors, 400 µg/m3 (CDC, 2004; Kado et al., 1991); casinos, 200 µg/m3 (Kado et al., 1991); and nonsmoking establishments or venues, 20 µg/m3.
Total average 24-hour PM2.5 exposure was estimated by assuming
TABLE 7-4 Estimates of Increased Risk of Ischemic Heart Disease and Annual Reduction in Hospital Admissions for Ischemic Heart Disease with Changes in Particulate-Matter Exposuresa
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Heart Failurec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
Nonsmoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
16.3 (33) |
2.19 (1.23, 2.94) |
5,498 (3,570, 7,399) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
64.0 (81) |
8.64 (5.63, 11.58) |
22,368 (14,360, 30,442) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
3.0 (20) |
0.40 (0.26, 0.54) |
992 (646, 1,331) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (93) |
10.26 (6.69, 13.76) |
26,781 (17,144, 36,553) |
|
Smoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
27.6 (45) |
3.72 (2.43, 4.99) |
9,404 (6,090, 12,689) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
75.3 (92) |
10.17 (6.63, 13.64) |
26,534 (16,989, 36,210) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
14.3 (31) |
1.93 (1.26, 2.59) |
4,829 (3,137, 6,495) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
87.5 (105) |
11.81 (7.70, 15.84) |
31,078 (19,840, 42,535) |
|
Nonsmoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
14.5 (50) |
1.96 (1.28, 2.62) |
4,900 (3,183, 6,591) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
59.0 (94) |
7.97 (5.19, 10.68) |
20,550 (13,209, 27,935) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
0.7 (36) |
0.09 (0.06, 0.12) |
223 (145, 299) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
64.7 (100) |
8.73 (5.69, 11.70) |
22,611 (14,514, 30,778) |
|
Smoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
25.8 (61) |
3.49 (2.27, 4.68) |
8,797 (5,699, 11,865) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
70.3 (105) |
9.50 (6.19, 12.73) |
24,688 (15,826, 33,651) |
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Heart Failurec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
12.0 (47) |
1.62 (1.06, 2.17) |
4,048 (2,631, 5,443) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (111) |
10.26 (6.69, 13.76) |
26,781 (17,144, 36,553) |
|
a Committee calculated changes in particulate-matter exposures for different exposure scenarios and estimated corresponding changes in risk of ischemic heart disease due to those changes and corresponding reductions in annual hospital admissions in 204 largest urban counties on basis of hospital admissions data from U.S. Medicare database. b Daily exposure to particulate matter in addition to the reference concentration. c Increased risk calculated by using a relative-risk estimate of 0.25 (95% CI, −0.12 to 0.62; Lag = 0) per 10-μg/m3 increase in PM2.5. That increased risk estimate is based on data from Peng et al. (2008). d Changes in number of hospital admissions is based on Medicare data from 204 largest urban counties, which has a total of 11.5 million Medicare enrollees. |
|||
that people spent 8 hours at work, a varied number of hours in the different public venues, and the remaining 9–16 hours at home or, if they were retired, a varied number of hours in the different public venues and the remaining hours at home. In its calculations, the committee also assumed that smoking bans did not affect home exposures. Reductions in 24-hour average PM2.5 exposures (from pre–smoking ban concentrations in workplaces and public venues) were calculated separately for those living with smokers and those who lived in homes without any smoking (see Tables 7-3, 7-4, and 7-5).
The committee assumed that the PM2.5 concentrations correlate with the concentrations of secondhand-smoke exposure in various venues. For each scenario, it calculated the difference in 24-hour average PM2.5 exposure that would result from smoking bans for those who lived with smokers and for those who lived in smoke-free homes. The committee used data on changes in daily exposure to PM2.5 and cardiovascular diseases from epidemiologic studies of the Medicare population (which includes only people at least 65 years old) and extracted the percentage increases in the risk of emergency hospital admissions for all cardiovascular diseases (Table 7-3), ischemic heart disease (Table 7-4), and heart failure (Table 7-5) associated with a 10-μg/m3 reduction in PM2.5 (Peng et al., 2008). For example, Peng et al. (2008) reported that, for the population over 65 years old living in
TABLE 7-5 Estimates of Increased Risk of Heart Failure and Annual Reduction in Hospital Admissions for Heart Failure with Changes in Particulate-Matter Exposuresa
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Heart Failurec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
Nonsmoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
16.3 (33) |
2.19 (1.23, 2.94) |
5,498 (3,570, 7,399) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
64.0 (81) |
8.64 (5.63, 11.58) |
22,368 (14,360, 30,442) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
3.0 (20) |
0.40 (0.26, 0.54) |
992 (646, 1,331) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (93) |
10.26 (6.69, 13.76) |
26,781 (17,144, 36,553) |
|
Smoking workplace, nonsmoking home (reference concentration, assuming 16 h at home, 17 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
27.6 (45) |
3.72 (2.43, 4.99) |
9,404 (6,090, 12,689) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
75.3 (92) |
10.17 (6.63, 13.64) |
26,534 (16,989, 36,210) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
14.3 (31) |
1.93 (1.26, 2.59) |
4,829 (3,137, 6,495) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
87.5 (105) |
11.81 (7.70, 15.84) |
31,078 (19,840, 42,535) |
|
Nonsmoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
14.5 (50) |
1.96 (1.28, 2.62) |
4,900 (3,183, 6,591) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
59.0 (94) |
7.97 (5.19, 10.68) |
20,550 (13,209, 27,935) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
0.7 (36) |
0.09 (0.06, 0.12) |
223 (145, 299) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
64.7 (100) |
8.73 (5.69, 11.70) |
22,611 (14,514, 30,778) |
|
Smoking workplace, smoking home (reference concentration, assuming 16 h at home, 35 μg/m3) |
|||
|
8 h at work; 15 h at home; 1 h at pub or bar |
25.8 (61) |
3.49 (2.27, 4.68) |
8,797 (5,699, 11,865) |
|
8 h at work; 12 h at home; 4 h at pub or bar |
70.3 (105) |
9.50 (6.19, 12.73) |
24,688 (15,826, 33,651) |
|
Exposure Scenario |
Additional Exposure (Total Exposure), μg/m3b |
Increased Risk of Heart Failurec (Lower Estimate, Upper Estimate) |
Annual Reduction in Hospital Admissionsd (Lower Estimate, Upper Estimate) |
|
8 h at work; 14.5 h at home; 1.5 h at bowling alley |
12.0 (47) |
1.62 (1.06, 2.17) |
4,048 (2,631, 5,443) |
|
8 h at work; 6 h at home; 2 h at pub or bar |
76.0 (111) |
10.26 (6.69, 13.76) |
26,781 (17,144, 36,553) |
|
a Committee calculated changes in particulate-matter exposures for different exposure scenarios and estimated corresponding changes in risk of heart failure due to those changes and corresponding reductions in annual hospital admissions in 204 largest urban counties on basis of hospital admissions data from U.S. Medicare database. b Daily exposure to particulate matter in addition to the reference concentration. c Increased risk calculated by using relative-risk estimate of 1.35 (95% CI, 0.88–1.81; Lag = 0) per 10-μg/m3 increase in PM2.5. That increased risk estimate is based on data from Peng et al. (2008). d Changes in number of hospital admissions is based on Medicare data from 204 largest urban counties, which has a total of 11.5 million Medicare enrollees. |
|||
the largest 204 urban counties in the United States (which contain about 12 million people, or one-fourth of the U.S. population), a daily increase in ambient PM2.5 of 10 μg/m3 is associated with an increase in the number of emergency hospital admissions for cardiovascular disease on a given day of 0.71% (95% CI, 0.45–0.96%). The corresponding increase in the number of admissions for ischemic heart disease is 0.25% (95% CI, −10.12 to 0.62%) and for heart failure 1.35% (95% CI, 0.88–1.81%).
The committee applied the calculated percentage increase in risk to the daily changes in PM2.5 that occurred from secondhand-smoke exposures outside the home, that is, when a person worked where smoking occurred or spent time in a venue with smoking, such as a restaurant, bar, or casino. For each scenario, two comparison populations were evaluated: those who did not live with smokers and those who lived with smokers. The baseline for each was no other secondhand-smoke exposure, that is, the experience under a strong smoking ban. For example, the first comparison group is a population of nonsmokers who work and live in a nonsmoking environment. They are exposed to a 24-hour average PM2.5 of 17 μg/m3. Without a smoking ban, their daily average PM2.5 exposure might increase to 33 μg/m3 if they spent 1 hour in a pub. By comparing the two populations, the committee found a decrease in daily average PM2.5 exposure of 16
μg/m3 as a result of the smoking ban.9 That decrease is associated with an annual reduction in hospital admissions for all cardiovascular diseases of 10,470 in about 11.5 million Medicare enrollees or, extrapolated to the entire U.S. population, about 40,000 (see Table 7-3). Those estimates indicate that changes in individual PM exposure that would be expected after implementation of smoking bans would be expected to result in substantial reductions in hospital admissions, and this implies that the results seen in the 11 key studies are plausible. Although there is uncertainty in the risk estimates associated with PM, especially for ischemic heart disease, much of the uncertainty is a result of the low numbers of hospital admission per day (and the committee would not necessarily recommend looking at the effects of smoking bans with that method); the analyses are clearly consistent with the magnitude of effects observed in the smoking-ban studies and strengthen confidence in the validity of the studies.
Analytic Issues
The studies used different analytic approaches; the most common was to estimate rate ratios, that is, to divide an admission rate after implementation of a ban by the admission rate before the ban. Some studies also used regression models to estimate age- and sex-adjusted rates of acute coronary events from monthly time-series data. Many of the analyses did not adjust for seasonality although some used data from the same months before and after implementation of a ban to control for seasonal differences.
Statistical analyses should be planned a priori. All planned analyses should be conducted and their results reported, and they should account for seasonality. Some of the epidemiologic studies of smoking bans and acute cardiovascular diseases used “interrupted time-series analysis methods” to estimate the effect of smoking bans on rates of hospital admissions for cardiovascular diseases. Those studies specify a regression model that includes several terms to account for different types of temporal confounding (such as seasonality and underlying trends). As is common in epidemiologic analysis of observational data, the results might be sensitive to the specification of the regression model and, more specifically, to the extent of control of unmeasured temporal confounding.
In this section, the committee examines the sensitivity of the results to the specification of the regression model in “interrupted time-series analysis methods” used in the studies of the public-health implications of smoking bans. The committee constructed a data set by using Medicare billing claims data for a population of elderly people. It constructed county-level age-adjusted monthly hospital admission rates for acute MI for the period
1999–2006 for the same 62 New York counties analyzed by Juster et al. (2007). This analysis does not replicate that of Juster et al. but illustrates the effect that model choice can have on results.
The committee used a Poisson regression model in which the outcome is the monthly number of hospital admissions for a given age group; the committee considered three age groups: 65–74 years, 75–84 years, and 85 years and over. The model included the following covariates:
-
The natural logarithm of the number of the monthly Medicare enrollees in each age group (offset).
-
A linear time-trend variable (month) to quantify changes in treatment, population risk factors, and other secular trends.
-
A binary variable to capture the main effect of the instantaneous change in rates of hospital admission at the time of the smoking-ban implementation (July 24, 2003); equal to zero before implementation and equal to 1 after implementation.
-
The interaction between the binary variable (representing the ban) and time; this analysis allows predicted hospital admission rates to continue to decline (or increase) linearly with time after implementation.
-
A county indicator to account for differences among counties in average rates of hospital admissions.
-
Interactions between county and time to control for county-specific secular changes; this analysis allows each county to have its own predicted linear trend.
-
Indicator variables of month of year to control for seasonality.
The committee assessed the sensitivity of the results to the regression model by using the following four scenarios:
Scenario 1 assumed that the underlying trend, common to all the counties, is linear for the entire period 1999–2006.
Scenario 2 assumed that the underlying trend, common to all the counties, is a spline with 3 degrees of freedom for the entire period 1999–2006.
Scenario 3 assumed that the underlying trend, common to all the counties, is linear for the entire period 1999–2006 (as in Scenario 1) but fitted the regression model to the data from before implementation of a smoking ban and predicted the outcome after implementation.
Scenario 4 assumed that the underlying trend, common to all the counties, is a spline with 3 degrees of freedom for the entire period 1999–2006 (as in Scenario 2) but fitted the regression model to the data from be-
fore implementation of a smoking ban and predicted the outcome after implementation.
Figures 7-1–7-4 show the observed admissions for acute MI and those predicted without the statewide smoking ban under Scenarios 1–4, respectively. Figure 7-5 shows the estimated underlying trend for the whole period when a spline with 3 degrees of freedom was used (Scenarios 2 and 4). Table 7-6 summarizes the point estimates, the 95% CIs, and the p-values of the main effect of the smoking ban and the interaction term between the smoking ban and the linear function of time. The committee estimated these quantities under two regression models defined under Scenarios 1 and 2, which use linear and spline trends, respectively. As can be seen in Table 7-6, the resulting estimate changed from 0.0338 (95% CI, 0.0038–0.057; p = 0.0272) with a linear trend to 0.0503 (95% CI, 0.0110–0.089; p = 0.0122) with a spline trend.
The difference in results between Figure 7-1 and Figure 7-2 depends on the assumption of linearity in the trend in rates of acute MI during the entire study period (Scenario 1). If the assumption of linearity is relaxed, the results change substantially because the committee is estimating the trend for the entire study period, that is, using data from before and after
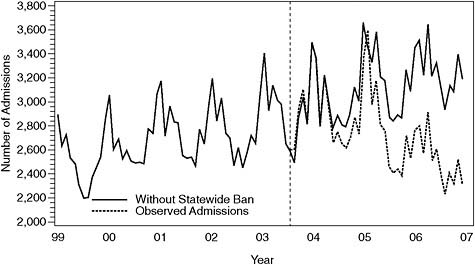
FIGURE 7-1 Observed admissions for acute MI and those predicted without statewide smoking ban on basis of Scenario 1. The dashed vertical line indicates when during 2003 the statewide ban was implemented.
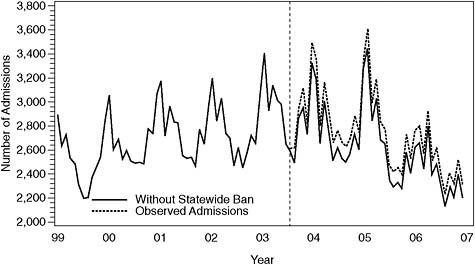
FIGURE 7-2 Observed admissions for acute MI and those predicted without statewide smoking ban on basis of Scenario 2. The dashed vertical line indicates when during 2003 the statewide ban was implemented.
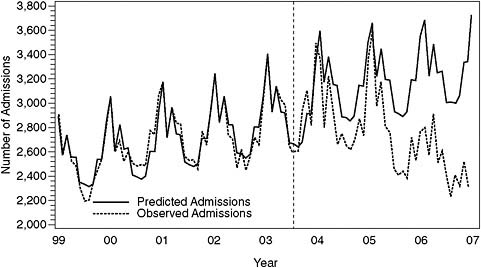
FIGURE 7-3 Observed admissions for acute MI and those predicted on basis of Scenario 3. The dashed vertical line indicates when during 2003 the statewide ban was implemented.
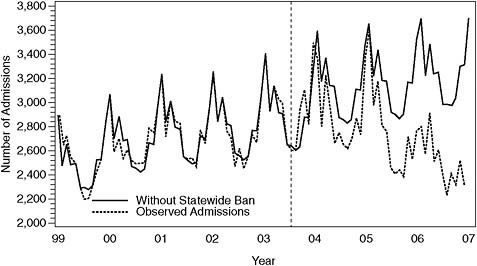
FIGURE 7-4 Observed admissions for acute MI and those predicted on basis of Scenario 4. The dashed vertical line indicates when during 2003 the statewide ban was implemented.
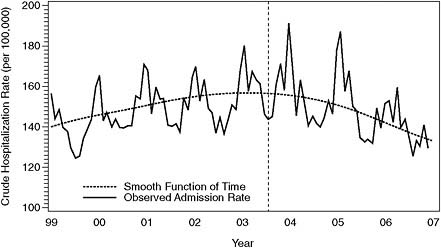
FIGURE 7-5 Crude acute MI hospitalization rate (per 100,000) with smooth function of time using 3 degrees of freedom. The dashed vertical line indicates when during 2003 the statewide ban was implemented.
TABLE 7-6 Summary of Point Estimates, 95% Confidence Intervals, and p-values of Main Effect of Smoking Ban and Interaction Term Between Smoking Ban and Linear Function of Time
|
|
Estimatea |
95% Confidence Interval |
p-value |
|
|
Acute MI scenario 1 |
||||
|
Statewide smoking ban |
0.0338 |
0.0038 |
0.0537 |
0.0272 |
|
Statewide smoking ban by time interaction |
−0.0077 |
−0.0094 |
−0.0059 |
<0.0001 |
|
Acute MI scenario 2 |
||||
|
Estimate of main effect of statewide smoking ban without statewide smoking ban by time interaction |
0.0503 |
0.0110 |
0.0896 |
0.0122 |
|
Estimate of main effect of statewide smoking ban with statewide smoking ban by time interaction. |
0.0706 |
0.0288 |
0.1123 |
0.0009 |
|
Statewide smoking ban by time interaction |
−0.0073 |
−0.0136 |
−0.009 |
0.0248 |
|
a Beta coefficient representing change in hospitalization rate over time after implementation of smoking ban. |
||||
implementation of a ban. Estimates of the trend (both linear and spline) based on only data from before the ban are less sensitive to the parametric specification of the trend. Another important assumption is in the interpretation of the results. In fitting a linear trend, the authors of all the studies assumed that any departure in the observed number of hospital admissions from the linear trend after implementation should be attributed entirely to the ban.
The committee did not explore which model and assumptions are most appropriate but presents this information to examine the effect of model choice. Given that model choice can affect the results substantially, it is important to discuss the rationale for and the sensitivity of the results to the choice of model in publications, especially for more statistically sophisticated analyses.
Publication Bias
The published studies all showed some statistically significant evidence that smoking bans reduced the risk of cardiovascular disease events. There is a possibility that if an investigation shows no reduction or a small re-
duction that is not statistically significant, the investigators will not be motivated to submit the results for publication or, if they do submit them, journal editors will consider such “negative studies” to be of low priority. Those considerations do not invalidate the published studies, but they suggest that a meta-analysis or quantitative estimate based on the published studies might overestimate the effects of smoking bans. The committee tried to identify and seek the results of all studies of the effects of smoking bans on the incidence of cardiovascular disease events. It searched CRISP and ClinicalTrials.gov to determine whether other studies of the effects of smoking bans on acute coronary events had been funded or approved and never published, and it found none. The National Association of City and County Health Officials Web site was also searched to determine whether other studies had been initiated, and the committee requested information from the Centers for Disease Control and Prevention and AHA on other studies that were under way or had been conducted and never published; no such studies were identified. There is still the possibility that studies showing no association were conducted but not published; this would bias the data toward there being an association between secondhand-smoke exposure or smoking bans and acute coronary events.
WEIGHT OF EVIDENCE FROM KEY STUDIES
The 11 studies reviewed in this chapter show remarkable consistency: all were observational studies that used different analyses and showed decreases in the rate of acute MI after implementation of eight smoking bans. Those decreases ranged from about 6 to 47%, depending on the study and the analysis. That consistency in the direction of change gave the committee confidence that smoking bans result in a real decrease in the rate of acute MIs.
Apart from their consistency, most studies drew conclusions that appear to be stronger than the data and analyses warranted. Some researchers have combined the results of the studies with meta-analytic methods to provide a point estimate of the decrease and an associated standard error (Glantz, 2008; Richiardi et al., 2009). The committee concluded that there are too many differences among the studies to have confidence in such a point estimate based on combining results of the different studies.
First, the nature of the “treatment”—the smoking ban and collateral programs—is far from clear in specific studies, so there may not be a common intervention to assess. Any form of causal analysis needs to be explicit about the details of the intervention and the fidelity with which it was implemented. In addition, some of the studies tested different “treatments” as part of their hypotheses: some looked simply at the effect of smoking bans, others looked more directly at changes in secondhand-smoke exposure.
Second, the population of interest varied from study to study in both explicit and implicit ways. Some looked at a population as a whole, others focused on smokers and nonsmokers separately. Population differences in responses to the interventions, such as changes in behavior, and differences in preexisting disease could exist. Those differences could be assessed and accounted for differently among studies, but many of the studies were silent on those issues; when they were not, they differed in how the issues are addressed.
Third, given the absence of randomization into treatment and nontreatment groups, the choice of comparison groups for assessing the effect of an intervention is problematic. The studies under review varied substantially in that regard. Some studies used historical controls, others used longitudinal statistical adjustments with such techniques as time-series analyses and stratification by demographic group. The problem with respect to estimating the magnitude of the overall effect is that the studies at hand did not adopt the same analytic strategy and did not make the ideal adjustments.
Fourth, the relative changes in the numbers of acute events appear to vary from study to study, and this poses problems in the examination of the heterogeneous responses to the interventions. There are two ways to try to deal with such heterogeneity: include possible confounding variables as part of the model to remove heterogeneity by adjustment, and consider adding an extra component of variation in the error term for heterogeneity to make the standard errors larger than they would have been if the results had been homogeneous. Several of the studies included adjustment variables to capture effects of demographic groups, seasonality, or both, but each made such adjustments differently. Small numbers of events, as observed in several of the studies, militate against elaborate statistical adjustments for demographic groups or considerations of seasonality, and the adjustments that several of the studies made appear far from optimal. That leaves open the question of whether studies should focus on individual-level rather than group-level assessments and, if so, how they should do that.
Finally, the studies varied widely in their measures of acute cardiovascular events and in the time until differences were observed. In some instances, investigators allowed the time to effect to be determined by the data; in others, they hypothesized different periods.
When all those and other factors are taken into account, no simple meta-analytic technique is adequate for assessing the magnitude of the effect of a smoking ban or of the effect of a reduction in exposure to secondhand smoke on acute cardiovascular events.
In summary, the studies all appear to have found substantial reductions in acute cardiovascular events after the implementation of smoking bans and in that sense were consistent, but separately and collectively they had statistical shortcomings. The committee concludes that the shortcomings
do not negate the evidence of an association between smoking bans and the incidence of acute MI or, for the relevant studies, secondhand-smoke exposure and the incidence of acute MI. As a consequence of the variability and the limitations, however, it is difficult to use them to estimate the magnitude of the effect of smoking bans or secondhand-smoke exposure on the incidence of acute MI.
CONCLUSIONS
-
The extent to which the studies assessed possible alternative causes of changes in hospitalizations—health-care availability, use of different cardiac medications, new diagnostic criteria, and a decrease in all hospital admissions during a period—should be considered, especially if before–after comparisons are being made in the absence of a comparison area. Given the multiple factors that could affect the rate of acute MIs, however, an assessment of secular trends is preferable.
-
Results of studies that included self-reported assessments of exposure to secondhand smoke cannot necessarily be compared with results of other studies that did the same thing unless the survey instruments (such as interviews) were similar.
-
All the studies are relevant and informative with respect to the questions posed to the committee, and overall they support an association between smoking bans and a decrease in acute cardiovascular events.
-
The magnitude of the effect cannot be determined on the basis of the studies, because of variability among and uncertainties within them.
-
In most of the studies, the portion of the effect attributable to decreased smoking by smokers as opposed to decreased exposure of nonsmokers to secondhand smoke cannot be determined.
-
The studies support, to the extent that it was evaluated, an association between a reduction in secondhand smoke and a decrease in acute cardiovascular events. The strongest data on that association in nonsmokers come from
-
Analyses of only nonsmokers (Monroe, Indiana, and Scotland).
-
Analyses that showed decreases in secondhand smoke after implementation of smoking bans.
-
-
At the population level, results of the key intervention studies reviewed by the committee are for the most part consistent with a decrease in risk as early as a month following reductions in secondhand-smoke exposure; however, given the variability in the
-
studies and the lack of data on the precise timing of interventions, the smoking-ban studies do not provide adequate information on the time it takes to see decreases in cardiovascular effects.
REFERENCES
Akbar-Khanzadeh, F., S. Milz, A. Ames, S. Spino, and C. Tex. 2004. Effectiveness of clean indoor air ordinances in controlling environmental tobacco smoke in restaurants. Archives of Environmental Health 59(12):677-685.
Alpert, H. R., C. M. Carpenter, M. J. Travers, and G. N. Connolly. 2007. Environmental and economic evaluation of the Massachusetts smoke-free workplace law. Journal of Community Health 32(4):269-281.
Anderson, R. N., A. M. Minino, D. L. Hoyert, and H. M. Rosenberg. 2001. Comparability of cause of death between ICD-9 and ICD-10: Preliminary estimates. National Vital Statistics Report 49(2):1-32.
Barone-Adesi, F., L. Vizzini, F. Merletti, and L. Richiardi. 2006. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. European Heart Journal 27(20):2468-2472.
Bartecchi, C., R. N. Alsever, C. Nevin-Woods, W. M. Thomas, R. O. Estacio, B. B. Bartelson, and M. J. Krantz. 2006. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation 114(14):1490-1496.
CDC (Centers for Disease Control and Prevention). 2004. Indoor air quality in hospitality venues before and after implementation of a clean indoor air law—western New York, 2003. MMWR—Morbidity & Mortality Weekly Report 53(44):1038-1041.
———. 2007. Reduced secondhand smoke exposure after implementation of a comprehensive statewide smoking ban—New York, June 26, 2003–June 30, 2004. MMWR—Morbidity & Mortality Weekly Report 56(28):705-708.
———. 2009. Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance—city of Pueblo, Colorado, 2002–2006. MMWR—Morbidity & Mortality Weekly Report 57(51):1373-1377.
Cesaroni, G., F. Forastiere, N. Agabiti, P. Valente, P. Zuccaro, and C. A. Perucci. 2008. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation 117(9):1183-1188.
Cirera Suarez, L., M. Rodriquez Barranco, E. Madrigal de Torres, J. Carillo Prieto, A. Hasiak Santo, R. Augusto Becker, A. Tobias Garcés, and N. Sánchez Carmen. 2006. [Correspondences from 10th to 9th revision of the International Classification of Diseases in the causes of death lists of the National Institute of Statistics and the Regional Health Authority of Murcia in Spain]. Revista Española de Salud Pública 80(2):157-175.
Dockery, D. W. 2009. Health effects of particulate air pollution. Annals of Epidemiology 19(4):257-263.
Ellingsen, D. G., G. Fladseth, H. L. Daae, M. Gjolstad, K. Kjaerheim, M. Skogstad, R. Olsen, S. Thorud, and P. Molander. 2006. Airborne exposure and biological monitoring of bar and restaurant workers before and after the introduction of a smoking ban. Journal of Environmental Monitoring 8(3):362-368.
French, B., and P. J. Heagerty. 2008. Analysis of longitudinal data to evaluate a policy change. Statistics in Medicine 27(24):5005-5025.
Gallus, S., P. Zuccaro, P. Colombo, G. Apolone, R. Pacifici, S. Garattini, and C. La Vecchia. 2006. Effects of new smoking regulations in Italy. Annals of Oncology 17(2):346-347.
Gevecker Graves, C., M. E. Ginevan, R. A. Jenkins, and R. G. Tardiff. 2000. Doses and lung burdens of environmental tobacco smoke constituents in nonsmoking workplaces. Journal of Exposure Analysis and Environmental Epidemiology 10(4):365-377.
Glantz, S. 2008. Meta-analysis of the effects of smokefree laws on acute myocardial infarction: An update. Preventive Medicine 47:452-453.
Goldacre, M. J., S. E. Roberts, and M. Griffith. 2003. Multiple-cause coding of death from myocardial infarction: Population-based study of trends in death certificate data. Journal of Public Health Medicine 25(1):69-71.
Gorini, G., A. Gasparrini, M. C. Fondelli, A. S. Costantini, F. Centrich, M. J. Lopez, M. Nebot, and E. Tamang. 2005. Environmental tobacco smoke (ETS) exposure in Florence hospitality venues before and after the smoking ban in Italy. Journal of Occupational & Environmental Medicine 47(12):1208-1210; author reply 1210.
Griffiths, C., A. Brock, and C. Rooney. 2004. The impact of introducing ICD-10 on trends in mortality from circulatory diseases in England and Wales. Health Statistics Quarterly 22:14-20.
Haw, S. J., and L. Gruer. 2007. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: National Cross Sectional survey. BMJ 335(7619):549.
HEI (Health Effects Institute) Accountability Working Group. 2003. Assessing the health impact of air quality regulations: Concepts and methods for accountability research. Communication 11. Boston, MA: Health Effects Institute.
HHS (U.S. Department of Health and Human Services). 2008. HHS proposes adoption of ICD-10 code sets and updated electronic transaction standards. Press release. (Accessed March 1, 2009, from http://www.hhs.gov/news/press/2008pres/08/20080815a.html.)
Juster, H. R., B. R. Loomis, T. M. Hinman, M. C. Farrelly, A. Hyland, U. E. Bauer, and G. S. Birkhead. 2007. Declines in hospital admissions for acute myocardial infarction in New York state after implementation of a comprehensive smoking ban. American Journal of Public Health 97(11):2035-2039.
Kado, N. Y., S. A. McCurdy, S. J. Tesluk, S. K. Hammond, D. P. Hsieh, J. Jones, and M. B. Schenker. 1991. Measuring personal exposure to airborne mutagens and nicotine in environmental tobacco smoke. Mutation Research 261(1):75-82.
Kavsak, P. A., A. R. MacRae, V. Lustig, R. Bhargava, R. Vandersluis, G. E. Palomaki, M. J. Yerna, and A. S. Jaffe. 2006. The impact of the ESC/ACC redefinition of myocardial infarction and new sensitive troponin assays on the frequency of acute myocardial infarction. American Heart Journal 152(1):118-125.
Khuder, S. A., S. Milz, T. Jordan, J. Price, K. Silvestri, and P. Butler. 2007. The impact of a smoking ban on hospital admissions for coronary heart disease. Preventive Medicine 45(1):3-8.
Kircher, T., J. Nelson, and H. Burdo. 1985. The autopsy as a measure of accuracy of the death certificate. New England Journal of Medicine 313(20):1263-1269.
Leaderer, B. P., and S. K. Hammond. 1991. Evaluation of vapor-phase nicotine and respirable suspended particle mass as markers for environmental tobacco smoke. Environmental Science and Technology 25(4):770-777.
Lemstra, M., C. Neudorf, and J. Opondo. 2008. Implications of a public smoking ban. Canadian Journal of Public Health 99(1):62-65.
Lightwood, J. M., and S. A. Glantz. 2009. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation 120:1373-1379.
Lofroth, G., and G. Lazaridis. 1986. Environmental tobacco smoke: Comparative characterization by mutagenicity assays of sidestream and mainstream cigarette smoke. Environmental Mutagenesis 8(5):693-704.
Luepker, R. V., F. S. Apple, R. H. Christenson, R. S. Crow, S. P. Fortmann, D. Goff, R. J. Goldberg, M. M. Hand, A. S. Jaffe, D. G. Julian, D. Levy, T. Manolio, S. Mendis, G. Mensah, A. Pajak, R. J. Prineas, K. S. Reddy, V. L. Roger, W. D. Rosamond, E. Shahar, A. R. Sharrett, P. Sorlie, and H. Tunstall-Pedoe. 2003. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: A statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 108(20):2543-2549.
Mahonen, M., V. Salomaa, M. Brommels, A. Molarius, H. Miettinen, K. Pyorala, J. Tuomilehto, M. Arstila, E. Kaarsalo, M. Ketonen, K. Kuulasmaa, S. Lehto, H. Mustaniemi, M. Niemela, P. Palomaki, J. Torppa, and T. Vuorenmaa. 1997. The validity of hospital discharge register data on coronary heart disease in Finland. European Journal of Epidemiology 13(4):403-415.
Menzies, D., A. Nair, P. A. Williamson, S. Schembri, M. Z. H. Al-Khairalla, M. Barnes, T. C. Fardon, L. McFarlane, G. J. Magee, and B. J. Lipworth. 2006. Respiratory symptoms, pulmonary function, and markers of inflammation among bar workers before and after a legislative ban on smoking in public places. JAMA 296(14):1742-1748.
Nashelsky, M. B., and C. H. Lawrence. 2003. Accuracy of cause of death determination without forensic autopsy examination. Am J Forensic Med Pathol 24(4):313-319.
National Center for Health Statistics. 2009. About the International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM). (Accessed March 1, 2009, from http://www.cdc.gov/nchs/about/otheract/icd9/abticd10.htm.)
Pajunen, P., H. Koukkunen, M. Ketonen, T. Jerkkola, P. Immonen-Raiha, P. Karja-Koskenkari, M. Mahonen, M. Niemela, K. Kuulasmaa, P. Palomaki, J. Mustonen, A. Lehtonen, M. Arstila, T. Vuorenmaa, S. Lehto, H. Miettinen, J. Torppa, J. Tuomilehto, Y. A. Kesaniemi, K. Pyorala, and V. Salomaa. 2005. The validity of the Finnish Hospital Discharge Register and Causes of Death Register data on coronary heart disease. European Journal of Cardiovascular Prevention & Rehabilitation 12(2):132-137.
Pell, J. P., S. Haw, S. Cobbe, D. E. Newby, A. C. H. Pell, C. Fischbacher, A. McConnachie, S. Pringle, D. Murdoch, F. Dunn, K. Oldroyd, P. Macintyre, B. O’Rourke, and W. Borland. 2008. Smoke-free legislation and hospitalizations for acute coronary syndrome. New England Journal of Medicine 359(5):482-491.
Peng, R. D., H. H. Chang, M. L. Bell, A. McDermott, S. L. Zeger, J. M. Samet, and F. Dominici. 2008. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among medicare patients. JAMA 299(18):2172-2179.
Pladevall, M., D. C. Goff, M. Z. Nichaman, F. Chan, D. Ramsey, C. Ortiz, and D. R. Labarthe. 1996. An assessment of the validity of ICD code 410 to identify hospital admissions for myocardial infarction: The Corpus Christi Heart Project. International Journal of Epidemiology 25(5):948-952.
Ravakhah, K. 2006. Death certificates are not reliable: Revivification of the autopsy. Southern Medical Journal 99(7):729-733.
Richiardi, L., L. Vizzini, F. Merletti, and F. Barone-Adesi. 2009. Cardiovascular benefits of smoking regulations: The effect of decreased exposure to passive smoking. Preventive Medicine 48(2):167-172.
RTI (Research Triangle Institute) International. 2004. First annual independent evaluation of New York’s Tobacco Control Program: Final report. Research Triangle Park, NC.
Rubin, D. B. 2008. For objective causal inference, design trumps analysis. Annals of Applied Statistics 2(3):808-840.
Sargent, R. P., R. M. Shepard, and S. A. Glantz. 2004. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: Before and after study. BMJ 328(7446):977-980.
Semple, S., K. S. Creely, A. Naji, B. G. Miller, and J. G. Ayres. 2007a. Secondhand smoke levels in Scottish pubs: The effect of smoke-free legislation. Tobacco Control 16(2):127-132.
Semple, S., L. Maccalman, A. A. Naji, S. Dempsey, S. Hilton, B. G. Miller, and J. G. Ayres. 2007b. Bar workers’ exposure to second-hand smoke: The effect of Scottish smoke-free legislation on occupational exposure. Annals of Occupational Hygiene 51(7):571-580.
Seo, D.-C., and M. R. Torabi. 2007. Reduced admissions for acute myocardial infarction associated with a public smoking ban: Matched controlled study. Journal of Drug Education 37(3):217-226.
Stranges, S., M. R. Bonner, F. Fucci, K. M. Cummings, J. L. Freudenheim, J. M. Dorn, P. Muti, G. A. Giovino, A. Hyland, and M. Trevisan. 2006. Lifetime cumulative exposure to secondhand smoke and risk of myocardial infarction in never smokers: Results from the western New York Health study, 1995-2001. Archives of Internal Medicine 166(18):1961-1967.
Teo, K. K., S. Ounpuu, S. Hawken, M. R. Pandey, V. Valentin, D. Hunt, R. Diaz, W. Rashed, R. Freeman, L. Jiang, X. Zhang, and S. Yusuf. 2006. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: A case-control study. Lancet 368(9536):647-658.
Valente, P., F. Forastiere, A. Bacosi, G. Cattani, S. Di Carlo, M. Ferri, I. Figa-Talamanca, A. Marconi, L. Paoletti, C. Perucci, and P. Zuccaro. 2007. Exposure to fine and ultrafine particles from secondhand smoke in public places before and after the smoking ban, Italy 2005. Tobacco Control 16(5):312-317.
Vasselli, S., P. Papini, D. Gaelone, L. Spizzichino, E. De Campora, R. Gnavi, C. Saitto, N. Binkin, and G. Laurendi. 2008. Reduction incidence of myocardial infarction associated with a national legislative ban on smoking. Minerva Cardioangiologica 56(2):197-203.
WHO (World Health Organization). 2009. International Classification of Diseases (ICD) (Accessed March 1, 2009, from http://www.who.int/classifications/icd/en/.)






































