Charting a Course for the Future of Health Care
Today, perhaps more than ever, health care is a key item on the nation’s agenda. Government policy makers, health professionals, scientists, industrial and civic leaders, patient advocates, and private citizens across the social spectrum are focusing on how best to obtain a high-quality health system that is efficient and affordable in its operation and that functions well for everyone.
The Institute of Medicine (IOM) regularly considers this challenge from a variety of perspectives. Recent efforts have focused on improving the organization and operation of the nation’s largest health agency; working to assess what diagnostic, therapeutic, and preventive services work best; gauging the overall health of the nation’s population; and identifying ways to build an even stronger foundation of evidence-based medicine that effectively captures the promise of scientific discovery and technological innovation and enables doctors, nurses, and other health professionals to provide the right care for the right patient at the right time.
Revitalizing Health and Human Services
The U.S. Department of Health and Human Services (HHS)—the largest of all federal departments, spending approximately $2 billion a day—profoundly affects the lives of all Americans. Its agencies and programs protect against domestic and global health threats, monitor the safety of food and drugs, advance the science of treating and preventing disease, safeguard society’s most vulnerable populations, and work to improve
health for everyone. However, HHS increasingly faces serious and complex obstacles, chief among them rising health care costs and a broadening range of health challenges. The department also faces internal challenges. Over time, the federal government has charged HHS with additional responsibilities and removed others, often without corresponding shifts in organizational procedures, structures, or resources.

Recognizing such concerns, Congress asked the IOM to examine whether HHS is “ideally organized” to meet the nation’s enduring and emerging health challenges. The study committee’s report, HHS in the 21st Century: Charting a New Course for a Healthier America (2008), identifies many factors that reduce the department’s ability to meet its range of responsibilities. These factors include divergence in the missions and goals of the department’s agencies, limited flexibility in spending, impending workforce shortages, difficulty in retaining skilled professionals, and problems in effectively partnering with the private sector.
The report emphasizes the need for HHS to improve performance and processes for goal setting, decision making, management, and account-ability—but it does not call for a large-scale reorganization of the entire department. Instead, it seeks action in five specific areas.
Defining a 21st-century vision
HHS currently lacks a clear vision of how to provide the greatest value in protecting and improving health in today’s climate of varied, complex, and sometimes changing health needs. By defining such a vision—along with a complementary mission statement that defines a small number of measurable, time-specific goals—HHS can help individuals in Congress, throughout the federal government and the health sector, and across the nation at large to understand the role and importance of the department’s work.
HHS—the largest of all federal departments, spending approximately $2 billion a day—profoundly affects the lives of all Americans.
Fostering adaptability and alignment
To best position itself to respond to the nation’s health challenges and to adapt quickly to changing circumstances, HHS must align all of its operations more effectively. Furthermore, the leaders of all of its various units should strive to ensure that their activities mesh with the department’s overall vision, mission, and goals. Among particular recommendations, HHS should reduce its number of senior-level officials; develop a more prominent and powerful role for the surgeon general; and provide predictable funding for its science agencies, including specific funding for the Agency for Healthcare Research and Quality that is independent of other departmental appropriations.
One area of public health that is ripe for change is food safety, which cannot be addressed adequately within HHS’s current structure. The department’s food-related agencies are insufficiently equipped and understaffed to keep pace with food safety issues, especially in light of the globalization of the food supply. As an important step, Congress should unify the Department of Agriculture’s Food Safety and Inspection Service and the Food and Drug Administration’s food safety activities, place the resulting entity under HHS, and provide it with adequate resources for high-quality inspection, enforcement, and research.
Increasing effectiveness and efficiency of the health care system
By all accounts, the nation’s current health care system is flawed, marked by rising costs, lack of evidence about the effectiveness of even the most widespread medical procedures, and a growing number of people who are uninsured. Among suggested changes, HHS should work with Congress to establish a capability for assessing the comparative value—including clinical and cost effectiveness—of medical interventions and procedures, preventive and treatment technologies, and methods of organizing and delivering care. This effort will require expanded information sharing, both within the department as well as with external organizations, in order to better evaluate and inform the health care system.
Strengthening the health care workforce
Analysts predict serious shortages across the health care spectrum of people with the right backgrounds, training, and skills. Such shortages will affect not only HHS, but also state and local public health agencies, the private
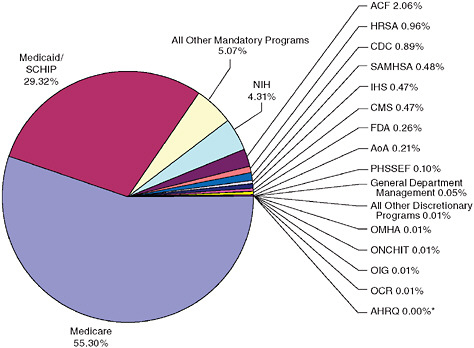
Distribution of HHS actual expenditures, FY 2007.
*The AHRQ is shown as representing 0 percent of the department’s budget because it receives funds only from other Public Health Service (PHS) agencies through the PHS evaluation set-aside and has not had its own separate budget allocation since 2002. In fact, the President’s budget request for AHRQ has been zero since 2001. Its 2009 program-level expenses were projected at $326 million, making it by far the smallest PHS agency.
NOTE: ACF = Administration for Children and Families; AHRQ = Agency for Healthcare Research and Quality; AoA = Administration on Aging; CDC = Centers for Disease Control and Prevention; CMS = Centers for Medicare and Medicaid Services; FDA = Food and Drug Administration; HRSA = Health Resources and Services Administration; IHS = Indian Health Service; OCR = Office for Civil Rights; OIG = Office of the Inspector General; OMHA = Office of Medicare Hearings and Appeals; ONCHIT = Office of the National Coordinator for Health Information Technology; PHSSEF = Public Health and Social Services Emergency Fund; SAMHSA = Substance Abuse and Mental Health Services Administration; SCHIP = State Children’s Health Program, a component of Medicaid.
SOURCE: HHS in the 21st Century: Charting a New Course for a Healthier America, p. 28.
health care sector, and the science establishment. Current workforce challenges include an aging workforce, new health challenges that require new skills, an imbalance between primary care physicians and specialists, and an underrepresentation of minority groups among the nation’s health professionals. In this light, HHS should place a high priority on developing a strategy for workforce recruitment and improvement within its own ranks, as well as in the public health and health care professions nationwide, and
in the biosciences. Special emphasis should be placed on assessing and addressing the current and projected gaps in the number, professional mix, geographic distribution, and diversity of the nation’s public health and health care workforces.
Improving accountability and decision making
A strong system of accountability will provide HHS with the incentive, as well as the information it needs, to improve its performance. Toward this end, Congress and HHS should form a “new compact” that would grant the department greater flexibility in its internal operations and decision making while requiring it to assume greater accountability for assessing its operations. As part of this arrangement, HHS would be required to provide Congress and the public with regular, rigorous reports detailing the department’s progress in improving the nation’s health.
Although improving the organization and efficiency of HHS will move the nation forward in meeting its health needs, this step alone will not solve the health care crisis. There are many other factors at play, and one critical question is whether doctors are delivering the best care possible. The IOM recently considered this question from multiple perspectives.
Assessing what works in health care
Solving some of the nation’s most pressing health policy problems may hinge on the capacity to identify which diagnostic, therapeutic, and preventive services work best for various patients and under various circumstances. As many studies have documented, spending on ineffective care contributes to rising health costs and insurance premiums. Variations in how multiple health care providers treat the same conditions reflect uncertainty and disagreement about what the clinical practice standards should be. Patients and insurers cannot always be confident that health professionals are delivering the best, most effective care. At the same time, health plans are burdened with the need to constantly learn how their covered populations might benefit from—or be harmed by—newly available health services. Meanwhile, some observers argue that consumers who are
Solving some of the nation’s most pressing health policy problems may hinge on the capacity to identify which diagnostic, therapeutic, and preventive services work best for various patients and under various circumstances.
equipped with good information will have the power to reduce the cost and improve the quality of care they receive. Yet even the most sophisticated and motivated health care consumer struggles to learn which care is appropriate for his or her circumstance.
To help correct this problem, The Robert Wood Johnson Foundation asked the IOM to recommend a sustainable, replicable approach to identifying effective clinical services. The resulting report, Knowing What Works in Health Care: A Roadmap for the Nation (2008), lays out a detailed action plan. As a key step, Congress should direct HHS to establish a single national program—either a public or joint public–private entity—with the authority, expertise, and resources necessary to set priorities for evaluating clinical services and to conduct systematic reviews of the evidence on clinical effectiveness.
The program should be guided, in part, by an independent advisory committee that would identify high-priority topics that merit systematic evidence assessment. The committee’s priority-setting process should be scientifically rigorous, transparent, efficient, and understandable by outsiders. The committee should consider a range of topics, including new, emerging, and well-established health services and technologies for prevention, diagnosis, and treatment. The highest priorities should be the clinical questions of patients and clinicians that have the potential for substantial impact on health outcomes across all ages by reducing the burden of disease, health disparities, and undesirable variation in the delivery of health services
As part of its charge, the program also would develop and promote rigorous standards for creating clinical practice guidelines, which could help clinicians and patients make informed decisions about appropriate health care for specific clinical circumstances, minimize use of questionable services, and target services to the patients most likely to benefit. At present, there are few protections against the proliferation of poorly developed guidelines. Moreover, there is a plethora of guidelines for some conditions (for example, as of 2007 there were more than 471 guidelines just for managing hypertension), and the guidelines sometimes offer conflicting and confusing advice. Guidelines would best be developed by a panel of experts who have access to the fullest array of evidence on a given medical
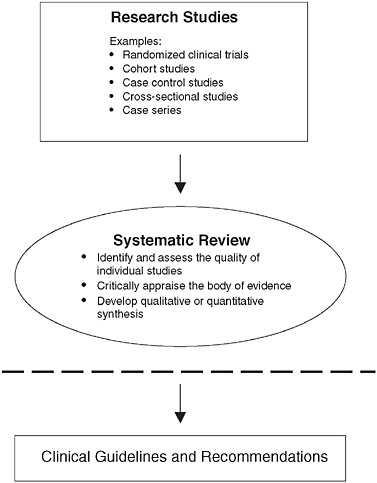
Continuum from research studies to systematic review to development of clinical guidelines and recommendations.
NOTE: The dashed line is the theoretical dividing line between the systematic review of the research literature and its application to clinical decision making, including the development of clinical guidelines and recommendations. Below the dashed line, decision makers and developers of clinical recommendations interpret the findings of systematic reviews to decide which patients, health care settings, or other circumstances they relate to.
SOURCE: Knowing What Works in Health Care: A Roadmap for the Nation, p. 23.
intervention, an understanding of the clinical problem and the appropriate research methods, and sufficient time and resources to absorb the information and make considered judgments.
In response to the report, the federal government has initiated several actions. In June 2008, Congress enacted the Medicare Improvement for Patients and Providers Act, authorizing, among other things, $3 mil-
lion for IOM studies on recommended standards for conducting systematic reviews and developing clinical practice guidelines. In addition, in July 2008, Senators Kent Conrad (D-ND) and Max Baucus (D-MT) introduced the Comparative Effectiveness Research Act, which incorporates a number of the IOM’s recommendations. It calls for a nonprofit entity called the Health Care Comparative Effectiveness Research Institute to set a national research agenda and to “conduct comparative effectiveness research on health interventions.” The legislation also would allow the IOM to serve in a consulting role to this institute.
Advancing evidence-based health care
American medicine has contributed fundamentally to the breadth, depth, and pace of advances in diagnosing and treating disease and injury. But this progress has, in many instances, outstripped the health care system’s capacity to know the circumstances under which a particular intervention is best applied. Without better information about the effectiveness of different treatment options, the resulting uncertainty can lead to the delivery of services that may be unnecessary, unproven, or even harmful. Other consequences of this gap between advancing treatment options and assessment capacity include a steady expansion in the national and personal costs of medical care, and a substantial growth in concern and distrust among physicians and patients alike. Accordingly, there is an acute need for better evidence to guide the decisions of patients and their caregivers on the approaches most appropriate to individual circumstances and preferences.
Without better information about the effectiveness of different treatment options, the resulting uncertainty can lead to the delivery of services that may be unnecessary, unproven, or even harmful.
This need for a more systematic approach to evidence development and application, as well as the prospect of new ways of meeting the need, provided the back-drop for the IOM’s 37th annual meeting, held in October 2007. The meeting drew heavily on discussions of the IOM’s Roundtable on Evidence-Based Medicine. Through the Roundtable, the IOM has characterized evidence-based medicine to mean that to the greatest extent possible, the decisions that shape the health and health care of Americans—by patients, providers, payers, and policy makers alike—will be grounded on a reliable evidence base, will account appropriately for individual variation
in patient needs, and will support the generation of new insights on clinical effectiveness. Evidence is generally considered to be information from clinical experience that has met some established test of validity, and the appropriate standard is determined according to the requirements of the intervention and clinical circumstance.
Evidence-Based Medicine and the Changing Nature of Health Care: Meeting Summary (2008) captures discussions at the 2007 IOM annual meeting on a range of issues—highlighting both challenges and opportunities to developing the health care system centered on the generation and application of evidence as a natural outcome of the care process. Discussion focused on four themes: the forces driving the need for better medical evidence; the challenges with which patients and providers must contend; the need to transform the speed and reliability of new medical evidence; and the legislative and policy changes that would enable an evidence-based health care system.
The report details a number of issues driving the need for a more central focus on evidence in health care. One underlying motif, for example, is the increasing complexity of health care. New pharmaceuticals, medical devices, technologies, and predictive data offer much promise for improving health care, but they also introduce a measure of uncertainty that requires changes on the parts of both caregivers and their patients.
Another frequent observation is that the current health care system is not designed to deliver value—a situation that leads to excessive medical spending, often on interventions of no clinical benefit. Unjustified discrepancies in care patterns also occur frequently. The intensity of health care services delivered for similar conditions varies significantly across geographic regions, particularly in areas that require discretionary decision making. However, the higher spending regions often do not deliver better quality care, and hence offer substantial opportunity for reduced spending without sacrificing health outcomes. Opportunities exist to eliminate wasteful spending with no reduction in health care, as well as to improve the overall health outcomes, but agreement is needed both on what constitutes best care and on what constitutes value in health care.
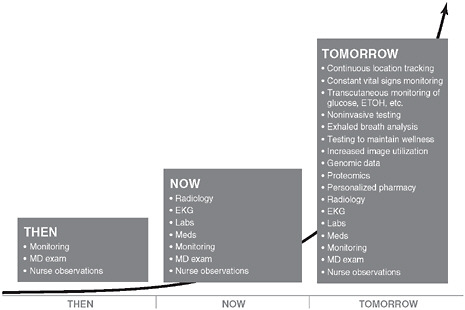
Data advances in medicine.
SOURCE: Evidence-Based Medicine and the Changing Nature of Health Care: Meeting Summary, p. 116.
These challenges illustrate the pressing need for more and better evidence development. Practice-based research approaches will help determine the effectiveness of new medical interventions and ways in which health care is delivered. Information technology offers additional promise to bring research closer to practice. Electronic medical records and clinical data registries, for example, offer tremendous potential both to generate new evidence and to augment randomized clinical trials. Capitalizing on such rewards will require addressing privacy and proprietary issues that now limit data access and sharing.
With the increasing complexity of care, and the need and demand for more patient involvement, the traditional “physician-as-sole-authority” model will need to adapt to support patients as integral partners in medical decisions.
Shifting to a culture of evidence-driven health care—what some observers call a “culture that learns”—will require health care providers and patients to support systems and procedures that foster the generation and application of evidence. Achieving such changes will mean developing new models of patient–provider part-
nerships. With the increasing complexity of care, and the need and demand for more patient involvement, the traditional “physician-as-sole-authority” model will need to adapt to support patients as integral partners in medical decisions.
As a foundation for these necessary changes, leadership promoting a focus on evidence in health care will need to stem from every quarter, with the public and private sectors working together, and with policy makers, providers, patients, insurers, and other stakeholders actively engaged in the steps toward change.
Gauging the nation’s health
In order to understand how to improve the collective health of everyone in the United States, it is important first to understand the most significant factors that contribute to health and the effects of health care. At the request of the nonprofit group State of the USA, an IOM study committee has provided detailed guidance for producing just such a yardstick.
Clearly, no single measure can possibly capture the health of the nation. Thus, State of the USA Health Indicators: Letter Report (2008) lists 20 factors key to determining overall health and well-being. The indicators—each backed by a substantial body of high-quality data—fall into three general categories: health outcomes, health-related behaviors, and health systems performance. Health outcomes cover factors such as life expectancy at birth, infant mortality, injury-related mortality, and the prevalence of chronic diseases and psychological distress. Behavioral factors include both healthful activities, such as engaging regularly in at least moderate physical exercise, and harmful behaviors, such as smoking, drinking to excess, or being obese. Factors related to the performance of health systems include per-capita spending on care, pervasiveness of insurance coverage among populations, and rates of childhood immunization and adult preventative services, among others.

State of the USA is incorporating detailed information about these various measures into a new interactive website that anyone can use to
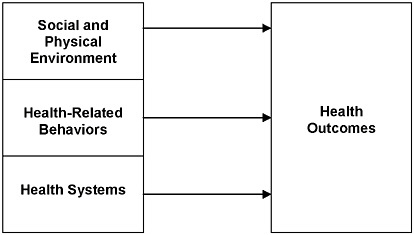
Framework for health and health care indicator development.
SOURCE: State of the USA Health Indicators: Letter Report, p. 5.
learn about critical health issues. They also will be able to track the nation’s progress—or the progress of a particular geographic region—in improving the health of its population (or subpopulations) and gauge changes in the effectiveness of public health and care systems. Until now, only experts with the technological capability to search arcane data had the capacity for this kind of examination. As the nation moves increasingly toward “patient-centered medicine,” in which patients play an active role in their treatment regimens, it will be important to develop effective ways to boost public knowledge about health issues. Certainly, technology is changing the game, allowing individuals to gather information directly and to use this information toward improving health—not only their own, but also the health of their community and of their country.












