9
Care Culture and System Redesign
INTRODUCTION
Lowering healthcare spending and improving care outcomes will not only necessitate better application of existing medical insights at the point of care, but also require significant changes to the delivery system (Center for American Progress and Institute on Medicine as a Profession, 2008; Hackbarth, 2009; Senate Finance Committee, 2009). Care fragmentation, non-value-added activities, workflow inefficiencies, and defensive medicine, among many others, reflect elements of a broken system and are highlighted in many of the earlier chapters. While the presentations in this session are diverse, all the strategies discussed throughout the chapter share the central idea of shifting the current culture to one of patient-centered care through such levers as streamlined and harmonized health insurance regulation, quality and consistency in treatment with a focus on the medically complex, sharable clinical records, and medical liability reform.
Michelle J. Lyn of the Duke University Medical Center discusses refocusing the paradigm from physicians in healthcare facilities to one of multidisciplinary partnerships involving community members, nonprofit organizations, governmental health and human services entities, hospitals, and medical practices. Illustrating the impact of these community-based strategies, Lyn discusses two examples of success that have not only improved clinical outcomes and decreased acute care needs, but also yielded significant savings. She concludes that, despite limited experience transitioning to systems of care for an increasingly diverse, aging population, community-engaged system redesign must be part of healthcare reform.
Focusing on workflow efficiency, Kim R. Pittenger of Virginia Mason Medical Center and Sandeep Green Vaswani of the Institute for Healthcare Optimization describe different approaches to maximize the current resources in the health system. Describing the Virginia Mason Medical Center (VMMC) production system, Pittenger emphasizes the importance of flow production, mistake proofing, and standardizing work, suggesting that nationwide use of this type of strategy (extrapolated from results seen at VMMC) could yield clinical and patient safety savings of $44 billion and operational savings of over $7 billion. Vaswani describes the related process of managing variability in hospital operations and management in order to improve patient safety and quality of care. While describing successful case studies and outlining the assumptions made to extrapolate nationally, he suggests that the annual savings opportunity from application of variability methodology at the national level is in the range of $35 to $112 billion.
Meanwhile, Timothy G. Ferris of Massachusetts General Hospital (MGH) discusses care coordination, specifically describing how one demonstration project has already yielded promising results. By focusing on those patients with the highest illness burden, a similar national effort could potentially save up to $1 billion for the Medicare program annually. He cautions that several of MGH’s characteristics—integration of hospital and physician services, existing electronic medical records system, extensive primary care service network—may limit generalizability of their success. However, he concludes that the apparent success of the MGH Care Management Program suggests that prospective payment for the enhanced management of high-risk patients holds some promise for reducing costs.
Building on the idea of integration, coordination across providers, and information technology as central elements of care coordination, Ashish Jha of Harvard University describes interoperability of health information technology as a method of facilitating health information exchange (HIE). He reviews the literature suggesting that widespread health information exchange can not only streamline the over 30 billion healthcare transactions occurring each year within the delivery system, but it can simultaneously decrease annual healthcare spending by nearly $80 billion annually. Jha cites the formation of a national strategy and standardized infrastructure protocols as keys to driving the success of HIE.
Turning to regulatory interventions, Roger Feldman of the University of Minnesota moves the discussion to the broader context of market competition and antitrust regulations. While he frames antitrust policy as an important tool for ensuring that markets provide goods and services at the lowest price to consumers, he elaborates on the reasons why it has not been as effective in the healthcare arena and provides specific suggestions to increase its impact. Frank A. Sloan of Duke University provides an overview of a strategy to control increases in capital healthcare expenditures: service capacity restrictions. After reviewing the history of certificate-of-
need (CON) requirements, he asserts that CON-type regulations have been hampered by major shortcomings, such as poor definition of “need” and lack of capital budgets for CON programs. However, if these issues are addressed, Sloan suggests that capital expenditure regulation may be a viable option for cost containment if used appropriately. Closing the session on system design, Randall R. Bovbjerg of the Urban Institute discusses the potential for malpractice liability reform to lower liability premiums and decrease the practice of defensive medicine. Although he calculates that tort reform could decrease medical expenditures by 0.9 percent (almost $20 billion in 2010), he believes that bundling liability reform with other reform initiatives could achieve even greater synergistic savings.
COMMUNITY-ENGAGED MODELS OF TEAM CARE
Michelle J. Lyn, M.B.A., M.H.A., Mina Silberberg, Ph.D., and J. Lloyd Michener, M.D.
Duke University Medical Center
Our nation’s healthcare system, which is predominately focused on acute care provided by physicians in healthcare facilities, has resulted in higher than necessary healthcare costs and lower than optimal healthcare outcomes for our population. Reforming healthcare financing alone will not resolve these problems. We need innovative models to provide care earlier, more effectively, and at lower cost. These models should be developed and implemented through a collaborative problem-solving approach that uses the knowledge and resources of all stakeholders and is attentive to the varying conditions of different communities. This approach requires fundamental redesign, not the creation of substitution models or “lesser” models of care.
Such an approach is embodied in the community-engaged, iterative, data-driven process that has been undertaken with communities around Duke University Medical Center in response to growing concerns about access, cost, and quality. Still early in our work, we have built multidisciplinary partnerships involving community members, nonprofit organizations, governmental health and human services entities, hospitals, and medical practices to craft responses to community health needs that improve health and reduce costs. Although the resulting healthcare models are varied, they share a number of common elements. The models employ teams of traditional and nontraditional providers; they stratify the population according to risk (medical, social, and environmental); and they use information technology to coordinate community, primary, and specialty care for some of our community’s most vulnerable populations. In this brief, we share examples, describe the prerequisites of—and potential platforms for—more widespread implementation of this approach, and suggest
policy changes that would allow health systems and providers more flexibility in meeting population health needs, creating a match between needs and resources, and promoting dissemination, adoption, and adaptation of effective models of care. These models must be accountable for improving health, meaning they should answer the basic question: What measurable improvement can we make in improving health outcomes for individuals and entire communities?
Changing Our Healthcare Models
The need for new models of care developed through community engagement begins with the failings of our current system. The well-documented persistence of socioeconomic and racial health disparities (which cannot be explained away by variation in insurance status [Smedley et al., 2003]) is but one indicator of the varied healthcare needs and barriers to health in our population. We also continue to demonstrate deficiencies in preventing and managing the chronic diseases that dominate healthcare needs and costs. Chronic disease management and prevention require the patient to change what he or she does on a daily basis, a challenge that requires ongoing education and support. Physicians are expensive and in short supply, and they are not well-suited for the counseling and coaching that lead to patient behavior change. Conversely, their limited time should be employed with the patients who require their unique clinical skills and knowledge. And while the medical community is not and cannot be responsible for changing environmental conditions that affect health and healthcare use, our efforts to improve health will fail if we do not take those conditions into account to the extent possible. For example, inadequate transportation is consistently found to be one of the major nonfinancial barriers to obtaining care (Arcury et al., 2005; Baker et al., 1996). Health care must be provided in locations that are accessible (something that varies by geographic communities and subpopulations), and other barriers to patient access must be identified and, when possible, addressed.
Collaborating with the community to determine what services can be most effectively provided (where, when, how, and by whom) starts with analyzing the health needs and strengths of our diverse communities. This should include small-area analyses of variations in disease burden and neighborhood-level clusters of illness and care patterns and the identification of institutional and community readiness for change. For effective and affordable health care, providers, payers, and patients have to be willing to use the right provider at the right time for the right level of care. The strategic and cost–benefit analyses should employ appropriate economic and health metrics and be iterative, as the needs and resources of communities change over time.
Just for Us
Just for Us (JFU), is an integrated in-home program of care for the low-income frail elderly and disabled, and it exemplifies the approach just described. The program was developed in 1999 in response to data showing high levels of unmet need among Durham’s elderly population. The model grew from a collaboration among Duke (the Division of Community Health and the Nursing School), local government entities (including the county department of social services, the local area mental health entity, and the housing authority), and Lincoln Community Health Center, the area’s federally qualified health center. The JFU program deploys an interdisciplinary team of providers to serve clients in their homes, providing medical care, management of chronic illnesses, and case management. Lincoln contracts with Duke to provide the clinical services of a part-time supervising physician and mid-level providers (nurse practitioners or physicians’ assistants) who offer primary care in the home every 5 to 6 weeks for chronic disease management and as needed for acute conditions. A social worker from the department of social services and a health educator employed by Duke provide case management. Patients are assisted in accessing mental health services, personal care assistance, and other medical and support services.
A review of Medicaid expenditures for Just for Us enrollees enrolled in both JFU and Medicaid over a 2-year period from (2003-2004) suggests how JFU has changed health and healthcare use for its enrollees. From the first to the second year, ambulance costs were down 49 percent, emergency room (ER) costs were down 41 percent, and inpatient costs were down 68 percent. At the same time, prescription costs were up 25 percent, and home health costs were up 52 percent (Yaggy et al., 2006). Another study, currently ongoing, shows statistically significant improvement in hypertension control among enrollees over the course of 1 year.
Community Care of North Carolina
Community Care of North Carolina (CCNC), a program of the North Carolina Department of Health and Human Services, demonstrates the community-engaged, team-based approach to systems change on a statewide level. Launched in 1998 for Medicaid, CCNC is composed of networks of physicians, hospitals, health departments, social services agencies, and so on. These networks form community-based delivery systems and collaboratively deploy teams of social workers, nurses, health educators, dieticians, community health workers, and others who work in concert with physicians to provide care and disease management and assure appropriate access to services. As the communities across North Carolina are different, each network has its own composition. The estimated overall annual state savings under CCNC compared to projected costs under primary care case
management were $150 million to $170 million for fiscal year (FY) 2006 (Mercer, 2007).
Evaluating This Approach
The fields of health services research and public health provide a number of tools for evaluating models such as those we describe. At Duke, sample evaluation measures include traditional Healthcare Effectiveness Data and Information Set (HEDIS) measures to assess clinical programs and ER diversion. More thought needs to be given, however, to how we would estimate the effect of the proposed approach at a national level. The challenges of access and chronic disease prevention and management are shared by all communities, but each community has its own starting point, and there is no one solution, no one team composition that fits all communities.
One thing that is certain is that we should strive to measure our success by patient outcomes and meaningful indicators of system–provider interactions, rather than by adherence to a specific set of structures (e.g., how many exam rooms a clinic has) and less meaningful but easily counted measures of process. Moreover, the community focus of the community-engaged, team-based approach to system change highlights the importance of analytic questions that are always relevant but more easily ignored in a context in which the unit of analysis is individual patients and the process being assessed is the physician–patient encounter. For example, what is the best time frame in which to assess the benefits of disease prevention, evolving health behaviors, and lifestyle changes that are potentially passed from one generation to the next? What ancillary costs and benefits or larger societal effects of our healthcare initiatives do we include in our estimate? Do we include, for example, the effects on workplace productivity of improved health, worksite health care that might reduce absenteeism, and school-based health centers that allow children to receive treatment without parents having to retrieve them from school?
We should be cautious about claims that any system change will rapidly improve outcomes cheaply. One study of primary care case management programs, for example, showed that many changes did indeed reduce healthcare expenditures for their enrollees. However, these savings were outweighed by the costs of the programs themselves (Wheatley, 2002). The study of Medicaid expenditures in the JFU example previously described did show a reduction in the targeted costs—ambulance, ER, and hospital. However, the simultaneous rise in prescription drug costs and personal care assistance resulted in a net increase in Medicaid expenditures. We continue to experiment with how to improve the health of JFU patients while reducing costs, such as by promoting physical activity, with the intention that this will prevent the need for personal care in some patients.
The Challenge of Accountability
The starting point of the approach we describe is the shift we must make as a nation to developing accountable health care that improves the health of populations, not just the health of individual patients. On a daily basis, however, accountability is an ongoing challenge, especially if we have a multiplicity of models to assess and a multiplicity of places people can get care in one community. The medical home model—through which a primary care provider, together with the patient, takes primary responsibility for a patient’s health and system utilization—will provide an answer in some, but likely not all cases. When realistic, patients should be more empowered to manage their own health, while physicians need to do what only they can do—complex care and unknown illnesses, and teams of providers manage the routine acute and chronic care.
The work is evolving, but the power of this approach comes from working with our communities to figure out how to develop and deploy the right providers, how to function as coordinated teams so as to deliver the right care, at the right time, at the right place, by the right level of provider. This approach shares a great deal in common with the movement toward Accountable Care Organizations and Medical Homes, and with Clinical Translational Science Awards, the goal of which is to translate evidence into clinical practice and ultimately population health, while promoting a bi-directional approach to understanding community priorities. Policy changes are needed that will permit and encourage state/local experiments to develop and implement new models of care. These include start-up funding and funding for demonstration projects, and the ability to scale demonstration projects to larger regional and national projects. Reform of the healthcare delivery system offers enormous potential for spending our healthcare dollars more effectively. Despite decades of small-scale experiments, the work of transitioning to systems of care for an increasingly diverse, aging population with growing rates of chronic disease is yet in its infancy. But we know enough to know that community-engaged system redesign must be part of healthcare reform.
USING PRODUCTION SYSTEM METHODS IN MEDICAL PRACTICE: IMPROVING MEDICAL COSTS AND OUTCOMES
Kim R. Pittenger, M.D.
Virginia Mason Medical Center
President Barack Obama’s Council of Economic Advisers estimates that 30 percent of U.S. healthcare expenditures do not contribute to positive healthcare outcomes (Romer, 2009). Inappropriate and unsafe care and waste probably make up the greater part of this estimate, representing costs
in the hundreds of billions nationally. In 2002, Virginia Mason Medical Center (VMMC) adopted a production system methodology, based on the Toyota Production System, to relentlessly improve quality and safety (BenTovim et al., 2008; Choe et al., 2008; King et al., 2007; Muder et al., 2008; Persoon et al., 2006; Raab et al., 2006; Wood et al., 2008). Production-system methods such as the VMMC production system reduce turnaround times of lab tests, improve accuracy of thyroid needle biopsies, and improve diabetic blood pressure control. Transformations of large departments or entire systems of hospital care reduce lengths of stay, waiting times for treatment, nurse dissatisfaction, and medicolegal events (Ben-Tovim et al., 2008; Choe et al., 2008; King et al., 2007; Muder et al., 2008; Persoon et al., 2006; Raab et al., 2006; Wood et al., 2008). The VMMC production system employs flow production, mistake proofing, and standard work to achieve these changes.
Flow production Production of small lots of work take place as the needs arise, instead of batch production, which is usually associated with waiting times, delays, errors, and higher costs of work (Virginia Mason Medical Center, 2004). For example, a physician processing a large batch of lab results every half day requires more time than processing two or three results in between patient visits. Additionally, if the assistant sorts the results according to abnormal and normal values before giving them to the doctor, costly delays in action are avoided.
Mistake proofing Devices and practices are refined in order to reduce errors at all levels of care. For example, a photographic “shadow board” of materials and instruments for a procedure prevents delays in procedures and mistakes in their execution. The VMMC health maintenance module sorts through each electronic chart as it is accessed and identifies disease management and preventive testing that is due or overdue.
Standard work Medical steps in care are specified and healthcare team members are trained and audited for performance. The production system ingrains standard work in care processes to prevent errors and sustain savings from redesign. Many errors in medicine are believed to arise from lack of discipline in standardizing work, so providers and medical assistants receive training on standard rooming and visit initiation. They are observed and audited for hand washing, adherence to standard use of the health maintenance module, and standard procedure setup.
The use of production systems to improve outcomes and reduce costs is in its infancy. Even though the literature is limited and no studies detail cost savings, our experience demonstrates that the application of production
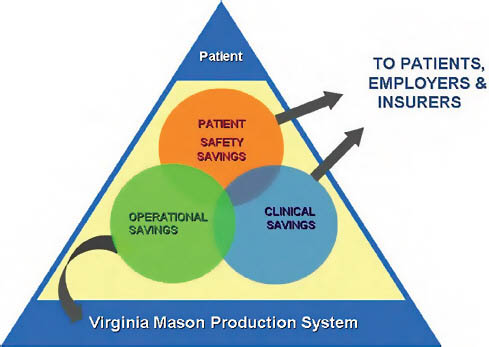
FIGURE 9-1 Savings accrued from the VMMC production system.
SOURCE: Virginia Mason Medical Center.
system methods to healthcare delivery can indeed yield significant savings. These dollar savings can be redirected internally to reinvest or can accrue to patients, their employers, and insurers. The types of savings experienced at VMMC have taken three forms: (1) operational, (2) clinical, and (3) patient safety (Figure 9-1).
Operational Savings
The production system reduces waste (time, space, mistakes) and yields direct savings for VMMC. Examples include
-
Savings of $11 million in planned capital investment over 8 years by using space more efficiently;
-
Savings of more than $1 million (35 percent) over 2 years in VMMC liability and malpractice premium costs since 2007;
-
Margin improvement of $5.6 million over 7 years in the department of gastroenterology as a result of flow production methods;
-
Savings of $2 million in the same department as access to care increased by 50 percent, delaying space expansion;
-
A decrease in cost per relative value unit (RVU) in primary care by 10 percent in 2.5 years, again as a result of flow production, now focused on result reporting, incoming phone calls, and refills; and
-
An increase in percent potential margin for primary care provider practices from 2 percent to 19 percent.
Driven by this production system, VMMC is on track to reach a 2009 margin of $28 million (3.6 percent operating margin) with no layoffs during the recession—a distinction in the healthcare market. These savings can translate to the national level as well.
Extrapolating Nationally
Taking the example of the savings in liability and malpractice premium costs experienced by VMMC, national premiums could drop by 30 percent yielding a savings of $3.2 billion from today’s estimated national cost of $10.7 billion (A.M. Best, 2009). Another dramatic example of potential national savings is in the reduction of cost per RVU. VMMC experienced a 10 percent reduction in its primary care cost per RVU, which at the national level could translate to savings of another $4.3 billion per year.1
Clinical Savings
In collaboration with Boeing, VMMC provided intensive management of 350 patients comprising the top 20 percent of Boeing’s healthcare spending. More than half had diabetes, and more than half had three chronic conditions. The Boeing Intensive Outpatient Care Program followed the VMMC production system to provide patients with standard care management in their medical home, complete with enhanced phone care enabled by a modest per member per month additional reimbursement. The results exceeded Boeing’s goal of a 15 percent reduction in healthcare costs. A 35 percent cost reduction was achieved compared to predictions based on current usual care. The VMMC model surpassed other participating deliv-
ery systems, which used an ambulatory intensive care unit model, disjoining patients from their primary care provider team.
Focusing on redesigned care for diabetes, the VMMC production system specified standard work for diabetic visits with physicians or registered nurses, phone care, pharmacist visits, registry management and pull systems, and evidence-based drug treatment. As a result, the outcomes of this definition of standard work translated into more than just cost savings—the care for diabetic patients has improved markedly since the beginning of this program and has surpassed national averages (Tables 9-1 and 9-2).
Extrapolating Nationally
Continuing with the example of diabetes, where disease management programs are most evolved, national savings could be as high as $35 billion from this effort. Reduction of HbA1c, LDL, and blood pressure are proven to postpone endpoints and may reduce costs (American Diabetes Association, 2002, 2009; McGuire et al., 1998; Sever et al., 2005; Wagner et al., 2001). Additionally, the room for reduction in cost is vast; estimates from 2007 of direct medical costs of diabetes care in the United States totaled $116 billion. A 30 percent savings using integrated care like that used at VMMC might achieve $35 billion in savings. If the Boeing population is representative of the nation’s “sicker,” employed, vascular disease patients,
TABLE 9-1 National and VMMC Outcomes on Quality Metrics, 2008
the savings could be even greater—in excess of $40 billion nationally. This supports Michael P. Pignone’s (2009) estimate of up to $45 billion in savings via disease management programs for complex chronic conditions, including diabetes, congestive heart failure, and post hospital transitions of care.
Patient Safety Savings
Lastly, the VMMC production system reduces costs and improves outcomes by enhancing patient safety in several nationally monitored metrics. This starts with all staff being empowered to call a patient safety alert (Figure 9-2).
As of June 2009, in the last 6 months of monitoring, VMMC patients have experienced no cases of ventilator-acquired pneumonia. In 2003, when we began our improvement efforts, we reported 13 cases. We have also seen reductions in central-line and surgical-site infections. All other patient safety metrics have remained static, leveling our costs (Table 9-3).
Based on these trends, VMMC clinical decision support has conservatively estimated the following percentage reductions in these three adverse events. For ventilator-associated pneumonia, we experienced a marked reduction in the past rolling year; however, we are reluctant to claim a 100 percent reduction. For the purposes of this manuscript we will assume we have a 50 percent reduction since the trend was not linear during 2005-2009. For central-line infection, we are certain of a 56 percent reduction between 2005 and 2008. And for surgical site infection, we are certain of a 39 percent reduction between 2000 and 2008.
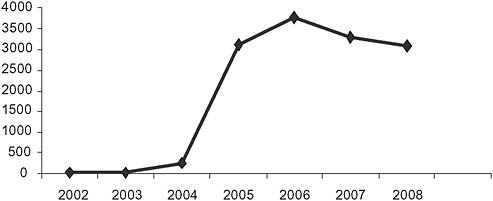
FIGURE 9-2 Reported patient safety alerts by year.
SOURCE: VMMC, 2009.
TABLE 9-3 National and VMMC Trends in Safety Metrics, 2005-2008
|
Safety Indicator |
VMMC 2005 (%) |
VMMC 2008 (%) |
VMMC 2009* (%) |
National (%) |
|
Ventilator-associated pneumonia (% per 100 ventilator days) |
1.79 |
1.97 |
0 |
10-20 |
|
Central-line infection (% per 1,000 central-line days) |
4.81 |
1.62 |
— |
1-5.6 |
|
Surgical site infection (% per 100 procedures) |
4.99 |
0.9 |
0.83 |
0.22-9.9 |
|
*Data through August 2009. |
||||
Extrapolating Nationally
Applying the same trends in the reduction of ventilator-associated pneumonia, central-line infections, and surgical site infections, the VMMC production system experience translates into national savings deliverable to patients, payers, and employers estimated at $4.1 billion.
Summary
Our experience with the VMMC production system suggests production systems can reduce institutional waste and medical errors while improving patient safety. The resultant cost per RVU, capital, and liability cost savings could yield $7.5 billion for medical provider groups. This, plus attendant margin improvement, provide a stable platform for relentless improvement and further savings. For VMMC, a strategy of cost reduction through improving access and quality is more reliable and sustainable than a strategy of revenue enhancement. The sum of the estimated clinical and patient safety savings on a national scale is more than $44 billion. We estimate this figure from a selected set of chronic care model and patient safety improvement yields.
The VMMC production system is the methodology that drives our improvements, providing a model for national savings. We propose that research and promotion of systematized care design and continuous improvement—which we call a production system—become a vital component of healthcare reform. The operating principles of a production system focus our effort on operational, clinical, and patient safety savings through relentless improvement of care—as opposed to relentless expansion of care. Although we know the “end line” in the expansion of medical costs—failure of the U.S. healthcare system—we do not know where it is in waste
reduction and defect reductions in care. It all depends upon how much waste and inefficiency we as a profession are willing to tolerate—or how much systematic improvement and standardization we are willing to build into our work.
MANAGING VARIABILITY IN HEALTHCARE DELIVERY
Eugene Litvak, Ph.D., Sandeep Green Vaswani, M.B.A., Michael C. Long, M.D., and Brad Prenney, M.S., M.P.A.
Institute for Healthcare Optimization
The healthcare delivery system falls short for all stakeholders: patients, providers, and payers. Indeed, despite record-breaking and fast growing costs, today’s healthcare system is still characterized by overcrowded ERs, stressed and overloaded clinicians, unnecessarily low quality of care, and extensive waste. And although many factors have been cited as drivers of this state of affairs, one key driver is often overlooked: unmanaged variability in patient flow.
Artificial Flow Variability
Variability, particularly in the flow of patients through the healthcare delivery process, impedes cost reduction and improvement of patient safety and quality of care (Aiken et al., 2002; Joint Commission Resources, 2009; Litvak, 2005, 2007; Litvak and Long, 2000; McManus et al., 2003). Some patient flow variability is natural, such as the flow of patients admitted to a hospital unit through the ER. However, it is the artificial variability where there is room for improvement. Artificial variability is the result of mismanagement. It is not driven by the timing of patients’ illnesses but by the mismanagement of scheduling and allocating limited hospital resources. Furthermore, it is simultaneously neither random nor predictable (Litvak and Long, 2000). The flow of elective admissions (such as elective surgical, catheterization lab, oncology admissions) to a hospital is just such an example of artificial variability. In fact, it is often comparable if not greater than the natural variability in ER admissions (see elective surgery example in Figure 9-3).
Effects of Artificial Variability in Patient Flow
While the most visible effects of artificial flow variability on hospital function are in ER overcrowding, boarding, and diversion, this unnecessary variation drives problems in quality, capacity, and cost.
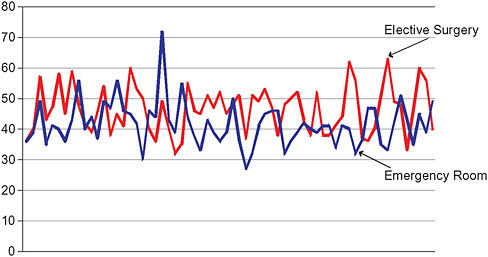
FIGURE 9-3 Daily weekday emergency and elective surgical admissions.
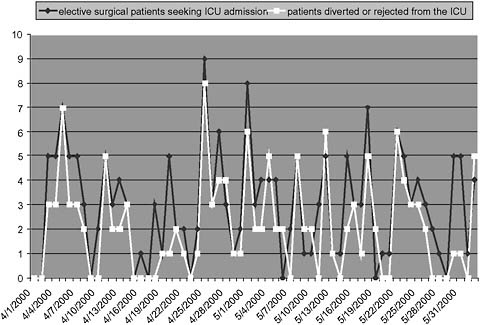
FIGURE 9-4 Elective surgical admission requests vs. patient diversion or rejection from an intensive care unit.
SOURCE: McManus, M. L., M. C. Long, A. Cooper, J. Mandell, D. M. Berwick, M. Pagano, and E. Litvak. 2003. Variability in surgical caseload and access to intensive care services. Anesthesiology 98(6):1491-1496. Reprinted with permission from Wolters Kluwer Health.
Unnecessary competition for inpatient beds Boston Children’s Hospital, (McManus et al., 2003) found that the number of elective surgical patients needing a bed in the pediatric intensive care unit (ICU) was highly correlated with the number of rejections or diversions from that unit (most of the other admissions were from the ER) (see Figure 9-4).
Worse health outcomes driven by extreme fluctuations in patient census Litvak and colleagues (2005) found that when the patient census increased 25 percent above the normal staffing level in an inpatient unit, the mortality risk for all patients jumped by 7 percent. The kind of extreme peaks and valleys in the patient census have real consequences for patients’ health outcomes.
Higher stress and lower satisfaction In addition to these glaring quality of care issues, artificial variability also results in increased staff stress, lower staff satisfaction, and lower patient satisfaction (as a result of delays and unpredictability) (Aiken et al., 2002; Litvak et al., 2005).
Higher costs and diminished access to care Paradoxically, artificial variability leads to both underuse of assets (as measured by inpatient bed occupancy or operating room prime time use) and frequent periods when demand approaches or exceeds capacity. The system-wide effects are unnecessary decreases in throughput and access to care and consequent increases in cost per patient.
Variability Methodology
The size and complexity of healthcare delivery systems makes it impossible to manage operations based on intuition, feeling, brainstorming, and benchmarking. While there is a robust science of operations management, it does not address the problem of artificial variability we see in health care. To address the problems in this system, the Institute for Healthcare Optimization has developed variability methodology. At its core, variability methodology involves identification, quantification, and elimination (i.e., smoothing) of artificial variability so that the smoothed elective flow and remaining naturally variable flow (of unscheduled cases) can be managed based on operations management principles (Joint Commission Resources, 2009).
As mentioned earlier, the primary drivers of artificial flow variability in a hospital setting are scheduled admissions through the operating room, cardiac catheterization labs, and other sources such as medical cancer services. Usually, the operating room is the most significant source of elective admissions to a hospital, which makes it a prime candidate for flow
smoothing, although the same principles apply to the other sources. The Institute of Medicine (IOM) has recognized the importance of variability methodology in making the following recommendation (IOM, 2006): “By applying variability methodology, queuing theory, and the Input-Transform-Outcome Model, hospitals can identify and eliminate many of the patient flow impediments caused by operational inefficiencies.” The American Hospital Association’s Quality Center has also recognized variability methodology as a key principle (American Hospital Association, 2009) for achieving IOM’s six aims for improvement: care that is safe, timely, effective, efficient, equitable, and patient centered.
Evidence of Quality Improvement and Cost Savings
Numerous hospitals have already succeeded in using variability methodology and operations management to increase throughput without addition of commensurate resources and to simultaneously decrease waiting times, particularly for urgent and emergent surgeries. In addition, patient and staff satisfaction has risen, as overtime and cancellations or delays of cases have fallen.
Cincinnati Children’s Hospital Medical Center Weekend waiting time (for urgent or emergent surgeries) decreased 34 percent despite a 37 percent volume increase. Weekday waiting time decreased 28 percent despite a 24 percent volume increase (results for the first 3 months after implementation). Surgery volume has sustained 7 percent growth per year for the last 2 years. The equivalent of one operating room (OR) capacity was freed up in the first year of the project, and OR overtime was down by 57 percent (approximately $0.5 million saved annually). Inpatient occupancy increased from 76 percent to 91 percent. One hundred new beds did not need to be purchased resulting in more than a $100 million savings in capital expense. Patient revenue has increased by $137 million per year (Joint Commission Resources, 2009). And the work satisfaction of the care providers substantially improved (Litvak, 2007).
Boston Medical Center Delayed or cancelled elective surgeries decreased 99.5 percent. Nurse stress was reduced by a half-hour reduction (6 percent) in nurse hours per patient day in one unit ($130,000 annual savings). ER waiting time decreased by 33 percent: a 2.8 hour wait in one of state’s busiest ERs versus waiting 4-5 hours or more for other leading academic institutions in Boston (Litvak, 2007).
Palmetto Health Richland Waiting time for urgent or emergent surgical cases decreased 38 percent while overall surgical volume grew about 3 per-
cent. An annual margin growth opportunity of $8 million per year was created. These results were achieved in less than 1 year (Joint Commission Resources, 2009).
National Opportunity
Until recently, the most common approaches to addressing the problem of hospital overcrowding has been to add more capacity and to decrease the length of the care delivery process, thereby increasing throughput in existing capacity (Litvak and Long, 2000; McManus et al., 2003). However, neither has proven a particularly successful strategy. Although the cost plus reimbursement environment has made adding capacity a common solution to address peaks in patient demand for services, the strategy is far too costly. For example, adding a new inpatient room can cost in excess of $1 million in up-front capital expense and $0.3 to $0.8 million in annual operating expenses (Butterfield, 2007) (Table 9-4). Inpatient discharges grew by about 9 percent from 1997 to 2006 based on Organisation for Economic Co-operation and Development (OECD) Health Data (OECD, 2009). If we were to project a similar growth over the next 10 years and assume inpatient length of stay remains unchanged, we will need to add 75,000 inpatient beds costing about $75 billion up-front, assuming $1 million per bed. Additionally, an annual operating cost of about $10 billion to $32 billion (see Table 9-4) will need to be absorbed by the healthcare system.
Decreasing the length of the care process has been underway for several years, particularly in the inpatient area. But since length of stay is partly determined by factors outside of a department’s control, such as bottlenecks in the downstream patient flow caused by artificial variability, the amount of achievable reduction is limited.
Increasing throughput by eliminating (i.e., smoothing) artificial vari-
TABLE 9-4 New Capacity Cost Estimates
|
Resource |
Cost |
|
Inpatient beds |
$1 million per bed in up-front capital, $250,000-$800,000 annual operating expense |
|
Operating rooms |
$2-$7 million per OR in up-front capital, $250,000 or more in annual operating expense |
|
Major imaging: CT, MRI, PET/CT, etc. |
Approx. $1 million or more in up-front capital |
|
Cardiac catheterization |
Approx. $2 million or more in up-front capital |
|
NOTE: CT = computed tomography; MRI = magnetic resonance imaging; PET/CT = positron emission tomography/computed tomography. |
|
ability in the flow of scheduled patients is a far more viable solution. To develop a preliminary national cost savings estimate, we took the example of inpatient beds alone. If all of the admissions to a hospital came through the ER and hence were random in nature, queuing theory would suggest that inpatient bed occupancy can be increased from the current 65 percent to 80 percent without creating excessive waiting times (Litvak, 2005). If a hospital has a significant portion of elective admissions, bed occupancy could be increased to more than 90 percent by smoothing artificial variability (Litvak, 2005).
Even if occupancy were to be increased only to 80 percent by closing unneeded beds, our preliminary estimate for nationwide annual savings opportunity is in the range of $35 billion to $112 billion (Table 9-5). If demand grows by 10 percent over the next 10 years, we would otherwise need to add about 75,000 beds nationwide, for an additional annual cost burden of $12 billion to $35 billion (see Table 9-4). But by employing these smoothing methodologies to eliminate artificial variability, we can completely obviate the need for this cost over the next decade.
More study is needed to refine these cost-saving estimates, and we present these with several caveats. First, we assume that current staffed beds are indeed fully staffed. If 5 percent of the staffed beds are actually not staffed, then the savings estimate without growth would decrease from $35 billion to $112 billion to $26 billion to $82 billion per year. Second, while the estimates here reflect only inpatient beds, other opportunities for cost savings can be found in clinics, ambulatory surgery centers, and post acute care facilities.
Policy Implications
The policy implications for the employment of variability methodologies are compelling. It is a key tool for policy makers and other healthcare leaders in tackling a number of major operational and cost burden issues in this system.
Staffing At least some, and potentially a large part of, clinical staff shortages are driven by inefficient use of personnel. Several attempts to mandate or control nurse-to-patient staffing ratios have not fully succeeded and are unlikely to succeed without smoothing out artificial variability.
Physical assets Addition of new facilities adds significantly to the national healthcare cost burden. It is most prudent to ensure that current assets are being efficiently used before making the significant investments required to increase physical assets.
TABLE 9-5 Preliminary Cost Saving Estimates from Management of Variability in Healthcare Delivery
|
Beds (year 2007 excluding nursing home units)a |
|
743,401 |
|
Occupancyb |
|
65% |
|
Current staffing (assumed) |
100% |
743,401 |
|
Beds used |
|
482,379 |
|
Beds needed based on queuing assuming all random demandb |
80% |
602,973 |
|
Cost saving from current base assuming no growth |
|
|
|
Number of beds that can be “un-staffed” |
|
140,428 |
|
Annual Operating Cost per bed and percent variable (alt. 1)c |
100% |
250,000 |
|
Annual Operating Cost per bed and percent variable (alt. 2)d |
100% |
800,000 |
|
Annual savings estimate 1 ($ M) [A] |
|
35,107 |
|
Annual savings estimate 2 ($ M) [B] |
|
112,342 |
|
Growth scenario |
|
|
|
Projected 10 year total growth |
|
10% |
|
Total Occupied beds needed |
|
48,238 |
|
Number of beds needed at 80% |
|
60,297 |
|
Number of new beds that would be needed at current occupancy |
|
73,340 |
|
Staffed beds at current levels (number of beds) |
|
73,340 |
|
Cost saving from current base assuming growth |
|
|
|
Beds needed per year ( @ 80% occupancy) |
|
6,030 |
|
10 year Average annual operating cost estimate 1 ($ M) [C] |
|
8,291 |
|
10 year Average annual operating cost estimate 2 ($ M) [D] |
|
26,531 |
|
10 year Average annual savings estimate 1 ($ M) [E=A-C] |
|
28,816 |
|
10 year Average annual savings estimate 2 ($ M) [F=B-D] |
|
85,811 |
|
Cost saving from trend assuming growth |
|
|
|
Beds added per year ( @ current occupancy) |
|
7,434 |
|
Capital cost ($ M based on $1M per bed)d |
|
7,434 |
|
10 year Annual depreciation cost assuming 15 year amortization |
|
496 |
|
Total 10 year depreciation expense |
|
27,258 |
|
Annual amortized capital over 15 years ($ M) [G] |
|
2,726 |
|
10 year Average annual operating cost estimate 1 ($ M) [H] |
|
10,222 |
|
10 year Average annual operating cost estimate 2 ($ M) [I] |
|
32,710 |
|
10 year Average annual savings estimate 1 ($ M) [E+G+H] |
|
39,764 |
|
10 year Average annual savings estimate 2 ($ M) [F+G+I] |
|
121,247 |
|
aAHA 2007 data. bLitvak Ph.D., Eugene, Optimizing Patient Flow by Managing its Variability, Front Office to Front Line, Joint Commission Resources. cACP Hospitalist, December 2007, A new Rx for crowded hospitals: Math, Stacey Butterfield interviews Eugene Livak, Ph.D. dEstimate based on IHO experience. |
||
Healthcare information technology (IT) Although significant investment is being directed toward clinical IT, we should not lose sight of what can be achieved by focusing also on operational (i.e., administrative) IT systems. For example, data on waiting times throughout the care delivery process are virtually unobtainable, thereby masking inefficiencies and making it harder to redesign operations. Unlike clinical IT, operational IT systems already exist; they just need to be directed to measure appropriate statistics.
Cost saving from managing clinical variability Efforts to contain use based on clinical variability are not sufficient as a strategy for cost containment. Cost savings necessitate addressing both clinical and artificial flow variability to decrease excess capacity in the healthcare system. Variability methodology and operational management complement comparative effectiveness research and other efforts to reduce clinical variability to realize cost savings in the near future.
Opportunities for Implementation: Short- and Long-Term Goals
The core principles of variability methodology have been well established and proof of the concept has been demonstrated. Once hospital executives and physician leaders are educated about variability methodology and operational management and the process changes involved, they typically become strong advocates. The main missing ingredient for large-scale adoption is the lack of technical expertise and educational resources for hospitals interested in these methods. The newly established Institute for Healthcare Optimization aims to train 10 percent of U.S. hospitals in application of variability methodology over the next 5 years. In the long run, variability methodology should become the standard for design and improvement of healthcare delivery systems.
COST SAVINGS FROM MANAGING HIGH-RISK PATIENTS
Timothy G. Ferris, M.D., M.P.H., Eric Weil, M.D., Gregg S. Meyer, M.D., M.Sc., Mary Neagle, M.P.H., James L. Heffernan, M.B.A., and David F. Torchiana, M.D.
Massachusetts General Hospital2
In all the current attention to healthcare costs, the concentration of healthcare costs among a relatively small fraction of patients presents one
of the most attractive opportunities for savings. Conventional wisdom suggests that a significant fraction of the costs of care of these patients reflects inefficient delivery and poor coordination of care. Despite the recent interest, efforts to better manage the care of the highest-risk patients are decades old, and the results have been mixed.
“Carve-outs,” including Medicare’s Program for All-Inclusive Care for the Elderly (Blumenthal and Buntin, 1998), have effectively contained costs among high-risk Medicare patients, but this approach has not been widely adopted (Gross et al., 2004). Working within the fee-for-service system, commercial insurance companies have approached cost reduction among the chronically ill primarily through nurse-based telephonic coaching services. Regardless of the effectiveness of these approaches, about which there is some debate, the applicability of these approaches to Medicare patients is unclear. Commercial populations have much lower costs than Medicare patients, and their costs are not as concentrated among a relatively small proportion of beneficiaries because commercially insured patients, generally being younger, are much less likely to have multiple chronic conditions. Delivery systems that operate within a budget (such as Kaiser Permanente and Group Health of Puget Sound) deploy care coordination services for high-risk patients, but because such services are not covered by conventional Medicare it is rare to find them in our predominantly fee-for-service delivery system. Care coordination services for high-risk patients are a key component of so-called medical home proposals.
Research on care coordination programs has shown mixed results; this highlights the difficulty of effectively improving quality and simultaneously reducing costs (Bott et al., 2009; Holtz-Eakin, 2004; Peikes et al., 2009; UnitedHealth Group, 2009). Explanations for the mixed results have included the heterogeneity of the interventions, numerous technical difficulties associated with conducting high-quality research on this topic, as well as the difficulties in effectively executing care coordination programs. Cost savings from care management requires the successful execution of a series of steps: (1) identification of patients who will eventually be high cost, (2) engagement of those patients in care management, (3) identification of the patient’s needs, and (4) effectively addressing the patients’ needs. As Eisenberg noted in his model of effective service delivery (Eisenberg and Power, 2000), imperfections at any of these steps will degrade the effectiveness of the service. Experience has shown that although a number of programs have done well with some of these steps, executing effectively on all is difficult (Ayanian, 2009).
CMS Demonstration at MGH
As part of their efforts to develop better systems of care delivery, Massachusetts General Hospital (MGH) and the Massachusetts General Physician’s Organization (MGPO) jointly applied to participate in the CMS Care Management for High Cost Beneficiaries demonstration (CMS, 2005). This 3-year demonstration was designed to identify effective models of care delivery for high-risk patients. Key terms of the demonstration agreement were (1) MGPO would be paid a monthly management fee ($120) for each enrolled patient, (2) the patients would continue to participate in their usual fee-for-service care leaving primary care relationships intact, and (3) MGPO would need to achieve 5 percent savings on the identified population in addition to covering the costs of the management fees. (The determination of savings was based on a comparison with a case-matched control group selected from other Boston academic medical centers and adjusted for baseline differences.)
This report provides a high-level description of the selection of patients and controls, the intervention and some preliminary results. A more detailed report is expected to be available in 2010.
The decision to participate included the assessment of several variables, but most importantly the hospital and physicians needed to know what fraction of the high-risk patient’s total costs was generated from care provided by MGH and the affiliated physicians. Given the fact that these patients could choose to receive their care anywhere, it was important to know that a substantial fraction of their costs was for care provided in a setting that the hospital and physicians could control. An analysis of preliminary data suggested that (1) the more expensive the patient, the higher proportion of care they received at MGH, and (2) for the highest-risk patients an average of 65 percent of their costs were from care delivered within MGH.
Selection of Intervention and Control Patients
We included the Medicare patients of all 19 of our primary care practices (190 internal medicine physicians). Medicare identified potentially eligible patients using the provider tax identification numbers of the MGH physicians and applied several inclusion and exclusion criteria (Figure 9-5). The claims of all 15,230 patients were placed in an analytic database. Table 9-6 shows the distribution of the patients by risk, using the Centers for Medicare & Medicaid Services (CMS) Hierarchical Condition Category (HCC) risk adjustment system (Pope et al., 2004), and cost. The shaded cells indicate the risk and cost strata of the 2,619 patients chosen to participate in the demonstration project.
Who were these patients? On average they were 76 years old and
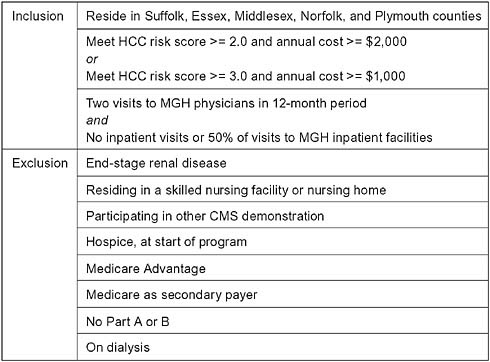
FIGURE 9-5 Participation criteria.
51 percent female. A significant fraction (11 percent) were under 65 years old and qualified for Medicare based on a disability. These patients averaged 3.4 acute care hospitalizations per year and had 12.6 active medications on their medication list. The eligible high-risk patients had average annual costs of $22,520 and total costs of $58,716,619 in the year prior to enrollment. When presented with the list of their own eligible patients, MGH physicians responded that the eligible patients were indeed among the sickest, most complex, and highest-risk patients in their panel.
Comparison group patients were selected from patients that visited other Boston medical centers and met the inclusion and exclusion criteria. Instead of using physician identifiers to attribute patients to these centers, we used an algorithm that relied on the frequency of physician visits. Once the pool of eligible comparison patients was identified, the comparison patients were selected using a matching process that included criteria based on age, sex, several common chronic conditions, risk score, and cost.
TABLE 9-6 The Number of Patients Falling Within Incremental Units of CMS-HCC Risk Score* and Costs for the Eligible Population. Shaded Cells Identify the Risk and Cost Cells from Which the Eligible Patients Were Selected for the MGH Program
MGH Care Management Program
The program enrolled patients using a combination of welcome letters, phone calls, and face-to-face meetings in physician offices. Among the 10 percent of eligible patients who declined to enroll, the most commonly stated reason was that the additional services were not necessary. Enrollment calls from the physician’s office and the physicians themselves were particularly effective, distinguishing this program from outreach under some other demonstration where no prior relationship with the beneficiary exists.
The intervention principally relied on the assignment of a nurse care manager to each of the enrolled patients. Each group of practicing physicians was assigned a care manager who worked directly with the physicians in their offices and managed the care of about 200 patients. Using a large-scale customization approach, each patient’s needs and care barriers were assessed, and interventions were tailored to meet their care needs or address their barriers to care. The major types of interventions included in the MGH Care Management Program are:
-
Annual nurse assessment and care plan review with an MD,
-
Telemonitoring for appropriate patients,
-
Surveillance calls,
-
Regular pharmacy review,
-
Assistance with transitions from home to hospital or hospital to home,
-
Advanced directives and end-of-life counseling,
-
Facilitated communication among care team members,
-
Urgent response and facilitated office access, and
-
Psychosocial evaluations and management.
Even with this list, care managers had considerable flexibility to be creative in addressing their patients’ care coordination issues. Physicians were paid a small management fee to cover the additional time they spent with the care managers, though as the program progressed they found that the care managers actually saved them time.
The program used information technology in three distinct ways. First, all physicians within the organization used an electronic record allowing real-time communication of changes in patient status or care plans. We facilitated communication by adding an icon to the electronic records of all enrolled patients. The icon identified the patient, the care manager, and the care manager’s contact information. Second, administrative systems allowed for tracking of patients, management of care manager workflow, and automatic notification of physicians and care managers of the arrival
of an enrolled patient in the ER. Third, data from care management systems and administrative systems were loaded into an analytic database on a weekly basis to create a performance dashboard that allowed tracking of trends in use.
Experience and Preliminary Results
After 3 years of operations and 2 years and 9 months of claims data there has been sufficient experience and data to make some preliminary statements about the performance of the program. On the operational side, the program appeared to perform well on the criteria for success noted above. The patient selection process using billing data correctly identified high-risk patients with significant ongoing healthcare needs. The high patient enrollment (90 percent), completion of assessments on all patients, and high contact rates between care managers and enrolled patients suggest that opportunities for care coordination were identified. The high retention of care managers (100 percent) and survey results indicating high physician satisfaction suggest the program was well integrated into the fabric of the organization.
Monitoring reports from CMS indicated that the intervention group had consistently lower costs and fewer admissions than the comparison group even after adjusting for baseline differences and trimming of outliers (Table 9-7). Costs of the eligible intervention population initially increased compared to the comparison population, but after 6 months the intervention group costs were consistently below the comparison group costs.
The following results include all eligible patients (intention to treat) and adjust for baseline differences between the intervention and comparison groups (difference in differences). The program reached the break-even point (savings in the claims experience of the intervention group exceeded the management payments from CMS) at 16 months. The cumulative savings at the end of 2 years of operations was $6 million, which represented 4.3 percent savings after covering the costs of management fees. During the third year of operations for which we have completed claims information (9 months), the cumulative savings after fees was 4.7 percent (savings peaked midway through the third year at 5.8 percent). This performance factored into the decision to grant the program a 3-year extension and expand the program to more sites (CMS, 2005). Internal data showed that much of the cost savings came from preventing admissions and readmissions to the hospital. Savings also accrued from increased use of hospice even though mortality in the intervention group was consistently lower than mortality in the comparison group.
A number of challenges related to the specific needs of the patient population and the work of the care managers surfaced during the program. The
TABLE 9-7 Calculation of Cost Savings to MGH Population Based on Savings Achieved Within the Eligible High-Risk Populationa
|
Characteristic |
High-Risk Population, n (%) |
|
Size, N = 15,230b |
2,619 (17.2) |
|
Total costc |
$58,619,716 (58.3) |
|
Various Savings Scenarios |
|
|
Savings on High-Risk Population (% of total population costsd) |
|
|
3 |
$1,758,591 (1.7) |
|
4 |
$2,344,789 (2.3) |
|
5 |
$2,930,986 (2.9) |
|
6 |
$3,517,183 (3.5) |
|
7 |
$4,103,380 (4.1) |
|
aData based on preliminary reports generated after 2.5 years of a 3-year project. bBecause of the way the population was selected, the exact size of the denominator is not known. cAssumes average cost across total population of $6,600 per year per patient. dUses baseline year cost; costs varied over time. eSavings after costs has varied between 3.5 and 6.8 percent over the period for which we have data. fBecause intervention was less costly than control at baseline, and thus potentially more managed, these savings projections may underestimate program savings in less managed populations. gOutlier trimming affected control group more than intervention group so these savings projections may underestimate actual savings. |
|
burden of issues related to mental health and cognitive impairment within this population (>50 percent with some impairment) required shifting resources to increase social services support. End-of-life issues were predictably common in this population (18 percent of the intervention patients died during each of the first 2 years of the program), and the associated care needs are challenging under the best of circumstances.
With regard to the care managers’ work, the patient load for each nurse care manager was relatively high, with an average of 30 active patients at any one time and approximately 170 patients receiving routine surveillance. Weekly case discussions helped the care managers address the unavoidable tension between spending less time with more patients or more time with fewer patients. Care managers also needed to balance time spent building relationships with patients and doctors, with time spent working to address specific patient issues. Finally, the software used for tracking the care manager’s work needed further optimization.
Demonstration leaders noted several opportunities to further improve
care and reduce costs, including incorporating a limited number of home visits (particularly to address urgent issues), improved office access, improved support from care managers during non-business hours, and an exemption from the rule requiring Medicare patients to remain within an acute care hospital for 72 hours before they can be discharged to a sub-acute facility. Admissions from post-acute care settings remained high among the intervention patients and were no better in the intervention than in the comparison group.
Potential Impact on Total Costs of Care
In determining the potential impact on costs of care for the Medicare population cared for at MGH, the first step is to determine the savings for the total population from which the high-risk group was selected. Table 9-7 shows a model for calculating population-level savings from the program. Although our program appears to be delivering net savings of between 4 and 5 percent, in order to provide additional context we show population-level savings of between 3 and 7 percent at 1 percent increments. This relatively simplistic approach to calculating savings has several limitations. Nonetheless, the sensitivity analysis suggests that the program delivers a 1 to 3 percent savings on the population as a whole (the high-risk population plus the population they were selected from).
Estimating the potential impact of similarly structured programs on national Medicare costs may be an illustrative exercise, but also requires additional assumptions.3 These assumptions lead to an estimated savings over a 2-year period of between $604 million and $1.5 billion.
Policy Considerations
The apparent success of the MGH Care Management Program suggests that prospective payment for the enhanced management of high-risk patients holds some promise for reducing costs. Nonetheless, several important considerations limit the translation of this demonstration to policy. First, MGH has several uncommon characteristics that may limit
|
3 |
We used a relatively simple model that shows 1.6 percent population savings (from Table 9-6) and 45 million Medicare beneficiaries with an average annual cost of $7,000. We also estimated (1) the size of the Medicare population receiving care within an integrated delivery system, and (2) the proportion of those integrated delivery systems that have the necessary information technology infrastructure. Both of these variables are currently in flux, and their rate of change will depend on future policy decisions, but for the sake of this exercise we assumed that between 40 percent and 60 percent of the U.S. population could receive care within an integrated delivery system and that between 30 percent and 50 percent of these delivery systems would have the required information technology infrastructure. |
the generalizability of the program. Important among these characteristics are the integration of physician and hospital services, universal use of an electronic medical record, advanced clinical and administrative information systems, an extensive primary care network, and a full range of acute and chronic care services. On the other hand, the lower baseline costs of the intervention population may suggest that the MGH patients were relatively well managed prior to the start of the program, possibly indicating that there is even greater opportunity in less well-managed populations. In addition, recent research suggests that the infrastructure required for operating this type of program is increasing among large physician organizations (DesRoches et al., 2008; Shortell et al., 2009). Also, the results described here are consistent with those found in a similar trial conducted at Johns Hopkins (Leff et al., 2009).
Unlike most proposals to fund the infrastructure for medical homes, of which care coordination of high-risk patients is a key component, the MGH program included financial risk for the management fees. Whether or not financial risk is an essential element of this type of care management program remains unclear though it would certainly be possible to put in place the infrastructure for care management without effectively reducing costs. Future demonstrations will be necessary to clarify or resolve these questions.
HEALTH INFORMATION EXCHANGE AND CARE EFFICIENCY
Ashish Jha, M.D., M.P.H.
Harvard University
It is widely believed that the adoption of electronic health records (EHRs) and the development of an interoperable health information infrastructure that facilitates the flow of clinical and administrative data throughout the healthcare delivery system is critical to realizing healthcare cost savings, increased efficiency, and improved quality of care. Federal (and state) policy makers are increasingly promoting health information exchange (HIE), recently investing nearly $30 billion to the Department of Health and Human Services in the American Recovery and Reinvestment Act of 2009 to spur adoption and promote the meaningful use of health information technology. Currently, over 30 billion healthcare transactions occur each year in an expensive, fragmented delivery system; most of these transactions are still conducted by phone, fax, or mail (Menduno, 1999). The lack of coordination and electronic data sharing between healthcare entities accrues large administrative costs and results in the absence of clinical information at the point of care. These system deficiencies yield redundant tests, unnecessary or harmful care that is often expensive, and
unnecessary hospitalizations that promote substantial wasteful expenses to the delivery system.
Although robust empirical data on the potential cost savings attributable to interoperable electronic health records and HIE is limited, studies indicate that substantial savings may be accrued while improving patient care if these systems are widely adopted and effectively used.
Effectiveness of EHRs and HIE
The 2005 Health Affairs publication by Richard Hillestad and colleagues presents the most comprehensive estimate of the potential national health benefits, savings, and costs from adoption and implementation of effective interoperable EHR systems (Hillestad et al., 2005). Projected savings are approximately $81 billion annually through improvements in healthcare safety and efficiency. The largest cost reductions were found from reducing hospital lengths of stay ($19.3 billion), nurses’ administrative time ($7.1 billion), drug usage in hospitals ($2.0 billion), and drug ($6.2 billion) and radiology usage ($1.7 billion) in the outpatient setting. Computerized physician order entry was projected to avoid 200,000 adverse drug events in the inpatient setting and 2 million adverse drug events in the ambulatory setting, yielding an annual savings of $2 billion and $3.5 billion, respectively. However, the majority of savings would not be immediately realized and require successful system implementation and appropriate process changes. These savings did not focus on electronic health information exchange per se.
A more targeted modeling exercise was performed by Jan Walker and colleagues, who estimated that the implementation of standardized, encoded, electronic HIE infrastructures would lead to $337 billion in savings over a 10-year implementation period (Walker et al., 2005). Savings after the 10-year implementation period are projected to equal $77.8 billion per year (2003 dollars). The savings will be achieved primarily through two mechanisms: (1) reducing administrative burden of paper-based data exchange (e.g., sending laboratory results, chart requests, and referrals), and (2) decreasing redundant tests (e.g., laboratory and radiology tests).
Despite unclear evidence of the cost savings of HIE, the adoption of a strategy for widespread HIE infrastructure is critical and will certainly promote numerous clinical benefits that were not included in the estimates by Hillestad or Walker. Such clinical gains include improved access to longitudinal patient data across providers, reduced fragmentation of care, better communication among providers, more robust referral processes, and earlier recognition of emerging disease outbreaks.
Primary Caveats and Assumptions
Despite the best efforts of the studies mentioned above, each contains limitations. The lack of strong evidence led Hillestad and colleagues to base savings, costs, and benefits projections on the adoption and effective use of an interconnected, interoperable EHR system, and thus report savings that would only accrue if pivotal delivery system changes occur. Further, the cost projections assumed that 20 percent of hospitals had adopted an EHR system. However, new data suggests that this figure is only 7.6 percent for a basic EHR and 1.5 percent for comprehensive EHRs, yielding larger adoption costs than included in projections (Jha et al., 2009). Savings that would result from less expensive transactions, reductions in malpractice costs, and public health savings, as well as certain domains such as long-term care, were also not included in the model. Technological advancements of more effective and efficient systems since the article’s publication may contribute to an understatement of savings. Results above the mean were also not reported, suggesting that the projected annual savings of $81 billion may be conservative. Monte Carlo simulations were used to account for variations in the data and to compensate for some weaknesses in the data. Yet, they assumed that benefits would be achieved by all newly adopting organizations, regardless of the presence or lack of the pivotal process and organizational changes that drive effectiveness.
Because of a dearth of empirical data on the value of HIE, estimates by Walker were based on expert consensus, which produces weak data. However, their projection that 14.3 percent of all tests are redundant, based on two small, single-institution studies have gained traction, because this estimate has significant face validity. The analysis model also included an expert-panel estimate of the administrative cost incurred per laboratory or radiology test to be $19.25, which is almost surely higher than the actual figure. The approach employed a static model that fails to consider that ease of ordering and receiving tests, which occurs when there is widespread deployment of EHRs and HIE, may encourage increased testing. Together, these factors may inflate overall savings projections. However, potentially important costs and benefits were not included in the model, such as increased access to clinical data and reduced fragmentation of care, suggesting that a fully standardized HIE network is likely to yield considerably larger savings than projected.
Current Strategies for HIE
The framework for a comprehensive HIE strategy may be developed from a regulatory approach, a market-based approached, or a combination of the two. To date, the main mechanisms for HIE in the United States are regional health information organizations (RHIOs) that use a
market-based approach. RHIOs bring together independent entities in a defined geographic region to create networks that will set up an electronic health information infrastructure. RHIOs’ efforts are focused on convening stakeholders, determining a governance approach, securing funding, designing and implementing technical infrastructure, launching the organization itself, building a sustainable business model, and planning for long-term growth.
A recent Health Affairs publication describes the current state of RHIOs in the United States, based on a survey of all identified RHIOS between January 2001 and June 2009 (Adler-Milstein et al., 2009). As of June 2008, there are 131 RHIOs, of which only 44 are operational and actively exchanging clinical data. The data exchanged by RHIOs falls short of comprehensive data exchange and are predominately limited to test results (84 percent of RHIOs exchanging data), inpatient data (70 percent), medication histories (66 percent), and ambulatory data (64 percent). Operational RHIOs commonly use time and in-kind resources, recurring fees, and grants as means of financial support. However, the majority are unable to remain financially self-sustainable as indicated by a high failure rate of 20 to –25 percent. RHIOs most commonly identified a lack of funding as a barrier to development, followed by privacy and security concerns, unexpectedly high costs, and competition. The survey found that characteristics associated with operationally successful RHIOs included convening a broad group of stakeholders and exchanging narrow types of data. Financially viable RHIOs were commonly associated with securing early financial support from participating organizations, relying on no or little grant support, and providers acting as the primary data recipients.
The sixth annual eHealth Initiative’s survey of the state of HIE identified 193 HIE initiatives in 2009, of which 57 are operational and exchanging data (eHealth Initiative, 2009). The survey reports substantially increased interest and progress of HIE efforts to improve efficiencies and quality of care in all 50 states and the District of Columbia. Results indicate that operational HIEs reported cost savings for multiple stakeholders, positive impacts on physician practice, increased focus on addressing privacy and security concerns, and decreased dependence on federal funding.
These data and a lack of interoperable standards are reason for concern if the United States decides to continue using the current RHIO model as a viable strategy for effective, sustainable growth.
Next Steps
Eliminating the waste associated with the billions of paper-based transactions that occur each year in a fragmented U.S. healthcare delivery system could save the system tens if not hundreds of billions of dollars each year. The best estimate to date places savings at $77.8 billion annually, or ap-
proximately 5 percent of all healthcare spending. To achieve savings like these, we need greater standardization of data, substantial interest in HIE by providers and the public to drive interoperability, and both quality and cost metrics that hold providers accountable for providing efficient, high-quality care. The National Health Information Network (NHIN) aims to provide a national health information infrastructure and develop standards for secure data exchange (Department of Health and Human Services, 2009b). The American Recovery and Reinvestment Act specifically allocated $300 million to support HIE efforts at the regional level (111th Congress, 2009). Furthermore, CMS will provide reimbursement incentives to hospitals and providers who are able to demonstrate “meaningful use” of EHRs through stimulus funds. The definition of meaningful use, currently being developed by the Office of the National Coordination for Health Information Technology, will require EHRs to be interoperable and able to “exchange meaningful clinical information among professional healthcare teams” (Department of Health and Human Services, 2009a).
The federal efforts will likely spur adoption rates, yet the state of the most prevalent HIE strategy in the United States causes reason for concern. Direct funding of RHIOs appears to be problematic, and policy makers will need to design a multifaceted approach to overcome financial issues for long-term success. To date, providers have little incentive to use data from outside sources even when available as these data are not integrated into the clinical workflow and thus lead to additional work. Further, which stakeholders accrue financial benefits from HIE is ambiguous in their current form. New payment reform models, such as patient-centered medical homes or accountable care organizations, are salient sources for integrating HIE at the point of care. The formation of a national strategy and standardized infrastructure protocols, as well as the ability for healthcare reform efforts to catalyze changes in the delivery system, will drive the success of HIE and its ability to improve patient outcomes while concurrently eliminating inefficiencies and saving billions of dollars.
ANTITRUST POLICY IN HEALTH CARE
Roger Feldman, Ph.D., M.S.
University of Minnesota
The two major federal antitrust laws are the Sherman Act (1890) and the Clayton Act (1914). Section 2 of the Sherman Act, prohibiting monopolization and attempts to monopolize, is intended to prevent monopoly power in a single firm. It does not prohibit monopoly gained passively or by merit (e.g., by being more efficient), only monopoly gained by acts that involve misconduct or coercion. Section 7 of the Clayton Act prohibits
mergers and acquisitions that may substantially lessen competition or create a monopoly. States in turn have their own antitrust laws patterned after the Sherman and Clayton Acts. Federal antitrust laws are enforced by the Department of Justice (DOJ) and the Federal Trade Commission (FTC).
The mechanisms used for antitrust enforcement today are driven by lesser known but important laws and regulations. The Hart-Scott-Rodino Act, passed in 1976, mandates that parties to certain mergers must notify the FTC and DOJ in advance of the merger and cannot close the transaction until one of the agencies has evaluated its effect on competition. The Hart-Scott-Rodino Act guarantees premerger review of many proposed mergers, but its financial trigger for premerger notification—indexed by the change in the gross national product (GNP) and equal to $130.3 million in 2009—is too high for many healthcare mergers.
Another antitrust tool is the business review letter, in which the parties to a proposed business practice request a prior opinion from the DOJ regarding whether it would challenge the proposed merger. Business review letters have been used in mergers involving physician groups.
Rising Prices, Falling Quality
Antitrust is important in hospital markets, as we see from the experience of the 1990s (Figure 9-6). In 1990, the average American lived in a city with a “moderately concentrated” hospital market, according to a widely used measure known as the Herfindahl-Hirschman Index or HHI (the HHI is the sum of squared market shares of the hospitals). By 2003, the HHI for those same cities had escalated to “highly concentrated” because of mergers and acquisitions.
Econometric estimates indicate that this increased concentration and, by extension, hospital mergers increase prices by between 5 and 40 percent (Vogt and Town, 2006). Estimates based on actual mergers (known as “event studies”) indicate prices increased by at least 10 percent following actual mergers, compared with prices at hospitals that did not merge. As these price increases translate into higher insurance premiums, mergers disproportionately hurt minorities and lower-income communities, as more and more people cannot afford insurance coverage (Town et al., 2007). Other evidence suggests that quality suffers as well; the quality of care for Medicare patients with acute myocardial infarction has been found to suffer as a result of hospital mergers (Kessler and McClellan, 2000).
Combining the data in Figure 9-6 with the median assessment of the effect of hospital mergers on prices, it is possible to conclude that hospital mergers from 1990 to 2003 raised prices by approximately 7.5 percent. Given that the demand for hospital care is highly price inelastic and that hospital spending accounted for 37 percent of personal healthcare spending
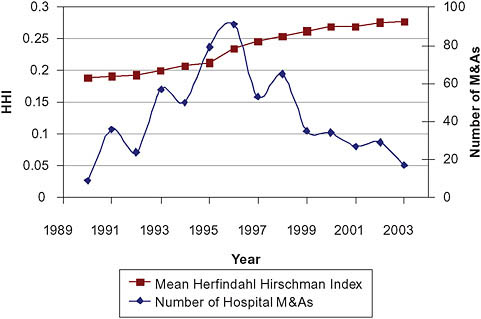
FIGURE 9-6 Hospital Mergers and Acquisitions and Market Concentration, 1990-2003.
SOURCE: Town, R. J., D. R. Wholey, R. D. Feldman, and L. R. Burns. 2007. Hospital consolidation and racial/income disparities in health insurance coverage. Health Affairs (Millwood) 26(4):1170-1180. Reproduced with permission from Wolters Kluwer Health.
in 2007, hospital mergers from 1990 to 2003 added about 2.75 percent to personal health spending in 2007.
Some of this increase in spending could have been offset by increased efficiency that would reduce costs after a merger. However, to achieve efficiency gains, hospitals would need to consolidate their services more fully, and the business incentives of mergers do not favor such consolidation. To the contrary, merged hospitals can increase their bargaining power vis-à-vis managed care plans by unconsolidating and locating some services exclusively in each hospital, thereby making both hospitals essential to include in the plans’ provider networks.
Despite the importance of hospital mergers, the FTC and DOJ were singularly unsuccessful in five challenges to hospital mergers from 1995 through 1999 (Table 9-8). In three cases, federal courts held that the mergers would not lessen competition because the geographic market was very large; in one case the court decided there was no danger of monopoly because the product market was very broad; and in another case the court accepted flimsy evidence that a merger of two nonprofit hospitals was ac-
TABLE 9-8 Hospital Merger Challenges, 1995-1999
|
Setting |
Year |
Reason for Court’s Rejection of Government Case |
|
Jopkin, MO |
1995 |
Large geographic market |
|
Dubuque, IA |
1995 |
Large geographic market |
|
Grand Rapids, MI |
1996 |
Not-for-profit hospitals |
|
Long Island, NY |
1997 |
Broad product market |
|
Poplar Bluff, MO |
1997 |
Large geographic market |
|
SOURCE: Haas-Wilson, 2003. Reprinted by permission of the publisher from MANAGED CARE AND MONOPOLY POWER: THE ANTITRUST CHALLENGE by Deborag HaasWilson, p. 91, Cambridge, Mass.: The Harvard University Press, Copyright © 2003 by the President and Fellows of Harvard College. |
||
ceptable even if it created market power because nonprofit hospitals would not abuse such power. Other hospital mergers have been allowed to proceed with “community payments” (e.g., the hospitals promise to provide more charity care). Yet, such promises are very difficult to enforce.
The Changing Tide
The tide has recently begun to turn. In 2004, the FTC challenged a merger of two hospitals in suburban Chicago, Illinois, that had occurred 4 years earlier. Although an administrative law judge ordered the merger dissolved, the FTC eventually decided that it was tolerable provided the hospitals set up separate teams to negotiate contracts with insurers (FTC, 2008a). In a second case involving a proposed hospital merger in northern Virginia, the parties called off the merger after the FTC announced that it would undertake a full administrative hearing of the matter (FTC, 2008b).
These cases, known respectively as “Evanston Hospital” and “Inova,” have demonstrated the FTC’s willingness to use its internal administrative processes to challenge hospital mergers rather than seeking relief through the federal courts. While the Evanston Hospital remedy is disappointing, the two recent cases set a precedent that may undo the deleterious effects of previous government failures to prevail in hospital merger cases.
Physician and Health Plan Mergers
While there are no national data on physician market structure levels and changes, there is plenty of anecdotal evidence that physicians have market power. For example, physician groups are threatening to withdraw from health plans’ provider networks unless their payment demands are met (Strunk et al., 2001). Nevertheless, the FTC and DOJ have not chal-
lenged any physician merger (although they have blocked attempts by physicians to fix prices). Despite the lack of formal challenges, the DOJ’s business review letters have established guidelines that indicate it will define the geographic market for physicians’ services locally and the product market narrowly.
The DOJ has prevailed in three mergers involving health plans: Aetna-Prudential (1999); UnitedHealth Group-Pacificare (2005); and United-Health Group-Sierra Health Services (2008) (DOJ, 1999, 2005, 2008). These cases have established clear rules for defining geographic markets for health plan merger cases: managed care plans require local provider networks, and plans located outside the local area (generally a metropolitan statistical area [MSA]) are not a competitive constraint to a merger.
Unanswered Questions
In a vertical merger, the merging firms are located “upstream” and “downstream” in a production process; for example, a hospital (downstream) may acquire a physician group (upstream). The economics and law of vertical mergers are not settled. On one hand, vertical mergers may increase efficiency. This is the idea behind proposals to create “accountable care organizations” (Fisher et al., 2009). On the other hand, vertical mergers may increase market power and lead to exclusion of competitors. The FTC and DOJ view vertical mergers using the rule of reason, and it remains to be seen whether this standard will be successful or not at protecting the quality and pricing of health services. The rule of reason in antitrust policy stipulates that monopolies or otherwise larger companies are not intrinsically illegal or anticompetitive. The question is whether they unreasonably restrain trade.
Limitations of Antitrust Policy
As already suggested, antitrust policy in health care has several significant shortcomings. Antitrust cases are long, complex, and expensive, and the outcome is subject to the whim of a court. Enforcement agencies have a poor track record in opposing hospital mergers and have not challenged a single physician merger. Most troublesome, healthcare mergers may be too numerous for antitrust to be a meaningful strategy. Health care is a local industry; in many markets physicians and hospitals have high market shares, making almost every merger potentially anticompetitive, yet they are too numerous to challenge.
However, short of government price controls and monopsony buying power, antitrust policy is the only recourse for controlling healthcare pric-
ing. The following reforms could make antitrust enforcement policy more effective:
-
The Hart-Scott-Rodino financial triggers for healthcare mergers should be lowered. This would allow mergers to be challenged before the fact when it is easy to prevent them, rather than after the fact when it is hard to dissolve them.
-
Federal and state agencies should coordinate their antitrust actions. In particular, state agencies should pursue local mergers, leaving the FTC and DOJ to investigate national consolidations. State attorneys general should be allowed to conduct administrative reviews of mergers, and the FTC and DOJ should not approve a proposed merger while the state agency is investigating.
-
The FTC and DOJ should challenge physician mergers such as the merger of two large, single-specialty physician groups in a midsize city.
-
The agencies should be prepared to insist on divestiture as a merger remedy.
-
The agencies should not accept the “community payments” justification for mergers.
Some of these changes (e.g., lowering the HSR triggers) require legislative action, but others could be accomplished through the agencies’ existing regulatory authority. The result would be strengthening this critical tool for preserving competition in health care.
REDUCING SERVICE CAPACITY: EVIDENCE AND POLICY OPTIONS
Frank A. Sloan, Ph.D.
Duke University
Since the 1950s and especially since the late 1960s, soon after Medicare and Medicaid were implemented, healthcare cost containment has been an important policy issue. Since the 1970s, excess capacity of the U.S. health system has reached center stage in the cost-containment discussion. Policy researchers argued that such excess capacity was increasing private and public expenditures on personal healthcare services.
The Medical Arms Race
The argument goes as follows. Because of widespread health insurance coverage, healthcare consumers are isolated from the costs they incur when
they use healthcare services. Thus, their demand for healthcare services is inelastic; this means that the use of health services is not very responsive to prices set by providers. Because consumers do not pay much extra when they use more services, they often demand services that offer little or no benefit. Physicians value high quantity and quality of care as reflected in high “intensity” of services for both financial and nonfinancial reasons. Hence, for example, when there is a choice between two hospitals at which to admit a patient, physicians will choose the one that offers a broader range of services and amenities (Devers et al., 2003; Robinson and Luft, 1987). Hospital administrators have no incentive to say “no” to demands from their medical staffs for more service offerings when hospitals were paid on a retrospective cost or a similar basis. Under retrospective cost reimbursement, the hospital is guaranteed recovery of its investment outlays. Roughly speaking, if Medicare beneficiaries receive 35 percent of all services delivered by a hospital in a given year, Medicare is responsible for 35 percent of hospital cost. Thus, even if a particular service, for example a computed tomography (CT) scanner, were highly underused, Medicare would cover 35 percent of the cost. Given this guarantee of revenue coupled with patient and physician demand for the service, hospital administrators would be foolish not to undertake the investment in the CT scanner.
A physician’s threat to admit patients elsewhere is more credible if there is competition among hospitals in the market. This process of non-price competition among facilities in which hospitals compete by investing in facilities and services has been termed the “medical arms race.” At the time this phrase was coined, competition worked perversely to increase the cost of care. When there was more competition, hospitals would compete by offering more and more types of services. Insurance coverage was more complete for hospital services than for physicians’ and other types of personal health services. Thus, the medical arms race in the hospital sector was most evident.
Roemer’s law stated that a bed created is a bed used. This term could apply to other health services capacity as well. Roemer’s law was said to have validity for at least two reasons. First, additional capacity increases patient access to care. If it is easier to be admitted near to one’s home, more persons will be admitted. Second, there was the notion that supply creates its own demand. When there is excess capacity under a “piece rate” system, provision of more services results in higher revenues.
Capital Expenditures Regulation
The National Health Planning and Resources Development Act of 1974 mandated that each state adopt a certificate-of-need (CON) law and form a health planning agency to enforce its CON program and made receipt of
federal funding for health resources contingent on state compliance with federal law. By 1974, several states had already adopted CON policies, starting with New York in 1968. CON policy required that healthcare facilities obtain permission from a state CON agency before beginning any construction of a new facility, expanding capacity, or introducing major new services. To obtain a CON, facilities had to provide evidence of need, based on criteria specified by the state CON program. In 1972, Section 1122 programs were implemented for Medicare and Medicaid programs. This federal law required prior review and approval of capital expenditures as a condition of Medicare and Medicaid coverage of a service that required the investment.
In sum, until the early 1980s, federal policy reflected the view that health cost containment could be achieved by setting limits on capacity. As the largest single component of health care, hospitals were the main target of CON, although nursing homes were also important targets. If there are fewer beds in nursing homes, it was argued, there would be fewer bed days for Medicaid to cover. Medicaid was and remains, an important source of payment for nursing home care. In states with CON, hospitals must provide evidence of need for their services and demonstrate qualifications to fulfill this need.
Competition in Markets for Healthcare Services
In 1982, California implemented a selective contracting law; such laws were implemented in other states subsequently. Previously, insurers were prohibited from channeling the persons they covered to particular providers. Such channeling was seen as an intrusion in the practice of medicine. Under selective contracting, insurers can channel the people they insure to those providers with whom they have contracts. Selective contracting gave insurers an important bargaining tool with hospitals. If the hospital did not agree to attractive contract terms (from the insurer’s standpoint), the insurer could credibly threaten to channel the individuals it insures elsewhere. At about the same time, in 1983, Congress passed the Prospective Payment Program for hospitals (PPS). The PPS phased out retrospective cost reimbursement for hospitals over 4 years and replaced it with a payment system that was prospective in that prices were set in advance, and these prices were fixed. Under retrospective cost reimbursement, inefficiency is rewarded in that a dollar of additional cost results in about a dollar of increased revenue. In contrast, under prospective payment, a dollar of extra cost results in virtually no additional revenue. Other payers followed Medicare’s lead although there are differences in details of how their payment programs have been implemented.
The change to a prospective payment system markedly altered hospital
incentives, as did the ability of insurers to channel patients to facilities with which they obtained contracts. The change in the laws also called the continued relevance of Roemer’s law into question. A hospital with a monopoly in its market area is not subject to much market discipline. However, when it faces competition, the hospital has to exercise particular care in not expanding capacity that would place it at a competitive disadvantage relative to its competitors. In the changed world of health insurance payment practices, coupled with selective contracting, reducing capacity and facility consolidation no longer achieves cost containment. In fact, this could result in higher rates of healthcare inflation.
Repeal of Capital Expenditure Regulation
Largely for this reason, the provision of the federal 1974 law that required states to have CON was repealed in 1983. Currently, 27 states have retained CON for acute care services. Other states, such as Ohio, have repealed CON for acute care services but retain CON regulation of nursing homes.
The Future—Will Capacity Reduction Achieve Cost Containment?
This much is history. As we look ahead, can we expect that reductions in service capacity will lead to reductions in spending on personal healthcare services? My answer is that of a two-armed economist. It depends on whether or not we will rely on market forces in health care in the future. If we continue to rely on market forces to contain healthcare outlays, capital expenditure/service regulation and capacity reduction are not relevant cost-containment tools. However, if healthcare prices are to be set by government agencies, capital expenditure regulation may be useful. Even in a government-financed and run system, price must cover cost of service provision. If cost is lower, prices can also be lower. However, if prices are set too high relative to cost, providers will compete on a nonprice basis. When airline fares were subject to government regulation and prices were set above average cost, airlines competed by offering the flying public various amenities, such as better food and service.
In the environment prevailing from the 1950s to the 1970s, less competition among hospitals (higher hospital concentration) led to lower hospital spending. In the late 1980s and 1990s, less competition among hospitals and less excess capacity led to higher hospital spending mainly through higher prices. More recently, the relationship between hospital concentration and spending may be reverting to the pattern prevailing before the late 1980s (Dranove et al., 2008). Likely causes of the change in the relationship between concentration and prices are (1) the increase in concentration of
hospitals in many markets (many hospitals having closed or merged in the past two decades), and (2) the difficulties insurers have faced in channeling patients to a fixed set of providers following the backlash against managed care. If insurers do not have the ability to credibly threaten to channel their patients to other competing providers, providers (hospitals) will not make price concessions (Wu, 2009).
If Capacity Reduction Is Desirable, How Should This Be Done?
To the extent that capacity reduction will be a desirable goal in the future, the question remains as to how this will be done. An advantage of CON policy is that we have about four decades’ experience with these programs. Overall, the empirical evidence suggests that CON programs have not succeeded in cost containment, and the evidence on their accomplishments in improving patient access to care and quality of care is mixed (see Salkever [2000] for a review of much of this evidence).
Structural weaknesses of CON programs have been identified. The concept of “need” is not well defined or even definable. Rather than think about need, policy makers should make decisions in terms of marginal benefit of the added services versus its marginal cost. CON coverage has generally excluded physicians’ offices. It more directly applies to capital expenditures while expenditures on labor are not directly affected. CON programs do not have a capital budget. Thus, saying “no” to one capital project does not leave more funds for approving others. This leaves CON programs open to pressures from the stakeholders. CON is designed to limit entry, but there is little or no ongoing supervision of facilities following CON approval. In effect, CON gives a de facto franchise to incumbents. It is not surprising that the empirical evidence shows quite conclusively that CON programs on average have not constrained cost growth. Further, when CON has been lifted by states, no surge in spending on personal healthcare services has occurred (Conover and Sloan, 1998). CON regulation has achieved some reduction in beds, but it increased hospital investment (in some studies) with no net impact on total hospital investment.4
Many of these deficiencies of CON programs could be remedied. CON applicants could provide cost–benefit analysis on a project-specific basis and assess uncertainties in the cost–benefit calculations. CON coverage could be expanded to include capital expenditures in physicians’ offices. State CON agencies could be provided with a capital budget out of which approved capital projects would be financed. This system would replace tax-exempt bond financing, which currently favors major healthcare capital projects over investments in other sectors. CON agency operating budgets could be increased to permit ongoing monitoring of whether promises made in CON applications are in fact kept. CON programs could gather and disseminate information on facility quality.
In conclusion, we cannot know whether or not service capacity reduction will constrain cost growth until we know how the healthcare system will be structured in the future. There are circumstances under which CON-type programs are desirable. But if capital expenditure regulation is desirable, it should be not ended but mended.
MALPRACTICE REFORM AND HEALTHCARE COSTS
Randall R. Bovbjerg, J.D.
The Urban Institute
Malpractice reforms, in the form of limits on traditional personal injury rules or processes, can save almost 1 percent of total health spending or health insurance premiums over the next decade. Three types of savings are achievable: (1) lower liability premiums, (2) lower incidence of defensive medicine, and (3) enhanced savings under other reforms enacted simultaneously. In addition, reforming liability as part of health reform also adds value for patients; successful health reform can offer better ways than do traditional liability laws to promote patient safety, rehabilitate the injured, and compensate for injuries (Berenson et al., 2009).
Conventional “tort reform” achieves savings by limiting traditional liability, not by fundamentally altering its approach. Other reforms would likely work better to improve the performance of the liability “system” in
achieving its three central goals of compensating injuries, deterring negligence that causes them, and promoting justice. Broader reforms include alternative compensation systems and institutional responsibility (Bovbjerg and Tancredi, 2005). An IOM committee has endorsed demonstrations of some alternative approaches to compensation and safety that hold great promise for improvement (IOM, 2002). Other reforms have not been widely implemented, however. Their evidence base is thus scant, so fiscal estimates are uncertain; and the measures are not yet “shovel ready” for implementation as part of health reform. Nonetheless, over time broader strategies are warranted to improve patient safety and achieve other goals not directly advanced by tort limitations.
The following discussion details the three forms of tort-reform savings just noted and ends with consideration of broader safety-oriented reforms.
Lower Liability Premiums
Some state tort reforms have reduced malpractice payouts (Danzon, 1986) and hence also the associated liability premiums charged to medical care providers (Zuckerman et al., 1990). The biggest impact comes from a cap on total malpractice awards or on their nonmonetary component, that is, “pain and suffering” (Nelson et al., 2007; U.S. Congress Office of Technology Assessment, 1994). The Congressional Budget Office (CBO) has estimated that implementing California-style reforms nationally, most importantly a $250,000 cap on noneconomic damage awards, would reduce physician liability premiums by an average of 25 to 30 percent, more in states with weak tort reform than where reform is already strong (CBO, 2004). These findings are consistent with providers’ persistent lobbying for tort reforms.
Changes in provider costs for malpractice insurance should thereafter be reflected in lower patient charges and hence in health insurance premiums.5 The CBO estimate implies a savings on malpractice premiums of $7 billion to $9 billion for 2007 (most recent data available)—or some 0.3 percent to 0.4 percent of national health spending in that year (CMS, 2008; Towers Perrin, 2008).
Lower Incidence of Defensive Medicine
Tort reforms also plausibly reduce the amount of defensive medicine practiced, the extra tests and procedures that medical providers say that they add to reduce the risk of lawsuit or to facilitate any needed legal defense. Practitioners have long reported such wastefulness, as early as the first congressional hearing on malpractice in 1969 (Medical Malpractice: The Patient Versus the Physician, 1969). How much have state tort reforms reduced defensiveness? The highest peer-reviewed estimate, from 1980s data, is that caps and similar reforms saved about 4 percent by cutting hospital spending (Kessler and McClellan, 1996). A more recent study found a 3 to 4 percent cut in state healthcare expenditures (Hellinger and Encinosa, 2006). However, the CBO was unable to replicate the former finding, and a recent extension of its methods that also included physician spending found no impacts (CBO, 2004; Sloan and Shadle, 2009). Most studies find savings in the range of 0 to 0.27 percent of health spending (Currie and MacLeod, 2008; Dubay et al., 1999; Sloan et al., 1997). A recent review of medical liability issues in health reform mentioned potential savings on defensiveness of 1 percent of health spending, though without documentation (Mello and Brennan, 2009). On balance, it seems plausible that savings from reduced defensiveness could equal or slightly exceed those on liability premiums, perhaps another 0.5 percent of total health spending, for a total savings of 0.9 percent.
Greater changes might be feasible if defensive services were simultaneously targeted by additional strategies, such as altered payment incentives, more effective utilization review, or enhanced promotion of evidence-based practice—which have merit in their own right and are discussed elsewhere in this volume. President Barack Obama has suggested a willingness to work with physicians to reduce defensive practices by creating some liability protection for defendants in compliance with authoritative guidelines (Stolberg and Pear, 2009). This position is promising, and there is some evidence that guidelines can protect against liability. But new approaches are needed to improve on unsuccessful prior state use of guidelines (Clark et al., 2008; LeCraw, 2007; Ransom et al., 2003).
Making Other Reforms More Effective
The estimated savings mentioned above on premiums and defensive medicine of 0.9 percent of all personal health spending would save almost $20 billion in 2010 and almost $260 billion over a full decade (Berenson et al., 2009). Savings would be shared across public- and private-sector spending.
Moreover, because malpractice reforms support other reform measures,
synergistic savings from bundling this effort with other reform initiatives will likely go further, as just noted (Gabel, 2009). For example, evidence-based medicine and other utilization initiatives may help promote the desired reductions in defensive practices beyond what has previously been observed.6 Simultaneously, tort reform undercuts provider resistance to utilization oversight based on fears that any change in accustomed practice could subject them to objectionable legal liability.
How Inclusion Within Health Reform Makes Tort Reform More Positive for Patients
Finally, apart from dollar savings, making tort reform part of larger health reform also makes changes in liability more positive for patients. Healthcare reform shifts the policy discussion dramatically from the political-legal context of prior battles over tort reform geared to benefit providers. Starting in California and other states in the mid-1970s, standalone tort limits have had a very contentious history (Sloan and Chepke, 2008). Caps and other limits have long met strong political resistance—especially from Democrats, including then Senator Obama. Stand-alone tort reforms are seen as mere takeaways of patient rights that undercut patient compensation and incentives for safety. Some courts have similarly found state caps unconstitutional, holding for example that a short-term insurance crisis does not justify legislative changes to court-made liability rules (Nelson et al., 2007).
However, if tort changes help to build coalitions for comprehensive health reform (Bradley, 2009), they will benefit all patients. People permanently injured during medical care would especially benefit, as otherwise their injuries might make them difficult or impossible to insure, and very few now receive liability awards. A system that provides nearly universal coverage will ensure that individuals do not have to rely upon tort awards to finance their medical care. Legislators and judges should appreciate these broader public benefits.7 Health reform also provides a platform for redoubling federal efforts to prevent medical injury, which should form part of health reform’s promotion of better medical care. The incidence of avoidable injury remains unacceptably high, despite generations of increasing liability pressure. Patient safety efforts have the potential to reduce health
spending and, regardless of their impact on spending, are important in their own right (Clinton and Obama, 2006; Schoenbaum and Bovbjerg, 2004).
REFERENCES
111th Congress. 2009. American Recovery and Reinvestment Act of 2009. Washington, DC.
A.M. Best. 2009. Best’s Market Share Reports (One-Year Premiums and Loss Study). http://www.ambest.com/sales/marketshare1ypls/ (accessed August 26, 2009).
Adler-Milstein, J., D. W. Bates, and A. K. Jha. 2009. U.S. regional health information organizations: Progress and challenges. Health Affairs (Millwood) 28(2):483-492.
Aiken, L. H., S. P. Clarke, D. M. Sloane, J. Sochalski, and J. H. Silber. 2002. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association 288(16):1987-1993.
American Diabetes Association. 2002. Implications of the United Kingdom Prospective Diabetes Study. http://care.diabetesjournals.org/content/25/suppl_1/s28.full (accessed September 2, 2009).
——. 2009. Direct and Indirect Costs of Diabetes in the United States. http://www.diabetes.org/diabetes-statistics/cost-of-diabetes-in-us.jsp (accessed September 2, 2009).
American Hospital Association. 2009. Hospitals in pursuit of excellence. http://www.ahaqualitycenter.org/qualitycenter/hpoe/content/hpoe_all.pdf (accessed September 2009).
Arcury, T. A., J. S. Preisser, W. Gesler, and J. M. Powers. 2005. Access to transportation and health care utilization in a rural region. Journal of Rural Health 21(1):31-38.
Ayanian, J. Z. 2009. The elusive quest for quality and cost savings in the Medicare program. Journal of the American Medical Association 301(6):668-670.
Baker, D. W., C. D. Stevens, and R. H. Brook. 1996. Determinants of emergency department use: Are race and ethnicity important? Annals of Emergency Medicine 28(6):677-682.
Ben-Tovim, D. I., M. L. Dougherty, T. J. O’Connell, and K. M. McGrath. 2008. Patient journeys: The process of clinical redesign. Medical Journal of Australia 188(6 Suppl): S14-S17.
Berenson, R., J. Holahan, L. Blumberg, R. Bovbjerg, T. Waidmann, A. Cook, and A. Williams. 2009. How We Can Pay for Health Care Reform. http://www.rwjf.org/files/research/46492full.pdf (accessed August 2009).
Blumenthal, D., and M. B. Buntin. 1998. Carve outs: Definition, experience, and choice among candidate conditions. American Journal of Managed Care 4 Suppl:SP45-SP57.
Bott, D. M., M. C. Kapp, L. B. Johnson, and L. M. Magno. 2009. Disease management for chronically ill beneficiaries in traditional Medicare. Health Affairs (Millwood) 28(1):86-98.
Bovbjerg, R. R., and L. R. Tancredi. 2005. Liability reform should make patients safer: “Avoidable classes of events” are a key improvement. Journal of Law, Medicine, & Ethics 33(3):478-500.
Bradley, B. 2009. Tax reform’s lesson for health care reform. New York Times, August 30, WK9.
Burt, C., L. McCaig, and E. Rechtsteiner. 2007. Ambulatory Medical Care Utilization Estimates for 2005. http://www.cdc.gov/nchs/data/ad/ad388.pdf (accessed August 2009).
Butterfield, S. M. 2007. A new rx for crowded hospitals: Math. Operations management expert brings queuing theory to healthcare. http://www.acphospitalist.org/archives/2007/12/math.htm (accessed August 2009).
CBO (Congressional Budget Office). 2004. Limiting Tort Liability for Medical Malpractice. Washington, DC: Congressional Budget Office.
Center for American Progress and Institute on Medicine as a Profession. 2008. The Healthcare Delivery System: A Blueprint for Reform. Washington, DC: Center for American Progress.
Choe, H. M., S. J. Bernstein, D. Cooke, D. Stutz, and C. Standiford. 2008. Using a multidisciplinary team and clinical redesign to improve blood pressure control in patients with diabetes. Quality Management in Health Care 17(3):227-233.
Clark, S. L., M. A. Belfort, G. A. Dildy, and J. A. Meyers. 2008. Reducing obstetric litigation through alterations in practice patterns. Obstetrics & Gynecology 112(6):1279-1283.
Clinton, H. R., and B. Obama. 2006. Making patient safety the centerpiece of medical liability reform. New England Journal of Medicine 354(21):2205-2208.
CMS (Centers for Medicare & Medicaid Services). 2005. Details for care management for high-cost beneficiaries demonstration. http://www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=3&sortOrder=ascending&itemID=CMS1198967&intNumPerPage=10 (accessed August 2009).
——. 2008. National health expenditures by type of service and source of funds, CY 1960-2007. http://www.cms.hhs.gov/NationalHealthExpendData/02_NationalHealthAccountsHistorical.asp (accessed August 26, 2009).
Conover, C. J., and F. A. Sloan. 1998. Does removing certificate-of-need regulations lead to a surge in health care spending? Journal of Health Politics, Policy & Law 23(3):455-481.
Currie, J., and W. MacLeod. 2008. First do no harm? Tort reform and birth outcomes. Quarterly Journal of Economics 123(2):795-830.
Danzon, P. M. 1986. The frequency and severity of medical malpractice claims: New evidence. Law and Contemporary Problems 49(2):57-84.
Delia, D., J. C. Cantor, A. Tiedemann, and C. S. Huang. 2009. Effects of regulation and competition on health care disparities: The case of cardiac angiography in New Jersey. Journal of Health Politics, Policy & Law 34(1):63-91.
Department of Health and Human Services. 2009a. Meaningful use matrix. http://healthit.hhs.gov/portal/server.pt/gateway/PTARGS_0_10741_872719_0_0_18/Meaningful%20Use%20Matrix.pdf (accessed August 2009).
——. 2009b. U.S. Department of Health and Human Services. Nationwide health information network (NHIN): Background & scope. http://healthit.hhs.gov/portal/server.pt?open=512&mode=2&cached=true&objID=1142 (accessed August 2009).
DesRoches, C. M., E. G. Campbell, S. R. Rao, K. Donelan, T. G. Ferris, A. Jha, R. Kaushal, D. E. Levy, S. Rosenbaum, A. E. Shields, and D. Blumenthal. 2008. Electronic health records in ambulatory care—A national survey of physicians. New England Journal of Medicine 359(1):50-60.
Devers, K. J., L. R. Brewster, and L. P. Casalino. 2003. Changes in hospital competitive strategy: A new medical arms race? Health Services Research 38(1 Pt 2):447-469.
DOJ (Department of Justice). 1999. Revised Final Judgement; No. 3-99cv1398-H. www.usdoj.gov/atr/cases/f214700/214734.htm (accessed August 2009).
——. 2005. Complaint, No. 1:05cv02436. www.usdoj.gov/atr/cases/f213800/213815.htm (accessed August 2009).
——. 2008. Complaint, No. 1:08cv0322. www.usdoj.gov/atr/cases/f230400/230447.htm (accessed August 2009).
Dranove, D., R. Lindrooth, W. D. White, and J. Zwanziger. 2008. Is the impact of managed care on hospital prices decreasing? Journal of Health Economics 27(2):362-376.
Dubay, L., R. Kaestner, and T. Waidmann. 1999. The impact of malpractice fears on cesarean section rates. Journal of Health Economics 18(4):491-522.
eHealth Initiative. 2009. Migrating toward meaningful use: The state of health information exchange. eHealth Initiative’s sixth annual survey.
Eisenberg, J. M., and E. J. Power. 2000. Transforming insurance coverage into quality health care: Voltage drops from potential to delivered quality. Journal of the American Medical Association 284(16):2100-2107.
Fisher, E. S., M. B. McClellan, J. Bertko, S. M. Lieberman, J. J. Lee, J. L. Lewis, and J. S. Skinner. 2009. Fostering accountable health care: Moving forward in Medicare. Health Affairs (Millwood) 28(2):w219-w231.
FTC (Federal Trade Commission). 2008a. Final order, docket #9315. http://www.ftc.gov/os/adjpro/d9315/080424finalorder.pdf (accessed August 2009).
——. 2008b. Order dismissing complaint, docket #9326. http://www.ftc.gov/os/adjpro/d9326/index.shtm (accessed August 2009).
Gabel, J. R. 2009. Congress’s health care numbers don’t add up. New York Times, August 26, 2009, A23.
Gross, D. L., H. Temkin-Greener, S. Kunitz, and D. B. Mukamel. 2004. The growing pains of integrated health care for the elderly: Lessons from the expansion of pace. Milbank Quarterly 82(2):257-282.
Haas-Wilson, D. 2003. Managed Care and Monopoly Power: The Antitrust Challenge. Cambridge: Harvard University Press.
Hackbarth, G. 2009. Reforming america’s health care delivery system. http://www.medpac.gov/documents/Hackbarth%20Statement%20SFC%20Roundtable%204%2021%20FINAL%20with%20header%20and%20footer.pdf (accessed October 1, 2009).
Hellinger, F. J., and W. E. Encinosa. 2006. The impact of state laws limiting malpractice damage awards on health care expenditures. American Journal of Public Health 96(8): 1375-1381.
Hillestad, R., J. Bigelow, A. Bower, F. Girosi, R. Meili, R. Scoville, and R. Taylor. 2005. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Affairs (Millwood) 24(5):1103-1117.
Ho, V., M. H. Ku-Goto, and J. G. Jollis. 2009. Certificate of need (CON) for cardiac care: Controversy over the contributions of CON. Health Services Research 44(2 Pt 1):483-500.
Holtz-Eakin, D. 2004. An analysis of the literature on disease management programs. http://www.cbo.gov/ftpdocs/59xx/doc5909/10-13-DiseaseMngmnt.pdf (accessed August 2009).
IOM (Institute of Medicine). 2002. Liability: Patient-centered, safety-focused, nonjudical compensation. In Fostering Rapid Advances in Health Care: Learning from System Demonstrations, edited by J. Corrigan, A. Greiner and S. Erickson. Washington, DC: The National Academies Press.
——. 2006. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press.
Jessee, W. 2009. Avoidable costs from delivery inefficiencies: Physician offices. The Healthcare Imperative: Lowering Costs and Improving Outcomes Workshop, May 21-22, Washington, DC.
Jha, A. K., C. M. DesRoches, E. G. Campbell, K. Donelan, S. R. Rao, T. G. Ferris, A. Shields, S. Rosenbaum, and D. Blumenthal. 2009. Use of electronic health records in U.S. hospitals. New England Journal of Medicine 360(16):1628-1638.
Joint Commission Resources. 2009. Managing Patient Flow: Strategies and Solutions, 2nd edition. Oakbrook Terrace: Joint Commission International.
Kessler, D., and M. McClellan. 1996. Do doctors practice defensive medicine? Quarterly Journal of Economics 111(2):353-390.
——. 2000. Is hospital competition socially wasteful? Quarterly Journal of Economics 115(2):577-615.
King, D., D. Ben-Tovim, and J. Bassham. 2007. Redesigning emergency department patient flows: Application of lean thinking to health care. Emergency Medicine Australasia 19(1):79.
LeCraw, L. 2007. Use of clinical practice guidelines in medical malpractice litigation. Journal of Oncology Practice 3(5):254.
Leff, B., L. Reider, K. D. Frick, D. O. Scharfstein, C. M. Boyd, K. Frey, L. Karm, and C. Boult. 2009. Guided care and the cost of complex healthcare: A preliminary report. American Journal of Managed Care 15(8):555-559.
Litvak, E. 2005. Optimizing patient flow by managing its variability. In Front Office to Front Line: Essential Issues for Health Care Leaders. Vol. 5, edited by S. Berman. Oakbrook Terrace: Joint Commission Resources. Pp. 91-111.
——. 2007. Improving patient flow and thoroughput in California hospitals operating room services. Oakland: California Healthcare Foundation.
Litvak, E., and M. C. Long. 2000. Cost and quality under managed care: Irreconcilable differences? American Journal of Managed Care 6(3):305-312.
Litvak, E., P. I. Buerhaus, F. Davidoff, M. C. Long, M. L. McManus, and D. M. Berwick. 2005. Managing unnecessary variability in patient demand to reduce nursing stress and improve patient safety. The Joint Commission Journal on Quality and Patient Safety 31(6):330-338.
McGuire, A., P. Fenn, I. Stratton, R. Holman, and R. Turner. 1998. Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: Ukpds 40. Uk Prospective Diabetes Study Group. British Medical Journal 317(7160):720-726.
McManus, M. L., M. C. Long, A. Cooper, J. Mandell, D. M. Berwick, M. Pagano, and E. Litvak. 2003. Variability in surgical caseload and access to intensive care services. Anesthesiology 98(6):1491-1496.
Mello, M. M., and T. A. Brennan. 2009. The role of medical liability reform in federal health care reform. New England Journal of Medicine 361(1):1-3.
Menduno, M. 1999. Apothecary.Now. Hospital Health Network 73(7):34-38, 40, 32.
Mercer. 2007. CCNC/Access Cost Savings, Analysis for State Fiscal Years 2003, 2004, 2005, and 2006. http://www.communitycarenc.com.
Muder, R. R., C. Cunningham, E. McCray, C. Squier, P. Perreiah, R. Jain, R. L. SinkowitzCochran, and J. A. Jernigan. 2008. Implementation of an industrial systems-engineering approach to reduce the incidence of methicillin-resistant staphylococcus aureus infection. Infection Control and Hospital Epidemiology 29(8):702-708.
Nelson, L. J., III, M. A. Morrisey, and M. L. Kilgore. 2007. Damages caps in medical malpractice cases. Milbank Quarterly 85(2):259-286.
OECD (Organisation for Economic Co-operation and Development). 2009. OECD Health Data 2009: Statistics and Indicators for 30 Countries. Paris: OECD.
Peikes, D., A. Chen, J. Schore, and R. Brown. 2009. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. Journal of the American Medical Association 301(6):603-618.
Persoon, T. J., S. Zaleski, and J. Frerichs. 2006. Improving preanalytic processes using the principles of lean production (toyota production system). American Journal of Clinical Pathology 125(1):16-25.
Pignone, M. 2009. Treatment costs from missed tertiary cost-saving prevention opportunities. The Healthcare Imperative: Lowering Costs and Improving Outcomes Workshop, May 21-22, Washington, DC.
Pope, G., J. Kautter, R. Ellis, A. Ash, J. Ayanian, L. Lezzoni, M. Ingber, J. Levy, and J. Robst. 2004. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financing Review 25(4):119-141.
Raab, S. S., D. M. Grzybicki, D. Sudilovsky, R. Balassanian, J. E. Janosky, and C. M. Vrbin. 2006. Effectiveness of toyota process redesign in reducing thyroid gland fine-needle aspiration error. American Journal of Clinical Pathology 126(4):585-592.
Ransom, S. B., D. M. Studdert, M. P. Dombrowski, M. M. Mello, and T. A. Brennan. 2003. Reduced medicolegal risk by compliance with obstetric clinical pathways: A case-control study. Obstetrics & Gynecology 101(4):751-755.
Robinson, J. C., and H. S. Luft. 1987. Competition and the cost of hospital care, 1972 to 1982. Journal of the American Medical Association 257(23):3241-3245.
Romer, C. 2009. The Economic Case for Health Care Reform. Executive Office of the President Council of Economic Advisers.
Ross, J. S., V. Ho, Y. Wang, S. S. Cha, A. J. Epstein, F. A. Masoudi, B. K. Nallamothu, and H. M. Krumholz. 2007. Certificate of need regulation and cardiac catheterization appropriateness after acute myocardial infarction. Circulation 115(8):1012-1019.
Salkever, D. S. 2000. Regulation of prices and investment in hospitals in the U.S. Handbook of Health Economics 1B:1489-1535.
Schoenbaum, S. C., and R. R. Bovbjerg. 2004. Malpractice reform must include steps to prevent medical injury. Annals of Internal Medicine 140(1):51-53.
Senate Finance Committee. 2009. Transforming the healthcare delivery system: Proposals to improve patient care and reduce healthcare costs. http://finance.senate.gov/sitepages/leg/LEG%202009/042809%20Health%20Care%20Description%20of%20Policy%20Option.pdf (accessed October 1, 2009).
Sever, P. S., N. R. Poulter, B. Dahlof, H. Wedel, R. Collins, G. Beevers, M. Caulfield, S. E. Kjeldsen, A. Kristinsson, G. T. McInnes, J. Mehlsen, M. Nieminen, E. O’Brien, and J. Ostergren. 2005. Reduction in cardiovascular events with atorvastatin in 2,532 patients with type 2 diabetes: Anglo-scandinavian cardiac outcomes trial—lipid-lowering arm (ascot-lla). Diabetes Care 28(5):1151-1157.
Shortell, S. M., and E. F. Hughes. 1988. The effects of regulation, competition, and ownership on mortality rates among hospital inpatients. New England Journal of Medicine 318(17):1100-1107.
Shortell, S. M., R. Gillies, J. Siddique, L. P. Casalino, D. Rittenhouse, J. C. Robinson, and R. K. McCurdy. 2009. Improving chronic illness care: A longitudinal cohort analysis of large physician organizations. Medical Care 47(9):932-939.
Sloan, F., and L. Chepke. 2008. Medical Malpractice. Cambridge: MIT Press.
Sloan, F., S. Entman, B. Reilly, C. Glass, G. Hickson, and H. Zhang. 1997. Tort liability and obstetricians’ care levels. International Review of Law and Economics 17(2):245-260.
Sloan, F. A., and J. H. Shadle. 2009. Is there empirical evidence for “defensive medicine”? A reassessment. Journal of Health Economics 28(2):481-491.
Smedley, B. D., A. Y. Stith, and A. R. Nelson, eds. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Edited by Board on the Health of Select Populations Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine. Washington, DC: The National Academies Press.
Stolberg, S., and R. Pear. 2009. Obama open to reining in medical suits. New York Times, June 15, A1.
Strunk, B. C., K. J. Devers, and R. E. Hurley. 2001. Health plan-provider showdowns on the rise. Issue Brief Center for Studying Health System Change (40):1-4.
Towers Perrin. 2008. Update on U.S. Tort Cost Trends. http://www.towersperrin.com/tp/getwebcachedoc?webc=USA/2008/200811/2008_tort_costs_trends.pdf (accessed August 26, 2009).
U.S. Congress Office of Technology Assessment. 1994. Defensive Medicine and Medical Malpractice. OTA-H-602. Washington, DC: U.S. Government Printing Office.
UnitedHealth Group. 2009. Federal health care cost containment—How in practice can it be done? Options with a real world track record of success. http://www.unitedhealthgroup.com/main/generalcontent.aspx?id=b97fbb73-53fa-436c-9e66-6743b47ba307 (accessed August 2009).
Vaughan-Sarrazin, M. S., E. L. Hannan, C. J. Gormley, and G. E. Rosenthal. 2002. Mortality in Medicare beneficiaries following coronary artery bypass graft surgery in states with and without certificate of need regulation. Journal of the American Medical Association 288(15):1859-1866.
VMMC (Virginia Mason Medical Center). 2004. Rapid Process Improvement Workshop Results. https://www.virginiamason.org/home/body.cfm?xyzpdqabc=0&id=156&action=detail&ref=65&ArticleRefs=1,2,3,4,5,6,7,8,9,10,11,12,13,65,66,67,68&issueref=1 (accessed September 2, 2009).
——. 2009. Clinical decision support. https://www.virginiamason.org/home/body.cfm?id=49 (accessed September 2, 2009).
Vogt, W., and R. Town. 2006. How Has Hospital Consolidation Affected the Price and Quality of Hospital Care? Princeton: Robert Wood Johnson Foundation.
Wagner, E. H., N. Sandhu, K. M. Newton, D. K. McCulloch, S. D. Ramsey, and L. C. Grothaus. 2001. Effect of improved glycemic control on health care costs and utilization. Journal of the American Medical Association 285(2):182-189.
Walker, J., E. Pan, D. Johnston, J. Adler-Milstein, D. W. Bates, and B. Middleton. 2005. The value of health care information exchange and interoperability. Health Affairs (Millwood) Suppl Web Exclusives:W5-10-W15-18.
Wheatley, B. 2002. Disease management: Findings from leading state programs. State Coverage Initiatives Issue Brief 3(3):1-6.
Wood, D. L., M. D. Brennan, R. Chaudhry, A. A. Chihak, W. L. Feyereisn, N. L. Woychick, P. T. Hagen, J. W. Curtright, J. M. Naessens, B. R. Spurrier, and N. F. Larusso. 2008. Standardized care processes to improve quality and safety of patient care in a large academic practice: The Plummer Project of the Department of Medicine, Mayo Clinic. Health Services Management Research 21(4):276-280.
Wu, V. Y. 2009. Managed care’s price bargaining with hospitals. Journal of Health Economics 28(2): 350-360.
Yaggy, S. D., J. L. Michener, D. Yaggy, M. T. Champagne, M. Silberberg, M. Lyn, F. Johnson, and K. S. H. Yarnall. 2006. Just for us: An academic medical center-community partnership to maintain the health of a frail low-income senior population. The Gerontologist 46(2).
Zuckerman, S., R. R. Bovbjerg, and F. Sloan. 1990. Effects of tort reforms and other factors on medical malpractice insurance premiums. Inquiry 27(2):167-182.






















































