1
Introduction
The global epidemic of hepatitis B and hepatitis C is a serious public-health problem. Using mortality data from 2003, Weiss and McMichael (2004) ranked the public-health importance of various infectious diseases and other conditions (see Figure 1-1). Those data underscore that chronic hepatitis B and hepatitis C are among the leading causes of preventable death worldwide.
Hepatitis B and hepatitis C are contagious liver diseases caused by the hepatitis B virus (HBV) and the hepatitis C virus (HCV), respectively. HBV is a 42-nanometer, partially double-stranded DNA virus classified in the Hepadnaviridae family; there are eight major HBV genotypes. HCV is a 55-nanometer, enveloped, positive-strand RNA virus classified as a separate genus, Hepacavirus, in the Flaviviridae family; there are at least six major HCV genotypes.
Hepatitis B and hepatitis C can be either acute or chronic. The acute form is a short-term illness that occurs within the first 6 months after a person is exposed to HBV or HCV. The diseases can become chronic, although this does not always happen and, particularly in the case of hepatitis B, the likelihood of chronicity depends on a person’s age at the time of infection. Chronic hepatitis B and chronic hepatitis C are serious and can result in liver cirrhosis and a type of liver cancer, hepatocellular carcinoma (HCC). The prevention of chronic hepatitis B and chronic hepatitis C prevents the majority of HCC cases because HBV and HCV are the leading causes of this type of cancer. Key characteristics of hepatitis B and hepatitis C are summarized in Table 1-1 and discussed below and in later chapters.
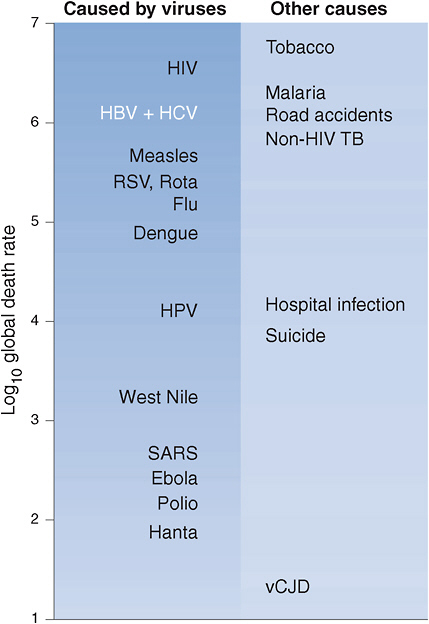
FIGURE 1-1 Approximate global preventable death rate from selected infectious diseases and other causes, 2003.
Abbreviations: HIV, human immunodeficiency virus; HBV, hepatitis B virus; HCV, hepatitis C virus; RSV, respiratory syncytial virus; HPV, human papilloma virus; SARS, severe acute respiratory syndrome; TB, tuberculosis; vCJD, variant Creutzfeldt-Jakob disease.
SOURCE: Weiss and McMichael, 2004. Reprinted with permission from Macmillan Publishers Ltd: Nature Medicine 10(12 Suppl):S70-S76, copyright 2004.
TABLE 1-1 Key Characteristics of Hepatitis B and Hepatitis C
|
|
Hepatitis B |
Hepatitis C |
|
Causative agent |
Partially double-stranded DNA virus |
Enveloped, positive-strand RNA virus |
|
|
Hepadnaviridae family |
Hepacavirus genus, Flaviviridae family |
|
Statistics |
In the United States, 0.8–1.4 million people are chronically infected with HBV |
In the United States, 2.7–3.9 million people are chronically infected with HCV |
|
Routes of transmission |
Contact with infectious blood, semen, and other body fluids, primarily through:
|
Contact with blood of an infected person, primarily through:
|
|
|
Less commonly through:
|
|
|
|
Less commonly through:
|
|
|
Persons at risk |
|
|
|
|
Hepatitis B |
Hepatitis C |
|
Persons at risk |
|
|
|
Potential for chronic infection |
Among newly infected, unimmunized persons, chronic infection occurs in:
|
75–85% of newly infected persons develop chronic infection |
|
Clinical outcomes |
|
|
|
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; HBsAg, hepatitis B surface antigen. SOURCE: Adapted from CDC, 2009a. |
||
PREVALENCE AND INCIDENCE OF HEPATITIS B AND HEPATITIS C WORLDWIDE
Worldwide, about 1 in 12 persons (480–520 million people) are chronically infected with HBV or HCV (Lavanchy, 2008; WHO, 2009). An estimated 78% of cases of primary liver cancer (HCC) and 57% of cases
of liver cirrhosis are caused by chronic HBV or HCV infection (Perz et al., 2006). Chronic liver disease due to coinfection with HBV or HCV has become a major cause of death in persons infected with HIV (Sulkowski, 2008), and coinfection presents additional treatment challenges (Kumar et al., 2008). It is estimated that HBV and HCV infections cause nearly a million deaths each year (Perz et al., 2006).
Chronic viral hepatitis is a silent killer. Without testing for infection, many chronically infected persons are not aware that they have been infected until symptoms of advanced liver disease appear. Advanced liver cancer has a 5-year survival rate of below 5% (American Cancer Society, 2009). Although much progress has been made in reducing the morbidity and mortality through effective treatment of chronic viral hepatitis, there is no global program to provide chronically infected persons with access to affordable treatment.
HBV is 50–100 times more infectious than HIV (WHO, 2009). Acute HBV infection in adults, although often asymptomatic, can cause severe illness and is associated with a 0.5–1% risk of death from liver failure (CDC, 2007). Chronic HBV infection, which occurs when the acute infection is not cleared by the immune system, is associated with a 15–25% risk of premature death from liver cancer or end-stage liver disease (Beasley and Hwang, 1991; WHO, 2009). The World Health Organization (WHO) estimates that up to 2 billion people worldwide have been infected with HBV; about 350 million people live with chronic HBV infection, and about 600,000 people die from HBV-related liver disease or HCC each year (WHO, 2009).
The major transmission routes and prevalence of chronic HBV infection vary by age and geography. Primary HBV infection acquired at an early age (through vertical transmission from an infected mother to her newborn or horizontal transmission during early childhood) is associated with the highest risk of chronic infection and is common in people born in or residing in the highly endemic countries of the western Pacific region, Asia, and sub-Saharan Africa (Shepard et al., 2006). In countries with a low prevalence of HBV carriers, primary infection usually occurs during adolescence or young adulthood as a result of unsafe injections and unprotected sexual activity. An estimated 21 million new HBV infections each year are due to unsafe injections in health-care settings (Hauri et al., 2004). Hepatitis B is also a major basis for social injustice in some endemic countries. For example, myths and misinformation about modes of HBV transmission have resulted in widespread discrimination against chronically infected persons in some endemic countries, such as China, the country with the world’s largest population of chronically infected people, who are not allowed to work in the food industry, are often required to undergo routine pre-employment HBV testing, and can be expelled from school or work because of a positive test (The Economist, 2006).
An estimated 130–170 million people live with chronic HCV infection worldwide, and an estimated 350,000 die of HCV-related liver disease each year (Perz et al., 2006). There are about 2.3–4.7 million new HCV infections each year from nosocomial transmission alone (Lavanchy, 2009). Unsafe mass immunization has led to exceedingly high HCV prevalence in some areas, such as Egypt, where 14–20% of the population has HCV antibodies (Frank et al., 2000; Lavanchy, 2008). In most populations in Africa, North America, South America, Europe, and Southeast Asia, the prevalence in the general population is less than 3% (Lavanchy, 2008).
HCV is efficiently transmitted via direct percutaneous exposure to infectious blood. Hepatitis C became a global epidemic in the 20th century as blood transfusions, hemodialysis, and the use of injection needles to administer licit and illicit drugs increased throughout the world (Drucker et al., 2001; Pybus et al., 2007). For example, the extremely high prevalence of HCV in Egypt is due to a schistosomiasis-eradication campaign that began in the 1960s, when more than 35 million injections were administered to about 6 million Egyptians (Deuffic-Burban et al., 2006; Frank et al., 2000; Lehman and Wilson, 2009). The identification of the virus in 1989 led to measures to reduce health-care–related exposure to HCV, particularly in industrialized nations. However, more than six billion unsafe injections are given worldwide each year (Hutin et al., 2003).
With the reduction in health-care–related exposures to HCV and the recent introduction of the practice of illicit-drug injection in new regions of the world, HCV infection through injection-drug use has become the major source of exposure to HCV worldwide. Explosive increases in HCV infection have occurred in regions of Asia and central and eastern Europe because of poor access to sterile injection equipment and lack of drug treatment. A recent meta-analysis reported that HCV prevalence was 84% in injection-drug users (IDUs) surveyed in the Guangxi region bordering the Golden Triangle in China (Xia et al., 2008). In that region, drug use is highly stigmatized, which reduces community support for prevention efforts and inhibits IDUs’ access to prevention services. Antiviral treatments for chronic HBV and HCV infections can effectively reduce the associated morbidity and mortality from liver disease. However, access to treatment is often limited by high costs of care and by the asymptomatic nature of chronic HBV and HCV infections. Therefore, many infected people are not identified in time to benefit from antiviral treatment.
Global eradication or elimination of new HBV infections is plausible because the infections can be prevented with the hepatitis B vaccine. No vaccine to prevent hepatitis C has been licensed. Given the limitations of the scope of the committee’s work, it did not assess global prevention and control efforts for hepatitis B and hepatitis C and did not consider the international effects of its recommendations.
PREVALENCE AND INCIDENCE OF HEPATITIS B AND HEPATITIS C IN THE UNITED STATES
HBV and HCV infections pose a major public-health problem in the United States and are major causes of chronic liver disease. Three to five times more people are living with chronic viral hepatitis infections than with HIV infection. Table 1-2 presents the burden of HBV, HCV, and HIV infections in the United States. The US Centers for Disease Control and Prevention (CDC) estimates that 3.5–5.3 million people in the United States—1–2% of the population—are living with chronic HBV or HCV infection—about 800,000 to 1.4 million people with chronic hepatitis B and an additional 2.7–3.9 million people with chronic hepatitis C (CDC, 2009d). However, an accurate estimate is difficult to obtain because there is no national chronic-hepatitis surveillance program. Each year, about 15,000 deaths are caused by HBV- or HCV-associated liver cancer or end-stage liver disease (CDC, 2009d). Almost half the liver transplantations in the United States are necessitated by end-stage liver disease associated with HBV or HCV infection (Kim et al., 2009).
The annual costs of HBV and HCV infections are difficult to determine. The direct medical cost associated with HBV infection has been estimated at $5.8 million based on the number of new cases in 2000 among persons 5–24 years old (Chesson et al., 2004). An estimated $1.8 billion in medical care costs was associated with HCV infections in 1997 (Leigh et al., 2001). Indirect costs, such as lost productivity, add to the HCV-associated cost burden. Because of the aging of people now infected (including some people with asymptomatic infections who will become symptomatic), HCV-related illnesses, deaths, and costs are all expected to rise substantially during the next two decades (Pyenson et al., 2009; Wong et al., 2000).
Hepatitis B
The national strategy for preventing new HBV infection in infants and children—including routine screening of pregnant women for hepatitis B surface antigen (a blood marker for chronic HBV infection), universal infant hepatitis B immunization, and catchup vaccination of unvaccinated children and adolescents—has resulted in a dramatic reduction in chronic HBV infection in infants and acute HBV infection in children of all ethnicities (CDC, 2004; Mast et al., 2005, 2006). Despite those achievements, the goal of eliminating perinatal HBV transmission has not been achieved, largely because coverage of newborns with a birth dose of hepatitis B vaccine is incomplete (CDC, 2008c). As a result, CDC estimates that each year about 1,000 newborns develop chronic HBV infection, which puts them at risk for premature death from HBV-related liver disease (Ward, 2008b).
TABLE 1-2 Burden of Selected Serious Chronic Viral Infections in the United States
|
Virus |
Vaccine-Preventable |
Transmission Routes |
Percentage of CDC NCHHSTP FY 2008 Budgetf |
|||
|
HBV |
0.8–1.4 million |
About 65% |
3,000 |
Yes |
Birth, blood, sex |
2% combined |
|
HCV |
2.7–3.9 million |
About 75% |
12,000 |
No |
Birth, blood, sex |
|
|
HIV/AIDS |
1.1 million |
About 21% |
14,016 |
No |
Birth, blood, sex |
69% (domestic activities) |
|
Abbreviations: CDC NCHHSTP, Centers for Disease Control and Prevention National Center for HIV/AIDS, Viral Hepatitis, Sexually Transmitted Disease, and Tuberculosis Prevention; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome. SOURCES: aCDC, 2009b; bCDC, 2009d; cLin et al., 2007; dHagan et al., 2006; eCDC, 2008b; fWard, 2008a. |
||||||
Based upon surveillance data and modeling, CDC estimates that there has been an 82% decline in incidence of acute HBV infection since 1990 with the total number of new infections in 2007 estimated at 43,000 (Daniels et al., 2009). Because many children have been vaccinated against HBV, most reported cases of acute HBV infection are in adults. The national strategy for preventing HBV transmission in adults—by recommending hepatitis B vaccination selectively for high-risk adults (including men who have sex with men, IDUs, and correctional-facility inmates)—has had only little success in reducing the incidence of acute HBV infection in US adults (Mast et al., 2006). Acute HBV infections are often asymptomatic or have symptoms similar to those of other common illnesses, such as influenza, so there is a high probability of underreporting.
In the United States, data on reported cases of acute HBV infection in 2007 indicate that the highest rate of infection is in non-Hispanic black men: 2.3 per 100,000. The incidence is substantially lower in other populations: 0.9 per 100,000 Asians and Pacific Islanders (APIs) and 1.0 per 100,000 non-Hispanic whites and Hispanics. There also appear to be geographic variations in incidence; the highest rates of acute HBV infection are in the South1 (Daniels et al., 2009).
Although the incidence of acute HBV infection is declining in the United States, the number of people who are living with chronic HBV infection may be increasing as a result of immigration from highly endemic countries (that is, the hepatitis B surface antigen prevalence is 2%). On the basis of immigration patterns in the last decade, it is estimated that every year 40,000–45,000 people enter the United States legally from HBV-endemic countries (Mast et al., 2006; U.S. Department of Homeland Security, 2009). Some populations are at higher risk for chronic HBV infection, including API Americans, who make up only 4.5% of the general US population (U.S. Census Bureau, 2008) but account for more than 50% of Americans who are living with chronic HBV infection (CDC, 2009c). The prevalence of chronic HBV infection in API Americans is as high as 15% in some studies and constitutes an important health disparity (CDC, 2006). Having been born in an HBV-endemic country appears to be the major risk factor for chronic HBV infection in the API population (Lin et al., 2007).
Recent studies suggest that routine HBV testing of all adult API Americans is cost-effective (Hutton et al., 2007), but almost two-thirds of chronically infected API Americans are unaware of their infection status because they have not been tested for HBV (CDC, 2006; Lin et al., 2007).
Hepatitis C
Persons likely to have chronic HCV infection include those who received a blood transfusion before 1992 and past or current IDUs. US veterans who use the Department of Veterans Affairs (VA) health-care system have a higher prevalence of HCV infection (4–35%) than the general population (about 2%) (Cheung, 2000; Dominitz et al., 2005; Groom et al., 2008; Sloan et al., 2004), so VA has established a program to test all VA patients for HCV infection and to manage HCV-positive patients clinically (Kussman, 2007). As is the case with HBV infection, most patients who have acute or chronic HCV infection are asymptomatic, and their disease remains undiagnosed (Kamal, 2008).
In the United States, most IDUs have serologic evidence of HCV infection, but the prevalence is highly variable. For example, in a study of young IDUs in four US cities, the prevalence of HCV antibody was 35% overall but varied from 14% in Chicago and 27% in Los Angeles to 51% in Baltimore and New York City (Amon et al., 2008). Prevalence is strongly associated with time engaged in risky behaviors, rising as the number of years of drug-injecting accumulates and reaching 65–90% in longer-term injectors (Hagan et al., 2008). HCV prevalence in IDUs in industrialized nations has fallen in recent years. For example, in IDUs injecting for less than 1 year, HCV prevalence fell from 46% before 1995 to 32% in a more recent period and in IDUs injecting for 5 years or more, prevalence fell from 67% before 1995 to 53% in the period after 1995 (Hagan et al., 2008). Most of the estimates of HCV incidence rates in IDUs in the United States have been between 15 and 30 per 100 person years at risk, with higher incidence found in recent-onset injectors (Garfein et al., 1998; Hagan et al., 2001, 2008; Hahn et al., 2002; Maher et al., 2006; Smyth et al., 2000; Thorpe et al., 2002).
The prevalence of HCV infection in the incarcerated population has been reported to vary from 12% to 35% (Boutwell et al., 2005; Weinbaum et al., 2003). Although some HCV transmission occurs within correctional settings (Hunt and Saab, 2009; Macalino et al., 2004), the vast majority of HCV-infected inmates became infected by injection-drug use in the community and not while incarcerated (Weinbaum et al., 2003).
Although reporting of acute HCV infection does not accurately reflect the underlying incidence in the United States, the number of acute HCV infections peaked in the late 1980s and declined throughout the 1990s (Armstrong et al., 2006; Shepard et al., 2005). The decline observed in the 1990s may reflect changes in IDUs’ behavior and practices, including greater participation in needle-exchange programs (Wasley et al., 2008). It is consistent with results of studies summarized previously that suggest that HCV seroconversion rates in IDUs have declined since 1995 (Armstrong
et al., 2006; Shepard et al., 2005). The decline slowed and then leveled off starting in 2003, and there was a slight increase in reported acute cases in 2006 (Wasley et al., 2008). Interpretation of those trends is complicated, however, inasmuch as reporting is related to access to health care and diagnosis of acute infection; many IDUs, who often have limited access to health care and no symptoms from infection, are not included in the trend analysis.
LIVER CANCER AND LIVER DISEASE FROM CHRONIC HEPATITIS B VIRUS AND HEPATITIS C VIRUS INFECTIONS
Both chronic HBV and HCV infections can lead to HCC, a type of liver cancer, and liver disease (But et al., 2008; McMahon, 2004, 2008; Tan et al., 2008). The two most important risk factors for HCC are chronic HBV and HCV infections. As stated above, an estimated 78% of HCC cases and 57% of liver cirrhosis cases are caused by chronic HBV and HCV infections (Perz et al., 2006).
In the United States, an estimated 3,000 people die each year from HCC or chronic liver disease caused by HBV infection (CDC, 2008a). However, risks of those outcomes vary and are higher in men and in people who are older, ingest large amounts of alcohol, and are coinfected with HIV (McMahon, 2004; Pungpapong et al., 2007). Outcomes of HBV infections occur much more often in those with high blood concentrations of HBV DNA, in persons over 40 years old, and in persons infected with HBV genotype C (Chen et al., 2006; Dehesa-Violante and Nuñez-Nateras, 2007; McMahon, 2004; Pungpapong et al., 2007). There are an especially high prevalence of chronic HBV infection and a high risk of HCC in the API American population, who make up the largest pool of chronically infected persons in the United States and are most commonly infected with HBV genotype C (Chang et al., 2007). HCC incidence tripled in the United States from 1975 through 2005, and the highest incidence is in API Americans who immigrated to the United States (Altekruse et al., 2009). American Indian and Alaska Native peoples have been found to have the highest rate of liver-related death of ethnic groups in the United States (Vong and Bell, 2004). The age-specific rate of death in American Indian and Alaska Native peoples due to chronic liver disease is much higher than that in any other population and chronic HBV infection and increasing rates of chronic HCV infection play a large role (Vong and Bell, 2004).
In the United States, about 12,000 people die from complications of chronic hepatitis C each year (CDC, 2008a). Deaths related to hepatitis C have increased; the highest number of deaths are in middle-aged men, non-Hispanic blacks, and American Indians (Wise et al., 2008). As is the case with chronic hepatitis B, complications occur more often in men and
in people who are older, have metabolic syndrome secondary to obesity, ingest large amounts of alcohol, and are coinfected with HIV (Ghany et al., 2009; Missiha et al., 2008; Pradat et al., 2007). There are also important ethnic and racial differences in the burden of chronic hepatitis C. The prevalence of HCV infection is higher in blacks than in whites (Armstrong et al., 2006; Thomas et al., 2000). Blacks also are less likely to respond to interferon-alpha-based treatment for chronic hepatitis C; this seems to be explained to a large extent by differences in DNA sequences near the interferon lambda 3 gene (Ge et al., 2009; Jeffers et al., 2004; Muir et al., 2004; Thomas et al., 2009). Likewise, there appears to be a greater burden of chronic hepatitis C and reduced response to treatment in Hispanic whites than in non-Hispanic whites (Armstrong et al., 2006; Bonacini et al., 2001; Rodriguez-Torres et al., 2009). In both Hispanics and blacks, HCC risk is increasing, in large part because of chronic hepatitis C (Altekruse et al., 2009). However, there is less evidence than in the case of HBV infection that different HCV genotypes or higher blood HCV concentrations increase the risk of long-term disease outcomes. Health-care use trends from 1994 to 2001 show a 20–30% yearly increase in HCV-related hospitalizations, length of hospital stays, total hospitalization costs, and hospital deaths (Grant et al., 2005).
THE COMMITTEE’S TASK
CDC has developed recommendations for the prevention and control of hepatitis B (Mast et al., 2005, 2006; Weinbaum et al., 2008) and hepatitis C (CDC, 1998, 2001). The National Institutes of Health (NIH) has developed consensus documents on the management of hepatitis B (NIH, 2008) and hepatitis C (NIH, 2002). WHO has published guidelines related to hepatitis B vaccination of children (WHO, 2001). A number of not-for-profit organizations have also worked to increase awareness of the diseases, educate the public about prevention, and advocate for those chronically infected with HBV and HCV. Although government and nongovernment efforts have led to a decline in the number of cases, chronic hepatitis B and hepatitis C continue to be serious public-health problems in the United States. For that reason, CDC in conjunction with the National Viral Hepatitis Roundtable, a not-for-profit coalition of public, private, and voluntary organizations; the Department of Health and Human Services Office of Minority Health; and VA sought guidance from the Institute of Medicine (IOM) in identifying missed opportunities related to the prevention and control of HBV and HCV infections. IOM was asked to focus on hepatitis B and hepatitis C because they are common in the United States and can lead to chronic disease. This report does not address hepatitis A virus, hepatitis E virus, or hepatitis D virus (also called the hepatitis delta virus) infections.
The specific charge to the committee follows:
The IOM will form a committee to determine ways to reduce new HBV and HCV infections and the morbidity and mortality related to chronic viral hepatitis. The committee will assess current prevention and control activities and identify priorities for research, policy, and action. The committee will highlight issues that warrant further investigations and opportunities for collaboration between private and public sectors. In conducting its work, the committee might want to consider:
Strategies for preventing new HBV and HCV infections:
-
Improving vaccine coverage among vulnerable populations to reach national transmission elimination goals.
-
Increasing the proportion of persons aware of their chronic infection status.
-
Identifying barriers to the identification, counseling, and testing of persons at risk for chronic hepatitis, and ways they can be reduced and eliminated.
-
Promoting prevention among adolescents and adults who engage in risky behaviors, particularly those known to have screened positive for HCV and HBV infection.
-
Determining optimal ways to identify, develop, and implement prevention programs among at-risk populations.
-
Development of an effective HCV vaccine.
Strategies for reducing morbidity and mortality from chronic HBV and HCV infections:
-
Providing appropriate medical referral, evaluation, and management of chronically infected persons.
-
Assessing health-care utilization and outcomes for persons with chronic infections, and opportunities for prevention and care to reduce healthcare-related costs.
-
Reducing health disparities in morbidity and mortality from viral hepatitis.
-
Improving clinical surveillance of markers of disease progression and stage of hepatocellular carcinoma associated with chronic viral hepatitis and associated cirrhosis.
Assess the type and quality of data needed from state and local viral hepatitis surveillance systems to guide and evaluate prevention services:
-
Assess the role of acute disease surveillance in monitoring new infections, detecting outbreaks, identifying vaccine failures and documenting the elimination of HBV transmission.
-
Assess the role of state and local chronic disease surveillance in describing the burden of morbidity and mortality related to chronic hepatitis B and hepatitis C and related liver cirrhosis and cancer, the extent of
-
ongoing risk behaviors, and the impact of HIV co-infection and other cofactors.
-
Assess the role of state and local disease registries in the delivery of prevention and care services for persons with chronic hepatitis B and persons with hepatitis C.
-
Assess the role of laboratory testing strategies for the identification of markers for acute HCV infection.
-
Assess laboratory testing strategies for identification of antiviral resistance for HBV and HCV.
Finally, the committee should pay attention to addressing the special needs of specific subpopulations at high risk, such as Asian Americans, African Americans, and persons born in HBV-endemic countries.
THE COMMITTEE’S APPROACH TO ITS TASK
To address its charge, the committee first reviewed available evidence on a variety of topics related to the prevention of hepatitis B and hepatitis C, management of these diseases, and surveillance activities related to viral hepatitis. The evidence was drawn from the published literature and from open-session presentations by recognized experts in the field (see Appendix B). Oral testimony presented by members of the public during the open sessions was also taken into account. Additional information was obtained from written testimony submitted to the committee (available from the National Academies’ Public Access Records Office, publicac@nas.edu).
A comprehensive review and evaluation of treatments for HBV and HCV infections (for example, which medications to use) is beyond the scope of this report. However, treatment information can be found in guidelines published by the American Association for the Study of Liver Diseases (Ghany et al., 2009; Lok and McMahon, 2009) and in NIH consensus statements on the management of hepatitis B (NIH, 2008) and hepatitis C (NIH, 2002).
The committee also has not been tasked with comprehensively reviewing information about the safety of the hepatitis B vaccine. Safety issues surrounding this vaccine were reviewed in the IOM report Immunization Safety Review: Hepatitis B Vaccine and Demyelinating Neurological Disorders (IOM, 2002). The committee that wrote that report concluded that the evidence favored rejection of a causal relationship between hepatitis B vaccine administered to adults and incident multiple sclerosis and multiple-sclerosis relapse. It also found the evidence inadequate for accepting or rejecting a causal relationship between hepatitis B vaccine and the first episode of a central nervous system demyelinating disorder, acute disseminated encephalomyelitis, optic neuritis, transverse myelitis, Guillain-Barré syndrome, or brachial neuritis. IOM has undertaken another review of the
safety of the hepatitis B vaccine, and the findings are expected to be available in 2011.
The committee that wrote the present report met five times in the period December 2008–August 2009. During the meetings, the committee evaluated the evidence and deliberated on issues relevant to its charge. Types of evidence taken into consideration included international, federal, state, and community guidelines, programs, and other activities aimed at preventing new cases of HBV and HCV infection, identifying chronic cases of hepatitis B and hepatitis C, and managing those cases. It also explored federal and state surveillance mechanisms for identifying and tracking hepatitis B and hepatitis C cases. The committee began by identifying problems with and gaps in the current prevention and control systems. It also examined model programs for other infectious diseases, such as those covered under the Ryan White CARE Act (Health Resources and Services Administration, 2009). The committee developed evidence-based recommendations to address the problems with the current systems to reduce the numbers of new HBV and HCV infections, to manage the care of chronically infected people more effectively by reducing morbidity and mortality, and to improve surveillance of chronic hepatitis B and hepatitis C cases.
The committee focused on making recommendations that could be implemented with existing knowledge and available tools to advance prevention and control of chronic viral hepatitis in a timely manner. Although the committee recognizes the importance of basic research in this field, it believes that given the scope of the problem and the lack of available resources, its focus should be on improving prevention and control services. As a result, the committee did not address basic-research questions in the field extensively. Nor did it conduct cost–benefit analyses of its recommendations.
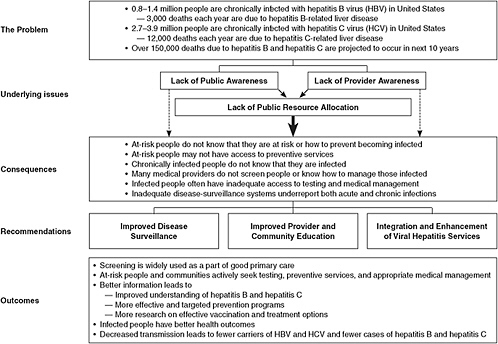
The committee’s general approach is presented in Figure 1-2. After defining the scope of the problem and reviewing the available evidence, the committee identified the primary underlying factors that impede current efforts to prevent and control hepatitis B and hepatitis C. The committee believes that a lack of awareness about viral hepatitis among both the general public and health-care and social-service providers is leading to continued high rates of morbidity and mortality from hepatitis B and hepatitis C. Consistent themes were found in all the materials reviewed by the committee; as a result, this report is organized according to four principal categories:
-
Increased hepatitis B vaccination rates in various populations (Chapter 4).
-
Improved integration and enhancement of viral hepatitis services for specific at-risk populations and in health-care and other settings (Chapter 5).
REFERENCES
Altekruse, S. F., K. A. McGlynn, and M. E. Reichman. 2009. Hepatocellular carcinoma inci-2009. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. Journal of Clinical Oncology 27(9):1485-1491.
American Cancer Society. 2009. Cancer facts & figures, 2009. Atlanta, GA.
Amon, J. J., R. S. Garfein, L. Ahdieh-Grant, G. L. Armstrong, L. J. Ouellet, M. H. Latka, D. Vlahov, S. A. Strathdee, S. M. Hudson, P. Kerndt, D. Des Jarlais, and I. T. Williams. 2008. Prevalence of hepatitis C virus infection among injection drug users in the United States, 1994-2004. Clinical Infectious Diseases 46(12):1852-1858.
Armstrong, G. L., A. Wasley, E. P. Simard, G. M. McQuillan, W. L. Kuhnert, and M. J. Alter. 2006. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Annals of Internal Medicine 144(10):705-714.
Beasley, R., and L. Hwang. 1991. Overview of the epidemiology of heptocellular carcinoma. In Viral hepatitis and liver disease. Proceedings of the 1990 international symposium on viral hepatitis and liver disease, edited by F. B. Hollinger, S. Lemon, and H. S. Margolis. Baltimore: Williams & Wilkins. Pp. 532-525.
Bonacini, M., M. D. Groshen, M. C. Yu, S. Govindarajan, and K. L. Lindsay. 2001. Chronic hepatitis C in ethnic minority patients evaluated in Los Angeles county. American Journal of Gastroenterology 96(8):2438-2441.
Boutwell, A. E., S. A. Allen, and J. D. Rich. 2005. Opportunities to address the hepatitis C epidemic in the correctional setting. Clinical Infectious Diseases 40(s5):S367-S372.
But, D. Y., C. L. Lai, and M. F. Yuen. 2008. Natural history of hepatitis-related hepatocellular carcinoma. World Journal of Gastroenterology 14(11):1652-1656.
CDC (Centers for Disease Control and Prevention). 1998. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Morbidity and Morality Weekly: Recommendations and Reports 47(RR-19):1-39.
———. 2001. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. Morbidity and Morality Weekly: Recommendations and Reports 50(RR-11):1-52.
———. 2004. Incidence of acute hepatitis B—United States, 1990-2002. Morbidity and Mortality Weekly Report 52(51-52):1252-1254.
———. 2006. Screening for chronic hepatitis B among Asian/Pacific Islander populations—New York City, 2005. Morbidity and Mortality Weekly Report 55(18):505-509.
———. 2007. FAQs for health professionals: Hepatitis B. http://www.cdc.gov/hepatitis/HBV/HBVfaq.htm#overview (accessed August 21, 2009).
———. 2008a. Disease burden from hepatitis A, B, and C in the United States. http://www.cdc.gov/hepatitis/statistics.htm (accessed August 21, 2209)
———. 2008b. HIV prevalence estimates—United States, 2006. Morbidity and Mortality Weekly Report 57(39):1073-1076.
———. 2008c. Newborn hepatitis B vaccination coverage among children born January 2003-June 2005—United States. Morbidity and Mortality Weekly Report 57(30):825-828.
———. 2009a. The ABCs of hepatitis. http://www.cdc.gov/hepatitis/Resources/Professionals/PDFs/ABCTable.pdf (accessed November 6, 2009).
———. 2009b. HIV/AIDS statistics and surveillance. http://www.cdc.gov/hiv/topics/surveillance/basic.htm (accessed August 24, 2009).
———. 2009c. Notice to readers: National hepatitis B initiative for Asian Americans/Native Hawaiian and other Pacific Islanders. Morbidity and Mortality Weekly Report 58(18):503.
———. 2009d. Viral hepatitis: Statistics and surveillance. http://www.cdc.gov/hepatitis/Statistics.htm (accessed August 24, 2009).
Chang, E. T., T. H. M. Keegan, S. L. Gomez, G. M. Le, C. A. Clarke, S. K. So, and S. L. Glaser. 2007. The burden of liver cancer in Asians and Pacific Islanders in the greater San Francisco Bay area, 1990 through 2004. Cancer 109(10):2100-2108.
Chen, G., W. Lin, F. Shen, U. H. Iloeje, W. T. London, and A. A. Evans. 2006. Past HBV viral load as predictor of mortality and morbidity from HCC and chronic liver disease in a prospective study. American Journal of Gastroenterology 101(8):1797-1803.
Chesson, H. W., J. M. Blandford, T. L. Gift, G. Tao, and K. L. Irwin. 2004. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspectives on Sexual and Reproductive Health 36(1):11-19.
Cheung, R. C. 2000. Epidemiology of hepatitis C virus infection in American veterans. American Journal of Gastroenterology 95(3):740-747.
Daniels, D., S. Grytdal, and A. Wasley. 2009. Surveillance for acute viral hepatitis—United States, 2007. Morbidity and Mortality Weekly Report: Surveillance Summaries 58(3):1-27.
Dehesa-Violante, M., and R. Nuñez-Nateras. 2007. Epidemiology of hepatitis virus B and C. Archives of Medical Research 38(6):606-611.
Deuffic-Burban, S., M. K. Mohamed, B. Larouze, F. Carrat, and A. J. Valleron. 2006. Expected increase in hepatitis C-related mortality in Egypt due to pre-2000 infections. Journal of Hepatology 44(3):455-461.
Dominitz, J. A., E. J. Boyko, T. D. Koepsell, P. J. Heagerty, C. Maynard, J. L. Sporleder, A. Stenhouse, M. A. Kling, W. Hrushesky, C. Zeilman, S. Sontag, N. Shah, F. Ona, B. Anand, M. Subik, T. F. Imperiale, S. Nakhle, S. B. Ho, E. J. Bini, B. Lockhart, J. Ahmad, A. Sasaki, B. van der Linden, D. Toro, J. Martinez-Souss, V. Huilgol, S. Eisen, and K. A. Young. 2005. Elevated prevalence of hepatitis C infection in users of United States Veterans Medical Centers. Hepatology 41(1):88-96.
Drucker, E., P. G. Alcabes, and P. A. Marx. 2001. The injection century: Massive unsterile injections and the emergence of human pathogens. Lancet 358(9297):1989-1992.
The Economist. 2006. Asia: B is for bigotry; hepatitis B in China. November 18, 2006, p. 66.
Frank, C., M. K. Mohamed, G. T. Strickland, D. Lavanchy, R. R. Arthur, L. S. Magder, T. El Khoby, Y. Abdel-Wahab, E. S. Aly Ohn, W. Anwar, and I. Sallam. 2000. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet 355(9207):887-891.
Garfein, R. S., M. C. Doherty, E. R. Monterroso, D. L. Thomas, K. E. Nelson, and D. Vlahov. 1998. Prevalence and incidence of hepatitis C virus infection among young adult injection drug users. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology 18 Suppl 1:S11-19.
Ge, D., J. Fellay, A. J. Thompson, J. S. Simon, K. V. Shianna, T. J. Urban, E. L. Heinzen, P. Qiu, A. H. Bertelsen, A. J. Muir, M. Sulkowski, J. G. McHutchison, and D. B. Goldstein. 2009. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 461(7262):399-401.
Ghany, M. G., D. B. Strader, D. L. Thomas, and L. Seeff. 2009. Diagnosis, management, and treatment of hepatitis C: An update. Hepatology 49(4):1335-1374.
Grant, W. C., R. R. Jhaveri, J. G. McHutchison, K. A. Schulman, and T. L. Kauf. 2005. Trends in health care resource use for hepatitis C virus infection in the United States. Hepatology 42(6):1406-1413.
Groom, H., E. Dieperink, D. B. Nelson, J. Garrard, J. R. Johnson, S. L. Ewing, H. Stockley, J. Durfee, Y. Jonk, M. L. Willenbring, and S. B. Ho. 2008. Outcomes of a hepatitis C screening program at a large urban VA medical center. Journal of Clinical Gastroenterology 42(1):97-106.
Hagan, H., J. Campbell, H. Thiede, S. Strathdee, L. Ouellet, F. Kapadia, S. Hudson, and R. S. Garfein. 2006. Self-reported hepatitis C virus antibody status and risk behavior in young injectors. Public Health Reports 121(6):710-719.
Hagan, H., E. R. Pouget, D. C. Des Jarlais, and C. Lelutiu-Weinberger. 2008. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: The influence of time and place. American Journal of Epidemiology 168(10):1099-1109.
Hagan, H., H. Thiede, N. S. Weiss, S. G. Hopkins, J. S. Duchin, and E. R. Alexander. 2001. Sharing of drug preparation equipment as a risk factor for hepatitis C. American Journal of Public Health 91(1):42-46.
Hahn, J. A., K. Page-Shafer, P. J. Lum, P. Bourgois, E. Stein, J. L. Evans, M. P. Busch, L. H. Tobler, B. Phelps, and A. R. Moss. 2002. Hepatitis C virus seroconversion among young injection drug users: Relationships and risks. Journal of Infectious Diseases 186(11):1558-1564.
Hauri, A. M., G. L. Armstrong, and Y. J. Hutin. 2004. The global burden of disease attributable to contaminated injections given in health care settings. International Journal of STD and AIDS 15(1):7-16.
Health Resources and Services Administration. 2009. The Ryan White HIV/AIDS program. http://hab.hrsa.gov/about/ (accessed August 21, 2009).
Hunt, D. R., and S. Saab. 2009. Viral hepatitis in incarcerated adults: A medical and public health concern. American Journal of Gastroenterology 104(4):1024-1031.
Hutin, Y. J. F., A. M. Hauri, and G. L. Armstrong. 2003. Use of injections in healthcare settings worldwide, 2000: Literature review and regional estimates. BMJ 327(7423):1075-1080.
Hutton, D. W., D. Tan, S. K. So, and M. L. Brandeau. 2007. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander adults for hepatitis B. Annals of Internal Medicine 147(7):460-469.
IOM (Institute of Medicine). 2002. Immunization safety review: Hepatitis B vaccine and demyelinating neurological disorders. Edited by K. Stratton, D. Almario, and M. C. McCormick. Washington, DC: The National Academies Press.
Jeffers, L. J., W. Cassidy, C. D. Howell, S. Hu, and K. R. Reddy. 2004. Peginterferon alfa-2a (40 kd) and ribavirin for black American patients with chronic HCV genotype 1. Hepatology 39(6):1702-1708.
Kamal, S. M. 2008. Acute hepatitis C: A systematic review. American Journal of Gastroenterology 103(5):1283-1297; quiz 1298.
Kim, W. R., N. A. Terrault, R. A. Pedersen, T. M. Therneau, E. Edwards, A. A. Hindman, and C. L. Brosgart. 2009. Trends in waitlist registration for liver transplantation for viral hepatitis in the US. Gastroenterology 137(5):1608-1686.
Kumar, R., V. Singla, and S. Kacharya. 2008. Impact and management of hepatitis B and hepatitis C virus co-infection in HIV patients. Tropical Gastroenterology 29(3):136-147.
Kussman, M. J. 2007. National hepatitis C program. VHA Directive 2007-022. Department of Veterans Affairs.
Lavanchy, D. 2008. Chronic viral hepatitis as a public health issue in the world. Best Practice and Research. Clinical Gastroenterology 22(6):991-1008.
———. 2009. The global burden of hepatitis C. Liver International 29(s1):74-81.
Lehman, E. M., and M. L. Wilson. 2009. Epidemic hepatitis C virus infection in Egypt: Estimates of past incidence and future morbidity and mortality. Journal of Viral Hepatitis 16(9):650-658.
Leigh, J. P., C. L. Bowlus, B. N. Leistikow, and M. Schenker. 2001. Costs of hepatitis C. Archives of Internal Medicine 161(18):2231-2237.
Lin, S. Y., E. T. Chang, and S. K. So. 2007. Why we should routinely screen Asian American adults for hepatitis B: A cross-sectional study of Asians in California. Hepatology 46:1034-1040.
Lok, A. S., and B. J. McMahon. 2009. Chronic hepatitis B: Update 2009. Hepatology 50(3):661-662.
Macalino, G. E., J. C. Hou, M. S. Kumar, L. E. Taylor, I. G. Sumantera, and J. D. Rich. 2004. Hepatitis C infection and incarcerated populations. International Journal of Drug Policy 15(2):103-114.
Maher, L., B. Jalaludin, K. G. Chant, R. Jayasuriya, T. Sladden, J. M. Kaldor, and P. L. Sargent. 2006. Incidence and risk factors for hepatitis C seroconversion in injecting drug users in Australia. Addiction 101(10):1499-1508.
Mast, E. E., H. S. Margolis, A. E. Fiore, E. W. Brink, S. T. Goldstein, S. A. Wang, L. A. Moyer, B. P. Bell, and M. J. Alter. 2005. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: Recommendations of the advisory committee on immunization practices (ACIP) part 1: Immunization of infants, children, and adolescents. Morbidity and Morality Weekly: Recommendations and Reports 54(RR-16):1-31.
Mast, E. E., C. M. Weinbaum, A. E. Fiore, M. J. Alter, B. P. Bell, L. Finelli, L. E. Rodewald, J. M. Douglas, Jr., R. S. Janssen, and J. W. Ward. 2006. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: Recommendations of the advisory committee on immunization practices (ACIP) part II: Immunization of adults. Morbidity and Morality Weekly: Recommendations and Reports 55(RR-16):1-33; quiz CE31-34.
McMahon, B. J. 2004. The natural history of chronic hepatitis B virus infection. Seminars in Liver Disease 24(Suppl 1):17-21.
———. 2008. Natural history of chronic hepatitis B—clinical implications. Medscape Journal of Medicine 10(4):91.
Missiha, S. B., M. Ostrowski, and E. J. Heathcote. 2008. Disease progression in chronic hepatitis C: Modifiable and nonmodifiable factors. Gastroenterology 134(6):1699-1714.
Muir, A. J., J. D. Bornstein, and P. G. Killenberg. 2004. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. New England Journal of Medicine 350(22):2265-2271.
NIH (National Institutes of Health). 2002. NIH consensus statement on management of hepatitis C: 2002. NIH Consensus and State-of-the-Science Statements 19(3):1-46.
———. 2008. NIH consensus development conference statement on the management of Hepatitis B. http://consensus.nih.gov/2008/hebB%20draft%20statement%20102208_FINAL.pdf (accessed August 21, 2009)
Perz, J. F., G. L. Armstrong, L. A. Farrington, Y. J. Hutin, and B. P. Bell. 2006. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. Journal of Hepatology 45(4):529-538.
Pradat, P., N. Voirin, H. L. Tillmann, M. Chevallier, and C. Trepo. 2007. Progression to cirrhosis in hepatitis C patients: An age-dependent process. Liver International 27(3):335-339.
Pungpapong, S., W. R. Kim, and J. J. Poterucha. 2007. Natural history of hepatitis B virus infection: An update for clinicians. Mayo Clinic Proceedings 82(8):967-975.
Pybus, O. G., P. V. Markov, A. Wu, and A. J. Tatem. 2007. Investigating the endemic transmission of the hepatitis C virus. International Journal for Parasitology 37(8-9):839-849.
Pyenson, B., K. Fitch, and K. Iwasaki. 2009. Consequences of hepatitis C virus (HCV). Costs of a baby boomer epidemic of liver disease. New York: Vertex Pharmaceuticals Incorporated.
Rodriguez-Torres, M., L. J. Jeffers, M. Y. Sheikh, L. Rossaro, V. Ankoma-Sey, F. M. Hamzeh, and P. Martin. 2009. Peginterferon alfa-2a and ribavirin in Latino and non-Latino whites with hepatitis C. New England Journal of Medicine 360(3):257-267.
Shepard, C. W., L. Finelli, and M. J. Alter. 2005. Global epidemiology of hepatitis C virus infection. The Lancet Infectious Diseases 5(9):558-567.
Shepard, C. W., E. P. Simard, L. Finelli, A. E. Fiore, and B. P. Bell. 2006. Hepatitis B virus infection: Epidemiology and vaccination. Epidemiologic Reviews 28:112-125.
Sloan, K. L., K. A. Straits-Troster, J. A. Dominitz, and D. R. Kivlahan. 2004. Hepatitis C tested prevalence and comorbidities among veterans in the US Northwest. Journal of Clinical Gastroenterology 38(3):279-284.
Smyth, B. P., E. Keenan, and J. J. O’Connor. 2000. Assessment of hepatitis C infection in injecting drug users attending an addiction treatment clinic. Irish Journal of Medical Science 169(2):129-132.
Sulkowski, M. S. 2008. Viral hepatitis and HIV coinfection. Journal of Hepatology 48(2):353-367.
Tan, A., S. H. Yeh, C. J. Liu, C. Cheung, and P. J. Chen. 2008. Viral hepatocarcinogenesis: From infection to cancer. Liver International 28(2):175-188.
Thomas, D. L., J. Astemborski, R. M. Rai, F. A. Anania, M. Schaeffer, N. Galai, K. Nolt, K. E. Nelson, S. A. Strathdee, L. Johnson, O. Laeyendecker, J. Boitnott, L. E. Wilson, and D. Vlahov. 2000. The natural history of hepatitis C virus infection: Host, viral, and environmental factors. Journal of the American Medical Association 284(4):450-456.
Thomas, D. L., C. L. Thio, M. P. Martin, Y. Qi, D. Ge, C. O’Huigin, J. Kidd, K. Kidd, S. I. Khakoo, G. Alexander, J. J. Goedert, G. D. Kirk, S. M. Donfield, H. R. Rosen, L. H. Tobler, M. P. Busch, J. G. McHutchison, D. B. Goldstein, and M. Carrington. 2009. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature 461(7265):798-801.
Thorpe, L. E., L. J. Ouellet, R. Hershow, S. L. Bailey, I. T. Williams, J. Williamson, E. R. Monterroso, and R. S. Garfein. 2002. Risk of hepatitis C virus infection among young adult injection drug users who share injection equipment. American Journal of Epidemiology 155(7):645-653.
U.S. Census Bureau. 2008. 2007 American community survey. http://factfinder.census.gov/servlet/STTable?_bm=y&-qr_name=ACS_2008_3YR_G00_S0502&-geo_id=01000US&-ds_name=ACS_2008_3YR_G00_&-_lang=en&-format=&-CONTEXT=st (accessed Au-gust 20, 2009).
U.S. Department of Homeland Security. 2009. Yearbook of immigration statistics: 2008. Table 3: Persons obtaining legal permanent resident status by region and country of birth: Fiscal years 1999 to 2008. http://www.dhs.gov/files/statistics/publications/yearbook.shtm (accessed August 21, 2009).
Vong, S., and B. P. Bell. 2004. Chronic liver disease mortality in the United States, 1990-1998. Hepatology 39(2):476-483.
Ward, J. 2008a. FY 2008 domestic enacted funds. Presentation to the committee: December 4, 2008.
Ward, J. W. 2008b. Time for renewed commitment to viral hepatitis prevention. American Journal of Public Health 98(5):779-781.
Wasley, A., S. Grytdal, and K. Gallagher. 2008. Surveillance for acute viral hepatitis—United States, 2006. Morbidity and Mortality Weekly Report: Surveillance Summaries 57(2):1-24.
Weinbaum, C., R. Lyerla, and H. S. Margolis. 2003. Prevention and control of infections with hepatitis viruses in correctional settings. Centers for Disease Control and Prevention. Morbidity and Morality Weekly: Recommendations and Reports 52(RR-1):1-36; quiz CE31-CE34.
Weinbaum, C. M., I. Williams, E. E. Mast, S. A. Wang, L. Finelli, A. Wasley, S. M. Neitzel, and J. W. Ward. 2008. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. Morbidity and Morality Weekly: Recommendations and Reports 57(RR-8):1-20.
Weiss, R. A., and A. J. McMichael. 2004. Social and environmental risk factors in the emergence of infectious diseases. Nature Medicine 10(12 Suppl):S70-S76.
WHO (World Health Organization). 2001. Introduction of hepatitis B vaccine into childhood immunization services: Management guidelines, including information for health workers and parents. Geneva: World Health Organization.
———. 2009. Hepatitis B fact sheet no. 204. http://www.who.int/mediacentre/factsheets/fs204/en/ (accessed October 20, 2008).
Wise, M., S. Bialek, L. Finelli, B. P. Bell, and F. Sorvillo. 2008. Changing trends in hepatitis C-related mortality in the United States, 1995-2004. Hepatology 47(4):1128-1135.
Wong, J., G. McQuillan, J. McHutchison, and T. Poynard. 2000. Estimating future hepatitis C morbidity, mortality, and costs in the United States. American Journal of Public Health 90(10):1562-1569.
Xia, X., J. Luo, J. Bai, and R. Yu. 2008. Epidemiology of hepatitis C virus infection among injection drug users in China: Systematic review and meta-analysis. Public Health 122(10):990-1003.