4
PRELIMINARY FINDINGS
This chapter highlights findings related to the health consequences of service in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) and readjustment needs resulting from deployment; it also examines the social consequences of deployment and the special issues faced by women and ethnic minorities; finally, it examines the need to plan for the long-term support of veterans, families, and communities affected by deployment to OEF and OIF. Inasmuch as this is the preliminary or initial phase of the committee’s report, the topics discussed in this chapter are not addressed in detail. Rather, the committee is raising and exploring issues and expects to examine all the topics of concern in more detail in phase 2. Data on OEF and OIF veterans are lacking, but the committee members have examined information from studies of Vietnam veterans if they believed them to be instructive with regard to OEF and OIF veterans. The paucity of data is not surprising as studies take time to design, sample strategies need to be approved, data need to be analyzed, and the wars are ongoing. It took at least 15 years after the Vietnam War before the National Vietnam Veterans Readjustment Study began.
CONSEQUENCES OF SERVICE IN OPERATION ENDURING FREEDOM AND OPERATION IRAQI FREEDOM FOR MILITARY PERSONNEL AND THEIR FAMILIES AND EFFECTS ON READJUSTMENT
Since the beginning of the wars in Afghanistan (OEF) and Iraq (OIF), there have been 5,286 fatalities among US military service members.1 During the same period, 36,021 have been wounded in Iraq and Afghanistan as a direct result of hostile actions; the Army has borne the brunt of the casualties (CRS, 2009). Blasts from improvised explosive devices (IEDs) have caused most of the deaths and nonfatal injuries. Injuries from blast exposure due to IEDs have resulted in numerous physical and mental health outcomes, such as traumatic brain injury (TBI), amputation, spinal-cord injury, chronic pain, headache, injury to the eye and ear, posttraumatic stress disorder (PTSD), and major depression. Military personnel exposed to multiple blasts have an increased probability of sustaining an injury that can lead to severe or long-term physical and psychologic impairments (Nelson et al., 2008). Various impairments often occur together, making treatment and readjustment more difficult. In recognition of the additional challenges faced by veterans suffering comorbid deployment-related conditions, the Department of Veterans
Affairs (VA) in 2005 defined polytrauma as “injury to the brain in addition to other body parts or systems resulting in physical, cognitive, psychological, or psychosocial impairments and functional disability” (VA, 2005). Since then, its definition has been expanded to include concurrent injury to two or more body parts or systems that results in cognitive, physical, psychologic, or other psychosocial impairments (VA, 2009b).
Many military personnel returning from OEF and OIF appear to have more complex and emotional trauma than has been seen in past wars (Friedemann-Sanchez et al., 2008). That observation may be due, in part, to an improved chance of survival because of the widespread use of body armor, improved battlefield medical response, and advances in aeromedical evacuation. Polytrauma patients in particular have complex rehabilitation needs, including addressing and treating for pain, TBI, PTSD, and other comorbid conditions to facilitate readjustment (Sayer et al., 2009). Although TBI, amputations, PTSD, and major depression are distinct postcombat health outcomes, they cause overlapping long-term, possibly lifelong, effects on people’s lives. People affected by those types of combat-related injuries and mental health disorders tend to report poorer health and impaired function in many life activities than people who do not suffer those types of injuries. Moreover, physical injuries and mental health disorders often require treatment by multiple health-care services for an extended period. The problem of polytrauma and the associated lifelong, recurring comorbid conditions, such as PTSD and chronic pain, requires the development of integrated approaches to clinical care that can replace traditional treatment systems that focus on isolated problems (Belanger et al., 2005; Gironda et al., 2009).
Those injuries also have the potential to affect family life even if the injured service members recover fully. For example, family members may need to relocate if the proper treatment facilities are not available close to home (Cozza et al., 2005). Injuries that result in long-term changes in behavior or abilities can seriously challenge marriages, thrusting the spouse into a caregiving role, increasing the risk of depression and other psychologic problems, and increasing the likelihood of divorce (Blais and Boisvert, 2005; Calhoun et al., 2002).
The committee has decided, in this preliminary report, to focus on the most serious health, psychologic, and social outcomes related to OEF and OIF service. Those outcomes and possible readjustment needs associated with them are discussed below.
Traumatic Brain Injury and Related Blast Injuries
Throughout OEF and OIF, explosive devices have become more powerful, their detonation systems more creative, and their additives more devastating. TBI2 is the most common injury among those wounded in OEF and OIF and is a significant cause of mortality and morbidity. In 2003–2007, the Military Health System (MHS) recorded that 43,779 patients had a diagnosis of TBI (CRS, 2009). The estimates vary: some studies have found that about 10–20% of veterans returning from OEF and OIF have TBI (Elder and Cristian, 2009; Tanielian and Jaycox, 2008), and others have found that TBI accounts for up to one-third of all battlefield injuries (Meyer et al., 2008). Although penetrating brain injuries are easily identified, closed TBI is more common and, when mild, can go unnoticed. A concern for troops, veterans, and their
family members is that substantial long-term effects have been associated with TBI (IOM, 2009). In some cases a TBI can go undetected until the service member returns home and can no longer function as he or she did before deployment; this can result in frustration and problems for both service member and family alike (Zeitzer and Brooks, 2008). A recent Institute of Medicine (IOM) report (2009) noted that numerous adverse long-term outcomes are related to TBI. Although some acute outcomes, such as some neurocognitive and psychosocial dysfunction, resolve or lessen over time, other sequelae, such as psychiatric outcomes, become more apparent several years after injury. Many studies have found a dose–response relationship with regard to TBI severity and outcome: generally, the more severe the TBI, the more severe the outcome. However, the IOM report identified several outcomes that can persist even after mild TBI, including unprovoked seizures, depression, aggression, and postconcussive symptoms, such as memory problems, dizziness, and irritability. TBI can cause life-long impairments, and rehabilitation and recovery might take many years.
One common complication of TBI is pain (Nampiaparampil, 2008), particularly headache, and there is growing evidence that it can be a long-term problem (Gironda et al., 2009). A study of OEF and OIF veterans diagnosed with TBI found that those with neurocognitive impairments were more likely to have headache, migraine-like headache, more severe pain, and more frequent headache than veterans without neurocognitive impairment (Ruff et al., 2008). Similarly, a recent study (Theeler and Erickson, 2009) found an association between a history of mild head trauma, usually caused by blast exposure, and onset or worsening of headache in combat troops; it was also noted that the soldiers diagnosed with TBI usually experienced migraine-type headaches.
There is clear evidence of increased mortality in the acute phase after moderate to severe TBI and for some time following in both military and civilian populations (Baguley et al., 2000; Brown et al., 2004; Corkin et al., 1984; Harrison-Felix et al., 2004; Lewin et al., 1979; Ratcliff et al., 2005; Rish et al., 1983; Selassie et al., 2005; Shavelle and Strauss, 2000; Walker et al., 1971; Weiss et al., 1982). In the military literature, posttraumatic epilepsy in patients who initially survive penetrating head injury is associated with an increased risk of death and about a 5-year decrease in life expectancy (Corkin et al., 1984; Walker et al., 1971; Weiss et al., 1982). Studies of the subset of more severely injured patients who survive initial hospitalization and require inpatient rehabilitation have shown a worse prognosis that is consistent with the greater degree of residual compromise: mortality some 2–7 times as high as that in age- and sex-matched comparison populations (Brown et al., 2004; Harrison-Felix et al., 2004; Ratcliff et al., 2005; Selassie et al., 2005).
TBI can also lead to disruptions in higher-level functions of everyday life, including social relationships, independent living, and employment. Numerous studies have documented that penetrating brain injuries have adverse consequences for long-term employment outcomes (Dikmen et al., 1994; Doctor et al., 2005; McLeod et al., 2004; Schwab et al., 1993). Moreover, although some impairments might be related to injuries to other parts of the body sustained at the time of TBI, moderate to severe TBI leads to more functional impairment than do injuries to other parts of the body alone (Dikmen et al., 1995; Gerberich et al., 1997; McLeod et al., 2004; Oddy et al., 1978; Ommaya, 1996). The adverse effects of TBI on leisure and recreation, social relationships, functional status, quality of life, and independent living clearly affect readjustment and family life and relationships. By one year after injury, psychosocial problems appear to be greater than problems in basic activities of daily living (IOM, 2009).
Most long-term outcomes of TBI were observed at or soon after the time of injury and persisted, presumably indefinitely. However, other outcomes were observed to develop later, possibly as a result of an interaction with aging processes. Conditions found, in at least some studies, to emerge or re-emerge in later life included cognitive deficits (e.g., Corkin et al., 1989), depression (e.g., Holsinger et al., 2002), suicide (e.g., Teasdale and Engberg, 2001), premature death (e.g., Harrison-Felix et al., 2004), progressive dementia (e.g., Plassman et al., 2000), and parkinsonism (e.g., Bower et al., 2003).
Posttraumatic Stress Disorder and Traumatic Brain Injury
PTSD (discussed in more detail below) can co-occur with TBI (Hill et al., 2009; IOM, 2008b). It has been noted that physical trauma and psychologic trauma reported by OEF and OIF service members and veterans rarely appear in isolation and often present with more than one medical condition simultaneously (that is, they are comorbid) (Lew et al., 2009). Although the data on rates of comorbidity in the OEF and OIF population are sparse, research in civilians suggests that those with co-occurring mental and physical problems typically require more specialized treatment and have poorer outcomes than those with a single condition only (Shalev et al., 1998). A recent RAND report (Tanielian and Jaycox, 2008) estimated that some combination of comorbid PTSD, major depression, and TBI is not uncommon in OEF and OIF veterans. The report noted that about one-third of service members who have been deployed have at least one of the three conditions, and about 5% manifest symptoms of all three (Tanielian and Jaycox, 2008). Furthermore, of 289,328 OEF and OIF veterans seen at VA health care facilities following deployment, 106,726 (36.9%) received mental health diagnoses and of those receiving any such diagnosis, 29% had two and 33% had 3 or more different mental health conditions (Seal et al., 2009). Of those veterans, 62,929 (21.8%) were diagnosed with PTSD and 50,432 (17.4%) with depression.
Hoge and Castro (2006) found that the prevalence of PTSD in soldiers who had physical injuries was 31.8%. In a more recent study of over 2,000 postdeployment active-duty service members, those who reported loss of consciousness had the highest rate of PTSD, 43.9%; the rate of PTSD was 27.3% in those who had altered mental status but no loss of consciousness, 16.2% in those who had only physical injuries, and 9.1% in those who reported no injury (Hoge et al., 2008). Moreover, mild TBI accompanied by symptoms of PTSD and other mental problems (Schneiderman et al., 2008) was more common in blast-injured patients than in those who had non-blast-related injuries. In a study of National Guard troops returning from the Gulf War, most of the PTSD reported at 2 years was present at 6 months after deployment, but symptom severity increased over the interval. Those who were highly symptomatic at 6 months were still highly symptomatic 2 years later (Southwick et al., 1995).
Auditory and Visual Impairment
Tympanic membrane perforation is a blast injury that occurs in about 10% of those wounded by combat-related explosions (Ritenour et al., 2008). In many cases, hearing loss accompanies TBI. Lew et al. (2007a) reported on the prevalence and characteristics of auditory dysfunction in patients admitted to a VA TBI inpatient unit before and after the start of OEF. Their findings indicated a high prevalence of hearing loss and tinnitus in a growing population of returning service members. Inasmuch as effective communication is needed for successful
rehabilitation, especially in patients who have comorbid TBI, clinically significant hearing loss presents problems for readjustment.
In addition to chronic pain, headaches, and hearing loss, ocular trauma is a direct consequence of blast injury and TBI. Combat troops who are exposed to a blast that results in mild TBI are at risk for visual dysfunction, and combat troops who have polytrauma are at risk for visual dysfunction and impairment (Brahm et al., 2009). It has been noted that TBI occurs in 67% of cases of combat ocular trauma, and that ocular trauma is a common finding in TBI cases (Weichel et al., 2009). Those outcomes, in addition to numerous long-term outcomes associated with TBI (discussed above), indicate that planning is needed for addressing injured service members’ long-term psychologic, psychosocial, and medical needs.
Polytrauma
As noted earlier, OEF and OIF active-duty military personnel are experiencing higher survival rates than in previous wars. The overall survival rate among wounded troops is about 90%; increased survival rates are attributed to the widespread use of body armor and improved battlefield procedures and medical evacuation (CBO, 2007b). However, the protection offered by body armor has probably resulted in more veterans surviving injuries that in past conflicts would have led to polytrauma and death, but which now result in immediate or later amputations. As reported by the Army Office of the Surgeon General, from September 2001 to January 12, 2009, there were 1,184 amputations in personnel deployed to OIF and OEF, nearly three-quarters of which were major amputations (CRS, 2009). IEDs caused 55% of the 1,184 OIF and OEF amputations. Of the 1,184 amputations, 77% were in the Army, 19% in the Marines, 2% in the Air Force, and 2% in the Navy (CRS, 2009). OIF and OEF amputees typically receive care at Landstuhl Regional Medical Center in Germany and are then sent to Walter Reed Army Medical Center, where they may stay for several months. Amputees often experience acute and chronic pain, including phantom limb and residual limb or stump pain (Ketz, 2008). They may also face long-term psychologic problems (Ebrahimzadeh and Rajabi, 2007). Ebrahimzadeh and Hariri (2009) reported that 54% of amputees having persistent functional, social, and psychiatric problems, yet only 26% of patients were receiving psychologic treatment.
Another common problem reported by returning service members that co-occurs with other injuries is chronic pain (Clark et al., 2007; Gironda et al., 2006; Lew et al., 2007b), itself a leading cause of disability in the civilian population (Stewart et al., 2003). In a study of 100 OEF and OIF veterans, about 47% reported at least mild pain, and 28% reported moderate to severe pain; among the 67 veterans with chronic pain conditions, 82% had a documented diagnosis of musculoskeletal or connective tissue disorders (Gironda et al., 2006). Moreover, pain is known to be associated with a high prevalence of mental health disorders, including PTSD (Otis et al., 2009). A more recent study of 429 OEF and OIF veterans (Helmer et al., 2009) found that more severe chronic pain, PTSD, and depression adversely affected veterans’ ability to perform daily activities and so made readjustment for the veterans and their family members more difficult.
In a recent review, pain from polytrauma was found to pose numerous challenges during and after rehabilitation treatment (Dobscha et al., 2009). Patients who present with both pain and mental health disorders may have more functional impairment than those with single conditions. Studies of patients treated for both pain and the mental health disorder do not consistently show improvement when the mental health disorder is treated alone; this suggests that both conditions
need to be addressed (Otis et al., 2009). Assessment and intervention efforts are further complicated when the injuries include TBI. Factors associated with worse outcomes include multiplicity of injuries, head injury or cognitive disability, and lower-limb injuries.
Research and program development are needed to substantiate the potential efficacy and cost effectiveness of developing protocols for the long-term management of TBI and polytrauma. The array of potential health outcomes associated with TBI suggests that injured service members will have long-term psychosocial and medical needs from both persistent deficits and problems that develop in later life. Access to rehabilitation therapies—including psychologic, social, and vocational—is required initially with the onset of deficits and will persist over time as personal and environmental factors change, leading to loss of functional abilities. VA has put into place a comprehensive system of rehabilitation services for polytrauma, including TBI (see Chapter 5), that addresses acute and chronic needs that arise in the initial months and years after injury. However, protocols to manage the lifetime effects of TBI are not in place and have not been studied for either military or civilian populations. As in other chronic health conditions, long-term management for TBI may be effective in reducing mortality, morbidity, and associated costs.
The committee recommends that the Department of Veterans Affairs conduct research to determine the potential efficacy and cost effectiveness of developing protocols for the long-term management of service members who have polytrauma and traumatic brain injury. The approaches considered should include
-
Prospective clinical surveillance to allow early detection and intervention for health complications.
-
Protocols for preventive interventions that target high-incidence or high-risk complications.
-
Protocols for training in self-management aimed at improving health and well-being.
-
Access to medical care to treat complications.
-
Access to rehabilitation services to optimize functional abilities.
Mental Health Disorders
High rates of service-related mental health disorders among military personnel and veterans who have deployed to OEF and OIF have been reported (Erbes et al., 2007; Hoge et al., 2004, 2006; Kolkow et al., 2007; Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command, 2006a, 2006b, 2008; Seal et al., 2007; Sundin et al., 2010; Tanielian and Jaycox, 2008; US Army Surgeon General, 2003, 2005), and the prevalence of those disorders will grow as the conflicts continue. Frequently diagnosed psychiatric disorders include mood disorders, such as depression, and anxiety disorders, such as PTSD, panic disorder, and generalized anxiety disorder. An increased risk of substance-use disorders (alcohol and drug abuse and dependence) and suicides often co-occurs with those mental disorders. This section describes the disorders, their reported prevalence in the OEF and
OIF military and veteran populations, and the readjustment challenges faced by people who have these disorders.
Major Depression
Major depression is the most common mood disorder reported in civilian populations; it is characterized by persistent feelings of sadness accompanied by several symptoms related to changes in appetite or sleeping patterns, loss of interest in activities, fatigue, inability to concentrate, and hopelessness or suicidal thoughts. A 2008 RAND report (Tanielian and Jaycox, 2008) reviewed 12 studies that assessed the prevalence of depression in active-duty service members who served in OEF and OIF. None of the studies used a diagnostic instrument to diagnose depression, and findings were based on self-report symptom measures only. However, on the basis of the prevalence estimates, major depression in active-duty service members ranged from 5% (Hoge et al., 2006; Kolkow et al., 2007; US Army Surgeon General, 2005) to 37% (Lapierre et al., 2007).
Depression is associated with a decrease in quality of life. The World Health Organization projects that it will be the second-most common contributor to disability worldwide in 2020; it is already the second-most common contributor to disability in people 15–44 years old in both sexes combined (WHO, 2010). In the general population, about 80% of persons who had depression reported some difficulty in daily functioning because of their symptoms (Pratt and Brody, 2008). In more severe cases, persons who had a lifetime history of major depression were 10 times as likely to report having thought about killing themselves (OR 9.6, 95% CI 7.5-12.3), 11 times as likely to have made a nonfatal suicide attempt (OR 11.0, 95% CI 7.1-20.3) (Kessler et al., 1999), and almost 4 times as likely to meet alcohol-dependence criteria (OR 3.7, 95% CI 3.1-4.4) (Grant et al., 2004). In military populations, those who had depression were less likely to be employed than those who did not (Savoca and Rosenheck, 2000). Vietnam veterans who had depression also had 45% lower hourly wages than veterans who did not (Savoca and Rosenheck, 2000). Similarly, Vietnam veterans who had depression tended to report more marital and family conflict, including domestic violence, than those who did not. In a survey of 11,870 white men randomly sampled from Army bases between 1989 and 1992, presence of depressive symptoms was positively associated with the presence and severity of domestic violence (Pan et al., 1994). The investigators found that for each 20% increase in depressive symptoms, there was a 74% increase in the likelihood of husband-to-wife aggression.
Posttraumatic Stress Disorder
PTSD is a commonly diagnosed mental health disorder in OEF and OIF service members. It can develop after the direct, personal experience or witnessing of an event that poses a perceived threat of death or serious injury. The risk of developing PTSD is also higher among those who have suffered pre-service trauma, such as childhood sexual abuse or physical abuse (Tolin and Foa, 2006). Symptoms that characterize PTSD arise in the aftermath of a traumatic exposure and include re-experiencing of the traumatic event through flashbacks and nightmares; avoidance of people, places, and situations associated with the trauma; and hyperarousal (difficulty in sleeping and in concentrating and exaggerated startle) (IOM, 2006). The Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), which is considered the gold standard for psychiatric diagnoses in the United States, recognizes that the onset of PTSD may be acute, beginning within 6 months of exposure to the traumatic event, or delayed, beginning 6
months or more after the traumatic event. Symptoms typically begin shortly after exposure— even on the first day (North et al., 1999). PTSD can be diagnosed only if symptoms persist for at least a month; similar symptoms that last less than a month are diagnosable as acute stress disorder. The latency period between exposure and development of symptoms that meet the diagnostic criteria is variable; it may be years before the symptoms become fully manifest (Bremner et al., 1996; Bryant and Harvey, 2002; Carty et al., 2006; Gray et al., 2004; Green et al., 1990; Op Den Velde et al., 1996; Port et al., 2001; Ruzich et al., 2005). Moreover, PTSD is considered to be chronic by DSM-IV-TR (DSM-IV Text Revision) criteria if symptoms persist for 3 months or longer. PTSD also can be chronic with no remission, or it can be recurrent with periods of remission and recurrence (Friedman, 2003).
In US troops deployed to Afghanistan and Iraq, symptoms of PTSD are most commonly reported after deployment. Service members who experience combat exposure and those who are wounded are at higher risk for PTSD. The Department of Defense (DOD) conducted a mental health survey of Army soldiers and marines deployed to Iraq in 2003, 2004, and 2006. In 2003, 16% of the soldiers and marines met the screening criteria (not necessarily DSM diagnosis) for PTSD while deployed; in 2004, 14% met the screening criteria; and in 2006, 17% of soldiers and 14% of marines met the screening criteria (Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command, 2006b). Moreover, the risk of PTSD symptoms 3–4 months after deployment was 6.2% in Army troops returning from Afghanistan and 12.9% in Army soldiers and 12.2% in marines returning from Iraq (Hoge et al., 2004). Since September 2001, the MHS has recorded positive screening results for PTSD in 39,365 service members. According to CRS (2009), the MHS has spent $63.8 million on care and $13.1 million on prescription drugs for treating those with PTSD symptoms.
In a RAND study of OEF and OIF veterans, 18.5% reported depression or PTSD (Tanielian and Jaycox, 2008), slightly higher than the prevalence found in its review of 22 other studies, which showed that 5–15% of veterans experienced PTSD symptoms when deployed to war zones. The study also suggested that prevalence of PTSD symptoms increases with time after deployment (the readjustment period) (Tanielian and Jaycox, 2008).
Studies of US service members deployed to war zones have used self-report screening instruments rather than structured diagnostic interviews conducted by mental health professionals to diagnose mental health conditions. According to the RAND report (Tanielian and Jaycox, 2008), due to methodologic differences in outcome measurement, the extant studies may have underestimated the prevalence of PTSD and depression in their postdeployment samples. Most studies also used convenience samples, which may not be representative of the entire force deployed to war zones. In addition, inasmuch as OEF and OIF are ongoing, the risks may yet change. For example, service members deployed to Iraq earlier in the conflict were at higher risk for PTSD than those deployed to Afghanistan, but recent changes in military focus in the two theaters might reverse that pattern.
PTSD can interfere with functioning and quality of life. There is considerable evidence that symptoms of combat-related trauma and posttraumatic stress are inversely associated with service members’ relationship quality and stability. For example, 30 years after their military service, 10% of the Vietnam veterans in a community sample reported they still had severe PTSD symptoms, and those 10% reported less satisfaction with their marriages and sex lives and more difficulties with parenting. Veterans with more severe PTSD symptoms were more likely to have been divorced, and veterans who had reported severe symptoms 15 years earlier had
become even less satisfied with their marriages and lives (Koenen et al., 2008). Cook et al. (2004) found similar relationship disruptions 50 years after World War II in a sample of US prisoners of war. In marriage, emotional numbing has been associated with loss of intimacy (Cook et al., 2004; Galovski and Lyons, 2004; Solomon et al., 2008). The PSTD arousal symptom cluster3 seems to promote veterans’ expressions of anger (Beckham et al., 2000) and violence toward their partners (Marshall et al., 2005; Solomon et al., 2008).
There is evidence that PTSD disrupts functioning in relationships with children. Fathers who have PTSD have been characterized as withdrawn, irritable, and controlling (Dekel and Goldblatt, 2008; Galovski and Lyons, 2004). In a study of 66 male Vietnam veterans who had combat-related PTSD, emotional numbing was more strongly related than other symptoms to aspects of the parent–child relationship, including positive sharing, contact, and overall quality (Ruscio et al., 2002).
A recent study focused on 199 military veterans who served in Iraq or Afghanistan after 2001 and who were referred to military behavioral health clinicians from primary care (Sayers et al., 2009). Veterans who had depression or PTSD were five times as likely to report problems with family readjustment as those who did not, including feeling like guests in their own homes and reporting that their children acted afraid or without warmth toward them. Almost one-third of the veterans reported that their partners were afraid of them.
In a study of PTSD in civilians, Breslau (2001) found that when symptoms were most severe, about 25% of both men and women in a population of young adults felt that they were unable to work during the entire 30-day period during which they experienced the symptoms. When inability to work was added to reports of reduced activity, almost 39% of the 20 men and 44% of the 44 women reported that they were unable to do their jobs or had to reduce their activities. When young people who had a diagnosis of PTSD, other psychiatric diagnoses, or no psychiatric diagnosis were compared, those who had PTSD were twice as likely to limit their activities as those who were diagnosed with other psychiatric disorders and four times as likely as those who had no diagnosis.
Adding to the mental health readjustment challenges of OEF and OIF service members and veterans is the shortage of mental health–care professionals being reported by the military and mass media. The committee’s own preliminary review found that the mental health services available to OEF and OIF service members and veterans are poorly distributed. For example, a shortage of mental health–care professionals, at least in some geographic areas (especially less-populated areas), has been reported. Feedback from health-care providers in the field showed concerns that at some army installations and VA hospitals, the mental health–care personnel are overwhelmed by the number of soldiers and veterans who seek treatment. Anecdotal evidence suggests that in some locations service members and veterans have long wait times or must travel long distances to see mental health providers.
In connection with the heavier case loads, there have been reports that facilities in remote areas are finding it difficult to recruit and retain highly qualified providers. The committee heard from providers—especially at the town hall meeting held in Killeen, Texas, near Fort Hood—who stated that it is difficult to retain mental health clinicians because they can be better
compensated in private practice (see Appendix B). They also noted that it is difficult to recruit qualified clinicians to remote areas because the clinicians have other opportunities to work and live in more attractive communities.
Suicide
Suicidal behavior is one of the most serious consequences of mental disorders. It is the 11th-most common cause of death in the United States (NIMH, 2009). In the Western world, women attempt suicide three times as frequently as men, but men are four times as likely to die from suicide as women because of the methods used (for example, men use firearms) (CDC, 2009).
A number of studies have assessed the association between combat exposure and suicide; the results have been inconsistent. In a study of Vietnam veterans, an increased risk of attempting suicide was observed during the early followup period (CDC, 1987), but the increase in risk did not persist in a 30-year followup of the cohort (Boehmer et al., 2004). In another study, veterans who had PTSD continued to have an increased risk of committing suicide 30 years after service (Boscarino, 2006); this suggests that those who have PTSD may be particularly vulnerable. In a prospective followup study of over 320,000 men, veterans were twice as likely to die of suicide as nonveterans in the general population (Kaplan et al., 2007).
Because of the high rates of mental disorders in service members returning from Afghanistan and Iraq, there are concerns about elevated rates of suicide. According to DOD, the rate of suicide in the military in 2003 was comparable with the rate across all ages of the general US population (about 10 per 100,000) (Allen et al., 2005). Since then, the Army has reported a record of over 140 suicides in active-duty soldiers in 2008; in November 2009, the Army released data suggesting that suicides in 2009 could exceed that number. In January–October 2009, there were 133 reported suicides (90 confirmed and 43 pending); in the same period in 2008, there were 115 confirmed suicides in active-duty soldiers (Department of the Army, 2009). Those figures do not take into account the other branches of the US military, and it is not possible to determine whether the rate of suicide in all military personnel has increased. However, some data suggest that there are especially vulnerable groups, notably veterans who served in the active component and veterans who have mental disorders (Kang and Bullman, 2008).
More people fail at suicide attempts than are successful. Those who fail at suicide attempts often injure themselves seriously and require medical care. The total lifetime cost of self-inflicted injuries among the general US population in 2000 was about $33 billion, of which $1 billion was for medical care and $32 billion for lost productivity (Corso et al., 2007). In addition, those who attempt suicide often suffer from depression and other mental disorders and are at increased risk for attempting it again.
Little research has been conducted to examine the consequences of suicide on family members. That lack of data is not limited to the consequences of suicide on the family and social networks, but also extends to the military unit. Those left behind have been found to be at risk for complicated grief reactions, mental disorders, and even suicide. A study by Farberow et al. (1992) found that spouses bereaved because of deaths from natural causes appeared less distressed 6 months after their spouse’s death than those whose spouses died of suicide. The study reported higher levels of grief and depression after the first year, and found that spouses
bereaved because of deaths from natural causes reported receiving more emotional support than those whose spouses committed suicide. Many feel guilt and blame themselves for their perceived failure to prevent the suicide (Reynolds and Cimbolic, 1988). In addition, survivors are judged more severely by society than those who suffer other types of loss (Range, 1998; Stillion, 1996).
The committee heard repeatedly that there is a critical shortage of health-care professionals—especially those specializing in mental health—to meet the demands of people returning from theater in Iraq and Afghanistan and their family members. The psychologists, psychiatrists, social workers, and other mental health professionals who do serve the military and veteran communities have large caseloads (especially in some locations), and this results in underserved patients and high rates of burnout and turnover. The committee is aware that DOD is taking steps to meet the mental health care needs of its service members, but more remains to be done.
The committee recommends that the Department of Defense and the Department of Veterans Affairs quantify the number and distribution of mental health professionals needed to provide treatment to the full population of returning service members, veterans, and their families who suffer from mental health disorders, such as PTSD, major depression, and substance abuse, so that they can readjust to life outside of theater. The committee also recommends that the Department of Defense and the Department of Veterans Affairs continue to implement programs for the recruitment and retention of mental health professionals, particularly to serve those in hard-to-reach areas.
Substance-Use Disorders
DSM-IV defines substance-use disorders as dependence4 on or abuse5 of drugs or alcohol. The disorders are often comorbid with depression and PTSD. A recent IOM report determined that there is evidence of an association between deployment to a war zone and alcohol and drug abuse and dependence (IOM, 2008a); however, there are no data available on drug abuse in OEF and OIF active duty and veterans. That lack of data is not surprising, inasmuch as active-duty soldiers who abuse drugs are at risk for dishonorable discharge. Thus, many studies do not collect data on substance abuse. Initial surveys, however, have suggested that problems with substance abuse and dependence, particularly alcohol abuse and dependence, in OEF and OIF veterans are being reported when they return (Hoge et al., 2004; Jacobson et al., 2008; Lande et al., 2008; Stahre et al., 2009). A recent study found that 43% of active-duty service members reported binge drinking6 in the preceding month (Stahre et al., 2009). Another study of three Army units and one Marine Corps unit found that deployment to Iraq or Afghanistan was associated with higher prevalence of alcohol misuse compared to predeployment prevalence (Hoge et al., 2004). In a study of reserve and National Guard personnel, those who were deployed to Iraq or Afghanistan and reported combat exposure were
at increased risk for new-onset heavy weekly drinking, binge drinking,7 and other alcohol-related outcomes (Jacobson et al., 2008).
Alcohol-related problems are reported frequently in veterans. A recent study by Seal et al. (2009) found a prevalence of alcohol-use disorder of 7.1%, which appears to be similar to that in the general population. In the United States, about 1 in 12 adults abuses or is dependent on alcohol; alcohol problems are most prevalent among in adults 18–29 years old (NIAAA, 2007). However, in a study of 1,508 OEF and OIF veterans (Calhoun et al., 2008), 40% screened positive for alcohol abuse, alcohol dependence, or harmful alcohol use; binge drinking was common (23%). Only 31% of those who were abusing alcohol reported that a VA provider had advised them to drink less (Calhoun et al., 2008).
Using data from the Millennium Cohort Study, researchers found that reserve and National Guard personnel who experienced combat exposure were significantly more likely to engage in new-onset heavy weekly drinking or experience alcohol-related problems than nondeployed personnel (Jacobson et al., 2008). The youngest members of the cohort were at highest risk for all alcohol-related outcomes. Baseline prevalences of heavy weekly drinking, binge drinking, and alcohol-related problems8 in reserve or National Guard personnel who deployed and were exposed to combat were 9.0%, 53.6%, and 15.2%, respectively; followup prevalence was 12.5%, 53.0%, and 11.9%.
The medical and nonmedical complications of alcoholism and alcohol abuse are well known. Excessive alcohol use has been associated with liver disorders, cardiovascular problems, neurologic conditions, and some kinds of cancer. Each year, 85,000 Americans die of alcohol-related causes, and nearly half of all traffic deaths are linked to alcohol (Mayo Clinic, 2008). In addition, excessive alcohol use is associated with a higher incidence of suicide or homicide, domestic abuse, and poor performance at work.
On the basis of responses from Millennium Cohort Study participants who submitted baseline data before deployment to Iraq or Afghanistan and upon return (n = 48,304), military deployment was associated with smoking initiation and more strongly with smoking recidivism, especially among those who had prolonged deployments, multiple deployments, or combat exposure (Smith et al., 2008). Those who were deployed and reported combat exposure were at 1.6 times greater odds of initiating smoking among baseline never-smokers and at about 25% greater odds of resuming smoking among baseline past smokers compared with those who did not report combat exposure.
No data on drug abuse in OIF and OEF veterans were available. The experience of past conflicts indicates that drug abuse and dependence will be problems where opiates are readily available, but there is no evidence at this time to indicate a serious problem with illicit drugs in OEF and OIF. That is not surprising, given that active-duty soldiers who abuse drugs are at risk
for dishonorable discharge. In light of the latter, many studies do not collect data on substance abuse (Charles Engel, personal communication, August 11, 2009).
The committee recommends that the Department of Defense actively promote an environment to reduce stigma and encourage treatment for mental health and substance-use disorders in an effort to improve military readiness and ability to serve. The committee also recommends that the Department of Defense undertake a systematic review of its policies regarding mental health and substance-abuse treatment with regard to issues of confidentiality and the relation between treatment-seeking and military advancement.
DEPLOYMENT
In addition to the stress of caring for or coping with a family member who has been injured (physically or psychologically) in combat, military families face unique stressors that can complicate readjustment. Those challenges are not shared by civilian families, such as repeated family relocations (both domestic and international) and deployment—periodic and extended separation of service members from their families—and the fear of the service member’s injury or death (Burrell et al., 2006; Reinkober Drummet et al., 2003).
About one-third of military families are relocated each year (Orthner and Rose, 2002), with the result that the average military family moves every 2–3 years (DOD, 1998; GAO, 2001). Historically, the military has moved its personnel to different installations and types of units to ensure that service members acquire the repertoire of specialized skills and training necessary for both their career advancement and the fulfillment of the military’s mission. The moves require families to leave the communities in which they are embedded (such as neighborhoods, schools, friends, places of worship, and work) and to rebuild their support networks in a new part of the country. Families’ adjustment includes cultural adaptation in the case of international relocations, the rates of which are four times higher for military families than for the civilian population (Reinkober Drummet et al., 2003).
Unlike civilian life, in which there is often some control or choice over relocation decisions, the military affords none. Frequent obligatory moves are associated with frustration and decreased satisfaction with military life (GAO, 2001); however, the norms and values of the military dictate that families adapt. In addition to the emotional upheaval involved, frequent relocations tend to disrupt the spouse’s ability to achieve educational or career goals (Eby et al., 1997; Harrell et al., 2004). That disruption is reinforced by the likelihood that the spouse, who is most commonly female, has to bear primary responsibility for child care and household management in the family (Defense Department Advisory Committee on Women in the Services, 2008). Adult children of military parents report geographic mobility as the most trying aspect of growing up in the service (Ender, 2000; Lincoln et al., 2008).
The remainder of this section focuses on the adverse effects of deployment on military families, military spouses, and children. It also discusses the effects of deployment on a host of social issues, including education and employment; income, earnings, and wages; and such adverse outcomes as debt, homelessness, incarceration, crime, and risky driving. In many cases, data on those issues have not yet been studied or clarified for OEF and OIF veterans, so the committee often relied on information from studies of Vietnam veterans or veterans of other
wars if it believed such information to be instructive in addressing the needs of current active-duty and veteran populations. In many instances, the current economic environment will influence the outcome of many of the issues discussed below.
Deployment and Military Families
Many men and women who return from the war zone adjust to their lives out of theater successfully; others have difficulty in adjusting or transitioning to family life, to their jobs, and to living in their communities. Families are stressed by routine physical separations from service members and profoundly so by soldiers’ deployments to active combat zones. Deployment lengths, once relatively predictable, are more uncertain because of the acceleration of conflicts in Afghanistan and Iraq and a heightened likelihood of extensions (Lincoln et al., 2008). Families must cope with the ever-present risk of injury or death. Longer deployments are particularly taxing for families’ well-being; data suggest that families experience greater stress and anticipate more difficulties when deployments extend beyond 6 months (Booth et al., 2007; Orthner, 2002).
Before deployment, families must prepare legally, logistically, and emotionally for separation and the possible death of their service member (McCarroll et al., 2005). McCreary et al. (2003) surveyed 180 members of the Canadian military 48 hours before departure for a peacekeeping mission in Bosnia and found that family self-reports of concerns explained more than half the variability in measures of depression, hyper-alertness, anxiety, and somatic complaints. Findings from a study by Kelley et al. (2001) also suggest that Navy mothers and fathers anticipating deployment suffer from separation anxiety; anxiety is greatest in servicewomen who have children or are single mothers.
During deployment, family members report experiencing psychologic stress and logistical challenges in caring for children and households (SteelFisher et al., 2008). Some spouses (30–50%) relocate during deployment; this increases proximity to extended family members but means leaving local military services and causing children to change schools and living arrangements (Flake et al., 2009). There may be economic challenges, such as loss of employment or difficulty in paying for child care or other household services usually provided by the deployed family member. Reserve-component members may lose income during deployment, although on the average they experience small income increases (Angrist and Johnson, 2000). Reserve-component families also may be required to switch medical providers during deployment if their primary health-insurance coverage moves to the military system.
Steelfisher and colleagues (2008) conducted telephone interviews in January and February 2004 with 744 Army spouses affiliated with units that were deployed early in the current conflict. Some of the spouses had experienced an unexpected extension of their partners’ deployment. The most common adverse effects of deployment on well-being were self-reported loneliness (78.2%), anxiety (51.6%), and depression (42.6%). Reported problems with overall health and perceived effects on jobs were more prevalent—21% and 18%, respectively—than financial problems or problems with relationships—12% and 4–10%, respectively; 9.9% of respondents reported problems with their marriages. Among deployment-induced problems in daily life, difficulty in communication (sent and received) with the deployed member was the most common (41.0%). Additional problems reported were problems with household and car maintenance (29.0%), fears about personal safety (23.6%), and problems finding child care (16.2%). A notable minority of the sample reported adverse perceptions of the military, the most
commonly cited problem being lack of accurate information surrounding the timing of deployment (48.4%). Those experiencing a deployment extension were more likely to report problems with work and were more likely to have scaled back or left work; they were also more likely to report problems in their marriages than spouses who did not experience a deployment extension.
During deployment, children and spouses of deployed service members have been found to experience increased self-reported levels of symptoms of depression. The families also report significantly more intervening stressors in the past year than families of nondeployed personnel (Jensen et al., 1996). Younger children and boys of deployed parents appear to have heightened vulnerability to maladjustment (Blount et al., 1992; Jensen et al., 1996). In a study of how adolescents cope with the uncertainty and “ambiguous loss” inherent in parental deployment, Huebner et al. (2007) found that adolescents tend to have increased awareness of the risks associated with parental deployment and to experience behavioral difficulties and symptoms of anxiety and depression.
Most studies conducted after return from deployment focus on the consequences of symptoms of posttraumatic stress in service members and their families; few studies focus on the normative course of reintegration. However, apart from the eventual transition out of the military, perhaps the most challenging transition for military families is the return home from deployment. Most military families adapt to the deployment by taking on additional roles and responsibilities; however, such adaptation can create tension during the immediate postdeployment stage. The service member and family may struggle to adjust to a vastly different lifestyle, reconnect with a different social support structure (for example, the spouse and children as opposed to the military unit), and perhaps return to a very different job if they are reserve or National Guard members. One longitudinal study of reintegration during OIF (Faber et al., 2008) reported that couples in a sample of reservists were preoccupied with relational communication and expectations, especially regarding independence, roles, and responsibilities. The transition from soldier to civilian was more difficult for service members whose return to the civilian workforce did not go smoothly.
Some of those challenges may include readjusting to partners who have assumed new roles during the separation period, coping with the loss of independence gained during the deployment, negotiating needs for personal space and family routines, re-establishing family roles, readjusting to children who have matured and may resent additional oversight, re-establishing bonds with spouses and children, and managing the long-term health problems that are common after deployment (American Psychological Association Presidential Task Force on Military Deployment Services for Youth, Families, and Servicemembers, 2007; Slone et al., 2009). Bowling and Sherman (2008) suggested that both service members and their family members cope with the stresses of deployment by suppressing their emotional responses and that this can impede processes of reconnecting with one another after return. During the current conflicts, the prospect of possible future deployments, and the resultant separation, makes the re-establishment of intimate relationships even more challenging.
As mentioned elsewhere in this report, the demands of the current conflicts have made compliance with DOD’s rotational policies (for example, maximum length of deployments and minimum length of dwell time between deployments) difficult. All the hardships noted in this chapter may be exacerbated by the number and frequency of repeat tours, which necessitate repeated transitions from life in theater to life after combat. A frequent need to adapt and readapt
creates more challenges for service members and their families. An extra stage in the process of returning from deployment, known as third-location decompression, has been used by other militaries to ease the stress of such transitions (Hughes et al., 2008). The goal of third-location decompression is to provide service members rotating off deployment with a period of decompression in a third location: a time in which they can be with their comrades and peers in a restful situation and prepare themselves for going back to their families and communities (National Defence and Canadian Forces Ombudsman, 2004). Little research has been conducted to evaluate whether service members who undergo third-location decompression have better outcomes than those who do not, but findings in other militaries have been favorable (Hughes et al., 2008; National Defence and Canadian Forces Ombudsman, 2004). For example, members of the Canadian Forces have returned home from Afghanistan via Guam or Cyprus by spending 5 days of structured time with their units. In addition, they are required to work about 3 half-days at their home base, and this provides additional time to adjust to life back in Canada and ease the transition to family life (Rossignol, 2007).
DOD does not have a formal policy in place to route returning US troops through third-location decompression, but the Marine Corps has instituted a rest and decompression period during which unit commanders, noncommissioned officers, and chaplains provide the Warrior Transition Brief (Hughes et al., 2008). The implications and potential consequences of shorter dwell time, more frequent deployment, and inability to meet DOD’s rotational standards are of obvious importance for understanding the readjustment needs of service members and their families; policies that help to ease reintegration are of paramount importance.
The committee recommends that the Department of Defense formally assess whether a third-location decompression program would be beneficial for US combat troops. Third-location decompression has the potential to give troops time to begin to readjust before returning to their homes and family responsibilities.
Deployment and Military Spouses
The challenges of deployment are different for service members and their spouses and the readjustment needs of military spouses are not secondary to those of the returning service member. In fact, some studies have suggested that spouses face similar levels of distress and appear to develop mental anxiety or trauma as a result of experiences prior to, during, and after the service member’s deployment (Mansfield et al., 2010). Eaton et al. (2008) studied over 700 military spouses seeking primary care at military facilities. According to both broad and strict screening criteria, spouses and service members reported similar levels of major depression and generalized anxiety disorders. Spouses were more likely than service members, however, to seek care and less likely to be impeded in doing so by worries about stigma. About 20% of spouses received care only from primary-care physicians rather than from mental health specialists.
Several studies now suggest that service members’ deployments are associated with increased stress during pregnancy and increased risk of postpartum depression. A survey of pregnant military and civilian patients at Camp Lejeune, North Carolina, indicated that partner deployment, active-duty status, and having more than one child at home were associated with higher levels of stress (Haas et al., 2005). A review of the charts of 450 women who completed the Edinburgh Postnatal Depression Scale revealed that new mothers whose partners were
deployed during the pregnancy were 2.75 times more likely to screen positive for postpartum depression than new mothers whose military partners were not deployed (Robrecht et al., 2008).
Flake et al. (2009) recently surveyed 101 Army parents who had children 5–12 years old and a deployed spouse. Some 42% reported clinically significant parenting stress, and 32% reported significant psychologic symptoms in their children. Parents who reported high levels of stress were 7 times as likely as those who did not to report symptoms in their children, but were only one-third as likely to do so when they perceived that there was good social support from the military and those around them.
Vormbrock (1993) reviewed the literature on spouses’ reactions to wartime and other marital separations in light of attachment theory, which would predict that adults will show the same protest–despair–detachment pattern as children in response to separation. Available data suggest that despair is followed by anger and reorganization of attachment perceptions. Vormbrock also predicted emotional detachment, anger, and anxious contact-seeking at reunion and found detachment and anger more on the part of the home-based spouse and contact-seeking by both partners. She predicted and found that separation length was positively related to distress, detachment, and damage to the attachment relationship. Separation distress was heightened by stressful events during the separation and lessened when adults had access to alternative attachment figures, but revival of childhood attachments, such as those to parents, could undermine the marital relationship. During deployment, service members may develop strong support relationships with fellow service members, whereas family members may rely on members of the community, other families experiencing deployment, and children (Bowling and Sherman, 2008). After return, service members and family members may both find it challenging to reorient themselves to their primary attachment partners and find comfortable ways to process their deployment experiences with one another and members of their support networks.
As expected, exposure to combat appears to threaten the quality of marriage. A report by IOM (2008a) found strong evidence that people who were deployed were more likely to have marital problems when they returned, including intimate partner violence, than people who were not deployed; however, most of those findings were based on studies of Vietnam veterans. Among Vietnam veterans, those who had PTSD were more likely to commit acts of interpersonal or intimate-partner violence than those who did not have PTSD (IOM, 2008a). One longitudinal study of Persian Gulf veterans found that veterans who had PTSD had less social support than those who did not.
Several studies have examined the effect of deployments on marital dissolution. In the National Survey of Families and Households, 3,800 veterans of World War II and the conflicts in Korea and Vietnam reported significantly higher rates of marital dissolution if they had served in combat than if they had not (Ruger et al., 2002). A large representative survey (n = 59,631) of military members showed that deployment to Operation Desert Storm was associated with a statistically significant increase, by 4.2 percentage points, in later divorce rates of female service members (Angrist and Johnson, 2000); no association was observed in male service members. An IOM study (2008a) on the health effects of the Gulf War concluded, however, that although there was a suggestive relationship between combat deployment and marital conflict, there was insufficient evidence to indicate an association with marital dissolution.
During deployment, military members worry about their relationships. Since 2003, family separation has consistently been among the top concerns of service members stationed in
Iraq and Afghanistan, and is more strongly related than any other concern to mental health problems (Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command, 2008). Length of deployment (but not number of deployments) appears to be positively correlated with the percentage of deployed service members who indicate that they plan to obtain a divorce or to separate after their return; for example, the MHAT-V estimates that around 6% of noncommissioned Army officers indicate plans to divorce at 1 month of deployment, compared to over 20% at 15 months of deployment (Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command, 2008). Plans to divorce or separate also appear to be inversely correlated with pay-grade: the MHAT-V reported that in 2007, 17.0% of junior enlisted soldiers in theater for 9 months were considering getting a divorce, compared to 12.3% of noncommissioned officers and 3.6% of officers. So far, however, there is little evidence that those intentions are realized, despite findings from prior wars that combat veterans experienced significantly increased divorce rates (Ruger et al., 2002).
Contrary to the view that longer deployments lead to a higher risk of marital dissolution, Karney and Crown (2007) found in a study of personnel records of over 560,000 service members who married in 2002–2005 that the longer a service member was deployed, the lower the risk of divorce or separation, especially if they were male, were younger, or had children. Those results, from the most definitive study of the current war to date, were consistent with the “hasty-marriage” hypothesis, which suggests that in response to impending deployment or to receive military benefits tied to marriage, some people enter hasty marriages that are more likely to end prematurely. This hypothesis differs from an alternate explanation which suggests that the stress of deployment undermines otherwise healthy marriages. The findings of Karney and Crown (2007), however, are preliminary; they focus only on relatively recent marriages followed for a relatively short period. In a recent study of graduates of the Air Force Academy, McCone and O’Donnell (2006) found some evidence to support the hasty-marriage hypothesis among graduates who timed their marriages to one another to occur very shortly after graduation so that they would be posted together as they began their Air Force careers.
Finally, there is evidence from two small studies of the current conflict that symptoms of combat-related trauma are related to marital distress for both partners. Wives were more distressed when they could not see an obvious cause for their husbands’ symptoms. That could occur when wives perceived symptoms that their husbands failed to acknowledge or when husbands reported more severe symptoms than their wives expected given what was known about their combat experience (Goff et al., 2007; Renshaw et al., 2008).
Although deployments are likely to present challenges for unmarried partners and for the parents and other family members of service members, no data on their experiences were found. To the extent that such people are called on to support service members during deployment cycles and during recovery from wounds and injuries, that omission requires attention.
Deployment and Children
Many parents, practitioners, and policy makers are concerned about the implications of deployment for children, but the research evidence remains sparse, and the research has used longitudinal or quasiexperimental designs relatively rarely. Most studies of prior conflicts have suggested that deployment is associated with a variety of internalizing and externalizing
symptoms in children that in most cases do not rise to the level of clinical significance (Cozza et al., 2005; Lincoln et al., 2008). It has been shown that children’s scores on academic achievement tests dropped slightly as a function of parental deployment (Lyle, 2006).
Thus far, the findings from the current war are consistent with those of earlier research. In a study of 169 preschoolers in child-development centers at a Marine Corps installation, teachers reported increased internalizing and externalizing behaviors in children who have deployed parents (Chartrand et al., 2008). One-third of the military adolescents who attended a summer camp reported changes in their mental health that are consistent with depression or anxiety (Huebner and Mancini, 2005). Another study of adolescents found that those who had deployed parents reported more reactions to stress and resource losses than those who had nondeployed or civilian parents (Barnes et al., 2007). More recently, a study by Chandra et al. (2010) found that children in military families reported higher levels of emotional difficulties than those observed in the general population. The authors also found that length of deployment was associated with a increased prevalence of adjustment difficulties (such as academic problems and anxiety) in children both during deployment and during reintegration. According to DOD health records, military children’s use of mental health–care services rose substantially from 2003 to 2008: inpatient days rose by 50% or more, and mental health appointments rose by more than 85% per capita.
Chartrand et al. (2008) found that spouses of deployed service members who had children 3 years old or older had significantly higher depression scores than spouses of nondeployed personnel; their children exhibited increased behavioral symptoms compared with peers who did not have a deployed parent. Another recent analysis of the psychosocial effects of deployment on military children found that families experiencing deployment identified one-third of children at “high risk” for psychosocial morbidity and that parenting stress was the most significant predictor of children’s psychosocial functioning (Flake et al., 2009).
Although there is considerable agreement that some children are especially vulnerable to the challenges of deployment, findings have been mixed. Several studies suggest that boys and younger children may be more vulnerable than girls and older children, but older girls are at greater risk for sexual abuse (Cozza et al., 2005; McCarroll et al., 2008). In the Chartrand et al. (2008) study of preschool children, however, younger children displayed fewer symptoms.
Deployment may affect rates of child maltreatment. Although rates in general appear to be no higher than those in the civilian population, child maltreatment by the nondeployed spouse appears to rise during deployment. A recent analysis of the occurrence of child maltreatment in military and nonmilitary families in 2000–2003 and the effect of deployment escalations after the September 2001 terrorist attacks in the United States found that the rate of substantiated maltreatment of children of military families doubled, whereas the rate in nonmilitary families was unchanged (Rentz et al., 2007). In Army families that experienced both deployment and child maltreatment in 2001–2004, there were 200%, 300%, and 400% increases in rates of physical abuse, maltreatment, and neglect, respectively (Gibbs et al., 2007). Reintegration also can be a dangerous period. Some studies have shown positive associations between length of deployment and later rates of intimate-partner violence, especially if service members are suffering from combat-related trauma (McCarroll et al., 2000), and the increases in rates of child maltreatment (Rentz et al., 2007) observed as service members left for deployment (reported earlier) also occurred when they returned.
Studies during the first Gulf War demonstrated that children’s psychologic symptoms were more severe when their mothers’ own well-being was seriously compromised (Cozza et al., 2005). Similarly, parents who reported high levels of stress were much more likely to report symptoms in their children (Flake et al., 2009). The diversity of children’s experiences as a function of deployment is not fully understood. Married service members who are parents leave their spouses as “geographically single” parents during deployment, sometimes on military installations and sometimes in civilian communities. Unmarried single parents must leave their children in the care of others through prior arrangements made via “family-care plans.” Service members who have noncustodial children also face challenges in maintaining their relationships with their children.
Parents who accessed military support services reported less child psychosocial morbidity. That finding both suggests that use of services may ease parenting stress and underscores the necessity of providing military families with the support they need to cope with and adjust to deployment circumstances. Families considered more vulnerable to adjustment difficulties and in need of targeted outreach include those simultaneously undergoing other major transitions, such as relocation, pregnancy (Haas and Pazdernik, 2007), and bereavement; families of junior personnel; and families that have multiple needs and problems before deployment (Booth et al., 2007).
As of March 2008, over 3,400 children had experienced the death of a parent during the OEF and OIF conflicts (HR 265, 110th Congress). Available data, although sparse, indicate that bereaved children are at increased risk for psychiatric disorders or behavioral or emotional problems (Cozza et al., 2005). Moreover, injured parents may have reduced capacity to respond sensitively to their children. Family roles may become ambiguous and unstable in the aftermath of a serious injury and long recovery (Cozza, 2007), when children may receive reduced attention from their noninjured parents because of the needs of the injured family members (Perlesz et al., 1999). Little guidance is available to help children to understand and adapt to the death or life-altering injury of a parent (Cozza, 2007).
Deployment and Social Outcomes
Education
Many studies have evaluated whether veterans and service members achieve more education than civilians, but few have evaluated whether educational attainment is affected by deployment. Two studies examined the effects of deployment (or combat) on education and suggested that deployment has a neutral or negative effect on educational attainment. Both studies focused on Vietnam veterans. One (Lyons et al., 2006) concluded that Vietnam veterans were negatively affected by deploying and attained fewer years of schooling; it used data from the Vietnam Era Twin Study of Aging and compared 44 twin pairs in which one twin was deployed to Vietnam and the other was not (Lyons et al., 2006). The other study, using data from the National Vietnam Veteran Readjustment Study (NVVRS), concluded that combat did not affect educational attainment (Vogt et al., 2004). However, the committee did not find published research on the effect of deployment on education among the service members returning from the current wars.
Most previous research has shown that veterans benefited from the funding for education provided by the Servicemen’s Readjustment Act of 1944, commonly known as the GI Bill. The
GI Bill provided funds for veterans to continue their education beginning at the end of World War II but was discontinued in 1955. In 1965, the bill was reinstated and covered veterans who had served in the interim. In every era, veterans have attained more education if they used the military educational benefits (Angrist, 1993; Sampson and Laub, 1996; Stanley, 2003). According to one study, the GI Bill led veterans to attain 15–20% more education than their nonveteran counterparts who were born in the 1920s and early 1930s (Stanley, 2003). During the decade (1955–1965) when GI Bill funds were not available, academically ambitious veterans were much less likely to attend and graduate from college than were comparable nonveterans (MacLean, 2005). It has been shown that economic opportunity is more strongly linked to the GI Bill than to military service itself (Sampson and Laub, 1996), and veterans had higher earnings if they used the educational benefits provided by the GI Bill (Angrist, 1993; Sampson and Laub, 1996; Stanley, 2003). None of the research on the GI Bill has examined whether the effects depend on whether a veteran was deployed.
Employment
There are sparse data on the effect of service in OEF and OIF on employment outcomes; however, studies from Vietnam might be instructive. Several studies examined the effect of service in Vietnam and the effect of PTSD on employment and earnings. Using archival data from the NVVRS that included a cohort of 1,200 male and 432 female Vietnam veterans and 412 male and 304 female era9 veterans, Zatzick et al. (1997a,b) examined the effect of PTSD on employment. Most male veterans were middle-aged and married at the time of their interviews; over 50% had some college education. Veterans who had PTSD were more likely not to be working at the time of the survey than veterans who did not have PTSD. The study of 432 female Vietnam veterans (Zatzick et al., 1997b) found that those who had PTSD (8.9% of the sample) were 10 times as likely to be not working as those who did not have PTSD (OR 10.4, 95% CI 1.8-61.9), after adjustment for age, ethnicity, marital status, educational attainment, region of country, and comorbid psychiatric disorders. That was the strongest association with PSTD that the authors found among the outcomes examined.
Recent data from the Department of Labor’s Bureau of Labor Statistics showed that the unemployment rate of all veterans of the US armed forces was 4.6%, and the unemployment rate of those who have served in the US armed forces since September 2001 was 7.3%. As with nonveterans, the jobless rates for veterans vary widely with age. Veterans 18–24 years old had an unemployment rate of 14.1%—nearly double the rate of those 25–34 years old, 7.3%, and almost three times the rate for those 35–44 years old, 4.9% (Bureau of Labor Statistics, 2009).
Research has shown that from 2002 to 2004 there was an increase in the number of veterans receiving unemployment compensation (UCX)10 and that the cost of the program to DOD had increased by about 75% (Loughran and Klerman, 2008). Loughran and Klerman noted that “the sharp and sustained increase in the UCX caseload since 2002 has contributed to the concerns that veterans of the wars in Iraq and Afghanistan are having difficulty transitioning to the civilian labor market.” In contrast, the overall youth unemployment rate declined in that period. Further research suggested that the rapid increase in UCX caseloads is attributable to the intensive use of the reserves in OEF and OIF; specifically, 58% of the increase from 2002 to
2005 is attributed to the Army reserve components (Loughran and Klerman, 2008). The authors noted that the Air Force, Navy, and Marine Corps reserves contribute a very small fraction of the overall increase in UCX caseloads. Thus, the balance (about 40%) of the increase is in the active components. The increases in veterans’ claims between 2002 and 2005 were not the result of a declining civilian job market, inasmuch as the civilian labor market generally improved during that period. It is believed, however, that longer deployments are associated with higher claim rates. Loughran and Klerman showed that the longer deployments account for more than one-third of the overall increase in Army active and reserve UCX caseloads from 2002 to 2005. Their analyses also demonstrated that self-reported health worsens with increasing length of deployment, and that is also associated with higher UCX claims.
There is evidence that veterans face discriminatory hiring practices. One study found that 66 midlevel managers and supervisors who were reviewing resumes of applicants were less likely to recommend the hiring of Vietnam veterans because of the perception of a higher probability of psychologic problems, although all the applicants (veterans and nonveterans) were equally qualified for the jobs to which they applied (Bordieri and Drehmer, 1984). Another study examined the effect of recent military service and hiring practices for entry-level jobs in urban markets. In that study of employers’ attitudes toward black job applicants, military veterans with transferable skills were preferred over black nonveterans. However, veterans who had military experience in combat positions did not receive preferential treatment regardless of racial or ethnic background (Kleykamp, 2009).
Savych (2007) examined the effect of deployment on spousal labor-force participation. It was noted that deployment to OEF or OIF reduced spousal labor-force participation by 2.8%, but that finding varies with the age of the youngest child in the family. Reduction in employment by 4.9% was seen in families that had children under 6 years old. Similarly, spouses decrease labor-force participation in the several months before their partner’s deployment.
Income, Earnings, Wages, and Debt
It has been noted that members of the reserve components earn more income when activated than before being activated (Loughran et al., 2006; Martorell et al., 2008). However, most reserve-component service members, in response to surveys conducted in 2004 and 2005, reported earnings losses when activated (GAO, 2009). A recent RAND report (Martorell et al., 2008) determined that on the average reserve-component service members experienced a net gain of about $1,400 per month in 2004 and about $1,600 per month in 2005 after activation. The study, however, identified specific military occupations (for example, general sonar operator, investigations, and military training instructor) in which on the average less income was earned after activation in 2004 than was earned before. The RAND study identified an additional 48 enlisted military occupations and 14 officer occupations in which more than 20% of the reserve-component service members sampled experienced an earnings loss after activation. Those occupations accounted for 18% of activated enlisted members and 31% of activated officers.
The Martorell et al. (2008) study examined the discrepancy between the analyses of Social Security data, which indicated that reservists earn more when they are activated, and the analyses of survey data, which indicated that they earn less. Reservists appear to earn less when the analyses are based on the 2004 and 2005 Status of Forces Survey of Reserve Component Members. The study matched the administrative data collected for the preceding analysis to data collected for the Status of Forces survey. When the data are matched, reservists appear to earn
much more when they are activated on the basis of administrative data; for example, they earned 43–44% more on active duty. However, according to the survey data, they earn 7–46% less when they are on active duty. The Status of Forces surveys provided data on 55,794 respondents in 2004 and 211,000 respondents in 2005. The authors speculated that the different conclusions stem from problems with the survey data and that the administrative data, which suggest that they earn more, are more accurate (Martorell et al., 2008).
It has been noted that young military families have been targeted for predatory payday and car-title loans, which resulted in substantial debt (DOD, 2006; Oron, 2006; Tanik, 2005). Many military families are young and inexperienced in managing finances. About 48% of enlisted service members are under 25 years old (DOD, 2007) and are without financial experience or savings to cushion them in an emergency.
Car-title loans enable borrowers to secure loans with their car titles. The typical loan is a small fraction of the car’s worth, has a 300% annual interest rate, and has a 1-month loan term. Failure to pay can result in repossession of the vehicle. The high cost and the risk of losing one’s car often result in borrowers’ repeated loan renewal (DOD, 2006). Payday loans are small loans secured by borrowers’ personal checks or agreement to automatically withdraw money from their accounts. Loans average $350, are due in full on the next payday (typically in 14 days), and have 390–780% annual interest rates (DOD, 2006). Payday lending can be found in storefronts, check-cashing outlets, pawnshops, and so on, and are heavily concentrated around military bases. DOD (2006) notes that the area around the southern gate of Camp Pendleton in Oceanside, California, has 22 payday lenders—17 more than would be expected for that ZIP code. Similarly, in the ZIP code in Killeen, Texas, outside Fort Hood, there are 9e payday lenders—7.3 more than would be expected for the population in that ZIP code (DOD, 2006).
Graves and Peterson (2005) documented the number of payday lenders near military bases by surveying 20 states, 1,516 counties, and 13,253 ZIP codes; 15,000 payday lenders; and 109 military bases. They looked at states that are home to military communities—such as California, Texas, and Virginia—and analyzed data on the distribution and density of payday lenders and banks by ZIP code. Their findings indicated that there are large concentrations of payday-lending businesses in the counties and ZIP codes near military bases (Graves and Peterson, 2005).
Active-duty service members are three times more likely as civilians to have taken out payday loans. It has been reported that one in five active-duty service members had used payday loans, which cost military families over $80 million in fees every year (Tanik, 2005).
Homelessness
The National Law Center on Homelessness and Poverty estimates that about 1% of the US population experiences homelessness—living on the streets, in shelters, or with relatives or friends—in any given year. VA reports that about one-third of the homeless population served in the military at some point (VA, 2009a). Many homeless veterans served during the Vietnam era (47%), although veterans of other periods are also homeless or at risk for being homeless. Almost half the homeless veterans have some mental disorder, almost 70% have a substance-use disorder, and over half are black or Hispanic (VA, 2009a).
A recent IOM report (2008a) evaluated the results of several studies that assessed whether deployment is associated with homelessness. It concluded that the results were mixed
with respect to whether there is an association between deployment to a war zone and homelessness. Only one of the studies (Rosenheck and Fontana, 1994) showed an association between combat exposure and homelessness in Vietnam veterans. The committee needs to explore the issue of homelessness in phase 2 of its study because the data that are available are based on previous wars. In general, the presence of a mental disorder was more strongly associated with homelessness than was combat exposure itself.
Incarceration
In 1998, over 225,000 veterans were in prison or jail in the United States—more than half for violent offenses. Of the incarcerated veterans, about 20% had served in combat duty in the Vietnam War or the Gulf War (Mumola, 2000). Black et al. (2005) investigated the prevalence of incarceration and its association with deployment among veterans who had been on active duty during the Gulf War. The study used a structured telephone interview and included military personnel who lived in Iowa in 1995–1996 and had been deployed to the gulf and a comparison sample of nondeployed military personnel. The sample included 3,695 participants (76% of eligible subjects) randomly drawn from four study populations: Gulf War regular military (n = 985), Gulf War National Guard and reserves (n = 911), non–Gulf War regular military (n = 968), and non–Gulf War National Guard and reserves (n = 831). Of the 3,695, 22.9% (845) reported that they had been incarcerated at some point in their lives, 14.5% had been incarcerated at least once before their deployment, and 8.3% had been incarcerated only during or after their deployment.
In the 1986–1987 NVVRS, Kulka et al. (1990) found that the 406 Vietnam-theater veterans who had high levels of war-zone stress were more likely to have been arrested or jailed than the 783 theater veterans who had moderate–low war-zone stress (39.1% versus 27.7%) and were more than three times as likely (8.8% versus 2.8%) to have been convicted of a felony. Involvement with the criminal-justice system was based on self-reports of number of times arrested since the age of 18 years, nights spent in jail or prison (since the age of 18 years), and number of lifetime convictions for a felony offense and on whether the veteran was in jail or prison at the time of the interview. Of the 319 Vietnam-theater veterans who had current PTSD, 45.7% had been arrested or jailed more than once in their lives compared with 11.6% of the 871 theater veterans who did not; 11.5% of the veterans who had PTSD had been convicted of a felony. PTSD symptom level at the time of the interview was assessed with the Mississippi Scale for Combat-Related PTSD; a study cutoff score of 94 was used as a threshold for an assessment of current PTSD.
Given that combat exposure has been associated with higher rates of arrests and convictions in past conflicts, it is possible that combat exposure in OEF and OIF will also be associated with higher rates of incarceration among service members and veterans. Moreover, there are data to suggest that inmates who have been convicted of a violent crime are more likely to have sustained a pre-crime TBI (CDC, 2006). Because TBI is the signature injury of OEF and OIF, those who suffer from that injury may be at higher risk of being incarcerated. Research on the OEF and OIF deployed population is needed to understand what the extent of the problem may be.
Communities
A few studies have examined the effect of deployment on businesses. Doyle et al. (2004) conducted an analysis of employer costs resulting from reserve-component mobilizations. Their findings suggest that for small employers the most important costs are caused by lost productivity rather than by requirements imposed by the Uniformed Services Employment and Reemployment Rights Act. The law is intended to ensure that people who serve or have served “(1) are not disadvantaged in their civilian careers because of their service; (2) are promptly reemployed in their civilian jobs upon their return from duty; and (3) are not discriminated against in employment based on past, present, or future military service” (Employer Support of the Guard and Reserve, 1994). Doyle et al. noted that reservists returning from active duty have the right to return to their previous positions or equivalent ones and to receive accumulated seniority raises and promotions. Thus, employers must bear the costs of temporarily replacing their reservist employees; however, there do not appear to be data on those costs.
On the basis of published civilian age-group and firm-size data, Doyle et al. (2004) estimated that 50–58% of employed reservists participate in an employer-provided retirement plan and that employers’ costs for reservists’ retirement plans average $372 per month. In additional, employers of reservists ordered to active duty for a month or less must continue health-insurance contributions for them. Using published civilian age-group and firm-size data, Doyle and colleagues estimated that about 65% of reservists participate in employer-provided health-insurance plans and that the monthly employer cost averages $215 for single people and $550 for families.
Small businesses might be disproportionately affected by the loss of reservists ordered to active duty, because the loss of an employee at a small firm constitutes a greater share of output than at a large firm. Doyle and colleagues interviewed a small number of recipients of Small Business Administration Military Reservist Economic Injury Disaster Loans, which are given to companies that are unable to meet their operating expenses after an essential employee has been called to active duty. The findings indicate that the most common effect of activation is lost business and that losses are experienced even after the reservists return from active duty. Furthermore, replacing a reservist, even if it is feasible, does not necessarily offset lost business; in some cases, the long-term effect of activation may result in permanent harm to the business (Doyle et al., 2004).
The Congressional Budget Office (CBO, 2007a) interviewed 19 employers of 28 reservists and found that small businesses that lose essential employees, businesses that employ highly skilled workers, and self-employed reservists were the most severely affected as a result of activation and federal job protections. Hope et al. (2009), in their review of the literature on the effect of reserve activation on small businesses, noted that small businesses are disproportionately affected and that the length of activation has a small but significant effect on the businesses’ revenue.
The sections above have focused on many issues related to families, spouses, children, women, and racial and ethnic minorities identified in studies of previous conflicts rather than studies of OEF and OIF active-duty personnel, veterans, and family members. The committee believes that many of the studies provide information that is relevant to the current conflict, but active-duty service members, reservists, and veterans face hardships because of service in Iraq and Afghanistan that not only extend beyond physical and mental health problems but might be
peculiar to these wars. They also face numerous readjustment issues that influence their ability to adjust to life outside theater and that can affect their families. Research on the OEF and OIF deployed population is needed not only to understand the extent of the readjustment but to understand how to provide assistance.
The committee recommends that the Department of Defense, the Department of Veterans Affairs, and other federal agencies fund research on the social and economic effects of deployment and multiple deployments on families. For example, research should examine the effects of multiple deployments on domestic violence and maltreatment of children, as well as on financial well-being.
WOMEN AND MINORITIES
The previous section described the stresses and potential health and social consequences that all service members and their family members face because of service in Iraq and Afghanistan. Select subpopulations in the military face unique stressors and may have other needs that require additional attention. In this section, the committee reviews and summarizes needs specific to women and racial minorities.
Women
Women now comprise over 14% of the active-duty force (DOD, 2007). As of April 2009, 218,000 women had been deployed to OEF or OIF—11% of all personnel deployed to Iraq and Afghanistan (Defense Manpower Data Center, 2009). Although women are technically barred from serving in combat specialties, such as armor or infantry, a growing and unprecedented number of female soldiers are deployed to combat areas where their lives are at risk (Burrelli, 1996); this is a relatively new phenomenon. They serve in a range of support positions (such as pilots, intelligence, transportation, and mechanics) that involve travel outside military bases, coming under direct fire, and working alongside combat soldiers.
All service members are exposed to exceptionally high levels of workplace stress, but women in the military face some unique stressors and trauma exposure that may affect their mental health and emotional well-being. Female veterans have a higher burden of medical illness, worse quality-of-life outcomes, and earlier psychologic morbidity than do men who are exposed to the same levels of trauma (Nayback, 2008). Both the military and family life require commitment and loyalty, and servicewomen who have families may experience intense conflict between the demands of their military and family roles, given the centrality of the maternal role for most women. Some of the issues specific to women are military-related sexual harassment and assault and the resulting mental health outcomes, histories of premilitary trauma, unique health-care needs, pregnancy and the postpartum period, and the configuration of family roles (such as mother, spouse, and caregiver for aging parents).
Military-Related Sexual Harassment and Assault and Mental Health
Women serving in the military face the risk of sexual harassment and sexual assault, both of which are associated with the development of mental health problems. Gradus et al. (2008) reported that 72.5% of women and 41.6% of men in their sample experienced sexual harassment during their military service; these findings are similar to those of earlier work that reported rates
of 78% and 38% in women and men, respectively (Bastian et al., 1996). The study also found an association between sexual harassment and harmful alcohol use in women but not in men (Gradus et al., 2008).
In a study of duty-related stress and sexual stress in the etiology of PTSD in women who sought treatment (Fontana and Rosenheck, 1998), 63% reported experiences of physical and sexual harassment during military service, and 43% reported rape or attempted rape. Both sources of stress were found to contribute significantly to the development of PTSD. On the basis of that pre-OEF and pre-OIF sample, the authors concluded that women’s exposure to sexual stress in the military was much more prevalent than previously believed and that it contributed substantially to the development of PTSD.
A study of a nationally representative sample of women in VA ambulatory care found that nearly one-fourth reported having experienced sexual assault while in the military (Hankin et al., 1999). The study also found that the prevalence of current depressive symptoms was three times higher and the prevalence of current alcohol-abuse symptoms two times higher in women who reported experiencing sexual assault during military service than in women who did not. Servicewomen’s use of mental health–care services was low: only half the women that experienced military sexual assault and exhibited depressive symptoms reported receiving any recent mental health treatment. There are now substantial shortages of qualified mental health specialists in the military, in which professional “burnout” and attrition rates are high (American Psychological Association Presidential Task Force on Military Deployment Services for Youth, Families, and Servicemembers, 2007; Department of Defense Task Force on Mental Health, 2007; Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command, 2008; Tanielian and Jaycox, 2008); this impedes soldiers’ access to needed care. That was a topic that the committee members often heard at their town hall meetings, particularly at the meeting in Killeen, Texas, outside Fort Hood (see Appendix B). Another important barrier to seeking mental health care is the persistence of stigma surrounding mental illness and treatment (Department of Defense Task Force on Mental Health, 2007; Hoge et al., 2004; Tanielian and Jaycox, 2008).
A small but growing body of research investigates the relationship between sexual harassment and sexual trauma and the development of PTSD in women. Kang et al. (2005) conducted a nested case-control study using National Health Survey data to evaluate the association of sexual harassment and assault during deployment with PTSD. They found that out of 2,131 female Gulf War veterans, almost 24% reported a history of sexual harassment and 3.3% reported a history of sexual assault; these rates are lower than those reported by other studies, which may be related to the collection of data 4–5 years after the subjects left the Gulf War theater. Among these 2,131 women veterans, deployment-based sexual harassment and assault were statistically significantly associated with the development of PTSD (OR 5.41, 95% CI 3.19-9.17, respectively) and conferred greater risk for PTSD than did exposure to combat. Furthermore, the analyses identified a dose–response relationship between PTSD status and self-reported degree of sexual trauma (no trauma, sexual harassment only, sexual assault only, and both harassment and assault). Himmelfarb et al. (2006) examined relationships among military sexual trauma, nonmilitary sexual trauma (before and after military service), and PTSD in female veterans and found that sexual trauma during military service was more strongly associated with PTSD than was premilitary or postmilitary trauma.
Premilitary Trauma
Among men and women in the military, rates of premilitary trauma (such as childhood sexual or physical abuse) are significant and higher than those in the general population (Caulfield et al., 2005; Merrill et al., 1999; Rosen and Martin, 1996). For example, a recent study (Caulfield et al., 2005) found childhood physical abuse prevalence of 38% and 27% among Marine Corps servicewomen and servicemen, respectively—far higher than the rates of 5% and 3% derived from the National Comorbidity Survey11 (Kessler et al., 1999).
Women entering military service are particularly likely to report prior trauma. Rosen and Martin (1996) found that 35% of active-duty Army servicemen and 58% of active-duty Army servicewomen reported experiences of childhood sexual or physical abuse. Another study found that 57% of a sample of 1,093 female Navy recruits reported childhood physical or sexual abuse—18% reported physical abuse only, 17% reported sexual abuse only, and 22% reported both (Merrill et al., 1999). In an analysis of the effect of premilitary interpersonal trauma on attrition, Caulfield et al. (2005) found that 48% of men and 68% of women reported a history of premilitary trauma. The investigators found that women who had histories of trauma were 1.6 times more likely to be discharged during recruit training, which is intensely demanding physically and emotionally, than women who did not have such histories. Among recruits who had premilitary trauma histories, women were discharged at a higher rate, 20%, than men, 13% (Caulfield et al., 2005).
Women are also more likely to have experienced chronic trauma before deployment, such as repeated childhood sexual assault or recurring intimate-partner violence, which confers increased risk for the subsequent development of PTSD (Tolin and Foa, 2006). Furthermore, 65% of health-care providers at Walter Reed Army Medical Hospital and Bethesda Naval Hospital reported in an informal survey that sexual trauma (either in childhood or in theater) is an issue in the treatment of female patients for PTSD (D. Benedek, 2008, unpublished data cited in Society for Women’s Health Research, 2008).
Women’s Health-Care Needs
Wartime conditions impose unique challenges for female soldiers who need routine or specialized gynecologic health services, particularly as deployments become longer (over 1 year) and more frequent. Inadequate hygiene facilities for women in combat zones can result in an increase in physical health issues, such as bladder infections (Society for Women’s Health Research, 2008). Furthermore, a substantial gap persists in predeployment gynecologic screenings and in-theater care (Nielsen et al., 2009; Thomson and Nielsen, 2006). For example, in a survey of 251 women deployed to OIF, 44% reported being unable to receive needed care for a variety of gynecologic complaints; barriers to receiving appropriate care included inadequate transportation, laboratory services, and staffing (Thomson and Nielsen, 2006).
Most women in the military are of childbearing age (Reeves, 1995). When pregnancy is confirmed in female soldiers, they are classified as nondeployable but have the option of remaining on active duty to complete their service obligation; however, they are restricted from participating in most unit training activities (such as aircraft flying, marksmanship, and field exercises). Typically, their duties are confined to indoor office work (Bucher, 1999). As a result
of those limitations, exemptions, and work redistribution, pregnant women in a unit are frequently perceived as increasing other soldiers’ workloads—a perception that fosters resentment (Harrell and Miller, 1997). A report from the Defense Women's Health Research Program suggests that those conditions may create an especially stressful environment for pregnant servicewomen (Evans et al., 1996).
The postpartum period can be particularly stressful for female service members, particularly when they are taking care of other children at the same time. A recent analysis (Weina, 2006) of the amount of time that postpartum female soldiers need to return to their prepregnancy fitness level and to perform the Army Physical Fitness Test12 concluded that the current assessment 6 months after delivery does not allow women enough time to recover and that 12 months would be a more suitable time to determine whether female soldiers had returned to their prepregnancy fitness level. The study also found that most women struggled to cope with the combination of roles required of them: mother of a new baby and potentially of other children, soldier, and potentially spouse or partner. In managing their lives, most servicewomen reported experiencing exhaustion to a degree that impeded their ability to exercise and return to their prepregnancy fitness levels by 6 months after delivery.
Caretakers
Women in the military may be particularly stressed by the enormous strain that deployment places on their multiple roles of mother, spouse, and, increasingly, the caretaker for aging parents. Although men might also assume the caretaker role, in general women continue to perform more housework than men and to be primary caregivers to their children regardless of their employment status (Coltrane, 2000). The greater likelihood of being their children’s primary caregiver may make female service members particularly vulnerable to mental health problems when military service demands, such as long and unpredictable hours even while based at home, conflict with their maternal role. Service members are expected to be on call for unexpected problems and emergencies, to maintain a state of readiness for deployment, and to regard the military mission as their top priority; meeting these expectations may be particularly stressful for military women who are raising children. Vinokur et al. (1999) found that in a representative sample of women who served in the Air Force during the Gulf War, parenting stress was associated with both increased family–work conflict and decreased parental involvement and emotional functioning.
Deployment involves being separated from children and families for months at a time and leaving children behind with spouses or alternative caregivers. Single mothers confront special challenges. They report greater disruption to family functioning and more concerns about separation from their children (Kelley, 1994) than do married mothers, probably because of the greater discontinuity in care that deployment imposes on their households.
Deployment appears to affect the marital stability of male and female soldiers differently. Angrist and Johnson (2000) found that deployment led to a large, statistically significant increase in divorce rates in women in the military, but not men. Wives of men in the military may derive more support from the military community, in which women are more likely to fulfill the traditional role of military spouse, and thus be able to adapt to their husbands’ absences to a greater degree. Husbands of servicewomen are in an atypical, potentially isolating position,
paralleling their wives’ experience to some extent. They may not use the community as a buffer against stress to the same degree as female military spouses and may object more to the military’s potentially adverse effect on their employment status due to frequent geographic relocations.
Women and Posttraumatic Stress Disorder
The literature shows that civilian women have higher rates of depression and anxiety disorders, including PTSD, than civilian men (Kessler et al., 2005; Tolin and Foa, 2006). Generally, PTSD affects twice as many women as men, and women who have PTSD report having a lower quality of life than men who have PTSD (Holbrook et al., 2002). Women who have PTSD experience a longer time to remission of symptoms than men, and their symptom remission rate is half that in men (Breslau et al., 1998). Some of the potential sex differences in PTSD may be that women react more negatively to interpersonal stressors, exhibit more ruminative coping, and tend to retain negative memories in such a way that they “relive” the traumatic event to a greater extent (Society for Women’s Health Research, 2008).
Studies of military populations that are posted at permanent bases have yielded findings similar to those in civilian populations (Hoge et al., 2002, 2007; Hourani and Yuan, 1999; Riddle et al., 2007). However, findings of studies that addressed sex differences in deployed military populations have been inconsistent (Hoge et al., 2007). The current knowledge of PTSD in women is sparse and has several important gaps related to the development and course of combat-related PTSD and treatment needs.
The committee recommends that the Department of Defense, the Department of Veterans Affairs, and other federal agencies fund studies to evaluate the effectiveness of mental health treatments currently being provided to women and to identify potential new treatments designed specifically to address women’s unique circumstances and stressors, such as sexual harassment and assault, PTSD, and premilitary trauma.
Ethnicity, Race, and Culture
The US military is a multicultural and racially integrated institution (Lundquist, 2004, 2008) with increasing ethnic and racial diversity. Table 4.1 summarizes the number of minority-group members in the military that have ever been deployed to OEF and OIF.
TABLE 4.1 Racial and Ethnic Characteristics of Deployed Personnel to OEF and OIF from September 11, 2001, to the Present, First Deployment Only
Even though the military is considered one of the most desegregated institutions, there is some evidence that minority-group members may experience discrimination that can have an adverse effect on their physical and mental health. A recent study (Sohn and Harada, 2008) examined the association between perceptions of discrimination and self-reported mental and physical health for Asian and Pacific Islander, black, and Hispanic veterans. Using the 2001 Veteran Identity Program Survey (VIPS), Sohn and Harada measured use of outpatient care, discrimination, and health status in three minority veteran groups. The sample (n = 3,227) was 44% black, 44% Hispanic, and 12% Asian and Pacific Islander. Racial and ethnic discrimination during military service was significantly associated with poorer physical health but not mental health (Sohn and Harada, 2008).
Data on whether there is a differential effect of race and ethnicity on military personnel ever deployed seem to be inconsistent. A study of racial equity (assessed according to examination of the racial distribution of US casualties in Iraq for the first 12 months of the conflict) of military service by Gifford (2005) found that blacks do not disproportionately bear the burden of US military operations, nor do other racial or ethnic minorities. Whites make up the majority of combat casualties given their majority status in active duty and their high representation in the US Army and Marine Corps combat specialties (Gifford, 2005). The data suggest that the probability of any person’s becoming a casualty is a function more of representation in units most likely to make hostile contact with enemy forces than of race or ethnic discrimination in the burden of war.
Nonetheless, there is some evidence that minorities can have the worst outcomes of exposure to war. Secondary data analyses of the NVVRS (n = 1,195) found that Hispanic veterans who served in Vietnam had significantly more severe PTSD symptoms and a higher probability of experiencing PTSD than nonminority veterans (Ortega and Rosenheck, 2000). The authors were unable to explain those differences when adjusting for exposure to stressors or acculturation.
Some reports have addressed the question of whether there are ethnic or racial differences in the receipt of military benefits. A study by Nayback (2008) of minority-group veterans treated in specialized intensive VA programs for war-related PTSD found that black veterans’ likelihood of receiving service-connected disability ratings for PTSD was significantly lower than that of other veterans. Similarly, a study by Murdoch and colleagues (2003) on the effect of veterans’
race or ethnicity on their likelihood of obtaining VA “service connection” benefits for PTSD established that black veterans’ success rate was significantly lower than that of other veterans.
Other findings are inconclusive regarding whether there are ethnic or racial differences in service delivery or outcomes of military personnel. Results of a study by Westermeyer et al. (2002) indicated that American Indian veterans (n = 573) were less likely to use VA mental health services than other professional and nonprofessional mental health services because of the great number of barriers experienced. However, the study did not include a comparison group. In a prospective study of 122 black and 403 white veterans who had PTSD, no consistent or sustained differences in improvement were observed between racial groups, whether it was measured as psychometric change or by clinicians' improvement ratings (Rosenheck and Fontana, 2002).
Results of research on the role of race and ethnicity as risk factors for stress-related illness are mixed, but in general they support the conclusion that blacks and Hispanics are at greater risk for psychiatric disorders, particularly PTSD, as a result of deployment. In the Vietnam Experience Study, nonwhite veterans had a poorer psychologic status 15–20 years after the war than did white veterans (CDC, 1988). Findings from the NVVRS indicate that black and Hispanic veterans had a higher prevalence of PTSD than whites (Kulka et al., 1990). Among theater veterans, the prevalence of current PTSD in the NVVRS was 27.9% in Hispanics, 20.6% in blacks, and 13.7% in whites and others (Kulka et al., 1990). Those proportions held even when racial differences in combat exposure were controlled for inasmuch as minority groups experienced more war-zone exposures.
The Hawaii Vietnam Veterans Project (HVVP), modeled on the NVVRS, determined that veterans of Japanese ancestry had a lower prevalence of PTSD than whites (Friedman et al., 2004). Schnurr et al. (2003) studied 530 veterans drawn from the NVVRS and the HVVP and found that black, Hispanic, and native Hawaiian men were more likely and Americans of Japanese descent less likely than white men to have a lifetime diagnosis of PTSD. Furthermore, they found that Hispanic male veterans were more likely to have current PTSD than men in other ethnic groups (Schnurr et al., 2004). In a study of 1,377 American Legionnaires who had served in Vietnam and were followed for 14 years, minority race contributed to a more chronic course of PTSD; however, the minority sample was too small for further investigation (Koenen et al., 2003).
It has been suggested that the racial gap in prevalence or course of PTSD in Vietnam veterans might stem from racism in the military, identification with a nonwhite enemy, exacerbation of existing stress by institutional racism, or lower financial or emotional resources after the war (Marsella et al., 1990, 1993). Some differences in ascertained rates may also be influenced by cultural differences, such as stigma, that can affect accuracy of reporting. A growing body of research documents racial and ethnic differences in beliefs, perceptions of stigma, and preferences related to mental health counseling and use of psychotropic drugs (Cooper et al., 2003; Menke and Flynn, 2009; Nadeem et al., 2007). Attitudinal barriers to seeking mental health care among racial and ethnic minority servicemen and servicewomen may be greater, particularly in the context of a military culture that continues to stigmatize mental health care.
Several studies of Gulf War veterans have found that minority-group veterans had a greater prevalence of PTSD. In a study by Kang et al. (2003), nonwhite veterans had a higher prevalence of PTSD than white veterans, but the category “nonwhites” was not divided into
minority subgroups, and there was no adjustment for socioeconomic factors other than age and marital status. A study of 653 Gulf War veterans from Louisiana with relatively high minority-group participation (35%) found that minority-group troops, particularly men, tended to report greater psychologic distress and more PTSD symptoms than white men (Sutker et al., 1995); however, as in the Kang et al. study, there was no stratification beyond “nonwhite status” and no adjustment for other factors that may have contributed to the reporting differences. After adjusting for age, sex, race, rank, branch, and military status, Black et al. (2004) found that nonwhite Gulf War veterans were at almost twice the risk of developing an anxiety disorder as white veterans, but the difference was not statistically significant (Black et al., 2004).
Hoge et al. (2002) assessed the incidence of first hospitalization for a mental disorder in active-duty military personnel in 1990–1999. The rates of hospitalization per 1,000 person-years were 9.34 for whites, 9.25 for Hispanics, 8.30 for blacks, 5.97 for Asians and Pacific Islanders, and 18.27 for American Indians and Alaskan Natives. Fontana et al. (2000) found that among US peacekeepers in Somalia, PTSD symptoms were more severe in blacks, although there was no adjustment for socioeconomic factors in the model.
Substance-abuse problems have been explored in a study of black and Hispanic veterans who were being treated in specialized intensive VA programs for people who had war-related PTSD (Rosenheck and Fontana, 2002). The results showed that at the time of program admission, black patients had more severe alcohol and drug problems but less severe PTSD symptoms than white or Hispanic patients.
In an analysis of how “veteran identity” varies with race and ethnicity and of which factors of veteran identity influence preferences for and use of VA outpatient care, Harada et al. (2002) found that black and Latino veterans were twice as likely as non-Latino whites to prefer VA outpatient care. However, Latino veterans were not more likely to use VA outpatient care. Washington et al. (2002) also examined race and ethnicity and the use of VA outpatient services. Using the 1992 National Survey of Veterans, they found that Latino and American Indian veterans were more likely than non-Latino white veterans to report an inability to get needed care (Washington et al., 2002). Those findings on access suggest a need for targeted outreach measures.
The increasing proportion of minorities in the military highlights the need to improve understanding of the potential role of perceived discrimination on health status. Sohn and Harada (2008) used the 2001 VIPS to assess the association between perceptions of discrimination and self-reported mental and physical health in Latino, Asian and Pacific Islander, black, and white veterans. They found that racial and ethnic discrimination during military service was significantly associated with poorer physical health but not mental health. Satisfaction with providers’ sensitivity to racial and ethnic background was significantly associated with better mental health. Those findings underscore the importance of developing policies that address racial and ethnic discrimination during military service while providing health care services for veterans.
The committee recommends that the Department of Defense, the Department of Veterans Affairs, and other federal agencies fund research on culturally sensitive treatment approaches targeted toward minorities. Research is also needed on utilization patterns of currently available services by minority populations and the efficacy of such services to improve health outcomes.
PROJECTING THE LIFELONG BURDEN OF WAR
Previous sections have considered the extent of knowledge about the effects of physical, mental, and other health outcomes and the effects of multiple deployments and reduced dwell times on service members’ spouses, children, and communities. To identify gaps in services and to plan for needed services, there is a requirement for useful information about the economic impact of service in OEF and OIF on individual veterans and their families; however, there is little information on the magnitude of that impact, especially with regard to how it changes over time. The committee will examine the topic more fully in phase 2 of its study, but this section provides a preliminary look at the long-term economic impact of deployment on troops, families, and the larger community.
To clarify what the committee means by economic impact, it is useful to briefly review the way in which economists define the various costs of war. The total social costs of war comprise public costs or budgetary costs, which comprise benefits paid to veterans directly by governments and taxpayers; social economic costs, which comprise the burdens felt and paid for by individual veterans and their households; macroeconomic costs, which are spread over entire economies; and interest costs, namely the extra spending in the future required to put off the payment of costs that come due today. The committee is charged with estimating the economic impact of deployment on those who have served in OEF or OIF and their families. Budgetary costs indicate the extent to which the federal government compensates veterans for negative economic outcomes resulting from their service, while social economic costs indicate the magnitude of additional economic burdens placed on veterans and their families for which the government does not compensate (i.e., indicates needs that are not met). The committee will not, at least in this phase 1 report, discuss macroeconomic or interest costs.
The human burdens of war extend far beyond the period of active conflict, and these burdens carry real economic impacts for veterans and their families. To best plan for alleviating or compensating for these impacts, government projections of readjustment needs should take a long-term view. Although the present report focuses on an initial assessment of the immediate readjustment needs of veterans, their families, and their communities, the fact remains that many wounds of war will persist over veterans’ lifetime. Combat injuries are the clearest example of persistent outcomes, but research has shown that combat deployment results in other, more subtle long-reaching effects. It is critical for VA and DOD to provide for the acute needs of returning veterans and their families, but it is equally important to plan for the long-term consequences and ensure that there will be adequate resources and infrastructure to continue to provide care, services, and compensation to OEF and OIF veterans and their families over many decades.
In the short run, a variety of factors will keep the public costs associated with deployment-related needs deceptively low: the low age of the average OEF or OIF veteran, the potential latency of service-related health conditions (such as PTSD), bottlenecks in access to services, and the relatively low cost of care today compared with care in the future. However, the human costs of coping with the lingering physical, mental, and social deployment-related outcomes will certainly continue to accrue after the conclusion of the Iraq and Afghanistan wars, as can be seen by examining trends in use of health care and benefits in veteran populations from past conflicts.
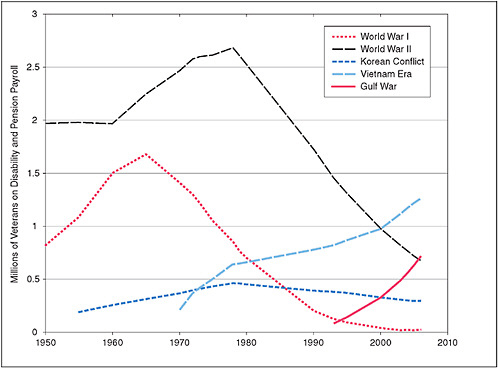
FIGURE 4.1 Number of veterans on disability and pension payrolls by period of service.
NOTE: Data include both living veterans and deceased veterans whose dependents received survivor benefits. Data are derived from the US Census Bureau’s Statistical Abstracts of the United States, 1970, Table 406; 1974, Table 534; 1980, Table 640; 1990, Table 570; 1995, Table 580; and 2008, Table 509, which up to 2000 cite the Annual Report of the Secretary of Veterans Affairs and after 2000 cite VA’s Annual Accountability Report.
Figure 4.1 plots the number of veterans receiving disability and pension benefits from 1950 to 2006, and Figure 4.2 depicts real total spending by cohort or the product of the number of veterans and their cohort-specific average benefit in each year.13 The figures suggest that the number of veterans in a given cohort who are receiving aid has historically peaked several decades after the war. For example, use by the largest and best documented cohort, World War II veterans, peaked around 1978, 33 years after the end of hostilities. The figures also show that the needs of World War I veterans appear to have peaked around 1965, 47 years after armistice. The pattern among veterans of the Korean War is less clear: the number of veterans receiving disability and pensions peaked around 1978, or 25 years after the war, but total real benefits appeared to plateau. The number of Vietnam veterans receiving disability and pensions and total real spending on their benefits are still rising, as are the number of veterans of the Persian Gulf War who receive disability and pensions.

FIGURE 4.2 Total real spending on disability compensation and pensions for veterans by period of service.
NOTE: Each point represents real spending in 2008 inflation-adjusted dollars on members of the veteran cohort, constructed as the product of inflated nominal spending per veteran and the number of veterans receiving benefits in each year. Source data are derived from the US Census Bureau’s Statistical Abstracts of the United States, 1970, Table 406; 1974, Table 534; 1980, Table 640; 1990, Table 569; 1995, Table 579; and 2008, Table 508, which up to 2000 cite the Annual Report of the Secretary of Veterans Affairs and after 2000 cite VA’s Annual Accountability Report.
On the basis of data from past wars, Figures 4.1 and 4.2 strongly suggest that the total number of OEF and OIF veterans seeking government assistance for their service-related healthcare and disability needs and the magnitude of public compensation for those needs will rise for many decades after the conclusion of the conflicts. As of 2008, 230,000 OEF and OIF veterans had filed disability claims. However, the majority of claims have yet to be submitted. Bilmes (2008) projects that a total of 791,000 veterans from the conflicts in Iraq and Afghanistan will seek disability benefits.
It should be noted, however, that the numbers are not perfectly indicative of the total burden of readjustment and coping needs of veterans and their families. Government spending on disability benefits and pensions approximates the magnitude of more latent sources of need—namely, the physical and psychologic effects of military service on veterans—but represents, in combination with direct medical costs paid by the government through VA or TRICARE, only the publicly compensated portion of the burden borne by veterans and their families. Missing
from this accounting method are the unknown social and financial burdens felt and paid by individual veterans and their households, as noted above—what economists refer to as social economic costs. For example, veterans’ disability benefits explicitly do not compensate veterans for any pain and suffering associated with their service-connected disabilities (IOM, 2007; Stiglitz and Bilmes, 2008), and thus pain and suffering are burdens borne by individual veterans. The magnitude of such burdens is poorly understood.
Finally, the historical data do not account for the education, retraining, vocational, and other social needs of returning service members and veterans. Educational benefits, most notably the GI Bill, are a major means of helping veterans to reintegrate into civilian life. Researchers view the 1944 GI Bill as having vastly expanded the educational attainment of birth cohorts with high rates of military service in World War II and Korea (Bound and Turner, 2002; Stanley, 2003). The Post-9/11 Veterans Educational Assistance Act of 2008 expanded the GI Bill to cover OEF and OIF veterans; it went into effect in August 2009. Spending on education benefits is substantial when compared to spending on medical and disability benefits. In 2008, the CBO estimated that through this bill, the government would pay out over $50 billion in benefits over the next 10 years (Orszag, 2008), about 4 times higher than CBO’s “high option” 10-year forecast of VA medical and disability spending (CBO, 2007b). The limited projection suggests that demand for veterans’ education and vocational services accounts for a significant slice of benefits spending, and should be included in comprehensive long-term forecasts of overall readjustment needs of this population.
As noted in Chapter 3 of this report, while lessons learned from past conflicts can be informative, many unique aspects of OEF and OIF might result in significant deviations from historical trends. For example, advances in battlefield medicine have resulted in saving the lives of many severely wounded service members who in past conflicts likely would have died from their wounds. These survivors of very severe injuries need more intensive care than the most severely wounded service members from prior wars, implying that extrapolating from past conflicts might result in an underestimation of the overall burden of need for persons impacted by OEF and OIF. Furthermore, accelerated and lengthened overseas deployment, reduced dwell times between deployments, and repeated reintegration into life outside theater for the returning OEF and OIF service members and their families may result in additional burdens that are poorly understood, including higher rates of divorce, juvenile delinquency, or disruptions in communities that lose workers called up to National Guard or reserve units. Little is known about the incidence of those outcomes or their connection with wartime service, and even less is known about how the burden of need associated with those outcomes evolves over time and more research is vitally needed. The committee will more fully examine these potential and emerging burdens on veterans, their families, and communities in phase 2.
The public and Congress receive forecasts of veterans’ programs very infrequently in the current system. The most consistently produced sets of formal projections are released by CBO, whose researchers sift through VA reports to the Office of Management and Budget to specify many of the key assumptions. At the time of writing of the present report, CBO has not publicly updated its forecasts in 2 years (CBO, 2007b). It appears that CBO does not have the personnel or funding to produce forecasts more frequently, and it is already charged by Congress with assessing a far wider array of government programs than those for veteran support. With CBO forecasts available only sporadically, it is difficult for outside observers to assess their quality or
the quality of private forecasts or, most important, to gain a clear, up-to-date picture of veterans’ service needs.
VA does not have the personnel, the funding, or the mandate from Congress to produce broad forecasts of service needs. The VA actuary generates an annual actuarial forecast of limited scope for the disability payment system that appears in VA’s Performance and Accountability Report, but there are no long-term forecasts of health-care use by the VA population. Meanwhile, the burden borne by wounded service members and their families, and thus the public responsibility to treat or compensate them, is large and probably will persist for the rest of their lives. Historically, as stated above, the peak demand for compensation has lagged the end of hostilities by 30 years or more, so the maximum stress on support systems for OEF and OIF veterans and their families might not be felt until 2040 or later. To produce timely, accurate, and transparent forecasts of veterans’ needs and demands on the system, it is important to put into place mechanisms for anticipating the needs of veterans and their families so that the needs can begin to be met.
The committee recommends that Congress appropriate funds and direct the Department of Veterans Affairs to expand the role of its actuary to produce annual long-term forecasts of costs associated with all health and disability benefits consistent with the practices of Social Security and Medicare.
REFERENCES
Allen, J. P., G. Cross, and J. Swanner. 2005. Suicide in the Army: A review of current information. Military Medicine 170(7):580-584.
American Psychological Association Presidential Task Force on Military Deployment Services for Youth, Families, and Servicemembers. 2007. The Psychological Needs of US Military Service Members and Their Families: A Preliminary Report. American Psychological Association. http://www.apa.org/releases/MilitaryDeploymentTaskForceReport.pdf (accessed July 20, 2009).
Angrist, J. D. 1993. The effect of veterans benefits on education and earnings. Industrial and Labor Relations Review 46(4):637-652.
Angrist, J. D., and J. H. Johnson, 4th. 2000. Effects of work-related absences on families: Evidence from the Gulf War. Industrial and Labor Relations Review 54(1):41-58.
Baguley, I., S. Slewa-Younan, R. Lazarus, and A. Green. 2000. Long-term mortality trends in patients with traumatic brain injury. Brain Injury 14(6):505-512.
Barnes, V. A., H. Davis, and F. A. Treiber. 2007. Perceived stress, heart rate, and blood pressure among adolescents with family members deployed in Operation Iraqi Freedom. Military Medicine 172(1):40-43.
Bastian, L. D., A. R. Lancaster, and H. E. Reyst. 1996. Department of Defense 1995 Sexual Harassment Survey. Washington, DC: Department of Defense.
Beckham, J. C., S. D. Moore, and V. Reynolds. 2000. Interpersonal hostility and violence in Vietnam combat veterans with chronic posttraumatic stress disorder: A review of theoretical models and empirical evidence. Aggression and Violent Behavior 5(5):451-466.
Belanger, H. G., S. G. Scott, J. Scholten, G. Curtiss, and R. D. Vanderploeg. 2005. Utility of mechanism-of-injury-based assessment and treatment: Blast Injury Program case illustration. Journal of Rehabilitation Research and Development 42(4):403-412.
Bilmes, L. 2008. Testimony presented before the US House of Representatives Veterans Affairs Committee Subcommittee on Disability Assistance and Memorial Affairs, February 13. Washington, DC.
Black, D. W., C. P. Carney, P. M. Peloso, R. F. Woolson, E. Letuchy, and B. N. Doebbeling. 2005. Incarceration and veterans of the first Gulf War. Military Medicine 170(7):612-618.
Black, D. W., C. P. Carney, P. M. Peloso, R. F. Woolson, D. A. Schwartz, M. D. Voelker, D. H. Barrett, and B. N. Doebbeling. 2004. Gulf War veterans with anxiety: Prevalence, comorbidity, and risk factors. Epidemiology 15(2):135-142.
Blais, M. C., and J. M. Boisvert. 2005. Psychological and marital adjustment in couples following a traumatic brain injury (TBI): A critical review. Brain Injury 19(14):1223-1235.
Blount, B. W., A. Curry, Jr., and G. I. Lubin. 1992. Family separations in the military. Military Medicine 157(2):76-80.
Boehmer, T., W. Flanders, M. McGeehin, C. Boyle, and D. Barrett. 2004. Postservice mortality in Vietnam veterans. Archives of Internal Medicine 164:1908-1916.
Booth, B., M. W. Segal, and D. B. Bell. 2007. What We Know about Army Families: 2007 Update. Department of the Army, Family and Morale, Welfare and Recreation Command. http://www.army.mil/fmwrc/documents/research/whatweknow2007.pdf (accessed July 17, 2009).
Bordieri, J. E., and D. E. Drehmer. 1984. Vietnam veterans: Fighting the unemployment war. Journal of Applied Social Psychology 14:341-347.
Boscarino, J. A. 2006. External-cause mortality after psychologic trauma: The effects of stress exposure and predisposition. Comprehensive Psychiatry 47(6):503-514.
Bound, J., and S. Turner. 2002. Going to war and going to college: Did World War II and the G.I. Bill increase educational attainment for returning veterans? Journal of Labor Economics 20(4):784-815.
Bower, J. H., D. M. Maraganore, B. J. Peterson, S. K. McDonnell, J. E. Ahlskog, and W. A. Rocca. 2003. Head trauma preceding PD: A case-control study. Neurology 60(10):1610-1615.
Bowling, U. B., and M. D. Sherman. 2008. Welcoming them home: Supporting service members and their families in navigating the tasks of reintegration. Professional Psychology: Research and Practice 39(4):451-458.
Brahm, K. D., H. M. Wilgenburg, J. Kirby, S. Ingalla, C. Y. Chang, and G. L. Goodrich. 2009. Visual impairment and dysfunction in combat-injured servicemembers with traumatic brain injury. Optometry and Vision Science 86(7):817-825.
Bremner, J. D., S. M. Southwick, A. Darnell, and D. S. Charney. 1996. Chronic PTSD in Vietnam combat veterans: Course of illness and substance abuse. American Journal of Psychiatry 153(3):369-375.
Breslau, N. 2001. The epidemiology of posttraumatic stress disorder: What is the extent of the problem? Journal of Clinical Psychiatry 62(17 Suppl):16-22.
Breslau, N., R. Kessler, H. Chilcoat, L. Schultz, G. Davis, and P. Andreski. 1998. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry 55:626-632.
Brown, A. W., C. L. Leibson, J. F. Malec, P. K. Perkins, N. N. Diehl, and D. R. Larson. 2004. Long-term survival after traumatic brain injury: A population-based analysis. NeuroRehabilitation 19(1):37-43.
Bryant, R. A., and A. G. Harvey. 2002. Delayed-onset posttraumatic stress disorder: A prospective evaluation. Australian and New Zealand Journal of Psychiatry 36(2):205-209.
Bucher, M. A. 1999. The Impact of Pregnancy on US Army Readiness, Air Command and Staff College, Air University. Maxwell Air Force Base, Alabama.
Bureau of Labor Statistics. 2009. Employment Situation of Veterans: 2008. Washington, DC: US Department of Labor. http://www.bls.gov/news.release/pdf/vet.pdf (accessed December 2, 2009).
Burrell, L. M., G. A. Adams, D. B. Durand, and C. A. Castro. 2006. The impact of military lifestyle demands on well-being, army, and family outcomes. Armed Forces and Society 33(1):43-58.
Burrelli, D. F. 1996. CRS Issue Brief for Congress: Women in the Armed Forces (updated 1998). Congressional Research Service. 92008. http://digital.library.unt.edu/govdocs/crs/permalink/meta-crs-8522:1 (accessed January 12, 2010).
Calhoun, P. S., J. C. Beckham, and H. B. Bosworth. 2002. Caregiver burden and psychological distress in partners of veterans with chronic posttraumatic stress disorder. Journal of Traumatic Stress 15(3):205-212.
Calhoun, P. S., J. R. Elter, E. R. Jones, H. Kudler, and K. Straits-Troster. 2008. Hazardous alcohol use and receipt of risk-reduction counseling among US veterans of the wars in Iraq and Afghanistan. Journal of Clinical Psychiatry 69(11):1686-1693.
Carty, J., M. L. O’Donnell, and M. Creamer. 2006. Delayed-onset PTSD: A prospective study of injury survivors. Journal of Affective Disorders 90(2-3):257-261.
Caulfield, M., J. Wolfe, K. Turner, T. L. Newton, K. Melia, J. Martin, and J. Goldstein. 2005. Gender and trauma as predictors of military attrition: A study of Marine Corps recruits. Military Medicine 170(12):1037-1043.
CBO (Congressional Budget Office). 2007a. The Effects of Reserve Call-Ups on Civilian Employers. Statement of Heidi Golding before the Commission on the National Guard and Reserves. Washington, DC: Commission on the National Guard and Reserves.
CBO. 2007b. Projecting the Costs to Care for Veterans of US Military Operations in Iraq and Afghanistan. Testimony presented by Matthew S. Goldberg, Deputy Assistant Director for National Security, before the US House of Representatives Committee on Veterans Affairs. October 17, Washington, DC. http://www.cbo.gov/ftpdocs/87xx/doc8710/10-17-VA-Admin_Testimony.pdf (accessed June 18, 2009).
CDC (Centers for Disease Control and Prevention). 1987. Postservice mortality among Vietnam veterans: The Centers for Disease Control Vietnam Experience Study. Journal of the American Medical Association 257(6):790-795.
CDC. 1988. Health status of Vietnam veterans, I: Psychosocial characteristics. Journal of the American Medical Association 259(18):2701-2707.
CDC, 2006. Traumatic Brain Injury: A Guide to Criminal Justice Professionals. http://www.cdc.gov/ncipc/tbi/FactSheets/Prisoner_Crim_Justice_Prof.pdf (accessed February 16, 2010).
CDC. 2009. Fact sheet: Understanding suicide. http://www.cdc.gov/violenceprevention/pdf/Suicide-FactSheet-a.pdf (accessed January 8, 2010).
Chandra, A., S. Lara-Cinisomo, L. H. Jaycox, T. Tanielian, R. M. Burns, T. Ruder, and B. Han. 2010. Children on the homefront: The experience of children from military families. Pediatrics 125(1):16-25.
Chartrand, M. M., D. A. Frank, L. F. White, and T. R. Shope. 2008. Effect of parents’ wartime deployment on the behavior of young children in military families. Archives of Pediatrics and Adolescent Medicine 162(11):1009-1014.
Clark, M. E., M. J. Bair, C. C. Buckenmaier, 3rd, R. J. Gironda, and R. L. Walker. 2007. Pain and combat injuries in soldiers returning from Operations Enduring Freedom and Iraqi Freedom: Implications for research and practice. Journal of Rehabilitation Research and Development 44(2):179-194.
Coltrane, S. 2000. Research on household labor: Modeling and measuring the social embeddedness of routine family work. Journal of Marriage and Family 62(4):1208-1233.
Cook, J. M., R. Thompson, D. S. Riggs, J. C. Coyne, and J. I. Sheikh. 2004. Posttraumatic stress disorder and current relationship functioning among World War II ex-prisoners of war. Journal of Family Psychology 18(1):36-45.
Cooper, L. A., J. J. Gonzales, J. J. Gallo, K. M. Rost, L. S. Meredith, L. V. Rubenstein, N.-Y. Wang, and D. E. Ford. 2003. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care 41(4):479-489.
Corkin, S., T. J. Rosen, E. V. Sullivan, and R. A. Clegg. 1989. Penetrating head injury in young adulthood exacerbates cognitive decline in later years. Journal of Neuroscience 9(11):3876-3883.
Corkin, S., E. V. Sullivan, and F. A. Carr. 1984. Prognostic factors for life expectancy after penetrating head injury. Archives of Neurology 41(9):975-977.
Corso, P. S., J. A. Mercy, T. R. Simon, E. A. Finkelstein, and T. R. Miller. 2007. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. American Journal of Preventive Medicine 32(6)474-482.
Cozza, S. J. (ed.). 2007. Proceedings of the Workgroup on Intervention with Combat Injured Families, December 11–12, 2007. Bethesda, MD: Center for the Study of Traumatic Stress. http://www.dcoe.health.mil/DCoEV2/Content/navigation/documents/csts_workshop_intervention_combat_injured_families_web.pdf (accessed January 11, 2010).
Cozza, S. J., R. S. Chun, and J. A. Polo. 2005. Military families and children during Operation Iraqi Freedom. Psychiatric Quarterly 76(4):371-378.
CRS (Congressional Research Service). 2009. United States Military Casualty Statistics: Operation Iraqi Freedom and Operation Enduring Freedom. Washington, DC. http://fas.org/sgp/crs/natsec/RS22452.pdf (accessed June 18, 2009).
Defense Department Advisory Committee on Women in the Services. 2008. 2008 Annual Report. http://dacowits.defense.gov/tablereports2008_subpage.html (accessed January 11, 2010).
Defense Manpower Data Center. 2009. Contigency Tracking System: Profile of Service Members Ever Deployed. Washington, DC: Office of the Secretary of Defense.
Dekel, R., and H. Goldblatt. 2008. Is there intergenerational transmission of trauma? The case of combat veterans’ children. American Journal of Orthopsychiatry 78(3):281-289.
Department of Defense Task Force on Mental Health. 2007. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board.
Department of the Army. 2009. Army Releases October Suicide Data. http://www.army.mil/-newsreleases/2009/11/13/30396-army-releases-october-suicide-data/?ref=news-releases-title1 (accessed November 30, 2009).
Dikmen, S. S., J. E. Machamer, H. Winn, and N. R. Temkin. 1995. Neuropsychological outcome at 1-year post head injury. Neuropsychology 9(1):80-90.
Dikmen, S. S., N. R. Temkin, J. E. Machamer, A. L. Holubkov, R. T. Fraser, and H. R. Winn. 1994. Employment following traumatic head injuries. Archives of Neurology 51(2):177-186.
Dobscha, S. K., M. E. Clark, B. J. Morasco, M. Freeman, R. Campbell, and M. Helfand. 2009. Systematic review of the literature on pain in patients with polytrauma including traumatic brain injury. Pain Medicine 10(7):1200-1217.
Doctor, J. N., J. Castro, N. R. Temkin, R. T. Fraser, J. E. Machamer, and S. S. Dikmen. 2005. Workers’ risk of unemployment after traumatic brain injury: A normed comparison. Journal of the International Neuropsychological Society 11(6):747-752.
DOD (Department of Defense). 1998. Selected Manpower Statistics, MO1 (The Directorate for Information, Operations, and Reports). Washington, DC: US Government Printing Office.
DOD. 2006. Report on Predatory Lending Practices Directed at Members of the Armed Forces and Their Dependents. Washington, DC: Department of Defense.
DOD. 2007. Demographics 2007: Profile of the Military Community. Washington, DC: Department of Defense.
DOD. 2009. Department of Defense Numbers for Traumatic Brain Injury. Washington, DC: Military Health System. http://www.health.mil/Pages/Page.aspx?ID=49 (accessed November 24, 2009).
Doyle, C. M., G. A. Gotz, N. M. Singer, and K. W. Tyson. 2004. Analysis of Employer Costs from Reserve Component Mobilization. Alexandria, VA: Institute for Defense Analyses. http://www.dtic.mil/cgi-bin/GetTRDoc?AD=ADA430719andLocation=U2anddoc=GetTRDoc.pdf (accessed January 11, 2010).
Eaton, K. M., C. W. Hoge, S. C. Messer, A. A. Whitt, O. A. Cabrera, D. McGurk, A. Cox, and C. A. Castro. 2008. Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine 173(11):1051-1056.
Ebrahimzadeh, M. H., and S. Hariri. 2009. Long-term outcomes of unilateral transtibial amputations. Military Medicine 174(6):593-597.
Ebrahimzadeh, M. H., and M. T. Rajabi. 2007. Long-term outcomes of patients undergoing war-related amputations of the foot and ankle. Journal of Foot and Ankle Surgery 46(6):429-433.
Eby, L. T., J. S. DeMatteo, and J. E. A. Russell. 1997. Employment assistance needs of accompanying spouses following relocation. Journal of Vocational Behavior 50(2):291-307.
Elder, G. A., and A. Cristian. 2009. Blast-related mild traumatic brain injury: Mechanisms of injury and impact on clinical care. Mount Sinai Journal of Medicine 76(2):111-118.
Employer Support of the Guard and Reserve. 1994. Uniformed Services Employment and Reemployment Rights Act of 1994 (USERRA, 38 U.S.C. § 4301–4335). http://esgr.org/userrathelaw.asp?P=43#sub1 (accessed December 30, 2009).
Ender, M. G. 2000. Beyond adolescence: The experiences of adult children of military parents. In The Military Family: A Practice Guide for Human Service Providers, edited by J. A. Martin, L. N. Rosen, and L. R. Sparacino. Westport, CT: Praeger.
Erbes, C., J. Westermeyer, B. Engdahl, and E. Johnsen. 2007. Post-traumatic stress disorder and service utilization in a sample of service members from Iraq and Afghanistan. Military Medicine 172(4):359-363.
Evans, M. A., L. Rosen, T. Boley, and W. Barth. 1996. Women in the Military; Pregnancy, Command Climate, Organizational Behavior, and Outcome. Part 1. Fort Sam Houston, TX: Defense Women’s Health Research Program and the Center for Healthcare Education and Studies, United States Army Medical Department Center and School. http://handle.dtic.mil/100.2/ADA308847 (accessed October 1, 2009).
Faber, A. J., E. Willerton, S. R. Clymer, S. M. MacDermid, and H. M. Weiss. 2008. Ambiguous absence, ambiguous presence: A qualitative study of military reserve families in wartime. Journal of Family Psychology 22(2):222-230.
Farberow, N. L., D. Gallagher-Thompson, M. Gilewski, and L. Thompson. 1992. Changes in grief and mental health of bereaved spouses of older suicides. Journal of Gerontology 47(6):P357-P66.
Flake, E. M., B. E. Davis, P. L. Johnson, and L. S. Middleton. 2009. The psychosocial effects of deployment on military children. Journal of Developmental and Behavioral Pediatrics 30(4):271-278.
Fontana, A., and R. Rosenheck. 1998. Duty-related and sexual stress in the etiology of PTSD among women veterans who seek treatment. Psychiatric Services 49(5):658-662.
Fontana, A., B. Litz, and R. Rosenheck. 2000. Impact of combat and sexual harassment on the severity of posttraumatic stress disorder among men and women peacekeepers in Somalia. Journal of Nervous and Mental Disease 188(3):163-169.
Friedemann-Sanchez, G., J. M. Griffin, N. A. Rettmann, M. Rittman, and M. R. Partin. 2008. Communicating information to families of polytrauma patients: A narrative literature review. Rehabilitation Nursing 33(5):206-213.
Friedman, M. J. 2003. Post-traumatic Stress Disorder: The Latest Assessment and Treatment Strategies. Kansas City, MO: Compact Clinicals.
Friedman, M. J., P. P. Schnurr, A. Sengupta, T. Holmes, and M. Ashcraft. 2004. The Hawaii Vietnam Veterans Project: Is minority status a risk factor for posttraumatic stress disorder? Journal of Nervous and Mental Disease 192(1):42-50.
Galovski, T., and J. A. Lyons. 2004. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran's family and possible interventions. Aggression and Violent Behavior 9(5):477-501.
GAO (Government Accountability Office). 2001. Military Personnel: Longer Time Between Moves Related to Higher Satisfaction and Retention. Washington, DC. GAO-01-841. http://www.gao.gov/new.items/d01841.pdf (accessed January 11, 2010).
GAO. 2009. Military Pay: Gaps in Pay and Benefits Create Financial Hardships for Injured Army National Guard and Reserve Soldiers. Washington, DC. GAO-05-125. http://www.gao.gov/new.items/d05125.pdf (accessed June 18, 2009).
Gerberich, S. G., R. W. Gibson, D. Fife, J. S. Mandel, D. Aeppli, C. T. Le, R. Maxwell, S. J. Rolnick, C. Renier, M. Burlew, and R. Matross. 1997. Effects of brain injury on college academic performance. Neuroepidemiology 16(1):1-14.
Gibbs, D. A., S. L. Martin, L. L. Kupper, and R. E. Johnson. 2007. Child maltreatment in enlisted soldiers’ families during combat-related deployments. Journal of the American Medical Association 298(5):528-535.
Gifford, B. 2005. Combat casualties and race: What can we learn from the 2003-2004 Iraq conflict? Armed Forces and Society 31(2):201-225.
Gironda, R. J., M. E. Clark, J. P. Massengale, and R. L. Walker. 2006. Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Medicine 7(4):339-343.
Gironda, R. J., M. E. Clark, R. L. Ruff, S. Chait, M. Craine, R. Walker, and J. Scholten. 2009. Traumatic brain injury, polytrauma, and pain: Challenges and treatment strategies for the polytrauma rehabilitation. Rehabilitation Psychology 54(3):247-258.
Goff, B. S., J. R. Crow, A. M. Reisbig, and S. Hamilton. 2007. The impact of individual trauma symptoms of deployed soldiers on relationship satisfaction. Journal of Family Psychology 21(3):344-353.
Gradus, J. L., A. E. Street, K. Kelly, and J. Stafford. 2008. Sexual harassment experiences and harmful alcohol use in a military sample: Differences in gender and the mediating role of depression. Journal of Studies on Alcohol and Drugs 69(3):348-351.
Grant, B. F., F. S. Stinson, D. A. Dawson, S. P. Chou, M. C. Dufour, W. Compton, R. P. Pickering, and K. Kaplan. 2004. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 61(8):807-816.
Graves, S. M., and C. L. Peterson. 2005. Predatory lending and the military: The law and geograpy of “payday” loans in military towns. Ohio State Law Review 66(4).
Gray, M. J., E. E. Bolton, and B. T. Litz. 2004. A longitudinal analysis of PTSD symptom course: Delayed-onset PTSD in Somalia peacekeepers. Journal of Consulting and Clinical Psychology 72(5):909-913.
Green, B. L., J. D. Lindy, M. C. Grace, G. C. Gleser, A. C. Leonard, M. Korol, and C. Winget. 1990. Buffalo Creek survivors in the second decade: Stability of stress symptoms. American Journal of Orthopsychiatry 60(1):43-54.
Haas, D. M., and L. A. Pazdernik. 2007. Partner deployment and stress in pregnant women. Journal of Reproductive Medicine 52(10):901-906.
Haas, D. M., L. A. Pazdernik, and C. H. Olsen. 2005. A cross-sectional survey of the relationship between partner deployment and stress in pregnancy during wartime. Women’s Health Issues 15(2):48-54.
Hankin, C. S., K. M. Skinner, L. M. Sullivan, D. R. Miller, S. Frayne, and T. J. Tripp. 1999. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. Journal of Traumatic Stress 12(4):601-612.
Harada, N. D., J. Damron-Rodriguez, V. M. Villa, D. L. Washington, S. Dhanani, H. Shon, M. Chattopadhyay, H. Fishbein, M. Lee, T. Makinodan, and R. Andersen. 2002. Veteran identity and race/ethnicity: Influences on VA outpatient care utilization. Medical Care 40(1 Suppl):117-128.
Harrell, M., and L. Miller. 1997. New Opportunities for Military Women: Effects Upon Readiness, Cohesion, and Morale. Santa Monica, CA: RAND Corporation.
Harrell, M. C., N. Lim, L. W. Castaneda, and D. Golinelli. 2004. Working Around the Military: Challenges of Military Spouse Employment and Education. Santa Monica, CA: RAND Corporation.
Harrison-Felix, C., G. Whiteneck, M. DeVivo, F. M. Hammond, and A. Jha. 2004. Mortality following rehabilitation in the Traumatic Brain Injury Model Systems of Care. NeuroRehabilitation 19(1):45-54.
Harvard School of Medicine. 2005. National Comorbidity Survey. http://www.hcp.med.harvard.edu/ncs/ (accessed March 18, 2010).
Helmer, D. A., H. K. Chandler, K. S. Quigley, M. Blatt, R. Teichman, and G. Lange. 2009. Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Medicine 10(7):1174-1182.
Hill, J. J., 3rd, B. H. Mobo, Jr., and M. R. Cullen. 2009. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: Preliminary findings from the Veterans Affairs traumatic brain injury screening program. American Journal of Physical Medicine and Rehabilitation 88(8):605-614.
Himmelfarb, N., D. Yaeger, and J. Mintz. 2006. Posttraumatic stress disorder in female veterans with military and civilian sexual trauma. Journal of Traumatic Stress 19(6):837-846.
Hoge, C. W., and C. A. Castro. 2006. Post-traumatic stress disorder in UK and US forces deployed to Iraq. Lancet 368(9538):837.
Hoge, C. W., J. L. Auchterlonie, and C. S. Milliken. 2006. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association 295(9):1023-1032.
Hoge, C. W., C. A. Castro, S. C. Messer, D. McGurk, D. I. Cotting, and R. L. Koffman. 2004. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351(1):13-22.
Hoge, C. W., S. E. Lesikar, R. Guevara, J. Lange, J. F. Brundage, C. C. Engel Jr, S. C. Messer, and D. T. Orman. 2002. Mental disorders among US military personnel in the 1990s: Association with high levels of health care utilization and early military attrition. American Journal of Psychiatry 159(9):1576-1583.
Hoge, C. W., D. McGurk, J. Thomas, A. L. Cox, C. C. Engel, and C. A. Castro. 2008. Mild traumatic brain injury in US soldiers returning from Iraq. New England Journal of Medicine 358(5):453-463.
Hoge, C. W., A. Terhakopian, C. A. Castro, S. C. Messer, and C. C. Engel. 2007. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq War veterans. American Journal of Psychiatry 164(1):150-153.
Holbrook, T. L., D. B. Hoyt, M. B. Stein, and W. J. Sieber. 2002. Gender differences in long-term posttraumatic stress disorder outcomes after major trauma: Women are at higher risk of adverse outcomes than men. Journal of Trauma 53(5):882-888.
Holsinger, T., D. C. Steffens, C. Phillips, M. J. Helms, R. J. Havlik, J. C. S. Breitner, J. M. Guralnik, and B. L. Plassman. 2002. Head injury in early adulthood and the lifetime risk of depression. Archives of General Psychiatry 59(1):17-22.
Hope, J. B., D. B. Christman, and P. C. Mackin. 2009. An Analysis of the Effect of Reserve Activation on Small Business. Annandale, VA: SAG Corporation.
Hourani, L. L., and H. Yuan. 1999. The mental health status of women in the Navy and Marine Corps: Preliminary findings from the Perceptions of Wellness and Readiness Assessment. Military Medicine 164(3):174-181.
Huebner, A. J., and J. A. Mancini. 2005. Adjustments Among Adolescents in Military Families When a Parent Is Deployed: Final Report to the Military Family Research Institute and Department of Defense Quality of Life Office. Alexandria, VA: National Military Family Association.
Huebner, A. J., J. A. Mancini, R. M. Wilcox, S. R. Grass, and G. A. Grass. 2007. Parental deployment and youth in military families: Exploring uncertainty and ambiguous loss. Family Relations 56(2):112-122.
Hughes, J. G., N. M. Earnshaw, N. Greenberg, R. Eldridge, N. T. Fear, C. French, M. P. Deahl, and S. Wessely. 2008. The use of psychological decompression in military operational environments. Military Medicine 173(6):534-538.
IOM (Institute of Medicine). 2006. Posttraumatic Stress Disorder: Diagnosis and Assessment. Washington, DC: The National Academies Press.
IOM. 2007. A 21st Century System for Evaluating Veterans for Disability Benefits. Washington, DC: The National Academies Press.
IOM. 2008a. Gulf War and Health: Volume 6. Physiologic, Psychologic, and Psychosocial Effects of Deployment-Related Stress. Washington, DC: The National Academies Press.
IOM. 2008b. Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC: The National Academies Press.
IOM. 2009. Gulf War and Health Volume 7: Long-Term Consequences of Traumatic Brain Injury. Washington, DC: The National Academies Press.
Jacobson, I. G., M. A. Ryan, T. J. Hooper, T. C. Smith, P. J. Amoroso, E. J. Boyko, G. D. Gackstetter, T. S. Wells, and N. S. Bell. 2008. Alcohol use and alcohol-related problems before and after military combat deployment. Journal of the American Medical Association 300(6):663-675.
Jensen, P. S., D. Martin, and H. Watanabe. 1996. Children’s response to parental separation during Operation Desert Storm. Journal of the American Academy of Child and Adolescent Psychiatry 35(4):433-441.
Kang, H. K., and T. A. Bullman. 2008. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. Journal of American Medical Association 300(6):652-653.
Kang, H., N. Dalager, C. Mahan, and E. Ishii. 2005. The role of sexual assault on the risk of PTSD among Gulf War veterans. Annals of Epidemiology 15(3):191-195.
Kang, H. K., B. H. Natelson, C. M. Mahan, K. Y. Lee, and F. M. Murphy. 2003. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: Population-based survey of 30,000 veterans. American Journal of Epidemiology 157:141-148.
Kaplan, M. S., N. Huguet, B. H. McFarland, and J. T. Newsom. 2007. Suicide among male veterans: A prospective population-based study. Journal of Epidemiology and Community Health 61(7):619-624.
Karney, B. R., and J. S. Crown. 2007. Families Under Stress: An Assessment of Data, Theory, and Research on Marriage and Divorce in the Military. Santa Monica, CA: RAND Corporation. http://www.rand.org/pubs/monographs/MG599/ (accessed January 11, 2010).
Kelley, M. L. 1994. The effects of military-induced separation on family factors and child behavior. American Journal of Orthopsychiatry 64(1):103-111.
Kelley, M. L., E. Hock, J. F. Bonney, M. S. Jarvis, K. M. Smith, and M. A. Gaffney. 2001. Navy mothers experiencing and not experiencing deployment: Reasons for staying in or leaving the military. Military Psychology 13(1):55-71.
Kessler, R. C., G. Borges, and E. E. Walters. 1999. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry 56(7):617-626.
Kessler, R., W. Chiu, O. Demler, and E. Walters. 2005. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:617-627.
Ketz, A. K. 2008. Pain management in the traumatic amputee. Critical Care Nursing Clinics of North America 20(1):51-57.
Kleykamp, M. 2009. A great place to start?: The effect of prior military service on hiring. Armed Forces and Society 35(2):266-285.
Koenen, K. C., J. M. Stellman, S. D. Stellman, and J. F. Sommer Jr. 2003. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology 71(6):980-986.
Koenen, K. C., S. D. Stellman, J. F. Sommer Jr., and J. M. Stellman. 2008. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in Vietnam veterans: A 14-year follow-up. Journal of Traumatic Stress 21(1):49-57.
Kolkow, T. T., J. L. Spira, J. S. Morse, and T. A. Grieger. 2007. Post-traumatic stress disorder and depression in health care providers returning from deployment to Iraq and Afghanistan. Military Medicine 172(5):451-455.
Kulka, R., W. Schlenger, J. Fairbank, R. Hough, B. Jordan, C. Marmar, and D. Weiss. 1990. Trauma and the Vietnam Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel.
Lande, R. G., B. A. Marin, A. S. Chang, and G. R. Lande. 2008. Survey of alcohol use in the US Army. Journal of Addictive Diseases 27(3):115-121.
Lapierre, C. B., A. E. Schwegler, and B. J. LaBauve. 2007. Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. Journal of Traumatic Stress 20(6):933-943.
Lew, H. L., J. F. Jerger, S. B. Guillory, and J. A. Henry. 2007a. Auditory dysfunction in traumatic brain injury. Journal of Rehabilitation Research and Development 44(7):921-928.
Lew, H. L., J. D. Otis, C. Tun, R. D. Kerns, M. E. Clark, and D. X. Cifu. 2009. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: Polytrauma clinical triad. Journal of Rehabilitation Research and Development 46(6).
Lew, H. L., J. H. Poole, R. D. Vanderploeg, G. L. Goodrich, S. Dekelboum, S. B. Guillory, B. Sigford, and D. X. Cifu. 2007b. Program development and defining characteristics of returning military in a VA Polytrauma Network Site. Journal of Rehabilitation Research and Development 44(7):1027-1034.
Lewin, W., T. F. Marshall, and A. H. Roberts. 1979. Long-term outcome after severe head injury. British Medical Journal 2(6204):1533-1538.
Lincoln, A., E. Swift, and M. Shorteno-Fraser. 2008. Psychological adjustment and treatment of children and families with parents deployed in military combat. Journal of Clinical Psychology 64(8):984-992.
Loughran, D. S., and J. A. Klerman. 2008. Explaining the Increase in Unemployment Compensation for Ex-Servicemembers During the Global War on Terror. Santa Monica, CA: RAND Corporation. TR-588-OSD. http://www.rand.org/pubs/technical_reports/TR588/ (accessed June 18, 2009).
Loughran, D. S., J. A. Klerman, and B. Savych. 2006. The Effect of Reserve Activations and Active-Duty Deployments on Local Employment During the Global War on Terrorism. Santa Monica, CA: RAND Corporation. http://www.rand.org/pubs/technical_reports/TR321/ (accessed December 4, 2009).
Lundquist, J. H. 2004. A Counterfactual Approach to the Black-White Differential in Family Trends: The Effect of a “Total Institution.” Dissertation. University of Pennsylvania, Philadelphia, PA.
Lundquist, J. H. 2008. Ethnic and gender satisfaction in the military: The effect of a meritocratic institution. American Sociological Review 73:477-496.
Lyle, D. S. 2006. Using military deployments and job assignments to estimate the effect of parental absences and household relocations on children’s academic achievement. Journal of Labor Economics 24(2):319-350.
Lyons, M. J., W. S. Kremen, C. Franz, M. D. Grant, H. T. Brenner, C. Boake, and S. Eisen. 2006. Vietnam service, combat, and lifetime educational attainment: Preliminary results from the Vietnam Era Twin Study of Aging. Research on Aging 28(1):37-55.
MacLean, A. 2005. Lessons from the cold war: Military service and college education. Sociology of Education 78(3):250-266.
Mansfield, A. J., J. S. Kaufman, S. W. Marshall, B. N. Gaynes, J. P. Morrissey, and C. C. Engel. 2010. Deployment and the use of mental health services among U.S. military wives. New England Journal of Medicine 362(2):101-109.
Marsella, A. J., C. Chemtob, and R. Hamada. 1990. Ethnocultural aspects of PTSD in Vietnam War veterans. National Center for PTSD Clinical Newsletter 1(1):3-4.
Marsella, A. J., M. Friedman, and E. H. Spain. 1993. Ethnocultural aspects of PTSD. In Review of Psychiatry, edited by J. Oldham, M. Riba, and A. Tasman. Washington, DC: American Psychiatric Press. Pp. 157-181.
Marshall, A. D., J. Panuzio, and C. T. Taft. 2005. Intimate partner violence among military veterans and active duty servicemen. Clinical Psychology Review 25(7):862-876.
Martorell, F., J. A. Klerman, and D. S. Loughran. 2008. How Do Earnings Change When Reservists Are Activated? A Reconciliation of Estimates Derived from Survey and Administrative Data. Santa Monica, CA: RAND Corporation. http://www.rand.org/pubs/technical_reports/TR565/ (accessed December 4, 2009).
Mayo Clinic. 2008. Alcoholism: Complications. http://www.mayoclinic.com/health/alcoholism/DS00340 (accessed December 7, 2009).
McCarroll, J. E., Z. Fan, J. H. Newby, and R. J. Ursano. 2008. Trends in US Army child maltreatment reports: 1990-2004. Child Abuse Review 17(2):108-118.
McCarroll, J. E., K. J. Hoffman, A. Grieger, and H. C. Holloway. 2005. Psychological aspects of deployment and reunion. In Military Preventive Medicine: Mobilization and Deployment. Vol. 2, edited by P. W. Kelley. Washington, DC: Office of the Surgeon General, Department of the Army and Borden Institute. Pp. 1395-1426.
McCarroll, J. E., R. J. Ursano, X. Liu, L. E. Thayer, J. H. Newby, A. E. Norwood, and C. S. Fullerton. 2000. Deployment and the probability of spousal aggression by US Army soldiers. Military Medicine 165(1):41-44.
McCone, D., and K. O’Donnell. 2006. Marriage and divorce trends for graduates of the US Air Force Academy. Military Psychology 18(1):61-75.
McCreary, D. R., M. M. Thompson, and L. Pasto. 2003. Predeployment family concerns and soldier well-being: The impact of family concerns on the predeployment well-being of Canadian Forces Personnel. The Canadian Journal of Police and Security Services 1:33-40.
McLeod, A., A. Wills, and J. Etherington. 2004. Employment retention after moderate-severe traumatic brain injury (TBI) in the British Army 1989-98. Occupational and Environmental Medicine 61(5):414-418.
Menke, R., and H. Flynn. 2009. Relationships between stigma, depression, and treatment in white and African American primary care patients. Journal of Nervous and Mental Disease 197(6):407-411.
Merrill, L. L., C. E. Newell, C. J. Thomsen, S. R. Gold, J. S. Milner, M. P. Koss, and S. G. Rosswork. 1999. Childhood abuse and sexual revictimization in a female navy recruit sample. Journal of Traumatic Stress 12(2):211-225.
Meyer, K., K. Helmick, S. Doncevic, and R. Park. 2008. Severe and penetrating traumatic brain injury in the context of war. Journal of Trauma Nursing 15(4):185-189.
Mumola, C. J. 2000. Veterans in Prison or Jail. US Department of Justice. NCJ 178888. http://bjs.ojp.usdoj.gov/content/pub/pdf/vpj.pdf (accessed January 11, 2010).
Murdoch, M., J. Hodges, D. Cowper, L. Fortier, and M. van Ryn. 2003. Racial disparities in VA service connection for posttraumatic stress disorder disability. Medical Care 41(4):536-549.
Nadeem, E., J. M. Lange, D. Edge, M. Fongwa, T. Belin, and J. Miranda. 2007. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psychiatric Services 58(12):1547-1554.
Nampiaparampil, D. E. 2008. Prevalence of chronic pain after traumatic brain injury: A systematic review. Journal of the American Medical Association 300(6):711-719.
National Defence and Canadian Forces Ombudsman. 2004. From Tents to Sheets: An Analysis of the CF Experience with Third Location Decompression After Deployment. http://www.ombudsman.forces.gc.ca/rep-rap/sr-rs/tld-dtl/index-eng.asp (accessed January 11, 2010).
Nayback, A. M. 2008. Health disparities in military veterans with PTSD: Influential sociocultural factors. Journal of Psychosocial Nursing and Mental Health Services 46(6):41-51.
Nelson, T. J., T. Clark, E. T. Stedje-Larsen, C. T. Lewis, J. M. Grueskin, E. L. Echols, D. B. Wall, E. A. Felger, and H. R. Bohman. 2008. Close proximity blast injury patterns from improvised explosive devices in Iraq: A report of 18 cases. Journal of Trauma 65(1):212-217.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2007. FAQs for the General Public. http://www.niaaa.nih.gov/FAQs/General-English/default.htm#whatis (accessed January 8, 2010).
Nielsen, P. E., C. S. Murphy, J. Schulz, S. H. Deering, V. Truong, T. McCartin, and J. L. Clemons. 2009. Female soldiers gynecologic healthcare in Operation Iraqi Freedom: A survey of camps with echelon three facilities. Military Medicine 174:1172-1176.
NIMH (National Institute of Mental Health). 2009. Suicide in the US: Statistics and Prevention. http://www.nimh.nih.gov/health/publications/suicide-in-the-us-statistics-and-prevention/index.shtml (accessed January 8, 2010).
North, C. S., S. J. Nixon, S. Shariat, S. Mallonee, J. C. McMillen, E. L. Spitznagel, and E. M. Smith. 1999. Psychiatric disorders among survivors of the Oklahoma City bombing. Journal of the American Medical Association 282(8):755-762.
Oddy, M., M. Humphrey, and D. Uttley. 1978. Subjective impairment and social recovery after closed head injury. Journal of Neurology, Neurosurgery and Psychiatry 41(7):611-616.
Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command. 2006a. Mental Health Advisory Team (MHAT III): Operation Iraqi Freedom 04-06. Washington, DC: Department of the Army.
Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command. 2006b. Mental Health Advisory Team (MHAT) IV: Operation Iraqi Freedom 05-07 Final Report. Washington, DC: Department of the Army.
Office of the Surgeon Multinational Force–Iraq and Office of the Surgeon General United States Army Medical Command. 2008. Mental Health Advisory Team V (MHAT-V) Operation Iraqi Freedom 06-08: Iraq; Operation Enduring Freedom 8: Afghanistan. Washington, DC: Department of the Army.
Ommaya, A. K. 1996. Traumatic Brain Injury in the US Army: Behavioral Sequelae and Medical Disability. Abstract, Executive Summary, and Dissertation. Johns Hopkins University, Baltimore, MD. School of Hygiene and Public Health. Agency for Health Care Policy and Research, Rockville, MD. Center for Research Dissemination and Liaison.
Op Den Velde, W., J. E. Hovens, P. G. H. Aarts, E. Frey-Wouters, P. R. J. Falger, H. Van Duijn, and J. H. M. De Groen. 1996. Prevalence and course of posttraumatic stress disorder in Dutch veterans of the civilian resistance during World War II: An overview. Psychological Reports 78(2):519-529.
Oron, A. 2006. Easy Prey: Evidence for Race and Military Related Targeting in the Distribution of Pay-Day Loan Branches in Washington state (Consulting Report). Department of Statistics, University of Washington.
Orszag, P. 2008. S. 22, Post 9/11 Veterans Educational Assistance Act of 2008: Cost Estimate for the Bill as Provided on April 23, 2008 (Letter to Hon. Judd Gregg, dated May 8, 2008). http://www.cbo.gov/ftpdocs/92xx/doc9212/s22.pdf (accessed January 14, 2010).
Ortega, A. N., and R. Rosenheck. 2000. Posttraumatic stress disorder among Hispanic Vietnam veterans. American Journal of Psychiatry 157(4):615-619.
Orthner, D. K. 2002. SAF IV Survey Report: Deployment and Separation Adjustment Among Army Civilian Spouses. Chapel Hill, NC: University of North Carolina, US Army Community and Family Support Center.
Orthner, D. K., and R. Rose. 2002. Relocation Adjustment Among Army Civilian Spouses. Washington, DC: Army Research Institute for the Behavioral and Social Sciences.
Otis, J. D., T. M. Keane, R. D. Kerns, C. Monson, and E. Scioli. 2009. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Medicine 10(7):1300-1311.
Pan, H. S., P. H. Neidig, and K. D. O’Leary. 1994. Predicting mild and severe husband-to-wife physical aggression. Journal of Consulting and Clinical Psychology 62(5):975-981.
Perlesz, A., G. Kinsella, and S. Crowe. 1999. Impact of traumatic brain injury on the family: A critical review. Rehabilitation Psychology 44(1):6-35.
Plassman, B. L., R. Havlik, D. Steffens, M. Helms, T. Newman, D. Drosdick, C. Phillips, B. Gau, K. Welsh-Bohmer, J. Burke, J. Guralnik, and J. Breitner. 2000. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology 55(8):1158-1166.
Port, C. L., B. Engdahl, and P. Frazier. 2001. A longitudinal and retrospective study of PTSD among older prisoners of war. American Journal of Psychiatry 158(9):1474-1479.
Pratt, L. A., and D. J. Brody. 2008. NCHS Data Brief: Depression in the United States Household Population, 2005–2006. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services. (PHS) 2008-1209. http://www.cdc.gov/nchs/data/databriefs/db07.pdf (accessed November 15, 2009).
Range, L. 1998. When a loss is due to suicide: Unique aspects of bereavement. In Perspectives on Loss: A Sourcebook, edited by J. H. Harvey. Philadelphia, PA: Brunner/Mazel. Pp. 213-220.
Ratcliff, G., A. Colantonio, M. Escobar, S. Chase, and L. Vernich. 2005. Long-term survival following traumatic brain injury. Disability and Rehabilitation 27(6):305-314.
Reeves, C. L. 1995. Dual-Service and Single Parents: What about the Kids? Minerva: Quarterly Report on Women and the Military XIII(3 and 4 Fall/Winter):25-68.
Reinkober Drummet, A., M. Coleman, and S. Cable. 2003. Military families under stress: Implications for family life education. Family Relations 52(3):279-287.
Renshaw, K. D., C. S. Rodrigues, and D. H. Jones. 2008. Psychological symptoms and marital satisfaction in spouses of Operation Iraqi Freedom veterans: Relationships with spouses’ perceptions of veterans’ experiences and symptoms. Journal of Family Psychology 22(4):586-594.
Rentz, E. D., S. W. Marshall, D. Loomis, C. Casteel, S. L. Martin, and D. A. Gibbs. 2007. Effect of deployment on the occurrence of child maltreatment in military and nonmilitary families. American Journal of Epidemiology 165(10):1199-1206.
Reynolds, F. M. T., and P. Cimbolic. 1988. Attitudes toward suicide survivors as a function of survivors’ relationship to the victim. Omega 19(2):125-133.
Riddle, J. R., T. C. Smith, B. Smith, T. E. Corbeil, C. C. Engel, T. S. Wells, C. W. Hoge, J. Adkins, M. Zamorski, and D. Blazer. 2007. Millennium Cohort: The 2001-2003 baseline prevalence of mental disorders in the US military. Journal of Clinical Epidemiology 60(2):192-201.
Rish, B. L., J. D. Dillon, and G. H. Weiss. 1983. Mortality following penetrating craniocerebral injuries. An analysis of the deaths in the Vietnam Head Injury Registry population. Journal of Neurosurgery 59(5):775-780.
Ritenour, A. E., A. Wickley, J. S. Ritenour, B. R. Kriete, L. H. Blackbourne, J. B. Holcomb, and C. E. Wade. 2008. Tympanic membrane perforation and hearing loss from blast overpressure in Operation Enduring Freedom and Operation Iraqi Freedom wounded. Journal of Trauma 64(2 Suppl):S174-S178.
Robrecht, D. T., J. Millegan, L. L. Leventis, J. B. Crescitelli, and R. N. McLay. 2008. Spousal military deployment as a risk factor for postpartum depression. Journal of Reproductive Medicine 53(11):860-864.
Rosen, L. N., and L. Martin. 1996. The measurement of childhood trauma among male and female soldiers in the US army. Military Medicine 161(6):342-345.
Rosenheck, R., and A. Fontana. 1994. Utilization of mental health services by minority veterans of the Vietnam era. Journal of Nervous and Mental Disease 182(12):685-691.
Rosenheck, R., and A. Fontana. 2002. Black and Hispanic veterans in intensive VA treatment programs for Posttraumatic stress disorder. Medical Care 40(1 Suppl):I52-I61.
Rossignol, M. 2007. Afghanistan: Military Personnel and Operational Stress Injuries. Parliamentary Information and Research Service. PRB 07-20E. http://www2.parl.gc.ca/Content/LOP/ResearchPublications/prb0720-e.pdf (accessed January 11, 2009).
Ruff, R. L., S. S. Ruff, and X.-F. Wang. 2008. Headaches among Operation Iraqi Freedom/Operation Enduring Freedom veterans with mild traumatic brain injury associated with exposures to explosions. Journal of Rehabilitation Research and Development 45(7):941-952.
Ruger, W., S. E. Wilson, and S. L. Waddoups. 2002. Warfare and welfare: Military service, combat, and marital dissolution. Armed Forces and Society 29(1):85-107.
Ruscio, A. M., F. W. Weathers, L. A. King, and D. W. King. 2002. Male war-zone veterans’ perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress 15(5):351-357.
Ruzich, M. J., J. C. L. Looi, and M. D. Robertson. 2005. Delayed onset of posttraumatic stress disorder among male combat veterans: A case series. American Journal of Geriatric Psychiatry 13(5):424-427.
Sampson, R. J., and J. H. Laub. 1996. Socioeconomic achievement in the life course of disadvantaged men: Military service as a turning point, circa 1940-1965. American Sociological Review 61(3):347-367.
Savoca, E., and R. Rosenheck. 2000. The civilian labor market experiences of Vietnam-era veterans: The influence of psychiatric disorders. The Journal of Mental Health Policy and Economics 3(4):199-207.
Savych, B. 2007. Away from Home: The Effect of Military Deployment on Spousal Labor Force Participation. Santa Monica, CA: RAND Corporation.
Sayer, N. A., D. X. Cifu, S. McNamee, C. E. Chiros, B. J. Sigford, S. Scott, and H. L. Lew. 2009. Rehabilitation needs of combat-injured service members admitted to the VA Polytrauma Rehabilitation Centers: The role of PM&R in the care of wounded warriors. PM & R: The Journal of Injury, Function, and Rehabilitation 1(1):23-28.
Sayers, S. L., V. A. Farrow, J. Ross, and D. W. Oslin. 2009. Family problems among recently returned military veterans referred for a mental health evaluation. Journal of Clinical Psychiatry 70(2):163-170.
Schneiderman, A. I., E. R. Braver, and H. K. Kang. 2008. Underdstanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology 167(12):1446-1452.
Schnurr, P. P., C. A. Lunney, and A. Sengupta. 2004. Risk factors for the development versus maintenance of posttraumatic stress disorder. Journal of Traumatic Stress 17(2):85-95.
Schnurr, P. P., C. A. Lunney, A. Sengupta, and L. C. Waelde. 2003. A descriptive analysis of PTSD chronicity in Vietnam veterans. Journal of Traumatic Stress 16(6):545-553.
Schwab, K., J. Grafman, A. M. Salazar, and J. Kraft. 1993. Residual impairments and work status 15 years after penetrating head injury: Report from the Vietnam Head Injury Study. Neurology 43(1):95-103.
Seal, K. H., D. Bertenthal, C. R. Miner, S. Sen, and C. Marmar. 2007. Bringing the war back home: Mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Archives of Internal Medicine 167(5):476-482.
Seal, K. H., T. J. Metzler, K. S. Gima, D. Bertenthal, S. Maguen, and C. R. Marmar. 2009. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002-2008. American Journal of Public Health 99(9):1651-1658.
Selassie, A. W., M. L. McCarthy, P. L. Ferguson, J. Tian, and J. A. Langlois. 2005. Risk of post-hospitalization mortality among persons with traumatic brain injury, South Carolina 1999-2001. Journal of Head Trauma Rehabilitation 20(3):257-269.
Shalev, A. Y., S. Freedman, T. Peri, D. Brandes, T. Sahar, S. P. Orr, and R. K. Pitman. 1998. Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry 155(5):630-637.
Shavelle, R., and D. Strauss. 2000. Comparative mortality of adults with traumatic brain injury in California, 1988-1997. Journal of Insurance Medicine 32(3):163-166.
Silver, J. M., T. W. Mc Allister, and S. C. Yudofsky. 2005. Textbook of Traumatic Brain Injury. Washington, DC: American Psychiatric Publishing, Inc.
Slone, L. B., A. S. Pomerantz, and M. J. Friedman. 2009. Vermont: A case history for supporting National guard troops and their families. Psychiatric Annals 39(2):89-95.
Smith, B., M. A. K. Ryan, D. L. Wingard, T. L. Patterson, D. J. Slymen, and C. A. Macera. 2008. Cigarette smoking and military deployment. A prospective evaluation. American Journal of Preventive Medicine 35(6):539-546.
Society for Women’s Health Research. 2008. PTSD in Women Returning from Combat: Future Directions in Research and Service Delivery. National Institute of Mental Health. http://www.womenshealthresearch.org/site/DocServer/PTSD_in_Women_Returning_From_Combat--reduced_file_size.pdf?docID=2661 (accessed January 12, 2010).
Sohn, L., and N. D. Harada. 2008. Effects of racial/ethnic discrimination on the health status of minority veterans. Military Medicine 173(4):331-338.
Solomon, Z., R. Dekel, and G. Zerach. 2008. The relationships between posttraumatic stress symptom clusters and marital intimacy among war veterans. Journal of Family Psychology 22(5):659-666.
Southwick, S., C. Morgan, 3rd, A. Darnell, D. Bremner, A. Nicolaou, L. Nagy, and D. Charney. 1995. Trauma-related symptoms in veterans of Operation Desert Storm: A 2-year follow-up. American Journal of Psychiatry 152(8):1150-1155.
Stahre, M. A., R. D. Brewer, V. P. Fonseca, and T. S. Naimi. 2009. Binge drinking among US active-duty military personnel. American Journal of Preventive Medicine 36(3):208-217.
Stanley, M. 2003. College education and the midcentury GI bills. The Quarterly Journal of Economics 118(2):671-708.
SteelFisher, G. K., A. M. Zaslavsky, and R. J. Blendon. 2008. Health-related impact of deployment extensions on spouses of active duty army personnel. Military Medicine 173(3):221-229.
Stewart, W. F., J. A. Ricci, E. Chee, D. Morganstein, and R. Lipton. 2003. Lost productive time and cost due to common pain conditions in the US workforce. Journal of the American Medical Association 290(18):2443-2454.
Stiglitz, J., and L. Bilmes. 2008. The Three Trillion Dollar War. New York: W.W. Norton.
Stillion, J. 1996. Survivors of suicide. In Living with Grief Aftersudden Loss: Suicide, Homicide, Accident, Heart Attack, Stroke, edited by K. J. Doka. Washington, DC: Hospice Foundation of America. Pp. 41-51.
Sundin, J., N. T. Fear, A. Iversen, R. J. Rona, and S. Wessely. 2010. PTSD after deployment to Iraq: Conflicting rates, conflicting claims. Psychological Medicine 40(3):367-382.
Sutker, P. B., J. M. Davis, M. Uddo, and S. R. Ditta. 1995. Assessment of psychological distress in Persian Gulf troops: Ethnicity and gender comparisons. Journal of Personality Assessment 64(3):415-427.
Tanielian, T., and L. H. Jaycox. 2008. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Arlington, VA: RAND Corporation.
Tanik, O. 2005. Payday Lenders Target the Military: Evidence Lies in Industry’s Own Data. Center for Responsible Lending, Issue Paper No. 11. http://www.responsiblelending.org/payday-lending/research-analysis/payday-lenders-target-the-military.html (accessed October 10, 2009).
Teasdale, T. W., and A. W. Engberg. 2001. Suicide after traumatic brain injury: A population study. Journal of Neurology, Neurosurgery and Psychiatry 71(4):436-440.
Theeler, B. J., and J. C. Erickson. 2009. Mild head trauma and chronic headaches in returning US soldiers. Headache 49(4):529-534.
Thomson, B. A., and P. E. Nielsen. 2006. Women’s health care in Operation Iraqi Freedom: A survey of camps with Echelon I or II facilities. Military Medicine 171(3):216-219.
Tolin, D. F., and E. B. Foa. 2006. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin 132(6):959-992.
US Army Surgeon General. 2003. Operation Iraqi Freedom (OIF) Mental Health Advisory Team (MHAT) Report. Washington, DC: Department of the Army.
US Army Surgeon General. 2005. Operation Iraqi Freedom (OIF) Mental Health Advisory Team (MHAT-II) Report. Washington, DC: Department of the Army.
VA (Department of Veterans Affairs). 2005. VHA Directive 2005-024: Polytrauma Rehabilitation Centers. Washington, DC.
VA. 2009a. Overview of Homelessness. http://www1.va.gov/homeless/page.cfm?pg=1 (accessed January 11, 2009).
VA. 2009b. VHA Directive 2009-028: Polytrauma-Traumatic Brain Injury (TBI) System of Care. Washington, DC.
Vinokur, A. D., P. F. Pierce, and C. L. Buck. 1999. Work-family conflicts of women in the air force: Their influence on mental health and functioning. Journal of Organizational Behavior 20(6):865-878.
Vogt, D. S., D. W. King, L. A. King, V. W. Savarese, and M. K. Suvak. 2004. War-zone exposure and long-term general life adjustment among vietnam veterans: Findings from two perspectives. Journal of Applied Social Psychology 34(9):1797-1824.
Vormbrock, J. K. 1993. Attachment theory as applied to wartime and job-related marital separation. Psychological Bulletin 114(1):122-144.
Walker, A. E., H. K. Leuchs, H. Lechtape-Gruter, W. F. Caveness, and C. Kretschman. 1971. Life expectancy of head injured men with and without epilepsy. Archives of Neurology 24(2):95-100.
Washington, D. L., N. D. Harada, V. M. Villa, J. Damron-Rodriguez, S. Dhanani, H. Shon, and T. Makinodan. 2002. Racial variations in Department of Veterans Affairs ambulatory care use and unmet health care needs. Military Medicine 167(3):235-241.
Weichel, E. D., M. H. Colyer, C. Bautista, K. S. Bower, and L. M. French. 2009. Traumatic brain injury associated with combat ocular trauma. Journal of Head Trauma Rehabilitation 24(1):41-50.
Weina, S. U. 2006. Effects of pregnancy on the Army Physical Fitness Test. Military Medicine 171(6):534-537.
Weiss, G. H., W. F. Caveness, H. Einsiedel-Lechtape, and M. L. McNeel. 1982. Life expectancy and causes of death in a group of head-injured veterans of World War I. Archives of Neurology 39(12):741-743.
Westermeyer, J., J. Canive, P. Thuras, D. Chesness, and J. Thompson. 2002. Perceived barriers to VA mental health care among Upper Midwest American Indian veterans: Description and associations. Medical Care 40(1 Suppl):I62-I71.
WHO (World Health Organization). 2010. Depression. http://www.who.int/mental_health/management/depression/definition/en/ (accessed December 30, 2009).
Zatzick, D. F., C. R. Marmar, D. S. Weiss, W. S. Browner, T. J. Metzler, J. M. Golding, A. Stewart, W. E. Schlenger, and K. B. Wells. 1997a. Posttraumatic stress disorder and functioning and quality of life in a nationally representative sample of male Vietnam veterans. American Journal of Psychiatry 154:1690-1695.
Zatzick, D. F., D. S. Weiss, C. R. Marmar, K. Wells, T. Metzler, J. M. Golding, A. L. Stewart, W. E. Schlenger, and W. S. Browner. 1997b. Posttraumatic stress disorder and functioning and quality of life outcomes in female Vietnam veterans. Military Medicine 162:661-665.
Zeitzer, M. B., and J. M. Brooks. 2008. In the line of fire: Traumatic brain injury among Iraq War veterans. AAOHN Journal: Official Journal of the American Association of Occupational Health Nurses 56(8):347-353.
























































