5
Reducing the Burden of Cardiovascular Disease: Intervention Approaches
The preceding chapters have described the many interrelated risk factors that influence cardiovascular health, which involve aspects of economies and societies that extend far beyond public health and health systems. This underscores the complexity of any undertaking to promote cardiovascular health and to prevent and manage cardiovascular disease (CVD). In addition to being complex, CVD is also a long-term problem. It cannot be addressed through a singular, time-limited commitment but rather requires long-term interventions and sustainable solutions.
This chapter first outlines the ideal vision of a comprehensive approach to promote cardiovascular health and reduce the burden of cardiovascular disease. The chapter then turns to a more pragmatic and focused discussion, starting first with a description of the committee’s approach to the evidence. This is followed by a more thorough consideration of the rationale and evidence for components of the ideal approach, which include population-based approaches such as policies and communications campaigns; delivery of health care; and community-based programs. Recognizing the complexity of the disease and the local realities and practical constraints that exist in developing countries, the goal of this final section of the chapter is to identify, based on the totality of the available evidence, what is most advisable and feasible in the short term and what might hold promise as part of longer-term strategies.
IDEAL STRATEGY TO ADDRESS GLOBAL CVD IN THE DEVELOPING WORLD
The factors described in Chapters 2 and 3 that contribute to the burden of CVD and related chronic diseases are the targets for change in the quest to promote global cardiovascular health. These can be divided into behavioral factors (such as tobacco use, diet, and physical activity); biological factors (such as blood pressure, cholesterol, and blood glucose); psychosocial factors (such as depression, anxiety, acute and chronic life stressors, and lack of social support); health systems factors (such as access to care, screening, diagnosis, and quality of care); and intersectoral factors (such as tobacco control policies and agricultural policies). The evidence describing the interrelated determinants of CVD provides a strong conceptual basis for a strategy that coordinates across multiple sectors and integrates health promotion, prevention, and disease management as part of a long-term, comprehensive approach. This approach would employ multiple intervention strategies in a mix of programs and policies that accomodate variations in need according to context and locale.
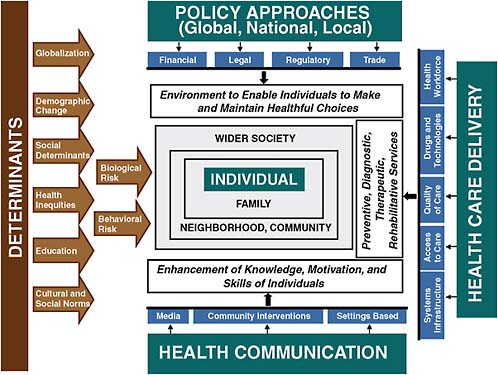
The ideal approach would take advantage of opportunities for intervention at all stages of the life course in order to promote cardiovascular health by preventing acquisition and augmentation of risk, detecting and reducing risk, managing CVD events, and preventing the progression of disease and recurrence of CVD events. Policies and programs to change the factors that contribute to CVD would be designed to work through population-wide approaches; through interventions within health systems; and through community-based programs with components in schools, worksites, and other community settings. A comprehensive strategy of this kind that takes into account the full range of complex determinants of CVD, illustrated in Figure 5.1, would have the theoretical potential to produce a synergistic interaction among approaches at individual and population levels. Concurrent modalities could include policy and regulatory changes, health promotion campaigns, innovative applications of communications technologies, efficient use of medical therapies and technologies, and integrated clinical programs. For individuals already at high risk or with existing disease, this approach would combine education, support, and incentives to both address behavioral risk factors and improve adherence to clinical interventions. Participation in this approach extends beyond clinical providers and public health approaches to also include public media outlets, community leaders, and related sectors, especially food and agriculture policy, transportation and urban planning, and private-sector entities such as the food and pharmaceutical industries. All these players are potential partners both in assessing needs and capacity and in developing and implementing solutions.
Such a comprehensive approach stands as an ideal for countries facing the burden of CVD and for global stakeholders in the fight against CVD and related chronic diseases. Reality, of course, complicates this ideal considerably. A comprehensive integrated approach of this kind has not been successfully implemented in a model that can be readily replicated in low and middle income country settings. Progress in high income countries points to models for many of the components that could make up such an ideal approach to CVD, but interventions that may be efficacious in certain settings cannot be assumed to be effective if they are implemented in settings that have significantly different available resources and differ significantly at the level of policy or population characteristics. Most of the intervention components described as part of the ideal approach do not have sufficient evidence to support scale-up for widespread implementation in low and middle income countries in the immediate term. Even with sufficient evidence to support implementation, many low and middle income country governments might not have adequate resources in place to undertake ambitious, comprehensive, full-scale approaches.
Nevertheless, although the components are likely to work best in synergy with each other, the lack of readiness and capacity to accomplish the comprehensive ideal is not reason to do nothing. An impact on the very high burden of CVD is possible even without doing everything that makes up the ideal. Indeed, developing countries will want to focus more pragmatically on efforts that promise to be economically feasible, have the highest likelihood of intervention success, and have the largest morbidity impact. The goal of this chapter is to provide an analysis to help determine (1) what policies, programs, and clinical interventions have sufficient evidence for priority implementation in developing countries in the near term and (2) what approaches have a solid conceptual basis but require greater knowledge based on specific policies and programs with demonstrated effectiveness and implementability in developing-country settings in order to make progress toward implementation in the medium and long term. Chapter 7 will continue the discussion of feasibility and prioritizing the use of limited resources in low and middle income countries with a synthesis of the available economic evidence and future economic research needs for the intervention approaches described in this chapter.
Building a Strategy to Address CVD
The following briefly outlines the series of components needed for countries and supporting global stakeholders to build a strategy to promote cardiovascular health. As described above, these components would ideally be integrated to work toward a comprehensive intervention strategy. The intent is to develop a supportive policy environment and build the capac-
ity to develop, implement, and evaluate intervention programs, with the ultimate goal of reducing the burden of CVD through reduction of risk factors and management of disease. This includes “top-down” policies and complementary “bottom-up” approaches in health care delivery systems and in community-based education and health promotion programs. The specific components within each of these steps and examples of the available evidence to support their implementation are described later in the chapter, along with more discussion of the limitations, taking into account gaps in the evidence and variations among countries in baseline capacity, economic status, and level of infrastructure.
Needs and Capacity Assessment
A crucial basis for developing policies and programs is for governments and communities to estimate and, where possible, measure the nature of the problem as it occurs in the local context where approaches will be implemented; to assess the needs of the population; to catalog current efforts; to assess the available capacity and infrastructure to address CVD and related chronic diseases; and to gauge the political will to support the available opportunities for action. This assessment will inform priorities and determine choices about the implementation of evidence-based policies and programs as well as capacity-building efforts. This should lead to specific and realistic goals for intervention strategies that are adapted to local baseline capacity and burden of disease and that also aim to improve that baseline capacity. This critical underlying step was discussed in full in Chapter 4.
Country-level measurement, assessment, and prioritization of this kind can occur at the level of national or local governments, such as provincial or city-level health authorities. In many low and middle income countries, this will require the development of sufficient capacity and infrastructure to carry out population-based approaches for measuring cause-specific mortality and behavioral and biological risk factors. In countries with very limited capacity at baseline, at first it may be nongovernmental organizations, foreign assistance agencies, and other donors who need to carry out a needs assessment and prioritization before implementing programmatic efforts. Regardless of the driving force behind the initiated action, this strategic planning can, to the extent possible, involve local authorities, be harmonized with local efforts, and be designed as an opportunity to improve local baseline capacity over time.
Policy Strategies
When a baseline is established and priorities are determined based on country-level data, the starting place for developing intervention ap-
proaches is policy strategies for population-based prevention. The primary population approach can be based on setting or changing policies, incentives, and regulations, especially those related to food, agriculture, and tobacco. There is evidence to support the implementation of some of these policies in the immediate term. For those developing countries where there exist democratic means to develop policies, where regulatory and enforcement capacity is sufficient, these policy changes may include, for example, taxation and regulations on tobacco production and sales; regulations on tobacco and food marketing and labeling; alterations in subsidies for foods and other food and agricultural policies; and strategies to make rapid urbanization more conducive to health. Regulatory change usually needs to be incremental and should be proportional to the possible impact and cost.
Health Communications
Both in coordination with policy changes and as a separate strategy for affecting crucial CVD-related behaviors, there is substantial promise in implementing health communications and education efforts. Public communication interventions that are coordinated with select policy changes can enhance the effectiveness of both approaches, which together can help create an environment in which more targeted programs in health systems and communities can succeed. Even in the absence of an ideal policy environment, well-constructed stand-alone population-level health communication efforts have the potential to be effective in encouraging population behavior change, for example, in areas such as smoking initiation and salt and fat consumption. Depending on the governmental infrastructure within a country, policies with coordinated communication and health education efforts can occur at the level of national or local authorities.
Delivery of Quality Health Care
Along with select population-based approaches, a key step in addressing CVD is to strengthen health systems to deliver high-quality, responsive care for the prevention and management of CVD. Improving health care delivery includes, for example, provider-level strategies, financing, integration of care, workforce development, and access to essential medical products. The need to strengthen health systems in low and middle income countries is not specific to CVD, and it is important that ongoing efforts in this area take into account not only traditional focus areas such as infectious disease and maternal and child health but also CVD and related chronic diseases as well as chronic care needs that are shared among chronic non-infectious diseases and chronic infections such as HIV/AIDS and tuberculosis (TB).
Community-Based Programs
Along with efforts to implement population-based approaches and to strengthen health systems, an ideal comprehensive integrated approach would also include community-based programs that offer opportunities to access individuals where they already gather, such as schools, worksites, and other community organizations. Depending on local priorities, there is potential for synergism in both effectiveness and economic feasibility through coordinated interventions that target multiple risk factors, are conducted in multiple settings in communities, and coordinate the health systems and population-based strategies described above with related, community-specific strategies. Because of the lack of community-based models that have been successfully implemented, evaluated, and sustained in low and middle income country settings, the critical next step in these settings is to support research to develop and evaluate demonstration projects through implementation trials. In many cases, the focus can be on adapting and evaluating programs with demonstrated success in developed countries. The design of demonstration programs will need to take into account local infrastructure and capacity to develop and maintain such programs over time, particularly if they are ultimately intended to affect a large portion of the population and operate on a large scale.
Scale-Up and Dissemination
The ultimate goal when intervention approaches in all these domains are demonstrated to be effective and feasible is scale-up, maintenance, and dissemination. In addition to implementing best practices and evidence-based policies and programs on a larger scale, this includes disseminating in a broader global context, by sharing knowledge among similar countries with analogous epidemiological characteristics, capacity, and cultural norms and expectations.
Ongoing Monitoring, Evaluation, and Assessment
As described in Chapter 4, ongoing surveillance and evaluation of implemented strategies will allow policy makers and other stakeholders to determine if implemented actions are having the intended effect and meeting the defined goals, and to reassess needs, capacity, and priorities over time. This will be critical to alter policies and programs as priorities change, as new lessons are learned, and as a country goes through inevitable transitions in its economy and its health or social environments.
Global Support
As described in more detail in Chapter 8, international agencies can play an important role in working toward comprehensive country-level approaches. These agencies can help initiate and enrich any country’s CVD prevention and management process through direct financial and technical assistance. In addition, external aid and coordination can facilitate the transfer of lessons learned among countries, allowing each country to actively contribute to the international repertoire of prevention strategies.
APPROACH TO THE EVIDENCE
This chapter is concerned with what works. The challenge is to define what qualifies as an intervention that works, to martial these findings together to establish a coherent evidence base, and then to use this as the basis to necessarily prioritize approaches. This section of the chapter briefly discusses the committee’s approach to considering evidence for evaluating intervention approaches for CVD at all levels. This includes how the methodology for evaluating large-scale programs and population-based and policy interventions differs from clinical interventions and small-scale projects as well as a special emphasis on the importance of effectiveness and implementation evidence in relevant contexts.
The attempt to define a broad-based set of effective approaches available for CVD promotion and prevention rests on data standards—notably data standards that continue to evolve. The aspirational standard is evidence that describes causal linkages between intervention and better health status (i.e., outcomes). These data should meet the additional standards of contextual generalizability so that the reported findings are feasible based on implementation evidence and economic evaluation and adaptable in a variety of settings.
The intent is that good epidemiologic observational data on the role of risk factors and the preventive effects of reductions in those risk factors will lead to hypotheses about causal pathways that interventions are designed to influence. Ideally, these hypotheses will be confirmed by prospective interventional studies that are repeated and reaffirmed in a variety of settings. Evidence from randomized trials can be highly valuable to infer causality. As a rigid evidence standard, however, this is not always available, feasible, necessary, or even optimal. For many intervention approaches, the best available evidence can also come from, for example, cohort evaluations and qualitative assessments as well as other research methodologies that support plausible causal linkages. For policy and public health approaches in particular, traditionally defined rigorous evaluation standards are often unrealistic, and it is instead a comprehensive perspective on the totality of
the available evidence that is weighed alongside other policy pressures to drive implementation decisions. Therefore, the committee did not apply randomization as a standard of evidence for consideration of the illustrative examples included in this chapter. However, the committee did restrict its review of the evidence to published studies that included some comparison condition, either through a control group or a comparison to before and after an intervention was implemented.
The second standard for evidence set out by the committee is one of relevancy, an issue of particular importance here, although it is by no means exclusive to low and middle income countries. Conceptually, the ideal is not narrowly defined evaluations focused on internal validity but instead evaluations that look beyond efficacy—the estimation of what is possible—to effectiveness—the determination of what actually was accomplished by an intervention in a real-world setting. This refers to what is often a tension between confident findings of causal influence and confident findings of the relevance of evidence. Studies imposing enough controls on the context to support strong causal statements often in the process have to create a context that is distant from the messy environment and constraints in which programs at scale will be implemented, particularly in low and middle income countries. This review of evidence by the committee respects that tension, and then puts substantial emphasis on relevance.
Beyond effectiveness and relevance, the ultimate ideal standard to inform large investments in programs and intervention approaches is evidence from implementation research, operations research, and health services research. In addition, evidence on economic feasibility is a critical factor in determining implementation readiness and prioritizing intervention approaches. The available evidence from economic evaluations of intervention approaches is the subject of Chapter 7.
Applying the standards described here to the available evidence for CVD in developing countries revealed significant gaps in the evidence base, especially given the desire to have a concrete basis for advocating policy change, system change, or program implementation. The committee, however, does not intend that the message about higher data mandates with a responsible exposure of these data gaps be equated with a suggestion of inaction. A principle throughout the report is one of being action-oriented based on available findings. The committee’s review of the available evidence according to these standards informed an analysis of which potential components of the ideal comprehensive approach warrant priority for implementation or, if near-term implementation is not supported, which components warrant other intermediate steps to develop the evidence base in support of implementation in the longer-term.
Given the broad and global scope of this study, a comprehensive systematic review of all available evidence related to every aspect of CVD and
related chronic diseases was not within the scope of this project. Nor was it feasible for this report to catalog every intervention approach that has been attempted and documented across all countries. Instead, to present the rationale put forth by the committee, the following sections include illustrative examples that represent the best available evidence to support the committee’s findings on the implementation potential for component strategies. In order to limit the length of this document and to avoid replication of existing work, the committee sought existing relevant, high-quality, systematic and narrative reviews. In content areas where these were available, this chapter includes summaries of key findings, but otherwise refers the reader to the available resources for more detailed information.
The focus is on intervention approaches for CVD with evidence for effectiveness and implementation in developing countries. Where this evidence is limited, generalizable examples are offered with evidence for effectiveness and implementation from both CVD-specific approaches in developed countries and developing-country evidence for non-CVD health outcomes. An assessment of the transferability of the evidence for these approaches is included. For components where there is limited or no effectiveness or implementation data, the logical basis for intervention approaches is discussed as being derived from knowledge about the determinants of CVD, modifiable risk factors, and characteristics of ideal intervention design and implementation.
Conclusion 5.1: Context matters for the planning and implementation of approaches to prevent and manage CVD, and it also influences the effectiveness of these approaches. While there are common needs and priorities across various settings, each site has its own specific needs that require evaluation. Additional knowledge needs to be generated not only about effective interventions but also about how to implement these interventions in settings where resources of all types are scarce; where priorities remain fixed on other health and development agendas; and where there might be cultural and other variations that affect the effectiveness of intervention approaches. Translational and implementation research will be particularly critical to develop and evaluate interventions in the settings in which they are intended to be implemented.
COMPONENTS OF A STRATEGY TO REDUCE THE BURDEN OF CVD
This section presents in more detail the rationale for the ideal approach described previously and the evidence for the main components, which include population-based approaches such as policies and health
communications campaigns; delivery of health care; and community-based programs. Recognizing the complexity of the disease and the local realities and practical constraints that exist in developing countries, the goal of this final section of the chapter is to identify, based on the totality of the available evidence, policies, programs, and strategies to improve clinical care that have sufficient evidence for advisable and feasible implementation in developing countries in the near term as well as approaches that have a solid conceptual basis but need more evidence for specific policies and programs with demonstrated effectiveness and implementability in developing country settings to progress toward implementation in the medium and long term.
Intersectoral Policy Approaches1
Chapter 2 described the complexity of the determinants of CVD, which are drawn from a range of broad social and environmental influences. As a result, many of the crucial actions that are needed to support the reduction of CVD burden are not under the direct control of health ministries, but rather include other governmental agencies as well as private-sector entities. For example, they rely on tax rates on tobacco set by economic agencies, food subsidy policies set at agricultural agencies, access rules for public service advertising set by communication agencies, curricular choices by education agencies, and commitments to product reformulation by multinational corporations. Thus, success in achieving the specific priority goals for CVD programs will rely heavily on decisions made outside of health agencies, and that success will only come if there is substantial intersectoral collaboration.
The specifics of how that collaboration will come about will vary with the particular political arrangements in a country, but there will be a common theme: success will depend on building a shared commitment across sectors in the whole of government. This will require engaging not only those already motivated by health-related goals but also those who have very different pressures and considerations driving their decision making. Therefore, it is important to acknowledge the different forces that drive policy decisions in different sectors in order to seek out shared objectives, including economic objectives. To this end, there will be a need not only to make a case that the population as a whole will benefit from addressing CVD, but also to make the specific case that work to target CVD-related behaviors and outcomes will be in the interest of each collaborating agency or stakeholder in the private sector. For example, it may not be enough to
talk up health benefits to encourage increased taxation on tobacco; evidence bearing on the likely gains and losses in revenues associated with such increased taxation and reduced tobacco consumption may have higher priority. To this end, a pragmatic approach will require a realistic assessment of what the fundamental requirements are for CVD-related needs, and what aspects of a proposed policy might be negotiable.
Intersectoral policy approaches for CVD will not be simple to implement, and a central part of intervention will be to form a strategy to stimulate such actions. In addition, just as with all interventions, policies need to be context specific and culturally relevant, and need to take into account infrastructure capacity and economic realities. A review commissioned for this committee identified the key success factors for implementing intersectoral approaches (Jean and St-Pierre, 2009). These include elements related to context, including political will and support; a favorable legislative, economic and organizational environment; and community support. There also needs to be a well-defined problem targeting an issue that is widely significant with a clear rationale for intersectoral action. Planning is also an important aspect of intersectoral approaches and requires credible organizers, as well as carefully chosen partners with a shared vision, clearly defined roles and responsibilities, and sufficient authority. It is also crucial to have evaluation based on concrete and measurable objectives. The final key success factor is a system for adequate communication, flexible and adaptable decision making, and conflict resolution.
The following sections present a more detailed discussion of the policy levers that have the most potential to affect the future course of CVD within an intersectoral approach by addressing specific goals, including tobacco control, reduced consumption of salt and unhealthful food, and increased physical activity. The rationale for these policy approaches are described, along with precedent for implementation. The focus is on examples from low and middle income countries when possible. Evaluations of policy interventions are not common, especially in low and middle income country settings, but where an evaluation has generated evidence on policy this is presented as well.
Tobacco Control Policies
Tobacco control, including efforts to reduce both tobacco use and exposure to secondhand smoke, is one of the most well-developed areas of CVD-related policy. Strategies for tobacco control in high income countries have been reviewed extensively elsewhere and will not be repeated here (Breslow and Johnson, 1993; Frieden and Bloomberg, 2007; IOM, 2010; Jha et al., 2006). This precedent in high income countries provides a strong
rationale for policy measures of this type in low and middle countries with adequate regulatory and enforcement capacity.
Indeed, strategies for tobacco control worldwide were laid out exhaustively as part of the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) (WHO, 2008b). The FCTC emphasizes the importance of both demand reduction and supply control strategies, including taxation measures on tobacco products, protection from exposure to tobacco smoke, packaging and labeling of tobacco products to include health warnings and to ban misleading terms like “light” and “mild,” education and public awareness campaigns, controls on tobacco advertising, tobacco cessation services, control of illicit trade in tobacco products, control of sales to minors, and provision of support for economically viable alternative economic activities. WHO has also presented a policy package for tobacco control to support implementation of the FCTC (WHO, 2008b). Known as the MPOWER package, the focus is on six key policy areas: monitor tobacco use, protect people from tobacco smoke, offer help to quit tobacco use, warn about the dangers of tobacco, enforce bans on tobacco advertising and promotion, and raise taxes on tobacco products.
However, although many low and middle income countries have signed the FCTC treaty, implementation has been achieved in only a limited number (Bump et al., 2009). Indeed, there are only a few well-documented examples of implementation of tobacco control policies in low and middle income countries to serve as models, including Bangladesh, Brazil, Poland, Thailand, and South Africa (de Beyer and Brigden, 2003). Therefore, evaluation strategies are needed to examine the effects of tobacco control policies in low and middle income settings, and there is a need for more knowledge and analysis of the barriers to successful implementation and how to overcome them (Bump et al., 2009).
In Bangladesh, systematic and concerted efforts by nongovernmental organizations (NGOs) provide a model of very low-budget advocacy (Efroymson and Ahmed, 2003). Similarly, in Thailand tobacco control policy has been significantly influenced by NGOs in the health sector with direct access to government officials (Vateesatokit, 2003). In Brazil, by contrast, persistent action led from within the government resulted in strong legislation and a nationwide, decentralized program, with training and support cascading down the levels of government (da Costa and Goldfarb, 2003). In South Africa, political and social change created new environments and policy windows that public health advocates were able to turn to their advantage. Comprehensive legislation was enacted in two steps, with a second law strengthening the first. Legislative efforts began with policies to inform consumers and to restrict smoking and advertising. Later, tax increases were put in place and helped reduce consumption. The availabil-
ity of strong local evidence, especially on the economic implications of tax increases, was very important in this case (Malan and Leaver, 2003).
Food and Agriculture Policies
Policies related to dietary changes can be thought of in terms of an integrated food system that goes from “farm to fork.” This system includes food production, food processing, supply chain including food delivery and food availability, food marketing, and food choices both at point of purchase and in individual dietary choices. This system can be influenced by a variety of policies and initiatives in the agriculture sector, the public health sector, and the private sector. By facilitating greater consumption of specific foods, which often replace more healthful traditional foods, changes in agricultural production and policy can be linked with the “nutrition transition,” much of which contributes to rising levels of CVD (Hawkes, 2006). Therefore, it is reasonable to conclude that there is potential for cardiovascular health to be promoted by finding economically feasible ways to globalize agricultural and food policies that promote more healthful food production and make more healthful foods affordable to developing country populations, including the poor.
In the past 25 years, agricultural production has increased for all major food groups around the world; however, the rate of increase has been markedly steeper for some foods associated with CVD and other diet-related chronic diseases. One example is Latin America—a major producer of vegetable oils, meat, fish, sugar, and fruit. As part of globalization, agricultural policy in the region shifted in the early 1990s from production to market-led policies. The food-consuming industries (distributors, manufacturers, processors, and retailers) played a key role in this shift. Case studies from Brazil, Colombia, and Chile show that these changes in agricultural policy are linked to changing consumption patterns. In Brazil the government instituted a series of market-led reforms in the early 1990s, which opened up the soybean oil market and encouraged production and enabled greater consumption in export markets (Hawkes, 2006). After investments in technology and infrastructure and trade liberalization during the 1980s in Colombia, the government implemented a market liberalization program, called “Apertura,” which eased imports on feed ingredients and reduced import duties in the early 1990s (Hawkes, 2006). In line with the market-led paradigm, the government in Chile deregulated agricultural policy, privatized land ownership, cut labor costs by dismantling organized activity, provided more favorable conditions for foreign investment, and liberalized trade. These actions increased foreign investment in the fruit industry and were strengthened in the mid-1980s, with the provision of tax incentives to boost exports, increased investment in export-oriented
agriculture, and more provisions to further increase foreign investment (Hawkes, 2006).
Agriculture is also a heavily traded sector, and trade policies affect what food is available within a country and its trading partners. The United States and Europe are major food exporters, and the composition of food available in their developing-country trading partners shows the influence of agricultural subsidies for animal-based products and coarse grains that provide animal feed. A recent study illustrates this by examining the increase in agricultural trade between the United States and Central America, following a new trade pact in 2004. The analysis suggests that “food availability change associated with trade liberalization, in conjunction with social and demographic changes, has helped to facilitate dietary change in Central American countries towards increased consumption of meat, dairy products, processed foods and temperate (imported) fruits. Such dietary patterns have been associated with the nutrition transition and the growing burden of obesity and non-communicable disease reported in the region” (Thow and Hawkes, 2009). The World Trade Organization (WTO) has recognized health consequences as a legitimate concern for trade policy in relation to access to essential drugs. This suggests that countries should have deliberate policies in relation to the health implications of their international trade. However, the WTO has to date not allowed countries to impose trade barriers against unhealthy foods (Clarke and McKenzie, 2007; Evans et al., 2001).
It is also important to note that agricultural trade will not necessarily worsen diets in developing countries. Diets can also be improved by trade through greater dietary diversification, greater food availability, lower consumer prices, and increases in domestic food production spurred by export demand.
In addition to the effects of agricultural production and trade, specific agriculture and food policies can also be linked to changes in food consumption related to CVD risks. For instance, as part of a broader set of chronic disease prevention approaches in Mauritius, the government implemented policies to change the composition of cooking oil made available to the population by limiting the content of palm oil. After 5 years, there were significant decreases in mean population cholesterol levels (Dowse et al., 1995; Uusitalo et al., 1996). Although this was a promising effect, it is important to note the mixed effects of the broader integrated intervention approach, which is described in more detail later in this chapter. In fact, obesity rose during the same time period and there were no other effects on CVD risk factors, indicating that the overall intervention approach was not sufficient to overcome secular trends (Hodge et al., 1996). Therefore, the Mauritius experience serves as an example of how a middle income country can mobilize governmental policies to achieve future health improvement,
but it cannot be used to define the specific tactics that are needed to achieve success, especially without comparison communities (or regions) to control for secular changes. In addition, the specific circumstances of policy implementation and enforcement in a small island nation like Mauritius may not be widely generalizable.
In Poland, changes in economic policy led to reductions in subsidies for animal fat products, and consumption patterns changed, characterized by decreasing amounts of saturated fat and increasing amounts of polyunsaturated fat intake. This was associated with rapid declines in coronary heart disease (CHD) mortality during the same time period (Zatonski and Willett, 2005; Zatonski et al., 1998). However, this is evidence from an unplanned natural experiment using retrospective data, which offers limited lessons on strategic approaches that could be duplicated in other settings. Indeed, in Hungary, Romania, and Bulgaria (neighboring countries with similar political and economic changes) there was little apparent decline in ischemic heart disease mortality.
There is also a history in developing countries of price-based policies to influence nutrition outcomes for their populations—primarily basic food subsidies to reduce undernutrition (Pinstrup-Andersen, 1998). Health goals beyond alleviating undernutrition have not always been a consideration in establishing those policies. Analyses of oil price policies in China (Ng et al., 2008) and staple commodity subsidies in Egypt (Asfaw, 2006) suggest that price policies can influence food choices, in these examples with a negative effect on CVD risk. The consumption of edible oils in China has increased substantially with recent drops in edible oil prices stemming from changes in trade patterns (with especially strong effects on the poor) (Ng et al., 2008). In Egypt, the government subsidizes energy-dense foods, and female body mass index (BMI) appears to be influenced by the availability of those subsidized foods, even as the cost of a high-quality diet is out of reach for many in the population (Asfaw, 2006). This analysis does not establish a causal relationship, but it does suggest that government food price policies are influential and that this potential for price policies to adjust consumer demand for specific food ingredients could be considered as a means to promote consumption of healthier foods. The theoretical argument in support of subsidizing healthy foods responds to the problem of food pricing in which healthier foods (fresh fruits and vegetables) are relatively expensive, and energy-dense foods (sugared and heavily processed) are relatively cheap (Drewnowski, 2004). Preliminary research suggests that a “thin subsidy” to lower the price of healthy foods in the United States would be a cost-effective intervention for CHD and stroke (Cash et al., 2005).
The evidence is not yet available as to the effectiveness of the reverse policy—taxing unhealthy food products. Because tobacco taxation has been a very effective and cost-effective policy tool for reducing CVD risk in a
broad range of countries, taxation of other products has been discussed (Brownell and Frieden, 2009) and even tried out on a limited basis in high-income countries. However, there is insufficient evidence on the effectiveness and health impact of this approach (Thow et al., 2010). In addition, for either of these potential price-based policy approaches it should be noted that changing the price of any one category of food or beverage may have impacts on consumption of other categories, which could be for the better or worse of heart health.
There is precedent for strategies to reduce salt in the food supply and in consumption that have been reviewed and documented extensively elsewhere (He and MacGregor, 2009). Salt-reduction strategies in high income countries include public health campaigns to increase consumer awareness of healthy salt intake and to encourage decreased consumption, product labeling legislation, and salt reduction by the food industry (He and MacGregor, 2009). These strategies have the potential to be adapted both to low and middle income country efforts as well as to be scaled up for broader, coordinated global efforts (He and MacGregor, 2009). However, evidence on salt-reduction strategies comes mostly from high income countries, where the majority of salt (80 percent) comes from processed foods (He and MacGregor, 2009; James et al., 1987). Therefore, it is important to note that in many low and middle income countries, even with increasing consumption of processed foods, most of the salt consumed is either added during cooking or in sauces (WHO Forum on Reducing Salt Intake in Populations, 2006). As a result, enhancements to prior policy strategies may be needed when adapting to this context, such as a public health campaign or other efforts to encourage consumers to use less salt. Similarly, precedent for reductions in transfat through policy initiatives, such as the experience in New York City (Angell et al., 2009), offers promise for potential adaptation to a wide range of settings. However, to adapt policy strategies related to the food supply, consideration must be given to the much greater representation of unregulated, informal food sales in most developing countries.
Environmental Policies
There are environmental consequences associated with some of the major CVD drivers that offer an opportunity for shared objectives with the environmental policy sector. Urbanization and increasing air pollution as well as changing global dietary patterns and changing agricultural trends, most notably the rapid increase in meat and palm oil consumption, have implications for CVD risk and also have a significant and often negative impact on the environment (Brown et al., 2005; Langrish et al., 2008; vonBrown et al., 2005; Langrish et al., 2008; vonvon Schirnding and Yach, 2002; Yach and Beaglehole, 2004).
Agriculture and food production in general is a resource-intensive endeavor, and significant portions of the global workforce, land area, water supply, and energy resources are dedicated to it (Schaffnit-Chatterjee, 2009). Meat and dairy production is particularly resource-intensive. Animal-sourced food requires significantly more energy, water, and land use to produce than do basic crops such as legumes, grain, fruits, and vegetables (Popkin, 2003; Steinfield et al., 2006). Indeed, it is estimated that the livestock sector is responsible for more than 8 percent of global human water use and accounts for 70 percent of all agricultural land (30 percent of Earth’s land surface) (Steinfeld et al., 2006).
Livestock production also erodes topsoil, causes land degradation, pollutes water, and threatens biodiversity. Livestock compact the soil and degrade the land, disrupting the water supply, contributing to erosion and necessitating expansion into new grazing lands. These are often created through deforestation, which destroys the habitat of other animals, threatening biodiversity. The livestock sector is also responsible for an estimated 18 percent of greenhouse gas emissions (a higher share than the transport sector)—a result of poor manure management and methane gas emissions from ruminant species such as cattle, sheep, and goats. Furthermore, manure, fertilizers used for growing feed crops, and waste materials from livestock processing are often dumped into waterways without proper treatment, polluting the water supply (Steinfeld et al., 2006).
The rapid rise in palm oil consumption in some low and middle income countries has also had a significant negative impact on the environment and has strained fragile natural ecosystems. In 2001, Malaysia and Indonesia produced 83 percent of the world’s palm oil and were responsible for 89 percent of global palm oil exports. Hundreds of thousands of square miles of rainforest have been cut or burned down to accommodate the growing industry. Palm oil production has also indirectly contributed to further deforestation by displacing local farmers, leading them to expropriate additional rainforest as new land for their subsistence farming. These rainforests are the only habitats for a number of critically endangered species such as the orangutan, the Sumatran tiger, and the Sumatran rhinoceros. Some zoologists believe these species will be pushed into extinction if rainforest destruction continues at its current pace (Brown and Jacobson, 2005; Gooch, 2009).
In addition to contributing to deforestation, palm oil production also contributes to soil and water pollution. As with other crops, extensive use of fertilizers and pesticides on oil palm plantations has led to pollution in the soil and waterways. Additional pollution is caused by oil palm processing, which creates effluent that ends up in rivers and waterways. Indeed, in some Indonesian rivers, pollution from palm oil mill effluent is so severe that fish cannot survive. In the past 6 years, the industry has tried to set
standards to ensure that palm oil production is sustainable; however, rainforests continue to be destroyed and effluent continues to be improperly dumped into waterways. While the production of some other oil crops leads to water pollution and rainforest destruction (for example, parts of the Brazilian Amazon are now being cut down to make way for soybean production), the exponential increase in palm oil use combined with the projected future rise in global demand make it a particularly glaring example of potential long-term harmful environmental effects (Brown and Jacobson, 2005; Gooch, 2009).
This opens a door for shared approaches between those trying to promote cardiovascular health and those trying to promote environmentally sustainable development. These shared approaches may include policies to limit overproduction of palm oil production and to encourage shifts in agricultural production from meat and dairy to more fruits and vegetables. Tobacco production, processing, and consumption have also been associated with negative environmental consequences (Bump et al., 2009). This provides an additional rationale for synergistic efforts to overcome the technical, political, and commercial barriers to implementing policy changes in the food and agriculture sectors that both promote health and protect the environment.
Urban Planning Policies and the Built Environment
A broad range of structural factors comprise the “built environment,” and many of these factors contribute to health outcomes. They encompass factors such as chemical, physical, and biological agents, as well as physical and social environments, including housing, urban planning, transport, industry, and agriculture (Papas et al., 2007). Thus urbanization is another area for potential synergy between promoting environmentally sustainable development and promoting cardiovascular health.
As described in Chapter 3, trends show that the changes in the built environment due to urbanization are generally associated with several risk factors for CVD, including an increase in tobacco use, obesity, and some aspects of an unhealthful diet, as well as a decline in physical activity and increased exposure to air pollution (Brook, 2008; Gajalakshmi et al., 2003; Goyal and Yusuf, 2006; Langrish et al., 2008; Ng et al., 2009; Steyn et al., 2006; Yang et al., 2008; Yusuf et al., 2001).
Motivated by the growing prevalence of obesity in many developed nations and the potential public health impacts stemming from subsequent CVD and diabetes, studies conducted within the United States, Europe, Australia, and New Zealand over the past three decades have successfully demonstrated the correlation between different aspects of the built environment and physical activity levels (Humpel et al., 2002). These correla-
tions provide a compelling rationale, and reports such as the U.S. Centers for Disease Control and Prevention’s Community Guide and the Institute of Medicine’s Local Government Actions to Prevent Childhood Obesity (2009) have produced guidance for different types of policy initiatives at several levels of jurisdiction, including changes to the built environment.
However, there is a lack of prospective studies investigating the effect of introducing changes to the built environment on individual and population health. These prospective data are much needed as the current cross-sectional analyses have limited ability to demonstrate causality. For example, it is difficult to ascertan if built environments that are more conducive to healthy lifestyles lead to increased physical activity, or whether individuals who are more physically active are more likely to live in a neighborhood that is more conducive to walking, bicycling, or playing sports. It is difficult to obtain prospective data, as there are a wide variety of exogenous variables to interfere with potential findings. In addition, these studies would require a significant financial investment, either on the part of the research funding institution or the local community (Sallis et al., 2009). There has also been little economic analysis of the potential costs associated with modifying an element of the built environment, which could be a barrier in developing countries.
In addition, it is important to note that the majority of data on the correlation of environments and increased physical activity comes from high income countries. With the exception of some work in Latin America described below, there is a lack of evidence from a range of developing country settings, and most guidance documents do not address generalizability or adaptation to low and middle income country settings. While there may be some commonalities between individuals from both urban and rural regions of the developed and developing world, differences in social norms, culture, existing built environment, and local variations in baseline daily activity levels are likely to have a substantial impact on the potential effectiveness of a change in the built environment in leading to behavior change.
On the other hand, low and middle income countries undergoing rapid development and urbanization provide promising opportunities to help fill the evidence gap through future prospective research given the multitude of neighborhoods and cities in the early stages of land use development. The need for investment of resources in this research may be lessened in settings where the intervention is not an alteration of an existing environment but rather an element of design planning where investment has already been committed to future urbanization projects. In fact, prospective studies in the context of planned urbanization in rapidly developing countries could also provide better evidence on the monetary investments required to achieve “successful” future urban design.
A few public health initiatives in middle income countries in Latin America, such as Muévete in Bogota and Agita São Paulo in Brazil, have altered the local built environment as a component of an overall program, but evaluations of their results are limited (Gamez et al., 2006; Matsudo, 2002). The Agita program in Brazil is one of the few programs with an evaluation that uses health outcomes. This was a multicomponent program that included changes in the environment through an increase in the number of walking areas, facilities for bicycling, and recreational facilities. Changes related to the practice of physical activity during the intervention period were observed. An annual survey showed that over 5 years there was a decrease from 14.9 percent to 11.2 percent in the population defined as inactive, a decrease from 30.3 percent to 27 percent in the population deemed irregularly active, and an increase from 54.8 percent to 61.8 percent in the population considered active or very active. Changes were also observed in targeted groups, such as groups of patients suffering from hypertension or diabetes and patients and workers in hospitals and health centers (Matsudo et al., 2006).
In summary, there is limited evidence of the effects on CVD-related outcomes of strategies and investments to alter the existing built environment, and urban planning policies are likely not a CVD priority in many low and middle income countries. However, for policy makers in countries undergoing rapid urbanization, there is a strong evidence-based rationale to take advantage of the opportunity going forward to implement and evaluate strategies to encourage cardiovascular health by making cities walkable, cyclable, safer, and free of air pollution. A more “heart-healthy” approach to growth and urbanization provides opportunities to avoid negative impacts, and possibly to even use the growing investment in new city development for health gains, including CVD prevention and health promotion.
Health Communication Programs
Health communication programs are typically designed to reach a large audience with messages as part of their established exposure to communication sources such as radio, television, billboards, newspapers and other printed material including mass mailings, and the Internet. Such exposure is often passive, relying on routinely accessed sources, rather than requiring the motivation of actively seeking a new communication source by an individual. Communication programs may affect behavior through three paths: (1) by directly educating and persuading individuals to change their behavior (e.g., by changing people’s minds and providing skills needed to quit smoking); (2) by changing the expectations of peers in social networks, which in turn influence individual behavior (e.g., by changing friends’ willingness to condemn smoking); and (3) by changing public opinion to
influence public policy, which then influences individual behavior (e.g., by changing the political climate to permit regulation of secondhand smoke and thus reducing opportunities for individuals to smoke).
The effectiveness of policies and programs can be enhanced if linked to health communication programs targeted to the same objective—for example, to complement lobbying of policy authorities and food manufacturers to restrict salt content with public education about salt reduction. In addition, linking communication programs to policy approaches can make them more likely to gain presence in the public mind and thus gain public support. A communication program may also be designed to precede the policy change to nurture the public support needed for legislative action. Health communication strategies can also be an important complementary component of health systems and community-based approaches. Depending on the infrastructure within a country, communication and health education efforts can occur at multiple levels, from the national government to local authorities and community-based organizations.
The following section describes the evidence and considerations for designing and implementing communication campaigns at scale under the kinds of conditions that would be expected in real-world public health systems rather than research programs. An analysis of the current literature, described in more detail below, indicates that what might be most feasible for short-term implementation, and for coordination with policy approaches, is a focus on reasonably narrowly defined CVD-related targets, rather than trying to change all determinants of CVD at once. This focus can be most effective when using multiple intervention approaches to achieve the same ends, with large-scale communication programs as one important component.
CVD-Related Communication Campaigns in Low and Middle Income Countries
There is currently very limited evidence about the effects of communication interventions on CVD-related behaviors (or morbidity) in low and middle income countries, with few reported examples of communication programs with rigorous evaluations. The evidence is also challenging to interpret because large-scale communication programs tend to be components of multifaceted programs. Even when such multifaceted programs are evaluated, the effects of separate components are difficult to distinguish. In addition, in many reported evaluations no control condition is present, and as a result the effects of secular change can be difficult to discriminate from the effects of intervention efforts.
There are descriptive reports about some programs implemented in middle income countries that incorporate communication elements (Grabowsky
et al., 1997). Some of these reports, described below, describe an evaluation and infer effects on CVD-related outcomes, but in some cases these effects are weakly supported, with little evidence of sustained impact.
The Coronary Risk Factor Study (CORIS), conducted in South Africa from 1979 to 1983, was a multilevel, multifactor intervention in which most of its effects were explained by use of a mass media campaign (Rossouw et al., 1993). There were three nonrandomized, matched towns: two treatment and one control. There was a mass media component plus community “events” in one town, and the same with the addition of a high-risk counseling program in a second treatment town. Before-and-after cross-sectional surveys measured knowledge of risk factors, smoking habits, and medical history as well as BMI, blood pressure, and cholesterol. Blood pressure, smoking, and composite risk were lowered compared to the control town, but there was no difference between the two treatment conditions. Thus, this was a replication of a successful use of a mass media strategy and was a test of these methods in a middle income country. However, the program focused only on middle income white South Africans, so the generalizability to other low and middle income countries may be limited. After the initial intervention was implemented, a maintenance program was established and surveyed at 4-year intervals. In a review of the project’s 12-year results Steyn et al. (1997) concluded that while the CORIS community intervention was successful in the short term, in the longer term both the control group and one of the two intervention groups showed decreased risk factors. The authors speculate that this can be explained by strong secular trends and local factors. This highlights the challenge of maintaining long-term effects in these interventions.
The Healthy Dubec Project was a single-community, 2-year education campaign in the country that was then Czechoslovakia, with a before-and-after analysis that surveyed height, weight, blood pressure, and cholesterol, as well as sociodemographic variables and behavioral CVD risk factors (Komarek et al., 1995). The education campaign was delivered primarily through print media, including newspaper columns and brochures distributed at community sites and events and to residents’ homes. Significant improvements were noted in blood pressure, cholesterol, and saturated fat intake. No effect was observed on smoking or BMI (Albright et al., 2000). This provides another example of some documented effects in a middle income country. Like many of the available examples of evaluated programs, this was a single-community model, which carries less evidentiary weight than studies with one or more control communities. Nonetheless, this study demonstrated the ability to achieve culturally appropriate adaptations of the print materials used in the Stanford Five City Project. This is an important lesson about the potential for transferability of materials tested in high income countries.
In Poland, the Polish Nationwide Physical Activity Campaign “Revitalize Your Heart” had the main goal of promoting an active lifestyle through education via mass media, including large broadcasting stations, public television, popular newspapers, magazines, and leading electronic media. This was accompanied by a country-wide contest and different local interventions (sports events, outdoor family picnics). Questionnaires administered to the participants of the contest and more than 1,000 people in the Polish population showed increased awareness of low physical activity as a problem. In addition, almost 60 percent of participants reported increased frequency and duration of exercise during the campaign (Ruszkowska-Majzel and Drygas, 2005).
Brazil’s Agita intervention, described in the previous section, had two main objectives: to increase the population’s awareness of how important physical activity is to health and to increase the level of physical activity within the population (Matsudo et al., 2003). To achieve these objectives, the program organized three main types of interventions: mega-events, specific activities with partner institutions, and partnerships with community organizations. The program succeeded in obtaining significant media coverage: 21 million people were reached by means of at least 30 newspapers distributed in the state’s various cities, as well as at least 7 national newspapers and 4 broadcasts on national television (Matsudo et al., 2002). As described in the previous section, an annual survey carried out over 4 years showed increased self-reported levels of physical activity (Matsudo et al., 2006).
Potential Lessons from CVD-Related Communication Campaigns in High Income Countries
Although evidence is limited from CVD-related programs in low and middle income countries, there are evaluations of programs in high income countries that offer some lessons for designing and implementing programs in low and middle income countries. This includes those that focused on a single outcome (smoking, physical activity, high blood pressure control, cholesterol reduction, salt consumption) and those that addressed multiple CVD risk factors within a single program. Some of these programs (whether they address a single risk factor or multiple risk factors) make communication a central (or the central) component of the intervention. Others make use of communication as one component of a multicomponent intervention. Even from these high income country programs the evidence is mixed, but a few general conclusions can be drawn.
Tobacco Use There is substantial evidence in support of youth antitobacco communication programs, which is described in more detail in
Chapter 6 (Wakefield et al., 2003). There is also some evidence, particularly time-series evidence, supporting the influence of communication on adult smoking (National Cancer Institute, 2008). A detailed synthesis of evidence on the effectiveness of media strategies employed in tobacco control campaigns, including marketing and advertising and news and entertainment media, can be found elsewhere and is not repeated here (National Cancer Institute, 2008).
In addition to tobacco control campaigns, there is good reason to believe that important reductions in tobacco use in part reflect deliberate efforts by the antitobacco movement to shift public opinion to recognize the dangers of secondhand smoke, to publicize the deliberate efforts by the tobacco industry to deceive the public and addict children and young people, and to achieve recognition of the right to restrict the free exercise of individual smoking rights when they affect the health of others. These efforts often included deliberate efforts to shape media coverage of the tobacco issue, and to use that as a path to changing public policy (Shafey et al., 2009). While it is not possible to make definitive attributions of influence, it is reasonable to connect this form of media advocacy to behavior change and to view it as an important model for tobacco control in low and middle income countries as well as for possible extension to other areas of behavior relevant to CVD.
Tobacco also offers an example of how communication can be used in ways that run counter to the promotion of health. For instance, the tobacco industry has used the media to promote tobacco products (Sepe et al., 2002; Shafey et al., 2009; Tye et al., 1987) and has spent billions of dollars a year on marketing initiatives in the United States (Frieden and Bloomberg, 2007). Tobacco advertising has proliferated on the Internet, and pro-tobacco messages are widely available on social networking websites (WHO, 2008). However, the media can also be effectively used for counter advertising, as has been demonstrated in different regions (Emery et al., 2007; Fichtenberg and Glantz, 2000; Goldman and Glantz, 1998; Ma’ayeh, 2002; Pierce, 1994). Moreover, controls on tobacco advertising and marketing can be effective if they are comprehensive, include both direct and indirect advertising and promotion, and are combined with other antitobacco efforts (Frieden and Bloomberg, 2007; Pierce, 1994; Saffer and Chaloupka, 2000).
Other Risk Factors There is some evidence in high income countries of the success of communication efforts in reducing salt consumption (He and MacGregor, 2009) and improving awareness, treatment, and control of hypertension (Roccella and Horan, 1988). There is less evidence for communication efforts alone to influence physical activity outcomes, par-
ticularly sustained physical activity changes (Kahn et al., 2002; Taskforce on Community Preventive Services, 2002).
There is also some credible evidence for the effects of communication programs targeted to multiple CVD-related risk factors (Schooler et al., 1997). Six successful community-based, multilevel, multifactor CVD prevention projects in high income countries in the 1970s and 1980s had effects that can be attributed largely to their use of a mass media health communication approach, which is the aspect of these programs discussed here. These projects are also discussed later in this chapter in the section on community-based programs. They were done in the United States, Finland, Australia, Switzerland, and Italy and have been reviewed extensively elsewhere (Schooler et al., 1997).
The North Karelia project in Finland continued for many years and, after its successes on all CVD risk factors during the first 5 years, its methods were applied throughout Finland and culminated in major declines in CVD mortality (Puska et al., 1995). The Stanford Three Community Study showed evidence for effects on important risk factors of smoking, blood pressure, cholesterol, and body weight and a large decrease in total CVD risk (Farquhar et al., 1977; Williams et al., 1981). The Stanford followon study (the Five City Project) showed relatively large effects on smoking and blood pressure, with somewhat lesser effects on overall risk than in the previous Three Community Study, and no effect on body weight (Altman et al., 1987; Farquhar et al., 1990; Sallis et al., 1985). The Three Community Study was also the basis for the design of the CORIS project described earlier (Rossouw et al., 1993). Indeed, the North Karelia program and Three Community Study galvanized substantial further major trials and worldwide consideration of community-focused programs to address CVD burdens.
Across the major projects that followed, including CORIS in South Africa, there has been replication of reductions in smoking and blood pressure in all seven projects, cholesterol in three, and body weight in two (Schooler et al., 1997). These replications provide evidence that rather small cities and towns in high income settings appear to have responded well in their risk-factor change to educational programs based largely on mass media.
In contrast, two other large programs that began somewhat later, in the mid-1980s, the Minnesota Heart Health Project and the Pawtucket Heart Health Project in Rhode Island, did not show appreciable effects (Carleton et al., 1995; Luepker et al., 1996). A likely reason for the lack of effect in the latter two programs is their relative lack (Luepker et al., 1996; Mittelmark, 1986) or absence (Carleton et al., 1995) of mass media. Other subsequent studies in Europe also tended to have greater success when
extensive broadcast and print media were used (Breckenkamp et al., 1995; Greiser, 1993; Schuit et al., 2006; Weinehall et al., 2001). These programs are also discussed again in the community interventions section below.
Another factor that may affect the success of health communication campaigns is secular trends that influence the novelty and potential effects of the campaign’s messages. The earlier studies, done in the 1970s and early 1980s, reflect the possibilities for mass education at that time, when radio and newspapers were a more important news source than at present, and while the trends for risk-factor levels and CVD events were beginning to decline. It was also a time before major changes had occurred in smoking rates, before the messages became more commonplace in the settings where they were implemented, and before the relatively easy changes in diet had occurred for many in the target populations. These studies also preceded the expansion of many of the broad drivers of CVD risk. Therefore, these earlier projects may have faced fewer obstacles to change than might be faced earlier or later in the epidemiological transition cycles.
Potential Lessons from Other Health Communication Programs in Low and Middle Income Countries
Even when communication programs in high income countries have demonstrated success, these programs may be difficult to generalize to developing-country contexts. Because there are so few models of CVD-related communication programs in low and middle income countries, it is worth looking to programs with evidence of effectiveness in these settings that have been targeted to other health-related behaviors for possible models of design and implementation, especially those programs that target outcomes that similarly require sustained behavioral change.
There is a rapidly growing evidence base for communications in low and middle income countries related to a range of health issues. For example, there is credible evidence for communication program effects on child survival-related outcomes including immunization (a repeated behavior requiring parents to bring their children to a clinic or other site), use of rehydration solutions for diarrheal disease (a repeated behavior undertaken at home in response to disease symptoms), and breastfeeding (a behavior already often performed but the campaigns are meant to shape the behavior and extend it in time) (Hornik et al., 2002). In addition, there is support for the effects of communication programs on HIV risk-related behaviors, particularly condom use with “casual” partners, and on family planning behaviors, particularly increasing initial visits to providers of contraceptive services (Bertrand et al., 2006; Hornik and McAnany, 2001).
Principles to Guide Future Design and Implementation of Communication Programs
Health communication campaigns require careful planning, ideally involving professionals with adequate training in health communication. Some of the key principles for designing and implementing these programs are described briefly here; existing resources that have informed communication strategies in developing world settings can provide more thorough guidance for planning CVD-related interventions (see, for example, NCI, 2002; O’Sullivan et al., 2003; Piotrow et al., 2003; Smith, 1999).
Strong communication programs choose messages based on behavior change theory and reflect thorough knowledge of their target audience, in terms of both their structural context—how the old and new behaviors fit into their lives—and their cognitive response to the behavior. Often audiences are heterogeneous and message strategies have to be differentiated by audience segment; formative research to precede widespread launching of a campaign can be used to test prototypes of the campaign’s messages with representative subsets of the intended target audience.
From the epidemiological perspective of preventing CVD, it is natural to look at the set of risk factors for CVD as interrelated and to consider how to construct a program that will influence all those factors. However, from the perspective of trying to prioritize and act synergistically with policy interventions to achieve change in risk factors or the behaviors associated with them, it may not be wise to try to address multiple CVD risk factors in one campaign. There may be greater potential to achieve behavior change by constructing independent programs that address each factor by itself (e.g., tobacco use, salt consumption, transfat consumption, saturated fat consumption, physical activity, and obesity). The institutional actors relevant to each of those risk factors are distinct, and the way one might construct communication campaigns for each can be sharply different. For example, there may be different focus audiences; different motivations for adopting new behaviors; and different types of behaviors with regard to timing, difficulty, and opportunity to act. The lack of commonalities among, for example, quitting smoking, maintaining physical activity, or purchasing foods low in saturated fats makes it very difficult to design one communication strategy that will maximally affect all relevant behaviors. However, hybrid campaigns may be preferred in some cases for greater efficiency when, for example, the trained health education staff is already in place.
A communication program can get exposure for the intended message through a number of means. For example, it can be required if the government controls media outlets. However, health authorities may not have access to the media even when it is government controlled. Exposure
can also be purchased, although purchasing media time can be expensive especially because the audience needs to be reached repeatedly with the intended messages. If it is necessary to purchase media time, achieving high levels of exposure and maintaining exposure over time could become the most expensive element of communication programs. Low and middle income countries therefore have an economic incentive to seek strategies to ensure the availability of low-cost educational media programming. Another strategy for program exposure is to make news and attract coverage from media outlets (e.g., National Power of Exercise Day in Thailand celebrity endorsement and involvement). However, media coverage may not be reliable and can be biased depending on factors such as whether media outlets are private entities or government agencies, and whether or not they operate within a system that guarantees freedom of the press.
New communications technologies may also provide opportunities to reach people with health-promoting messages and research suggests that channels such as computer programs, websites, and videogames may reach audiences missed by traditional health communication (Barrera et al., 2009; Boberg et al., 1995; Hawkins et al., 1987; Levy and Strombeck, 2002; Walters et al., 2006). However, although programs are emerging that depend on interactive communication technology, there is insufficient evidence at this time to determine if these approaches will be effective in low and middle income countries. One potential disadvantage to these kinds of digital media interventions (at least as they have been implemented up until now) is that they require audiences to seek out, have access to, and make continuing active use of the sources. This is unlike mass media interventions, which assume that the audience can be reached passively through its routine use of media. The requirement for active seeking is likely to limit the proportion of the unreached population who are engaged. This essential weakness runs up against a frequent goal of population-focused programs, which is to involve people who are not substantially motivated to act.
Another critical aspect of effective communication programs, like most behavior change programs, is that they cannot be single, fixed interventions. Rather, they need to evolve in response to changes in their audiences, to changes in the context in which the behavior is to be performed, and to changes in the social expectations of those around the individual. A good program is not defined by its specific communication actions (such as the number of messages on specific channels over a specific time period) but by the methods employed for changing messages and diffusion channels as circumstances change over time. They are more analogous to what a practicing physician might do, ideally, in working with a patient whose symptoms and illness level, readiness to comply with recommendations, and family support change over time.
Finally, capacity is a consideration that cannot be ignored since the ca-
pacity to design, implement, and evaluate interventions is generally weak in governments and local nongovernmental organizations in low and middle income countries. Additionally, in local markets the capacity to produce creative executions of messages is often weak. Formally addressing weak capacity must nearly always be an objective, even within the overarching objective of improved health outcomes. Decisions to implement communication campaigns also need to take into account the competition among health communication campaigns for resources, government attention, and target group attention (Smith, 2009).
Conclusion 5.2: Risk for CVD and related chronic diseases is increased by modifiable behavioral factors such as tobacco use; high intake of salt, sugar, saturated and transfats, and unhealthful oils; excessive total caloric intake; lack of consumption of fruits and vegetables; physical inactivity; and excessive alcohol consumption. For some of these risk factors, behavior modification and risk reduction have been successfully achieved through health promotion and prevention policies and communications programs in some countries and communities. However, most policies and programs with evidence of effectiveness have been developed and implemented in high income countries, and even in these settings little population-level progress has been made in some areas, such as reducing total calorie consumption and sedentary behavior. Adaptations to the culture, resources, and capacities of specific settings will be required for population-based interventions to have an impact in low and middle income countries.
Recommendation: Implement Policies to Promote Cardiovascular Health
To expand current or introduce new population-wide efforts to promote cardiovascular health and to reduce risk for CVD and related chronic diseases, national and subnational governments should adapt and implement evidence-based, effective policies based on local priorities. These policies may include laws, regulations, changes to fiscal policy, and incentives to encourage private-sector alignment. To maximize impact, efforts to introduce policies should be accompanied by sustained health communication campaigns focused on the same targets of intervention as the selected policies.
Health Care Delivery
One of the key components in reducing the burden of CVD is an adequate health system to implement the services needed to promote car-
diovascular health and control CVD. The need for adequate health care delivery is of course not unique to CVD, although there are aspects of care that need to be disease specific, such as guidelines and training. This section focuses on both areas of health care delivery within which there are specific CVD needs and also touches on broader health systems needs that are relevant for chronic diseases and synergistic with the emerging emphasis on global health systems strengthening and integrated primary care rather than disease-specific clinical programs. Efforts to improve broad health systems functioning are the focus of significant current efforts in global health and have been well described elsewhere (Lewin et al., 2008; Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009; WHO, 2007a).
The World Health Organization (WHO) defines a health system as consisting of “all organizations, people, and actions whose primary intent is to promote, restore, or maintain health” (WHO, 2007a). This encompasses public health approaches such as those described in the preceding sections of this chapter as well as the delivery of clinical health care services to identify and treat patients at high risk and to manage patients with diagnosed disease. Although the definition of health systems is an area of evolving discussions in the global health community, there is emerging consensus around six key building blocks of health systems articulated by WHO: efficient, high-quality health services; equitable access to essential medical products and technologies; financing; the health workforce; information systems (discussed in Chapter 4); and leadership and governance (WHO, 2007a).
There is also agreement that one fundamental goal of a health system is to provide effective, responsive, equitable, and efficient care (Committee on the State of the USA Health Indicators, 2009; Kruk and Freedman, 2008; Liu et al., 2008; Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009). Effective care is timely, safe, improves health outcomes, and continues until a health issue is resolved; or, in the case of chronic diseases, provides ongoing care as needed. This care should also be responsive to the needs of patients through not only the technical competence but also the interpersonal quality of providers. Equity in health systems means that essential health services are accessible to and utilized by all members of society—including those who are disadvantaged or marginalized—and that payment for care is equitable and does not result in catastrophic health care expenditures. This is especially critical for chronic diseases, which require ongoing expenditures on health services. Efficiency means that the health system yields the greatest health gains from the resources that are available and that the system functions productively (Kruk and Freedman, 2008).
There is considerable knowledge of clinical care solutions for treatment
of acute cardiovascular events, for management of CVD, and for prevention in high-risk patients that target blood pressure control, blood lipid control, blood glucose control, and smoking cessation. The effectiveness of these clinical solutions themselves, such as pharmacological interventions, are highly generalizable across countries and, as described in more detail below, guidelines and established practices for these clinical solutions, especially pharmacological interventions, are well developed. However, knowing an optimal clinical intervention that works to improve health outcomes is not sufficient. Clinical interventions need to be delivered appropriately to the patients who need them, which requires an effective and equitable system of health care delivery.
In addition to CVD-specific clinical solutions, there are common elements to effective delivery of chronic disease care that have potential to work for many health problems in low and middle income countries (e.g., diabetes, cancer, prenatal care, growth monitoring in children, TB, and HIV). These core elements include first, as a precondition, access and affordability. Other elements include guidelines or established practices that, when followed, lead to clinical success, routine assessment and improvement of quality of care, and monitoring of health status and health outcomes. Ideally, to enhance support for the behavior changes needed to maximize the effectiveness of clinical interventions, these clinical strategies would also be implemented in the context of the broader public health system, including population-based and community-based strategies described elsewhere in this chapter.
Therefore, the work that lies ahead is in improving health care delivery to reduce the burden of CVD in developing countries. There are several challenges that will need to be confronted when building on known, effective interventions in order to adapt and scale up to achieve equitable health care delivery. One challenge is that interventions and delivery mechanisms must be context-specific rather than generic applications of blueprint, uniform approaches. A second is to optimize comprehensive, integrated health programs and greater capacity in a fashion that encourages innovation yet addresses equitable distribution (Victora et al., 2004; WHO Maximizing Positive Synergies Collaborative Group, 2009). It is also critical that the delivery of health care be equitable. Ensuring an equitable health system requires establishing goals specifically for improved coverage for the poor, rather than in entire populations; planning and health interventions directed toward the needs of the disadvantaged; and empowerment of poor stakeholders to be vitally involved in health system design and operation (Gwatkin et al., 2004). Meeting these challenges, although formidable, will go a long way to ensure that the benefits of CVD control programs reach the greatest number of individuals in need.
This section considers in more detail the components of health care
delivery that will be crucial to successfully implementing effective clinical prevention and disease management for CVD. These include patient-level interventions, provider-level interventions to improve the quality of care, human resources and workforce, access to care, financing, access to essential medical products and technologies, integration of care delivery, and information technology. For some of these components, there is evidence specific to CVD-related interventions and programs or to approaches that can be generalized to CVD. For others, the discussion focuses on the principles in place in current efforts to strengthen health care delivery in general, which can be inclusive of CVD and related chronic diseases. The tools and strategies described are options for decision makers, managers, and clinicians that can be used to strengthen health care in different country contexts in order to deliver interventions effectively, efficiently, and equitably.
With resource and infrastructure constraints in developing countries, the translation of these strategies into improved health care delivery remains a challenge. However, it is possible to deliver good-quality care, even in resource-poor settings. The best strategies are often incremental and gradual and need to encompass action and motivation at all levels, from national leadership to local support (Jamison et al., 2006). In recent years, infectious disease programs in resource-limited settings have begun to build health care delivery infrastructure, especially in the development of laboratory capacity, supply chain management, quality assurance, and renovation of health centers (Justman et al., 2009). Such developments have brought a growing appreciation for the opportunity to use infectious disease-related systems strengthening to strengthen health systems in general (Jamison et al., 2006). Here, efforts to address chronic disease have the opportunity to build on, rather than duplicate, health systems strengthening efforts. Indeed, as global health begins to shift toward generalized strengthening efforts with a focus on primary care, chronic diseases and models of chronic care and disease management cannot be overlooked.
Patient-Level Interventions
The following section reviews patient-level interventions that are delivered within the health care system to reduce CVD risk and manage disease, including behavior change strategies and clinical interventions for prevention and treatment. Guidelines for delivering clinical interventions are discussed in the section on provider-level interventions, followed by a section on integrated disease management and chronic care strategies. Although different interventions are described in separate categories, they are not intended to be used in isolation from each other but rather as components of a health care provider’s services for patients, as well as in synergy with
population- and community-based approaches described in other sections of this chapter.
Strategies to Change Behaviors Provider advice and education are among the interventions delivered to patients as part of health care. There is mixed evidence on the effectiveness of these approaches. In fact, in a review of counseling and education interventions to reduce multiple risk factors for prevention of CHD in settings including primary care, the authors concluded that “[i]t is essential that the current concepts and practices of multiple risk factor intervention … through individual risk factor counseling are not exported to poorer countries as the best policy option for dealing with existing and projected burdens of cardiovascular disease” (Ebrahim et al., 2006, p. 23). Therefore, more work is needed to determine the appropriate role and best delivery mechanisms for these intervention approaches.
Economic incentives have also been used to influence consumers’ preventive health behaviors. A review by Kane et al. (2004) concluded that economic incentives (including cash, gifts, lotteries, and other free/reduced-price goods or services) appear to be effective in the short run for simple preventive care and distinct, well-defined behavioral goals. According to the review, incentives were effective 73 percent of the time and small incentives produced finite changes. While this is encouraging, the authors recognize that although economic incentives for prevention appear to work, their mechanisms are not well understood. For example, it is not clear what size of incentive is needed to yield a major sustained effect and there is less evidence that economic incentives can sustain the long-term lifestyle changes required for health promotion. In addition, the generalizability of these findings to low and middle income country contexts is not known.
Several randomized trials in high income countries have demonstrated the effectiveness of financial incentives to address tobacco use. Incentives ranged from small amounts of money ($20) for each class attended to an incrementally higher amount for smoking cessation and continued abstinence at 1, 4, and 6 months after the program initiation (Donatelle et al., 2000; Volpp et al., 2006, 2009). A financial incentive for smoking cessation has also been evaluated in the Philippines (Giné et al., 2008). CARES, a voluntary commitment program to help smokers quit smoking, offered smokers a savings account in which they deposited money (a minimum of 50 pesos, or approximately $1) for 6 months without interest. Participants were given a lockbox to aid in daily savings, with a weekly deposit collection service available. Within 1 week of the 6-month maturity date, participants took a urine test for nicotine and its primary metabolite, cotinine. If they passed, their money was returned; otherwise, their money was forfeited to charity. Eleven percent of smokers offered CARES signed a contract, and smokers randomly offered CARES were 3 percentage points more likely to pass the
6-month test than the control group. This effect persisted in surprise tests at 12 months, indicating that CARES produced lasting smoking cessation.
Conditional cash transfers are another strategy to provide incentives to promote adoption of healthy behaviors. In conditional cash transfer programs a cash payment is made to an individual or family contingent upon complying with certain conditions, such as preventive health requirements and nutrition supplementation, education, and monitoring designed to improve health outcomes and promote positive behavior change (Lagarde et al., 2009). Programs of this kind have been implemented by governments or other organizations in low and middle income countries with the goal of improving options for poor families through interventions in health, nutrition, and education. A recent review supports the potential for conditional cash transfer programs to increase the uptake of preventive services and encourage some preventive behaviors (Lagarde et al., 2009). However, mixed results and insufficient evaluations make it difficult to draw conclusions about the potential that these programs have for wide-scale implementation.
There are few published examples that are directly related to CVD outcomes, but a program in Mexico can be informative for addressing related CVD risk factors, specifically child nutrition and obesity. PROGRESA/ Oportunidades examined the effect of conditional cash transfers in 506 rural, low income communities that were randomly assigned to be enrolled immediately or after an 18-month period, allowing for comparison between the two groups during the waiting period. The intervention linked payment to mothers for health behaviors, such as participation in health and nutrition programs including prenatal care, immunization, and nutrition supplementation, and incentives to promote children’s school attendance (Rivera et al., 2004).
It was recently evaluated for its impact on several CVD-related outcomes, and the cash transfer component was associated with better outcomes in children (Fernald et al., 2008b). After 5 years, children (n = 2,449) aged 24-68 months who had been enrolled in the program their entire lives were assessed for a range of outcomes related to CVD risk. A doubling of cash transfers was associated with lower body mass index (BMI) for age percentile and lower prevalence of being overweight. Although this is a promising result, the cash component was also negatively associated with adult health outcomes (Fernald et al., 2008a). After 5 years of the program, adults (n = 1,649 early, n = 2,039 late intervention) aged 18-65 years were assessed. A doubling of cumulative cash transfers to the household was associated with higher BMI, higher diastolic blood pressure, and higher prevalence of overweight, grade I obesity, and grade II obesity while controlling for a wide range of covariates, including household composition at baseline.
Clinical Interventions to Reduce Risk and Manage and Treat CVD There is considerable knowledge of effective clinical solutions to reduce risks for CVD using pharmaceutical interventions to lower blood pressure, blood lipids, and blood glucose and to assist in smoking cessation. There is also considerable technical knowledge on the diagnosis of CVD, treatment of acute cardiovascular events, and post-event treatment and management (Fuster, 2009).
There is particularly strong evidence on the pharmacological management and control of high blood pressure (or hypertension), with a corresponding reduction in cardio- and cerebro-vascular mortalities and morbidities (Fuster, 2009). Low-cost generic blood pressure-lowering medications are in use for controlling hypertension throughout the world (Pereira et al., 2009). As described in more detail in the section on economic analysis in Chapter 7, hypertension control is also one of the interventions with the most potential to be cost-effective in low and middle income countries. Pharmacological interventions to lower blood cholesterol and its main components, such as LDL cholesterol and serum triglycerides, have also proven to be very effective in reducing the cardiovascular mortality and morbidity in populations around the world (Adult Treatment Panel III, 2002; Brugts et al., 2009; Smith, 1997).
Indeed, aspirin, beta-blockers, ACE-inhibitors, and lipid-lowering therapies all have established effectiveness to lower the risk of future vascular events in high-risk patients. The benefits of each of these pharmaceutical interventions appear to be largely independent so that when used together in appropriate patients it is reasonable to expect that about two-thirds to three-quarters of future vascular events could be prevented. Therefore, the potential gains from combined drug therapies are large (Yusuf, 2002). This has led to the development of combination pills, known as “polypills” in an effort to achieve a lower cost, more efficient, and more convenient treatment option for patients at high risk for CVD. The effectiveness and safety of this promising approach is currently being evaluated in a number of trials in both developed and developing countries (Holt, 2009; Xavier et al., 2009).
Adherence to clinical interventions Lack of adherence to medical treatment is a widespread problem that can lead to worsening health status and increased future treatment costs. Treatment regimens that are easy to administer, accessible, and affordable can help to increase adherence. As described above, improving adherence through simplicity, convenience, and reduced costs is one of the hopes for the emerging “polypill” concept. Affordability and access are discussed in more detail as part of the next section on access to clinical interventions.
Financial incentives are one possible intervention to improve adherence.
In a review of financial incentives to enhance patient compliance, Giuffrida and Torgerson (1997) found that 10 of 11 studies showed improved patient compliance with the use of financial incentives. However, the clinical aim of each study was different and the incentives varied. It is also important to note that all the randomized studies reviewed were carried out in the United States; thus, the results may not translate directly to another country with a different socioeconomic and cultural context.
Adherence to TB treatment is an analogous challenge that is common in developing countries and may provide transferable lessons for pharmaceutical interventions for CVD. In two pilot sites in Tajikistan, Project HOPE used food incentives to enhance adherence to a TB treatment regimen, enable patients to complete treatment without burden on their families, and increase access to directly observed therapy (DOT) for the poor and vulnerable. In this intervention, directly observed therapy was linked with the incentive of a nutritious meal. Among new sputum positive patients who received directly observed therapy, 88 percent of those receiving meal supplements completed treatment and were cured, compared to 63 percent in the non-supplemented patients (Mohr et al., 2005).
Access to clinical interventions An evidence-based, cost-effective primary health care-centered approach that includes targeting screening for high-risk individuals and the provision of treatment for symptom control is critical to ensuring access to appropriate CVD care. Risk-prediction tools that assess risk on the basis of multiple risk factors and CVD history have been developed in the United States and other high income countries (Bannink, 2006; Kannel, 1976), but cannot be assumed to be directly applicable to all populations and settings. For greatest feasibility, screening in resource-limited areas may need to focus on simple methods like family history, medical history and physical measurements such as blood pressure and body mass index or waist-to-hip ratio (Joshi et al., 2008).
As a necessary follow-up to effective screening, access to essential medicines, medical products, and technologies is a critical part of access to care. While one of the Millennium Development Goal targets is to “provide access to affordable essential drugs in developing countries,” (United Nations Department of Economic and Social Affairs, 2008, p. 47) recent WHO reports have indicated that essential CVD medicines are largely not available in the public sector in low and middle income countries (Cameron et al., 2009; Mendis et al., 2007a). While there is better availability of these medicines in the private sector, the end-user cost of these private-sector medicines is often quite burdensome to the majority of low and middle income populations. For example, a 1-month course of combined therapy for secondary prevention (aspirin, beta-blocker, ACE-inhibitor, and statin) for patients with established CVD could cost as much as 18 days’ wages in
Malawi (Mendis et al., 2007a). In addition, the pharmaceutical component of CVD prevention requires daily, long-term medication treatment, rather than short-course or one-time therapy, which increases the lifetime financial burden. Individuals may not be able to afford continuous treatment for long periods of time. Given that anywhere from 50 to 90 percent of the cost of medicines are financed through individual out-of-pocket payments in low and middle income countries (Quick et al., 2002), the financial burden on individuals and families has the potential to be substantial. Clearly, much needs to be done to ensure a guaranteed supply of affordable CVD medicines to the majority of the low and middle income country population.
Several possible initiatives could potentially help address this problem, although the potential costs of these are difficult to estimate. As described above, the polypill, although not yet evaluated, is an attractive option that could be administered to a broad range of patients, especially if manufactured with generic components. If proven safe and effective, this has the potential to be a pragmatic response to the need for both simplified and affordable treatment regimens in low income countries with weak health systems (Wald and Law, 2003; Yusuf, 2002). Another initiative to help address costs is generic substitution policies, which allow for generic medications to be offered as an alternative to more expensive brand-name medications (Andersson et al., 2007). Elimination of tariffs on medicines, generally a regressive form of taxation, could also increase the equitable access to essential CVD medicines without significant impact on government revenues (Olcay and Laing, 2005). In addition, negotiations with pharmaceutical companies have led to decreases in the price of anti-retroviral medications for HIV in low and middle income countries (Borght et al., 2009). New advocacy and private-sector collaboration could lead to improved affordability of medicines for CVD in low and middle income countries. Government-sponsored health insurance schemes can also reduce the end-user cost of both drugs and other health services, as has been done in Rwanda, although this strategy still faces concerns about financial sustainability and availability of services and medicines. Health financing mechanisms are discussed later in this chapter (Twahirwa, 2008).
Finally, improved drug distribution and procurement efficiency has the potential to make drugs more readily available through the public system and affordable through the private system (Joshi et al., 2008). The delivery of drugs, including statins, antihypertensives, nicotine replacement, or a newly created polypill to low-resource settings in a manner timely and reliable enough to maintain individual treatment regimens is an enormous logistical challenge. However, there exists growing expertise in supply chain management in developing countries from both the HIV/AIDS and malaria community as program implementers attempt to scale up their respective initiatives. The Supply Chain Management System was initiated as part of
the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) to deliver antiretroviral medications to local implementing partners and programs involved in rapid scale-up efforts (Supply Chain Management System, 2010). The strategies employed by the Supply Chain Management System include combining orders to purchase at wholesale rates, warehousing and distribution through regional distribution centers, preventing product expiration through inventory management that focuses on stock rotation and monitoring, forecasting demand and anticipating country needs, and benefiting from the establishment of long-term contracts (Supply Chain Management System, 2009). These strategies could all potentially be adopted to improve CVD drug delivery.
However, it is important to ensure that CVD-related procurement needs are coordinated with existing efforts in the global health community, so as not to perpetuate the difficulties caused by parallel distribution systems. In HIV/AIDS for example, The Global Fund to Fight AIDS, Tuberculosis and Malaria and PEPFAR each have their own supply chain management protocols, funding streams, and procurement requirements. While each of these agencies expressly endorses coordination wherever possible, local actors still must balance the needs of distinct international funders (The Global Fund, 2009; Partnership for Supply Chain Management Systems, 2010). In order not to compound this problem, it is important for the global CVD community to identify ways to work within or help adapt existing frameworks and supply chains.
In addition to the existing efforts driven by global health organizations, extensive research and efficiency improvement efforts have also been undertaken by the private sector as businesses expand into global markets, and these strategies may offer uncommon insights that can benefit CVD initiatives (Accenture, 2010; Council of Supply Chain Management Professionals, 2010; Kinaxis, 2010). While supply chain systems have grown steadily over the past decade, there is still a great deal of infrastructure and capacity yet to be developed. Ensuring that CVD medications are included during the planning and design phases of these new endeavors is a positive opportunity in which the global CVD community could take an important leadership role.
As with medicines, CVD-related technologies—diagnostics and interventions—have the potential to contribute greatly to the control of global CVD; however, an effort equal in energy and intensity must be made to ensure equitable distribution and access to these technologies as they develop and proliferate. The development of novel diagnostics has accelerated in the area of communicable diseases such as HIV and TB (Houpt and Guerrant, 2008); similar initiatives can be envisioned for CVD. However, for diagnostic technologies to make any noticeable impact on CVD mortality, they need to be suitable to and affordable in the developing world, and
there needs to be sufficient provision of health care following diagnosis, or the improved ability to correctly identify patients will be of little use. Some of these new technologies, such as portable electrocardiogram machines, are being produced or are under development in health technology companies in high income countries. They are being rolled out primarily for middle-income developing markets, but are already spreading more widely to poor countries, at least to segments of the population that can afford them (Immelt et al., 2009).
Although the delivery and implementation of the latest, state-of-the-art technologies may have potential to help reduce the burden of disease, in some settings with more developed health systems, a patient’s access to the preexisting technologies that are already being used in the local or national health system can have a more profound impact on their survival status than the absolute level of technology in the country or community. For example, it has been shown that poor patients in India suffer higher mortality after acute coronary syndromes, but that this mortality difference is eliminated after controlling for access to treatments (Xavier et al., 2008). Thus, in some countries improving access to essential CVD-related services within broader efforts to improve access and maximize the equitable use of existing health systems infrastructure will likely enhance the role of technology for diagnosis and treatment, even without costly efforts specifically to increase technological capacity within a country.
Provider-Level Interventions to Improve the Quality of Care
Quality of care was defined by the Institute of Medicine (IOM) as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (IOM, 2001, p. 232). There are three main aspects of quality: process (the actions performed in the delivery of care), outcomes (the observable consequences of care), and structure (the characteristics of health systems, facilities, and staff) (Donabedian, 1988).
Quality improvement strategies that act directly on provider behavior may focus on two aspects of performance—technical and interpersonal. Technical performance refers to the extent to which services are performed according to standards and can be improved through supervision and lifelong training (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009). Like the patient-level interventions described in the previous section, these approaches need to incorporate sufficient CVD specificity to provide relevant technical knowledge, although the strategies to deliver technical performance improvements can be generalized in a chronic disease model. Interpersonal quality improvement strategies involve meeting users’ expectations and values to provide responsive care.
Competence in this area is particularly important for CVD and other diseases that require chronic care and long-term relationships with providers. Establishing norms and codes of conduct, and the provision of supervision and basic amenities, are effective methods for increasing interpersonal performance (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
The strategies to improve quality of care by changing provider behavior described below include guidelines, disease management programs, audit and feedback on performance, public reporting, and performance incentive programs such as pay for performance. This is an area of quality improvement that has become well established in high income countries, but is much less well developed in low and middle income countries. A review of quality improvement intervention studies in low and middle income countries suggests that dissemination of guidelines alone is not effective, but that supervision and audit with feedback show more promise, as well as systems interventions at the level of the hospital or clinic. In addition, interventions with multiple components are likely to be more effective than single components (Rowe et al., 2005). However, the review acknowledged the limited information on strategies to improve performance in low and middle income countries. There is a need for better understanding of the determinants of provider performance, better methods to measure performance, high quality studies to assess long-term effectiveness and costs, and a better understanding of the extent to which results for one setting and area of care can be applied to others (Rowe et al., 2005). This knowledge gap is particularly striking for interventions related to improving CVD-related care in developing countries. Therefore, where evidence is lacking quality improvement on strategies to address CVD and related risk factors in low and middle income countries, there is a discussion in the following sections of evidence that can be generalized from relevant chronic disease-related approaches in high income countries and in some cases, from strategies targeted at other areas of health care in low and middle income countries in order to develop strategies for CVD and related chronic diseases in low and middle income countries.
Guidelines There are multiple national and international guidelines for prevention, treatment, management, and control of CVD and CVD-related risk factors, including hypertension and elevated lipids, many of which have been tailored for a range of high income countries and low and middle income countries. These include, for example, the American Heart Association (AHA) Guidelines (Fuster, 2009); the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (U.S. Department of Health and Human Services, 2004); the European Guidelines on Cardiovascular Disease Prevention in Clinical Practice
(Graham et al., 2007); the Chinese Guidelines on Prevention and Treatment of Hypertension (Committee for Revision of Chinese Guidelines for Prevention and Treatment of Patients with Hypertension, 2005); the Canadian Guidelines for the Diagnosis and Treatment of Dyslipidemia and Prevention of Cardiovascular Disease in the adult (Genest et al., 2005); the Canadian Hypertension Education Program (Canadian Hypertension Education Program, 2009); and the WHO/International Society of Hypertension (ISH) Hypertension Risk Prediction charts (Mendis et al., 2007b).
In principle, these existing, well-established guidelines describe effective care that should be highly transferable across settings. However, this requires that clinicians learn the guidelines and adhere to them in practice, which is not an insignificant barrier. For example, a study of European guidelines for CVD prevention found that guidelines were not being followed. The objectives of the European Action on Secondary Prevention through Intervention to Reduce Events (EUROASPIRE) survey were (1) to determine in patients with CHD whether the European guidelines on CVD prevention were being followed and (2) to determine whether the practice of preventive cardiology in patients with CHD in EUROASPIRE III improved by comparison with the previous surveys, EUROASPIRE I and II, after efforts were implemented to improve adherence to guidelines (Kotseva, 2009b). The study outcomes indicated that most guidelines were not being followed, showing no change in the prevalence of smoking and continued adverse trends in the prevalence of obesity and central obesity. Despite increased use of antihypertensive medications, there was also no change in blood pressure control. An increased prevalence of diabetes, both self-reported and undetected, and deteriorating therapeutic control was found. The study did show an increased use of antiplatelets, beta-blockers, ACE/ angiotensin II receptor blockers, and statins along with continued improvement in lipid control (Kotseva, 2009a).
A recent review found that improvements in guideline adherence, as measured by performance indicators, have led to significant reductions in mortality (Mehta et al., 2007). Their findings suggest that improving quality achieves reductions in death in excess of those seen for any new therapy. It is estimated that the use of clinical guidelines for acute myocardial infarction can prevent 80,000 deaths annually in the United States alone (Bahit et al., 2000). Therefore, the potential global implications are significant if effective ways to improve adherence to guidelines can be developed.
Audit and Feedback Audit of performance and feedback have been used in a variety of settings to affect provider behavior and quality of care (Jamtvedt et al., 2006). The potential for an effect on quality of care rests on the general premise that knowledge of one’s own performance motivates
improvement. With the increased use of electronic medical records, audit and feedback has increasing potential as a measurement tool that can be implemented with greater ease and be linked to performance-based incentives such as pay-for-performance programs (Hysong, 2009).
However, reviews of the literature on audit and feedback have not found consistent evidence of its effectiveness as an intervention to improve quality (Grimshaw et al., 2004; Jamtvedt et al., 2006). A review of 118 randomized trials of audit and feedback reflected these mixed results but concluded that audit and feedback can be effective in improving professional practice. When it is effective, the effects are generally small to moderate. The relative effectiveness of audit and feedback is likely to be greater when baseline adherence to recommended practice is low and when feedback is delivered more intensively (Jamtvedt et al., 2006). A more recent analysis suggests that the effectiveness of audit and feedback is also improved when specific suggestions for improvement are offered along with measurement feedback (Hysong, 2009). However, the vast majority of the studies included in these reviews were conducted in developed countries.
Interest in provider measurement and feedback as a quality-improvement tool in developing countries is growing. For example, studies to date have shown that feedback of health worker performance data on managing childhood diseases in Africa improved compliance with standards of care (Kelley et al., 2001), and audits using a simple checklist of maternal health indicators improved performance in the Philippines (Loevinsohn et al., 1995). Even self-assessment of compliance with standards of care can improve quality, as shown in Mali (Kelley et al., 2003).
Using clinical performance vignettes, the Quality Improvement Demonstration Study (QIDS) in the Philippines provides recent evidence from a middle income country of links between clinical performance feedback and improvements in quality, outcomes, and satisfaction. QIDS was an evaluation to compare the impact of two interventions on physician practices, health behaviors, and health status of children under 5 years: (1) expanded insurance coverage to increase access to care and (2) a pay-for-performance scheme for physicians (Shimkhada et al., 2008). In all sites, randomly selected physicians were administered clinical performance vignettes every 6 months, and their scores were reported back to them individually, along with their rank compared to other physicians. The effects of the pay-for-performance intervention are described in more detail later, but of interest here is that with time—even in the control condition, which had no change to the existing insurance or payment schemes—there were observable quality improvements. This suggests that performance evaluation and dissemination of scores alone affected quality scores (Luck and Shimkhada, 2009; Peabody et al., 2010b; Quimbo et al., 2010).
Public Reporting and Consumer Choice In the United States and other Western nations, public reporting of provider quality data has been employed as a means to support and stimulate quality improvement (Marshall et al., 2000). The ability of public reporting to incite change rests on the assumption that consumers demand and use comparative data in making choices about health care providers. Recent reviews of the literature have sought to assess the impact of public reporting. The results generally point to a limited body of evidence on the effects of provider quality information on consumer choice (Faber et al., 2009; Fung et al., 2008) and weak evidence of provider changes stemming from public reporting (Fung et al., 2008; Robinowitz and Dudley, 2006). Further analysis shows that public reporting of outcomes does appear to have an impact on quality improvements at the hospital level (Fung et al., 2008). However, public reporting appears to have limited impact on quality improvement if consumers have a difficult time understanding the results, particularly when there is little variation among providers (Robinowitz and Dudley, 2006). Poorly constructed report cards do not help consumers in making choices; a summary table of benchmark provider measures may be a better way to communicate provider performance (Devers et al., 2004; Hibbard, 2008).
Shaller et al. (2003, p. 95) have asserted that providing comparative quality information to consumers will drive improvements in health care quality, only if five conditions are met: “(1) consumers are convinced that quality problems are real and consequential and that quality can be improved; (2) purchasers and policymakers make sure that quality reporting is standardized and universal; (3) consumers are given quality information that is relevant and easy to understand and use; (4) the dissemination of quality information is improved; and (5) purchasers reward quality improvements and providers create the information and organizational infrastructure to achieve them.”
Work on public reporting in developing countries is limited. However, there have been documented examples of its use. In Uganda, a community-based monitoring system for primary health care providers resulted in improved child outcomes (Bjorkman and Svensson, 2007; McNamara, 2006). In India and the Philippines, provider report cards using data from patient satisfaction surveys have been used (McNamara, 2006). These examples demonstrate feasibility, but more work is needed to assess the value of this type of information on influencing patient behavior and its applicability across other settings.
Performance Incentive Programs Pay-for-performance programs that link financial incentives with quality measures to reward good clinical practice at the level of both providers and institutions have been used extensively in the United States and Europe, with some modest evidence of success
(Campbell et al., 2009; Epstein, 2007; Grossbart, 2006; Lindenauer et al., 2007; Petersen et al., 2006).This approach is gaining popularity in the developing world (Eichler et al., 2009) with substantial donor support, although this support is not necessarily being devoted to CVD care. Pay for performance may confer some unique benefits in a developing-country setting. Namely, in resource-constrained settings, where the quality of care and the health of populations are consistently low and thus targeted by governments and donor agencies alike, the marginal health benefits may be expected to be higher. Providers may be more responsive to incentivized measurement and feedback (Eichler et al., 2009).
There are few rigorous evaluations of pay for performance in developing countries. Taken together, however, efforts in developing countries suggest that an infrastructure for provider measurement, feedback and incentives, can be developed and implemented (McNamara, 2006). QIDS in the Philippines, described earlier, compared the impact on physician practices, health behaviors, and health status of children under 5 years of either expanded insurance coverage to increase access to care or a pay-for-performance scheme in which bonus payments were given to physicians based on quality scores using a randomized design (Shimkhada et al., 2008). Clinical performance vignette scores improved over a period of 2 years in the pay-for-performance sites compared to controls (Peabody et al., 2010b; Solon et al., 2009). Improved access to care and overall system-level reimbursement in the expanded insurance coverage arm also led to changes in quality. In addition, for both intervention arms, there were clinical improvements as measured by the number of children who were not wasted (underweight for height) (Peabody et al., 2010b). Quality improvements were also associated with patient satisfaction (Peabody et al., 2010a).
In another example, in Haiti, incentives for achieving health targets led to significant changes in provider practice such as immunization coverage and attended deliveries (Eichler et al., 2009; McNamara, 2005). In Rwanda, performance-based financing was adopted by the government as a national policy, with performance payments to public and private health facilities (Eichler, 2009; Soeters et al., 2006). The impact on prenatal care utilization, the quality of prenatal care, institutional delivery, and child preventive care utilization was assessed using data produced from a prospective quasi-experimental design nested into a phased program rollout in 165 rural facilities, which allowed for comparisons between first- and second-phase facilities during the 2-year delay in rollout. The incentive effect was isolated from the resource effect by increasing the second-phase facilities’ traditional budgets an amount equal to the average pay-for-performance payments to the first-phase facilities. The pay-for-performance program had a large and significant positive impact on some outcomes, including institutional deliveries and young children’s preventive care visits. The pro-
gram also improved the quality of prenatal care as measured by process indicators of the clinical content of care and tetanus toxoid vaccination (Basinga et al., 2009).
Chronic Care and Disease Management Models
Comprehensive models for managing chronic illnesses have been developed with the goal of combining and integrating approaches to increase quality of care by providers, provide appropriate interventions, and improve accompanying behavior change and patient self-management. This is an area where professionals in primary care and in CVD and related chronic diseases have a wealth of experience in developing models that can be offered not only to manage noncommunicable chronic diseases, but also to assist in the evolution of health systems to better address the transition to chronic care needs for patients with chronic infectious diseases such as TB and HIV/AIDS. Multiple models for managing chronic illness have been developed and implemented in high income countries, focusing on improvements in a range of elements such as health systems, clinical decision support, delivery-system redesign, clinical information systems, community resources, and self-management support. These have been described extensively elsewhere (Bodenheimer et al., 2002; CDC, 2003; Feachem et al., 2002; Kane et al., 2003; Klingbeil and Fiedler, 1988; Singh and Ham, 2006; Wagner et al., 1996; WHO Noncommunicable Diseases and Mental Health Cluster, 2002). This is an area of great promise, but it is not always straightforward in its implementation and, although specific components do have a strong evidence base, there have not been many rigorous evaluations of the health impact of the existing overall frameworks. In addition, most available evidence is drawn from the United States, reinforced by recent studies from Europe, Canada, New Zealand, and Australia (Singh and Ham, 2006). Thus evidence from low and middle income countries is sparse and the potential for effective transfer of chronic care models to low and middle income settings remains to be demonstrated (Beaglehole et al., 2008).
A systematic review of randomized clinical trials of disease management programs specifically designed for patients with coronary heart disease showed positive impacts on processes of care and moderate effects on risk-factor profiles (McAlister et al., 2001). However, like most evidence for chronic care models more generally, these trials were all from high income countries, and there has been little implementation or evaluation of care management approaches in low and middle income countries.
A current trial in Shanghai is evaluating a case management model that is intended to be deployed to community hospitals to increase effectiveness of hypertension control through attention to the workflow and process
details; an integrated hypertension intervention approach; and intensive education and training to increase the competency of community health providers. The trial initially enrolled 1,442 hypertensive patients randomly assigned to intervention (IG, n = 480) and control (CG, n = 962) groups and was subsequently expanded to 19 districts in Shanghai and a total of 15,200 patients (11,400 in IG/3,800 in CG). The results have not yet been published, but preliminary results have been reported and show promising effects on blood pressure control and quality of life in patients as well as on the knowledge and skill of community hospital physicians. The program has also shown lower costs per mmHg systolic blood pressure or diastolic blood pressure reduction in IG compared to CG over a 12-month period (Lu et al., 2009).
Initiatives to Strengthen Health Systems Capacity and Infrastructure
Human Resources Currently, more than a billion people worldwide have insufficient access to health services (Crisp et al., 2008), which is due in part to a shortage of health workers. The 2006 World Health Report has estimated that there is already a global shortage of more than 4 million health workers, with the greatest shortage being experienced by low income countries (WHO, 2006). With the expected increase in the burden of the global CVD epidemic, it is likely that the shortage in the global health care workforce and leadership will be even more acutely felt in low income countries during the upcoming several decades. Guided by the principles of coverage, motivation, and competence, it will be crucial to meet this challenge with initiatives to increase the health care workforce; to promote task-shifting to less-specialized workers; to provide specialized continuous training at several professional levels of health care worker in clinical, public health, health communications, and behavioral disciplines, as well as health systems and program management; to promote motivation by improving management and providing satisfactory remuneration, adequate resources, appropriate infrastructure, and career development; and to cultivate leadership and innovation (Chen et al., 2004; Lehmann et al., 2009; Willis-Shattuck et al., 2008).
Successful initiatives in this arena will require sustained involvement, leadership, and support of national governments in several realms: (1) to establish a regulatory framework that encourages training, monitoring, and assessment; (2) to implement policies that liberalize resources and create career development and promotion pathways; (3) to guide and support training institutions; (4) to marshal the resources necessary to create incentives for growth in the supply and retention of health care workers; and (5) to secure the support of the multiple stakeholders, including funding sources, educational institutions, practitioners, administrative personnel,
and community members (Chen et al., 2004; Crisp et al., 2008; Lehmann et al., 2009). In addition, the input and influence of multilateral organizations will also be of paramount importance in facilitating dialogue and partnership among different stakeholders.
WHO has created the Global Health Workforce Alliance, which is a partnership of national governments, civil society, international agencies, finance institutions, researchers, educators, and professional associations dedicated to working toward solutions for the global health care workforce shortage issue (Global Health Workforce Alliance, no date). Although CVD is not specifically addressed by the Alliance, many of the same principles and proposals apply to the global CVD agenda.
One strategy for increasing the workforce is task-shifting. Examples of successful programs exist. The Integrated Management of Childhood Illnesses recently reported that quality of childcare was equivalent across several categories of health workers irrespective of the duration and level of pre-service training, thus demonstrating that task-shifting to less-specialized workers can yield equivalent results (Huicho et al., 2008). The use of nonphysician clinicians is notable for its lower training costs, shorter training periods, and increased placement in rural resource-deficient communities (Mullan and Frehywot, 2007). In addition, community health workers (CHWs) who are trusted, respected members of the community but do not have formal health training, have been used for decades in several areas of global health, and have proven beneficial in terms of community development, community health education, increased access to basic health services, cultural sensitivity, cost-effectiveness, and improvement in community self-reliance (Berman, 1984; Brownstein et al., 2005; Friedman et al., 2007; Lehman and Sanders, 2007; Prasad and Mulaleedharan, 2007). A review of work in the United States suggests that interventions for prevention and control of CVD can be effectively delivered by community health workers, which suggests that there may be potential for adapting this approach to develop CVD-specific strategies in low and middle income countries (Brownstein et al., 2005). In order to determine the optimal task-shifting policy and use of nonphysician clinicians to meet CVD-specific needs, it will be necessary to determine the optimal mix of specialization and training required to meet the CVD control challenge within individual countries. Successful adoption of such strategies to address the global CVD epidemic would require integrated reconfiguration of health systems with altered scopes of practice at all levels, enhanced training infrastructure, availability of reliable medium- to long-term funding for both training and employment incentives, and community input and participation (Lehmann et al., 2009).
Another strategy is to enhance the cultivation of leadership positions and enhance career development through the creation of academic train-
ing partnerships between institutions in high and low income countries. Examples of such successful academic partnerships exist, built upon the following principles: (1) leveraging the institutional resources and credibility of academic medical centers to provide the foundation to build systems of care with long-term sustainability; (2) development of a work environment that inspires personnel to connect with others, make a difference, serve those in great need, provide comprehensive care to restore healthy lives, and grow as a person and as a professional; and (3) training of health care workers at all levels (Einterz et al., 2007; Inui et al., 2007).
The train-the-trainer model is another strategy for increasing workforce capacity. These models have been used extensively for training in the infectious disease field, but the adaptation of chronic disease approaches in this area in developed countries to low and middle income settings remains largely an untapped opportunity. The National Heart, Lung, and Blood Institute (NHLBI), partnering with organizations like the National Council of La Raza and the U.S. Health Resources and Services Administration, has utilized this approach in its Promotora de Salud model for addressing CVD risk factors in high-risk Hispanic communities in the United States (Balcazar et al., 2005, 2009). Based on self-report, trained “promotores” obtained the knowledge and skills to recruit community members to participate, to pass on their knowledge gained, and to support community members in making changes in lifestyle that promote cardiovascular health (Balcazar et al., 2005).
In another example that could be expanded to meet chronic disease needs in developing countries, the U.S. Centers for Disease Control and Prevention (CDC) has developed Field Epidemiology and Lab Training Programs as part of its systems strengthening efforts in developing countries. To establish a training program, the CDC typically provides ministries of health with an in-country resident advisor for 4 to 6 years to help guide training and technical assistance (CDC, 2009b). Since 1992, the CDC’s Management for International Public Health course has trained 379 management trainers from 68 countries. Graduates have trained thousands of public health professionals, who subsequently implemented hundreds of management and leadership improvement projects (CDC, 2009a).
A critical issue that will also need to be addressed in order to manage workforce capacity is health worker migration. Several authors have commented that health worker migration contributes to health worker shortages in low income countries and inequity in health care (Agwu and Llewelyn, 2009; O’Brien and Gostin, 2008). In fact, a system of “restitution” has been proposed, in which destination countries (generally high income countries) should compensate or reimburse the source countries (generally low income countries) (Mensah et al., 2005). One proposal to feasibly accomplish this is to shift development assistance toward building health systems in low
income countries (O’Brien and Gostin, 2008). If this directed foreign aid assists in the development of sustainable, rewarding, and credible health care-related career pathways in low income countries, this may decrease the supply of migrant health workers. Analogously, in order to decrease the demand for health worker migration, one proposal has been to increase the national self-sufficiency of the high income country health workforce and reduce reliance on recruitment of migrant health workers from low income countries (O’Brien and Gostin, 2008). In the midst of this debate, WHO has drafted a code of practice that addresses the issue of health worker migration, emphasizing that “the development of voluntary international standards and the coordination of national policies on international health worker recruitment are desirable in order to maximize the benefits to and mitigate the potential negative impact on countries and to safeguard the rights of health workers” (WHO, 2008a, p. 1). While there is no current consensus on solutions to this issue, it deserves attention as the global community proceeds to address the global CVD epidemic.
Integration of Care Disease-specific programs have had success in many areas of global health, but as fragmentation occurs, the need for service integration is emerging. Although there are too few evidence-based examples of successful CVD programs in developing countries to be able to assess the effects of fragmentation, it has affected aspects of the management of other chronic diseases such as TB and HIV in some regions. Both fragmentation and duplication of services are likely to be risks if CVD programs are implemented using a similar disease-specific approach (WHO Maximizing Positive Synergies Collaborative Group, 2009).
Integration of different types of service delivery is currently gaining attention in developing countries as health systems capacity needs to be improved to address chronic infectious diseases. This has the potential to be valuable for addressing chronic noncommunicable diseases as well. However, the evidence for integrating care is not yet convincing. Operational research is needed to provide information about the relative costs and benefits of vertical versus integrated health delivery. A move toward integration of care delivery should recognize the benefits of starting with a strong delivery system and the compatibility of the intervention protocols being integrated (Wallace et al., 2009). This is the basis on which economies of scale have a higher probability of being realized.
Integration approaches need to be selected according to the health issues being addressed, the population being targeted, the urgency of the need for services, the capability of the health systems and other contextual factors. Necessary to the success of integrating programs is the support of government officials and key stakeholders; the avoidance of overburdening existing services; sufficient staff training to implement integration; staff
workloads that can be managed to incorporate new responsibilities; overcoming discrimination; and factoring in initial costs (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
Also of important consideration when planning for integration of services are the needs for scale-up to the national level. These include political commitment, human resources, financing, coordinated program management, and effective decentralization (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009). Before the decision to expand programs is even made, the strength of the existing system and supports must be considered. After the existing system has been assessed, service integration can be phased in beginning with limited services at the community level and expanding gradually as services strengthen (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
Even though chronic disease prevention and treatment is becoming an increasingly important component of primary health care and primary health care is a growing area of emphasis on the global health agenda, there is limited evidence about how to effectively integrate care for chronic diseases into developing primary care systems (Beaglehole et al., 2008). Therefore, while integration is compelling in principle, there is still a need to develop and evaluate interventions to better integrate CVD with other care delivery programs, including maternal and child health programs and programs for prevention and management of chronic infectious diseases such as HIV/AIDS and TB.
In one example of an integrated care approach for chronic diseases, Médecins Sans Frontières (MSF) initiated an outpatient program in collaboration with the ministry of health of Cambodia that integrated diabetic and hypertension care in two hospital-based chronic disease clinics in rural high-prevalence, low-resource settings. The program featured standardized diagnosis and treatment protocols, multidisciplinary teams, and heavily subsidized care (Raguenaud et al., 2009). Compared to baseline values in the patient population, there were significant and clinically important mean improvements in glycemia and blood pressure that were sustained over the 5-year study period; however, a relatively low proportion of patients reached optimal treatment targets for diabetes control (Raguenaud et al., 2009). These results and the high loss to follow-up rate highlight the challenges of delivering diabetic care in rural, resource-limited settings.
Strategies to Change Structural Conditions Health care delivery can also be affected by changes in structural conditions. The Taskforce on Innovative International Financing for Health Systems (2009) recently considered potential mechanisms for structural changes as part of its review of ap-
proaches to support health systems strengthening. These changes can include approaches such as contracting, decentralization, adjusting the ratio of public and private provision of care and services, and innovative use of the private sector such as tailoring interventions to be implemented in nonhealth settings (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
Contracting can be employed by governments to, for example, subsidize the services of faith-based and other civil society providers or to contract with NGOs for their services. Government contracting with for-profit organizations has not been as extensively explored, although for-profits have been contracted for hospital and clinic management. Contracts can extend services quickly and to previously underserved areas and are often financed based on results. However, a contracting approach requires that governments must have the capacity to manage contracts and provide supervision. In addition, further study should be considered to explore the capacity of nonstate entities to provide large-scale, long-term services; the effects of introducing private contracts where public services already exist; the sustainability of contracts that depend on outside funding; and the implications of contracting out what might be regarded as core functions of the state (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
In one example in Cambodia, management of government health services was contracted out to NGOs in five selected districts that had randomly been made eligible for contracts that specified targets for improving maternal and child health services. The contracted services increased the availability of 24-hour service, reduced provider absence, and increased supervisory visits. The targeted outcomes improved relative to comparison districts, but changes in non-targeted outcomes were small. CVD-related health care activities were not measured in either set of outcomes. The program required increased public health funding, but this was roughly offset by reductions in private expenditure as residents in districts managed by the NGOs switched from unlicensed drug sellers and traditional healers to the provided clinics (Bloom et al., 2006).
Information Technology and E-Health2
Information is crucial for both clinical and public health practice. As described in Chapter 4, the use of electronic and mobile technologies is emerging in a range of global health contexts with the potential to be adapted or expanded to include chronic diseases. Investment in information and communication technology is an important potential component
of health care delivery for CVD and related chronic diseases. Electronic records are the focus of attention in industrialized countries and best practices are beginning to emerge (Fraser et al., 2005). Although challenging to implement, they hold potential for developing countries (Williams and Boren, 2008). In addition, communication technologies, such as mobile phones, are becoming increasingly common in developing countries (ITU, 2009) and are a potential mechanism to reach a wide representation of the population.
The importance of organized, efficient, and up-to-date information-gathering systems is illustrated by the experience of global HIV programs. Given the shared importance of long-term patient follow-up, the principles underlying successful developing country implementation of electronic records for HIV and TB care (Fraser et al., 2007) are quite relevant to CVD. OpenMRS, one example of an electronic medical records system for HIV/ AIDS care in several countries in Sub-Saharan Africa, demonstrates the use of information technology for clinical care, treatment adherence optimization, coordination with laboratory results, strategic planning, reports to national and donor agencies, and research (Allen et al., 2007; OpenMRS, 2010). This type of platform and information architecture can be expanded to include data for CVD care (Braitstein et al., 2009). The OpenMRS experience also illustrats potential benefits to be gained from sharing intellectual and human resources across universities, institutions, and countries. Such types of open formats and open-source software will be crucial elements of the information and communication technology-related aspects of future public health programs (Reidpath and Allotey, 2009).
In addition to better management of information, communications technology offers new mechanisms to deliver interventions. A recent review aimed to determine the effectiveness of telehealth in CHD management (Neubeck et al., 2009). Eleven studies were reviewed that evaluated telephone, videoconference, or web-based interventions and provided objective measurements of mortality, changes in multiple risk-factor levels, or quality of life. Telehealth interventions were associated with significantly lower total cholesterol and systolic blood pressure, and fewer smokers. These results support the potential for telehealth interventions to be adapted for use to address CVD in developing-country settings.
There have been some examples of intervention approaches using mobile health (m-health) technology in low and middle income countries, in some cases with applications for chronic diseases. UKIERI’s Mobile Disease Management System is a joint effort by engineers at universities in the United Kingdom and India. A monitoring system was developed that uses a mobile phone to collect up to four different physiological measures from patients, including electrocardiogram (ECG), blood pressure, oxygen satu-
ration, and blood glucose level. These are relayed to health professionals for remote assessment (Jadad, 2009).
MDNet creates free mobile phone networks to facilitate communication among physicians within countries in Africa. MDNet Ghana created the first country-wide mobile network of doctors. This made the first country-wide directory of physicians available, allowing for the delivery of bulk text messages to all physicians in Ghana and improving country-wide emergency response capabilities and communication. MDNet Liberia was subsequently launched as a partnership among the Liberian Ministry of Health, the Liberian Medical & Dental Association, and the Liberian Medical Board. After less than a year, the free communication network already linked 100 percent of physicians in the country (Jadad, 2009).
FrontlineSMS is a free open-source software application that allows a laptop and a mobile phone to be used to create a central communications hub. The program, which has been successfully tested in Malawi, enables text messages to be sent and received among large groups of users through mobile phones, without an Internet connection or need for additional training. This communication allows for timely remote support among health care professionals. FrontlineSMS:Medic works with any existing plan on all Global System for Mobile Communications (GSM) phones, modems, and networks and can be used anywhere in the world simply by switching the cell phone’s Subscriber Identity Module (SIM) card. Recently, FrontlineSMS:Medic has created a collaboration with Hope Phones, a U.S.-based nation-wide mobile phone collection campaign that supports m-health programs at medical clinics in more than 30 countries (Jadad, 2009).
Health Care Financing
The scope of financing health care delivery involves the following four components: (1) raising money, or raising revenue for health systems through general taxation and social insurance; community-based insurance; and private insurance; (2) pooling risk, which is the accumulation and management of revenue so that the risk of paying for health care is borne by all members of the pool (out-of-pocket payments are the least desirable method of pooling risk, yet are often a significant source of funding in low income countries); (3) purchasing services, which is how funds are allocated to lower levels of the health system, and how health providers are paid for the services they provide. This can be done through global budgets, capitation, fee-for-service, and specific incentive payments; and (4) financing the institutional framework of the health system (Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009).
Health care financing in developing countries has some significant differences that make it less equitable, less efficient, and less certain than
health financing in developed countries (Schieber et al., 2007; Taskforce on Innovative International Financing for Health Systems Working Group 1, 2009). Combining all sources, relatively little is spent on health in developing countries, far less than in richer countries. Taking into account variations in national data due to limitations in availability, reliability, and validity, WHO-standardized National Health Expenditure account data show that in 2006 low income countries spent, on average, 4.3 percent of gross domestic product (GDP) on health-related expenditures, lower-middle income countries 4.5 percent of GDP, upper-middle income countries 6.3 percent of GDP, and high income countries 11.2 percent of GDP (WHO, 2006). Instead of the social or private insurance systems or tax-funded systems of health care that prevail in developed countries, people in developing countries pay the bulk of their own health care expenses, and generally receive care from a mix of public and private settings—depending on their ability to pay and access. This section describes the sources of health care funding in developing countries, including donors, national governments, and individuals and households.
Global Donors Donor financing of health care is a significant share of total health expenditures in low income countries, much more so than in middle and high income countries. WHO reported that 17.2 percent of total health spending in low income countries came from external sources in 2006, an increase from 11.1 percent in 2000 (Figure 5.2) (WHO, 2006). This change over time reflects the rapidly rising amounts of external resources for health in recent years (Ravishankar et al., 2009).
National Governments and Health Systems National governments are fundamentally responsible for the health of their citizens and are the primary decision makers regarding health policy and resource allocations to health. However, national governments are not the primary financiers of health in poor countries. In low income countries, the public sector finances only 36.8 percent of all health care, compared to 61.6 percent in high income countries (WHO, 2006). Taxpayer-financed health care programs are more progressive than privately financed systems. A number of middle income developing countries—Chile, Mexico, Thailand, and others (Bastias et al., 2008; Frenk et al., 2009; Hu, 2010)—have created universal health insurance in part to help manage the financing needs of chronic conditions equitably.
The percentage of national health spending that goes to prevention, treatment, and care of CVD and related chronic diseases is not documented across countries. According to WHO’s Global Survey on the Progress in National Chronic Disease Prevention and Control, 68 percent of responding countries reported having a specific budget for chronic disease pre-
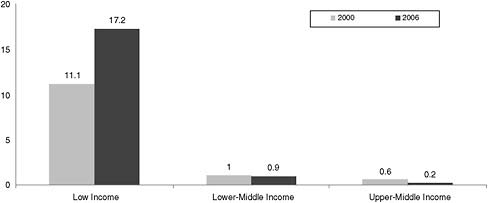
FIGURE 5.2 External resources as percentage of total expenditure on health.
SOURCE: World Health Organization National Health Accounts.
vention and control, ranging from a high of 83 percent in the South-East Asian region to a low of 58 percent in the African region (WHO, 2007b). Unfortunately, however, most developing countries do not maintain a sufficiently detailed national health account to allow national spending on CVD to be estimated.
Individuals and Households In developing-country settings, individual households bear the primary burden of financing health care needs beyond primary care because out-of-pocket spending is the predominant way that health care is financed. In a recent analysis of global health financing the average share of total health spending from out-of-pocket payments was 70 percent for low income countries, 43 percent for low-middle income countries, and 30 percent for upper-middle income countries. This was compared to 15 percent for high income countries (Scheiber et al., 2007).
The proportion of individual/household income spent on health care also varies markedly across low and middle income countries. In Nepal, on average, individuals spent 5.5 percent of their total per-capita expenditures on health (Hotchkiss et al., 1998), while in Guatemala, health expenditures are 16 percent of household income (McIntyre et al., 2006). Unofficial or “under the table” costs are an additional financial requirement placed on individuals in many low and middle income settings. In Bulgaria, unofficial payments were found to be common, averaging 21 percent of the minimum monthly salary for the country (Balabanova and McKee, 2002). In addition, lower income households generally pay more out-of-pocket for health care than wealthier households.
Knowledge is limited on the share of household health care costs spent
specifically on cardiovascular disease in low and middle income countries, but it is known that costs to the patient and caregivers are very high for chronic and long-term illness. Much of the data about household health expenditures for chronic illness comes from studies of spending related to malaria and HIV/AIDS (Babu et al., 2002; Goudge et al., 2009a, 2009b; Hansen et al., 1998).
Chapter 3 described the economic effects on households and frequent impoverishment that results from health spending. The consistency of this finding across very disparate countries suggests a need for health financing to pay for persistent health expenditures (Somkotra et al., 2009). An example is Seguro Popular in Mexico, which has succeeded in improving access to health services and improving blood glucose levels for poor diabetics (Sosa-Rubi et al., 2009). Another informative example for the design of health financing schemes for CVD is the Philippines health insurance plan (PhilHealth). The plan does not cover outpatient medicines and is spending more than $56 million annually on inpatient care for hypertension. Most households cannot afford the repeated expense of pharmacologic therapy. An outpatient medicines benefit could be a very cost-effective option to reduce intensive treatment for hypertension and relieve the burden on households of choosing between antihypertensives and other essential needs (Wagner et al., 2008).
Conclusion 5.3: Reduction of biological risk factors such as elevated blood pressure, blood lipids, and blood glucose can reduce individual risk for CVD. However, implementation of these approaches requires an adequate health systems infrastructure, including a trained workforce and sufficient supplies with equitable access to affordable essential medicines and diagnostic, preventive, and treatment technologies. Many countries do not currently have sufficient infrastructural capacity. Current efforts to strengthen health systems in many low and middle income countries provide an opportunity to improve delivery of high-quality care to prevent and manage CVD, including chronic care approaches that are applicable to other chronic diseases and infectious diseases requiring chronic management, such as HIV/AIDS.
Recommendation: Include Chronic Diseases in Health Systems Strengthening
Current and future efforts to strengthen health systems and health care delivery funded and implemented by multilateral agencies, bilateral public health and development agencies, leading international nongovernmental organizations, and national and subnational health authorities should include attention to evidence-based prevention, di-
agnosis, and management of CVD. This should include developing and evaluating approaches to build local workforce capacity and to implement services for CVD that are integrated with primary health care services, management of chronic infectious diseases, and maternal and child health.
Community-Based Intervention Approaches
Health behaviors and health status are influenced by many nonbiological factors, including economic, political, cultural, and socioeconomic factors (Schooler et al., 1997; Stokols, 1992, 1996). Health care focusing on the individual and relying primarily on clinical services provided by physicians can neither prevent most chronic disease nor reach the entire population in need. Therefore, efforts to change behavior and improve health will be more successful if they go beyond the individual to include family, social, and cultural contexts. A primary tenet of community prevention programs is the opportunity to intervene in multiple settings and domains, focusing on the interdependencies among environmental, social, and individual factors and the potential for public health strategies to interact with individual-level therapeutic and medical strategies (Farquhar and Fortmann, 2007; Kasl, 1980; Schooler et al., 1997; Shea and Basch, 1990a).
Community-based programs offer an opportunity to approximate the ideal multicomponent approach described at the beginning of this chapter by coordinating population-based policy and health communication and education strategies with intervention programs in local communities. Social norms and community attributes have an important impact on health. Governmental and private institutions in the community influence health behaviors by controlling, for example, health, recreational, and transportation services and youth access to tobacco. The health and safety policies and worksite health promotion practices of businesses can also affect health. Stores and restaurants also shape health when they determine what types of food to sell (Schooler et al., 1997).
Thus, the ideal program design would include programs established through worksites, schools, recreation sites, libraries, churches, local business organizations, and other sites in order to supplement and expand the effects of policy and health education approaches and appropriate delivery of health care. This broad reach into the community is advantageous because nearly all people in a community are at some level of risk for CVD and may benefit from interventions to encourage and reinforce healthful behavior, leading to potential population impact on highly prevalent risk factors. In fact, most CVD does not occur among the relatively few adults at highest risk, but rather than among the many at modeeate risk (Blackburn, 1983; Kottke et al., 1985; Puska et al., 1985; Schooler et al., 1997). There-
fore, promotion of cardiovascular health has to happen at a population level and among people who may not be engaged with the health system or particularly motivated to reduce a possible distant risk of CVD.
While some behavior change reflects only an individual recognizing risk and deciding to reduce that risk, a population-wide impact may be more than the accumulation of individual risk assessments; rather, diffusion of behavior change may reflect a social process—individuals learning about new behaviors from neighbors, or individuals being encouraged to adopt new behaviors by people important to them in their social networks. This sort of social diffusion will likely result best from increasing opportunities to learn about and implement new behaviors, with an accompanying increase in social expectations for doing so. This requires building a surrounding environment that coherently and consistently favors behavior change. In addition to the policy changes and large-scale communications campaigns described earlier in this chapter, this total environmental change may be accomplished through the work of entrepreneurs recognizing a growing market and developing new products to accelerate behavior change, through workplaces that fund wellness programs, through schools that modify food available to children and require physical activity, and through programs in other settings in the community. Thus, the goal is to create a cascade of behavior change, and that may come from the synergistic interactive effects that can occur when individual components are embedded in a total community-based program campaign that encourages institutional change, leaves space for entrepreneurs, and includes mass media and environmental change (Schooler et al., 1997).
A multifactor community intervention approach also has the potential to act synergistically with clinical services rendered by physicians and other health professionals. Adherence to dietary and exercise advice from health care professionals may be easier to follow when family members, friends, and colleagues are aware of and are practicing some of the same principles. Motivation to adhere to medication regimens may also be easier when others in the patient’s social network have also learned the importance, for example, of controlling blood pressure and blood lipids. Health professionals, and the sites of their practices, have the potential to contribute to the “total push” for better health by, for example, making print materials on health available and publicizing forthcoming health fairs and other events. Classes can be made available in hospital and other clinical settings. The local media can call upon local health professionals to speak and to contribute to the “health news.”
In summary, comprehensive community-based efforts that include multiple types of interventions can be designed to modify the environment in ways that support healthy or inhibit unhealthy individual actions, to create organizational and institutional support for programs, and to influence
the knowledge, attitudes, and behaviors of individuals (Schooler et al., 1997). However, it is important to take a pragmatic view on implementing community-based programs. There is good reason to be skeptical about investing in programs that rely on institutions for whom reducing the CVD burden is not central to their primary missions. For workplaces, schools, and community organizations the advantages may be abstractly logical as a way to reach people and provide needed services, but implementing these approaches is often not logical in practice, especially for long-term viability.
Community-level organizations may not be able to commit limited resources to programs over the long term if the incentives for doing so are weak and the interventions are complex to implement, manage, and maintain. The programs may dissipate even if there is early enthusiasm, and there is very little knowledge about what it will take to put such programs together and diffuse them on a large scale in low and middle income countries. For example, businesses that have insurance incentives to reduce smoking and obesity might invest in CVD prevention programs, but there is not a lot of precedent for long-term sustainability and effectiveness in high income countries—and the potential incentives for businesses in low and middle income countries are even less clear. Similarly, physical activity may be central in some schools, but schools may not be able to stay engaged if there is competition for limited resources with their primary academic mission. The infrastructure and capacity may be even more fragile in other less formalized community organizations.
CVD-Related Community-Based Programs in Low and Middle Income Countries
Although the evidence for successful implementation of multicomponent programs in community settings is reasonably strong in high income countries, it is weak in middle income countries and nearly absent in low income countries. Some community programs in middle income countries, because their efforts relied heavily on the use of mass media, were described earlier in this chapter, including programs in South Africa (Rossouw et al., 1993), Brazil (Matsudo, 2002), the Czech Republic (Komarek, 1995), and Poland (Ruszkowsk-Majzel and Drygas, 2005).
Another example of a “total country” effort in Mauritius, a middle income country, was also described previously because the effect was mainly due to a change in agriculture and food policy. Multiple approaches were organized with the goal of combating rising CVD risk factors, including mass media; fiscal and legislative measures; and widespread community, school, and workplace health education activities (Dowse et al., 1995; Hodge et al., 1996; Uusitalo et al., 1996). Total cholesterol fell due to a government-sponsored switch from palm to soybean oil. However, body
weights rose and there were no other effects on CVD risk factors (Uusitalo et al., 1996). This is testimony to the fact that secular trends can overcome educational and organizational efforts to combat obesity and hypertension. The Mauritian investigators described their findings as highlighting “the difficulty of reversing the adverse effects of lifestyle change in rapidly modernizing countries” (Hodge et al., 1996, p. 137). This may be an example of the difficulty that many low and middle income countries will face during economic development, while CVD risk factors and CVD events are rising.
Potential Lessons from CVD-Related Community Trials in High Income Countries
The evidence for effective community-based programs in high income countries is mixed, and the reasons for success and failure can provide some useful lessons to inform the design of future efforts to adapt these programs for trials in low and middle income settings. A wave of successful community trials in the 1970s and 1980s in the United States, Finland, Australia, Switzerland, and Italy were described earlier in this chapter because, although they involved a number of intervention components, a dominance of broadcast and print mass media underlied their success in reducing smoking, blood pressure, and body weight. These were followed by five later high income country studies in the United States, Sweden, Holland, Denmark, and Germany that demonstrated only limited success. These studies included intervention components such as broadcast and print media, classes, clinical screening, community events, policy changes, school programs, and close involvement of civic and business leaders. These programs have all been described extensively elsewhere (Schooler et al., 1997) and therefore are not described in detail here. Rather this discussion focuses on the potential lessons learned that could inform the design of future interventions in low and middle income countries.
A key factor of success was the extent of the use of broadcast and print mass media. Indeed, one of the possible reasons for the lack of robust results in the Minnesota Heart Health Project and the Pawtucket Heart Health Project in Rhode Island (Carleton et al., 1995; Luepker et al., 1996) was the diversion of resources for education efforts into community events, school programs, and clinical screening, resulting in a relatively low use of broadcast media compared to the more successful Stanford and North Karelia projects (Farquhar et al., 1977; Puska et al., 1995). This reinforces an emphasis on health communications campaigns as a greater priority for intervention strategies to address CVD than other kinds of community programs, especially in the short term. In addition, the overall community effects were not materially improved with the addition of a high-risk com-
ponent in the Three Community Study, the Australian study, nor the CORIS project in South Africa (Schooler et al., 1997).
Another factor of success is local community participation and support, which was exemplified in the Stanford Five City Project (Farquhar et al., 1990; Flora et al., 1993; Mittelmark et al., 1993). This may indicate that affinity and cooperation with local health and education resources is a predictor of both initial success and longer-term maintenance of an intervention. The successful Norsjo project in Sweden (Weinehall et al., 2001) and Hartslag-Limburg project in the Netherlands (Schuit et al., 2006), both of which made efforts to target low income residents, also show that local community support is important. Another important factor in these two projects was linkage to their excellent health care systems, which unfortunately in many low and middle income countries is not available.
Another characteristic of successful programs in high income countries is the length of the intervention. The Slangerup project in Denmark was of 1-year duration and led to no differences in classical risk factors between the intervention and control area (Osler and Jespersen, 1993), perhaps to be expected from the brevity and relatively low intensity of the interventions.
The “dose” and the likely cost of community interventions are especially important to consider in determining the feasibility of replicating an intervention design. However, there are many country-specific determinants for both so the information may have limited generalizability, and in any case it is rare for either of these to be reported except in very general terms. For the Stanford Five City Project, there were about 100 exposures per year for each adult from all varieties of educational experience for an intervention dose of about 5 hours of exposure for each adult per year (Farquhar et al., 1990). Of these, about 70 per year were from broadcast media, for less than 1 hour per year. In comparison, each adult’s exposure to television advertising of all types during the early 1980s was estimated at 292 hours per year, of which one-third contained often misleading health-related content (Farquhar et al., 1990; Schooler et al., 1997). The yearly delivery cost during 5 years at the time, excluding research, was found to be close to $4 per capita per year (Farquhar et al., 1990). Therefore, both delivery costs and message exposure are relatively low for the result achieved, which was a 16 percent fall in total CHD risk (Farquhar et al., 1990). The previous Stanford Three Community Study also had a quite low-cost broadcast and print mass media approach, with a 23 percent net reduction in overall CVD risk (Schooler et al., 1997; Shea and Basch, 1990b).
These levels of estimated CVD risk reduction were comparable to that found in the first 5 years of the Finnish North Karelia project, which was later translated into a very large decrease in CVD events, including mortality. An assessment of the cost savings from the first 20 years of the project
offers some sense of the potential for monetary returns from investments in well-designed and well-implemented community-based interventions (Puska et al., 2009). Given the very large drop in CVD in North Karelia, the proportional reduction in CVD-related costs within the province itself, a population of about 180,000, was estimated to be about $30 million for the 20th year (1992) alone (Puska et al., 2009). Although the Finnish authors warn that this is a “crude estimate,” this would translate into a much larger total over all 20 years.
To determine feasibility for adaptation and replication it is also eminently desirable that maintenance and dissemination should follow the major effort of a demonstration project or intervention trial. Unfortunately, in high income countries it has been uncommon for health promotion to continue in force after the main research phase of CVD community-based interventions. Two major exceptions to this are found in the Stanford Five City Project and the NKP. In the former, the health department of Monterey County in Northern California, where the project occurred, was the major continuation force, and the county’s political leadership was a critical supporter of this expansion. In the later years of the research phase, the health department began to support project activities, indicating a trend toward maintenance by the community. Thereafter, county activities moved into health promotion for all residents, with attention to chronic disease prevention needs and of the growing Hispanic population (Flora et al., 1993; Monterey County Health Department, 2007). A recent activity enlisted the local Mexican-American owners of 35 Taquerias to include healthier items on their menus, including a switch from lard to vegetable oils in their cooking (Hanni et al., 2009). Successes in the initial and subsequent health promotion activities have engendered continued support by the county’s government, its residents, the voluntary health agencies, and the health system.
In the case of North Karelia, the ministry of health of Finland adopted and augmented the methods in a remarkable expansion throughout Finland, so both maintenance and dissemination occurred (Puska et al., 1995, 2009). Expansion began in earnest after the first 5 years of the project, when the national health authorities adopted the education methods and added major policy changes in agriculture (e.g., a switch to margarine from butter and from dairying to berry farming) and public health policy. The public enthusiasm in the province was also disseminated nation-wide (e.g., through the powerful housewives association “Martta”). The expansion was successful because the effects of the NKP in reducing CVD mortality were seen within 5 years, the economic benefits became clear to the nation’s leaders, and the international acceptance of the lessons of North Karelia reinforced the Finnish government’s support.
Therefore, maintenance is achieved in settings where public health
institutions and their political leadership adopt and support continuation of health promotion methods. Such support is founded on demonstrated success in changing health patterns and in a common understanding of the science behind the need for change. Initiation by respected academic institutions, public awareness of the health problems being addressed, and enlightened leadership are essential.
Potential Lessons from Community-Based Programs Targeting HIV/AIDS in Low and Middle Income Countries
Community-based methods analogous to those used in high and middle income countries to target CVD have been used to target other outcomes in low and middle income countries, such as HIV/AIDS; this provides some reason for optimism regarding transferability of these approaches. These methods include community organizing and mobilizing, use of mass media for social marketing to total community populations, policy interventions, and reliance on the concept of diffusion of innovation.
As an example, after widespread media-based social marketing, condom sales in Zaire increased from fewer than 1 million per year in 1987 to more than 18 million in 1991 (Auerbach and Coates, 2000). Policy interventions also can effectively change social norms and behaviors to promote HIV prevention, as shown in the “100% Condom Program” initiated by the government of Thailand in 1990. This program made condom use mandatory in all brothels and was implemented in the community through partnerships among brothel owners, police, and public health clinics. Among sex workers there was a 90 percent increase in consistent condom use and a 75 percent decrease in sexually transmitted diseases. In addition, among military recruits, who frequent brothels, the prevalence of HIV infection declined from about 11 percent before to 6.7 percent after the policy change was enacted (Auerbach and Coates, 2000). The strategy of community organizing and mass media to mobilize at the community level has been effective in increasing condom sales and distribution in a variety of populations in Sub-Saharan Africa including truckers, urban and peri-urban adults, male miners, adolescents, and men and women seeking services for sexually transmitted infections. “Project Accept” used community mobilization to increase counseling and testing, thus increasing the rate of HIV testing, knowledge of status, and frequency of discussions about HIV. They did so through social marketing that increased adoption of needed innovations and fit the criteria of “diffusion theory” (Rogers, 1962). In one aspect of this type of intervention, Project Accept recruited indigenous opinion leaders as change agents to use their social networks to increase adoption (Khumalo-Sakutukwa et al., 2008).
As described in these examples, the community intervention strategies
that have been important to the success of CVD community-based interventions in high income countries have been used successfully in HIV/AIDS interventions in developing countries. This is a strong indication that these strategies will be transferable to the design of CVD interventions that are appropriate to the culture present in any particular country.
Intervention Components Implemented in Community Settings in Low and Middle Income Countries
Although very few multicomponent community-based approaches have been reported in low and middle income countries, there have been some documented interventions that have been implemented and evaluated in trials in community facilities or in community settings in low and middle income countries. These are not comprehensive, multicomponent, community-based programs, but they are discussed here for their potential to offer lessons learned and to be considered as components or rationale for the design of future community-based programs.
A project in China targeted sodium intake, hypertension, and other CVD risk factors in the city of Tianjin (Nissinen et al., 2001; Tian et al., 1995; Yu et al., 1999, 2000). The intervention included activities such as health education and a community-based hypertensive management system with local health worker visits. Population surveys at a 7-year interval showed mixed effects on CVD risk factors, including blood pressure, smoking, and obesity (Yu et al., 1999, 2000). A specific sodium reduction project was also carried out within the Tianjin project. In collaboration with local health workers, lay people were trained to implement health education efforts, which included the door-to-door dissemination of nutrition information leaflets, posters and stickers at food retail stores, and health exhibitions. Other interventions included the distribution of smaller teaspoons to measure salt used in cooking and the availability of mineral salt in retail stores in the intervention areas. A comparison of geographically defined intervention areas to reference areas showed significant reductions over the 3-year project period in sodium intake in men and in systolic blood pressure in the total population (Tian et al., 1995).
Randomized trials in a rural community in China (The China Salt Substitute Study Collaborative Group, 2007) and in retirement homes in Taiwan (Chang et al., 2006) have also demonstrated effectiveness in salt reduction efforts. In the China Salt Substitute Study, participants were randomly assigned to replace their household salt with either the study salt substitute or normal salt for a 12-month period. At follow-up, systolic blood pressure was significantly lower in the salt-substitute group than in the normal salt group, with no differences in diastolic blood pressure (The China Salt Substitute Study Collaborative Group, 2007). In Taiwan, five kitchens of a
veteran retirement home were randomized into two groups, and veterans assigned to those kitchens were given either potassium-enriched salt or regular salt for 31 months. The substitution of potassium-enriched salt reduced the CVD mortality hazard ratio to 60 percent that of the control group, and the experimental group had a longer life expectancy than did the control group. However, the authors note that the effect may primarily be due to the increase in potassium intake, because the sodium reduction achieved was moderate (Chang et al., 2006).
A small double-blind controlled trial in South Africa determined that the modification of salt in commonly consumed foods significantly lowered blood pressure in hypertensive participants of low socioeconomic status. In this 8-week study among 80 Cape Town residents aged 50-75 years with mild to moderate hypertension, the intervention group had five commonly consumed food items (brown bread, margarine, stock cubes, soup mixes, and flavor enhancer) with reduced sodium content and modified potassium, magnesium, and calcium content delivered to them. The control group was provided the same foods, but of standard commercial composition (Charlton et al., 2008). Results showed a significantly gre0ater reduction in blood pressure from baseline to post intervention in the intervention group compared to the control group (Charlton et al., 2008). The results of this study further support the positive effects of blood pressure reduction through consumption of products with modified salt contents. However, the short duration and small sample size of this study warrant considerations when generalizing results. In addition, the direct provision of food in this study is not likely to be feasible to replicate on a large scale.
A project on salt reduction from Ghana provides important lessons on intervention approaches delivered in community settings in a low income country (Cappuccio et al., 2006). The Ghana Salt Reduction Study was a project in which 12 villages were randomized into intervention and control. In each condition, half were rural and half semi-urban. Education was provided by indigenous health workers in 1-hour meetings in communal areas, weekly for 6 months. A small but significant reduction in diastolic blood pressure occurred, but without a between-group urinary sodium difference. However, an anticipated correlation was shown within all samples between urinary sodium and systolic blood pressure. Also, a significant difference between the rural and semi-urban samples occurred, with lower blood pressures in the rural villages. The major lesson is that in Sub-Saharan villages, including those without electricity or piped water, a moderately successful intervention can be mounted, probably at reasonably low cost. Initial commitment made through tribal leaders and village elders represented successful use of a method analogous to one of the initial steps in any successful high income country’s community-based intervention. The results, although not robust, represent an example of successfully carrying out a community-
based intervention trial that may have applicability in many Sub-Saharan locales and in other low income countries.
Another small randomized cross-over trial recently evaluated an education-based intervention in Jamaica and Nigeria. Individuals were allocated to either a low-salt diet or a high-salt diet with additional salt added to the participants’ normal diet. This was followed by a washout period and a cross-over phase. During the low-salt phase, individuals were given case managers to provide information and counseling. Jamaican participants were also provided with low-sodium spices and were offered the option of purchasing specially prepared low-sodium food at their own expense (Forrester et al., 2005). The trial showed reductions in sodium intake and systolic blood pressure of an average of 5 mmHg in normotensive adults. However, this was a very brief and small study of only 114 participants with only 3 weeks on the low-sodium diet in the cross-over design (Forrester et al., 2005). Therefore, it is difficult to determine the feasibility of delivering the intervention more widely and the likelihood of longer-term adherence to the low-salt diet.
Principles to Guide Future Design and Evaluation of Community-Based Programs
Despite the strong rationale for the approach, there is very limited evidence demonstrating effectiveness and successful implementation of broad multicomponent community-based approaches to reduce CVD or risk for CVD in developing countries. The capacity for planned community organizing that favors reduction in CVD risk has been demonstrated, on a very limited scale, in middle income settings in China, Mauritius, and South Africa and in low income settings in Ghana, Jamaica, and Nigeria, although evidence for effectiveness was limited in these programs. In addition, mass media-based community interventions with community-level organization have succeeded in middle income countries, as described earlier in this chapter. However, these are diverse examples that make it difficult to extract any comprehensive findings to apply broadly. Lifestyles, such as tobacco use, dietary habits, and exercise patterns, are strongly influenced by custom and culture. In addition, resources and capacity can be quite limited and varied in developing-country communities. Therefore, based on the available documented evidence, multifactor community-based prevention approaches for CVD are not ready to be implemented widely at scale in developing countries.
However, three decades of trials of the “total community” health promotion approach for CVD prevention in high income settings support the potential feasibility of these approaches and the potential to result in significant changes in health habits of populations. Therefore, these approaches
hold promise as a potential component of comprehensive approaches to address global CVD, and the critical next step is better setting-specific design and evaluation of demonstration projects and subsequent dissemination of these approaches. Transferability of the methods and components used in high income countries is not assured. However, theories of self-efficacy and common biological attributes, such as responses to nutrients and to nicotine, allow some prediction of transferability. The use of similar principles in successful HIV/AIDS interventions in developing countries is also a strong indication that these strategies will be transferable to the design of CVD interventions, with attention to message design and appropriateness to the culture specific to any particular country.
The methods for the design of the approaches in high income countries have been reviewed extensively elsewhere (Farquhar and Fortmann, 2007), and only a few key messages that relate to transferability to low and middle income country settings are repeated here. The steps needed to design and evaluate community-based programs include problem identification; organizing the community; planning, design, and implementation; evaluation; changes based on evaluation results; maintenance; and dissemination. Organizing and educating communities requires advocacy, activism, coalition building, and leadership. Regulatory change can enhance the success of community efforts. In addition, community-level efficacy that can result when the population gains self-efficacy through education can enhance capacity to change institutional policy and practice, thus maintaining community change. Theory and intervention methods matter, an adequate reach and duration of health communication is needed, and use of well-designed electronic and print media can provide education that is more cost-effective than that provided by more intensive classroom approaches. Intervention effectiveness requires formative evaluation, both before onset and during the intervention period. This ensures cultural appropriateness through tailoring and adapting messages to a particular community. A strong evaluation design is also critical, including assessments not only of outcomes but also of economic feasibility and implementation strategies, such as mobilizing communities and training interventionists.
Schools and Worksites
Schools and worksites have received particular attention as settings that offer an opportunity to implement prevention programs, whether implemented individually or as a synergistic part of the integrated approach described above. Therefore, these specific components are discussed separately here.
School-Based Interventions Schools provide one possible setting for delivering interventions to promote healthful eating and exercise in children. Health education programs that are integrated into academic curricula have a greater potential to be accepted by school administrators, teachers, parents, and students. School-based programs can also be readily incorporated into family-based and community-based chronic disease prevention projects that target a wide range of chronic disease risk factors in children and adults. Many schools have limited access to healthful foods and inadequate physical education facilities and hours. Thus, school-based programs can potentially have synergistic effects if physical education and classroom health education are implemented alongside broader changes in physical environment, food services, and policies.
School-based and other programs targeted to children and adolescents are discussed in full in Chapter 6. In summary, intensive, longer-term social influence-oriented programs have been effective to reduce tobacco use in youth. There is some evidence to support physical education-based approaches, school-environmental approaches, and integrated multicomponent approaches to increase physical activity and physical fitness among children. In addition, school-environment changes and policy-oriented approaches to improve diet and physical activity and reduce childhood obesity have been studied. Reducing sugar-sweetened beverages has promise to prevent childhood obesity, and reduction of screen time, especially TV watching, is a potential avenue to reduce childhood obesity, improve diet, and increase physical activity. There is little evidence that school-based programs significantly affect intermediate CVD risk factors such as blood pressure, blood lipids, or blood glucose.
Like many of the intervention components discussed in this chapter, it is very important to note that the vast majority of these studies were conducted in high income countries, with very little evidence from low and middle income countries. In addition, a number of methodological problems have hindered the interpretation of the results and the development of best practice recommendations in school-based interventions. These include small sample sizes, short duration, nonrandomized design, high attrition rate, lack of theoretical framework, low intervention intensity, inadequate assessment tools for diet, physical activity, and adiposity in children. There have also been no economic analyses of these intervention programs. Many of the interventions do not seem to have high resource requirements if a sufficient school infrastructure is already in place, so there is some potential for successful adaptation in settings that are analogous to the high income country settings in which these programs have been evaluated. However, evaluations of interventions adapted to local contexts are needed to inform future implementation of school-based approaches.
Workplace Interventions The workplace has historically been a common site of public health interventions. It will continue to be an important site for CVD prevention and health promotion activities in the context of the global spread of CVD. Several large corporations in developed countries, recognizing both the economic and social responsibility rationales, have initiated programs aimed at improving the health behaviors of their employees. In addition, several corporations in a variety of industries have instituted tobacco-free workplace policies, independent of local and state tobacco regulations. The World Economic Forum (WEF) and WHO (WHO and WEF, 2008) jointly produced a report that reviewed wellness-in-the-workplace programs targeting chronic disease risk factors.
The WEF/WHO report identified the following elements as critical to the success of workplace interventions: (1) establishing clear goals and objectives and linking health promotion programs to business objectives; (2) clear and strong support of the management; (3) adopting a multistake-holder approach and securing the involvement of government agencies and ministries, NGOs, trade unions, and employees at all levels of the corporation; (4) creating supportive environments; (5) adapting the intervention to social norms and building social support; and (6) considering incentives to foster adherence to the programs and improving self-efficacy of the participants.
The report found that such programs improve health, increase productivity, and reduce health care costs. Indeed, workplace interventions in diet, physical activity, and tobacco cessation are beneficial to both the employee and the employer. Such programs have been shown to reduce absenteeism, workers’ compensation, and job stress and increase worker health and job satisfaction. In a review of worksite health promotion studies, Chapman (2003) reported a 27 percent average reduction in sick leave absenteeism, a 26 percent average reduction in health care costs, and a 32 percent average reduction in workers’ compensation and disability claim costs. However, it should be noted that the majority of studies that have examined the effectiveness and the economic impact of workplace interventions have occurred in high income countries, and cost-effectiveness data for workplace interventions are still not largely available.
Muévete Bogotá is one of only a few examples of a well-documented program implemented in workplaces in a developing-country setting. This program seeks to increase physical activity by means of a media campaign coupled with programs aimed at changing behavior tied to physical activity (Gamez et al., 2006). The interventions within the program take place in various settings, but workplace interventions to promote physical activity are the program’s main focus (Bauman et al., 2005). Muévete has been successful in gaining strong support of workplace managers through regular training and capacity-building sessions. Additionally, the program draws
in and prepares partner companies for program implementation through advisory services. This approach has garnered the involvement of stakeholders such as the Secretary of Health of Bogotá, the Colombian Heart Association, the Colombian Diabetes Association, university departments, the Fundación FES Social/Bogotá, the U.S. Centers for Disease Control and Prevention, and the Pan American Health Organization (Gamez et al., 2006). Although process measures indicate successful implementation of the program, there has been little analysis of effects on levels of physical activity or on health outcomes (Bauman et al., 2005; Gamez et al., 2006). In addition, it is worth noting that although the program has been a model for programs throughout Latin America, considerations for transferability need to include the availability of adequate human resources and funding for interventions carried out by companies (Bauman et al., 2005).
Another example of a successful worksite intervention was recently described in India (Prabhakaran et al., 2009). A combination of individual-and population-based intervention activities, as well as health fairs and group motivational sessions, yielded superior results with respect to risk-factor control such as lipids, blood pressure, and waist circumference. Health-related behaviors such as tobacco use, fruit consumption, salt consumption, and physical activity all were better among the industrial groups who received the workplace intervention. Another workplace intervention in China’s Capital Steel and Iron Company demonstrated benefits in health-related knowledge, salt intake, blood pressure, and stroke mortality. The intervention included strategies for health education and promotion as well as strategies for individual detection and management of hypertension (Chen et al., 2008).
In Malaysia, a quasi-experimental study was conducted among Malay-Muslim male security guards working in a public university in Kuala Lumpur (intervention group) and men working in the teaching hospital of the same university (comparison group). The intervention group members received intensive individual and group counseling on diet, physical activity, and quitting smoking and showed a significant reduction in their mean total cholesterol levels as compared with the comparison group at a 2-year follow-up. The intervention group also reported a reduction in the amount of cigarettes smoked (Moy et al., 2006). Although implemented in a limited population, this example is useful in demonstrating how the adoption of healthy behaviors can be incorporated into workplace policies.
There remain gaps in the current knowledge about the optimum workplace intervention characteristics, especially in low income countries. These include data on effectiveness of programs on risk-factor control, cost–benefit analysis of various programs and models, whether healthful behavior in the workplace translates into healthful behavior at home, and the impact on health outcomes such as myocardial infarction and stroke. In
addition, practical issues still need to be clarified and resolved, such as the incorporation of diet and physical activity interventions in the workplace, development of validated instruments for diet and physical activity evaluation, cost-sharing agreements between government agencies and the private sector, and taking into account local cultural factors, size of businesses, and informal worksites (Leurent et al., 2008).
CONCLUSION
Risk for CVD can be modified through a combination of individual-level and population-level interventions. For some of these risk factors, reductions have been successfully achieved through health promotion and prevention programs in some countries and communities. Because of its broad determinants, it is clear that the prevention of CVD extends beyond the realm of the health sector. A coordinated approach at the governmental level is required so that policies in non-health sectors of government can be developed synergistically to promote, or at least not adversely affect, cardiovascular health. This is especially important for those sectors involved in agriculture, urban development, transportation, education, and in the private sector.
However, most policies and programs with evidence of effectiveness have been developed and implemented in high income countries. Even in high income countries little population-level progress has been made in some areas, such as obesity-related risk factors including total calorie consumption and reduction of sedentary behavior. Adaptations to the culture, resources, and capacities of specific settings are required for interventions to have an impact in low and middle income countries.
Reduction of risk for CVD through clinical interventions requires an adequate health systems infrastructure, including a trained workforce and sufficient supplies with equitable access to affordable essential medicines and diagnostic, preventive, and treatment technologies. Many countries do not currently have sufficient infrastructural capacity. Current efforts to strengthen health systems in many low and middle income countries provide an opportunity to improve delivery of high-quality care to prevent and manage CVD, including chronic care approaches that are applicable to other chronic diseases and infectious diseases requiring chronic management, such as HIV/AIDS.
Conclusion 5.4: Developing countries will want to focus efforts on goals that promise to be economically feasible, have the highest likelihood of intervention success, and have the largest morbidity impact. While priorities will vary across countries, the evidence suggests that substantial progress in reducing CVD can be made in the near term
through a prioritized subset of goals and intervention approaches, including tobacco control, reduction of salt in the food supply and in consumption, and improved delivery of clinical prevention using pharmaceutical interventions in high-risk patients. Many countries will want to focus their efforts on achieving these goals on the grounds that they have limited financial and human resources and political energy to allocate to CVD programming, that the evidence for lowered CVD morbidity associated with achieving these goals is credible, and that there are examples of successful implementation of programs in each of these focus areas with the potential to be adapted for low and middle income countries.
Local context matters enormously for the planning and implementation of any of the approaches to prevent and manage CVD described in this chapter. Context also influences the effectiveness of these approaches. While there are common needs and priorities across settings, each site has its own specific needs that require evaluation. Knowledge needs to be developed on how to implement programs with proven effectiveness in settings where resources of all types are scarce, where priorities remain fixed on other health and development agendas, and where there might be cultural and influences vary. Implementation and translational research will be critical to develop and evaluate interventions in the settings in which they are intended to be implemented.
REFERENCES
Accenture. 2010. High performance in a volatile world: Seven imperatives for acheiving dynamic supply chains. https://microsite.accenture.com/management_consulting/dynamic-supply-chains/Pages/default.aspx (accessed February 3, 2010).
Adult Treatment Panel III. 2002. Detection, evaluation, and treatment of high blood cholesterol in adults: Final report. Bethesda, MD: National Institutes of Health.
Agwu, K., and M. Llewelyn. 2009. Compensation for the brain drain from developing countries. Lancet 373(9676):1665-1666.
Allen, C., D. Jazayeri, J. Miranda, P. G. Biondich, B. W. Mamlin, B. A. Wolfe, C. Seebregts, N. Lesh, W. M. Tierney, and H. S. Fraser. 2007. Experience in implementing the OpenMRS medical record system to support HIV treatment in Rwanda. Studies in Health Technology and Informatics 129(Pt 1):382-386.
Altman, D. G., J. A. Flora, S. P. Fortmann, and J. W. Farquhar. 1987. The cost-effectiveness of three smoking cessation programs. American Journal of Public Health 77(2):162-165.
Andersson, K., G. Bergstrom, M. G. Petzold, and A. Carlsten. 2007. Impact of a generic substitution reform on patients’ and society’s expenditure for pharmaceuticals. Health Policy 81(2-3):376-384.
Angell, S. Y., L. D. Silver, G. P. Goldstein, C. M. Johnson, D. R. Deitcher, T. R. Frieden, and M. T. Bassett. 2009. Cholesterol control beyond the clinic: New York City’s trans fat restriction. Annals of Internal Medicine 151(2):129-134.
Asfaw, A. 2006. Do government food prices affect the prevalence of obesity? Empirical evidence from Egypt. World Development 35(4):687-701.
Auerbach, J., and T. Coates. 2000. HIV prevention research: Accomplishments and challenges for the third decade of AIDS. American Journal of Public Health 90(7):1029-1032.
Babu, B. V., A. N. Nayak, K. Dhal, A. S. Acharya, P. K. Jangid, and G. Mallick. 2002. The economic loss due to treatment costs and work loss to individuals with chronic lymphatic filariasis in rural communities of Orissa, India. Acta Tropica 82(1):31-38.
Bahit, M., C. Granger, K. Alexander, J. Kramer, et al. 2000. Applying the evidence: Opportunity in U.S. for 80,000 additional lives saved per year (abstract). Circulation 102(Suppl 2).
Balabanova, D., and M. McKee. 2002. Understanding informal payments for health care: The example of Bulgaria. Health Policy 62(3):243-273.
Balcazar, H., M. Alvarado, M. L. Hollen, Y. Gonzalez-Cruz, and V. Pedregon. 2005. Evaluation of salud para su corazon (health for your heart)—national council of La Raza promotora outreach program. Preventing Chronic Disease 2(3):A09.
Balcazar, H., M. Alvarado, F. Cantu, V. Pedregon, and R. Fulwood. 2009. A promotora de salud model for addressing cardiovascular disease risk factors in the U.S.-Mexico border region. Preventing Chronic Disease 6(1):A02.
Bandura, A., D. Ross, and S. A. Ross. 1963. Imitation of film-mediated agressive models. Journal of Abnormal and Social Psychology 66:3-11.
Bannink, L., S. Wells, J. Broad, T. Riddell, and R. Jackson. 2006. Web-based assessment of cardiovascular disease risk in routine primary care practice in New Zealand: The first 18,000 patients (predict CVD-1). New Zealand Medical Journal 119(1245):U2313.
Barrera, A. Z., E. J. Pérez-Stable, K. L. Delucchi, and R. F. Muñoz. 2009. Global reach of an internet smoking cessation intervention among spanish- and english-speaking smokers from 157 countries. International Journal of Environmental Research and Public Health 6(3):927-940.
Basinga, P., P. Gertler, A. Binagwaho, A. Soucat, J. Sturdy, and C. Vermeersch. 2009. Impact of paying primary health care centers for performance in Rwanda. Washington, DC: World Bank.
Bastias, G., T. Pantoja, T. Leisewitz, and V. Zárate. 2008. Health care reform in Chile. Canadian Medical Association Journal 179(12):1289-1292.
Bauman, A., S. Schoeppe, and M. Lewicka. 2005. Review of best practice in interventions to promote physical activity in developing countries: Background document prepared for the WHO workshop on physical activity and public health. Edited by T. Armstrong, V. Candeias, and J. Richards. Geneva: World Health Organization.
Beaglehole, R., J. Epping-Jordan, V. Patel, M. Chopra, S. Ebrahim, M. Kidd, and A. Haines. 2008. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet 372(9642): 940-949.
Berman, P. A. 1984. Village health workers in Java, Indonesia: Coverage and equity. Social Science and Medicine 19(4):411-422.
Bertrand, J. T., K. O’Reilly, J. Denison, R. Anhang, and M. Sweat. 2006. Systematic review of the effectiveness of mass communication programs to change HIV/AIDS-related behaviors in developing countries. Health Education Research 21(4):567-597.
Bjorkman, M., and J. Svensson. 2007. Power to the people: Evidence from a randomized field experiment of a community-based monitoring project in Uganda. Washington, DC: World Bank.
Blackburn, H. 1983. Research and demonstration projects in community cardiovascular disease prevention. Journal of Public Health Policy 4(4):398-421.
Bloom, E., E. King, I. Bhushan, M. Kremer, D. Clingingsmith, B. Loevinsohn, R. Hong, and J. B. Schwartz. 2006. Contracting for health: Evidence from Cambodia. Unpublished working paper. Washington, DC: Brookings Institution.
Boberg, E. W., D. H. Gustafson, R. P. Hawkins, C.-L. Chan, E. Bricker, S. Pingree, H. Berhe, and A. Peressini. 1995. Development, acceptance, and use patterns of a computer-based education and social support system for people living with AIDS/HIV infection. Computers in Human Behavior 11(2):289-311.
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness. JAMA 288(14):1775-1779.
Borght, S. V. D., V. Janssens, M. S. V. D. Loeff, A. Kajemba, H. Rijckborst, J. Lange, and T. R. D. Wit. 2009. The accelerating access initiative: Experience with a multinational workplace programme in Africa. Bulletin of the World Health Organization 87:794-798.
Braitstein, P., R. M. Einterz, J. E. Sidle, S. Kimaiyo, W. Tierney, P. Braitstein, R. M. Einterz, J. E. Sidle, S. Kimaiyo, and W. Tierney. 2009. “Talkin’ about a revolution”: How electronic health records can facilitate the scale-up of HIV care and treatment and catalyze primary care in resource-constrained settings. Journal of Acquired Immune Deficiency Syndromes 52(Suppl 1):S54-S57.
Breckenkamp, J., U. Laaser, and S. Meyer. 1995. The German cardiovascular prevention study: Social gradient for the net effects in the prevention of hypercholesterolemia. Zeitschrift fur Kardiologie 84(9):694-699.
Breslow, L., and M. Johnson. 1993. California’s Proposition 99 on tobacco, and its impact. Annual Review of Public Health 14:585-604.
Brook, R. D. 2008. Cardiovascular effects of air pollution. Clinical Science 115(5-6): 175-187.
Brown, E., and M. Jacobson. 2005. Cruel oil: How palm oil harms health, rainforest & wildlife. Washington, DC: Center for Science in the Public Interest.
Brownell, K. D., and T. R. Frieden. 2009. Ounces of prevention: The public policy case for taxes on sugared beverages. New England Journal of Medicine 860(18):1805-1808.
Brownstein, J. N., L. R. Bone, C. R. Dennison, M. N. Hill, M. T. Kim, and D. M. Levine. 2005. Community health workers as interventionists in the prevention and control of heart disease and stroke. American Journal of Prevention 29(551):128-133.
Brugts, J. J., T. Yetgin, S. E. Hoeks, A. M. Gotto, J. Shepherd, R. G. J. Westendorp, A. J. M. de Craen, R. H. Knopp, H. Nakamura, P. Ridker, R. van Domburg, and J. W. Deckers. 2009. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: Meta-analysis of randomised controlled trials. British Medical Journal 338:b2376.
Bump, J. B., M. R. Reich, O. Adeyi, and S. Khetrapal. 2009. Towards a political economy of tobacco control in low- and middle-income countries. Washington, DC: World Bank.
Cameron, A., M. Ewen, D. Ross-Degnan, D. Ball, and R. Laing. 2009. Medicine prices, availability, and affordability in 36 developing and middle-income countries: A secondary analysis. Lancet 373(9659):240-249.
Campbell, S. M., D. Reeves, E. Kontopantelis, B. Sibbald, and M. Roland. 2009. Effects of pay for performance on the quality of primary care in England. New England Journal of Medicine 361(4):368-378.
Canadian Hypertension Education Program. 2009. 2009 CHEP recommendations for the management of hypertension http://hypertension.ca/chep/wp-content/uploads/2009/04/09-complete-recs.pdf (accessed December 10, 2009).
Cappuccio, F. P., S. M. Kerry, F. B. Micah, J. Plange-Rhule, and J. B. Eastwood. 2006. A community programme to reduce salt intake and blood pressure in Ghana. BMC Public Health 6:13.
Carleton, R. A., T. M. Lasater, A. R. Assaf, H. A. Feldman, and S. McKinlay. 1995. The Pawtucket heart health program: Community changes in cardiovascular risk factors and projected disease risk. American Journal of Public Health 85(6):777-785.
Cash, S., D. Sunding, and D. Zilberman. 2005. Fat taxes and thin subsidies: Prices, diet, and health outcomes. Acta Agriculturae Scandinavica, Section C—Economy 2:167-174.
CDC (U.S. Centers for Disease Control and Prevention). 2003. Promising practices in chronic disease prevention and control: A public health framework for action. Atlanta, GA: Department of Health and Human Services.
CDC. 2009a. Capacity and development news: Working together for a healthier world. Spring 2009 Newsletter. Atlanta, GA: CDC.
CDC. 2009b. Division of Global Public Health and Capacity Development 2008 Field Epidemiology Training Program. Atlanta, GA. Washington, DC: U.S. Department of Health and Human Services.
Chang, H.-Y., Y.-W. Hu, C.-S. J. Yue, Y.-W. Wen, W.-T. Yeh, L.-S. Hsu, S.-Y. Tsai, and W.-H. Pan. 2006. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. American Journal of Clinical Nutrition 83(6):1289-1296.
Chapman, L. 2003. Meta evaluation of worksite health promotion economic return studies. Art of Health Promotion 6(5):1-16.
Charlton, K. E., K. Steyn, N. S. Levitt, N. Peer, D. Jonathan, T. Gogela, K. Rossouw, N. Gwebushe, and C. J. Lombard. 2008. A food-based dietary strategy lowers blood pressure in a low socio-economic setting: A randomised study in South Africa. Public Health Nutrition 11(12):1397-1406.
Chen, C., and F. C. Lu. 2004. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomedical and Environmental Sciences 17 Suppl:1-36.
Chen, J., X. Wu, and D. Gu. 2008. Hypertension and cardiovascular diseases intervention in the Capital Steel and Iron Company and Beijing Fangshan community. Obesity Review 9 (Suppl 1):142-145.
Chen, L., T. Evans, S. Anand, J. I. Boufford, H. Brown, M. Chowdhury, M. Cueto, L. Dare, G. Dussault, G. Elzinga, E. Fee, D. Habte, P. Hanvoravongchai, M. Jacobs, C. Kurowski, S. Michael, A. Pablos-Mendez, N. Sewankambo, G. Solimano, B. Stilwell, A. de Waal, and S. Wibulpolprasert. 2004. Human resources for health: Overcoming the crisis. Lancet 364(9449):1984-1990.
The China Salt Substitute Study Collaborative Group. 2007. Salt substitution: A low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. Journal of Hypertension 25(10):2011-2018.
Clarke, D., and T. McKenzie. 2007. Legislative interventions to prevent and decrease obesity in Pacific Island countries: Report prepared for WHO Western Pacific Regional Office. Geneva: WHO.
Committee for Revision of Chinese Guidelines for Prevention and Treatment of Patients with Hypertension. 2005. Chinese guidelines for prevention and treatment of patients with hypertension [in Chinese]. Chinese Journal of Hypertension 134:2-41.
Committee on the State of the USA Health Indicators. 2009. State of the USA Health Indicators: Letter report. Washington, DC: The National Academies Press.
Cooper, R. S., C. N. Rotimi, J. S. Kaufman, W. F. Muna, and G. A. Mensah. 1998. Hypertension treatment and control in Sub-Saharan Africa: The epidemiological basis for policy. British Medical Journal 316(7131):614-617.
Council of Supply Chain Management Professionals. 2010. Council of Supply Chain Management Professionals. http://cscmp.org/ (accessed February 3, 2010).
Crisp, N., B. Gawanas, and I. Sharp. 2008. Training the health workforce: Scaling up, saving lives. Lancet 371(9613):689-691.
da Costa, L. M., and S. Goldfarb. 2003. Government Leadership in Tobacco Control: Brazil’s Experience. In Tobacco control policy: Strategies, successes, and setbacks, edited by J. de Beyer and L. W. Brigden. Washington, DC: The World Bank and The International Development Research Centre.
de Beyer, J., and L. W. Brigden, eds. 2003. Tobacco control policy: Strategies, successes, and setbacks. Washington, DC: World Bank and International Development Research Centre.
Devers, K. J., H. H. Pham, and G. Liu. 2004. What is driving hospitals’ patient-safety efforts? Health Affairs 23(2):103-115.
Donabedian, A. 1988. The quality of care: how can it be assessed? Journal of the American Medical Association 260(12):1743-1748.
Donatelle, R. J., S. L. Prows, D. Champeau, and D. Hudson. 2000. Randomised controlled trial using social support and financial incentives for high risk pregnant smokers: Significant other supporter (SOS) program. Tobacco Control 9(90003):67-69.
Dowse, G. K., H. Gareeboo, K. G. Alberti, P. Zimmet, J. Tuomilehto, A. Purran, D. Fareed, P. Chitson, and V. R. Collins. 1995. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non-communicable disease intervention programme in Mauritius. Mauritius Non-communicable Disease Study Group. British Medical Journal 311(7015):1255-1259.
Drewnowski, A. 2004. Obesity and the food environment: Dietary energy density and diet costs. American Journal of Preventive Medicine 27(3 Suppl):154-162.
Ebrahim, S., A. Beswick, M. Burke, and G. Davey Smith. 2006. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database of Systematic Reviews (4):CD001561.
Efroymson, D., and S. Ahmed. 2003. Building momentum for tobacco control: The case of Bangladesh. In Tobacco control policy: Strategies, successes, and setbacks, edited by J. de Beyer and L. W. Brigden. Washington, DC: The World Bank and The International Development Research Center.
Eichler, R., R. Levine, and the Performance-Based Incentives Working Group. 2009. Performance incentives for global health: Potential and pitfalls. Washington, DC: Center for Global Development.
Einterz, R. M., S. Kimaiyo, H. N. Mengech, B. O. Khwa-Otsyula, F. Esamai, F. Quigley, and J. J. Mamlin. 2007. Responding to the HIV pandemic: The power of an academic medical partnership. Academic Medicine 82(8):812-818.
Emery, S. L., G. Szczypka, L. M. Powell, and F. J. Chaloupka. 2007. Public health obesity-related T.V. advertising: Lessons learned from tobacco. American Journal of Preventive Medicine 33(4 Suppl):S257-S263.
Epstein, A. M. 2007. Pay for performance at the tipping point. New England Journal of Medicine 356(5):515-517.
Evans, M., R. C. Sinclair, C. Fusimalohi, and V. Liava’a. 2001. Globalization, diet, and health: An example from Tonga. Bulletin of the World Health Organization 79:856-862.
Faber, M. P., M. M. Bosch, H. M. D. P. Wollersheim, S. P. Leatherman, and R. P. Grol. 2009. Public reporting in health care: How do consumers use quality-of-care information?: A systematic review. Medical Care 47(1):1-8.
Faeh, D., J. William, L. Tappy, E. Ravussin, and P. Bovet. 2007. Prevalence, awareness and control of diabetes in the Seychelles and relationship with excess body weight. BMC Public Health 7:163.
Farquhar, J., and S. Fortmann. 2007. Community-based health promotion. In Handbook of epidemiology. Vol. 11. Edited by W. Ahrens and I. Peugot. Berlin Heidelberg: Springer-Verlag. Pp. 1306-1321.
Farquhar, J. W., N. Maccoby, P. D. Wood, J. K. Alexander, H. Breitrose, B. W. Brown, Jr., W. L. Haskell, A. L. McAlister, A. J. Meyer, J. D. Nash, and M. P. Stern. 1977. Community education for cardiovascular health. Lancet 1(8023):1192-1195.
Farquhar, J. W., S. P. Fortmann, J. A. Flora, C. B. Taylor, W. L. Haskell, P. T. Williams, N. Maccoby, and P. D. Wood. 1990. Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. Journal of the American Medical Association 264(3):359-365.
Feachem, R. G., N. K. Sekhri, and K. L. White. 2002. Getting more for their dollar: A comparison of the NHS with California’s Kaiser Permanente. British Medical Journal 324(7330):135-141.
Fernald, L. C., P. J. Gertler, and X. Hou. 2008a. Cash component of conditional cash transfer program is associated with higher body mass index and blood pressure in adults. Journal of Nutrition 138(11):2250-2257.
Fernald, L. C. H., P. J. Gertler, and L. M. Neufeld. 2008b. Role of cash in conditional cash transfer programmes for child health, growth, and development: An analysis of Mexicos oportunidades. Lancet 371(9615):828-837.
Fichtenberg, C. M., and S. A. Glantz. 2000. Association of the California tobacco control program with declines in cigarette consumption and mortality from heart disease. New England Journal of Medicine 343(24):1772-1777.
Flora, J. A., R. C. Lefebvre, D. M. Murray, E. J. Stone, A. Assaf, M. B. Mittelmark, and J. R. Finnegan, Jr. 1993. A community education monitoring system: Methods from the Stanford Five-City Project, the Minnesota Heart Health Program and the Pawtucket Heart Health Program. Health Education Research 8(1):81-95.
Forrester, T., A. Adeyemo, S. Soarres-Wynter, L. Sargent, F. Bennett, R. Wilks, A. Luke, E. Prewitt, H. Kramer, and R. S. Cooper. 2005. A randomized trial on sodium reduction in two developing countries. Journal of Human Hypertension 19(1):55-60.
Fraser, H., P. Biondich, B. Mamlin, et al. 2005. Deploying electronic medical record systems in developing countries. Primary Care Informatics 13:88-95.
Fraser, H., C. Allen, C. Bailey, G. Douglas, S. Shin, and J. Blaya. 2007. Information systems for patient follow-up and chronic management of HIV and tuberculosis: A life-saving technology in resource-poor areas. Journal of Medical Internet Research 9(4):e29.
Frenk, J., O. Gomez-Dantes, and F. M. Knaul. 2009. The democratization of health in Mexico: Financial innovations for universal coverage. Bulletin of the World Health Organization 87(7):542-548.
Frieden, T. R., and M. R. Bloomberg. 2007. How to prevent 100 million deaths from tobacco. Lancet 369(9574):1758-1761.
Fung, C. H., Y.-W. Lim, S. Mattke, C. Damberg, and P. G. Shekelle. 2008. Systematic review: The evidence that publishing patient care performance data improves quality of care. Annals of Internal Medicine 148(2):111-123.
Fuster, V., ed. 2009. The AHA guidelines and scientific statements handbook. Sussex, UK: Wiley-Blackwell.
Gajalakshmi, V., R. Peto, T. S. Kanaka, P. Jha, V. Gajalakshmi, R. Peto, T. S. Kanaka, and P. Jha. 2003. Smoking and mortality from tuberculosis and other diseases in India: Retrospective study of 43,000 adult male deaths and 35,000 controls.[see comment]. Lancet 362(9383):507-515.
Gamez, R., D. Parra, M. Pratt, and T. L. Schmid. 2006. Muévete Bogotá: Promoting physical activity with a network of partner companies. Promotion et Education 13(2):138-143, 164-169.
Genest, J., R. McPherson, J. Frohlich, T. Anderson, N. Campbell, A. Carpentier, P. Couture, R. Dufour, G. Fodor, G. A. Francis, S. Grover, M. Gupta, R. A. Hegele, D. C. Lau, L. Leiter, G. F. Lewis, E. Lonn, G. B. Mancini, D. Ng, G. J. Pearson, A. Sniderman, J. A. Stone, and E. Ur. 2009. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Canadian Journal of Cardiology 25(10):567-579.
Giné, X., D. Karlan, and J. Zinman. 2008. Put your money where your butt is: A commitment contract for smoking cessation. Washington, DC: World Bank.
Giuffrida, A., and D. J. Torgerson. 1997. Should we pay the patient? Review of financial incentives to enhance patient compliance. British Medical Journal 315(7110):703-707.
The Global Fund (The Global Fund to Fight AIDS, Tuberculosis and Malaria). 2009. Guidelines to the Global Fund’s policies on procurement and supply management. Geneva: The Global Fund to Fight AIDS, Tuberculosis and Malaria.
Global Health Workforce Alliance. no date. Highlights. http://www.who.int/workforce alliance/en/ (accessed August 27, 2009).
Goldman, L., and S. Glantz. 1998. Evaluation of antismoking advertising campaigns. Journal of the American Medical Association 279(10):772-777.
Gooch, L. 2009. Success of palm oil brings plantations under pressure to preserve habitats. The New York Times, September 18.
Goudge, J., L. Gilson, S. Russell, T. Gumede, and A. Mills. 2009a. Affordability, availability and acceptability barriers to health care for the chronically ill: Longitudinal case studies from South Africa. BMC Health Services Research 9:75.
Goudge, J., L. Gilson, S. Russell, T. Gumede, and A. Mills. 2009b. The household costs of health care in rural South Africa with free public primary care and hospital exemptions for the poor. Tropical Medicine and International Health 14(4):458-467.
Goyal, A., and S. Yusuf. 2006. The burden of cardiovascular disease in the Indian subcontinent. Indian Journal of Medical Research 124(3):235-244.
Grabowsky, T. A., J. W. Farquhar, K. R. Sunnarborg, V. S. Bales, and Stanford University School of Medicine. 1997. Worldwide efforts to improve heart health: A follow-up to the Catalonia Declaration—selected program descriptions. http://www.internationalhearthealth.org/Publications/catalonia.pdf (accessed February 5, 2009).
Graham, I., D. Atar, K. Borch-Johnsen, G. Boysen, G. Burell, R. Cifkova, J. Dallongeville, G. D. Backer, S. Ebrahim, B. Gjelsvikg, C. Herrmann-Lingen, A. Hoes, S. Humphries, M. Knapton, J. Perk, S. G. Priori, K. Pyorala, Z. Reiner, L. Ruilope, S. Sans-Menendez, W. S. O. Reimer, P. Weissberg, D. Woods, J. Yarnell, and J. L. Zamorano. 2007. European guidelines on cardiovascular disease prevention in clinical practice: Fourth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice. European Journal of Cardiovascular Prevention and Rehabilitation 14(Suppl 2):S1-S113.
Greiser, E. 1993. Risk factor trends and cardiovascular mortality risk after 3.5 years of community-based intervention in the German cardiovascular prevention study. Annals of Epidemiology 3:S13-S27.
Grimshaw, J. M., R. E. Thomas, G. MacLennan, C. Fraser, C. R. Ramsay, L. Vale, P. Whitty, M. P. Eccles, L. Matowe, L. Shirran, M. Wensing, R. Dijkstra, and C. Donaldson. 2004. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technology Assessment 8(6):iii-iv, 1-72.
Grossbart, S. R. 2006. What’s the return? Assessing the effect of “pay-for-performance” initiatives on the quality of care delivery. Medical Care Research and Review 63(Suppl 1):29S-48S.
Gwatkin, D. R., A. Bhuiya, and C. G. Victora. 2004. Making health systems more equitable. Lancet 364(9441):1273-1280.
Hanni, K. D., E. Garcia, C. Ellemberg, and M. Winkleby. 2009. Steps to a healthier Salinas: Targeting the taqueria: Implementing healthy food options at Mexican American restaurants. Health Promotion Practice 10(Suppl 2):91S-99S.
Hansen, K., G. Woelk, H. Jackson, R. Kerkhoven, N. Manjonjori, P. Maramba, J. Mutambirwa, E. Ndimande, and E. Vera. 1998. The cost of home-based care for HIV/AIDS patients in Zimbabwe. AIDS Care 10(6):751-759.
Hawkes, C. 2006. Agricultural and food policy for cardiovascular health in Latin America. Prevention and Control 2(3):137-147.
Hawkins, R. P., D. H. Gustafson, P. M. Day, B. Chewning, and K. Bosworth. 1987. Interactive computer programs as public information campaigns for hard-to-reach populations: The barn project example. Journal of Communication 37(2):8-28.
He, F. J., and G. A. MacGregor. 2009. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. Journal of Human Hypertension 23(6):363-384.
Hibbard, J. H. 2008. What can we say about the impact of public reporting? Inconsistent execution yields variable results. Annals of Internal Medicine 148(2):160-161.
Hodge, A. M., G. K. Dowse, H. Gareeboo, J. Tuomilehto, K. G. Alberti, and P. Z. Zimmet. 1996. Incidence, increasing prevalence, and predictors of change in obesity and fat distribution over 5 years in the rapidly developing population of Mauritius. International Journal of Obesity and Related Metabolic Disorders 20(2):137-146.
Holt, S. 2009. Time to implement the polypill approach. New Zealand Medical Journal 122(1296):88-89.
Hornik, R., and E. McAnany. 2001. Mass media and fertility change. In Diffusion processes and fertility transition. Edited by J. Casterline. Washington, DC: National Academy Press. Pp. 208-239.
Hornik, R., J. McDivitt, S. Zimicki, P. S. Yoder, E. C. Budge, J. McDowell, and M. Rasmuson. 2002. Communication in support of child survival: Evidence and explanations from eight countries. In Public health communication: Evidence for behavior change. Mahwah, NJ: Lawrence Erlbaum.
Hotchkiss, D. R., J. J. Rous, K. Karmacharya, and P. Sangraula. 1998. Household health expenditures in Nepal: Implications for health care financing reform. Health Policy and Planning 13(4):371-383.
Houpt, E. R., and R. L. Guerrant. 2008. Technology in global health: The need for essential diagnostics. Lancet 372(9642):873-874.
Hu, J. 2010. The role of health insurance in improving health services use by thais and ethnic minority migrants. Asia-Pacific Journal of Public Health 22(1):42-50.
Huicho, L., R. W. Scherpbier, A. M. Nkowane, and C. G. Victora. 2008. How much does quality of child care vary between health workers with differing durations of training? An observational multicountry study. Lancet 372(9642):910-916.
Humpel, N., N. Owen, and E. Leslie. 2002. Environmental factors associated with adults’ participation in physical activity: A review. Am J Prev Med 22(3):188-199.
Hysong, S. J. P. 2009. Meta-analysis: Audit and feedback features impact effectiveness on care quality. Medical Care 47(3):356-363.
Ibrahim, M. M., H. Rizk, L. J. Appel, W. E. Aroussy, S. Helmy, Y. Sharaf, Z. Ashour, H. Kandil, E. Roccella, and P. K. Whelton. 1995. Hypertension prevalence, awareness, treatment, and control in Egypt: Results from the Egyptian national hypertension project (NHP). Hypertension 26(6):886-890.
Immelt, J., V. Govindarajan, and C. Trimble. 2009. How GE is disrupting itself. Harvard Business Review. October 2009.
Inui, T. S., W. M. Nyandiko, S. N. Kimaiyo, R. M. Frankel, T. Muriuki, J. J. Mamlin, R. M. Einterz, and J. E. Sidle. 2007. Ampath: Living proof that no one has to die from HIV. Journal of General Internal Medicine 22(12):1745-1750.
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2009. Local government actions to prevent childhood obesity. Washington, DC: The National Academies Press.
IOM. 2010. Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. Washington, DC: The National Academies Press.
ITU (International Telecommunications Union). 2009. Key global telecom indicators for the world telecommunication service sector. http://www.itu.int/ITU-D/ict/statistics/at_glance/Key Telecom99.html (accessed March 12, 2010).
Jadad, A. 2009. Preventing and managing cardiovascular diseases in the age of mHealth and global telecommunications: Lessons from low- and middle-income countries. Prepared for the Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease in Developing Countries. Toronto, Canada.
James, W. P., A. Ralph, and C. P. Sanchez-Castillo. 1987. The dominance of salt in manufactured food in the sodium intake of affluent societies. Lancet 1(8530):426-429.
Jamison, D. 2006. Effective strategies for noncommunicable diseases, risk factors, and behaviors. In Priorities in health. Edited by D. Jamison, J. Breman, A. Measham, G. Alleyne, M. Claeson, D. Evans, P. Jha, A. Mills, and P. Musgrove. New York: Oxford University Press. Chapter 5.
Jamtvedt, G., J. M. Young, D. T. Kristoffersen, M. A. O’Brien, and A. D. Oxman. 2006. Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback. Quality & Safety in Health Care 15(6):433-436.
Jean, M.-C., and L. St-Pierre. 2009. Applicability of the success factors for intersectorality in developing countries. France: IUHPE. Background paper commissioned by the Committee.
Jha, P., F. J. Chaloupka, M. Corrao, and B. Jacob. 2006. Reducing the burden of smoking world-wide: Effectiveness of interventions and their coverage. Drug and Alcohol Review 25(6):597-609.
Joshi, R., S. Jan, Y. Wu, and S. MacMahon. 2008. Global inequalities in access to cardiovascular health care: Our greatest challenge. Journal of the American College of Cardiology 52(23):1817-1825.
Justman, J., S. P. Koblavi-Deme, A. Tanuri, A. B. A. Goldberg, L. F. Gonzalez, and C. R. P. Gwynn. 2009. Developing laboratory systems and infrastructure for HIV scale-up: A tool for health systems strengthening in resource-limited settings. Journal of Acquired Immune Deficiency Syndromes 52(Suppl 1):S30-S33.
Kahn, E. B., L. T. Ramsey, R. Brownson, et al. 2002. The effectiveness of interventions to increase physical activity: a systematic review. American Journal of Preventive Medicine 22(4S):73-107.
Kane, R. L., G. Keckhafer, S. Flood, B. Bershadsky, and M. S. Siadaty. 2003. The effect of evercare on hospital use. Journal of the American Geriatrics Society 51(10):1427-1434.
Kane, R. L., P. E. Johnson, R. J. Town, and M. Butler. 2004. A structured review of the effect of economic incentives on consumers’ preventive behavior. American Journal of Preventive Medicine 27(4):327-352.
Kannel, W. B., D. McGee, and T. Gordon. 1976. A general cardiovascular risk profile: The Framingham study. American Journal of Cardiology 38(1):46-51.
Kasl, S. V. 1980. Cardiovascular risk reduction in a community setting: Some comments. Journal of Consulting and Clinical Psychology 48(2):143-149.
Kelley, E., C. Geslin, S. Djibrina, and M. Boucar. 2001. Improving performance with clinical standards: The impact of feedback on compliance with the integrated management of childhood illness algorithm in Niger, West Africa. The International Journal of Health Planning and Management 16(3):195-205.
Kelley, E., A. G. Kelley, C. H. T. Simpara, O. Sidibé, and M. Makinen. 2003. The impact of self-assessment on provider performance in Mali. The International Journal of Health Planning and Management 18(1):41-48.
Khumalo-Sakutukwa, G., S. F. Morin, K. Fritz, E. D. Charlebois, H. van Rooyen, A. Chingono, P. Modiba, K. Mrumbi, S. Visrutaratna, B. Singh, M. Sweat, D. D. Celentano, and T. J. Coates. 2008. Project Accept (hptn 043): A community-based intervention to reduce HIV incidence in populations at risk for HIV in Sub-Saharan Africa and Thailand. Journal of Acquired Immune Deficiency Syndromes 49(4):422-431.
Kinaxis. 2010. Four essential requirements for today’s global supply chain management. http://www.kinaxis.com/whitepapers/Four-Essential-Supply-Chain-Management-Requirements.cfm (accessed February 3, 2010).
Klingbeil, G. E., and I. G. Fiedler. 1988. Continuity of care. A teaching model. American Journal of Physical Medicine and Rehabilitation 67(2):77-81.
Komarek, L., V. Kebza, L. Lhotska, K. Osancova, J. Janovska, J. Okenkova, Z. Roth, J. Vignerova, J. Potockova, R. J. Havel, C. L. Albright, J. W. Farquhar, R. Poledne, M. Andel, J. Malkova, P. Kraml, H. Bartakova, D. Herman, S. Palmer, and I. Stankova. 1995. “Healthy Dubec” design of a joint Czech-American community project for the reduction of cardiovascular and cerebrovascular disease (adapted from American experience). Central European Journal of Public Health 3(4):230-233.
Kotseva, K., D. Wood, G. De Backer, D. De Bacquer, K. Pyorala, and U. Keil. 2009a. Cardio-vascular prevention guidelines in daily practice: A comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 373(9667):929-940.
Kotseva, K., D. Wood, G. De Backer, D. De Bacquer, K. Pyorala, U. Keil, and Euroaspire Study Group. 2009b. EUROASPIRE III: A survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. European Journal of Cardiovascular Prevention & Rehabilitation 16(2):121-137.
Kottke, T., P. Puska, J. T. Salonen, J. Tuomilehto, and A. Nissinen. 1985. Projected effects of high-risk versus population-based prevention strategies in coronary heart disease. American Journal of Epidemiology 121(5):697-704.
Kruk, M. E., and L. P. Freedman. 2008. Assessing health system performance in developing countries: A review of the literature. Health Policy 85(3):263-276.
Lagarde, M., A. Haines, and N. Palmer. 2009. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews. http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD008137/frame.html (accessed November 10, 2009).
Langrish, J. P., N. L. Mills, and D. E. Newby. 2008. Air pollution: The new cardiovascular risk factor. Internal Medicine Journal 38(12):875-878.
Lehman, U., and D. A. Sanders. 2007. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs, and impact on health outcomes of using community health workers. Geneva: World Health Organization.
Lehman, U., I. Friedman, and D. Sanders. 2004. Review of the utilisation and effectiveness of community-based health workers in Africa: Joint Learning Initiative on Human Resources for Health and Development working paper.
Lehmann, U., W. Van Damme, F. Barten, and D. Sanders. 2009. Task shifting: The answer to the human resources crisis in Africa? Human Resources for Health 7(1):49.
Leurent, H., K. S. Reddy, J. Voute, and D. Yach. 2008. Wellness in the workplace: A multi-stakeholder health-promoting initiative of the World Economic Forum. American Journal of Health Promotion 22(6):379-380, ii.
Levy, J. A., and R. Strombeck. 2002. Health benefits and risks of the internet. Journal of Medical Systems 26(6):495-510.
Lewin, S., J. N. Lavis, A. D. Oxman, G. Bastias, M. Chopra, A. Ciapponi, S. Flottorp, S. G. Marti, T. Pantoja, G. Rada, N. Souza, S. Treweek, C. S. Wiysonge, and A. Haines. 2008. Supporting the delivery of cost-effective interventions in primary health-care systems in low-income and middle-income countries: An overview of systematic reviews. Lancet 372(9642):928-939.
Lindenauer, P. K., D. Remus, S. Roman, M. B. Rothberg, E. M. Benjamin, A. Ma, and D. W. Bratzler. 2007. Public reporting and pay for performance in hospital quality improvement. New England Journal of Medicine 356(5):486-496.
Liu, Y., K. Rao, J. Wu, and E. Gakidou. 2008. China’s health system performance. Lancet 372(9653):1914-1923.
Loevinsohn, B. P., E. T. Guerrero, and S. P. Gregorio. 1995. Improving primary health care through systematic supervision: A controlled field trial. Health Policy and Planning 10(2):144-153.
Lu, W., X. Li, M. Chen, Y. Zhang, Y. Qian, S. Chen, and D. Zhu. 2009. Clinical studyClinical study for disease management of hypertension in Shanghai community hospitals: DMaP-Shanghai. PowerPoint Presentation. Shanghai: Shanghai Municipal Center for Disease Control and Prevention.
Luck, J., and R. Shimkhada. 2009. The Effectiveness and Impact of Measurement to Improve Health. Prepared for the Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease in Developing Countries. Los Angeles, CA.
Luepker, R. V., L. Rastam, P. J. Hannan, D. M. Murray, C. Gray, W. L. Baker, R. Crow, D. R. Jacobs, Jr., P. L. Pirie, S. R. Mascioli, M. B. Mittelmark, and H. Blackburn. 1996. Community education for cardiovascular disease prevention. Morbidity and mortality results from the Minnesota Heart Health Program. American Journal of Epidemiology 144(4):351-362.
Ma’ayeh, S. 2002. Jordan: Mass media campaign combating smoking requires serious commitment and not just words. http://www.who.int/tobacco/training/success_stories/en/best_practices_jordan_media.pdf (accessed June 20, 2009).
Maibach, E., J. A. Flora, and C. Nass. 1991. Changes in self-efficacy and health behavior in response to a minimal contact community health campaign. Health Communication 3(1):1-15.
Malan, M., and R. Leaver. 2003. Political Change in South Africa: New Tobacco Control and Public Health Policies. In Tobacco control policy: Strategies, successes, and setbacks, edited by J. de Beyer and L. W. Brigden. Washington, DC: The World Bank and The International Development Research Center.
Marshall, M. N., P. G. Shekelle, S. Leatherman, and R. H. Brook. 2000. The public release of performance data: What do we expect to gain? A review of the evidence. Journal of the American Medical Association 283(14):1866-1874.
Matsudo, S. M., and V. R. Matsudo. 2006. Coalitions and networks: Facilitating global physical activity promotion. Promotion and Education 13(2):133-138, 158-163.
Matsudo, S. M., V. R. Matsudo, T. L. Araujo, D. R. Andrade, E. L. Andrade, L. C. de Oliveira, and G. F. Braggion. 2003. The agita São Paulo program as a model for using physical activity to promote health. Revista Panamericana de Salud Publica 14(4):265-272.
Matsudo, S. M., V. R. Matsudo, D. R. Andrade, T. L. Araújo, E. Andrade, L. d. Oliveira, and G. Braggion. 2004. Physical activity promotion: Experiences and evaluation of the agita São Paulo program using the ecological mobile model. Journal of Physical Activity and Health 1(2):81-94.
Matsudo, V. 2002. The agita São Paulo experience in promoting physical activity. West Indian Medical Journal 51(Suppl 1):48-50.
Matsudo, V., S. Matsudo, D. Andrade, T. Araujo, E. Andrade, L. C. de Oliveira, and G. Braggion. 2002. Promotion of physical activity in a developing country: The agita São Paulo experience. Public Health and Nutrition 5(1A):253-261.
McAlister, F. A., F. M. Lawson, K. K. Teo, and P. W. Armstrong. 2001. Randomised trials of secondary prevention programmes in coronary heart disease: Systematic review. British Medical Journal 323(7319):957-962.
McIntyre, D., M. Thiede, G. Dahlgren, M. Whitehead, D. McIntyre, M. Thiede, G. Dahlgren, and M. Whitehead. 2006. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Social Science and Medicine 62(4):858-865.
McNamara, P. 2005. Quality-based payment: Six case examples. International Journal for Quality in Health Care 17(4):357-362.
McNamara, P. 2006. Provider-specific report cards: A tool for health sector accountability in developing countries. Health Policy and Planning 21(2):101-109.
Mehta, R. H., E. D. Peterson, and R. M. Califf. 2007. Performance measures have a major effect on cardiovascular outcomes: A review. American Journal of Medicine 120(5):398-402.
Mendis, S., K. Fukino, A. Cameron, R. Laing, A. F. Jr., O. Khatib, J. Leowski, and M. Ewen. 2007a. The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bulletin of the World Health Organization 85(4):279-288.
Mendis, S., L. H. Lindholm, G. Mancia, J. Whitworth, M. Alderman, S. Lim, and T. Heagerty. 2007b. World Health Organization (WHO) and International Society of Hypertension (ISH) risk prediction charts: Assessment of cardiovascular risk for prevention and control of cardiovascular disease in low and middle-income countries. Journal of Hypertension 25(8):1578-1582.
Mensah, K., M. Mackintosh, and L. Henry. 2005. The “skills drain” of health professionals from the developing world: A framework for policy formulation. http//:www.medact.org/content/Skills%20drain/Mensah%20et%20al.%202005.pdf (accessed June 28, 2009).
Mittelmark, M. B., R. V. Luepker, D. R. Jacobs, et al. 1986. Communitywide prevention ofCommunitywide prevention of cardiovascular disease: education strategies of the Minnesota Heart Health Program. Preventive Medicine 15:1-17.
Mittelmark, M. B., M. K. Hunt, G. W. Heath, and T. L. Schmid. 1993. Realistic outcomes: Lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. Journal of Public Health Policy 14(4):437-462.
Mohr, T., O. Rajobov, Z. Maksumova, and R. Northrup. 2005. Using incentives to improve tuberculosis treatment results: lessons from Tajikistan. Washington, DC: The Core Group.
Monterey County Health Department. 2007. Health profile 2007: Conditions and behaviors. http://www.co.ca/us/health/publications (accessed December 16, 2009).
Moy, F., A. A. Sallam, and M. Wong. 2006. The results of a worksite health promotion programme in Kuala Lumpur, Malaysia. Health Promotion International 21(4):301-310.
Mullan, F., and S. Frehywot. 2007. Non-physician clinicians in 47 Sub-Saharan African countries. Lancet 370(9605):2158-2163.
NCI (National Cancer Institute). 2002. Making health communication programs work. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services.
NCI. 2008. The role of the media in promoting and reducing tobacco use. NCI tobacco control monograph 19. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services.
Neubeck, L., J. Redfern, R. Fernandez, T. Briffa, A. Bauman, and S. B. Freedman. 2009. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review. European Journal of Cardiovascular Prevention and Rehabilitation 16(3):281-289.
Ng, S. W., F. Zhai, and B. M. Popkin. 2008. Impacts of China’s edible oil pricing policy on nutrition. Social Science and Medicine 66(2):414-426.
Ng, S. W., E. C. Norton, et al. 2009. Why have physical activity levels declined among Chinese adults? Findings from the 1991-2006 China health and nutrition surveys. Social Science & Medicine 68(7): 1305-1314.
Nissinen, A., X. Berrios, and P. Puska. 2001. Community-based noncommunicable disease interventions: Lessons from developed countries for developing ones. Bulletin of the World Health Organization 79(10):963-970.
O’Brien, P., and L. Gostin. 2008. Health worker shortages and inequalities: The reform of United States policy. Global Health Governance 2(2):1-29.
Olcay, M., and R. Laing. 2005. Pharmaceutical tariffs: What is their effect on prices, protection of local industry and revenue generation? Geneva: WHO Commission on Intellectual Property Rights, Innovation and Public Health.
OpenMRS. 2010. OpenMRS. http://openmrs.org/ (accessed February 1, 2010).
Osler, M., and N. B. Jespersen. 1993. The effect of a community-based cardiovascular-disease prevention project in a Danish municipality. Danish Medical Bulletin 40(4):485-485.
O’Sullivan, G. A., J. A. Yonkler, W. Morgan, and A. P. Merritt. 2003. A field guide to designing a health communication strategy. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs.
Papas, M. A., A. J. Alberg, R. Ewing, K. J. Helzlsouer, T. L. Gary, and A. C. Klassen. 2007. The built environment and obesity. Epidemiologic Reviews 29:129-143.
Partnership for Supply Chain Management Systems. 2010. http://www.pfscm.org (accessed February 3, 2010).
Peabody, J. W., P. J. Gertler, and A. Leibowitz. 1998. The policy implications of better structure and process on birth outcomes in Jamaica. Health Policy 43(1):1-13.
Peabody, J. W., J. Florentino, R. Shimkhada, O. Solon, and S. Quimbo. 2010a. Quality variation and its impact on costs and satisfaction: Evidence from the QIDS study. Medical Care 48(1):25-30.10.1097/MLR.1090b1013e3181bd1047b1092.
Peabody, J. W., S. Quimbo, J. Florentino, M. F. Bacate, K. Woo, R. Shimkhada, and O. Solon. 2010b. A randomized experiment introducing incentives to improve quality of care. Health Affairs.
Pereira, M., N. Lunet, A. Azevedo, and H. Barros. 2009. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. Journal of Hypertension 27(5):963-975.
Petersen, L. A., L. D. Woodard, T. Urech, C. Daw, and S. Sookanan. 2006. Does pay-for-performance improve the quality of health care? Annals of Internal Medicine 145(4): 265-272.
Pierce, J., N. Evans, A. J. Farkas, S. W. Cavin, C. Berry, M. Kramer, et al. 1994. Tobacco use in California: An evaluation of the tobacco control program, 1989-1993. A report to the California Department of Health Services. http://www.escholarship.org/uc/item/3c7259dj (accessed January 11, 2010).
Pinstrup-Andersen, P., ed. 1988. Food subsidies in developing countries: Costs, benefits, and policy options. London and Baltimore: The Johns Hopkins University Press (for the International Food Policy Research Institute).
Piotrow, P. T., J. G. I. Rimon, A. Payne Merritt, and G. Saffitz. 2003. Advancing health communication: The PCS experience in the field. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs.
Popkin, B. M. 2003. Dynamics of the nutrition transition and its implications for the developing world. Forum on Nutrition 56:262-264.
Prabhakaran, D., P. Jeemon, S. Goenka, R. Lakshmy, K. R. Thankappan, F. Ahmed, P. P. Joshi, B. V. Mohan, R. Meera, M. S. Das, R. C. Ahuja, R. K. Saran, V. Chaturvedi, and K. S. Reddy. 2009. Impact of a worksite intervention program on cardiovascular risk factors: A demonstration project in an Indian industrial population. Journal of the American College of Cardiology 53(18):1718-1728.
Prasad, B., and Y. Mulaleedharan. 2007. Community health workers: A review of concepts, practice, and policy concerns. HRH Global Resource Center.
Puska, P., A. Nissinen, J. Tuomilehto, J. T. Salonen, K. Koskela, A. McAlister, T. E. Kottke, N. Maccoby, and J. W. Farquhar. 1985. The community-based strategy to prevent coronary heart disease: Conclusions from the ten years of the North Karelia project. Annual Review of Public Health 6:147-193.
Puska, P., J. Tuomilehto, A. Nissinen, et al. 1995. The North Karelia project. 20 year results and experiences. Helsinki: The National Public Health Institute (KTL).
Puska, P., E. Vartiainen, T. Laatinkainen, P. Jousilahti, and M. Paavola, eds. 2009. The North Karelia project: From North Karelia to national action. Helsinki: Helsinki University Printing House.
Quick, J. D., H. V. Hogerzeil, G. Velasquez, and L. Rago. 2002. Twenty-five years of essential medicines. Bulletin of the World Health Organization 80(11):913-914.
Quimbo, S., J. W. Peabody, R. Shimkhada, and O. Solon. Evidence of a causal link between health outcomes, insurance coverage and a policy to expand access: experimental data from children in the Philippines. Health Economics.
Raguenaud, M.-E., P. Isaakidis, T. Reid, S. Chy, L. Keuky, G. Arellano, and W. Van Damme. 2009. Treating 4,000 diabetic patients in Cambodia, a high-prevalence but resource-limited setting: A 5-year study. BMC Medicine 7(1):33.
Ravishankar, N., P. Gubbins, R. J. Cooley, K. Leach-Kemon, C. M. Michaud, D. T. Jamison, and C. J. Murray. 2009. Financing of global health: Tracking development assistance for health from 1990 to 2007. Lancet 373(9681):2113-2124.
Reidpath, D. D., and P. Allotey. 2009. Opening up public health: A strategy of information and communication technology to support population health. Lancet 373(9668): 1050-1051.
Rivera, J. A., D. Sotres-Alvarez, J. P. Habicht, T. Shamah, and S. Villalpando. 2004. Impact of the Mexican program for education, health, and nutrition (progresa) on rates of growth and anemia in infants and young children: A randomized effectiveness study. Journal of the American Medical Association 291(21):2563-2570.
Robinowitz, D. L., and R. A. Dudley. 2006. Public reporting of provider performance: Can its impact be made greater? Annual Review of Public Health 27(1):517-536.
Roccella, E. J., and M. J. Horan. 1988. The national high blood pressure education program: Measuring progress and assessing its impact. Health Psychology 7:297-303.
Rogers, E. M. 1983. Diffusion of Innovations. New York: Free Press.
Rossouw, J. E., P. L. Jooste, D. O. Chalton, E. R. Jordaan, M. L. Langenhoven, P. C. Jordaan, M. Steyn, A. S. Swanepoel, and L. J. Rossouw. 1993. Community-based intervention: The coronary risk factor study (CORIS). International Journal of Epidemiology 22(3):428-438.
Rowe, A. K., D. de Savigny, C. F. Lanata, and C. G. Victora. 2005. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet 366(9490):1026-1035.
Ruszkowska-Majzel, J., and W. Drygas. 2005. The great nationwide physical activity campaign “revitalize your heart” as an effective method to promote active lifestyle in Poland. Przeglad Lekarski 62(Suppl 3):23-26.
Saffer, H., and F. Chaloupka. 2000. The effect of tobacco advertising bans on tobacco consumption. Journal of Health Economics 19(6):1117-1137.
Sallis, J. F., J. A. Flora, S. P. Fortmann, C. B. Taylor, and N. Maccoby. 1985. Mediated smoking cessation programs in the Stanford Five-City Project. Addictive Behaviors 10(4):441-443.
Sallis, J. F., M. Story, and D. Lou. 2009. Study designs and analytic strategies for environmental and policy research on obesity, physical activity, and diet: Recommendations from a meeting of experts. American Journal of Preventive Medicine 36(Suppl 2):S72-S77.
Schaffnit-Chatterjee, C. 2009. The global food equation: Food security in an environment of increasing scarcity. Frankfurt, Germany: Deutsche Bank Research.
Schieber, G., C. Baeza, D. Kress, and M. Maier. 2006. Financing health systems in the 21st century. In Disease control priorities in developing countries. 2nd ed, edited by D. T. Jamison, J. G. Breman, A. R. Measham, G. Alleyne, M. Claeson, D. B. Evans, P. Jha, A. Mills and P. Musgrove. New York: Oxford University Press. Pp. 225-242.
Schieber, G. J., P. Gottret, L. K. Fleisher, and A. A. Leive. 2007. Financing global health:Financing global health: Mission unaccomplished. Health Affairs 26(4):921-934.
Schooler, C., J. W. Farquhar, S. P. Fortmann, and J. A. Flora. 1997. Synthesis of findings and issues from community prevention trials. Annals of Epidemiology 7(Suppl 1):S54-S68.
Schuit, A. J., G. C. W. Wendel-Vos, W. M. M. Verschuren, E. T. Ronckers, A. Ament, P. Van Assema, J. Van Ree, and E. C. Ruland. 2006. Effect of 5-year community intervention Hartslag Limburg on cardiovascular risk factors. American Journal of Preventive Medicine 30(3):237-242.
Sepe, E., and S. A. Glantz. 2002. Bar and club tobacco promotions in the alternative press: targeting young adults. American Journal of Public Health 92(1):75-78.
Shafey, O., M. Eriksen, H. Ross, and J. Mackay. 2009. The tobacco atlas. 3rd ed. Atlanta: American Cancer Society.
Shaller, D., S. Sofaer, S. D. Findlay, J. H. Hibbard, D. Lansky, and S. Delbanco. 2003. Consumers and quality-driven health care: A call to action. Health Affairs 22(2):95-101.
Shea, S., and C. Basch. 1990a. A review of five major community-based cardiovascular disease prevention programs. Part II: Intervention strategies, evaluation methods, and results. American Journal of Health Promotion 4(4):279-287.
Shea, S. and C. Basch. 1990b. A review of five major community-based cardiovascular disease prevention programs. Part I: Rationale, design, and theoretical framework. American Journal of Health Promotion 4(3):203-213.
Shimkhada, R., J. Peabody, S. Quimbo, and O. Solon. 2008. The quality improvement demonstration study: An example of evidence-based policy-making in practice. Health Research Policy and Systems 6(1):5.
Singh, D., and C. Ham. 2006. Improving care for people with long-term conditions: A review of UK and international frameworks. Birmingham, UK: University of Birmingham.
Smith, B. 2009. Social marketing programs in health in developing countries. Presentation at Public Information Gathering Session for the Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease, Washington, DC.
Smith, S. C. 1997. Review of recent clinical trials of lipid lowering in coronary artery disease. American Journal of Cardiology 80(Suppl 2):10H-13H.
Smith, W. A., ed. 1999. Social marketing lite: Ideas for folks with small budgets and big problems. Washington, DC: AED (Academy for Educational Development).
Soeters, R., C. Habineza, and P. B. Peerenboom. 2006. Performance-based financing and changing the district health system: Experience from Rwanda. Bulletin of the World Health Organization 84(11):884-889.
Solon, O., K. Woo, S. A. Quimbo, R. Shimkhada, J. Florentino, and J. W. Peabody. 2009. A novel method for measuring health care system performance: Experience from QIDS in the Philippines. Health Policy and Planning 24(3):167-174.
Somkotra, T., L. P. Lagrada, T. Somkotra, and L. P. Lagrada. 2009. Which households are at risk of catastrophic health spending: Experience in Thailand after universal coverage. Health Affairs 28(3):w467-w478.
Sosa-Rubi, S. G., O. Galarraga, and J. E. Harris. 2009. Heterogeneous impact of the “Seguro Popular” Program on the utilization of obstetrical services in Mexico, 2001-2006: A multinomial probit model with a discrete endogenous variable. Journal of Health Economics 28(1):20-34.
Steinfeld, H., Food and Agriculture Organization of the United Nations Livestock, Environment, and Development Initiative. 2006. Livestock’s long shadow: Environmental issues and options. Rome: Food and Agriculture Organization of the United Nations.
Steyn, K., M. Steyn, A. S. Swanepoel, P. C. Jordaan, P. L. Jooste, J. M. Fourie, and J. E. Rossouw. 1997. Twelve-year results of the coronary risk factor study (CORIS). International Journal of Epidemiology 26(5):964-971.
Steyn, N. P., D. Bradshaw, R. Norman, J. Joubert, M. Schneider, and K. Steyn. 2006. Dietary changes and the health transition in South Africa: Implications for health policy. Cape Town: South African Medical Research Council.
Stokols, D. 1992. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. American Psychologist 47(1):6-22.
Supply Chain Management System. 2009. Three years of saving lives through stronger HIV/ AIDS supply chains: A report on the global impacts of SCMS. Arlington, VA: Supply Chain Management System.
Supply Chain Management System. no date. http://scms.pfscm.org/scms/about (accessed February 3, 2010).
Task Force on Community Preventive Services. 2002. Recommendations to increase physical activity in communities. American Journal of Preventive Medicine 22(4S):67-72.
Taskforce on Innovative International Financing for Health Systems Working Group 1. 2009. Constraints to scaling up and costs: Working group 1 report. Geneva: International Health Partnership.
Thow, A. M., and C. Hawkes. 2009. The implications of trade liberalization for diet and health: A case study from Central America. Globalization and Health 5(1):5.
Thow, A. M., S. Jan, S. Leeder, and B. Swinburn. 2010. The effect of fiscal policy on diet, obesity and chronic disease: A systematic review. Bulletin of the World Health Organization.
Tian, H. G., Z. Y. Guo, G. Hu, S. J. Yu, W. Sun, P. Pietinen, and A. Nissinen. 1995. Changes in sodium intake and blood pressure in a community-based intervention project in China. Journal of Human Hypertension 9(12):959-968.
Twahirwa, A. 2008. Sharing the burden of sickness: Mutual health insurance in Rwanda. Bulletin of the World Health Organization 86(11):823-824.
Tye, J. B., K. E. Warner, et al. 1987. Tobacco advertising and consumption: Evidence of a1987. Tobacco advertising and consumption: Evidence of a causal relationship. Journal of Public Health Policy 8(4):492-508.
United Nations Department of Economic and Social Affairs. 2008. The millennium development goals report. Geneva: United Nations.
United Nations Statistics Division. 2008. Millenium development goals indicators. http://unstats.un.org/unsd/mdg/Host.aspx?Content=Indicators/OfficialList.htm (accessed May 21, 2010).
U.S. Department of Health and Human Services. 2004. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Institutes of Health.
Uusitalo, U., E. J. Feskens, J. Tuomilehto, G. Dowse, U. Haw, D. Fareed, F. Hemraj, H. Gareeboo, K. G. Alberti, and P. Zimmet. 1996. Fall in total cholesterol concentration over five years in association with changes in fatty acid composition of cooking oil in Mauritius: Cross sectional survey. British Medical Journal 313(7064):1044-1046.
Vateesatokit, P. 2003. Tailoring Tobacco Control Efforts to the Country: The Example of Thailand. In Tobacco control policy: Strategies, successes, and setbacks, edited by J. de Beyer and L. W. Brigden. Washington, DC: The World Bank and The International Development Research Centre.
Victora, C. G., K. Hanson, J. Bryce, and J. P. Vaughan. 2004. Achieving universal coverage with health interventions. Lancet 364(9444):1541-1548.
Volpp, K. G., A. Gurmankin Levy, D. A. Asch, J. A. Berlin, J. J. Murphy, A. Gomez, H. Sox, J. Zhu, and C. Lerman. 2006. A randomized controlled trial of financial incentives for smoking cessation. Cancer Epidemiology Biomarkers & Prevention 15(1):12-18.
Volpp, K. G., A. B. Troxel, M. V. Pauly, H. A. Glick, A. Puig, D. A. Asch, R. Galvin, J. Zhu, F. Wan, J. DeGuzman, E. Corbett, J. Weiner, and J. Audrain-McGovern. 2009. A randomized, controlled trial of financial incentives for smoking cessation. New England Journal of Medicine 360(7):699-709.
von Schirnding, Y., and D. Yach. 2002. Unhealthy consumption threatens sustainable development. Revista de Saude Publica 36(4):379-382.
Wagner, A. K., M. Valera, A. J. Graves, S. Lavina, and D. Ross-Degnan. 2008. Costs of hospital care for hypertension in an insured population without an outpatient medicines benefit: An observational study in the Philippines. BMC Health Services Research 8(161).
Wagner, E. H., B. T. Austin, and K. Michael Von. 1996. Organizing care for patients with chronic illness. The Milbank Quarterly 74(4):511-544.
Wakefield, M., B. Flay, M. Nichter, and G. Giovino. 2003. Effects of anti-smoking advertising on youth smoking: A review. Journal of Health Communication 8(3):229-247.
Wald, N. J., and M. R. Law. 2003. A strategy to reduce cardiovascular disease by more than 80%. British Medical Journal 326(7404):1419.
Wallace, A., V. Dietz, and K. L. Cairns. 2009. Integration of immunization services with other health interventions in the developing world: What works and why? Systematic literature review. Tropical Medicine and International Health 14(1):11-19.
Walters, S. T., J. A. Wright, J. and R. Shegog. 2006. A review of computer and internet-based interventions for smoking behavior. Addictive Behaviors 3(2):264-277.
Weinehall, L., G. Hellsten, K. Boman, and G. Hallmans. 2001. Prevention of cardiovascular disease in Sweden: The Norsjo community intervention programme—motives, methods and intervention components. Scandinavian Journal of Public Health 29(Suppl 56):13-20.
WHO (World Health Organization). 2003. WHO framework convention on tobacco control. Geneva: World Health Organization.
WHO. 2006. WHO country health information. http://www.who.int/nha/country/en/ (accessed February 17, 2010).
WHO. 2007a. Everybody’s business—strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization.
WHO. 2007b. Report of the global survey on the progress in national chronic diseases prevention and control. Geneva: World Health Organization.
WHO. 2008a. Draft: The WHO code of practice on the international recruitment of health personnel. http://www.who.int/hrh/migration/code/draft_code_en.pdf (accessed December 16, 2009).
WHO. 2008b. Mpower: A policy package to reverse the tobacco epidemic. Geneva: World Health Organization.
WHO. 2008c. WHO report on the global tobacco epidemic, 2008: The MPOWER package. Geneva: World Health Organization.
WHO and WEF (World Economic Forum). 2008. Preventing noncommunicable diseases in the workplace through diet and physical activity: WHO/World Economic Forum report of a joint event. http://www.weforum.org/pdf/Wellness/WHOWEF_report.pdf (accessed April 11, 2009.
WHO Forum on Reducing Salt Intake in Populations. October 2006. Reducing salt intake in populations: Report of a WHO forum and technical meeting. Paris: World Health Organization.
WHO Maximizing Positive Synergies Collaborative Group. 2009. An assessment of interactions between global health initiatives and country health systems. Lancet 373(9681): 2137-2169.
WHO Noncommunicable Diseases and Mental Health Cluster. 2002. Innovative care for chronic conditions: Building blocks for actions: Global report. Geneva: World Health Organization.
Williams, F., and S. Boren. 2008. The role of the electronic medical record (EMR) in care delivery in developing countries: Case study, Ghana. International Journal of Information Management 16(2):139-145.
Williams, P. T., S. P. Fortmann, J. W. Farquhar, A. Varady, and S. Mellen. 1981. A comparison of statistical methods for evaluating risk factor changes in community-based studies: An example from the Stanford Three-Community Study. Journal of Chronic Diseases 34(11):565-571.
Willis-Shattuck, M., P. Bidwell, S. Thomas, L. Wyness, D. Blaauw, and P. Ditlopo. 2008. Motivation and retention of health workers in developing countries: A systematic review. BMC Health Services Research 8:247.
Xavier, D., P. Pais, P. J. Devereaux, C. Xie, D. Prabhakaran, K. S. Reddy, R. Gupta, P. Joshi, P. Kerkar, S. Thanikachalam, K. K. Haridas, T. M. Jaison, S. Naik, A. K. Maity, and S. Yusuf. 2008. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet 371(9622):1435-1442.
Xavier, D., P. Pais, A. Sigamani, J. Pogue, R. Afzal, and S. Yusuf. 2009. The need to test the theories behind the polypill: Rationale behind the Indian polycap study. Nature Clinical Practice Cardiovascular Medicine 6(2):96-97.
Yach, D., and R. Beaglehole. 2004. Globalization of risks for chronic diseases demands global solutions. Perspectives on Global Development and Technology 3(1):213-233.
Yang, G., L. Kong, W. Zhao, X. Wan, Y. Zhai, L. C. Chen, and J. P. Koplan. 2008. Emergence of chronic non-communicable diseases in China. Lancet 372(9650):1697-1705.
Yu, Z., G. Song, Z. Guo, G. Zheng, H. Tian, E. Vartiainen, P. Puska, and A. Nissinen. 1999. Changes in blood pressure, body mass index, and salt consumption in a Chinese population. Preventive Medicine 29(3):165-172.
Yu, Z., A. Nissinen, E. Vartiainen, G. Song, Z. Guo, and H. Tian. 2000. Changes in cardiovascular risk factors in different socioeconomic groups: Seven year trends in a Chinese urban population. Journal of Epidemiology and Community Health 54(9):692-696.
Yusuf, S. 2002. Two decades of progress in preventing vascular disease. Lancet 360(9326): 2-3.
Yusuf, S., S. Reddy, S. Ounpuu, and S. Anand. 2001. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104(22):2746-2753.
Zatonski, W. A., and W. Willett. 2005. Changes in dietary fat and declining coronary heart disease in Poland: Population based study. British Medical Journal 331(7510):187-188.
Zatonski, W. A., A. J. McMichael, and J. W. Powles. 1998. Ecological study of reasons for sharp decline in mortality from ischaemic heart disease in Poland since 1991. British Medical Journal 316(7137):1047-1051.