2
Epidemiology of Cardiovascular Disease
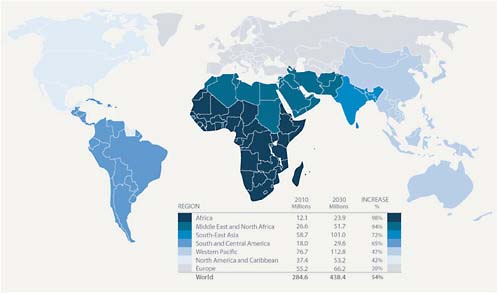
In recent years, the dominance of chronic diseases as major contributors to total global mortality has emerged and has been previously described in detail elsewhere (Adeyi et al., 2007; WHO, 2008b). By 2005, the total number of cardiovascular disease (CVD) deaths (mainly coronary heart disease, stroke, and rheumatic heart disease) had increased globally to 17.5 million from 14.4 million in 1990. Of these, 7.6 million were attributed to coronary heart disease and 5.7 million to stroke. More than 80 percent of the deaths occurred in low and middle income countries (WHO, 2009e). The World Health Organization (WHO) estimates there will be about 20 million CVD deaths in 2015, accounting for 30 percent of all deaths worldwide (WHO, 2005). The projected trends in CVD mortality and the expected shifts from infectious to chronic diseases over the next few decades are shown in Figure 2.1. By 2030, researchers project that noncommunicable diseases will account for more than three-quarters of deaths worldwide; CVD alone will be responsible for more deaths in low income countries than infectious diseases (including HIV/AIDS, tuberculosis, and malaria), maternal and perinatal conditions, and nutritional disorders combined (Beaglehole and Bonita, 2008). Thus, CVD is today the largest single contributor to global mortality and will continue to dominate mortality trends in the future (WHO, 2009e).
This chapter describes the incidence and trends over time of CVD globally, as well as in specific regions and nations throughout the world. Moreover, it lays out the major individual risk factors associated with acquisition and augmentation of risk for coronary heart disease and stroke throughout the life course. Furthermore, infectious causes of CVD and
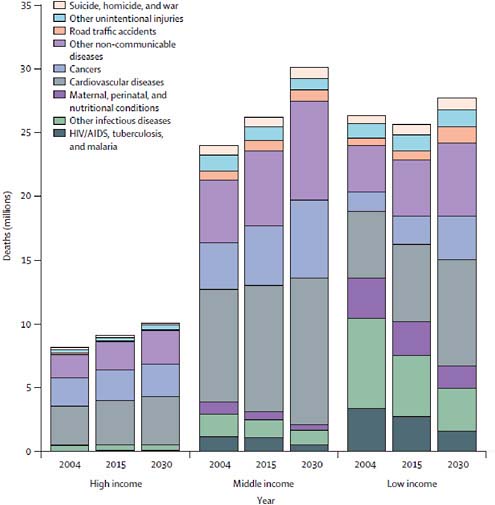
FIGURE 2.1 Projected global deaths by cause.
SOURCE: Beaglehole and Bonita, 2008.
the interface between chronic infectious diseases and CVD risk are briefly discussed later in this chapter. Broad systemic drivers that contribute to the global burden of CVD, such as urbanization and globalization, are referred to in this chapter where they relate to trends in CVD burden and to the classically defined individual risk factors. These are then discussed in more detail in Chapter 3, which focuses on the relationship between CVD and development. Together, these two chapters describe the drivers and trends in CVD worldwide, providing a compelling rationale for the need to act. The remainder of the report proceeds to discuss approaches to influence these factors in order to reduce the burden of disease.
GLOBAL TRENDS IN CVD BURDEN
Global trends in CVD are based on models that use country-specific data from a diverse range of developed and developing countries including those of the European Union (HEM Project Team, 2008; Kotseva et al., 2009a), Saudi Arabia (Al-Hamdan et al., 2005), Pakistan (Nishtar et al., 2004), South Africa (Steyn, 2006), China (Yang et al., 2008), Indonesia (Ng, 2006; Ng et al., 2006), Mexico (Fernald and Neufeld, 2007), India (Goyal and Yusuf, 2006; Reddy, 2007), and the United States (Danaei et al., 2009; Flegal et al., 2007). Over the past decade, the quality and availability of country-specific data on CVD risks, incidence, and mortality has increased in accordance with one of the major recommendations of the 1998 IOM report. What emerges are nationally derived data on risks and CVD outcomes. Therefore, in many developing countries, the lack of country-specific data on risks and CVD outcomes that was prominently highlighted in the 1998 IOM report is less of an impediment to policy development and action.
Nonetheless, before beginning a discussion of CVD trends and risk factor incidence around the world and in specific countries and regions, it is important to note several persistent limitations with the available data. Although many countries have established health surveillance systems with death registration data, the quality of the data collected varies substantially across countries. In many countries—especially in low and middle income countries—health statistics are often based on surveillance that does not cover all areas of the country, is incomplete in the areas it does cover, or is collected by undertrained staff who do not, or cannot, accurately report the pertinent data. These realities limit the reliability of some country health data (Mathers et al., 2005; Rao et al., 2005). Despite these limitations, WHO and country health statistics are often the most complete, comparable, or only data available and thus remain a key tool for evaluating the status of a CVD epidemic within and between countries. The importance of country-level epidemiological data and the ongoing need to standardize methodologies, increase data collection capacity, and improve the accuracy of national reporting are discussed further in Chapter 4.
This chapter uses the most recent data available in each area discussed below, such as deaths by cause, contributions of risk factors to deaths by cause, the composition by risk factor of deaths by a specific cause, and risk factor levels. This introduces some inconsistencies as not all data cited comes from a single source. However, there is available data that is more recent for some of these measures than for others, and this was valued above the consistency of a single data source. Wherever possible, this chapter references burden, incidence, and prevalence data from countries’ national health statistics, WHO country and global statistics (which are based on
national health statistics provided by Member States), or the latest Global Burden of Disease: 2004 Update data (also based on WHO country data) (2008a).
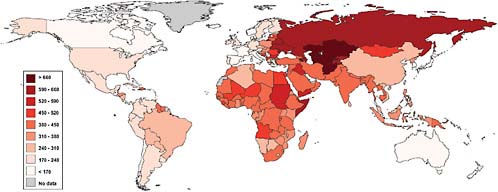
Global Cardiovascular Mortality
Globally, there is an uneven distribution of age-adjusted CVD mortality that is mapped in Figure 2.2. The lowest age-adjusted mortality rates are in the advanced industrialized countries and parts of Latin America, whereas the highest rates today are found in Eastern Europe and a number of low and middle income countries. For example, age-standardized mortality rates for CVD are in excess of 500 per 100,000 in Russia and Egypt; between 400 and 450 for South Africa, India and Saudi Arabia; and around 300 for Brazil and China. This is in contrast to rates of between 100 and 200 per 100,000 for Australia, Japan, France, and the United States. Overall, age-adjusted CVD death rates are today higher in major low and middle income countries than in developed countries (WHO, 2008b).
Examination of coronary heart disease (CHD) mortality trends across countries reveals considerable variability in the shape and magnitude of CHD epidemics since the 1950s. Trends are not consistent even among countries within the same geographic region. In general, three trending patterns of CHD mortality can be observed: a rise-and-fall pattern where mortality rates increased, peaked, and then fell significantly; a rising pattern, where rates have steadily increased indicating an ongoing epidemic; and a flat pattern, where CHD mortality rates have remained relatively low and stable. The rise-and-fall pattern is most notable in high income Anglo-Celtic, Nordic, and Northwestern Continental European countries as well as in the United States and Australia. In these countries, CHD mortality rates peaked in the 1960s or early 1970s and have since fallen precipitously, by an average of about 50 percent (Beaglehole, 1999; Hardoon et al., 2008; Mirzaei et al., 2009; Unal et al., 2004). The rising pattern of CHD is most notable in Eastern European and former Soviet countries, where mortality rates have continued to increase at an alarming pace and where the highest mortality rates ever recorded are currently being observed. By contrast, CHD mortality rates in Japan and several European Mediterranean countries have remained relatively low, following the flat pattern (Beaglehole, 1999; Mirzaei et al., 2009).
Mortality rates generally appear to be most closely linked to a country’s stage of epidemiological transition. Epidemiological transition, a concept first proposed by Abdel Omran in the 1970s (Omran, 1971), refers to the changes in the predominant forms of disease and mortality burdening a population that occur as its economy and health system develops. In underdeveloped countries at the early stages of epidemiological transition,
infectious diseases predominate, but as the economy, development status, and health systems of these countries improve, the population moves to a later stage of epidemiological transition, and chronic noncommunicable diseases become the predominant causes of death and disease (Gaziano et al., 2006).
Although this general pattern connecting trends in causes of mortality and stage of development can be observed, it is difficult to make generalized observations about CHD mortality trends for most low and middle income regions. This is due to limited trending data from many low and middle income countries as well as considerable country-to-country variability within regions. The data are strongest from Latin America, where several countries—specifically Argentina, Brazil, Chile, and Cuba—have experienced declines in CHD mortality rates in the past several decades. However, with the exception of Argentina, where rates declined by more than 60 percent between 1970 and 2000, the declines have generally occurred more recently (in the 1980s and 1990s) and have been less dramatic (between 20 and 45 percent) than those in high income countries. By contrast, the epidemic in Mexico appears to be worsening, with CHD mortality rates increasing by more than 90 percent between 1970 and 2000 (Mirzaei et al., 2009; Rodriguez et al., 2006). Mortality rates in Peru have remained relatively low, following the flat pattern. In Asia, some high income countries—such as Singapore—have followed the rise-and-fall pattern, while CHD deaths in other countries (such as the Philippines and urban China) appear to be rising (Mirzaei et al., 2009). Although trending data for most of Africa is not available, Mayosi et al. (2009) report that mortality rates for CVD and diabetes are rising in South Africa. Because there can be so much variability in the nature of CVD epidemics within regions, Mirzaei et al. (2009) conclude that the most prudent strategy when grouping countries in similar epidemiological situations is to group according to CVD mortality pattern rather than by geographic region.
Conclusion 2.1: Chronic diseases are now the dominant contributors to the global burden of disease, and CVD is the largest contributor to the chronic disease cluster. Although CVD death rates are declining in most high income countries, trends are increasing in most low and middle income countries.
Age at Death from CVD
Not only do age-adjusted CVD death rates tend to be higher in developing countries, but a significantly higher percentage of cardiovascular deaths also occur in younger people in the developing world than in developed countries. For example, the proportion of CVD deaths reported for 35 to
64 years is 41 percent in South Africa, 35 percent in India, and 28 percent in Brazil, compared to only 12 percent in the United States and 9 percent in Portugal (Leeder et al., 2004).
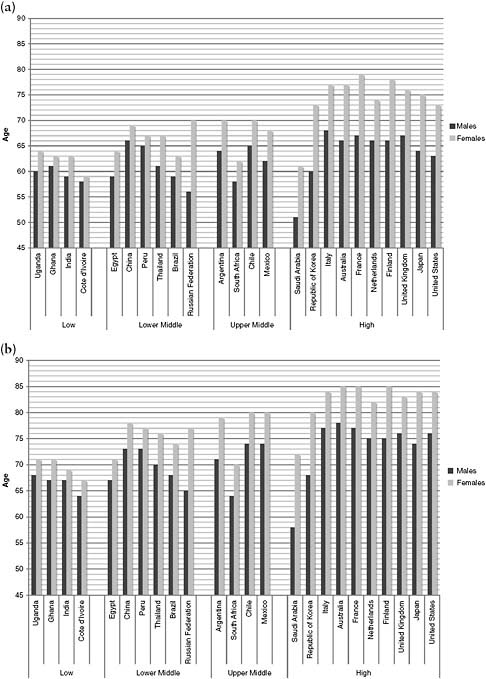
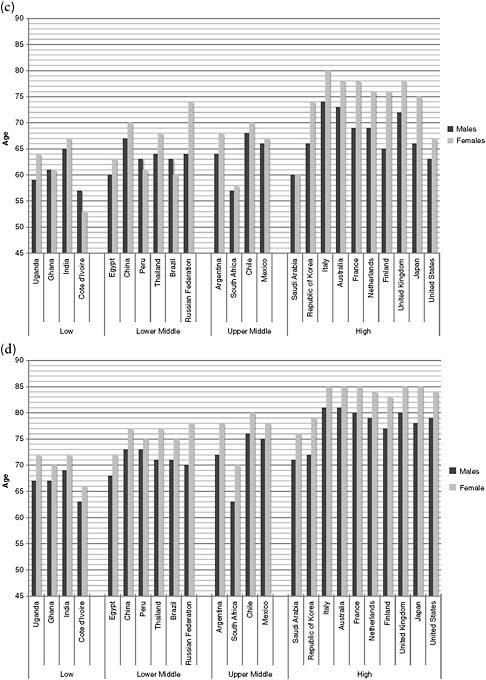
The median age of heart attack and first stroke and the median age at death from ischemic heart disease (IHD) and stroke offer a means to compare countries and groups in terms of their population experiences of CVD. The WHO 2004 Global Burden of Disease study estimated these variables for countries across the development spectrum. The results for selected countries are summarized in Figure 2.3. As a general trend, men and women in countries with higher development status (measured in terms of gross domestic product [GDP] per capita) experience CVD events older and die much later than in less developed countries. For example, in Japan, Australia, France, and Sweden, the median age at death from IHD averages 85 years in women and 77 years in men. Men in these countries experience an acute myocardial infarction (AMI) more than a decade before their median age at death (WHO, 2009a). Indeed, the survival of individuals after a cardiovascular event has increased in high income countries. This trend of increased survival with CVD has caused an increased prevalence of CVD in many high income countries despite decreasing incidence over time (Davies et al., 2007).
A second set of countries experienced median events at much younger ages despite having among the highest measures of GDP growth in the world. They include many Middle Eastern countries with considerable oil wealth. A third set of countries at intermediate levels of GDP per capita achieved above-average median ages at AMI and first stroke occurrence and death. They include Malaysia, Nicaragua, China, and Jamaica. In contrast, Brazil and South Africa, in the same development group as the preceding countries but with higher degrees of social inequality (United Nations Development Program [UNDP], 2007), achieved worse cardiovascular outcomes. Thus, even with countries at similar levels of development, some achieve substantially better CVD outcomes than others. These relative success stories give some indication of how preventable and treatable CVD can be. Comparative studies across countries are needed to build a better understanding of the factors that lead to the relative successes in these countries and to help inform the development of more effective approaches to control CVD.
REASONS FOR CVD TRENDS OVER TIME
A continuing understanding of how trends in CVD change over time is important, as knowledge evolves about the underlying causes of CVD and their relative impact. The empirical base for understanding the specific reasons for changes in CVD trends over time comes from two different
sets of observations and studies. First, there are those that investigate the causes for the increases in CVD death and incidence rates being experienced in many developing countries. Second, there are others that have analyzed the reasons for the substantive decline experienced in developed countries over the past few decades. As described below, the same set of major risk factors consistently play a large role in explaining trends in CVD incidence and death across the world. Taken together, the data indicate that poor diet, tobacco use, physical inactivity, excess alcohol use, and psychosocial factors are the major contributors to CVD increases (Anand et al., 2008; Clarke et al., 2009; Critchley et al., 2004; Lopez-Jaramillo et al., 2008; Mayosi et al., 2009; Rosengren et al., 2004; Stein et al., 2005; Yusuf et al., 2004). However, the reasons for the increase or decrease of these risks in various parts of the world are more complex. This section describes the trends in these risks, and subsequent sections of this chapter describe the nature of the relationship between these factors and risk for CVD in more detail.
Causes of the Ascent in CVD Mortality and Incidence
Data are limited on the specific causes of the increases in CVD incidence and mortality that occurred in developed countries in the early 20th century and in developing countries more recently. It is clear that by 1920 CVD was already the leading cause of death in the United States. Scientific articles from the 1930s and 1940s suggest hypertension, cholesterol, poor nutrition, obesity, smoking, physical inactivity, and psychosocial stress as the leading factors contributing to heart disease, but they do not provide strong evidence to support this assertion (Ellis, 1948; Gager, 1931; Heart disease likely fate, 1937). The original publications outlining the rationale for the Framingham Study also cite these potential risk factors, although, again, they do not provide specific supporting evidence (Dawber and Kannel, 1958; Dawber et al., 1951, 1957). Tobacco use has been the most reliably documented, and historical trends in CVD mortality and tobacco use in the United States from 1900 to 1990 closely mirror each other, with both rates increasing through the 1950s, followed by a precipitous fall beginning in the 1960s (Fox et al., 2004; Mirzaei et al., 2009; Shopland, 1995). In the United Kingdom, a 38-year follow-up of men showed that baseline differences in tobacco use, high blood pressure, and cholesterol were associated with a 10- to 15-year shorter life expectancy from age 50 (Clarke et al., 2009). The study has significance for developing countries since many of the baseline levels of risk common in the late 1960s in the United Kingdom are the norm in many developing countries today.
There are a few studies that provide more direct insight into the causes of recent increases in CVD incidence and mortality in low and middle in-
come countries. For example, in their study on the rise of CHD mortality in Beijing from 1984 to 1990, Critchley et al. found that blood lipid increases were the largest contributor—responsible for 77 percent of increased CHD mortality (Critchley et al., 2004).
Another likely contributor is a rise in smoking. There has been a steady rise in global cigarette consumption since the 1970s, which is expected to continue over the next decade if current trends continue. In 2010, researchers estimate that 6.3 trillion cigarettes—or more than 900 cigarettes for every person on the earth—will be consumed. This increase in the total number of smokers around the world is driven predominantly by global population growth and is expected to continue unless smoking rates are drastically reduced. By 2020, if current smoking and population growth trends continue, the global annual cigarette consumption could rise to between 6.7 and 6.8 trillion cigarettes (ERC, 2007; Guindon and Boisclair, 2003; Shafey et al., 2009). This growing burden of tobacco is increasingly falling on low and middle income countries. In fact, three of the top five cigarette-consuming countries are low or middle income countries (China, the Russian Federation, and Indonesia). China alone consumes approximately 2.163 trillion cigarettes every year—37 percent of the world’s annual consumption (ERC, 2007; Guindon and Boisclair, 2003; Shafey et al., 2009). By 2030, WHO projects that more than 80 percent of tobacco-related deaths will occur in developing countries (Shafey et al., 2009; WHO, 2008c). In addition to increasing consumption trends, the amount of tobacco produced globally has nearly doubled since 1960, with production increasing more than 300 percent in low and middle income countries, where by 2007, approximately 85 percent of tobacco was grown (Shafey et al., 2009). In addition, as tobacco use has declined in rich countries, transnational tobacco companies have increasingly focused on expanding markets for their products in low and middle income countries (Bump et al., 2009; Chelala, 1998; Connolly, 1992; Holzman, 1997; Mackay, 1992; Mackay and Eriksen, 2002; Martinez and Grise, 1990; Wagner and Romano, 1994).
An emerging body of evidence suggests that rapid dietary changes associated with nutritional transition, along with a decrease in levels of physical activity in many rapidly urbanizing societies, also may play a particularly important role in the rise of CVD observed in developing countries (Stein et al., 2005). The nutritional transition currently occurring in many low and middle income countries has created a new phenomenon in which it is not uncommon to see both undernutrition and obesity coexist in the same populations (Caballero, 2005; Dangour and Uauy, 2006; Reddy et al., 2003). Undernutrition has been the hallmark of the low and middle income countries of Africa, Latin America, and South Asia for decades. This situation is progressively being replaced by a distinct trend at the other end of the spectrum. While the global undernourished population is plateauing,
obesity and other chronic diseases have been increasing exponentially as a result of lifestyle and behavior change, resulting in a transition from communicable to noncommunicable diseases. WHO has estimated that while the undernourished global population has declined to approximately 1.2 billion, the overweight population has increased to the same figure. Of these, an estimated 300 million are clinically obese (Misra and Khurana, 2008). As an associated problem, the global prevalence of overweight in children between the ages of 5 and 17 years is 10 percent, varying from under 2 percent in Sub-Saharan Africa to more than 30 percent in the United States (Bhardwaj et al., 2008).
Epidemiological evidence suggests that dietary changes associated with the nutritional transition, specifically the increasing consumption of energy-dense diets high in unhealthy fats, oils, sodium, and sugars, have contributed to an increase in CVD incidence in low and middle income countries (Hu, 2008). Traditionally, monitoring of dietary consumption trends in low and middle income countries has been difficult due to poor availability of quality data. The Food and Agricultural Organization (FAO) of the United Nations examines trends in the amounts of various foods that are produced, which can serve as a rough proxy for consumption. This measure usually overestimates consumption, but trends remain valid indicators of the broad changes underway. FAO data indicate that the total kilocaloric intake per capita per day (KCD) in many low and middle income countries as well as the consumption of animal products and some tropical oils (e.g., palm oil)—major sources of saturated fat—have been increasing.
To illustrate these trends, kilocaloric intake from selected food groups in China, India, Mexico, Egypt, and South Africa from 1980 to 1982 were compared to kilocaloric intake in 2001 to 2003 using data derived from FAOSTAT (Food and Agriculture Organization of the United Nations Statistical Database) (see Table 2.1). In China, total KCD increased from 2,327 kilocalories to 2,940 kilocalories, and meat consumption increased by more than 246 percent during the period.
There was also a significant increase in the intake of oils in China, with three types of oils increasing more than 100 percent: palm oil (+640 percent), soybean oil (+635 percent), and vegetable oils (+259 percent). On the positive side, the intake of fruits and vegetables also skyrocketed—by 600 and 367 percent, respectively—over the same period. On balance, these changes provided the Chinese with a mix of healthier calories; however, increased risks brought about by the increased consumption of meat and foods cooked in tropical oils are associated with adverse blood lipid changes. A similar picture was repeated in India, Mexico, and South Africa, with soaring kilocalorie intake of palm oil reported.
The exponential growth in the use of tropical oils (specifically palm oil) and partially hydrogenated soybean oil in low and middle income countries
TABLE 2.1 Percentage Change in Consumption by Kilocalories per Capita per Day in Selected Countries from 1980 to 2003
|
Food Type |
China |
Egypt |
India |
Mexico |
South Africa |
|
Total Kilocalories |
26.3 |
16.2 |
25.7 |
1.5 |
5.7 |
|
Meat |
247 |
48.3 |
40.0 |
18.3 |
6.9 |
|
Cereals |
−13.9 |
17.6 |
13.8 |
−1.4 |
4.7 |
|
Sugar and Sweeteners |
51.9 |
8.8 |
27.2 |
2.4 |
−18.3 |
|
Fruits |
600 |
103 |
60.0 |
19.4 |
33.3 |
|
Vegetables |
367 |
10.3 |
37.5 |
40.7 |
0.0 |
|
Palm Oil |
640 |
No Data |
730 |
2100 |
2400 |
|
Soybean Oil |
635 |
35.5 |
48.2 |
50.0 |
189 |
|
Vegetable Oil |
259 |
−47.8 |
84.6 |
14.7 |
75.4 |
|
SOURCE: FAOSTAT food consumption data. |
|||||
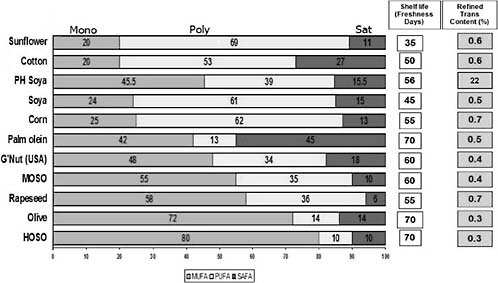
is troubling because both these oils contain high levels of fatty acids that are atherogenic and linked to an increased risk of MI. Palm oil has a saturated fatty acid content of 45 percent, and partially hydrogenated soybean oil, although much lower in saturated fat, contains transfatty acids introduced as a byproduct of hydrogenation (see Figure 2.5 later in this chapter for a comparison of the fatty acid composition of selected cooking oils). Globally, from 1980-1981 until the present, FAO estimates that there has been a 780 percent increase in palm oil production, a 286 percent increase in soybean production, and a 400 percent increase in rapeseed production. By contrast, olive oil production has increased by only 58 percent during this period (Khan and Mensah, 2009). Although the effects of unhealthy oils on CVD risk have been established (mainly in developed countries), the population consequences for CVD of these very steep and rapid production trends have yet to be directly quantified in developing countries. Gaining a better understanding of the implications of oil production trends as well as those for several other food categories that impact CVD risk is necessary to better inform current and future actions to address CVD, including those related to agricultural policy.
Causes of the Decline in CVD Mortality and Incidence in Developed Countries
Relative Contributions of Risk-Factor Reduction and Treatment
The causes of the decline in CVD in developed countries offer potential lessons for achieving similar results in developing countries. Taken together, studies examining the causes of the decline in CHD mortality and incidence observed in developed countries since the mid-1960s suggest that risk-factor
reductions and treatment each account for between 40 and 60 percent of the reduction in CVD mortality, with undetermined causes accounting for between 0 and 10 percent of additional reduction. The majority of these studies, described in more detail below, included all risk factor-reducing medications (such as statins for dyslipidemia) in the treatment category; thus, the data on risk-factor reduction are the result of lifestyle rather than medical interventions.
Several studies from Western Europe and New Zealand attributed a slightly higher percentage of the decline to the reduction of risk factors (Beaglehole, 1999; Capewell et al., 1999, 2000; Unal et al., 2004). This was particularly marked in Finland and New Zealand, where studies attributed more than 50 percent of the decline to risk-factor reductions (Laatikainen et al., 2005; Unal et al., 2004; Vartiainen et al., 1994b). Indeed, both studies from Finland found that treatments accounted for less than 25 percent of the reduction (Laatikainen et al., 2005; Vartiainen et al., 1994b), although the average declines occurred in an era of less effective treatments than are available today. Similarly, one study in the United Kingdom identified the contribution of improved treatment options in that country to be responsible for 40 percent of the reduction in mortality, with a concurrent reduction in risk factors accounting for the majority of the decline (Davies et al., 2007).
In contrast, reports from WHO’s Multinational Monitoring of Trends and Determinants in Cardiovascular Disease study have suggested the role of treatment was significantly higher, accounting for the majority of the decline (Davies et al., 2007). In the United States, some studies have attributed a slightly higher percentage to treatment than to risk-factor reductions (Goraya et al., 2003; Hunink et al., 1997), although a number of other studies found that risk-factor reduction and treatment strategies contribute evenly (approximately 50 percent each) to the decline in CVD mortality rates (Ford et al., 2007; Hardoon et al., 2008).
Importantly, with each decade, the relative impact of treatment versus prevention has increased (Ford et al., 2007). This effect could be due to the increasing availability of more effective diagnostics and treatment, higher population uptake of treatment, or the relative failure to fully implement effective prevention programs at a population level.
These data reinforce the importance of a balanced approach to combating CVD that includes both treatment and prevention. Better diagnosis and treatment can extend and improve the lives of those individuals who have established disease or high risk, but successful prevention of CVD and CVD risk factors will be required to reduce the incidence of CVD. This will require successful prevention. The need for this balance leads to important cost considerations for developed and developing countries in order to limit potential inflation of medical care costs as well as to develop and implement
affordable primary prevention programs. Chapters 3 and 5 discuss further the potential feasibility and relevance in developing countries of medication and other technologically based treatments versus behavioral or lifestyle risk-reduction approaches to reduce CVD burden.
Major Contributors to Risk Factor–Based Reductions in CVD
Although the numbers from each study differ, the body of evidence suggests that smoking, blood lipids, and blood pressure were the three most important risk factors in reducing CHD mortality and incidence in developed countries. In the various studies, cholesterol reductions were responsible for between 0.4 and 50 percent of the reductions and population-level blood pressure reductions were responsible for between 6 and 21 percent of the reductions (Capewell et al., 1999, 2000; Ford et al., 2007; Hunink et al., 1997; Laatikainen et al., 2005; Unal et al., 2004; Vartiainen et al., 1994b). Smoking reduction alone was responsible for between 6 and 56 percent of the reductions in the various studies.
Several studies have also provided analyses of the role that dietary changes may have played in the reduction of CHD mortality and incidence. Slattery and Randall (1988) reviewed dietary trends in the decades prior to the decline of CVD in the United States and found a series of changes in eating patterns that occurred 10 to 20 years before the decline and could have contributed to it. This is supported further by Hu et al. (2000), who found that improvements in diet accounted for a 16 percent decline in CHD incidence from 1980 to 1994 in the women in the Nurses’ Health Study. In Finland, Pietenin et al. (1996) found that dietary changes instituted in the 1970s explained nearly all the reduction in cholesterol observed in the Finnish population. This is significant because the reduction in cholesterol was the most important factor in the overall reduction of CHD mortality in Finland between the 1970s and early 1990s (Laatikainen et al., 2005; Vartiainen et al., 1994b).
Indeed, few countries have documented their declines in CVD risk and CVD mortality as well as Finland. Since the 1970s both stroke and CHD mortality in Finland have declined 75 to 80 percent and the average life expectancy has increased by 5 to 6 years (Karppanen and Mervaala, 2006). These declines came about when government, health professionals, farmers, food companies, and local nongovernmental organizations invested decades of sustained work implementing efforts to support a more healthful diet (reducing saturated fat and sodium consumption, increasing fruit and vegetable consumption), reduce smoking prevalence, and promote the use of risk factor-reducing medications where indicated. As a result of these comprehensive efforts to reduce CVD risk, between 1972 and 2007, serum cholesterol declined 21 percent among men and 23 percent among
women, systolic blood pressure declined by 10.1 mmHg in men and 18.6 mmHg in women, and male smoking prevalence declined from 52 to 31 percent in the North Karelia Province (Puska et al., 2009). These results have implications as a potential model for intervention, which is discussed further in Chapter 5.
Conclusion 2.2: The broad causes for the rise and, in some countries, the decline in CVD over time are well described. The key contributors to the rise across countries at all stages of development include tobacco use and abnormal blood lipid levels, along with unhealthy dietary changes (especially related to fats and oils, salt, and increased calories) and reduced physical activity. Key contributors to the decline in some countries include declines in tobacco use and exposure, healthful dietary shifts, population-wide prevention efforts, and treatment interventions.
In summary, examination of global trends in CVD burden and mortality as well as analysis of the causal factors driving these trends provide a compelling argument in support of the prioritization of CVD prevention and reduction efforts worldwide—and especially in low and middle income countries. Countries and regions are either currently experiencing high CVD burden and mortality rates or they can expect to see CVD burden and mortality rates increase because of disturbing trends in the prevalence of well-established CVD risk factors in their population. Even countries that have been successful in reducing the burden of CVD over the past 40 years cannot be complacent, as certain risk factors, such as the prevalence of overweight and obesity, continue to grow despite successes in the reduction of other risk factors.
A LIFE-COURSE PERSPECTIVE ON CVD
The life-course perspective to chronic disease recognizes that CVD and other chronic diseases are the result of risks that accumulate throughout an individual’s lifetime. The perspective further recognizes that these risks can and must be reduced and prevented at all stages of life (Aboderin et al., 2002). In keeping with this principle, risk for CVD begins to accumulate as early as fetal life and continues to do so through infancy, childhood, adolescence, and adult life.
The 1998 IOM report sounded the alarm about the possible role that early factors in infancy play in increasing CVD incidence later in life and the growing worldwide recognition—based on new data from prospective cohort studies—of the importance of the fetal and early childhood stages to the later onset of CVD (IOM, 1998; Victora et al., 2008; Walker and
George, 2007). Since the 1998 report, there has been a large body of evidence linking undernutrition in early life to increased chronic disease risk later in life. Gluckman and Hanson (2008) have described how important it is for infants to be of optimal weight; when they are either under or overweight, they are at risk for a higher incidence of CVD in later life. In addition, low birth weight (LBW) and rapid weight gain after infancy are now recognized to increase the risk of CVD and diabetes in adulthood (Barker et al., 2005; Prentice and Moore, 2005). These findings raise important considerations for addressing global CVD as LBW and exposure to undernutrition in utero are common in many developing countries (Caballero, 2009; Kelishadi, 2007). A consensus has not yet emerged on what constitutes optimal nutrition and growth, but greater consideration of lifetime risk in nutrition programs currently implemented in many maternal and child health programs is an opportunity to promote cardiovascular health early in life. The influences of these factors in pregnancy and early childhood on risk for CVD are discussed in greater detail in Chapter 6.
Many major risk factors for CVD are established in childhood and adolescence (Barker et al., 1993; Celermajer and Ayer, 2006; Freedman et al., 2001; Strong et al., 1999). These include tobacco use, dietary and physical activity behaviors, overweight and obesity, and adverse childhood experiences (Celermajer and Ayer, 2006; Dong et al., 2004; Freedman et al., 2001). Poor social circumstances in childhood have also been linked to CVD later in life in a number of different cohorts conducted in the United States and Europe (Davey Smith et al., 2001; Galobardes et al., 2006). The acquisition and augmentation of risk for CVD in childhood and adolescence are also discussed in more detail in Chapter 6.
By middle age, many individuals have often already accumulated significant risk, yet the potential for ongoing accumulation exists. This is demonstrated by the effectiveness of rigorous prevention and reduction of risk factors during middle age, including continued management of blood pressure, blood lipids, and diabetes; promotion of exercise and healthful eating; and quitting smoking (Goldman et al., 2009; Kalache et al., 2002). Aside from preventing the onset of disease and premature death, another key goal of risk factor reduction efforts, especially in middle age, is to prevent premature morbidity and disability (Fries, 1980; Kalache et al., 2002; Olshansky and Ault, 1986).
The accumulation of risk in later life is especially important given that, over the past 150 years, life expectancies in most parts of the world have increased dramatically (WHO, 1999). All indications suggest that this trend will continue through the 21st century, making it likely that most babies born in countries with long life expectancies since 2000 will live to see their 100th birthday (Christensen et al., 2009). This rise in the elderly population is not only occurring in developed countries. Demographers predict that by
2020, 70 percent of the world’s elderly population will be living in developing countries (Kalache, 1999). As more and more people live into old age, an emphasis on delaying the onset of disability due to chronic diseases becomes increasingly important. Research has found that CVD is the second leading cause of disability among Americans aged 65 years and older, and that even subclinical CVD can significantly increase frailty, hospitalizations, and institutionalizations. However, research also indicates that ongoing risk factor-reduction efforts, particularly the promotion of increasing levels of physical activity, can significantly reduce disability and help prevent adverse cardiovascular outcomes among the elderly (Rich and Mensah, 2009, 2010; Sattelmair et al., 2009). Studies of nonagenarians, centenarians, and super-centanarians (individuals aged 110 to 119 years) reveal that it is possible to live independently and without significant assistance into the 10th and 11th decades of life; however, minimizing the accumulation of risks throughout the life course through health promotion is critical to this postponement of disability (Christensen et al., 2009).
Taken together, the evidence reinforces the need for a rigorous, life-course approach to the prevention of CVD that starts in utero and continues throughout life. The acquisition and augmentation of risk throughout the life course underscores the importance of building an array of health-promoting and disease prevention strategies that address specific age-sensitive periods of life and have long-term impacts over decades. This unifies CVD prevention with early childhood development as well as with efforts to promote healthy aging. Opportunities for interventions throughout the life course are discussed in more detail in Chapters 5 and 6.
INDIVIDUAL RISKS FOR CVD
Proximal risks for CVD include those associated with consumption patterns (mainly linked to diets, tobacco and alcohol use), activity patterns, and health service use as well as biological risk factors such as increased cholesterol, blood pressure, blood glucose, and clinical disease. The Framingham Study first centered attention on the concept of “risk factors” associated with CVD, and most recently reported substantial 30-year risk data showing the accumulation of risk over time (Pencina et al., 2009). Importantly, risk factors for the incidence of CVD and those associated with CVD severity or mortality are not synonymous. Risk factors for incidence become important starting very early in life and accumulate with behavioral, social, and economic factors over the life course to culminate in biological risks for CVD such as increased cholesterol, blood pressure, blood glucose, and clinical disease. Over the past few decades, the effectiveness of early screening and long-term treatment for biological risks or early
disease has contributed to the sharp declines in CVD mortality seen in many countries (Hunink et al., 1997).
This section focuses on these proximal behavioral and biological risks for CVD, while Chapter 3 includes a more detailed discussion of broad systemic drivers of CVD.
Better Data on Individual Risk Factors
The recent WHO Global Health Risks Report of 2009 (Lopez et al., 2006) and the earlier World Health Report of 2002 provide comparable and robust estimates of the contribution of risks to total mortality and measures of disability (Mathers et al., 2003; WHO, 2002, 2009b). This kind of data, which was explicitly called for in the 1998 IOM report, allows policy makers to shift their focus upstream from diseases and deaths to risks. Relatively few major behavioral and biological risk factors account for CVD incidence around the world. Tobacco use, diet (including alcohol, total calorie intake, and specific nutrients) and physical inactivity serve as the three major behavioral risks. Between them, they account for a significant proportion of cancer, diabetes, and chronic respiratory disease incidence in addition to CVD (Hu et al., 2001; van Dam et al., 2008; WHO, 2002; Yach et al., 2004, 2005). Concerted action focused on these behavioral risks, along with biological risks such as high blood pressure, high blood lipids, and high blood glucose, would have a wide impact on the global incidence and burden of disease (WHO, 2009b).
Reflecting the predominant role of CVD and its related risk factors in global mortality, Table 2.2 highlights the role of these biological and behavioral factors as the leading global risks for mortality from all causes. High blood pressure, tobacco use, elevated blood glucose, physical inactivity, and overweight and obesity are the five leading factors globally. In middle income countries, alcohol replaces high blood glucose in the top five; in low income countries, a lack of safe water, unsafe sex, and undernutrition are important. These latter points are discussed further in this report in relation to both the role of early childhood nutrition in the later onset of CVD as well as the need to integrate the management of HIV/AIDS more closely with CVD in low income countries (WHO, 2009b).
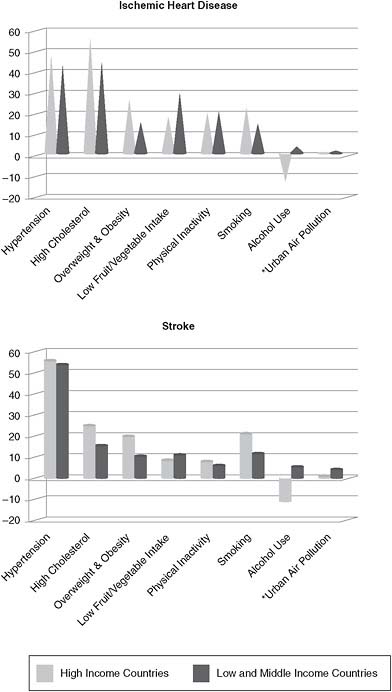
The Global Burden of Disease and Risk Factors report provides additional analysis of the relative contribution of individual risk factors specifically to CVD burden. Using 2001 data, the report estimates the percentage decrease in IHD and stroke burden that could be expected if population exposure to a risk factor were reduced to zero by calculating the population attributable fraction for each of the key CVD risk factors. This analysis is summarized in Table 2.3 and Figure 2.4. The report found that hypertension, high cholesterol, overweight and obesity, smoking, low fruit
TABLE 2.2 Ranking of 10 Selected Risk-Factor Causes of Death by Income Group, 2004
|
Region |
Rank |
Risk Factor |
Deaths (Millions) |
% of Total |
|
World |
1 |
High Blood Pressure |
7.5 |
12.8 |
|
|
2 |
Tobacco Use |
5.1 |
8.7 |
|
|
3 |
High Blood Glucose |
3.4 |
5.8 |
|
|
4 |
Physical Inactivity |
3.2 |
5.5 |
|
|
5 |
Overweight and Obesity |
2.8 |
4.8 |
|
|
6 |
High Cholesterol |
2.6 |
4.5 |
|
|
7 |
Unsafe Sex |
2.4 |
4.0 |
|
|
8 |
Alcohol Use |
2.3 |
3.8 |
|
|
9 |
Childhood Underweight |
2.2 |
3.8 |
|
|
10 |
Indoor Smoke from Solid Fuels |
2.0 |
3.3 |
|
High Income Countriesa |
1 |
Tobacco Use |
1.5 |
17.9 |
|
|
2 |
High Blood Pressure |
1.4 |
16.8 |
|
|
3 |
Overweight and Obesity |
0.7 |
8.4 |
|
|
4 |
Physical Inactivity |
0.6 |
7.7 |
|
|
5 |
High Blood Glucose |
0.6 |
7.0 |
|
|
6 |
High Cholesterol |
0.5 |
5.8 |
|
|
7 |
Low Fruit and Vegetable Intake |
0.2 |
2.5 |
|
|
8 |
Urban Outdoor Air Pollution |
0.2 |
2.5 |
|
|
9 |
Alcohol Use |
0.1 |
1.6 |
|
|
10 |
Occupational Risks |
0.1 |
1.1 |
|
Middle Income Countriesa |
1 |
High Blood Pressure |
4.2 |
17.2 |
|
|
2 |
Tobacco Use |
2.6 |
10.8 |
|
|
3 |
Overweight and Obesity |
1.6 |
6.7 |
|
|
4 |
Physical Inactivity |
1.6 |
6.6 |
|
|
5 |
Alcohol Use |
1.6 |
6.4 |
|
|
6 |
High Blood Glucose |
1.5 |
6.3 |
|
|
7 |
High Cholesterol |
1.3 |
5.2 |
|
|
8 |
Low Fruit and Vegetable Intake |
0.9 |
3.9 |
|
|
9 |
Indoor Smoke from Solid Fuels |
0.7 |
2.8 |
|
|
10 |
Urban Outdoor Air Pollution |
0.7 |
2.8 |
|
Low Income Countriesa |
1 |
Childhood Underweight |
2.0 |
7.8 |
|
|
2 |
High Blood Pressure |
2.0 |
7.5 |
|
|
3 |
Unsafe Sex |
1.7 |
6.6 |
|
|
4 |
Unsafe Water, Sanitation, Hygiene |
1.6 |
6.1 |
|
|
5 |
High Blood Glucose |
1.3 |
4.9 |
|
|
6 |
Indoor Smoke from Solid Fuels |
1.3 |
4.8 |
|
|
7 |
Tobacco Use |
1.0 |
3.9 |
|
|
8 |
Physical Inactivity |
1.0 |
3.8 |
|
|
9 |
Suboptimal Breastfeeding |
1.0 |
3.7 |
|
|
10 |
High Cholesterol |
0.9 |
3.4 |
|
a Countries grouped by gross national income per capita—low income ($825 or less), high income ($10,066 or more). SOURCE: Adapted from WHO, 2009b. |
||||
and vegetable intake, and physical inactivity were the leading contributors to IHD and stroke burden worldwide (Lopez et al., 2006). These findings are consistent with other large-scale studies of risk-factor contributions to overall CVD burden (see the discussion of the INTERHEART study in the following paragraphs); however, it should be noted that the report did not examine the role of elevated blood glucose in its analyses.
In addition to calling for better global data on CVD risks, the 1998 IOM report also recommended the use of case-control studies to establish the role of major risks for CVD (IOM, 1998). The INTERHEART study was an important response to this call (Iqbal et al., 2008; Yusuf et al., 2004). It enrolled approximately 15,000 cases and 15,000 controls from 52 countries in Western, Central, and Eastern Europe; the Middle East; Asia; and Africa to examine the impact of risk factors on incidence of AMI. Although there are limitations in comparing the INTERHEART study, a case-control study, to a classical prospective cohort study, its major findings are reminiscent of the conclusions of the original Framingham Study several decades ago as well as its 30-year follow-up studies (Yusuf et al., 2004). The INTERHEART study found that abnormal blood lipids are the most important contributors to CVD globally. Tobacco was the second most important risk factor, coequal to lipids in men but lower in women. Other key risk factors included abdominal obesity, psychosocial factors, hypertension, and diabetes (Yusuf et al., 2004).
While the INTERHEART study showed that the top risk factors contributing to CVD are generally consistent globally, the study also found distinct regional differences, much like the data described previously on the rising trends in CVD prevalence over time. For example, while abdominal obesity was the greatest or second-greatest contributor to CVD risk in 8 of the 10 regions studied, it was the smallest contributor in China. In addition, while psychosocial factors were among the top three risk factors by both population attributable risk and odds ratio (measures of risk-factor burden and impact, respectively) in Western Europe, the Middle East, China, and North America, they appeared to be much less influential in Central and Eastern Europe and South Asia (Iqbal et al., 2008; Yusuf et al., 2004).
Few studies have quantified the consequent impact of these risks on the risk of stroke in developing country populations. However, findings from a study in the United Kingdom are informative. A cohort of 20,040 people was followed over 11 years to determine the risk of stroke incidence. Four measures of health behaviors combined—smoking, low physical activity, low plasma vitamin C levels (used as a proxy for fruit and vegetable intake), and not drinking alcohol in moderation (abstaining from alcohol or consuming more than 14 drinks per week)—predicted more than a two-fold increase in stroke incidence (Myint et al., 2009). This is consistent with prior findings in large cohorts of men and women in the United States that
TABLE 2.3 Contribution of Selected Risk Factors (by Population Attributable Fractions [PAF]) to IHD and Stroke Burdens, 2001
|
|
Risk Factor |
World |
High Income Countries |
Low and Middle Income Countries |
|
Ischemic Heart Disease |
High Blood Pressure |
45% |
48% |
44% |
|
|
High Cholesterol |
48% |
57% |
46% |
|
|
Overweight and Obesity |
18% |
27% |
16% |
|
|
Low Fruit and Vegetable Intake |
28% |
19% |
30% |
|
|
Physical Inactivity |
21% |
21% |
21% |
|
|
Smoking |
17% |
23% |
15% |
|
|
Alcohol Use |
2% |
–13% |
4% |
|
|
Urban Air Pollutiona |
2% |
1% |
2% |
|
Stroke |
High Blood Pressure |
54% |
56% |
54% |
|
|
High Cholesterol |
16% |
25% |
15% |
|
|
Overweight and Obesity |
12% |
20% |
10% |
|
|
Low Fruit and Vegetable Intake |
11% |
9% |
11% |
|
|
Physical Inactivity |
7% |
8% |
6% |
|
|
Smoking |
13% |
21% |
12% |
|
|
Alcohol Use |
3% |
–11% |
5% |
|
|
Urban Air Pollutiona |
3% |
1% |
4% |
|
a PAFs for Urban Air Pollution have large uncertainty. SOURCE: Data from Lopez et al., 2006. |
||||
a healthful diet and lifestyle—not smoking, regular exercise, moderate alcohol consumption, and not being overweight—was associated with nearly 80 percent lower risk of ischemic stroke compared to having none of these healthy lifestyle components (Chiuve et al., 2008).
Conclusion 2.3: The major contributing individual risk factors for CVD are generally consistent across the globe and include abnormal blood lipids, tobacco use and exposure, abdominal obesity, psychosocial factors, hypertension, and diabetes. However, the detailed underlying risk profile differs across populations and varies over time. Interventions and prevention strategies need to focus on current local risk profiles to ensure they are adapted to the specific settings where they will be applied.
Major Proximal Risk Factors for CVD
This section described the major risk factors for CVD in more detail. The section begins with behavioral risk factors, including tobacco use, di-
etary factors, alcohol, and physical activity. This is followed by the major biological risk factors that mediate the role of these behaviors in leading to CVD, including obesity, blood pressure, blood lipids, and diabetes. Finally, additional contributing factors are also discussed, including mental health, genetics, and air pollution.
Tobacco
There are currently more than 1 billion smokers worldwide. Although use of tobacco products is decreasing in high income countries, it is increasing globally, with more than 80 percent of the world’s smokers now living in low and middle income countries (Jha and Chaloupka, 1999). In China alone, there are 303 million adult smokers and 530 million people passively exposed to secondhand smoke (Yang et al., 2008). Tobacco use kills 5.4 million people a year—more than the annual deaths due to tuberculosis (TB), HIV/AIDS, and malaria combined—and accounts for 1 in 10 adult deaths worldwide (Mathers and Loncar, 2006; WHO, 2009e). In the 20th century 100 million deaths were caused by tobacco, and, if current trends continue, there will be up to 1 billion deaths in the 21st century (WHO, 2008c). By 2030, researchers estimate that 80 percent of tobacco-related deaths will occur in low and middle income countries (Mathers and Loncar, 2006).
In the Global Burden of Disease study, Lopez et al. (2006) estimated that in 2000, 880,000 deaths from CHD and 412,000 deaths from stroke were attributable to tobacco. These data are based on updated estimates of the relative risk of death among smokers for CHD, stroke, and hypertensive heart disease. The relative risks are highest in young people (as found by the INTERHEART study and described earlier). However, the most common type of tobacco-related CVD deaths varies around the world. For example, in India, a higher proportion of smokers die from CHD; in China, tobacco kills more through stroke (Ezzati et al., 2005).
Smoking cessation has been shown to have significant impacts on reducing CHD. In a major review of the evidence, Critchley and Capewell (2003) determined that successful smoking cessation reduced CHD mortality risk by up to 36 percent. Smoking cessation leads to significantly lower rates of reinfarction within 1 year among patients who have had a heart attack and reduces the risk of sudden cardiac death among patients with CHD (Gritz et al., 2007). There is consensus in the literature that CVD risk drops precipitously within the first 2 to 3 years of smoking cessation. Although the specific timeline of risk reduction depends on the number of years as a smoker and the quantity of tobacco smoked daily, it is conceivable that, over time, former smokers’ CVD risk can drop to levels similar
to that of someone who has never smoked (Gritz et al., 2007; Mackay and Eriksen, 2002).
Two major trends are of real concern with respect to the future of tobacco-related CVD. First, in most parts of the world, the smoking rates are higher among the poorest populations (WHO, 2008c). The second worrisome trend is in smoking among girls. The disparity in smoking prevalence between boys and girls in their teenage years is much less than the ratio reported among adults from the same regions (Brands and Yach, 2002). In most parts of the developing world, women smoke at a significantly lower rate than men, a disparity that could help explain the lower rates of cardiovascular mortality among women (see the discussion of gender differences in CVD later in this chapter) (Pilote et al., 2007). However, the Global Youth Tobacco Survey found that girls smoked at the same rate as boys in more than 60 percent of the countries included in the survey (Shafey et al., 2009; Warren, 2003; Warren et al., 2008). If future generations of girls catch up to boys and smoke at the rates that men do today, CVD and associated tobacco-related death rates will rise sharply. On the other hand, if policies could instead bring both men’s and women’s smoking rates to below those of women today, the preventive gain would be immense.
In addition to active smoking, it has become increasingly apparent that exposure to secondhand smoke significantly increases cardiovascular risk. A recent IOM review of the effects of secondhand smoke exposure concluded that exposure to secondhand smoke significantly increases cardiovascular risk and that public smoking bans can significantly reduce the rate of heart attacks. The report concluded that secondhand smoke exposure increases cardiovascular risk by 25 to 30 percent and that there is sufficient evidence to support a causal relationship between secondhand smoke exposure and AMI. This causality was reinforced by the report’s conclusion that smoking bans significantly reduce the rate of AMIs, with declines ranging from 6 to 47 percent (IOM, 2009).
Dietary Factors
The relationship between CVD and diet is one of the most studied relationships in epidemiology. Several key relationships identified decades ago remain valid, while others have evolved in the light of better-quality research. For example, current evidence does not support the use of general terms like “lipids” or “fats” without qualifying their type and considering the amount used in the diet. Although nutritional research has traditionally focused on the effect of individual food groups or nutrients on CVD, there has been a shift in recent years toward comparing how different types of dietary patterns in their entirety affect CVD risk. The following sections reflect this shift by first discussing research on oils and salt—two key di-
etary components that have clear and well-demonstrated impacts on CVD risk—and then moving on to a discussion of different dietary patterns and CVD risk.
WHO and FAO reviewed the evidence on the relationship between diet, physical activity, and CVD in the context of a broader review of the impact on all chronic diseases (Joint WHO/FAO Expert Consultation, 2003). The most convincing evidence for decreasing dietary risk involves addressing the following factors: reducing saturated fat intake, maintaining low to moderate intake of alcohol, and increasing the consumption of linoleic acid, fish and fish oils, vegetables and fruits, and potassium. On the other hand, intake of myristic and palmitic acids, transfatty acids, high levels of sodium, overweight, and heavy alcohol use increase the risk of CVD (Joint WHO/ FAO Expert Consultation, 2003). Recent evidence augments this list with the addition of whole grains, nuts, beans, and seeds (Danaei et al., 2009). The evidence for these dietary factors is derived from studies in developed and, increasingly, developing countries.
As described earlier, the analysis and interpretation of dietary factors has been hampered by the poor availability of high-quality data for detecting broad-based trends. Data derived from actual consumption surveys (such as the U.S. National Health and Nutrition Examination Survey [NHANES] data) are important if we are to base policy on evidence. However, few countries provide basic data on the contribution of various food groups to the total intake of calories, sodium, or other major nutrients of interest to CVD. Improved data about details of the contribution of major food groups to diets around the world are needed to better inform future agricultural policy and gain a more accurate picture of how changes in consumption affect CVD risk.
Oils1 As discussed earlier, the rapid rise in the production and consumption of tropical oils has worried many CVD researchers because of their adverse effects on CVD risk. Healthy oils are those that contain no commercially introduced transfatty acids, are low in saturated fatty acids, and are high in mono- and polyunsaturated fatty acids (see Figure 2.5 for a comparison of the fatty acid composition and shelf life of selected cooking oils). Nutritionally, the most important mono- and polyunsaturated fatty acids are oleic acid and linoleic acid, respectively. Olive and canola oils have high concentrations of oleic acid, whereas nonhydrogenated soybean oils and sunflower oils have high concentrations of linoleic acid. All four of these oils are also low in saturated and transfats, but their shelf lives and cooking properties (smoke point, flavor, etc.) vary. High- and mid-oleic
sunflower oils both have long shelf lives, but unfortunately they remain relatively expensive and less abundant in many low and middle income countries. In order to be truly effective, low and middle income countries that have high levels of oil consumption will need to develop affordable supplies of healthy oils at prices that are competitive with tropical oils (Khan and Mensah, 2009).
Transitioning from less healthful tropical oils to more healthful oils could significantly reduce the amount of saturated and transfatty acids used in highly processed foods and daily cooking. However, such a transition is challenging because the relatively low price of palm oil drives its predominance in oil production. In order to transition away from tropical oils, there is a need to find or develop oils that are healthful and have favorable cooking properties but are also affordable and have a long shelf life. Some countries, such as Argentina, Chile, Brazil, and Turkey, have had modest success in increasing the availability and reducing the costs of healthful oils through oilseed plantation and production projects. Other initiatives have had less success, such as in Peru, where pilot programs concluded that low yields and high costs make the transition unprofitable (Khan and Mensah, 2009).
In sum, the challenge of transitioning to healthier oils highlights a critical need for agricultural policy and production to be better aligned with a heart-healthy diet. Dramatic changes in the food supply in developing countries have occurred over the past two decades. Changes in agricultural opportunities and investments have driven many of these changes, without careful consideration of the system-wide impacts on CVD. Further, the sharp increases in palm oil deserve special focus given the ubiquity of palm oil use, especially in emerging economies where its relatively low price acts as a barrier to the development and production of heart-healthier oils. The rationale for supporting transitions to more healthful oils is discussed further in Chapter 5.
Salt There is a strong and robust base of evidence that excessive sodium intake significantly increases CVD risk and that reduction in sodium intake on a population level decreases CVD burden (He and MacGregor, 2009). The most well-established mechanism by which sodium intake increases CVD risk is by increasing blood pressure. Numerous studies have found that there is a continuous and graded relationship between salt intake and blood pressure. This relationship has been confirmed in epidemiological, animal, population, migration, intervention, and genetic studies. Furthermore, population studies have established that reductions in sodium intake lead to declines in systolic and diastolic blood pressure, which in turn leads to a decrease in heart attacks and strokes (He and MacGregor, 2009). For example, since the 1970s, salt intake in Finland has been reduced by ap-
proximately one-third. This has led to a reduction in systolic and diastolic blood pressure (BP) by more than 10 mmHg (Karppanen and Mervaala, 2006). In their recent major review of sodium trends and impact, He and MacGregor concluded that a reduction in salt from the current global intake of 9 to 12 g/day to the recommended levels of 5-6 g/day would have a major impact on BP and on CVD (He and MacGregor, 2009). Salt’s impact on CVD, however, extends beyond blood pressure. Animal and epidemiological studies have found that a diet high in sodium may directly increase risk of stroke, which is independent and additive to salt’s effect on BP (He and MacGregor, 2009).
Dietary Patterns The effect on CVD risk of diets rich in whole grains and low in processed foods that are high in fat, sodium, and sugars has been increasingly investigated in both developed and developing countries. In parallel with economic development, radical dietary shifts toward Westernized diets that are high in animal products and refined carbohydrates and low in whole grains and other plant-based foods have occurred in many developing countries (Hu, 2008). In the INTERHEART study, three major dietary patterns were identified: Oriental (high intake of tofu and soy); Western (high in fried foods, salty snacks, eggs, and meat); and prudent (high in fruits and vegetables). The Western dietary pattern was associated with an increased risk of CHD in all regions of the world, whereas the prudent pattern was associated with a lower risk (Iqbal et al., 2008).
Substantial evidence has accumulated to support the notion that the traditional Mediterranean dietary pattern is protective against CVD (Fung et al., 2009; Martinez-Gonzalez et al., 2009). This pattern is characterized by an abundance of fruits, vegetables, whole grain cereals, nuts, and legumes; olive oil as the principal source of fat; moderate consumption of fish; lower consumption of red meat; and moderate consumption of alcohol. It is important to note, however, that the dominance in research on the Mediterranean diet has come at the cost of research on other diets commonly consumed around the world that may also have heart health benefits. A review of PubMed, Google Scholar, and EBSCOhost indicated that the Mediterranean, American/Western, Japanese and prudent diets were by far the most common dietary patterns studied, while very few researchers focused on other Asian, South American, or Middle Eastern diets. Comparative studies of whole diets constitute an important neglected research area with potentially profound implications for policy development.
Alcohol
The global burden of diseases attributable to alcohol has recently been summarized, leading to the conclusion that alcohol is one the largest avoid-
able risk factors in low and middle income countries (Rehm et al., 2009). Indeed, WHO estimates that the harmful use of alcohol was responsible for 3.8 percent of deaths and 4.5 percent of the global burden of disease in 2004 (WHO, 2009b). In the past few decades, consumption of alcohol has increased dramatically in men in countries undergoing nutrition transition, such as India and China, and has been extremely high in Russia for many decades, where it contributes significantly to overall mortality among men (WHO Expert Committee on Problems Related to Alcohol Consumption and WHO, 2007).
It has long been known that excessive alcohol intake is associated with increased risk for hypertension, stroke, coronary artery disease, and other forms of CVD; however, there is also a robust body of evidence in a range of populations that suggests that light to moderate intake of alcohol may reduce the risk of CHD. Indeed, research suggests that the relationship between alcohol intake and CVD outcomes follows a “J” curve, with the lowest rates being associated with low to moderate intakes of alcohol (Beilin and Puddey, 2006; Lucas et al., 2005). This protective effect of low to moderate intake has been replicated in numerous studies, across populations and gender, and persists even when controlling for potential confounders such as the “sick quitter” effect (Anand et al., 2008; Mukamal and Rimm, 2001; Yusuf et al., 2004). The definition of “low to moderate” continues to be a subject of debate; however, given the totality of the evidence, a prudent recommendation appears to be no more than one drink per day for women and no more than two drinks per day for men (Beilin and Puddey, 2006; Lucas et al., 2005; Mukamal et al., 2006).
It is important to recognize that, as with any discussion of alcohol and health, the key issues are the quantity of alcohol consumed and the risk or benefit conferred by consumption. Although evidence indicates that low to moderate alcohol use can reduce the risk of CHD, excessive and harmful use clearly increases CVD risk (Beilin and Puddey, 2006; Lucas et al., 2005). Alcohol may also contribute to overweight and obesity as it is a significant source of daily calories in many countries (Foster and Marriott, 2006; Jequier, 1999). It is also important to consider the demonstrated negative health effects of excessive and harmful alcohol use on other diseases such as neuropsychiatric disorders, cirrhosis of the liver, and various cancers. Taking into account these factors, it is important that approaches to reduce the burden of CVD not neglect the importance of reducing excessive alcohol consumption. WHO has proposed interventions for alcohol that are being considered in developing a global strategy for alcohol control. These include pricing policies, restricting the sale of alcohol, drunk-driving countermeasures, restrictions on marketing, awareness and education, and access to effective treatment (WHO, 2009d).
Physical Activity
WHO and FAO highlighted the importance of physical activity as a key determinant of obesity, CVD, and diabetes (Joint WHO/FAO Expert Consultation, 2003). For decades, evidence of the relationship between physical activity and CVD, independent of effects on weight and obesity, has strengthened. Increasing physical activity—including through brisk walking—has been shown to decrease the risk of chronic diseases such as CHD, stroke, some cancers (e.g., colorectal and breast cancer), type 2 diabetes, osteoporosis, high blood pressure, and high cholesterol (Physical Activity Guidelines Advisory Committee, 2008). Physical activity is also important for weight control and maintenance. In addition, regular physical activity is associated with a decreased risk of depression and improved cognitive function. Moreover, people who are physically active have improved quality of life and reduced risk of premature death (Physical Activity Guidelines Advisory Committee, 2008). Despite this powerful evidence, measurement weaknesses have contributed to the generally poor quality and availability of data on worldwide physical activity trends and impacts.
Guthold et al. (2008) recently published new data on levels of physical inactivity in 51 countries, most of which were low or middle income, and observed several trends. Globally, with the exception of several Eastern European countries (Croatia, the Czech Republic, Hungary, Kazakhstan, the Russian Federation, Slovenia, and the Ukraine), women were more likely to be physically inactive than men. Further, adults over 50 years of age were more likely to be inactive than younger adults, and city dwellers were more likely to be inactive than those who lived in rural areas. Physical inactivity levels were, with a few exceptions, similar in Eastern European, South Asian, and Western Pacific countries. In most of these countries, between 5 and 10 percent of men and between 10 and 16 percent of women were found to be physically inactive. By contrast, there was considerable variation in the levels of physical activity in both men and women within and across African, American, and Eastern European countries. For example, while women in 7 of the 18 African countries surveyed had the lowest levels of physical inactivity (fewer than 10 percent classified as physically inactive), Guthold found that more than 40 percent of women in Namibia, Swaziland, and South Africa were physically inactive. Despite the heterogeneity of the data, the study indicated that levels of physical inactivity in a number of low and middle income countries and among certain subgroups, particularly women aged 60-69 years, are disconcertingly high.
Few studies have explored the reasons why levels of physical activity are declining in developing countries. Therefore, the recent work by Ng et al. (2009) from China is important. The authors estimate that, between 1991 and 2006, average weekly physical activity among adults fell by 32
percent. This period was associated with rapid urbanization (especially improved housing and transport infrastructure) and industrialization leading to profound shifts in how people in China eat, move, and work. Meanwhile, sedentary behaviors such as prolonged television watching have increased dramatically. Many aspects of improving quality of life (such as better educational and sanitation facilities) were strongly associated with declines in physical activity, suggesting that multisectoral approaches involving workplace, transit, school, and leisure time need to be tackled if the trends are to be reversed. For this to happen, health professionals and policy makers need to fully appreciate the value of physical activity, both as a means to address energy balance and as an important avoidable cause of the global burden of chronic diseases. Currently this is not the case in most countries.
Overweight and Obesity
Another broad trend related to physical activity and nutrition, especially excess calorie intake, is obesity and overweight. This topic was not raised as an important issue at the inception of the Framingham Study, possibly because population levels of overweight in the 1940s were relatively low. It was also only briefly mentioned in the 1998 IOM report. During the past several decades, however, there have been steady increases in levels of overweight and obesity reported from developed and developing countries (Sassi et al., 2009). Even in low and middle income countries where undernutrition is still highly prevalent, overweight and obesity—especially among women—is a bourgeoning issue (Caballero, 2005). For instance, in South Africa, 59 percent of women and 29 percent of men over age 15 are overweight or obese (South African Department of Health and Medical Research Council, 2007). In China, trend lines for obesity are going up fairly sharply among all geographic groups in communities of all sizes, from rural villages to megacities (Wang et al., 2007). As described in more detail in Chapter 6, rates of overweight and obesity in children are also rising in low and middle income countries (WHO, 2008a).
As mentioned earlier, WHO and FAO reviewed the evidence on the relationship between obesity and the risk of CVD and concluded that overweight and obesity confer a significantly elevated risk of CHD (Joint WHO/FAO Expert Consultation, 2003). Increased body mass index (BMI) is also associated with greater risk of stroke in both Asian and Western populations (WHO/FAO, 2003). The association between obesity and CVD is partly, but not completely, mediated through hypertension, high cholesterol, and diabetes. Abdominal or central obesity measured by waist-to-hip ratio or waist circumference is associated with both CHD and stroke independent of BMI and other cardiovascular risk factors. Moreover, obesity is
also an independent risk factor for other cardiovascular outcomes, such as congestive heart failure and sudden cardiac death.
Excess energy intake is one of the key contributors to obesity. As highlighted earlier, the lack of data limits policy makers’ abilities to focus attention on which dietary components lend themselves to effective interventions that would reduce total calorie intake. In those countries that do have data, the collection methods vary so direct comparisons are not possible; however, a review of the data does indicate that the dietary contributors to total energy intake vary by country. National surveys of calorie intake from India indicate that in urban areas, cereals account for 56 percent of intake, compared to about 9 percent each for edible oils and dairy, 1 percent for meat and fish, and 0.4 percent for all beverages (Chatterjee et al., 2007). In China, cereals also dominate and account for 58 percent of total calorie intake compared to meat (13 percent) and cooking oils (17 percent) (Wang et al., 2005). As discussed earlier, trends in consumption indicate very rapid increases in oil use and slow decline in the consumption of cereals as contributors to calories. These trends in developing countries are in contrast to data for the United Kingdom, which could indicate where trends are headed in developing countries. National data from 2003 indicate that cereals and related products account for 31 percent of calories with other major categories including meat (15 percent), milk and related products (19 percent), and beverages (10 percent) (Office of National Statistics et al., 2003).
One category that has been well studied in developed countries relates to sugar consumption, primarily in the form of sugar-sweetened beverages (including soft drinks, juice drinks, and energy and vitamin water drinks). Recent NHANES data shows that up to 5.5 percent of dietary calories come from sugar-sweetened beverages in the United States (Bosire et al., 2009), which has led the American Heart Association to recommend an upper limit of 100 calories per day for women and 150 calories per day for men from added sugars, including soft drinks (Johnson et al., 2009).
In some developing countries, consumption of sugar-sweetened beverages has increased dramatically in recent decades. In Mexico, for example, it is estimated that adolescents consume more than 20 percent of their total energy intake from caloric beverages (Barquera et al., 2008). Because of its excess caloric and sugar content, increasing consumption of sugar-sweetened beverages may have important implications for obesity and cardiometabolic risk. Maintaining the relatively low per capita consumption of sugar-sweetened beverages in countries like India and China is a potential target of prevention programs. In India, all beverages account for less than 0.5 percent of total calories (Chatterjee et al., 2007). The equivalent figure in the United Kingdom is about 16 percent for all beverages for young adult men between 19 and 24 years of age with sweetened soft drinks accounting for about a third and alcohol the remainder (Henderson et al., 2003). This
indicates how critical it is to have national and even age- and gender-specific data if we are to develop effective nutrition messages and policies.
In summary, obesity has become a major global contributor to CVD incidence and mortality. It needs to be placed more centrally within future CVD policy initiatives. Better data on the sources of calorie intake and especially those calories that are high in salt, sugar, and saturated fat are also needed in order to develop science-based approaches to obesity prevention and control.
Blood Pressure
A recent review of the global burden of high blood pressure found that approximately 54 percent of stroke, 47 percent of IHD, 75 percent of hypertensive disease, and 25 percent of other CVDs were attributable to hypertension. This equates to an annual burden of approximately 7.6 million deaths, or 13.5 percent of the total number of annual global deaths, attributable to high blood pressure (Lawes et al., 2008). Furthermore, Lawes et al. (2008) found that more than 80 percent of the attributable burden of hypertension in 2001 occurred in low and middle income countries, and both another recent review and an analysis commissioned for this report found the prevalence of hypertension to be equally high in developed and developing countries (Gaziano and Kim, 2009; Pereira et al., 2009).
In China alone, it is estimated that the current age-standardized prevalence rate of hypertension is 17.7 percent, which translates into 177 million people, and that approximately 20 percent of deaths in China are attributable to high blood pressure (He et al., 2009; Yang, 2008). A significant contributor to these levels is the high average daily salt intake in China, which is estimated at 12 g per day—twice the Chinese and WHO recommended levels. Further, only 30 percent of adults with hypertension are aware of their condition, and of those only 6 percent manage their hypertension effectively (Yang et al., 2008). While antihypertensive medications have become more effective, their widespread use remains low and the number of people with uncontrolled blood pressure is increasing (Chobanian, 2009).
In Sub-Saharan Africa, hypertension is a predominant driver of CVD. Hypertensive heart disease and stroke, rather than ischemic heart disease, account for the majority of the CVD burden in the region, especially among black Africans (Mayosi et al., 2009; Mbewu and Mbanya, 2006; Muna, 1993). Prevalence of hypertension is particularly high in urban Sub-Saharan Africa, with between 8 and 25 percent of adults affected, depending on how hypertension is defined (Mbewu and Mbanya, 2006). In South Africa, the 2003 Demographic and Health Survey found that 12.5 percent of men and 17.9 percent of women were hypertensive (South African Department of Health and Medical Research Council, 2007). Unfortunately, the number
of people with uncontrolled hypertension is also high in the region (Mbewu and Mbanya, 2006). Researchers found that more than 70 percent of South African hypertensive patients’ blood pressure remained uncontrolled (South African Department of Health and Medical Research Council, 2007).
Among the major underlying risks for hypertension are sodium, body weight, and access to treatment (He and MacGregor, 2009; Reuser et al., 2009; Steyn, 2006; Yang et al., 2008). Primary prevention focused on sodium reduction, fruit and vegetable intake, weight control, and avoidance of excessive alcohol intake has been shown to make a difference. Finland’s experience (Karppanen and Mervaala, 2006) has potential applications for low and middle income countries where treatment levels remain extremely low and health systems have yet to adapt to managing chronic diseases like hypertension.
Blood Lipids
Researchers have studied the role of blood lipids in the development of atherosclerosis and the increase of CVD risk for decades. The Framingham Study first demonstrated the link between hypercholesterolemia and increased risk of CHD in the 1960s with the finding that lower levels of high-density lipoprotein (HDL) cholesterol as well as elevated levels of low-density lipoprotein (LDL) cholesterol were associated with increased CHD risk (Kannel et al., 1961, 1971). Subsequent studies confirmed these results and further established that elevated triglycerides also increase CVD risk (Gotto, 2005; Manninen et al., 1992). Furthermore, randomized controlled trials have shown that reduction of LDL cholesterol, both in primary and secondary prevention, is associated with reduced coronary event rates (Downs et al., 1998; Sacks et al., 1996; Shepherd et al., 1995). Reductions in LDL cholesterol have also been associated with a lowered incidence of stroke, although the data are not as strong as for CHD (Collins et al., 2004). In addition, lipoprotein(a) (Lp(a)) is an LDL–like particle that was independently associated with CHD and stroke in a recent comprehensive meta-analysis (Erqou et al., 2009).
The INTERHEART study recently confirmed that there was a graded relationship between abnormal lipid levels and risk for CHD in all regions of the world. In fact, the INTERHEART study found that abnormal blood lipids were the most important risk factor for myocardial infarction by odds ratio in all global regions (Yusuf et al., 2004). Further underscoring this, the Global Burden of Disease study estimated that elevated cholesterol was the third leading risk factor for worldwide mortality in general, after hypertension and smoking (Lopez et al., 2006).
While it is clear that dyslipidemia is one of the leading risk factors for CVD, there is significant regional variation in the prevalence of hyperlipid-
emia. Hypercholesterolemia was found in 22 percent of subjects enrolled in the Heart of Soweto study of patients with newly diagnosed CVD in South Africa (Sliwa et al., 2008). In Mongolia, the Ministry of Health, in collaboration with WHO, performed a STEPS survey across the country and reported 7 percent prevalence of hypercholesterolemia (WHO Regional Office for the Western Pacific, 2007). In contrast, a nationally representative population-based study in Iran found the prevalence of hypercholesterolemia to be more than 45 percent (Alikhani et al., 2009). In accordance with this geographic variability in the prevalence of hypercholesterolemia, the population-attributable risk of dyslipidemia for CHD in the INTERHEART study varied widely by geographic region (Yusuf et al., 2004). Although systematic data specifically regarding Lp(a) and its relationship to CVD among different populations around the world are lacking, levels have been shown to vary among different ethnic groups; in general, Asian Indians have higher Lp(a) levels than ethnic Chinese and Caucasian populations (Anand et al., 1998, 2000; Low et al., 1996). In addition, African Americans have higher average Lp(a) levels than Caucasians (Marcovina et al., 1996; Srinivasan et al., 1991), and studies in Africa have also shown higher average Lp(a) levels than in Caucasians (Evans et al., 1997).
Successful intervention programs in a number of countries have further supported the causal link between dyslipidemia and CVD by demonstrating that reductions in cholesterol lead to decreased CVD morbidity and mortality. In Finland, a nationwide multisectoral program targeted at multiple cardiovascular risk factors decreased population mean serum cholesterol levels as well as CVD mortality between 1972 and 1992 (Puska et al., 1998; Vartiainen et al., 1994a). These reductions in cholesterol were largely credited to reductions in saturated fat intake as well as more comprehensive cholesterol monitoring and treatment (Puska et al., 2009). Further analysis showed that among men the 13 percent reduction in cholesterol levels was singlehandedly responsible for a 26 percent reduction in CVD mortality (Vartiainen et al., 1994b). The proven success of interventions to reduce cholesterol has shifted thinking on the inevitability of atherosclerosis, with researchers now realizing that it is not an unavoidable byproduct of aging, but rather that it can be prevented and largely reversed through the use of diet modification and secondary prevention with statins.
Diabetes
Around the world, diabetes is growing increasingly common and is a significant contributor to CVD risk. People with diabetes have a more than two-fold greater risk of fatal and nonfatal CVD compared to non-diabetics, with some indication that diabetes mellitus may confer an equivalent risk of having had a cardiovascular event (Asia Pacific Cohort Studies Collabora-
tion, 2003; Haffner et al., 1998; Stamler et al., 1993). In fact, CVD is the leading cause of morbidity and mortality in people with diabetes (Booth et al., 2006a; Diabetologia, 2007; Kengne et al., 2007, 2009; Thomas et al., 2003).
The magnitude of the risk of CVD associated with diabetes is even greater in women and younger individuals. Indeed, there is substantial evidence that diabetes mellitus may erase, or substantially attenuate, the “female advantage” in the risk of CVD observed in non-diabetics, and that having diabetes may be equivalent to aging by at least 15 years with regard to the clinical manifestations of CVD (Booth et al., 2006b; Huxley et al., 2006).
Cardiovascular risk associated with blood glucose is continuous; thus, individuals without established clinical diabetes, but who are at increased risk of developing diabetes in the future, also have a higher risk of CVD (Asia Pacific Cohort Studies Collaboration, 2004). Based on this continuous association, higher-than-optimum blood glucose (fasting plasma glucose > 4.9 mmol/l) has been identified as the leading cause of cardiovascular deaths in most regions (Danaei et al., 2006). In 2001, for instance, 1.49 million deaths from IHD (21 percent of all IHD deaths) and 709,000 from stroke (13 percent of all stroke deaths) were attributable to high blood glucose in addition to the 950,000 deaths directly attributed to diabetes mellitus in the world (Danaei et al., 2006). These figures are particularly worrisome given that it is estimated that more than 344 million people around the world will have impaired glucose tolerance in 2010 (IDF, 2006).
Obesity is the single most important risk factor for type 2 diabetes, but unhealthy diet and physical inactivity also independently raise the population risk for diabetes (Schulze and Hu, 2005). According to the International Diabetes Federation’s Diabetes Atlas 2010, the global estimated prevalence of diabetes for 2010 among people aged 20 to 79 years will be approximately 285 million people (6.4 percent of the global population), of which some 70 percent will be living in developing countries (International Diabetes Federation, 2010). By 2030 this figure is expected to increase by more than 50 percent to some 438 million people, or 7.7 of the world’s population if preventive interventions are not put in place. The largest increases will take place in the regions dominated by developing economies (see Figure 2.6). Close to 4 million deaths in the same age group will be attributable to diabetes in 2010, representing 6.8 percent of all-cause global mortality. The highest number of deaths due to diabetes are expected to occur in countries with large populations—1,008,000 deaths in India, 575,000 in China, 231,000 in the United States, and 182,000 in the Russian Federation (Roglic and Unwin, 2010). Currently, 83 percent of all diabetes deaths occur in low and middle income countries (WHO, 2009b).
Diabetes is emerging as a particular concern in Asia, where more
than 110 million individuals were living with diabetes in 2007, a large proportion of whom were young and middle aged. Asians tend to develop diabetes at a relatively young age and low BMI, and by 2025 the number of individuals with diabetes in the region is expected to rise to almost 180 million, of which approximately 70 million will be in India and almost 60 million in China (Chan et al., 2009). The reasons for this increased risk are still being fully elucidated; however, “normal weight” Asians often exhibit features of abdominal or central obesity, which is particularly detrimental to insulin resistance and glucose metabolism. Moreover, the increased risk of gestational diabetes combined with exposure to poor nutrition in utero and overnutrition in later life may contribute to increased diabetes, resulting in a situation of “diabetes begetting diabetes” (Chan et al., 2009).
The balance of risks and benefits associated with intensive glucose control has been assessed in recent clinical trials, which have convincingly demonstrated beneficial microvascular outcomes of diabetes. By contrast, these trials have individually failed to show such an effect on cardiovascular outcomes. However, the extension of the follow-up of the Diabetes Control and Complications Trial in type 1 diabetes (Nathan et al., 2005) and the United Kingdom Prospective Diabetes Study in type 2 diabetes (Holman et al., 2008) have shown that intensive glucose control substantially lowered the risk of cardiovascular outcomes, suggesting a legacy effect with still unexplained underlying mechanisms. Recently conducted meta-analyses of relevant trials in people with type 2 diabetes have also consistently shown that intensive glucose control reduces the risk of major cardiovascular events by approximately 10 percent, primarily driven by a 10 to 15 percent reduction in the risk of CHD, compared with standard treatment in people with diabetes. Interestingly, this benefit appeared to be independent of concurring cardiovascular risk factors (Kelly et al., 2009; Ray et al., 2009; Stettler et al., 2006; Turnbull et al., 2009).
In sum, as with the escalating obesity epidemic, the prevalence of diabetes has increased dramatically worldwide. It is associated with serious health consequences and is a major risk factor for CHD and stroke. As such, prevention and management of diabetes are critical in reducing the global burden of CVD.
Psychosocial Risk and Mental Health
Psychosocial factors have been consistently associated with both the onset and the progression of CVD in large prospective and epidemiologic studies in multiple populations and regions, yet they remain underrecognized when compared with more traditional CVD risk factors. The factors that have been associated with CVD include depression, anxiety, anger, hostility, acute and chronic life stressors, and lack of social support (Everson-
Rose and Lewis, 2005; Figueredo, 2009; Shen et al., 2008). Although the causal pathways are not as well elucidated as for other risk factors, a robust body of evidence supports the conclusion that psychosocial factors independently and significantly increase both the risk of developing CVD and CVD morbidity and mortality.
Of all the psychosocial stressors associated with CVD, the link between depression and CVD is probably the best documented. There have been more than 100 published reviews and numerous meta-analyses since the early 1990s that have consistently found that depression and depressive symptoms are associated with an increased likelihood of developing CVD, a higher incidence of CVD events, poorer outcomes after CVD treatment and prevention efforts, and increased mortality from CVD. These associations remain even after controlling for other CVD risk factors and most studies have found a dose-response relationship between severity of depression and depressive symptoms and the frequency and severity of cardiac events (Everson-Rose and Lewis, 2005; Frasure-Smith and Lesperance, 2006; Glassman et al., 2003; Lesperance and Frasure-Smith, 2007; Lichtman et al., 2008; Rugulies, 2002). In one meta-analysis, Rugulies (2002) found that clinical depression increased risk of MI or coronary death by more than 2.5-fold and that depressed mood increased the likelihood of a future cardiac event by approximately 1.5-fold.
Depression and depressive symptoms are also associated with behaviors that increase CVD risk. Depressed patients are more likely to smoke, have poor diets, and be physically inactive. Furthermore, depression has been found to significantly increase the risk of nonadherence to medical treatment regiments and lifestyle changes, making depressed patients with CVD or high CVD risk less likely to adhere to prevention efforts (Lichtman et al., 2008; Ziegelstein et al., 2000). This has significant implications as most CVD risk-reduction interventions require patients to adopt long-term lifestyle changes or remain on risk factor–lowering medications for long periods of time. Poor adherence to long-term therapies for chronic diseases significantly reduces their effectiveness, increases the cost of treatment, and leads to a higher disease burden (Sabaté et al., 2003).
Depression is also significantly more common among patients with CVD than among the general population. Depression is approximately three times more common in patients after an AMI than among the general population, and between 15 and 20 percent of hospitalized patients with CHD meet the Diagnostic and Statistical Manual of Mental Disorders criteria for major depression (Burg and Abrams, 2001; Frasure-Smith and Lesperance, 2006; Lichtman et al., 2008). The evidence for this link is so compelling that the American Heart Association recently released a science advisory asserting that “the need to screen and treat depression [in cardiac patients] is imperative” (Lichtman et al., 2008, p. 1769).
Anger, hostility, anxiety, chronic and acute stress, and lack of social support have all been associated with increased CVD morbidity and mortality. Numerous studies dating back to the 1950s have linked individuals with so-called type A personalities (extremely hard driving, ambitious, competitive, time-urgent, and unusually quick-tempered) with increased risk of developing CHD (Everson-Rose and Lewis, 2005; Shen et al., 2008). General anxiety has been linked to increased risk of sudden cardiac death, as well as increased CVD morbidity, especially among men. Chronic stress, most often studied by examining work-related stress, has been associated with negative behaviors such as low physical activity and poor diet, increased likelihood of recurrent CVD, as well as physiological consequences such as decreased heart rate variability. Acute stress from traumatic life events such as the death of a relative, earthquakes, or terrorist attacks have all been associated with significant temporal increases in the incidence of MI (Everson-Rose and Lewis, 2005; Figueredo, 2009).
The varied psychosocial factors that have been associated with CVD are believed to effect CVD risk through largely the same direct (physiological) and indirect (nonphysiological) mechanisms. There is also a high degree of clustering of psychosocial risk factors, with individuals often experiencing multiple psychosocial conditions at once. Although the definitive causal physiological pathways by which psychosocial factors increase CVD morbidity and mortality have not been elucidated, there is consensus within the research community around several hypotheses. Psychosocial stressors have been shown to activate several nervous system pathways, such as the hypothalamic-pituitary-adrenocortical (HPA) axis as well as alter hormonal and pro-inflammatory secretions. All these responses have been shown to contribute to atherogenesis. Furthermore, as discussed earlier, psychosocial factors have also been associated with higher prevalence of unhealthy behaviors such as smoking, alcohol abuse, poor diet, physical inactivity, and nonadherence to medical regimens, thus representing an indirect means of increasing CVD risk (Everson-Rose and Lewis, 2005; Figueredo, 2009; Lesperance and Frasure-Smith, 2007; Lichtman et al., 2008).
While the associations between psychosocial factors and CVD have been found in numerous studies in a variety of different populations, the majority of these studies were conducted in high income countries with mostly male, Caucasian samples. Women and diverse ethnic groups have been underrepresented, and limited research has been conducted in low and middle income countries. There are, however, a few examples of studies examining the association between psychosocial factors and CVD in low and middle income countries and non-Caucasian, mixed-gender samples. Sarker and Mukhopadhyay (2008) examined stress among the Bhuttia population in Sikkim, India, and found that perceived psychosocial stress significantly affected blood pressure as well as the ratio of total cholesterol
over HDL cholesterol in both males and females. The INTERHEART study found that psychosocial risk factors (measured by answers to questions assessing levels of financial stress, work and home stress, major life events in the past year, and presence of depression) were significantly associated with increased risk of MI in all global regions and across gender and ethnic groups. Indeed, of the nine risk factors examined, psychosocial risk factors were the fourth most significant factor in the risk of MI globally in terms of population-attributable risk, and they appear to be particularly influential in China, North America, Western Europe, the Middle East, and Africa (Rosengren et al., 2004).
It is clear that psychosocial factors play an important role in increasing CVD risk through both direct and indirect means. Continued research is needed to further elucidate the mechanisms by which psychosocial stressors and mental illness affect CVD risk. It is also important that clinicians are made aware of the effect of psychosocial factors on CVD risk, prognosis, and adherence to prevention efforts through improved training and knowledge sharing.
Air Pollution
Over the past 20 years, there has been a growing body of evidence linking air pollution to increased CVD incidence and mortality. While many people intuitively associate air pollution with respiratory problems, research has shown that the majority of the adverse health outcomes related to air pollution are cardiovascular in nature (Brook, 2008).
Air pollution is composed of a mix of gaseous and particulate matter and is created largely as a result of fossil fuel combustion. In developing countries, cooking and wood burning are also significant contributors. Although there is evidence that gaseous components of air pollution may have an adverse effect on human health, the majority of research to date has focused on the detrimental effects of particulate matter air pollution, with the majority of this research focusing on the effects of fine particulate air pollution (particles that are 2.5 μm or less in diameter) (Brook, 2008; Brook et al., 2004).
Numerous epidemiological studies in both developed and developing regions of the world have found that both short-term (several hours to a few days) and long-term exposure to particulate matter air pollution significantly increases cardiovascular events and CVD deaths (Brook, 2008; Brook et al., 2004; Dominici et al., 2006; Gouveia et al., 2006; IOM, 2004, 2009; Langrish et al., 2008; Peng et al., 2008; Pope and Dockery, 2006; Pope et al., 2004). These studies indicate that the relative risk of CVD mortality increases by approximately 1 percent for every 10 μg/m3 increase in daily concentration of fine particle air pollution. Although this increased
risk of CVD mortality from short-term changes in particulate matter concentration translates into a fairly small increase in absolute number of deaths, evidence from long-term studies have found larger increases in risk. These studies, of which there are fewer, have found relative risk of CVD mortality increases between 9 and 95 percent for every 10 μg/m3 increase in annual average fine particle air pollution concentration, with the majority finding increases of less than 34 percent per 10 μg/m3 increase. It should be noted that while short-term studies have been conducted in many regions throughout the world, all the large-scale long-term studies have taken place in the United States and Europe (Pope and Dockery, 2006).
One of the reasons that this data causes concern is that concentrations of particulate matter air pollution in some cities, especially the rapidly growing mega-cities in some developing countries, reach alarmingly high levels. Although air pollution levels in most cities in the United States and Europe have been decreasing—with current concentrations between 5 and 30 μg/m3—levels in some large cities in the developing world have been increasing, with daily particulate concentrations that may exceed 200-500 μg/m3. At these high levels, particulate matter concentration in the air approaches that found in smoke-filled bars (Brook, 2008).
Indeed, the evidence of air pollution’s negative effect on cardiovascular health is consistent and strong enough that, in 2004, the American Heart Association published a scientific statement on the link, stating, “At the very least, short-term exposure to elevated PM [particulate matter] significantly contributes to increased acute cardiovascular mortality, particularly in certain at-risk subsets of the population…. The evidence further implicates prolonged exposure to elevated levels of PM in reducing overall life expectancy on the order of a few years” (Brook et al., 2004, p. 2666). The Institute of Medicine has also highlighted the detrimental effects of particulate matter air pollution on CVD incidence and mortality in several studies (IOM, 2004, 2009).
Despite the robust epidemiological evidence of air pollution’s negative effect on CVD incidence and mortality, the specific mechanisms by which particulate matter increases CVD risk are still unclear. A number of different mechanisms by which particulate matter air pollution could increase CVD risk have been proposed, specifically through autonomic mechanisms related to the activation of the sympathetic nervous system or the withdrawal of the parasympathetic nervous system, the release of pro-inflammatory or oxidative stress-inducing compounds from the lungs, and soluble particulate matter entering the blood-stream after inhalation that directly act on the cardiovascular system (Brook, 2008; Brook et al., 2004; Pope and Dockery, 2006). Many of these mechanisms are similar to those that have been proposed for second-hand smoke (which is, in and of itself, a component of air pollution and a significant contributor to indoor air
pollution) (Brook et al., 2004; IOM, 2009). Additional research is necessary to better elucidate the biological mechanisms by which air pollution increases CVD risk.
Genetics
Researchers have recognized for decades that family history of CVD is associated with increased atherosclerotic risk of heart disease, which led to the presumption of a genetic component to CVD. There are several well-characterized single-gene disorders that contribute to CVD, such as certain forms of familial hypercholesterolemia linked to mutations of the apolipoprotein B gene, and during the past few years, there have been major advances in the identification of genetic risk factors for CHD, stroke, and CVD risk factors such as blood pressure, blood lipids, obesity, and diabetes (Arking and Chakravarti, 2009; Arnett et al., 2007). The identification of genetic loci associated with CVD, such as 9p21 (Palomaki et al., 2010), has led to major advances in understanding the pathophysiology of CVD, but genetic variants identified to date have explained only a fraction of heritability and do not appear to have substantial added value in predicting CVD beyond traditional CVD risk factors. These genetic risk factors are unlikely to have substantial clinical utility with respect to prediction, diagnosis, and treatment in the near future (Arking and Chakravarti, 2009). The prevailing view within the research community is that the genetic underpinnings of most common forms of CVD involve a complex interplay of many different genes, and much work remains to develop a more thorough understanding of the complex gene–gene and gene–environment interactions involved in the development of CVD (Arnett et al., 2007).
Indeed, in addition to the investigation of genes that influence CVD and its risk factors, there has recently been a surge in research examining how environmental factors affect gene expression. Although research indicates that gene expression is most sensitive to environmental influence from conception to early life, there is also evidence that environmentally related gene expression changes can occur throughout life (Gluckman et al., 2009). This is an important emerging area of research for CVD. Future findings could have implications to help elucidate the physiological processes by which individuals with similar CVD risk profiles have different outcomes. Future research also could conceivably help develop new prevention and treatment strategies aimed at taking advantage of exogenous mechanisms that enhance or suppress the expression of key genes that play a role in mediating the development of CVD.
Looking forward, the explosive growth in molecular genetics techniques, advanced statistical methods, high-throughput technologies, and progress in studying gene–environment interactions should provide re-
searchers with the ability to broaden the scope and applicability of their research. Techniques such as proteomics could lead to potential biomarkers to profile CVD risk more accurately, which could, for example, improve prediction of acute vascular events (Arnett et al., 2007). In addition, there is also significant promise in the emerging field of pharmacogenetics, which could not only help researchers develop more effective medications, but also better understand why certain drugs appear to be more effective in certain people. Since the initial availability of statins in late 1980, few new CVD drugs have emerged. Advances in genomic research could prompt more effective use of existing drugs and new drug development. At this stage, however, research in these fields has only modest potential for influencing population outcomes (Arnett et al., 2007).
Gender Differences in CVD Risk
Although CVD has sometimes been considered a disease that predominantly affects men, it is the leading cause of death among both men and women globally (Blauwet and Redberg, 2007; Jackson, 2008). There are, however, a number of notable gender differences in CVD incidence, mortality, risk-factor profiles, outcomes, and clinical presentation. These differences remain consistent across populations and regions and are thus important to consider when developing CVD prevention and treatment programs.
In all but the oldest age groups, CVD prevalence, incidence, and mortality rates tend to be higher for men than for women. This finding has remained consistent historically (Lawlor et al., 2001) and across countries and regions (Allen and Szanton, 2005; Pilote et al., 2007; WHOSIS, 2009). In addition, women experience their first cardiovascular events later in life than men. The INTERHEART study found that, on average, women experience their first MI 9 years later than men (Anand et al., 2008). Similarly, a recent review of stroke epidemiology found that men have their first stroke an average of 4.3 years earlier than women (Appelros et al., 2009). These findings are supported by WHO Global Burden of Disease data, which show that the average age of MI and first stroke is consistently lower among men across countries (WHO, 2009a).
The reason most often cited for these gender differences is a protective effect of estrogen on the development of CVD risk factors, most notably hypertension and dyslipidemia (Regitz-Zagrosek, 2006; Roeters van Lennep et al., 2002). Estrogen is thought to contribute to premenopausal women’s tendency to have lower systolic blood pressure, higher levels of HDL cholesterol, and lower triglyceride levels than men (Buchanan and Brister, 2001; Pilote et al., 2007; Roeters van Lennep et al., 2002). The specific mechanisms of this protection have not been fully elucidated; however, estrogen
is known to affect the atherosclerotic and blood-lipid control process in a number of different ways (Roeters van Lennep et al., 2002). The erosion of this protection that occurs after menopause provides further evidence of estrogen’s protective role. Indeed, by age 75, women tend to have higher rates of hypertension and CVD than men (Legato, 1998; Narkiewicz et al., 2006).
However, despite the protective effect of endogenous estrogen on CVD development, estrogen replacement therapy in postmenopausal women does not reduce CVD risk and is not recommended as a method of primary or secondary prevention. In fact, recent evidence from clinical trials indicates that hormone replacement therapy increases the risk of adverse CVD events, especially stroke (Regitz-Zagrosek, 2006; Rossouw et al., 2002; Schaefer et al., 2003; Wassertheil-Smoller et al., 2003). In addition, oral contraceptives have also been associated with an increased risk of hypertension. Early formulations of these drugs contained a higher dose of hormones and increased risk of hypertension two- to three-fold. The current generation of oral contraceptives contain less than one-seventh the amount of hormones of the original generation of drugs, and most researchers believe they increase CVD risk far less than the contraceptives of the 1960s (Schaefer et al., 2003). However, smoking while taking oral contraceptives does increase CVD risk more than smoking alone (Rao, 1998).
The lower prevalence of smoking among women is another factor that could contribute to their decreased CVD incidence and mortality rates. Around the world, the prevalence of female smoking is lower than that of men (Pilote et al., 2007). These differences are particularly marked in low and middle income countries; however, they are also apparent in high income countries (see the discussion of regional differences in CVD earlier in this chapter). Unfortunately, this trend appears to be changing, as the gap between male and female smoking prevalence among adolescents aged 13 to 15 years is much narrower (WHOSIS, 2009). Furthermore, although smoking rates among both men and women have declined in high income countries since the middle of the 20th century, this has been less pronounced among women (Jackson, 2008). These trends are particularly troubling given that smoking lowers the age of menopause and there is evidence that it may be a stronger risk factor for MI among middle-aged women than men (Roeters van Lennep et al., 2002).
Although rates of smoking, dyslipidemia, and hypertension are generally lower among women than men, women tend to have less favorable profiles for other key CVD risk factors. Worldwide, women are more likely to be sedentary than men (Guthold et al., 2008). Some researchers have suggested that women’s subservient social status in many cultures and their lack of leisure time due to childcare and other familial responsibilities likely
contribute to their lower levels of physical activity (Brands and Yach, 2002; Pilote et al., 2007).
Another troubling gender difference is the increased prevalence of obesity among women. WHO data indicate that although overweight (BMI ≥ 25 kg/m2) is more common among men globally, obesity (BMI ≥ 30 kg/m2) is more common among women. This trend of increased obesity prevalence among women is consistent around the world, including in Sub-Saharan Africa (Barnighausen et al., 2008; Steyn, 2006), but it is particularly striking in a number of Middle Eastern countries where prevalence among women is more than 40 percent (WHOSIS, 2009). The trend is of particular concern in part because of the close association between obesity and diabetes. Diabetes is currently more common in men than women; however, its prevalence is increasing in both sexes and it appears to be a much stronger risk factor for CVD in women (Jackson, 2008; Pilote et al., 2007; Rao, 1998; Regitz-Zagrosek, 2006). Indeed, the presence of diabetes appears to eliminate any premenopausal protection associated with female gender (Roeters van Lennep et al., 2002).
In addition to traditional CVD risk factors, there are also several situations unique to women that can place them at increased CVD risk. During pregnancy and the post partum period, women are at an increased risk of stroke. Indeed, some researchers have found that women in their childbearing years (aged 15-35 years) have a higher incidence of stroke than men of the same age (Turtzo and McCullough, 2008). Furthermore, preeclampsia and eclampsia increase this risk and increase the risk of hypertension later in life (Jamieson and Skliut, 2009).
Finally, research has shown that women experience poorer outcomes when they have a CVD event. Studies in North America and Western Europe have found that women delay longer before seeking medical treatment at the onset of symptoms, wait longer to receive life-saving cardiac interventions, and have poorer outcomes following MI or stroke (Allen and Szanton, 2005; Pilote et al., 2007). Indeed, after a stroke or MI, women tend to have longer hospital stays, increased prevalence of depression and anxiety, higher short-term mortality, greater long-term disability, and higher rates of reinfarction than men (Allen and Szanton, 2005; Blauwet and Redberg, 2007; Pilote et al., 2007; Polk and Naqvi, 2005; Reeves et al., 2008).
CVD researchers have proposed a number of different reasons why women might delay seeking medical attention, receive delayed treatment, and experience poorer outcomes during and after an MI or stroke. One often-cited reason that women tend to wait longer to seek treatment during an AMI or a stroke is that many do not perceive themselves as being at risk. Studies in the United States and Europe have found that many women are
not aware of the signs of an MI or stroke and do not know that CVD is the number one cause of death among women (Jensen and Moser, 2008). Women are also more likely than men to present with atypical symptoms of stroke or MI, which researchers have cited as a possible reason for the delays in the administration of appropriate care (Allen and Szanton, 2005; Appelros et al., 2009; Blauwet and Redberg, 2007; Jamieson and Skliut, 2009; Pilote et al., 2007; Polk and Naqvi, 2005; Reeves et al., 2008; Turtzo and McCullough, 2008; Witt and Roger, 2003). Additionally, some researchers have postulated that much of the poorer outcomes women experience post MI or stroke might be because women tend to be older with more comorbid conditions than men when they experience a CVD event (Reeves et al., 2008). Whatever the reasons, because of the robust evidence demonstrating gender differences in CVD incidence, morbidity, and outcomes, these differences, as well as the unique needs of women, should be considered when developing CVD research priorities, policies, and health service interventions.
HEALTH SYSTEMS AND CVD
The status of health systems can have a profound impact on CVD outcomes. Significant gaps in the health care infrastructure and access to health care in many low and middle income countries contribute to CVD incidence and mortality (Yach et al., 2004). These include gaps in adequate systems for all health needs as well as specific imbalances when it comes to chronic disease needs. Mayosi et al. (2009) recently highlighted the reality of health systems in many low and middle income countries dealing with a diverse set of health problems, noting that HIV/AIDS and TB require similar approaches to disease management as CVD, yet health care systems are too often neither integrated nor adapted to tackle chronic conditions. In China, for example, the health care system has been set up for maternal and child health and controlling infectious diseases and is extremely weak for meeting the challenges of chronic diseases. Only 47 percent of people with hypertension are aware of their conditions (Gu et al., 2002). Among those who are treated, less than 10 percent have good control of their blood pressure or blood glucose (Gu et al., 2002). Because only 61 percent of urban residents and 46 percent of rural residents in China have health insurance (Liu et al., 2008), millions of people forgo medical care when they are ill because they cannot afford care for chronic diseases. Clearly, the system is too vulnerable to meet the increasing challenges of chronic diseases (Liu et al., 2008). Reports from Sub-Saharan Africa also reveal a disturbing imbalance in access to care for chronic diseases. Lack of diagnosis, drug stock-outs, ignorance and community indifference, and
TABLE 2.4 Comparison of Treatment Usage in EUROASPIRE and PREMISE Surveys of Patients with Coronary Heart Disease
premature death are common for diabetes and hypertension patients even while a successful treatment model for chronic infectious disease is widely available (Harries et al., 2008). Poor households in South Africa trying to access care for chronic illness face a range of breakdowns in the public health system (Goudge et al., 2009).
The WHO-led Prevention of Occurrences of Myocardial Infarction and Stroke (PREMISE) study included developing countries from the Middle East, Asia, and Latin America (Mendis et al., 2005) and gives some indication of gaps in delivery of needed health care for CVD in these settings. The PREMISE study quantified the size of the treatment gap for patients with CHD and, as shown in Table 2.4, showed much lower use of beta-blockers and statins compared to data in Europe from the European Action on Secondary Prevention by Intervention to Reduce Events (EUROASPIRE), which in particular reflected improvements in access to statins over time with a concomitant 51 percent decline in blood cholesterol levels (Kotseva et al., 2009b).
Although differences in methodology prevent rigorous comparisons of these data, the relative lack of implemented use of pharmaceutical interventions in the PREMISE study is illustrative of the potential link between rising trends in risk factors, lack of availability of and access to medicines, and inadequate delivery of health care services in developing countries. Importantly, in 2007, statins were added to the WHO Essential Medicine List (WHO, 2007). Furthermore, in 2009, nicotine replacement therapy for smoking cessation was approved (WHO, 2009c). While being on the list does not guarantee improved availability and access, these decisions may help ensure that governments can increase the access of their populations to pharmaceutical products needed to tackle leading risk factors for CVD.
Developing countries experience multiple simultaneous burdens of disease in settings where health systems are generally weak and where public health infrastructure is suboptimal. It is critical that decision makers consider this reality when determining which CVD interventions to prioritize. Interventions need to be appropriate to the health development capacity of the country. Because of this similarity in approaches to disease management, there is the potential for synergy between AIDS, TB, and CVD programs to achieve better integrated chronic disease models of care in rural and urban settings. The role of improved health care delivery in reducing the burden of CVD is discussed in more detail in Chapter 5.
THE INTERFACE BETWEEN INFECTIOUS DISEASES AND CARDIOVASCULAR DISEASE
Infectious Causes of Heart Disease
Although often overlooked because of their low incidence in developed countries, heart diseases caused by infectious agents remain a significant problem in many low and middle income countries (Muna, 1993; WHO, 2003; WHO Study Group on Rheumatic Fever and Rheumatic Heart Disease and WHO, 2004). These infection-related heart diseases include rheumatic heart disease (RHD), chagas heart disease, as well as pericarditis and cardiomyopathies caused by TB and HIV.
Rheumatic Heart Disease
RHD is probably the most well-known form of heart disease caused by infection. The pathophysiology of RHD involves several stages—an initial upper respiratory infection with group A streptococcus triggers a delayed immune response leading to acute rheumatic fever (ARF), with recurrent bouts of ARF leading ultimately to RHD. Once RHD has affected a person’s heart valves, the damage is permanent and can lead to heart failure, atrial fibrillation, sudden cardiac death, and embolic stroke later in life (Gaziano et al., 2006; Mackay et al., 2004). WHO estimates that an average of 1.5 percent of people living with RHD die each year (WHO Department of Child and Adolescent Health and Development, 2005).
Over the past 50 years, prevalence of RHD has declined significantly in high income countries; however, it remains common in low and middle income countries (Karthikeyan and Mayosi, 2009). A recent WHO Department of Child and Adolescent Health and Development assessment estimated that at least 15.6 million people are living with RHD and that between 200,000 and 300,000 deaths occur each year due to the disease and its sequelae (Carapetis et al., 2005; WHO Department of Child and
Adolescent Health and Development, 2005). This annual mortality is approximately the same as that of rotavirus and about half that of malaria (Watkins et al., 2009). Nearly 80 percent of the individuals with RHD live in less developed countries, making RHD—perhaps more than any other form of CVD—a disease that almost exclusively affects the poor and disenfranchised (Karthikeyan and Mayosi, 2009).
Although prevalence rates vary by region, RHD appears to be most common in Africa, Southeast Asia, and the Western Pacific with the greatest number of annual deaths in China, Indonesia, and the Indian subcontinent (Steer et al., 2002; WHO Department of Child and Adolescent Health and Development, 2005). The disease is also common among indigenous populations such as Australian Aborigines and the Maori in New Zealand (Steer et al., 2002).
Of all forms of heart disease, RHD is responsible for the greatest toll on children. The disease and its sequelae are the most common cause of cardiac problems in children in low and middle income countries, and WHO estimates that it affects nearly 2.4 million children aged 5-14 years worldwide (Steer et al., 2002; WHO Department of Child and Adolescent Health and Development, 2005). Of these, approximately 1 million live in Sub-Saharan Africa, 750,000 live in South-Central Asia (Southeast Asia and some Eastern Mediterranean countries), and more than 175,000 live in China (WHO Department of Child and Adolescent Health and Development, 2005).
The decline of RHD in developed countries has been attributed to a number of factors. One is better access to prevention of RHD through the diagnosis and treatment of streptococcal throat infections in children with penicillin and through the continuous administration of antibiotics to patients with RHD or to individuals with a previous attack of ARF in order to prevent recurrent attacks of ARF and subsequent RHD. Another factor is the reduction of risk for streptococcal infection through improved hygiene and underlying socioeconomic factors, especially with respect to living conditions and overcrowding (Steer et al., 2002; WHO Study Group on Rheumatic Fever and Rheumatic Heart Disease and WHO, 2004).
Unfortunately, many low and middle income countries have not seen such a drastic decline, and some regions, such as Sub-Saharan Africa, have experienced no significant declines. This is most likely because many in developing regions have poor access to basic primary care and living conditions that do not promote reduction of risk of initial infection. In addition, many low and middle income countries rely almost exclusively on providing prophylactic antibiotics to those already diagnosed with RHD to control the disease rather than on other prevention efforts. (Karthikeyan and Mayosi, 2009). There remains a large unmet need for a widespread strategy using all levels of preventive efforts to prevent the onset of RHD.
Targeting strategies to help avoid and treat initial infections in children has the potential for a major impact on mortality, morbidity, and quality of life, especially given the difficulties of treating and managing RHD in its advanced stages of valvular disease and heart failure (Carapetis, 2007; Steer and Carapetis, 2009).
Chagas Heart Disease
Chagas heart disease is another form of CVD caused by an infectious agent. The disease is endemic throughout Central and South America but does not exist outside of the continent. In the 1980s, countrywide surveillance found the prevalence of Chagas to be approximately 17 million cases in 18 countries, with an incidence of 700,000 to 800,000 new infections and approximately 45,000 deaths each year (Morel and Lazdins, 2003). Between 10 and 30 percent of individuals infected with the Trypanosoma cruzi parasite that causes Chagas develop some form of cardiac damage, although this damage does not usually occur until 10 to 20 years after the acute phase of the disease. Chagas can lead to a variety of clinical symptoms including heart failure and death, with chagistic cardiomyopathy being the deadliest form of the disease (Marin-Neto et al., 2007; Moncayo and Yanine, 2006).
Since the 1980s, Central and South America have experienced significant declines in both incidence and prevalence of Chagas as a result of wide-scale prevention efforts, with the transmission of the disease successfully interrupted in Chile, Uruguay, and Brazil. These have primarily consisted of widespread spraying of insecticides to prevent the parasite’s insect hosts from entering homes and careful screening of the blood supply. The current estimated prevalence of Chagas is 13 million cases in 15 countries, with an annual incidence of 200,000 new infections and 21,000 annual deaths from Chagas heart disease (Moncayo and Yanine, 2006; Morel and Lazdins, 2003; WHO Expert Committee on the Control of Chagas Disease and WHO, 2002).
Infectious Pericarditis and Cardiomyopathies
Certain infections, most notably HIV and TB, can lead to pericarditis and cardiomyopathies. Autopsy studies indicate that tuberculosis pericarditis occurs in approximately 1 percent of TB cases and 1 to 2 percent of pulmonary TB cases. It is the most common cause of pericarditis in Africa and other regions with high TB prevalence. Because of the HIV/AIDS epidemic, incidence of TB pericarditis is increasing in Africa (Mayosi et al., 2005). HIV infection itself, especially in its later stages, has also been associated with inflammation of the endothelium, pericarditis, pericardial
effusion, myocarditis, cardiomyopathy, pulmonary hypertension, and a number of different types of vascular lesions (Aberg, 2009; Kamin and Grinspoon, 2005; Krishnaswamy et al., 2000). As the prevalence of TB, HIV, and TB/HIV co-infection continue to increase, it is likely that such TB- and HIV-related cardiovascular complications will also become more common (Mayosi et al., 2005). This poses major treatment and diagnostic challenges for the future especially as noninfectious causes increasingly occur in conjunction with infectious causes of heart disease.
Conclusion 2.4: Rheumatic heart disease, Chagas, and infectious pericarditis and cardiomyopathies continue to cause a substantial burden of disease and death in some low and middle income countries despite having been nearly eliminated in high income countries. Their ongoing prevalence in developing countries further widens the gap between the rich and poor, yet they are easily prevented through basic primary health care screenings or proven interventions. Additional surveillance is necessary to obtain a better epidemiological picture of these infectious forms of CVD in developing countries, and efforts to improve health care delivery are needed to facilitate the widespread delivery of existing interventions to prevent and treat these diseases.
CVD Risk and Other Chronic Infectious Diseases
The past 15 years have produced considerable research investigating the associations among HIV infection, antiretroviral therapy, and cardiovascular disease and between CVD risks and TB, and to a lesser extent, the similarities from a health systems perspective of HIV/AIDS, TB, and CVD. Here the focus lies on the first two aspects.
HIV/AIDS and CVD Risks and Diseases
Studies among middle-aged patients in developed countries have found that there is a high prevalence of CVD risk factors among the HIV-infected population, and both HIV infection and highly active antiretroviral treatment (HAART) are associated with an increased risk of CVD. This increased risk is mostly mediated through HIV and HAART’s effects on traditional CVD risk factors such as dyslipidemia and insulin resistance; however, there is also evidence that HIV infection and HAART themselves contribute an additional risk beyond what can be explained by other factors (Aberg, 2009; Boccara, 2008; Martinez et al., 2009).
By contrast, in Sub-Saharan Africa, where many HIV patients are younger, access to HAART is more limited, and tuberculosis is endemic, the predominant forms of heart disease associated with HIV/AIDS are peri-
carditis, cardiomyopathy, and pulmonary hypertension. Indeed, coronary artery disease, lipodystrophy, and metabolic syndrome are still not significant clinical problems among HIV patients in Sub-Saharan Africa (Ntsekhe and Mayosi, 2009).
CVD Prevalence Among HIV Patients While there are limited data on the prevalence of clinical CVD events among HIV patients worldwide, estimation can be extrapolated from the prevalence rates of CVD events from some of the major studies. The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study, one of the largest prospective studies of CVD risk among HIV-infected patients in 21 mostly high income countries in North America, Europe, and Australia, found that the incidence rate of a patient’s first cardio or cerebrovascular event was 5.7 per 1000 person-years. From this data set, the authors concluded that although HIV and HAART do increase the risk of CVD, the absolute prevalence is still quite low, although it should be noted that the cohort is relatively young (The Writing Committee, 2004).
Data are generally lacking on the prevalence and characteristics of CVD among the HIV-infected population in most developing regions, although there have been several reviews of CVD in HIV-infected populations in Africa. In Sub-Saharan Africa, studies have found that the prevalence of cardiac abnormalities among African with HIV (most commonly involving the pericardium or myocardium as discussed in the previous section) is up to 60 percent, although patients are often asymptomatic and the profile of these cardiac abnormalities can be quite different from developed countries, as described above (Ntsekhe and Mayosi, 2009).
HIV’s Direct Effects on CVD Risk Factors There is a growing body of evidence that HIV infection itself may result in metabolic and inflammatory events that increase cardiovascular risk. Uncontrolled HIV infection has been associated with lowered HDL cholesterol, increased triglyceride levels, and increased insulin resistance (Aberg, 2009; Boccara, 2008; Kamin and Grinspoon, 2005). Currently, data are lacking to quantify the exact magnitude of the increased CVD risk conferred by HIV disease itself.
HAART Effects on CVD HAART, especially those regimens containing protease inhibitors, has been the focus of extensive research regarding its effects on cardiovascular risk. Certain HAART regimens have been associated with dyslipidemia (increased LDL cholesterol, increased triglycerides, increased total cholesterol, and decreased HDL cholesterol), increased insulin resistance, body fat redistribution, and diabetes (Aberg, 2009; Boccara, 2008; Pao et al., 2008). These associations between HAART and CVD risk factors have also been demonstrated in HIV-infected children (Miller et al.,
2008). HAART regimens have also been associated with increased rates of myocardial infarction and other cardio- and cerebrovascular events, an association that appears to get stronger the longer a patient is on HAART (Law et al., 2006).
It is important to note that while the increase in risk of CVD caused by HIV and HAART is significant, the absolute risk of having a CVD event remains low, and there is universal agreement that the life-saving benefits of HAART outweigh the added CVD risks (Aberg, 2009; Adeyemi, 2007; Friis-Moller et al., 2007). In addition, a large prospective study found that intermittent use of HAART (stopping treatment once patients had stabilized CD4+ cell counts and then restarting when cell counts dropped below threshold) resulted in significantly poorer CVD outcomes (Strategies for Management of Antiretroviral Therapy Study Group et al., 2006).
HIV and Tobacco Smoking One of the consistent findings in many of the studies on the link between CVD and HIV is the high prevalence of tobacco smoking among HIV-infected individuals, which is often significantly higher than that of the general population (De Socio et al., 2008; Furber et al., 2007; Gritz et al., 2007). In the D:A:D study, more than 50 percent of the HIV-infected participants were smokers (Friis-Moller et al., 2003), and other studies have recorded that up to two-thirds of their HIV-positive participants smoked (Burkhalter et al., 2005). One study suggested that tobacco smoking could be an independent risk factor for acquiring HIV infection, although a causal relationship has not been established (Furber et al., 2007).
These high rates of smoking are worrisome because in addition to being a significant contributor to cardiovascular risk, there is evidence that smoking is also associated with poorer outcomes in HIV. In HIV-infected patients, smoking has been associated with an increased risk of tuberculosis and other opportunistic infections (Arcavi and Benowitz, 2004; Burkhalter et al., 2005; Furber et al., 2007), a lower adherence to HAART (Shuter and Bernstein, 2008), and a reduction in the efficacy of HAART (Miguez-Burbano et al., 2003).
CVD Risk Factors and TB
Recently WHO reviewed the relationship between major risk factors for CVD and TB. They concluded that both tobacco use and diabetes were important TB risk factors in the 22 high-burden TB countries in the world (Dye et al., 2009). The evidence is strongest for the links between smoking tobacco and tuberculosis. Taken together, there is sufficient evidence to conclude a causal link between tobacco use and TB (Chiang et al., 2007; Lin et al., 2007; Slama et al., 2007). In various studies, tobacco use has
been associated with significantly increased risk of TB infection, increased conversion from latent to active TB, poorer treatment outcomes (Bates et al., 2007; Dhamgaye, 2008), increased mortality (Gajalakshmi et al., 2003; Hassmiller, 2006; Lin et al., 2007; Slama et al., 2007), increased drug resistance (Chiang et al., 2007), and increased rate of relapse (d’Arc Lyra Batista et al., 2008). One large study in India found that the mortality rate from TB was four times greater for ever smokers than for never smokers (Gajalakshmi et al., 2003a). There is a strong dose-response association between both the quantity of tobacco smoked and duration of smoking and risk of TB infection, disease, and mortality (Chiang et al., 2007; Dhamgaye, 2008; Slama et al., 2007). Unfortunately, smoking cessation is not actively supported in most TB treatment settings (Schneidera and Novotnya, 2007).
These associations have been found to be consistent across populations (both developing and industrialized), geographical regions, socioeconomic statuses, and cultures. Furthermore, studies have found these associations to be independent of confounding factors often associated with smoking such as alcohol use (Chiang et al., 2007; Hassmiller, 2006; Slama et al., 2007). Because smoking is generally more prevalent in men than in women, the majority of studies have focused on risk to male smokers. Indeed, Watkins and Plant (2006) proposed that smoking might explain some of the sex difference in the global TB epidemic, although this was based on an ecological study and needs to be assessed with individual-level data.
Recent major reviews of the relationship between diabetes and TB (Jeon and Murray, 2008; Young et al., 2009a, 2009b) suggest that there is a bidirectional relationship between the diseases. Diabetes is associated with a three-fold increased risk of TB, and TB contributes to the risk of developing diabetes (Young, 2009a). This relationship becomes critical to understand in countries where the burden of TB infection is already high (as in South Africa, India, China, and other developing countries) and where overweight and obesity are drivers of increased prevalence of diabetes.
In sum, TB and HIV/AIDS are common in many countries where CVD incidence is increasing. Furthermore, they share common risk factors, which suggests opportunities for integrated approaches to prevention and disease management at the health service and broader policy levels. As the HIV and TB epidemics continue to spread and more people get placed on long-term treatment, these opportunities for integrated approaches will likely increase.
CONCLUSION
Large parts of the world today are at moderate or high levels of risk for CVD, and cumulative behavioral, biological, and social risks will increase
the global impact of chronic diseases in the future. CVDs (mainly IHD and stroke) are, and will remain for decades, the major causes of death in the world. This chapter has presented evidence on the determinants of CVD, establishing a rationale for intervention approaches that will be discussed later in this report.
The breadth of determinants that contribute to CVD points to the need for lifelong and multisectoral approaches. Because unhealthful diet, tobacco use, and decreased physical activity levels are among the major drivers of the CVD epidemic, prevention through promoting healthful diet and lifestyle should remain one of the cornerstones of global CVD reduction efforts. This does not exclude the importance of the potential to reduce CVD burden through better health care delivery, including better integration and development of chronic disease care models. Together, these approaches have the potential to address the burden of disease and overlapping determinants that are common in most emerging economies.
Prevention efforts need to start early in life and continue through the life course. A new and far greater emphasis on early childhood development is warranted, including greater attention to chronic disease risk in maternal and child health programs. However, trends in major risks will continue to influence incidence for many decades even if childhood prevention is rapidly implemented. Therefore, concerted and combined primary and secondary prevention efforts are also needed to reduce death rates in middle age and beyond.
Finally, although the epidemiological data described in this chapter provide a clear rationale for the proximal risk factors and broader determinants that need to be targeted in prevention efforts as well as compelling evidence that if these factors can be reduced, the burden of CVD will decrease. However, the epidemiological data does not detail how specifically to design and implement programs that will effectively achieve these goals, nor does it provide sufficient guidance on how to tailor such interventions to work in disparate settings with different cultural, structural, and epidemiological backdrops. The complex, interrelated determinants of global CVD and the variation in both risk profiles and capacity among low and middle income countries means that prevention efforts will only be effective if they are adapted to account for the specific needs of the settings in which they will be applied. To achieve this, additional surveillance and implementation research in all global regions, but especially in low and middle income countries, is required. These important issues are the subject of the remaining chapters of this report.
REFERENCES
Aberg, J. A. 2009. Cardiovascular complications in HIV management: Past, present, and future. Journal of Acquired Immune Deficiency Syndromes 50(1):54-64.
Aboderin, I., A. Kalache, Y. Ben-Shlomo, J. W. Lynch, C. S. Yajnik, D. Kuh, and D. Yach. 2002. Life course perspectives on coronary heart disease, stroke and diabetes: Key issues and implications for policy and research. Geneva: World Health Organization.
Adeyemi, O. 2007. Cardiovascular risk and risk management in HIV-infected patients. Topics in HIV Medicine 15(5):159-162.
Adeyi, O., O. Smith, and S. Robles. 2007. Public policy and the challenge of chronic noncommunicable diseases. Washington, DC: The World Bank.
Al-Hamdan, N., A. Kutbi, A. J. Choudhry, R. Nooh, M. Shoukri, and S. Mujib. 2005. WHO stepwise approach to NCD surveillance country-specific standard report Saudi Arabia. Geneva: World Health Organization.
Alikhani, S., A. Delavari, F. Alaedini, R. Kelishadi, S. Rohbani, and A. Safaei. 2009. A province-based surveillance system for the risk factors of non-communicable diseases: A prototype for integration of risk factor surveillance into primary healthcare systems of developing countries. Public Health 123(5):358-364.
Allen, J., and S. Szanton. 2005. Gender, ethnicity, and cardiovascular disease. Journal of Cardiovascular Nursing 20(1):1-6; quiz 7-8.
Anand, S. S., E. A. Enas, J. Pogue, S. Haffner, T. Pearson, and S. Yusuf. 1998. Elevated lipoprotein(a) levels in South Asians in North America. Metabolism 47(2):182-184.
Anand, S. S., S. Yusuf, V. Vuksan, S. Devanesen, K. K. Teo, P. A. Montague, L. Kelemen, C. Yi, E. Lonn, H. Gerstein, R. A. Hegele, and M. McQueen. 2000. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: The Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet 356(9226):279-284.
Anand, S. S., S. Islam, A. Rosengren, M. G. Franzosi, K. Steyn, A. H. Yusufali, M. Keltai, R. Diaz, S. Rangarajan, and S. Yusuf. 2008. Risk factors for myocardial infarction in women and men: Insights from the INTERHEART study. European Heart Journal 29(7):932-940.
Appelros, P., B. Stegmayr, and A. Terent. 2009. Sex differences in stroke epidemiology: A systematic review. Stroke 40(4):1082-1090.
Arcavi, L. M. D., and N. L. M. D. Benowitz. 2004. Cigarette smoking and infection. Archives of Internal Medicine 164(20):2206-2216.
Arking, D. E., and A. Chakravarti. 2009. Understanding cardiovascular disease through the lens of genome-wide association studies. Trends in Genetics 25(9):387-394.
Arnett, D. K., A. E. Baird, R. A. Barkley, C. T. Basson, E. Boerwinkle, S. K. Ganesh, D. M. Herrington, Y. Hong, C. Jaquish, D. A. McDermott, and C. J. O’Donnell. 2007. Relevance of genetics and genomics for prevention and treatment of cardiovascular disease: A scientific statement from the American Heart Association Council on Epidemiology and Prevention, the Stroke Council, and the Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation 115(22):2878-2901.
Asia Pacific Cohort Studies Collaboration. 2003. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia Pacific region. Diabetes Care 26(2): 360-366.
Asia Pacific Cohort Studies Collaboration. 2004. Blood glucose and risk of cardiovascular disease in the Asia Pacific region. Diabetes Care 27(12):2836-2842.
Asia Pacific Cohort Studies Collaboration. 2007. Cholesterol, diabetes and major cardiovascular diseases in the Asia-Pacific region. Diabetologia 50(11):2289-2297.
Barker, D. J., C. N. Martyn, C. Osmond, C. N. Hales, and C. H. Fall. 1993. Growth in utero and serum cholesterol concentrations in adult life. British Medical Journal 307(6918):1524-1527.
Barker, D. J. P., C. Osmond, T. J. Forsen, E. Kajantie, and J. G. Eriksson. 2005. Trajectories of growth among children who have coronary events as adults.[see comment]. New England Journal of Medicine 353(17):1802-1809.
Barnighausen, T., T. Welz, V. Hosegood, J. Batzing-Feigenbaum, F. Tanser, K. Herbst, C. Hill, and M. L. Newell. 2008. Hiding in the shadows of the HIV epidemic: Obesity and hypertension in a rural population with very high HIV prevalence in South Africa. Journal of Human Hypertension 22(3):236-239.
Barquera, S., L. Hernandez-Barrera, M. L. Tolentino, J. Espinosa, W. N. Shu, J. A. Rivera, and B. M. Popkin. 2008. Energy intake from beverages is increasing among Mexican adolescents and adults. Journal of Nutrition 138(12):2454-2461.
Bates, M. N., A. Khalakdina, M. Pai, L. Chang, F. Lessa, and K. R. Smith. 2007. Risk of tuberculosis from exposure to tobacco smoke: A systematic review and meta-analysis. Archives of Internal Medicine 167(4):335-342.
Beaglehole, R. 1999. International trends in coronary heart disease mortality and incidence rates. Journal of Cardiovascular Risk 6(2):63-68.
Beaglehole, R., and R. Bonita. 2008. Global public health: A scorecard. Lancet 372(9654): 1988-1996.
Beilin, L. J., and I. B. Puddey. 2006. Alcohol and hypertension: An update. Hypertension 47(6):1035-1038.
Bhardwaj, S., A. Misra, L. Khurana, S. Gulati, P. Shah, and N. K. Vikram. 2008. Childhood obesity in Asian Indians: A burgeoning cause of insulin resistance, diabetes and subclinical inflammation. Asia Pacific Journal of Clinical Nutrition 17(Suppl 1):172-175.
Blauwet, L. A., and R. F. Redberg. 2007. The role of sex-specific results reporting in cardiovascular disease. Cardiology in Review 15(6):275-278.
Boccara, F. 2008. Cardiovascular complications and atherosclerotic manifestations in the HIV-infected population: Type, incidence and associated risk factors. AIDS 22 (Suppl 3):S19-S26.
Booth, G. L., M. K. Kapral, K. Fung, and J. V. Tu. 2006a. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care 29(1):32-37.
Booth, G. L., M. K. Kapral, K. Fung, and J. V. Tu. 2006b. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: A population-based retrospective cohort study. Lancet 368(9529):29-36.
Bosire, C., J. Reedy, and S. M. Krebs-Smith. 2009. Sources of energy and selected nutrient intakes among the US population, 2005-06: A report prepared for the 2010 dietary guidelines advisory committee. Bethesda, MD: National Cancer Institute.
Brands, A., and D. Yach. 2002. Women and the rapid rise of noncommunicable diseases. World Health Organization NMH Reader (1):1-22.
Brook, R. D. 2008. Cardiovascular effects of air pollution. Clinical Science 115(5-6): 175-187.
Brook, R. D., B. Franklin, W. Cascio, Y. Hong, G. Howard, M. Lipsett, R. Luepker, M. Mittleman, J. Samet, S. C. Smith Jr., and I. Tager. 2004. Air pollution and cardiovascular disease: A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation 109(21):2655-2671.
Buchanan, M. R., and S. J. Brister. 2001. Sex-related differences in the pathophysiology of cardiovascular disease: Is there a rationale for sex-related treatments? Canadian Journal of Cardiology 17(Suppl D):7D-13D.
Bump, J. B., M. R. Reich, O. Adeyi, and S. Khetrapal. 2009. Towards a political economy of tobacco control in low- and middle-income countries. Washington, DC: The World Bank.
Burg, M. M., and D. Abrams. 2001. Depression in chronic medical illness: The case of coronary heart disease. Journal of Clinical Psychology 57(11):1323-1337.
Burkhalter, J. E., C. M. Springer, R. Chhabra, J. S. Ostroff, and B. D. Rapkin. 2005. Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine & Tobacco Research 7(4):511-522.
Caballero, B. 2005. A nutrition paradox—underweight and obesity in developing countries. New England Journal of Medicine 352(15):1514-1516.
Caballero, B. 2009. Early undernutrition and risk of CVD in the adult. Presentation at Public Information Gathering Session for the Institute of Medicine Committee on Preventing the Global Epidemic of Cardiovascular Disease, Washington, DC.
Capewell, S., C. E. Morrison, and J. J. McMurray. 1999. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 81(4):380-386.
Capewell, S., R. Beaglehole, M. Seddon, and J. McMurray. 2000. Explanation for the decline in coronary heart disease mortality rates in Auckland, New Zealand, between 1982 and 1993. Circulation 102(13):1511-1516.
Carapetis, J. R. 2007. Rheumatic heart disease in developing countries. New England Journal of Medicine 357(5):439-441.
Carapetis, J. R., A. C. Steer, E. K. Mulholland, and M. Weber. 2005. The global burden of group a streptococcal diseases. Lancet Infectious Diseases 5(11):685-694.
Celermajer, D. S., and J. G. Ayer. 2006. Childhood risk factors for adult cardiovascular disease and primary prevention in childhood. Heart 92(11):1701-1706.
Chan, J. C., V. Malik, W. Jia, T. Kadowaki, C. S. Yajnik, K. H. Yoon, F. B. Hu. 2009. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. Journal of the American Medical Association 301(20):2129-2140.
Chatterjee, S., R. Allan, and R. Ranjan. 2007. Discussion paper no. 07.05: Food consumption and calorie intake in contemorary India. Palmerston North, New Zealand: Massey University Department of Applied and International Economics.
Chelala, C. 1998. Tobacco corporations step up invasion of developing countries. Lancet 351(9106):889.
Chiang, C. Y., K. Slama, and D. A. Enarson. 2007. Associations between tobacco and tuberculosis. International Journal of Tuberculosis and Lung Disease 11(3):258-262; Erratum. 11(8):936.
Chiuve, S. E., K. M. Rexrode, D. Spiegelman, G. Logroscino, J. E. Manson, E. B. Rimm. 2008. Primary prevention of stroke by healthy lifestyle. Circulation 118(9):947-954.
Chobanian, A. V. 2009. Shattuck lecture. The hypertension paradox—more uncontrolled disease despite improved therapy. New England Journal of Medicine 361(9):878-887.
Christensen, K., G. Doblhammer, R. Rau, and J. W. Vaupel. 2009. Ageing populations: The challenges ahead. Lancet 374(9696):1196-1208.
Clarke, R., J. Emberson, A. Fletcher, E. Breeze, M. Marmot, M. J. Shipley. 2009. Life expectancy in relation to cardiovascular risk factors: 38 year follow-up of 19,000 men in the Whitehall study. British Medical Journal 339:b3513.
Collins, R., J. Armitage, S. Parish, P. Sleight, and R. Peto. 2004. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet 363(9411):757-767.
Connolly, G. N. 1992. Worldwide expansion of transnational tobacco industry. Journal of the National Cancer Institute Monographs (12):29-35.
Critchley, J. A., and S. Capewell. 2003. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: A systematic review. Journal of the American Medical Association 2003 290:1.
Critchley, J., J. Liu, D. Zhao, W. Wei, and S. Capewell. 2004. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation 110(10):1236-1244.
d’Arc Lyra Batista, J., M. de Fatima Pessoa Militao de Albuquerque, R. A. de Alencar Ximenes, and L. C. Rodrigues. 2008. Smoking increases the risk of relapse after successful tuberculosis treatment. International Journal of Epidemiology 37(4):841-851.
Danaei, G., C. M. Lawes, S. Vander Hoorn, C. J. Murray, and M. Ezzati. 2006. Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: Comparative risk assessment. Lancet 368(9548):1651-1659.
Dangour, A. D., and R. Uauy. 2006. Nutrition challenges for the twenty-first century. British Journal of Nutrition 96 (Suppl 1)S5-S7.
Davey Smith, G., P. McCarron, M. Okasha, and J. McEwen. 2001. Social circumstances in childhood and cardiovascular disease mortality: Prospective observational study of Glasgow University students. Journal of Epidemiology and Community Health 55(5): 340-341.
Davies, A. R., L. Smeeth, and E. M. Grundy. 2007. Contribution of changes in incidence and mortality to trends in the prevalence of coronary heart disease in the UK: 1996-2005. European Heart Journal 28(17):2142-2147.
Dawber, T. R., and W. B. Kannel. 1958. An epidemiologic study of heart disease: The Framingham Study. Nutrition Reviews 16(1):1-4.
Dawber, T. R., G. F. Meadors, and F. E. Moore, Jr. 1951. Epidemiological approaches to heart disease: The Framingham Study. American Journal of Public Health and the Nations Health 41(3):279-281.
Dawber, T. R., F. E. Moore, and G. V. Mann. 1957. Coronary heart disease in the Framingham Study. American Journal of Public Health and the Nations Health 47(4 Pt 2):4-24.
De Socio, G. V. L., G. Parruti, T. Quirino, E. Ricci, G. Schillaci, B. Adriani, P. Marconi, M. Franzetti, C. Martinelli, F. Vichi, G. Penco, C. Sfara, G. Madeddu, and P. Bonfanti. 2008. Identifying HIV patients with an unfavorable cardiovascular risk profile in the clinical practice: Results from the Simone study. Journal of Infection 57(1):33-40.
Dhamgaye, T. M. 2008. Tobacco smoking and pulmonary tuberculosis: A case-control study. Journal of the Indian Medical Association 106(4):216-219.
Dominici, F., R. D. Peng, M. L. Bell, L. Pham, A. McDermott, S. L. Zeger, and J. M. Samet. 2006. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. Journal of the American Medical Association 295(10):1127-1134.
Dong, M., W. H. Giles, V. J. Felitti, S. R. Dube, J. E. Williams, D. P. Chapman, and R. F. Anda. 2004. Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation 110(13):1761-1766.
Downs, J. R., M. Clearfield, S. Weis, E. Whitney, D. R. Shapiro, P. A. Beere, A. Langendorfer, E. A. Stein, W. Kruyer, and A. M. Gotto, Jr. 1998. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: Results of AFCAPS/TEXCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. Journal of the American Medical Association 279(20):1615-1622.
Dye, C., K. Lönnroth, E. Jaramillo, B. G. Williams, and M. Raviglione. 2009. Trends in tuberculosis incidence and their determinants in 134 countries. In Bulletin of the World Health Organization. Geneva: World Health Organization.
Ellis, L. B. 1948. Underlying causes of heart disease. The American Journal of Nursing 48(11):697-698.
ERC. 2007. World cigarettes 1: The 2007 report. Suffolk, England: ERC Statistics Intl Plc.
Erqou, S., S. Kaptoge, P. L. Perry, E. Di Angelantonio, A. Thompson, I. R. White, S. M. Marcovina, R. Collins, S. G. Thompson, J. Danesh. 2009. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. Journal of the American Medical Association 302(4):412-423.
Evans, R. W., C. H. Bunker, F. A. Ukoli, and L. H. Kuller. 1997. Lipoprotein (a) distribution in a Nigerian population. Ethnicity Health 2(1-2):47-58.
Everson-Rose, S. A., and T. T. Lewis. 2005. Psychosocial factors and cardiovascular diseases. In Annual Review of Public Health 26(1):469-500
Ezzati, M., S. J. Henley, M. J. Thun, and A. D. Lopez. 2005. Role of smoking in global and regional cardiovascular mortality. Circulation 112(4):489-497.
Fernald, L. C., and L. M. Neufeld. 2007. Overweight with concurrent stunting in very young children from rural Mexico: Prevalence and associated factors. European Journal of Clinical Nutrition 61(5):623-632.
Figueredo, V. M. 2009. The time has come for physicians to take notice: The impact of psychosocial stressors on the heart. American Journal of Medicine 122(8):704-712.
Flegal, K. M., B. I. Graubard, D. F. Williamson, M. H. Gail, K. M. Flegal, B. I. Graubard, D. F. Williamson, and M. H. Gail. 2007. Cause-specific excess deaths associated with underweight, overweight, and obesity. Journal of the American Medical Association 298(17):2028-2037.
Ford, E. S., U. A. Ajani, J. B. Croft, J. A. Critchley, D. R. Labarthe, T. E. Kottke, W. H. Giles, and S. Capewell. 2007. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. New England Journal of Medicine 356(23):2388-2398.
Foster, R. K., and H. E. Marriott. 2006. Alcohol consumption in the new millennium—weighing up the risks and benefits for our health. Nutrition Bulletin 31(4):286-331.
Fox, C. S., J. C. Evans, M. G. Larson, W. B. Kannel, and D. Levy. 2004. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: The Framingham Heart Study. Circulation 110(5):522-527.
Frasure-Smith, N., and F. Lesperance. 2006. Recent evidence linking coronary heart disease and depression. Canadian Journal of Psychiatry—Revue Canadienne de Psychiatrie 51(12):730-737.
Freedman, D. S., L. K. Khan, W. H. Dietz, S. R. Srinivasan, and G. S. Berenson. 2001. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics 108(3):712-718.
Fries, J. F. 1980. Aging, natural death, and the compression of morbidity. New England Journal of Medicine 303(3):130-135.
Friis-Moller, N., R. Weber, P. Reiss, R. Thiébaut, O. Kirk, A. D’Arminio Monforte, C. Pradier, L. Morfeldt, S. Mateu, M. Law, W. El-Sadr, S. De Wit, C. A. Sabin, A. N. Phillips, and J. D. Lundgren. 2003. Cardiovascular disease risk factors in HIV patients—association with antiretroviral therapy. Results from the DAD study. AIDS 17(8):1179-1193.
Friis-Moller, N., P. Reiss, C. A. Sabin, R. Weber, A. d’Arminio Monforte, W. El-Sadr, R. Thiebaut, S. De Wit, O. Kirk, E. Fontas, M. G. Law, A. Phillips, and J. D. Lundgren. 2007. Class of antiretroviral drugs and the risk of myocardial infarction. New England Journal of Medicine 356(17):1723-1735.
Fung, T. T., K. M. Rexrode, C. S. Mantzoros, J. E. Manson, W. C. Willett, and F. B. Hu. 2009. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation 119(8):1093-1100.
Furber, A. S., R. Maheswaran, J. N. Newell, and C. Carroll. 2007. Is smoking tobacco an independent risk factor for HIV infection and progression to AIDS? A systemic review. Sexually Transmitted Infections 83(1):41-46.
Gager, L. T. 1931. Heart disease: Its nature, study, and prevention. American Journal of Nursing 31(4):397-406.
Gajalakshmi, V., R. Peto, T. S. Kanaka, and P. Jha. 2003a. Smoking and mortality from tuberculosis and other diseases in India: Retrospective study of 43 000 adult male deaths and 35 000 controls. Lancet 362(9383):507-515.
Galobardes, B., G. D. Smith, and J. W. Lynch. 2006. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of Epidemiology 16(2):91-104.
Gaziano, T., and G. I. Kim. 2009. Cost of treating non-optimal blood pressure in select low and middle income countries in comparison to the United States. Background paper commissioned by the Committee on Preventing the Global Epidemic of Cardiovascular Disease.
Gaziano, T. A., K. S. Reddy, F. Paccaud, S. Horton, and V. Chaturvedi. 2006. Cardiovascular disease. In Disease control priorities in developing countries. 2nd ed, Edited by D. T. Jamison, J. G. Breman, A. R. Measham, G. Alleyne, M. Claeson, D. B. Evans, P. Jha, A. Mills and P. Musgrove. New York: Oxford University Press. Pp. 645-662.
Glassman, A., P. A. Shapiro, D. E. Ford, L. Culpepper, M. S. Finkel, J. R. Swenson, J. T. Bigger, B. L. Rollman, and T. N. Wise. 2003. Cardiovascular health and depression. Journal of Psychiatric Practice 9(6):409-421.
Gluckman, P. D., and M. A. Hanson. 2008. Developmental and epigenetic pathways to obesity: An evolutionary-developmental perspective. International Journal of Obesity 32(Suppl 7):S62-S71.
Gluckman, P. D., M. A. Hanson, T. Buklijas, F. M. Low, and A. S. Beedle. 2009. Epigenetic mechanisms that underpin metabolic and cardiovascular diseases. Nature Reviews Endocrinology 5(7):401-408.
Goldman, D. P., Y. Zheng, F. Girosi, P.-C. Michaud, S. J. Olshansky, D. Cutler, and J. W. Rowe. 2009. The benefits of risk factor prevention in Americans aged 51 years and older. American Journal of Public Health 99(11):2096-2101.
Goraya, T. Y., S. J. Jacobsen, T. E. Kottke, R. L. Frye, S. A. Weston, and V. L. Roger. 2003. Coronary heart disease death and sudden cardiac death: A 20-year population-based study. American Journal of Epidemiology 157(9):763-770.
Gotto, A. M., Jr. 2005. Evolving concepts of dyslipidemia, atherosclerosis, and cardiovascular disease: The Louis F. Bishop lecture. Journal of the American College of Cardiology 46(7):1219-1224.
Goudge, J., L. Gilson, S. Russell, T. Gumede, and A. Mills. 2009. Affordability, availability and acceptability barriers to health care for the chronically ill: Longitudinal case studies from South Africa. Biomed Central Health Services Research 9:75.
Gouveia, N., C. U. De Freitas, L. C. Martins, and I. O. Marcilio. 2006. Respiratory and cardiovascular hospitalizations associated with air pollution in the city of Sao Paulo, Brazil. Hospitalizacoes por causas respiratorias e cardiovasculares associadas a contaminacao atmosferica no Municipio de Sao Paulo, Brasil. Cadernos de Saúde Pública 22(12):2669-2677.
Goyal, A., and S. Yusuf. 2006. The burden of cardiovascular disease in the Indian subcontinent. Indian Journal of Medical Research 124(3):235-244.
Gritz, E. R., D. J. Vidrine, and M. Cororve Fingeret. 2007. Smoking cessation. A critical component of medical management in chronic disease populations. American Journal of Preventive Medicine 33(6 Suppl):S414-S422.
Gu, D., K. Reynolds, X. Wu, J. Chen, X. Duan, P. Muntner, G. Huang, R. F. Reynolds, S. Su, P. K. Whelton, J. He, and InterAsia Collaborative Group. The International Collaborative Study of Cardiovascular Disease in Asia. 2002. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension 40(6):920-927.
Guindon, E. G., and D. Boisclair. 2003. Current and future trends in tobacco use. Geneva: World Health Organization Tobacco Free Initiative.
Guthold, R., T. Ono, K. L. Strong, S. Chatterji, and A. Morabia. 2008. Worldwide variability in physical inactivity—a 51-country survey. American Journal of Preventive Medicine 34(6):486-494.
Haffner, S. M., S. Lehto, T. Ronnemaa, K. Pyorala, and M. Laakso. 1998. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. New England Journal of Medicine 339(4): 229-234.
Hardoon, S. L., P. H. Whincup, L. T. Lennon, S. G. Wannamethee, S. Capewell, and R. W. Morris. 2008. How much of the recent decline in the incidence of myocardial infarction in British men can be explained by changes in cardiovascular risk factors? Evidence from a prospective population-based study. Circulation 117(5):598-604.
Harries, A. D., A. Jahn, R. Zachariah, and D. Enarson. 2008. Adapting the DOTS framework for tuberculosis control to the management of non-communicable diseases in Sub-Saharan Africa. PLoS Med 5(6):e124.
Hassmiller, K. M. 2006. The association between smoking and tuberculosis. Salud Publica de Mexico 48(Suppl 1):S201-S216.
He, F. J., and G. A. MacGregor. 2009. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. Journal of Human Hypertension 23(6):363-384.
He, J., D. Gu, J. Chen, X. Wu, T. N. Kelly, J.-F. Huang, J.-C. Chen, C.-S. Chen, L. A. Bazzano, K. Reynolds, P. K. Whelton, and M. J. Klag. 2009. Premature deaths attributable to blood pressure in China: A prospective cohort study. Lancet 374(9703):1765-1772.
Heart disease likely fate of young men in big cities. 1937. The Science News-Letter 32(847): 10-11.
HEM Project Team. 2008. Closing the health gap in the European union. Warsaw, Poland: Maria Skłodowska-Curie Cancer Memorial Cancer Center and Institute of Oncology, Epidemiology and Prevention Division.
Henderson, L., J. Gregory, K. Irving, and G. Swan. 2003. National diet & nutrition survey: Adults aged 19 to 64: Energy, protein, carbohydrate, fat, and alcohol intake. London: Office of National Statistics.
Holman, R. R., S. K. Paul, M. A. Bethel, D. R. Matthews, and H. A. Neil. 2008. 10-year follow-up of intensive glucose control in type 2 diabetes. New England Journal of Medicine 359(15):1577-1589.
Holzman, D. 1997. Tobacco abroad: Infiltrating foreign markets. Environmental Health Perspectives 105(2):178-183.
Hu, F. B. 2008. Globalization of food patterns and cardiovascular disease risk. Circulation 118(19):1913-1914.
Hu, F. B., M. J. Stampfer, J. E. Manson, F. Grodstein, G. A. Colditz, F. E. Speizer, and W. C. Willett. 2000. Trends in the incidence of coronary heart disease and changes in diet and lifestyle in women. New England Journal of Medicine 343(8):530-537.
Hu, F. B., J. E. Manson, M. J. Stampfer, G. Colditz, S. Liu, C. G. Solomon, and W. C. Willett. 2001. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. New England Journal of Medicine 345(11):790-797.
Hunink, M. G., L. Goldman, A. N. Tosteson, M. A. Mittleman, P. A. Goldman, L. W. Williams, J. Tsevat, and M. C. Weinstein. 1997. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. Journal of the American Medical Association 277(7):535-542.
Huxley, R., F. Barzi, and M. Woodward. 2006. Excess risk of fatal coronary heart disease associated with diabetes in men and women: Meta-analysis of 37 prospective cohort studies. British Medical Journal 332(7533):73-78.
IDF (International Diabetes Federation). 2006. The diabetes atlas. Brussels: IDF.
IDF. 2010. The diabetes atlas. Brussels: IDF.
IOM (Institute of Medicine). 1998. Control of cardiovascular diseases in developing countries. Washington, DC: National Academy Press.
IOM. 2004. Research priorities for airborne particulate matter: IV. Continuing research progress. Washington, DC: The National Academies Press.
IOM. 2009. Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. Washington, DC: The National Academies Press.
Iqbal, R., S. Anand, S. Ounpuu, S. Islam, X. Zhang, S. Rangarajan, J. Chifamba, A. Al-Hinai, M. Keltai, and S. Yusuf. 2008. Dietary patterns and the risk of acute myocardial infarction in 52 countries: Results of the INTERHEART study. Circulation 118(19):1929-1937.
Jackson, G. 2008. Gender differences in cardiovascular disease prevention. Menopause International 14(1):13-17.
Jamieson, D. G., and M. Skliut. 2009. Gender considerations in stroke management. Neurologist 15(3):132-141.
Jensen, L. A., and D. K. Moser. 2008. Gender differences in knowledge, attitudes, and beliefs about heart disease. Nursing Clinics of North America 43(1):77-104; vi-vii.
Jeon, C. Y., and M. B. Murray. 2008. Diabetes mellitus increases the risk of active tuberculosis: A systematic review of 13 observational studies. PLoS Med 5(7):e152.
Jequier, E. 1999. Alcohol intake and body weight: A paradox. American Journal of Clinical Nutrition 69(2):173-174.
Jha, P., and F. J. Chaloupka. 1999. Curbing the epidemic: Governments and the economics of tobacco control. Washington, DC: World Bank.
Johnson, R. K., L. J. Appel, M. Brands, B. V. Howard, M. Lefevre, R. H. Lustig, F. Sacks, L. M. Steffen, J. Wylie-Rosett, P. A. American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity, and Metabolism, and the the Council on Epidemiology and Prevention. 2009. Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation 120(11):1011-1020.
Joint WHO/FAO Expert Consultation on Diet Nutrition and the Prevention of Chronic Diseases and World Health Organization Department of Nutrition for Health and Development. 2003. Diet, nutrition and the prevention of chronic diseases: Report of a joint WHO/FAO expert consultation, Geneva, 28 January-1 February 2002, WHO technical report series. Geneva: World Health Organization.
Kalache, A. 1999. Active ageing makes the difference: Editorial. Bulletin of the World Health Organization 77(4):299.
Kalache, A., I. Aboderin, and I. Hoskins. 2002. Compression of morbidity and active ageing: Key priorities for public health policy in the 21st century: Public health classics. Bulletin of the World Health Organization 80(3):243-244.
Kamin, D. S., and S. K. Grinspoon. 2005. Cardiovascular disease in HIV-positive patients. AIDS 19(7):641-652.
Kannel, W. B., T. R. Dawber, A. Kagan, N. Revotskie, and J. Stokes, 3rd. 1961. Factors of risk in the development of coronary heart disease—six year follow-up experience. The Framingham Study. Annals of Internal Medicine 55:33-50.
Kannel, W. B., W. P. Castelli, T. Gordon, and P. M. McNamara. 1971. Serum cholesterol, lipoproteins, and the risk of coronary heart disease. The Framingham Study. Annals of Internal Medicine 74(1):1-12.
Karppanen, H., and E. Mervaala. 2006. Sodium intake and hypertension. Progress in Cardiovascular Diseases 49(2):59-75.
Karthikeyan, G., and B. M. Mayosi. 2009. Is primary prevention of rheumatic fever the missing link in the control of rheumatic heart disease in Africa? Circulation 120(8):709-713.
Kelishadi, R. 2007. Childhood overweight, obesity, and the metabolic syndrome in developing countries. Epidemiologic Reviews 29:62-76.
Kelly, T. N., L. A. Bazzano, V. A. Fonseca, T. K. Thethi, K. Reynolds, and J. He. 2009. Glucose control and cardiovascular disease in type 2 diabetes. Annals of Internal Medicine 151(6):1-10.
Kengne, A. P., A. Patel, F. Barzi, K. Jamrozik, T. H. Lam, H. Ueshima, D. F. Gu, I. Suh, and M. Woodward. 2007. Systolic blood pressure, diabetes and the risk of cardiovascular diseases in the Asia-Pacific region. Journal of Hypertension 25(6):1205-1213.
Kengne, A. P., K. Nakamura, F. Barzi, T. H. Lam, R. Huxley, D. Gu, A. Patel, H. C. Kim, and M. Woodward. 2009. Smoking, diabetes and cardiovascular diseases in men in the Asia Pacific region. Journal of Diabetes 1(3):173-181.
Khan, M., and G. Mensah. 2009. Changing practices to improve dietary outcomes and reduce cardiovascular risk: A food company’s perspective. Purchase, NY: Background Paper Commissioned by the Committee.
Kotseva, K., D. Wood, G. De Backer, D. De Bacquer, K. Pyorala, and U. Keil. 2009a. Cardiovascular prevention guidelines in daily practice: A comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 373(9667):929-940.
Kotseva, K., D. Wood, G. De Backer, D. De Bacquer, K. Pyorala, U. Keil, and EUROASPIRE Study Group. 2009b. EUROASPIRE iii: A survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. European Journal of Cardiovascular Prevention & Rehabilitation 16(2):121-137.
Krishnaswamy, G. M., D. S. P. Chi, J. I. M. L. P. Kelley, F. M. Sarubbi, K. J. M. Smith, and A. M. Peiris. 2000. The cardiovascular and metabolic complications of HIV infection. Cardiology in Review 8(5):260-268.
Laatikainen, T., J. Critchley, E. Vartiainen, V. Salomaa, M. Ketonen, and S. Capewell. 2005. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. American Journal of Epidemiology 162(8):764-773.
Langrish, J. P., N. L. Mills, and D. E. Newby. 2008. Air pollution: The new cardiovascular risk factor. Internal Medicine Journal 38(12):875-878.
Law, M. G., N. Friis-Moller, W. M. El-Sadr, R. Weber, P. Reiss, A. D’Arminio Monforte, R. Thiebaut, L. Morfeldt, S. De Wit, C. Pradier, G. Calvo, O. Kirk, C. A. Sabin, A. N. Phillips, J. D. Lundgren, and D. A. D. Study Group. 2006. The use of the Framingham equation to predict myocardial infarctions in HIV-infected patients: Comparison with observed events in the D:A:D study. HIV Medicine 7(4):218-230.
Lawes, C. M. M., S. Vander Hoorn, A. Rodgers, and International Society of Hypertension. 2008. Global burden of blood-pressure-related disease, 2001. Lancet 371(9623):1513-1518.
Lawlor, D. A., S. Ebrahim, and G. Davey Smith. 2001. Sex matters: Secular and geographical trends in sex differences in coronary heart disease mortality. British Medical Journal 323(7312):541-545: Erratum 325(7364):580.
Leeder, S., S. Raymond, and H. Greenberg. 2004. A race against time: The challenge of cardiovascular disease in developing economics. New York: Columbia University.
Legato, M. J. 1998. Cardiovascular disease in women: Gender-specific aspects of hypertension and the consequences of treatment. Journal of Women’s Health 7(2):199-209.
Lesperance, F., and N. Frasure-Smith. 2007. Depression and heart disease. Cleveland Clinic Journal of Medicine 74(Suppl 1):S63-S66.
Lichtman, J. H., J. T. Bigger Jr., J. A. Blumenthal, N. Frasure-Smith, P. G. Kaufmann, F. Lesperance, D. B. Mark, D. S. Sheps, C. B. Taylor, and E. S. Froelicher. 2008. Depression and coronary heart disease: Recommendations for screening, referral, and treatment—a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation 118(17):1768-1775.
Lin, H. H., M. Ezzati, and M. Murray. 2007. Tobacco smoke, indoor air pollution and tuberculosis: A systematic review and meta-analysis. PLoS Medicine 4(1).
Liu, G. G., W. H. Dow, A. Z. Fu, J. Akin, and P. Lance. 2008. Income productivity in China: On the role of health. Journal of Health Economics 27(1):27-44.
Lopez, A. D., C. D. Mathers, M. Eszati, D. T. Jamison, and C. J. L. Murray. 2006. Global burden of disease and risk factors. Washington, DC: World Bank.
Lopez-Jaramillo, P., S. Y. Silva, N. Rodriguez-Salamanca, A. Duran, W. Mosquera, and V. Castillo. 2008. Are nutrition-induced epigenetic changes the link between socioeconomic pathology and cardiovascular diseases? American Journal of Therapeutics 15(4):362-372.
Low, P. S., C. K. Heng, N. Saha, and J. S. Tay. 1996. Racial variation of cord plasma lipoprotein(a) levels in relation to coronary risk level: A study in three ethnic groups in Singapore. Pediatric Research 40(5):718-722.
Lucas, D. L., R. A. Brown, M. Wassef, and T. D. Giles. 2005. Alcohol and the cardiovascular system research challenges and opportunities. Journal of the American College of Cardiology 45(12):1916-1924.
Mackay, J. 1992. US tobacco export to third world: Third world war. Journal of the National Cancer Institute Monographs (12):25-28.
Mackay, J., and M. Eriksen. 2002. The tobacco atlas. Geneva: World Health Organization.
Mackay, J., G. Mensah, S. Mendis, K. Greenlund, and World Health Organization Department of Management of Noncommunicable Diseases. 2004. The atlas of heart disease and stroke. Geneva: World Health Organization.
Manninen, V., L. Tenkanen, P. Koskinen, J. K. Huttunen, M. Manttari, O. P. Heinonen, and M. H. Frick. 1992. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation 85(1):37-45.
Marcovina, S. M., J. J. Albers, E. Wijsman, Z. Zhang, N. H. Chapman, and H. Kennedy. 1996. Differences in Lp[a] concentrations and apo[a] polymorphs between black and white Americans. Journal of Lipid Research 37(12):2569-2585.
Marin-Neto, J. A., E. Cunha-Neto, B. C. Maciel, and M. V. Simões. 2007. Pathogenesis of chronic Chagas heart disease. Circulation 115(9):1109-1123.
Martinez, D., and V. Grise. 1990. With U.S. sale down, tobacco industry looks abroad. Farm-line US Department of Agriculture Economic Research Service 11(3):18-20.
Martinez, E., M. Larrousse, and J. M. Gatell. 2009. Cardiovascular disease and HIV infection: Host, virus, or drugs? Current Opinion in Infectious Diseases 22(1):28-34.
Martinez-Gonzalez, M. A., M. Bes-Rastrollo, L. Serra-Majem, D. Lairon, R. Estruch, A. Trichopoulou, M. A. Martinez-Gonzalez, M. Bes-Rastrollo, L. Serra-Majem, D. Lairon, R. Estruch, and A. Trichopoulou. 2009. Mediterranean food pattern and the primary prevention of chronic disease: Recent developments. Nutrition Reviews 67(Suppl 1): S111-S116.
Mathers, C. D., and D. Loncar. 2006. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(11):e442.
Mathers, C. D., C. Bernard, K. M. Iburg, M. Inoue, D. M. Fat, K. Shibuya, N. Timijuma, and H. Xu. 2003. Global burden of disease in 2002: Data sources, methods, and results. Global Programme on Evidence for Health Policy Discussion Paper No. 54. Geneva: World Health Organization.
Mathers, C. D., D. Ma Fat, M. Inoue, C. Rao, and A. D. Lopez. 2005. Counting the dead and what they died from: An assessment of the global status of cause of death data. Bulletin of the World Health Organization 83:171-177c.
Mayosi, B. M., L. J. Burgess, and A. F. Doubell. 2005. Tuberculous pericarditis. Circulation 112(23):3608-3616.
Mayosi, B. M., A. J. Flisher, U. G. Lalloo, F. Sitas, S. M. Tollman, and D. Bradshaw. 2009. The burden of non-communicable diseases in South Africa. Lancet 374(9693):934-947.
Mbewu, A., and J. Mbanya. 2006. Cardiovascular disease. In Disease and mortality in Sub-Saharan Africa. Edited by D. Jamison, R. G. Feachem, M. W. Makgoba, E. R. Bos, F. K. Baingana, K. J. Hofman and K. O. Rogo. Washington, DC: World Bank Group. Pp. 305-328.
Mendis, S., D. Abegunde, S. Yusuf, S. Ebrahim, G. Shaper, H. Ghannem, and B. Shengelia. 2005. WHO study on prevention of recurrences of myocardial infarction and stroke (WHO-PREMISE). Bulletin of the World Health Organization 83(11):820-828.
Miguez-Burbano, M. J., X. Burbano, D. Ashkin, A. Pitchenik, R. Allan, L. Pineda, N. Rodriguez, and G. Shor-Posner. 2003. Impact of tobacco use on the development of opportunistic respiratory infections in HIV seropositive patients on antiretroviral therapy. Addiction Biology 8(1):39-43.
Miller, T. L., E. J. Orav, S. E. Lipshultz, K. L. Arheart, C. Duggan, G. A. Weinberg, L. Bechard, L. Furuta, J. Nicchitta, S. L. Gorbach, and A. Shevitz. 2008. Risk factors for cardiovascular disease in children infected with human immunodeficiency virus-1. Journal of Pediatrics 153(4):491-497.
Mirzaei, M., A. S. Truswell, R. Taylor, and S. R. Leeder. 2009. Coronary heart disease epidemics: Not all the same. Heart 95(9):740-746.
Misra, A., and L. Khurana. 2008. Obesity and the metabolic syndrome in developing countries. Journal of Clinical Endocrinology and Metabolism 93(11 Suppl 1):S9-S30.
Moncayo, A., and M. I. O. Yanine. 2006. An update on Chagas disease (human American trypanosomiasis). In Annals of Tropical Medicine and Parasitology: Maney Publishing. 100(8):663-677.
Morel, C. M., and J. Lazdins. 2003. Chagas disease. Nature Reviews Microbiology 1(1): 14-15.
Mukamal, K. J., and E. B. Rimm. 2001. Alcohol’s effects on the risk for coronary heart disease. Alcohol Research and Health 25(4):255-261.
Mukamal, K. J., S. E. Chiuve, E. B. Rimm, K. J. Mukamal, S. E. Chiuve, and E. B. Rimm. 2006. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Archives of Internal Medicine 166(19):2145-2150.
Muna, W. F. T. 1993. Cardiovascular disorders in Africa. World Health Statistics Quarterly 46(2):125-133.
Myint, P. K., R. N. Luben, N. J. Wareham, S. A. Bingham, and K. T. Khaw. 2009. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years’ follow-up in Norfolk cohort of European prospective investigation of cancer (EPIC Norfolk): Prospective population study. British Medical Journal 338:b349.
Narkiewicz, K., S. E. Kjeldsen, and T. Hedner. 2006. Hypertension and cardiovascular disease in women: Progress towards better understanding of gender-specific differences? Blood Pressure 15(2):68-70.
Nathan, D. M., P. A. Cleary, J. Y. Backlund, S. M. Genuth, J. M. Lachin, T. J. Orchard, P. Raskin, and B. Zinman. 2005. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. New England Journal of Medicine 353(25):2643-2653.
Ng, N. 2006. Chronic disease risk factors in a transitional country: The case of rural Indonesia, Folkhälsa och klinisk medicin, Umeå.
Ng, N., H. Stenlund, R. Bonita, M. Hakimi, S. Wall, and L. Weinehall. 2006. Preventable risk factors for noncommunicable diseases in rural Indonesia: Prevalence study using WHO STEPS approach. Bulletin of the World Health Organization 84(4):305-313.
Ng, S. W., E. C. Norton, and B. M. Popkin. 2009. Why have physical activity levels declined among Chinese adults? Findings from the 1991-2006 China health and nutrition surveys. Social Science and Medicine 68(7):1305-1314.
Nishtar, S., A. M. A. Faruqui, M. A. Mattu, K. B. Mohamud, and A. Ahmed. 2004. The national action plan for the prevention and control of non-communicable diseases and health promotion in Pakistan—cardiovascular diseases. Journal of the Pakistan Medical Association 54(12 Suppl 3):S14-S25.
Ntsekhe, M., and B. M. Mayosi. 2009. Cardiac manifestations of HIV infection: An African perspective. Nature Clinical Practice Cardiovascular Medicine 6(2):120-127.
Office of National Statistics, L. Henderson, K. Irving, and J. Gregory. 2003. The national diet & nutrition survey: Adults aged 19 to 64 years. London: Office of National Statistics.
Olshansky, S. J. 2006. Commentary: Prescient visions of public health from Cornaro to Breslow. International Journal of Epidemiology 35(1):22-23.
Olshansky, S. J., and A. B. Ault. 1986. The fourth stage of the epidemiologic transition: The age of delayed degenerative diseases. Milbank Quarterly 64(3):355-391.
Omran, A. R. 1971. The epidemiologic transition. A theory of the epidemiology of population change. The Milbank Memorial Fund Quarterly 49(4):509-538.
Palomaki, G. E., S. Melillo, and L. A. Bradley. 2010. Association between 9p21 genomic markers and heart disease: A meta-analysis. Journal of the American Medical Association 303(7):648-656.
Pao, V., G. A. Lee, and C. Grunfeld. 2008. HIV therapy, metabolic syndrome, and cardiovascular risk. Current Atherosclerosis Reports 10(1):61-70.
Pencina, M. J., R. B. D’Agostino, M. G. Larson, J. M. Massaro, and R. S. Vasan. 2009. Predicting the 30-year risk of cardiovascular disease: The Framingham Heart Study. Circulation 119(24):3078-3084.
Peng, R. D., H. H. Chang, M. L. Bell, A. McDermott, S. L. Zeger, J. M. Samet, and F. Dominici. 2008. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among medicare patients. Journal of the American Medical Association 299(18):2172-2179.
Pereira, M., N. Lunet, A. Azevedo, and H. Barros. 2009. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. Journal of Hypertension 27(5):963-975.
Physical Activity Guidelines Advisory Committee. 2008. Physical activity guidelines advisory committee report, 2008. Washington, DC: U.S. Department of Health and Human Services.
Pietinen, P., E. Vartiainen, R. Seppanen, A. Aro, and P. Puska. 1996. Changes in diet in Finland from 1972 to 1992: Impact on coronary heart disease risk. Preventive Medicine 25(3):243-250.
Pilote, L., K. Dasgupta, V. Guru, K. H. Humphries, J. McGrath, C. Norris, D. Rabi, J. Tremblay, A. Alamian, T. Barnett, J. Cox, W. A. Ghali, S. Grace, P. Hamet, T. Ho, S. Kirkland, M. Lambert, D. Libersan, J. O’Loughlin, G. Paradis, M. Petrovich, and V. Tagalakis. 2007. A comprehensive view of sex-specific issues related to cardiovascular disease. Canadian Medical Association Journal 176(6):S1-S44: Erratum 176(9):1310.
Polk, D. M., and T. Z. Naqvi. 2005. Cardiovascular disease in women: Sex differences in presentation, risk factors, and evaluation. Current Cardiology Reports 7(3):166-172.
Pope, C. A., and D. W. Dockery. 2006. Health effects of fine particulate air pollution: Lines that connect. EM: Air and Waste Management Association’s Magazine for Environmental Managers (JUN).
Pope, C. A., R. T. Burnett, G. D. Thurston, M. J. Thun, E. E. Calle, D. Krewski, and J. J. Godleski. 2004. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation 109(1):71-77.
Prentice, A. M., and S. E. Moore. 2005. Early programming of adult diseases in resource poor countries. Archives of Disease in Childhood 90(4):429-432.
Puska, P., E. Vartiainen, J. Tuomilehto, V. Salomaa, and A. Nissinen. 1998. Changes in premature deaths in Finland: Successful long-term prevention of cardiovascular diseases. Bulletin of the World Health Organization 76(4):419-425.
Puska, P., E. Vartiainen, T. Laatinkainen, P. Jousilahti, and M. Paavola, eds. 2009. The North Karelia project: From North Karelia to national action. Helsinki: Helsinki University Printing House.
Rao, A. V. 1998. Coronary heart disease risk factors in women: Focus on gender differences. Journal of the Louisiana State Medical Society 150(2):67-72.
Rao, C., A. D. Lopez, G. Yang, S. Begg, and J. Ma. 2005. Evaluating national cause-of-death statistics: Principles and application to the case of China. Bulletin of the World Health Organization 83:618-625.
Ray, K. K., S. R. K. Seshasai, S. Wijesuriya, R. Sivakumaran, S. Nethercott, D. Preiss, S. Erqou, and N. Sattar. 2009. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: A meta-analysis of randomised controlled trials. Lancet 373(9677):1765-1772.
Reddy, K. S. 2007. India wakes up to the threat of cardiovascular diseases. Journal of the American College of Cardiology 50(14):1370-1372.
Reddy, S. P., S. Panday, D. Swart, C. C. Jinabhai, S. L. Amosun, S. James, K. D. Monyeki, G. Stevens, N. Morejele, N. S. Kambaran, R. G. Omardien, and H. W. Van den Borne. 2003. Umthenthe uhlaba usamila: The South African Youth Risk Behavior Survey 2002. Cape Town: South African Medical Research Council.
Reeves, M. J., C. D. Bushnell, G. Howard, J. W. Gargano, P. W. Duncan, G. Lynch, A. Khatiwoda, and L. Lisabeth. 2008. Sex differences in stroke: Epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurology 7(10):915-926.
Regitz-Zagrosek, V. 2006. Therapeutic implications of the gender-specific aspects of cardiovascular disease. Nature Reviews Drug Discovery 5(5):425-438.
Rehm, J., C. Mathers, S. Popova, M. Thavorncharoensap, Y. Teerawattananon, and J. Patra. 2009. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373(9682):2223-2233.
Reuser, M., L. G. Bonneux, and F. J. Willekens. 2009. Smoking kills, obesity disables: A multistate approach of the US Health and Retirement Survey. Obesity 17(4):783-789.
Rich, M. W., and G. A. Mensah. 2009. Fifth pivotal research in cardiology in the elderly (price-v) symposium: Preventive cardiology in the elderly—executive summary. Part I: Morning session. Preventive Cardiology 12(4):198-204.
Rich, M. W., and G. A. Mensah. 2010. Fifth pivotal research in cardiology in the elderly (price-v) symposium: Preventive cardiology in the elderly—executive summary. Part II: Afternoon session. Preventive Cardiology 13(1):42-47.
Rodriguez, T., M. Malvezzi, L. Chatenoud, C. Bosetti, F. Levi, E. Negri, and C. La Vecchia. 2006. Trends in mortality from coronary heart and cerebrovascular diseases in the Americas: 1970-2000. Heart 92(4):453-460.
Roeters van Lennep, J. E., H. T. Westerveld, D. W. Erkelens, and E. E. van der Wall. 2002. Risk factors for coronary heart disease: Implications of gender. Cardiovascular Research 53(3):538-549.
Roglic, G., and N. Unwin. 2009. Mortality attributable to diabetes: Estimates for the year 2010. Diabetes Research and Clinical Practice 87(1):15-19.
Rosengren, A., S. Hawken, S. Ounpuu, K. Sliwa, M. Zubaid, W. A. Almahmeed, K. N. Blackett, C. Sitthi-amorn, H. Sato, and S. Yusuf. 2004. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet 364(9438):953-962.
Rossouw, J. E., G. L. Anderson, R. L. Prentice, A. Z. LaCroix, C. Kooperberg, M. L. Stefanick, R. D. Jackson, S. A. Beresford, B. V. Howard, K. C. Johnson, J. M. Kotchen, J. Ockene, and Writing Group for the Women’s Health Initiative. 2002. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women’s Health Initiative randomized controlled trial. Journal of the American Medical Association 288(3):321-333.
Rugulies, R. 2002. Depression as a predictor for coronary heart disease: A review and meta-analysis. American Journal of Preventive Medicine 23(1):51-61.
Sabaté, E., WHO Adherence to Long Term Therapies Project, Global Adherence Interdisciplinary Network, and World Health Organization Deptartment of Management of Noncommunicable Diseases. 2003. Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization.
Sacks, F. M., M. A. Pfeffer, L. A. Moye, J. L. Rouleau, J. D. Rutherford, T. G. Cole, L. Brown, J. W. Warnica, J. M. Arnold, C. C. Wun, B. R. Davis, and E. Braunwald. 1996. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and recurrent events trial investigators. New England Journal of Medicine 335(14):1001-1009.
Sarkar, S., and B. Mukhopadhyay. 2008. Perceived psychosocial stress and cardiovascular risk: Observations among the Bhutias of Sikkim, India. Stress and Health 24(1):23-34.
Sassi, F., M. Cecchini, J. Lauer, and D. Chisholm. 2009. Improving lifestyles, tackling obesity: The health and economic impact of prevention strategies. Paris: OECD.
Sattelmair, J. R., J. H. Pertman, and D. E. Forman. 2009. Effects of physical activity on cardiovascular and noncardiovascular outcomes in older adults. Clinics in Geriatric Medicine 25(4):677-702.
Schaefer, B. M., V. Caracciolo, W. H. Frishman, and P. Charney. 2003. Gender, ethnicity, and genes in cardiovascular disease. Part 2: Implications for pharmacotherapy. Heart Disease 5(3):202-214.
Schneidera, N. K., and T. E. Novotnya. 2007. Addressing smoking cessation in tuberculosis control. Bulletin of the World Health Organization 85(10):820.
Schulze, M. B., F. B. Hu. 2005. Primary prevention of diabetes: What can be done and how much can be prevented? Annual Review of Public Health 26:445-467.
Shafey, O., M. Eriksen, H. Ross, and J. Mackay. 2009. The tobacco atlas. 3rd ed. Atlanta: American Cancer Society.
Shen, B. J., Y. E. Avivi, J. F. Todaro, A. Spiro III, J. P. Laurenceau, K. D. Ward, and R. Niaura. 2008. Anxiety characteristics independently and prospectively predict myocardial infarction in men. The unique contribution of anxiety among psychologic factors. Journal of the American College of Cardiology 51(2):113-119.
Shepherd, J., S. M. Cobbe, I. Ford, C. G. Isles, A. R. Lorimer, P. W. MacFarlane, J. H. McKillop, and C. J. Packard. 1995. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland coronary prevention study group. New England Journal of Medicine 333(20):1301-1307.
Shopland, D. R. 1995. Tobacco use and its contribution to early cancer mortality with a special emphasis on cigarette smoking. Environmental Health Perspectives 103(Suppl 8):131-142.
Shuter, J., and S. Bernstein. 2008. Cigarette smoking is an independent predictor of nonadherence in HIV-infected individuals receiving highly active antiretroviral therapy. Nicotine and Tobacco Research 10(4):731-736.
Slama, K., C. Y. Chiang, D. A. Enarson, K. Hassmiller, A. Fanning, P. Gupta, and C. Ray. 2007. Tobacco and tuberculosis: A qualitative systematic review and meta-analysis. International Journal of Tuberculosis and Lung Disease 11(10):1049-1061.
Slattery, M. L., and D. E. Randall. 1988. Trends in coronary heart disease mortality and food consumption in the united states between 1909 and 1980. American Journal of Clinical Nutrition 47(6):1060-1067.
Sliwa, K., D. Wilkinson, C. Hansen, L. Ntyintyane, K. Tibazarwa, A. Becker, and S. Stewart. 2008. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto study): A cohort study. Lancet 371(9616):915-922.
South African Department of Health and Medical Research Council. 2007. South Africa Demographic and Health Survey 2003. Pretoria, South Africa: South African Department of Health.
Srinivasan, S. R., G. H. Dahlen, R. A. Jarpa, L. S. Webber, and G. S. Berenson. 1991. Racial (black-white) differences in serum lipoprotein (a) distribution and its relation to parental myocardial infarction in children. Bogalusa Heart Study. Circulation 84(1):160-167.
Stamler, J., R. Stamler, and J. D. Neaton. 1993. Blood pressure, systolic and diastolic, and cardiovascular risks: US population data. Archives of Internal Medicine 153(5):598-615.
Steer, A. C., and J. R. Carapetis. 2009. Prevention and treatment of rheumatic heart disease in the developing world. Nature Reviews Cardiology 6(11):689-698.
Steer, A. C., J. R. Carapetis, T. M. Nolan, and F. Shann. 2002. Systematic review of rheumatic heart disease prevalence in children in developing countries: The role of environmental factors. Journal of Paediatrics and Child Health 38(3):229-234.
Stein, A. D., A. M. Thompson, and A. Waters. 2005. Childhood growth and chronic disease: Evidence from countries undergoing the nutrition transition. Maternal & Child Nutrition 1(3):177-184.
Stettler, C., S. Allemann, P. Juni, C. A. Cull, R. R. Holman, M. Egger, S. Krahenbuhl, and P. Diem. 2006. Glycemic control and macrovascular disease in types 1 and 2 diabetes mel-litus: Meta-analysis of randomized trials. American Heart Journal 152(1):27-38.
Steyn, N. P., D. Bradshaw, R. Norman, J. Joubert, M. Schneider, and K. Steyn. 2006. Dietary changes and the health transition in South Africa: Implications for health policy. Cape Town: South African Medical Research Council.
Strong, J. P., G. T. Malcom, C. A. McMahan, R. E. Tracy, W. P. Newman, 3rd, E. E. Herderick, and J. F. Cornhill. 1999. Prevalence and extent of atherosclerosis in adolescents and young adults: Implications for prevention from the pathobiological determinants of atherosclerosis in youth study. Journal of the American Medical Association 281(8):727-735.
Thomas, R. J., P. J. Palumbo, L. J. Melton Iii, V. L. Roger, J. Ransom, P. C. O’Brien, and C. L. Leibson. 2003. Trends in the mortality burden associated with diabetes mellitus: A population-based study in Rochester, Minn, 1970-1994. Archives of Internal Medicine 163(4):445-451.
Turnbull, F. M., C. Abraira, R. J. Anderson, R. P. Byington, J. P. Chalmers, W. C. Duckworth, G. W. Evans, H. C. Gerstein, R. R. Holman, T. E. Moritz, B. C. Neal, T. Ninomiya, A. A. Patel, S. K. Paul, F. Travert, and M. Woodward. 2009. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. DOI 10.1007/s00125-00009-01470-00120.
Turtzo, L. C., and L. D. McCullough. 2008. Sex differences in stroke. Cerebrovascular Diseases 26(5):462-474.
Unal, B., J. A. Critchley, and S. Capewell. 2004. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 109(9): 1101-1107.
United Nations Development Program. 2007. Human development report 2007/2008: Fighting climate change: Human solidarity in a divided world. New York: United Nations Development Program.
van Cappelle, F. 2009. StatPlanet: Interactive Data Visualization and Mapping Software, Southern and Eastern Africa Consortium for Monitoring Educational Quality, Paris. http://www.sacmeq.org/statplanet (accessed January 21, 2010).
van Dam, R. M., T. Li, D. Spiegelman, O. H. Franco, F. B. Hu, R. M. van Dam, T. Li, D. Spiegelman, O. H. Franco, and F. B. Hu. 2008. Combined impact of lifestyle factors on mortality: Prospective cohort study in US women. British Medical Journal 337:a1440.
Vartiainen, E., P. Puska, P. Jousilahti, H. J. Korhonen, J. Tuomilehto, and A. Nissinen. 1994a. Twenty-year trends in coronary risk factors in North Karelia and in other areas of Finland. International Journal of Epidemiology 23(3):495-504.
Vartiainen, E., P. Puska, J. Pekkanen, J. Tuomilehto, and P. Jousilahti. 1994b. Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. British Medical Journal 309(6946):23-27.
Victora, C. G., L. Adair, C. Fall, P. C. Hallal, R. Martorell, L. Richter, and H. S. Sachdev. 2008. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 371(9609):340-357.
Wagner, S., and R. M. Romano. 1994. Tobacco and the developing world: An old threat poses even bigger problems. Journal of the National Cancer Institute 86(23):1752.
Walker, S., and S. George. 2007. Young@heart. USA: Fox Searchlight Pictures.
Wang, L., X. Qi, C. Chen, J. Ma, L. Li, K. Rao, L. Kong, G. Ma, H. Xiang, J. Pu, J. Chen, Y. Chen, C. Chen, Y. He, J. Zhang, S. Jin, Y. Wu, X. Yang, J. Hu, C. Yao, W. Zhao, K. Ge, and F. Zai, eds. 2005. Survey and report on the status of nutrition and health of the Chinese people: A comprehensive report for 2002. Beijing: People’s Medical Publishing House.
Wang, Y., J. Mi, X. Y. Shan, Q. J. Wang, and K. Y. Ge. 2007. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. International Journal of Obesity 31(1):177-188.
Warren, C. W. 2003. Differences in worldwide tobacco use by gender: Findings from the global youth tobacco survey global. Journal of School Health 73(6):207-215.
Warren, C. W., N. R. Jones, A. Peruga, J. Chauvin, J. P. Baptiste, V. Costa de Silva, F. el Awa, A. Tsouros, K. Rahman, B. Fishburn, D. W. Bettcher, and S. Asma. 2008. Global youth tobacco surveillance, 2000-2007. MMWR Surveillance Summaries 57(1):1-28.
Wassertheil-Smoller, S., S. L. Hendrix, M. Limacher, G. Heiss, C. Kooperberg, A. Baird, T. Kotchen, J. D. Curb, H. Black, J. E. Rossouw, A. Aragaki, M. Safford, E. Stein, S. Laowattana, and W. J. Mysiw. 2003. Effect of estrogen plus progestin on stroke in postmenopausal women: The Women’s Health Initiative: A randomized trial. Journal of the American Medical Association 289(20):2673-2684.
Watkins, D. A., L. J. Zuhlke, M. E. Engel, and B. M. Mayosi. 2009. Rheumatic fever: Neglected again. Science 324(5923):37.
Watkins, R. E., and A. J. Plant. 2006. Does smoking explain sex differences in the global tuberculosis epidemic? Epidemiology and Infection 134(2):333-339.
WHO (World Health Organization). 1999. The world health report: 1999: Making a difference. Geneva: World Health Organization.
WHO. 2002. The world health report 2002—reducing risks, promoting healthy life. Geneva: World Health Organization.
WHO. 2003. The world health report: 2003: Shaping the future. Geneva: World Health Organization.
WHO. 2005. Preventing chronic diseases: A vital investment. http://www.who.int/chp/chronic_disease_report/full_report.pdf (accessed April 23, 2009).
WHO. 2007. WHO model list of essential medicines: 15th edition, revised March 2007. Geneva: World Health Organization.
WHO. 2008a. Childhood overweight and obesity. http://www.who.int/dietphysicalactivity/childhood/en/ (accessed December 12, 2008).
WHO. 2008b. The global burden of disease: 2004 update. Geneva: World Health Organization.
WHO. 2008c. WHO report on the global tobacco epidemic, 2008: The MPOWER package. Geneva: World Health Organization.
WHO. 2009a. Global burden of disease 2004 data. Geneva, provided by Colin Mathers.
WHO. 2009b. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization.
WHO. 2009c. WHO model list of essential medicines: 16th edition, revised March 2009. Geneva: World Health Organization.
WHO. 2009d. Working document for developing a draft global strategy to reduce harmful use of alcohol. Geneva: World Health Organization.
WHO. 2009e. World health statistics 2009. Geneva: World Health Organization.
WHO Department of Child and Adolescent Health and Development. 2005. The current evidence for the burden of group a streptococcal diseases, Discussion papers on child health. Geneva: World Health Organization.
WHO Expert Committee on Problems Related to Alcohol Consumption and WHO. 2007. Second report, World Health Organization technical report series. Geneva: World Health Organization.
WHO Expert Committee on the Control of Chagas Disease and WHO. 2002. Control of Chagas disease: Second report of the WHO Expert Committee, WHO technical report series. Geneva: World Health Organization.
WHO Regional Office for the Western Pacific. 2007. Mongolian STEPS survey on the prevalence of noncommunicable disease risk factors 2006. Manila, Philippines: WHO Regional Office for the Western Pacific.
WHO Study Group on Rheumatic Fever and Rheumatic Heart Disease and WHO. 2004. Rheumatic fever and rheumatic heart disease: Report of a WHO expert consultation, Geneva, 20 October–1 November 2001, World Health Organization technical report series. Geneva: World Health Organization.
WHOSIS (World Health Organization Statistical Information System). 2009. World Health Organization.
Witt, B. J., and V. L. Roger. 2003. Sex differences in heart disease incidence and prevalence: Implications for intervention. Expert Opinion on Pharmacotherapy 4(5):675-683.
The Writing Committee. 2004. Cardio- and cerebrovascular events in HIV-infected persons. AIDS 18(13):1811-1817.
Yach, D., C. Hawkes, C. L. Gould, and K. J. Hofman. 2004. The global burden of chronic diseases: Overcoming impediments to prevention and control. Journal of the American Medical Association 291(21):2616-2622.
Yach, D., S. R. Leeder, J. Bell, and B. Kistnasamy. 2005. Global chronic diseases. Science 307(5708):317.
Yang, G., L. Kong, W. Zhao, X. Wan, Y. Zhai, L. C. Chen, and J. P. Koplan. 2008. Emergence of chronic non-communicable diseases in China. Lancet 372(9650):1697-1705.
Young, F., J. Critchley, and N. Unwin. 2009a. Diabetes & tuberculosis: A dangerous liaison & no white tiger. Indian Journal of Medical Research 130(1):1-4.
Young, F., J. A. Critchley, L. K. Johnstone, and N. C. Unwin. 2009b. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and diabetes mellitus, HIV and metabolic syndrome, and the impact of globalization. Global Health 5:9.
Yusuf, P. S., S. Hawken, S. Ounpuu, T. Dans, A. Avezum, F. Lanas, M. McQueen, A. Budaj, P. Pais, J. Varigos, and L. Lisheng. 2004. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 364(9438):937-952.