5
Interventions Directed at Individuals with Hypertension
The previous chapter discusses population-based interventions that can be beneficial irrespective of hypertension status. This chapter focuses more narrowly on interventions directed at individuals who have been diagnosed with hypertension. A wide range of strategies are considered to reduce adverse health consequences associated with hypertension through early detection, treatment, and control. Strategies range from those that offer access to health care providers who screen and treat individuals with high blood pressure, reduce the cost of medications for those in treatment (insurance coverage, benefit design, cost sharing), support hypertension control (e.g., quality control measures), and increase hypertension awareness, treatment, and control (e.g., worksite wellness initiatives). The chapter also considers community health workers as a potential strategy to increase treatment adherence among individuals with hypertension.
ACCESS TO CARE AND CONTROL OF HYPERTENSION
Access to health care, including access to providers, is generally considered important to improved health outcomes (IOM, 2003b,d). Data are somewhat mixed, however, about whether hypertension control is improved if patients have a regular source of care (Ahluwalia et al., 1997; Col et al., 1990; Fihn and Wicher, 1988; He et al., 2002). Studies that have shown improvement in care include data from multiple surveys. For example, national survey data (e.g., the 1987 Medical Expenditure Panel Survey [MEPS]) have shown that having a regular source of care is associated with
hypertension screening, follow-up care, and the use of medication (Moy et al., 1995). Data from the 1990 National Health Interview Survey (NHIS) showed a strong association between seeing a physician in the past year and taking action to control hypertension (taking medication, reducing salt, reducing weight) (CDC, 1994). Similarly, in an analysis of the NHANES (National Health and Nutrition Examination Survey) III, He et al. (2002) found that the percentage of persons with controlled hypertension was higher for those who visited the same facility (Odds Ratio [OR] = 2.77 [1.88-4.09]) or saw the same provider (OR = 2.29 [1.74-3.02]) for their health care. Another study reported that severe, uncontrolled hypertension was more common among Medicaid patients who could not identify a source of care (Lurie et al., 1984).
A few case control studies have reported similar findings. Shea et al. (1992b) found that severe, uncontrolled hypertension was more common among those who did not have a primary care physician (adjusted OR = 3.5 [1.6-7.7]) and those who did not comply with antihypertensive treatment (adjusted OR = 1.9 [1.4-2.5]). Ahluwalia and colleagues (1997) also found that controlled hypertension was associated with having a regular place of care (OR = 7.93 [3.86-16.29]. In a study of medically stable Department of Veterans Affairs (VA) patients terminated from regular outpatient care, compared with those retained in care, 41 percent of discharged patients had blood pressure that was uncontrolled compared to 5 percent at the time of discharge; blood pressures were taken 13 months after discharge (p < 0.001) (data for the control group were 17 percent at follow-up vs. 9 percent, a nonsignificant difference). Among discharged patients with diagnosed hypertension, systolic blood pressure rose an average of 11.2 mm Hg; diastolic blood pressure rose an average of 5.6 mm Hg (p < 0.001). Of the discharged group, 47 percent reduced their prescription medications compared with 25 percent in the control group (p = 0.002) (Fihn and Wicher, 1988).
Another study found that one of the factors associated with a hospitalization due to noncompliance with medication (medications included an ACE [angiotensin-converting enzyme] inhibitor) was the number of physicians seen regularly (p = 0.007). The adjusted OR for seeing a greater number of physicians was 2.0 (p < 0.005) (Col et al., 1990).
On the other hand, Kotchen and colleagues reported that neither having seen a provider within the past three months (p > 0.4) nor receiving care from the same provider at each encounter (p > 0.8) was associated with improved hypertension control (Kotchen et al., 1998). Similarly, Stockwell and colleagues found that a greater number of physician visits was not associated with awareness of hypertension, the number of antihypertensive drug days, or blood pressure control (Stockwell et al., 1994).
One of the reasons for the lack of a consistent association between
access to health care and hypertension control may be because control of hypertension is inadequate even in those with access to health care. The NHANES III data have shown that 86 percent of individuals with uncontrolled hypertension have a usual source of care and average 4.3 physician visits per year; 75 percent of those who are unaware of their hypertension had had their blood pressure measured in the previous year. Lack of awareness of hypertension (OR = 7.69; p < 0.001) and being aware but uncontrolled (OR = 2.08; p < 0.001) were more likely in those ages 65 years or older, a population that has access to health care. In fact, most uncontrolled hypertension was mild systolic hypertension in older adults with access to health care and frequent physician contact (Hyman and Pavlik, 2001).
In a cohort study of a hypertensive VA population examined over a two-year period, less than 25 percent had adequate blood pressure control (<140/90 mm Hg), and 40 percent had blood pressure >160/90 mm Hg despite having an average of 6.4 (+3.3) hypertension-related physician visits. In addition, the mean systolic blood pressure (SBP) was virtually unchanged at the end of two years (146.2 and 145.4 mm Hg, not significant), while the diastolic blood pressure (DBP) decreased (from 84.3 to 82.6, p < 0.001) (Berlowitz et al., 1998). In the Stockwell et al. (1994) study of a well-insured population, 71 percent of individuals with hypertension were aware of their hypertension, only 49 percent were being treated, and only 12 percent of these were controlled (<140/90 mm Hg), despite frequent utilization of the health care system. Other researchers have also reported poor hypertensive control despite access to health care. Framingham study participants are highly compliant with follow-up exams, and findings on exam are discussed with them and also sent to their primary care providers. Still, in a Framingham cohort followed for four years, only 32 percent of untreated individuals with hypertension were subsequently on treatment, and only 40 percent of those not under control initially (>140 mm Hg SBP or >90 mm Hg DBP) were brought under control. Older age was a strong predictor for lack of control overall and among those under treatment (Lloyd-Jones et al., 2002).
In a survey of African Americans, 27 percent were unaware of their hypertension, despite 77 percent of them having had a blood pressure measurement by a physician within the previous 2 years; most had mild systolic hypertension. Those unaware of their hypertension were only slightly less likely to have had their blood pressure checked in the past year and were nearly equally likely as those who were aware to have had it checked in the prior 2 years (Pavlik et al., 1997). Kotchen et al. (1998) reported that only 70 percent of inner-city individuals with hypertension were aware of their hypertension, 55 percent were taking medication, and 26 percent were under control despite most having seen a physician within the previous 6 months.
Hyman and Pavlik calculated the attributable risk of lack of awareness of hypertension (Table 5-1): 46 percent of the attributable risk was being age 65 years or older; 22 percent was being male; 5 percent was being African American; and 9 percent was having no recent visit to a physician. They also calculated the attributable risk of being aware but having uncontrolled hypertension: 32 percent of the attributable risk was being age 65 years or older; 12 percent was being male; and only 8 percent was having had no recent physician visit (Hyman and Pavlik, 2001).
Consequences of Racial and Ethic Disparities in Awareness, Treatment, and Control
The above demographic differences in awareness, treatment, and control of hypertension directly contribute to the nation’s long-standing racial, ethnic, gender, and age disparities from cardiovascular disease (CVD) and kidney disease. For example, using data from the NHANES III Mortality Follow-up Study (mean duration = 8.5 years; 143,551 person-years), Gu et al. (2008) observed a 3.86 greater risk (hazard ratio = 3.86, 95 percent confidence interval [95% CI]: 1.60-9.32) of CVD deaths among individuals with hypertension under age 65 compared to similar-age individuals with normal blood pressure levels. For non-Hispanic whites, the hazard ratio for hypertensives vs. normotensives was 1.70 (95% CI: 1.09-2.65); however, when non-Hispanic white hypertensives with controlled blood pressure were compared to their normotensive counterparts, the excess CVD mortality risk was no longer statistically significant (hazard ratio = 1.17, 95% CI: 0.72-1.91). For non-Hispanic blacks, a considerably smaller reduction in the hazard ratio was observed—4.65 (95% CI: 2.26-9.57) for controlled hypertensives vs. 3.93 for normotensives (95% CI: 1.78-8.68). The comparable hazard ratios for Mexican Americans were 2.09 (95% CI: 0.93-4.65) vs. 1.27 (95% CI: 0.46-3.52), a reduction slightly greater than that for non-Hispanic whites. Gu et al. (2008) speculated that the much smaller reduction in excess CVD mortality for blacks with controlled hypertension was probably due to several factors, including an earlier onset and greater severity of hypertension, less adequate blood pressure control, and less access to health care services. The cumulative effects of these factors probably led to more severe hypertensive target organ damage in blacks, thereby elevating CVD mortality rates even among those whose hypertension was controlled.
Lopes et al. (2003) described some of the most promising recent advances in nonpharmacologic (e.g., diet, physical activity) as well as pharmacologic approaches to treating hypertension in African Americans. First, they noted the acceptability (Vollmer et al., 1998) and the effectiveness (Svetkey et al., 1999) of the DASH (Dietary Approaches to Stop Hypertension) diet (low-fat dairy food, fruit or vegetables, and foods low in total and
saturated fat) among African Americans who enrolled in the DASH clinical trial. Bray and colleagues, in an analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure, also reported that the lower the sodium level, the greater the mean reduction in blood pressure. The effect was even more pronounced and beneficial for African Americans (Bray et al., 2004).
Lopes et al. (2003) also highlighted findings from a randomized controlled clinical trial (Kokkinos et al., 1995) wherein African-American men with stage three hypertension were assigned, or not, to a regimen of moderately intense, aerobic physical activity for 16 weeks. Engaging in aerobic exercise was associated with a significant decrease in blood pressure among the men randomized to the exercise arm. In addition, significant reductions in thickness of the interventricular septum and left ventricular mass, and in the left ventricular index, were observed for men assigned to the exercise arm. Collectively, these findings from well-designed and executed clinical trials of nonpharmacologic interventions for hypertension provide encouraging evidence that carefully supervised nonpharmacologic interventions focused on African Americans will likely reduce their excess risk for serious medical complications known to be caused by uncontrolled hypertension.
In summarizing advances in pharmacologic approaches to treating hypertension in African Americans, Lopes et al. (2003) concluded that studies continue to support the use of diuretics and beta-blockers as first-line antihypertensive therapy for everyone, regardless of race. However, they noted that findings from the African-American Study of Kidney Disease and Hypertension, or the AASK trial (Wright et al., 2002), also provided some support for the use of ACE inhibitors as first-line antihypertensive drugs in African Americans. An ACE inhibitor-based treatment program, they concluded, was more beneficial than calcium channel blockers and beta-blockers in reducing the progression of renal failure in blacks with hypertensive nephropathy.
Thus, recent studies indicate that closely supervised administration of nonpharmacologic as well as pharmacologic antihypertensive interventions by primary care providers could substantially reduce the black-white racial disparities in medical complications due to poorly controlled blood pressure. As is true of much of the extant literature on disparities in U.S. health care, the literature on hypertension continues to be disproportionately focused on blacks and whites and there is a lack of evidence-based recommendations that address disparities in hypertension awareness, treatment, and control for the nation’s other high-risk populations.
TABLE 5-1 Proportion of Cases of Uncontrolled Hypertension in Each Population Subgroup Attributable to Identified Risk Factors
Physician Adherence to Guideline Recommendations and Hypertension Control
Although patient compliance with treatment is one reason for lack of hypertension control, it is also clear that lack of physician adherence to hypertensive guidelines is a major problem and a significant reason for the lack of awareness, lack of pharmacologic treatment, and lack of hypertension control in the United States (Chiong, 2008; Pavlik et al., 1997). Notably, older age and SBP predicted lack of control, even if the blood pressure was being treated (Lloyd-Jones et al., 2000; Pavlik et al., 1997). The NHANES III data show that lack of awareness of hypertension (OR = 7.69; p < 0.001) and being aware but uncontrolled (OR = 2.08; p < 0.001) were more likely in those ages 65 years or older: persons >65 years of age comprise 45 percent of the unaware, 32 percent of the aware but untreated, and 57 percent of the treated but uncontrolled hypertensives. Lack of hypertension control was associated with older age: OR = 2.43 (1.79-3.29) for ages 61-75 years, and OR = 4.34 (3.10-6.09) for those >75 years of age (Lloyd-Jones et al., 2000). In fact, most uncontrolled hypertension was mild systolic hypertension in older adults with access to health care and frequent physician contact. In addition, 75 percent of the unaware, 60 percent of the known but untreated, and 75 percent of the treated but not controlled hypertensives had a DBP <90 mm Hg (Hyman and Pavlik, 2001). A Framingham study found that only 33 percent were controlled to a systolic blood pressure goal, whereas 83 percent were controlled to a diastolic blood pressure goal. Of those on medication (61 percent), 49 percent were controlled to a systolic blood pressure goal compared with 90 percent to a diastolic blood pressure goal (Lloyd-Jones et al., 2000).
Physician Nonadherence to Recommendations for Treatment of Hypertension
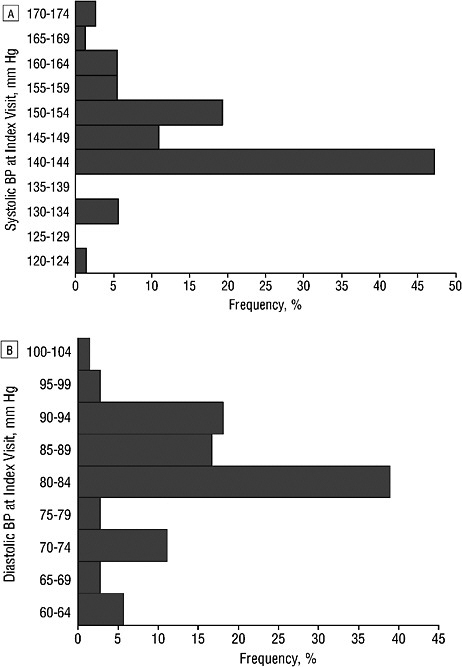
Systolic hypertension may be more complex to treat than diastolic pressure (SHEP Cooperative Research Group, 1991), but multiple studies show that physicians are unlikely to treat or intensify treatment for mild to moderate systolic hypertension (<165 mm Hg) if the DBP is <90 mm Hg (Figures 5-1 and 5-2) (Berlowitz et al., 1998; Hyman et al., 2000). Berlowitz and colleagues (in a VA cohort study) found that if SBP was >155 mm Hg and the DBP >90 mm Hg, treatment was intensified 25.6-35.0 percent of the time (the larger percentage was if the medication had been changed during the previous visit); if the SBP was >165 mm Hg and the DBP was <90 mm Hg, medication was increased 21.6 percent of the time, but if the SBP was <165 mm Hg, medication was increased only 3.2 percent of the time when the DBP was <90 mm Hg. Overall, treatment was
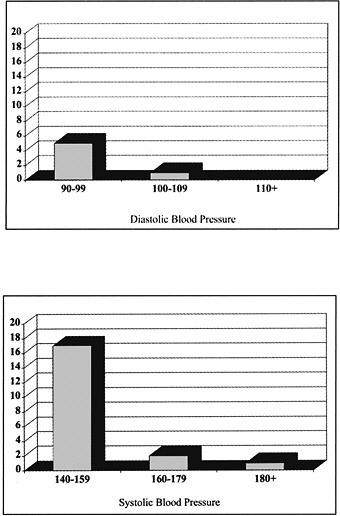
FIGURE 5-1 The proportion of patients over a 24-month period that was not diagnosed with hypertension, separated by average diastolic and systolic blood pressure.
SOURCE: Physician Role in Lack of Awareness and Control of Hypertension, Hyman, D.J., V.N. Pavlik, and C. Vallbona, 2000. Copyright © 2000 Journal of Clinical Hypertension. Reproduced with permission of Blackwell Publishing Ltd.
intensified in only 6.7 percent of visits (Berlowitz et al., 1998). Oliveria and colleagues also identified patients with uncontrolled hypertension. Pharmacologic therapy was initiated or changed at only 38 percent of the visits, despite documented hypertension for at least 6 months prior to the most recent visit (Oliveria et al., 2002).
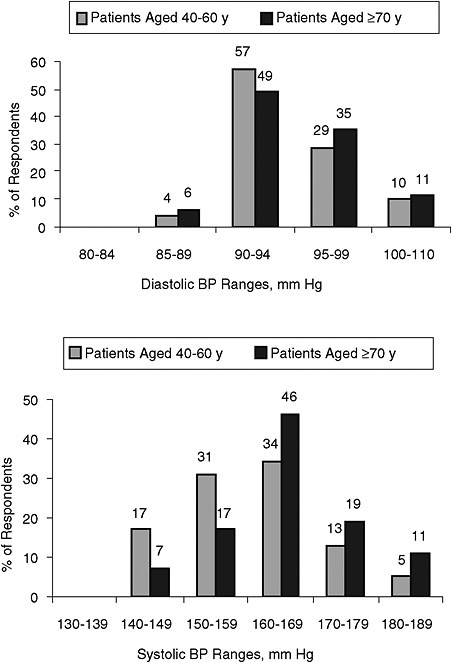
FIGURE 5-2 The diastolic and systolic blood pressure ranges at which physicians would start drug treatment in patients with uncomplicated hypertension. SOURCE: Hyman and Pavlik, Archives of Internal Medicine, August 14, 2000, 160: 2283. Copyright © (2000) American Medical Association. All rights reserved.
In a study that linked adults’ survey responses to their medical records, Hyman and colleagues found that these adults averaged 5.7 physician visits (median 4.0 visits). Of those with a 24-month average blood pressure >140/90, 25 percent were not diagnosed with hypertension. This proportion of “unaware” is comparable to the national rate reported by the NHANES III. Only 5 percent of those with a DBP greater than 90 mm Hg did not have a diagnosis of hypertension, but two-thirds were not diagnosed if the blood pressure was 140-159/<90 mm Hg. Of those on medication, the average blood pressure was 147/86, and only 24 percent had a blood pressure <140/90. When the DBP was >90 mm Hg, 98 percent had medication prescribed and treatment was intensified 24 percent of the time if the blood pressure remained >90 mm Hg. Treatment was intensified only 4 percent of the time when the SBP was >140 and the DBP <90 mm Hg. There was almost no action taken for persistently high SBP over many consecutive visits (Figure 5-1) (Hyman et al., 2000).
A recent study by Okonofua et al. (2006) assessed the extent of therapeutic inertia, defined as providers’ failure to increase therapy when treatment goals are unmet, in 62 diverse clinical sites participating in the Hypertension Initiative medical record audit and feedback program conducted in the Southeastern part of the United States. The researchers found that antihypertensive therapy was not intensified in 86.9 percent of visits when blood pressure was ≥140/90. They estimated that improvement of 20 percent in the percentage of visits in which treatment is intensified, blood pressure control could increase from the study’s observed 46.2 percent to a projected 65.9 percent in one year. The study did not provide information on the reasons for therapeutic inertia.
Physician adherence to guidelines for nonpharmacological strategies to manage hypertension is also problematic. Lifestyle modifications (weight management, healthy diet, exercise) or nonpharmacologic strategies have been found to be effective in managing hypertension as discussed in Chapter 4. Few physicians however, encourage patients to make such modifications. Based on data from the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) for 1999-2000, only about 35 percent of patients with hypertension received counseling for diet and 26 percent for exercise (Mellen et al., 2004). Asians and Hispanics received the highest levels of counseling and non-Hispanic whites the least. Patients with Medicaid had the highest exercise counseling rates compared to patients with other payment providers. Diet counseling did not differ by payment provider. Diet counseling rates were also higher for patients with co-occurring diabetes, obesity, or dyslipidemia. With respect to exercise counseling, patients with obesity, had significantly higher odds of receiving exercise counseling. Patients with two or more cardiovascular morbidities were also more likely to receive diet and exercise counseling com-
pared to those with less than one co-occurring morbidity. In NAMCS office-based practices, 36 percent of hypertension patients received diet counseling and 27 percent received exercise counseling. In NHAMCS hospital-based clinics, 25 percent received diet counseling and 14 percent counseling for exercise.
A more recent study found that health care providers fail to counsel patients with hypertension to increase physical activity as a measure to lower blood pressure. Halm and Amoako (2008), in an analysis of the NHANES III data, found that only one-third of patients with hypertension reported having received a physical activity recommendation from their health care provider. However, 70 percent of those counseled followed the recommendation and had on average a systolic blood pressure that was 3 to 4 mm Hg lower than those who did not follow the recommendation. Given the potential impact of nonpharmacologic strategies on hypertension management, this is an area that deserves greater attention.
Reasons for Poor Physician Adherence with Guidelines
Survey data shows that U.S. physicians are more likely to report that they adhere to diastolic threshold recommendations for initiating or intensifying treatment than for systolic thresholds (Chiong, 2008). In a national survey of primary care physicians, Hyman found that 33 percent would not start treatment for middle-aged patients with uncomplicated hypertension unless the DBP was >95 mm Hg; 52 percent of physicians would not start treatment for an SBP of 140-160, and 43 percent would not start treatment unless the SBP was greater than 160 mm Hg. For patients ages 40-60 years without complications who were on drug treatment, 25 percent of physicians would not intensify drug therapy for a persistent DBP of 94 mm Hg; 33 percent would not intensify drug treatment for an SBP of 158 mm Hg. Providers were even less aggressive in older patients: 48 percent would not take action for an elevated DBP of 94 mm Hg, and 67 percent would not take action for those ages 70 years or older with an SBP <160 mm Hg (Hyman and Pavlik, 2000).
Similarly, in a survey of primary care clinicians at three VA medical centers compared with the clinical database of patients cared for by these providers, clinicians overestimated the proportion of patients who were prescribed guideline-concordant medications (75 percent perceived vs. 67 percent actual, p < 0.001) and the proportion of patients who had blood pressures levels <140/90 at their last visit (68 percent perceived vs. 43 percent actual, p < 0.001). Physicians with lowest actual performance were the most likely to overestimate their adherence and rates of control (Steinman et al., 2004).
Oliveria and colleagues (2002) identified patients with uncontrolled
hypertension. The treating primary care physicians were then asked to complete a survey about the patient visit (and given a copy of their office notes). The most frequently cited reason for no initiation or intensification of therapy was that there was a need to continue monitoring (35 percent); satisfaction with BP level (30 percent); it was not the focus of the visit (29 percent); the presence of a satisfactory DBP (16 percent); and the presence of only borderline hypertension (10 percent). For 93 percent of visits in which the physician reported being satisfied with the BP level, SBP was >140 mm Hg; 35 percent had a blood pressure >150 mm Hg; and the DBP was >90 mm Hg at 22 percent of these visits. Physicians attributed a higher risk to elevated DBP than to elevated SBP, and on average, physicians reported that 150 mm Hg was the lowest SBP at which they would recommend pharmacologic treatment for those without comorbidities (compared to 91 mm Hg for DBP) (Figure 5-3) (Oliveria et al., 2002).
In an older study in Wales, the reasons given for not starting or intensifying treatment in older patients with isolated systolic hypertension were fear that side effects would decrease the quality of life (39 percent); isolated systolic hypertension was an inevitable consequence of aging (35 percent); systolic hypertension was not as great a problem as diastolic hypertension (32 percent); isolated systolic hypertension was a compensatory mechanism to force blood through arteriosclerotic arteries (28 percent); and there was no beneficial effect of treating hypertension in the elderly (14 percent) (Ekpo et al., 1993).
Despite 1988 guidelines recommending treatment if SBP >140 mm Hg or DBP >90 mm Hg, 41 percent of primary care physicians had not heard of or were not familiar with the Joint National Committee (JNC) guidelines. Familiarity with the JNC guidelines was consistently associated with having more aggressive blood pressure goals, including statistically significant increases in initiating treatment for SBP in older patients and intensifying treatment for mildly elevated SBP and DPB in younger patients. However, familiarity with the guidelines was associated with a lower likelihood of intensifying treatment among older patients with mildly elevated SBP, particularly if they have isolated systolic hypertension (Hyman and Pavlik, 2000).
According to the NHANES III data, isolated systolic hypertension in the elderly comprises the majority of uncontrolled hypertension in the United States (Franklin et al., 2001; Hyman and Pavlik, 2001). Isolated systolic hypertension was also the majority subtype of uncontrolled hypertension among those >50 years of age. Additionally, only 29 percent of those with an SBP >140 mm Hg knew they were hypertensive, and 80 percent of both the untreated and the inadequately treated older individuals with hypertension had isolated systolic hypertension (Figure 5-4) (Franklin et al., 2001; Izzo et al., 2000). Factors that could lead to reduced control of

FIGURE 5-4 (Top) Frequency and distribution of untreated hypertensive individuals by age and hypertension subtype. Numbers at the tops of bars represent the overall percentage distribution of all subtypes of untreated hypertension in that age group. (Bottom) Frequency distribution of hypertensive individuals classified as inadequately treated by age and hypertension (HTN) subtype. Numbers at top of bars represent overall percentage distribution of all subtypes of inadequately treated hypertension in that age group. ■, Isolated Systolic Hypertension (SBP ≥ 140 mm Hg and DBP <90 mm Hg); ![]() , Systolic-Diastolic Hypertension (SBP ≥ 140 mm Hg and DBP ≥90 mm Hg); □, Isolated Diastolic Hypertension (SBP <140 mm Hg and DBP ≥90 mm Hg).
, Systolic-Diastolic Hypertension (SBP ≥ 140 mm Hg and DBP ≥90 mm Hg); □, Isolated Diastolic Hypertension (SBP <140 mm Hg and DBP ≥90 mm Hg).
SOURCE: Franklin et al., Predominance of Isolated Systolic Hypertension Among Middle-Aged and Elderly US Hypertensives. Hypertension 37(3):871.
hypertension in the elderly include potential biological resistance to therapy because of longer duration of hypertension and more target organ damage (Franklin et al., 2001; Izzo et al., 2000; Lloyd-Jones et al., 2002). However, it is also clear that physicians are less aggressive in treating older patients and less aggressive in treating isolated systolic hypertension (Berlowitz et al., 1998; Chiong, 2008; Hyman et al., 2000; Izzo et al., 2000; Lloyd-Jones et al., 2002). “Undiagnosed hypertension and treated but uncontrolled hypertension occurs largely under the watchful eye of the health care system”
(Hyman and Pavlik, 2001). Furthermore, physicians are not providing treatment consistent with the JNC guidelines, particularly in the treatment of isolated systolic hypertension, yet the largest attributable fraction for lack of awareness and lack of control of hypertension is being age 65 years or older and having isolated systolic hypertension.
Patient Nonadherence to Treatment of Hypertension
Patient noncompliance with prescribed antihypertensive medications is also a problem that contributes to suboptimal rates of blood pressure control. It is estimated that 50 percent of patients discontinue drug treatment after one year, and only 10 percent continue to follow advice concerning lifestyle modifications (Elliott, 2003). This problem can be addressed in part by increased attention from providers in identifying barriers to medication adherence and engaging patients in treatment decisions (Harmon et al., 2006). One study investigating how providers assess antihypertensive medication adherence revealed that patients were not asked about medication taking in 39 percent of encounters (Bokhour et al., 2006). Effective communication strategies and patient-centered counseling can be employed as a means to improve treatment adherence.
Krousel-Wood and colleagues (2005) suggest that future research should focus on the development of adherence models that consider the influence of social, psychological, and biological variables on antihypertensive medication adherence. Some established methods of improving adherence to long-term therapies include the provision of verbal and written instructions and patient education materials, simplification of regimen, once a day dosing (when possible), minimizing the number of pills, recommendation of well-tolerated therapies, and sensitivity concerning cost of pills and attempt to minimize out-of-pocket costs (Elliott, 2003).
Quality of Care and Performance Measurement for Hypertension Care
Shortfalls in the general quality of health care in the United States have been well documented (IOM, 2000, 2001b, 2003c). Studies discussed previously also indicate that the quality of care for hypertension received by some patients, particularly the elderly, is suboptimal (Oliveria et al., 2002). Further, the First National Report Card on Quality of Health Care in America published by the RAND Corporation in 2004 documented that patients with hypertension received less than 65 percent of recommended care (RAND, 2006).
Since the release of the Institute of Medicine (IOM) health care quality report series (IOM, 2000, 2001b, 2003c), improving quality of care has become of paramount concern for a whole host of health care sys-
tem stakeholders (plans, providers, purchasers). In support of healthcare quality improvement, organizations such as the National Committee for Quality Assurance (NCQA) and the American Medical Association (AMA)-Physician Consortium for Performance Improvement (PCPI) have developed performance measure for determining benchmarks by which health care providers and organizations can assess their progress in improving health care services, processes, and outcomes. These organizations include specific performance measures for care of hypertension (Table 5-2). The Healthcare Effectiveness Data and Information Set (HEDIS®) performance measures put forth by the NCQA are widely used to assess quality of care and service of health plans. Health plans use HEDIS® results to determine the need for and focus of quality improvement efforts. In an analysis of the potential effects of eight HEDIS® performance measures related to the quality of care for cardiovascular disease and diabetes, Eddy et al. (2008) concluded that “[f]rom the perspective of the population as a whole, the most important single measure is the hypertension measure, which is very effective in reducing the risk of both MIs [myocardial infarctions] and strokes. This is due to the large number of people who had diagnosed but uncontrolled hypertension (approximately 14 percent of adults in the pre-HEDIS population) and the effectiveness of available treatments in preventing CVD events in people who have uncontrolled hypertension.”
The PCPI is a physician-led initiative to develop tools by physicians for physicians. Members of the consortium include clinical experts representing more than 50 national medical specialty societies, state medical
TABLE 5-2 HEDIS® and Physician Consortium for Performance Improvement Hypertension Measures
|
Measures |
|
HEDIS® Measures Controlling High Blood Pressure: Percentage of patients 18-85 years of age with a diagnosis of hypertension whose blood pressure was adequately controlled (less than 140/90 mm Hg) during the management year |
|
PCPI Measures Blood Pressure Screening: Percentage of patient visits for patients aged 18 years and older with a diagnosis of hypertension with blood pressure recorded |
|
Plan of Care: Percentage of patient visits for patients aged 18 years and older with a diagnosis of hypertension with either systolic blood pressure is greater than or equal to 140 mm Hg or diastolic blood pressure is greater than or equal to 90 mm Hg, with documented plan of care for hypertension |
|
SOURCES: AMA, 2006; NCQA, 2009. |
societies, methodological experts, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Medicare & Medicaid Services. The PCPI develops evidence-based clinical performance measures and outcomes reporting tools for physicians. Both organizations (NCQA and PCPI) envision that routine measurement of hypertensive care quality among provider groups or plans can lead to improved care processes and blood pressure control (Table 5-2).
Organizations or providers seeking to improve care processes, services, and outcomes can turn to a number of potential strategies. The AHRQ (2004) commissioned a review of the literature related to specific strategies for improving the quality of hypertension treatment. Among the quality strategies assessed were physician and patient reminder systems, continuing education for physicians, education for patients, and electronic transfer of patient data from specialty clinics to primary care physicians, among other strategies. The researchers found that most of the quality improvement strategies contributed to some improvement in the detection and control of high blood pressure, but it was difficult to determine which strategy was superior. The researchers also noted that multiple strategies are often used so it is difficult to identify which have the greatest effect on patient outcomes. The researchers observed that few of the quality improvement strategies had an impact on providers’ adherence to optimal treatment guidelines. In summary, performance measurement can catalyze action toward quality improvement, some quality improvement strategies can improve hypertension detection and control, but improving physician adherence to treatment guidelines poses an elusive problem requiring further attention.
Cost of Medication and Hypertension
One reason for patient nonadherence with treatment is out-of-pocket costs for medication (Chockalingam et al., 1998). Controlling for health status, financial burden (out-of-pocket costs compared to income) has been shown to be significantly greater for persons with chronic conditions such as hypertension (Rogowski et al., 1997). Many studies, using a variety of methodologies, have documented a relationship between cost to patients, poorer adherence to treatment, and poorer control of hypertension (Fihn and Wicher, 1988).
Several studies have utilized survey data to assess the relationship between cost and adherence to treatment (Ahluwalia et al., 1997; Clark, 1991; Col et al., 1990). Generally these studies have reported that cost is a significant problem (Mojtabai and Olfson, 2003), particularly for ethnic minorities, those with lower incomes, and those with higher out-of-pocket costs (Fihn and Wicher, 1988; Steinman et al., 2001). In a 2002 nationally
representative survey of chronically ill U.S. adults, 9 percent had cost-related antihypertensive medication underuse in the previous year, and 7 percent underused at least monthly. Income and high out-of-pocket costs (OR = 4.6; p < 0.001) were each associated with cost-related underuse of antihypertensive medications (Piette et al., 2004). In a 1981 survey, a larger proportion of people with uncontrolled or moderate to severe hypertension than controlled hypertension reported economic barriers to pharmacologic and medical care. Cost was a barrier to getting initial medication (36 percent for uncontrolled vs. 22 percent for those with controlled hypertension); medication refills (36 percent vs. 16 percent); and office visits (26 percent vs. 16 percent) (Shulman et al., 1986). In an older Gallup survey, 6 percent of respondents reported that they stopped their antihypertensive medication because they could not afford the cost (Gallup and Cotugno, 1986). A case control study found that control of hypertension was associated with reporting that cost was not a deterrent to buying medications (OR = 3.63 [1.59-8.28]) (Ahluwalia et al., 1997).
A few studies have looked at the cost of treatment and linked it to health outcomes. In the 2000 Health and Retirement Study, cost-related poor medication adherence was related to self-reported adverse health outcomes: 7 percent vs. 4 percent had worsening of hypertension (OR = 1.76; p < 0.05), and the odds of BP not being controlled were 1.92 (p < 0.01) (Mojtabai and Olfson, 2003). Noncompliance with antihypertensive medication is associated with increased hospital admissions (Maronde et al., 1989). McCombs et al. (1994) found that continuous antihypertensive therapy was associated with statistically significant reductions in hospital expenditures per patient that were greater than the accompanying drug costs; they estimated that an additional day of uninterrupted drug therapy would save $3 per day in total costs. In a study of medically stable VA patients discharged from regular care (compared with those retained in care), those discharged who reported a financial barrier to receiving care had a mean increase in SBP of 14.0 mm Hg and a mean increase in DBP of 6.4 mm Hg; this was significantly greater than the 3.2 mm Hg increase in SBP and 0.5 mm Hg increase in DBP among those reporting no financial barriers (p = 0.001 and 0.0001, respectively) (Fihn and Wicher, 1988).
Insurance Coverage and Control of Hypertension
One way of reducing patient costs of treatment is through insurance coverage. Many studies have examined the impact of insurance coverage on hypertension. Many of the data come from observational studies.
Insurance and Screening for Hypertension
Data from national surveys (1982 NHIS, 1987 MEPS) support the association of insurance coverage with hypertension screening, follow-up care, and use of medication (Chiong, 2008; Moy et al., 1995; Woolhandler and Himmelstein, 1988). For example, inadequate screening for hypertension was 18 percent among the uninsured vs. 11 percent for the insured (adjusted OR = 1.46 [1.28-1.67]; p < 0.01) (Woolhandler and Himmelstein, 1988). In another survey, the long-term uninsured (19.5 percent) and short-term uninsured (8.6 percent) were less likely than the insured (5.8 percent) to have been screened for hypertension in the previous 2 years (both were statistically significant differences) (Ayanian et al., 2000). In a randomized controlled trial that was representative of the U.S. population, the Rand Health Insurance Experiment, hypertensive individuals given free care were more likely to see a physician and to have their hypertension detected and a medication prescribed (Keeler et al., 1985, 1987).
Studies have assessed the impact of insurance coverage on utilization of antihypertensive medications (Adams et al., 2001b; Blustein, 2000). In a state survey among hypertensives, the adjusted odds ratio of prescription treatment for those with prescription drug coverage compared to those without prescription drug coverage was 1.20 (0.87-1.64) (Stuart and Grana, 1998). Data from the 2000 Health and Retirement Study showed that going from full coverage to partial coverage and from partial coverage to no coverage reduced compliance with antihypertensive medications (adjusted OR = 0.46; p < 0.001). The percentages with poor adherence due to cost were 11 percent for those with no coverage, 5 percent for those with partial coverage, and 4 percent for those with full coverage (Mojtabai and Olfson, 2003). Two studies used the 1995 Medicare Current Beneficiary Survey: Blustein (2000) reported that hypertensives without drug coverage (21.8 percent) were more likely than those with coverage (17.1 percent) to have not purchased any antihypertensive medication (p < 0.01); the adjusted percentage was 22.2 percent versus 16.9 percent (OR = 1.4; p = 0.002). Insurance coverage was not significantly associated with the number of tablets purchased in the unadjusted analysis, but in the multivariate analysis, medication coverage increased the number of tablets purchased per year by 37 (p = 0.02) (Blustein, 2000). Adams and colleagues reported that the utilization of antihypertensive medications was 1.26 (p = 0.043) among Medicare enrollees with coverage compared with those who had no coverage. Better insurance coverage led to greater use of antihypertensive medications and purchase of a greater number of tablets (Adams et al., 2001b). In a 2002 nationally representative survey of chronically ill U.S. adults, the OR was 3.3 (p < 0.001) for underuse of antihypertensive medi-
cation among those with no prescription coverage compared to those with such coverage (Piette et al., 2004).
On the other hand, in a study of low-income black and Hispanic patients diagnosed with hypertensive emergency or hypertensive urgency (compared to controls who were hypertensive patients hospitalized or seen in the emergency room [ER] for other acute conditions), Shea et al. (1992a) found that self-reported nonadherence to medication was not significantly associated with insurance coverage (OR = 1.6 [0.84-3.10]).
Some studies have assessed the relationship between insurance coverage and control of hypertension (Ahluwalia et al., 1997). An analysis of the NHANES III data showed that the percentage of persons with controlled hypertension was higher among those with private insurance as compared with uninsured or government-insured individuals (OR = 1.59 [1.02-2.49]) (He et al., 2002). In a survey of low-income African Americans, those having no insurance were significantly more likely to have uncontrolled hypertension (Pavlik et al., 1997). In a case series of consecutive hospital admissions, lack of insurance coverage for prescription drugs was associated with hospitalization due to medication noncompliance (medications implicated in hospitalizations due to noncompliance included an ACE inhibitor). The elderly (whose medications were not covered by insurance) were most likely to be noncompliant with their medication (52 percent vs. 31 percent; p = 0.04) (Col et al., 1990). Being switched from free care to paying $20-$30 per visit led to a significant worsening of hypertension at 6 months (10 mm Hg higher vs. no change in the control group) and one year (6 mm Hg higher than baseline [p < 0.001]). At 1 year, the percentage of people with a diastolic blood pressure <90 mm Hg was 51 percent, compared with 75 percent at baseline (p < 0.01); the percentage with DBP >100 mm Hg was 19 percent, compared with 3 percent at baseline (p < 0.01) (Lurie et al., 1986). Another study in two states assessed the relative risk of admission for avoidable hospital conditions (AHCs). The uninsured and those on Medicaid were more likely than the insured to be hospitalized with AHCs. For malignant hypertension, the odds of AHCs for the uninsured vs. those with private insurance were 2.38 (1.83-2.93; p < 0.05) in Massachusetts and 1.93 (1.41-2.44; p < 0.05) in Maryland. For Medicaid recipients, the odds ratios were 1.56 (1.29-1.82; p < 0.05) and 1.74 (1.36-2.13; p < 0.05), respectively (Weissman et al., 1992). A study of indigent inner-city hypertensive patients showed that hypertension control was associated with having insurance (OR = 2.15 [1.02-4.52]) (Ahluwalia et al., 1997). Another study of low-income black and Hispanic patients reported that severe, uncontrolled hypertension was more common among persons with no health insurance (adjusted OR = 2.2 [1.0-4.6]; p = 0.04) (Shea et al., 1992b).
The NHANES III data show that 92 percent of persons with uncon-
trolled hypertension have health insurance (Hyman and Pavlik, 2001). Similarly, among a well-insured population in New York, only 71 percent were aware of their hypertension, only 49 percent were treated, and only 12 percent had their blood pressure controlled at recommended levels (Stockwell et al., 1994).
Hypertension Control and Cost Sharing Among Those with Insurance
Cost sharing is described by AHRQ as the contribution consumers make toward the cost of their health care as defined in their health insurance policy. Rising health care costs have resulted in a shift toward greater cost sharing, particularly for prescription medications. There is a substantial body of literature (primarily observational studies) investigating the implications of cost sharing on medication utilization. Several studies have examined the impacts and health outcomes associated with cost sharing of “essential” medications such as antihypertensives.
A Cochrane review and other studies have reported that out-of-pocket costs (whether imposed as copayments, caps, ceilings, tiered drug categories, and/or restricted formularies) can reduce medication utilization, often substantially (Adams et al., 2001a; Artz et al., 2002; Austvoll-Dahlgren et al., 2008; Blustein, 2000; Cox et al., 2001; Fairman et al., 2003; Goldman et al., 2004, 2007; Harris et al., 1990; Huskamp et al., 2003; Kamal-Bahl and Briesacher, 2004; Landsman et al., 2005; Lexchin and Grootendorst, 2004; Motheral and Henderson, 1999a; Nair et al., 2003; Poirier and Le-Lorier, 1998; Reeder and Nelson, 1985; Schneeweiss et al., 2002a; Shrank et al., 2006; Solomon et al., 2009; Soumerai et al., 1991, 1994; Taira et al., 2006; Tamblyn et al., 2001; Tseng et al., 2004). In some cases, patients faced with out-of-pocket costs do not start their medication, reduce the amount of medication taken to make it last longer, switch medication, discontinue the medication, or take someone else’s medicine (Cox et al., 2001; Schulz et al., 1995; Tseng et al., 2004). However, not all studies have shown significant impacts associated with cost sharing (Blais et al., 2001; Motheral and Fairman, 2001; Motheral and Henderson, 1999b). A review article, after excluding studies with very small cost-sharing changes and those without an adequate control group, estimated that cost-sharing increases of 10 percent would be associated with a 2-6 percent decrease in prescription drug use or expenditures (Goldman et al., 2007).
Most studies assessing the impact of cost sharing on essential drugs such as antihypertensives have reported a significant decrease in use (4-28 percent), with smaller impact seen for essential medications than nonessential medications (Adams et al., 2001a; Austvoll-Dahlgren et al., 2008; Goldman et al., 2007; Harris et al., 1990; Hsu et al., 2006; Landsman et al., 2005; Lexchin and Grootendorst, 2004; Motheral and Henderson, 1999a;
Nair et al., 2003; Reeder and Nelson, 1985; Schneeweiss et al., 2002a; Shrank et al., 2006; Soumerai et al., 1991, 1994; Tamblyn et al., 2001). A few studies, however, showed no significant difference in the use of essential drugs or between use of essential and nonessential drugs (Goldman et al., 2007; Johnson et al., 1997b; Lohr et al., 1986; Motheral and Fairman, 2001; Motheral and Henderson, 1999b). For example, Fairman and colleagues (2003) compared an intervention group of members switched from a two-tier to a three-tier plan with a comparison group retained in the two-tier plan (tiered plans employ formularies with differential copayments to encourage the use of generic drugs, or brand drugs that have been made available at a discounted rate). Although there was lower use of nonformulary (tier 3) medications in the first year, antihypertensive therapy continuation rates were not significantly different during the second year. Similarly, Motheral and Fairman (2001) found that moving from a two-tier to a three-tier plan resulted in no significant decrease in use of antihypertensive medication.
A Cochrane review concluded that the impact of cost sharing was greater for the chronically ill and persons on multiple drugs (AustvollDahlgren et al., 2008). Most studies that have assessed the differential impact have found a greater impact of cost sharing among low-income patients (Brook et al., 1983; Goldman et al., 2007; Schneeweiss et al., 2002a; Shrank et al., 2006; Tamblyn et al., 2001), but not all (Poirier and LeLorier, 1998). It has also been reported that low-income patients were more likely than high-income patients to stop all antihypertensive therapy (Schneeweiss et al., 2002a).
Studies Assessing Impact of Cost Sharing on Antihypertensive Medication Utilization
The impact of cost sharing specifically related to the use of antihypertensive medication has been assessed (Adams et al., 2001a; Blais et al., 2001; Blustein, 2000; Brook et al., 1983; Fairman et al., 2003; Goldman et al., 2004; Hsu et al., 2006; Huskamp et al., 2003; Johnson et al., 1997b; Kamal-Bahl and Briesacher, 2004; Keeler et al., 1985; Landsman et al., 2005; Motheral and Fairman, 2001; Motheral and Henderson, 1999a; Poirier and LeLorier, 1998; Schneeweiss et al., 2002a; Taira et al., 2006). In an analysis of the 1995 Medicare Current Beneficiary Survey, Blustein (2000) found that a $1 increase in out-of-pocket per-tablet cost resulted in the purchase of 114 fewer hypertension pills per year. In a study by Schneeweiss (2002a), 3 percent of individuals subject to cost sharing discontinued all antihypertensive medications; however, Johnson (1997b) found that the largest price increase led to fewer days of antihypertensive medication use, but not discontinuance of treatment.
In a cross-sectional study of Medstat’s 1999 MarketScan database, Kamal-Bahl and Briesacher (2004) noted that the average annual use of antihypertensive medication was lower in the two- or three-tier plans with higher copayments, but not in single-tier plans. The average antihypertensive use in two-tier plans dropped from 18.9 prescriptions to 14.5 prescriptions with copayment increases of $5-$10 for brand-name products even though less costly generics were available. When brand-name copayments were increased to at least $14, the average annual use of antihypertensive medication fell to 10.8 prescriptions, despite a large increase in generic spending. The effect was greatest for angiotension II receptor blockers (ARBs) and ACE inhibitors.
Claims data have been used as a means to compare the impact of various benefit designs on the use of antihypertensive medication. Doubling copayments has been shown to reduce antihypertensive use by 26 percent, with less impact among those under regular care (Goldman et al., 2004). Higher cost sharing has been associated with delayed initiation of hypertensive therapy. Solomon and colleagues (2009) found that doubling copays led to initiation of therapy in 39.9 percent (compared with 54.8 percent) at one year and 66.2 percent (compared with 81.6 percent) by 5 years. The authors concluded that the effect of cost sharing is greatest soon after diagnosis and then declines over time; however, in those without prior medication experience it declines more slowly. Taira and colleagues (2006) found that medication compliance decreased substantially with increasing copayments.
In a study examining the effect of a preferred drug list restricting 17 antihypertensive medications, 21 percent of individuals on antihypertensives were found to discontinue their medication (Wilson et al., 2005). Another study found that a 66-100 percent increase in copayments led to a significant decrease in use of calcium channel blockers (CCBs) (4.1 percent) and ACE inhibitors (4.1 percent) and a nonsignificant decrease in ARBs (3.2 percent). There were also significantly higher discontinuance rates for ACE inhibitors (23.8 percent net increase) and ARBs (25.7 percent net increase) and a nonsignificant increase in discontinuance rate for CCBs in the three-tier plans (Landsman et al., 2005). In a prospective cohort study, Hsu et al. (2006) found that 15 percent of persons on long-term antihypertensive therapy whose drug benefits were capped were nonadherent the next year; significantly more than among those whose drug benefits were not capped.
Cost sharing is not always consistent with decrease in utilization. In one study, the intervention group with the change in benefits was less likely than the control group to stop using ACE inhibitors (Huskamp et al., 2003). In another study, the introduction of a new cost sharing led to a significant decrease in antihypertensive medication use at three months, but only a 1.1 percent decline (not significant) at 13 months (Blais et al., 2001). Fairman
and colleagues (2003) compared those switched from a two- to a three-tier plan with those retained in the two-tier plan, and found that continuation rates for antihypertensive medications did not differ significantly at 6 through 38 months’ follow-up. A RAND randomized controlled trial found that cost sharing had little impact on compliance with medication, but that those under free care were more likely to be taking medication (due to improved case finding, prescription of medication, and more frequent follow-up) (Keeler et al., 1985, 1987; Lohr et al., 1986).
Cost Sharing for Medication and Health Impacts
Although concerns have been raised about adverse health outcomes from reductions in “essential” drugs to treat chronic diseases, only a few studies have examined the impact of cost sharing on health outcomes, ER visits, or hospitalization (Adams et al., 2001a; Anis et al., 2005; Austvoll-Dahlgren et al., 2008; Brook et al., 1983; Goldman et al., 2007; Hsu et al., 2006; Lexchin and Grootendorst, 2004; Soumerai et al., 1991, 1994), and very few have specifically assessed the impact on hypertensive patients. Studies focusing on chronically ill patients have consistently shown greater use of inpatient and ER services with higher cost sharing; however, studies across broader ranges of drugs showed mixed results as to whether cost sharing leads to adverse health outcomes or increased costs (Goldman et al., 2007).
In a large study restricted to persons using medication for which a reduction in use might be expected to have an adverse affect on health, a 25 percent cost-sharing policy for prescription drugs up to an income-dependent deductible was associated with reductions in essential drug use and an increase in serious adverse events and emergency room visits among the elderly and welfare recipients. In contrast, reductions in use of less essential drugs were not associated with an increase in risk of adverse events or ER visits (Tamblyn et al., 2001). In a prospective cohort study, Hsu and colleagues (2006) reported that those whose prescriptions were capped had fewer office visits and worse physiologic outcomes (systolic blood pressure >140 mm Hg) than those whose prescriptions were not capped. Capped individuals also had an increase in ER visits, increase in nonelective hospitalizations, and higher death rates. The rates of elective hospitalization were not significantly different between the two groups.
In an older randomized controlled trial that was representative of the U.S. population (the RAND Health Insurance Experiment), those who had only catastrophic coverage had the highest blood pressures. Hypertensive individuals given free care were more likely than those under cost-sharing plans to be compliant with dietary recommendations, to have a BP <140/90 (43 percent in free care vs. 37 percent for those in a cost-sharing plan), and
to have a BP <160/95 (65 percent vs. 56 percent). The impact was greater for those of lower socioeconomic status (SES). The authors estimated a 5-8 percent difference in the probability of death in the next year as a result of poorer hypertension control in the cost-sharing plan (Brook et al., 1983; Keeler et al., 1985, 1987). Hypertensive individuals in the cost-sharing plans were less likely to be diagnosed with hypertension despite having a blood pressure 4 mm Hg higher than those with free care who had also seen a physician This failure to diagnose and treat resulted in most of the overall difference in blood pressure control between plans at the end of the study (Keeler et al., 1985, 1987).
Not all research has demonstrated adverse health outcomes associated with cost sharing. For example, Johnson et al. (1997a) reported no consistent changes in office visits, emergency room visits, home health care visits, or hospitalization with copayment changes over four time periods. In comparing members switched from a two-tier to a three-tier plan with those retained in the two-tier plan, Fairman and colleagues (2003) found that the two groups did not differ significantly with respect to the number of office visits, emergency department visits, or inpatient hospitalizations. Another study assessing the impact of moving from a two-tier to a three-tier system also found no significant difference in emergency room visits or hospitalizations (Motheral and Fairman, 2001). A study comparing patients whose ACE inhibitors were put on reference pricing with those switched to an ACE inhibitor that was not subject to the price increase found a transient (2-month) increase in physician visits and hospitalization through the emergency room for those who were switched to reference pricing, but no evidence that reference pricing resulted in increased long-term health care utilization (Schneeweiss et al., 2002b). In a prospective cohort study, Hsu and colleagues (2006) reported that those whose prescriptions were capped had lower pharmacy and outpatient visit costs, but higher hospitalization costs and higher ER costs than individuals not subject to a cap. Total medical costs were comparable in the two groups. In a study of individuals who were switched to a no-cost ACE inhibitor compared with those who had cost sharing for ACE inhibitors, overall health care costs decreased (a slight increase in costs of physician visits but large decreases in medication costs) (Schneeweiss et al., 2002b).
EMPLOYER INITIATIVES TO ADDRESS HYPERTENSION
Traditional worksite health promotion programs strive to maintain worker health, improve work productivity, lower health care costs, and enhance organizational image and future interests (Goetzel and Ozminkowski, 2008). Increasingly, worksite health promotion programs are an element of corporate “health management” programs. Typically these programs
provide a number of workforce-based initiatives that may include health promotion services, disease management, and other efforts to improve employee productivity by improving employee health (Goetzel et al., 2007).
Healthy People 2010 further describes workplace health promotion to include not only health education that focuses on skill development and lifestyle behavior change but also programs that help employees assess health risks and link to health plan benefits to provide appropriate medical follow-up and treatment. Key to these programs is their integration within the organizational structure and a supportive environment in which organizational values, norms, policies, and initiatives reinforce and support a healthy work culture (Partnership for Prevention, 2001).
The evidence supporting worksite prevention interventions is addressed in the Guide to Community Preventive Services (2009). The Task Force on Community Preventive Services reviewed the 31 studies to determine if health risks assessment with feedback plus health education with or without other interventions could lead to changes in employees’ health outcomes; blood pressure was included among these outcomes. Of the studies reviewed, significant changes were seen in systolic and diastolic blood pressure. The median decrease in systolic blood pressure was 2.6 mm Hg, and the median decrease in diastolic blood pressure was 1.8 mm Hg. A decrease of 4.5 percentage points (median) in the proportion of employees with a high-risk blood pressure reading was also noted. The Task Force concluded that there is strong evidence of effectiveness to support worksite interventions that include the assessment of health risks with feedback plus health education with or without other interventions.
Worksite prevention programs may be attractive to employers if they can yield a return on investment (ROI). Koffman et al. (2005), for example, found a $3 to $6 ROI for every dollar invested over a 2- to 5-year period to implement a comprehensive worksite health promotion program focused on employee cardiovascular health. Aldana (2001) reported an average ROI of $3.48 in health care savings for every dollar expended on a health promotion program. Of the 12 studies reviewed to assess the financial impact of health promotion programs on health care costs, 7 studies had a positive ROI and 4 studies reported no effects of the programs on health care costs. Aldana (2001) also reported significant ROI (from $2.50 to $10.00 saved for every dollar invested) related to reductions in employee absenteeism.
Some employers have begun to explore benefit-based or value-based interventions as a means to address financial barriers that may hinder an employee’s treatment. Benefit- or value-based insurance design refers to programs that provide a reduction in costs to targeted patients for targeted interventions that are deemed from the medical evidence to be highly beneficial. For example, a program might provide lower copayments for hyperten-
sion patients for blood pressure medications that are known to be effective (Chernew et al., 2007) Pitney Bowes, a Fortune 500 company, reduced or removed coinsurance on maintenance drugs for diabetes, hypertension, and asthma. Data available on diabetes care indicated that ER use decreased by 26 percent and pharmacy costs decreased by 7 percent. Total direct health care costs per plan participant with diabetes decreased by 6 percent. The hotel chain Marriott also began waiving employee copayments on generic drugs and reducing copayments by half for brand name drugs for diabetes, asthma, and heart disease (Capozza, 2008); health outcomes and other results are still pending.
To promote worksite wellness, the Centers for Disease Control and Prevention (CDC) Division for Heart Disease and Stroke Prevention (DHDSP) has partnered with the National Business Coalition on Health, the National Business Group on Health (NBGH), and other private entities. In 2006, NBGH released A Purchaser’s Guide to Clinical Preventive Services: Moving Science into Coverage developed in cooperation with the CDC and the AHRQ (CDC and NBGH, 2006). The guide provides advice to employers to assist them in purchasing health services that have the greatest impact on health improvement and are cost-effective. Hypertension screening, counseling, and treatment are identified among the top 25 high-value preventive services identified in the guide. The document ranked hypertension screening, counseling, and treatment with the highest score of clinical preventive burden of disease (on a scale of 1 to 5 where 5 is the highest score) and a medium score of 3 for cost-effectiveness (on the 5-point scale). Overall, hypertension screening, counseling, and treatment was ranked sixth out of the top 25 high-value preventive services (CDC, 2009; Maciosek et al., 2006; Partnership for Prevention, 2006).
Other products useful for employers include the CDC’s Successful Business Strategies to Prevent Heart Disease and Stroke Toolkit, which provides guidance and resources to be used by state heart disease and stroke prevention programs to engage the business community (CDC, 2008b). The toolkit includes a check list to help employers choose and negotiate health benefit packages that fit the needs of their employees. The American College of Sport Medicine’s Worksite Health Handbook is another resource for employers. It provides a compilation of research, evidence, and practice information that supports worksite health promotion as a means to enhance productivity management, health promotion, and chronic disease management (American College of Sports Medicine, 2009).
COMMUNITY HEALTH WORKERS AND HYPERTENSION
Previous sections have addressed a number of system factors that influence the control of hypertension. Individual factors such as motivation to
take prescribed medication and healthy lifestyle choices also play a role. Community health workers (CHWs) have been studied as a strategy to help improve hypertension control (Brownstein et al., 2005, 2007). Community health workers are broadly defined as “community members who work almost exclusively in community settings and who serve as connectors between healthcare consumers and providers to promote health among groups that have traditionally lacked access to care” (Witmer et al., 1995). They serve as lay educators, coaches, navigators, advocates, and liaisons to the health care system (Brownstein et al., 2005).
Brownstein et al. (2007) reviewed randomized controlled trials (RCTs) and other studies to examine the effectiveness of CHWs in supporting the care of individuals with hypertension. Highlights from the review include positive behavioral changes in 9 of 10 studies: improved appointment keeping, improved adherence to medications, and improved blood pressure control. Among the 5 studies that addressed adherence to medications, 2 RCTs saw significant improvement in the intervention groups that included CHWs compared to the control group. Another RCT found 26 percent greater compliance among patients receiving intense CHW interventions. A time-series study and a before-and-after study also noted improvement with CHW interventions. With respect to blood pressure control, 9 of 10 studies reported positive improvements. Improvement in blood pressure control ranged from 4 to 46 percent over different time periods (6 to 24 months). One study did not find differences between CHW and control groups.
The roles and duties of CHWs tend to be similar across studies and reflect the common objective of improving blood pressure control through a range of physician- or nurse-supervised behavioral and social support interventions. The latter typically include measuring and monitoring blood pressure; providing health education to patients and families about behavioral risk factors for hypertension; recommending changes in diet and physical activity; explaining treatment protocols, health insurance matters, and the importance of adhering to medication regimens; providing help with obtaining transportation to medical appointments; serving as mediators between patients and health care and social service systems; arranging for translation services; and finally, listening to patients and their family members, motivating them, reducing their isolation, and leading self-help groups.
Some of the roles and the successes achieved appear to be similar to those of nurses who have provided educational interventions aimed at hypertension control and suggest an efficient strategy for bringing about enhanced treatment and sustained blood pressure control for targeted racially or ethnically diverse, high-risk populations. Although trained laypeople cannot perform in the same capacity as professional nurses and health educators, with appropriate training and supervision they can successfully
contribute to the care of community members with hypertension (Bosworth et al., 2005).
Community health workers may also play an important role in linking diverse communities to the health care system (HRSA, 2007; IOM, 2003e). The IOM committee that produced the report Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care found that “community health workers offer promise as a community-based resource to increase racial and ethnic minorities’ access to healthcare and to serve as a liaison between healthcare providers and the communities they serve.” Based on this finding, the committee recommended supporting the use of community health workers. “Programs to support the use of community health workers (e.g., as healthcare navigators), especially among medically underserved and racial and ethnic minority populations, should be expanded, evaluated, and replicated” (IOM, 2003e, p. 195).
Federal agencies, including the CDC and the National Heart, Lung, and Blood Institute, recognize the potential contributions of CHWs in the prevention and control of cardiovascular disease, including hypertension. Training manuals for community health workers and lay health educators have been developed and disseminated by these agencies (CDC, 2008a; NHLBI, 2006a,b, 2007, 2008a,b).
CONCLUSIONS
Access to health care and the quality of health care have been areas of serious review and analysis at the Institute of Medicine. In the early 2000s, the IOM produced a series of reports on the general benefits of having health insurance and the adverse health consequences when insurance is lacking (IOM, 2001a, 2002a,b, 2003b,d, 2004). The IOM also published landmark reports on the poor state of quality in the health care delivery system and on a comprehensive vision for how the health care system might be transformed to be safe, effective, patient-centered, timely, efficient, and equitable (IOM, 2001b, 2003c). These reports do not specifically address access to hypertension care or providers. One report, Priority Areas for National Action: Transforming Health Care Quality (IOM, 2003c), however, identified hypertension (with a focus on appropriate management of early disease) as one of 20 priority areas for improvement in health care quality.
The committee, in its review of the evidence related to hypertension control and access to care and providers, found that although lack of health insurance is associated with poorer screening rates, poorer compliance with medication, and poorer blood pressure control; the vast majority of individuals with uncontrolled hypertension in the United States are insured. In fact, the committee found that lack of health insurance or lack of access to
health care accounts for a relatively low proportion of poor awareness or poor control of hypertension. Within the context of the current health care reform debate, the committee supports the recommendations by a former IOM committee for “comprehensive and affordable health care to every person residing in the United States” and that “all public and privately funded insurance include appropriate preventive services as recommended by the U.S. Preventive Services Task Force” (IOM, 2003a). The committee encourages the Division for Heart Disease and Stroke Prevention to be supportive of such efforts but directs the division’s attention to addressing the quality of care for hypertension, especially as it relates to health care providers’ capacity to deliver quality hypertensive care.
Based on the review of the literature, there is strong evidence that physicians are not paying adequate attention to treating and controlling systolic hypertension. The goal of improving the education and training of health care providers in the prevention of cardiovascular disease is central to the Public Health Action Plan to Prevent Heart Disease and Stroke, the DHDSP Strategic Plan, and the National Heart Disease and Stroke Prevention Program (as described in Chapter 3). For example, under the National Heart Disease and Stroke Prevention Program, Virginia, Georgia, and South Carolina have programs to support professional education and training to promote quality health care.1 The committee believes that understanding the reasons behind nonadherence and increasing physician awareness, understanding, and implementation of JNC treatment guidelines are essential to increasing the number of individuals with controlled hypertension, especially systolic hypertension. This is especially salient among the elderly, given the aging of the U.S. population. The committee is concerned that undiagnosed hypertension and treated but uncontrolled hypertension are occurring under “the watchful eye of the health care system” and that physicians are not adhering to JNC guidelines. While a number of studies have documented the problem, little information is available to understand clearly why providers do not adhere to JNC guidelines related to screening and treating or intensifying treatment for mild to moderate systolic hypertension. As one study reported, some physicians were satisfied with blood pressure levels above 140 mm Hg and 90 mm Hg, and some physicians attributed higher risk to elevated diastolic pressure than to elevated systolic pressure, especially in the elderly (Oliveria et al., 2002). Numerous ques-
tions remain regarding whether the lack of adherence is related to a lack of physician agreement with the new treatment guidelines, physician lack of knowledge regarding the guidelines, inertia due to treating at the previous guideline of 160/95 mm Hg, or other barriers.
5.1 The committee recommends that the Division for Heart Disease and Stroke Prevention give high priority to conducting research to better understand the reasons behind poor physician adherence to current JNC guidelines. Once these factors are better understood, strategies should be developed to increase the likelihood that primary providers will screen for and treat hypertension appropriately, especially in elderly patients.
Educating clinicians about the importance of treating and controlling systolic hypertension may be one important strategy but is not expected to be the only one.
Furthermore, high levels of uncontrolled hypertension are indicative of poor-quality care. The committee agrees with the IOM recommendation that identified hypertension (with a special focus on appropriate management of early disease) as one of the top 20 priorities for improvement in health care quality (IOM, 2003c). The evidence reviewed indicates that although physicians screen for blood pressure, screening does not always lead to treatment or to intensified treatment when appropriate.
5.2 The committee recommends that the Division for Heart Disease and Stroke Prevention work with the Joint Commission and the health care quality community to improve provider performance on measures focused on assessing adherence to guidelines for screening for hypertension, the development of a hypertension disease management plan that is consistent with JNC guidelines, and achievement of blood pressure control.
Out-of-pocket cost of medication has been identified in the literature as a significant barrier to patient adherence with hypertension treatment. It is estimated that for every 10 percent increase in cost sharing, overall prescription drug spending decreases by 2-6 percent (Goldman et al., 2007). Goldman and colleagues compared the impact of reducing cost barriers with other interventions designed to improve adherence with medications for chronic conditions and noted that even the most successful interventions designed to increase patient adherence to medication did not result in larger improvements in adherence than reducing the costs, and generally relied on complicated, labor-intensive regimens (Goldman et al., 2007).
The committee finds the evidence convincing that reducing costs of
antihypertensive medication is an important and efficient way to increase medication adherence.
5.3 The committee recommends that the Division for Heart Disease and Stroke Prevention should encourage the Centers for Medicare & Medicaid Services to recommend the elimination or reduction of deductibles for antihypertensive medications among plans participating under Medicare Part D, and work with state Medicaid programs and encourage them to eliminate deductibles and copayment for antihypertensive medications. The committee also recommends that the DHDSP work with the pharmaceutical industry and its trade organizations to standardize and simplify applications for patient assistance programs that provide reduced-cost or free antihypertensive medications for low-income, underinsured, or uninsured individuals.
The committee notes that the DHDSP is also well positioned to educate the private sector that eliminating or reducing the costs of antihypertensive medications is an important and efficient way to increase medication adherence. Through collaborations with the National Forum for Heart Disease and Stroke Prevention (Chapter 3) and cooperative agreements and partnerships with the private sector, the division provides support and guidance to the employer community on hypertension and cardiovascular disease prevention and control. The division’s product, The Business of Heart Disease and Stroke Prevention Toolkit, for example, although extremely informative and useful, does not address benefit or value-based benefit purchasing that can help reduce costs of essential antihypertensive medications. The private sector is already experimenting with reducing the copayments associated with drugs commonly prescribed for diabetes, asthma, and hypertension (Pitney Bowes, Marriott, others). The results of these experiments should be shared broadly with the business community.
5.4 The committee recommends that the Division for Heart Disease and Stroke Prevention collaborate with leaders in the business community to educate them about the impact of reduced patient costs on antihypertensive medication adherence and work with them to encourage employers to leverage their health care purchasing power to advocate for reduced deductibles and copayments for antihypertensive medications in their health insurance benefits packages.
The DHDSP might also consider working with the business community to evaluate and disseminate broadly the research on the health impacts of efforts to reduce financial burdens associated with the treatment of hypertension.
The use of community health workers to support the care of individuals with hypertension has been identified as a promising strategy. Community health workers have contributed to greater medication adherence among individuals with hypertension and have been shown to play an important role in linking diverse communities to the health care system and navigating that system.
5.5 The committee recommends that the Division for Heart Disease and Stroke Prevention work with state partners to leverage opportunities to ensure that existing community health worker programs include a focus on the prevention and control of hypertension. In the absence of such programs, the division should work with state partners to develop programs of community health workers who would be deployed in high-risk communities to help support healthy living strategies that include a focus on hypertension.
REFERENCES
Adams, A. S., S. B. Soumerai, and D. Ross-Degnan. 2001a. The case for a Medicare drug coverage benefit: A critical review of the empirical evidence. Annual Review of Public Health 22:49-61.
———. 2001b. Use of antihypertensive drugs by Medicare enrollees: Does type of drug coverage matter? Health Affairs 20(1):276-286.
Ahluwalia, J. S., S. E. McNagny, and K. J. Rask. 1997. Correlates of controlled hypertension in indigent, inner-city hypertensive patients. Journal of General Internal Medicine 12(1):7-14.
AHRQ (Agency for Healthcare Research and Quality). 2004. Closing the quality gap: A critical analysis of hypertension care strategies. http://www.ahrq.gov/qual/hypertengap.htm (accessed October 28, 2009).
Aldana, S. G. 2001. Financial impact of health promotion programs: A comprehensive review of the literature. American Journal of Health Promotion 15(5):296-320.
AMA (American Medical Association). 2006. Hypertension (HTN): Algorithm for measures calculation—EHRS. http://www.ama-assn.org/ama1/pub/upload/mm/370/htnanalyticnarr 307_7.pdf (accessed February 5, 2010).
American College of Sports Medicine. 2009. ACSM’s worksite health handbook-2nd edition: A guide to building healthy and productive companies. Edited by N. P. Pronk. Champaign, IL: American College of Sports Medicine.
Anis, A. H., D. P. Guh, D. Lacaille, C. A. Marra, A. A. Rashidi, X. Li, and J. M. Esdaile. 2005. When patients have to pay a share of drug costs: Effects on frequency of physician visits, hospital admissions and filling of prescriptions. Canadian Medical Association Journal 173(11):1335-1340.
Artz, M. B., R. S. Hadsall, and S. W. Schondelmeyer. 2002. Impact of generosity level of out-patient prescription drug coverage on prescription drug events and expenditure among older persons. American Journal of Public Health 92(8):1257-1263.
Austvoll-Dahlgren, A., M. Aaserud, G. Vist, C. Ramsay, A. D. Oxman, H. Sturm, J. P. Kosters, and A. Vernby. 2008. Pharmaceutical policies: Effects of cap and co-payment on rational drug use. Cochrane Database of Systematic Reviews (1).
Ayanian, J. Z., J. S. Weissman, E. C. Schneider, J. A. Ginsburg, and A. M. Zaslavsky. 2000. Unmet health needs of uninsured adults in the United States. Journal of the American Medical Association 284(16):2061-2069.
Berlowitz, D. R., A. S. Ash, E. C. Hickey, R. H. Friedman, M. Glickman, B. Kader, and M. A. Moskowitz. 1998. Inadequate management of blood pressure in a hypertensive population. New England Journal of Medicine 339(27):1957-1963.
Blais, L., J. M. Boucher, J. Couture, E. Rahme, and J. LeLorier. 2001. Impact of a cost-sharing drug insurance plan on drug utilization among older people. Journal of the American Geriatrics Society 49(4):410-414.
Blustein, J. 2000. Drug coverage and drug purchases by Medicare beneficiaries with hypertension. Health Affairs 19(2):219-230.
Bokhour, B. G., D. R. Berlowitz, J. A. Long, and N. R. Kressin. 2006. How do providers assess antihypertensive medication adherence in medical encounters? Journal of General Internal Medicine 21(6):577-583.
Bosworth, H. B., M. K. Olsen, P. Gentry, M. Orr, T. Dudley, F. McCant, and E. Z. Oddone. 2005. Nurse administered telephone intervention for blood pressure control: A patient-tailored multifactorial intervention. Patient Education and Counseling 57(1):5-14.
Bray, G. A., W. M. Vollmer, F. M. Sacks, E. Obarzanek, L. P. Svetkey, and L. J. Appel. 2004. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: Results of the DASH-sodium trial. American Journal of Cardiology 94(2):222-227.
Brook, R. H., J. E. Ware, W. H. Rogers, E. B. Keeler, A. R. Davies, C. A. Donald, G. A. Goldberg, K. N. Lohr, P. C. Masthay, and J. P. Newhouse. 1983. Does free care improve adults health—results from a randomized controlled trial. New England Journal of Medicine 309(23):1426-1434.
Brownstein, J. N., L. R. Bone, C. R. Dennison, M. N. Hill, M. T. Kim, and D. M. Levine. 2005. Community health workers as interventionists in the prevention and control of heart disease and stroke. American Journal of Preventive Medicine 29(5 Suppl 1):128-133.
Brownstein, J. N., F. M. Chowdhury, S. L. Norris, T. Horsley, L. Jack Jr, X. Zhang, and D. Satterfield. 2007. Effectiveness of community health workers in the care of people with hypertension. American Journal of Preventive Medicine 32(5):435-447.
Capozza, K. 2008. First-dollar coverage for chronic disease care: Can it save money and improve patient outcomes? Berkeley, CA: UC Berkeley Labor Center.
CDC (Centers for Disease Control and Prevention). 1994. Health objectives for the nation: Adults taking action to control their blood pressure—United States, 1990. Morbidity and Mortality Weekly Report 43(28):509-511.
———. 2008a. The community health worker’s sourcebook: A training manual for preventing heart disease and stroke. Atlanta, GA: Division for Heart Disease and Stroke Prevention.
———. 2008b. Successful business strategies to prevent heart disease and stroke. Atlanta, GA: Centers for Disease Control and Prevention.
———. 2009. The National Business Group on Health. http://www.cdc.gov/Partners/Business/NBGH.html (accessed November 4, 2009).
CDC and NBGH (National Business Group on Health). 2006. A Purchaser’s Guide to Clinical Preventive Services: Moving Science into Coverage. Washington, DC: National Business Group on Health.
Chernew, M. E., A. B. Rosen, and A. M. Fendrick. 2007. Value-based insurance design. Health Affairs 26(2):w195-w203.
Chiong, J. R. 2008. Controlling hypertension from a public health perspective. International Journal of Cardiology 127(2):151-156.
Chockalingam, A., M. Bacher, N. Campbell, H. Cutler, A. Drover, R. Feldman, G. Fodor, J. Irvine, V. Ramsden, R. Thivierge, and G. Tremblay. 1998. Adherence to management of high blood pressure: Recommendations of the Canadian coalition for high blood pressure prevention and control. Canadian Journal of Public Health (Revue Canadienne de Sante Publique) 89(5):I5-I11.
Clark, L. T. 1991. Improving compliance and increasing control of hypertension: Needs of special hypertensive populations. American Heart Journal 121(2 Pt 2):664-669.
Col, N., J. E. Fanale, and P. Kronholm. 1990. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Archives of Internal Medicine 150(4):841-845.
Cox, E. R., C. Jernigan, S. J. Coons, and J. L. Draugalis. 2001. Medicare beneficiaries’ management of capped prescription benefits. Medical Care 39(3):296-301.
Eddy, D. M., L. G. Pawlson, D. Schaaf, B. Peskin, A. Shcheprov, J. Dziuba, J. Bowman, and B. Eng. 2008. The potential effects of HEDIS performance measures on the quality of care. Health Affairs 27(5):1429-1441.
Ekpo, E. B., I. U. Shah, M. U. Fernando, and A. D. White. 1993. Isolated systolic hypertension in the elderly: Survey of practitioners’ attitude and management. Gerontology 39(4):207-214.
Elliott, W. J. 2003. Optimizing medication adherence in older persons with hypertension. International Urology and Nephrology 35(4):557-562.
Fairman, K. A., B. R. Motheral, and R. R. Henderson. 2003. Retrospective, long-term follow-up study of the effect of a three-tier prescription drug copayment system on pharmaceutical and other medical utilization and costs. Clinical Therapeutics 25(12):3147-3161; discussion 3144-3146.
Fihn, S. D., and J. B. Wicher. 1988. Withdrawing routine outpatient medical services: Effects on access and health. Journal of General Internal Medicine 3(4):356-362.
Franklin, S. S., M. J. Jacobs, N. D. Wong, G. J. L’Italien, and P. Lapuerta. 2001. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: Analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 37(3):869-874.
Gallup, G., and H. E. Cotugno. 1986. Preferences and practices of Americans and their physicians in antihypertensive therapy. American Journal of Medicine 81(6C):20-24.
Goetzel, R. Z., and R. J. Ozminkowski. 2008. The health and cost benefits of work site health-promotion programs. Annual Review of Public Health 29:303-323.
Goetzel, R. Z., D. Shechter, R. J. Ozminkowski, P. F. Marmet, M. J. Tabrizi, and E. C. Roemer. 2007. Promising practices in employer health and productivity management efforts: Findings from a benchmarking study. Journal of Occupational and Environmental Medicine 49(2):111-130.
Goldman, D. P., G. F. Joyce, J. J. Escarce, J. E. Pace, M. D. Solomon, M. Laouri, P. B. Landsman, and S. M. Teutsch. 2004. Pharmacy benefits and the use of drugs by the chronically ill. Journal of the American Medical Association 291(19):2344-2350.
Goldman, D. P., G. F. Joyce, and Y. Zheng. 2007. Prescription drug cost sharing: Associations with medication and medical utilization and spending and health. Journal of the American Medical Association 298(1):61-69.
Gu, Q., V. L. Burt, R. Paulose-Ram, S. Yoon, and R. F. Gillum. 2008. High blood pressure and cardiovascular disease mortality risk among U.S. adults: The Third National Health and Nutrition Examination Survey Mortality Follow-up study. Annals of Epidemiology 18(4):302-309.
Guide to Community Preventive Services. 2009. Assessment of health risks with feedback to change employees’ health. www.thecommunityguide.org/worksite/ahrf.html (accessed November 4, 2009).
Halm, J., and E. Amoako. 2008. Physical activity recommendation for hypertension management: Does healthcare provider advice make a difference? Ethnicity and Disease 18(3):278-282.
Harmon, G., J. Lefante, and M. Krousel-Wood. 2006. Overcoming barriers: The role of providers in improving patient adhereence to antihypertensive medications. Current Opinion in Cardiology 21(4):310-315.
Harris, B. L., A. Stergachis, and L. D. Ried. 1990. The effect of drug co-payments on utilization and cost of pharmaceuticals in a health maintenance organization. Medical Care 28(10):907-917.
He, J., P. Muntner, J. Chen, E. J. Roccella, R. H. Streiffer, and P. K. Whelton. 2002. Factors associated with hypertension control in the general population of the United States. Archives of Internal Medicine 162(9):1051-1058.
HRSA (Health Resources and Services Administration). 2007. Community health worker national workforce study: U.S. Department of Health and Human Services.
Hsu, J., M. Price, J. Huang, R. Brand, V. Fung, R. Hui, B. Fireman, J. P. Newhouse, and J. V. Selby. 2006. Unintended consequences of caps on Medicare drug benefits. New England Journal of Medicine 354(22):2349-2359.
Huskamp, H. A., P. A. Deverka, A. M. Epstein, R. S. Epstein, K. A. McGuigan, and R. G. Frank. 2003. The effect of incentive-based formularies on prescription-drug utilization and spending. New England Journal of Medicine 349(23):2224-2232.
Hyman, D. J., and V. N. Pavlik. 2000. Self-reported hypertension treatment practices among primary care physicians—blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Archives of Internal Medicine 160(15):2281-2286.
———. 2001. Characteristics of patients with uncontrolled hypertension in the United States. [see comment] [erratum appears in 2002 New England Journal of Medicine 346(7):544]. New England Journal of Medicine 345(7):479-486.
Hyman, D. J., V. N. Pavlik, and C. Vallbona. 2000. Physician role in lack of awareness and control of hypertension. Journal of Clinical Hypertension (Greenwich) 2(5):324-330.
IOM (Institute of Medicine). 2000. To err is human: Building a safer health system. Washington, DC: National Academy Press.
———. 2001a. Coverage matters: Insurance and health care. Washington, DC: National Academy Press.
———. 2001b. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2002a. Care without coverage: Too little, too late. Washington, DC: The National Academies Press.
———. 2002b. Health insurance is a family matter. Washington, DC: The National Academies Press.
———. 2003a. The future of public health in the 21st century. Washington, DC: The National Academies Press.
———. 2003b. Hidden costs, value lost: Uninsurance in America. Washington, DC: The National Academies Press.
———. 2003c. Priority areas for national action: Transforming health care quality. Washington, DC: The National Academies Press.
———. 2003d. A shared destiny: Community effects of uninsurance. Washington, DC: The National Academies Press.
———. 2003e. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington DC: The National Academies Press.
———. 2004. Insuring America’s health: Principles and recommendations. Washington, DC: The National Academies Press.
Izzo, J. L., Jr., D. Levy, and H. R. Black. 2000. Clinical advisory statement. Importance of systolic blood pressure in older Americans. Hypertension 35(5):1021-1024.
Johnson, R. E., M. J. Goodman, M. C. Hornbrook, and M. B. Eldredge. 1997a. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Medical Care 35(11):1119-1131.
———. 1997b. The impact of increasing patient prescription drug cost sharing on therapeutic classes of drugs received and on the health status of elderly HMO members. Health Services Research 32(1):103-122.
Kamal-Bahl, S., and B. Briesacher. 2004. How do incentive-based formularies influence drug selection and spending for hypertension? Health Affairs 23(1):227-236.
Keeler, E. B., R. H. Brook, G. A. Goldberg, C. J. Kamberg, and J. P. Newhouse. 1985. How free care reduced hypertension in the Health Insurance Experiment. Journal of the American Medical Association 254(14):1926-1931.
Keeler, E. B., E. M. Sloss, R. H. Brook, B. H. Operskalski, G. A. Goldberg, and J. P. Newhouse. 1987. Effects of cost sharing on physiological health, health practices, and worry. Health Services Research 22(3):279-306.
Koffman, M., M. Molloy, L. Agin, and L. Sokler. 2005. Reducing the risk of heart disease and stroke: A six-step guide for employers. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services.
Kokkinos, P. F., P. Narayan, J. A. Colleran, A. Pittaras, A. Notargiacomo, D. Reda, and V. Papademetriou. 1995. Effects of regular exercise on blood-pressure and left-ventricular hypertrophy in African-American men with severe hypertension. New England Journal of Medicine 333(22):1462-1467.
Kotchen, J. M., B. Shakoor-Abdullah, W. E. Walker, T. H. Chelius, R. G. Hoffmann, and T. A. Kotchen. 1998. Hypertension control and access to medical care in the inner city. American Journal of Public Health 88(11):1696-1699.
Krousel-Wood, M., A. Hyre, P. Muntner, and D. Morisky. 2005. Methods to improve medication adherence in patients with hypertension: Current status and future directions. Current Opinion in Cardiology 20(4):296-300.
Landsman, P. B., W. Yu, X. Liu, S. M. Teutsch, and M. L. Berger. 2005. Impact of 3-tier pharmacy benefit design and increased consumer cost-sharing on drug utilization. American Journal of Managed Care 11(10):621-628.
Lexchin, J., and P. Grootendorst. 2004. Effects of prescription drug user fees on drug and health services use and on health status in vulnerable populations: A systematic review of the evidence. International Journal of Health Services 34(1):101-122.
Lloyd-Jones, D. M., J. C. Evans, M. G. Larson, C. J. O’Donnell, E. J. Roccella, and D. Levy. 2000. Differential control of systolic and diastolic blood pressure: Factors associated with lack of blood pressure control in the community. Hypertension 36(4):594-599.
Lloyd-Jones, D. M., J. C. Evans, M. G. Larson, and D. Levy. 2002. Treatment and control of hypertension in the community: A prospective analysis. Hypertension 40(5):640-646.
Lohr, K. N., R. H. Brook, C. J. Kamberg, G. A. Goldberg, A. Leibowitz, J. Keesey, D. Reboussin, and J. P. Newhouse. 1986. Use of medical care in the Rand Health Insurance Experiment. Diagnosis- and service-specific analyses in a randomized controlled trial. Medical Care 24(9 Suppl):S1-S87.
Lopes, A. A., S. A. James, F. K. Port, A. O. Ojo, L. Y. Agodoa, and K. A. Jamerson. 2003. Meeting the challenge to improve the treatment of hypertension in blacks. Journal of Clinical Hypertension (Greenwich) 5(6):393-401.
Lurie, N., N. B. Ward, M. F. Shapiro, and R. H. Brook. 1984. Termination from Medi-Cal—does it affect health? New England Journal of Medicine 311(7):480-484.
Lurie, N., N. B. Ward, M. F. Shapiro, C. Gallego, R. Vaghaiwalla, and R. H. Brook. 1986. Termination of Medi-Cal benefits. A follow-up study one year later. New England Journal of Medicine 314(19):1266-1268.
Maciosek, M. V., A. B. Coffield, N. M. Edwards, T. J. Flottemesch, M. J. Goodman, and L. I. Solberg. 2006. Priorities among effective clinical preventive services: Results of a systematic review and analysis. American Journal of Preventive Medicine 31(1):52-61.
Maronde, R. F., L. S. Chan, F. J. Larsen, L. R. Strandberg, M. F. Laventurier, and S. R. Sullivan. 1989. Underutilization of antihypertensive drugs and associated hospitalization. Medical Care 27(12):1159-1166.
McCombs, J. S., M. B. Nichol, C. M. Newman, and D. A. Sclar. 1994. The costs of interrupting antihypertensive drug therapy in a Medicaid population. Medical Care 32(3):214-226.
Mellen, P. B., S. L. Palla, D. C. Goff Jr., and D. E. Bonds. 2004. Prevalence of nutrition and exercise counseling for patients with hypertension. Journal of General Internal Medicine 19(9):917-924.
Mojtabai, R., and M. Olfson. 2003. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Affairs 22(4):220-229.
Motheral, B., and K. A. Fairman. 2001. Effect of a three-tier prescription copay on pharmaceutical and other medical utilization. Medical Care 39(12):1293-1304.
Motheral, B. R., and R. Henderson. 1999a. The effect of a closed formulary on prescription drug use and costs. Inquiry-the Journal of Health Care Organization Provision and Financing 36(4):481-491.
———. 1999b. The effect of a copay increase on pharmaceutical utilization, expenditures, and treatment continuation. American Journal of Managed Care 5(11):1383-1394.
Moy, E., B. A. Bartman, and M. R. Weir. 1995. Access to hypertensive care. Effects of income, insurance, and source of care. Archives of Internal Medicine 155(14):1497-1502.
Nair, K. V., P. Wolfe, R. J. Valuck, M. M. McCollum, J. M. Ganther, and S. J. Lewis. 2003. Effects of a 3-tier pharmacy benefit design on the prescription purchasing behavior of individuals with chronic disease. Journal of Managed Care Pharmacy 9(2):123-133.
NCQA (National Committee for Quality Assurance). 2009. The state of health care quality. Washington, DC: National Committee for Quality Assurance.
NHLBI (National Heart, Lung, and Blood Institute). 2006a. Honoring the gift of heart health: A heart health educator’s manual for Alaska Natives. Bethesda, MD: U.S. Department of Health and Human Services.
NHLBI. 2006b. Honoring the gift of heart health: A heart health educator’s manual for American Indians. Bethesda, MD: U.S. Department of Health and Human Services.
NHLBI. 2007. With every heartbeat is life: A community health worker’s manual for African Americans. Bethesda, MD: U.S. Department of Health and Human Services.
NHLBI. 2008a. Healthy heart, healthy family: A community health worker’s manual for the Filipino community. Bethesda, MD: U.S. Department of Health and Human Services.
NHLBI. 2008b. Your heart, your life: A community health worker’s manual for the Hispanic community. Bethesda, MD: U.S. Department of Health and Human Services.
Okonofua, E. C., K. N. Simpson, A. Jesri, S. U. Rehman, V. L. Durkalski, and B. M. Egan. 2006. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension 47(3):345-351.
Oliveria, S. A., P. Lapuerta, B. D. McCarthy, G. J. L’Italien, D. R. Berlowitz, and S. M. Asch. 2002. Physician-related barriers to the effective management of uncontrolled hypertension. Archives of Internal Medicine 162(4):413-420.
Partnership for Prevention. 2001. Healthy workforce 2010: An essential health promotion sourcebook for employers, large and small. Washington, DC: Partnership for Prevention.
———. 2006. Priorities for America’s health: Capitalizing on life-saving, cost-effective preventive services. Washington, DC: Partnership for Prevention.
Pavlik, V. N., D. J. Hyman, C. Vallbona, C. Toronjo, and K. Louis. 1997. Hypertension awareness and control in an inner-city African-American sample. Journal of Human Hypertension 11(5):277-283.
Piette, J. D., M. Heisler, and T. H. Wagner. 2004. Cost-related medication underuse among chronically ill adults: The treatments people forgo, how often, and who is at risk. American Journal of Public Health 94(10):1782-1787.
Poirier, S., and J. LeLorier. 1998. The effect of a $2 co-payment on prescription refill rates of Quebec elderly and its relationship to socioeconomic status. Canadian Pharmacy Journal 131(1):30-34.
RAND. 2006. The first national report card on quality of health care in America. Santa Monica, CA: RAND Corporation.
Reeder, C. E., and A. A. Nelson. 1985. The differential impact of copayment on drug use in a Medicaid population. Inquiry 22(4):396-403.
Rogowski, J., L. A. Lillard, and R. Kington. 1997. The financial burden of prescription drug use among elderly persons. Gerontologist 37(4):475-482.
Schneeweiss, S., S. B. Soumerai, R. J. Glynn, M. Maclure, C. Dormuth, and A. M. Walker. 2002a. Impact of reference-based pricing for angiotensin-converting enzyme inhibitors on drug utilization. Canadian Medical Association Journal 166(6):737-745.
Schneeweiss, S., A. M. Walker, R. J. Glynn, M. Maclure, C. Dormuth, and S. B. Soumerai. 2002b. Outcomes of reference pricing for angiotensin-converting-enzyme inhibitors. New England Journal of Medicine 346(11):822-829.
Schulz, R. M., E. W. Lingle, S. J. Chubon, and M. A. Coster-Schulz. 1995. Drug use behavior under the constraints of a Medicaid prescription cap. Clinical Therapeutics 17(2):330-340.
Shea, S., D. Misra, M. H. Ehrlich, L. Field, and C. K. Francis. 1992a. Correlates of nonadherence to hypertension treatment in an inner-city minority population. American Journal of Public Health 82(12):1607-1612.
———. 1992b. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. New England Journal of Medicine 327(11):776-781.
SHEP Cooperative Research Group. 1991. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP cooperative research group. Journal of the American Medical Association 265(24):3255-3264.
Shrank, W. H., T. Hoang, S. L. Ettner, P. A. Glassman, K. Nair, D. DeLapp, J. Dirstine, J. Avorn, and S. M. Asch. 2006. The implications of choice: Prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Archives of Internal Medicine 166(3):332-337.
Shulman, N. B., B. Martinez, D. Brogan, A. A. Carr, and C. G. Miles. 1986. Financial cost as an obstacle to hypertension therapy. American Journal of Public Health 76(9):1105-1108.
Solomon, M. D., D. P. Goldman, G. F. Joyce, and J. J. Escarce. 2009. Cost sharing and the initiation of drug therapy for the chronically ill. Archives of Internal Medicine 169(8):740-748; discussion 748-749.
Soumerai, S. B., D. Ross-Degnan, J. Avorn, T. McLaughlin, and I. Choodnovskiy. 1991. Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. New England Journal of Medicine 325(15):1072-1077.
Soumerai, S. B., T. J. Mclaughlin, D. Rossdegnan, C. S. Casteris, and P. Bollini. 1994. Effects of limiting Medicaid drug-reimbursement benefits on the use of psychotropic agents and acute mental-health-services by patients with schizophrenia. New England Journal of Medicine 331(10):650-655.
Steinman, M. A., L. P. Sands, and K. E. Covinsky. 2001. Self-restriction of medications due to cost in seniors without prescription coverage. Journal of General Internal Medicine 16(12):793-799.
Steinman, M. A., M. A. Fischer, M. G. Shlipak, H. B. Bosworth, E. Z. Oddone, B. B. Hoffman, and M. K. Goldstein. 2004. Clinician awareness of adherence to hypertension guidelines. American Journal of Medicine 117(10):747-754.
Stockwell, D. H., S. Madhavan, H. Cohen, G. Gibson, and M. H. Alderman. 1994. The determinants of hypertension awareness, treatment, and control in an insured population. American Journal of Public Health 84(11):1768-1774.
Stuart, B., and J. Grana. 1998. Ability to pay and the decision to medicate. Medical Care 36(2):202-211.
Svetkey, L. P., D. Simons-Morton, W. M. Vollmer, L. J. Appel, P. R. Conlin, D. H. Ryan, J. Ard, and B. M. Kennedy. 1999. Effects of dietary patterns on blood pressure: Subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Archives of Internal Medicine 159(3):285-293.
Taira, D. A., K. S. Wong, F. Frech-Tamas, and R. S. Chung. 2006. Copayment level and compliance with antihypertensive medication: Analysis and policy implications for managed care. American Journal of Managed Care 12(11):678-683.
Tamblyn, R., R. Laprise, J. A. Hanley, M. Abrahamowicz, S. Scott, N. Mayo, J. Hurley, R. Grad, E. Latimer, R. Perreault, P. McLeod, A. Huang, P. Larochelle, and L. Mallet. 2001. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. Journal of the American Medical Association 285(4):421-429.
Tseng, C. W., R. H. Brook, E. Keeler, W. N. Steers, and C. M. Mangione. 2004. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. Journal of the American Medical Association 292(8):952-960.
Vollmer, W. M., L. P. Svetkey, L. J. Appel, E. Obarzanek, P. Reams, B. Kennedy, K. Aicher, J. Charleston, P. R. Conlin, M. Evans, D. Harsha, and S. Hertert. 1998. Recruitment and retention of minority participants in the DASH controlled feeding trial. DASH Collaborative Research Group. Dietary Approaches to Stop Hypertension. Ethnicity and Disease 8(2):198-208.
Weissman, J. S., C. Gatsonis, and A. M. Epstein. 1992. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. Journal of the American Medical Association 268(17):2388-2394.
Wilson, J., K. Axelsen, and S. Tang. 2005. Medicaid prescription drug access restrictions: Exploring the effect on patient persistence with hypertension medications. American Journal of Managed Care 11(Spec No):SP27-SP34.
Witmer, A., S. D. Seifer, L. Finocchio, J. Leslie, and E. H. O’Neil. 1995. Community health workers: Integral members of the health care work force. American Journal of Public Health 85(8 Pt 1):1055-1058.
Woolhandler, S., and D. U. Himmelstein. 1988. Reverse targeting of preventive care due to lack of health insurance. Journal of the American Medical Association 259(19):2872-2874.
Wright, J. T., Jr., G. Bakris, T. Greene, L. Y. Agodoa, L. J. Appel, J. Charleston, D. Cheek, J. G. Douglas-Baltimore, J. Gassman, R. Glassock, L. Hebert, K. Jamerson, J. Lewis, R. A. Phillips, R. D. Toto, J. P. Middleton, S., and G. Rostand, for the African American Study of Kidney Disease and Hypertension Study Group. 2002. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: Results from the AASK trial. [see comment] [erratum appears in 2006 Journal of the American Medical Association 295(23):2726]. Journal of the American Medical Association 288(19):2421-2431.