6
Patients, Clinical Decisions, and Health Information Management in the Information Age
INTRODUCTION
Until recently, health care was characterized by an information asymmetry in which physicians served as the dominant source of medical information for patients. The Internet has rapidly transformed the health information landscape—initially opening up myriad resources, targeted to the general public, for health-related guidance and information, and then, with the emergence of Web 2.0, enabling the public to easily create and share health-related content online. Patients have responded to this shift by increasingly seeking health-related information outside of the care environment (Fox and Jones, 2009) and creating and contributing to a wide variety of social networks and health websites (Sarasohn-Kahn, 2008). Perhaps the most important opportunity that comes with greater information availability is the emergence of a culture that recognizes and supports the unique contributions of both patients and providers to care decisions and health management.
Such a shift moves patient-centered care beyond a focus on “information, communication, and education of patients” (IOM, 2001) to a system in which patients are engaged as full partners in their care and disease management. Greater engagement of patients is imperative, with more than 90 million Americans now being afflicted with one or more chronic conditions. Chronic disease management, for example, requires continuous monitoring and evaluation of disease progression and treatment effects, coordination of care across specialists and organizations, and patient adherence to long-term treatment regimens. Another tool for achieving patient
engagement is through electronic health records (EHRs) and patient portals, which are beginning to be adopted nationwide as novel ways for providers to partner with patients by providing information and support for care management.
The papers in this chapter review lessons learned from efforts to support the active engagement of patients in their healthcare decisions and health management and identify priorities and strategies for progress. In the first paper, George D. Lundberg of Cancer Commons provides an overview of the Internet revolution, which has democratized information. He reviews opportunities to improve the information available to or accessed by patients, as well as to use the Internet as a platform to engage patients in real-time, rapid learning communities.
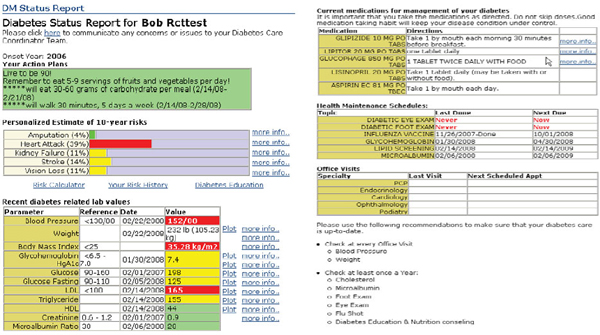
In the second paper, Paul C. Tang of the Palo Alto Medical Foundation demonstrates the critical importance of engaging patients in their own care to close gaps in health outcomes and system performance. He reviews how information technology applications such as patient dashboards has helped make patients part of the health team, fostered patient and provider collaboration in tracking progress toward health goals, and provided tools to transform data into information from which patients can learn.
Dorianne C. Miller, formerly of the University of Chicago Medical Center, draws attention to initiatives that are helping to extend health care to settings outside of the clinical encounter. Shifts in patient population demographics and in the focus and capacity of health systems are driving the creation of applications to ensure that patients receive care (e.g., patient health records and portals, e-visits) and support beyond the traditional care environment. In addition to highlighting opportunities, she discusses barriers to expanded use of such technologies, such as social acceptability, lack of Internet access, and clinician reimbursement.
PUBLIC AND PATIENT INFORMATION ACCESS AND USE AS A CORE CARE COMPONENT
George D. Lundberg, M.D.
Cancer Commons
Change is everywhere and affects everyone. People handle change in three different ways:
- Fear it; fight it; not recognize that change is inevitable; lose.
- Fail to recognize the need for and reality of change and be swept away by it.
- Seek it; recognize it; harness it; guide it; and eventually win with it.
The future is very difficult to predict; in fact, the only certain way to predict the future is to create it. Change for the sake of change may not be necessary or desirable. Too often, however, the need for change is not evident until it is too late.
The Democratization of Information
Three individuals merit mention when one is discussing information as a core component of care: the late Archie Cochrane, for his demand that evidence underpin clinical decisions; the late Dr. Tom Ferguson, the original e-patient, who was in many ways the father of participatory medicine and use of the Internet to empower patients; and Don Berwick, who has been a major leader in patient-centered care.
Most health care is self-care. In some ways, basic self-screening for health concerns is a routine part of everyday life; however, people should be better supported in taking charge of their health. Moreover, all medical care is personal. The credo of the Lundberg Institute states: “one patient; one physician; one moment; one decision.”1 Health decisions should be shared by the patient and physician, be informed by the best available evidence, and include consideration of cost (regardless of who—the patient, the insurance company, the government, the provider [charity care]—pays the bill) and of whether there is a lower-cost alternative with equivalent safety and effectiveness. That is economic informed consent. In a nonemergency, noncritical care situation in which the patient has control of his/her mental faculties, the patient and physician should know the cost before making an informed decision.
The Internet changed everything, much as electricity did. Health information began appearing on the Internet in the mid-1990s. Physicians On-Line began in 1994, Medscape in May 1995, and the American Medical Association (AMA) website with the Journal of the American Medical Association (JAMA) and the Archives Journals in August 1995. In 1995, e-Medicine began. About that time, GlaxoWellcome provided a $250,000 grant to AMA to start an HIV/AIDS online information base with JAMA. Initially, this resource was aimed at sophisticated HIV researchers and physicians, but the actual audience was HIV patients and their families, loved ones, and caregivers. This illustrates the principle that more than any other medium, the Internet democratizes information. The reader really does choose.
____________
1 See http://www.lundberginstitute.org (accessed October 14, 2010).
Caveat Lector
Consumer choice, however, raises concerns about misinformation. In 1997, an editorial in JAMA addressed this issue (Silberg et al., 1997). Titled “Assessing, Controlling, and Assuring the Quality of Medical Information on the Internet. Caveat Lector et Viewor—Let the Reader and the Viewer Beware,” the article outlines key questions that readers should ask about any serious information on health and medicine posted on the web:
- Who wrote this?
- Where does that person work?
- If the information comes from elsewhere, what is its attribution; when was it published?
- If it was updated, when?
- Who owns the site where the article is published, and what is the funding source?
This editorial is frequently cited, and these criteria have had some influence as a result of being widely quoted and applied in practice by many publishers, editors, and authors. However, these caveats are routinely ignored by readers who consume whatever information search engines lead them to. Readers seek out trusted brands and return to sites they perceive to have helped them; thus, it is an information provider’s responsibility not to mislead the reader.
Although many dismiss the Internet because so much of the information is suspect or worthless, the same is true of most media. The web is simply another medium, albeit a very powerful one.
Ensuring Open Access to Quality Information
Patients and consumers, like physicians, now receive most of their new medical and health information from the Internet (Fox and Jones, 2009). In many cases, patients receive more health information from the Internet than from their own physicians (Gualtieri, 2009). Typically, instead of bringing their printouts to their physician’s office, patients log on after seeing their physician to check on findings, diagnoses, and diagnostic tests performed and drugs prescribed (Diaz et al., 2002). These searches likely start with the few details the patient remembers from the provider visit. Usually, the patient starts with a general search engine, most likely Google, Yahoo, or Bing. Given this common practice, the information age presents an enormous opportunity for savvy physicians to deliver an “information prescription” to patients who are motivated to learn and have access to the world’s greatest library at their fingertips.
An informal survey of which medical/health websites provide the most consumer-friendly and useful information on cancer identified the following as key resources for patients:
- www.cancer.gov (National Cancer Institute website)
- www.pubmed.gov (Medline Plus)
- www.cancer.org (American Cancer Society website)
- A tie between www.webmd.com, www.mayoclinic.com, and www.wikipedia.com
- www.nccn.org (National Comprehensive Cancer Network website)
- www.intelihealth.com (Harvard Medical School and Aetna website)
- www.ACOR.org (Association of Cancer Online Resources website)
- www.cancer.net (American Society of Clinical Oncology website)
Additional suggestions for new websites that are interesting and useful for consumers include www.keas.com and www.medhelp.com; additionally, although intended for medical professionals, www.medscape.com, www.medpagetoday.com, and www.emedicine.com are all very useful for patients. All of these sources are open access—available to anyone with access to the Internet, free of charge, and usually without user registration requirements.
The deliberate practice of limiting the flow of medical information on the part of most of the medical publishing industry compromises the public interest. Although most new medical information in the United States emanates from tax-supported research, such as that funded by the National Institutes of Health, the authors of papers reporting the results of such studies still overwhelmingly choose to submit the papers to journals owned by those that are, or function as, for-profit publishers. The taxpayers, who own the information by virtue of having paid for it, are therefore impeded by these publishers from using the data to treat (if a physician) or be treated (if a patient). As much as 90 percent of the medical research literature is still provided by such “closed” sources.
The case for the unfairness of this situation has been made since about 1999 and has led to great progress in creating more open-access sources. Leaders in this field include www.pubmedcentral.gov, www.biomedcentral.com, the Public Library of Science/Medicine, the Medscape Journal of Medicine (1999–2009), Medscape’s Publishers Circle, Lund University Library’s Directory of Open Access Journals, the Cochrane Collaboration (easily available through MedPage Today), and the Effective Care Program of the Agency for Healthcare Research and Quality.
Many believe that the single greatest barrier to successful public access to and use of medical information as a core care component is the general lack of reliable information sources in the traditional public media
(e.g., newspapers, magazines, radio, and television—all major information sources for patients) (Schwitzer et al., 2005). Gary Schwitzer, a professor of journalism at the University of Minnesota, publishes www.healthnewsreview.org, which weekly rates the handling of major health-related news stories. He uses ten criteria to assess the quality of these reports. Did the news report:
- establish the availability of the treatment, test, product or procedure;
- address costs;
- avoid disease-related fear mongering;
- evaluate the quality of evidence;
- quantify potential harm;
- establish the true novelty of the treatment, test, product, or procedure;
- quantify potential benefits;
- rely solely or largely on a press release;
- use independent sources and report conflicts of interest; and
- compare the new approach with existing alternatives?
Major medical and health reports emerge every day, but few receive passing grades in the Schwitzer reviews. Network television reports are consistently the worst, and the situation is not improving. Many major newspapers and local television stations no longer even have health reporters on their staffs, relying on general beat reporters to cover health.
The Next Phase: Open-Access, Real-Time Information for Personalized Health
The poet Alexander Pope wrote, “The proper study of mankind is man.” In health, one might say, “The proper study of me is me.” While 99.9 percent of all DNA is shared, the remaining 0.1 percent make all the difference. With some diseases, “the proper study of my disease is my disease.” This statement is particularly important when one is considering the molecular genomics of cancer because one person’s cancer may actually be unique. This fact constitutes the basis for personalized molecular oncology and pharmacogenomics. Increased recognition of the uniqueness of individuals and individual diseases has led to a conflict between two perspectives on information needs and approaches to evidence development.
On the one hand is Archie Cochrane’s basic tenet: the gold standard for evidence development is a large randomized controlled trial (RCT) that has sufficient statistical power to be meaningful. If there are conflicts among clinical trial results, those conflicts are settled through meta-analysis
(Juni et al., 1999). RCTs work well when the populations to be studied are molecularly and genomically homogeneous, allowing standardized interventions to be tested.
On the other hand, an important movement to a more personalized approach to medicine is taking place. This approach seeks to address the needs of patients who fall outside the traditional groups that participate in RCTs—the outliers and those whose diseases are molecularly and genomically heterogeneous (West et al., 2006).
For many decades, case studies have been out of vogue in medical journals, but they may now be returning to favor. Some time ago, JAMA published the hierarchy of evidence based on quality: RCTs are at the top, while Level II-3 includes “dramatic results in uncontrolled experiments,” such as the results of the introduction of penicillin therapy. During the JAMA centennial, 68 of the best articles over 100 years of the journal were selected and published as “landmark articles.” Notably, 5 were case reports: in 1933, Graham’s first removal of an entire lung for bronchial carcinoma; in 1939, Gross’s report of the successful ligation of a patient with ductus arteriosus; also in 1939, Levine’s discovery of the Rh factor; in 1956, Merrill and Murray’s homotransplantation of a human kidney between two homozygous twins; and in 1956, DeBakey’s first aorto-coronary bypass with a saphenous vein graft. These were all crucial events in medicine, and all were case reports.
Cancer as a Case Study
Each year, 3.5 million Americans are diagnosed with some form of cancer. Skin cancer is diagnosed in 2 million and other forms of the disease, including melanoma, in 1.5 million. During 1969–1971, President Nixon declared a war on cancer, initiating a massive outlay of research funding and effort that continues today. The result has been tremendous advances in cancer science and some therapeutic progress, primarily against childhood cancers, leukemia, lymphoma, and germ cell tumors. Extensive anti-tobacco efforts have prevented many cancers. And the movement toward palliative and hospice care continues to grow. However, between 500,000 and 600,000 Americans still die of cancer each year, and progress on significantly reducing that number has been distressingly slow.
The slow progress of the translation of research into positive outcomes in the treatment of cancer is disappointing. The multiyear delays from observation to successful implementation are in part a product of a system of excessive bureaucracy; old-fashioned communication methods; and an academic and publishing establishment that sometimes appears to care more about preserving its ancient institutions, procedures, and self-interest than about defeating cancer.
Two concurrent revolutions in medicine and technology are currently under way:
• The genomics and molecular medicine revolution—Advances in understanding of cancer biology are leading to the rapid development of molecular diagnostics and targeted therapies that can work together with traditional pathology to lower costs and improve patient care and outcomes.
— Next-generation sequencing, proteomics, and other such technologies are rapidly becoming available at dramatically lower costs.
— Personalized, molecular medicine (oncology) is now being added to traditional large-scale clinical trials as an approach to creating evidence that can inform clinical decision making.
— Patient-centric research focusing in depth on individuals or small groups is delivering results that can apply to patients with similar disease profiles whose cancer has not responded to “standard-of-care” treatments. This research has proven that so many cancers are so unique that large trials are problematic in addressing the disease.
• The Internet revolution—The Internet has democratized access to information for patients, physicians, and researchers so they can rapidly learn more about diseases and treatment options. The result is demand for new services, tools, and approaches for cancer care, including
— the organization, indexing, and personalization of credible information to make it actionable and computable for individual cases;
— the development of decision tools and resources specific to cancer care;
— open science that allows physicians and researchers to collaborate in real time to defeat cancer, one patient at a time;
— new approaches to funding research, including patient-funded research and individualized fund raising, now possible at a rapidly decreasing cost; and
— active participation of patients in their own treatment decisions, as well as in rapid-learning communities that share what they learn and experience with each other—what works, side effects and quality of life—a development that raises the possibility of every patient taking charge of his/her destiny and leaving no stone unturned in the quest for a cure.
CollabRx is a company that seeks to harness both of the above revolutions to improve individual patient care. Its initial approach was to develop
an Internet platform called Cancer Commons for real-time translational cancer research and personalized oncology. Key goals are:
- to bring together patients, primary care physicians, oncologists, and researchers in academia and industry interested in applying the latest developments in personalized, molecular oncology;
- to provide them with the latest information, tools, and resources they need to enable each patient to achieve the best possible outcome and to defeat cancer, one patient at a time;
- to capture and aggregate the results over all studied patients to improve cancer treatment generally;
- to share what is learned from each patient with the clinical community in real time so the next patient can benefit through a reduction in the time from observation, to trial, to presentation, to publication, to treatment guidelines; and
- as the overarching goal, to run this translational loop in real time so that what is learned from one patient can be applied to the next, rather than waiting many years for the traditional process to play out.
Cancer Commons is likely the only rapid-learning community that links researchers, clinicians, and patients to defeat cancer, one patient at a time. It is intended to disrupt traditional thinking by promoting real-time, open-source science that includes patient input, especially from those highly motivated individuals known as “super patients” or “disease warriors.” The medical writing and publishing industry will also be disrupted, as it will rely on house vetting, rapid sharing, and postpublication peer review that promote the open exchange of creative information. The bias that inevitably results from a principal reliance on prepublication peer review will decrease, including the potential bias against the publication of unpopular or surprising results.
HEALTH INFORMATION TECHNOLOGY–BASED APPROACHES TO HEALTH MANAGEMENT
Paul C. Tang, M.D., M.S.
Palo Alto Medical Foundation
Effective use of health information technology (HIT) can drive significant improvements in physician and health system performance. Without engaging patients and supporting their active participation in managing their own health, however, the nation will still fall short of its health goals—for both individuals and the population. A learning health system
for patients places priority on meaningful applications of HIT to help patients gain access to their health data, relevant knowledge, and tools to guide self-care and health management. Shared information can help to create an effective partnership between the professional health team and patients in order to improve patients’ health.
The Palo Alto Medical Foundation (PAMF) has developed several promising approaches to using HIT to support a learning health system for patients. These approaches involve providing information and tools at the point of care and in the home to support better decision making and to engage patients in active learning and health management.
Status Quo for Health System Improvement
Overall, national healthcare quality scores are improving by only 2 percent per year (AHRQ, 2009). In just about any other industry, this rate of improvement would be unacceptable. What can we do differently to accelerate the rate of improvement in health and health care? A key enabler is to provide data, knowledge, and tools to all decision makers—clinicians, patients, and their families.
Driving Physician Change Through Data
Providing health professionals with accurate, relevant information in real time is one of the most powerful means by which EHRs can drive care improvement. HIT-enabled clinical decision support and quality-reporting feedback have demonstrated significant and immediate impact on physician performance. Using clinical decision support tools embedded in its EHR, PAMF has been able to better support informed decision making by physicians, resulting in orders that reflect up-to-date clinical information and medical knowledge. EHR systems can also provide near real-time feedback on physician performance. PAMF provides its physicians with unblinded quarterly performance data displayed alongside data from their home medical department. Of importance, the quality metrics are derived from clinical data from the EHR, which the physicians find credible. In contrast, most public reporting measures are derived from billing data, which contain significant errors, making them less reliable to use. Credible data are key to changing behavior.
The effect of providing point-of-care decision support and frequent performance reporting has been striking. The national benchmark for control of diabetes—a hemoglobin A1c (HbA1c) level below 7—is around 50 percent. In contrast, PAMF has seen quarterly improvements in HbA1c control and is performing 40 percent better than the national average. Having a 70 percent score is still not optimal, however. For the organization
to close that 30 percent gap, patients must be included in the process of managing their health.
HIT to Transform the Patient Experience
For patients, diabetes is a ravaging disease that is lived with by making hundreds of decisions, such as what to eat and whether to exercise, remembering to take their medications, checking their blood glucose, and so on. If patients are going to make the decisions that can keep their diabetes under control, they also must have good and timely information. Not surprisingly, as with physician performance improvement, patients benefit from the provision of real-time information more than from a physician critique 3 months after making a decision. Moreover, information must be understandable to patients and relevant to their individual health goals and concerns.
Personalized Health Goals
Physicians need to understand their patients’ preferences and individual health goals. Some patients want to live until 90, others may want to see their grandchildren graduate, and some want to avoid having a stroke. The way to learn about patient goals is to ask. A Stanford University project sponsored by The Robert Wood Johnson Foundation, called Living Profile,2 illustrates the power of this approach.
In the project, children with serious chronic diseases were asked what information they would like to put in their personal health record (PHR) for their doctor to read. One teenage girl described her life activities, not referring explicitly to her chronic condition: “I don’t think that my condition makes me who I am.” When the same question was asked of adults with diabetes, their responses were also insightful, revealing opportunities to teach and to better understand patient needs and concerns. For example, an individual with type 2 diabetes asked, “If I do all the right things, can I reverse this diagnosis?” If the provider community does not clearly and consistently answer this question for people with diabetes—many of whom have lived with their condition for decades—it is missing an important opportunity to improve health.
Understanding patient goals also enables physicians to clarify or express guidance on aspects of the patient’s situation more effectively. Sometimes patients have very specific goals. For example, one woman had a daughter in kidney failure, and her goal was to be healthy enough to give her daughter a kidney. Such strong, motivating health goals offer a physi-
____________
2 For more information see http://livingprofiles.net/ (accessed October 14, 2010).
cian the chance to develop, in collaboration with the patient, care management plans to reflect progress toward and attainment of patients’ personal health goals.
Personal goals do not change medical advice, but they change the approach and agenda for providing the advice. Some patients may say they need help in quitting smoking. Others may say that exercise is boring. Still others may want to understand how to control their diet. In every case, patients’ goals are key to helping them make decisions that can improve their health. Not many physicians engage in these sorts of discussions with their patients; thus, a focus on identifying personalized goals holds great potential for providing insight on the approaches and information that that can best help the patient.
Use of HIT to Help Patients Monitor Health Data
Once patients’ goals are understood, HIT offers a means to help them achieve those goals. Take, for example, patients who want to control their diet. The physician can provide a list of appropriate foods, as well as a glucometer to help monitor blood glucose. PAMF has taken this approach a step further and distributed wireless glucometers to patients with diabetes. This changes the device from a tool that simply measures glucose into an instrument that changes behavior. Rather than requiring patients to record their glucose readings in a diary, followed by a trip to the physician’s office for consultation, the electronic glucometer transmits data to the patient’s cell phone, which forwards the data to PAMF’s EHR system. If the graph of home glucose readings shows a little blip, patients can annotate the reading online with a short note so they can explain to the physician the circumstance causing this change.
The personal health goal therefore provides an important context for discussions with the physician about glucose data. The patient may be concerned that a relative lost a leg to diabetes or that a coworker had a heart attack or a stroke from diabetes. Using an EHR-produced diabetes dashboard, the physician can illustrate the patient’s risk of experiencing the same thing. After reviewing the glucose data, the physician can review other, related tests, such as the lipid profile, the HbA1c, and blood pressure readings. Teaching the patient how certain values increase the risk for bad outcomes can help the patient select new health goals. The physician can show how certain test results relate to the goal. These data provide a learning experience for patients—connecting, in this case, the need for active monitoring of blood glucose with the effect of diet, exercise, and medications.
From Learning to Changing Behavior
The diabetes dashboard helps patients see how things change in response to their behavior and adherence to a health management plan (Figure 6-1). Its features illustrate the impact of certain behaviors and reinforce what is needed to achieve personal health goals.
PAMF is conducting a randomized controlled trial to evaluate the impact of its online disease management system, including the tools discussed above. An early focus group discussion conducted with beta trial participants reinforced the potential of the approach. Patients initially participated in measuring and tracking their glucose because PAMF clinicians were looking at the results—in a sense, because they were told to. However, focus group discussions revealed that as time went on, patients became more engaged and started using the system for themselves because the information illustrated how what they ate affected their readings, or it enabled them to actively learn and watch how their behavior and their decisions impacted their health outcomes. Comments from the focus group members also underscored the role of the dashboard in helping them make better decisions. For example, denial became more difficult because they now knew how a decision, say, on whether to eat a piece of pastry would affect their readings and their risk. Such a decision is just one of the hundreds that patients must make to improve their health.
The use of HIT can drive improvements in physician and health system performance, but it can also transform patients, patients’ lives, and their health decisions. The use of PHRs provides patients with access to their health information; tools with which to visualize and learn from these data; and, more important, a means to engage them in their health care by making them part of the health team. Enabling learning among the entire health community, which includes patients, must be the goal of a learning health system.
HEALTH AND DISEASE MANAGEMENT OUTSIDE THE CLINIC DOORS: THERE’S AN APP FOR THAT!
Doriane C. Miller, M.D.
University of Chicago Medical Center (former)
Institute for Healthcare Improvement
The availability of HIT applications, changing population demographics, and changes in capacity to deliver primary care are impacting the growth of health and disease management activities that occur outside the clinical setting. This paper reviews the context of primary care delivery for providers and patients, the challenges of providing care outside of the office visit, promising HIT approaches to help patients access information and
care, and policy implications of these approaches and barriers to their dissemination.
The public image of the physician of the 1940s was one of being available 24 hours a day, 7 days a week; tolerating conditions of adverse weather; and neglecting personal commitments to attend to the urgent healthcare needs of patients. Indeed, a popular cigarette manufacturer promoted this image as one reason why physicians should smoke cigarettes (Gardner and Brandt, 2006).
Although scientific evidence has subsequently refuted the need for cigarettes as a “therapeutic” stimulant for physicians, the image of the availability of physicians for health information on demand has persisted. Physicians have continued to seek ways in which health care can be extended to patients outside of the clinic doors, particularly to improve health outcomes for the chronically ill.
As medical costs skyrocketed in the 1990s, payer groups concerned about the effects of healthcare costs on both the corporate bottom line and the health of the workforce made significant investments in disease management organizations that could work in conjunction with healthcare providers to improve care outside the clinical setting and encourage better outcomes (DMAA, 2006). However, the environment of healthcare delivery continues to evolve as society changes and medical advances are achieved. What are some of the environmental factors driving this change, and how is HIT helping to achieve the goal of extending care beyond the clinical setting?
Societal Changes
Personalized Medicine
In 2003, the National Human Genome Research Institute completed the mapping of the entire human genome, heralding the age of personalized medicine. Seeing the enormous potential for generating therapies specifically targeted to individuals based on their genetic profiles, environmental risk factors, and lifestyles, bench scientists, clinicians, pharmaceutical companies, information technology experts, and patients began seeking ways to link this burgeoning information to treatment of the individual. One of the recommendations generated by the Personalized Medicine Coalition through its public education arm, The Age of Personalized Medicine,3 was to have a secure, interoperable EHR for every American, bringing together personal, clinical, and molecular information that can facilitate improve-
____________
3 See http://www.ageofpersonalizedmedicine.org/center/policy/hit.asp (accessed October 14, 2010).
ments in therapeutic care in a patient-centered fashion. The ability to capture electronically information submitted by both patients and clinicians, as well as genomic information, will lead to better therapeutics and better outcomes for people with chronic health conditions.
Baby Boomers and Health Care: Supply and Demand
In 2011, 78 million people, the first wave of the Baby Boom generation, will reach age 65. By 2030, it is estimated that one of five people in the United States will be over age 65. The average American over age 75 has three chronic health conditions and takes four medications. Although older Americans are living longer and healthier lives, their healthcare needs are often complex. An Institute of Medicine report titled Retooling for an Aging America: Rebuilding the Health Care Workforce contains the recommendations that the number of physicians trained in care of the elderly be substantially increased, that the nonphysician long-term care workforce be expanded, and that informal caregivers be better prepared to provide care to aging loved ones (IOM, 2008). Despite a 1-year trend toward increased numbers of students selecting primary care careers, however, the Association of American Medical Colleges predicts there will be a shortage of approximately 50,000 primary care physicians by 2025 (AAMC, 2010). Most aging adults are cared for by general internists or family physicians—the adult primary care physicians—but estimates suggest that there will not be enough of these physicians. Can HIT help to fill this gap?
Incentives Through Accreditation: The Patient-Centered Medical Home and HIT
In 2007, the American College of Physicians, the American Osteopathic Association, the American Academy of Family Physicians, and the American Academy of Pediatrics joined forces to delineate the principles of the patient-centered medical home (PCMH). One of the hallmark values of this document is that health care should be facilitated by the presence of registries, health information exchanges, and EHRs to ensure that patients receive care when and where they need and want it in a culturally and linguistically appropriate manner. HIT should be used to support optimal patient care, performance measurement, patient education, and enhanced communication (NCQA, 2008). The National Committee for Quality Assurance operates the voluntary accreditation PCMH demonstration through its Physician Practice Connections® program. Although not a mandatory component, advanced electronic communication—including the availability of an interactive website, electronic patient identification, and electronic care management support—was included as a 2009 update.
Approaches to Health and Disease Management Outside the Clinic Doors
With the changing demands of consumers, the aging of the population, and incentives for quality improvement, how can HIT facilitate better healthcare outcomes at lower cost? Following are three examples of approaches that might be adopted more widely with the growth of HIT.
Patient Electronic Health Record Portals
As part of the demonstration initiative Pursuing Perfection, a project of the Institute for Healthcare Improvement, participants from Whatcom County, Washington, decided to fully embrace the concept of patient-centered care by facilitating communication between chronically ill patients and their healthcare delivery system. With patients as part of the planning team, they developed the website www.patientpowered.org, which includes information on initiatives to improve patient-centeredness, as well as useful information and tools for self-management of chronic conditions. Part of the Patient Powered website is a shared care plan (SCP)—a document, either web-based or on paper, that allows patients to gather all their health-related information in one place. The document includes the patient’s personal profile, healthcare team members, chronic and long-term diagnoses, self-management and lifestyle goals and action steps, treatment goals, names of prescriptions, medications and allergies, and advance directives. An SCP is designed to be much more user-friendly than a dense medical record, which typically is organized chronologically and fragments information by individual providers and locations. Patients can store the SCP information on paper or on a secure website linked to patientpowered.org and can upload information themselves or have other family members add vital information about their care. An evaluation of the implementation of the SCP through patientpowered.org in conjunction with a clinical care specialist (nurse or social worker) demonstrated increased patient satisfaction with clinical care and a cost savings of approximately $3,000 per year for enrolled patients (Safford).
The Missing Link: Web-Based Support Groups and the Patient’s Medical Home
In the national demonstration effort New Health Partnerships: Improving Care by Engaging Patients, 35 teams around the United States developed demonstration projects designed to improve self-management support within and beyond the clinical setting. One of the demonstration sites, Fargo Health Center, a federally qualified health center in Fargo, North Dakota, decided to concentrate on diabetes as a target condition.
Patients at Fargo Family Health Center decided they wanted to create a blog and listserv for patients living with diabetes. Instead of joining a public blog/support group for patients with diabetes, the patient advisors in the demonstration felt it was important that their providers know about their struggles and celebrations in living with diabetes. They also wanted to learn from other patients being treated at the health center. Patients registered for the site, and individual peer-to-peer phone calls were available for additional support. In the spirit of the phrase “all politics is local,” patients decided to create a geographic and condition-specific community of support for themselves that could be accessed by their clinical providers. Technical issues such as security and sharing of clinical information were challenges for this team. However, the opportunity to create a local community of patients who could offer each other support, provide information to their clinical partners, and impact the care provided at the local level helped the team decide to take on these issues and find effective ways of managing concerns about privacy and security for their participants (Miller, 2006).
eVisits: Saving Time and Money and Improving Satisfaction
Electronic provider visits hold the potential for enhancing patient–provider communication and enhancing the ability of primary care providers to offer care for nonurgent medical issues. The webVisit Study: Impact of Online Doctor-Patient Communication on Satisfaction and Cost of Care, conducted by researchers at Stanford and the University of California at Berkeley, evaluated whether using the eVisit platform offered by the company Relay Health was associated with satisfaction. Participating organizations included several health plans and large medical groups in California and Connecticut and 10 large self-insured employers. The intervention group included 282 physicians and 3,688 patients. Compared with controls, patients were 50 percent less likely to miss work; 45 percent were less likely to need a face-to-face visit with a physician, and 36 percent were less likely to telephone the physician’s office. Physicians reported that the system was easy to use (72 percent), satisfying (53 percent), and preferable to an office visit for nonurgent care (56 percent). Analysis of health claim costs for the intervention group showed a statistically significant lower cost for office-based claims (p <0.01) and total claims (p <0.05) (Zimmerman et al.).
Barriers to Adoption
Social Acceptability
Are patients ready, willing, and able to “visit” their physicians via the web? In an August 2008 study from the Center for Studying Health Systems Change, investigators demonstrated a dramatic change in the way consumers are seeking health information, with a doubling of the number of survey respondents stating that they seek health information from the Internet (Figure 6-2) (Tu and Cohen, 2008). However, in a July 2008 study posing the question “Does the Internet replace health professionals?, 86 percent of all adults said they ask a health professional versus 57 percent who said they use the Internet (Lee, 2008). Blending the convenience of the Internet with a trusted source who understands one’s personal medical history, the use of eVisits and personal health portals may be an acceptable way to communicate with physicians.
The Digital Divide: Race, Ethnicity, and Poverty
Given social acceptability, will patients have access to the Internet so they can communicate with their physicians? The Pew Internet and American Life Project tracks trends and issues related to age, race, ethnicity, and health. In
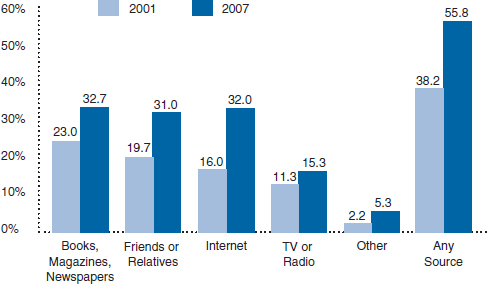
FIGURE 6-2 Consumers are increasingly seeking health information from the Internet.
SOURCE: Image appears courtesy of the Center for Studying Health System Change.
a 2009 survey, 79 percent of whites, 67 percent of blacks, and 80 percent of Latinos said they used the Internet. Use of wireless handheld devices was actually greater for blacks and Latinos than for whites (Horrigan, 2009). In addition, Latinos with annual incomes below $30,000 had increased their use of the Internet by 17 points between 2006 and 2008 (Fox, 2009). Internet use is increasing across the board, and the differential use of web-enabled handheld devices may signal just-in-time health management opportunities for some patient populations.
The Penetration of Electronic Medical Records: Supply and Demand
In a 2007–2008 national survey of 2,758 physicians, only 17 percent of practices reported having EHR systems, with 26 percent indicating that they planned to buy such a system within the next 2 years (DesRoches et al., 2008). Physicians most likely to have EHR systems belonged to large practice groups, hospitals, or medical centers. Cost has been described as a barrier to purchasing such systems. The impact of the 2010 federal healthcare reform legislation supporting technical assistance for primary care providers in establishing EHR systems should be studied.
Reimbursement for Electronic Communication: Fact or Fiction
Many physicians continue to be concerned that they cannot bill third-party payers for Internet communications with patients. Although specific reimbursement policies vary from insurer to insurer, in 2008 the American Medical Association’s Current and Procedural Terminology was revised to allow for billing for online patient services. Online services have a designated code that can be used once per episode of care over a 7-day period and can include any follow-up issues, including prescriptions, laboratory services, and ordering of imaging studies (Porter, 2008).
Looking to the Future
Primary care delivery capacity, evolving HIT platforms, and demographic and market forces will shape the future use of the Internet as a vehicle for extending health care beyond the clinical practice setting. Recent studies show that the delivery and support of care through web-based platforms can increase patient and provider satisfaction while decreasing cost. As these web-based platforms continue to grow, developers should keep in mind the importance of the input of patients and their caregivers in the creation of these products.
REFERENCES
AAMC (Association of American Medical Colleges). 2008. The complexities of physician supply and demand: Projections through 2025. https://services.aamc.org/publications/index.cfm?fuseaction=Product.displayForm&prd_id=244 (accessed September 3, 2010).
AHRQ (Agency for Healthcare Research and Quality). 2009. National healthcare disparities report. http://www.ahrq.gov/qual/nhqr09/nhqr09.pdf (accessed October 14, 2010).
DesRoches, C. M., E. G. Campbell, S. R. Rao, K. Donelan, T. G. Ferris, A. Jha, R. Kaushal, D. E. Levy, S. Rosenbaum, A. E. Shields, and D. Blumenthal. 2008. Electronic health records in ambulatory care—a national survey of physicians. New England Journal of Medicine 359(1):50-60.
Diaz, J. A., R. A. Griffith, J. J. Ng, S. E. Reinert, P. D. Friedmann, and A. W. Moulton. 2002. Patients’ use of the internet for medical information. In JGIM: Journal of General Internal Medicine: Springer Science & Business Media B.V.
DMAA (Disease Management Association of America). 2006. Disease Management Association of America annual report. http://www.dmaa.org/pdf/DMAA_2006_Annual_Report.pdf (accessed March 28, 2010).
Fox, S. 2009. Latinos online, 2006-2008. http://www.pewinternet.org/Commentary/2009/December/Latinos-Online-20062008 (accessed October 14, 2010).
Fox, S., and S. Jones. 2009. The social life of health information. http://www.pewinternet.org/Reports/2009/8-the-social-life-of-health-information (accessed October 14, 2010).
Gardner, M. N., and A. M. Brandt. 2006. “The doctors’ choice is America’s choice”: The physician in US cigarette advertisements, 1930-1953. American Journal of Public Health 96(2):222-232.
Gualtieri, L. N. 2009. The doctor as the second opinion and the internet as the first. Paper presented at Proceedings of the 27th international conference extended abstracts on Human factors in computing systems, Boston, MA, USA.
Horrigan, J. 2009. Wireless internet use. http://www.pewinternet.org/Reports/2009/12-WirelessInternet-Use.aspx (accessed October 14, 2010).
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2008. Retooling for an aging America: Building the health care workforce. Washington, DC: The National Academies Press.
Juni, P., A. Witschi, R. Bloch, and M. Egger. 1999. The hazards of scoring the quality of clinical trials for meta-analysis. Journal of the American Medical Association 282(11):1054-1060.
Lee, C.-J. 2008. Does the internet displace health professionals? Journal of Health Communication: International Perspectives 13(5):450-464.
Miller, D. 2006. Self-management support and the information technology superhighway: Stories from the road. http://www.hetinitiative.org/sub-resources/health_e-bytes/20061121health_e-bytes.html (accessed October 14, 2010).
NCQA (National Committee for Quality Assurance). 2008. Standards and guidelines for physician practice connections—patient centered medical home. http://www.ncqa.org/LinkClick.aspx?fileticket=3vQKgtlkp7g%3d&tabid=631&mid=2435&forcedownload=true (accessed October 14, 2010).
Porter, S. 2008. New, revised CPT codes target online, telephone services. http://www.aafp.org/online/en/home/publications/news/news-now/practice-management/20080229cptcodes.htm (accessed October 14, 2010).
Safford, B. Pursuing perfection: Report from Whatcom county, Washington on patient-centered care. http://www.ihi.org/IHI/Topics/ChronicConditions/AllConditions/ImprovementStories/PursuingPerfectionReportfromWhatcomCountyWashingtononPatientCenteredCare.htm (accessed October 14, 2010).
Sarasohn-Kahn, J. 2008. Reaching patients in a Health 2.0 world. Marketing Health Services 28(3):43.
Schwitzer, G., G. Mudur, D. Henry, A. Wilson, M. Goozner, M. Simbra, M. Sweet, and K. A. Baverstock. 2005. What are the roles and responsibilities of the media in disseminating health information? PLoS Medicine 2(7):e215.
Silberg, W. M., G. D. Lundberg, and R. A. Musacchio. 1997. Assessing, controlling, and assuring the quality of medical information on the internet: Caveat lector et viewor—let the reader and viewer beware. Journal of the American Medical Association 277(15):1244-1245.
Tu, H. T., and G. R. Cohen. 2008. Striking jump in consumers seeking health care information. http://www.hschange.com/CONTENT/1006/# (accessed October 14, 2010).
West, M., G. S. Ginsburg, A. T. Huang, and J. R. Nevins. 2006. Embracing the complexity of genomic data for personalized medicine. Genome Research 16(5):559-566.
Zimmerman, E., J. Rideout, and L. Baker. The WebVisit study: Impact of online doctor-patient communication on satisfaction and cost of care. http://hetinitiative.org/sub-resources/ea-abstract_satisfaction.html (accessed October 14, 2010).