8
Team-Based Care and the Learning Culture
INTRODUCTION
The value of a team-based approach to health care has been recognized for more than a decade (Grumbach and Bodenheimer, 2004; IOM, 2001; Leape et al., 2009; Wagner, 2000). It has been shown that a team-based approach adds value to the learning culture throughout health systems by preventing medical errors (IOM, 1999) and improving patient-centered outcomes and chronic disease management (Bodenheimer et al., 2002; Ponte et al., 2003; Wagner et al., 2001).
Team-based care is one of the guiding principles of a learning health system. It stresses interdependence, efficient care coordination, and a culture that encourages parity among all team members (IOM, 2001, 2007). Teamwork should be reinforced at all levels, from leadership to the unit level, and individual patients should understand that they are working with a team. Team-based care has yet to proliferate widely, yet numerous excellent team-based programs around the United States demonstrate their added value in generating superb patient-centered health outcomes and science-driven care.
The papers in this chapter delve into three aspects of team-based care as they apply to a learning health system: general concepts in team-based care; strategies for using teams to promote clinical excellence, continuous improvement, and real-time feedback; and the added value and efficiency that team care brings to streamline care transitions.
In the first paper, Allan S. Frankel and Michael Leonard of Pascal Metrics describe the essential elements that underpin team-based care and
a learning culture. Teams work by planning forward, reflecting back, communicating clearly, and resolving conflict. Data and information are continuously analyzed so that problems can be identified early on; actions can be taken; and feedback can be provided to clinicians, employees, and leaders.
Joyce Lammert of the Virginia Mason Medical Center (VMMC) explores team-based learning and care through the experiences of VMMC. She highlights changes in medicine brought about by the digital age and changes in the patient-physician compact that give more authority to the patient. Lammert offers several recommendations for accelerating team-based care and driving centers of excellence, including a shift in medical schools’ teaching strategies to more of an interactive, team-based model; rapid process improvement workshops; and incorporation of routine learning collaboration in real practice settings.
Alice Bonner, formerly of the Massachusetts Department of Health (now Centers for Medicare & Medicaid Services), Craig Schneider of the Massachusetts Health Data Consortium, and Joel S. Weissman of Harvard Medical School address the importance of team-based care in the context of care transitions. They underscore the importance of interdisciplinary teams that are able to deliver safe, effective, culturally appropriate, and timely care within and across settings. Standardized procedures can improve the quality of care and reduce suboptimal outcomes and patient experiences, leading to more appropriate use of services and lower costs.
PRACTICAL EXPERIENCE WITH COLLABORATIVE MODELS IN THE HEALTH PROFESSIONS
Allan S. Frankel, M.D., and Michael Leonard, M.D.
Pascal Metrics, Inc.
Across a variety of settings and industries, groups that effectively coordinate teamwork and improve science tend to achieve their goals (Mathieu et al., 2008). Since the Institute of Medicine (IOM) report To Err Is Human (1999) was published, the healthcare industry has learned a great deal about teamwork and improvement, but few in health care methodically combine the two in order to reap their full potential. Instead, teamwork and improvement are taught and applied separately. As a result, goals take longer to attain. Healthcare leaders have little in-depth knowledge of teamwork and improvement and therefore a limited ability to integrate the two concepts in order to improve practice. This paper explores the components of a continuous learning environment (Batalden and Splaine, 2002; Mohr and Batalden, 2002), positing that teamwork and improvement are essential—and inextricably linked—components of a successful learning environment.
Continuous Learning Environments
Figure 8-1 offers a simple description of a continuous learning environment, applicable at both a departmental and organizational level (Frankel et al., 2009). Raw data and information from a wide variety of sources—such as quality audits or an individual’s concerns—are collected and made available for analysis. A management group regularly evaluates the data to identify concerns that might undermine safety or reliability. Possible solutions are discussed. Specific individuals are given responsibility for taking action to address the findings using formal improvement methods and told to report back on their efforts. The learning that occurs from this action is encapsulated and fed back to all interested individuals and groups, especially those who initially brought the raw data or information to attention. This final feedback step validates why it is worthwhile for individuals to speak up about concerns—because they see response by the organization. The end result is an engaged front line that feel their concerns are heard and acted upon and an effective management team that has a finger on the pulse of front-line activity and can respond quickly when variation in process becomes troublesome or things go wrong.
This description of a continuous learning environment might best be viewed as conceptually simple but difficult to accomplish. The difficulty exists because stellar continuous learning environments rely on outstanding leadership, teamwork, and improvement. Organizations and individuals
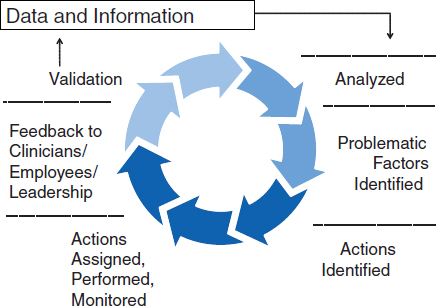
FIGURE 8-1 Components of a continuous learning environment.
must be able to manage and apply these components. Of note is that even if the three elements are excellent, that is insufficient unless they are also linked together.
A Recent History of Teamwork Practice in Health Care
Aviation in the late l980s looked to teamwork to address human error, building on a science called human factors that examined the limitations of human performance in complex environments (Porter, 1964). Scientists focused on how human beings interact cognitively and physically with their environment and cognitive frailty and physical limitations to understand the causes of error. They formed hypotheses based on concepts by psychologists such as Rasmussen (Rasmussen et al., 1991) and Reason (Dekker, 2002; Reason, 1997) that divided cognition into three discrete categories—automatic, rule-based, and knowledge-based thought—each generating specific types of errors (Table 8-1).
Initial efforts in aviation to decrease error focused on ergonomics and the physical environment, but the industry realized that most error occurred because of team dynamics (Dekker, 2002). Helmreich (1993) and others sought to understand the relationship between teamwork and error and to develop a training program to address the issues involved. The end result was a program entitled Cockpit Resource Management, so named because the goal was to have groups work effectively with the members of the team and whatever was available in the physical environment. This title quickly became Crew Resource Management (CRM), reflecting that the aviation
TABLE 8-1 Cognition: Automatic, Rule-based, and Knowledge-based Thinking
| Example | Error | Example | ||
| Automatic thinking | Driving a car | Slips and lapses | Taking the wrong route because daydreaming | |
| Rule-based thinking | A door handle telegraphs whether to push or pull the door | Rule-based error | Walking into a door because of misreading the visual cues on the door handle | |
| Knowledge-based thinking | The slow, laborious process of integrating new information | Knowledge-based error | Being influenced by the most recent fact because of its timing, not its importance | |
SOURCE: Data derived from Reason, 1997.
team included more than the cockpit members. In time, both CRM training became part of aviation’s high-fidelity simulation program that combined training in skills and teamwork (Helmreich, 1997, 2000).
This new body of knowledge was initially applied to some healthcare teams (such as emergency helicopter response teams) and eventually became part of training for emergency rooms. The great leap forward occurred when Helmreich and Leonard applied CRM concepts to Kaiser Permanente’s obstetric departments, whose combined hospitals deliver approximately 80,000 babies per year (Leonard et al., 2004a, 2004b). Companies such as Dynamics Research Corporation and Pascal Metrics diffused these teamwork programs. Other groups stepped forward to consult and teach on the basis of CRM concepts. From this work, the Agency for Healthcare Research and Quality (AHRQ) developed TeamSTEPPS (Team Strategies and Tools to Enhance Performance and Patient Safety),1 a programmatic team training effort that is an extension of the training started in aviation 30 years ago.
The body of teamwork literature and teamwork videos available at AHRQ is impressive, albeit daunting. Overall, the teaching style is behaviorally based and rigid, requiring modification in order to be acceptable to physicians. It brings useful behaviors into the healthcare environment that, once sorted through and simplified, can be codified into a group of behaviors that make up good teamwork and team leadership.
Health care, however, has thus far mistakenly assumed that CRM alone, with minor modification, can be imported effectively from aviation; in fact, it cannot. One difference is that the cockpit is better suited to simulation than is the more complex healthcare environment. Furthermore, aviation altered its management structure based on CRM concepts. Delta Airlines, for example, made its chief pilot, in many ways the equivalent of a chief medical or nursing officer, responsible for simulation training. In health care, by contrast, senior leaders commonly assign “teamwork training” to subordinates or “teamwork champions,” as if it is appropriately accomplished by midlevel managers. Aviation incorporated CRM concepts as a central component of its core strategy, while for the most part, health care continues to view patient-centered care and evidence-based medicine as the two mainstays for achieving excellence. Teamwork is perceived as necessary but also soft and fuzzy, peripheral to the real work at hand and assignable to the simulation center and patient safety office.
Pilots who left aviation to focus on the healthcare industry did not realize that they were leaving an industry with 30 years of sophisticated thinking about team behaviors and entering a naïve environment. Having
______________
1 For more information see http://teamstepps.ahrq.gov/index.htm (accessed October 15, 2010).
learned about teamwork in aviation’s high-fidelity simulators, they assumed that CRM-based training would suffice. They were, and are, mistaken. This misperception has also stymied clinicians who teach teamwork in the healthcare setting. In fact, although high-fidelity operating room simulators have positively influenced and transformed anesthesiology practice in the United States over the past 25 years, they have been unable to penetrate further into the healthcare system because they did not garner interest from hospital leaders and, initially, lacked a strong evidence base showing the value of simulation training (Cooper and Gaba, 2002). Today, other disciplines are becoming engaged, but hospital leadership has been slow to do so.
Since the publication of To Err Is Human (IOM, 1999), teamwork trainers have also struggled to compress multiple-day aviation- and simulation-based teamwork programs into a shorter curriculum for health care. Hospitals and clinical units have balked at the idea of releasing physicians and nurses from duty, often with pay, for multiple-day sessions. Consultants and trainers, competing with each other for contracts and eager to satisfy, have shortened their sessions to accommodate demand. Even today, as an indication of just how far some organizations still have to go, some department chairs wonder whether their physicians can learn teamwork in the hour or two available for departmental meetings or grand rounds.
In health care, evidence that teamwork influences reliability is slowly appearing in the literature (Pronovost et al., 2006). However, the paucity of statistically proven links between clinical outcomes and team models is frustrating for those who believe in the value of teamwork. In aviation, by contrast, the training became an integral part of the industry as a response to the identification of human error as the major factor in accidents. Aviation did not wait for double-blind controlled trials to prove the training’s efficacy. Today CRM has been a part of civil aviation for 30 years and is perceived as instrumental in producing aviation’s enviable safety record. No one is suggesting that aviation CRM training be withdrawn because of a lack of evidence showing its value.
Comparing the roots of teamwork against those of improvement reveals why health care has not effectively linked the two. Teamwork training is based on a marriage of psychology, sociology, and engineering. Robert Helmreich, a psychologist, wrote the first comprehensive text on CRM. In contrast, improvement models such as LEAN and the Institute for Healthcare Improvement’s (IHI) Model for Improvement are focused primarily on using statistics to manage variation in stable industrial processes, and derive from the teachings of skilled statisticians and managers such as Shewhart, Juran, and Deming (Juran, 1995). Teamwork is a social science in which measurement is difficult, and linking process to outcome is an elusive challenge. Improvement, by contrast, centers on numbers collected from definable steps that lead to clearly measurable outcomes.
Improvement Science
William Edwards Deming proposed that the science of improvement comprises four domains: psychology, appreciation of a system, understanding variation, and theory of knowledge. Although Deming described effective leadership and management behavior, he did not go into detail about team behaviors and norms of conduct. He states in The New Economics, “Psychology helps us to understand people, interaction between people and circumstance, interaction between customer and supplier, interaction between teacher and pupil, interaction between a manager and his people and any system of management” (Deming, 2000). By contrast, the other three domains are extraordinary in their elegance and application. They are why Japanese car manufacturers gained such an advantage over U.S. companies. In health care, Deming’s work is the underpinning for IHI’s Model for Improvement.
Shewhart and Deming’s improvement science looks at stable industrial processes, evaluates the variation in output of the end product, and applies improvement techniques when appropriate to minimize unnecessary variation. Applied to health care, the industrial process is the care path of patients, and the output is the outcome of care for those patients. Standardization of care processes is necessary, facilitated by measurement of the processes and the outcomes. In diabetes, a standardized method of optimizing blood sugar levels culminates in good HgBA1Cs. In hip and knee surgeries, optimizing time, cost, and patient rehabilitation culminates in patients’ achieving good postoperative functional outcomes. The improvement model is applicable in every aspect of health care, from ambulatory to intensive care, from billing to central sterilization.
The backgrounds of these experts differ from providers of team training. Improvement science requires the setting of measurable aims that identify how a group is going to accomplish “what by when” (Langley et al., 2009). The aims require careful and reproducible measurement, subject to the full range of statistical manipulation. Means, medians, variance, standard deviation, and the like are all part of the nomenclature, a process very different from discussing team behaviors such as briefings and debriefings and the psychology of team relationships.
The improvement advisors at IHI are a good example. IHI trains these advisors, who then support clinicians engaged in activities by helping them perform small tests of change and measure the outcome. Those who do the teaching are mainly statisticians and their primary areas of interest are variation and its management in stable environments. Some have backgrounds in sociology and psychology, and spend some time teaching about the qualities of leadership and teamwork. However, their focus is on teaching how to apply the improvement model, not how to influence groups of clinicians to function in teams.
Weaving the Two Disciplines Together
The weaving together of these two disciplines is the responsibility of hospital leaders and healthcare managers. In reality, the end result is more than a responsibility—it is the core function of management. This is an important insight for newly appointed department chairs, division chiefs, and healthcare managers and directors, yet few healthcare leaders assume these positions knowing how to do this work.
Effective managers establish a learning-to-action cycle that gathers information from across their span of authority and then shapes improvement activities. Managers know what is happening across their work area because they continuously receive information about how it is functioning. Data become information, then knowledge, then understanding, and finally wisdom about poorly functioning aspects of their units. “Poorly” in this context is likely to mean that the managers have insight into the variation that is occurring in the steps of care and can see when the variation increases. They target these areas for evaluation and assign responsibility as appropriate to members of their team for taking actions that will improve the problematic steps. Those actions must be based on improvement science, and the individuals accountable should be able to describe formally the work performed. This means being able to state what they hope to accomplish, what change they are making, and how they will learn from that change. They should make predictions about the impact of the change and be able to describe any tasks they must perform before making the change. If a series of these tests of change leads to desired improvements, the managers are responsible for making that information widely known. This process is not an addition to managers’ work—it is their core function. The question then becomes, “How do managers obtain the information that becomes grist for the improvement mill?”
Debriefing: The Link Between Teamwork and Improvement
The link between teamwork and improvement is manifest in the first part of the continuous learning cycle—the collection of information. A leader responsible for running a department knows how well the department is functioning only if he or she has an open conduit for receiving data. Information technology facilitates the collection of some data, especially in the technical aspects of care. But healthcare delivery is more than clinical decision trees and quality audits; it is a social process among providers and with patients. Much is dependent on humans interacting well with each other in complex settings. Managers must get good information from their coworkers and those they manage in order to understand their clinical, technical, and social concerns. Concerns in each of these areas can under-
mine reliability and increase variation in care. The means of obtaining this information is called debriefing.
Debriefing, in concept, is simple enough. Team members should pause at appropriate times in their daily routine, or at the end of procedures, to ask as a group what has gone well, what has not, and what they would want to do differently the next day. Debriefing is not simply an event or behavior; it should be an ongoing process that is periodically highlighted. In other words, when team members notice something is not running as desired or when they have a concern, they should note it down, state it to someone, or in some way capture their thoughts. At the appropriate time, those insights should be collected and eventually conveyed to the manager. The manager can then use these pieces of information to form a better picture of the functioning of the unit, turning the concerns of providers into data that feed into the continuous learning-action cycle.
Caregivers, as unit team members, have a responsibility to participate in debriefings. This norm of conduct, however, is feasible only in a management system that appreciates its importance. Collecting worker insights and concerns requires that clinical leaders create an environment of mutual respect and psychological safety in which concerns emerge quickly and transparently. Mutual respect across disciplines and the creation of an environment in which all concerns are heard and addressed are the responsibility of unit leadership. Managers and clinical chairs and chiefs need to foster this kind of culture to know what is happening at the sharp end of care. There is no substitute.
Other behaviors will support the debriefing process. Briefing, also labeled a “time out,” “pause,” or “checklist,” is when team members look ahead at the work to be performed, consider together the strengths and challenges in the group and in the work to be done, and formulate a plan of action. The goal of a briefing is to ensure that an optimal game plan is formulated, and that everyone knows that game plan as well as their roles and responsibilities. By contrast, a debriefing involves reflecting back and thinking about what has happened and how that compares against the game plan. Briefing and debriefing are the bookends of every process and support each other. Debriefing is more likely to be useful if team members have and know the game plan and whether actions taken helped achieve it. For that matter, debriefing can help improve the briefing process, ensuring that team members function more effectively when formulating the next game plan.
Conclusion
Health care has a long way to go from its current state to one comprising continuous learning environments. First, every healthcare environment
suffers from a hierarchical structure that causes some nurses and ancillary personnel to feel constrained about speaking up to physicians. In some settings, the constraint is based on academic stature, while in others it is based on hospital-physician relationships. In others, the issues may be gender and ethnically based. Second, managers currently have a limited appreciation of the components of a continuous learning environment and how to achieve such an environment. Finally, senior leaders have more work to do through strategies and resources to ensure that continuous learning systems thrive. We in health care are just beginning on this journey, although it is one that offers great promise.
MEASURES AND STRATEGIES FOR CLINICAL EXCELLENCE AND CONTINUOUS IMPROVEMENT
Joyce Lammert, M.D., Ph.D.
Virginia Mason Medical Center
In 2001, the Institute of Medicine (IOM) released the report Crossing the Quality Chasm: A New Health System for the 21st Century. That report identified six key clinical dimensions in need of improvement: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. To achieve progress in these dimensions will require a fundamental change in the approach to learning and the application of that learning in providing health care.
Developing new models of collaborative care requires engaging all team members, including patients, in the development of evidence and the use of evidence to make healthcare decisions grounded in effectiveness, safety, and value. However, the physician is currently regarded as the leader of the healthcare team, and in order to move successfully to new models of care it will be critical to redefine what constitutes clinical excellence for providers and develop measures to ensure excellence in all six dimensions.
Abraham Flexner’s report to the American Medical Association Council on Medical Education in 1910 helped establish the fundamental elements of how physicians are trained and how care is delivered to patients (Beck, 2004; Flexner, 1910). That system of training has survived fundamentally intact to this day. Much as Gutenberg’s movable type changed the power structure of society in the Middle Ages, the Internet and Google have fundamentally changed the balance of knowledge and the ability, as well as the expectations, of patients to be engaged in their health care. Rapid advances in science and technology, coupled with the complexity of 21st-century care, make the old paradigms of learning and caring for patients obsolete. The old underlying assumptions about what it means to be a physician—which continue to be reinforced in training—are in conflict with what is
needed to provide care that is aligned with the six aims of the Chasm report as well as foster a learning health system (Table 8-2).
Changes to the culture must start in medical school (Table 8-3). Today, two years of basic science followed by two years of clinical science form the backbone of physician training. This system is largely unchanged from the days of the 19th century. In this hierarchical system, physicians in training also pick up the underlying assumptions and attitudes about medicine and patients of their residents and attending physicians. A recent Lucian Leape Institute report calls for a change in medical education from the current focus on “courses” and content to a focus on examining patient care processes, systems thinking, leadership, and teamwork (Lucian Leape Institute, 2010). Team learning for medical students has until now been
TABLE 8-2 Changing Provider Culture in Health Care
|
|
|
|
20th Century |
21st Century |
|
|
|
|
Taking care of the sick |
Promoting health and well-being |
|
Physician-centered |
Patient-centered |
|
Gestalt |
Evidence-based |
|
See one, do one, teach one |
Simulation, simulator |
|
Know it all |
Know what to ask and how to find the answer |
|
Autonomy |
Collaborative/team |
|
The health of my patient |
The health of a population of patients |
|
My fault |
Faulty systems |
|
Total patient care commitment, 24/7 |
Work hour restrictions, physician wellness |
|
Learning: batched, episodic |
Learning: continuous, embedded |
|
|
|
TABLE 8-3 Changing Culture: Medical School
|
|
|
|
20th Century |
21st Century |
|
|
|
|
Unidirectional learning |
Interactive, team learning |
|
Knowing everything |
Knowing essentials, asking questions, finding answers |
|
Individual accountability |
Team accountability |
|
Departments |
Service line training |
|
Role models: lengthy resumés and grants |
Role model: “quality provider” |
|
Passing boards |
Competency- and milestone-based training and certification |
|
|
|
limited. The use of Team STEPPS by Emory University School of Medicine and Woodruff School of Nursing is an example of what is possible in training. All third-year medical students and fourth-year nursing students now participate in team training (Morrison et al., 2010).
Much of the “content” that students learn is out of date by the time they graduate. Instead of requiring medical students to memorize large amounts of material that they may never use and will soon forget, it is time for medical schools to decide what not to teach. Medical schools should be teaching students how to ask the right questions and leverage information systems to provide just-in-time answers that are evidence based and reflect best practices. These are the skills that are needed for life-long learning.
It may also be necessary to look at the basic organizational structures of medical schools. Traditional departments such as medicine and surgery encourage and reward siloed thinking and training. Academic advancement and funding are integrated into the department structure. The formation of cardiovascular, neuroscience, and cancer institutes represents a move toward more collaborative care models. Ideally, medical student training would include training in working in interdisciplinary teams that cross service lines.
Role models for medical students and residents should be providers who are highly accomplished in the competencies outlined by the IOM: patient-centered care, the ability to work in interdisciplinary teams, evidence-based practice, understanding and application of quality and safety improvement concepts, and skill in using and applying information technology in the care of patients (IOM, 2003). Successful completion of medical school should require demonstration of competency in those core areas.
Residency training reinforces what students learn in medical school. In 1999, the Accreditation Council for Graduate Medical Education (ACGME) approved six general competencies that would be required of all residents. They included the traditional medical knowledge and patient care, but also included practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice (ACGME Outcome Project, 1999; Meyers et al., 2007; Sachdeva et al., 2007). Training in these competencies has been gradual and varied, depending on the institution.
Virginia Mason Medical Center (VMMC) in Seattle, Washington, adopted the Toyota Production System philosophies and practices and applied them to health care in 2001. The system focuses process design work on the patient and the care processes, which results in improved quality and safety. Value streams are used to help analyze processes, and the team develops standard work processes around best practices and mistake proofing for safety and quality. Rapid process improvement workshops (RPIWs) are one of the tools used to implement process improvement at VMMC. All
residents must be a member of at least one workshop during their residency. The workshops involve taking a team of people offline for a week to work on a problem. A typical team comprises all the people involved in the process, including, ideally, a patient. On the first day, the team is trained in the tools, the problem to be tackled is reviewed, and the team applies innovation techniques to generate improvement ideas. The next four days are spent on the floor conducting trials of these ideas, followed by a report to the medical center on Friday. Follow-up reports after 30, 60, and 90 days ensure rigor.
An RPIW held on ambulatory teaching demonstrates the power of this work. The teaching process for residents in the specialty clinic had remained largely unchanged from the 1920s, despite changes in the complexity of the work. Cardiology was chosen for the workshop because it was the rotation in the department of medicine ranked lowest by the residents. The attendings viewed teaching as a burden that lengthened their day, and in-service test scores were low. For the RPIW, the team included a cardiologist, residents, medical assistants, and a scheduler. The solutions were simple and included developing clear rotation expectations; an orientation for residents; daily huddles of the resident with the medical assistant and attending; visual control so everyone could easily see where the patient, attending, and resident were located; anticipation of “flow busters,” such as getting called away to the cath lab; and the development of parallel rather than sequential processes. A year and a half later, residents ranked cardiology as one of the top rotations, and 70 percent of the attendings were rated as “top teachers.” A powerful lesson learned for the residents was that improving processes is part of a provider’s job and that there are tools and science to help achieve that improvement.
Training across silos to ensure the best care for patients is another lesson residents learn. An example is the work on door-to-balloon time for cardiac patients. The team includes medics, emergency department staff, residents, cath lab staff, and cardiologists. Work is standardized, including single-pager notification of the entire team; external setup with kits; and standardized processes, including where to put EKG patches and IVs. Regular drills are held, as well as debriefs with the team to identify improvements for the future.
Training in the internal medicine residents’ continuity clinic is another example of the power of the LEAN management system. Several years of process improvement work have centered on improving the primary care experience for patients, providers, and staff. The improvements have included skill-task alignment and the provision of patient-centered care as a team. A collaborative practice model was developed for the internal medicine residents’ continuity clinic. The residents practice in the same flow station with the same attending for the duration of their residency.
They learn to work with a “flow manager” who performs preliminary activities—including medication reconciliation, taking and recording of vital signs in the electronic medical record (EMR), teeing up of the health maintenance module, and agenda setting—before the resident sees a patient. While the resident is in with the patient, the flow manager sets up indirect work for the resident, such as phone messages, lab results, and medication refills. When the resident finishes with the patient visit, he/she will do the indirect work that is already set up before seeing the next patient. Visits related to chronic diseases such as diabetes or congestive heart failure are linked to visits with the nurse. The EMR has built-in mistake proofing to ensure that patients receive the screenings they need; safe medications; and appropriate, value-added labs. Evidence-based guidelines and pathways and patient teaching aids are readily available online for both patient and provider to use in discussions about care. Residents learn communication skills (huddles, warm hand-offs to care nurses) and how to provide efficient evidence-based care in flow. As they gain skill in providing care in flow, they find that at the end of the session, they do not face batches of charts to dictate or lab letters to send. The residents begin to see internal medicine as a sustainable career and gain an appreciation of the importance of improving processes to improve care for patients.
These examples demonstrate that training in the ACGME competencies can be accomplished as an integral part of providing safe, quality care for patients. They reinforce the importance of continuous improvement and learning among the entire healthcare team. ACGME also recommended outcome-based assessment of residents during their training. Years after the initial recommendations, however, educational outcome measures remain rudimentary. It is said that what is measured is what is considered important. Further progress in training residents and changing the culture of care will require progress in measuring educational outcomes (Table 8-4).
TABLE 8-4 Changing Culture: Evaluation of Resident
|
|
|
|
20th Century |
21st Century |
|
|
|
|
In-service exams |
Medical content: critical elements that must be known |
|
Board exams |
Skill in asking the right clinical questions and finding answers |
|
Rotation evaluations |
Educational outcomes to include |
|
• Subjective • Evaluators not trained or skilled in feedback |
• Patient and staff satisfaction • Team skills (leadership/following) • Communication skills • Training in giving and receiving feedback |
|
|
|
For an organization or practice to evolve into a learning system, training of medical students and residents is critical but not sufficient. Practices and organizations need to recruit not just for medical and technical knowledge but also for the other dimensions outlined by ACGME. At VMMC, a physician compact makes explicit the expectations around patient care, including the focus on patients, collaboration, and communication with the team. The physician compact is used in the recruitment process, and providers are chosen for both technical and cultural fit.
Once in practice, physicians would ideally find themselves in an environment that supports continuous learning and provides tools to help them apply evidence and best practices to the care they provide. The evolution of the EMR from a documentation and ordering tool to one that supports learning is critical for physicians who are overwhelmed by the volume of new learning, along with uncertainty about the efficacy of current treatments. Embedding such capabilities as risk calculators, checklists, automatic feedback, online information search engines, and patient educational material into the EMR can enable physicians and patients to learn just-in-time during the care process (Davenport and Glaser, 2002; Enthoven and Vorhaus, 1997; Schiff and Bates, 2010).
Most physicians practicing today began practice before EMRs were available. For physicians, who have been trained to have all of the answers, reluctance to ask for help is often a barrier to learning how to use available tools. It is important to provide training that is designed for individual learning styles, easy to access, and efficient with regard to time. At VMMC, more than half of providers have taken the “Getting On-Line and Up to Speed in Evidence Based Medicine” course. The course is taught by physicians, it is hands-on, and there is one teacher for every two learners. The course is grounded in a four-step, case-based model. Providers learn how to form search questions; find evidence (search primary studies, vetted sites, consensus tools); appraise information (level of evidence/strength); and save the sites so that they will appear on their exam room computers and can begin to be used with patients the next day.
Learning organizations also need to find ways to engage physicians in guideline development, patient safety initiatives, and leadership/team training. Physicians are data driven, and providing accurate data on clinical outcomes and patient satisfaction can lead to organizational and individual improvement. In order to help physicians improve, it is important that this data sharing be coupled with courses/tools in such areas as shared decision making.
Knowledge assessment for physicians in practice continues to be based on multiple-choice tests, which serves to reinforce the need to know the right answer every time (Brooks, 2010). Certification tests that allow the use of online resources; that are primarily case based; and that test the
ability to use guidelines, evidence, and statistics in making clinical decisions would come closer to measuring the skills needed for continuous learning and improvement. Maintenance of certification should be seamless and not another barrier and add-on for physicians. Continuing medical education credits should be automatically updated in a database that would be available to all credentialing bodies. Instead of more work, recertification could become embedded in the daily work of the provider.
The movement to a learning health system will also require a change in the current payment system. The current system rewards primarily the amount of work done by individuals. The result is a system that is too expensive, of variable quality, and inequitably distributed. If healthcare systems are to move to a care model that is evidence based and focuses on outcomes, quality, and safety, a payment model that is aligned with those goals will be necessary.
Ensuring clinical excellence and continuous improvement will require letting go of traditional ways of teaching and learning. It will require engaging every member of the healthcare team, including the patient. Finally, it will require major institutional leadership in medical schools, in graduate medical education, and in specialty groups for continuing medical education.
CARE COOPERATION AND CONTINUITY ACROSS CLINICIANS, FACILITIES, AND SYSTEMS
Alice Bonner, Ph.D., R.N., Craig Schneider, Ph.D., and
Joel S. Weissman, Ph.D.
Massachusetts Department of Public Health
(formerly, now Centers for Medicare & Medicaid Services),
Massachusetts Health Data Consortium,
and Harvard Medical School
The Massachusetts Strategic Plan for Care Transitions:
A Model for a Learning Health System
The healthcare system in the United States demonstrates significant patient safety and quality deficiencies (Snow et al., 2009) and therefore fails to provide value for those who use and pay for it. The United States spends more on health care than any other country in the world. In the past, it was generally agreed that higher costs signaled better quality of care. However, emerging research is beginning to question this assumption by demonstrating that higher-cost regions of the country experience worse quality of care and lower patient satisfaction (Elmendorf, 2009). The opportunity exists to make significant changes in the healthcare system that can enhance both quality and efficiency.
The Institute of Medicine (IOM) has helped characterize a learning health system as the most promising approach for addressing the complex array of healthcare decisions facing the nation in the future (IOM, 2007). Achieving this vision will require fundamental changes, including better synchronization of efforts, use of shared EMRs, and public engagement. At the core of a learning health system is the goal of transforming the current system from one that operates for the convenience of providers and institutions to one that is patient-centered. Nowhere is this need more evident than when patients transition from one setting or one set of providers to another during an episode of care. Furthermore, it has become increasingly clear that no single entity can achieve significant changes in healthcare delivery on its own. The involvement of the public sector is crucial as a means for fragmented providers to interact—especially in efforts aimed at improving the management of transitions that cross treatment silos.
Given the range of healthcare settings and the number of providers involved in treating patients, it is not surprising that communication problems and other errors in treatment persist as patients move across the continuum of care (see Box 8-1). Patients and families are unassisted as they navigate different providers and care settings.
BOX 8-1
Barriers to Effective Care Transitions
Structural
- Lack of integrated care systems
- Lack of longitudinal responsibility
- Lack of standardized forms and processes
- Incompatible information systems
- Lack of care coordination and team-based training
- Lack of established community links
Procedural
- Ineffective communication
- Failure to recognize cultural, educational, or language differences
- Processes neither patient-centered nor longitudinal
Performance Measurement and Alignment
- Underuse of measures to indicate optimal transitions
- Compensation and performance incentives not aligned with care coordination and transitions
- Payment for volume of services rather than incentivized for outcomes
Massachusetts state leaders believe that poor communication and a lack of clear accountability for patients among multiple providers lead to medical errors, waste, and duplication. Adverse events often occur during care transitions, most often with complex, chronically ill, and vulnerable patients. Such events can result from failure to communicate critical information related to a patient’s medical care, safety, medications, advance directives, in-home support services, and social situation. Failure to identify issues in such areas as health literacy and cultural preferences may also lead to higher rates of hospitalization, particularly in vulnerable populations. The result is high expenditures for the chronically ill, driven primarily by hospital admissions and readmissions.
We envision a future in which interdisciplinary teams deliver safe, effective, and timely care that is culturally and linguistically appropriate—within and across settings. This vision calls for care that is organized around regions and communities; that is delivered by integrated systems coordinated across settings; and in which the flow of patient information is seamless and secure among all of a patient’s providers, insurers, and patients themselves. To accomplish this transformational change, the Massachusetts healthcare community will require collaboration and effective partnerships focused on the creation of a patient-centered care model delivered within learning healthcare systems and encompassing the entire continuum of care. This paper describes the process undertaken by the Commonwealth of Massachusetts to identify and quantify issues associated with care transitions, and to develop and implement a statewide strategic plan for beginning to address those issues. This strategic plan is designed to delineate actionable steps to help the Massachusetts healthcare community realize the vision of integrated, high-value, coordinated, and efficient healthcare delivery.
Background and Significance
Health care in the United States has evolved into a complex array of settings, providers, payers, and procedures. Settings of care include hospitals; subacute and postacute nursing facilities; the patient’s home; primary and specialty care offices; community health centers; rehab facilities; home health agencies; hospice; long-term care facilities; and other institutional, ambulatory, and ancillary care providers. In each setting, multiple clinicians care for each patient, sometimes independently and at other times as part of an interdisciplinary team. Figure 8-2 depicts the interdependencies among many different organizations and settings involved in realizing this vision in Massachusetts.
Improving care transitions has the potential to save lives, reduce adverse events and disability due to gaps or omissions in care, and reduce unnecessary costs. Several national clinical and policy models were
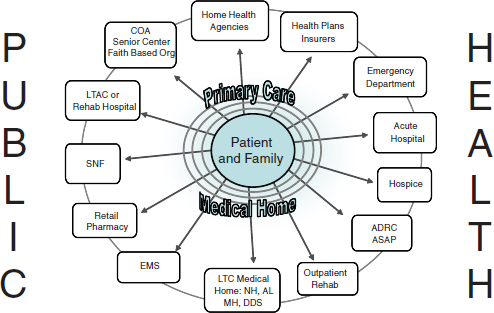
FIGURE 8-2 Interdependencies among organizations: settings of care that must work together and be interdependent to achieve a patient-centered, integrated health system.
SOURCE: Reprinted with permission from the Massachusetts Care Transitions Forum.
reviewed in developing the strategic plan, three of which are highlighted here.
First was the University of Colorado “Care Transitions Intervention,” which employs an interdisciplinary team model using a transitions coach. The intervention focuses on four pillars: (1) medication self-management, (2) use of a dynamic patient-centered record, (3) timely primary care/specialty follow-up, and (4) recognition of red flags.
The model was tested on 750 patients aged 65 and older at the University of Colorado Health Sciences Center, randomized at the time of hospitalization to receive either the coaching intervention or usual care. Intervention patients experienced significantly lower rehospitalization rates at 30 and 90 days relative to control subjects, as well as lower rates of rehospitalization for the condition precipitating the index admission at 90 and 180 days. Mean hospital costs were lower for intervention patients than for controls at 180 days (Coleman et al., 2006).
Second was the Transitional Care Model, which focuses on several components, including screening, engaging the elder/caregiver, managing symptoms, educating and promoting self-management, collaborating, ensur-
ing continuity, coordinating care, and maintaining relationships. The model is implemented by a single advanced practice nurse using evidence-based protocols and with a focus on long-term outcomes. The model was initially tested in a randomized controlled trial of 276 older adults at the University of Pennsylvania Hospital (Naylor et al., 2004). It resulted in fewer hospital readmissions, fewer total days rehospitalized, lower readmission charges, and lower charges for healthcare services after discharge.
The final model emerged from a collaboration among the American College of Physicians, the Society of Hospital Medicine, the American Geriatric Society, the American College of Emergency Physicians, and the Society for Academic Emergency Medicine to develop consensus standards to address quality gaps in care transitions. The Transitions of Care Consensus Conference, held in fall-winter 2006, developed several principles and clinical standards for care transitions: accountability, communication of treatment plans and follow-up expectations, timely feedback, involvement of the patient and family, respect for the hub of coordination of care, the patient’s ability to identify a medical home, patients knowing who is responsible at every point along the transition, national standards for transitions in care, and standardized metrics for continuous quality improvement and accountability (NTOCC, 2009; Snow et al., 2009).
Creating the Plan
Although efforts to improve care transitions had been ongoing for some time, those efforts were fragmented and uncoordinated. About 3 years ago, a small group of clinicians, healthcare administrators, and government agency staff, coordinated by the Massachusetts Health Data Consortium and Massachusetts Senior Care Foundation, came together to discuss gaps in such efforts and how to disseminate individual work more broadly. That group grew to more than 100 stakeholders and is now known as the Care Transitions Forum, representing a community of interest that meets quarterly to share best practices and provide mentorship to institutions and organizations across the state. Concurrently, senior policy staff from the Massachusetts Executive Office of Health and Human Services had been developing statewide initiatives around patient-centered medical homes and accountable care organizations. They determined that none of these reforms would attain maximum effectiveness unless coordination across care settings was improved. The policy staff members were active participants in the Care Transitions Forum, and with the Secretary’s approval, the idea of creating a strategic plan was put forth. The development work was a learning process involving public and private stakeholders from across the Commonwealth. A working group composed of senior administration officials working together with the policy community began by reviewing the
BOX 8-2
A Vision for the Future of Health Care
• Interdisciplinary teams delivering safe, effective, and timely care that is culturally and linguistically appropriate within and across settings
• Aligning of
— Clinical care (individuals)
— Public health (populations)
— Health policy (payment and organization of services)
literature and identifying best practices in care. To effect system change, the group explored innovations along multiple dimensions—medical practice, public health, and healthcare financing—and eventually composed a vision for the future (Box 8-2). A strategic plan was drafted over the subsequent months.
Content of the Strategic Plan
The strategic plan2 contains five main sections. An introduction defines care transitions and identifies the healthcare system’s problems in this area. The next section reviews what is known about effective transitions based on national models and randomized trials. The next two sections summarize current projects in Massachusetts that form the infrastructure for future work, and place them in the state and federal policy context. The final section presents the vision for improving care transitions, including principles, recommendations, action steps, and measures for consideration. One goal is to weave the many currently fragmented care transition projects in Massachusetts into a fabric that covers the state. We believe Massachusetts can be a model healthcare learning state and can lead the nation in improving care transitions and reducing avoidable hospitalizations.
Objectives
We had a number of objectives in writing the strategic plan. A central tenet of the process was ensuring the patient’s voice. To this end, we
______________
2 The document referred to in this section can be found at: https://www.mass.gov/Ihqcc/docs/meetings/stratetic_plan_for_care_transitions.doc.
included patients, families, and advocates in the development and review of each stage of the plan. Still, the first few drafts appeared to lack a strong enough patient focus, so an unfolding case study was added to the document. This enabled us to tell a story from the patient’s point of view, and put a very real face on the problem of unsafe care transitions and rehospitalizations.
Another objective was to build consensus among the many stakeholders as to the most important care transition principles; to this end, it was necessary to get people to agree to work together outside of their individual institutions for the good of state health policy. For example, many institutions have their own patient transfer form or process. Numerous forms, very similar but each somewhat unique, exist. To improve consistency and institute a standardized, evidence-based process, each institution must agree to give up some customization so that a unified form and process can be adopted statewide. Bringing stakeholders in early, obtaining their input, and listening to their concerns have been essential parts of our process. We are currently moving forward with final development and deployment of our statewide resident transfer form, which we anticipate will be posted on the Massachusetts Department of Public Health website in the next few months.
A third objective was to include guidance addressing accountability between sending and receiving institutions. When a patient leaves one setting of care, someone must be prepared to receive that patient in the next setting of care. Longitudinal responsibility rests with the sending provider until the receiving provider has acknowledged and accepted the patient. While we anticipated that hospitals and physicians would be resistant to this concept, they accepted the significance of this component of care transitions and the need to address this difficult problem. Ongoing discussions in 22 communities are currently under way as part of the State Action to Avoid Rehospitalizations project, supported by a grant from the Commonwealth Fund.
Measurement
As a learning healthcare system and state, we must be able to measure performance improvement in care transitions. Put simply, how will we know a safe and effective transition when we see it?
The Massachusetts strategic plan for care transitions outlines a strategy for tracking progress and measuring successes and challenges. Performance measurement is essential if the best practices and lessons learned from state demonstrations and national research and care models are to be implemented effectively on a statewide basis. The measures described in the plan have been endorsed by recognized national and state panels of experts. The
plan presents a menu of options for measurement, and proposes that the selection process involve providers, payers, and patients/advocates to ensure that measurement is balanced and reflects the essential roles of providers, insurers, and patients in improving the process.
The National Quality Forum has endorsed several measures for care transitions: the three-item Care Transitions Measure, the 30-day all-cause risk-standardized readmission rate following hospitalization for heart failure developed by the Centers for Medicare & Medicaid Services (CMS), the CMS 30-day all-cause risk-standardized readmission rate following hospitalization for acute myocardial infarction, the CMS 30-day all-cause risk-standardized readmission rate following hospitalization for pneumonia, and the all-cause readmission index (NQF, 2007).
Certain process measures are linked to successful outcomes: the timely transfer of information across settings and professionals involved in care transitions, the effective coordination of transitions across settings and professionals, the timely delivery of care, improvement in patient understanding of and adherence to the treatment plan, improvement in patient awareness of emergency provider contact information, and improvement in patient engagement in care (ABIM, 2009). Ongoing work to refine measures is part of the Massachusetts strategic plan.
Dissemination and Next Steps
In his book Agendas, Alternatives, and Public Policies, John Kingdon explains how policy issues rise and fall on public agendas (Kingdon, 2003). He describes three independent streams of activities—problems, policies, and politics—that must occur before effective decision making takes place in government. For a problem to be identified, there must at some point in time be agreement that solutions exist. Policies are generated by specialists, staffers, academics, and interest groups. The creation of the strategic plan accomplished these first two activities. The third required careful vetting of the plan with interested parties. The most prominent of these was the Health Care Quality and Cost Council, which had been established under Massachusetts’ landmark healthcare reform law in 2006.
With the Kingdon policy hurdles passed, Massachusetts has now moved into the implementation phase, with workgroups already engaged in the refinement and deployment of a statewide interfacility transfer form and process, as well as state surveyor education around effective care transitions. As more cross-continuum teams are established in more communities, Massachusetts will continue to evolve as a learning health system at the state level.
REFERENCES
ABIM (American Board of Internal Medicine). 2009. Care transitions performance measurement set. http://www.guideline.gov/content.aspx?id=15179 (accessed.
ACGME Outcome Project. 1999. General competencies: Minimum program requirements language approved by the ACGME. http://www.acgme.org/outcome/comp/compMin.asp (accessed October 15, 2010).
Batalden, P., and M. Splaine. 2002. What will it take to lead the continual improvement and innovation of health care in the twenty-first century? Quality Management in Healthcare 11(1):45-54.
Beck, A. 2004. The Flexner report and the standardization of American medical education. Journal of the American Medical Association 291:2139-2140.
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness: The chronic care model, part 2. Journal of the American Medical Association 288(15):1909-1914.
Brooks, R. 2010. Continuing medical education: Let the guessing begin. Journal of the American Medical Association 303:359-360.
Coleman, E., C. Parry, S. Chalmers, and S. Min. 2006. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine 166(17):1822-1828.
Cooper, J., and D. Gaba. 2002. No myth: Anesthesia is a model for addressing patient safety. Anesthesiology 97:1335-1337.
Davenport, T., and J. Glaser. 2002. Just-in-time delivery comes to knowledge management. Harvard Business Review 80:107-111.
Dekker, S. 2002. The field guide to human error investigations Hampshire: Ashgate Publishing.
Deming, E. 2000. The new economics for industry, government, education. Cambridge, MA: First MIT Press.
Elmendorf, D. W. 2009. Testimony before the Subcommittee on Health, Committee on Energy and Commerce, U.S. House of Representatives. Options for controlling the cost and increasing the efficiency of health care. Washington, DC: Congressional Budget Office.
Enthoven, A., and C. Vorhaus. 1997. A vision of quality in health care delivery. Health Affairs 19:44-57.
Flexner, A. 1910. Medical education in the United States and Canada. New York: Carnegie Foundation for the Advancement of Teaching.
Frankel, A., M. Leonard, T. Simmonds, C. Haraden, and K. B. Vega. 2009. The essential guide for patient safety officers. Oak Brook, IL: Joint Commission Resources.
Grumbach, K., and T. Bodenheimer. 2004. Can health care teams improve primary care practice? Journal of the American Medical Association 291(10):1246-1251.
Helmreich, R. 1993. Cockpit resource management. London: Academic Press.
———. 1997. Managing human error in aviation. Scientific American 276:62-67.
———. 2000. On error management: Lessons from aviation. BMJ 320:781-785.
IOM (Institute of Medicine). 1999. To err is human. Washington, DC: National Academy Press.
———. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2003. Health professions education: A bridge to quality. Washington, DC: The National Academies Press.
———. 2007. The learning healthcare system: Workshop summary. Washington, DC: The National Academies Press.
Juran, J. 1995. A history of managing for quality: The evolution, trends and future direction of managing for quality. Milwaukee: Irwin Professional Publishing
Kingdon, J. 2003. Agendas, alternatives and public policies. New York: Addison, Wesley, Longman, Inc.
Langley, G., et al. 2009. The improvement guide—a practical approach to enhancing organizational performance. San Francisco: Josey-Bass.
Leape, L., D. Berwick, C. Clancy, J. Conway, P. Gluck, J. Guest, D. Lawrence, J. Morath, D. O’Leary, P. O’Neill, D. Pinakiewicz, and T. Isaac. 2009. Transforming healthcare: A safety imperative. Quality and Safety in Health Care 18(6):424-428.
Leonard, M., A. Frankel, T. Simmonds, and K. Vega. 2004a. Achieving safe and reliable healthcare: Strategies and solutions, Management. Chicago, IL: Health Administration Press.
Leonard, M., S. Graham, and D. Bonacum. 2004b. The human factor: The critical importance of effective teamwork and communication in providing safe care. Quality and Safety in Health Care 13(1):85-90.
Lucian Leape Institute. 2010. Unmet needs: Teaching physicians to provide safe patient care. Boston, MA: National Patient Safety Foundation.
Mathieu, J., M. T. Maynard, T. Rapp, and L. Gilson. 2008. Team effectiveness 1997-2007: A review of recent advancements and a glimpse into the future. Journal of Management 34(3):410-476.
Meyers, F., S. Weinberger, J. Fitzgibbons, et al. 2007. Redesigning residency training in internal medicine: The consensus report of the alliance for academic internal medicine education redesign task force. Academic Medicine 82:1211-1219.
Mohr, J., and P. Batalden. 2002. Improving safety on the front lines: The role of clinical microsystems. Quality and Safety in Health Care 11(1):45-50.
Morrison, G., S. Goldfarb, and P. Lanken. 2010. Team training of medical students in the 21st century: Would Flexner approve? Academic Medicine 85:254-259.
Naylor, M., D. Brooten, R. Campbell, G. Maislin, K. McCauley, and J. Schwartz. 2004. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatric Society 52(5):675-684.
NQF (National Quality Forum). 2007. Safe practices for better healthcare 2006 update, a consensus report. Washington, DC: National Quality Forum.
NTOCC (National Transitions of Care Coalition). 2009. National transitions of care coalition. www.ntocc.org (accessed.
Ponte, P., G. Conlin, J. Conway, et al. 2003. Making patient-centered care come alive: Achieving full integration of the patient’s perspective. Journal of Nursing Administration 33(2):82-90.
Porter, E. H. 1964. Manpower development: The system training concept. New York: Harper and Row.
Pronovost, P., D. Needham, S. Berenholtz, et al. 2006. An intervention to decrease catheter-related bloodstream infections in the ICU. New England Journal of Medicine 355:2725-2732.
Rasmussen, J., B. Brehmer, and J. Leplat. 1991. Distributed decision making: Cognitive models for cooperative work. Chichester, England: Wiley.
Reason, J. 1997. Managing the risk of organizational accidents. Hampshire: Ashgate.
Sachdeva, A., R. Bell, L. Britt, et al. 2007. National efforts to reform residency education in surgery. Academic Medicine 1200-1210.
Schiff, G., and D. Bates. 2010. Can electronic clinical documentation help prevent diagnostic errors? New England Journal of Medicine 362:1066-1069.
Snow, V., D. Beck, T. Budnitz, D. Miller, J. Potter, R. Wears, et al. 2009. Transitions of care consensus policy statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. Journal of General Internal Medicine 24(8):971-976.


























