INTRODUCTION AND CONTEXT
The prosperity of a nation is tied fundamentally to the health and well-being of its citizens. It follows, then, that citizens—each one a past, current, or future patient—should represent both the healthcare system’s unwavering focus, and its fully engaged agents for change. This precept has several major implications. It means that the quality of health care should not be judged solely by whether clinical decisions are informed by the best available scientific evidence, but also by whether care accounts for a patient’s personal circumstances and preferences. It implies that careful listening should be the starting point for every patient encounter. And it suggests that the success of and innovations in healthcare delivery should depend on direct consumer engagement in the design of healthcare models and their aims.
One of the central lessons of the Institute of Medicine (IOM) report Crossing the Quality Chasm: A New Health System for the 21st Century is that much of health care in the United States has lost its focus on the patient (IOM, 2001). Instead, the healthcare system has been designed and motivated primarily by the perspectives of its component facilities, companies, payers, and providers. Crossing the Quality Chasm urges that care be refocused around six aims: care should be safe, effective, patient-centered, timely, efficient, and equitable. In the decade since the report was published, it has become even clearer that citizen and patient engagement is central to taking advantage of advances in the personalization of care based on genetics, preferences, and circumstances. Meeting this challenge is the core goal of what the Institute of Medicine’s (IOM’s) Roundtable on
Value & Science-Driven Health Care has termed a learning health system. Central to such a system is the notion that advances in biological research, clinical medicine, and information technology provide powerful tools for health improvement if applied within a system that promotes the mutually dependent aims of science, value, and patient-centered care (IOM, 2007, 2010b, 2010c, 2011a, 2011b).
Currently, health care in the United States falls substantially short of what should be possible given the nation’s substantial healthcare investment. At $2.5 trillion, $7,500 a person, and 17 percent of gross domestic product in 2009, that investment totaled twice the expenditure levels of other industrial countries, yet the United States consistently rates poorly (currently 37th) on overall health system performance and on key component measures such as infant mortality (39th) and life expectancy (36th) (IOM, 2010a; Murray and Frenk, 2010). Although the overall quality of care in the United States compared with other developed nations varies by condition—for example, the United States is a leader in cancer care but lags behind other nations in asthma and hip fracture mortality—perhaps the most compelling illustration of system shortfalls is found in the wide variation in the quality of care from state to state and practice to practice. It is not unusual to see several-fold differences in care intensity and costs, with no effect on outcomes (Docteur and Berenson, 2009; Fisher et al., 2003; OECD, 2009). This geographic variation in quality of care has been shown to extend to cities in the same state and hospitals in the same city.
The systematic barriers to effective and efficient healthcare decisions have contributed to the development of a system that, by some estimates, delivers recommended care less than half of the time and often lacks definitive research evidence to guide clinical practice (IOM, 2008, 2009). Across the United States, however, many organizations deliver high-value care, and collectively, these organizations illustrate the many missed opportunities for healthcare improvement, such as system fragmentation, a lack of infrastructure and healthcare culture to support learning and continuous improvement, and incentives that reward care volume over value.
Perhaps the greatest missed opportunity for creating a health system that delivers the right care to the right patient at the right time is the failure to fully engage patients and the public as active partners in advancing the delivery of care that works best for the circumstances and ensuring that the care delivered is of value. Despite the potential to achieve this engagement, evidence suggests that such efforts are limited at both the health systems level, where provider preferences and supply often shape the care delivered, as well as at the level of individual healthcare decisions (Berwick, 2009; Sepucha and Barry, 2009; Zikmund-Fisher et al., 2010).
In part, this shortfall is a communication problem with respect to public awareness as well as encouragement and support by the healthcare
system. Patients may express frustration with their care because they do not feel they have adequate input into the clinical decision-making process or that the decisions made reflect their preferences. Currently, however, more than two-thirds of U.S. consumers believe their personal care is “evidence-based”—derived from the best available science and appropriately targeted to individual patient needs—and consistently of high quality (Campaign for Effective Patient Care, 2009). Increased public awareness of and appreciation for current shortfalls in health care and the role patients and the public can play in effecting needed improvements are essential for progress (Carman et al., 2010).
THE ROUNDTABLE AND THE LEARNING HEALTH SYSTEM SERIES
Since 2006, the Roundtable has provided a venue for health leaders from various stakeholder sectors—health professionals, patients, health system leaders, insurers, employers, manufacturers, information technology, research—to work cooperatively to address their common interest in improving the effectiveness and efficiency of health care. Roundtable members have set the goal that, by 2020, 90 percent of clinical decisions will be supported by accurate, timely, and up-to-date information and will reflect the best available evidence. Over the past 5 years, the Roundtable’s Learning Health System series of workshops has identified and considered the key elements whose transformation can be central to achieving this goal: clinical research, clinical data, information technology, evidence standards, healthcare tools, caregiver culture, patient engagement, and financial incentives. For each of these elements, the workshops have explored priorities and approaches integral to harnessing interests and expertise across healthcare sectors to drive improvements in the value of medical care delivered in the United States. The following publications summarizing these workshops offer perspectives on the issues involved, and identify priorities and projects in need of cooperative stakeholder engagement:
- The Learning Healthcare System (2007)
- Evidence-Based Medicine and the Changing Nature of Health Care (2008)
- Leadership Commitments to Improve Value in Health Care: Finding Common Ground (2009)
- Value in Health Care: Accounting for Cost, Quality, Safety, Outcomes, and Innovation (2010)
- Redesigning the Clinical Effectiveness Research Paradigm: Innovation and Evidence-Based Approaches (2010)
- Clinical Data as the Basic Staple of Health Learning: Creating and Protecting a Public Good (2011)
- The Healthcare Imperative: Lowering Costs and Improving Outcomes (2011)
- Engineering a Learning Healthcare System: A Look at the Future (2011)
- Learning What Works: Infrastructure Required for Comparative Effectiveness Research (2011)
- Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care (2011)
In addition to the meeting series focused on exploring concepts and strategies for the learning health system, the Roundtable operates a series of Innovation Collaboratives, aimed at stewarding joint projects among organizations key to field advancement.
Across the range of issues engaged in the Learning Health System workshops and the Innovation Collaboratives, greater public interest and patient engagement have emerged as essential and potentially transformative elements for driving health system change. Empowering and supporting the public in these new roles requires the creation of a healthcare culture that supports continuous improvement and learning; elicits and considers public perspectives on key healthcare issues; and better characterizes needed partnerships, resources, tools, and communication approaches. Listed in the front of this publication are members of the IOM planning committee1 charged with guiding the development of a workshop to consider these issues in detail. The committee worked with IOM staff to develop the workshop objectives and emphases and to plan the agenda. Box 1-1 summarizes the motivating issues and objectives for the workshop.
The planning committee designed day 1 of the workshop to focus on key elements of progress in science-driven health care—care culture, clinical research and the evidence process, clinical data, health information technology systems—with specific attention to the role of patient engagement in the success of each. Day 2 was devoted to understanding opportunities to develop the communications, culture, and incentives that will help in reorienting the focus and performance of a value- and science-driven health system. The workshop agenda is provided in Appendix A, speaker biographical sketches in Appendix B, a listing of workshop participants in Appendix C, and an overview of common themes from each workshop in the Learning Health System series in Appendix D. This publication summa-
______________
1 Institute of Medicine planning committees are solely responsible for organizing the workshop, identifying topics, and choosing speakers. The responsibility for the published workshop summary rests with the workshop rapporteurs and the institution.
BOX 1-1
Motivating Issues and Objectives
Motivating Issues
- Implications of knowledge advances. Progress in medical science, basic research, information technology, and operations research offers the potential for immediate, continuous, and transformative improvement in health care. In the context of increasing understanding of the importance of individual factors to patient outcomes, reaching health care’s full potential requires a reorientation to the patient.
- Performance shortfalls. In terms of both effectiveness and efficiency, the nation’s healthcare system is underperforming. The United States has the highest per capita health expenditures—twice the average for other developed countries—yet consistently rates no better than the middle tier of developed nations on such key indicators as infant mortality, life expectancy, and overall health system performance.
- Disconnects in core aims. The core aim of health care is improved outcomes: to maintain or enhance patient status with respect to disease, injury, functional status, and sense of well-being. Yet often the system’s dominant characteristics are oriented more to clinician preferences or interests and economic rewards for volume over value.
- Anchor misalignment. The primary focus of care should be on outcomes rather than service volume and on the interdependent aims of patient-centeredness, better science, better value, and continuous improvement.
- Imperative to make patients a central element. Efforts of the IOM and others have underscored the necessity of making patient perspectives, preferences, and needs a strong, central focus of a learning health system, for several reasons, including: the basic fact that patients are the health system’s key focus and its agents for change; the fact that care has been shown to be more effective and efficient with more patient involvement; and the growth of preference-sensitive care as new interventions are developed.
- Importance of communication. Central to progress are the communication strategies necessary to inform and engage the public and patient communities as understanding advocates, partners, and change agents.
Objectives
- Identify the state of play with respect to the foundational elements of a learning health system, the role of patients and the public in achieving progress on each element, and the most important priorities and policy levers for accelerating progress.
- Explore and clarify the integral links among three key desired characteristics of care: science-driven, patient-centered, and value-enhancing.
- Discuss communication and public engagement strategies important to improving the awareness and patient-focused action necessary for the transition to a learning health system.
rizes the workshop presentations and discussions and the issues addressed. Summaries of common themes and of the workshop presentations and discussions are provided below; further detail is provided in the main text.
This chapter provides contextual information for that discussion, including an overview of opportunities presented by the recent healthcare reform legislation and a summary of the keynote remarks of Harvey V. Fineberg, president of the Institute of Medicine, to help set the stage for the workshop. The remainder of this volume contains speaker-authored papers presented at the workshop in the areas of clinical research, patient care, and learning that is real-time and continuous (Chapter 2); clinical data as a public good for discovery (Chapter 3); engaging patients to improve science and value in a learning health system (Chapter 4); health information technology as the engine for learning (Chapter 5); patients, clinical decisions, and health management in the information age (Chapter 6); applying evidence for patient-centered care: standards and expectations (Chapter 7); team-based care and the learning culture (Chapter 8); and incentives aligned with value and learning (Chapter 9).
HEALTHCARE REFORM AND A LEARNING HEALTH SYSTEM
Many of the basic aims of the American Recovery and Reinvestment Act of 2009 (ARRA) and the Patient Protection and Affordable Care Act of 2010 (ACA) reflect key features of the Roundtable’s vision for health care. These features are focused on better harnessing technology and innovation—by advancing information networks and research methodologies—as well as the expertise and resources of all healthcare stakeholders to promote greater coordination, communication, transparency, and accountability in health care.
A learning health system is one that maintains a constant focus on improving the value of the return on the nation’s healthcare investment. Emerging from the Roundtable’s work on reducing healthcare costs and improving outcomes and on advancing the infrastructure required for comparative effectiveness research (CER) are many immediate opportunities to improve the overall value of health care delivered (IOM, 2010c, 2011b). Echoing this work are efforts targeting the reduction of unnecessary services, waste, and other system inefficiencies; the alignment of incentives to reward care value rather than volume; and establishment of a means for continuous measurement, tracking, and improvement of the effectiveness and efficiency of the healthcare system. Reflecting the interdependence between controlling costs and providing coverage that ensures timely and appropriate care to all, the ACA also significantly expands health insurance coverage.
A focus on the development and application of evidence on what works best for whom is fundamental to understanding and ensuring the
value of health care delivered. Funds provided as part of the ARRA represent an important initial investment in several components of a learning health system, including $19 billion allocated for improved deployment and application of electronic health records (EHRs) and $1.1 billion for expanded capacity for CER, which encompasses funding for the conduct of such research and the development of key infrastructure elements such as databases and other clinical data resources. Efficient use of these new resources for quality improvement and evidence development is contingent upon recognition of their qualities as a public good and assessment of issues related to ownership, availability, and use of clinical data as a public utility for real-time clinical insights.
Underscoring the importance of developing the point of care as a knowledge engine, provisions in the ACA also target healthcare delivery systems as a vehicle for driving improvements in system performance and efficiency. Building the capacity to learn as a natural outgrowth of clinical care will foster a health system that continually improves the quality of health care delivered. Furthermore, developing capacity to measure and track quality and efficiency will not only improve transparency and accountability in health care, but also lay the foundation for building innovative clinical effectiveness research into practice to improve the speed and relevance of evidence development.
The fragmented nature of the U.S. health system compounds the challenge of healthcare delivery but at the same time creates system-wide opportunities for innovation and improvement. Healthcare reform provisions such as the Innovation Center at the Centers for Medicare & Medicaid Services (CMS) aim at accelerating sharing and dissemination of this learning across the system and supporting greater efficiency and effectiveness in the delivery of high-quality health care by fostering greater synchrony, consistency, and coordination in the development, interpretation, and application of clinical evidence.
In addition to these healthcare reform provisions, a trusted scientific intermediary could help both broker the perspectives of different parties and ensure that leadership stems from every sector. Strong, visible, and multifaceted leadership from all involved sectors will be essential to marshal the vision, nurture the strategy, and motivate the actions necessary to create a learning health system.
CREATING A LEARNING CULTURE
The passage of the ARRA and ACA does not guarantee dramatic gains in the efficiency or effectiveness of medical care. Careful implementation of the legislation will be necessary to better orient health care toward science and value, and reform will be ongoing and constantly evolving. Sustain-
ing these efforts will require the creation of a learning culture that fosters continuous learning, improvement, and innovation.
Fundamental to a learning culture is the full engagement of patients and the public. The Roundtable envisions learning in health care as a partnership in which the patient is central to ensuring improved health and the delivery of appropriate care, and the public is engaged in the evidence process. Supporting patients and the public in these roles will require improved communications between patients and health professionals about the nature of the evidence base and its use and strengthening of the patient–provider relationship.
Many workshop participants stressed that such a culture will require not only outreach to patients and the public, but also adoption in full of patient-centered care across health sectors and stakeholders. Although identified nearly 10 years ago by the IOM as a key dimension of quality, patient-centered care still feels unfamiliar, even disruptive, to many stakeholders (Berwick, 2009; IOM, 2001). Ultimately, value and science-driven health care comes from a sustained, system-wide focus on fostering a health-care culture and activities that reflect the interests, values, and priorities of patients and the public. Attention is needed to the identification and development of opportunities, across health system activities, to better elicit and act on patient and public perspectives and input.
THE LEARNING HEALTH SYSTEM IN 2010 AND TO COME
Harvey V. Fineberg, M.D., Ph.D.
Institute of Medicine
The U.S. healthcare system is vast, complicated, and multifaceted. Unlike many other countries, the United States has several alternative healthcare models across the nation, each with its own niche. While some systems differ in their financial infrastructure, designed as either integrated, prepaid, or privately insured, others specialize in innovation, incentive schemes, or primary care and other specialties. For example, the Veterans Health Administration, an integrated, prepaid, wholly central system, differs largely from privatized health coverage programs such as health maintenance or preferred provider organizations, yet both are successful in their own light. Thus, the U.S. healthcare system currently is characterized by pockets of innovation and demonstrated success. These successes, however, are swimming in a sea of chaos and lack of achievement. Aspects of our current healthcare system are not working well and must be addressed.
Flaws of the Current Healthcare System
Healthcare spending in the United States surpasses that in most other countries, yet the nation’s patient care outcomes fall well below those of most other Organisation for Economic Co-operation and Development (OECD) countries. A comparison of life expectancy and health spending per capita across different countries illustrates that the United States is an outlier along these two dimensions, spending by far the most and yet achieving less than many other countries (see Figure 1-1). Despite monetary investments amounting to 17 percent of the nation’s gross domestic product, the United States ranks among the lowest in life expectancy and highest in infant mortality rate, and has poor system performance. Moreover, it has been estimated that about one-third of healthcare expenditures do not improve patient outcomes (McGlynn et al., 2003; OECD, 2009; Truffer et
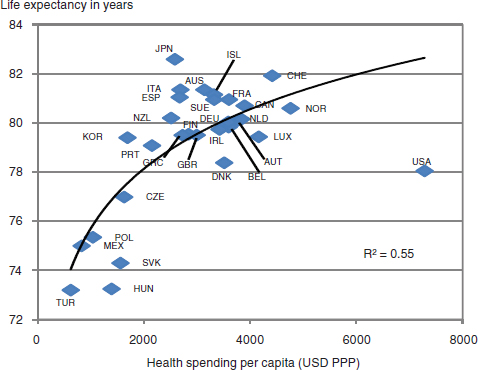
FIGURE 1-1 Healthcare outcomes in the United States compared with other countries. The graph shows life expectancy at birth in different countries versus per capita expenditures on health care in dollar terms, adjusted for purchasing power. The United States is a clear outlier on the curve, spending far more than any other country yet achieving less.
SOURCE: OECD, 2009.
al., 2010). With $2.5 trillion spent in 2009 on health care, the United States sees a low return on a high investment.
Still, addressing healthcare expenditures is only one facet of the larger issue of healthcare reform. Classic problems of overuse, underuse, and misuse of interventions still exist as critical challenges for U.S. health care—challenges that will not disappear with the adoption of universal healthcare coverage. Similarly, universal healthcare coverage will not be possible unless these critical issues of health spending and intervention variabilities are addressed. U.S. health care must address both of these concerns in conjunction to ensure that people are receiving care and the system is getting the right care to the people who need it. The systems perspective of a learning health system is therefore the first step toward achieving this high level of care.
A Comprehensive, Systematic Focus
Learning in health care does not apply solely to the practicing physician or professional. Although formal training and education are vital components of learning in health care, a systems perspective encompasses a number of different foci and catalyzes learning among all healthcare stakeholders. The system involves individual interventions and constituents, thus placing focus on what providers can do for their patients. However, it also encompasses the performance of individuals and organizations, the role of patients in everything from health literacy to participation in decision making, and the engagement of technologies such that equipment and information systems deliver better services. We must consider these individual components holistically to comprehend what it means for the healthcare system to be operating at a higher level; a level characterized by better outcomes, better value, and better ability to address patient needs. Five key tools will be instrumental in achieving this level of performance:
- Health information technology, electronic medical records, and integrated systems that involve both patient management and the ability to learn can engage patients and help make them active participants in their own care.
- New research and innovation in diagnosis and treatment can increase the scope of what healthcare providers can do for their patients and the ways in which they can provide those services.
- Insights in genetics are enabling the move into an era of personalized medicine, wherein patients have access to information that is relevant to them as individuals. This knowledge can be a powerful tool, encouraging patients to fundamentally alter their lifestyles and take charge of their own health.
- Innovative care delivery approaches go beyond individual technologies and place the emphasis on systems of care delivery and a holistic perspective.
- Public engagement is a root source of progress and a critical tool in achieving a learning system.
A Vision of a Learning Health System
The charter of the Roundtable on Value & Science-Driven Health Care describes a learning health system as a system designed to generate and apply the best evidence for collaborative healthcare choices for each patient and provider; to drive the process of discovery as a natural outgrowth of patient care; and to ensure innovation, quality, safety, and value in health care. In working toward this vision, discussions in previous efforts of the Roundtable and, more generally, the IOM have identified key features of a learning health system (Box 1-2).
Together, these characteristics allude to a virtuous cycle in which all healthcare stakeholders deliver established best practices and learn how to improve from the care delivered. This cycle ensures that learning can be perpetuated and that effective, quality care is delivered. The clinician is both the steward of information and the agent acting on behalf of the patient, but decision making and action are centered on the patient’s needs. Furthermore, it is not enough to be able to provide best practices; a learning health system must ensure that best practices are provided every time, all the time. These elements should all be embedded in a system that feeds back information and action in a seamless way, a system that regards knowledge and data as a public trust, respecting privacy yet acting in the public interest. Information technology is a clear foundation for the engine of a knowledge-driven system. Health care must depend on individuals who can be trusted without conflict to provide science-based advice and act for the well-being of the people they serve. Finally, all these parts must be brought together in a network that requires not only good leadership but also good followership, as individuals recognize and quickly adopt proven methods that work elsewhere. In realizing a learning health system, each of these elements must be embedded in an integrated model that provides relevant, real-time results to enable more effective care, encourage participatory and science-based decision making, and foster continuous learning for all healthcare stakeholders.
Moving Forward
In actuating this vision of a learning health system, value, science, and policy will be the fundamental driving forces. Value, or performance at
BOX 1-2
Learning Health System Characteristics
Culture: participatory, team-based, transparent, improving
Design and processes: patient-anchored and tested
Patients and public: fully and actively engaged
Decisions: informed, facilitated, shared, and coordinated
Care: starting with best practice, every time
Outcomes and costs: transparent and constantly assessed
Knowledge: ongoing, seamless product of services and research
Health information: a reliable, secure, and reusable resource
The data utility: data stewarded and used for the common good
Digital technology: the engine for continuous improvement
Trust fabric: strong, protected, and actively nurtured
Leadership: multi-focal, networked, and dynamic
SOURCE: Adapted from The Learning Healthcare System (IOM, 2007).
cost, denotes what is gained per dollar spent. Science generates evidence that informs and shapes care delivery, and policy encompasses the choices individuals make that define the rules of the game. Together, these three drivers make a holistic, systematic perspective on health care possible.
Current policy efforts are aimed at helping to bring a learning health system into practice. Just seven days before this workshop was held, President Barack Obama signed the ACA. The legislation not only created a new independent payment advisory board, but also established the Innovation Center at CMS and the Patient-Centered Outcomes Research Institute (PCORI). As a center dedicated to testing innovative payment and program service delivery methods, the Innovation Center has the potential to reduce Medicare and Medicaid costs substantially while enhancing health care quality. With a health system populated by countless alternative care delivery models, the United States can benefit immensely from the Center’s
testing of the feasibility, cost-effectiveness, and quality outcomes of different models. PCORI, another key provision of the ACA, has as its goal to advance the quality and relevance of evidence concerning medical conditions and ailments; this goal parallels a learning health system’s pursuit of evidence-based care and focus on value and quality. In establishing both of these centers, the healthcare reform legislation helps align provider incentives with patient-centered value and spurs the development of an integrated learning health system.
Furthermore, the ARRA will accelerate the adoption of health information technology and expand comparative CER through increased investment. The official establishment of the Office of the National Coordinator for Health Information Technology and the Federal Coordinating Council for Comparative Effectiveness Research has proven instrumental in fostering the adoption of electronic health records and the assessment of research on health care treatments and strategies, respectively.
Setting the Agenda
Moving forward with a learning health system will require identifying, understanding, and assessing both challenges and opportunities. These workshop sessions illustrate how to move forward on key elements such as science, patients, and value, as well as the communication and patient engagement that are so critical to success. In highlighting programs currently under way and discussing information technology as the engine for an integrated system, these sessions explore the next steps that will lead to the development of a learning health system.
REFERENCES
Berwick, D. 2009. What “patient-centered” should mean: Confessions of an extremist. Health Affairs 28(4):w555-w565.
Campaign for Effective Patient Care. 2009. Perception vs. reality: Evidence-based medicine, California voters, and the implications for health care reform. http://www.effectivepatientcare.org/images/0909%20CEPC%20Brownlee%20Report%20on%20EBM.pdf (accessed February 7, 2011).
Carman, K. L., M. Maurer, J. M. Yegian, P. Dardess, J. McGee, M. Evers, and K. O. Marlo. 2010. Evidence that consumers are skeptical about evidence-based health care. Health Affairs 29(7):1-7.
Docteur, E., and R. A. Berenson. 2009. How does the quality of U.S. health care compare internationally? Timely Analysis of Immediate Health Policy Issues. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1482677 (accessed June 17, 2011)
Fisher, E., D. Wennberg, T. Stukel, D. Gottlieb, F. Lucas, and Ã. Pinder. 2003. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Annals of Internal Medicine 138(4):273-287.
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2007. The learning healthcare system: Workshop summary. Washington, DC: The National Academies Press.
———. 2008. Knowing what works in health care : A roadmap for the nation. Washington, DC: The National Academies Press.
———. 2009. Initial national priorities for comparative effectiveness research. Washington, DC: The National Academies Press.
———. 2010a. Healthcare imperative : Lowering costs and improving outcomes : Workshop series summary. Washington, DC: The National Academies Press.
———. 2010b. Redesigning the clinical effectiveness research paradigm: Innovation and practice-based approaches: Workshop summary. Washington, DC: The National Academies Press.
———. 2010c. Value in health care accounting for cost, quality, safety, outcomes, and innovation : Workshop summary. Washington, DC: The National Academies Press.
———. 2011a. Clinical data as the basic staple of health learning: Creating and protecting a public good: Workshop summary. Washington, DC: The National Academies Press.
———. 2011b. Learning what works: Infrastructure required for comparative effectiveness research: Workshop summary. Washington, DC: The National Academies Press.
McGlynn, E. A., C. K. Cassel, S. T. Leatherman, A. DeCristofaro, and H. L. Smits. 2003. Establishing national goals for quality improvement. Med Care 41(1 suppl):I16-I29.
Murray, C. J. L., and J. Frenk. 2010. Ranking 37th—measuring the performance of the U.S. health care system. New England Journal of Medicine 362(2):98-99.
OECD (Organisation for Economic Co-Operation and Development). 2009. OECD health data. http://www.oecd.org/health/healthdata (accessed February 7, 2011).
Sepucha, K. R., and M. J. Barry. 2009. Making patient-centered cancer care a reality. Cancer 115(24):5610-5611.
Truffer, C. J., S. Keehan, S. Smith, J. Cylus, A. Sisko, J. A. Poisal, J. Lizonitz, and M. K. Clemens. 2010. Health spending projections through 2019: The recession’s impact continues. Health Affairs (Millwood) 29(3):522-529.
Zikmund-Fisher, B. J., M. P. Couper, E. Singer, C. A. Levin, F. J. Fowler, S. Ziniel, P. A. Ubel, and A. Fagerlin. 2010. The DECISIONS study: A nationwide survey of United States adults regarding 9 common medical decisions. Medical Decision Making 30(5 suppl):20S-34S.














