5
Governance and Accountability
Workshop chair Arthur Kellermann opened the second day of the workshop by noting that participants had done an excellent job of identifying the potential benefits and pitfalls of regionalization, as well as the many obstacles—political, economic, cultural, and other—that stand between us and the Institute of Medicine’s (IOM’s) vision of a regionalized, coordinated, and accountable emergency care system. He said that day 2 would focus on key strategies for moving the idea of regionalization forward, and doing so in a way that is effective, sustainable, creates a more efficient and resilient health care system, and improves patient outcomes.
The second day began with a presentation by Ricardo Martinez, M.D., former administrator of the National Highway Traffic Safety Administration (NHTSA) and in Dr. Kellermann’s words, “a driving force behind the creation of the Emergency Medical services (EMS) Agenda for the Future and many other contributions to emergency and trauma care in the United States.”
REGIONALIZATION IN THE MARKETPLACE OF IDEAS
Martinez began by asserting that the regionalization model will be adopted if it solves people’s problems. If it doesn’t, it won’t. It is the model itself that drives the rate of adoption. The market embraced iPod, Google, and other products, he said, because they worked very, very well. Great business models come out all the time, but you see a lot of them fall apart because they don’t actually solve a problem.
Martinez said the historical view that drives regionalization is getting
the right patient to the right place at the right time. “That’s a laudable goal. In fact, that is a goal that I have pushed for many, many years.” But this model has also driven a lot of what we see today, which is a surplus of resources at the top end of the scale, he said. For example, approximately two-thirds of physicians work in the tertiary, urban environment. Specialists and specialized interventions are increasingly concentrated there. At the other extreme, about 32-35 percent of emergency medicine physicians are non-board certified, and they are more likely to be in smaller hospitals in rural and suburban areas—facilities that have far fewer resources.
Martinez said that the intent of the regionalization model is to identify a certain number of patients in the EMS environment and move them to higher-level facilities. But he said this raises two structural questions. First, does this help a narrow group of patients or a broad group of patients? He would argue that the system helps a small number of emergency care patients quite a lot. However, he estimates that 95-98 percent of emergency care patients get no benefit from this system. While he is a strong believer in having the trauma system focus on those who need it most, the question becomes: what about all these other patients? “We are not focused on those patients right now,” he said.
Second, does this model help or hurt the facilities that participate in regionalized systems? He said he works with 150 emergency departments and many of them are suffering because of what he called a “one-way valve.” Because they have no way to work with the top-end facilities (through telemedicine or other means), a significant number of patients are transferred out. “In fact,” he said, “there are a lot of hospitals where their transfer rates are actually higher than their admission rates.” However, these hospitals only make money on admissions, and “so what is happening is they are dying off.” All those patients who are sick are transferred up, he said, not just for trauma, but often for evaluations, second opinions, and that type of thing. It is really a huge economic shift. “So what’s happening is, we are actually killing the access to care for [a] percentage of the population.”
Martinez asked whether this model is sustainable. Does it help everyone? Does it help just a little bit? “This is what we are putting in the marketplace of ideas.” It is a great idea to get the right patient to the right place at the right time. But the model has been “out there in the market for 30 years. Who is picking it up? Who is saying, ‘This works for me. This is great. I want this’?”
Martinez concluded that if you can’t change the market, and you can’t change the basic funding issues, “maybe what you need to do is change the model, so that all the other players see the benefit.” We are talking about emergency care coordination and emergency care patients, “yet we have been focusing [only] on a small part of that. Maybe we are missing a bigger opportunity.”
A key question, he said, is why can’t these lower-level hospitals take care of these patients, and what is the system doing to assist these hospitals? There are lots of opportunities in this area, Martinez said. Resources come in two categories—fixed or mobile. Equipment and technology are typically placed in fixed locations. Patients must be moved to them. Procedural skills are also often fixed (this is where the specialist is). Again, the patient has to be moved to the proceduralist. But he said, with the information technology infrastructure we have, cognitive skills can be moved to the patient.
In fact, he said, “we have an infrastructure that now allows us to think differently. It’s like us talking about telephone systems in the 1980s. It wouldn’t be the same conversation today, because things have changed.” For example, electronic collaboration is occurring more and more. Doctors needing a quick consult can send a picture and a note to another doctor and ask their opinion. He said, “The technology is already there. We just haven’t adapted it to our use.” Electronic medical records could easily include images. Remote consults could occur through text messaging; everything would be recorded as part of the patient record and would be reimbursable. That would be easy to do, and it would meet a currently unmet need.
He observed that in the medical home model, providers are being paid for integration and collaboration. “I would argue that these emergency care systems do that.” But, he added, emergency care and emergency physicians are currently excluded from the health information technology money. “We chose not to be involved,” he said. “But I’m telling you, these systems are all about integration and collaboration. It’s cutting off your nose to spite your face not to participate in that. That money should be used to build the systems we need in emergency care, without a doubt.”
In the past, Martinez said, system development was about getting the right patient to the right place at the right time. But he believes the focus should be: get the right resource to the right patient at the right place at the right time. “Just a small change [in wording],” he said, “but what it does is it opens up greater good to more patients.”
Rather than everything moving from community hospitals to referral centers, this re-envisioned model can go in both directions (see Figure 5-1). “You can start in one spot. Begin to develop nodes. Those nodes connect, because you can connect them, to become clusters, and clusters become networks. It doesn’t have to be top-down.” He said, “The reason why people opt out of these things is because there is nothing in it for them. CEOs say, ‘These people just take my patients and I never hear from them again. I get no financial value from it.’” Martinez declared, “We can change that.”
The goal should be to do the greatest good for the greatest number. Drive value through measurable quality for the entire system, so all of the players play with each other and there is something in it for everyone. Do no harm to those in the network.
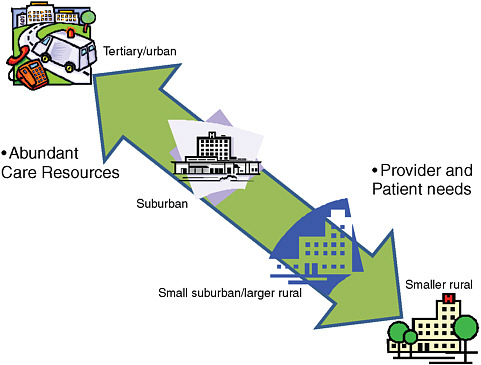
FIGURE 5-1 A more inclusive regionalization model.
SOURCE: Martinez (2009).
Martinez added, “I don’t even like the word ‘regionalization,’ because it has a lot of baggage.” He said, “Just change the name. ValuJet became AirTran. Change the name and start over—bring new people into the fold and begin to do things differently.” He proposed using the term “Integrated Networks of Care.”
THE STATE’S ROLE IN REGIONALIZATION
Bob Bass, executive director of the Maryland Institute for EMS Systems, said that grant programs were initiated to promote regionalization at the old U.S. Department of Health, Education, and Welfare (DHEW) and the Department of Transportation (DOT) in the 1970s. However, the consensus is that this approach to regionalization was not successful. Many of the regions failed.
An after-action report on the DHEW program completed in 1980 pointed to the critically important role that states played in legally empowering, funding, and coordinating regions. Bass said that in the cases where
states did not play that sort of role, regions struggled and generally were not successful.
After the demise of the DOT and DHEW grant programs, the DOT program continued, but without a significant grant component. There were efforts around the country to continue with a regionalized approach. Some were successful, but many were not, Bass said. Generally speaking, there was a lot of state involvement in the cases that were successful.
The 2006 IOM report on the Future of Emergency Care pointed to the need for coordinated, accountable regions where care is integrated. Bass said the IOM was really saying that there needs to be regionalization, which means the patients get to the most appropriate facility. But in some cases regionalization might be nothing more than a hospital declaring itself as a specialty center and telling EMS, “Bring your patients to us.” You really don’t have a system, he said, until you have the components that were presented in the IOM report. “It means that hospital and prehospital systems are integrated; that they are categorized; there are protocols and clinical pathways and standards of care that are uniform across the region; there is interoperable communications and data; and the system is legally empowered, funded, and publicly accountable.”
There have been varying degrees of success, he said, with respect to regionalization efforts. But he would argue that, based on history, it is critically important that states play a role. This helps to ensure that rather than just regions or regionalization, there is a systems approach that includes all of these elements, which are critically important to success and good outcomes.
OPERATION REGIONALIZATION
Dia Gainor, chief of the Emergency Medical Services Bureau for the State of Idaho and past-president of the National Association of EMS Officials, said that governance and accountability are “the core issue at hand” when considering what would be necessary to achieve regionalized and accountable emergency care systems. A unified sense of mission and purpose and a coherent strategy need to be deployed nationwide. This program and policy should be “military-like” in its cohesion and should perhaps have the title “Operation [Something].”
Demonstration projects are definitely in order, Gainor said, but there needs to be some common thinking about the kinds of systems that we are referring to, and the terminology that is used to describe them. There is a difference between the words “regionalization,” (whether it is used as a verb or not), and “systems” or “systemization.”
It is “very, very important,” Gainor continued, that we establish an extremely high degree of accountability, whether it’s in the planning pro-
cesses, the demonstration projects, or the long-term program. There will have to be multiple levels of ownership and multiple desks that bear the sign: “the buck stops here.” Someone needs to be held accountable for the performance in each of the various systems. With respect to performance assessment, we need to actively measure, quantify, and understand how systems are performing and hold them accountable for that performance.
Ownership and turf is an issue that affects hospitals, but also local EMS systems, she said. She said that after 17 years as state EMS director, she has the scars to prove that this can be a very dangerous crowd. “So understanding what their motivations and needs are is very important.”
This comes into play not only with respect to governance, but also with respect to sharing resources. She asked, “Is it really possible for the fire department to share personnel, equipment, devices, or data-reporting processes with the neighboring—if not competing—hospital-run ambulance service? Can that really be done?”
Ultimately, she said, there are some things that we should not tolerate—differences that occur when we cross a state line or a county line. There is a minimum standard that we should not allow to be lowered, as in the case of aviation standards that are applied by the Federal Aviation Administration. EMS is something that local elected officials, the public at large, and others need to regard as a public utility—as trustworthy as flipping a switch to turn on the lights in the house or clean drinking water. Those are expectations that we have, and it is what is owed to citizens.
To fully realize this vision, great effort will need to be placed on reviewing and overhauling state EMS laws throughout the nation. Many are now 35 years old, and health care has evolved dramatically over that time. With only a few exceptions—notably, North Carolina and Illinois—states by and large are focused on individual agency regulation rather than combinations of agencies or systems. Few consider their performance within regions.
WHAT’S IN IT FOR US?
Ed Racht, chief medical officer and vice president of medical affairs for Piedmont-Newnan Hospital in Georgia, said that 2 years ago he had attended a meeting in Austin, Texas that brought together hospital CEOs, cardiologists, and interventional cardiologists to discuss regionalization and ways to improve ST-elevation myocardial infarction (STEMI) care. They discussed prehospital transmission, intervention, and how patients would be distributed.
Racht said one of the hospital CEOs stood up and asked the toughest question he had heard in his career: “if revascularization in the shortest period of time is our goal and it’s the best thing we can do for our patients. … If we commit that every single STEMI patient you bring us
will be revascularized within 20-30 minutes after they enter our facility, will you commit to bring every STEMI [patient] in the region to our hospital?”
Racht said, “It’s the first time I have ever heard sphincters slam shut in an entire group of individuals.” Everyone had agreed that getting patients revascularized was the goal and it was why they were all there. Having one facility put the cardiologists in the hospital and in the catheterization lab and provide 24/7 staffing for whatever was needed would be very costly. But they said they would only do it if they received every eligible patient—a strategy that would deprive all other hospitals in the region of the revenue from these cases.
Racht said “the governance and accountability piece really gets to the heart of who is in charge, who is accountable, who makes the decisions.” Players have different motivations and different fears. Every CEO, chief medical officer, every director has the view: I’m in charge of my world. If someone else is going to try to come in and be in charge of my world, “I’m going to have to sort out whether I want that to happen or not, because I have decisions that I’m personally accountable for.”
People only collaborate, Racht said, if they feel like it will have value for them. Efforts to regionalize stroke care, for example, will be met with questions centered on “what’s in it for us?” But everybody should be at the table.
Efforts to promote accountability require additional transparency, and transparency is extraordinarily threatening to some, he continued. “You can see what our mortality is and I can see what your mortality is. … You can read all of it in USA Today and anywhere else you want to read it. There is generally a fair amount of discomfort.” But transparency is central in driving change, Racht maintained.
The current reimbursement model does not promote “systemness,” Racht said, and the regulatory structure is not ideal. He noted that paramedics can’t be placed in the operating room to learn intubation skills—depending on state and local regulations. However, there are opportunities for improvement, such as the efficiencies that collaborations and innovative approaches can provide.
BUILDING “SYSTEMNESS”
Greg Mears, medical director for the North Carolina Office of Emergency Medical Services, said that North Carolina’s trauma system was born out of the 1966 National Academy of Sciences publication Accidental Death and Disability: The Neglected Disease of Modern Society and the 1973 EMS Act. The system is now very mature, he said (see Box 5-1).
It was originally developed through state legislation in a very top-down
|
BOX 5-1 Lessons Learned in North Carolina
Lessons Learned
SOURCE: Mears (2009). |
approach. Mears said “we have done very well with our trauma system, but we certainly have a lot to learn from the non-trauma systems of care.” Also, while the state has 122 hospitals, only 12 are trauma centers. They now must move to an inclusive approach where all hospitals participate in the trauma system at some level.
Mears said North Carolina has taken a different approach with respect to STEMI, stroke, and now, pediatric systems. With stroke, there was an initial attempt to replicate the more top-down trauma approach, using a legislative template from the American Heart Association (AHA); however, that model “had issues [and it] created some division among the health care community.” He said “the stroke legislation was successful once we started from a local perspective and built up to a regional approach, instead relying on a top-down model.” He noted that North Carolina’s STEMI system of care is now used as a model by the AHA and has been very successful using a more regional approach. These programs are very similar conceptually, Mears said, but one has grown up locally, one regionally, and one from the top down at the state level. He said North Carolina has sought to implement a system approach instead of promoting individual silos. For example,
North Carolina is one of the few states in the country that requires counties to group together all of their EMS resources, write a plan, and operate as a system, instead of operating as individual EMS agencies.
In North Carolina there are 540 EMS agencies, but they operate as 100 systems. “That has made a huge difference in how we approach individual patient scenarios and how we structure the entry point to regionalization.” This approach “allows us to coordinate and be much more reactive,” Mears said.
The state requires a “high level of accountability,” Mears said, but regions “have been given a lot of latitude to develop,” based on their individual needs. One size certainly does not fit all. North Carolina has been able to push forward with data systems and performance measures to establish metrics for optimal patient care. Transparency and benchmarking have helped to pull everyone on board, Mears said. For those health care entities with measures that aren’t equivalent to their peers, they are still in a better position to improve than those who have not provided measures at all, since missing information is likely to generate even more questions. The transparency piece has pulled in many of the larger health care facilities and EMS agencies that weren’t initially interested in participating.
The other thing is that money doesn’t buy everything. “It is certainly possible to throw a lot of money at a lot of projects and still not be successful,” Mears said. Instead, “we have put a lot of effort into building collaborative relationships. The data systems we have developed promote the concept of linkage,” he said. Rather than focusing on parameters that capture door-to-treatment endpoint, they prefer parameters that focus on initial health care contact-to-treatment. “That encourages everybody to work together, where each component of a patient’s care is dependent on another. They have to communicate. Information has to flow well.” Measuring performance improvement, increasing transparency, and peer pressure all drive the concept of “systemness.” But system-building still occurs one patient at a time, Mears said.
AUDIENCE DISCUSSION
Neurosurgeon Alex Valadka said it seems clear that one of the major lessons here is that there needs to be a combination of strong leadership with collaboration and buy-in—people willing to work together.
But to follow up with Racht, he asked what happened in that room when the CEO proposed to pour in tons of resources and take every STEMI patient, alienating the other providers in the region. How was that resolved?
Racht said, “Interestingly, nothing happened in that room. The question wasn’t answered.” But, ironically, two things did come up after that,
he said. First, one of the cardiovascular groups said that in that case, they would be looking into every single case to make sure the care had been done right. And second, some requested to see an organizational chart of the local EMS system to see who had the authority to make that kind of change. So, he said, it was all about, “who is in charge here?” Who can force us to do X, Y, or Z?
Martinez commented that the model was wrong. The business proposition was, “You send me everything. In return, I’ll take everything you have.” Instead, the model should be: “You send me everything, and with this resource I’m creating, I will give you access to cardiology consultations and other resources, so you can keep all the [other] patients who don’t need to come here.” Racht commented that a proposal that did come up later was about rotating that function, on a calendar basis, through the various facilities and cardiovascular groups so that the patient load would be shared.
Defining Terms
Panel chairman Bob Bailey asked if someone on the panel would clearly define the terms region, regionalization, system, and catchment area. Bass said that regionalization is the concept of getting patients to the most appropriate facility, based on their condition. A region is simply a geographic area. It could be one county, two counties, or less than a county. Typically, it has an administrative lead entity that is responsible for coordinating regionalization within that area.
A region is very different from a catchment area, Bass continued. A catchment area is something Maryland has examined a lot, through geographic information system (GIS) mapping and color-coding, to look at patient distributions on a statewide basis. Those patients cross a lot of regional and, sometimes, state lines. Sometimes they end up going from one region to another, because a specialty-care resource is not available within a particular region.
Bass said that a regional system is not simply a region in which regionalization occurs. It is much more comprehensive. “You have additional capabilities, beyond simply saying you are going to take a patient to a particular hospital. Your resources are integrated. The care is integrated. It’s a continuum of care, from prehospital to hospital care. The care is integrated and coordinated. The prehospital people work together and the hospitals work together. You have EMS protocols that require that patients be taken to hospitals that are most appropriate for their care—in some cases, bypassing other hospitals—and transfer protocols and guidelines along the same lines.”
Bass elaborated further: “You have uniform clinical pathways for, let’s say, stroke care within the hospital. If you are taking a patient for stroke care to a hospital, regardless of which hospital you are taking them to that is a stroke center, they are going to have the same clinical pathway, the same quality of care. You have interoperable communications, where you have real-time situational awareness, where you know what’s happening in the system, who has capacity, what is happening day-to-day, or during a mass casualty incident. You have data that is interoperable, exchangeable, and addresses a continuum of care—not just prehospital, not just hospital, but care in its entirety—the concept that [Racht] raised and that others have raised. It’s not about just door-to-balloon; it’s initial patient contact in the field or, in an ER [emergency room] that is not PCI-capable [percutaneous coronary intervention-capable], to when that patient gets revascularized. It’s accountability, meaning that we have the data, we look at it, and what is happening is transparent. It’s the legal empowerment that is necessary to ensure that all of those things can occur and the funding exists to make them happen,” Bass concluded.
Gainor said that, structurally, a system is an area within which multiple fixed, mobile, and human resources operate within a universal boundary, with a single body of governance. Most often this is state-based, with one or more regions, she said.
Valadka said that an explicit part of the definition of regionalization has to be efficient use of resources. He said this will become a much bigger issue in the future, as the population continues to age and the number of physicians, and especially nurses, lags behind. “We are not going to be able to dump everything on the local Mecca,” he said, “so we need to be much more efficient in how we do this.”
However, Valadka observed that the Committee on Trauma takes “a very loose approach” to defining a region. He said they have surveyed entire states, such as Wyoming, which are geographically large but thinly populated, and they have surveyed parts of states, such as San Diego.
Some of the most interesting areas are those that jut up against several states, such as Memphis, Tennessee; St. Louis, Missouri; and Kansas City, Missouri. The Cincinnati regional area includes three states—Ohio, Kentucky, and Indiana. Discussions about how to define and govern a region often seem to follow along natural political lines—a state boundary or parts of states. But in these areas, the dividing lines are not as clean. Valadka asked Bass to describe how Maryland, Virginia, and the District of Columbia [DC] work together.
Bass said that that was a sensitive question. Looking back over his career, one of his most significant failures has been the inability to create interoperability between Northern Virginia, DC, and Maryland, particularly
as it relates to mass casualty incidents, but also just the day-to-day exchange of data that would enable them to gain situational awareness and be aware if one area is overloaded and spilling over into the other state.
“It has been a challenge,” he said. “I probably had a concussion for the first five years that I tried to do that, just beating my head against an immovable object.” He noted that “the laws in the three jurisdictions are very different. The liability exposure is very different. They are very siloed.”
Still, he said, “We share a catchment area.” We recognize that from a catchment standpoint, we have to cross those boundaries. On a day-to-day basis, in terms of regionalization, “we do okay.” But, he acknowledged, “We certainly don’t have all the tools at our disposal that we would like to have, to make sure that the system in that area of our state and DC and Northern Virginia is better integrated. But I’m not going to give up. We are going to keep trying.”
Variable State-Level Leadership
David Stuhlmiller, an emergency physician at Westchester Medical Center, noted that regionalization already occurs across the country in certain situations. But it’s very haphazard. State leadership is inconsistent across the country. Not every state is interested in trying to regulate what hospitals do, and especially what inter-facility transports occur and who is providing the care in those inter-facility transports.
Bass replied that states were late getting into the game in the 1970s, but eventually did get in. By the late 1970s, many states were engaged. He agrees that if you go look at what happened to those state offices of EMS over the last two or three decades, there is great variability. “There is great variation state to state [and] great variation region to region.”
But, “You sort of get what you pay for,” Bass said. In some states, some state offices of EMS are down to two and three employees. In some states, these offices don’t even license EMS providers and are relegated to a coordinating/planning function.
So many states are really not up to the task today, Bass said. “They don’t have the funding. They don’t have the resources. In certain circumstances, as you point out, they don’t have the motivation.” Sometimes that is because they are strained by what they are already trying to do. “For many offices of EMS, their principal function is to license ambulances, it’s not about building a system.”
But in places like Maryland, North Carolina, and Idaho, Bass noted, “the state offices have managed to hang in there and have been appropriately supported by their states and have created an environment in which this regionalization can occur, with a systems approach, with all of these different elements.”
Mears agreed that “the state EMS offices certainly have to be leaders.” When you look historically at regionalization in any state, Mears said, it typically occurred because there was some enabling legislation or law. Prior to that law and the regulatory ability it brought, there was a lot of collaboration, advocacy, and behind-the-scenes work. “In order to manage anything, you have to have information.” Once you have information, then you can empower the process. “I think [that] is the future for state EMS offices,” Mears said.
He said an example of a cross-state solution that was worked out by a local region in North Carolina related to STEMIs. An EMS agency could take a patient by helicopter to a facility in the center of the state or they could take a patient the same distance and reach a facility in a neighboring state. If they took the patient into the other state, they could not obtain any outcome information on the patient or get feedback on the quality of care. This out-of-state-hospital was not willing to share their door-to-balloon times or any related information. But if EMS kept the patient in state, they could get that information.
Essentially, the EMS agency told the out-of-state hospital, “If you want us to continue to bring patients, we need this data, and until we start seeing it, all of our patients will be transported to the facility that is willing to provide information and partner in the system of care.” Within 30 days, data was flowing both ways from the out-of-state hospital and the system of care was functional, Mears said.
So, he concluded, part of this can be worked out locally. “But you have to have the information. You have to have the performance measures.” You can drive that at the state level, he said.
Regionalization of Pediatric Services
Jeffrey Upperman, from Children’s Hospital in Los Angeles, asked Mears if he would expand on his earlier comments about pediatric regionalization. In pediatrics, Upperman said, resources are typically focused on the 0-4 or 0-5 age range (especially relating to congenital anomalies). For a host of reasons, it has been “hard to get folks to focus on the medically injured population.”
Upperman said the unintended consequence of our system—or our environment—has been that, “if you want to take care of all these kids, you have to take care of everything. If we are taking some of those neonatal cases and those other cases and not giving back to other facilities, they will say, you can go ahead and take this 10-year-old [with a] runny nose and other cases like that. So now we have capacity issues—we don’t even have beds for the high-end things that supposedly we want to help them with.” He said, “My view is we’re all in this together, let’s share.” But there had
been unintended consequences in terms of flow and resources and he said it might be helpful to hear more about North Carolina’s experience.
Mears said that “the concept we try to promote in developing these systems is to start from the bottom up.” EMS agencies are grouped into systems at the county level. The next layer is to require that system to communicate with all of the hospitals in their referral area and with their specialty centers, including the trauma centers, PCI centers, and stroke centers (the state has no pediatric trauma centers). They then pull together and work out a plan that says, if we have a patient that meets specific criteria, here are these facilities that we have identified that have the resources and the patient will be taken there. So the transports are based on specific patient parameters and the resources that are in the area. “It’s not a complete bypass perspective,” Mears said.
“That has, in general, worked well,” Mears added. We have gotten through this on the STEMI side and the stroke side. For pediatrics, trying to identify the patients has been more challenging. They have used some of the Illinois criteria and other approaches.
Fundamentally, though, Mears continued, “the concept is collaboration.” It relies heavily on data. “We have 100 percent of our EMS data [and] 100 percent of our emergency department data,” plus quarterly hospital inpatient data. This provides “a pretty good picture” which can be used to evaluate results. He said this approach has worked much better than they had anticipated.
Building Comfort with Telemedicine
Linda Cole, from Children’s Healthcare of Atlanta, said that a lot of the ED overcrowding problem stems from people who are transferred from outlying facilities. She said the hospital has started looking at tele-trauma, tele-emergency department visits. They have visited other states to learn from their experience and have consistently heard one thing: you can get the consultants to the table, but the real fear lies with the referring physician. The hospital CEOs want to keep those patients, because that’s the livelihood of their hospital. But it’s the ED physician or the specialist in the ED that wants to get the patient out and doesn’t particularly want to go into the telemedicine consult. She asked if the panelists had any advice on helping these physicians feel more comfortable and supported in the process, aside from education and a lot of handholding.
Racht agreed that even when a seasoned clinician says “you’re good, you’re okay,” the referring physician may still be uncomfortable and may still have liability concerns. “If I’m on the ground, I still feel like it’s my responsibility,” Racht said. “Frankly,” he said, “tele-consultation and telemedicine is such a new and odd concept, it’s going to take some time to say
that it’s just like having your consultant buddy right beside you, except he or she is electronic.” If the referring physician is uneasy, he or she will say “I’m not comfortable with what you are giving me. Can you help me move [this patient] to the next level?”
Replicating Successful State Models
David Sklar, from the University of New Mexico Health Sciences Center, said “Yesterday we heard a lot about how regionalization has improved care in a variety of areas and also how there are multiple barriers to overcome. As Kellermann said, our challenge for today is to figure out how to come up with some solutions to these barriers.” Sklar added, “It seems we will not all be able to replicate Maryland or other states. What we need to do is identify the problems—whether it be in trauma care or pediatric care or sepsis care—and then realize, along with the public, that if we do things differently, it will make a difference. We can then present that to states or regions or community groups and give them the responsibility to solve the problem in the way that they can with the resources they have.”
Bass agreed, saying, “I don’t think you can take Maryland, or Idaho, or North Carolina, or Texas, and transpose that.… The approach that we use in Maryland would never work” in certain other places. But he said, “I think we know the building blocks.” We know “the functions and components that have to be there.” Most importantly, the goal has to be to get the right patient to the right hospital in the right time with the right care.
Bass agreed that each state and region will have to find solutions that are suited to (and realistic for) that local area. But he added, “In my heart of hearts, I believe that you need a strong state. Not just a regulator, but a resource, somebody who can help facilitate.” Mears observed that many regionalized approaches exist in different branches of state government, but they don’t communicate with each other. The states that have been successful are the ones that talk and have collaborated, even within state government.
John Fildes of the University of Nevada and the American College of Surgeons said, “I’m increasingly uncomfortable with the tone of the discussion this morning, about people wanting to fall back, people saying we couldn’t possibly emulate the best practice of one state in another state, that we couldn’t possibly emulate the best practice in IT, because we just can’t do that. I think what we need to do is catch this train, or it’s going to leave us behind.” He said we need to “move forward and find a way to get it done.”
“We are here,” Fildes continued, “because there was a report in 2006 that said emergency care is in crisis, and one of the steps in remedying that might be regionalization, which … means IT support, access, and quality.” He noted that we have challenges in each of these areas. There are quality concerns stemming from specialty surgical and specialty care shortages and
from poor IT infrastructure and poor IT support, and there is legislative and regulatory language that actually binds our hands from doing the right thing, he said. We have access problems because we have limited manpower or manpower that is now distributed, particularly for time-sensitive conditions; we have barriers, because many people we serve are uninsured or under-insured. There is defensive medicine because of liability, which prevents us from bending the cost curve down. We are being asked to look forward and come up with some solutions to move us out of this position.
Bass said we have general agreement on what needs to be in place, but that we all can’t take the same road in terms how it is implemented. “There has to be variation.” But, he said, “I would hope that we are all in agreement that regionalization of care, a systems approach to providing care for people with time-critical conditions, is something we are all committed to.”
Gainor agreed that “clearly, no cookie cutters would work.” But, she added, “At the same time, uncontrolled, random variation is dangerous.”
Generating Political Will
Nels Sanddal, president of the Critical Illness and Trauma Foundation, said that trauma systems seem to have four different kinds of challenges relating to governance—in particular, to statutory and administrative authority. Three of these are fairly easy to make recommendations on, but the fourth is more challenging.
For those who don’t have a statute or any authority—“that’s easy, get some,” he said. For those who have statutory authority and we aren’t using it well—“that’s easy: do some more, do it better, refine it.” For those who have statutory authority, but don’t have the financial or human resources to implement it—“that’s easy. Get some financial resources.”
But the final one is harder: we have the authority and we have the administrative structure, but we don’t have the political will. Even if we can demonstrate clearly that that lack of political will is killing patients, it’s not enough. Sanddal asked the panelists, “where does that political will come from? How can it be engendered?”
Bass responded that Maryland has struggled recently with respect to STEMI care. He said this has been “a wake-up call,” because earlier efforts with regard to perinatal, eye/hand trauma, and stroke were much easier. He said “we are pretty good at bringing stakeholders together, [and] building consensus. We are flexible. We have been successful.”
But he said that for the last two years he has been stymied on the STEMI issue. There have been three drafts of the regulation and each one has received a strong political reaction, including letter-writing campaigns to the leaders of the House and Senate, the governor, and every key committee
chairman. “It’s clear to me that it’s nothing short of a buzz-saw if we walk through it, and so we [had to] regroup.”
Bass said that they plan to continue their efforts. “We will talk to the stakeholders, put out the data, show how this makes a difference, and then seek to develop some transparency. The key is to put the information out there and let the public know. In the end, as a little state agency, we are going to get torn up if we try to go against this. But I think if we use the power of information and work with stakeholders and the public will, we can show that this, in fact, will save lives. That’s how we are planning to continue to tackle this issue.”
Mears said, “We have no state regulation for a STEMI system at all. But we have great data and great transparency.” This has driven large hospitals in the state to participate. “I think there are many ways that you can bring a system of care together,” he said. Certainly it’s nice to have the legislation and the authority, but you get into the issues you mentioned: “Do you have the manpower to enforce it? Do you have the political ability to enforce it?” Transparency with data systems and performance measures is “a big soother of all that.”
Bailey added that, historically, “it also helps to have an outside-the-bureaucracy champion. They can have more clout than a state EMS director who is part of the bureaucracy standing by themselves and trying to push that issue forward,” he said.
Gainor asserted that there are some things that are too important to leave to political will. She said “none of us have to worry about whether there is sufficient political will in communities or a county about whether stop signs should be red and octagonal, with white letters of this font and size. It’s too important to leave to geopolitical variation. There are times like that where … a judicious level of higher common denominator needs to get implemented nationally.”
But Racht added, “The most important reference material for an elected official is the morning paper… . The Newsweek article with the guy floating in the pool probably did more for systems implementing out-of-hospital hypothermia … than anything we can publish in Resuscitation.” Bass agreed, saying, “It’s not only important for an elected official, but it may be even more so for an appointed official.”
REFERENCES
Martinez, R. 2009. PowerPoint slide presented at the Regionalizing Emergency Care Workshop, Washington, DC.
Mears, G. 2009. PowerPoint slide presented at the Regionalizing Emergency Care Workshop, Washington, DC.
NAS and NRC (National Academy of Sciences and National Research Council). 1966. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: National Academy of Sciences.


















