11
Impact of Cultural, Social, and Community Environments on Home Care
Steven M. Albert
The home environment is critical for maintaining health and well-being among the medically ill and people living with disabilities. Access to appropriate supportive care technologies and home health care services depends in part on where homes are located, what sorts of spaces are available for care in the home, and whether basic services (such as utilities) are reliable. These aspects of home environments are difficult to measure, even when features of homes are narrowly defined and only a single attribute, such as safety, is considered (Gitlin, 2003). Measurement challenges become more complex when considering that each of these environmental features also has a cultural or social component. Homes are located in neighborhoods, where home health care providers may not feel welcome or safe because of crime in a low-income neighborhood and discrimination or suspicion in a higher income one. Homes differ in their spaces available for care but also in the willingness of families to make these spaces available, adapt them as needed, and work with home health staff to provide care. Also, utilities, telephone service, and access to services differ by community, with some communities well serviced and others shortchanged. Thus, the home environment is nested in social and cultural layers that may lead to different home care outcomes, even with similar patients and common home environments (Barris et al., 1985).
The cultural component is immediately visible in family adaptation to home care. Families differ in the degree to which they reorganize themselves and their living spaces to accommodate care for the disabled or medically unstable (Albert, 1990), with different tolerance for disorder and different strategies for reducing such disorder (Rubinstein, 1990).
Consider the family facing end-of-life care for a medically unstable older person or child. For some families, hospice and death in the home is unthinkable (or perhaps not possible if home hospice services are unavailable). For other families, hospice and death in the home is the preferred outcome. The same may apply to other medical technologies, such as home infusion technologies, or to different types of care, such as managing the demented or incontinent patient at home. In the broadest sense, what kind of home care a patient receives depends to some degree on the meaning of “home”—that is, whether families consider these sorts of adaptations appropriate, along with more obvious home and community environmental constraints.
In this sense, cultural, social, and community environments must also be considered as human or ergonomic factors relevant to the adoption and successful use of home care technologies. Consider one model of technology adoption that has been applied to the use of consumer health information technology, the patient technology acceptance model (Or et al., 2006; Or and Karsh, 2009). In this approach, key determinants of acceptance of Internet monitoring of health status among patients with cardiac disease included perceived usefulness of the technology (performance expectancy), perceived ease of use (effort expectancy), and the perceived sense that others would use such a technology in similar circumstances (subjective norm). Each of these determinants has a cultural, social, or community component. Perceived usefulness depends in part on contact with providers, which is affected by features of a patient’s community. Perceived ease of use depends on social support from families, whether families will help maintain technologies, and how receptive they are to instruction from home health care providers. Finally, subjective norms involve social influence and clearly depend on the kinds of social contact families have, where they live, and how insular they are in culture or language.
The significance of this dimension of home care should not be underrated. One middle-aged African American caregiver followed in our research had adapted her home to accommodate advanced dementia care of her mother. The hospital bed was centrally placed in the living room. She had attached a crib mobile to the bed and replaced its objects with photographs of family members and other keepsakes important to her mother. A commode was placed near the bed, and she herself slept in an adjacent room to monitor her mother at night. The bookcases and closet served as storage spaces for medical supplies and adult diapers. Guests who visited had to pass by the elder as they entered the house and were expected to engage her in conversation. The caregiver said her mother was “the best looking and best cared-for person with Alzheimer’s disease in Philadelphia.” Not every family is willing or able to make these accommodations, as in the case of another caregiver in this case series, who removed a similarly impaired
person from her home because of strain with her husband and fear of the effect of such care on her children.
This kind of variation suggests a need to consider the full spectrum of social-ecological factors in home care. The social-ecological approach considers the interplay among individual factors, social relationships, and community environments (McElroy et al., 1988). Visually, it can be imagined as a series of concentric circles, with the individual in the smallest circle at the center. Progressively expanding circles radiate outward that first include social relationships and then community environments. Beyond the community sphere is a larger circle encompassing public policies and laws that regulate provision of home care. The value of this approach is its ability to show how actions in one domain depend on, or may influence, actions in another domain; thus, changes in the individual domain may depend on changes in family or social relationships. More particularly, how families think about the meaning of a home or household may affect decisions to bring certain medical technologies or services into the home. How families think about these issues will depend on cultural factors (shared ideas about what’s appropriate in a household or living space) and social norms, such as community accommodation of home care.
To examine the effect of cultural, social, and community environments on home care, I begin with a brief treatment of the social-ecological model as it applies to these home care environments. I focus particularly on culture as it may be relevant to home care, the least studied of these elements.
HOME CARE AND THE SOCIAL-ECOLOGICAL MODEL
The social-ecological model emerged from ecological systems theory (Bronfenbrenner, 1979), which explicitly sought to examine transactions between persons and their environments. The model stresses cross-level influences, in which community or organizational environments can shape individual behavior (top-down effects), but also examines how individuals form groups or take actions that may affect higher level organizational or community spheres (bottom-up effects). The Centers for Disease Control and Prevention has incorporated social-ecological models into a number of its health promotion and disease prevention efforts.
The simple onion or Russian doll rendering of social-ecological relations as concentric circles is not in itself very informative. However, flowchart models based on such relationships can be useful for specifying hypothesized cross-level influences. One such flow diagram for decisions to adapt homes for advanced medical technology is shown in Figure 11-1.
The figure shows the four levels mentioned earlier: (1) individual, (2) family social relations, (3) community-neighborhood effects, and (4) the policy domain. At each level, the relevant agent faces a challenge. At the
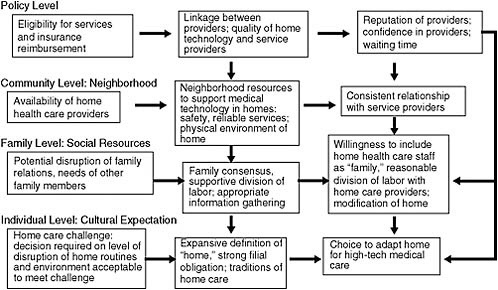
FIGURE 11-1 Social-ecological model adapted for home care research: Adaptation of homes for advanced medical technologies.
level of the individual is a home care challenge, in which a family caregiver must decide what level of disruption of home routines and environments is acceptable and whether to adapt a home for an advanced medical technology, such as home infusion or ventilator support. At the level of the family and social relations, the challenge is potential disruption of family relations and reconciling the demands of home care with the needs of other family members. At the level of the community, the challenge is the availability of home health care providers for a neighborhood. The policy level includes constraints on home care involving program eligibility and insurance.
Each of these challenges is addressed by resources (or ineffectively managed because of particular obstacles) specific to that level of social ecology. At the individual level, cultural expectations, such as an expansive definition of “home” that includes medical care, a strong sense of filial obligation, and traditions of home care, may allow families to decide in favor of adapting homes for advanced medical technologies. At the level of family social relations, family consensus, a supportive division of labor, and appropriate information gathering respond to the challenge of potential disruption of family relations. Similarly, community factors, such as neighborhood resources to support medical technology in homes, may lessen the impact of low availability of home health care agency services.
Most significant for the social-ecological approach are cross-level influences shown by arrows that cut across levels indicated in the figure. Thus, family consensus, a supportive division of labor, and appropriate information gathering at the level of social relations may support individual cultural expectations about home care. Likewise, a consistent relationship with service providers at the level of the neighborhood may reinforce proadaptation resources at the level of the family, such as willingness to include home health care staff as “family,” and a reasonable division of labor with home care providers. These in turn will support cultural expectations for adapting homes to provide care.
Few studies have examined the full range of determinants of home care specified in the social-ecological framework. Most studies cover only a few of the levels or paths linking levels. I turn now to features of each level in the social-ecological model relevant to home care.
THE CULTURAL CONTEXT OF HOME CARE
Culture affects the day-to-day organization of care. Consider the idea of partnership between families and nurses sought by home health care agencies. Agencies rightly recognize that optimal self-management of disease and a person’s return to function depend on a reasonable division of labor, shared information, and the willingness of family caregivers to learn rehabilitation and nursing protocols, medication administration, the use of assistive technologies, and the like (Wolff et al., 2009). But a family’s involvement may depend on how they define this partnership and, in particular, whether or not the home health care provider is considered part of the family (Knox and Thobaben, 1997; McGarry, 2009). Similar effects of culture may be evident in the willingness of families to accept telehealth technology, express their degree of burden or need for help, or seek hospice care at the end of life.
By culture anthropologists refer to shared beliefs, knowledge, feelings, and objects that have a “directive force” or motivational quality (D’Andrade, 1995). Culture leads people to categorize and assign meanings, expect certain behaviors, and act in particular ways. A simple example can be seen in ideas about gender and height. Americans for the most part prefer that husbands be taller than wives. People notice when this expectation is violated. Some may even make this a consideration in the choice of a spouse. This gendered approach to height may reflect other asymmetries between men and women, such as disparities in wages. While the strength of this cultural expectation may be waning (and may vary across groups defined by socioeconomic status), it gives a feel for the subtle but powerful influence of culture.
How do people identify these cultural expectations, and how might they be relevant for decisions about home care? One productive approach is
to elicit concepts using techniques from cognitive anthropology. Essentially, this approach extends investigation of folk taxonomies (e.g., colors, plants, pottery, kinship, emotions), the stock-in-trade of cognitive anthropology, into broader domains. Early on, in such an investigation I conducted for caregiver tasks, I determined that caregivers distinguished among emotional, cognitive, and physical disability support (Albert, 1991). More recently, the same technique has been used to elicit expectations regarding more abstract cultural domains, such as what makes success in life, leisure activity, social support, and family relationships (Dressler et al., 2005). For the latter, Dressler and colleagues asked a sample of Brazilians to list the goods or possessions people need to lead a good life, or the activities people typically engage in during their free time, or who they typically turn to for different kinds of support and subjected these lists to formal analysis designed to examine the degree of consensus across respondents. As evidence of shared culture, they found a single shared “cultural answer key,” along with individual variation. Notably, people whose lists or ratings were not consonant with the dominant cultural pattern were more likely to have poorer mental and physical health and even higher blood pressure.
In the cultural domain of home care, it would be valuable to conduct a similar investigation. Some potential elicitation frames might include the following:
-
What changes in your home would be appropriate when a family member is seriously ill and may die?
-
What changes in your household would you need to make in order to provide quality care for a family member receiving home health care services?
-
What aspects of a home make it hard or easy for a home health care worker to do his or her job?
Family members with experience of home care would be likely to generate a long list of answers to the first elicitation, which might include hospice services, infusion technologies, a hospital bed, a commode, smart home telemonitoring, more reliable telephone or utility service, modifications to the home to increase access, a place to store medical supplies, a separate place for visitors or other family members, and perhaps others. Some caregivers would produce shorter lists, some longer, but it is likely that a single cultural consensus would emerge. This elicitation would allow a first look at the cultural domain of home care. A reasonable hypothesis would involve less efficient decision making (and perhaps poorer outcomes for patients) by caregivers who do not express the consensus view.
This approach to culture does not involve differences among ethnicities or people who speak different languages but rather the operation of culture in
a population. Family caregivers and health care professionals in a single culture may differ in expectations for care or home accommodation, but these differences may be less salient than cross-cultural differences associated with ethnicity, race, country, or language. A growing body of research suggests that expectations regarding care differ across cultures (Sommer et al., 1999). For example, cultures differ in the degree to which pain, limitation in activity, or cognitive impairment is considered an appropriate cause for medical intervention. In the United States, minorities are less likely to use skilled nursing facilities and perhaps more likely to tolerate dementia and old-age disability at home (Hinton and Levkoff, 1999; Whitehouse et al., 2005).
The elicitation of home care culture described above can be used to identify subcultures and also differences across cultures. We turn now to some cross-cultural differences identified for expectations of home care.
Commitment to Family Care
Ethnic and cultural groups differ in their commitment to family care. African Americans are more likely than whites to endorse the primacy of family care (Dilworth-Anderson et al., 2005) and accordingly are less likely to make use of formal long-term care, including respite, home care, adult day programs, skilled nursing facilities, and hospice. Similarly, Latinos delay institutionalization relative to whites; a higher cultural value assigned to family care leads to more positive views of family caregiving, which in turn leads to a negative evaluation of skilled nursing facilities as an option for dementia or end-of-life care (Mausbach et al., 2004).
Differences in commitment to family care are based on cultural norms of filial piety or obligation. The concept of xiao, or filial piety, is a well-developed element in Chinese culture. However, it is strongly gendered, so that the burden of such care falls on adult daughters or daughters-in-law, not sons (Zhan, 2004). Caregiving in American families shows a more variegated pattern, both in underlying concepts and in the division of labor (although caregiving remains mostly women’s work). Norms of filial obligation are heavily influenced by education, with greater acceptability and use of skilled nursing home care evident among more highly educated people. As minorities advance through the educational and occupational ladders, these differences in recourse to skilled care may lessen.
Little information is available for differences among cultural groups in receptivity to home adaptation. Given differences in recourse to institutional placement, as described earlier, cultures with a strong bias toward home care may be more receptive to adaptation of homes to accommodate medical technologies. However, these households may face other social or community constraints that make it difficult to deliver such technologies. I return to these points below.
Caregiving Burden and Satisfaction
With norms of filial obligation and positive appraisals of caregiving demands, ethnic and cultural minorities are more likely to report satisfaction in caregiving. Latina caregivers report lower appraisals of stress and greater perceived benefits of caregiving; they also make greater use of religious coping than white caregivers (Coon et al., 2004). Similarly, African American caregivers report lower anxiety, greater well-being, and more perceived benefits of caregiving than white caregivers (Haley et al., 2004). More generally, cultures differ in how well reciprocity between care receivers and caregivers is maintained after the onset of caregiving (Becker et al., 2003).
Communication with Health Professionals
A central finding in medical anthropology is the difference between illness and disease (Kleinman, Eisenberg, and Good, 1978). Clinicians diagnose and treat disease (abnormalities in body structure or function), but patients suffer illness, in which symptoms carry social significance and force changes in social function. Illness depends on social status and systems of meaning used to understand symptoms. Thus, families and health professionals may start with completely different premises when they collaborate to ameliorate disease or manage disability.
A striking example is a culture-bound syndrome, susto. Susto, sometimes translated as “fright disease” or “separation of body and soul,” is a prevalent condition throughout Latin America. It is a folk or culture-bound syndrome to the extent that it is not associated with a particular abnormality in body structure or function recognized by Western medicine. Although it involves fatigue, anxiety, and withdrawal from social roles, it is not simply a psychological disorder. People suffering susto do not differ in psychological profiles from a matched sample and they benefit from antibiotic treatment (Rubel, O’Nell, and Collado-Ardon, 1984). The person with susto views the condition as a spiritual affliction triggered by negative social interaction, speaks of it this way, and as a result seeks treatment from a traditional healer rather than a physician.
Clearly, how people understand symptoms affects how they speak about a condition, to whom they disclose symptoms, when they seek treatment, and who they think can help them. In the case of home care, if expectations for rehabilitation are low or people view disability as inherent to aging, or if they consider incontinence, muscular dyscontrol, or agitation shameful, they may be less likely to involve health care professionals or paraprofessionals. They may seek to deny or hide the condition. Arranging optimal home care in this case may be complicated and require exquisite skill in bridging cultures.
Patient and family willingness to seek help, to disclose symptoms, or simply to cooperate in care depends in part on the personal relationships that patients develop with home care providers. Patients are more or less comfortable with different providers (and providers are similarly more or less comfortable with different patients, families, or home settings). Concordance in race or ethnicity may not be the most important factor in such comfort. One systematic review did not find concordance in race or ethnicity a significant predictor of receipt of services or satisfaction with care (Meghani et al., 2009). Such concordance may be more important for more generalized trust in communication with physicians or satisfaction with health services overall (Sohler et al., 2007).
Still, the role of cultural differences and lack of concordance between patients and health care providers should not be underestimated. In urban centers, such as New York City, it is very common for home health care providers and patients to speak different languages, come from different neighborhoods, and have very different expectations for care. Yet home care paraprofessionals are expected to work in patient homes, to serve to some extent as surrogate family, and to help disabled or critically ill patients function on their own terms. The potential for misunderstanding and frustration is high, as described below.
Health Decision Making
Culture may be relevant for decisions to seek treatment or receive clinical preventive services. For example, ethnic and racial minorities are less likely to take advantage of preventive health services, such as vaccinations and cancer screening, even when these are available (Chen et al., 2005). However, it is hard to know how much of this difference in service use is related to aspects of culture (such as a different understanding of prevention in late life or differences in the degree to which people view health as a matter of personal agency) and how much may be due to the cultural insularity that characterizes many ethnic enclaves. “Cultural insularity” in this context refers to restrictions in access to health information related to culture, such as not speaking English, but also to religious proscriptions against contact with mainstream culture, for example, watching television or reading English-language newspapers.
This kind of insularity may have an important significance for health in ethnic communities organized around religious beliefs. For example, in an orthodox Jewish sample of older women in New York City, the prevalence of mammography, Pap smears, and colorectal cancer screening was low compared with other women of similar age and education. Use of these preventive services was lowest in the orthodox women who reported least exposure to mainstream sources of health information (Albert, Harlap, and
Caplan, 2004). For ethnic and cultural communities that wish to maintain traditions yet participate in effective disease prevention or home care, it is important that they mobilize community resources, perhaps in partnership with service providers, to develop appropriate delivery of information in culturally acceptable ways.
The Stigma of Disability
Tolerance of disability in families appears to be linked to socioeconomic status (SES), with greater tolerance associated with lower SES (Murphy, 1990). More broadly, consider cultural attitudes toward aging. With each additional decade of life, adults will see not only declines in strength and walking speed and slowing in reaction time but also declines in addictive behaviors and crime, reduction in severe psychiatric disorders, and increased contact with close family (Albert and Freedman, 2010). American culture stresses the negative features of aging, something to be fought or covered up. In other cultures, the stress may be on the more positive elements, as among the Samia of Kenya, who boast of aging as a time to sit by the fire and be fed (Albert and Cattell, 1994). Americans, by contrast, may consider dependence and need for help in old age worse than death (Clark, 1972).
INTERPERSONAL RELATIONSHIPS
The second level in the social-ecological model is family and social relationships. Social relationships differ across cultures in the relative priority assigned to individual and family interests. When family concerns are placed above those of the individual, sociologists speak of “familism.” A consistent body of research has documented the greater familism among non-U.S.-born and U.S.-born Latinos, and the greater tendency of minority groups to receive social support from family members rather than friends (Almeida et al., 2009). African American caregivers who endorsed family-based justifications for caregiving showed better health outcomes and reported less caregiving stress than caregivers not endorsing these justifications (Dilworth-Anderson, Goodwin, and Williams, 2004). However, other research suggests that familism can also intensify the stresses and mental health consequences of home care (Kim, Knight, and Longmire, 2007; Rozario and DeRienzis, 2008).
When an individual’s interests are subordinated to family interests, families may be more likely to adapt the home for medical care. That is, the disruption of the home and restrictions on other family members inherent in complex home care (in which family members may have to maintain equipment, not have friends visit, not be able to leave the home, etc.) may
be more acceptable if home care is considered a dominant family obligation that trumps individual interests. In the social-ecological framework described earlier, familism at the level of social relationships may reinforce individual cultural expectations for home care.
Families and Receptivity to Use of Home Care Services and Medical Technologies
Whether minority groups use home care services and home-based medical technologies more or less than nonminorities use them depends in part on how these services are defined, how available they are in particular localities (and often what kind of state Medicaid waiver policy is in play), and whether differences in SES are adequately controlled. Because of these differences, studies differ in estimates of the independent role of cultural group or ethnicity in home care utilization. This line of research is most developed for aging services. One review through the 1990s found no differences in home care utilization by race (Kadushin, 2004). Other studies report lower utilization, for example, among Mexican Americans (Crist et al., 2009). In New York City, where home care for seniors is generously supported by state and city, Medicaid home care utilization did not differ among whites, African Americans, and Caribbean Latinos (Navaie-Waliser et al., 2001; Albert et al., 2005).
The absence of differences in home care service use by cultural group may or may not mean equal likelihood of use of medical technologies in the home. Here higher levels in the social-ecological framework may become more relevant (see Figure 11-1). Even if families in different cultural groups are equally receptive to adaptation of homes for medical technologies, minority families in less resourced neighborhoods or communities may be less likely to gain access to these technologies. Likewise, smaller homes or neighborhoods with less reliable infrastructural support may pose additional challenges to adapting homes, even when families are receptive. Again, this suggests a need for social-ecological approaches that consider cross-level influences on health care decision making.
What about family relationships or culture would lead to potential differences in home care utilization or the adaptation of homes? Despite some thought that ethnic or cultural minorities may differ in the recognition of medical symptoms, such as dementia in elders (e.g., finding dementia behaviors more acceptable), such differences in fact appear to be an artifact of knowledge about dementia or access to dementia care (Mahoney et al., 2005). Similarly, while poorer mental health (anxiety, depressive symptoms, panic syndromes) has been reported for a number of different cultural groups in the United States, the greater prevalence is probably due to the challenges of assimilating to a new and often very different society and not
to features of culture per se (Gonzalez, Haan, and Hinton, 2001). Many differences attributed to culture may actually be artifacts of low access to services or limited knowledge of a disease process.
Confidence in Home Care Services
One study of home care service use by Mexican Americans showed that familism was related to confidence in the services; elders and caregivers who endorsed familism more highly were less convinced of the value of home care and were accordingly less likely to use such services (Crist et al., 2009). In this analysis, confidence in home care services was an independent predictor of service use and directly related to familism. Interestingly, Crist and colleagues in this study defined home care use as two or more visits from a provider, not just a single one. One reason for this approach was the observation that “elders or family caregivers agree to an initial visit, out of politeness or feeling pressured while in the hospital, but refuse return visits” (Crist et al., 2009, p. 30).
Discrimination
Discrimination in experiences with medical providers (or more generally) may affect receptivity to home care. In the Mexican American sample mentioned earlier, experiencing discrimination was associated with less confidence in home care services and lower usage (Crist et al., 2009). Another question is whether minority and nonminority families receive the same services at home. One study found higher use of physical and occupational therapy among whites and Asians relative to black and Hispanic home health recipients, but this difference was no longer significant with adjustment for case mix (Peng, Navaie-Waliser, and Feldman, 2003). Here, too, it is difficult to tell whether differences are based on insurance coverage status (which is often associated with socioeconomic status and race/ethnicity) or on differences in culture. In a study of home health care of elders discharged from hospitals after a stroke or traumatic brain injury, elders who had private insurance in addition to Medicare were more likely to receive occupational and physical therapy. Minority families were less likely to have private insurance and for this reason were less likely to receive rehabilitative care (Levine et al., 2006). Similar factors may be at work for adaptation of homes for medical technologies.
Psychosocial Preferences for Care: Dignity, Privacy, Comfort, Trust
Cultural “hot button” issues, which include feeding, personal assistance and privacy, and end-of-life care, are surprisingly understudied. A
recent qualitative study did not find differences in care preferences across African American, Chinese, Hispanic, Native American, and non-Hispanic white families (Mullan et al., 2009). These ethnically diverse caregivers were much more concerned with access to appropriate care, avoiding unmet need, and navigating challenging bureaucracies. They did describe cultural differences between family and agency staff concerns, but these were less salient in their experience of receiving home care. Similarly, privacy concerns and receptivity to telemedicine technologies do not appear to differ across cultural groups, at least in initial pilot studies (Dang et al., 2008; Demiris et al., 2009). More research is required to establish psychosocial preferences for care among families providing home care and patients with different disabilities and medical needs.
The social-ecological approach may help explain the absence of differences at the level of families and social relationships in psychosocial preferences for care. Given the overwhelming need to access services and the key position of community resources in gaining such access, families may need to accept greater flexibility or standardization of services, whatever their own preferences. The potential for conflict between families and providers in such cases is clear.
It is also important to recognize that the boundaries of families are not always obvious. As mentioned earlier, families differ in the degree they allow outsiders, such as home care providers or therapists, to become “family.” It may also be complicated for a home care provider to discern who belongs in a patient’s family and how the family defines its functions, which in turn may be relevant for communication and clear expectations regarding care (Knox and Thobaben, 1997). If home care providers must become family to have reasonable access to patients and support from families, then establishing appropriate professional boundaries may also be difficult.
Finally, patient groups differ in the trust they place in medical providers and medical care. Research suggests different kinds of trust: in one’s personal physician, in the competence of a physician’s care, and in formal and informal sources of health information. One study found that African American adults had less trust in their physicians and greater trust in informal health information sources than whites (Musa et al., 2009). Greater trust in one’s own physician was associated with use of preventive health care. Trust may also be relevant for adoption of home care technologies, but little research is available in this area. If informal sources of health information are more important for some cultural groups for the adoption of home health care technologies, then it will be important to work through these informal networks for changing social norms regarding acceptability.
COMMUNITY AND NEIGHBORHOOD FACTORS
Community factors represent the third level in the social-ecological model. These clearly affect access to home care and perhaps also outcomes of home care. For example, in a neighborhood with a high crime rate, it may be difficult to attract agency care, and home care paraprofessionals may be reluctant to make home visits. Home care equipment and technologies brought into a home may make it a target for theft or attract attention a family may not want. Homes in these neighborhoods may not have local providers, making it more complicated to replenish supplies or monitor effective use of technologies.
Also, physical characteristics of homes may complicate the delivery of home care. For example, a home in a low-income neighborhood may not have reliable telephone service. Intermittent telephone service may affect the ability of health providers to contact clients and conduct appropriate follow-up. Similarly, inability to pay electric bills may affect the use of home care technologies, especially nasal ventilation devices for neuromuscular disease, oxygen devices, and telemedicine devices. Even devices that automatically upload device readings require access to wireless networks. More generally, families struggling to maintain a home may have difficulty providing the kind of stability and security needed for effective home care. Chapter 10 presents an extensive discussion of the physical environment and its effects on home care.
The American Geriatrics Society recognizes the importance of home and neighborhood in the effective delivery of home care: “In some cases, the home environment itself may be a barrier to continuing home care. Unsafe neighborhoods, household disruptions from alcohol or drug use, and inadequate room for equipment or environmental modifications may make home care a poor or risky option” (see http://www.healthinaging.org/agingintheknow).
Neighborhoods and personal risk factors in some cases travel together and increase the risk of adverse outcomes in the use of home care technologies. Consider the case of long-term oxygen therapy. About 1 million people in America use oxygen in the home, mostly for the treatment of smoking-related respiratory illness, such as chronic obstructive pulmonary disease. The risk of fire is high if users smoke because oxygen saturates clothing, fabric, and hair and serves as a fire accelerant. Thus, a cigarette will burn faster and hotter in an oxygen-rich setting. As many as 43 percent of oxygen users smoke. Because the prevalence of smoking is higher in low-income neighborhoods, adverse effects of oxygen therapy are more likely in these settings. Fire-related mortality and injury with oxygen use is rare but significant enough for the U.S. Public Health Service to issue warnings (Mortality and Morbidity Weekly Review, 2008).
The role of neighborhoods in shaping health and well-being more generally has also become increasingly clear. To take only one example, an important study by Klinenberg (2004) shows the critical role of neighborhoods in the risk of death from extreme summer heat. Isolation, usually thought of as a problem for individuals, turns out to be heavily dependent on features of communities. In this study of the July 1995 heat wave in Chicago, similarly impoverished communities did not bear the same brunt of heat mortality. For example, North and South Lawndale, contiguous communities with equal proportions of both elderly and elderly living below the poverty level, differed by a factor of 10 in heat deaths. The difference, Klinenberg argues, was in their community social capital, that is, health resources related to social ties. South Lawndale’s predominantly Latino community was economically vibrant, less crime-ridden, more densely populated, with active civic organizations. North Lawndale, predominantly African American, stood out among Chicago communities for its loss of population over the prior 30 years, crime, decaying housing stock, and, most critically, absence of economic activity and civic organizations. Isolated elders in North Lawndale were most at risk of heat death. They lived in fear of crime and nailed windows shut. They feared opening doors to city social workers sent to check up on them. Even if they ventured outside, they had no place to go because there were few stores, parks, or community gathering places to seek cooler air or information about services. Most critically, they had no one to check up on them as part of the normal course of daily life.
Social capital may be involved in quite distal health processes, such as likelihood of recovery from coronary disease (Scheffler et al., 2008). Similarly, measures of community integration that appear quite remote from health processes, such as the proportion of people in a community performing volunteer service, may turn out to be critical resources for health. Even more striking, what is apparent in the risk of heat death or other extreme health events may also apply to a far more general range of health behaviors and outcomes. Wight et al. (2006) used data from the Health and Retirement Survey, merged with community ecological indicators (i.e., census tract indicators of median levels of education or income) to show that community status and individual cognitive health are related.
Home Care in Dangerous Places
In a study of home care in New York City, home care paraprofessionals were asked how they handled assignments in buildings they felt were unsafe because of crime or gang violence (Albert, 2002). They suggested a number of strategies for potentially dangerous assignments. First, they stressed the need in some cases not to accept an assignment. “We have a choice. If
we are sent on a case, you stay the first day. If you don’t like it, call your supervisor and say, ‘The client is OK, but the neighborhood is dangerous and I don’t want to go back there.’”
A second strategy is to make clear one’s position as a home attendant or therapist, a neutral party, and to enlist neighbors as supporters or protectors. As one reported, “When I go into a project, when I see the people there, the first thing I do is introduce myself. Whoever I meet downstairs, the first time, I introduce myself. I say I am here to work, and I ask if I can count on them to help me do my job.”
Home care paraprofessionals in this study often felt a need to call agency supervisors. Many stressed the necessity of a cell phone (actually prohibited by some home care agencies in the 1990s) and the need to call 9-1-1 and seek police interventions: “If it’s a dangerous situation where you are going to be hurt, you take yourself out of there. [But] you don’t go away. If you’re in danger, you call the agency, you call the family; you take yourself out of there and call 9-1-1.” Home attendants are required to stay with clients even in situations of danger (and many did so in the neighborhoods surrounding the World Trade Center following the 9/11 terror attacks). They stressed that they would leave a home or apartment only in a situation of immediate danger and even then would call their agencies on the way out, as they are required to do.
Violence against home care workers is not well documented. In the Minnesota Nurses Study, violence directed at nurses was actually lower among home care nurses than nurses working in hospitals. It was highest among nurses working in skilled nursing settings (Gates, 2004; Gerberich et al., 2004). The study, however, cannot be considered definitive. Only 10 percent of the nurses worked in home care agencies, and these were grouped with school and public health nurses. Also, the study stressed violence directed at nurses by patients. The potential for other forms of violence outside the hospital and skilled nursing home setting is likely to be much higher. For example, in the New York City study of home attendants providing personal assistance care, many reported thefts, pressure if not overt threats from family members, and great concern for personal safety (Albert, 2002).
Home Care in Inhospitable Places
Home attendants also described difficult home situations, and these descriptions often included physically difficult environments (Albert, 2002). Surprisingly, homes in the winter were said to be too warm for the most part, rather than cold and drafty. Home care paraprofessionals were well aware of dangerous home conditions, such as loose floor boards, inadequate windows, obstacles to mobility, and antiquated kitchens. These impressions
accord with a recent survey in the United Kingdom. The prevalence of “nondecent” homes among vulnerable families was surprisingly high and linked to residence in older structures, one unintended consequence of otherwise desired household stability and aging in place (Donald, 2009). The same situation prevails in the United States. Golant (2008) draws attention to low-income elderly homeowners living in the oldest housing stock in the country. These seniors were vulnerable, living in housing that put them at great risk of having unmet health care needs. This, in turn, had spillover effects on neighborhoods, once these elderly were unable to maintain their homes. For this reason, geriatric care managers have begun to look for alliances with community developers to help ensure adequate access to services and repairs (Austin, McClelland, and Gursansky, 2006).
The aging housing stock may also make it difficult to provide adequate home care. Home and community environmental facilitators and barriers are relevant for rehabilitation outcomes (Keysor et al., 2006), and they are likely to be relevant as well for effective delivery of home care, although few studies address the topic.
Access to Home Health Care Workers and Technologies: A Social Capital Perspective
Access to home care may be affected by more subtle community effects, apart from the environmental limitations of homes and barriers posed by the low SES of communities. Weak neighborhoods mean weak social ties, with fewer neighbors to check in on elders, absence of common safe areas (such as stores or parks) that allow people to seek refuge or make contact with others, and less support for home care personnel seeking to deliver services to shut-in elders. Thus, social networks can have properties that are protective of health, and their absence or weakness may make it quite difficult to deliver services to homes. Strong networks allow people with disabilities or health concerns to obtain direct support (both instrumental and emotional) and also enable people to obtain the information they need to access services.
The value of these sorts of community support for home care is clear. They shore up families, allow home care personnel to do their jobs more effectively, and keep people connected to communities even when they face serious illness.
Other evidence suggests more diffuse benefits for social capital. Communities that are well served by medical facilities and home care agencies indirectly provide high-quality, timely information about services and new technologies. They link families in search of such information and thus promote more effective use of resources (and also indirectly promote greater health differentials between high- and low-income neighborhoods).
One study examining child care resources suggests that differences in these social capital effects may be responsible for poorer outcomes in low-income neighborhoods even when they are adequately served (Small and Jacobs, 2008). Provider agencies in higher income communities in this study were more closely linked than agencies in lower income communities. Thus, the flow of information is more efficient in high-income communities and allows greater efficiencies in service delivery.
GAPS AND DIRECTIONS FOR RESEARCH
The social-ecological approach suggests that improvement in home care outcomes will depend on adequate recognition of the role of culture, family and social relationships, and communities in the delivery of care. Interest in the first and second areas is long-standing. Attention to community factors and linkages across levels is more recent, and research in this area is much less developed. I conclude with a series of recommendations derived from the social-ecological approach, as well as a series of hypotheses suggested by this inquiry.
Cultural Assessment in Home Care
A first need is better tools for the assessment of cultural expectations for home care and psychosocial preferences for care delivery. Transcultural nursing has taken the lead in developing methodologies for assessing cultural differences among patients as well as the receptivity of health care providers to these differences (Narayan, 1997; Davidhizar and Bechtel, 1998; Heineken and McCoy, 2000). These approaches recognize the necessity of seeing the world through a patient’s eyes and point out the need for “cultural synergy” between nurse and patient, that is, mutual recognition of different cultures in the service of care.
Campinha-Bacote (2002) has developed a screening instrument for the assessment of cultural competence in nursing. This approach includes three key elements: cultural awareness (“Am I aware of my personal biases and prejudices towards cultural groups different than mine?”), cultural skill (“Do I have the skill to conduct a cultural assessment in a culturally sensitive manner?”), and cultural knowledge (“Do I have knowledge of the client’s worldview?”). As an example of the utility of this approach, Campinha-Bacote notes that hypertension treatment may have a very different meaning among African American elderly, for whom hypertension implies emotional pressure or tension and not just a stiffening of arterial walls. Explanations to patients must take these different understandings into account if patients are to adhere to medication regimens and adopt lifestyle prescriptions.
The challenge of crossing cultural boundaries obviously becomes more difficult when home care personnel and patients do not speak the same language. Family or other translators become critical. My research with home care in New York City suggests that differences in language are quite common—not surprising when one notes that New York City’s fastest growing populations include Mandarin, Russian, and Spanish speakers. One home health care agency director suggested that 80 percent of her agency’s clients and home attendants differed in culture. The agency had to develop guidelines for cases in which clients and home care workers do not speak the same language or share a common culture. As one home attendant stated, “You go into their homes. You have to learn to cook their food, their way. We are all from different cultures. You have to learn to respect different things.” These home attendants reported that the best way to cross cultures was to try to learn key words from a different language. This in itself becomes a bond between clients and workers and a bridge across cultures.
Despite the concern for cultural competence and its assessment, it is difficult to identify studies that examine the relationship between cultural competence and home care outcomes. One would expect a host of better outcomes to follow from culturally sensitive home care: for example, greater adherence to medication, quicker return to function, greater consumer satisfaction, and lower rates of rehospitalization. But at this point empirical data are unavailable. A recent systematic review of home nursing interventions is notable for the absence of any cultural variables in assessing home care outcomes (Liebel et al., 2009).
Including Families in Home Care
A second need suggested by the social-ecological approach is investigation of better ways to include families in home care. As indicated earlier, the bedrock of home- and community-based services is family care (Levine et al., 2006). Studies of the actual work of family caregivers, how these tasks relate to “formal” or paid care, and the impact of such tasks on caregivers’ own lives are critical for understanding the kinds of services that will be needed to allow patients with extensive needs to remain in their homes. Yet despite extensive research on family caregiving, it is surprising how little research examines interactions between families and home care providers. Since the combination of family and paid formal care is increasingly common (and modal in service-rich urban areas, such as New York City), this gap is doubly surprising. Also, the challenges of agency handoffs to families, as when home health care coverage ends (and cases are closed), remain mostly unexplored. Few studies follow family caregivers through the process of beginning and ending formal home care or training and continued recalibration of home medical technologies.
By all indications, families are extremely active even when patients are receiving paid home care services. In our study of patients discharged with stroke and traumatic brain injury (Levine et al., 2006), we found that family caregivers provided about three-quarters of the weekly care (32 of 43 total hours) while families received weekly insurance-based home health care services, regardless of type of insurance coverage. About three-quarters of the families were providing personal care, and most were delivering nursing services, including dispensing medications, monitoring symptoms, checking blood pressure, and other tasks performed by nurses on their visits. A smaller proportion was managing equipment and providing physical/occupational therapy, speech therapy, and cognitive remediation.
Thus, families are by no means passive and must be considered active partners in care. Yet home care agencies do not, for the most part, treat them this way. Our study showed that families in some cases are barred from seeing complete medical information or care plans (because of Health Insurance Portability and Accountability Act regulations), even in their own homes. Nor are they always alerted in advance of the date of case closings. Only about half the family caregivers in our study were notified of case closing in time to make adequate preparations.
A key gap in research and policy, then, is to understand how families and formal home care providers interact: what the points of friction are and how coordination between the two can be enhanced. A randomized trial of greater inclusion of families in the home care process might be very informative for improving outcomes.
One such experiment is currently being assessed—a form of consumer-directed care. The Cash and Counseling Demonstration and Evaluation allowed families eligible for personal assistance home care services in Arkansas, Florida, and New Jersey to take greater control of the hiring, training, and use of aides for people with severe disabilities, including mental illness, across the life span.1 As part of the evaluation of the program, a comparison group receiving traditional agency-directed care was identified in each state. Results from a number of the programs suggest that greater inclusion of families in care planning and management results in positive outcomes, including satisfaction with care arrangements, reliability of paid caregivers, meeting patient needs, caregiver stress, and patient quality of life. Notably, risks of adverse events and new health problems did not differ between control and treatment groups, suggesting that greater family inclusion is at least as safe as agency-directed care (Shen et al., 2008). Direct-care workers in the experimental condition also reported better
|
1 |
As of 2009, the Cash and Counseling program had been renamed and extended to at least 12 additional states (see http://www.bc.edu/schools/gssw/nrcpds/meta-elements/pdf/NewCenterReleaseDraf.pdf). |
work conditions and greater satisfaction with their jobs (Foster, Dale, and Brown, 2007).
The Cash and Counseling Demonstration and Evaluation suggests that greater inclusion of families and due recognition of cultural expectations for care may improve home care. The demonstration focused mainly on personal assistance services, but it would be valuable to determine if families in the intervention arm also used medical technologies more effectively or were better able to adapt homes for the use of such technologies.
Recognizing the Key Role of Neighborhoods and Communities
The role of neighborhoods in home care is perhaps the least well researched of the three elements in the social-ecological framework. Many studies report an independent effect of neighborhood on access to primary care, emergency care, hospice services, and specialist services; but I was not able to identify studies that examine neighborhood factors in access to home care. As mentioned earlier, even when low-income communities are adequately serviced by home care agencies, the effectiveness of such services may be lower than in other communities because of poor housing stock, unreliable access to electricity or telephone service, crime, and lack of community supports. More subtle effects of social capital are likely to be relevant as well, with fewer linkages between agencies and poorer integration of agencies with other community-based institutions. The result is less efficient exchange of information and slower diffusion of innovations. The latter may be particularly important for the use of new home care technologies.
A key gap in research in this domain is a multilevel analysis of neighborhood factors in home care outcomes. Such research would determine if outcomes for home care are poorer in lower income communities after appropriate control for case mix and service delivery. Positive findings would be a strong argument for the relevance of social capital in individual health outcomes and would support other studies that have shown such neighborhood effects as, for example, the recurrence of coronary syndromes and risk of rehospitalization (Scheffler et al., 2008).
Finally, in keeping with the social-ecological approach, it is important to conduct analyses that examine cross-level relationships among culture, social relationships, and communities. These will be difficult until further studies, as suggested here, are conducted in each of the component areas.
Workforce Training
Training the home care workforce in cultural differences and the complexities of family relationships is critical. As mentioned earlier, many home health care agencies have begun such efforts. The Cash and Counseling
program suggests that families themselves can train the workforce in such sensitivity, with benefits to both consumer and provider.
Personal assistance paraprofessionals, respiratory technicians, physical and occupational therapists, home health care nurses, and social work case managers all bring their own cultural expectations to home care. These expectations are drawn from personal experience as well as professional training and socialization.
Among home care paraprofessionals, differences in culture of origin between providers and consumers are likely to be large. This is low-income work, with minimal training and little opportunity for career advancement. In urban areas, home care paraprofessionals are likely to be minorities or immigrants. In our research, these workers reported discrimination and often exploitation from patient consumers. The home attendants we interviewed were frankly embarrassed by the lack of compassion some families showed for their clients and had much higher expectations for care than these families. This, in itself, made for some tension, as when home care attendants stayed longer than required to address a need that should have been a family’s responsibility. Home attendants had to be resocialized in some cases as caregivers not to give out their telephone numbers, not to accept gifts, and not to buy food for a neglected client. They had to learn that some home situations were unsuitable for home care and required agency intervention.
Professional organizations have begun to develop appropriate training for home care workers, particularly in social work, paraprofessional home care, and nursing. But similar programs are not available for the growing group of technicians who train families in respiratory care, the use of communication assistance devices, or new and emerging technologies. This is an area ripe for development, and professional licensing organizations would do well to learn from other clinical specialties and consider requiring such training for certification.
HYPOTHESES FOR FUTURE RESEARCH
This inquiry suggests a number of hypotheses for future research, some of which were mentioned earlier, all drawing on the social-ecological framework developed for home care. I conclude with a list of hypotheses relevant to the adaptation of homes to accommodate advanced medical technologies. These may help guide future research in the area:
-
Family caregivers who do not express the consensus view on home adaptation for medical or supportive care will be less efficient in decision making regarding home care and perhaps risk poorer outcomes for patients.
-
Families with a more expansive meaning of the home as a site for care will be more receptive to adapting homes for advanced medical technologies.
-
Cultures with a strong bias toward home care and away from institutional care will be more receptive to the adaptation of homes.
-
Greater subordination of an individual’s interests to those of the family (familism) will be associated with greater adaptation of homes.
-
Even if families in different cultural groups are equally receptive to the use of medical technologies, minority families in less resourced neighborhoods or communities may be less likely to gain access.
-
Families in resource-poor communities will accept greater flexibility or standardization of services to obtain home care, whatever their own preferences, with potential for conflict between families and providers.
Interventions in which families exert greater control over vendors and providers, like the Cash and Counseling Demonstration and Evaluation, may promote more effective home use of emerging medical technologies.
How to Enhance Home Health Care with What Is Known Now
This review suggests that successful adoption of home care technologies depends on individual human factors but also the context in which individuals live, including the social, cultural, and community resources available to them. One implication of the social-ecological approach to home health care, then, is the need to consider these factors in adoption decisions, which implies an expanded approach to human factors. By way of conclusion, it is worth highlighting two approaches to enhancing home health care, currently available, suggested by this approach.
First, the focus on social factors suggests that patients may adapt technologies in ways unanticipated by designers. People fit the technologies into their daily lives and in ways that accommodate culture and family dynamics. For example, patients seek ways to use the technologies but also to be free of them (Fex, Ek, and Soderhamn, 2009). They may begin with attention to instruction but then innovate and improvise as they fit the use of the technologies into the rhythms of family life. When possible, patients find ways to make technologies less bulky, noisy, clumsy, and heavy. These innovations could suggest changes in design.
Second, social and community factors can also be seen as resources rather than constraints in the adoption of technologies. For example, low self-efficacy is an important obstacle to successful adoption. It may be possible to harness social and community factors to promote self-efficacy. In
fact, community self-help organizations organized around home health care technologies already go a long way toward this end. Many patient support groups seek to develop patient self-efficacy in this area. These groups invite vendors or therapists to demonstrate equipment and often introduce new patients to patients who have already adopted it. These efforts represent important enhancements to home health care that emerge from a social-ecological perspective.
ABOUT THE AUTHOR
Steven M. Albert is professor in the Graduate School of Public Health at the University of Pittsburgh. His research focuses on the assessment of health outcomes in aging and chronic disease, including physical and cognitive function, health service use and the cost of care, quality of life, and clinical decision making.
REFERENCES
Albert, S.M. (1990). The dependent elderly, home health care, and strategies of household adaptation. In J.F. Gubrium and A. Sankar (Eds.), The home care experience: Ethnography and policy (pp. 19-36). Newbury Park, CA: Sage.
Albert, S.M. (1991). Cognition of caregiving tasks: Multidimensional scaling of the caregiver task domain. Gerontologist, 13(6), 726-734.
Albert, S.M. (2002). Home attendants speak about home care: A guide to home care, spoken by the women who provide personal assistance/home attendant care to frail elders in New York City. New York: Fan Fox and Leslie R. Samuels Foundation.
Albert, S.M., and Cattell, M.G. (1994). Old age in global perspective: Cross-cultural and cross-national views. New York: G.K. Hall.
Albert, S.M., and Freedman, V.A. (2010). Public health and aging: An introduction to maximizing function and well-being. New York: Springer.
Albert, S.M., Harlap, S., and Caplan, L. (2004). Cancer screening among older women in a culturally insular community. Preventive Medicine, 39, 649-656.
Albert, S.M., Simone, B., Brassard, A., Stern, Y., and Mayeux, R. (2005). Medicaid home care services and survival in New York City. Gerontologist, 45, 609-616.
Almeida, J., Molnar, B.E., Kawachi, I., and Subramanian, S.V. (2009). Ethnicity and nativity status as determinants of perceived social support: Testing the concept of familism. Social Science and Medicine, 68, 1,852-1,858.
Austin, C.D., McClelland, R.W., and Gursansky, D. (2006). Linking case management and community development. Care Management Journal, 7, 162-168.
Barris, R., Kielhofner, G., Levine, R.E., and Neville, A. (1985). Occupation as interaction with the environment. In G. Kielhofner (Ed.), A model for human occupation (pp. 42-62). Baltimore: Williams and Wilkins.
Becker, G., Beyene, Y., Newsom, E., and Mayen, N. (2003). Creating continuity through mutual assistance: Intergenerational reciprocity in four ethnic groups. Journal of Gerontology: Social Sciences, 58, S151-S159.
Bronfenbrenner, U. (1979). The ecology of human development. Cambridge, MA: Harvard University Press.
Campinha-Bacote, J. (2002). The process of cultural competence in the delivery of healthcare services: A model of care. Journal of Transcultural Nursing, 13, 181-184.
Chen, J.Y., Diamant, A., Pourat, N., and Kagawa-Singer, M. (2005). Racial/ethnic disparities in the use of preventive services among the elderly. American Journal of Preventive Medicine, 29, 388-395.
Clark, M. (1972). Cultural values and dependency in later life. In D.O. Cowgill and L.D. Holmes (Eds.), Aging and modernization (pp. 263-274). New York: Appleton-Century-Crofts.
Coon, D.W., Rubert, M., Solano, N., Mausbach, B., Kraemer, H., Arguelles, T., Haley, W.E., Thompson, L.W., and Gallagher-Thompson, D. (2004). Well-being, appraisal, and coping in Latina and Caucasian female dementia caregivers: Findings from the REACH study. Aging and Mental Health, 8, 330-345.
Crist, J.D., Kim, S.-S., Pasvogel, A., and Velazquez, J.H. (2009). Mexican American elders’ use of home care services. Applied Nursing Research, 22, 26-34.
D’Andrade, R.G. (1995). The development of cognitive anthropology. Cambridge, UK: Cambridge University Press.
Dang, S., Remon, N., Harris, J., Malphurs, J., Sandals, L., Cabrera, A.L., and Need, D. (2008). Care coordination assisted by technology for multiethnic caregivers of persons with dementia: A pilot clinical demonstration project on caregiver burden and depression. Journal of Telemedicine and Telecare, 14, 443-447.
Davidhizar, R., and Bechtel, G.A. (1998). Assessing the patient from a cultural perspective. Journal of Practical Nursing, 48, 16-21.
Demiris, G., Oliver, D.P., Giger, J., Skubic, M., and Rantz, M. (2009). Older adults’ privacy-considerations for vision-based recognition methods of eldercare applications. Technology and Health Care, 17, 41-48.
Dilworth-Anderson, P., Brummett, B.H., Goodwin, P., Williams, S.W., Williams, R.B., and Siegler, I.C. (2005). Effect of race on cultural justifications for caregiving. Journal of Gerontology: Psychological Sciences, 60, S257-S262.
Dilworth-Anderson, P., Goodwin, P.Y., and Williams, S.W. (2004). Can culture help explain the physical health effects of caregiving over time among African American caregivers? Journal of Gerontology: Social Sciences, 59, S138-S145.
Donald, I.P. (2009). Housing and health care for older people. Age and Ageing, 38, 364-367.
Dressler, W.W., Borges, C.D., Balieiro, M.C., and Dos Santos, J.E. (2005). Measuring cultural consonance: Examples with special relevance to measurement theory in anthropology. Field Methods, 17, 331-355.
Fex, A., Ek, A-C., and Soderhamn, O. (2009). Self-care among persons using advanced medical technology at home. Journal of Clinical Nursing, 18, 2,809-2,817.
Foster, L., Dale, S.B., and Brown, R. (2007). How caregivers and workers fared in Cash and Counseling. Health Services Research, 42, 510-532.
Gates, D.M. (2004). The epidemic of violence against healthcare workers. Occupational and Environmental Medicine, 61, 649-650.
Gerberich, S.G., Church, T.R., McGovern, P.M., Hansen, H.E., Nachreiner, N.M., Geisser, M.S., Ryan, A.D., Mongin, S.J., and Watt, G.D. (2004). An epidemiological study of the magnitude and consequences of work related violence: The Minnesota Nurses’ Study. Occupational and Environmental Medicine, 61, 495-503.
Gitlin, L.N. (2003). Conducting research on home environments: Lessons learned and new directions. Gerontologist, 43, 628-637.
Golant, S.M. (2008). Commentary: Irrational exuberance for the aging in place of vulnerable low-income older homeowners. Journal of Aging and Social Policy, 20, 379-397.
Gonzalez, H.M., Haan, M.N., and Hinton, L. (2001). Acculturation and the prevalence of depression in older Mexican Americans: Baseline results of the Sacramento Area Latino Study on Aging. Journal of the American Geriatrics Society, 49, 948-953.
Haley, W.E., Gitlin, L.N., Wisniewski, S.R., Mahoney, D.F., Coon, D.W., Winter, L., Corcoran, M., Schinfeld, S., and Ory, M. (2004). Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: Findings from the REACH study. Aging and Mental Health, 8, 316-329.
Heineken, J., and McCoy, N. (2000). Establishing a bond with clients of different cultures. Home Healthcare Nurse, 18, 45-51.
Hinton, W.L., and Levkoff, S. (1999). Constructing Alzheimer’s: Narratives of lost identities, confusion, and loneliness in old age. Culture Medicine Psychiatry, 23, 453-475.
Kadushin, G. (2004). Home health care utilization: A review of the research for social work. Health and Social Work, 29, 219-245.
Keysor, J.J., Jette, A.M., Coster, W., Bettger, J.P., and Haley, S.M. (2006). Association of environmental factors with levels of home and community participation in an adult rehabilitation cohort. Archives of Physical Medicine and Rehabilitation, 87, 1,566-1,575.
Kim, J.H., Knight, B.G., and Longmire, C.V. (2007). The role of familism in stress and coping processes among African American and white dementia caregivers: Effects on mental and physical health. Health Psychology, 26, 564-576.
Kleinman, A., Eisenberg, L., and Good, B. (1978). Culture, illness, and care: Clinical lessons from anthropologic and cross-cultural research. Annals of Internal Medicine, 88, 251-258.
Klinenberg, E. (2004). Heat wave: A social autopsy of disaster in Chicago. Chicago: University of Chicago Press.
Knox, C., and Thobaben, M. (1997). Partnerships between home care providers and client families. Home Care Provider, 2, 57-59.
Levine, C., Albert, S.M., Hokenstad, A., Halper, D., Hart, A.Y., and Gould, D.A. (2006). “This case is closed”: The transition in family caregiving when home health care services end. Milbank Quarterly, 84, 305-331.
Liebel, D.V., Friedman, B., Watson, N.M., and Powers, B.A. (2009). Review of nurse home visiting interventions for community-dwelling older persons with existing disability. Medical Care Research Review, 66, 119-146.
Mahoney, D.F., Cloutterbuck, J., Neary, S., and Zhan, L. (2005). African-American, Chinese, and Latino family caregivers’ impressions of the onset and diagnosis of dementia: Cross-cultural similarities and differences. Gerontologist, 45, 783-792.
Mausbach, B.T., Coon, D.W., Depp, C., Rabinowitz, Y.G., Wilson-Arias, E., Kraemer, H.C., Thompson, L.W., Lane, G., and Gallagher-Thompson. D. (2004). Ethnicity and time to institutionalization of dementia patients: A comparison of Latina and Caucasian female family caregivers. Journal of the American Geriatrics Society, 52, 1,077-1,084.
McElroy, K.R., Bibeau, D., Steckler, A., and Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351-377.
McGarry, J. (2009). Defining roles, relationships, boundaries and participation between elderly people and nurses within the home: An ethnographic study. Health Social Care Community 17, 83-91.
Meghani, S.H., Brooks, J.M., Gipson-Jones, T., Waite, R., Whitfield-Harris, L., and Deatrick, J.A. (2009). Patient-provider race-concordance: Does it matter in improving minority patients’ health outcomes? Ethnicity and Health, 14, 107-130.
Mortality and Morbidity Weekly Review. (2008). Fatal fires associated with smoking during long-term oxygen therapy: Maine, Massachusetts, New Hampshire, and Oklahoma, 2000-2007. Reported by T. Wendling and A. Pelletier. Mortality and Morbidity Weekly Review, 57(31), 852-854. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5731a3.htm [accessed June 2010].
Mullan, J.T., Grossman, B.R., Hernandez, M., Wong, A., Eversley, R., and Harrington, C. (2009). Focus group study of ethnically diverse low-income users of paid personal assistance services. Home Health Care Services Quarterly, 28, 24-44.
Murphy, R.F. (1990). The body silent: The different world of the disabled. New York: W.W. Norton.
Musa, D., Schulz, R., Harris, R., Silverman, M., and Thomas, S.B. (2009). Trust in the health care system and the use of preventive health services by older black and white adults. American Journal of Public Health, 99, 1,293-1,299.
Narayan, M.C. (1997). Cultural assessment in home healthcare. Home Healthcare Nurse, 15, 663-670.
Navaie-Waliser, M., Feldman, P.H., Gould, D.A., Levine, C., Kuerbis, A.N., and Donelan, K. (2001). Experiences and challenges of informal caregivers: Common themes and differences among whites, blacks, and Hispanics. Gerontologist, 41, 733-741.
Or, C.K.L., and Karsh, B-T. (2009). A systematic review of patient acceptance of consumer health information technology. Journal of the American Medical Informatics Association, 16, 550-560.
Or, C.K.L., Karsh, B-T, Severtson, D.J., and Brennan, P.F. (2006). Patient technology acceptance model (PTAM): Exploring the potential characteristics of consumer health information technology acceptance by home care patients with chronic illness. Santa Monica, CA: Human Factors and Ergonomics Society.
Peng, T., Navaie-Waliser, M., and Feldman, P.H. (2003). Social support, home health service use, and outcomes among four racial-ethnic groups. Gerontologist, 43, 503-513.
Rozario, P.A., and DeRienzis, D. (2008). Familism beliefs and psychological distress among African American women caregivers. Gerontologist, 48(6), 772-780.
Rubel, A.J., O’Nell, C.W., and Collado-Ardon, R. (1984). Susto: A folk illness. Berkeley: University of California Press.
Rubinstein, R.L. (1990). Culture and disorder in the home care experience: The home as sick room. In J.F. Gubrium and A. Sankar (Eds.), The home care experience: Ethnography and policy (pp. 19-36). Newbury Park, CA: Sage.
Scheffler, R.M., Brown, T.T., Syme, L., Kawachi, I., Tolstykh, I., and Iribarren, C. (2008). Community-level social capital and recurrence of acute coronary syndrome. Social Science and Medicine, 66, 1,603-1,613.
Shen, C., Smyer, M., Mahoney, K.J., Simon-Rusinowitz, L., Shinogle, J., Norstrand, J., Mahoney, E., Schauer, C., and del Vecchio, P. (2008). Consumer-directed care for beneficiaries with mental illness: Lessons from New Jersey’s Cash and Counseling program. Psychiatric Services, 59, 1,299-1,306.
Small, M.L., and Jacobs, E.M. (2008). Why organizational ties matter for neighborhood effects: Resource access through childcare centers. Social Forces, 87, 387-414.
Sohler, N.L., Fitzpatrick, L.K., Lindsay, R.G., Anastos, K., and Chinazo, O.C. (2007). Does patient-provider racial/ethnic concordance influence ratings of trust in people with HIV infection? AIDS and Behavior, 11, 884-896.
Sommer, B., Avis, N., Meyer, P., Ory, M., Madden, T., Kagawa-Singer, M., Mouton, C., Rasor, N.O., and Adler, S. (1999). Attitudes toward menopause and aging across ethnic/racial groups. Psychosomatic Medicine, 61, 868-875.
Whitehouse, P.J., Gaines, A.D., Lindstron, H., and Graham, J.E. (2005). Anthropological contributions to the understanding of age-related cognitive impairment. Lancet Neurology, 4, 320-326.
Wight, R.G., Anechensel, C.S., Miller-Martinez, D., Botticello, A.L., Cummings, J.R., and Karlamanga, A.S. (2006). Urban neighborhood context, educational attainment, and cognitive function among older adults. American Journal of Epidemiology, 163, 1,071-1,078.
Wolff, J.L., Roter, D.L., Given, B., and Gitlin, L.N. (2009). Optimizing patient and family involvement in geriatric home care. Journal of Healthcare Quality 31, 24-33.
Zhan, H.J. (2004). Through a gendered lens: Explaining Chinese caregivers’ task performance and care reward. Journal of Women and Aging, 16, 123-142.




























