6
The Health Care Challenge: Matching Care to People in Their Home Environments
Neil Charness
My tasks in this chapter are to (1) review the demographics concerning current and future home health care users; (2) examine data on their capabilities; (3) assess their attitudes and how these might be expected to impact successful interaction with current and future home health care technology; (4) provide some examples of how user characteristics may influence the ability to perform home health care tasks, particularly involving technology; and (5) identify important gaps in the understanding of these relationships and make some recommendations. I stress a human factors perspective in attempting to address these issues.
THE SHIFT TO HOME HEALTH CARE
Justification for concern with these issues lies in the remarkable shift in the way in which health care has been delivered to individuals in the past century in the United States. The major changes include the diversity in the population being treated and in their attitudes about health care, who pays for treatment, what type of health conditions are treated, where people are treated, and the demands made on those who are treated by current technology products. As one example of change in treatment locale, today about 99 percent of children in the United States are born in hospitals or clinics (DeClercq, Paine, and Winter, 1995), whereas home births probably predominated before 1900. In contrast, place of death has begun to shift away from hospital settings (dropping from 78 to 61 percent from 1994 to 2004 in a Canadian study; Wilson et al., 2009) to homes and hospice facilities. Finally, except for occasional programs that cater to housebound
older adults (e.g., Beck et al., 2009), one travels to an office or clinic to see a health care professional today or is taken by ambulance to a hospital in an emergency. (The author can remember a childhood visit by a physician to diagnose and schedule an emergency appendectomy.) Perhaps the greatest change is the treatment of patients with serious health conditions at home instead of in hospitals, a trend being driven in part by treatment cost considerations.
A motivator for such treatment locale changes is the rapidly rising cost of health care coupled with a shift in the burden of payment. Individuals now pay directly for less than half their medical care expenses, with public and private insurance entities picking up the bulk of the payment, whereas as few as 50 years ago these relationships were reversed. Finally, people a century ago came in contact (sparingly) with medical care providers to address acute health concerns, such as communicable illnesses and injuries. In contrast, it was estimated that about 78 percent of health care expenditures in the United States in 1996 were made to treat people with chronic conditions (Anderson and Horvath, 2002). By 2005 that figure had risen to 90 percent (Machlin, Cohen, and Beauregard, 2008), in part because of the high prevalence of these conditions in the population. About 60 percent of adult civilian noninstitutionalized people have at least one chronic condition, although only about half of total medical care expenditures were for treatment of them. (Those with chronic conditions also experience disproportionate treatment for acute conditions.) The definition of chronic diseases by the Centers for Disease Control and Prevention is that they are “noncommunicable illnesses that are prolonged in duration, do not resolve spontaneously, and are rarely cured completely.” The five most costly ones in 2006 were (1) heart conditions, (2) cancer, (3) trauma-related disorders, (4) mental disorders, and (5) asthma that includes chronic obstructive pulmonary disease (Soni, 2009). Many of these disorders are experienced throughout the life course (trauma-related, such as auto accidents), although some are more strongly associated with childhood (asthma), some are associated more with young adulthood (mental disorders, such as schizophrenia), and some are most associated with old age (heart disease, cancer, Alzheimer’s disease). I focus primarily on older adult health care examples because that part of the population bears the greatest burden from chronic diseases.
Given the aging of the population, the percentage of health care cost expended to treat chronic diseases will undoubtedly rise because of the strong relation between age and chronic disease prevalence (see Figure 6-1). The Government Accountability Office projected a quadrupling of spending on older adult long-term care alone between 2000 and 2050 (Allen, 2005). There is also concern that other trends, such as increased prevalence of diabetes, which is variously projected to increase from 11 million in 2000
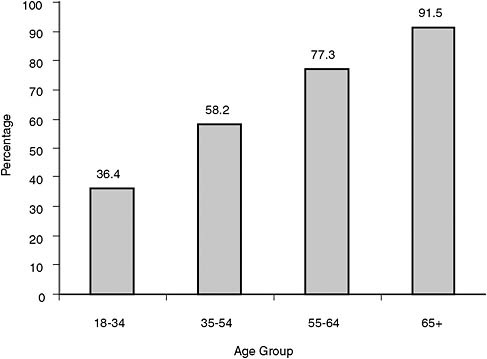
FIGURE 6-1 Relation between age and prevalence of a chronic condition.
SOURCE: Based on data from Machlin, Cohen, and Beauregard (2008).
to 29 million in 2050 (Boyle et al., 2001) or to 38 million in 2031 (Mainous et al., 2007), coupled with improved survival from traumas that used to lead to death (e.g., traffic crashes and battlefield injuries), will also increase demands on the health care system.
The future population of home health care users is already in place: it is the current U.S. population ranging from young to old and living with a variety of ailments whose treatment regimen makes a variety of demands on themselves and their caregivers. Examples are prematurely born infants on ventilators, children with diabetes requiring insulin injections, young adults with AIDS who must adhere to complicated medication regimens, middle-aged adults with “silent” hypertension that requires medication with unpleasant side effects, older adults with sleep apnea who must use uncomfortable equipment to maintain continuous positive airway pressure, and people with renal failure who use home dialysis to avoid costly kidney transplants (with comparable outcomes; Pauly et al., 2009). As well, children and adults also experience acute conditions, such as infections (influenza) and injuries (broken bones), that make demands of shorter duration
on their capabilities and those of their caregivers but are typically treated mostly at home.
What will change is that today’s relatively healthy children and young adults will, as they age, develop chronic conditions in addition to the acute conditions that affect health for shorter periods of time. In addition, many of those who have chronic conditions now (e.g., spinal cord injuries, diabetes) will continue to consume home health care services as their general health deteriorates and as comorbidities develop. The changing ethnic composition of the population, coupled with differential susceptibility to some diseases, means that one can also anticipate a change in the mix of morbidities, such as diabetes, whose incidence tends to be greater in minority groups (Mainous et al., 2007).
Given the enormous expenditures made on health care in the United States (discussed below), the model of providing continuing care through the traditional hospital and physician system is being questioned. One can expect to see more and more health care migrating into the home, with increased monitoring of health status being accomplished through technological systems, such as remote vital sign monitoring equipment. The goal is that such systems will provide more efficient health care delivery. However, designers of technology systems need to consider human factors in their design and deployment, because a badly designed system may fail to accomplish the goal of efficient delivery of health care and can even lead to fatal errors (e.g., Leveson and Turner, 1993; Institute of Medicine, 2000). Another example is assistive devices such as hearing aids, which have a high rate of abandonment (e.g., 30-50 percent) despite their potential benefit to users (Fuhrer, 2001). Some of the problems that arise may be the result of a poor fit between a device and the abilities and expectations of a specific user. Human factors and ergonomics specialists can offer insights into how best to design better health self-care systems.
THE HEALTH CARE ENVIRONMENT
People in the United States consumed $2.1 trillion of health care in 2006, that is, $7,026 per capita, representing 16 percent of gross domestic product (National Center for Health Statistics, 2008). About 84 percent of the expenditures were on personal health care and about 16 percent were on administrative costs, government public health activities, research, structures, and equipment. The highest percentage of those personal expenditures was for in-hospital care, followed by physician services (see Figure 6-2).
As many have noted (e.g., Schoen et al., 2006), Americans pay more than citizens of most other developed countries for their health care, yet by most health outcome measures, they fail to obtain benefits commensurate with these expenditures. Thus, using the figure above as a guide, in order
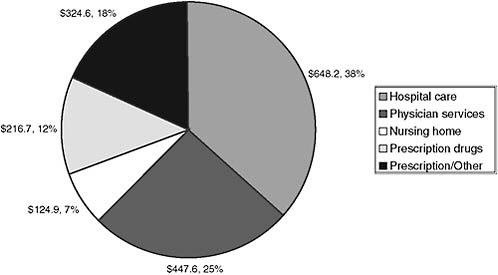
FIGURE 6-2 U.S. health care expenditures, 2006.
SOURCE: National Center for Health Statistics (2008).
to cut health care costs, the most likely candidates would be to diminish unnecessary contacts with hospitals and physicians and to consume fewer unnecessary over-the-counter and prescription drugs. Deployment of home health care technologies may reduce some of these expenditures by enabling people to be monitored from home by less skilled health care workers (in some cases, the user and family members) and by identifying health care problems before they require expensive treatments.
THE PERSON-ENVIRONMENT FIT FRAMEWORK
I consider health care somewhat broadly to include not only treatment of acute or chronic disorders but also such processes as information seeking and advice provision for health-related activities (e.g., exercise and diet) that might occur through a search of the Internet.1 A useful framework for envisioning how best to match care to people in their home environments is that of capability-demand fit. A sample framework, based on Czaja et al. (2001), is presented in Figure 6-3, one that exemplifies demands for a telehealth tool, such as a videoconferencing system used in telemedicine interventions. The person would be asked to use this device at home (e.g., to receive therapy for a mental health disorder). The device presents challenges
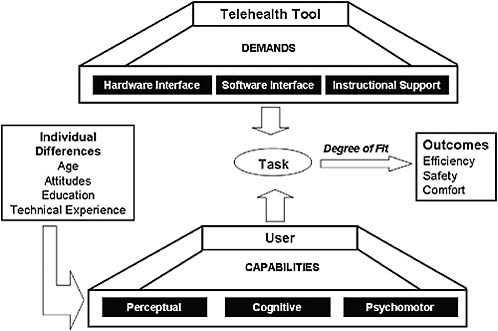
FIGURE 6-3 Capability-demand fit framework.
SOURCE: Adapted from Czaja et al. (2001).
in the form of its hardware interface, software interface, and instructional support. The user brings a range of abilities to bear, including perceptual, cognitive, and psychomotor capabilities. In short, systems make demands on users and the capabilities of the users will determine whether there is an adequate fit, which can affect acceptance and use of the system. Use of the (health care) system may in turn determine whether someone has a positive or negative health outcome.
As another example, think of some of the demands made by newer mobile vital sign monitoring devices now entering the home health care market. Consider a wristwatch-like device that, in the presence of a wireless network in the home, streams information, such as the user’s temperature, location, and potential falls (via an embedded accelerometer), to a remote server. The information is aggregated, filtered through an intelligent program that tests for out-of-bounds values for vital sign parameters, and is presented to a health care provider via a password-protected website. However, the watch is battery-operated and needs to be recharged once a week on a charging station. If the user is somewhat cognitively impaired or simply forgetful, it is possible for the watch to fail based on a too-low battery state. Worse yet, the charging station may require precise placement of the watch within the station for effective charging to take place. If the
older adult has a tremor, he or she may fail to align the watch with the charging contacts. Although the watch can signal its low-battery state to the server and present an alarm (via the web-based interface, or with an alert sent through the cellular phone system), unless someone is monitoring for the low-battery alarm, a fall could be missed before the user is alerted and reminded to recharge the watch (or the fall could occur while the watch is being charged). Even if the watch puts out a low-battery warning on the watch face, unless the user is carefully monitoring the watch and remembers what the low-battery icon means, that signal could be missed. Thus, user perceptual, cognitive, and psychomotor capabilities set a limit on how effectively the tool can function, despite the presence of a sophisticated hardware and software interface and instructional support.
As an example of how user characteristics, such as attitudes, can affect degree of fit for technology, consider a newly diagnosed older adult diabetic who is told to monitor blood sugar levels and inject insulin accordingly,2 as well as to change diet and exercise levels. Blood glucose meters are relatively easy (although somewhat painful) to use with appropriate instruction (e.g., Mykityshyn, Fisk, and Rogers, 2002), but they may come with inadequate instructions, hobbling both cognitively fit young adults and less fit older adults (Rogers et al., 2001). Similarly, advice to change diet and to increase exercise levels may not yield adherence if the senior sees little linkage between glucose meter readings and short-term diet or exercise changes. The user may have unrealistic expectations and attitudes at the outset, which are reinforced by difficulties and unpleasantness associated with glucose meter use and the injection of insulin. All these difficulties may lead to poor adherence to diet, exercise, and monitoring/injection schedules. Better instructional materials, the training of expectations, quick access to skilled health care professionals for troubleshooting with equipment (e.g., through videoconferencing), and better designed equipment (e.g., noninvasive glucose measurement, automated insulin pumps) could lead to superior outcomes by making the treatment demands better match user capabilities and attitudes. One could also argue that having better health instruction earlier in the life span might have led to a lifestyle that would have avoided adult-onset diabetes.
For most health self-care, the proximal environment includes the home, its residents, and health care devices. In the United States, some relevant characteristics of households for the noninstitutionalized civilian population are shown in Table 6-1 and Figure 6-4. Of the roughly 117 million households in 2008, about two-thirds are family households, although composition varies with age of householder. For those ages 20-24, about half dwell
TABLE 6-1 U.S. Households by Type and Age, 2008 (numbers in thousands)
|
U.S. Households |
Total |
Age of Householder |
|||
|
Under 20 Years |
20-24 Years |
25-29 Years |
30-34 Years |
||
|
Total all households |
116,783 |
862 |
5,691 |
9,400 |
9,825 |
|
Family households |
|
|
|
|
|
|
Total |
77,873 |
535 |
2,824 |
5,869 |
7,384 |
|
Married couple |
58,370 |
58 |
1,166 |
3,753 |
5,240 |
|
Male householder |
22,972 |
361 |
2,124 |
2,724 |
2,140 |
|
Female householder |
35,442 |
443 |
2,401 |
2,923 |
2,444 |
|
Proportion family households |
0.67 |
0.62 |
0.50 |
0.62 |
0.75 |
|
Nonfamily households |
|
|
|
|
|
|
Total |
38,910 |
327 |
2,867 |
3,531 |
2,440 |
|
Male householder |
17,872 |
147 |
1,521 |
2,074 |
1,595 |
|
Female householder |
21,038 |
180 |
1,346 |
1,457 |
845 |
|
Size of household |
|
|
|
|
|
|
One member |
32,167 |
143 |
1,507 |
2,167 |
1,764 |
|
Two members |
38,737 |
269 |
1,992 |
2,966 |
2,340 |
|
Three members |
18,522 |
215 |
1,230 |
1,934 |
1,988 |
|
Four members |
15,865 |
121 |
611 |
1,394 |
2,133 |
|
Five members |
7,332 |
63 |
222 |
597 |
1,062 |
|
Six members |
2,694 |
29 |
80 |
222 |
383 |
|
Seven+ members |
1,467 |
22 |
50 |
120 |
155 |
|
Proportion one-member households |
0.28 |
0.17 |
0.26 |
0.23 |
0.18 |
|
SOURCE: Based on data from U.S. Census Bureau (2009). |
|||||
with family members, and that percentage increases to a high of 78 percent by ages 35-39 and then declines to a low of 42 percent by age 75+.
Household composition is likely to affect the willingness (and ability) of another household member to provide help with activities of daily living (ADLs) and instrumental activities of daily living (IADLs) and, more specifically, with health technology products. Research on problem solving suggests that two heads are sometimes better than one (Hinsz, Tindale, and Volrath, 1997), although 28 percent of all households have single members, and the proportion by age rises from 17 percent for those under age 20 to 56 percent for those over age 75. Also, as seen in Figure 6-4, women are
|
35-39 Years |
40-44 Years |
45-49 Years |
50-54 Years |
55-64 Years |
65-74 Years |
75+ Years |
|
10,900 |
11,548 |
12,685 |
11,851 |
19,909 |
12,284 |
11,829 |
|
|
|
|
|
|
|
|
|
8,605 |
8,996 |
9,438 |
8,511 |
13,218 |
7,503 |
4,990 |
|
6,406 |
6,583 |
7,105 |
6,737 |
11,144 |
6,365 |
3,813 |
|
1,956 |
2,113 |
2,363 |
2,163 |
3,457 |
1,765 |
1,804 |
|
2,537 |
2,852 |
3,217 |
2,951 |
5,308 |
4,153 |
6,213 |
|
0.79 |
0.78 |
0.74 |
0.72 |
0.66 |
0.61 |
0.42 |
|
|
|
|
|
|
|
|
|
2,295 |
2,552 |
3,247 |
3,340 |
6,690 |
4,781 |
6,839 |
|
1,442 |
1,567 |
1,766 |
1,696 |
2,944 |
1,568 |
1,552 |
|
853 |
985 |
1,481 |
1,644 |
3,746 |
3,213 |
5,287 |
|
|
|
|
|
|
|
|
|
1,760 |
2,040 |
2,702 |
2,877 |
5,995 |
4,542 |
6,671 |
|
1,974 |
2,152 |
3,183 |
3,954 |
9,307 |
6,243 |
4,358 |
|
2,060 |
2,280 |
2,494 |
2,350 |
2,535 |
915 |
521 |
|
2,803 |
2,790 |
2,593 |
1,707 |
1,248 |
310 |
156 |
|
1,465 |
1,503 |
1,102 |
645 |
473 |
129 |
70 |
|
557 |
522 |
406 |
187 |
210 |
68 |
29 |
|
281 |
262 |
205 |
131 |
140 |
76 |
24 |
|
0.16 |
0.18 |
0.21 |
0.24 |
0.30 |
0.37 |
0.56 |
much less likely to be living in family households than are men at advanced ages. By age 85+, of those not institutionalized, about 64 percent of men compared with 39 percent of women live in family households. Particularly when it comes to managing and maintaining complex technology, having help accessible may be the difference between succeeding or failing with a task. Technology can provide access to such support when it does not reside in the household.
A more inclusive definition of the health care environment would consider other providers outside the home (physicians, nurses, formal and informal caregivers), including health care staff or advisors associated with schools and workplaces as well as other service providers who enter the home (e.g., to prepare meals, help with bathing). Thus, it is also likely that home health
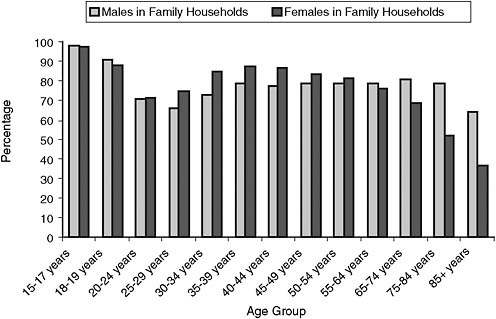
FIGURE 6-4 Male and female percentages for living with a family member, by age and sex.
SOURCE: U.S. Census Bureau (2009).
care will resemble a team environment, one in which team members will vary widely in their skills. Communication skills are central to expert team performance. Team environments also place a high premium on training members for their roles (Salas and Cannon-Bowers, 2001), a usually neglected aspect of home health care settings. I restrict consideration mainly to noninstitutionalized dwellings (apartments, detached and semidetached houses) rather than congregate housing (e.g., assisted living and chronic care institutions), primarily because the vast majority of Americans live in such dwellings for most of their lives, spending only a few years in assisted living or other chronic care residences. For example, for people ages 65+, only about 5 percent live in congregate housing settings, although percentages rise steeply with age.
DEMOGRAPHICS OF HEALTH CARE USERS
Every member of the population is a potential home health care user. So, for example, knowing the palm-down press and twist strength of children, young adults, and older adults is helpful for designing the cap mechanisms on prescription drug containers. One needs to ensure that opening requirements are too great for toddlers but not for older adults with arthritic hands. There are good sources of ergonomic information for different
subsets of the population (e.g., Kroemer, 2005), although chronicling user capabilities for the entire population (e.g., some disabled veterans have lost limbs and use prostheses) is beyond the scope of this chapter. However, given that those with chronic conditions incur about 90 percent of the health care expenditures, they are the primary focus of this review.
Although it is difficult to predict trends for home health care utilization (or cost; Manton, Lamb, and Gu, 2007), given current promising trends of increasing disability-free longevity (e.g., Manton, Gu, and Lowrimore, 2008), one relatively safe prediction is that those already suffering from impairments are candidates to reach old age with fewer financial resources and with disabilities that will complicate treatment of other chronic conditions likely to arise. Those with disabilities are much less likely to be employed full time. For example, the unemployment rate in May 2009 for those ages 16 and over who were not institutionalized in the United States was 8.9 percent for persons without a disability and 13.7 percent for those with one (see http://www.bls.gov/cps/cpsdisability.htm [accessed June 2010]). Thus, at least for expected income levels, which strongly influence health care consumption, the life chances for those with a disability are likely to be poorer. There are two obvious subgroups for disability: civilians and wounded veterans who are classified as disabled.
Disability
According to the American Community Survey (ACS), in 2006 there were approximately 41.3 million people in the United States who reported some form of disability. Disability rises with age, particularly after age 65. Figure 6-5 shows percentage data for men and women derived from the 2006 ACS. (Data were downloaded as an Excel spreadsheet for a Factfinder query based on the U.S. population.) Disability is defined in that survey as “a long-lasting sensory, physical, mental, or emotional condition or conditions that make it difficult for a person to do functional or participatory activities such as seeing, hearing, walking, climbing stairs, learning, remembering, concentrating, dressing, bathing, going outside the home, or working at a job.”
Percentages can be misleading, so Figure 6-6 shows the numbers in millions from the ACS. Although percentage of disability rises with age past 65, the majority of disabled individuals are in their working years. Assuming that a moderate percentage of them reach old age (mortality can be expected to be higher than in the general population, e.g., three times higher for those with an intellectual disability; Tyrer, Smith, and McGorther, 2007), they will constitute a very large cohort that will need significant assistance with self-care activities, and many others in the nondisabled segments of the population can be expected to transition into their ranks as they age.
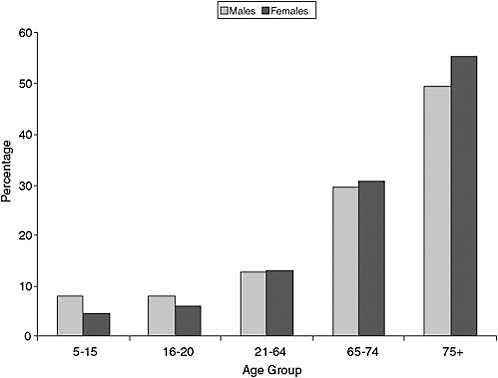
FIGURE 6-5 Percentage of the U.S. civilian noninstitutionalized population reporting any disability, 2006.
SOURCE: Based on data from U.S. Census Bureau (2010).
Veterans
According to a recent report sponsored by the Veterans Administration (VA), approximately 2.6 million veterans were receiving disability compensation benefits in September 2007 (Economic Systems Inc., 2008). Disabled veterans include those from World War II onward, including Korea, Vietnam, and more recent conflicts in Iraq and Afghanistan.
The types of service-connected disability classifications that are most prevalent are musculoskeletal (45 percent) and mental disorders, including posttraumatic stress disorder (PTSD) (15 percent), with other categories comprising less than 10 percent each. For recent disability compensation enrollees in the period 2001-2007 (approximately 776,500 individuals), the most common disorders reported were tinnitus (215,000 cases, 8.3 percent) and defective hearing (171,000 cases), followed by diabetes (143,000 cases) and PTSD (113,000 cases).
Note that not all veterans with impairments apply for and receive
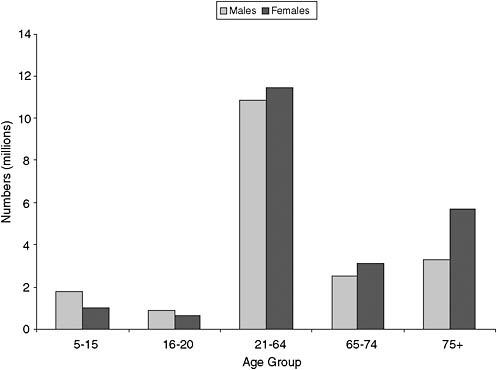
FIGURE 6-6 Numbers of the U.S. civilian noninstitutionalized population reporting any disability, 2006.
SOURCE: Based on data from U.S. Census Bureau (2010).
disability compensation from the VA, so the number of uncompensated cases in the general population could be significant (although presumably they would be captured in ACS data sets). Also, one article (http://www.nytimes.com/2009/07/13/us/13backlog.html?hpw [accessed July 2009]) suggests that there is a significant backlog for processing VA disability claims of about 400,000 cases. Nonetheless, even if one assumed that a significant proportion of disabled veterans are in institutional settings not counted in the ACS survey, disabled veterans represent about 6 percent of the total disabled population in the United States. However, one should note that the VA definition of disability and the definition in surveys such as the ACS are quite different.
Finally, the types of disability in veteran populations are likely to differ from those in the civilian population and have implications for home health care system design. Given the very high prevalence of musculoskeletal and hearing problems, health care device manufacturers need to pay heed to ease of manipulation (for example, permit one-handed operation of devices similar
to requirements for keyboard use in Section 508 of the Rehabilitation Act) and provision of instruction through text rather than through voice. Similarly, for these veteran populations, vision rather than audition should be the preferred channel for providing information about system states and warnings.
Diversity in Users of Home Health Care
The U.S. population, like that of many other nations, is changing. And the changes encompass characteristics that relate to health status, such as age, gender, education level, and ethnicity. I briefly review some of those changes, at the general population level, as they pertain to health care utilization and, when information is available, to health technology use. What becomes obvious for each category is that there is enormous diversity in the United States, making the tasks of designing home health care devices and training challenging ones.
Age
The U.S. population continues to age because of its relatively low birth rates coupled with declining death rates. The population pyramid is also “lumpy” because of the very large cohort of babies (baby boom generation) born between 1946 and 1964, although it is expected to become more rectangular by 2050.
Assuming that war or natural disasters (such as epidemics) do not suddenly increase mortality rates in the United States, the projected population pyramids indicate that there will be greater than a doubling in the size of the group ages 65 and older (from about 35 million in 2000 to 80 million in 2050) and a quadrupling in the size of the group ages 85 and older (from about 5 to 20 million). These age ranges are associated with high consumption of health care, in part because chronic conditions show strong age-related increases, and some dementing diseases, such as Alzheimer’s, occur very rarely before the age of 50. An example of age-related increases in serious health conditions can be seen in Figure 6-7, showing moderate or severe memory impairment. Advanced age is a strong negative predictor of information technology use for current elders (Czaja and Lee, 2008). This trend of lower use with age goes back at least a quarter of a century (e.g., the 1981 survey of technology use reported in Brickfield, 1984) and can be expected to hold in future older cohorts.
Gender
The older population, now and somewhat less so in the future, is likely to be predominantly female, and hence women living alone are likely targets
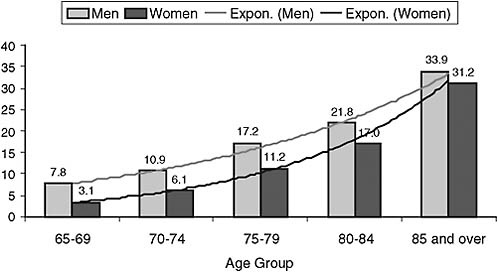
FIGURE 6-7 Percentage of the elderly with moderate or severe memory impairment, 2006.
NOTE: The definition of “moderate or severe memory impairment” is four or fewer words recalled (out of 20) on combined immediate and delayed recall tests.
SOURCE: National Institute on Aging, National Institutes of Health, and U.S. Department of Health and Human Services (2007).
of home health care in old age. Although there were early indications that women were less likely than men to be technology adopters (particularly computer and Internet users), this has changed (Cooper and Kugler, 2008). There are still gender-related differences in types of use, however. As an example, the author’s 84-year-old mother uses e-mail and instant messaging as well as some web browsing, and his 86-year-old father primarily uses stock market software and a fax machine, relying on a telephone to communicate with relatives and friends. However, as discussed below, use of such technology is sharply lower in today’s elders.
Education
In general, there has been a remarkable increase in educational achievement over the past 70 years in the United States. The percentage of the population ages 25 and older with four years of high school has risen from less than 40 percent in 1940 to nearly 90 percent in 2008. For four or more years of college, there was a sixfold increase, from 5 to over 30 percent. Part of the increase in attainment may be attributed to a concomitant increase in cognitive ability worldwide (measured with intelligence tests,
such as the Army Alpha administered to military draftees), known as the Flynn effect (Flynn, 1987). Higher educational attainment is associated with higher income, better health, and greater longevity. These education and cognitive increases bode well for the ability of future generations to cope with complex health care equipment, with the caveat that as people age, such “fluid” abilities can show dramatic declines (Salthouse, 2010).
Ethnicity
There are also going to be marked changes in the ethnic composition of the United States over the coming decades, particularly in the older population (see Figure 6-8). The non-Hispanic white population of seniors is expected to increase about 80 percent, whereas blacks will increase about threefold, and Hispanics, Asians, and American Indians will increase nearly sevenfold in total. There are health status disparities across ethnic groups. Also, with respect to technology generally, such as computer and Internet use, nonwhites currently show less use than whites. Also, as discussed below, attitudes toward health care issues vary with ethnicity.
Language Use
A critical issue for providing instructions to home health care technology users is determining people’s language comprehension abilities, particularly in English. Data from the American Community Survey for 2005-2007 show that, of those who report that they do not speak English at home, about 37 percent report that they speak English less than “very well.” For the largest language group, Spanish, 16 million speak English less than “very well.” An earlier (2003) assessment of adult basic English reading skills (Baer, Kutner, and Sabatini, 2009) yielded similar findings, showing about 11 million Americans with below basic literacy skills (reading letters, numbers, words, and comprehending simple texts, such as one from a medicine container). So, for example, when meeting with a health care professional, Spanish-speaking Americans may not easily express themselves (speaking skills), comprehend complex instructions when given in English (listening comprehension skills), or be able to use a health care device like a glucose meter when provided with written English instructions (reading comprehension skills). Translators (human or computer) may be needed in some instances, although current language translation software cannot compete with skilled human translators. However, the Internet does provide free and convenient access to short-passage written language translation in many common languages (e.g., http://babelfish.yahoo.com/ [accessed May 2010]).
Thus, it is obvious that for a significant number of people their English language skills will be weak (and their education level is likely to be low),
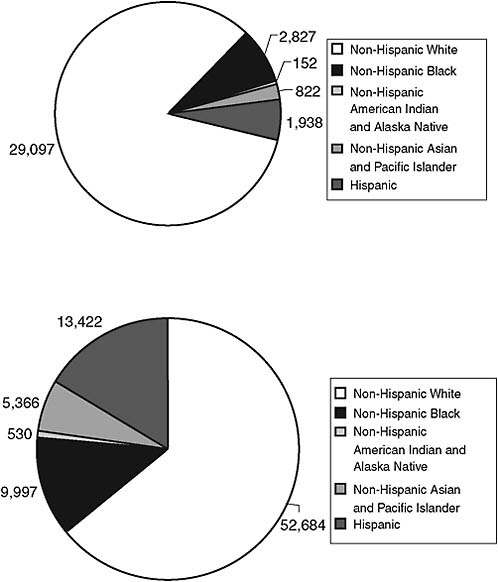
FIGURE 6-8 Ethnic composition of the U.S. population ages 65+ in 2000 and projections for 2050.
SOURCE: U.S. Census Bureau, Population Projections of the United States by Age, Sex, Race, Hispanic Origin, and Nativity: 1999 to 2100. Available: http://www.census.gov/population/www/projections/natproj.html and http://www.census.gov/population/projections/nation/detail/np-d2.txt [accessed August 2010].
and English-only instructions will not be adequate to ensure accurate comprehension. Whether such barriers as weak language or cognitive skills can be surmounted by having instructional materials that make greater use of symbols, diagrams, or video is not yet well understood (e.g., Morrell and Park, 1993) although video demonstrations of the use of some health care devices are already available on the Internet in languages other than English (e.g., a glucose meter with Spanish instructions on YouTube). At present, people with weak comprehension skills are likely to have lower socioeconomic status and hence be less likely to have fast, convenient access to the Internet.
Home Health Care Use
There are few good sources for assessing home health care use, simply because people do not typically provide records of minor injuries or short-term illnesses that are typically treated at home. As an example, the author’s spouse broke her ankle in 2008 and became quite disabled while confined for a month in a nonwalking cast, having significant initial difficulty performing ADLs. There are few if any public records of this incident, aside from an application filed with the state of Florida for a handicapped parking sticker. However, once people (older or low income) use public funding for medical care, such as the Medicare/Medicaid system, records are available to track such incidents.
Medicare tracks home health expenditures through the Medical Expenditures Panel. The cost of such usage is increasing, although policy changes implemented in 1997 reduced expenditures from 1997 to 1999, more so for the lowest income groups and the frailest patients (Zhu, 2004). Expenditures for home health care since 1999 have continued to increase, although not as fast as for nursing home care (see Figure 6-9). Such patterns suggest that if health care could be delivered more effectively in the home, chronic care treatment costs for older adults could be significantly curtailed. There is evidence through meta-analysis that home care modestly reduces hospital use/cost (Hughes et al., 1997). There is considerable interest in updating technology in the home to produce so-called smart homes or aware homes; however, a recent report looking at smart home technology failed to find a single study suitable for inclusion in the analysis of the efficacy of such homes (Martin et al., 2008).
There is no lack of imagination for how to supply home health care devices and systems (e.g., Dishman, Matthews, and Dunbar-Jacob, 2004; Horgas and Abowd, 2004). However, there is reason to be cautious about seeing this brave new world any time soon, in part because those who would provide and use such systems have not been fully involved in their design and sometimes have unrealistic expectations about ease of use or
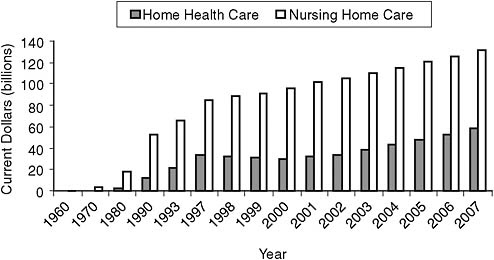
FIGURE 6-9 Expenditures (in constant dollars) on nursing home care and home health care.
SOURCE: Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. Available: http://www.cms.gov/NationalHealthExpendData/downloads/tables.pdf [accessed August 2010].
cost. Thus, one must consider the person-environment fit for any home health care device and system, and this leads to the first commandment of human factors and ergonomics, sometimes phrased as “Honor thy user” or “Know thy user.”
PERCEPTUAL, COGNITIVE, AND PSYCHOMOTOR CAPABILITIES OF USERS
I now briefly review some of the normative changes with age (and disability) that can affect interactions with home health care technology, giving some examples for such abilities as perception, cognition, and psychomotor ability, and anthropometrics.
Perception
In order for a user to interact with a home health care device, it must be perceived in some way. That information channel could be visual, haptic (touch), aural (smell or taste is less likely), or some combination of these modalities. The disabled population and the older population typically have impairments in some or all of these sensory and perceptual systems. Even
the general population above the age of 45-50 is highly unlikely to be able to focus the lens of the eye on fine visual details without corrective lenses.
Thus, text should minimally be about 12 points (x-height) and shown with high contrast (e.g., black on white), and diagrams with fine visual details should be magnified in any materials provided to instruct or train the user. Such guidelines are often violated with printed medication information, as seen in Figure 6-10, in part due to constraints of packaging. Prescription drug containers are now often accompanied by page-sized instruction sheets that do use larger print (although that information may easily become separated from the pill container). As well, lighting in homes generally needs to be increased, although glare should be avoided, given changes to the eye that result in less effective transmission of light through to the retina. There is also some loss of color sensitivity at short wavelengths, making violet-blue-green discrimination more difficult. Given that a significant percent of males in the general population have defective color vision (about 5-8 percent), signaling important information solely through color cues (e.g., red versus green) should be avoided.
Furthermore, particularly for aging men, audition is likely to be impaired, meaning that sounds need to be more intense and environmental noise needs to be minimized to permit adequate comprehension of speech or perception of auditory warnings. For example, alarms on home health care equipment, such as oxygen concentrators, follow standards set by the U.S. Food and Drug Administration and international bodies (e.g., ISO standard IEC 60601-1-8) that specify details, such as the number of frequencies pres-
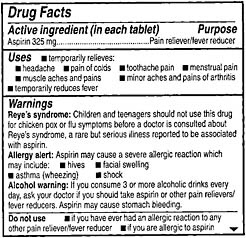
FIGURE 6-10 Scanned image (actual size) of medication information for an aspirin bottle. Print size is too small for older adults with presbyopia and those with visual impairments.
ent in the warning sound, but apparently not the decibel level for the alarm, relying on “the experience of medical equipment designers.” For users who are hard of hearing, such audible alarms may not be very audible, although the devices also use flashing light indicators. See Fisk et al. (2009) for a review of older adult capabilities and a guide to design.
Cognition
Some aspects of cognition improve with age, particularly the accumulation of knowledge tapped by tests of certain aspects of intelligence and, in young children, the ability to hold and manipulate information in working memory (e.g., as indexed with memory span measures; Dempster, 1981). Thus, particularly when considering adherence to routines that require prospective memory (i.e., remembering to carry out future actions), young children are likely to be disadvantaged. An example might be medication adherence, for which a caregiver would be required to assist the child in taking prescription drugs. Another case would be remembering to carry an inhaler to school to treat potential asthma attacks (see American Academy of Pediatrics, 2009, for general advice about home health care for children).3
In adulthood, the usual pattern is for abstract problem-solving skills (fluid abilities) to decline sharply, with a drop of about 1.5 to 2 standard deviations between the 20s and the 80s (Salthouse, 2010). Such declines are likely to have an impact on the ability to troubleshoot new malfunctioning health care devices. A particularly striking change in cognition is slowing in the learning rate. An older adult may require twice as much time as younger adults to learn to use software (e.g., Charness et al., 2001). Thus, when needing to learn to use a new home health care device from instructional materials, both very young children and older adults are likely to be disadvantaged, as will be those with poor English comprehension skills and veterans with closed head injuries (increasingly common for recent veterans because of roadside bomb incidents). Maximizing ease of comprehension by ensuring that instructional prose is at a grade 8 or lower level, coupled with providing some indication of training time needed (to provide realistic expectations), could help less cognitively able users. See Charness and Czaja (2006) for an overview of issues in training older workers that has relevance to the use of health care devices.
Normal aging is likely to impair working memory capacity (ability
to store and manipulate cognitive representations) and speed of processing generally—and even more so for abnormal aging or dementia (see Jastrzembski and Charness, 2007, for information processing parameters for younger and older adults). Such cognitive changes could, for example, make it difficult to learn and remember the step-by-step procedure needed for blood glucose monitoring (which might be 50-60 steps long; Rogers et al., 2001). Thus, users need better “environmental support” (Morrow and Rogers, 2008), by having relevant cues to procedures out in the environment (e.g., having the device provide prompts to the user for tasks), rather than stressing working memory capacity by requiring memory for a long procedure.
Although knowledge tends to increase with age, there are major individual differences in knowledge in the population (e.g., as a function of education) and particularly in knowledge about health, termed health literacy (e.g., in the ability to comprehend written health instructions, see Benson and Forman, 2002; measured in national surveys, see National Center for Education Statistics, 2006). However, this construct may overlap substantially with general cognitive ability (Morrow et al., 2006; Levinthal et al., 2008).
Cognitive changes associated with normal aging, with a dementing illness, and with closed head injuries may also have effects on health care decision making. In some cases—for example, for breast cancer and prostate cancer treatment—there can be considerable uncertainty about the best course of action (e.g., see decision making by younger and older adults in Meyer, Talbot, and Ranalli, 2007). For a review of the heuristics involved in decision making under uncertainty, see Kahneman and Tversky (1979) and Gigerenzer and Goldstein (1996). A recent meta-synthesis outlines some of the factors involved in shared decision-making processes among patients and health care providers (Edwards, Davies, and Edwards, 2008). Factors involved in the information exchange process during health consultations were broken into practitioner influences, patient influences, and joint influences. Practitioner factors included receptiveness to informed patients and patient choice, knowledge of cultural differences, and degree of patient centeredness or stereotyping. Patient factors included motivation to seek information, appraisal of information (particularly before the interview), cultural identity, and how risk was managed for poor information. Joint influences included differing illness notions, role expectations, and language. Health literacy was identified as an important mediator. Diminished cognition in a health care recipient will obviously affect most facets of joint decision making.
Psychomotor Ability
The slowing in basic information processing speed in middle adulthood mentioned above is also accompanied by less precision in physical movements, such as moving a cursor with a mouse or moving from one key to another on an input device. Accurate movement involves making micro-corrections at the end of movement trajectories, as people undershoot or overshoot on their approach to a target, and general slowing will impact such corrections. Older adults need larger targets (e.g., large, well-spaced keys on keyboard devices) or shorter distances to move to ensure fast, accurate movement. Good design of input devices for home health care systems becomes even more important when considering those with limb tremor or movement initiation disorders (e.g., Parkinson’s disease).
Older adults often also have slower walking speeds and experience negative changes to the vestibular system that make balance less stable, increasing the risk of injury when performing caregiver tasks, such as helping a spouse with transfers from bed or toilet, although help is coming from robotics advances.
Anthropometrics
The size, shape, and flexibility of the human body set important constraints on the way that people interact with tools and environments. One important variation in anthropometric capabilities involves gender. Women are about five inches shorter and two-thirds as strong, on average, as men (for age-related values for anthropometric capabilities, see Steenbekkers and van Beijsterveldt, 1998; Kroemer, 2005). This can affect IADLs, such as cooking (e.g., retrieving and opening jars), caregiver activities, such as assisting a mobility-impaired spouse, and even opening a childproof prescription drug container. As well, there are normative changes in height (people shrink in size) as well as in strength (which diminishes) as people age. However, one of the concerns with population-based approaches to design is that the average capability may describe no member of the sample particularly well. For example, a classic guideline is to design for the 85th percentile capability of a population, but this tends to have an adverse impact on important population subgroups, such as women and children.
USER AND PROVIDER ATTITUDES TOWARD HEALTH CARE AND HEALTH CARE TECHNOLOGY
Attitudes are frequently invoked as an important factor in health care utilization, although most studies provide associations. General attitudes toward health and health care may constrain utilization and treatment
adherence no matter what a person’s cognitive, perceptual, or psychomotor capabilities. An individual’s social network may also play an important role in the process. As an example, a national survey of health care professionals treating child and adolescent obesity found that health care providers cited as barriers to successful treatment both parental involvement and patient motivation (Story et al., 2002).
The well-known observation that men consume less health care than women has prompted considerable speculation about whether attitudes may play a role, such as greater reluctance on the part of men to seek help for health conditions. However, after adjusting for reproductive-related care and age-specific mortality rate differences, there are no sex differences in per capita expenditures when universal health care coverage is available (Mustard et al., 1998). There is evidence consistent with the view that cultural differences in attitudes toward seeking help might underlie ethnic differences in health care utilization (e.g., underutilization by Vietnamese Americans; Thang, Patrick, and Nash, 2009).
Attitudes That Influence Use of Home Health Care Technology
There is not enough space to describe the vast literature on the role of attitudes in health behavior.4 Chapter 11, on social and cultural environments, addresses some key issues; see Cameron (2009) for an overview of major models of persuasion that involve attitude effects. Probably the most popular framework is the theory of planned behavior (Ajzen, 1991), which postulates that behavioral intentions (e.g., for health this might involve diet, exercise, medication adherence, safe sex practices) are best predicted from attitudes toward the behavior, subjective norms about the behavior (e.g., family and friend opinions), willingness to comply with those norms, as well as beliefs about one’s ability to engage in the behavior (control beliefs, such as self-efficacy). Here I focus primarily on the narrower case of attitudes that may influence home health care technology use. Both user and prescriber attitudes are potential barriers to adoption. Attitudes can be differentiated as general (e.g., feelings of self-efficacy approaching any new device) or specific (e.g., feeling inadequate about computer troubleshooting, trusting that a device will work safely or reliably).
As noted in an Institute of Medicine report (1996), demands on health care personnel to learn and deploy telemedicine systems (which are increasingly being used for home health care) are a sticking point for adoption. Similarly, unfamiliarity with technology may be a barrier to adoption. Technology adoption in the United States has accelerated over the past century
(Charness, 2008a) in part because of falling prices, the presence of infrastructure to support deployment, and the exponential increase in wealth. To take the iconic case of the digital computer, there has been a major shift in the public’s perceptions and attitudes toward the computer (e.g., from being seen as scary or threatening; Lee, 1970) as it downsized from a huge, vacuum-tube-laden mass of hardware to a compact consumer product. Still, a Pew Internet and American Life survey (Charness, 2008b) showed that older adults and those with less education were less likely to endorse an item that “technology provides more control over life” and that this control belief was a significant predictor of technology use.
One barrier to widespread delivery of health care information and telehealth services to the home is lack of access to high-speed communication channels, and particularly the Internet, for older adults and low-income users. As Figure 6-11 shows for a recent data set, although Internet access has nearly quadrupled in the past decade for those ages 65 and older, this age group (with chronic health conditions) was still at very low levels of Internet use, 40 percent. Use dropped strikingly with age if this age group was divided into more typical young-old, middle-old, and old-old
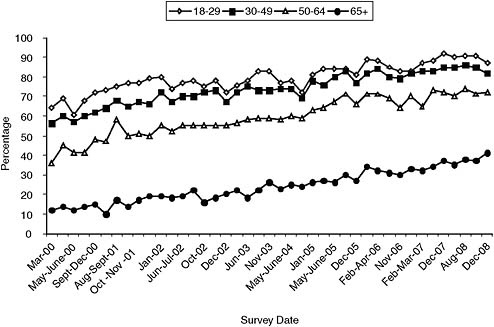
FIGURE 6-11 Percentage of Internet use by age group from March 2000-December 2008.
SOURCE: Pew Internet and American Life Project trend data for “usage over time.” Available: http://www.pewinternet.org/Trend-Data/Usage-Over-Time.aspx [accessed August 2010].
age categories (39, 24, and 8 percent, respectively, for March 2007 data; Charness and Boot, 2009). Furthermore, a significant predictor of computer and Internet use is education and income (Kaiser Family Foundation, 2005); economically disadvantaged groups, who are also the most likely to be in poorer health (e.g., Marmot and Shipley, 1996; Crimmins, Kim, and Seeman, 2009), are the least able to access health care information and services in this way.5
Survey research suggests that attitudes toward health care and health care technology are related to a number of factors, including age, gender, and ethnicity. Katz and Rice (2009) gathered survey data (n = 1,106) that was representative of the U.S. population on interest in getting new or existing services on mobile devices, and particularly radio-frequency identification (RFID) devices attached to the arm or mobile phone. Medical information, such as a hotline to a doctor or notices about health information on mobile devices, was rated less highly on a 1-5 scale (2.2-2.3) than having those devices provide television programs or ads about services (3.7-3.8). There was more interest in monitoring health on the mobile phone (3.1 rating) and very little concern about privacy threat (ratings 2.0-2.5) or privacy rights (rating of 1.5).
In a qualitative analysis of focus groups with congestive heart failure and chronic obstructive pulmonary disease (Rahimpour et al., 2008), low self-efficacy and anxiety were factors identified as affecting perceptions and potential acceptance of a home telecare system (shown in a video). Those with lower self-efficacy and greater anxiety about the video expressed more negative attitudes about intention to use the system.
Blackhall and colleagues (1999) examined general and personal attitudes toward the use of life-sustaining technology (with such questionnaire items as “If life prolonging technology exists, it should always be used”) in a diverse sample of 200 older adults in Los Angeles County. They found greater acceptability of such technology use in Korean American than in African American and Mexican American, and least in European American groups. Men were more accepting than women. Income (less acceptable for higher income than lower) and personal experience with illness (those with more experience about withholding care were less accepting) also played a role in acceptability.
When the question was, “If you were in a coma, and your physicians felt that there was a small but uncertain chance of regaining full awareness and function but a greater chance of surviving with severe mental dis-
abilities, would you want: (a) cardiopulmonary resuscitation; (b) mechanical ventilation?”—the significant factors associated with acceptance were ethnicity, gender, and access to health care, all operating in the same direction as above. In general, people tended to be more accepting of the use of life support technology on others than on themselves. This fits with models of attitudes being differentiable so that general tendencies are less associated with actions to be taken than are specific attitudes (Ajzen and Fishbein, 1977).
A sparsely researched topic in attitudes is the role of religion or religiosity in health care practice. The research literature has found that religiosity is associated with better health (e.g., Krause, 2008), perhaps through the mediating effects of belonging to a close-knit social group and the sense of meaning in life that religious beliefs support. Religiosity can play a major role in home health care when congregants of a religious organization provide services to people who are ill at home. Although some religious beliefs directly affect willingness to accept certain treatments—for example, blood transfusions, or to permit autopsies to be carried out to diagnose causes of death—there are undoubtedly also subtle influences from beliefs, such as what constitutes God’s will, that will affect willingness to seek or to accept home health care treatment. There are also not so subtle effects of religious/political attitudes when political authorities such as a state intervene to enforce medical treatment.6
Another sparsely investigated area of research is individual differences in trust about home health care. For example, trust may play a role in whether someone will seek or accept (care recipient) or offer (provider) help. General trust in medical advice may vary with ethnicity (Krakauer, Crenner, and Fox, 2002).
With respect to attitudes toward technology and computer anxiety, the older adult literature has shown that rather than attitudes predicting people’s performance when trained with that technology, their attitudes change as a function of success with training (e.g., Czaja and Lee, 2008). So there is reason to be optimistic that those with negative attitudes toward health care technology might change in a positive direction if the equipment is well designed and well supported.
Privacy and Confidentiality
Privacy and confidentiality are often cited as concerns for those hoping to provide remote monitoring in homes (or even just for entry of home health care workers), and several frameworks for distinguishing and
understanding these concerns have been advanced (Caine, Fisk, and Rogers, 2006; Hensel, Demiris, and Courtney, 2006). However, data are scarce, with early studies being based on very small focus group samples (Demiris et al., 2004; Mynatt et al., 2004). Fox (2000) looked at a large (n = 2,117) representative sample of Americans in the Pew Internet and American Life Project and found that, although Internet users have a strong stated preference for privacy when they go online, their risky behavior online does not match their stated concerns (19 percent reported credit card or identity theft, although only 8 percent of those cases involved online theft). If anything, older Americans were more concerned than younger ones with privacy (concern was reported as “notably higher” in Fox’s report). One randomized controlled study found greater concern with confidentiality (item was “I was worried that others were listening or watching”) between patients in a telemedicine intervention compared with face-to-face treatment (Chua et al., 2001).
Aside from the Katz and Rice (2009) study mentioned above, which did not have privacy as the sole focus, one large-sample privacy study, Beach et al. (2009), used a web-based survey (hence unlikely to be representative of the older adult population) and was unique in its focus on both older and disabled populations. The critical finding in that study was that more impaired people (older, more disabled) were more willing to share health information (about toileting, medications, movement in the home, cognitive ability, driving behavior) with family members and health care workers, although not with insurance companies or government entities, for the expectation of better care. Curiously, there were few age differences in privacy concerns in this sample, with older adults slightly more willing to share (age ranges: 45-64, 65+). It appears that privacy issues (that is, who has access to what information) are not a strong barrier to home monitoring or mobile monitoring, any more than they have been to electronic commerce.7 As long as perceived usefulness and ease of use (benefits) outweigh perceived costs, people, including older adults (Melehnorst, Rogers, and Bouwhuis, 2006), are willing to adopt technology (e.g., the technology acceptance model of Venkatesh and Davis, 2000).
Nonetheless, it is apparent that different user subgroups exist in the general population with respect to familiarity with, positive attitudes toward, and ability to use home health care technology, and the design community needs to keep this in mind.
|
7 |
Two purveyors of database systems for industry and government were perhaps prescient a decade ago in their comments. Larry Ellison, chief executive officer of Oracle, said “The privacy you are concerned about is largely an illusion.” (http://valleywag.gawker.com/152187/larry-ellisons-privacy-is-largely-an-illusion [accessed May 2010]). And Scott McNealy, chief executive officer of Sun Microsystems, said “You have zero privacy. Get over it.” (http://www.wired.com/politics/law/news/1999/01/17538 [accessed May 2010]). |
Joint Influences on Technology Adoption
Although it is challenging enough to study the simple effects of cognition, perception, and attitudes on home health care use, it is even more challenging to look at joint effects. A salient study that looked at how attitudes, age, and cognitive factors affected technology use, including computer and Internet use, is Czaja et al. (2006). They found that measures of cognitive ability, either fluid or crystallized ones, were strong independent predictors of technology use, including computer and Internet use. Other predictors were attitudes toward technology (computer anxiety, computer self-efficacy) and age.
Thus, it is not surprising that technology use clearly declines with age in nationally representative samples (e.g., Pew Internet and American Life studies of computer and Internet use; Mobilate study in Europe: Tacken et al., 2005). Although this is discouraging from the perspective that older adults (who have chronic conditions) are the most likely to be in need of health care information and access to the Internet might help, it is not the case that they are averse to adopting all health-related technology. As Figure 6-12 illustrates, in contrast to Internet and computer use, mobile phone adoption is relatively high, even in older age categories (50 percent at ages 75-84). Thus, use of mobile phones in telemedicine interventions (e.g., Quinn et al., 2009) is feasible for that group, assuming that people can be convinced to adopt smart phone technology and adopt data plans that provide Internet access from the phone. However, at present, such devices represent a small percentage of overall mobile phone use in the United States (about 25 percent of mobile phone users; see http://news.cnet.com/8301-10787_3-10157264-60.html [accessed May 2010]). Communication devices are central to remote delivery of health care, the burgeoning field of telehealth.
Telehealth Technology
Some of the most promising approaches to supplying home health care come from the field of telemedicine or, as it is also known, telehealth (or e-health). Human factors aspects of telehealth are discussed in Demiris et al. (in press). The practice of supplying health care advice at a distance dates back at least to the 17th century, when plague-stricken English villages would post warning signs at the village entrance (Darkins and Cary, 2000). The next big source of remote health care advice and delivery was the wired line telephone. There is evidence that offering advice through phone conversations leads to better mortality outcomes for Medicare-managed settings (e.g., Alkema et al., 2007). Today we take for granted such services as the ubiquitous 9-1-1 emergency number in the United States and
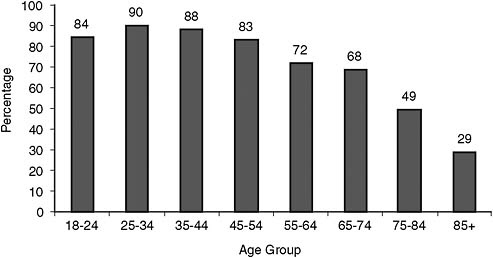
FIGURE 6-12 Mobile phone use by age group.
SOURCE: Pew Internet and American Life Project data for “usage over time.” Available: http://www.pewinternet.org/Trend-Data/Usage-Over-Time.aspx [accessed August 2010].
elsewhere, except for controversies over how to access such services with mobile phone technology. Today, websites on the Internet are a potentially important source of health information for those with Internet access, despite expressed concerns with the accuracy of information on some sites. However, even reputable sites are not necessarily easy to navigate to find relevant information (e.g., the Medicare website; Czaja, Sharit, and Nair, 2008).
An important area for home health care is the monitoring of chronic conditions. Many telehomecare (remote home care) interventions attempt to monitor and treat such conditions as diabetes, congestive heart failure, and hypertension. Monitoring can take many forms, from question-administering devices that report back daily over telephone lines, to sensor sets deployed through the home to track activity and communicate over Internet connections, to complex wearable devices that monitor pulse, temperature, blood oxygen, location, and falls and can report back over wireless channels. In some cases, an instrumented (“aware”) home (Mynatt et al., 2004) can become a coach.
As an Institute of Medicine (1996) report indicated, it is difficult to evaluate clinical applications of telemedicine for a number of reasons, including rapid advances that render some technologies obsolete, infrastructure that is not user-friendly and distracts from practical projects, and high demands on reluctant health care providers. Field and Grigsby (2002)
noted that advances in remote monitoring seem to be driven by work with astronauts and elite athletes. Also, better technology was beginning to lower costs for transmitting information. These trends have continued with deployment of cellular (mobile phone) technologies that are increasing bandwidth, so-called third- and fourth-generation (3G, 4G) networks, although monthly bandwidth caps by providers make them impossible to use for videoconferencing at the moment (author’s 2009 inquiry in Tallahassee, Florida). Together with changes in the subscription to high-speed wired connections in homes (copper wire for DSL, coaxial and fiber optic cable), there is now a better opportunity to transmit data to and from homes.
One can evaluate the impact of an intervention from such perspectives as clinical benefit and cost.8 I use the term “efficacy” to refer to whether the treatment or intervention is better than no treatment or a placebo in a typical clinical trial. A more rigorous test of the intervention would be comparative clinical effectiveness: whether the new intervention is better than the current best clinical practice, also assessed with a clinical trial. However, clinical trials are typically carefully planned interventions with select populations and blinding, and some have argued that regular clinical practice situations may vary in important ways, suggesting the need for “pragmatic trials” (Macpherson, 2004) that use normal clinical settings without blinding. One could argue that human factors approaches can play an important role in ensuring that ideal interventions be implemented successfully in typical clinical settings. Finally, cost-effectiveness refers to the clinical benefit in the context of its cost. For example, if a telemedicine intervention has the same clinical benefit (efficacy or comparative clinical effectiveness) but costs less than a usual treatment, it would be more cost-effective.
An early review (Currell et al., 2000) was equivocal about the cost savings and clinical benefit of telemedicine. A later review was more positive (Hersh et al., 2001), showing significant clinical benefits for management of chronic conditions, including hypertension and AIDS, with less evidence of efficacy for diabetes. A quick review by the author of studies conducted subsequent to those reports indicates that cost-effectiveness was shown for management of congestive heart failure, although in a very small sample (Lehmann, Mintz, and Giacini, 2006) and in a randomized trial for controlling blood pressure (Parati et al., 2009) but not for rehabilitation in a large, quasi-experimental VA study (Bendixen et al., 2009). One can conclude that clinical efficacy for telemedicine is comparable to usual treatment and that patient satisfaction is usually very high. Cost-effectiveness is
|
8 |
There does not appear to be complete agreement on terminology in this area. See http://www.hhs.gov/recovery/programs/cer/draftdefinition.html [accessed May 2010] for a framework on comparative effectiveness research. |
generally unproven, except for cases in which costly transportation expense can be bypassed via videoconferencing.
Telehealth technology has been used for all phases of medical care, from diagnosis to treatment. Telehomecare has been shown to be cost-effective (Bowles and Baugh, 2007). A recent example in the area of mental health is diagnosis of dementia remotely through the use of a screening tool, the mini-mental state examination (Ciemins et al., 2009). Nonetheless, few evaluations have been made of the demands that such systems make on users with chronic conditions or on the willingness of users and their insurers to pay for this form of care.
EXAMPLES OF CONSTRAINTS IN TECHNOLOGY USE: HANDHELD DEVICES
The trend toward miniaturizing devices threatens to exclude potential users with diminished vision, hearing, or touch, although this may pose less of a problem for children. Portable device technology is now being introduced to get information to and from home health care users. Personal digital assistants for medication reminding (Mayhorn et al., 2005) and smart phones employed as part of a wireless communication system (Varshney, 2007) are somewhat handicapped by poor legibility (small screens with tiny fonts) and awkward input capabilities (small, closely spaced buttons or touchable icons). Although such systems are usable by those without significant impairments and can be improved for those with low vision when designed with appropriate tactile and audio feedback for key presses, they are not ideally suited for an aging or disabled health care-using population. Many devices are moving from stylus and button to touch screen input in the expectation that natural gestures will improve usability. But so-called natural gestures, such as a pinching movement on a touchscreen, could prove difficult or impossible for those with movement disorders or prosthetic limbs. Speech recognition may be a viable alternative to requiring fine motor movements (although only in quiet environments). See Lewis and colleagues (2008) for a discussion of human factors issues in designing handheld digital devices.
Personal anecdotes also underline the need for a better person-environment fit for mobile phone use at the level of device design and particularly for instructional support (which is often sparse for mobile phones). Take the case of two nonusing seniors being taught to use mobile phone technology following an acute health problem. When a woman more than 80 years old was in rehabilitation following an auto accident and out of touch (no telephone access could be quickly arranged in the facility), family members brought her a mobile phone and tried to instruct her to use it. However, given her background (high school education, limited technology
experience), disabilities in cognition (mild dementia), pain (broken back), and poor vision (prior unsatisfactory cataract surgery), she was unable to use it effectively. Another similarly elderly woman coming from a more advantaged background (university education, computer user), when hospitalized with an acute gastric incident, was able to learn to use a mobile phone; however, her cognition and eyesight were very good, and the phone was a less complicated, large button model with carefully designed step-by-step instructions (courtesy of the author).
HUMAN FACTORS TOOLS FOR ASSESSING AND DESIGNING PERSON-ENVIRONMENT FIT
In order to assess and design for person-environment fit, the discipline of human factors and ergonomics has developed a number of tools, including task analysis, usability testing, modeling and simulation, questionnaires, and focus group techniques.
Task Analysis
A basic tool for assessing fit is a task analysis (based on Drury’s presentation). This involves breaking down a complex task into a sequence of component operations, usually in a hierarchical fashion corresponding to the goals and subgoals that need to be achieved in order to complete the task successfully. The level of decomposition depends on the goals of the analysis as well as the type of device or environment. For an example, see the task analysis of using a blood glucose meter by Rogers and colleagues (2001). The idea behind such analyses is to uncover components of a task that are difficult to perform or error prone in order to redesign the device or its operating procedures (e.g., to make fewer demands on the user’s limited-capacity working memory or speed of performance) or design better training materials to enable people to perform the task successfully (see the redesign of training materials for a glucose meter by Mykityshyn, Fisk, and Rogers, 2002).
Usability Testing
Often in conjunction with task analysis a usability test will be designed. Here the goal is to observe people attempting to perform representative tasks with the device under realistic conditions (e.g., in a home) in order to identify design and instructional flaws that can be remediated before the device is made available to a targeted user population. Depending on the level of detail needed for assessing performance, an experimenter may simply observe the user by taking notes with the aid of a checklist, make
video recordings, ask the person to think aloud and record their voice while performing the task to reveal the problem-solving processes that they engage in, make eye movement recordings, and perhaps monitor the user with EEG or neuroimaging equipment if records of brain activity are needed. The device may be a working prototype, or a “Wizard of Oz” technique might be used, in which a human substitutes for some function in a device under development. An example of the latter might be having a human listener substitute for a speech comprehension module in a computer coaching system for a smart home that is not yet fully capable of speech comprehension. The human would type the words, which appear on the user’s screen.
Modeling and Simulation
Either as an adjunct to usability testing or as an independent technique, models (e.g., mathematical) and simulations (e.g., computer models) can be used to predict typical human performance without the expense of bringing a user into a laboratory or following their activities in a home environment. Often this involves making use of preexisting simulation environments (e.g., for handheld medical devices, there is Bonnie John’s CogTool; http://cogtool.hcii.cs.cmu.edu/ [accessed May 2010]) or using task analysis in combination with model human processor parameters (Card, Moran, and Newell, 1983) to predict how long tasks would take for different user groups or different devices. Such simulation techniques can uncover design flaws in devices (e.g., inadequate time-out intervals for input on some mobile phones; Jastrzembski and Charness, 2007) without the need for expensive usability testing and can do so for different populations (e.g., younger and older adults) when parameter estimates are available. Typically, a task, such as accessing a health message on a mobile phone, is decomposed into unit tasks (e.g., basic cognitive, perceptual, and motor operations) for which there are estimates of the unit task time or probability of error. The times (or errors) are then summed to estimate total task completion time (or error). Such analysis takes into account technology demands and user capabilities (see Figure 6-3) with degree of fit being determined by the time to complete the task or the probability of making an error.
Questionnaires and Focus Groups
Questionnaires can be an efficient way to assess some of the dimensions of person-environment fit, for either a high-tech or a low-tech device (e.g., an illuminated magnifying lens to help those with low vision to read health care instructions). Either standard instruments (e.g., that assess ease of use and perceived usefulness) or tailored ones can quickly probe user attitudes,
satisfaction, and degree of workload experienced for a device. Similarly, focus group studies with transcription and coding of user discussion can uncover concerns and preferences in a reasonably cost-effective manner. For tutorials on these techniques, see Fisk et al. (2009).
GAPS IN KNOWLEDGE
Research is needed to fill in gaps about user attitudes, knowledge about the home environment, and knowledge about what home health care interventions are cost-effective.
Knowledge of User Attitudes
There is a lack of representative data on attitudes toward health care technologies (e.g., privacy concerns and trust), health care technology adoption, and, more importantly, technology abandonment. Surveys could be commissioned to address these issues as part of the U.S. Census Bureau’s Current Population Survey. In general, there are few population-representative studies about health care technology attitudes and health care technology adoption. Few studies investigate the influence of potentially important mediators or moderators, such as ethnicity, gender, education/income, and age.
There are relatively well-developed models about factors that influence technology adoption that might be adapted to studying home health care technology adoption (e.g., the technology acceptance model). Technologies (and attitudes toward technologies) change rapidly, which makes knowledge acquisition a moving target. A related gap is knowledge about factors influencing abandonment of health care technology. It is evident that maintenance of technology is not simple or easy, so maintenance and repair are important issues to address, particularly for users with low income and education. Mass adoption of home telehealth technology is not likely until there is widespread, competent, and relatively inexpensive technical support available to users.
Knowledge of the Home
Recall that person-environment fit depends on characteristics of both the person and the environment. One reason for the rise of specialized environments for health care delivery, such as hospitals and clinics, is that, in theory, they provide standardized environments for tending to those in ill health. They can provide well-lit, quiet, clean, well-equipped rooms for treatment of patients with fast access to highly trained health care specialists. How does the typical home or apartment environment compare?
There are no systematic surveys of the home health care environment. How many households have access to modern telecommunications links (wireless, broadband)? How many homes have adequate wiring to support modern equipment?9 Something as simple as lighting (which influences legibility of written instructions) varies enormously in homes, partly as a function of the age of the homeowner (Charness and Dijkstra, 1999). I would recommend incorporation of such questions into health care surveys (see as well Chapter 10 on the physical environment).
Knowledge of Home Health Care Efficacy and Cost-Effectiveness
What are the risks and benefits of treating chronic (and acute) conditions in the home? Cochrane reports indicate that there are too few randomized trials to assess efficacy (or cost-effectiveness) of telemedicine with much confidence. Undoubtedly, clinical trials are under way and further meta-analyses are being prepared, but given the unique features of each study from the perspective of population sampled and intervention chosen and also what constitutes usual care for the control group, it will be some time before there are definitive answers to the question of what form of home health care works best. One promising way to proceed is to abandon usual treatment as a comparison point and replace it with currently recognized best treatment.
RECOMMENDATIONS
In order to have successful deployment of home health care, there must be access, sound design, and appropriate training to ensure good person-environment fit. I make three recommendations to promote successful deployment.
-
Promotion of Secure High-Speed Internet Access to Households. Given the importance of access to health care information, coupled with the rapid movement of such information to the Internet, having high-speed Internet access in households is becoming more of a necessity than a luxury. Telehealth applications to homes, including diagnosis, treatment, and rehabilitation, would be facilitated by such access. However, such televisits will depend on having secure communication channels to comply with regulations (e.g., the Health Insurance Portability and Accountability Act, HIPAA, in the United States), as well as on having standardized protocols
-
and interfaces for home health care equipment (e.g., stethoscopes, scales, vital sign monitoring equipment) to minimize cost and training difficulty. Whether such access should be mandated in the same way as basic wired phone service or electricity and provided (with government subsidies if necessary) by current wired cable and phone connections (often unavailable in rural communities) or by soon-to-be-deployed wireless networks is open to debate. However, I recommend that the Federal Communications Commission carry out studies to advise Congress about the best way to bring secure, high-speed access to U.S. households capable of hosting telehealth services, such as videoconferencing.
-
Promotion of Usability Testing for Home Health Care Devices. It is not wise to design and then deploy a health care device or system in a home and expect it to work well for an increasingly diverse population of users. Usability testing should be encouraged with relevant user populations. Universal design (see Chapter 9) is a potential solution, by designing so that anyone, from a child to an impaired adult, could use a device, but it is unrealistic given the range of abilities/disabilities in the population. So inclusive design is the more sensible goal, making it ever easier to use devices, based on a cycle of design, testing, and redesign. Ideally, users of devices would fall into a few well-defined categories so that manufacturers could target them efficiently for testing. Simulation and modeling may prove to be a viable option to potentially expensive usability testing, as models are extended to cover people with more diverse abilities. The Food and Drug Administration currently requires manufacturers of medical devices to attend to human factors concerns. However, many devices not specifically classified as medical devices either could be or are now used to provide information about health care or delivery of home health care services (e.g., mobile phones, computers equipped with webcams for videoconferencing, videogame systems intended to promote physical and mental exercise). I recommend that manufacturers of such products and system integrators be strongly encouraged to provide evidence of efficacy through usability testing (or modeling) of the device with likely user populations.
-
Researching and Promoting Sound Instructional and Training Principles. Too little is known about the most effective techniques to instruct and train the use of home health care devices and how to search for and evaluate health care information (e.g., from the web) in the increasingly diverse population of home health care users. A good example is the recent Guidelines for Pediatric Home Health Care (American Academy of Pediatrics, 2009), which highlights, in chapter after chapter, the need to train caregivers but offers few if any suggestions for how to do this training or how to assess its efficacy. What are the optimal training principles
-
and techniques for those with low health literacy, those with poor English comprehension skills, those from minority ethnic communities? Although guidelines have been proposed for training older adults (e.g., Fisk et al., 2009), the empirical support behind such recommendations is relatively weak (e.g., being based on those who volunteer for lab-based experiments rather than representative samples). Thus, I recommend that further research be conducted into potential ability-by-treatment interactions for training diverse populations of health care users, emphasizing the use of representative sampling. That is, studies need to assess whether and how ability levels for such variables as literacy, ethnicity, education, and age moderate the effectiveness of different training techniques.
ABOUT THE AUTHOR
Neil Charness is William G. Chase professor of psychology and an associate in the Pepper Institute on Aging and Public Policy at Florida State University. His research interests include understanding relations between age and technology use, expert performance, and work performance.
REFERENCES
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179-211.
Ajzen, I., and Fishbein, M. (1977). Attitude-behavior relations: A theoretical analysis and review of empirical research. Psychological Bulletin, 84, 888-918.
Alkema, G.E., Wilber, K.H., Shannon, G.R., and Allen, D. (2007). Reduced mortality: The unexpected impact of a telephone-based care management intervention for older adults in managed care. Health Services Research, 42, 1,632-1,650.
Allen, K.G. (2005). Long-term care financing: Growing demand and cost of services are straining federal and state budgets. GAO Testimony Before the Subcommittee on Health, Committee on Energy and Commerce, House of Representatives. GAO-05-564T. Available: http://www.gao.gov/new.items/d05564t.pdf [accessed July 2009].
American Academy of Pediatrics. (2009). Guidelines for pediatric home health care (2nd ed.) Elk Grove Village, IL: Author.
Anderson, G., and Horvath, J. (2002). Chronic conditions: Making the case for ongoing care. Baltimore, MD: Johns Hopkins University Press.
Baer, J., Kutner, M., and Sabatini, J. (2009). Basic reading skills and the literacy of America’s least literate adults: Results from the 2003 National Assessment of Adult Literacy (NAAL) supplemental studies (NCES 2009-481). Washington, DC: National Center for Education Statistics, U.S. Department of Education. Available: http://nces.ed.gov/pubs2009/2009481.pdf [accessed August 2009].
Beach, S.R., Schulz, R., Downs, J., Matthews, J., Barron, B., and Seelman, K. (2009). Disability, age, and informational privacy attitudes in quality of life technology applications: Results from a national web survey. ACM Transactions on Accessible Computing (TACCESS), 2(1), 1-21.
Beck, R.A., Arizmendi, A., Purnell, C., Fultz, B.A., and Callahan, C.M. (2009). House calls for seniors: Building and sustaining a model of care for homebound seniors. Journal of the American Geriatric Society, 57(6), 1,103-1,109.
Bendixen, R.M., Levy, C.E., Olive, E.S., Kobb, R.F., and Mann, W.C. (2009). Cost effectiveness of a telerehabilitation program to support chronically ill and disabled elders in their homes. Telemedicine and e-Health, 15, 31-38.
Benson, J.G., and Forman, W.B. (2002). Comprehension of written health care information in an affluent geriatric retirement community: Use of the Test of Functional Health Literacy. Gerontology, 48, 93-97.
Blackhall, L.J., Frank, G., Murphy, S.T., Michel, V., Palmer, J.M., and Azen, S.P. (1999). Ethnicity and attitudes towards life sustaining technology. Social Science and Medicine, 48, 1,779-1,789.
Bowles, K.H., and Baugh, A.C. (2007). Applying research evidence to optimize telehomecare. Journal of Cardiovascular Nursing, 22, 5-15.
Boyle, J.P., Honeycutt, A.A., Venkat Narayan, V.M., Hoerger, T.J., Giess, L.S., Chen, H., and Thompson, T.J. (2001). Projection of diabetes burden through 2050: Impact of changing demography and disease prevalence in the United States. Diabetes Care, 24, 1,936-1,940.
Brickfield, C.F. (1984). Attitudes and perceptions of older people toward technology. In P.K. Robinson and J.E. Birren (Eds.), Aging and technological advances (pp. 31-38). New York: Plenum.
Caine, K.E., Fisk, A.D., and Rogers, W.A. (2006). Benefits and privacy concerns of a home equipped with a visual sensing system: A perspective from older adults. Proceedings of the Human Factors and Ergonomics Society, 50th Annual Meeting, pp. 180-184. Available: http://awarehome.imtc.gatech.edu/publications/Caine-Fisk-Rogers-2006P.pdf [accessed May 2010].
Cameron, K.A. (2009). A practitioner’s guide to persuasion: An overview of 15 selected persuasion theories, models and frameworks. Patient Education and Counseling, 74, 309-317.
Card, S.K., Moran, T.P., and Newell, A. (1983). The psychology of human-computer interaction. Hillsdale, NJ: Lawrence Erlbaum Associates.
Centers for Disease Control and Prevention. (2008). Self-reported falls and fall-related injuries among persons aged > 65 years—United States, 2006. Morbidity and Mortality Weekly Report, 57, 225-229. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5709a1.htm [accessed July 2009].
Charness, N. (2008a). Technology as multiplier effect for an aging work force. In K.W. Schaie and R. Abeles (Eds.), Social structures and aging individuals: Continuing challenges (pp. 167-192). New York: Springer.
Charness, N. (2008b). Computer and Internet use in the United States of America: Influence of age, attitude, employment status, and education. International Society for Gerontechnology Proceedings, June 4, Pisa, Italy.
Charness, N., and Boot, W.R. (2009). Aging and information technology use: Potential and barriers. Current Directions in Psychological Science, 18, 253-258.
Charness, N., and Czaja, S.J. (2006). Older worker training: What we know and don’t know. AARP Public Policy Institute #2006-22. Washington, DC: AARP. Available: http://assets.aarp.org/rgcenter/econ/2006_22_worker.pdf [accessed June 2010].
Charness, N., and Dijkstra, K. (1999). Age, luminance, and print legibility in homes, offices, and public places. Human Factors, 41, 173-193.
Charness, N., Kelley, C.L., Bosman, E.A., and Mottram, M. (2001). Word processing training and retraining: Effects of adult age, experience, and interface. Psychology and Aging, 16, 110-127.
Chua, R., Craig, J., Wootton, R., and Patterson, V. (2001). Randomized controlled trial of telemedicine for new neurological outpatient referrals. Journal of Neurology, Neurosurgery, and Psychiatry, 71, 63-66.
Ciemens, E.L., Holloway, B., Coon, P.J., McClosky-Armstron, T., and Min, S-J. (2009). Telemedicine and the mini-mental state examination: Assessment from a distance. Telemedicine and e-Health, 5, 476-478.
Cooper, J., and Kugler, M.B. (2008). The digital divide: The role of gender in human computer interaction. In A. Sears and J.A. Jacko (Eds.), The human-computer interaction handbook: Fundamentals, evolving technologies, and emerging applications (pp. 763-775). Boca Raton, FL: CRC Press.
Crimmins, E.M., Kim, J.K., and Seeman, T.E. (2009). Poverty and biological risk: The earlier “aging” of the poor. Journals of Gerontology Series A: Biological and Medical Sciences, 64A, 286-292.
Currell, R., Urquhart, C., Wainwright, P., and Lewis, R. (2000). Telemedicine versus face to face patient care: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, 2, CD002098. DOI: 10.1002/14651858.
Czaja, S.J., and Lee, C.C. (2008). Information technology and older adults. In J.A. Jacko and A. Sears (Eds.), The human-computer interaction handbook: Fundamentals, evolving technologies, and emerging applications (pp. 777-792). New York: Lawrence Erlbaum Associates.
Czaja, S.J., Charness, N., Fisk, A. D., Hertzog, C., Nair, S. N., Rogers, W. A., and Sharit, J. (2006). Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychology and Aging, 21, 333-352.
Czaja, S.J., Sharit, J., and Nair, S.N. (2008). Usability of the Medicare health web site. Journal of the American Medical Association, 300, 790-792.
Czaja, S.J., Sharit, J., Charness, N., Fisk, A.D., and Rogers, W. (2001). The Center for Research and Education on Aging and Technology Enhancement (CREATE): A program to enhance technology for older adults. Gerontechnology, 1, 50-59.
Darkins, A.W., and Cary, M.A. (2000). Telemedicine and telehealth: Principles, policies, performance and pitfalls. New York: Springer.
Declercq, E.R., Paine, L.L., and Winter, M.H. (1995). Home birth in the United States, 1989-1992: A longitudinal descriptive report of national birth certificate data. Journal of Nurse-Midwifery, 40, 478-481.
Demiris, G., Charness, N., Krupinski, E., Ben-Arieh, D., Washington, K., and Farberow, B. (in press). Human factors and telehealth: A white paper of the ATA human factors SIG. Submitted to Telemedicine and E-health.
Demiris, G., Rantz, M.J., Aud, M.A., Marek, K.D., Tyrer, H.W., Skubic, M., and Hussam, A.A. (2004). Older adults’ attitudes towards and perceptions of “smart home” technologies: A pilot study. Informatics for Health and Social Care, 2, 87-94.
Dempster, F.N. (1981). Memory span: Sources of individual and developmental differences. Psychological Bulletin, 89, 63-100.
Dishman, E., Matthews, J., and Dunbar-Jacob, J. (2004). Everyday health: Technology for adaptive aging. In National Research Council, Technology for adaptive aging (pp. 179-208). Steering Committee for the Workshop on Technology for Adaptive Aging. R.W. Pew and S.B. Van Hemel (Eds.). Board on Behavioral, Cognitive, and Sensory Sciences, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Economic Systems Inc. (2008). A study of compensation payments for service-connected disabilities: Volume I, executive report. (2008). Available: http://www1.va.gov/op3/docs/ProgramEvaluations/CompPaymentStudy/DS_VOLUME_I_Executive_Report.pdf [accessed April 2009].
Edwards, M., Davies, M., and Edwards, A. (2008). What are the external influences on information exchange and shared decision-making in healthcare consultations? A metasynthesis of the literature. Patient Education and Counseling, 75, 37-52.
Field, M.J., and Grigsby, J. (2002). Telemedicine and remote patient monitoring. Journal of the American Medical Association, 288, 423-425.
Fisk, A.D., Rogers, W.A., Charness, N., Czaja, S.J., and Sharit, J. (2009). Designing for older adults: Principles and creative human factors approaches (2nd ed.). Boca Raton, FL: CRC Press.
Flynn, J.R. (1987). Massive gains in 14 nations: What IQ tests really measure. Psychological Bulletin, 101, 171-191.
Fox, S. (2000). Trust and privacy online: Why Americans want to rewrite the rules. Washington, DC: Pew Internet and American Life Project. Available: http://www.pewinternet.org/~/media//Files/Reports/2000/PIP_Trust_Privacy_Report.pdf.pdf [accessed July 2009].
Fox, S., and Jones, S. (2009). The social life of health information: Americans’ pursuit of health takes place within a widening network of both online and offline sources. Washington, DC: Pew Internet and American Life Project. Available: http://www.pewinternet.org/~/media//Files/Reports/2009/PIP_Health_2009.pdf [accessed August 2009].
Fuhrer, M.J. (2001). Assistive technology outcomes research: Challenges met and yet unmet. American Journal of Physical and Rehabilitation Medicine, 80, 528-535.
Gigerenzer, G., and Goldstein, D.G. (1996). Reasoning the fast and frugal way: Models of bounded rationality. Psychological Review, 103, 650-669.
Hensel, B.K., Demiris, G., and Courtney, K.L. (2006). Defining obtrusiveness in home telehealth technologies: A conceptual framework. Journal of the American Informatics Association, 13, 428-431.
Hersh, W.R., Helfand, M., Wallace, J., Kraemer, J., Patterson, P., Shapiro, S., and Greenlick, M. (2001). Clinical outcomes resulting from telemedicine interventions: A systematic review. BMC Medical Informatics and Decision Making, 1, 1-5. Doi:10.1186/1472-6947-1-5.
Hinsz, V.B., Tindale, R.S., and Vollrath, D.A. (1997). The emerging conceptualization of groups as information processors. Psychological Bulletin, 121, 43-64.
Horgas, A., and Abowd, G. (2004). The impact of technology on living environments for older adults. In National Research Council, Technology for adaptive aging (pp. 230-252). Steering Committee for the Workshop on Technology for Adaptive Aging. R.W. Pew and S.B. Van Hemel (Eds.). Board on Behavioral, Cognitive, and Sensory Sciences, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Hughes, S.L., Ulasevich, A., Weaver, F.M., Henderson, W., Manheim, L., Kubal, J.D., and Bonarigo, F. (1997). Impact of home care on hospital days: A meta analysis. Health Services Research, 32, 415-418.
Institute of Medicine. (1996). Telemedicine: A guide to assessing telecommunications in health care. Committee on Evaluating Clinical Applications of Telemedicine, M.J. Field (Ed.). Division of Health Care Services. Washington, DC: National Academy Press.
Institute of Medicine. (2000). To err is human: Building a safer health system. Committee on Quality of Health Care in America, L.T. Kohn, J.M. Corrigan, and M.S. Donaldson, Eds. Washington, DC: National Academy Press.
Jastrzembski, T.S., and Charness, N. (2007). The model human processor and the older adult: Parameter estimation and validation within a mobile phone task. Journal of Experimental Psychology: Applied, 13, 224-248.
Kahneman, D., and Tversky, A. (1979). Prospect theory: An analysis of decision under risk. Econometrica, 47, 263-292.
Kaiser Family Foundation. (2005). E-health and the elderly: How seniors use the Internet for health information. Report #7223. Menlo Park, CA: Author. Available: http://www.kff.org/entmedia/7223.cfm [accessed June 2010].
Katz, J.E., and Rice, R.E. (2009). Public views of mobile medical devices and services: A U.S. national survey of consumer sentiments towards RFID healthcare technology. International Journal of Medical Informatics, 78, 104-114.
Krakauer, E.L., Crenner, C., and Fox, K. (2002). Barriers to optimum end-of-life care for minority patients. Journal of the American Geriatric Society, 50, 182-190.
Krause, N. (2008). Aging in the church: How social relationships affect health. West Conshohocken, PA: Templeton Foundation Press.
Kroemer, K.H.E. (2005). “Extra-ordinary” ergonomics: How to accommodate small and big persons, the disabled and elderly, expectant mothers, and children. Boca Raton, FL: CRC Press.
Lee, R.S. (1970). Social attitudes and the computer revolution. Public Opinion Quarterly, 34, 53-59.
Lehmann, C.A., Mintz, N., and Giacini, J.M. (2006). Impact of telehealth on healthcare utilization by congestive heart failure patients. Disease Management and Health Outcomes, 14, 163-169.
Leveson, N., and Turner, C.S. (1993). An investigation of the Therac-25 accidents. IEEE Computer, 25, 18-41.
Levinthal, B.R., Morrow, D.G., Tu, W., Wu, J., and Murray, M.D. (2008). Cognition and health literacy in patients with hypertension. Journal of General Internal Medicine, 23, 1,172-1,176.
Lewis, J.R., Commarford, P.M., Kennedy, P.J., and Sadowski, W.J. (2008). Hand-held digital devices. In C. Melody Carswell (Ed.), Reviews of Human Factors and Ergonomics, 4, 105-148. Santa Monica, CA: Human Factors and Ergonomics Society.
Machlin, S., Cohen, J. and Beauregard, K. (2008). Health care expenses for adults with chronic conditions, 2005. Statistical brief #203, May. Rockville, MD: Agency for Healthcare Research and Quality. Available: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st203/stat203.pdf [accessed September 2009].
Macpherson, H. (2004). Pragmatic clinical trials. Complementary Therapies in Medicine, 12, 136-140.
Mainous, A.G., Baker, R., Koopman, R.J., Saxena, S., Diaz, V.A., Everett, C.J., and Majeed, A. (2007). Impact of the population at risk of diabetes on projections of diabetes burden in the United States: An epidemic on the way. Diabetalogia, 50, 934-940.
Manton, K.G., Gu, X., and Lowrimore, G.R. (2008). Cohort changes in active life expectancy in the U.S. elderly population: Experience from the 1982-2004 National Long-Term Care Survey. Journal of Gerontology: Social Sciences, 63B, S269-S281.
Manton, K.G., Lamb, V.L., and Gu, X. (2007). Medicare cost effects of recent U.S. disability trends in the elderly: Future implications. Journal of Aging and Health, 19, 359-381.
Marmot, M.G., and Shipley, M.J. (1996). Do socioeconomic differences in mortality persist after retirement? 25-year follow up of civil servants from the first Whitehall study. British Medical Journal, 313, 1,177-1,180.
Martin, S., Kelly, G., Kernohan, W.G., McCreight, B., and Nugent, C. (2008). Smart home technologies for health and social care support. Cochrane Database of Systematic Reviews, 4, CD006412. DOI:10.1002/14651858.CD006412.pub2.
Mayhorn, C.B., Lanzolla, V.R., Wogalter, M.S., and Watson, A.M. (2005). Personal digital assistants (PDAs) as medication reminding tools: Exploring age differences in usability. Gerontechnology, 4, 128-140.
Melenhorst, A., Rogers, W.A., and Bouwhuis, D.G. (2006). Older adults’ motivated choice for technological innovation: Evidence for benefit-driven selectivity. Psychology and Aging, 21, 190-195.
Meyer, B.J.F., Talbot, A.P., and Ranalli, C. (2007). Why older adults make more immediate treatment decisions about cancer than younger adults. Psychology and Aging, 22, 505-524.
Morrell, R.W., and Park, D.C. (1993). The effects of age, illustrations, and task variables on the performance of procedural assembly tasks. Psychology and Aging, 8, 389-399.
Morrow, D.G., and Rogers, W.A. (2008). Environmental support: An integrative framework. Human Factors, 50, 589-613.
Morrow, D., Clark, D., Tu, W., Wu, J., Weiner, M., and Steinley, D. (2006). Correlates of health literacy in patients with chronic heart failure. The Gerontologist, 46, 669-676.
Mustard, C.A., Kaufert, P., Kozyrskyj, A., and Mayer, T. (1998). Sex differences in use of health care services. New England Journal of Medicine, 338, 1,678-1,683.
Mykityshyn, A.L., Fisk, A.D., and Rogers, W.A. (2002). Learning to use a home medical device: Mediating age-related differences with training. Human Factors, 44, 354-364.
Mynatt, E.D., Melenhorst, A.S., Fisk, A.D., and Rogers, W.A. (2004). Aware technologies for aging in place: Understanding user needs and attitudes. IEEE Pervasive Computing, 3, 36-41.
National Center for Education Statistics. (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). M. Kutner, E., Greenberg, Y. Jin, and C. Paulsen, Eds. Washington, DC: U.S. Department of Education.
National Center for Health Statistics. (2008). Health, United States, 2008 with chartbook. Available: http://www.cdc.gov/nchs/data/hus/hus08.pdf [accessed April 2009].
National Institute on Aging, National Institutes of Health, and U.S. Department of Health and Human Services. (2007). Growing older in America: Health and retirement study. Institute for Social Research, University of Michigan. Available: http://hrsonline.isr.umich.edu/index.php?p=dbook [accessed August 2010].
Parati, G., Omboni, S., Abini, F., Piantoni, L., Giuliano, A, Revera, M., Illyes, M., and Mancia, G. (2009). Home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. Journal of Hypertension, 27, 198-203.
Pauly, R.P., Gill, J.S., Rose, C.L., Asad, R.A., Chery, A., Pierratos, A., and Chan, C.T. (2009). Survival among nocturnal home haemodialysis patients compared to kidney transplant recipients. Nephrology Dialysis Transplantation, 24, 2,915-2,919.
Quill, T.E. (2005). Terri Schiavo—A tragedy compounded. New England Journal of Medicine, 352, 1,630-1,633.
Quinn, C.C., Gruber-Baldini, A.L., Shardell, M., Weed, K., Clough, S.S., Peeples, M., Terrin, M., Bronich-Hall, L., Barr, E., and Lender, D. (2009). Mobile diabetes intervention study: Testing a personalized treatment/behavioral communication intervention for blood glucose control. Contemporary Clinical Trials, 30, 334-346.
Rahimpour, M., Lovell, N.H., Celler, B.G., and McCormick, J. (2008). Patient’s perceptions of a home telecare system. International Journal of Medical Informatics, 77, 486-498.
Rogers, E.M. (2003). Diffusion of innovations (5th ed.). New York: Free Press.
Rogers, W.A., Mykitshyn, A.L., Campbell, R.H., and Fisk, A.D. (2001). Analysis of a “simple” medical device. Ergonomics in Design, 9, 6-14.
Salas, E., and Cannon-Bowers, J.A. (2001). The science of training: A decade of progress. Annual Review of Psychology, 52, 471-499.
Salthouse, T.A. (2010). Major issues in cognitive aging. Oxford: Oxford University Press.
Schoen, C., Davis, K., How, S.K., and Schoenbaum, S.C. (2006). U.S. health system performance: A national scorecard. Health Affairs, 25, W457-W475.
Soni, A. (2009). The five most costly conditions, 1996 and 2006: Estimates for the U.S. civilian noninstitutionalized population. Statistical brief #248, July. Rockville, MD: Agency for Healthcare Research and Quality. Available: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st248/stat248.pdf [accessed September 2009].
Steenbekkers, L.P.A., and van Beijsterveldt, C.E.M. (Eds.). (1998). Design-relevant characteristics of ageing users. Delft, The Netherlands: Delft University Press.
Story, M.T., Neumark-Stzainer, D.R., Sherwood, N.E., Holt, K., Sofak, D., Trowbridge, F.L., and Barlow, S.E. (2002). Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics, 110, 210-214.
Tacken, M., Marcellini, F., Mollenkopf, H., Ruoppila, I., and Széman, Z. (2005). Use and acceptance of new technology by older people. Findings of the international MOBILATE survey: “Enhancing mobility in later life.” Gerontechnology, 3, 126-137.
Thang, L., Patrick, L., and Nash, S.G. (2009). Help-seeking attitudes among Vietnamese Americans: The impact of acculturation, cultural barriers, and spiritual beliefs. Social Work in Mental Health, 7, 476-493.
Tyrer, F., Smith, L.K., and McGrother, C.W. (2007). Mortality in adults with moderate to profound intellectual disability: A population-based study. Journal of Intellectual Disability Research, 51, 520-527.
U.S. Census Bureau. (2009). Current population survey, 2008 annual social and economic supplement. Available: http://www.census.gov/population/socdemo/hh-fam/cps2008/tabH2-all.xls [accessed June 2009].
U.S. Census Bureau. (2010). American community survey, 2006. Available: http://www.census.gov/acs/www/ [accessed July 2010].
Varshney, U. (2007). Pervasive healthcare and wireless health monitoring. Mobile Network Applications, 12, 113-127. DOI 10.1007/s11036-007-0017-1.
Venkatesh, V., and Davis, F.D. (2000). A theoretical extension of the technology acceptance model: Four longitudinal case studies. Management Science, 46, 186-204.
Wilson, D.M., Truman, C.D., Thomas, R., Fainsinger, R., Kovacs-Burns, K., Forggatt, K., and Justice, C. (2009). The rapidly changing location of death in Canada, 1994-2004. Social Science and Medicine, 68, 1,752-1,758.
Zhu, C.W. (2004). Effects of the balanced budget act on Medicare home health utilization. Journal of the American Geriatric Society, 52, 989-994.
Suggested General Readings
Carayon, P., and Friesdorf, W. (2006). Human factors and ergonomics in medicine. In G. Salvendy (Ed.), Handbook of human factors and ergonomics (3rd ed., pp. 1,517-1,537). Hoboken, NJ: Wiley.
Fisk, A.D., Rogers, W.A., Charness, N., Czaja, S.J., and Sharit, J. (2009). Designing for older adults: Principles and creative human factors approaches (2nd ed.). Boca Raton, FL: CRC Press.
Jacko, J.A., and Sears, A. (Eds.). (2008). The human-computer interaction handbook Part V: Designing for diversity (2nd ed.). New York: Lawrence Erlbaum Associates.
Krupinski, E., Dimmick, S., Grigsby, J., Mogel, G., Puskin, D., Speedie, S., Stamm, B., Wakefield, B., Whited, J., Whitten, P., and Yellowlees, P. (2006). Research recommendations for the American Telemedicine Association. Telemedicine and e-Health, 12, 579-589.












































