10
Congenital Heart Disease
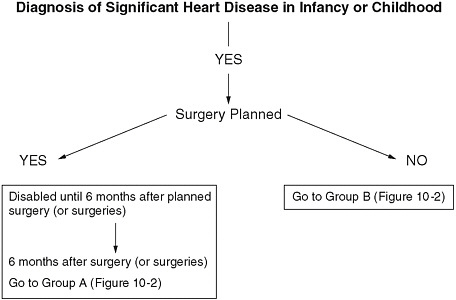
This chapter includes a recommendation that evaluation for disability due to congenital heart disease be divided into four age groupings consistent with the changed timing of surgery for these defects and the developmental capacities of these age groups; criteria for evaluating functional impairment for each age group; a recommendation that one form of congenital heart disease of great severity meet the listing without additional evaluation of functional limitation; and a recommendation that all persons with congenital heart disease being evaluated for disability have information included in their applications about comorbidities, specifically any learning disability, cognitive impairment, depression, and anxiety.
DESCRIPTION
Congenital heart disease is an umbrella term that covers all heart defects present at birth, including dozens of defects that may occur singly or in combination. The abnormal structure of the cardiac chambers, valves, or great vessels in patients with congenital heart disease alters the normal pattern of blood flow. Additionally, individuals with congenital heart disease may develop cardiac complications such as arrhythmias, heart failure, and valve insufficiency, even after surgical correction of the structural abnormalities. In the 1980s, survival to 1 year of age of all individuals born with congenital heart defects was 81 percent (Ferencz et al., 1993), but by 2003 this had improved to 92 percent (Tennant et al., 2010).
Surgery is the mainstay of treatment for congenital heart disease, and the expected results can be classified as follows:
-
Curative: Patients with these conditions rarely have long-term sequelae after surgical correction in childhood. These conditions are patent ductus arteriosus, secundum atrial defect, and uncomplicated ventricular septal defect.
-
Reparative: Patients with these defects are improved after corrective surgery, yet have lifelong sequelae, and some proportion will have significant late impairment. These defects are aortic stenosis, atrioventricular canal, coarctation of the aorta, partial anomalous pulmonary venous return, pulmonary stenosis, tetralogy of Fallot, total anomalous pulmonary venous return, d-transposition of the great arteries, and l-transposition (also called congenital corrected transposition of the great arteries).
-
Palliative: Surgery in these patients (if done) does not fully correct the underlying defect, so they are likely to have significant lifelong impairment of function. These defects are Eisenmenger syndrome, hypoplastic left heart syndrome, malaligned atrioventricular canal with single ventricle repair, single ventricle, tricuspid atresia, and unrepaired cyanotic heart disease.
EPIDEMIOLOGY
Eight out of 1,000 infants are born with congenital heart disease. Of these, approximately 25 percent require immediate surgical or catheter-based intervention (Ferencz et al., 1993). Even with treatment, the lifespan of individuals with congenital heart disease is limited compared with their peers; 89.5 percent of individuals with congenital heart disease are alive at age 20, but for some diagnoses (e.g., truncus arteriosus and single ventricle), the survival is much poorer (Tennant et al., 2010). Survival in individuals with congenital heart disease who reach adulthood is reduced (Verheugt et al., 2010). Death is commonly due to heart failure or sudden death, and risk is increased by arrhythmia, endocarditis, myocardial infarction, and pulmonary hypertension.
In 2000, 1 million adults in the United States were living with congenital heart disease. An estimated half of them had relatively simple residual disease, one quarter had moderately complex residual disease, and one quarter had severe residual disease (Warnes et al., 2001). However, functional disability is not limited to those with “severe” disease, as even an individual with “simple” disease may be disabled due to a complication.
DIAGNOSTIC CRITERIA AND METHODS
The diagnosis of congenital heart disease is made by physical examination, echocardiography, magnetic resonance imaging, cardiac computed tomography, cardiac catheterization, and open-heart surgery. The ICD-9 diagnosis codes indicating congenital heart disease fall primarily between 745.0 and 747.9. Distinguishing among the various congenital heart disease defects can be difficult, and accurate diagnosis can require special expertise and training. Children with congenital heart disease are best evaluated, when possible, in pediatric cardiology centers and by echocardiographic centers certified in congenital heart disease. Adults with congenital heart disease are best evaluated by specialized centers devoted to the evaluation and treatment of such adults. These centers are recommended for their ongoing care (Warnes et al., 2008).
CONSIDERATION OF NONCARDIAC CONGENITAL ANOMALIES
The evaluation of disability status in individuals with congenital heart disease is further complicated by the presence of concomitant noncardiac congenital abnormalities in about 20 percent of cases (e.g., diGeorge syndrome and Down syndrome, among others). Individuals with congenital heart disease also have a higher prevalence of neuropsychiatric disorders, including learning disabilities, cognitive impairment, depression, and anxiety.
TREATMENT
Recent Advances
Surgical intervention for congenital heart disease began in the mid-1960s and was first applied to infants in the mid-1970s. Advances in surgical techniques have continued since that time. These include the development of staged palliation for hypoplastic left heart syndrome. Catheter-based treatment is also evolving rapidly, permitting the placement of valves and closure of atrial and ventricular defects percutaneously in some patients. Drug treatments for the complications of congenital heart disease have also advanced, including the development of medications for pulmonary hypertension (Eisenmenger syndrome) and better drug treatments for heart failure and arrhythmias.
Side Effects of Treatments
With improvement in infant surgery and palliation of more complex lesions, the number of survivors of congenital heart disease has increased
and the population of children and adults with congenital heart disease in the United States has grown.
Residual defects after surgical repair may contribute to functional impairment (Perloff and Warnes, 2001: adapted from information presented in Table 2). They can be classified as follows:
-
Valvular: Mitral or tricuspid insufficiency, pulmonary insufficiency, mitral stenosis
-
Ventricular
-
Ventricular inversion, atrial baffling of blood flow
-
Hypertrophy
-
Abnormal systolic or diastolic function
-
-
Vascular: Abnormal venous connections
-
Prosthetic: Synthetic conduits, artificial valves
Even when surgical treatment corrects the abnormal anatomy, patients may still have late complications and sequelae. The incidence of atrial arrhythmias increases with age: up to 40 percent of adults with congenital heart disease may have atrial arrhythmias by age 50 (Bouchardy et al., 2009). Pulmonary vascular resistance may be increased as a result of longstanding left-to-right shunting.
Trends in Morbidity and Mortality
Survival improved for infants to 90 percent by the 1990s, but long-term survival remains diminished compared with the general population. With extended lifespan after surgery, more late sequelae of congenital heart disease are evident among adults.
DISABILITY
Congenital Heart Disease and Work/Effort
In one European database, 59 percent of adults with complex congenital heart disease had paid employment, compared with 76 percent of patients with mild, complex congenital heart disease. The employment rate among adults with complex disease was significantly less than the general population (Kamphuis et al., 2002). Learning disabilities, depression, and syndromic comorbidities may also impair the ability of individuals with congenital heart disease to hold gainful employment.
Other conditions that may affect overall functional status among congenital heart patients include developmental abnormalities, mental retardation, growth retardation, somatic abnormalities (auditory, dental,
facial, musculoskeletal), central nervous system abnormalities, seizures, visual abnormalities, and medical disorders (e.g., renal insufficiency or liver cirrhosis).
Congenital Heart Disease and Functional Limitation
Children
Prior to cardiac surgery many children are unable to feed normally, requiring frequent prolonged or enteral feedings. Children may lack normal muscle strength and, consequently, may have delayed development. They may be unable to attend day care because of weakness or intolerance to respiratory infections. Infants may require home monitoring of heart rate, respiratory rate, daily weight, and pulse oximetry prior to surgery, compromising their ability to function (Kugler et al., 2009). Some infants have additional noncardiac congenital abnormalities that contribute to medical morbidity or developmental delay.
Following cardiac surgery, children may have variable degrees of disability. At school age, 11 to 17 percent of children who have had an operation for their congenital heart disease have significant limitations in adaptive behavior, socialization, communication skills, and daily living skills (Majnemer et al., 2008). Even after arterial switch operation for transposition of the great arteries, one of the surgical procedures thought to be most successful, one quarter of children were functionally impaired 15 years later. Psychosocial deficits are common (Williams et al., 2003).
Patients who have had only palliative surgery typically have severe lifelong functional limitations. Individuals born with single ventricles, for instance, have exercise capacity of only 50 to 60 percent of what is normal for their ages (Reybrouck and Mertens, 2005), and older individuals are more functionally impaired than younger individuals. Exercise capacity is also decreased in many other complex congenital heart diseases and declines at repeat testing (Manlhiot et al., 2009; Samman et al., 2008; Weipert et al., 1997).
Persons with congenital heart disease may be limited in school or work ability by intrinsic or extrinsic factors. Intrinsic factors may include arrhythmia, chronic heart failure, depression, learning disability, and pulmonary hypertension. Extrinsic factors may include intolerance of lifting weight, intolerance of heat or humidity, lack of stamina, and decreased aerobic capacity. Many patients with congenital heart disease have restrictive lung disease in addition to chronic heart disease (Lubica, 1996).
Neuropsychiatric symptoms (fears, depression, or anxiety) have been identified in 40 to 50 percent of children and adults with complex congenital heart
disease (Bromberg et al., 2003; Cohen et al., 2007; Gupta et al., 1998; Karsdorp et al., 2007; Kovacs et al., 2009; Loup et al., 2009; McCrindle et al., 2006; Norozi et al., 2006.; Spijkerboer et al., 2007; Toren and Horesh, 2007).
Functional limitation in older children and adults with congenital heart disease may be assessed objectively by exercise testing with measurement of maximal oxygen consumption. Effort can be measured by the respiratory exchange ratio. Although measured exercise capacity correlates with perceived quality of life, children and adults with congenital heart disease tend to report greater exercise capacity than would be judged by peak exercise performance (Hager and Hess, 2005).
Age-Related Issues in Evaluation
The functional consequences of congenital heart disease change as children grow into adolescence and adulthood. In addition, surgery alters the natural history of disease in both predictable and unpredictable ways.
Surgery is the mainstay of treatment for congenital heart disease, but the timing and extent of surgery varies according to the specific defect. Most congenital heart defects are now repaired in infancy, certainly by age 1. Single ventricle defects, however, are repaired with staged surgery, using a sequence of several procedures over the first 2 to 3 years of life. Other defects that can be corrected in a single procedure are occasionally delayed until the child reaches a defined size or age.
After the completion of planned corrective surgery, a patient with congenital heart disease may be restored to full functional capacity (e.g., after “curative” procedures) or have residual function limitations. These are best assessed after about 6 months of recovery from the last planned operation.
Growth and development continues through childhood and may alter functional capabilities. The functional status of patients should be relatively stable by age 12, at which time children can cooperate sufficiently to undergo exercise testing. Reevaluation of patients with congenital heart disease at this age can establish their longer-term capacities and facilitate educational and vocational planning. Functional limitations may develop at any age, however, due to the development of arrhythmia, heart failure, endocarditis, or pulmonary hypertension, among other problems.
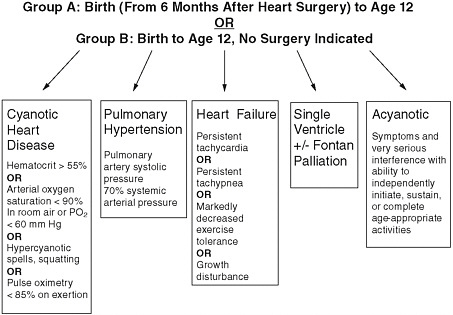
See Figures 10-1 through 10-4 for documentation of congenital heart defects likely to require surgery, from diagnosis of significant heart disease in infancy or childhood through age 12 to adult.
CURRENT LISTINGS
The current listings for children and adults are found in Boxes 10-1 (children) and 10-2 (adults).
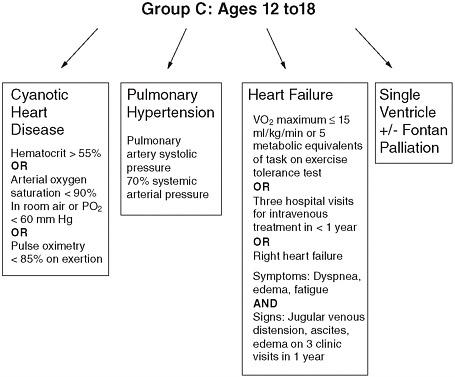
FIGURE 10-3 Documentation of congenital heart defect, disabled by Group C, ages 12 to 18.
CONCLUSIONS AND RECOMMENDATIONS
All Individuals
RECOMMENDATION 10-1. Learning disabilities, cognitive impairment, and associated noncardiac congenital anomalies are frequent comorbidities for individuals with congenital heart disease. Disability evaluators should be trained to understand the effects of these comorbidities to better evaluate if a combination of impairments, no one of which meets a listing, equals a listing.
RECOMMENDATION 10-2. Assessment of disability in children should account for the natural history of congenital heart disease and patterns of development by dividing children into three age/treatment groups:
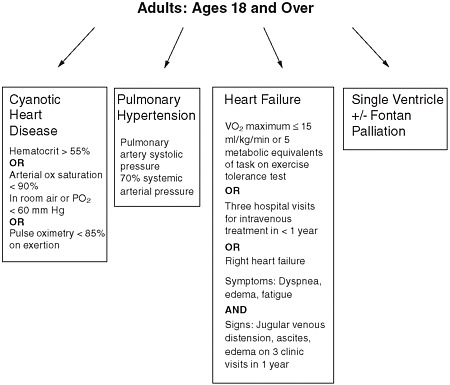
FIGURE 10-4 Documentation of congenital heart defect disabled as adults, ages 18 and over.
Group A: Infants prior to and for 6 months after definitive cardiac surgery;
Group B: Children from 6 months after definitive surgery until age 12 and children from birth onward for whom surgery is not indicated; and
Group C: Children age 12 and older.
RECOMMENDATION 10-3. Infants with a medically confirmed diagnosis of cardiac malformation requiring open-heart surgery should be considered disabled until 6 months after definitive corrective surgery. A diagnosis of significant cardiac disease and documentation of a surgical plan or surgical event should be sufficient evidence of disability.
RECOMMENDATION 10-4. Children from 6 months after definitive cardiac surgery until their 12th birthday and children from birth
|
BOX 10-1 Current Congenital Heart Disease Listing for Children 104.06 Congenital heart disease, documented by appropriate medically acceptable imaging (see 104.00A3d) or cardiac catheterization, with one of the following:
OR
OR
OR
SOURCE: SSA, 2008b. |
|
BOX 10-2 Current Congenital Heart Disease Listing for Adults 4.06 Symptomatic congenital heart disease (cyanotic or acyanotic), documented by appropriate medically acceptable imaging (see 4.00A3d) or cardiac catheterization, with one of the following:
OR
OR
SOURCE: SSA, 2008a. |
onward for whom surgery is not indicated, with congenital heart disease documented by appropriate medically acceptable imaging or cardiac catheterization, with one of the following criteria should be considered disabled:
-
Cyanotic heart disease, with persistent, chronic hypoxemia as manifested by:
-
Hematocrit of 55 percent or greater; or
-
Arterial O2saturation of less than 90 percent in room air, or resting arterial PO2of 60 Torricelli or less; or
-
Hypercyanotic spells, syncope, characteristic squatting, or other incapacitating symptoms directly related to documented cyanotic heart disease; or
-
Exercise intolerance with increased hypoxemia on exertion measured by pulse oximetry.
-
OR
-
Secondary pulmonary vascular obstructive disease with pulmonary arterial systolic pressure elevated to at least 70 percent of the systemic arterial systolic pressure determined by echocardiography or right heart catheterization;
OR
-
Symptomatic acyanotic heart disease interfering seriously with the ability to independently initiate, sustain, or complete activities;
OR
-
Chronic heart failure manifested by:
-
Persistent tachycardia at rest (see Table I1); or
-
Persistent tachypnea at rest (see Table II2); or
-
Markedly decreased exercise tolerance; or
-
Growth disturbance with:
-
An involuntary weight loss or failure to gain weight at an appropriate rate for age, resulting in a fall of 15 percentiles from an established growth curve (on the current Centers for Disease Control and Prevention [CDC] growth chart), which is currently present (see 104.00A3f) and has persisted for 2 months or longer; or
-
An involuntary weight loss or failure to gain weight at an appropriate rate for age, resulting in a fall to below the third percentile from an established growth curve (on the current CDC growth chart), which is currently present (see 104.00A3f) and has persisted for 2 months or longer.
-
-
RECOMMENDATION 10-5. Children age 12 and older should be considered disabled if they have congenital heart disease documented by appropriate medically acceptable imaging or cardiac catheterization, with one of the following criteria:
-
Cyanosis at rest, and:
-
Hematocrit of 55 percent or greater; or
-
Arterial O2saturation of less than 90 percent in room air, or resting arterial PO2of 60 Torricelli (Torr) or less.
-
OR
-
Intermittent right-to-left shunting resulting in cyanosis on exertion (e.g., Eisenmenger’s physiology) as determined by pulse oximetry and with arterial PO2of 60 Torr or less or pulse oximetry 85 percent or less at a workload equivalent to 5 metabolic equivalents of task (METs) or less;
OR
-
Secondary pulmonary vascular obstructive disease with pulmonary arterial systolic pressure elevated to at least 70 percent of the systemic arterial systolic pressure determined by echocardiography or cardiac catheterization;
OR
-
Single ventricle, including hypoplastic left heart syndrome, double inlet left ventricle, and Fontan operation for single ventricle;
OR
-
Chronic heart failure manifested by:
-
Exercise capacity with maximal oxygen consumption less than 15 ml/kg/min or work load less than 5 METs; or
-
Three hospitalizations or emergency room visits with use of intravenous medications for heart failure management in 1 year; or
-
Evidence of right heart failure manifested by:
-
-
-
-
-
Symptoms of dyspnea, edema, or exercise intolerance; and
-
Jugular venous distension, hepatomegaly, ascites, and/or dependent edema on three clinic visits in 1 year.
-
-
-
RECOMMENDATION 10-6. Adults with a medically confirmed diagnosis of congenital heart disease should be considered disabled if they also demonstrate one of the following:
-
Cyanosis at rest, and:
-
Hematocrit of 55 percent or greater; or
-
Arterial O2saturation of less than 90 percent in room air, or resting arterial PO2of 60 Torricelli (Torr) or less;
-
OR
-
Intermittent right-to-left shunting resulting in cyanosis on exertion (e.g., Eisenmenger’s physiology) as determined by pulse oximetry and with arterial PO2of 60 Torr or less or pulse oximetry 85 percent or less at a workload equivalent to 5 metabolic equivalents of task (METs) or less;
OR
-
Secondary pulmonary vascular obstructive disease with pulmonary arterial systolic pressure elevated to at least 70 percent of the systemic arterial systolic pressure determined by echocardiography or right heart catheterization;
OR
-
Single ventricle including hypoplastic left heart syndrome, double inlet left ventricle, and Fontan operation for single ventricle;
OR
-
Diagnosis of congenital heart disease and chronic heart failure manifested by:
-
Exercise capacity with maximal oxygen consumption less than 15 ml/kg/min or work load less than 5 METs; or
-
-
-
Three hospitalizations or emergency room visits with intravenous medication administration for heart failure management in 1 year; or
-
Evidence of right heart failure manifested by:
-
Symptoms of dyspnea, edema, or exercise intolerance; and
-
Jugular venous distension, hepatomegaly, ascites, and dependent edema on three clinic visits in 1 year.
-
-
REFERENCES
Bouchardy, J., J. Therrien, L. Pilote, R. Ionescu-Ittu, G. Martucci, N. Bottega, and A. J. Marelli. 2009. Atrial arrhythmias in adults with congenital heart disease. Circulation 120(17):1679–1686.
Bromberg, J. I., P. J. Beasley, E. J. D’Angelo, M. Landzberg, and D. R. DeMaso. 2003. Depression and anxiety in adults with congenital heart disease: A pilot study. Heart & Lung 32(2):105–110.
Cohen, M., D. Mansoor, H. Langut, A. Lorber. 2007. Quality of life, depressed mood, and self-esteem in adolescents with heart disease. Psychosomatic Medicine 69(4):313–318.
Ferencz, C., J. D. Rubin, C. A. Loffredo, and C. M. Magee. 1993. Epidemiology of congenital heart disease: The Baltimore-Washington Infant Study, 1981–1989. Mount Kisco, NY: Futura Publishing Company.
Gupta, S., R. M. Giuffre, S. Crawford, and J. Waters. 1998. Covert fears, anxiety and depression in congenital heart disease. Cardiology in the Young 8(4):491–499.
Hager, A., and J. Hess. 2005. Comparison of health related quality of life with cardiopulmonary exercise testing in adolescents and adults with congenital heart disease. Heart 91(4):517–520.
Kamphuis, M., T. Vogels, J. Ottenkamp, E. E. Van Der Wall, S. P. Verloove-Vanhorick, and H. W. Vliegen. 2002. Employment in adults with congenital heart disease. Archives of Pediatrics & Adolescent Medicine 156(11):1143–1148.
Karsdorp, P. A., W. Everaerd, M. Kindt, and B. J. M. Mulder. 2007. Psychological and cognitive functioning in children and adolescents with congenital heart disease: A meta-analysis. Journal of Pediatric Psychology 32(5):527–541.
Kovacs, A. H., A. S. Saidi, E. A. Kuhl, S. F. Sears, C. Silversides, J. L. Harrison, L. Ong, J. Colman, E. Oechslin, and R. P. Nolan. 2009. Depression and anxiety in adult congenital heart disease: Predictors and prevalence. International Journal of Cardiology 137(2):158–164.
Kugler, J. D., R. H. Beekman III, G. L. Rosenthal, K. J. Jenkins, T. S. Klitzner, G. R. Martin, S. R. Neish, and C. Lannon. 2009. Development of a pediatric cardiology quality improvement collaborative: From inception to implementation. From the Joint Council on Congenital Heart Disease Quality Improvement Task Force. Congenital Heart Disease 4(5):318–328.
Loup, O., C. von Weissenfluh, B. Gahl, M. Schwerzmann, T. Carrel, and A. Kadner. 2009. Quality of life of grown-up congenital heart disease patients after congenital cardiac surgery. European Journal of Cardio-Thoracic Surgery 36(1):105–111.
Lubica, H. 1996. Pathologic lung function in children and adolescents with congenital heart defects. Pediatric Cardiology 17(5):314–315.
Majnemer, A., C. Limperopoulos, M. Shevell, C. Rohlicek, B. Rosenblatt, and C. Tchervenkov. 2008. Developmental and functional outcomes at school entry in children with congenital heart defects. Journal of Pediatrics 153(1):55–60.
Manlhiot, C., S. Knezevich, E. Radojewski, G. Cullen-Dean, W. G. Williams, and B. W. McCrindle. 2009. Functional health status of adolescents after the Fontan procedure—Comparison with their siblings. Canadian Journal of Cardiology 25(9):e294–e300.
McCrindle, B. W., R. V. Williams, P. D. Mitchell, D. T. Hsu, S. M. Paridon, A. M. Atz, J. S. Li, J. W. Newburger, and Pediatric Heart Network Investigators. 2006. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation 113(8):1123–1129.
Norozi, K., M. Zoege, R. Buchhorn, A. Wessel, and S. Geyer. 2006. The influence of congenital heart disease on psychological conditions in adolescents and adults after corrective surgery. Congenital Heart Disease 1(6):282–288.
Perloff, J. K., and C. A. Warnes. 2001. Challenges posed by adults with repaired congenital heart disease. Circulation 103:2637–2643.
Reybrouck, T., and L. Mertens. 2005. Physical performance and physical activity in grown-up congenital heart disease. European Journal of Cardiovascular Prevention & Rehabilitation 12(5):498–502.
Samman, A., M. Schwerzmann, O. H. Balint, D. Tanous, A. Redington, J. Granton, S. C. Siu, and C. K. Silversides. 2008. Exercise capacity and biventricular function in adult patients with repaired tetralogy of Fallot. American Heart Journal 156(1):100–105.
Spijkerboer, A. W., W. A. Helbing, A. J. J. C. Bogers, R. T. Van Domburg, F. C. Verhulst, and E. M. W. J. Utens. 2007. Long-term psychological distress, and styles of coping, in parents of children and adolescents who underwent invasive treatment for congenital cardiac disease. Cardiology in the Young 17(6):638–645.
SSA (Social Security Administration). 2008a. Listing of impairments—Adult listings (Part A). Disability evaluation under Social Security (Blue Book). http://www.socialsecurity.gov/disability/professionals/bluebook/AdultListings.htm (accessed July 22, 2010).
SSA. 2008b. Listing of impairments—Childhood listings (Part B). Disability evaluation under Social Security (Blue Book). http://www.socialsecurity.gov/disability/professionals/bluebook/ChildhoodListings.htm (accessed July 22, 2010).
Tennant, P. W., M. S. Pearce, M. Bythell, and J. Rankin. 2010. 20-year survival of children born with congenital anomalies: A population-based study. Lancet 375(9715):649–656.
Toren, P., and N. Horesh. 2007. Psychiatric morbidity in adolescents operated in childhood for congenital cyanotic heart disease. Journal of Paediatrics and Child Health 43(10):662–666.
Verheugt, C. L., C. S. P. M. Uiterwaal, E. T. van der Velde, F. J. Meijboom, P. G. Peiper, A. P. J. van Dijk, H. W. Vliegen, D. E. Grobbee, and B. J. M. Mulder. 2010. Mortality in adult congenital heart disease. European Heart Journal 31(10):1220–1229.
Warnes, C. A., R. Liberthson, G. K. Danielson Jr, A. Dore, L. Harris, J. I. E. Hoffman, J. Somerville, R. G. Williams, and G. D. Webb. 2001. Task Force 1: The changing profile of congenital heart disease in adult life. Journal of the American College of Cardiology 37(5):1170–1175.
Warnes, C. A., R. G. Williams, T. M. Bashor, J. S. Child, H. M. Connolly, J. A. Dearani, P. del Nido, J. W. Fasules, T. P. Graham Jr, Z. M. Hijazi, S. A. Hunt, M. E. King, M. J. Landzberg, P. D. Miner, M. J. Radford, E. P. Walsh, and G. D. Webb. 2008. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease) developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital
Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology 52(23):e143–e263.
Weipert, J., W. Koch, J. C. Haehnel, and H. Meisner. 1997. Exercise capacity and mid-term survival in patients with tricuspid atresia and complex congenital cardiac malformations after modified Fontan-operation. European Journal of Cardio-Thoracic Surgery 12(4):574–580.
Williams, W. G., B. W. McCrindle, D. A. Ashburn, R. A. Jonas, C. Mavroudis, E. H. Blackstone, and the Congenital Heart Surgeon’s Society. 2003. Outcomes of 829 neonates with complete transposition of the great arteries 12-17 years after repair. European Journal of Cardio-Thoracic Surgery 24(1):1–9.