13
Renewed Progress in Life Expectancy: The Case of the Netherlands
Johan Mackenbach and Joop Garssen
During the 1980s and 1990s a complete stagnation of mortality decline in older age groups has occurred in the Netherlands, while other high-income countries continued their rapid mortality declines. At first, the stagnation of old-age mortality decline was misinterpreted as a (hopeful) sign of the “rectangularization” of the survival curve as predicted by Fries (Nusselder and Mackenbach, 1996, 1997). Later comparative analyses of old-age mortality developments in a range of high-income countries made clear, however, that the Netherlands is an exception to the rule of continuing old-age mortality decline (Janssen, Mackenbach, and Kunst, 2004). Analyses of cause-of-death patterns showed that the stagnation of old-age mortality decline in the Netherlands could partly be attributed to smoking-related causes of death. The evidence also showed a contribution of ill-defined causes of death, which are typical for old age (e.g., mental and neurological disorders) (Janssen et al., 2003).
A stagnation of mortality decline among the elderly has also been observed in a small number of other countries, particularly the United States and Denmark (Meslé and Vallin, 2006; Glei, Meslé, and Vallin, Chapter 2, in this volume). Interestingly, however, progress in mortality decline among the elderly resumed in Denmark around 1995 (Juel, Bjerregaard, and Madsen, 2000) and in the Netherlands around 2002. The reversal of stagnation into renewed decline in the Netherlands was first noted by Statistics Netherlands in 2002, when the final count of the absolute annual number of deaths in 2001 was slightly lower than the number of deaths in 2000, despite the fact that the proportion of elderly in the population continued to rise. In the first press releases by Statistics Netherlands this was tentatively
ascribed to climatic factors (mild winters, cool summers). When the period of continuous mortality decline became longer, however, it became more and more unlikely that it would be due solely to milder temperatures (Garssen and van der Meulen, 2007).
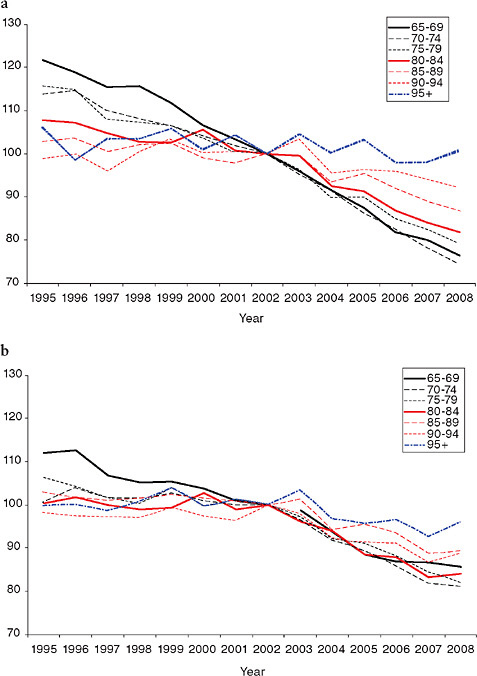
As Figure 13-1 shows, from 2002 to 2008 life expectancy at birth increased by almost 2 years (from 76.0 to 78.3 years among men and from 80.7 to 82.3 years among women). A substantial part of this increase of life expectancy at birth is due to advances at higher ages, as is evident from the fact that life expectancy at age 65 has increased by more than a year (from 15.6 to 17.3 years among men and from 19.3 to 20.5 years among women). The sharpest upturn in life-expectancy trends is seen at age 85, for which 2002 marked a reversal from almost complete stagnation to a period of rapid increases.
No systematic analysis of possible determinants of this remarkable development has been made until now. This chapter aims to assess the possible causes of the reversal from stagnation to renewed decline of old-age mortality in the Netherlands. After an analysis of patterns of decline by age, gender, and cause of death, we review all main groups of determinants: biological factors, factors in the physical and social environment, lifestyle factors, and health care factors. We used readily available data to assess whether changes in these factors have occurred preceding or coinciding with the changes in mortality that could plausibly explain the change in old-age mortality trend.
DATA AND METHODS
Mortality data were extracted from the registry kept at Statistics Netherlands, which is derived from the municipal population registries in the Netherlands. Underlying causes of death were coded according to the International Classification of Diseases (9th and 10th revisions). No changes in coding occurred around 2002. In order to calculate the cause-specific contributions to the gain in life expectancy, we calculated, for both periods, the number of life-years that would be gained if only the observed age-specific mortality risk for a specified cause changed during the period, keeping all other age- and cause-specific mortality risks constant.
Data on determinants of mortality were extracted from various registries and surveys kept at Statistics Netherlands, which are mostly available online at http://statline.cbs.nl/statweb/ [accessed June 8, 2010]. Data on self-reported health problems, lifestyles, and medical care utilization were collected in a multipurpose survey (Permanent Onderzoek Leef Situatie) that is conducted on a continuous basis among a representative sample of the noninstitutionalized population.
Data on clinical incidence (i.e., incidence of the first clinical episode for
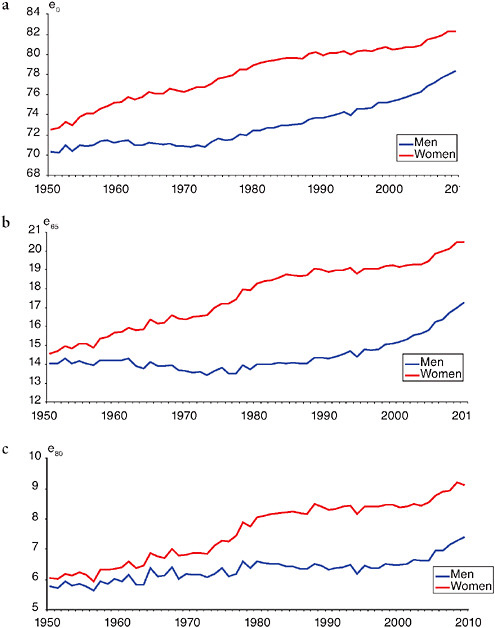
FIGURE 13-1 Life expectancy at birth, age 65 and age 80, by gender, the Netherlands, 1950-2008.
(a) At birth
(b) At age 65
(c) At age 80
SOURCE: Data from Statistics Netherlands (see http://statline.cbs.nl/statweb/ [accessed June 2010]).
a particular disease) and case fatality (i.e., 1-year mortality after the first clinical episode for a particular disease) of specific conditions were extracted from a database constructed by Statistics Netherlands. To construct this database, a linkage has been made between the population registry and the national registry of hospital admissions, which covers more than 90 percent of the Dutch population. This linkage was used to eliminate readmissions of the same individual for the same condition, and to estimate case-fatality rates in a 1-year follow-up period of individuals admitted for a particular condition. Results of these linkages are available for the period 2000-2005 only. The registry of hospital admissions includes clinical as well as day care admissions.
Detailed cost-of-illness studies have been performed by the National Institute for Public Health and the Environment of the Netherlands for the years 1999, 2003, and 2007. These studies are based on a wide range of administrative data covering all health care sectors. Age- and gender-specific patterns of health care expenditure have been determined for 2003 (Slobbe et al., 2006), and data from the 1999 and 2007 studies have been reanalyzed for this chapter to determine time trends of health care expenditure by age and gender.
RESULTS
Mortality Decline
The exact turning point in the mortality trend is difficult to establish because of year-to-year fluctuations in the number of deaths, which are partly determined by climatic conditions (cold winters, hot summers) and influenza epidemics. Around the year 2000 there were several such events: large winter peaks in mortality in early 1999 (around 2,000 additional deaths due to influenza) and early 2000 (around 2,000 additional deaths due to cold), and large summer peaks in mortality in 2003 (between 1,000 and 2,000 additional deaths due the large European heat wave) and in 2006 (two heat waves causing more than 1,000 additional deaths). These events may have partly obscured the starting point of an “underlying” mortality decline.
A simple look at the absolute number of deaths shows that an almost uninterrupted decline in mortality started in 2003. The total numbers of deaths were 140,487 in 1999, 140,527 in 2000, 140,377 in 2001, 142,355 in 2002, 141,936 in 2003, 136,553 in 2004, 136,402 in 2005, 135,372 in 2006, and 133,022 in 2007 (see http://statline.cbs.nl/statweb/ [accessed June 8, 2010]). Despite the 2003 heat wave, the number of deaths in that year was already lower than in 2002, and a year-to-year decline in the absolute number of deaths continued into 2007. The exceptionally large
decline from 2003 to 2004 can probably be explained by the fact that an already declining mortality trend was partly obscured by a temporary rise in mortality due to the 2003 heat wave.
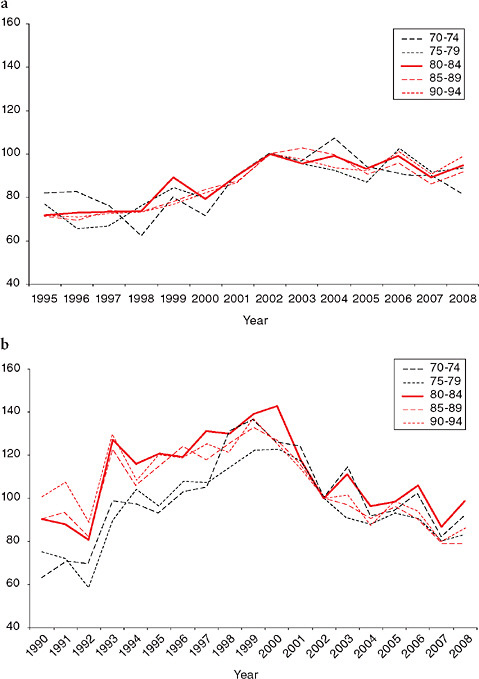
After 2002, mortality declined in all age groups. In younger age groups this represented a continuation of preexisting trends, but in older age groups it reflected a reversal from stable to declining mortality rates. Figure 13-2 shows that this reversal occurred for men in all age groups above age 85, and for women in all age groups above age 65. The simultaneous acceleration of mortality trends in a wide range of age groups also indicates that this was a period rather than a cohort effect.
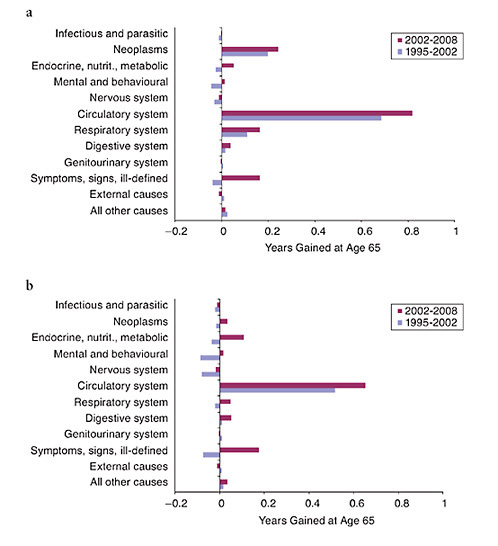
Many causes of death have contributed to the rise in life expectancy at age 65 after 2002, as shown in Figure 13-3. As expected, cardiovascular disease is the main contributor (more than 0.8 years among men, more than 0.6 years among women), but this disease group does not account for most of the trend reversal, because it contributed only slightly less to the rise in life expectancy at age 65 between 1995 and 2002 than to that between 2002 and 2008. The main contributors to the acceleration of the rise in life expectancy at age 65 are causes of death for which the trends were distinctly more favorable in the second as compared with the first period. These include symptoms and ill-defined conditions (mortality from this cause of death category increased during the earlier period and declined during the second period), stroke, diabetes, dementia, and pneumonia. Figure 13-4 illustrates some of the striking changes in trends.
Changes in Determinants
Reviewing trends in a wide range of determinants of mortality, we did not find favorable trends among the elderly in health status indicators paralleling the trend in mortality, which suggests that declining mortality in this period cannot be attributed to improved biological conditions. Table 13-1 shows a few examples. The prevalence of self-reported health problems among the elderly shows a stable or increasing trend, both for generic indicators, like functional limitations, and for specific indicators, like diabetes and hypertension. The clinical incidence of specific diseases has also mostly increased, although there has been a 9 percent decline in the clinical incidence of acute myocardial infarction.
The physical and social environments of the elderly also have not substantially improved in the period under consideration (see Table 13-1). Environmental protection measures have gradually reduced emissions of a number of air pollutants. The main air pollutant which is still contributing to a large number of deaths in the Netherlands is fine dust (PM10), for which emissions have been reduced by about 10 percent, following more rapid declines in the 1990s. Due to climate change, winters are gradually becom-
ing warmer, but this started far before the turn of the century, and winters were not significantly warmer after 2002 than during the 1990s. There have not been very favorable trends for social determinants, either. For example, poverty rates among the elderly have been more or less stable.
Health-related lifestyles also have not substantially improved during this period (see Table 13-1). Smoking rates among the elderly have been stable since the turn of the century. Historical data show that the prevalence of smoking among women ages 65 and above has hovered between 10 and 15 percent since 1980, and among men it has come down substantially during the 1980s and 1990s (Stivoro, 2009). This may partly explain the divergence of old-age mortality trends between men and women during the 1980s and 1990s, but, assuming a time-lag between smoking trends and mortality trends, this divergence cannot account for the reversal among women since 2002. Excessive alcohol consumption and regular exercise among the elderly have been stable as well, while obesity has increased.
The only category of determinants for which substantial changes were seen since the turn of the century are health care factors (see Table 13-1). Modest increases occurred in the proportion of elderly vaccinated against influenza (about 5 percentage points, after more rapid rises during the 1990s), the proportion of elderly seeing a medical specialist (about 3 percentage points), and the proportion of elderly using prescribed drugs (an increase of about 5 percentage points). More substantial increases occurred in the hospital admission rate. In the Netherlands, hospital admission rates rose slowly during the 1990s, but the rate of increase suddenly accelerated after 2001. This acceleration was seen for all age groups, but the strongest acceleration occurred among the elderly (see Table 13-1). This acceleration was seen for many disease groups, including cancer, diseases of the nervous system, cardiovascular diseases, and injuries.
At the same time, mortality within 1 year after hospital admission declined for many conditions (see Table 13-1). Although declines in case fatality were larger for younger people, they were substantial for elderly patients as well. Among those ages 80 and over, the average decline (for all conditions combined) was about 14 percent (from 26 to 22 percent). This decline occurred for many conditions, including coronary heart disease (for which 1-year case fatality declined from 34 to 28 percent) and stroke (for which 1-year case fatality declined from 52 to 45 percent).
More About the Changes in Health Care
The acceleration of the hospital admission trend coincided with a clear-cut change in growth of health care expenditure in the Netherlands. Long-term trends in health care spending in the Netherlands show a very distinct pattern, characterized by rapid growth in the 1960s and 1970s, relatively
TABLE 13-1 Determinants of Mortality, the Netherlands, 1991-2007
|
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
|
|
|
11.4 |
10.5 |
10.4 |
13.0 |
12.6 |
13.2 |
14.1 |
|
|
|
24.5 |
29.9 |
31.3 |
31.6 |
32.8 |
35.5 |
34.9 |
|
|
31.6 |
33.6 |
30.6 |
31.3 |
35.5 |
32.7 |
31.2 |
30.0 |
|
|
18.1 |
19.2 |
18.6 |
17.0 |
21.6 |
20.9 |
17.5 |
18.9 |
|
|
68.3 |
68.9 |
71.3 |
67.5 |
65.8 |
62.1 |
58.0 |
59.3 |
|
|
101.7 |
103.8 |
106.0 |
111.4 |
115.4 |
118.2 |
115.7 |
113.7 |
|
|
57.2 |
52.4 |
57.6 |
64.5 |
67.7 |
79.5 |
83.6 |
84.6 |
|
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
|
|
51.0 |
50.0 |
49.0 |
46.0 |
46.0 |
45.0 |
45.0 |
45.0 |
|
4.4 |
5.0 |
4.1 |
4.8 |
2.4 |
4.1 |
3.6 |
2.8 |
6.5 |
|
1.1 |
1.2 |
1.4 |
1.5 |
1.7 |
1.9 |
2.0 |
2.2 |
2.3 |
|
55.0 |
55.0 |
55.0 |
55.0 |
56.0 |
56.0 |
56.0 |
57.0 |
57.0 |
|
|
0.28 |
0.27 |
0.27 |
0.27 |
0.27 |
0.27 |
0.26 |
0.27 |
|
|
22.6 |
22.9 |
22.0 |
21.5 |
20.8 |
19.6 |
19.4 |
19.0 |
|
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
|
|
|
18.0 |
17.2 |
17.0 |
17.3 |
17.6 |
19.6 |
16.8 |
|
|
3.0 |
4.3 |
4.1 |
3.1 |
5.0 |
3.4 |
4.5 |
4.3 |
|
|
|
58.0 |
59.0 |
59.0 |
57.0 |
58.0 |
58.0 |
58.0 |
|
|
12.0 |
12.8 |
10.8 |
13.4 |
12.6 |
13.7 |
14.4 |
14.0 |
|
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
|
77.9 |
80.1 |
84.2 |
87.5 |
81.5 |
81.3 |
82.6 |
84.7 |
85.4 |
|
86.4 |
88.7 |
88.7 |
85.7 |
86.7 |
85.6 |
85.8 |
85.8 |
84.9 |
|
59.1 |
58.4 |
61.5 |
59.3 |
60.6 |
63.0 |
64.4 |
62.9 |
64.8 |
|
74.5 |
74.4 |
74.6 |
75.3 |
77.1 |
78.1 |
79.2 |
79.8 |
80.4 |
|
3854 |
3892 |
3962 |
4273 |
4592 |
4899 |
5196 |
5452 |
5731 |
|
788 |
771 |
796 |
827 |
855 |
899 |
933 |
957 |
980 |
|
|
25.8 |
25.2 |
24.7 |
24.0 |
23.1 |
22.3 |
|
|
|
|
34.3 |
33.1 |
33.8 |
32.0 |
30.3 |
28.2 |
|
|
|
|
52.2 |
51.3 |
50.7 |
48.1 |
47.1 |
44.6 |
|
|
|
42.1 |
43.6 |
46.0 |
48.0 |
50.0 |
51.7 |
53.1 |
54.5 |
56.2 |
|
2774 |
2949 |
3276 |
3639 |
3910 |
4026 |
4155 |
4316 |
4524 |
|
11.4 |
11.2 |
11.7 |
12.6 |
13.3 |
13.3 |
13.2 |
13.1 |
13.1 |
|
SOURCE: Data from Statistics Netherlands (see http://statline.cbs.nl/statweb/ [accessed June 2010]). |
||||||||
slow growth in the 1980s and 1990s, and rapid growth again in the first years of the new millennium. The growth of health care expenditure (in constant prices, i.e., adjusted for inflation and compared to the year before) was exceptionally high in 2001, 2002, and 2003. It was 3.1 percent in 1999, 3.6 percent in 2000, 5.4 percent in 2001, 4.4 percent in 2002, 4.3 percent in 2003, 3.2 percent in 2004, 2.9 percent in 2005, 2.6 percent in 2006, and 3.1 percent in 2007. A similar acceleration in 2001 and subsequent years was seen for health care expenditure per capita (see Table 13-1).
Detailed studies of health care expenditure by age and health care sector have been performed for 1999, 2003, and 2007 (see Figure 13-5). Between 1999 and 2003 health care expenditure per head of population (in nominal prices) rose by more than 40 percent. In relative terms, the increase was shared among all age groups, including the old and very old, and benefited most health care sectors, including hospital care and care for the elderly. For men above age 85, health care expenditure rose from €17,128 per person per year in 1999 to €23,331 per person per year in 2003, representing a rise of 36 percent, or more than €6000. The corresponding figures for women above age 85 were €21,638 and €30,446, representing a rise of 41 percent, or almost €9000 per person per year.
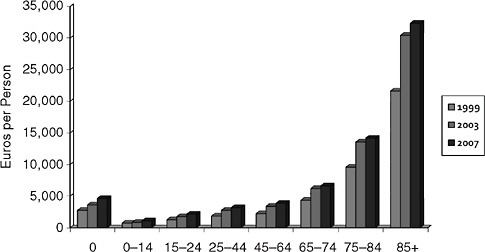
FIGURE 13-5 Health care expenditure by age, women, the Netherlands, nominal prices in Euros per person, 1999-2007.
SOURCE: L.C.J. Slobbe (personal communication, National Institute for Public Health and the Environment, 2009). Data collected and analyzed by the National Institute for Public Health and the Environment.
DISCUSSION
The reversal from stagnation to renewed decline of old-age mortality in the Netherlands shows some very distinct patterns. It was abrupt and shared by a wide range of age groups (particularly among women), suggesting that the causal factor or factors acted immediately rather than with a long delay, and pointing at a period rather than a cohort effect.
The pattern of cause-of-death contributions to this renewed decline is also rather striking. While the stagnation of old-age mortality during the 1980s and 1990s was partly due to smoking-related causes, the decline of old-age mortality after 2002 is not. Striking accelerations or even reversals of mortality trends are seen for causes like stroke, pneumonia, dementia, and symptoms and ill-defined conditions.
Of the four categories of determinants that we reviewed, health care factors seems the best candidate to explain the reversal of mortality trends among the elderly. There have been no sudden changes in health status among the elderly, in their physical or social environment or in their lifestyles that could explain this reversal. Most of these factors have been stable, and some have even deteriorated. When they have changed for the better, as in the case of fine dust air pollution, the cause-of-death pattern of mortality decline does not suggest a causal connection.
By contrast, health care for the elderly, particularly in the hospital sector, has grown rapidly. The timing of these changes roughly corresponds to the timing of the renewal of mortality decline. Substantial and sustained mortality decline started in 2003, and if one assumes a certain delay between improved treatment and reduced death rates, the improvements in treatment should have started slightly earlier. This may indeed have been the case: the most rapid increases in health care expenditure occurred in 2001, 2002, and 2003, and the most rapid increases in hospitalization rates occurred in 2002, 2003, and 2004.
That a more liberal administration to elderly patients of life-saving treatments in hospital has played a role in mortality decline is consistent with the decline in 1-year case fatality that we have observed, although this should be interpreted with care because of the possibility that the increase in admission rates has brought milder cases of disease into the hospital after 2001. Some real declines in case fatality must have occurred as well, because case fatality for coronary heart disease among the elderly has declined along with a decline in the clinical incidence of myocardial infarction (see Table 13-1). In the case of stroke, a plausible explanation for the acceleration of mortality decline and the decline of the 1-year case fatality rate is more rapid and more aggressive treatment for stroke in specialized stroke units, which were implemented on a large scale from about 2000 onward (van Exel et al., 2005).
In the case of pneumonia, dementia, and symptoms and ill-defined
conditions, too, a more active approach toward the treatment of seriously ill elderly patients may have played a role in mortality decline. Changes in mortality from these conditions are often regarded as indicative of “artifacts” of certification or coding, but if the rules have not changed, systematic changes as observed here must have a deeper explanation. Both pneumonia and dementia are often considered to be problematic “underlying” causes of death. Among elderly patients with one or more serious chronic diseases, pneumonia will often act as the direct cause of death, but should not be certified as the underlying cause. If the death is certified as being caused by pneumonia, then this can be interpreted as a decision by the physician not to search for a better diagnosis, or if a better diagnosis is available not to treat the patient for this disease, but to let him or her die from what has been called the “old man’s friend.” Among elderly patients, deaths from pneumonia can therefore often be seen as the outcome of a conscious or unconscious nontreatment decision. The same applies to dementia, which as long as its complications are adequately treated will in itself not lead to death. If a death is being certified as caused by dementia, the physician actually acknowledges that he or she has decided that further treatment is ineffective. For this very reason, dementia has long not been accepted as a possible underlying cause of death (Van der Meulen and Keij-Deerenberg, 2003).
A more active approach toward the treatment of seriously ill elderly patients is also suggested by the decreasing proportion of deaths in which treatment was withheld or withdrawn. In the Netherlands, data on the frequency of end-of-life practices were collected in four surveys in 1990, 1995, 2001, and 2005. The overall frequency of end-of-life decisions rose from 39 to 43 percent during the first half of the 1990s and remained stable thereafter. The frequency of specific end-of-life practices, however, showed some important changes coinciding with the reversal of old-age mortality trends. From 2001 to 2005 the frequency of euthanasia, assisted suicide, and withholding or withdrawing life-prolonging treatment declined, while the frequency of intensified alleviation of symptoms increased (Van der Heide et al., 2007).
The sudden rise in health care expenditure after 2001, which seems to have facilitated the increase in health care for the elderly, was due to a conscious decision by the Dutch government to relax the budgetary restraints of the 1980s and 1990s. During these two decades, the Dutch government had successfully limited the growth of health care expenditure, first by a strict regulation of supply (hospital beds, expensive equipment, specialized personnel, etc.), then by imposing budget constraints for in-patient care. As a result, the proportion of gross domestic product spent on health care in the Netherlands rose less than in other high-income countries. By 2001 public dissatisfaction with waiting lists and other problems of access to the
health care system had become so massive that the government decided to remove budgetary restraints. In the plan “Zorg verzekerd”—“Care insured (or ensured)”—the government promised that all necessary treatments would be eligible for reimbursement (Actieplan Zorg Verzekerd, 2000). As a result, health care costs exploded, until new but less tight restrictions were reimposed around 2004.
As is often the case with trends in aggregate population health, it is difficult to produce direct evidence on cause-effect relationships. The evidence presented here for a role of health care utilization in the reversal of old-age mortality trends in the Netherlands is only circumstantial. It is partly by exclusion that we have arrived at health care factors as the most plausible candidate, and it is mainly on the basis of consistency of most of the descriptive findings with this interpretation that we feel confident in proposing this as a hypothesis—but it is currently not much more than that.
Sometimes international comparisons can help to test such hypotheses, but in this case these will not bring us very far. There are only three countries with similar histories of stagnation of old-age mortality decline, Denmark, the Netherlands, and the United States. While stagnation started around the same time in these three countries, suggesting similar explanations, the reversal from stagnation to progress differs strongly in timing. Denmark’s renewed decline already started in 1995, and in the United States it has not yet started at all. On one hand, for Denmark, improvements in lifestyle as well as in medical and surgical treatment have been suggested as explanations (Chapter 14, in this volume), which is partly similar to what we have proposed. On the other hand, the United States has a much higher level of health care expenditure than Denmark and the Netherlands, which reduces the likelihood that a reversal of life expectancy trends there can be expected to occur when health care expenditure would rise even further.
In conclusion, although important questions remain, the most plausible hypothesis for explaining the sudden reversal of old-age mortality trends in the Netherlands is more health care for the elderly, facilitated by a sudden relaxation of budgetary restraints.
ACKNOWLEDGMENTS
Lany Slobbe of the National Institute for Public Health and the Environment provided the data in Figure 13-5. Agnes de Bruin helped with collecting data for Table 13-1. Agnes van der Heide provided useful comments on the trend in end-of-life practices in the Netherlands.
REFERENCES
Actieplan Zorg Verzekerd. (2000, November). The Hague: Ministerie van Volksgezondheid, Welzijn en Sport. Available: http://www.minvws.nl/artikelen/staf/actieplan_zorg_verzekerd.asp [accessed June 2010].
Garssen, J., and van der Meulen, A. (2007). Overlijdensrisico’s naar herkomstgroep: Daling en afnemende verschillen. Bevolkingstrends, 55(4), 56-72.
Janssen, F., Nusselder, W.J., Looman, C.W.N., Mackenbach, J.P., and Kunst, A.E. (2003). Stagnation in mortality decline among elders in the Netherlands. Gerontologist, 43, 722-734.
Janssen, F., Mackenbach, J.P., and Kunst, A.E. (2004). Trends in old-age mortality in seven European countries, 1950-1999. Journal of Clinical Epidemiology, 57, 203-216.
Juel, K., Bjerregaard, P., and Madsen, M. (2000). Mortality and life expectancy in Denmark and other European countries. What is happening to middle-aged Danes? European Journal of Public Health, 10, 93-100.
Löfmark, R., Nilston, T., Cartwright, C., Fischer, S., van der Heide, A., Mortier, F., et al. (2008). Physicians’ experiences with end-of-life decision-making: Survey in 6 European countries and Australia. BMC Medicine, 6, 4.
Meslé, F., and Vallin, J. (2006). Diverging trends in female old-age mortality: The United States and the Netherlands versus France and Japan. Population and Development Review, 31, 123-145.
Nusselder, W.J., and Mackenbach, J.P. (1996). Rectangularization of the survival curve in the Netherlands, 1950-1992. Gerontologist, 36, 773-782.
Nusselder, W.J., and Mackenbach, J.P. (1997). Rectangularization of the survival curve in the Netherlands: An analysis of underlying causes of death. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 52, S145-S154.
Nusselder, W.J., and Mackenbach, J.P. (2000). Lack of improvement of life expectancy at advanced ages in the Netherlands. International Journal of Epidemiology, 29, 140-148.
Polder, J.J. (2009). De zorguitgaven als januskop. Trends in getallen en gezichtspunten. In J.P. Mackenbach (Ed.), Trends in Volksgezondheid en Gezondheidszorg. Maarssen, Netherlands: Elsevier.
Slobbe, L.C.J., Kommer, G.J., Smit, J.M., Groen, J., Meerding, W.J., and Polder, J.J. (2006). Kosten van Ziekten in Nederland 2003 [Costs of Illnesses in The Netherlands 2003]. Bilthoven, Netherlands: National Institute for Public Health and the Environment [in Dutch].
Stivoro. (2009). Feiten en Cijfers [Facts and figures]. Available: http://www.stivoro.nl/Voor_professionals/Feiten___Cijfers.aspx?mId=9929&rId=77 [accessed June 2010].
Van der Heide, A., Onwuteaka-Philipsen, B., Rurup, M.L., Buiting, H.M., van Delden, J.J.M., Hanssen-de Wolff, J.E., et al. (2007). End-of-life practices in the Netherlands under the Euthanasia Act. New England Journal of Medicine, 356, 1957-1965.
Van der Meulen, A., and Keij-Deerenberg, I. (2003). Sterfte aan dementie. Bevolkingstrends, 51(3), 24-28.
Van Exel, N.J.A., Koopmanschap, M.A., Scholte op Reimer, W., Niessen, L.W., and Huijsman, R. (2005). Cost-effectiveness of integrated stroke services. Quarterly Journal of Medicine, 98(6), 415-425.