3
Are International Differences in Health Similar to International Differences in Life Expectancy?
Eileen M. Crimmins, Krista Garcia, and Jung Ki Kim
The question addressed in this chapter is whether people in countries with relatively low life expectancy after age 50 have worse health than those in countries with longer life expectancy. We begin with a short discussion of the theoretical relationships between mortality and population health and the potential complexity of the link between measures of health and mortality. We then examine how indicators of health vary across countries and how closely differences in a set of health indicators correspond to differences in mortality across 10 countries. We note at the outset that most of the data we examine reflect analysis of cross-sectional differences in health; without comparable longitudinal data, there is little we can say about how the differences arose. The countries compared include Australia, Canada, Denmark, England, France, Italy, Japan, the Netherlands, Spain, and the United States.
MEASURES OF POPULATION HEALTH
A number of people have addressed the question of whether populations that live longer are or should be “healthier.” Answers range from yes, because there is a “compression of morbidity” (Fries, 1980), to no, as there is a “failure of success” (Gruenberg, 1977), to no change, as there is dynamic equilibrium (Manton, 1982). It was probably true that improved health and increased life expectancy went together in the past, when mortality was highly related to death from infectious disease. It is not necessarily true when mortality is largely the result of chronic conditions that exist over long periods of the life span and are treated but not cured. Successful treat-
ment can leave more people with a condition surviving in the population. If more people survive with more health problems, it becomes difficult to know when one country is “healthier” than another.
At the moment, most of the data available for cross-national comparisons indicate the prevalence of health problems in the population. The prevalence of a health problem at a given time depends on how many people have experienced the onset of the problem or condition and how long they survived with the problem. The onset rate or incidence of a problem depends on risk for the condition in the exposed population, whereas the survival rate can depend on whether the case is treatable and, if treated, whether death or the progression of severity of disease is delayed. Populations can be in better health because the incidence of a disease is lower, but they could also have a lower prevalence of poor health if those with diseases did not survive as long. For instance, if life expectancy among the diseased and disabled increases, population health as measured by disability could deteriorate. Two countries with the same level of disease incidence but different approaches to treatment could have differences in population health; where disease is aggressively treated and death prevented, the level of disease prevalence as well as life expectancy could be higher. So the health status of a population depends on a set of processes of onset and survival that cannot be inferred from one or more snapshots of the prevalence of health problems in the population.
There can also be variation in the presence of diseases and conditions across countries and across time for a number of reasons. Diagnostic definitions can differ across countries and change over time. For instance, the blood pressure cutoff value indicating hypertension has gotten lower over time, so that diagnosis occurs at an earlier stage of severity in more recent years. Countries may adopt changes in definitions at different times, leading to variability of the definition of conditions at one time. Another example is differences in the diagnostic criteria for diabetes (DECODE Study Group, 1998; Wareham and O’Rahilly, 1998). Differences in national emphasis on screening for conditions can also affect variability in knowledge of the existence of diseases and reported prevalence. This is true for cancer, hypertension, high cholesterol, and diabetes (Ashworth, Medina, and Morgan, 2008; Gregg et al., 2004; Wareham and O’Rahilly, 1998). It is also possible that recognition of disease varies over time and across countries. For instance, Alzheimer’s disease (AD) is now a recognized cause of both morbidity and mortality but was virtually unknown and unrecognized in the 1950s. The timing of accepting AD as a cause of mortality and morbidity can differ across countries. It is also possible that there are national or cultural differences in the way doctors disclose conditions to patients (Asai, 1995).
There are multiple dimensions of health to be considered in evaluating national differences in health. Health change with age in populations begins
with the onset of risk factors, progresses to diseases and impairments, and then to functioning loss and to the inability to perform expected tasks or disability, frailty, and death (Crimmins, Kim, and Vasunilashorn, 2010). This can be termed the “morbidity process.” No one individual needs to experience problems reflecting all of these dimensions, as some people die very suddenly with no warning that their health has begun to deteriorate. In addition, for individuals the process is not always unidirectional, but back and forth movement is possible (Crimmins, Hayward, and Saito, 1994). These dimensions of population health relate to mortality differently. For instance, many important causes of disability are not highly related to mortality, for instance, arthritis. In contrast, cancer is highly related to mortality but not disability. Heart disease tends to be a major cause of both mortality and disability. In this analysis, we examine self-reported indicators of functioning, disability, and disease presence and cancer incidence from registries. We also examine both self-reports and measured prevalence of high cholesterol and high blood pressure, along with body mass index based primarily on self-reports.
DATA
Where possible, our analysis uses information on health for the population ages 50 and older, or 65 and older, in the 10 countries. However, in some cases, we expand or limit the age range because of data unavailability. Most of the countries have conducted national surveys of their older populations, which provide individual-level data on a number of health indicators, risk factors, and drug usage. Many of the self-reported indicators of health status come from a family of surveys designed to be comparable: (1) the Health and Retirement Study (HRS) for 2004 for the United States (Health and Retirement Study, 2006); (2) the Surveys of Health, Ageing and Retirement in Europe (SHARE) for 2004 for Denmark, France, Italy, the Netherlands, and Spain (Börsh-Supan and Jurges, 2005; Börsch-Supan et al., 2005); and (3) the English Longitudinal Study of Ageing (ELSA) for England collected in 2002 (Marmot et al., 2007). Sometimes we employ information for England and Wales or the United Kingdom when we use other sources. All of these surveys use similar formats for their questionnaires and survey national samples of people ages 50+. The Nihon University Japanese Longitudinal Study on Aging (Nihon University Japanese Longitudinal Study on Aging, 2009) provides a representative sample of those ages 65+ for Japan, with most of the data used in this analysis from the 2003 wave. For Canada, much of the self-reported information comes from the 2003 Canadian Community Health Survey (CCHS), and for Australia, the source is often the National Health Survey 2004-2005.
Our comparison of national cancer rates is not based on self-reports from surveys but is taken from the GLOBOCAN 2002 database from the
Descriptive Epidemiology Group of the International Agency for Research on Cancer (IARC), part of the World Health Organization (WHO). Cancer registries reflecting national populations or samples from selected regions of countries are the basis for these data (Ferlay et al., 2004).
Our data on measured biological risk draw on resources from the WHO Global Infobase (World Health Organization, 2009), Organisation for Economic Co-operation and Development (OECD) (2008), the U.S. National Health and Nutrition Examination Survey (NHANES) (2001-2006), ELSA (2004) for England, and the Japanese Health and Nutrition Survey Report (2004) (Ministry of Health, Labour and Welfare of Japan, 2006). For Australia, data came from a report based on the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) conducted in 1999-2000 (Dunstan et al., 2001). We link our health measures to estimates of life expectancy at age 50 and differences in life expectancy relative to those in the United States due to specified causes from Glei, Meslé, and Vallin (Chapter 2, in this volume) and to life expectancy at ages 50 and 65 in 2004 from the Human Mortality Database.
After examining country differences in the prevalence of health conditions and risk factors, we use the microdata in a pooled equation for surveys designed to be comparable to examine country differences among individuals in health outcomes with controls for age, diseases, and health behaviors.
CROSS-NATIONAL DIFFERENCES IN POPULATION HEALTH
We begin our examination of health differences at the end of the morbidity process with indicators of loss of functioning and disability. We then examine diseases that are important causes of mortality. Finally, we turn to selected risk factors and bioindicators related to the diseases we have examined.
Disability and Functioning Loss
Many studies of health trends in older populations have focused on trends in disability and functioning loss. Trends in the United States have shown that there has been some improvement in functioning and reduction in disability over the past 25 years (Freedman et al., 2004). The improvement in less severe disability began earlier, and improvement in the most severe category of disability began later and has probably been the smallest. It should be noted that some recent studies have found that improvement in disability may no longer be occurring among the U.S. young-old population (Seeman et al., 2010). Time trends in disability have varied in the other countries we are comparing to the United States (Aijanseppa et al.,
2005). A study comparing trends in severe disability in 12 OECD countries for people ages 65+ (Lafortune, Balestat, and the Disability Study Expert Group Members, 2007) found clear evidence of a decline in disability in Denmark, Italy, the Netherlands, and the United States; an increase in disability in Japan; and no clear direction of change in France or the United Kingdom. Not all studies of trends agree; Schoeni et al. (2006) find some recent improvement in disability in Japan.
We examine two indicators of problems with functioning and disability self-reported in surveys collected in the first half of the decade: (1) having difficulty performing at least 1 of 10 functioning tasks known as Nagi functions and (2) having difficulty performing at least 1 of 6 activities of daily living (ADLs). Difficulties with functioning problems should reflect problems with strength, balance, mobility, and dexterity, and they are an indicator of less severe functioning loss. ADL difficulty reflects difficulty in performing tasks related to self-maintenance and more severe disability. Although some measures of disability can be influenced by the challenge of the environment, as well as the intrinsic health of the person, these measures should primarily reflect perceptions of intrinsic ability.
An examination of the prevalence of functioning problems in the 50+ populations across countries in the early 2000s indicates that people in the United States report more functioning problems than any of the other countries (see Table 3-1). People in Denmark and the Netherlands report the fewest functioning problems. For men, the prevalence of functioning problems in these two countries is about half of the U.S. level; for women, it is about two-thirds of the U.S. level. When the sample is limited to persons ages 65+, the differences between the United States and other countries are not as great. From this, one can infer that U.S. functioning ability is worse relative to that in other countries in the 50-64 range than at older ages. Among women ages 65+, levels of functioning problems in France, Italy, England, and Spain are close to those among U.S. women; U.S. men exceed men in all countries in functioning problems. The country with the lowest level of reported functioning problems at ages 65+ is Japan, for which data were not available in the 50-64 age range. Among the older age group, Denmark and the Netherlands have relatively good functioning.
Americans age 50 and over report more ADL difficulty than anyone except the British. In the older age range, ADL difficulties are fairly similar among Denmark, France, Italy, Spain, and the United States. Again, ADL functioning problems are greater among the English. Only in Japan and the Netherlands is the level of ADL disability notably lower. Differences between the United States and other countries in ADL difficulties also appear to be greater in the younger part of the age range than after age 65.
TABLE 3-1 Functioning Difficulty, Difficulty with Activities of Daily Living (ADLs), and Ratios to U.S. Level, by Gender and Country
The relationship between national level of life expectancy at age 50 or 65 and the percentage of the population with functioning problems or ADL disability is not very strong. An example of the relationship between national levels of ADL disability and life expectancy at age 65 is shown in Figure 3-1, which displays a statistically insignificant relationship between lower life expectancy and worse ADL functioning.
Differences in Disease Prevalence
We examine cross-national differences in self-reports of three diseases from national surveys: heart disease, stroke, and diabetes (see Table 3-2). Heart disease accounts for more than half of the female gap in life expectancy at age 50 between the United States and nine other countries studied here (0.8 years out of 1.4) and the difference in the gap in life expectancy due to heart disease is greater than the overall male gap (0.8 out of 0.6) (Chapter 2, in this volume, see Table 2A-8). We also examine differences in stroke prevalence, as the U.S. ranking for cerebrovascular death rates relative to other countries has fallen recently, although Americans still have lower death rates than in the average of the nine countries (Chapter 2, in this volume, Table 2A-8). Diabetes deaths contribute to lower life expectancy in the United States compared with the average of the other nine countries of 0.1 year for both men and women at age 50 (Chapter 2, in this volume, see Table 2A-8).
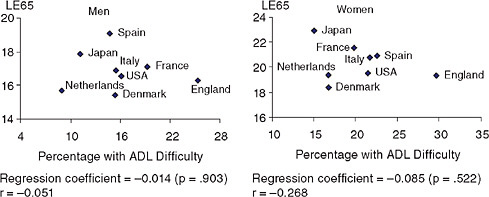
FIGURE 3-1 National percentage of activities of daily living (ADL) difficulty at ages 65+ and life expectancy at age 65 (LE65).
SOURCES: Data on ADL difficulty from Table 3-1; data on life expectancy for 2004 from the Human Mortality Database (see http://www.mortality.org [accessed March 2009]). Life expectancy data extracted from country-specific life tables from the HMD.
TABLE 3-2 Prevalence of Self-Reported Disease in the 50+ and 65+ Populations
|
Country |
Ages 50+ |
Ages 65+ |
||||||
|
Men |
Women |
Men |
Women |
|||||
|
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
|
|
(a) Heart Disease |
|
|
|
|
|
|
|
|
|
United States |
28.4 |
1.00 |
22.1 |
1.00 |
36.4 |
1.00 |
28.0 |
1.00 |
|
Denmark |
9.9 |
0.35 |
7.8 |
0.35 |
15.9 |
0.44 |
13.0 |
0.46 |
|
France |
18.5 |
0.65 |
10.8 |
0.49 |
28.8 |
0.79 |
16.3 |
0.58 |
|
Italy |
12.4 |
0.44 |
10.1 |
0.46 |
18.7 |
0.51 |
14.3 |
0.51 |
|
Netherlands |
13.6 |
0.48 |
8.8 |
0.40 |
21.7 |
0.60 |
12.9 |
0.46 |
|
Spain |
11.3 |
0.40 |
11 |
0.50 |
15.1 |
0.41 |
15.5 |
0.55 |
|
England |
23.0 |
0.81 |
19.0 |
0.86 |
32.2 |
0.88 |
26.4 |
0.94 |
|
Japan |
NA |
NA |
NA |
NA |
14.4 |
0.40 |
12.2 |
0.44 |
|
Canada |
13.8 |
0.49 |
10.7 |
0.48 |
21.8 |
0.60 |
18.1 |
0.65 |
|
(b) Stroke |
|
|
|
|
|
|
|
|
|
United States |
7.3 |
1.00 |
6.4 |
1.00 |
9.4 |
1.00 |
8.6 |
1.00 |
|
Denmark |
6.0 |
0.82 |
4.9 |
0.77 |
9.9 |
1.05 |
7.3 |
0.85 |
|
France |
3.5 |
0.48 |
3.8 |
0.59 |
5.5 |
0.59 |
5.8 |
0.67 |
|
Italy |
3.7 |
0.51 |
2.7 |
0.42 |
5.8 |
0.62 |
4.0 |
0.47 |
|
Netherlands |
4.4 |
0.60 |
4.8 |
0.75 |
7.1 |
0.76 |
7.8 |
0.91 |
|
Spain |
2.4 |
0.33 |
1.9 |
0.30 |
2.9 |
0.31 |
2.8 |
0.33 |
|
England |
4.9 |
0.67 |
4.0 |
0.63 |
8.2 |
0.87 |
6.4 |
0.74 |
|
Japan |
NA |
NA |
NA |
NA |
9.3 |
0.99 |
6.0 |
0.70 |
|
Canada |
2.8 |
0.38 |
2.4 |
0.38 |
5.2 |
0.55 |
3.9 |
0.45 |
|
(c) Diabetes |
|
|
|
|
|
|
|
|
|
United States |
19.5 |
1.00 |
16.5 |
1.00 |
21.4 |
1.00 |
17.6 |
1.00 |
|
Denmark |
8.2 |
0.42 |
6.8 |
0.41 |
11.1 |
0.52 |
8.7 |
0.49 |
|
France |
10.9 |
0.56 |
8.6 |
0.52 |
13.0 |
0.61 |
10.8 |
0.61 |
|
Italy |
12.8 |
0.66 |
11.4 |
0.69 |
17.6 |
0.82 |
15.7 |
0.89 |
|
Netherlands |
7.8 |
0.40 |
9.2 |
0.56 |
10.6 |
0.50 |
12.2 |
0.69 |
|
Spain |
15.3 |
0.78 |
13.9 |
0.84 |
20.4 |
0.95 |
17.1 |
0.97 |
|
England |
8.6 |
0.44 |
6.2 |
0.38 |
11.2 |
0.52 |
8.0 |
0.45 |
|
Japan |
NA |
NA |
NA |
NA |
10.1 |
0.47 |
7.5 |
0.43 |
|
Canada |
11.9 |
0.61 |
9.1 |
0.55 |
15.6 |
0.73 |
11.9 |
0.68 |
|
Australia |
|
|
|
|
16.2 |
0.76 |
11.5 |
0.65 |
|
NOTE: ADL = activities of daily living. NA = not available. SOURCE: Data on self-reported diseases from HRS (2004) for the United States; from ELSA (2002) for England; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; for NUJLSOA (2003) for Japan; from CCHS (2003) for Canada; and from the Australian Bureau of Statistics (2006a) [http://www.abs.gov.au/ausstats, accessed December 5, 2009] and NHS (2004-2005) for Australia. |
||||||||
Heart Disease
Americans ages 65+ report more heart disease than persons in any of the other countries. The prevalence is only slightly lower in England than in the United States. Denmark and Japan have prevalence values of only about half of the U.S. values (see Table 3-2[a]).1 Each country’s age-sex group ratio to the U.S. value is higher among the 50+ population than among the 65+ population, indicating larger differences at younger ages. National heart disease prevalence is not closely related to national life expectancy (see Figure 3-2[a]).
A number of studies in the United States have reported increases over time in the prevalence of heart disease in the population (Crimmins and Saito, 2001; Cutler and Richardson, 1997), although a recent study reports that this increase may have ended after 1997 (Freedman et al., 2007). An increase in the proportion of the population with heart disease is perhaps not surprising in light of the fact that declining death rates from heart disease have been such a strong contributor to mortality trends (Jemal et al., 2005). Even in the short period from 2000 to 2006, U.S. cases of atrial fibrillation increased by 30 percent and heart failure cases increased by 8 percent among Medicare beneficiaries (Chronic Condition Data Warehouse, 2009).2
Stroke
At ages 50+, Americans report the highest prevalence of stroke. For women, the Netherlands and Denmark have prevalences that are about three-fourths of the U.S. level. For the 65+ population, the prevalence of self-reported stroke is highest among Danish men. U.S. and Japanese men have levels very similar to those of the Danes, followed closely by English men (see Table 3-2[b]).3 This high level of stroke among Japanese men is not surprising, as high levels of stroke with low levels of heart disease have long characterized the Japanese (Reed, 1990). For women, the highest levels
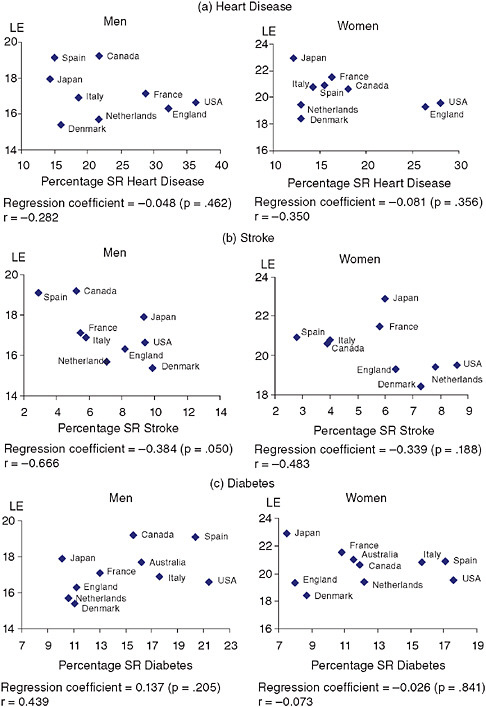
FIGURE 3-2 National percentage self-reporting (SR) disease (65+) and life expectancy (LE) at age 65.
SOURCES: Data on disease from Table 3-2; data on life expectancy for 2004 from the Human Mortality Database (HMD) (see http://www.mortality.org [accessed March 2, 2009]). Life-expectancy data extracted from country-specific life tables from HMD.
of stroke are reported among Americans; Japanese women have lower levels of stroke than Americans, Danes, the Dutch, and the English. This finding that Japanese women now have a lower prevalence of stroke than Americans fits with the observation that, in recent years, mortality related to stroke among Japanese women has been lower than that for U.S. women (Crimmins et al., 2008).
National levels of mortality and stroke prevalence have a stronger association than that observed for heart disease. For women, it is the countries with adverse mortality trends—Denmark, the Netherlands, and the United States—that have relatively high levels of female stroke prevalence (see Figure 3-2[b]).
Diabetes
For those ages 50 and older, diabetes prevalence is reported to be the highest in the United States. For men, only Italy, France, and Spain have levels that exceed half of the U.S. value. Among women, Denmark and England have levels of diabetes only about 40 percent of that in the United States. At ages 65+, the United States has the highest level, followed closely by that of Spain and Italy (see Table 3-2[c]). In Denmark, England, and Japan, self-reported diabetes prevalence at ages 65+ is only about half of that of the United States (Table 3-2[c]).4 Again, the differences between the United States and other countries appear to be greater in the younger part of the age range examined, as the ratios to the U.S. values are higher at older ages in every case. The link between national levels of self-reported diabetes and mortality is not significant (see Figure 3-2[c]).
In sum, self-reports of disease presence tend to place people in the United States in the high-prevalence group for each of these diseases. Although other countries tend to be high in only one of the three diseases, the United States tends to have high levels in all three. The differences between the United States and other countries in the prevalence of all three diseases are greater among those ages 50-64 than over age 65.
Figure 3-3 shows the level of the three diseases self-reported in each country as related to country-level life expectancy differences from U.S. life expectancy due to heart disease (for heart disease), cerebrovascular disease (for stroke), and diabetes (for diabetes) from Glei, Meslé, and Vallin. (Chapter 2, in this volume). Neither heart disease nor stroke is significantly
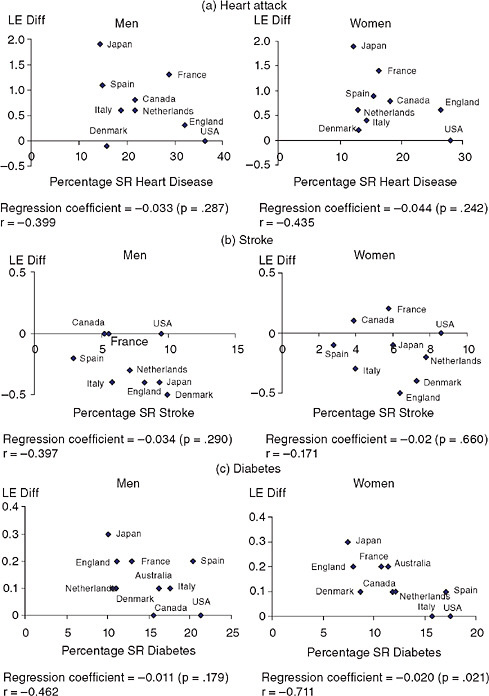
FIGURE 3-3 National percentage self-reporting (SR) disease (65+) and difference from U.S. life expectancy (LE) at age 50 from heart disease, stroke, and diabetes. SOURCES: Data on disease from Table 3-2; data on life expectancy from Glei et al. (Chapter 2, in this volume, Table 2A-8). Life-expectancy data extracted from country-specific life tables from HMD.
related to the national life expectancy differentials, but the level of diabetes and life expectancy lost due to diabetes are significantly related for women, indicating some link between the level of disease and differences in life expectancy.
Cancer
Overall, cancer death rates for men in the United States are shown to be lower than those for the other countries we are considering (contribution to the life expectancy gap between the United States and the other nine countries is −0.4 years); however, for women, lung cancer is a cause of lower life expectancy in the United States (contribution to the gap of lung cancer is 0.3) (Chapter 2, in this volume). We examine differences in incidence of all cancers except nonmelanoma skin cancer but also for four specific cancers: prostate cancer for men, breast cancer for women, lung cancer, and colorectal cancer. The recorded incidence or onset rate of prostate, breast, and colorectal cancers will be affected by policies toward screening, which vary markedly across countries (Banta and Oortwiin, 2001; Hakama et al., 2008; Preston and Ho, Chapter 9, in this volume; Quinn, 2003). Countries with intensive screening are likely to find more cancers. This will include early cancers and cancers that might never produce any symptoms or lead to death. Identifying and treating cancers early should reduce mortality. We also examine mortality rates from cancer to assess incidence relative to mortality (see Figure 3-4).
The United States has the highest recorded incidence of all cancers for both men and women. However, all-cancer mortality rates are moderate for men in the United States; national all-cancer mortality rates for U.S. women could be characterized as among the higher but not the highest levels. The incidence of both prostate and breast cancers are highest in the United States. Mortality from these cancers is not particularly high in the United States. Prostate cancer mortality is higher in Denmark and the Netherlands; breast cancer mortality is higher in Denmark, the Netherlands, and the United Kingdom. Incidence and mortality from both of these cancers are particularly low in Japan.
For both men and women, lung cancer incidence is highest in the United States. Lung cancer mortality is highest among men in the Netherlands; among women, rates are highest among the Danes, and almost as high in the United States and Canada. The difference between the incidence rate and the mortality rate is greatest in the United States. The incidence of colorectal cancer is highest among Japanese men, and it is high among Australians of both genders. Colorectal cancer mortality rates vary little across countries, with the exception that Denmark appears to have higher mortality from colorectal cancer than other countries.
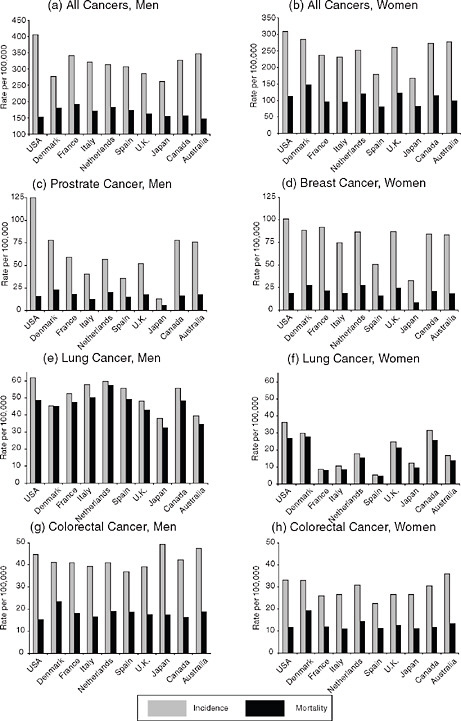
FIGURE 3-4 Age-standardized cancer incidence and mortality rates, 2002. All cancers excluding nonmelanoma skin cancer.
SOURCE: GLOBOCAN 2002 database (Ferlay et al., 2004; see http://www-dep.iarc.fr [accessed June 2010]). Data from summary tables created in online database.
The high incidence of breast and prostate cancers in the United States could reflect high levels of screening (Preston and Ho, Chapter 9, in this volume). This is not true for lung cancer. In contrast to the cardiovascular diseases and diabetes discussed above, the United States does not have particularly high mortality from cancer except for lung cancer for women.
Differences in Risk Factors
Recent research has reported higher levels of some biological risk factors among Americans compared with English and Japanese persons of the same age (Banks et al., 2006; Crimmins et al., 2008). We examine national differences in the prevalence of three indicators of physiological dysregulation that are risk factors for mortality, cardiovascular disease, and diabetes: high cholesterol, high blood pressure, and obesity. Each of these can be either self-reported or measured in populations; we report both types of data. In comparing countries, measured risk avoids some of the problems of self-report that could reflect cultural differences in knowledge about health; however, measured values are much less available. It is also true that measured levels of cholesterol and blood pressure are affected by the use of medications, which is rapidly changing in most countries, making it difficult to compare data collected in different years.
Cholesterol
First, we examine self-reports of having ever been told one has high cholesterol. Self-reported high cholesterol is very high in the United States, 2-3 times higher than in other countries examined (see Table 3-3). About half of the U.S. population ages 50+ reported being told they had high cholesterol (48.2 percent for men; 49.0 percent for women); values are similar at ages 65+ (49.3 percent for men and 42.7 percent for women).
Measured high cholesterol is available for older age groups for a smaller number of countries in the early 2000s. The prevalence of people with high measured cholesterol is low in the United States relative to that in other countries (see Table 3-3). Among those ages 50-64, the percentage with raised measured cholesterol is highest among persons in England. In this age group, U.S. women have the lowest levels of raised measured cholesterol; the percentage of U.S. men with measured high cholesterol is higher than that of the Japanese but lower than in all other countries. Among those ages 65+, Americans and Japanese have relatively low values compared with other countries.
National levels of measured high cholesterol are shown relative to levels of life expectancy in Figure 3-5. In this small group of countries, there is no statistical association between a country’s level of raised cholesterol and life expectancy in either the 50-64 or 65+ age group.
TABLE 3-3 Self-Reported Prevalence of High Cholesterol, Measured Level of High Cholesterol, and Ratios to U.S. Level
|
Country |
Men |
Women |
Men |
Women |
||||
|
% |
Ratio/U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
|
|
|
Self-Reported High Cholesterol |
|||||||
|
|
Ages 50+ |
Ages 65+ |
||||||
|
United States |
48.2 |
1.00 |
49.0 |
1.00 |
49.3 |
1.00 |
42.7 |
1.00 |
|
Denmark |
17.1 |
0.35 |
13.6 |
0.28 |
21.2 |
0.43 |
15.4 |
0.36 |
|
France |
23.7 |
0.49 |
22.5 |
0.46 |
23.7 |
0.48 |
26.3 |
0.62 |
|
Italy |
18.5 |
0.38 |
20.5 |
0.42 |
19.8 |
0.40 |
20.5 |
0.48 |
|
Netherlands |
16.3 |
0.34 |
13.4 |
0.27 |
15.3 |
0.31 |
14.9 |
0.35 |
|
Spain |
22.5 |
0.47 |
24.9 |
0.51 |
21.3 |
0.43 |
28.2 |
0.66 |
|
Australia |
23.8 |
0.49 |
21.6 |
0.44 |
16.3 |
0.33 |
16.6 |
0.89 |
|
|
Measured Prevalence of High Cholesterol (≥240mg/dL)a |
|||||||
|
|
Ages 50-64 |
Ages 65+ |
||||||
|
United States |
19.7 |
1.00 |
26.7 |
1.00 |
10.1 |
1.00 |
23.2 |
1.00 |
|
Netherlands |
23.8 |
1.21 |
28.3 |
1.06 |
15.5 |
1.53 |
32.2 |
1.39 |
|
Spain |
24.3 |
1.23 |
32.8 |
1.23 |
|
|
|
|
|
England |
38.7 |
1.96 |
51.2 |
1.92 |
24.2 |
2.40 |
48.0 |
2.07 |
|
Japan |
14.4 |
0.73 |
28.6 |
1.07 |
10.7 |
1.06 |
15.7 |
0.68 |
|
Canada |
27.8 |
1.41 |
28.6 |
1.07 |
25.0 |
2.48 |
44.0 |
1.90 |
|
aMany values estimated for age groups from the original data. The definition of measured high cholesterol in the Netherlands (≥250mg/dL); England ages 52-64; Canada ages 65-74. Data collection year for measured high cholesterol: United States (2001-2006), the Netherlands (2001), Spain-subnational (1992), England (2004), Japan (2004), and Canada (1990). SOURCE: Data on self-reported high cholesterol: from NHANES (2001-2006) for the United States; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; and from AIHW (2006) and NHS (2004-2005) for Australia. Data on measured high cholesterol: from NHANES (2001-2006) for the United States; from ELSA (2004) for England; from the Ministry of Health, Labour and Welfare of Japan (2006) and NHNS (2004) for Japan; and from the WHO Global InfoBase for the Netherlands, Spain, and Canada. |
||||||||
High cholesterol can be fairly effectively controlled by lipid-lowering drugs, so high national use of drugs will reduce the number of persons with high measured cholesterol. The high use of lipid-lowering drugs in the United States is the explanation for why ever having a diagnosis of high cholesterol is relatively high but the prevalence of measured high cholesterol is relatively low. While we do not have data for all of the countries, we have self-reports of the use of lipid-lowering drugs around the same time period in eight countries. The United States has the highest use of lipid-lowering drugs; only Canada and France come close to it in the level of drug use for high cholesterol (see Table 3-4). The United States has been recognized
![FIGURE 3-5 Measured high cholesterol (≥240mg/dL) and life expectancy (LE). SOURCES: Data on measured high cholesterol from Table 3-3; data on life expectancy for 2004 from the Human Mortality Database (see http://www.mortality.org [accessed March 2009]). Life-expectancy data extracted from country-specific life tables from HMD.](/openbook/12945/xhtml/images/p2001cc0eg84001.jpg)
FIGURE 3-5 Measured high cholesterol (≥240mg/dL) and life expectancy (LE). SOURCES: Data on measured high cholesterol from Table 3-3; data on life expectancy for 2004 from the Human Mortality Database (see http://www.mortality.org [accessed March 2009]). Life-expectancy data extracted from country-specific life tables from HMD.
as a country that aggressively treats with pharmaceuticals, but a number of European countries have markedly increased the use of lipid-lowering drugs in this decade. In only three years, from 2000 to 2003, the number of daily doses per person almost tripled in England, more than doubled in Italy, and increased by more than 50 percent in France and the Netherlands (Mantel-Teeuwisse et al., 2002; Walley et al., 2005). Usage also continues to increase in the United States (Crimmins et al., 2010).
TABLE 3-4 Percentage of the Population Taking Lipid-Lowering Drugs
|
Country |
Ages 50+ |
Ages 65+ |
||
|
Men |
Women |
Men |
Women |
|
|
United States |
26.8 |
24.1 |
33.1 |
31.3 |
|
Denmark |
12.9 |
9.4 |
19.9 |
11.3 |
|
France |
23.3 |
21.6 |
25.3 |
26.9 |
|
Italy |
12.2 |
12.9 |
14.9 |
14.3 |
|
Netherlands |
15.0 |
12.3 |
18.4 |
15.5 |
|
Spain |
15.4 |
16.1 |
16.5 |
19.6 |
|
Japan |
8.3 |
15.1 |
11.3 |
20.6 |
|
Canada |
24.5 |
20.3 |
30.7 |
28.9 |
|
Australia |
16.3 |
16.5 |
16.6 |
20.9 |
|
SOURCES: Data from NHANES (2001-2006) for United States; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; from Ministry of Health, Labour and Welfare of Japan (2006) and NHNS (2004) for Japan; from CCHS (2003) for Canada; and from Dunstan et al. (2001) and AusDiab (1999-2000) for Australia. |
||||
High Blood Pressure
The United States has been described in the past as having levels of measured blood pressure lower than a number of European countries (Wolf-Maier et al., 2003). Based on an analysis of people ages 35-64 and using data from the late 1990s and early 2000s, measured blood pressure was shown to be lower in the United States and Canada and higher in European countries including Italy, England, and Spain. The treatment of hypertension in the United States was also more prevalent, which led to the conclusion that hypertensive treatment was more aggressive there (Wang, Alexander, and Stafford, 2007).
We examine available data on more recent national differences in the prevalence of self-reports of having been told one has hypertension, measured hypertension, and measured hypertension or using antihypertensive medications in Table 3-5. On one hand, self-reports of having been diagnosed with hypertension from survey data are highest for Americans. For those ages 50+, the range across countries of the ratio of national levels to the U.S. level is .43 to .70. At age 65, the range is .48 to .79.
On the other hand, the United States has relatively low levels of measured hypertension. Only English and Australian women ages 50+ and English women ages 65+ have lower levels of measured hypertension than Americans. In France, ratios indicate levels 1.48 to 2.35 times higher than those of Americans. The Japanese also have higher levels of measured hypertension, particularly men.
Some countries report hypertension by combining measured high blood pressure with reported use of drugs to control hypertension. If we consider
TABLE 3-5 Prevalence of High Blood Pressure and Ratio to U.S. Level
|
Country |
Men |
Women |
Men |
Women |
||||
|
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
|
|
|
Self-Reported Hypertension |
|||||||
|
|
Ages 50+ |
Ages 65+ |
||||||
|
United States |
53.6 |
1.00 |
55.1 |
1.00 |
57.2 |
1.00 |
62.7 |
1.00 |
|
Denmark |
30.4 |
0.57 |
28.1 |
0.51 |
41.8 |
0.73 |
32.6 |
0.52 |
|
France |
25.5 |
0.48 |
31.7 |
0.58 |
31.4 |
0.55 |
39.3 |
0.63 |
|
Italy |
35.8 |
0.67 |
38.1 |
0.69 |
43.8 |
0.77 |
46.4 |
0.74 |
|
Netherlands |
22.8 |
0.43 |
27.8 |
0.50 |
27.4 |
0.48 |
32.7 |
0.52 |
|
Spain |
27.0 |
0.50 |
37.6 |
0.68 |
34.3 |
0.60 |
49.5 |
0.79 |
|
England |
36.0 |
0.67 |
38.7 |
0.70 |
41.7 |
0.73 |
47.0 |
0.75 |
|
Japan |
NA |
NA |
NA |
NA |
30.5 |
0.53 |
34.3 |
0.55 |
|
Canada |
29.5 |
0.55 |
35.2 |
0.64 |
37.3 |
0.65 |
47.1 |
0.75 |
|
Australia |
24.4 |
0.46 |
29.2 |
0.53 |
36.7 |
0.64 |
41.8 |
0.67 |
|
|
Measured High Blood Pressure (≥140/90mmHg) |
|||||||
|
|
Ages 50-64 |
Ages 65+ |
||||||
|
United States |
28.1 |
1.00 |
36.6 |
1.00 |
34.3 |
1.00 |
49.5 |
1.00 |
|
France |
60.6 |
2.16 |
65.2 |
1.78 |
80.5 |
2.35 |
73.1 |
1.48 |
|
England |
33.4 |
1.19 |
27.9 |
0.76 |
44.6 |
1.30 |
46.3 |
0.94 |
|
Japan |
52.5 |
1.87 |
41.2 |
1.13 |
66.7 |
1.94 |
62.7 |
1.27 |
|
Australia |
39.0 |
1.39 |
33.4 |
0.91 |
72.2 |
2.10 |
71.8 |
1.45 |
|
|
Measured High (≥140/90mmHg) or Using Medication |
|||||||
|
|
Ages 50-64 |
Ages 65+ |
||||||
|
United States |
50.6 |
1.00 |
57.9 |
1.00 |
61.9 |
1.00 |
73.2 |
1.00 |
|
Netherlands |
53.0 |
1.05 |
47.0 |
0.81 |
76.0 |
1.23 |
71.0 |
0.97 |
|
Spain |
52.3 |
1.03 |
53.9 |
0.93 |
60.3 |
0.97 |
65.2 |
0.89 |
|
England (2003) |
53.1 |
1.05 |
44.7 |
0.77 |
66.6 |
1.08 |
72.1 |
0.98 |
|
Japan |
48.8 |
0.96 |
39.7 |
0.69 |
68.7 |
1.11 |
68.7 |
0.94 |
|
Canada |
|
|
|
|
61.1 |
0.99 |
43.5 |
0.59 |
|
Australia |
46.7 |
0.92 |
42.7 |
0.74 |
71.8 |
1.16 |
70.5 |
0.96 |
|
NOTES: For measured data, estimates made for specified age groups for Australia, France, and Japan. SOURCES: Data on self-reported hypertension from HRS (2004) for United States; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; from ELSA (2002) for England; from NUJLSOA (2003) for Japan; from CCHS (2003) for Canada; from AIHW (2006) and NHS (2004-2005) for Australia (50+); and from Australian Bureau of Statistics (2006a) [http://www.abs.gov.au/ausstats, accessed December 5, 2009] and NHS (2004-2005) for Australia (65+). Data on measured hypertension from NHANES (2001-2006) for the United States; from ELSA (2004) for England; and from the WHO Global Infobase for France (1996), Japan (2000), and Australia (1999-2000). Data on measured and measured plus medication from NHANES (2001-2006) for the United States; from the WHO Global Infobase for the Netherlands (2001), Spain (1990), England (2003), Canada limited to Ontario (1990), and Japan (2000); and from Dunstan et al. (2001) and AusDiab (1999-2000) for Australia. |
||||||||
the proportions who either have measured hypertension, or are using medication, American women have the highest level of hypertension, and the difference is greater in the 50-64 age range.5 For men ages 50-64, there is almost no variability in the proportion with measured hypertension or who use medication across countries; ages 65+, U.S. men appear to have a relatively low level and men in the Netherlands appear to have the highest level. National levels of the percentage with measured high blood pressure and hypertension levels defined as including antihypertensive use are shown relative to life expectancy in Figure 3-6. The relationship is not significant.
Trends in the use of antihypertensives have been similar to those for lipid-lowering drugs, although the uptake of these drugs initially occurred a decade or so earlier. Self-reports of the use of antihypertensives are available for all 10 countries (see Table 3-6). Use of antihypertensives is highest in the United States, although it has increased recently in Europe (Ashworth, Medina, and Morgan, 2008; Primatesta, Brookes, and Poulter, 2001). Italy is the country with the next highest usage, and the ratio of Italian use to American use is .72 and .77 for men and women ages 50+, and .86 and .85 for men and women ages 65+. Overall, the Netherlands appears to be the country with the lowest use of antihypertensives. All of this makes it somewhat hard to determine the relative risk across countries due to elevated blood pressure. Quite clearly, the United States has the most diagnosed high blood pressure but also the fewest people with measured high levels because of the aggressive use of drugs.
Weight
Weight has been increasing throughout the developed world in recent decades, and the increase in the United States has been larger and at earlier ages (Andreyeva, Michaud, and van Soest, 2007; Bleich et al., 2008; Rabin, Boehmer, and Brownson, 2007). Recent rates of increase in obesity have been fastest in the United States, England, and Australia. Data in Table 3-7 are developed from self-reports of height and weight in most countries and measured in others. Self-reports from HRS and SHARE are corrected for tendencies to misreport height and weight (Michaud, van Soest, and Andreyeva, 2007). This is not true for Canada, Australia, or older (65+) Japanese. Body mass index, which is based on measured height and weight, is included for England, the United States, and Japanese ages 50+.
At ages 50+, the level of obesity is highest in the United States. Only English men and Spanish women have levels of obesity even close to those in the United States (ratios of .88 and .89, respectively). Among the Japanese,
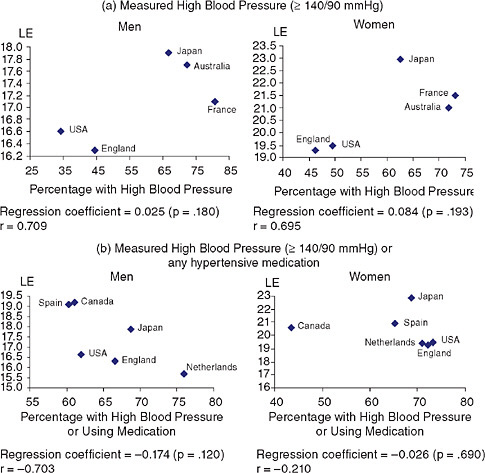
FIGURE 3-6 Measured high blood pressure and life expectancy (LE) at age 65.
SOURCES: Data on high blood pressure from Table 3-5; data on life expectancy for 2004 from the Human Mortality Database (see http://www.mortality.org [accessed March 2, 2009]). Life-expectancy data extracted from country-specific life tables from HMD.
obesity is almost nonexistent (ratios to the United States at 50+ of .10 for men and .08 for women). At ages 65+, obesity in English men and women and Spanish women actually exceeds that in the United States. Again, obesity at this age is extremely low in Japan.
The national prevalence of obesity is graphed against life expectancy at age 50 in Figure 3-7; again, there is no significant relationship, although the association appears stronger among women than men.
TABLE 3-6 Use of Antihypertensive Drugs
|
Country |
Ages 50+ |
Ages 65+ |
||||||
|
Men |
Women |
Men |
Women |
|||||
|
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
|
|
United States |
47.2 |
1.00 |
50.4 |
1.00 |
52.1 |
1.00 |
58.3 |
1.00 |
|
Denmark |
28.3 |
0.60 |
25.8 |
0.51 |
44.0 |
0.84 |
33.1 |
0.57 |
|
France |
29.4 |
0.62 |
34.6 |
0.69 |
39.3 |
0.75 |
45.2 |
0.78 |
|
Italy |
34.1 |
0.72 |
38.8 |
0.77 |
45.0 |
0.86 |
49.4 |
0.85 |
|
Netherlands |
22.4 |
0.47 |
27.7 |
0.55 |
31.7 |
0.61 |
38.2 |
0.66 |
|
Spain |
24.6 |
0.52 |
36.9 |
0.73 |
32.5 |
0.62 |
51.3 |
0.88 |
|
England |
27.7 |
0.59 |
29.8 |
0.59 |
35.4 |
0.68 |
39.9 |
0.68 |
|
Japana |
28.0 |
0.59 |
31.0 |
0.62 |
38.6 |
0.74 |
44.5 |
0.76 |
|
Canada |
27.0 |
0.57 |
30.7 |
0.61 |
39.3 |
0.75 |
46.1 |
0.79 |
|
Australiaa |
28.0 |
0.59 |
36.2 |
0.72 |
34.1 |
0.65 |
45.1 |
0.77 |
|
aEstimates made for specified age groups. SOURCES: Data from HRS (2004) for the United States; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; from ELSA (2002) for England; from CCHS (2003) for Canada (using medication in past month); from the Ministry of Health, Labour and Welfare of Japan (2006) and NHNS (2004) for Japan; and from Dunstan et al. (2001) and AusDiab (1999-2000) for Australia. |
||||||||
MICRO-LEVEL ANALYSIS OF DISEASE PRESENCE, FUNCTIONING LOSS, AND DISABILITY
Taking advantage of the harmonization of the HRS, SHARE, and ELSA data, we can also examine results from individual-level regressions indicating the effect of being a resident of each country while controlling for age and two individual health behaviors: smoking and weight. This analysis does not include data from Australia, Canada, or Japan. Without controls for the behaviors, the odds ratios from logit models for self-reported presence of disease provide an indication of country-level differences assuming the same age distribution. These results should largely reproduce the descriptive results above. With controls for health behaviors, the odds ratios provide an indication of country-level differences in the health indicators, assuming the levels of past and current smoking and weight are similar. Country effects are shown relative to the United States, the omitted category.
The relative level of heart disease is lower in every country than in the United States, with the odds ratios ranging from .31 to .72 (see Table 3-8). There is very little change when health behaviors are controlled, although being obese and having been a smoker are linked to more heart disease. The effect of being obese on heart disease presence is to increase by 50 to 60 percent the relative likelihood of heart disease compared with those who
TABLE 3-7 Prevalence of Obesity and Ratio to U.S. Level
|
Country |
Ages 50+ |
Ages 65+ |
||||||
|
Men |
Women |
Men |
Women |
|||||
|
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
% |
Ratio/ U.S. |
|
|
United States (HRS 2004, self-reported) |
30.7 |
1.00 |
37.9 |
1.00 |
21.2 |
1.00 |
21.8 |
1.00 |
|
Denmark |
17.5 |
0.57 |
18.2 |
0.48 |
12.3 |
0.58 |
12.4 |
0.57 |
|
France |
16.2 |
0.53 |
20.3 |
0.54 |
13.8 |
0.65 |
15.2 |
0.70 |
|
Italy |
15.6 |
0.51 |
23.4 |
0.62 |
14.7 |
0.69 |
17.4 |
0.80 |
|
Netherlands |
15.3 |
0.50 |
23.2 |
0.61 |
11.5 |
0.54 |
15.9 |
0.73 |
|
Spain |
20.8 |
0.68 |
33.6 |
0.89 |
19.8 |
0.93 |
26.3 |
1.21 |
|
England |
27.0 |
0.88 |
30.7 |
0.81 |
24.1 |
1.14 |
29.6 |
1.36 |
|
Japan |
3.0 |
0.10 |
3.0 |
0.08 |
1.1 |
0.04 |
2.5 |
0.11 |
|
Canada |
18.1 |
0.59 |
17.7 |
0.47 |
14.2 |
0.67 |
15.1 |
0.69 |
|
Australia |
19.2 |
0.63 |
19.9 |
0.53 |
13.9 |
0.66 |
14.7 |
0.67 |
|
United States (NHANES 2001-2006, measured) |
32.9 |
1.07 |
35.5 |
0.94 |
27.8 |
1.31 |
30.8 |
1.41 |
|
NOTES: Obesity is defined as a body mass index (BMI) ≥ 30. Self-reported data from SHARE (50+) for Denmark, France, Italy, the Netherlands, and Spain have been corrected for misreporting by Michaud et al. (2007). Measured data used for England (52+). For Japan estimates were made for BMI ≥ 30 for the 50+ population because only overweight (BMI ≥ 25) is reported; for the 65+ population, estimates were computed from self-reports in the NUJLSOA (2003). For Canada and Australia, BMI was calculated from self-reported height and weight. Estimates were made for specified age groups for Australia. Data collection year: for the United States, self-report (2004), measured (2001-2006); for Denmark (2004), France (2004), Italy (2004), the Netherlands (2004), Spain (2004), England (2004), Japan 50+ (2004), 65+ (2003), Canada (2003), Australia (2004-2005). SOURCES: Data on obesity (50+) from Michaud et al. (2007, Table 1) for the United States, Denmark, France, Italy, the Netherlands, and Spain; from ELSA (2004) for England; from the Ministry of Health, Labour and Welfare of Japan (2006) and NHNS (2004) for Japan; from Statistics Canada (see http://www.statcan.gc.ca [accessed July 7, 2009]) and CCHS (2003) for Canada; from the Australian Bureau of Statistics (2006b) (see http://www.abs.gov.au/ausstats [accessed December 5, 2009]) and NHS (2004-2005) for Australia; from NHANES (2001-2006) for the United States (measured). Data on obesity (65+) from HRS (2004) for United States; from SHARE (2004) for Denmark, France, Italy, the Netherlands, and Spain; from ELSA (2004) for England; from NUJLSOA (2003) for Japan; from CCHS (2003) for Canada; and from the Australian Bureau of Statistics (2006b) (see http://www.abs.gov.au/ausstats [accessed December 5, 2009]) and NHS (2004-2005) for Australia. |
||||||||
are not obese. Having been a smoker increases the relative likelihood of heart disease by more than 30 percent.
Relative to the United States, male stroke prevalence is significantly lower in each of these countries except Denmark (OR .33 to .73). This is true with or without controls for health behaviors. Women in the United States, Denmark, and the Netherlands have similar levels of stroke; in other
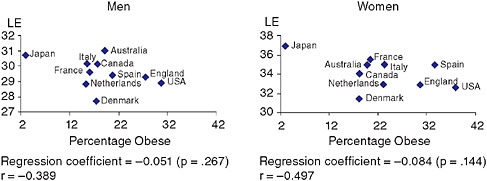
FIGURE 3-7 National percentage obese and national life expectancy at age 50.
SOURCE: Data on obesity from Table 3-7; data on life expectancy for 2004 from the Human Mortality Database (see http://www.mortality.org [accessed March 2009]). Life-expectancy data extracted from country-specific life tables from HMD.
countries, the levels are lower than those in the United States. Having been a smoker for both sexes, currently smoking for men, and being obese for women are strongly associated with having had a stroke.
Every country has significantly lower levels of diabetes than the United States for both men and women, with or without the controls for weight. The odds ratios for other countries on diabetes range from .29 to .82 and are not changed much by controls for weight and smoking, although being overweight or obese is strongly associated with being diabetic. Overweight is linked to odds ratios indicating a doubling of the relative likelihood of having diabetes, whereas being obese multiplies the odds ratios by 3.54 times for men and 5.2 times for women.
The effects of country of interview on functioning and ADLs disability with and without controls for the health behaviors and for the presence of the three diseases (heart disease, diabetes, and stroke) that are potential causes of disability and functioning loss are shown in Table 3-9. When controlled for all these variables, these odds ratios for countries represent the level of functioning and ADL problems in each country relative to the United States if the prevalence of these diseases and the health behaviors were the same across countries.
Both men and women in the United States have more functioning problems. Without controls, the odds ratios for functioning problems for other countries range from .36 to .73. With controls, the odds ratios generally become higher or closer to the United States, indicating that some of the explanations of the difference in functioning problems are the higher level of disease and obesity among Americans. Each disease as well as higher weight and smoking raises the likelihood of functioning problems.
TABLE 3-8 Odds Ratios from Logistic Regressions of Country, Age, and Health Behaviors on Self-Reported Prevalence of Heart Disease, Stroke, and Diabetes
|
|
Heart Disease |
Stroke |
Diabetes |
|||||||||
|
|
Men |
Women |
Men |
Women |
Men |
Women |
||||||
|
|
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
|
Age |
1.06* |
1.06* |
1.05* |
1.06* |
1.05* |
1.06* |
1.06* |
1.07* |
1.02* |
1.03* |
1.02* |
1.03* |
|
United States (ref) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Denmark |
0.34* |
0.35* |
0.31* |
0.33* |
1.01 |
0.97 |
0.84 |
0.82 |
0.41* |
0.48* |
0.38* |
0.49* |
|
France |
0.68* |
0.72* |
0.44* |
0.50* |
0.55* |
0.57* |
0.62* |
0.72* |
0.54* |
0.63* |
0.50* |
0.60* |
|
Italy |
0.40* |
0.43* |
0.42* |
0.46* |
0.58* |
0.58* |
0.44* |
0.49* |
0.65* |
0.73* |
0.66* |
0.75* |
|
Netherlands |
0.48* |
0.50* |
0.36* |
0.38* |
0.73* |
0.70* |
0.84 |
0.87 |
0.38* |
0.45* |
0.51* |
0.60* |
|
Spain |
0.36* |
0.38* |
0.43* |
0.47* |
0.33* |
0.32* |
0.31* |
0.36* |
0.75* |
0.80* |
0.82* |
0.78* |
|
England |
0.64* |
0.63* |
0.72* |
0.68* |
0.41* |
0.40* |
0.44* |
0.41* |
0.38* |
0.36* |
0.29* |
0.25* |
|
Overweight |
|
1.08 |
|
1.08 |
|
1.02 |
|
1.05 |
|
1.79* |
|
2.02* |
|
Obese |
|
1.47* |
|
1.61* |
|
1.12 |
|
1.32* |
|
3.54* |
|
5.20* |
|
Current smoker |
|
0.90 |
|
0.98 |
|
1.34* |
|
1.21 |
|
0.98 |
|
0.96 |
|
Ever smoker |
|
1.36* |
|
1.31* |
|
1.47* |
|
1.42* |
|
1.24* |
|
1.00 |
|
N |
15,211 |
|
19,493 |
|
15,216 |
|
19,498 |
|
15,212 |
|
19,495 |
|
|
*p < 0.05. SOURCE: Data from HRS, SHARE, ELSA Countries, 50+ Sample, 2004. |
||||||||||||
TABLE 3-9 Odds Ratios from Logistic Regressions of Country, Age, and Health Behaviors on Self-Reported Prevalence of Functioning and ADL Difficulty
|
|
Functioning Difficulty |
ADL Difficulty |
||||||
|
|
Men |
Women |
Men |
Women |
||||
|
|
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
M1 |
M2 |
|
Age |
1.06* |
1.06* |
1.05* |
1.06* |
1.05* |
1.05* |
1.06* |
1.06* |
|
United States (ref) |
|
|
|
|
|
|
|
|
|
Denmark |
0.39* |
0.46* |
0.39* |
0.49* |
0.82 |
1.00 |
0.60* |
0.77* |
|
France |
0.45* |
0.53* |
0.56* |
0.74* |
1.09 |
1.39* |
0.70* |
0.93 |
|
Italy |
0.56* |
0.69* |
0.57* |
0.72* |
0.80* |
1.02 |
0.80* |
1.03 |
|
Netherlands |
0.36* |
0.41* |
0.42* |
0.50* |
0.52* |
0.64* |
0.62* |
0.77* |
|
Spain |
0.53* |
0.60* |
0.66* |
0.76* |
0.73* |
0.91 |
0.78* |
0.93 |
|
England |
0.69* |
0.75* |
0.73* |
0.73* |
1.50* |
1.83* |
1.31* |
1.49* |
|
Heart disease |
|
2.13* |
|
2.42* |
|
1.68* |
|
1.87* |
|
Stroke |
|
2.55* |
|
2.51* |
|
3.45* |
|
3.11* |
|
Diabetes |
|
1.68* |
|
1.46* |
|
1.62* |
|
1.81* |
|
Overweight |
|
1.22* |
|
1.58* |
|
1.00 |
|
1.19* |
|
Obese |
|
2.43* |
|
3.89* |
|
1.93* |
|
2.47* |
|
Current smoker |
|
1.33* |
|
1.30* |
|
1.35* |
|
1.42* |
|
Ever smoked |
1.43* |
1.10* |
1.28* |
1.05 |
||||
|
N |
15,204 |
|
19,478 |
|
15,203 |
|
19,484 |
|
|
*p < 0.05. SOURCE: Data from HRS, SHARE, ELSA Countries, 50+ Sample, 2004. |
||||||||
Differences in ADL functioning between men in the United States and those in other countries are not so consistent as those found above for funtioning difficulty. Without controls, there is no difference in ADL functioning among men in Denmark, France, and the United States. English men have more ADL problems than Americans. Men in the United States have worse ADL functioning than men in Italy, Spain, and the Netherlands. If all the countries had the same presence of the three diseases, smoking, and obesity, U.S. men would only have more ADL functioning problems than men in the Netherlands. U.S. women have worse ADL functioning than those in all other countries except England. If the prevalence of the included diseases and the health behaviors were the same across countries, U.S. women would only fare worse than Dutch and Danish women. These results seem to indicate that the relatively poor ranking of Americans in terms of ADL functioning is largely due to the presence of more diseases, more overweight, and higher smoking levels.
DISCUSSION
Reviewing this complex set of health differences, two conclusions stand out. For many indicators of health, the United States ranks as the country with the highest prevalence of problems. This includes functioning, heart disease, stroke at some ages, diabetes, and obesity. The other generalization is that Japan is often the country ranking as best in a number of health indicators. This includes functioning and ADL disability levels, prevalence of heart disease, diabetes, and obesity, and incidence of some cancers. Many other countries rank poorly in some health indicators but do not rank poorly in others, so it is hard to determine a clear ranking for other countries. Denmark and the Netherlands stand out as having relatively high levels of stroke and mortality from some cancers, yet these countries appear to have relatively good levels of physical functioning. The poor position of the United States and the good position of Japan provide some support for a link between levels of life expectancy and levels of population health, but the overall association is weak for many of the indicators.
Banks and colleagues (2006) have pointed out that Americans in their 50s and 60s had more diseases and worse levels of a number of biomarkers than the English. Crimmins and colleagues (Crimmins et al., 2008; Reynolds et al., 2008) have noted that levels of functioning problems and disability, diseases, and a number of biomarkers are worse among Americans than the Japanese. Poor relative health appears to characterize comparisons of Americans with multiple additional countries. The diseases with higher prevalence among Americans are conditions that are related to health behaviors and lifestyle factors.
For a number of indicators, the relatively poor position of the United States was more exaggerated among people ages 50-64 than in the group ages 65+. This included functioning and ADL disability, heart disease, stroke, and obesity. Although we do not have the ability to examine the effects of mortality and disease onset with these data, these findings could be compatible with earlier onset of disease among Americans.
Obesity is a potential explanation of some of the poor health indicators in the United States, as it is related to each of the diseases we examined, and the diseases are, in turn, related to more functioning problems. Our microlevel analysis indicated the substantial effect of obesity on the presence of each of these diseases, functioning loss, and disability; however, our analysis controlling for overweight and obesity indicates that Americans would report more heart disease, stroke, diabetes, and functioning problems even if they had the same levels of overweight, obesity, and smoking patterns as in the SHARE countries and England. In further analysis, we replicated the regressions in Tables 3-8 and 3-9 after eliminating all obese persons, and the results are hardly changed: nonobese Americans are still likely to have more diseases and worse functioning problems. Both obese and the
nonobese Americans have more diseases and disabilities than persons in other countries.
Our disease-specific analyses do not indicate the level of concentration of health problems in individuals. It is possible that the concentration of health problems in individuals differs across countries and is one explanation of why mortality is not strongly related to the prevalence of individual health problems. One hypothesis for why some countries do poorly is that health problems are concentrated in a smaller group in the population. For the countries for which we have individual data, we examined the occurrence of comorbidity of heart disease, stroke, and diabetes. We found dramatically higher levels of comorbidity in the United States than in other countries, indicating a larger portion of the population with multiple serious health risks in the United States (see Table 3-10). The proportion of people with more than one of the three conditions—heart disease, stroke, and diabetes—is generally at least twice as high in the United States as in the other countries. Further analysis should include better information on
TABLE 3-10 Percentage Self-Reporting More Than One of the Three Conditions—Heart Disease, Stroke, and Diabetes
the concentration of risks and comorbid conditions among individuals. This chapter has not examined social differences in health risks across countries, but they are known to be relatively large in the United States (Avendano et al., 2009; Avendano et al., Chapter 11, in this volume). Both social disadvantages and health disadvantages may be more concentrated in the United States, while health disadvantage may be distributed more equally across the population in other countries.
Our data also have some implications for assessing performance of the U.S. health care system relative to those in other countries. The United States does relatively well at diagnosing and treating hypertension and high cholesterol. Risk is reduced well below what it would be without the widespread use of drug treatment. It is hard to say how countries rank in the relative risk from hypertension and high cholesterol given that the United States has the highest diagnosed levels of these risks but almost the lowest measured levels of current risk, indicating high levels of control. This provides an indication of the role of the U.S. health care system in reducing the risk associated with hypertension and high cholesterol. However, the significantly worse health in the United States for people ages 50-64 occurs in an age group whose health care insurance availability is lower than at older ages.
Cancer death rates, except for lung cancer among women, are relatively low in the United States (see also Preston and Ho, Chapter 9, in this volume). Cancer screening appears to identify a relatively high number of cases in the United States and to result in a lower rate of mortality among incident cases. This could reflect good treatment or the fact that extensive screening identifies cases that have a lower chance of dying. Again, it becomes somewhat difficult to determine relative cancer risk across countries, as our observations are so affected by screening. This high identification of screenable cancers is another indication of the positive role of the U.S. health care system.
Can we rely on the results of our analyses of diseases and functioning problems based on self-reports? Research has shown relatively high agreement between the self-report and medical record report for some conditions: diabetes, stroke, and myocardial infarction (Bush et al., 1989; Goldman et al., 2003; Okura et al., 2004). Because our analysis relied on self-reports of diagnosed heart disease, not limited to myocardial infarction, it is possible that national differences in the prevalence of heart disease are affected by reporting and diagnostic differences. The level of agreement between self-report and medical records for hypertension is generally thought to be lower than that for some other conditions, and this may be the case for the European countries included in SHARE in our analysis. Functioning difficulties and disability are generally self-reported in surveys, not based on a doctor’s diagnosis.
Two recent analyses of how Americans and the Dutch report disability
have come to different conclusions about relative reporting tendencies. Comparing responses to vignettes indicates that, with a given description of a disability, Americans are less likely than the Dutch to see a person as disabled (Kapteyn, Smith, and van Soest, 2007); however, another comparison of American and Dutch self-reports of disability to measured disabilities shows Dutch individuals have greater limitation when they report themselves disabled (Melzer et al., 2004). It is hard to know how to assess the overall effect of national differences in reporting or diagnostic tendencies; however, most of the differences we observe are quite large, and they are relatively consistent across many conditions. It is hard to believe that all differences arise from differential reporting. Additional sources of differential reporting include cultural context, sociodemographic characteristics, and environmental circumstances (Bago d’Uva, O’Donnell, and van Doorslaer, 2008; Bago d’Uva et al., 2008; Iburg et al., 2001; Melzer et al., 2004).
Finally, to return to our initial discussion about population health, with prevalence data it is difficult to determine the process that resulted in the observed differences. It is obvious that current health status, including mortality, reflects past heath, health behaviors, and health care use. Thus, in order to understand the process leading to mortality, we need information on earlier health behaviors, incidence of, and survival from certain conditions. However, most of our data indicate current prevalence, cancer being the exception. While our results show higher levels of some conditions and risk factors in the United States, longitudinal data are required for a better understanding of the roles of incidence, treatment, and survival in creating current health, including mortality. As we mentioned earlier, increasing survival among people with diseases and functioning problems can lead to a higher prevalence of health problems in the population. Finally, our cross-sectional data are limited in making any connection between earlier risk factors, lifelong health behaviors, and lifetime circumstances that could affect later health.
ACKNOWLEDGMENTS
Support was provided by the U.S. National Institutes of Health (P30 AG17265) and the University of Southern California Humanities and Social Sciences Fund. This chapter uses data from the early release of SHARE 2004. SHARE data collection was primarily funded through the European Commission through the 5th framework program (Project QLK6-CT-2001-0060 in the thematic program “Quality of Life”). Additional funding came from the U.S. National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12816, Y1-AG-4553-01, and OGHA 04-064). Data collection in Austria, Belgium, and Switzerland was nationally funded. The collection of the Health and Retirement Study was supported by the U.S.
National Institute on Aging (U01 AG009740) and is conducted by the University of Michigan. ELSA was developed by a team of researchers based at the National Centre for Social Research, University College London, and the Institute for Fiscal Studies. The data were collected by the National Centre for Social Research and made available through the UK Data Archive. The funding is provided by the U.S. National Institute on Aging and a consortium of United Kingdom government departments coordinated by the Office for National Statistics. This analysis is based on Statistics Canada’s Canadian Community Health Survey, Cycle 2.1 (2003), Public Use Microdata File, which contains anonymized data. All computations on these microdata were prepared by University of Southern California, and the responsibility for the use and interpretation of these data is entirely that of the authors. The developers and funders of the data sets do not bear any responsibility for the analyses or interpretations presented here.
REFERENCES
Aijanseppa, S., Notkola, I.L., Tijhuis, M., van Stavern, W., Kromhout, D., and Nissinen, A. (2005). Physical functioning in elderly Europeans: 10-year changes in the north and south: The HALE project. Journal of Epidemiology and Community Health, 59(5), 413-419.
Andreyeva, T., Michaud, P.C., and van Soest, A. (2007). Obesity and health in Europeans aged 50 years and older. Public Health, 121, 497-509.
Asai, A. (1995). Should physicians tell patients the truth? Western Journal of Medicine, 163(1), 6-39.
Ashworth, M., Medina, J., and Morgan, M. (2008). Effect of social deprivation on blood pressure monitoring and control in England. British Medical Journal, 337, a2030.
Australian Bureau of Statistics. (2006a). Health of Older People in Australia: A Snapshot, 2004-2005. No. 4833.0.55.001. Canberra: Australian Bureau of Statistics. Available http://www.abs.gov.au/ausstats [accessed December 2009].
Australian Bureau of Statistics. (2006b). National Health Survey: Summary of Results, Australia 2004-2005. No. 4364.0. Canberra: Australian Bureau of Statistics. Available http://www.abs.gov.au/ausstats [accessed December 2009].
Australian Institute of Health and Welfare. (2006). Chronic Diseases and Associated Risk Factors in Australia, 2006. No. PHE 81. Canberra: Author.
Avendano, M., Glymour, M., Banks, J., and Mackenbach, J.P. (2009). Health disadvantage in U.S. adults aged 50-74 years: A comparison of the health of rich and poor Americans with that of Europeans. American Journal of Public Health, 99, 540-548.
Bago d’Uva, T., O’Donnell, O., and Van Doorslaer, E. (2008). Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. International Journal of Epidemiology, 37, 1375-1383.
Bago d’Uva, T., Van Doorslaer, E., Lindeboom, M., and O’Donnell, O. (2008). Does reporting heterogeneity bias the measurement of health disparities? Health Economics, 17, 351-375.
Banks, J., Marmot, M., Oldfield, Z., and Smith, J.P. (2006). Disease and disadvantage in the United States and in England. Journal of the American Medical Association, 295, 2037-2045.
Banta, H.D., and Oortwiin, W. (2001). Health technology assessment and screening in the Netherlands: Case studies of mammography in breast cancer, PSA screening in prostate cancer, and ultrasound in normal pregnancy. International Journal of Technology Assessment in Health Care, 17(3), 369-379.
Bleich, S., Cutler, D., Murray, C., and Adams, A. (2008). Why is the developed world obese? Annual Review of Public Health, 29, 273-295.
Börsch-Supan, A., and Jürges, H. (Eds.). (2005). The Survey of Health, Ageing and Retirement in Europe: Methodology. Mannheim, Germany: Mannheim Research Institute for the Economics of Ageing.
Börsch-Supan, A., Brugiavini, A., Jürges, H., Makenbach, J., Siegrist, J., and Weber, G. (Eds.). (2005). Health, Ageing, and Retirement in Europe: First Results from the Survey of Health, Ageing, and Retirement in Europe. Mannheim, Germany: Mannheim Research Institute for the Economics of Ageing.
Bush, T., Miller, S., Golden, A., and Hale, W. (1989). Self-report and medical record report agreement of selected medical conditions in the elderly. American Journal of Public Health, 79, 1554-1556.
Chronic Condition Data Warehouse. (2009). Medicare Beneficiary Prevalence for Chronic Conditions for 2000-2007 (Table B.2). Available http://ccwdata.org/downloads/data_tables/CCW_Web_Site_Table_B.2.pdf [accessed June 2009].
Crimmins, E.M., and Saito, Y. (2001). Trends in healthy life expectancy in the United States, 1970-1990: Gender, racial, and educational differences. Social Science and Medicine, 52, 1629-1641.
Crimmins, E., Hayward, M., and Saito, Y. (1994). Changing mortality and morbidity rates and the health status and life expectancy of the older U.S. population. Demography, 31, 159-175.
Crimmins, E.M., Kim, J.K., Vasunilashorn, S., Hagedorn, A., and Saito, Y. (2008). A comparison of biological risk factors in two populations: The United States and Japan. Population and Development Review, 34, 457-482.
Crimmins, E.M., Kim, J.K., and Vasunilashorn, S. (2010). Biodemography: New approaches to understanding trends and differences in population health and mortality. Submitted to Demography.
Cutler, D.M., and Richardson, E. (1997). Measuring the health of the U.S. population. In M. Baily, P. Reiss, and C. Winston (Eds.), Brookings Papers on Economic Activity: Microeconomics (pp. 214-282). Washington, DC: Brookings Institution.
DECODE Study Group, on behalf of the European Diabetes Epidemiology Study Group. (1998). Will new diagnostic criteria for diabetes mellitus change phenotype of patients with diabetes? Reanalysis of European epidemiological data. British Medical Journal, 317, 371-375.
Dunstan, D., Zimmet, P., Welborn, T., Sicree, R., Armstrong, T., Atkins, R., Cameron, A., Shaw, J., and Chadban, S. (2001). Diabetes and Associated Disorders in Australia—2000: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Available http://www.diabetes.com.au/pdf/AusDiab_Report.pdf [accessed December 2009].
Ferlay, J., Bray, F., Pisani, P., and Parkin, D.M. (2004). GLOBOCAN 2002: Cancer Incidence, Mortality and Prevalence Worldwide. IARC CancerBase No. 5. version 2.0. Lyon, France: IARC Press.
Freedman, V.A., Crimmins, E., Schoeni, R.F., Spillman, B.C., Aykan, H., Kramarow, E., Land, K., Lubitz, J., Manton, K., Martin, L.G., Shinberg, D., and Waidmann, T. (2004). Resolving inconsistencies in old-age disability trends: Report from a technical working group. Demography, 41, 417-441.
Freedman, V.A., Schoeni, R.F., Martin, L.G., and Cornman, J.C. (2007). Chronic conditions and the decline in late-life disability. Demography, 44(3), 450-477.
Fries, J.F. (1980). Aging, natural death, and the compression of morbidity. New England Journal of Medicine, 303, 130-135.
Goldman, N., Lin, I., Weinstein, M., and Lin,Y. (2003). Evaluating the quality of self-reports of hypertension and diabetes. Journal of Clinical Epidemiology, 56, 148-154.
Gregg, E.W., Cadwell, B.L., Cheng, Y.J., Cowie, C.C., Williams, D.E., Geiss, L., Engelgau, M.M., and Vinicor, F. (2004). Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the United States. Diabetes Care, 27(12), 2806-2812.
Gruenberg, E.M. (1977). The failures of success. Milbank Memorial Fund Quarterly/Health and Society, 55, 3-24.
Hakama, M., Coleman, M.P., Alexe, D.M., and Auvinen, A. (2008). Cancer screening: Evidence and practice in Europe 2008. European Journal of Cancer, 44(10), 1404-1413.
Health and Retirement Study. (2006). 2004 HRS Core. Final, v.1.0 (data file). Available http://hrsonline.isr.umich.edu/ [accessed January 2009].
Human Mortality Database. (2009). Life Tables (data file). University of California Berkeley, and Max Planck Institute for Demographic Research (Germany). Available http://www.mortality.org [accessed March 2009].
Iburg, K., Salomon, J.A., Tandon, A., and Murray, C.J.L. (2001). Cross-Population Comparability of Physician-Assessed and Self-Reported Measures of Health: Evidence from the Third National Health and Nutrition Examination Survey. Discussion Paper No.14. Available http://www.who.int/healthinfo/paper14.pdf [accessed November 2009].
Jemal, A., Ward, E., Hao, Y., and Thun, M. (2005). Trends in the leading causes of death in the United States, 1970-2002. Journal of the American Medical Association, 294(10), 1255-1259.
Kapteyn, A., Smith, J.P., and van Soest, A. (2007). Vignettes and self-reports of work disability in the United States and the Netherlands. American Economic Review, 97(1), 461-473.
Lafortune, G., Balestat, G., and the Disability Study Expert Group Members. (2007). Trends in Severe Disability Among Elderly People: Assessing the Evidence in 12 OECD Countries and the Future Implications. Working Paper No. 26. Available http://www.oecd.org/dataoecd/13/8/38343783.pdf [accessed March 2009].
Mantel-Teeuwisse, A.K., Klungel, O.H., Verschuren, W.M., Porsius, A.J., and de Boer, A. (2002). Time trends in lipid lowering drug use in the Netherlands. Has the backlog of candidates for treatment been eliminated? British Journal of Clinical Pharmacology, 53, 379-385.
Manton, K.G. (1982). Changing concepts of morbidity and mortality in the elderly population. Milbank Memorial Fund Quarterly/Health and Society, 60, 183-244.
Marmot, M., Banks, J., Blundell, R., Lessof, C., and Nazroo, J. (Eds.). (2007). Health, Wealth, and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study of Aging. Report No. P2058. London, England: Institute for Fiscal Studies, National Center for Social Research.
Melzer, D., Lan, T.Y., Tom, B.D.M., Deeg, D.J.H., and Guralnik, J. (2004). Variation in thresholds for reporting mobility disability between national population subgroups and studies. Journal of Gerontology: Medical Sciences, 59A(12), 1295-1303.
Michaud, P., van Soest, A., and Andreyeva, T. (2007). Cross-country variation in obesity patterns among older Americans and Europeans. Forum for Health Economics and Policy, 10(2), Article 8.
Ministry of Health, Labour and Welfare of Japan. (2006). National Health and Nutrition Survey Report, 2004. (In Japanese). Tokyo, Japan: Daiichi Shuppan.
Nihon University Japanese Longitudinal Study of Aging. (2009). Nihon University Japanese Longitudinal Study of Aging. Available http://www.usc.edu/dept/gero/CBPH/nujlsoa/ [accessed February 19, 2009].
Okura, Y., Urban, L., Mahoney, D., Jacobsen, S., and Rodeheffer, R. (2004). Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. Journal of Clinical Epidemiology, 57, 1096-1103.
Organisation for Economic Co-operation and Development. (2008). OECD Health Data 2008 (Version 06/28/2008) [Statistics]. Available http://new.sourceoecd.org [accessed October 8, 2008].
Parikh, N.I., Gona, P., Larson, M.G., Fox, C.S., Benjamin, E.J., Murabito, J.M., O’Donnell, C.J., Vasan, R.S., Levy, D. (2009). Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute’s Framingham Heart Study. Circulation, 10, 1203-1210.
Primatesta, P., Brookes, M., and Poulter, N.R. (2001). Improved hypertension management and control: Results from the health survey for England 1998. Hypertension, 38, 827-832.
Quinn, M.J. (2003). Cancer trends in the United States: A view from Europe. Journal of the National Cancer Institute, 95(17), 1258-1261.
Rabin, B.A., Boehmer, T.K., and Brownson, R.C. (2007). Cross-national comparison of environmental and policy correlates of obesity in Europe. European Journal of Public Health, 17(1), 53-61.
Reed, D.M. (1990). The paradox of high risk of stroke in population with low risk of coronary heart disease. American Journal of Epidemiology, 131(4), 579-588.
Reynolds, S.L., Hagedorn, A., Yeom, J., Saito, Y., Yokoyama, E., and Crimmins, E.M. (2008). A tale of two countries—the United States and Japan: Are differences in health due to differences in overweight? Journal of Epidemiology, 18, 280-290.
Schoeni, R.F., Liang, J., Bennett, J., Sugisawa, H., Fukaya, T., and Kobayashi, E. (2006). Trends in old-age functioning and disability in Japan, 1993-2002. Population Studies, 60(1), 39-53.
Seeman, T., Merkin, S.S., Crimmins, E.M., and Karlamangla, A. (2010). Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988-1994 and 1999-2004. American Journal of Public Health, 100(1), 100-107.
Statistics Canada. (2010). CANSIM, Table 105-0501. No. 82-221-X. [Statistics]. Available http://www.statcan.gc.ca [accessed July 7, 2009].
Walley, T., Folino-Gallo, P., Stephens, P., and Van Ganse, E. (2005). Trends in prescribing and utilization of statins and other lipid lowering drugs across Europe 1997-2003. British Journal of Clinical Pharmacology, 60(5), 543-551.
Wang, Y.R., Alexander, G.C., and Stafford, R.S. (2007). Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Archives of Internal Medicine, 167, 141-147.
Wareham, N.J., and O’Rahilly, S. (1998). The changing classification and diagnosis of diabetes: New classification is based on pathogenesis, not insulin dependence. British Medical Journal, 317(7155), 359-360.
Wolf-Maier, K., Cooper, R.S., Banega, J.R., Giampaoli, S., Hense, H.W., Joffres, M., Kastarinen, M., Poulter, N., Primatesta, P., Rodríguez-Artalejo, F., Stegmayr, B., Thamm, M., Tuomilehto, J., Vanuzzo, D., and Vescio, F. (2003). Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. Journal of the American Medical Association, 289(18), 2363-2369.
World Health Organization. (2009). WHO Global InfoBase Online [Statistics]. Available https://apps.who.int/infobase/report.aspx [accessed January 2009].



































