3
Transforming Practice
|
Key Message #1: Nurses should practice to the full extent of their education and training. Patients, in all settings, deserve care that is centered on their unique needs and not what is most convenient for the health professionals involved in their care. A transformed health care system is required to achieve this goal. Transforming the health care system will in turn require a fundamental rethinking of the roles of many health professionals, including nurses. The Affordable Care Act of 2010 outlines some new health care structures, and with these structures will come new opportunities for new roles. A number of programs and initiatives have already been developed to target necessary improvements in quality, access, and value, and many more are yet to be conceived. Nurses have the opportunity to play a central role in transforming the health care system to create a more accessible, high-quality, and value-driven environment for patients. If the system is to capitalize on this opportunity, however, the constraints of outdated policies, regulations, and cultural barriers, including those related to scope of practice, will have to be lifted, most notably for advanced practice registered nurses. |
The Affordable Care Act of 2010 (ACA) will place many demands on health professionals and offer them many opportunities to create a system that is more patient centered. The legislation has begun the long process of shifting the focus of the U.S. health care system away from acute and specialty care. The need for this shift in focus has become particularly urgent with respect to chronic conditions; primary care, including care coordination and transitional care; prevention and wellness; and the prevention of adverse events, such as hospital-acquired infections. Given the aging population, moreover, the need for long-term and palliative care will continue to grow in the coming years (see Chapter 2). The increase in the insured population and the rapid increase in racial and ethnic minority groups who have traditionally faced obstacles in accessing health care will also demand that care be designed for a more socioeconomically and culturally diverse population.
This chapter examines how enabling nurses to practice to the full extent of their education and training (key message #1 in Chapter 1) can be a major step forward in meeting these challenges. The first section explains why transforming nursing practice to improve care is so important, offering three examples of how utilizing the full potential of nurses has increased the quality of care while achieving greater value. The chapter then examines in detail the barriers that constrain this transformation, including regulatory barriers to expanding nurses’ scope of practice, professional resistance to expanded roles for nurses, fragmentation of the health care system, outdated insurance policies, high turnover rates among nurses, difficulties encountered in the transition from education to practice, and demographic challenges. The third section describes the new structures and opportunities made possible by the ACA, as well as through technology. The final section summarizes the committee’s conclusions regarding the vital contributions of the nursing profession to the success of these initiatives as well as the overall transformation of the health care system, and what needs to be done to transform practice to ensure that this contribution is realized. Particular emphasis is placed on advanced practice registered nurses (APRNs), including their roles in chronic disease management and increased access to primary care, and the regulatory barriers preventing them from taking on these roles. This is not to say that general registered nurses (RNs) should not have the opportunity to improve their practice and take on new roles; the chapter also provides such examples.
THE IMPORTANCE OF TRANSFORMING NURSING PRACTICE TO IMPROVE CARE
As discussed in Chapter 2, the changing landscape of the health care system and the changing profile of the population require that the system undergo a fundamental shift to provide patient-centered care; deliver more primary as opposed to specialty care; deliver more care in the community rather than the acute care setting; provide seamless care; enable all health professionals to practice to the
full extent of their education, training, and competencies; and foster interprofessional collaboration. Achieving such a shift will enable the health care system to provide higher-quality care, reduce errors, and increase safety. Providing care in this way and in these areas taps traditional strengths of the nursing profession. This chapter argues that nurses are so well poised to address these needs by virtue of their numbers, scientific knowledge, and adaptive capacity that the health care system should take advantage of the contributions they can make by assuming enhanced and reconceptualized roles.
Nursing is one of the most versatile occupations within the health care workforce.1 In the 150 years since Florence Nightingale developed and promoted the concept of an educated workforce of caregivers for the sick, modern nursing has reinvented itself a number of times as health care has advanced and changed (Lynaugh, 2008). As a result of the nursing profession’s versatility and adaptive capacity, new career pathways for nurses have evolved, attracting a larger and more broadly talented applicant pool and leading to expanded scopes of practice and responsibilities for nurses. Nurses have been an enabling force for change in health care along many dimensions (Aiken et al., 2009). Among the many innovations that a versatile, adaptive, and well-educated nursing profession have helped make possible are
-
the evolution of the high-technology hospital;
-
the possibility for physicians to combine office and hospital practice;
-
lengths of hospital stay that are among the shortest in the world;
-
reductions in the work hours of resident physicians to improve patient safety;
-
expansion of national primary care capacity;
-
improved access to care for the poor and for rural residents;
-
respite and palliative care, including hospice;
-
care coordination for chronically ill and elderly people; and
-
greater access to specialty care and focused consultation (e.g., incontinence consultation, home parenteral nutrition services, and sleep apnea evaluations) that complement the care of physicians and other providers.
With every passing decade, nursing has become an increasingly integral part of health care services, so that a future without large numbers of nurses is impossible to envision.
|
1 |
This discussion draws on a paper commissioned by the committee on “Nursing Education Policy Priorities,” prepared by Linda H. Aiken, University of Pennsylvania (see Appendix I on CD-ROM). |
Nurses and Access to Primary Care
Given current concerns about a shortage of primary care health professionals, the committee paid particular attention to the role of nurses, especially APRNs,2 in this area. Today, nurse practitioners (NPs), together with physicians and physician assistants, provide most of the primary care in the United States. Physicians account for 287,000 primary care providers, NPs for 83,000, and physician assistants for 23,000 (HRSA, 2008; Steinwald, 2008). While the numbers of NPs and physician assistants are steadily increasing, the numbers of medical students and residents entering primary care have declined in recent years (Naylor and Kurtzman, 2010). The demand to build the primary care workforce, including APRNs, will grow as access to coverage, service settings, and services increases under the ACA. While NPs make up slightly less than a quarter of the country’s primary care professionals (Bodenheimer and Pham, 2010), it is a group that has grown in recent years and has the potential to grow further at a relatively rapid pace.
The Robert Wood Johnson Foundation (RWJF) Nursing Research Network commissioned Kevin Stange, University of Michigan, and Deborah Sampson, Boston College, to provide information on the variation in numbers of NPs across the United States. Figures 3-1 and 3-2, respectively, plot the provider-to-primary care doctor of medicine (MD) ratio for NPs and physician assistants by county for 2009.3 The total is calculated as the population-weighted average for states with available data. Between 1995 and 2009, the number of NPs per primary care MD more than doubled, from 0.23 to 0.48, as did the number of physician assistants per primary care MD (0.12 to 0.28) (RWJF, 2010c). These figures suggest that it is possible to increase the supply of both NPs and physician assistants in a relatively short amount of time, helping to meet the increased demand for care.
In addition to the numbers of primary care providers available across the United States and where specifically they practice, it is worth noting the kind of care being provided by each of the primary care provider groups. According to the complexity-of-care data shown in Table 3-1, the degree of variation among primary care providers is relatively small. Much of the practice of primary care—whether provided by physicians, NPs, physician assistants, or certified nurse midwives (CNMs)—is of low to moderate complexity.
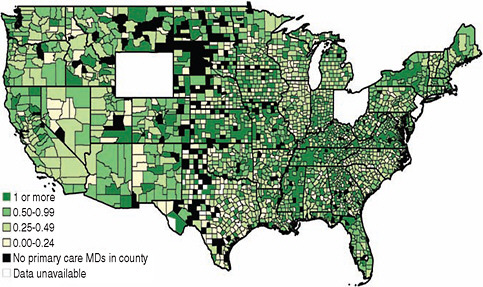
FIGURE 3-1 Map of the number of NPs per primary care MD by county, 2009.
SOURCE: RWJF, 2010a. Reprinted with permission from Lori Melichar, RWJF.
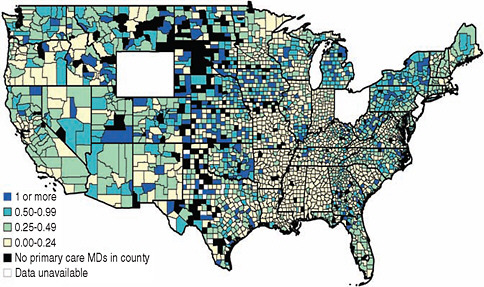
FIGURE 3-2 Map of the number of physician assistants per primary care MD by county, 2009.
SOURCE: RWJF, 2010b. Reprinted with permission from Lori Melichar, RWJF.
TABLE 3-1 Complexity of Evaluation and Management Services Provided Under Medicare Claims Data for 2000, by Practitioner Type
Nurses and Quality of Care
Beyond the issue of pure numbers of practitioners, a promising field of evidence links nursing care to a higher quality of care for patients, including protecting their safety. According to Mary Naylor, director of the Robert Wood Johnson Foundation’s Interdisciplinary Nursing Quality Research Initiative (INQRI), several INQRI-funded research teams have provided examples of this link. “[Nurses] are crucial in preventing medication errors, reducing rates of infection and even facilitating patients’ transition from hospital to home.”4
INQRI researchers at The Johns Hopkins University have found that substantial reductions in central line–associated blood stream infections can be achieved with nurses leading the infection control effort. Hospitals that adopted INQRI’s intensive care unit safety program, as well as an environment that supported nurses’ involvement in quality improvement efforts, reduced or eliminated bloodstream infections (INQRI, 2010b; Marsteller et al., 2010).
Other INQRI researchers linked a core cluster of nurse safety processes to fewer medication errors. These safety processes include asking physicians to clarify or rewrite unclear orders, independently reconciling patient medications, and providing patient education. A positive work environment was also important. This included having more RNs per patient, a supportive management structure, and collaborative relationships between nurses and physicians (Flynn et al., 2010; INQRI, 2010a).
Examples of Redesigned Roles for Nurses
Many examples exist in which organizations have been redesigned to better utilize nurses, but their scale is small. As Marilyn Chow, vice president of the Patient Services Program Office at Kaiser Permanente, declared at a public forum hosted by the committee, “The future is here, it is just not everywhere” (IOM, 2010b). For example, over the past 20 years, the U.S. Department of Veterans Affairs (VA) has expanded and reconceived the roles played by its nurses as part of a major restructuring of its health care system. The results with respect to quality, access, and value have been impressive. In addition, President Obama has lauded the Geisinger Health System of Pennsylvania, which provides comprehensive care to 2.6 million people at a greater value than is achieved by most other organizations (White House, 2009). Part of the reason Geisinger is so effective is that it has aligned the roles played by nurses to accord more closely with patients’ needs, starting with its primary care sites and ambulatory areas. The following subsections summarize the experience of the VA and Geisinger, as well as Kaiser Permanente, in expanding and reconceptualizing the roles of nurses. Because these institutions also measured outcomes as part of their initiatives, they provide real-world evidence that such an approach is both possible and necessary. Of note in these examples is not only how nurses are collaborating with physicians, but also how nurses are collaborating with other nurses.
Department of Veterans Affairs5
In 1996, Congress greatly expanded the number of veterans eligible to receive VA services, which created a need for the system to operate more efficiently and effectively (VHA, 2003). Caring for the wounded from the wars in Afghanistan and Iraq has further increased demand on the VA system, particularly with respect to brain injuries and posttraumatic stress disorder. Moreover, the large cohort of World War II veterans means that almost 40 percent of veterans are aged 65 or older, compared with 13 percent of the general population (U.S. Census Bureau, 2010; VA, 2010).
Anticipating the challenges it would face, the VA began transforming itself in the 1990s from a hospital-based system into a health care system that is focused on primary care, and it also placed emphasis on providing more services, as appropriate, closer to the veteran’s home or community (VHA, 2003, 2009). This strategy required better coordination of care and chronic disease management—a role that was filled by experienced front-line RNs. More NPs were hired as primary care providers, and the VA actively promoted a more collaborative professional culture by organizing primary care providers into health teams. It
also developed a well-integrated information technology system to link its health professionals and its services.
The VA uses NPs as primary care providers to care for patients across all settings, including inpatient and outpatient settings. In addition to their role as primary care providers, NPs serve as health care researchers who apply their findings to the variety of settings in which they practice. They also serve as educators, some as university faculty, providing clinical experiences for 25 percent of all nursing students in the country. As health care leaders, VA NPs shape policy, facilitate access to VA health care, and impact resource management (VA, 2007).
The results of the VA’s initiatives using both front-line RNs and APRNs are impressive. Quality and outcome data consistently demonstrate superior results for the VA’s approach (Asch et al., 2004; Jha et al., 2003; Kerr et al., 2004). One study found that VA patients received significantly better health care—based on various quality-of-care indicators6—than patients enrolled in Medicare’s fee-for-service program. In some cases, the study showed, between 93 and 98 percent of VA patients received appropriate care in 2000; the highest score for comparable Medicare patients was 84 percent (Jha et al., 2003). In addition, the VA’s spending per enrollee rose much more slowly than Medicare’s, despite the 1996 expansion of the number of veterans who could access VA services. After adjusting for different mixes of population and demographics, the Congressional Budget Office determined that the VA’s spending per enrollee grew by 30 percent from 1999 to 2007, compared with 80 percent for Medicare over the same period.
Geisinger Health System7
The Geisinger Health System employs 800 physicians; 1,900 nurses; and more than 1,000 NPs, physician assistants, and pharmacists. Over the past 18 years, Geisinger has transformed itself from a high-cost medical facility to one that provides high value—all while improving quality. It has borrowed several restructuring concepts from the manufacturing world with an eye to redesigning care by focusing on what it sees as the most critical determinant of quality and cost—actual caregiving. “What we’re trying to do is to have [our staff] work up to the limit of their license and … see if redistributing caregiving work can increase quality and decrease cost,” Glenn Steele, Geisinger’s president and CEO, said in a June 2010 interview (Dentzer, 2010).
Numerous improvements in the quality of care, as well as effective innovations proposed by employees, have resulted. For example, the nurses who
used to coordinate care and provide advice through the telephone center under Geisinger’s health plan suspected that they would be more effective if they could build relationships with patients and meet them at least a few times face to face. Accordingly, some highly experienced general-practice nurses moved from the call centers to primary care sites to meet with patients and their families. The nurses used a predictive model to identify who might need to go to the hospital and worked with patients and their families on creating a care plan. Later, when patients or families received a call from a nurse, they knew who that person was. The program has worked so well that nurse coordinators are now being used in both Geisinger’s Medicare plan and its commercial plan.8 Some of the nation’s largest for-profit insurance companies, including WellPoint and Cigna, are now trying out the approach of employing more nurses to better coordinate their patients’ care (Abelson, 2010). As a result, an innovation that emerged when a few nurses at Geisinger took the initiative and changed an already well-established program to deliver more truly patient-centered care may now spread well beyond Pennsylvania. Geisinger was also one of the very first health systems in the country to create its own NP-staffed convenient care clinics9—another innovation that reflects the organization’s commitment to providing integrated, patient-centered care throughout its community.
As one of the largest not-for-profit health plans, Kaiser Permanente provides health care services for more than 8.6 million members, with an employee base of approximately 165,000. Kaiser Permanente has facilities in nine states and the District of Columbia, and has 35 medical centers and 454 medical offices. The system provides prepaid health plans that emphasize prevention and consolidated services designed to keep as many services as possible in one location (KP, 2010). Kaiser is also at the forefront of experimenting with reconceptualized roles for nurses that are improving quality, satisfying patients, and making a difference to the organization’s bottom line.
Nurses in San Diego have taken the lead in overseeing the process for patient discharge, making it more streamlined and efficient and much more effective. Discharge nurses now have full authority over the entire discharge process until home health nurses, including those in hospice and palliative care, step in to take over the patient’s care. They have created efficiencies relative to previous
processes by using time-sensitive, prioritized lists of only those patients who are being discharged over the next 48 hours (instead of patients who are being discharged weeks into the future). Home health care nurses and discharge planners stay in close contact with one another on a daily basis to make quick decisions about patient needs, including the need for home health care visitation. In just 3 months, the number of patients who saw a home health care provider within 24 hours increased from 44 to 77 percent (Labor Management Partnership, 2010).
In 2003, Riverside Medical Center implemented the Riverside Proactive Health Management Program (RiPHM)™, an integrated, systematic approach to health care management that promotes prevention and wellness and coordinates interventions for patients with chronic conditions. The model strengthens the patient-centered medical home concept and identifies members of the health care team (HCT)—a multidisciplinary group whose staff is centrally directed and physically located in small units within the medical office building. The team serves panel management and comprehensive outreach and inreach functions to support primary care physicians and proactively manage the care of members with chronic conditions such as diabetes, hypertension, cardiovascular disease, asthma, osteoporosis, and depression. The expanded role of nurses as key members of the HCT is a major factor in RiPHM’s success. Primary care management nurse clinic RNs and licensed practical nurses (LPNs) provide health care coaching and education for patients to promote self-management of their chronic conditions through face-to-face education visits and telephone follow-up. Using evidence-based clinical guidelines, such as diabetes and hypertension treat-to-target algorithms, nurses play important roles in the promotion of changes in chronic conditions and lifestyles, coaching and counseling, self-monitoring and goal setting, depression screening, and the use of advanced technology such as interactive voice recognition for patient outreach.
Through this model of care, nurses and pharmacists have become skilled users of health information technology to strengthen the primary care–based, patient-centered medical home. Nurses use disease management registries to work with assigned primary care physicians, and review clinical information that addresses care gaps and evaluate treatment plans. RiPHM has provided a strong foundation for the patient-centered medical home. By implementing this program and expanding the role of nurses, Riverside has sustained continuous improvement in key quality indicators for patient care.
Guided care is a new model for chronic care that was recently introduced within the Kaiser system. Guided care is intended to provide, within a primary care setting, quality care to patients with complex needs and multiple chronic conditions. An RN, who assists three to four physicians, receives training in such areas as the use of an electronic health record (EHR), interviewing, and the particulars of health insurance coverage. RNs are also provided skills in managing chronic conditions, providing transitional care, and working with families and community organizations (Boult et al., 2008).
The nurse providing guided care offers eight services: assessment; planning care; monitoring; coaching; chronic disease self-management; educating and supporting caregivers; coordinating transitions between providers and sites of care; and facilitating access to community services, such as Meals-on-Wheels, transportation services, and senior centers. Results of a pilot study comparing surveys of patients who received guided care and those who received usual care revealed improved quality of care and lower health care costs (according to insurance claims) for guided care patients (Boult et al., 2008).
Summary
The VA, Geisinger, and Kaiser Permanente are large integrated care systems that may be better positioned than others to invest in the coordination, education, and assessment provided by their nurses, but their results speak for themselves. If the United States is to achieve the necessary transformation of its health care system, the evidence points to the importance of relying on nurses in enhanced and reconceptualized roles. This does not necessarily mean that large regional corporations or vertically integrated care systems are the answer. It does mean that innovative, high-value solutions must be developed that are sustainable, easily adopted in other locations, and rapidly adaptable to different circumstances. A website on “Innovative Care Models” illustrates that many other solutions have been identified in other types of systems.12 As patients, employers, insurers, and governments become more aware of the benefits offered by nurses, they may also begin demanding that health care providers restructure their services around the contributions that a transformed nursing workforce can make. As discussed later in the chapter, the committee believes there will be numerous opportunities for nurses to help develop and implement care innovations and assume leadership roles in accountable care organizations and medical homes as a way of providing access to care for more Americans. As the next section describes, however, it will first be necessary to acknowledge the barriers that prevent nurses from practicing to the full extent of their education and training, as well as to generate the political will on the part of policy makers to remove these barriers.
BARRIERS TO TRANSFORMING PRACTICE
Nurses have great potential to lead innovative strategies to improve the health care system. As discussed in this section, however, a variety of historical, regulatory, and policy barriers have limited nurses’ ability to contribute to widespread transformation (Kimball and O’Neil, 2002). This is true of all RNs, including those practicing in acute care and public and community health settings, but is most notable for APRNs in primary care. Other barriers include
professional resistance to expanded roles for nurses, fragmentation of the health care system, outdated insurance policies, high rates of nurse turnover, difficulties for nurses transitioning from school into practice, and an aging workforce and other demographic challenges. Many of these barriers have developed as a result of structural flaws in the U.S. health care system; others reflect limitations of the present work environment or the capacity and demographic makeup of the nursing workforce itself.
Regulatory Barriers
As the committee considered how the additional 32 million people covered by health insurance under the ACA would receive care in the coming years, it identified as a serious barrier overly restrictive scope-of-practice regulations for APRNs that vary by state. Scope-of-practice issues are of concern for CNMs, certified registered nurse anesthetists (CRNAs), NPs, and clinical nurse specialists (CNSs). The committee understands that physicians are highly trained and skilled providers and believes strongly that there clearly are services that should be provided by these health professionals, who have received more extensive and specialized education and training than APRNs. However, regulations in many states result in APRNs not being able to give care they were trained to provide. The committee believes all health professionals should practice to the full extent of their education and training so that more patients may benefit.
History of the Regulation of the Health Professions
A paper commissioned by the committee13 points out that the United States was one of the first countries to regulate health care providers and that this regulation occurred at the state—not the federal—level. Legislatively, physician practice was recognized before that of any other health profession (Rostant and Cady, 1999). For example, legislators in Washington defined the practice of medicine broadly as any action to “diagnose, cure, advise or prescribe for any human disease, ailment, injury, infirmity, deformity, pain or other condition, physical or mental, real or imaginary, by any means or instrumentality” or to administer or prescribe “drugs or medicinal preparations to be used by any other person” or to “[sever or penetrate] the tissues of human beings.”14 Even more important were corresponding provisions making it illegal for anyone not licensed as a physician to undertake any of the acts included in this definition. These provisions
|
13 |
This and the following paragraph draw on a paper commissioned by the committee on “Federal Options for Maximizing the Value of Advanced Practice Registered Nurses in Providing Quality, Cost-Effective Health Care,” prepared by Barbara J. Safreit, Lewis & Clark Law School (see Appendix H on CD-ROM). |
|
14 |
Washington Rev. Code §18.71.011 (1)-(3) (1993). |
rendered the practice of medicine not only comprehensive but also (in medicine’s own view) exclusive,15 a preemption of the field that was reinforced when physicians obtained statutory authority to control the activities of other health care providers.
Most APRNs are in the opposite situation. Because virtually all states still base their licensure frameworks on the persistent underlying principle that the practice of medicine encompasses both the ability and the legal authority to treat all possible human conditions, the scopes of practice for APRNs (and other health professionals) are exercises in legislative exception making, a “carving out” of small, politically achievable spheres of practice authority from the universal domain of medicine. As a result, APRNs’ scopes of practice are so circumscribed that their competence extends far beyond their authority. At any point in their career, APRNs can do much more than they may legally do. As APRNs acquire new skills, they must seek administrative or statutory revision of their defined scopes of practice (a costly and often difficult enterprise).
As the health care system has grown over the past 40 years, the education and roles of APRNs have continually evolved so that nurses now enter the workplace willing and qualified to provide more services than they previously did. As the services supported by evolving education programs expanded, so did the overlap of practice boundaries of APRNs and physicians. APRNs are more than physician extenders or substitutes. They cover the care continuum from health promotion and disease prevention to early diagnosis to prevent or limit disability. These services are grounded in and shaped by their nursing education, with its particular ideology and professional identity. NPs also learn how to work with teams of providers, which is perhaps one of the most important factors in the successful care of chronically ill patients. Although they use skills traditionally residing in the realm of medicine, APRNs integrate a range of skills from several disciplines, including social work, nutrition, and physical therapy.
Almost 25 years ago, an analysis by the Office of Technology Assessment (OTA) indicated that NPs could safely and effectively provide more than 90 percent of pediatric primary care services and 75 percent of general primary care services, while CRNAs could provide 65 percent of anesthesia services. OTA concluded further that CNMs could be 98 percent as productive as obstetricians in providing maternity services (Office of Technology Assessment, 1986). APRNs also have competencies that include the knowledge to refer patients with complex problems to physicians, just as physicians refer patients who need services they are not trained to provide, such as medication counseling, developmental screening, or case management, to APRNs. As discussed in Chapter 1 and reviewed in Annex 1-1, APRNs provide services, in addition to primary care, in a wide range of areas, including neonatal care, acute care, geriatrics, community health, and
psychiatric/mental health. Most NPs train in primary care; however, increasing numbers are being trained in acute care medicine and other specialty disciplines (Cooper, 1998).
The growing use of APRNs and physician assistants has helped ease access bottlenecks, reduce waiting times, increase patient satisfaction, and free physicians to handle more complex cases (Canadian Pediatric Society, 2000; Cunningham, 2010). This is true of APRNs in both primary and specialty care. In orthopedics, the use of APRNs and physician assistants is a long-standing practice. NPs and physician assistants in gastroenterology help meet the growing demand for colon cancer screenings in either outpatient suites or hospital endoscopy centers. Because APRNs and physician assistants in specialty practice typically collaborate closely with physicians, legal scope-of-practice issues pose limited obstacles in these settings.
Variation in Nurse Practitioner Scope-of-Practice Regulations
Regulations that define scope-of-practice limitations vary widely by state. In some states, they are very detailed, while in others, they contain vague provisions that are open to interpretation (Cunningham, 2010). Some states have kept pace with the evolution of the health care system by changing their scope-of-practice regulations to allow NPs to see patients and prescribe medications without a physician’s supervision or collaboration. However, the majority of state laws lag behind in this regard. As a result, what NPs are able to do once they graduate varies widely across the country for reasons that are related not to their ability, their education or training, or safety concerns (Lugo et al., 2007) but to the political decisions of the state in which they work. For example, one group of researchers found that 16 states plus the District of Columbia have regulations that allow NPs to see primary care patients without supervision by or required collaboration with a physician (see Figure 3-3). As with any other primary care providers, these NPs refer patients to a specialty provider if the care required extends beyond the scope of their education, training, and skills.
Other legal practice barriers include on-site physician oversight requirements, chart review requirements, and maximum collaboration ratios for physicians who collaborate with more than a single NP. See Safriet (2010, Appendix H on the CD-ROM in the back of this book) for further discussion of inconsistencies in the regulation of NP practice at the state level.
There are fundamental contradictions in this situation. Educational standards—which the states recognize—support broader practice by all types of APRNs. National certification standards—which most states also recognize—likewise support broader practice by APRNs. Moreover, the contention that APRNs are less able than physicians to deliver care that is safe, effective, and efficient is not supported by the decades of research that has examined this question (Brown and Grimes, 1995; Fairman, 2008; Groth et al., 2010; Hatem et al.,
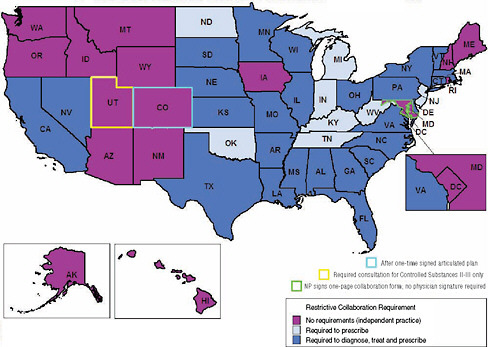
FIGURE 3-3 Requirements for physician–nurse collaboration, by state, as a barrier to access to primary care.
NOTE: Collaboration refers to a mutually agreed upon relationship between nurse and physician.
SOURCE: AARP, 2010b. Courtesy of AARP. All rights reserved. This figure combines Map 1, Overview of Diagnosing and Treating Aspects of NP Practice and Map 2, Overview of Prescribing Aspects of NP Practice, both developed by Linda Pearson (2010).
2008; Hogan et al., 2010; Horrocks et al., 2002; Hughes et al., 2010; Laurant et al., 2004; Mundinger et al., 2000; Office of Technology Assessment, 1986). No studies suggest that care is better in states that have more restrictive scope-of-practice regulations for APRNs than in those that do not. Yet most states continue to restrict the practice of APRNs beyond what is warranted by either their education or their training.
Depending on the state, restrictions on an APRN’s scope of practice may limit or prohibit the authority to prescribe medications, admit patients to hospitals, assess patient conditions, and order and evaluate tests. Box 3-1 provides an example of the variation in state licensure regulations, detailing examples of the services an APRN would not be permitted to provide if she practiced in a more restrictive state (Safriet, 2010). In addition to variations among states, the scope of practice for APRNs in some cases varies within a state by geographic location of the practice within the state or nature of the practice setting.
|
BOX 3-1* Variation in State Licensure Regulations Several states permit APRNs to provide a broad list of services, such as independently examining patients, ordering and interpreting laboratory and other tests, diagnosing and treating illness and injury, prescribing indicated drugs, ordering or referring for additional services, admitting and attending patients in a hospital or other facility, and directly receiving payment for services. In other states, however, those same APRNs would be prohibited from providing many of these services. The following list provides examples of restrictions that APRNs face in states that have adopted more restrictive scope-of-practice regulations. These restrictions could greatly limit the ability of APRNs to fully utilize their education and training. Examination and Certification A nurse may not examine and certify for:
Referrals and Orders A nurse may not refer for and order:
|
|
Examination and Treatment A nurse may not:
Prescriptive Authority A nurse may not:
|
Compensation A nurse may not be:
|
Current laws are hampering the ability of APRNs to contribute to innovative health care delivery solutions. Some NPs, for example, have left primary care to work as specialists in hospital settings (Cooper, 2007), although demand in those settings has also played a role in their movement. Others have left NP practice altogether to work as staff RNs. For example, restrictive state scope-of-practice regulations concerning NPs have limited expansion of retail clinics, where NPs provide a limited set of primary care services directly to patients (Rudavsky et al., 2009). Similarly, the roles of NPs in nurse-managed health centers and patient-centered medical homes can be hindered by dated state practice acts.
Credentialing and payment policies often are linked to state practice laws. A 2007 survey of the credentialing and reimbursement policies of 222 managed care organizations revealed that 53 percent credentialed NPs as primary care providers; of these, 56 percent reimbursed primary care NPs at the same rate as primary care providers, and 38 percent reimbursed NPs at a lower rate (Hansen-Turton et al., 2008). Rationales stated by managed care staff for not credentialing NPs as primary care providers included the fact that NPs have to bill under a physician’s provider number, NPs do not practice in physician shortage areas, NPs do not meet company criteria for primary care providers, state law does not require them to credential NPs, and the National Committee for Quality Assurance (NCQA) accreditation process prevents them from recognizing NPs as primary care provider leads in medical homes. As discussed above, some states require NPs to be supervised by physicians in order to prescribe medications, while others do not. In this survey, 71 percent of responding insurers credentialed NPs as primary care providers in states where there was no requirement for physicians to supervise NPs in prescribing medications. In states that required more physician involvement in NP prescribing, insurers were less likely to credential
A nurse may:
|
NPs. Of interest, this was the case even though the actual level of involvement by the physician may be the same in states where supervision is required as in states where it is not. Also of note is that Medicaid plans were more likely than any other category of insurer to credential NPs.
Although there is a movement away from a fee-for-service system, Table 3-2 shows the current payment structure for those providing primary care.
The Federal Government and Regulatory Reform16
Precisely because many of the problems described in this report are the result of a patchwork of state regulatory regimes, the federal government is especially well situated to promote effective reforms by collecting and disseminating best practices from across the country and incentivizing their adoption. The federal government has a compelling interest in the regulatory environment for health care professions because of its responsibility to patients covered by federal programs such as Medicare, Medicaid, the VA, and the Bureau of Indian Affairs. Equally important, however, is the federal government’s responsibility to all American taxpayers who fund the care provided under these and other programs to ensure that their tax dollars are spent efficiently and effectively. Federal actors already play a central role in a number of areas that would be essential to effective reform of nursing practice, especially that of APRNs. They pay for the majority of health care services delivered today, they pay for research on the safety and effectiveness of existing and innovative practice models and encourage
TABLE 3-2 Medicare Claims Payment Structure by Provider Type
|
Provider |
Office Services |
Hospital Services |
Incident to a Physician’s Servicesa |
Surgery Services |
Medicare Provider ID |
Direct Reimbursement |
|
Physician |
100% of physician fee |
100% of physician fee |
N/A |
Usually receives a global fee |
Own provider ID required |
Physician or employer may be reimbursed directly |
|
Nurse practitioner (NP) |
85% of physician fee, 100% if billed “incident to”a in a physician’s office or clinic using MD’s provider ID |
Usually salaried; nursing costs are part of hospital payment |
100% of physician fee (must bill under the MD’s provider ID) |
Usually accounted for in surgeon’s global fee |
Own ID possible, but not required |
NP or employer may be reimbursed directly |
|
Certified nurse midwife (CNM) |
65% of physician feeb |
|
100% if billed “incident to” in a physician office or clinic using MD’s provider ID |
Usually accounted for in surgeon’s global fee |
Own ID possible, but not required |
CNM or employer may be reimbursed directly |
|
Physician assistant (PA) |
Lesser of the actual charge or 85% of physician fee |
Lesser of the actual charge or 75% of physician fee |
100% if billed “incident to” in a physician office or clinic using MD’s provider ID |
Use assistant surgeon modifier |
Own ID required |
Only employer can be reimbursed directly |
|
a“Incident to” is used by Medicare to denote cases in which work is performed under the direction and supervision of a physician. Criteria for “incident to” billing require that the physician be on site (in the suite of offices) at the time the service is performed, that the physician treat the patient on the patient’s first visit to the office, and that the service be within the NP scope of practice in the state. bCNM payment will increase to 100 percent of physician fee as of January 1, 2011. SOURCE: Chapman et al., 2010. Copyright © 2010 by the authors. Reprinted by permission of SAGE Publications. |
||||||
their adoption, and they have a compelling interest in achieving more efficient and value-driven health care services. The federal government also appropriates substantial funds for the education and training of health care providers, and it has an understandable interest in ensuring that the ever-expanding skills and abilities acquired by graduates of these programs are fully utilized for the benefit of the American public.
In particular, the Federal Trade Commission (FTC) has a long history of targeting anticompetitive conduct in health care markets, including restrictions on the business practices of health care providers, as well as policies that could act as a barrier to entry for new competitors in the market. The FTC has responded specifically to potential policies that might be viewed predominantly as guild protection rather than consumer protection, for example, taking antitrust actions against the American Medical Association (AMA) for policies restricting access to clinical psychologists to cases referred by a physician and for ethical prohibitions on collaborating with chiropractors, podiatrists, and osteopathic physicians. In 2008, the FTC evaluated proposed laws in Massachusetts, Illinois, and Kentucky, finding that several provisions could be considered anticompetitive, including limits on advertising, differential cost sharing, more stringent physician supervision requirements, restrictions on clinic locations and physical configurations or proximity to other commercial ventures, and limits on the scope of professional services that can be provided that are not applicable to professionals with similar credentials who practice in similar “limited care settings” (for example, urgent care centers) (DeSanti et al., 2010; Ohlhausen et al., 2007, 2008). Likewise, the FTC initiated an administrative complaint against the North Carolina Board of Dental Examiners in June 2010 (FTC, 2010). The Board had prohibited nondentists from providing teeth-whitening services. The FTC alleged that by doing this the Board had hindered competition and made it more difficult and costly for consumers in the state to obtain this service.
As a payer and administrator of health insurance coverage for federal employees, the Office of Personnel Management (OPM) and the Federal Employees Health Benefits program have a responsibility to promote and ensure employee/subscriber access to the widest choice of competent, cost-effective health care providers. Principles of equity would suggest that this subscriber choice would be promoted by policies ensuring that full, evidence-based practice is permitted for all providers regardless of geographic location.
Finally, the Centers for Medicare and Medicaid Services (CMS) has the responsibility to promulgate rules and policies that promote access of Medicare and Medicaid beneficiaries to appropriate care. CMS therefore should ensure that its rules and polices reflect the evolving practice abilities of licensed providers, rather than relying on dated definitions drafted at a time when physicians were the only authorized providers of a wide array of health care services.
Expanding Scopes of Practice for Nurses
For several decades, the trend in the United States has been toward expansion of scope-of-practice regulations for APRNs, but this shift has been incremental and variable. Most recently, the move to expand the legal authority of all APRNs to provide health care that accords with their education, training, and competencies appears to be gathering momentum. In 2008, after 5 years of study, debate, and negotiation, a group of nursing accreditation, certification, and licensing organizations, along with several APRN groups, developed a consensus model for the education, training, and regulation of APRNs (see Appendix D). The stated goals of the APRN consensus process are to:
-
“strive for harmony and common understanding in the APRN regulatory community that would continue to promote quality APRN education and practice;
-
develop a vision for APRN regulation, including education, accreditation, certification, and licensure;
-
establish a set of standards that protect the public, improve mobility, and improve access to safe, quality APRN care; and
-
produce a written statement that reflects consensus on APRN regulatory issues” (see Appendix D).
The consensus document will help schools and programs across the United States standardize the education and preparation of APRNs. It will also help state regulators establish consistent practice acts because of education and certification standardization. And of importance, this document reflects the consensus of nursing organizations and leaders and accreditation and certification boards regarding the need to eliminate variations in scope-of-practice regulations across states and to adopt regulations that more fully recognize the competence of APRNs.
In March 2010, the board of directors of AARP concluded that statutory and regulatory barriers at the state and federal levels “are short-changing consumers.” Acknowledging that nurses, particularly APRNs, can provide much of the care that Americans need and that barriers to their doing so must be lifted, the organization updated its policy on scope of practice. AARP states that “the policy change allows us to work together to ensure that our members and all health care consumers, especially in underserved settings such as urban and rural communities, have increased access to high quality care.” The amended policy reads as follows:
Current state nurse practice acts and accompanying rules should be interpreted and/or amended where necessary to allow APRNs to fully and independently practice as defined by their education and certification. (AARP, 2010a)
Meanwhile, after passage of the ACA, 28 states began considering expanding their scope-of-practice regulations for NPs (Johnson, 2010). Expanding the scope
of practice for NPs is particularly important for the rural and frontier areas of the country. Twenty-five percent of the U.S. population lives in these areas; however, only 10 percent of physicians practice in these areas (NRHA, 2010). People who live in rural areas are generally poorer and have higher morbidity and mortality rates than their counterparts in suburban and urban settings, and they are in need of a reliable source of primary care providers (NRHA, 2010). The case study in Box 3-2, describing an NP in rural Iowa, demonstrates the benefits of a broad scope of practice with respect to the quality of and access to care.
Scope of Practice for Non-APRN Nurses
Generalist nurses are expanding their practices across all settings to meet the needs of patients. Expansions include procedure-based skills (involving, for example, IVs and cardiac outputs), as well as clinical judgment skills (e.g., taking health histories and performing physical examinations to develop a plan of nursing care). According to Djukic and Kovner (2010), there has been “no formal examination of the impact of RN role expansion on care cost or on physician and RN workload.” The authors describe the expansion as a shifting of skills and activities, which in the long run, given the physician shortage, could free up physician resources, especially in long-term care, community health, and school-based health. On the other hand, given the projected nursing shortage, task shifting to overworked nurses could create unsafe patient care environments, especially in acute care hospitals. To avert this situation, nurses need to delegate to others, such as LPNs, nursing assistants, and community health workers, among others. A transformed nursing education system that is able to respond to changes in science and contextual factors, such as population demographics, will be able to incorporate needed new skills and support full scopes of practice for non-APRNs to meet the needs of patients (see Chapter 4).
Professional Resistance
Increasing access to care by expanding state scope-of-practice regulations so they accord with the education and competency of APRNs is a critical and controversial topic. Practice boundaries are constantly changing with the emergence of new technologies, evolving patient expectations, and workforce issues. Yet the movement to expand scopes of practice is not supported by some professional medical organizations. Professional tensions surrounding practice boundaries are not limited to nurses and physicians, but show a certain continuity across many disciplines. Psychiatrists and psychologists have been disagreeing about prescriptive privileges for more than two decades (Daly, 2007). In the dental field, one new role, the advanced dental hygiene practitioner, functions under a broadened scope similar to that of an APRN. The American Dental Association does not
Evidence that it is safe to remove restrictions on APRNs comes from an annual review of state laws and regulations governing APRNs that now includes malpractice claims in its analysis. The 2010 Pearson Report documents no increase in claims registered in the Healthcare Integrity and Protection Data Bank in states where APRNs have full authority to practice and prescribe independently. The report also notes that the overall ratio of claims against NPs is 1 for every 166 NPs in the nation, compared with 1 for every 4 physicians (Pearson, 2010). In June 2010 President Barack Obama addressed the House of Delegates of the American Nurses Association to announce “a number of investments to expand the primary care workforce.” These included increased funding for NP students and for nurse- and NP-run clinics—two important steps, the President said, in “a larger effort to make our system work better for nurses and for doctors, and to improve the quality of care for patients” (White House, 2010).  A mother brings her son for an appointment with nurse practitioner Cheryll Jones, who provides high-quality care in the rural community of Ottumwa, IA. |
recognize this new type of practitioner as an independent clinician, but mandates that all dental teams be headed by a professional dentist (Fox, 2010). Likewise, physical therapists are challenging traditional scope-of-practice boundaries established by chiropractors (Huijbregts, 2007).
Physician Challenges to Expanded Scope of Practice
The AMA has consistently issued resolutions, petitions, and position papers supporting opposition to state efforts to expand the scope of practice for professional groups other than physicians.17 The AMA’s Citizens Petition, submitted to the Health Care Financing Administration in June 2000, and the AMA-sponsored Scope of Practice Partnership (SOPP), announced in January 2006, both focused on opposing scope-of-practice expansion. The SOPP in particular, an alliance of the AMA and six medical specialty organizations, was an effort on the part of organized medicine to oppose boundary expansion and to defeat proposed legislation in several states to expand scope of practice for allied health care providers, including nurses (Croasdale, 2006; Cys, 2000).
The SOPP, with the assistance of a special full-time legislative attorney hired for the purpose, spearheaded several projects designed to obstruct expansion of scopes of practice for nurses and others. These projects included comparisons between the medical profession and specific allied health professions on education standards, certification programs, and disciplinary processes; development of evidence to discredit access-to-care arguments made by various allied health professionals, particularly in rural areas of a state; and identification of the locations of physicians by specialty to counter claims of a lack of physicians in certain areas (Cady, 2006). One of the policies pursued by the SOPP is the AMA’s 2006 resolution H-35.988,18 Independent Practice of Medicine by “Nurse Practitioners.” This resolution opposes any legislation allowing the independent practice of medicine by individuals who have not completed state requirements to practice medicine.
The AMA has released a set of 10 documents for members of state medical associations to help them explain “to regulators and legislators the limitations in the education and training of non-physician providers” (AMA, 2009). One of these, the AMA Scope of Practice Data Series: Nurse Practitioners, uses the term “limited licensure health care providers.” The document argues that these providers—NPs—seek scope-of practice expansions that may be harmful to the public (AMA, 2009). Other organizations, such as the American Society of Anesthesiologists and the American Association of Family Physicians (AAFP), have also issued statements that do not support nurses practicing to their fullest
ability (ASA, 2004), although the AAFP supports nurses and physicians working together in collaborative teams (Phillips et al., 2001). The AAFP recently released a press packet—a “nurse practitioner information kit.”19 The kit includes a set of five papers and a new piece of legislation “clarifying” why NPs cannot substitute for physicians in primary care, although as Medicare and Medicaid data show, they already are doing so. There are also new guidelines on how to supervise CNMs, NPs, and physician assistants. The AAFP notes that its new proposed legislation, the Health Care Truth and Transparency Act of 2010, “ensures that patients receive accurate health care information by prohibiting misleading and deceptive advertising or representation of health care professionals’ credentials and training.” The legislation is also endorsed by 13 other physician groups.
Action has been taken at the state level as well. For example, in 2010, the California Medical Association (CMA) and the California Society of Anesthesiologists (CSA) sued the state of California after Governor Schwarzenegger decided to opt out of a Medicare provision requiring physician supervision of CRNAs (Sorbel, 2010). At the time of release of this report, the case had not yet been heard.
Reasons for Physician Resistance
The CMA and CSA both cited patient safety as the reason for protesting the governor’s decision—although evidence shows that CRNAs provide high-quality care to California citizens, there is no evidence of patient harm from their practice, and 14 other states have taken similar opt out actions (Sorbel, 2010). A study by Dulisse and Cromwell (2010) found no increase in inpatient mortality or complications in states that opted out of the CMS requirement that an anesthesiologist or surgeon oversee the administration of anesthesia by a CRNA. As noted earlier in this chapter, the contention that APRNs are less able than physicians to deliver care that is safe, effective, and efficient is not supported by research that has examined this question (Brown and Grimes, 1995; Fairman, 2008; Groth et al., 2010; Hatem et al., 2008; Hogan et al., 2010; Horrocks et al., 2002; Hughes et al., 2010; Laurant et al., 2004; Mundinger et al., 2000; Office of Technology Assessment, 1986).
Some physician organizations argue that nurses should not be allowed to expand their scope of practice, citing medicine’s unique education, clinical knowledge, and cognitive and technical skills. Opposition to this expansion is particularly strong with regard to prescriptive practice. However, evidence does not support an association between a physician’s type and length of preparation and the ability to prescribe correctly and accurately or the quality of care (Fairman, 2008). Similar questions have been raised about the content of nursing education (see the discussion of nursing curricula in Chapter 4).
Support for Expanded Scope of Practice for Nurse Practitioners
Some individual physicians support expanded scope of practice for NPs. The Robert Wood Johnson Foundation Nursing Research Network (described in Appendix A) conducted a survey of 100 physician members of the online physician site Sermo.com20 and found that more than 50 percent of respondents agreed either somewhat or strongly that “allowing NPs to practice independently would increase access to primary care in the U.S.” (RWJF, 2010e). As Figure 3-4 shows, however, physicians were more skeptical that expanding NPs’ scope of practice in this way would decrease costs, and they feared a decrease in average quality of care provided to patients.
In addition to support for expanded scope of practice for NPs among some physicians, public support for NP practice is indicated by satisfaction ratings for retail-based health clinics. Approximately 95 percent of providers in these clinics are NPs, with the remaining 5 percent comprising physician assistants and some physicians.21 According to a survey of U.S. adults by the Wall Street Journal.com/Harris Interactive (Harris Interactive, 2008), almost all respondents who had used a retail-based health clinic (313 total) were very or somewhat satisfied with the quality of care, cost, and staff qualifications (see Figure 3-5). Such public support can be backed up with high-quality clinical outcomes (Mehrotra et al., 2008).
Despite opposition by some physicians and specialty societies, the strong trend over the past 20 years has been a growing receptivity on the part of state legislatures to expanded scopes of practice for nurses. There simply are not enough primary care physicians to care for an aging population now, and their patient load will dramatically increase as more people gain access to care. For example, in 2007 Pennsylvania Governor Edward Rendell announced a blueprint for reform, known as Prescription for Pennsylvania (Rx for PA), to promote access to care for the state’s residents and reduce health care expenses (see the case study in Chapter 5). One initiative under Rx for PA was expanding the legal scope of practice for physician assistants, APRNs, CNSs, CNMs, and dental hygienists. This initiative has had an important impact on access to care. Outcome data after the first year of Rx for PA show an increase in the number of people with diabetes receiving eye and foot examinations and a doubling of the number of children with asthma who have a plan in place for controlling exacerbations (Pennsylvania Governor’s Office, 2009).
The experience of states that have led these changes offers important reas-
|
20 |
Sermo.com respondents are all members of the online community sermo.com. Sermo.com members are distributed across age, gender, geography, and specialty groups in patterns that mimic those of the U.S. population. For this study, respondents were randomly recruited to participate in the IOM survey activity via e-mail; others were allowed to join the survey by volunteering when they visited the site. The majority of respondents have specialties in cardiology (6 percent), family medicine (35 percent), internal medicine (26 percent), and oncology (4 percent). The remaining physicians surveyed are distributed across a wide range of specialties. |
|
21 |
Personal communication, Tine Hansen-Turton, CEO, National Nursing Centers Consortium, and Vice President, Public Health Management Corporation, August 6, 2010. |
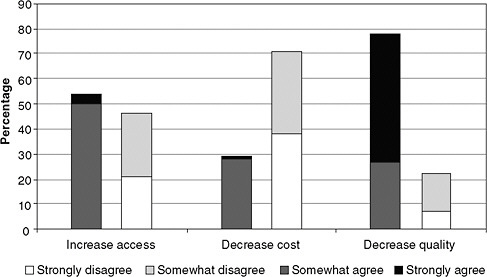
FIGURE 3-4 Physician opinions about the impact of allowing nurse practitioners to practice independently.
SOURCE: RWJF, 2010d. Reprinted with permission from Lori Melichar, RWJF.
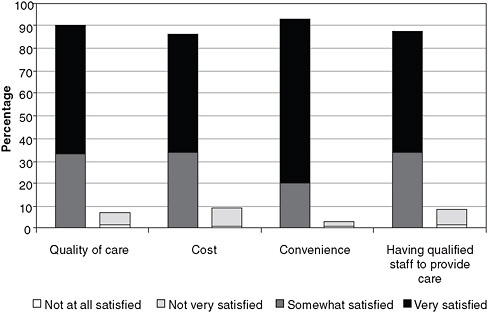
FIGURE 3-5 Patient satisfaction with retail-based health clinics.
NOTES: Question asked: Overall, how satisfied were you with your or your family member’s experience using an onsite health clinic in a pharmacy or retail chain on the following items?
Percentages may not add up to 100 because of the small percentage not included here that chose “not sure.”
SOURCE: Harris Interactive, 2008.
surance to physicians who continue to believe that patient care may be adversely affected, or that expanded nursing practice autonomy threatens the professional and economic roles of physicians. States with broader nursing scopes of practice have experienced no deterioration of patient care. In fact, patient satisfaction with the role of APRNs is very high. Nor has expansion of nursing scopes of practice diminished the critical role of physicians in patient care or physician income (Darves, 2007). With regard to the quality of care and the role of physicians, it is difficult to distinguish states with restrictive and more expanded scopes of practice. Finally, the committee believes that the new medical home concept, based on professional collaboration, represents a perfect opportunity for nurses and physicians to work together for the good of patient care in their community.
Fragmentation of the Health Care System
The U.S. health care system is characterized by a high degree of fragmentation across many sectors, which raises substantial barriers to building value. A fragmented health care system is characterized by weak connections among multiple component parts. Fragmentation makes simple tasks—such as assigning responsibility for payment—much more difficult than they need to be, while more complex tasks—such as coordination of home health care, family support, transportation, and social services after a hospital stay—become more difficult because they require following many separate sets of often contradictory rules. As a result, people may simply give up trying rather than take advantage of the services to which they are entitled. An examination of fragmentation in hospital services explores its origins in American pluralism, historical accident, and the hybridization of business and charity (Stevens, 1999). A review by Cebul and colleagues identifies three broad areas of fragmentation: (1) the U.S. health insurance system; (2) the provision of care; and (3) the inability of health information systems to allow a “seamless flow of information between hospitals, providers and insurers” (Cebul et al., 2008).
In the United States, there is a disconnect between public and private services, between providers and patients, between what patients need and how providers are trained, between the health needs of the nation and the services that are offered, and between those with insurance and those without (Stevens, 1999). Communication between providers is difficult, and care is redundant because there is no means of sharing results. For example, a patient with diabetes covered by Medicaid may have difficulty finding a physician to help him control his blood sugar. If he is able to find a physician, that individual may not have admitting privileges at the hospital to which the patient is transported after a hypoglycemic reaction. After the patient has been admitted to the emergency room, a new cadre of physicians is responsible for him but has no information about previous blood sugar determinations, other medications he is taking, or other health problems. The patient is stabilized and a discharge is arranged, but he is
ineligible under his insurance plan for reimbursement for the further education in diet and glucose control, materials (such as a glucometer), and referral to an ophthalmologist that are indicated. Home follow-up is needed, but the visiting nurse agency is certified to provide only two visits when the patient could use five. No one calls the initial primary care physician to share discharge planning or information, and no one gives the patient a summary of the visit to take to that physician. The ophthalmologist will not accept the patient because of his status as a Medicaid recipient. A major challenge to repairing this fragmentation lies in the fee-for-service structure of the payment system, which indiscriminately rewards increasing volume of services regardless of whether it improves health outcomes or provides greater value (MedPAC, 2006).
Effect of Fragmentation on Realizing the Value of Nurses
Within this system, the contributions of nursing are doubly hidden. Accounting systems of most hospitals and health care organizations are not designed to capture or differentiate the economic value provided by nurses. Thus, all nursing care is treated equally in its effect on revenue. A 2007 review of 100 demonstration projects that provided incentives for high-value care to hospitals and physicians found no examples that specifically delineated or rewarded nurses’ contributions (Kurtzman et al., 2008). Yet nurses’ work is estimated to vary by 15 to 40 percent for any given diagnosis-related group (Laport et al., 2008). The effect on the provision of health care is difficult to document, but a closer look at staffing ratios suggests some of the consequences. Generally speaking, as an analysis by the Lewin Group concludes, because health care facilities cannot capture the full economic value of the services nurses provide, they have an economic incentive—whether they decide to heed it or not—to staff their organizations “at levels below where the benefit to society equals the cost to employ an additional nurse” (Dall et al., 2009).
Barriers to measuring and realizing the economic value generated by nurses exist outside the hospital setting as well. In many states, APRNs are not paid directly but must be reimbursed through the physician with whom they have a collaboration agreement. Payments are funneled through the physician provider number, and the nurse is salaried.
For years, professional nursing organizations have sought to counter the inequitable aspects of the fee-for-service payment system by lobbying to increase the types of services for which NPs can independently bill Medicare, Medicaid, and other providers. They have had some success in that regard in the past (Sullivan-Marx, 2008). However, according to Mark McClellan and Gail Wilensky, both former directors of CMS, this approach has become a losing proposition. As McClellan and Wilensky testified to the committee in September 2009, while fee-for-service is not going to disappear any time soon, its future is severely limited in any sustainable health care system.
Proposals to Address Fragmentation
Alternative proposals for financing the health care system have coalesced around the idea of providing “global payments” that are shared among a predetermined group of providers, such as hospitals, physicians, nurses, social workers, nutritionists, and other professionals, and “bundled payments” that are linked to a single episode of care, such as treatment of and recovery from a heart attack. A full exploration of all the benefits and caveats of such alternative payment proposals is beyond the scope of this report. However, as the Medicare Payment Advisory Commission (MedPAC) noted in its June 2008 report to Congress, “[b]undling payment raises a range of implementation issues because under bundled payment the entity accepting the payment—rather than Medicare—has discretion in the amount it pays providers for care provided, whether to pay for services not now covered by Medicare, and how it rewards providers for reducing costs and improving quality” (MedPAC, 2008). It will be up to the entity accepting payment to determine how and indeed whether to valuate nurses’ contributions. Yet the tendency of human nature is to follow the practices and behaviors with which one is most familiar. Without the presence of nurses in decision-making positions in these new entities, the legacy of undervaluing nurses, characteristic of the fee-for-service system, will carry over into whatever new payment schemes are adopted. The services of nurses must be properly and transparently valued so that their contributions can fully benefit the entire system.
Outdated Policies of Insurance Companies
As noted in Chapter 2, many NPs and CNMs have cared for underserved populations that are either uninsured or rely on Medicaid. Expanding their services to the private insurance market is another matter altogether. The health care reform experience of Massachusetts shows the extent to which corporate policy can negate government regulation. An estimated 5,600 NPs work in Massachusetts (Pearson, 2010), falling under the authority of the Commonwealth’s Board of Nursing as well as its Board of Medicine. NPs are required to collaborate with a physician and may prescribe drugs only under a written collaborative agreement with a physician (Christian et al., 2007). The law allows them to act as primary care providers (PCPs), and the Massachusetts Medicaid program formally named NPs as PCPs.
Despite the shortage of PCPs that occurred after the Massachusetts legislature enacted health care reform in 2006, no private insurance companies listed NPs as PCPs in Massachusetts. As a matter of policy, one major New England carrier stated that it would not list NPs as PCPs unless required to do so by the legislature. This same carrier, however, listed NPs as PCPs in its service directories for the neighboring states of New Hampshire and Maine. Eventually, Massachusetts passed a second health care reform law in 2008 that amended the
state’s insurance regulations to recognize NPs as PCPs in the private as well as the public market. Massachusetts was thereby able to expand the supply of its PCPs without changing its scope-of-practice laws (Craven and Ober, 2009). The policy differences among states may have to do with different scope-of-practice regulations or differences in the states’ insurance industries. There is some evidence that insurers are more likely to recognize NPs as PCPs in states where NPs have independent practice authority (Hansen-Turton et al., 2008).
The actions of private insurance companies toward APRNs are having an effect on government-funded programs as well. Nurse-managed health centers (NMHCs) have long provided care for populations served by Medicare, Medicaid, and children’s health insurance programs. However, federal and state governments are increasingly turning to the private sector to manage these programs (Hansen-Turton et al., 2006). The insurance companies’ continued policy of not credentialing and/or recognizing NPs as PCPs—and the federal government’s refusal to mandate that they do so—creates a barrier for NMHCs as they seek to continue serving these populations (Hansen-Turton et al., 2006).
One specific model of the medical/health home—the Patient-Centered Medical Home™ (PCMH)—does not permit management by nurses. In other words, a nurse may manage an organization that in every way adheres to the principles of PCMHs, but the practice will not be recognized as a PCMH by NCQA, a “not-for-profit organization dedicated to improving health care quality” (NCQA, 2010). Without public recognition, nurse-led medical/health homes cannot qualify for insurance reimbursement, which in turn leaves substantial populations underserved. NCQA, which administers the recognition for the medical homes, is a physician-dominated organization receiving its member dues from physicians. Its board, although currently reconsidering its stance on whether NPs can lead medical homes, has decided that physicians are more able to serve in PCMH leadership positions. The original concept for the medical home came from physicians, and NCQA adopted their principles of operation.22 Several state agencies have contacted NCQA to request that it recognize NPs’ ability to lead PCMHs. NCQA has appointed an advisory committee to review the policy that medical homes must be physician led. Meanwhile, the Joint Commission is developing a competitive certification program that will allow for leadership by NPs.23
High Turnover Rates
As the health care system undergoes transformation, it will be imperative that patients have highly competent nurses who are adept at caring for them across all settings. It will be just as important that the system have enough nurses at any
given time. Both having enough nurses and having the right kind of highly skilled nurses will contribute to the overall safety and quality of a transformed system. Although the committee did not focus solely on the upcoming shortage of nurses, it did devote time to considering how to retain experienced nurses and faculty.
Some solutions have been researched, proposed, and reproposed for so long that it is difficult to understand why they have not yet been implemented more widely. High turnover rates continue to destabilize the nurse workforce in the United States and other countries (Hayes et al., 2006). Figure 3-6 indicates some of the reasons that have been cited for not working in the nursing profession. For nurses under 50, personal or family reasons were most frequently cited.
The costs associated with high turnover rates are significant, particularly in hospitals and nursing homes (Aiken and Cheung, 2008). The literature shows that the workplace environment plays a major role in nurse turnover rates (Hayes et al., 2006; Tai et al., 1998; Yin and Yang, 2002). Staff shortages, increasing work-
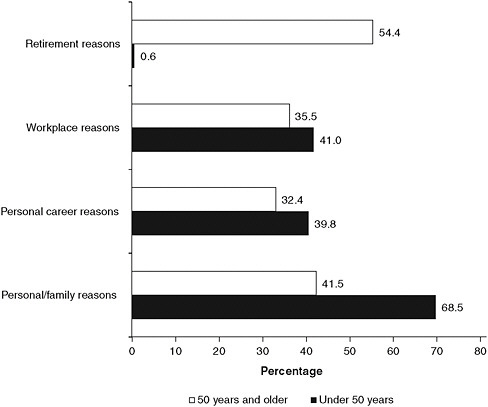
FIGURE 3-6 Reasons cited for not working in nursing, by age group.
NOTES: Percents do not add to 100 because registered nurses may have provided more than one reason. Includes only RNs who are not working in nursing.
SOURCE: HRSA, 2010.
loads, inefficient work and technology processes, and the absence of effective pathways for nurses to propose and implement improvements all have a negative impact on job satisfaction and contribute to the decision to leave. Tables 3-3 and 3-4, respectively, show the intentions of nurses with regard to their employment situation (e.g., plan to leave current job) and the percentage of nurses who left their job in 2007–2008, by setting. New research has also highlighted the contribution to the problem of disruptive behavior—ranging from verbal abuse to physical assault or sexual harassment of nurses, often by physicians but also by other nurses (Rosenstein and O’Daniel, 2005, 2008). For more than a quarter century, blue ribbon commissions and policy experts have concluded that wide-reaching changes in nurses’ practice environments would significantly reduce their high turnover rates and improve productivity (Aiken and Cheung, 2008).
Many individual facilities and programs have adopted those recommenda-
TABLE 3-3 Plans Regarding Nursing Employment, by Graduation Cohort, 2008
|
Plans |
Graduated before 2001 (%) |
Graduated 2001–2008 (%) |
|
Plans regarding current position |
|
|
|
No plans to leave job |
57.8 |
42.8 |
|
Undecided about plans |
15.1 |
17.8 |
|
Have left job or plan to leave in 12 months |
14.5 |
23.2 |
|
Plan to leave in 1 to 3 years |
12.6 |
16.2 |
|
Total that plan to leave within 3 years |
27.1 |
39.3 |
|
For those who plan to leave their job |
|
|
|
Plan to remain in nursing work |
77.9 |
96.7 |
|
Plan to leave nursing |
22.1 |
3.3 |
|
SOURCE: HRSA, 2010. |
||
TABLE 3-4 Changes in Position Setting, by 2007 Setting, for Registered Nurses Who Graduated in 2001–2008
|
Setting in 2007 |
Percent Who Left Setting Between 2007 and 2008 |
|
Hospital |
11.1 |
|
Nursing home/extended care |
25.8 |
|
Home health |
21.2 |
|
Public/community health |
23.2 |
|
Ambulatory care |
20.8 |
|
Other |
18.9 |
|
NOTES: Public/community health includes school health and occupational health. Other settings include academic education and insurance/benefits/utilization review. SOURCE: HRSA, 2010. |
|
tions. Much of the data showing the impact of reducing turnover by focusing on workplace environment comes from the acute care setting. Nonetheless, these data are instructive in their demonstration of a triple win: improving the workplace environment reduces nurse turnover, lowers costs, and improves health outcomes of patients. For example, the Transforming Care at the Bedside (TCAB) initiative is a national program that engages nurses to lead process improvement efforts so as to improve health outcomes for patients, reduce costs, and improve nurse retention (Bolton and Aronow, 2009). TCAB relies on nurses developing small tests of change that are continuously planned, assessed, and rapidly adopted or dropped, with each round building on previous successes. According to Bolton and Aronow (2009), as the TCAB principles and locally proposed and tested interventions spread throughout Cedars-Sinai Hospital, administrators noted the emergence of “a culture that emphasizes performance improvement and value-adding activities on nursing units.” Physician–nurse rounding, physician–nurse education teams, recognition programs, and collaborative efforts of nursing staff with other, non-nursing departments were the major reason, the authors believe, behind a decrease in nurse turnover rates from 7 percent in 2004 to 3 percent in 2008.
Some employers have also discovered that making it easier for nurses to obtain advanced degrees while continuing to work has increased retention rates. Chapter 4 includes an example of this phenomenon from the Carondelet Health Network in Tucson, Arizona. Based on workforce data Carondelet regularly collects for use in its strategic planning, the network has concluded that its educational efforts have had a positive effect on recruiting and retention. Its percentage of staff (as opposed to contract) nurses has increased from 81.7 to 89.2 percent. Because so many newly graduated nurses have begun seeking work at Carondelet, the average age of its staff nurses fell from 50 years in 2004 to 45.2 years in 2007 (The Lewin Group, 2009).
Difficulties of Transition to Practice
High turnover rates among newly graduated nurses highlight the need for a greater focus on managing the transition from school to practice (Kovner et al., 2007). Some turnover is to be expected—and is even appropriate if new nurses discover they are not really suited to the care setting or employer they have chosen. However, some entry-level nurses who leave first-time hospital jobs leave the profession entirely, a situation that needs to be avoided when possible. In a 2007 survey of entry-level nurses, those who had already left their first job cited reasons such as poor management, stress, and a desire for experience in a different clinical area (Kovner et al., 2007).
In 2002, the Joint Commission recommended the development of nurse residency programs—planned, comprehensive periods of time during which nursing graduates can acquire the knowledge and skills to deliver safe, quality care that
meets defined (organization or professional society) standards of practice. This recommendation was most recently endorsed by the 2009 Carnegie study on the nursing profession (Benner et al., 2009). Versant24 and other organizations have launched successful transition-to-practice residency programs for nurses in recent years, while the University HealthSystem Consortium (UHC) and the American Association of Colleges of Nursing (AACN) have developed a model for postbaccalaureate nurse residencies (Goode and Williams, 2004; Krugman et al., 2006; Williams et al., 2007). The residency model developed by the UHC/AACN addresses needs identified by new nursing graduates and organizations that employ them. These needs included developing skills in ways to organize work and establish priorities; communicate with physicians, other professionals as well as patients and their families. In addition, nurses and employers indicated the need for nurses to develop leadership and technical skills in order to provide quality care (Beecroft et al., 2001, 2004; Halfer and Graf, 2006). As an example, in one hospital, the total cost for a residency program is $93,100, with a cost per resident of $2,023.91. Given that the average cost of replacing just one new graduate RN is $45,000, a return on investment can be significantly dependent on a reduction in RN turnover (AAN, 2010a).
The AACN has also adopted accreditation standards for these programs (AACN, 2008). Meanwhile, the National Council of State Boards of Nursing, after reviewing the evidence in favor of nursing residencies, has developed a regulatory model for transition-to-practice programs, recommending that state boards of nursing enforce a transition program through licensure (NCSBN, 2008).
Residencies Outside of Acute Care
Residency programs are supported predominantly in hospitals and larger health systems, with a focus on acute care. This has been the area of greatest need since most new graduates gain employment in acute care settings, and the proportion of new hires (and nursing staff) that are new graduates is rapidly increasing (Kovner et al., 2007). It is essential, however, that residency programs outside of acute care settings be developed and evaluated. Chapter 2 documents the demographic changes on the horizon; the shift of care from hospital to community-based settings; and the need for nursing expertise in chronic illness management, care of older adults in home settings, and transitional services. In this context, nurses need to be prepared for new roles outside of the acute care setting.
|
24 |
Versant is a nonprofit organization that provides, supervises, and evaluates nurse transition-to-practice residency programs for children’s and general acute care hospitals. See http://www.versant.org/item.asp?id=35. |
It follows that new types of residency programs appropriate for these types of roles need to be developed.25
Several community care organizations are already acting on their own perceived need for a residency-type program lasting 3 months or longer for new employees. At the Visiting Nurse Services of New York, nurses receive a great deal of education and training on the job. New nurses with a bachelor’s degree participate in an internship that provides hands-on experience and mentoring from experienced staff that prepares them for home-based nursing. “We really have to do a lot of our own education and training to compensate for the fact that most of the nurses don’t come with the experience, the competencies, or the comfort and confidence with technology that we think they need,” said Carol Raphael, the organization’s president and CEO (IOM, 2010a).
There are a few successful transition-to-practice initiatives in the field of public health, although they are commonly called internships, orientations, or mentoring programs. For example, the North Carolina State Health Department has begun a pilot effort with four public health departments in an effort to educate new nurses about population-based health. The 6-month mentoring program is being used as a recruitment and retention tool and has very explicit objectives, including an increase in retention and understanding of population health and a willingness to serve as a mentor as the program goes forward.26 Another successful community-based transition-to-practice program, called LEAP (Linking Education and Practice for Excellence in Public Health Nursing), was recently demonstrated in Milwaukee Wisconsin. Two public health departments and three community health centers not only collaborated to diversify the nurses entering public and community health settings, but also offered them paid traineeships to transition into their settings. The public health departments partnered with the Wisconsin Center for Nursing and a collaborative of five baccalaureate schools of nursing to first boost the community health curriculum in those schools and then help with the development of the internship upon graduation for 17 nurses. The program has been successful in recruiting more minorities into community and public health settings with the knowledge they need to practice successfully outside of the acute care setting. Financial support was secured from a variety of sources, including foundations, corporations, and partnership members themselves. The program is new and is currently undergoing an evaluation to deter-
|
25 |
This paragraph draws on a paper commissioned by the committee on “Transforming Pre-licensure Nursing Education: Preparing the New Nurse to Meet Emerging Health Care Needs,” prepared by Christine A. Tanner, Oregon Health & Science University School of Nursing (see Appendix I on CD-ROM). |
|
26 |
Personal communication, Joy Reed, Head, Public Health Nursing for the NC Division of Public Health, August 24, 2010. |
mine its financial sustainability.27 Such programs are not widespread, however, and need to be.
Evidence in Support of Residencies
Much of the evidence supporting the success of residencies has been produced through self-evaluations by the residency programs themselves. For example, Versant has demonstrated a profound reduction in turnover rates for new graduate RNs—from 35 to 6 percent at 12 months and from 55 to 11 percent at 24 months—compared with new graduate RN control groups hired at a facility prior to implementation of the residency program (Versant, 2010). Other research suggests residencies may be useful to help new graduates transition into practice settings (Goode et al., 2009; Krozek, 2008).
The UHC/AACN nurse residency program described above also reports reduced rates of turnover and cites cost savings to its participants. According to the UHC (2009) and AACN,28 since 2002 the program:
-
saved participating organizations over $6 million per year on the costs of turnover for a first-year nurse (the cost to recruit and retain a replacement nurse was estimated at $88,000);
-
increased its retention rate from 87 percent in 2004 to 94 percent in 2009;
-
increased stability in staffing levels, thereby reducing stress, improving morale, increasing efficiency, and promoting safety;
-
achieved a return on investment of up to 14:1; and helped first-year nurses in the program achieve the following:
-
develop their ability in clinical decision making,
-
develop clinical autonomy in providing patient care,
-
incorporate research-based evidence into their practices, and
-
increase commitment to nursing as a career.
-
The committee focused its attention on residencies for newly licensed RNs because these residencies have been most studied. Looking forward, however, the committee acknowledges the need for RNs with more experience to take part in residency programs as well. Such programs may be necessary to help nurses transition from, for example, the acute care to the community setting. As a growing number of nurses pursue advanced practice degrees immediately after receiving a bachelor’s degree—with no break between for employment in
a clinical setting—the benefit to APRNs of completing a residency is likely to grow as well. The committee believes that regardless of where the residency takes place—whether in the acute care setting or the community—nurses should be paid a salary, although the committee does not take a position on whether this should be a full or reduced salary. Loan repayment and educational debt should be postponed during residency, especially if a reduced salary is offered.
At the committee’s December 2009 Forum on the Future of Nursing: Care in the Community, Margaret Flinter, vice president and clinical director, Community Health Center, Inc., spoke about her organization’s decision to develop nurse residency programs for APRNs. The intensity and demands of providing service in the complex setting of a federally qualified health center (FQHC), Flinter testified, often discourage newly graduated NPs from joining an FQHC and the clinics from hiring newly graduated NPs. In 2006, she continued, her organization started the country’s first formal NP residency training program. The goal was to ensure that new NPs would find the training and transition support they needed to be successful as PCPs. The program is a 12-month, full-time, intensive residency that provides extensive precepting, specialty rotations, and additional didactic education in the high-risk/high-burden problems commonly seen in FQHCs. The NP residents are trained in a chronic care/planned care approach that features both prevention and chronic disease management, advance access to eliminate waits and delays, integrated behavioral health and primary care, and expert use of the electronic health record. In Flinter’s view and that of her organization, the initial year of residency training is essential to transitioning a new NP into a fully accountable PCP (Flinter, 2009). And indeed, the ACA allocates $200 million from 2012 to 2015 as part of a demonstration project that will pay hospitals for the costs of clinical training to prepare APRNs with the skills necessary to provide primary and preventive care, transitional care, chronic care management, and other nursing services appropriate for the Medicare population.
Residency provides a continuing opportunity to apply important knowledge for the purpose of remaining a safe and competent provider in a continuous learning environment. Paying for residencies is a challenge, but the committee believes that funds received from Medicare can be used to help with these costs. In 2006, about half of all Medicare nursing funding went to five states that have the most hospital-based diploma nursing programs (Aiken et al., 2009). The diploma programs in these states directly benefit from receiving these funds. Most states, however, and most hospitals do not receive Medicare funding for nursing education. The committee believes it would be more equitable to spread these funds more widely and use it for residency programs that would be valuable for all nurses across the country.
Demographic Challenges
As discussed in Chapter 2, the population of the United States is growing older and is becoming increasingly diverse in terms of race, ethnicity, and
language. To achieve the goal of increasing access to high-quality, culturally relevant care among the diverse populations in the United States, the nursing profession must increase its appeal to young people, men, and nonwhite racial/ethnic groups.
An Aging Workforce
Like the U.S. population, the nurse workforce continues to grow older. Over the past three decades, there has been a profound shift in the age composition of nurses. In 1983, approximately 50 percent (596,000 full-time equivalents [FTEs]) of the workforce was between the ages of 20 and 34, while only 17 percent (202,000 FTEs) was over the age of 50. Since the 1980s, the number of FTEs in the nursing workforce has doubled, and there has been a dramatic increase in the number of middle-aged and older RNs. From 1983 to 2009, the number of nurses over age 50 more than quadrupled, and the number of middle-aged nurses (aged 35–49) doubled to approximately 39 percent (977,000).These older and middleaged nurses now represent almost three-quarters of the nursing workforce, while nurses younger than 34 now make up only 26 percent (Buerhaus et al., 2009a). Figure 3-7 shows the age shift in the nursing workforce that has occurred over the past two decades.
The figure shows that since 1980, the nursing workforce has grown older, as reflected by more RNs reporting that they fall within the older age categories with each successive survey. At the same time, the figure indicates that in both 2004 and especially 2008, the number of young RNs in the workforce was growing relative to earlier years. This increase may reflect, in part, the impact of the Johnson & Johnson Campaign for Nursing’s Future, which launched a large national media initiative in 2002 aimed at attracting people into nursing. As other similar recruitment initiatives followed, more, younger people chose to become nurses, reversing a 20-year trend of declining entry into nursing by young people.
The shift in the age composition of the nursing workforce can be attributed in part to the large number of baby boomers who became RNs in the 1970s and 1980s, followed by much smaller cohorts in the later decades (Buerhaus et al., 2009a). These smaller cohorts were a result of not only the decrease in births, but also a decrease in interest in the profession during the 1980s and 1990s when women began entering other professions that had typically been dominated by men (Staiger et al., 2000). The physician workforce has also been aging, but in much smaller numbers. Figure 3-8 compares the average age of nurses with varying levels of education with that of physicians and physician faculty. Between 2001 and 2009, the number of physicians aged 50–64 grew by 77,000 FTEs, while the number of RNs in that same age group grew by almost five times as many (368,000 FTEs) (Staiger et al., 2009). Compared with the size of the nursing workforce, however, the size of the physician workforce is less dependent on interest in profession. The supply of physicians is influenced more by institutional factors that govern the number of available slots in medical schools and residency
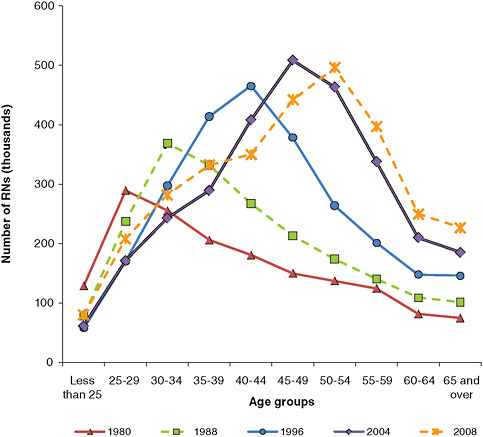
FIGURE 3-7 Age distribution of registered nurses, 1980–2008
SOURCE: HRSA, 2010.
programs. For example, the supply of physicians was deliberately expanded in the 1960s with the introduction of the Medicare and Medicaid programs but has remained fairly constant since then. This pattern has resulted in large successive cohorts of physicians who are replacing smaller groups of retiring physicians (Staiger et al., 2009).
As the coming decades unfold, nurses and physicians will continue to age. Many of the large numbers of older RNs will retire, and increasing numbers of middle-aged RNs will enter their 50s. Although the number of younger RNs has recently begun to grow, the increase is not expected to be large enough to offset the number of RNs anticipated to retire over the next 15 years (Buerhaus et al., 2009b). To fill gaps created by retirement and the increasing demand for nursing services, resulting in part from an aging population and increased rates of insurance coverage, the nursing workforce will need to expand by attracting younger
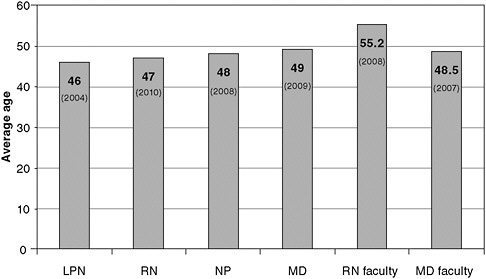
FIGURE 3-8 Average age of nurses at various levels of education and of MDs.
NOTE: LPN = licensed practical nurse; MD = doctor of medicine; NP = nurse practitioner; RN = registered nurse.
SOURCE: Based on data for LPNs (HRSA, 2004); for RNs (HRSA, 2010); for NPs (AANP, 2010); for MDs (Sermo.com, 2009); for RN faculty (AACN, 2010b); for MD faculty (AAMC, 2009).
individuals into the profession—a challenge that has been more difficult for the nursing profession than it has been for medicine (Kimball and O’Neil, 2002).
Gender Diversity
Throughout much of the 20th century, the nursing profession was composed mainly of women. While the absolute number of men who become nurses has grown dramatically in the last two decades, from 45,060 in 1980 to 168,181 in 2004 (HRSA, 2006), men still make up just over 7 percent of all RNs (HRSA, 2010). Overall, male RNs tend to be younger than female RNs, with an average age of 44.6 years. Men are also more likely to begin their careers with slightly more advanced nursing degrees (HRSA, 2006).
Efforts to recruit more men into the civilian nursing profession have had minimal success, and a body of research indicates gender-based reasons for entering the nursing profession. The evidence is generally thin, but men tend to list factors associated with security and professional growth that led them to the nursing profession: salary, ease of obtaining work, job security, and opportunities for leadership. By contrast, women tend to list factors that represent social encouragement from family or friends (Zysberg and Berry, 2005). While more men
are being drawn to nursing, especially as a second career, the profession needs to continue efforts to recruit men; their unique perspectives and skills are important to the profession and will help contribute additional diversity to the workforce.
Racial and Ethnic Diversity
To better meet the current and future health needs of the public and to provide more culturally relevant care, the current nursing workforce will need to grow more diverse. Previous IOM reports have found that greater racial and ethnic diversity among providers leads to stronger relationships with patients in nonwhite communities. These reports argue that the benefits of such diversity are likely to be felt across health professions and to grow as the U.S. population becomes increasingly diverse (IOM, 2004, 2006). The IOM’s report Unequal Treatment: Addressing Racial and Ethnic Disparities in Health Care identifies the diversification of the health care workforce as an important step toward responding to racial and ethnic disparities in the health care system (IOM, 2003). Because nurses make up the largest proportion of the health care workforce and work across virtually every health care and community-based setting, changing the demographic composition of nurses has the potential to effect changes in the face of health care in America.
Although nurses need to develop the ability to communicate and interact with people from differing backgrounds, the demographic characteristics of the nursing workforce should be closer to those of the population at large to foster better interaction and communication (AACN, 2010a). The 2008 National Sample Survey of Registered Nurses (NSSRN) documented the lack of diversity in the nursing workforce, with 5.4 percent of nurses describing themselves as Black/African American, 3.6 percent as Hispanic/Latino, 5.8 percent as Asian or Native Hawaiian/Pacific Islander, 0.3 percent as American Indian/Alaska Native, and 1.7 percent as multiracial (HRSA, 2010). Figure 3-9 compares the racial/ethnic diversity of RNs with that of the U.S. population.
Numerous programs nationwide are aimed at increasing the number of health professionals from underrepresented ethnic and racial groups. One program that seeks to increase diversity while also responding to the health needs of underserved populations is the Harambee Nursing Center (HNC) in Louisville, Kentucky (AAN, 2010c). The name refers to an African tribal word that means “let’s pull together.” HNC was founded in 2003 by the University of Louisville School of Nursing, in partnership with the University of Louisville hospital and several religious groups, “to improve the health of the approximately 11,000 lowincome, primarily African-American, urban, underserved Smoketown-Shelby Park-Phoenix Hill neighborhood” (Roberts and Hayes, 2005). It is managed by nurses with the help of a volunteer family practice physician. Since its inception, a goal of the program has included attracting greater numbers of minority persons into nursing and other health professions and providing opportunities to enhance

FIGURE 3-9 Distribution of registered nurses and the U.S. population by racial/ethnic background.
SOURCE: HRSA, 2010.
the cultural competence of nursing students and faculty.29 Strategies to increase diversity in nursing include
-
providing supervised clinical experiences for nursing and other health professional students at HNC;
-
offering group educational programs to community members and persons working in community agencies and one-to-one mentoring of community residents who are interested in a nursing career (which includes providing clinical experiences, taking participants to planning meetings, having them talk directly to student advisers at the School of Nursing, arranging experiences at the hospital or nursing home, and holding conversations with interested persons);
-
creating structured opportunities for nursing students and faculty to be engaged in service to the community so they can begin to comprehend the life experiences of the residents and be more sensitive to their needs when advising and creating recruitment programs;
-
distributing literature and pictures related to the history of African Americans in nursing; and
-
collaborating with other community agencies to include nursing education and career options in their educational and jobs programs.
Outcomes cited by Dr. Roberts include the following:
-
Nursing careers and educational pathways are now formally included in job-related programs implemented by the Presbyterian Community Center (PCC). For example, over the past 2 years, PCC has selected 50 community residents into the Changemaker program, which targets 19- to 25-year-olds to engage them in self-discovery, goal setting, and progress toward career goals, with the condition of giving back to the community. Each year about four to six Changemakers examine health careers in depth. HNC included nursing and health careers in the proposal that funded this pathway and provides supervised clinical experiences, mentoring, part-time job opportunities where possible, and education about nursing.
-
Arrangements have been made to connect interested residents with entry into a medical assistant program that provides articulation to associate’s degree education and then mentoring to advance to the bachelor’s of science in nursing (BSN) and further, in addition to baccalaureate programs.
-
The University of Louisville School of Nursing hosts a recruitment booth at the Annual Health Fair at HNC.
-
Community health students and faculty now provide education at the community middle school regarding careers in nursing.
-
Based on HNC’s feedback to the School of Nursing, criteria for selection of students into the RN–BSN program are under scrutiy. Last year no African American student was accepted. One of HNC’s mentorees missed selection by only a few points. Dialogue with faculty led to an examination of policies that resulted in the omission of minority students.
-
Literally hundreds of undergraduate and graduate nursing students (from several academic institutions) have supervised learning experiences in the community. These include at least 10 undergraduate community health nursing students each semester, a class of 30 graduate nursing students enrolled in a health promotion class each year, and 2 or more NP students based in the clinic each semester. About 5 NP and 10 undergraduate students participate in a Back to School event each fall where Harambee offers school physicals and immunizations for underserved middle school students. Each year 2 to 4 graduate nursing students serve as research or program assistants and/or researchers, and nursing students in the PhD program engage in research-related projects.
Conclusion: Demographic Challenges
The nurse workforce is slowly becoming more diverse, and the proportion of racially and ethnically diverse nursing graduates has increased by 10 percent in the last two decades, growing from 12.3 to 22.5 percent (HRSA, 2010). Nonetheless, additional commitments are needed to further increase the diversity of the nurse workforce. Steps should be taken to recruit, retain, and foster the success of diverse individuals. One way to accomplish this is to increase the diversity of the nursing student body, an issue addressed in Chapter 4. The combination of age, gender, race/ethnicity, and life experiences provides individuals with unique perspectives that can contribute to advancing the nursing profession and providing better care to patients.
NEW STRUCTURES, NEW OPPORTUNITIES
The ACA will bring new opportunities to overcome some of the barriers discussed above and use nurses in new and expanded capacities. This section offers a brief look at four of the current initiatives—the accountable care organization (ACO), the medical/health home, the community health center (CHC), and the NMHC—that are designed to implement these changes at an affordable price regardless of whether the providers involved are part of a large, integrated health care organization like the VA, Geisinger, or Kaiser Permanente. All four initiatives have shown enough promise that they were selected to receive additional financial support under the ACA.
Depending on their outcomes, these exemplars may lead the way to broader changes in the health care system. Given this possibility, the creation of the new Center for Medicare and Medicaid Innovation within the Department of Health and Human Services may prove to be one of the most important provisions of the ACA (Whelan and Russell, 2010). The Center is designed “to test innovative payment and service delivery models to reduce program expenditures … while preserving or enhancing the quality of care.”30 CMS can expand the duration and scope of successful programs with priority given to programs that also apply to private payers. They can also terminate or modify programs that are not working well. These types of decisions had previously been allowed only after congressional action.
The committee offers no predictions as to which combination, if any, of these four exemplars—ACOs, medical/health homes, CHCs, and NMHCs—will best succeed at meeting patients’ needs. However, it wishes to emphasize to the Center for Medicare and Medicaid Innovation that each of these four initiatives depends on high-functioning, interprofessional teams in which the competencies and skills of all nurses, including APRNs, can be more fully utilized. New models of care, still to be developed, may deliver care that is better and more efficient than that
provided by these four initiatives. Nursing, in collaboration with other professions, should be a part of the design of these initiatives by shaping and leading solutions. Innovative solutions are most likely to emerge if researchers from the nursing field work in partnership with other professionals in medicine, business, technology, and law to create them.
Accountable Care Organizations
The ACO is a legally defined entity consisting of a group of primary care providers, a hospital, and perhaps some specialists who share in the risk as well as the rewards of providing quality care at a fixed reimbursement rate (Fisher et al., 2009; MedPAC, 2009). (The use of the phrase “primary care ACO professionals” in the ACA is inclusive of APRNs as well as physicians.) Payment for this set of services, as provided for in the ACA, will move beyond the traditional fee-for-service system and may include shared savings payments or capitated payments for all services. The goal of this payment structure is to encourage the ACO to improve the quality of the care it provides and increase care coordination while containing growth. ACOs that use APRNs and other nurses to the full extent of their education and training in such roles as health coaching, chronic disease management, transitional care, prevention activities, and quality improvement will most likely benefit from providing high-value and more accessible care that patients will find to be in their best interest.
Medical/Health Homes
The concept of a medical home was first developed by pediatricians in the late 1960s (AAP, 1967). The original impetus was to create a single place to house all of individual children’s medical records—particularly children with special health needs who often must see multiple clinicians (Sia et al., 2004). Over the years, however, the term “medical home” has evolved to refer to a specific type of primary care practice that coordinates and provides comprehensive care; promotes a strong relationship between patient and provider; measures, monitors, and improves the quality of care; and is not necessarily limited to children.
Medical homes play a prominent role in the ACA, but the law is not consistent in its terminology for them. In various places, the ACA refers to “medical homes,” “health homes,” and even the above-discussed PCMH that is recognized by NCQA. The ACA indicates that medical/health homes should be supported by community-based interprofessional teams or “health teams” that include physicians, nurses, and other health professionals.31
The medical/health home concept has been adopted and adapted in several ways. The latest phase of the broader nursing strategy at the VA, for example,
consists of the implementation of a medical home model with expanded roles for RNs. Previously, primary care providers (physicians and NPs) at the VA felt that they were not receiving enough professional support to do their jobs effectively. The new strategy calls for including staff nurses on the primary care teams. “This is not your typical staff nurse role in primary care settings,” said Catherine Rick, chief nursing officer of the VA.32 What the staff nurse brings to primary care that has not been there before is the provision of chronic care management, care coordination, health risk appraisal, health promotion, and disease prevention. Work on rolling out the VA’s medical home model began in August 2009, and the program was officially launched in April 2010. The case study in Box 3-3 illustrates how the medical home concept is being applied in the VA health system.
Community Health Centers
CHCs have a long track records of providing high-value, quality primary and preventive care in poor and underserved parts of the United States. Many also offer dental, mental health, and substance abuse and pharmacy services as well. CHCs generally are very team oriented and depend on nurses to deliver services. Nurses provide primary care, preventive services, and home visits, and many serve in administrative and leadership positions. At present, 20 million Americans receive care at CHCs in 7,500 communities (NACHC, 2009). CHC patients are less likely to have unmet medical needs, visit the emergency department for nonurgent care, or need hospitalization relative to the general population. A 2007 report by the National Association of Community Health Centers found that medical expenses for patients who receive the majority of their care at a CHC are 41 percent lower ($1,810 per person) than those for comparable patients who receive most of their care elsewhere (NACHC et al., 2007). As a result, the organization estimates that CHCs save the health care system $9.9–$17.6 billion a year (NACHC, 2009).
In 2002, the Bush Administration began a significant expansion of the CHC program, which began in the 1960s as part of the “war on poverty.” The program received another big boost in 2009 with a $2 billion investment as part of the American Recovery and Reinvestment Act. And in 2010, as part of the ACA, Congress allocated an additional $11 billion in funds to further expand the program (Whelan, 2010).
Nurse-Managed Health Centers
NMHCs have provided care for populations served by Medicare, Medicaid, and children’s health insurance programs, as well as the uninsured, since the
|
BOX 3-3 Case Study: The Patient-Centered Medical Home A Team Approach to Primary Care for Veterans When a veteran with diabetes who was experiencing hyperglycemia visited the Overton Brooks VA Medical Center in Shreveport, Louisiana, a nurse practitioner (NP) made adjustments to his medications. But that visit was different from others he had made: he also talked with a team of providers about exercise, diet, and blood glucose self-monitoring, and they discussed what support he would need to make changes in these areas as well. After 2 weeks, Helen Rasmussen, BSN, RN, CDE, a care manager in primary care at the facility, called the patient, who reported his daily blood glucose levels. An NP made further medication adjustments, and Ms. Rasmussen called again in 2 weeks. “The results were much improved, and he was very happy that he didn’t have to come in to see a provider each time for these changes,” she said. Ms. Rasmussen has been a primary care nurse with the U.S. Department of Veterans Affairs (VA) for more than 12 years, and until recently, she said, she would not have had the time to make those followup calls; her caseload would have been too high. But in 2009 VA secretary Eric Shinseki announced a major push toward more “veteran-centered care” for the 6 million veterans using the system (VA, 2009). One element of that new initiative is the Patient-Centered Medical Home™ (PCMH). The PCMH is not a new concept. Four decades after the American Academy of Pediatrics developed the concept of a medical home, however, its meaning has evolved. Many now think of the PCMH as a “health home”—a team approach to primary care that involves better care coordination and information systems (including the electronic health record) and gives patients greater access to care and to their providers (including e-mail exchanges). The patient is necessarily at the center of decision making.
The VA’s nearly 65,000 licensed nurses are fundamental to this approach at the VA. “We decided to have a full-time RN [registered nurse] care manager for every full-time primary care provider,” said Catherine Rick, MSN, RN, NEA-BC, FACHE, the VA’s chief nursing services officer. The RN care manager works with others on a four-person team—including a primary care provider (a physician or an NP) and support staff—to help veterans better manage their illnesses and coordinate transitions in care, such as hospital admission. |
|
Another aspect of the PCMH at the VA is the clinical nurse leader—which, Ms. Rick said, “is probably one of the most transformational roles that the nursing profession has to offer the health care industry.” The American Association of Colleges of Nursing has defined it as a new leadership role for nurses that is neither administrative nor managerial (AACN, 2007); rather, this nurse with a master’s degree supervises the care provided by the team. At the VA, the clinical nurse leader oversees the care provided by more than one team, while the RN care manager focuses on the care provided by just his or her team. The VA intends to employ clinical nurse leaders in all of its medical centers by 2016 (ONS, 2009). Too few support staff may prevent some facilities from implementing the PCMH, said Colette S. Torres, MSN, RN, CCM, associate director of primary care, Robert J. Dole VA Medical Center, Wichita, Kansas, until savings from reduced rates of hospitalization are realized. Also, the VA is measuring outcomes of the PCMH, but data have not yet been released. Ms. Torres said that what she particularly appreciates about this model “is that we carry our patients through acute and chronic issues.” Under the old model, when a veteran was hospitalized, the primary care providers would wait to see the patient. Now, she said, they visit a veteran in the hospital. “We go up and say, ‘How are you doing? We’re not here to provide your care; we’re here because we’re a part of your team.’ And they absolutely love it.”  As part of Helen Rasmussen’s role as a nurse care manager, she takes the time to explain health information to her patients. |
1960s. There are 250 NMHCs across the United States serving 1.5 million medically underserved people, nearly half of whom are uninsured (NNCC, 2005). As the name implies, they are run by nurses—although many employ physicians, social workers, health educators, and outreach workers as members of a collaborative health team. Services generally include comprehensive primary care, family planning, prenatal services, mental/behavioral health care, and health promotion and disease prevention.
The majority of NMHCs are affiliated with a nursing school and about half with a community-based nonprofit organization (King and Hansen-Turton, 2010). NMHCs report that their clients make 15 percent fewer emergency department visits than the general population, have 35–40 percent fewer nonmaternity hospital days, and spend 25 percent less on prescriptions (NNCC, 2005). The ACA authorizes an additional $50 million in 2010 and “such sums as may be necessary for each of the fiscal years 2011 through 2014”33 to NMHCs that offer primary care to low-income and medically underserved patients, although as of this writing, this funding specifically for NMHCs has not been allocated. The case study presented in Box 3-4 shows how an NMHC worked with community leaders to reduce health disparities in an underserved poor neighborhood in Philadelphia.
Opportunities Through Technology
There is perhaps no greater opportunity to transform practice than through technology. Information technology has long been used to support billing and payments but has become increasingly important in the provision of care as an aid to documentation and decision making. Diagnostic and monitoring machines have proven invaluable in the treatment of cancer, heart disease, and many other ailments. Examples cited by the IOM in Crossing the Quality Chasm: A New Health System for the 21st Century include “growing evidence that automated order entry systems can reduce errors in drug prescribing and dosing” and “improvements in timeliness through the use of Internet-based communication (i.e., e-visits, telemedicine) and immediate access to automated clinical information, diagnostic tests, and treatment results” (IOM, 2001). Since that report was published, the expanded use of online communication has resulted in so-called telehealth services that are not limited to diagnosis or treatment but also include health promotion, follow-up, and coordination of care. Delivery of telehealth services has, however, like that of APRN services, been complicated by variability in state regulations, particularly whenever online communications cross state lines.
Impact of Technology on the Design of Health Care Delivery
In 2009, the American Recovery and Reinvestment Act (ARRA) (Public Law 111-5) included provisions to create incentives for the adoption and meaningful use of health information technology (HIT). ARRA strengthened standards for maintaining the privacy and security of health information. ARRA provided grants to help state and local governments as well as health care providers in their efforts to adopt and use HIT. CMS also provided incentives, under ARRA to encourage eligible hospitals and health professionals to become “meaningful users” of certified EHRs. A definition of “meaningful use” was developed by the Secretary of HHS by official rulemaking procedures, providing opportunity for public and professional input (HHS, 2009). The meaningful use objectives will likely continue to be refined but outline core requirements that should be included in every EHR. By adopting these recommendations, users will be eligible for federal incentive payments and will be able to report information on the clinical quality of care. States can add or modify additional objectives to this definition for their Medicaid programs (CMS, 2010).
A recent article in the New England Journal of Medicine summarizes the meaningful use criterion as follows: “use by providers to achieve significant improvements in care” (Blumenthal and Tavenner, 2010). Given the nature of patient data collection, nurses will be integral to proper collection of meaningful use data. For example, among the first set of criteria to be measured include patient demographics, vital signs, and lists of patient’s diagnoses, allergies, and active medications. As EHRs become more refined and integrated, nurses will have the opportunity to help define additional meaningful use objectives.
Implications for Time and Place of Care
Care supported by interoperable digital networks will shift in the importance of time and place. The patient/consumer will not always have to be in the same location as the provider, and the provider will not always have to interact with the patient in real time. As EHRs, computerized physician order entry systems, laboratory results, imaging systems, and pharmacies are all linked into the same network, many types of care can be provided without regard to location, as the “care grid” is available anywhere, anytime.
Remote patient monitoring is expanding exponentially. An ever-growing array of biometric devices (e.g., indwelling heart or blood sugar monitors) can collect, monitor, and report information from the patient in real time, in either an institution or the home. Some of these devices can also provide direct digitally mediated care; the automated insulin pump and implantable defibrillators are two examples.
The implications of these developments for nursing will be considerable and as yet are not fully understood (Abbott and Coenen, 2008). It is not clear
|
BOX 3-4 Case Study: 11th Street Family Health Services of Drexel University A Nurse-Managed Health Center Reduces Health Disparities in Philadelphia Lisa Scardigli, age 44, has suffered periodically from spasticity, a symptom of the multiple sclerosis she has lived with for more than 20 years. She had been receiving physical therapy at 11th Street Family Health Services in Philadelphia when she had a pump implanted for spinal infusion of a drug that reduces spasticity. But the pump’s catheter punctured in late 2009, and she was hospitalized for several weeks. When she returned to 11th Street, she said, she got “holy heck” from the staff there; they had been worried about her. “Even the people at the front desk were up in arms over the fact that I didn’t call,” Ms. Scardigli said. “It went from the physical therapist to the primary care person to the security guard. I was actually missed.” This is a small story, but it illustrates a big reason for this health center’s success: it not only serves its community (there were 26,000 clinical visits in 2009); it also creates community. And that may have something to do with the fact that it is run by nurses. This nurse-managed health center provides primary care and other services in a neighborhood in North Philadelphia where most of the 6,000 residents are African American, have low incomes, and are medically underserved. Nurse practitioners (NPs) and social workers make up teams that are augmented as needed by physicians, nutritionists, and others. Having been launched in 1998 in a recreation center, 11th Street is now a federally qualified health center housed in a $3.3 million, 17,000-square-foot facility, with a staff of 53.
The center’s work began gradually, as a joint project of the Philadelphia Housing Authority and Drexel University’s College of Nursing and Health Professions. In 1996 director Patricia Gerrity, PhD, RN, FAAN, placed a public health nurse at each of four housing developments in the neighborhood. The nurses responded to residents’ immediate concerns: the need for stop signs, animal control, food assistance, and training in CPR. “Over that first year or two we gained the trust of the residents because we weren’t defining the issues; they were,” Dr. Gerrity said. “And it showed that we were making a longterm commitment.” From there, she met with area representatives to discover their visions for the community. They |
|
wanted a health care center, they said, one they could access regardless of their ability to pay. A community advisory board was formed, and the search for funding began. (Over the years the center has received funding from federal, state, and private sources.) Dr. Gerrity uses the word “transdisciplinary” rather than “multidisciplinary” or “interdisciplinary” to describe the care provided at 11th Street. “Transdisciplinary means you start to break down the barriers between disciplines. Each person learns something about the other person’s discipline, and it enriches their own practice,” Dr. Gerrity said. For example, behavioral health care has been incorporated into every primary care visit, with NPs and social workers closely collaborating. The range of services provided is remarkably diverse. Patients like Ms. Scardigli undergo physical therapy. Patients with diabetes join cooking classes that make use of locally grown produce. First-time mothers receive home visits through the Nurse–Family Partnership. Six to eight mother–infant pairs meet through the Centering Parenting program. A fitness center with a fulltime personal trainer is on site, full dental care is available, and chronic illness management groups provide peer support. Unpublished outcome data for patients with diabetes show that in an 18-month period, the proportion who had glycosylated hemoglobin levels below 7 percent doubled and that low-density lipoprotein cholesterol and blood pressure levels fell as well. Also seen were reductions in depression and low-birth-weight infants and increases in immunization and breast cancer screening.  A nurse at 11th Street Family Health Services uses the food pyramid to educate patients about a healthy diet. Access to payment for care coordination through medical home designation is important to the center’s sustainability. Despite meeting the criteria set by the National Committee for Quality Assurance for qualifying as a Patient-Centered Medical Home™, 11th Street was denied the designation because it is led by nurses rather than physicians—an issue for the 250 nurse-managed health centers across the nation. Lisa Scardigli is so impressed by all the center does that she now sits on the community advisory board. Recently, she brought in a neighbor of hers who needed new dentures. “She loves it,” Ms Scardigli said. “She’s 90, and she’s from down south, so it reminds her of when the doctor used to come to your house and knew the family and sat down and broke bread.” |
how much of nursing care might be independent of physical location when HIT is fully implemented, but it will likely be a significant subset of care, possibly in the range of 15–35 percent of what nurses do toda. That is, for this proportion of care, nurses need not be in the same locale (or even the same nation) as their patients. As new technologies impact the hospital and other settings for nursing services, this phenomenon may increase.
Implications for Nursing Practice
HIT will fundamentally change the ways in which RNs plan, deliver, document, and review clinical care. The process of obtaining and reviewing diagnostic information, making clinical decisions, communicating with patients and families, and carrying out clinical interventions will depart radically from the way these activities occur today. Moreover, the relative proportion of time RNs spend on various tasks is likely to change appreciably over the coming decades. While HIT arguably will have its greatest influence on how RNs plan and document their care, all facets of care will be mediated increasingly by digital workflow, computerized knowledge management, and decision support.
In the future, virtually every facet of nursing practice in each setting where it is rendered will have a significant digital dimension around a core EHR. Biometric data collection will increasingly be automated, and diagnostic tests, medications, and some therapies will be computer generated and managed and delivered with computer support. Patient histories and examination data will increasingly be collected by devices that interface directly with the patient and automatically stream into the EHR. Examples include automated blood pressure cuffs, personal digital assistant (PDA)–based functional status, and patient history surveys.
In HIT-supported organizations, a broader array and higher proportion of services of all types will be provided within the context of computer templates and workflows. Care and its documentation will less frequently be “free-hand.” As routine aspects of care become digitally mediated and increasingly rote, RNs and other clinicians can be expected to shift and expand their focus to more complex and nuanced “high-touch” tasks that these technologies cannot readily or appropriately accomplish, such as communication with and guidance and support for patients and their families. There will likely be greater opportunities for such interventions as counseling, behavior change, and social and emotional support—interventions that lie squarely within the province of nursing practice.
Impact of Technology on Quality, Efficiency, and Outcomes
Adoption of HIT is expected to increase the efficiency and effectiveness of clinician interactions with each patient and the target population. EHRs and other HIT should lower the cost per unit of service delivered and/or improve the qual-
ity of care as measured by outcomes or achievement of other end points, such as increased adherence to optimal guidelines. HIT will lead to greater efficiency if it takes less time for a clinician to provide the same unit of service or if a lowercost clinician practicing with extensive HIT support can deliver the same type of care as a higher-cost non-HIT-supported provider. Controlled time and motion studies that have compared clinicians performing the same task with and without HIT support have produced mixed findings on time efficiencies gained across clinicians and settings. One area with emerging evidence is hospital nursing time spent in documentation, with studies showing a 23–24 percent reduction (Poissant et al., 2005). On the other hand, these efficiency gains may be partially offset by the information demands of quality improvement initiatives and similar programs undertaken by a growing number of institutions (DesRoches et al., 2008).34
According to a review of the literature conducted for the committee, although research on the impact of HIT on the quality of nursing care is limited, documentation quality and accessibility generally improve after the implementation of HIT. Medication errors almost always decrease after the implementation of bar code medication administration (Waneka and Spetz, 2009). DesRoches and colleagues (2008) conducted a national survey of more than 3,436 RNs (1,392 responses) and found that hospitals with basic EHR systems were more likely to be recognized for nursing excellence (magnets/magnet-like) and to have quality improvement programs. No differences were found in time spent on patient care activities for nurses in hospitals with and without minimally functioning systems.
Technology is also used to measure patient outcomes, with varying results. While measuring outcomes is critical to the provision of 21st-century health care, complications have developed in ensuring that outcome measures from different institutions and organizations are, in fact, comparable. Even ensuring that outcome measures from different parts of the same organization are comparable can be problematic. Researchers in Colorado conducted a comprehensive review of the use of rescue agents—a Joint Commission–approved quality measure—based on the EHRs at the Children’s Hospital in Aurora. They found that variations in the way information was entered in the EHRs accounted for significant variations within the institution and could be responsible for as much as a 40-fold difference in outcome measures among hospitals (Kahn and Ranade, 2010). The researchers concluded that “more detailed clinical information may result in quality measures that are not comparable across institutions due [to] institution-specific workflow.”
|
34 |
This paragraph draws on a paper commissioned by the committee on “Health Care System Reform and the Nursing Workforce: Matching Nursing Practice and Skills to Future Needs, Note Past Demands,” prepared by Julie Sochalski, University of Pennsylvania School of Nursing, and Jonathan Weiner, Johns Hopkins University Bloomberg School of Public Health (see Appendix F on CD-ROM). |
A longitudinal study of 326 hospitals found that those that had implemented more advanced EHR systems over the time period had higher costs and increased nurse staffing levels (Furukawa et al., 2010). Patient complications increased in these hospitals, while mortality for some conditions declined. It should be noted, however, that these results may be difficult to interpret because of the implementation of minimum nurse staffing regulations at the same time that the implementation of EHRs ramped up. During that time, nurse staffing rose, and thus costs per patient rose, and if there is any correlation between implementation of EHRs and increased nurse staffing due to the ratios, the results may confound the two. In addition, the study did not control for hospital ownership (e.g., nonprofit, forprofit) or system affiliation, both of which might be important.
Finally, a systematic review of the literature (fewer than 25 articles) showed that the time spent on documentation of care may increase or decrease with EHRs (Thompson et al., 2009). The increases in time however, may be compensated for by the use of EHRs in other activities, such as giving/receiving reports, reconciling medications, and planning care.
Technology Transforming Roles for Nurses
The new practice milieu—where much of nursing and medical care is mediated and supported within an interoperable “digital commons”—will support and potentially even require much more effective integration of multiple disciplines into a collaborative team focused on the patient’s unique set of needs. Furthermore, interoperable EHRs linked with personal health records and shared support systems will influence how these teams work and share clinical activities. It will increasingly be possible for providers to work on digitally linked teams that will collaborate with patients and their families no longer limited by real-time contact.35
As the knowledge base and decision pathways that previously resided primarily in clinicians’ brains are transferred to clinical decision support and CPOE modules of advanced HIT systems, some types of care most commonly provided by nurses can readily shift to personnel with less training or to patients and their families. Similarly, many types of care previously provided by physicians and other highly trained personnel can be provided effectively by APRNs and other specialty trained RNs. Furthermore, the performance of these fundamentally restructured teams will be monitored through the use of biometric, psychometric, and other types of process and outcome “e-indicators” extracted from the HIT infrastructure.
|
35 |
This and the next paragraph draw on a paper commissioned by the committee on “Health Care System Reform and the Nursing Workforce: Matching Nursing Practice and Skills to Future Needs, Note Past Demands,” prepared by Julie Sochalski, University of Pennsylvania School of Nursing, and Jonathan Weiner, Johns Hopkins University Bloomberg School of Public Health (see Appendix F on CD-ROM). |
Increasingly, technology is allowing nurses and other health care providers to offer their services in a wider range of settings. For example, the ability of the Visiting Nurse Service of New York to tap into mobile technology, as described in Chapter 2, allowed that organization to provide ever more complex care in the home setting (IOM, 2010a).
Involving Nurses in Technology Design and Implementation
As the largest segment of the health care workforce with some of the closest, most sustained interactions with patients, nurses are often the greatest users of technology. In many instances, they may know what will work best with regard to technological solutions, but they are asked for their opinions infrequently. According to a survey of nurses at 25 leading acute care facilities across the United States, nurses find “that existing systems are often splintered, unable to interface and require multiple log-on to access or enter data. They call repeatedly for integrated systems to ease their workload and help them reach clinical transformation” (Bolton et al., 2008).
Studies show that involving nurses in the design, planning, and implementation of technology systems leads to fewer problems during implementation (Hunt et al., 2004). The TIGER Initiative (for Technology Informatics Guiding Education Reform) is a collaborative effort of 1,400 nurses from various organizations, government agencies, and vendors whose goal is “to interweave informatics and enabling technologies transparently into nursing practice” (TIGER, 2009). As leaders from the TIGER Initiative told the committee, “Regardless of the setting or environment of care, the best, most up to date information is required to support safe, effective care and promote optimal outcomes.” And yet, they pointed out, “Today, health information is not shared across the various providers and stakeholder groups who provide, fund and research care.” The members of the TIGER Initiative hope to help change that situation by developing the capacity of nursing students and members of the nursing workforce “to use electronic health records to improve the delivery of health care” and “engage more nurses in leading both the development of a national health care information technology (NHIT) infrastructure and health care reform.” They also see the need to “accelerate adoption of smart, standards based, interoperable technology that will make health care delivery safer, more efficient, timely, accessible, and patient-centered, while also reducing the burden of nurses” (TIGER, 2009).
Nurses have also invented new technology to help them care for their patients. For instance, Barbara Medoff Cooper, professor in pediatric nursing and director of the Center for Biobehavioral Research at the University of Pennsylvania School of Nursing, developed a microchip device that is situated between the nipple and the rest of the baby bottle. It measures the sucking ability of premature neonatal babies, which has been shown to be an accurate indication of the infant’s ability to feed successfully and thus survive discharge. The information
thus gathered has helped guide parents and providers in better planning for the care of high-risk neonates at home (Bakewell-Sachs et al., 2009; Medoff-Cooper et al., 2009).
Another effort, called TelEmergency, brings a certified emergency room physician to 12 rural hospitals in Mississippi from the University of Mississippi via a T-1 line, but only when needed. The system is managed by a group of 35 APRNs who provide care in these rural communities, including management of the technology as a referral system. The nurses are able to handle 60 percent of all emergency care, saving the hospital consortium $72,000 per month (AAN, 2010b).
The case study in Box 3-5 shows how nurses at one institution are working to ensure that they spend their time in patient care and not on the technology associated with delivering modern health care.
CONCLUSION
The nursing profession has evolved more rapidly than the public policies that affect it. The ability of nurses to better serve the public is hampered by the constraints of outdated policies, particularly those involving nurses’ scopes of practice. Evidence does not support the conclusion that APRNs are less able than physicians to provide safe, effective, and efficient care (Brown and Grimes, 1995; Fairman, 2008; Groth et al., 2010; Hatem et al., 2008; Hogan et al., 2010; Horrocks et al., 2002; Hughes et al., 2010; Laurant et al., 2004; Mundinger et al., 2000; Office of Technology Assessment, 1986). The roles of APRNs—and the roles of all nurses—are undergoing changes that will help make the transformative practice models outlined at the beginning of this chapter a more common reality. Such changes must be supported by a number of policy decisions, including efforts to remove the existing regulatory barriers to nursing practice. If the current conflicts between what nurses can do based on their education and training and what they may do according to state and federal policies and regulations are not addressed, patients will continue to experience limited access to high-quality care.
Despite the evidence demonstrating that APRNs are educated, trained, and competent to provide safe, high-quality care without the need for physician supervision, states’ legislative decisions regarding legal scopes of practice range from restrictive to permissive. While medicine and a number of other professions enjoy practice regulations that are comparable across states, this goal has been elusive for nurses, particularly those working in advanced practice. With the availability now of a consensus document that offers agreed-upon standards for APRN education, training, and regulation, states that have been reluctant in the past may move toward broader scopes of practice. Such a move, however, considered by the committee to be a critical one, is not guaranteed. And while the committee defers to the rights of states to continue their regulation of health
professionals, it also wishes to note why and how the federal government can play an important role in this arena.
The primary reason the federal government has a compelling interest in state regulation of health professionals is the responsibility to patients covered by federal programs such as Medicare and Medicaid. If access to care is hindered, if costs are unduly high, or if quality of care could be improved for these millions of patients through evidence-based changes to the ways in which professionals may practice, the federal government has a right to explore the options and encourage change. An additional reason is the federal government’s unique perspective—somewhat removed from that of the individual states—enabling it to shed light on the value and benefit to all Americans of harmonizing practice regulations among the states.
Certain federal entities may both defer to the states in adopting their own practice regulations and encourage the adoption of regulations that are consistent with current clinical evidence and comparable across the country. Congress, CMS, OPM, and the FTC each have specific authority or responsibility for decisions that either must be made at the federal level to be consistent with state efforts to remove scope-of-practice barriers or could be made to encourage and support those efforts. While no single actor or agency can independently make a sweeping change to eliminate current barriers, the various state and federal entities can each make relevant decisions that together can lead to much-needed improvements.
In addition to regulatory barriers, cultural and organizational barriers constrain nurses’ ability to identify solutions and implement them quickly, knowing that patients’ lives and well-being are at stake. Moreover, an important priority in national health care reform is achieving better value for the expenditures made on health care services. Since health care is labor intensive, getting more value from the health care system will depend in large part on enhancing the productivity and effectiveness of the workforce. Nurses therefore represent a large and unexploited opportunity to achieve greater value in health care.
The committee believes that any proposed changes in the responsibilities of the nursing workforce should be evaluated against their ability to support the provision of seamless, affordable, quality care that is accessible to all. In particular, the committee argues that now is the time to finally eliminate the outdated regulations and organizational and cultural barriers that limit the ability of nurses, including APRNs, to practice to the full extent of their education, training, and competence. The committee also believes that nurses must be allowed to lead improvement and redesign efforts (see Chapter 5).
Specifically, in order that all Americans may have access to high-quality, safe health care, federal and state actions are required to update and standardize scope-of-practice regulations to take advantage of the full capacity and education of nurses. Cultural and organizational barriers should also be eliminated. States and insurance companies must follow through with specific regulatory,
|
BOX 3-5 Case Study: Technology at Cedars-Sinai Medical Center Sending Alerts via Text Message Shortens Nurses’ Response Times to Critical Alarms In January 2010 a California hospital was fined for the death of a man whose cardiac alarm had been set to an inaudible level; when his heart stopped, the emergency room nurses were unaware of it and failed to intervene (California Department of Public Health, 2009). That same month a man died in a Massachusetts hospital after his heart rate declined over a 20-minute period; nurses did not hear his cardiac alarm, investigators found, and a second alarm had been turned off (McKinney, 2010). Nurses attend to a variety of alarms and alerts during a shift, and there is often no system in place for prioritizing urgency. Confusion and “alarm fatigue” can result, with potentially lethal consequences: the ECRI Institute lists alarm hazards as the second most serious of the top 10 technology hazards in health care for 2010 (ECRI Institute, 2010). The problem has been shown to pose a danger to patient safety (Graham and Cvach, 2010), as have problems with clinical alarms in general (ACCE Healthcare Technology Foundation, 2006). Unfortunately, nurses are rarely involved in decisions about new technologies in health care, although the patient’s bedside has been identified as the area most in need of technological innovation (Bolton et al., 2008). At a combined telemetry and medical–surgical unit at CedarsSinai Medical Center in Los Angeles, nurses are taking the lead in testing ways to aggregate and prioritize the alarms to which they must respond, most recently via text messages sent to nurses’ and nursing assistants’ BlackBerry devices. This system has replaced pagers and many bedside alarms, with promising results.
Timely, Accurate Messaging. In a unit where routine alerts might range in importance from an out-of-reach water pitcher to cardiac arrest, getting “the right message to the right person at the right time” is critical, said Joanne Pileggi, MSN, RN, the unit’s nurse manager. Working with Emergin, a communications software company, the unit’s nurses and nursing assistants categorized the alarms they receive—from cardiac monitors, patients’ call buttons, bed alarms, code blues, and the laboratory—according to their urgency, classifying them as red (most critical), blue (moderately critical), or yellow (least critical). |
|
For example, if a patient’s cardiac monitor detects a dangerous arrhythmia, that information is sent to the unit’s “command center,” where a cardiac nurse sends out a red alert via text message to that patient’s nurse and the charge nurse. A beep or vibration from the nurse’s BlackBerry indicates that a new text message has arrived. The nurse can glance at the device, see that the alert is red, and reply immediately, eliminating several problems with overhead paging systems: the need for repeated pages, the inability of the nurse to respond, excessive noise on the unit, and delays in response. The 30-bed unit employs nine registered nurses (RNs) on the day shift and nine on the night shift and has been testing a variety of devices for more than 2 years. Staff were involved from the beginning, Ms. Pileggi said, and everyone, including aides, received training from Emergin. An Investment in Safety. Use of the BlackBerry devices has cut the number of overhead pages on the unit by more than half. Nurses report less alarm fatigue and faster response times to alarms, and they receive critical laboratory values 10 minutes sooner under the new system than under the old one. They also save time by not handling alarms that do not require a nurse’s attention. Darren Dworkin, chief information officer for Cedars-Sinai, said the initial costs of purchasing the devices and training the staff have paid off in more efficient and safer care. “Enabling nurses to spend more time at the bedside is a goal we want to achieve,” he said, “and so if the technology achieves that, then we are achieving our return on investment.” The unit has not conducted a cost–benefit analysis.  Los Angeles hospital Cedars-Sinai is a leader in using mobile devices for text message patient alerts and notifications. Few manufacturers are designing technologies with nurses in mind, and limitations of the available technology have meant that not all ideas for improving processes can be tested. For example, the unit could not incorporate IV pump alarms into the most recent test. Still, bedside nurses and patients are quite pleased. The nurses are looking forward to a test of iPhones, which will display cardiac rhythms on screen. Said Ms. Pileggi, “We’re anticipating patients’ needs, so there hasn’t been the need for patients to call as often.” |
policy, and financial changes that uphold patient-centered care as the organizing principle for a reformed health care system. The education and training of nurses support their ability to offer a wider range of services safely and effectively—as documented by numerous studies. And nurses must respond to the challenge, reinventing themselves as needed in a rapidly evolving health care system. Nursing is, of course, not the only profession to confront the need to transform itself in response to new realities; similarly disruptive challenges have been faced in other fields, such as medicine, health care, publishing, education, business, manufacturing, and the military. In the field of health care, expansion of scopes of practice to reflect the full extent of one’s education and training should occur for all health professionals to maximize the contributions of each to patient care. For example, one impact of enhancing nurses’ scopes of practice may be to allow the currently inadequate numbers of physicians to better use their time and skills on the most complex and challenging cases and tasks, as well as broaden the array of services they can offer as part of a collaborative team of providers (e.g., within new models of care—ACOs, medical homes, transitional care—that are part of the ACA, as well as in groups of specialty providers). To facilitate the most effective transition to team practice, as well as practice that encompasses the full extent of their scope, all providers will require continual teaching and learning to facilitate the highest level of team functioning (see Chapter 4).
Key factors that will contribute to the success of managing such a transition include technological literacy, good communication skills, adaptability to organizational changes, and a willingness to evaluate and reinvent how work is organized and accomplished (Kimball and O’Neil, 2002). Going forward under the ACA and whatever reforms may follow, the health care system is likely to change so rapidly that building the adaptive capacity of the nursing workforce to work across settings and in different types of roles in new models of care will require intentional development, expanded resources, and policy and regulatory changes.
Finally, the committee believes that if practice is to be transformed, nurses graduating with a bachelor’s degree must be better prepared to enter the practice environment and confront the challenges they will encounter. Therefore, the committee concludes that nurse residency programs should be instituted to provide nurses with an appropriate transition to practice and develop a more competent nursing workforce.
REFERENCES
AACN (American Association of Colleges of Nursing). 2007. White paper on the education and role of the clinical nurse leader. http://www.aacn.nche.edu/Publications/WhitePapers/ClinicalNurseLeader07.pdf (accessed March 26, 2010).
AACN. 2008. The essentials of baccalaureate education for professional nursing practice. Washington, DC: AACN. http://www.aacn.nche.edu/education/pdf/BaccEssentials08.pdf.
AACN. 2010a. Enhancing diversity in the nursing workforce. http://www.aacn.nche.edu/Media/FactSheets/diversity.htm (accessed July 1, 2010).
AACN. 2010b. Nursing faculty shortage fact sheet. http://www.aacn.nche.edu/Media/Factsheets/facultyshortage.htm (accessed September 23, 2010).
AAMC (Association of American Medical Colleges). 2009. Analysis in brief: The aging of full-time U.S. Medical school faculty: 1967-2007. http://www.aamc.org/data/aib/aibissues/aibvol9_no4.pdf (accessed September 23, 2010).
AAN (American Academy of Nursing). 2010a. Edge Runner directory: Post-baccalaureate nurse residency. http://www.aannet.org/i4a/pages/index.cfm?pageid=3303 (accessed September 13, 2010).
AAN. 2010b. Edge Runner directory: Telemergency: Distance emergency care using nurse practitioners. http://www.aannet.org/custom/edgeRunner/index.cfm?pageid=3303&showTitle=1 (accessed September 13, 2010).
AAN. 2010c. Edge Runner directory: The Harambee Nursing Center: Community-based, nurse-led health care. http://www.aannet.org/custom/edgeRunner/index.cfm?pageid=3303&showTitle=1 (accessed May 19, 2010).
AANP (American Academy of Nurse Practitioners). 2010. Nurse practitioner facts. http://www.aanp.org/AANPCMS2/AboutAANP/NPFactSheet.htm (accessed July 2, 2010).
AAP (American Academy of Pediatrics). 1967. Pediatric records and a “Medical home” Edited by Council on Pediatric Practice, Standards of child care. Evanston, IL: AAP.
AARP. 2010a. AARP 2010 policy supplement: Scope of practice for advanced practice registered nurses. http://championnursing.org/sites/default/files/2010%20AARPPolicySupplementScopeofPractice.pdf (accessed September 10, 2010).
AARP. 2010b. Consumer access & barriers to care: Physician-nurse practitioner restrictive collaboration requirements by state (map). http://championnursing.org/aprnmap (accessed August 26, 2010).
Abbott, P. A., and A. Coenen. 2008. Globalization and advances in information and communication technologies: The impact on nursing and health. Nursing Outlook 56(5):238-246, e232.
Abelson, R. 2010. A health insurer pays more to save. New York Times, June 21.
ACCE (American College of Clinical Engineering) Healthcare Technology Foundation. 2006. Impact of clinical alarms on patient safety. http://www.acce-htf.org/White%20Paper.pdf (accessed March 22, 2010).
Aiken, L., and R. Cheung. 2008. Nurse workforce challenges in the United States: Implications for policy. OECD Health Working Paper No. 35. Available from http://www.oecd.org/dataoecd/34/9/41431864.pdf.
Aiken, L. H., R. B. Cheung, and D. M. Olds. 2009. Education policy initiatives to address the nurse shortage in the United States. Health Affairs 28(4):w646-w656.
AMA (American Medical Association). 2009. The AMA scope of practice data series: Nurse practitioners. Chicago, IL: AMA.
AP (Associated Press). 2010. 28 states seek to expand the role of nurse practitioners (April 14, 2010). http://www.dallasnews.com/sharedcontent/dws/news/nation/stories/DN-drnurse_14nat.ART.State.Edition1.4c7c973.html (accessed June 27, 2010).
ASA (American Society of Anesthesiologists). 2004. The scope of practice of nurse anesthetists. Washington, DC: ASA.
Asch, S., E. McGlynn, M. Hogan, R. Hayward, P. Shekelle, L. Rubenstein, J. Keesey, J. Adams, and E. Kerr. 2004. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Annals of Internal Medicine 141(12):938-945.
Bakewell-Sachs, S., B. Medoff-Cooper, J. Silber, G. Escobar, J. Silber, and S. Lorch. 2009. Infant functional status: The timing of physiologic maturation of premature infants. Pediatrics 123: e878-e886.
Beecroft, P. C., L. Kunzman, and C. Krozek. 2001. RN internship: Outcomes of a one-year pilot program. Journal of Nursing Administration 31(12):575-582.
Beecroft, P. C., L. A. Kunzman, S. Taylor, E. Devenis, and F. Guzek. 2004. Bridging the gap between school and workplace: Developing a new graduate nurse curriculum. Journal of Nursing Administration 34(7-8):338-345.
Benner, P., M. Sutphen, V. Leonard, and L. Day. 2009. Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass.
Blumenthal, D., and M. Tavenner. 2010. The “meaningful use” regulation for electronic health records. New England Journal of Medicine 636(6):501-504.
Bodenheimer, T., and H. H. Pham. 2010. Primary care: Current problems and proposed solutions. Health Affairs 29(5):799-805.
Bolton, L., and H. Aronow. 2009. The business case for TCAB: Estimates of cost savings with sustained improvement. American Journal of Nursing 109(11):77-80.
Bolton, L. B., C. A. Gassert, and P. F. Cipriano. 2008. Smart technology, enduring solutions: Technology solutions can make nursing care safer and more efficient. Journal of Healthcare Information Management 22(4):24-30.
Boult, C., L. Karm, and C. Groves. 2008. Improving chronic care: The “guided care” model. The Permanente Journal 12(1):50-54.
Brown, S. A., and D. E. Grimes. 1995. A meta-analysis of nurse practitioners and nurse midwives in primary care. Nursing Research 44(6):332-339.
Buerhaus, P., D. Staiger, and D. Auerbach. 2009a. The future of the nursing workforce in the United States: Data, trends, and implications. Boston: Jones & Bartlett.
Buerhaus, P. I., D. I. Auerbach, and D. O. Staiger. 2009b. The recent surge in nurse employment: Causes and implications. Health Affairs 28(4):w657-668.
Cady, D. M. 2006. Reports of Board of Trustees. http://www.ama-assn.org/ama1/pub/upload/mm/38/a-06bot.pdf (accessed September 21, 2010).
California Department of Public Health. 2009. Statement of deficiencies and plan of correction. http://www.cdph.ca.gov/certlic/facilities/Documents/HospitalAdministrativePenalties-2567FormsLNC/2567StJudeMedicalCenter-Fullerton-EventC0IX11.pdf (accessed March 22, 2010).
Canadian Paediatric Society. 2000. Advanced practice nursing roles in neonatal care. Paediatric Child Health 5(3):178-182.
Cebul, R. D., J. B. Rebitzer, L. J. Taylor, and M. E. Votruba. 2008. Organizational fragmentation and care quality in the U.S healthcare system. Journal of Economic Perspectives 22(4):93-113.
Chapman, S. A., C. D. Wides, and J. Spetz. 2010. Payment regulations for advanced practice nurses: Implications for primary care. Policy, Politics, & Nursing Practice 11(2):89-98. http://ppn.sagepub.com/content/early/2010/09/08/1527154410382458.
Christian, S., C. Dower, and E. O’Neil. 2007. Chart overview of nurse practitioner scopes of practice in the United States. San Francisco, CA: Center for Health Professions, University of California, San Francisco.
CMS (Centers for Medicare and Medicaid Services). 2010. Medicare and Medicaid programs; electronic health record incentive program. Federal Register 75(144):44314-44588.
Cooper, R. 1998. Current and projected workforce of nonphysician clinicians. JAMA 280(9): 788-794.
Cooper, R. A. 2007. New directions for nurse practitioners and physician assistants in the era of physician shortages. Academic Medicine 82(9):827-828.
Craven, G., and S. Ober. 2009. Massachusetts nurse practitioners step up as one solution to the primary care access problem. Policy, Politics, & Nursing Practice 10(2):94-100.
Croasdale, M. 2006. Physician task force confronts scope-of-practice legislation. American Medical News, September 21. http://www.ama-assn.org/amednews/2006/02/13/prl10213.htm.
Cunningham, R. 2010. Tapping the potential of the health care workforce: Scope of practice and payment policies for advanced practice nurses and physician assistants (background paper no. 76). Washington, DC: National Health Policy Forum.
Cys, J. 2000. Physicians: Medicare nurse pay too broad. American Medical News, July 24. http://www.ama-assn.org/amednews/2000/07/24/gvsb0724.htm.
Dall, T. M., Y. J. Chen, R. F. Seifert, P. J. Maddox, and P. F. Hogan. 2009. The economic value of professional nursing. Medical Care 47(1):97-104.
Daly, R. 2007. Psychiatrists, allies defeat psychology-prescribing bills. Psychiatric News 42(16):6.
Darves, B. 2007. Physician employment and compensation outlook for ’07. http://www.nejmjobs.org/physician-compensation-trends.aspx (accessed September 9, 2010).
Dentzer, S. 2010. Geisinger chief Glenn Steele: Seizing health reform’s potential to build a superior system. Health Affairs 29(6):1200-1207.
DeSanti, S. S., J. Farrell, and R. A. Feinstein. 2010. Letter to Kentucky Cabinet for Health and Family Services, January 28. http://www.ftc.gov/os/2010/02/100202kycomment.pdf.
DesRoches, C., K. Donelan, P. Buerhaus, and L. Zhonghe. 2008. Registered nurses use of electronic health records: Findings from a national survey. Medscape Journal of Medicine 10(7).
Djukic, M., and C. T. Kovner. 2010. Overlap of registered nurse and physician practice: Implications for U.S. Health care reform. Policy, Politics, & Nursing Practice 11(1):13-22.
Dulisse, B., and J. Cromwell. 2010. No harm found when nurse anesthetists work without supervision by physicians. Health Affairs 29(8):1469-1475.
ECRI Institute. 2010. 2010 top 10 technology hazards. https://www.ecri.org/Forms/Documents/Top_Ten_Technology_Hazards_2010.pdf (accessed March 22, 2010.
Fairman, J. 2008. Making room in the clinic: Nurse practitioners and the evolution of modern health care. 1st ed. Piscataway, NJ: Rutgers University Press.
Fisher, E., M. McClellan, J. Bertko, S. Lieberman, J. Lee, J. Lewis, and J. Skinner. 2009. Fostering accountable health care: Moving forward in Medicare. Health Affairs 28:W219-W231.
Flinter, M. 2009. Testimony submitted to inform the Forum on the Future of Nursing: Community health, public health, primary care, and long-term care. Philadelphia, PA, December 3.
Flynn, L., D. Suh, G. Dickson, M. Xie, and C. Boyer. 2010. Effects of nursing structures and processes on med errors. Poster presented at The 2010 State of the Science Congress on Nursing Research, September 27, Washington, DC.
Fox, K. 2010. Keeping the conversation going. ADA News Daily, September 24. Available from http://www.ada.org/news/2769.aspx.
Freidson, E. 1970. Profession of medicine: A study of the sociology of applied knowledge. Chicago: University of Chicago Press.
FTC (Federal Trade Commission). 2010. Federal Trade Commission complaint charges conspiracy to thwart competition in teeth-whitening services: North Carolina dental board charged with improperly excluding non-dentists. http://www.ftc.gov/opa/2010/06/ncdental.shtm (accessed September 29, 2010).
Furukawa, M. F., T. S. Raghu, and B. B. M. Shao. 2010. Electronic medical records, nurse staffing, and nurse-sensitive patient outcomes: Evidence from california hospitals. Health Services Research 45(4):941-962.
Goode, C. J., M. R. Lynn, C. Krsek, and G. D. Bednash. 2009. Nurse residency programs: An essential requirement for nursing. Nursing Economic$ 27(3):142-147, 159; quiz 148.
Goode, C. J., and C. A. Williams. 2004. Post-baccalaureate nurse residency program. Journal of Nursing Administration 34(2):71-77.
Graham, K., and M. Cvach. 2010. Monitor alarm fatigue: Standardizing use of physiological monitors and decreasing nuisance alarms. American Journal of Critical Care 19(1):28-34.
Groth, S. W., L. Norsen, and H. Kitzman. 2010. Long-term outcomes of advanced practice nursing. In Nurse practitioners: Evolution and future of advanced practice. 5th ed., edited by E. M. Sullivan-Marx, D. O. McGivern, J. A. Fairman, and S. A. Greenberg. New York: Springer. Pp. 93-110.
Halfer, D., and E. Graf. 2006. Graduate nurse perceptions of the work experience. Nursing Economic$ 24(3):150-155.
Hansen-Turton, T., A. Ritter, H. Begun, S. L. Berkowitz, N. Rothman, and B. Valdez. 2006. Insurers’ contracting policies on nurse practitioners as primary care providers: The current landscape and what needs to change. Policy, Politics, & Nursing Practice 7(3):216-226.
Hansen-Turton, T., A. Ritter, and R. Torgan. 2008. Insurers’ contracting policies on nurse practitioners as primary care providers: Two years later. Policy, Politics, & Nursing Practice 9(4):241-248.
Harris Interactive. 2008. New WSJ.com/Harris Interactive study finds satisfaction with retail-based health clinics remains high. http://www.harrisinteractive.com/NEWS/allnewsbydate.asp?NewsID=1308 (accessed August 6, 2010).
Hatem, M., J. Sandall, D. Devane, H. Soltani, and S. Gates. 2008. Midwife-led versus other models of care for childbearing women. Cochrane Database of Systematic Reviews (4):CD004667.
Hayes, L. J., L. O’Brien-Pallas, C. Duffield, J. Shamian, J. Buchan, F. Hughes, H. K. Spence Laschinger, N. North, and P. W. Stone. 2006. Nurse turnover: A literature review. International Journal of Nursing Studies 43(2):237-263.
HHS (Department of Health and Human Services. 2009. CMS and ONC issue regulations proposing a definition of ‘meaningful use’ and setting standards for electronic health record incentive program. http://www.hhs.gov/news/press/2009pres/12/20091230a.html (accessed September 29, 2010).
Hogan, P. F., R. F. Seifert, C. S. Moore, and B. E. Simonson. 2010. Cost effectiveness analysis of anesthesia providers. Nursing Economic$ 28(3):159-169.
Hooker, R., and L. Berlin. 2002. Trends in the supply of physician assistants and nurse practitioners in the United States. Health Affairs 21(5):174-181.
Horrocks, S., E. Anderson, and C. Salisbury. 2002. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 324(7341):819-823.
HRSA (Health Resources and Services Adminsitration). 2004. Supply, demand, and use of licensed practical nurses. Rockville, MD: HRSA.
HRSA. 2006. The registered nurse population: Findings from the National Sample Survey of Registered Nurses, March 2004. Rockville, MD: HRSA.
HRSA. 2008. The physician workforce. Rockville, MD: HRSA.
HRSA. 2010. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. Rockville, MD: HRSA.
Hughes, F., S. Clarke, D. A. Sampson, J. A. Fairman, and E. M. Sullivan-Marx. 2010. Research in support of nurse pracitioners. In Nurse practitioners: Evolution and future of advanced practice. 5th ed., edited by E. M. Sullivan-Marx, D. O. McGivern, J. A. Fairman, and S. A. Greenberg. New York: Springer. Pp. 65-92.
Huijbregts, P. A. 2007. Chiropractic legal challenges to the physical therapy scope of practice: Anybody else taking the ethical high ground? Journal of Manual & Manipulative Therapy 15(2):69-80.
Hunt, E., S. Sproat, and R. Kitzmiller. 2004. The nursing informatics implementation guide, edited by K. Hannah and M. Ball. New York: Springer-Verlag.
INQRI (The Blog of the Interdisciplinary Nursing Quality Research Initiative). 2010a. Interrupting a nurse can lead to errors. http://inqri.blogspot.com/2010_07_01_archive.html (accessed September 29, 2010).
INQRI. 2010b. Lessons learned from 9 states on building successful HAI reporting programs. http://inqri.blogspot.com/2010/08/lessons-learned-from-9-states-on.html (accessed September 29, 2010).
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2004. In the nation’s compelling interest: Ensuring diversity in the health care workforce. Washington, DC: The National Academies Press.
IOM. 2006. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2010a. A summary of the December 2009 Forum on the Future of Nursing: Care in the community. Washington, DC: The National Academies Press.
IOM. 2010b. A summary of the October 2009 Forum on the Future of Nursing: Acute care. Washington, DC: The National Academies Press.
Jha, A., J. Perlin, K. Kizer, and R. Dudley. 2003. Effect of the transformation of the Veterans Affairs health care system on the quality of care. New England Journal of Medicine 348(22): 2218-2227.
Johnson, C. 2010. Doctor shortage? 28 states May expand nurses’ role with doctor shortage, ‘Dr. Nurses’ seek bigger role in primary care; 28 states consider (April 13, 2010). http://abcnews.go.com/Health/wireStory?id=10363562 (accessed May 19, 2010).
Kahn, M. G., and D. Ranade. 2010. The impact of electronic medical records data sources on an adverse drug event quality measure. Journal of the American Medical Informatics Association 17(2):185-191.
Kerr, E., R. Gerzoff, S. Krein, J. Selby, J. Piette, J. Curb, W. Herman, D. Marrero, K. Narayan, M. Safford, T. Thompson, and C. Mangione. 2004. Diabetes care quality in the Veterans Affairs health care system and commercial managed care: The triad study. Annals of Internal Medicine 141(4):272-281.
Kimball, B., and E. O’Neil. 2002. Health care’s human crisis: The American nursing shortage. Princeton, NJ: RWJF.
King, E. S., and T. Hansen-Turton. 2010. Nurse-managed health centers. In Nurse practitioners: The evolution and future of advanced practice, edited by E. M. Sullivan-Marx, D. O. McGivern, J. A. Fairman and S. A. Greenberg. New York: Springer Publishing Company. Pp. 183-198.
Kovner, C. T., C. S. Brewer, S. Fairchild, S. Poornima, H. Kim, and M. Djukic. 2007. Newly licensed RNs’ characteristics, work attitudes, and intentions to work. American Journal of Nursing 107(9):58-70; quiz 70-51.
KP (Kaiser Permanente). 2010. Fast facts about Kaiser Permanente. http://xnet.kp.org/newscenter/aboutkp/fastfacts.html (accessed September 29, 2010).
Krozek, C. 2008. The new graduate RN residency: Win/win/win for nurses, hospitals, and patients. Nurse Leader 6(5):41-44.
Krugman, M., J. Bretschneider, P. Horn, C. Krsek, R. Moutafis, and M. Smith. 2006. The national post-baccalaureate graduate nurse residency program: A model for excellence in transition to practice. Journal for Nurses in Staff Development 22(4):196-205.
Kurtzman, E. T., E. M. Dawson, and J. E. Johnson. 2008. The current state of nursing performance measurement, public reporting, and value-based purchasing. Policy, Politics, & Nursing Practice 9(3):181-191.
Labor Management Partnership. 2010. San Diego’s home health care team sees more patients, faster. http://www.lmpartnership.org/node/344 (accessed September 29, 2010).
Laport, N., W. Sermeus, G. Vanden Boer, and P. Van Herck. 2008. Adjusting reimbursement for nursing care. Policy, Politics, & Nursing Practice 9(2):94-102, 103-111.
Laurant, M., D. Reeves, R. Hermens, J. Braspenning, R. Grol, and B. Sibbald. 2004. Substitution of doctors by nurses in primary care. Cochrane Database of Systematic Reviews(2):CD001271.
Lenz, E., M. Mundinger, R. Kane, S. Hopkins, and S. Lin. 2004. Primary care outcomes in patients treated by nurse practitioners or physicians: Two-year follow-up. Medical Care Research and Review 61(3):332-351.
The Lewin Group. 2009. Wisdom at work: Retaining experienced RNs and their knowledge—case studies of top performing organizations. Falls Church, VA: The Lewin Group.
Lugo, N. R., E. T. O’Grady, D. R. Hodnicki, and C. M. Hanson. 2007. Ranking state NP regulation: Practice environment and consumer healthcare choice. American Journal for Nurse Practitioners 11(4):8-24.
Lynaugh, J. E. 2008. Kate Hurd-Mead lecture. Nursing the great society: The impact of the Nurse Training Act of 1964. Nursing History Review 16:13-28.
Marsteller, J., Y.-J. Hsu, P. Pronovost, and D. Thompson. 2010 June 28. The relationship of nursing hours to ICU central line-associated bloodstream infections and length of stay. Poster presented at AcademyHealth Annual Research Meeting, Boston, MA.
McKinney, M. 2010. Alarm fatigue sets off bells: Mass. Incident highlights need for protocols check. Modern Healthcare 40(15):14.
Medoff-Cooper, B., J. Shults, and J. Kaplan. 2009. Sucking behavior of preterm neonates as a predictor of developmental outcomes. Journal of Developmental and Behavioral Pediatrics 30(1):16-22.
MedPAC (Medicare Payment Advisory Commission). 2006. Report to the Congress: Increasing the value of Medicare. Washington, DC: MedPAC.
MedPAC. 2008. Report to the Congress: Reforming the delivery system. Washington, DC: MedPAC.
MedPAC. 2009. Report to the Congress: Improving incentives in the Medicare program. Washington, DC: MedPAC.
Mehrotra, A., M. C. Wang, J. R. Lave, J. L. Adams, and E. A. McGlynn. 2008. Retail clinics, primary care physicians, and emergency departments: A comparison of patients’ visits. Health Affairs 27(5):1272-1282.
Mundinger, M. O., R. L. Kane, E. R. Lenz, A. M. Totten, W. Y. Tsai, P. D. Cleary, W. T. Friedewald, A. L. Siu, and M. L. Shelanski. 2000. Primary care outcomes in patients treated by nurse practitioners or physicians: A randomized trial. JAMA 283(1):59-68.
NACHC (National Association of Community Health Centers). 2009. America’s health centers. Bethesda, MD: NACHC.
NACHC, The Robert Graham Center, and Capital Link. 2007. Access granted: The primary care payoff. Washington, DC: NACHC, The Robert Graham Center, Capital Link.
Naylor, M. D., and E. T. Kurtzman. 2010. The role of nurse practitioners in reinventing primary care. Health Affairs 29(5):893-899.
NCSBN (National Council of State Boards of Nursing). 2008. Toward an evidence-based regulatory model for transitioning new nurses to practice. https://www.ncsbn.org/Pages_from_Leader-toLeader_FALL08.pdf (accessed September 13, 2010).
NCQA (National Committee for Quality Assurance). 2010. About NCQA. http://www.ncqa.org/tabid/675/Default.aspx (accessed July 9, 2010).
NNCC (National Nursing Centers Consortium). 2005. Fact sheet. Philadelphia, PA: NNCC.
NRHA (National Rural Health Association). 2010. What’s different about rural health care? http://www.ruralhealthweb.org/go/left/about-rural-health/what-s-different-about-rural-health-care (accessed September 13, 2010).
Office of Technology Assessment. 1986. Health technology case study 37: Nurse practitioners, physician assistants, and certified nurse-midwives: A policy analysis. Washington, DC: U.S. Government Printing Office.
Ohlhausen, M. K., M. R. Baye, J. Schmidt, and L. B. Parnes. 2007. Letter to Louann Stanton, September 27. Available from http://www.ftc.gov/os/2007/10/v070015massclinic.pdf.
Ohlhausen, M. K., M. R. Baye, J. Schmidt, and L. B. Parnes. 2008. Letter to Elaine Nekritz, May 29. Available from http://www.ftc.gov/os/2008/06/V080013letter.pdf.
ONS (Office of Nursing Services, Department of Veterans Affairs). 2009. VA nursing: Connecting all the pieces of the puzzle to transform care for veterans. http://www1.va.gov/NURSING/docs/OfficeofNursingServices-ONS_Annual_Report_2009-WEB.pdf (accessed March 27, 2010).
Pearson, L. 2010. The Pearson report: A national overview of nurse practitioner legislation and healthcare issues. http://www.pearsonreport.com/ (accessed June 26, 2010).
Pennsylvania Governor’s Office. 2009. Governor Rendell thanks “pioneers” for making Pennsylvania the national leader on chronic care management and creating patient-centered medi-
Phillips, R., L. Green, G. Fryer, and S. Dovey. 2001. Trumping professional roles: Collaboration of nurse practitioners and physicians for a better U.S. health care system. American Family Physician 64(8):1325.
Phillips, S. 2010. 22nd annual legislative update: Regulatory and legislative successes for APNs. Nursing Practice 35(1):24-47.
Poissant, L., J. Pereira, R. Tamblyn, and Y. Kawasumi. 2005. The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. Journal of the American Medical Informatics Association 12(5):505-516.
Roberts, K., and G. Hayes. 2005. The Harambee Nursing Center. Kentucky Nurse Oct-Dec. http://findarticles.com/p/articles/mi_qa4084/is_200510/ai_n15716986/.
Rosenstein, A. H., and M. O’Daniel. 2005. Disruptive behavior and clinical outcomes: Perceptions of nurses and physicians. American Journal of Nursing 105(1):54-64; quiz 64-55.
Rosenstein, A. H., and M. O’Daniel. 2008. A survey of the impact of disruptive behaviors and communication defects on patient safety. Joint Commission Journal on Quality and Patient Safety 34(8):464-471.
Rostant, D. M., and D. M. Cady. 1999. Liability issues in perinatal nursing. Philadelphia, PA: Lippincott Williams & Wilkins.
Rudavsky, R., C. E. Pollack, and A. Mehrotra. 2009. The geographic distribution, ownership, prices, and scope of practice at retail clinics. Annals of Internal Medicine 151(5):315-320.
RWJF (Robert Wood Johnson Foundation). 2010a. Map of the number of nurse practritioners per primary care doctor by county, 2009. http://thefutureofnursing.org/NursingResearchNetwork1 (accessed December 15, 2010).
RWJF. 2010b. Map of the number of physician assistants per primary care doctor by county, 2009. http://thefutureofnursing.org/NursingResearchNetwork2 (accessed December 6, 2010)
RWJF. 2010c. Nurse practitioners and physician assistants in the United States: Current patterns of distribution and recent trends. http://thefutureofnursing.org/NursingResearchNetwork7 (accessed December 6, 2010)
RWJF. 2010d. Sermo.com physicians’ opinions about the impact of allowing NPs to practice independently. http://thefutureofnursing.org/NursingResearchNetwork4 (accessed December 6, 2010)
RWJF. 2010e. Sermo.Com survey data on physicians’ opinions of nurse practitioners and nurses’ educational preparation. http://thefutureofnursing.org/NursingResearchNetwork8 (accessed December 6, 2010)
Safriet, B. J. 2010. Federal options for maximizing the value of advanced practice nurses in providing quality, cost-effective health care. Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix H on CD-ROM).
Sermo.com. 2009. Survey of U.S. Physicians indicates AMA no longer represents them. http://www.sermo.com/about-us/pr/07/july/3/sermo-survey-us-physicians-indicates-ama-no-longer-represents-them (accessed September 23, 2010).
Sia, C., T. Tonniges, E. Osterhus, and S. Taba. 2004. History of the medical home concept. Pediatrics 113(5):1473-1478.
Sorbel, A. L. 2010. Calif. doctors sue to ensure nurse anesthetists are supervised. http://www.amaassn.org/amednews/2010/02/22/prsa0222.htm (accessed September 10, 2010).
Staiger, D., D. Auerbach, and P. Buerhaus. 2000. Expanding career opportunities for women and the declining interest in nursing as a career. Nursing Economic$ 18(5):230-236.
Staiger, D. O., D. I. Auerbach, and P. I. Buerhaus. 2009. Comparison of physician workforce estimates and supply projections. JAMA 302(15):1674-1680.
Steinwald, B. 2008. Primary care professionals: Recent supply trends, projections, and valuation of services. Washington, DC: GAO.
Stevens, R. 1999. In sickness and wealth, American hospitals in the twentieth century. Baltimore, MD: The Johns Hopkins University Press.
Sullivan-Marx, E. M. 2008. Lessons learned from advanced practice nursing payment. Policy, Politics, & Nursing Practice 9(2):121-126.
Tai, T. W., S. I. Bame, and C. D. Robinson. 1998. Review of nursing turnover research, 1977-1996. Social Science and Medicine 47(12):1905-1924.
Thompson, D., P. Johnston, and C. Spurr. 2009. The impact of electronic medical records on nursing efficiency. Journal of Nursing Administration 39(10):444-451.
TIGER (Technology Informatics Guiding Education Reform). 2009. Testimony submitted to inform the Forum on the Future of Nursing: Community health, public health, primary care, and longterm care. Philadelphia, PA, December 3.
UHC (University HealthSystem Consortium). 2009. The UHC/AACN residency program. Oak Brook, IL: UHC. Available from https://www.uhc.edu/docs/003733604_NRP_brochure.pdf.
U.S. Census Bureau. 2010. State & county quickfacts. http://quickfacts.census.gov/qfd/states/00000. html (accessed August 19, 2010).
VA (Department of Veterans Affairs). 2007. VA employment brochures: Advanced practice nursing. http://www.vacareers.va.gov/Resources_Download/APN_Brochure_021210.txt (accessed September 29, 2010).
VA. 2009. Remarks by Secretary Eric K. Shinseki: Veterans Health Administration national leadership board strategic planning summit, Annapolis, MD, April 22, 2009. http://www1.va.gov/opa/speeches/2009/09_0422.asp (accessed March 27, 2010).
VA. 2010. VA benefits & health care utilization. http://www1.va.gov/VETDATA/Pocket-Card/4X6_summer10_sharepoint.pdf (accessed August 19, 2010).
Versant. 2010. The versant RN residency solution. http://www.versant.org/item.asp?id=81 (accessed September 29, 2010).
VHA (Veterans Health Administration). 2003. VHA vision 2020. http://purl.access.gpo.gov/GPO/LPS35526 (accessed September 29, 2010).
VHA. 2009. Quality initiatives undertaken by the Veterans Health Administration. http://www.cbo.gov/doc.cfm?index=10453&zzz=39420 (accessed March 25, 2010).
Waneka, R., and J. Spetz. 2009. 2007-2008 annual school report: Data summary and historical trend analysis. Sacramento, CA: California Board of Registered Nursing.
Whelan, E.-M. 2010. The importance of community health centers: Engines of economic activity and job creation. http://www.americanprogress.org/issues/2010/08/community_health_centers.html (accessed September 13, 2010).
Whelan, E., and L. Russell. 2010. Better health care at lower costs why health care reform will drive better models of health care delivery. http://www.americanprogress.org/issues/2010/03/health_delivery.html (accessed July 9, 2010).
White House. 2009. Remarks by the President to a joint session of Congress on health care on September 9, 2009. http://www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care (accessed September 29, 2010).
White House. 2010. Remarks by the President to the American Nurses Association. http://www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care (accessed June 26, 2010).
Williams, C. A., C. J. Goode, C. Krsek, G. D. Bednash, and M. R. Lynn. 2007. Postbaccalaureate nurse residency 1-year outcomes. Journal of Nursing Administration 37(7/8):357-365.
Yin, J. C., and K. P. Yang. 2002. Nursing turnover in Taiwan: A meta-analysis of related factors. International Journal of Nursing Studies 39(6):573-581.
Zysberg, L., and D. M. Berry. 2005. Gender and students’ vocational choices in entering the field of nursing. Nursing Outlook 53(4):193-198.
ANNEX 3-1
STATE PRACTICE REGULATIONS FOR NURSE PRACTITIONERS
TABLE 3-A1 State-by-State Regulatory Requirements for Physician Involvement in Care Provided by Nurse Practitioners
|
State |
Physician Involvement Requirement (for Prescription) |
On-Site Oversight Requirement |
Quantitative Requirements for Physician Chart Review |
Maximum NP-to-Physician Ratio |
|
Alabama |
MD Collaboration Required |
10% of the time |
10% of all charts, all adverse outcomes |
1 MD - 3 full-time NPs or max. total of 120 hours/week |
|
Alaska |
None |
None |
No |
N/A |
|
Arizona |
None |
None |
No |
N/A |
|
Arkansas |
MD Collaboration Required |
None |
No |
None stated |
|
California |
MD Supervision Required |
None |
No |
4 prescribing NPs - 1 MD |
|
Colorado |
None (although preceptor and mentoring period required for prescribing during the first 3,600 hours of prescriptive practice) |
None |
No |
5 NPs - 1 MD; board may waive restriction |
|
Connecticut |
MD Collaboration Required |
None |
No |
None stated |
|
Delaware |
MD Collaboration Required |
None |
No |
None stated |
|
Florida |
MD Supervision Required |
None |
No |
1 MD - no more than 4 offices in addition to MD’s primary practice location (If MD provides primary health care services) |
|
State |
Physician Involvement Requirement (for Prescription) |
On-Site Oversight Requirement |
Quantitative Requirements for Physician Chart Review |
Maximum NP-to-Physician Ratio |
|
Georgia |
MD Delegation Required |
None |
All controlled substance Rx w/in 3 mos of issuance of Rx, all adverse outcomes w/in 30 days of discovery, 10% of all other charts at least annually |
4 NPs - 1 MD |
|
Hawaii |
MD Collaboration Required* |
None |
No |
None stated |
|
Idaho |
None |
None |
No |
N/A |
|
Illinois |
MD Delegation Required |
At least once per month (no duration specified) |
Yes, periodic review required for Rx orders |
None stated |
|
Indiana |
MD Collaboration Required |
None |
Yes, at least 5% random sample of charts and medications prescribed for patients |
None stated |
|
Iowa |
None |
None |
No |
N/A |
|
Kansas |
MD Collaboration Required |
None |
No |
None stated |
|
Kentucky |
MD Collaboration Required |
None |
No |
None stated |
|
Louisiana |
MD Collaboration Required |
None |
No |
None stated |
|
Maine |
None (although supervision by a physician or nurse practitioner is required for first 24 months of NP practice) |
None |
No |
N/A |
|
Maryland |
MD Collaboration Required |
None |
Yes (percentage left to MD & NP discretion) |
None stated |
|
State |
Physician Involvement Requirement (for Prescription) |
On-Site Oversight Requirement |
Quantitative Requirements for Physician Chart Review |
Maximum NP-to-Physician Ratio |
|
Massachusetts |
MD Supervision Required |
None |
Yes (for Rx only - once every 3 months, percentage left to MD & NP discretion) |
None stated |
|
Michigan |
MD Delegation Required |
None |
No |
None stated |
|
Minnesota |
MD Delegation Required |
None |
No |
None stated |
|
Mississippi |
MD Collaboration Required |
At least once every 3 months |
Yes - a representative sample of either 10% or 20 charts, whichever is less, every month |
None stated |
|
Missouri |
MD Delegation Required |
NP must first practice for at least one month at same location of collaborating MD, after which time MD must be on-site once every 2 weeks |
Yes - once every 2 weeks |
3 FTE NPs - 1 MD |
|
Montana |
None |
None |
15 or 5% of charts, whichever is less, reviewed quarterly (may be reviewed by MD or NP peer) |
None stated |
|
Nebraska |
MD Collaboration Required |
None |
No |
None stated |
|
Nevada |
MD Collaboration Required |
Part of a day, once a month |
Yes (percentage left to MD & NP discretion) |
3 NPs - 1 MD |
|
New Hampshire |
None |
None |
No |
N/A |
|
New Jersey |
MD Collaboration Required |
None |
Yes - periodic review (percentage left to MD & NP discretion) |
None stated |
|
New Mexico |
None |
None |
No |
N/A |
|
State |
Physician Involvement Requirement (for Prescription) |
On-Site Oversight Requirement |
Quantitative Requirements for Physician Chart Review |
Maximum NP-to-Physician Ratio |
|
New York |
MD Collaboration Required |
None |
Yes at least once every 3 months (percentage left to MD & NP discretion) |
4:1 NPs to physicians (only applies if more than 4 NPs practice off-site) |
|
North Carolina |
MD Supervision Required |
None |
Yes (for initial 6 months of collaboration, must be review and countersigning by MD w/in 7 days of NP-patient contact & meetings of NP-MD on weekly basis for first month, & then at least monthly for next 5 months) |
None stated |
|
North Dakota |
MD Collaboration Required |
None |
No |
None stated |
|
Ohio |
MD Collaboration Required |
None |
Yes - periodic review (annually, percentage left to MD & NP discretion) |
3 NPs - 1 MD |
|
Oklahoma |
MD Supervision Required |
None |
No |
2 FTE NPs or max 4 PT NPs - 1 MD |
|
Oregon |
None |
None |
No |
N/A |
|
Pennsylvania |
MD Collaboration Required |
None |
Yes (percentage left to MD & NP discretion) |
4 NPs - 1 MD |
|
Rhode Island |
MD Collaboration Required |
None |
No |
None stated |
|
South Carolina |
MD Delegation Required |
None |
No |
3 NPs - 1 MD |
|
South Dakota |
MD Collaboration Required |
No less than one half day a week or 10% of the time |
Yes (percentage left to MD & NP discretion) |
4 NPs - 1 MD |
|
Tennessee |
MD Supervision Required |
Once every 30 days (no duration specified) |
20% of all charts every 30 days |
None stated |
|
State |
Physician Involvement Requirement (for Prescription) |
On-Site Oversight Requirement |
Quantitative Requirements for Physician Chart Review |
Maximum NP-to-Physician Ratio |
|
Texas |
MD Delegation Required |
For sites serving medically underserved populations: at least once every 10 days (no duration specified). 10% for designated alternative practice sites. |
10% of all charts |
3 NPs or FTE - 1 MD (for alternative practice sites, 4 - 1; can be waived up to 6 - 1) |
|
Utah |
MD Collaboration Required** |
None |
No |
None stated |
|
Vermont |
MD Collaboration Required |
None |
Yes (percentage left to MD & NP discretion) |
None stated |
|
Virginia |
MD Supervision Required |
MD must “regularly practice” at location where |
NP practices Yes - periodic review (percentage left to MD & NP discretion) |
4 NPs - 1 MD |
|
Washington |
None |
None |
No |
N/A |
|
West Virginia |
MD Collaboration Required |
None |
Periodic and joint review of Rx practice (no percentage specified) |
None stated |
|
Wisconsin |
MD Collaboration Required |
None |
No |
None stated |
|
Wyoming |
None |
None |
No |
None stated |
|
NOTES: For the purposes of this chart, “collaboration” includes all collaboration-like requirements (such as “collegial relationship,” etc.). FTE = full-time equivalent; MD = medical doctor; NP = nurse practitioner; PT = part time; Rx = prescription. * This requirement will be altered pending new rules in 2011. ** For controlled substance schedules II-III only. SOURCE: NNCC, 2009. Reprinted with permission from Tine Hansen-Turton, NNCC. Copyright 2009 NNCC. |
||||
REFERENCE
NNCC. 2009. NNCC’s state-by-state guide to regulations regarding nurse practitioner and physician practice 2009. http://www.nncc.us/research/ContractingToolkit/contractingtoolkitgrid.pdf (accessed December 6, 2010).














































































