5
Strategies to Build Capacity for Prevention, Treatment, and Care of HIV/AIDS in Africa
|
Key Findings
|
This chapter describes a variety of strategies to build capacity1 for prevention, treatment, and care of HIV/AIDS in Africa. Strategies for African governments and institutions as well as the United States (and other donor nations) are explored. First, however, the chapter provides a context for these strategies by briefly reviewing the present state of human resources for health care in Africa.
PRESENT STATE OF HUMAN RESOURCES FOR HEALTH CARE IN AFRICA
As discussed in Chapter 1, current resource constraints in donor nations and the growing HIV-related needs and demand for treatment in Africa are at odds. Lacking well-functioning health systems,2 African nations are ill prepared to confront the looming HIV/AIDS burden of 2020 to 2025. Accordingly, the international community must focus on enabling them to muster the necessary internal resources. A major requirement to this end is to strengthen health care systems, in particular by building institutional and human resource capacity.
The Health Workforce Crisis
Health workforces play a crucial role in achieving the United Nations’ Millennium Development Goals (MDGs). For example, the supply of health workers impacts the health of women and children. Yet only 5 of 49 low-income countries have the minimum 23 doctors per 10,000 inhabitants, recommended by the World Health Organization (WHO) (WHO, 2010a). Three major forces challenge the health workforce in Africa. First is the devastation of HIV/AIDS, increasing workloads, exposing workers to infection, and trying their morale. Second is accelerating labor migration, causing losses of nurses and doctors from countries that can least afford the “brain drain.” Third is the legacy of chronic underinvestment in human resources; frozen recruitment and salaries; and restricted public budgets, depleting work environments of basic supplies, drugs, and facilities (JLI, 2004). Continued underinvestment in the health care workforce is detrimental to staff morale and the ethos of care.
In addition to health workers being compensated insufficiently and asked to work under harsh conditions with few supplies and little support, an extreme imbalance exists in the distribution of credentialed health professionals among regions and countries (and by geographic location within the same country). The problem of insufficient human resources for health care is particularly acute in Africa, which bears 25 percent of the world’s burden of disease but is home to only 1.3 percent of the world’s health workforce (Commission for Africa, 2005; High-Level Forum on the Health MDGs, 2004). Currently, an estimated 750,000 health workers serve the 682 million people of sub-Saharan Africa, representing an extremely low health care provider-to-population ratio; by comparison, the ratio is 10 to 15 times higher in Organisation for Economic Co-operation and Development (OECD) countries (see Figure 5-1) (High-Level Forum on the Health MDGs, 2004).
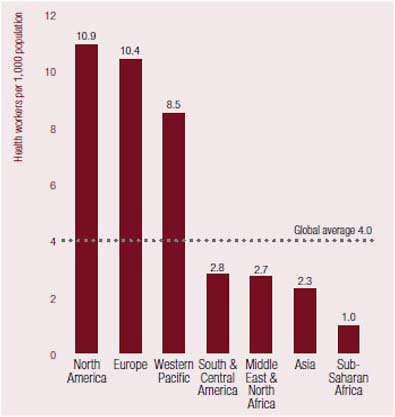
FIGURE 5-1 Health worker density by region.
SOURCE: JLI, 2004, compiled from WHO, 2004.
Any efforts to stabilize and improve health in the region must address this shortage of human resources for health care. Health care services cannot be delivered in the absence of a viable workforce. Any sustainable solution to Africa’s health problems will require a stable cadre of medical officers, nurses, clinical officers,3 dentists, and allied health workers—not only as clinicians, but also as teachers, managers, and leaders. A 2005 analysis of the human resource requirements of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) found that providing even 90 minutes of physician time per year to each of the 2 million patients on antiretroviral therapy (ART) would require about 20 percent or more of the existing physician workforce in 5 of the 14 PEPFAR countries (Ethiopia, Mozambique, Rwanda, Tanzania, and Zambia). The severity of the
human resource shortage was found to vary widely; some countries are much better positioned for a rapid scale-up of services than others (IOM, 2005c). The training of the necessary cadre of health workers, prepared and supported to confront their countries’ health issues, is a key challenge that all African nations must face (SAMSS, 2010).
The Lack of Education and Training
Educational systems of developing countries are a major impediment to the ongoing production and retention of health workers. Europe produces 173,800 physicians a year and Africa only 5,100 (see Figure 5-2) (Chen et al., 2004; JLI, 2004). One physician is produced for every 5,000 people in Central and Eastern
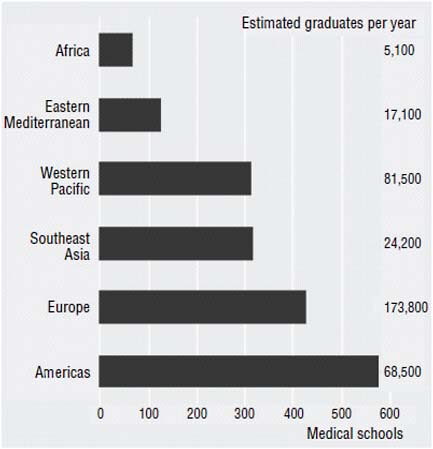
FIGURE 5-2 Regional disparities in numbers of medical schools and graduates.
NOTE: “Region” refers to World Health Organization (WHO) regions.
SOURCE: Eckhert, 2002; JLI, 2004.
Europe and the Baltic States, compared with one for every 115,000 people in Africa (IOM, 2005a). Similarly, the output of nurses in Africa lags far behind that in economically developed countries of the world. In 2005, for example, Cape Verde had only 100 nursing school graduates and Mozambique just 128, while in 2006, Guinea Bissau had only 62 (WHO, 2010b). The United States has one nurse for every 125 people, while Uganda has one nurse for every 5,000 people. And in all of Rwanda, there are only 11 pharmacists (IOM, 2005a).
Universities in low-income countries often face a number of challenges in meeting the need to educate and train the health workforce, including a lack of funds, weak infrastructure, outdated or misaligned training programs, overcrowded classrooms, and overburdened and underpaid staff (Dovlo, 2003; Tettey, 2006). For students in training, the shortage of teachers translates into little mentorship or academic support. Health program graduates are often ill equipped to perform the critical tasks for which they are needed and are unprepared to deal with the challenges of working in underresourced hospitals and clinics (IOM, 2009; Taché et al., 2008; WHO, 2006). The overall lack of opportunity and career advancement results in low morale, providing little incentive to work in academia or the public sector, or even to remain in the country (IOM, 2009).
STRATEGIES TO BUILD CAPACITY FOR PREVENTION, TREATMENT, AND CARE OF HIV/AIDS IN AFRICA
Governments and nongovernmental organizations in the United States and other donor countries and within Africa can help build capacity for prevention, treatment, and care of HIV/AIDS in Africa. This section details the gaps to be filled by partnering and the structures, systems, and professions necessary to implement partnerships and other capacity-building strategies, and describes promising strategies that can be implemented now by African nations and the United States to prepare for the long-term burden of HIV/AIDS in Africa.
Gaps to Be Filled by Partnering
Projects made possible through partnerships, including “twinning,”4 can fill a variety of gaps in current HIV/AIDS prevention, treatment, and care programs. With respect to teaching, for example, partnerships increase access to faculty experts currently in short supply in Africa. Partnerships can also:
-
facilitate the introduction of new, cutting-edge technologies for laboratories, informatics, logistics, communications, and teaching through training by partners more familiar with these innovations;
-
provide a consultation network offering access to high-level technical consultants for patient care in such areas as clinical care, pathology, radiography, and public health;
-
facilitate access to relatively rare clinical services, such as reference laboratory support for anatomic or clinical pathology (e.g., pathologic diagnosis of complications of HIV/AIDS);
-
enable electronic sharing of curricula and library resources;
-
provide access to professional development to improve the teaching ability of faculty;
-
assist in developing grant management capacities to enable African institutions to obtain support for operations research and evaluation;
-
provide training in operations research; and
-
provide resources to strengthen the entire health system, not just clinical services.
Structures, Systems, and Professions Necessary to Implement Partnerships and Other Capacity-Building Strategies
The objectives of HIV/AIDS partnerships depend on both the needs and interests of the host country and the resources available to the partner organizations. Careful consideration of the partners’ basic capacity is essential for sustainable and mutually beneficial partnerships. Each organization involved must have at least the minimum institutional capacity (including staff, capital, infrastructure, and funding) necessary to support the scope of the planned partnership (ICAD, 1999). If staffing is already stretched thin at one or both of the organizations prior to partnering, the endeavor should be reconsidered. Table 5-1 lists the common types of partnerships for capacity building.
Additionally, it is crucially important for the partners to engage within not only the cultural and contextual reality but also the governmental and national planning framework of the host country, as well as to coordinate with other organizations on the ground. Successful capacity building supports national health plans and health system development and is fundamentally based in and guided and led by host country partners—particularly since government capacity is itself crucial to the future course of the African HIV/AIDS epidemic.
Promising Strategies for Highly Affected Nations in Africa: Making the Most of Existing Capacities
Governments and nongovernmental organizations within Africa can build additional capacity for prevention, treatment, and care of HIV/AIDS by making
TABLE 5-1 The Partnership Continuum
|
Type of Partnership |
Description |
|
Short-term consultation/technical assistance |
A partnership involving the transfer of knowledge or skills from an organization in a developed, donor country to individual employees working for a partner organization in a developing country (Jensen et al., 2007). This transfer of knowledge and skills is accomplished through the provision of physical infrastructure (buildings, vehicles, and equipment), formal education and consultation, and training of staff at large (Jones and Blunt, 1999). |
|
Individual to individual |
A partnership involving training, coaching, and mentoring from an experienced individual to a less experienced individual through on-site shadowing, site visits, or telephone/Internet consultation (McCarthy et al., 2006). |
|
Institution to institution
|
A long-term collaboration between two organizations. Institutional partnerships are the basis for familiar, long-term relationships in which the partners share values and experiences (Dada et al., 2009). |
|
Government to government |
A partnering of national governments or subsets and agencies thereof, such as ministries of health, for the purpose of leadership strengthening and information sharing. These partnerships encourage effective “discharge [of the host country’s] responsibilities for stewardship and governance of country-level health systems” (Omaswa and Ivey Boufford, 2010) (Foreword). |
the most of existing capacities. This section highlights promising strategies that can be used to this end. These strategies fall into two broad categories: employing appropriate staffing models to optimize impact and utilizing the capacity of local institutions.
Appropriate Staffing Models to Optimize Impact
In many settings, HIV/AIDS prevention, treatment, and care are provided through complex, overburdened delivery systems that require specialist physicians. Yet many in need of these services live in rural settings, far from specialized care. To illustrate the point, Figure 5-3 shows that 67 percent of the cost of treatment is not for medication, but for the systems used to deliver it to patients and maintain them on it (UNAIDS, 2010a,b). Given increasing numbers of patients, shortages of trained medical personnel, and financial constraints, there is a need to provide services for HIV/AIDS more efficiently (UNAIDS, 2010b). The committee identified a number of strategies that could be implemented to achieve this goal: use of management and support staff, task sharing, harnessing of the informal health sector, use of modern information technology, analytic planning for the health workforce, and investment in women as health workers.
Management and support staff The 2008 Kampala Declaration and Agenda for Global Action recommended that “governments, civil society, [the] private sector, and professional organizations [work together] to strengthen leadership and management capacity at all levels” (WHO, 2008a). In addition to health care professionals, scale-up of HIV/AIDS prevention, treatment, and care programs must rely heavily on personnel from outside the clinical health sector who can
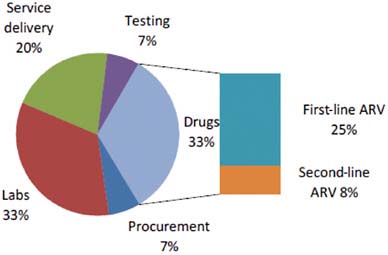
FIGURE 5-3 Breakdown of HIV/AIDS treatment costs in low- and middle-income countries.
NOTE: ARV = antiretroviral drug.
SOURCE: UNAIDS, 2010a.
TABLE 5-2 Imbalance in Health Worker Ratios
|
WHO Region |
Percentage of Total Health Workforce |
Ratio |
|
|
Health Service Provider |
Health Management and Support |
||
|
Africa |
83 |
17 |
4.9:1 |
|
Eastern Mediterranean |
75 |
25 |
3.0:1 |
|
South East Asia |
67 |
33 |
2.0:1 |
|
Western Pacific |
78 |
23 |
3.4:1 |
|
Europe |
69 |
31 |
2.7:1 |
|
Americas |
57 |
43 |
1.3:1 |
|
The World |
67 |
33 |
2.0:1 |
|
SOURCE: Dare, 2010. Adapted from WHO, 2006. |
|||
free up time for health care providers to perform clinical work. For example, laboratory technicians can play an essential role in the administration and monitoring of ART. Other types of personnel with needed competencies include, for example, nutritionists; counselors; behavioral specialists; management personnel; information technologists; procurement and distribution professionals; drug regulatory professionals; data analysts; and experts in monitoring, evaluation, and operations research.
Furthermore, it is important that management and support functions be performed by personnel with expertise in those roles and not by clinical service providers, whose time is much better spent attending to medical matters. Yet as Table 5-2 shows, there is a global imbalance in health worker ratios. In the Americas, the ratio of clinical service providers to management and support staff is almost 1:1; in Africa, that ratio is almost 5:1 (Dare, 2010; WHO, 2006). A considerable increase in clinical care could be delivered without adding more clinicians if the management and support capacity of others in HIV/AIDS prevention, treatment, and care were increased.
Task sharing Sharing of roles and responsibilities is not a new concept in the provision of health care; realignment of roles and responsibilities has been a long-standing response to changing health care needs, particularly in emergency situations or underserved areas.5 As a result of the HIV/AIDS crisis, the concept has reemerged with increased urgency. One term used to describe shared or realigned responsibilities is “task shifting.” WHO defines task shifting as
the process whereby specific tasks are transferred, when appropriate, to health workers with less training and fewer qualifications (WHO, 2008c). Although this term does not adequately encompass the concepts of realignment and recognition of appropriate responsibility, it does capture a narrower and sometimes temporary arrangement to meet emergency needs. The underlying assumption is that shifting specific tasks enables more efficient use of existing human resources and eases bottlenecks in service delivery. When additional human resources are needed, task shifting may also involve the delegation of some clearly delineated tasks to newly created cadres of health workers who receive specific competency-based training (WHO, 2008c).
The delegation of the health care responsibilities of nurses, physicians, clinical officers, dentists, and other health professionals to others, including community health workers, has been effective in addressing the severe human resource shortages in many African countries (Buchan and Poz, 2003; Glenngård and Anell, 2003; Morris et al., 2009). Because these responsibilities require not only skills but also relevant knowledge, this delegation goes beyond the mere performance of specific tasks. The committee has therefore elected to use the term “task sharing” rather than “task shifting” in this report. Task sharing that is needs-based, is not hierarchical or territorial, and allows roles to expand or contract according to need is the most appropriate approach to health care delivery in low-resource environments.
Health workers who are normally viewed as auxiliary are increasingly becoming the main providers of health services in many countries. In Africa, for example, nurse aids, medical assistants, and clinical officers are performing essential medical tasks, especially in rural areas. A good example is Malawi, where clinical officers are a major resource, performing surgical procedures and administering anesthesia, as well as providing medical care (Hongoro and McPake, 2004).
Another example is South Africa, where the unprecedented challenges of people requiring care and treatment for HIV/AIDS are forcing a rethinking and reorganization of health resources and health systems and a reappraisal of the role of nurses in care for complex and chronic illnesses. South Africa’s health system has historically been nurse driven, and nurses outnumber physicians five to one. Yet while the majority of the population receives formal health care from nurses rather than doctors, it is clear that nurses have been insufficiently empowered, resourced, and compensated to carry out their key roles effectively (Dohrn et al., 2009). Developing HIV/AIDS expertise among nurses has become a national priority, as is illustrated in South Africa’s National HIV/AIDS Strategic Plan (South African Department of Health, 2006). Accordingly, the South African Department of Health initiated new certificate courses in prevention of mother-to-child transmission (PMTCT) and ART for nurses in 2002 (Dohrn et al., 2009). The new ““PMTCT nurses’’ and ““ART nurses’’ are the unofficial gatekeepers of HIV/AIDS knowledge and skills at the primary health care level.
They direct HIV testing and counseling services, prepare patients for ART initiation, diagnose and manage side effects and opportunistic infections, partner with midwives to provide PMTCT services during the perinatal period, and provide early infant diagnostic services. They are trained to refer patients ready for ART initiation and those with advanced illness and complications (Dohrn et al., 2009; Morris et al., 2009).
A recent randomized controlled trial in South Africa compared nurse and physician management of HIV-infected patients receiving ART at two South African primary care clinics and found that primary health nurses were noninferior to doctors in monitoring of first-line ART (Sanne et al., 2010). The inclusion of PMTCT and ART initiation programs in health service basic training programs within African institutions of higher education (rather than during in-service training) could alleviate much of the need for posteducation in-service training and prepare graduates who can enter the workforce capable of initiating and managing ART and related complications.
The expansion of the numbers and roles of auxiliaries whose qualifications are not internationally recognized appears to be a quiet success story, providing large numbers of health workers who keep the system running in a number of countries (Hongoro and McPake, 2004). These alternatives are worth investigating given that there is a long lead time to increase the health care workforce. Depending on the type of degree and the specific country, the amount of training required can vary. For example, in South Africa it takes 4 years to train nursing or midwife students, 2 years to train pupil nurses, and 1 year to train pupil nursing auxiliaries (South African Nursing Council, 2010). By contrast, in Mozambique basic nurses are educated to grade 10 and have an additional 18 months of training; medium nurses are also educated to grade 10, but receive an additional two and a half years of training thereafter; and superior nurses are educated through grade 12 and must graduate from a 4-year university with a baccalaureate degree (August-Brady, 2010). As with nurses, the amount of training required for physicians varies by country. In Mozambique it takes a medical student 7 years to attain a medical degree (Ferrinho et al., 2010). In South Africa, medical school courses last 5 years (University of KwaZulu-Natal, 2010), followed by 2 years of internship and 1 year of community service, for a total requirement of 8 years to become a practicing physician.
Task sharing may not be readily accepted by various professions. Physicians and pharmacists have objected to the delegation of their tasks to those whom they perceive as professionals with less specialized training, while nurses have resisted taking on physicians’ roles without commensurate salary increases. Policies to enable task sharing, such as remuneration packages and clear job descriptions and strategic plans delineating professional boundaries and responsibilities, need to be established (Zachariah et al., 2009). The pivotal issue for the sustainability of task sharing will be how governments and international and bilateral organizations help prepare health systems to implement the practice, develop adequate
understanding of existing capacity, and make full use of existing roles and personnel. African government regulations supportive of task sharing would help optimize the impact of heath care workers in low-resource contexts. National governments also must garner the support of the various stakeholders who affect and are affected by the reconfiguration of tasks (such as professional bodies and associations; trade unions; ministries of health, education, finance, and public service; nongovernmental and community organizations; and local health structures). Otherwise, task sharing will exist on the political and organizational periphery of the formal health system; be exposed to shifts in policy and funding; and become fragile and unsustainable, further depleting a demoralized health system.
Harnessing of the informal health sector Home-based care of patients is becoming increasingly important in many societies, particularly where health facilities are overwhelmed by HIV/AIDS, and patients are returned to their homes to be cared for or await death (Omaswa, 2006). The care provided in the home by unpaid and untrained family members and friends and neighbors of those living with HIV/AIDS is not linked with any formal care or support services.6 Up to 90 percent of care for the ill is provided by this unlinked system of home care (Ogden et al., 2004; Uys, 2003). This care is provided primarily by women and is largely overlooked in both governmental and nongovernmental efforts to mitigate the impact of the epidemic (Ogden et al., 2004).
In a number of African countries with high HIV/AIDS prevalence, overburdened health systems, and a lack of resources (including hospital beds and health workers), the option of treating HIV/AIDS patients at home can be attractive to governments (Avert, 2010). One South African hospital reported that patients’ average stay decreased from 14 days to 3.5 days when they were referred to a home-based care organization (Fox et al., 2002). Home-based community care allows clinics and hospitals to minimize patient admissions; lowers the costs of health services and hospitalizations; and alleviates the pressures on clinic and hospital staff, enabling them to serve other clients (Ogden et al., 2004).
In addition to unlinked home-based care, a significant proportion of health care is provided in commercial settings such as markets, shops, and elsewhere in many African communities. Vendors are regularly called upon to advise purchasers on the effects of the health products they sell and how the products should be used. In many cases, these merchants and shopkeepers interview buyers, take medical histories, and proceed to diagnose and prescribe. Where formal health care facilities are not easily accessed, this group of informal health workers is the first and most important point of call for people in search of health services (Omaswa, 2006).
It is estimated that some 70 percent of Africans access traditional healers
(Mills et al., 2006). In rural South Africa, over 60 percent of the population seeks health advice and treatment from traditional healers before visiting a physician (AMREF, 2010). Thus, the strategy of partnering with traditional healers and bringing them into the formal health system should be considered. Indeed, rather than ostracizing traditional healers, WHO has advocated for their inclusion in national HIV/AIDS programs since the early 1990s; in 1994, WHO suggested upgrading traditional healers’ skills rather than training a new cadre of health workers (UNAIDS, 2000). In the future, it may be important to provide forums where biomedical practitioners and traditional healers can share experiences and be trained together so they can become sources of mutual referral.
Informal health workers are found in every health system, and the impact of their role increases as the strength of the formal sector weakens. Unlinked health care providers—such as those providing home-based care, informal drug vendors, and traditional healers—play important roles in some communities and deserve to be acknowledged, encouraged, and supported (Omaswa, 2006).
Use of modern information technology Recent advances have resulted in a dramatic increase in the use of information and communication technology (ICT) applications in health care, collectively known as “e-Health” (WHO, 2010c). e-Health applications, including teleconsultations, telereferrals, forward-storage concepts (e.g., teleradiology and teleprescriptions), and electronic patient records, can directly support training of community health workers, prevention, patient diagnosis, and patient management and care (WHO, 2007b).
Cellular and smart phones, for example, can be used to increase the efficiency of overburdened health workers, extending their reach by overcoming barriers of distance and time. Box 5-1 provides examples of how smart phone technology is being used to improve case management and drug tracking. Modern ICT can also facilitate distance learning. Web-based or electronic applications can deliver training to health workers on an asynchronous (i.e., not in real time) and independent basis. Such distance learning models offer cost savings because they do not require dedicated lecturers or administrators, nor do they incur travel or lodging expenses or require trainees to spend time away from their jobs (Accordia Global Health Foundation, 2010). In addition to these technologies, clinical teaching labs with simulation mannequins for self-teaching of clinical skills, as well as computerized scenarios and self-teaching guides, could be considered for training the African health care workforce.
Analytic planning for the health workforce The 2008 Kampala Declaration and Agenda for Global Action called for governments to “determine the appropriate health workforce skill mix” and “create health workforce information systems, to improve research and to develop capacity for data management in order to institutionalize evidence-based decision-making and enhance shared learning” (WHO, 2008a, pp. 10–11). Similarly, the 2010 World Health Assembly encour-
|
BOX 5-1 Smart Phones for Health Worker Efficiency: eMOCHA and SmartTrack eMOCHA is a free open-source application developed by the Johns Hopkins Center for Clinical Global Health Education. It is designed to assist health programs in developing countries in improving provider communication, education, and patient care by coordinating wireless devices with local server-based clinical training and patient care support services (eMOCHA, 2010). eMOCHA combines the power of wireless mobile collection of patient data and the capacity of the new Android-supported devices to display high-quality interactive touch screen forms, as well as video and audio files, with the power of server-based applications. These capabilities make it possible to analyze and map large amounts of data from the community and to create new training content in a variety of formats (eMOCHA, 2010). SmartTrack is another example of how cellular phones can assist with the management of HIV/AIDS programs. SmartTrack is a telehealth project aimed at addressing the problem of theft and counterfeiting of HIV/AIDS medications. The goal is to create a highly reliable, secure, and ultra-low-cost cell phone–based distributed drug information system that can be used to track the flow and consumption of antiretroviral drugs, as well as monitor how patients respond to treatment (Michael et al., 2009). The project, supported with financing, hardware, and software by Microsoft Research, is a collaborative effort of New York University’s Computer Science Department and School of Medicine and the West Africa AIDS Foundation in Ghana (Microsoft Corporation, 2008). |
aged member states “to establish or strengthen and maintain … health personnel information systems … to collect, analyze and translate data into effective health workforce policies and planning” (WHO, 2010d, p. 6). The African health workforce needs to be planned on the basis of projected needs (IOM, 2005c). Such planning must be done jointly, involving not only ministries of health but also ministries of education, finance, public service, and labor. Additionally, the private sector and the academic and medical communities should be brought to the table.
Begun in 2002 as a project to track the supply and deployment of Kenya’s nursing workforce, the Kenya Health Workforce Information System (KHWIS) is today a comprehensive health workforce surveillance system that provides regulatory and staffing data on Kenya’s nurses, doctors, dentists, midwives, clinical officers, and laboratory technicians and technologists. The project represents an ongoing collaboration among the Government of Kenya’s Ministry of Medical Services; the Ministry of Public Health and Sanitation; and the professional nursing, medical, laboratory, and clinical officer councils. The Lillian Carter
Center for International Nursing at Emory University and the U.S. Centers for Disease Control and Prevention (CDC) provide ongoing technical assistance (Kenya Health Workforce Information System, 2010). A promising example of building African capacity for analytic planning of the health workforce, the project created a database, installed computer and satellite equipment, and trained data entry personnel on a computerized system that includes every Kenyan nurse licensed from 1960 to the present. For such efforts to be useful, they must be supported by trained statistical staff who can focus on such issues as assessment of data quality; accommodation of missing data; and estimation of temporal, geographic, and demographic trends. Developing information systems requires not just collecting data, but also sufficiently training staff in the use of systems and data analysis.
KHWIS installed hardware at the Ministry of Health offices in Nairobi and at the provincial level to facilitate the collection of deployment data. The nursing supply and regulatory database was linked with the health facility and deployment database at the Department of Nursing in the Ministry of Medical Services in Nairobi, allowing the chief nursing officer to access information on nursing workforce supply and demand. The system provides for national coordination of data collection for the entire nursing profession, a capability lacking even in industrialized countries such as the United States and the United Kingdom (Nursing Sector Study Corporation, 2004); the availability of this information provides an evidence base for decision makers on human resources for health (Riley et al., 2007). In 2009, the project was extended to other health professional cadres; it is now creating regulatory databases to track the supply of physicians, dentists, laboratory workers, and clinical officers in Kenya (Emory University School of Nursing, 2010).
Using data from the KHWIS, the Government of Kenya supported studies aimed at evaluating the country’s health worker training capacity, the outcome of public–private partnerships with respect to the distribution of nurses and the subsequent effect on health services, and the impact of outmigration on Kenya’s nursing workforce. Officials in Kenya’s health ministry have also used information from the KHWIS to determine facility placements for newly hired personnel and identify staff qualifying for promotion, as well as employees needing to upgrade their skills (Kenya Health Workforce Information System, 2010).
Investment in women as health workers Investing in the training and education of women as health workers can have both direct and indirect positive impacts on HIV/AIDS. The direct impact is that of building the health workforce for enhanced service provision to those living with HIV/AIDS. The indirect impact is the positive downstream effect on both the health of the women themselves (a significant benefit given that women account for nearly 60 percent of HIV infections in Africa [UNAIDS, 2008]) and the health of their families and communities. Educational achievements of women can have ripple effects within
the family and across generations (Belhadj and Touré, 2008) because educated women can recognize the importance of health care and know how to seek it for themselves and their children (UNFPA, 2005).
Employing women in the health workforce and thereby providing them with income has further downstream benefits. Increasing women’s income has a positive impact on the educational and nutritional status of their children (Littlefield et al., 2003; Rogers and Youssef, 1988). Similarly, women’s unmet contraceptive needs have been shown to decrease significantly with educational level and paid employment (Al Riyami et al., 2004). The ability to earn a decent income empowers poor women in many aspects of their lives, influencing sexual and reproductive health choices, education, and healthy behavior (UNFPA, 2007).
Utilization of the Capacity of Local Institutions
Existing local African institutions hold great potential for mitigating the future impact of the HIV/AIDS burden. The capacity of these local resources—including South–South partnerships and regional collaborations, African science academies, national public health institutes, and health resource partner institutions—should be recognized and exploited.
South–South partnerships and regional collaborations with universities and other training programs South–South partnerships and regional collaborations can be a highly effective model for diffusing successful practices. Natural partners for such collaborations include universities; public health, nursing, and medical schools; technical and vocational institutions (which serve as major sources of education and training for ancillary health workers, including the array of technicians who form the backbone of any health care system, such as laboratory technicians, X-ray technicians, and procurement specialists); and other academic training programs. Chapter 4 addresses the role of technical/vocational schools and universities in creating the health workforce of the future.
An example of a South–South partnership is a model developed by Partners in Health to build human capacity for HIV/AIDS and primary health care services in Haiti and Lesotho. Because these two countries face similar human resources challenges, they are well suited to collaboration (Ivers et al., 2010). The partnership emphasizes providing community-based support to people living with HIV/AIDS and other diseases, recruiting and training paid community health workers in each country, developing human capacity, and scaling up services in collaboration with ministries of health (Ivers et al., 2010).
Another example of a South–South partnership is the Leadership Initiative for Public Health in East Africa (LIPHEA). LIPHEA recognizes that the health workforce in the developing world is unable to meet current health challenges, especially in the area of public health leadership. The initiative aims to strengthen the capacity of Uganda’s Makerere University School of Public Health
(MUPH) and Tanzania’s Muhimbili University College of Health Sciences to provide training for public health leaders, not just in Uganda and Tanzania but throughout east Africa. The goal is to establish long-term partnerships between academic institutions in the United States and east Africa and to provide substantial assistance to east Africa through curriculum revision; the development of in-service, short-term training for public health practitioners; the development of faculty who can prepare the next generation of public health professionals for national and regional public health systems; and reduction of the “brain drain” by improving professional development opportunities for public health leaders (LIPHEA, 2010).
A number of unique challenges must be overcome in creating South–South partnerships in Africa. One of these challenges is that Africans from different countries may have difficulty working together for several reasons: (1) partners from the same continent may still have cultural differences, (2) the lack of human and institutional resources is often a greater challenge for a South than for a North (developed-country) assisting partner, and (3) engaging the U.S. government team in the country in which the assisting partner is located is often challenging when the recipient partner is in a different country, because the U.S. government team does not see the benefit to its country program (Conviser, 2009). In addition, the “stovepiping” of PEPFAR funds to various African countries and to U.S. government agencies makes it difficult to undertake cooperative, multicountry projects.
African science academies Science academies, especially in resource-poor countries, are a unique resource for improving the effectiveness of a country’s policies and programs involving an aspect of science, medicine, or engineering. While more economically developed countries typically have large numbers of scientists in government to call upon, the scientific capacities of less economically developed countries are more thinly spread. This situation makes it desirable to engage expertise beyond government scientists in formulating policy and implementing programs. Moreover, while scientific expertise from the international development community can be plentiful, in-country advice has particular advantages with respect to trust, contextual understanding, and sustainability (Kelley, 2009).
Unlike many sources that policy makers can tap for advice, science academies have the capability to provide balanced, multidisciplinary, authoritative, and culturally appropriate advice that is valued for its unbiased, evidence-based approach. African science academy members and those scientists appointed to academy deliberative committees tend to be the most well-known and -respected scientists and scholars in the country. As such, they are often known to the country’s political leaders (Kelley, 2009). A science academy operates in a manner that is apolitical and not motivated by profit, which adds to its credibility. Likewise, most science academies receive some government funding but maintain independence from such benefactors (Hassan and Schaffer, 2009), receiving grants from private sources (Nature, 2010). African science academies can therefore offer
an independent, credible perspective on politically charged issues (Hassan and Schaffer, 2009; Nature, 2010).
For example, the HIV/AIDS, TB and Nutrition report released in 2007 by the Academy of Science of South Africa (ASSAf) played a timely and important role in informing South African policy. ASSAf published the report when the South African Ministry of Health was taking nonscientific positions. The report was commissioned to review the scientific evidence on the dynamics of the interaction of HIV, tuberculosis (TB), and nutrition. The study panel found a dearth of data on the influence of nutrition on HIV and TB (ASSAf, 2007). The report’s findings and its recommendations concerning the urgent need for research in this area were able to correct the government’s prevailing misunderstandings.
Since 1986, the Institute of Medicine (IOM) has produced a series of 26 reports on various aspects of HIV/AIDS, beginning with Confronting AIDS: Directions for Public Health, Health Care, and Research (IOM, 1986). Other reports followed, such as HIV and the Blood Supply: An Analysis of Crisis Decision Making, on blood safety and HIV (IOM, 1995); Review of the HIVNET 012 Perinatal HIV Prevention Study, on the effectiveness of nevirapine in PMTCT (IOM, 2005b); and Healers Abroad: Americans Responding to the Human Resource Crisis in HIV/AIDS, addressing the crisis in human resources for health (IOM, 2005a). These reports demonstrate the range of questions that a science academy can usefully address.
The committee sees promise in the African science academies’ emerging role in science and health policy at the country level, although there is much work to be done before they can become strong, self-sufficient institutions. In contrast to the high visibility of the U.S. National Academies, science academies in Africa tend to be less well funded, less active, less visible, and fewer in number (Nature, 2006). To address this problem and assist in building the capacity of African science academies, the U.S. National Academy of Sciences launched the African Science Academy Development Initiative (ASADI) (Hassan and Schaffer, 2009). ASADI’s vision is to develop the capacity of African science academies so they will be regarded as trusted, credible sources of scientific advice in their respective countries (ASADI, 2008). African science academies can help bridge the gaps among technology, information, and health impact in Africa, and as they continue to evolve, their positive impacts will continue to grow.
National public health institutes National public health institutes (NPHIs) are science-based governmental organizations, such as CDC in the United States, FIOCRUZ (Fundação Oswaldo Cruz) in Brazil, RIVM (National Institute for Public Health and the Environment) in the Netherlands, and CDC in China, that provide expertise and leadership for core public health functions, including research, disease surveillance, outbreak investigation, laboratory science, policy formulation, and health education and promotion. NPHIs vary in scope, function, and size, ranging from fledgling institutes to organizations with comprehensive responsi-
bility for research, programs, and policy for almost all public health threats. Most NPHIs, including the U.S. CDC, began as focused public health or research institutes charged with identifying and combating infectious disease threats. Over time, CDC and many other NPHIs in mid- to higher-resource countries have evolved and expanded to meet new public health challenges, including death and disability from chronic diseases, environmental and occupational threats, and injury prevention. The growth of NPHIs over the years—including both their successes and failures—provides an important frame of reference for those contexts with more limited current capacity in considering how to move forward (IANPHI, 2010; IOM, 2009).
Coordinating core public health functions through NPHIs can result in more efficient use of resources, improved delivery of public health services, and increased capacity to respond decisively to public health threats and opportunities. NPHIs are particularly beneficial in low-resource countries, where they provide public health professionals with a group of technically oriented colleagues and a prestigious career path, helping to stem the tide of experts leaving government service for higher-paying jobs with international nongovernmental organizations. NPHIs in low-resource countries also encourage governments to set science-based public health priorities and policies, better integrate and leverage funds from numerous vertical programs, and plan strategically and systematically for future human resource and infrastructure needs (IANPHI, 2010; IOM, 2009).
Moving NPHIs toward more technical depth and comprehensive capacity is the primary goal of the International Association of National Public Health Institutes (IANPHI). IANPHI serves as a professional organization for NPHI directors, assisting them in their professional and institutional growth through scientific meetings, leadership development activities, and seed grants for research and training. IANPHI’s fundamental philosophy is that the collective history, knowledge, and scientific expertise of its member institutes is a powerful force for transforming public health systems in low-resource countries (IANPHI, 2010; IOM, 2009).
IANPHI is collaborating with nine low-resource countries to create new NPHIs or substantially increase capacity at fledgling institutes. Its nine long-term NPHI development sites include Burkina Faso, Ethiopia, Guinea Bissau, Mozambique, and Tanzania, with projects being explored in Bangladesh, Cambodia, Central America, and Ghana. In addition to its strategic investments of up to $670,000 in each of the nine long-term project sites, IANPHI leverages substantial strategic planning and organizational design expertise, scientific technical assistance, and public health training for each project from other IANPHI members. For example, Guinea Bissau received technical assistance and training from Brazil; Finland is providing technical assistance and training to Tanzania; the Netherlands and Norway have committed to providing assistance to Ethiopia; and Morocco has pledged technical assistance and training to Burkina Faso. In addition, IANPHI links each project with the specialized expertise of other part-
ners, including WHO, and with key funders and programs, including the Health Metrics Network, the Global Fund, bilateral aid groups, and the U.S. government (IANPHI, 2010; IOM, 2009).
Health resource partner institutions in countries and regional networks The health and HIV/AIDS operating environment in countries (and globally) is complex and challenging. Ensuring country leadership and stewardship of the African continental response to HIV/AIDS requires the support of institutions in other countries to ensure that the HIV/AIDS agenda is permanently visible and that needed resources are mobilized both internally and externally and properly utilized. Examples of such institutions include advocacy groups, universities, science academies, professional associations, think tanks, businesses, and media. Governments are encouraged to work closely with these health resource partner institutions to strengthen national health systems for advocacy and oversight of HIV/AIDS programs, as well as the programs’ integration into broader health and national development plans. At the regional level, networks of such groups already exist. For example, Equinet supports country networks of community-based health care providers, while the African Health Systems Governance Network, created in 2009 and based at the African Center for Global Health and Social Transformation (ACHEST), supports a regional network of institutions that promote better stewardship and governance of health in Africa.
Another example of a regional network is the WHO global network of collaborating centers in nursing and midwifery, whose primary responsibility is to support the regional WHO offices and the headquarters office in Geneva in achieving the MDGs. In addition to working as individual units, the centers are encouraged to maximize opportunities by working together as a network (Parfitt, 2010). More than 40 centers worldwide work in the following areas:
-
Capacity building—For example, the WHO African Regional Office provided support to the University of South Africa in publishing the first African journal for nursing and midwifery researchers in the region (WHO, 2001).
-
Collaborative research projects—An example is a joint research project between South Korean and Thai universities in community action research (WHO, 2001).
-
Interregional initiatives—The Pan American Network for Nursing and Midwifery Collaborating Centers emphasize North–South collaborations such as that between the University of Illinois in the United States and the University of Botswana (WHO, 2001).
Strategies for the United States: Supporting Partnerships and Other Capacity-Building Programs
The United States and other donor nations can support a number of strategies in an effort to strengthen health systems, develop African institutions, and build long-term capacity so Africa can move forward independently toward a sustainable and healthier future. These strategies include institutional partnerships and other capacity-building programs.
Institutional Partnerships
A variety of institutions have engaged in partnerships to combat the burden of HIV/AIDS in Africa. Examples of partnerships between the public and private sectors, faith-based organizations (FBOs), militaries, and academic institutions are described below.
Public–private partnerships PEPFAR defines a public–private partnership as a “collaborative endeavor that combines resources from the public sector with resources from the private sector to accomplish the goals of HIV/AIDS prevention, treatment and care” (PEPFAR, 2009). Such partnerships contribute to the fight against HIV/AIDS by bringing outside resources to areas of local need. They ensure sustainability of programs by enhancing the skills and capacities of local organizations; increasing the public’s access to the unique expertise and core competencies of the private sector; facilitating scale-up of proven, cost-effective interventions through private-sector networks and associations; expanding the reach of interventions by accessing target populations (for instance, through workplace programs); and sharing program costs and promoting synergy in programs. Additionally, partners make in-kind contributions that otherwise would be beyond the reach of implementers (PEPFAR, 2009).
There are many examples of successes achieved by such partnerships. In 2007, for example, PEPFAR—through CDC and Becton, Dickinson and Company (BD), a leading global medical technology company with laboratory expertise—launched a 5-year public–private partnership to improve overall laboratory systems and services in African countries severely affected by HIV/AIDS and TB (CDC, 2010). The partnership’s implementation strategy includes three key components developed in collaboration with ministries of health, national reference laboratories, and implementing partners:
-
country-specific laboratory strengthening programs based on national laboratory strategic plans,
-
fellowship programs for BD associates to work closely with implementing partners, and
-
short-term technical assistance by both BD and PEPFAR partners to provide laboratory training and develop a framework to reach all levels of laboratory service.
The collaboration is greatly expanding the amount of laboratory training offered to all PEPFAR-supported countries in Africa, and is increasing the number of health care workers trained to provide quality HIV testing and improved TB diagnostics (CDC, 2010).
In Uganda, this partnership between PEPFAR and BD implements laboratory quality management training for all laboratories performing CD4 testing and is assisting in the development of a specimen referral system for the National Tuberculosis Reference Laboratory (NTRL). To support the NTRL, the partnership uses Global Positioning System/geographic information system (GPS/GIS) technology for mapping multiple laboratory sites to develop a transportation network and monitor specific improvements in the identified laboratories (CDC, 2010).
Corporate partnerships also exist to increase African capacity for prevention of HIV/AIDS. One example is the Safe Blood for Africa program in Nigeria—a partnership among the Nigerian Ministry of Health, CDC, the U.S. Agency for International Development (USAID), and ExxonMobil. Since 2003, the program has trained more than 1,000 blood service and health care staff in how to ensure a safe blood supply. With the support of ExxonMobil, the program has provided HIV test kits to hospitals in areas of Nigeria where there previously was no capacity to conduct even minimal testing (Safe Blood for Africa Foundation, 2008).
Corporate commitment to the prevention of HIV/AIDS is also evidenced by the commitment of Pfizer, Inc. and others to the Infectious Disease Institute (IDI) in Kampala, Uganda. With help from Pfizer and others, IDI has achieved the goal of building capacity in Africa for the delivery of sustainable, high-quality prevention and care for HIV/AIDS and related infectious diseases through training and research. Since 2001, IDI has trained more than 3,500 health care providers from 27 African countries, currently providing care to approximately 10,000 patients, and has helped build research capacity in the region by pairing promising new investigators with established researchers from North America and Europe through mentoring arrangements and fellowships (Pfizer Inc., 2010).
Another example of a corporate partnership supporting HIV/AIDS prevention is the African Comprehensive HIV/AIDS Partnerships (ACHAP). Founded in 2000, ACHAP is a joint effort of the Government of Botswana, the Bill & Melinda Gates Foundation, and the Merck Company Foundation/Merck & Co., Inc. The partnership supports and enhances the government of Botswana’s national response to the HIV/AIDS epidemic through a comprehensive approach to prevention, treatment, care, and support (Merck Sharp & Dohme Corporation, 2010).
Faith-based organization partnerships FBOs can make unique contributions to international development because they exist in cities, villages, and even the most rural regions of low-income countries. These organizations provide 30–40 percent of health care services in low-income countries (Kawasaki and Patten, 2002). While governments and political climates change over time, moreover, communities of faith remain intact as support systems. Box 5-2 illustrates the contributions FBOs can make to the fight against HIV/AIDS.
Military partnerships As part of the U.S. Department of Defense’s directive to support foreign militaries in mitigating HIV among their forces, the U.S. Military HIV Research Program (MHRP) provides assistance to militaries in Kenya, Nigeria, and Tanzania. Various activities associated with HIV prevention, treatment, and care are carried out at military sites throughout the respective countries. These activities support services to men and women in uniform and their dependents. In Nigeria and Tanzania, these services are also provided to the civilian populations surrounding the barracks and military medical facilities. With close to 80 percent of their patient populations being civilians, these military facilities are an important component of their respective national health care systems (U.S. Military HIV Research Program, 2010).
All military–military collaborations strive to support partners’ military development and strengthening of local health systems. To this end, they assist in building the partners’ infrastructure and capacity to provide necessary services, including behavioral interventions tailored to the risk factors faced by their forces. In all countries, programs, initiatives, and activities are managed and overseen through direct in-country cooperation between MHRP and partners’ senior military leadership (U.S. Military HIV Research Program, 2010).
In Nigeria, PEPFAR supports a military partnership with the Nigerian Armed Forces to fight HIV/AIDS. In April 2006, a need for ART services was identified in the state of Benue, which has Nigeria’s highest HIV prevalence rate. With support from PEPFAR, Nigerian military staff worked in partnership with the U.S. government and key stakeholders to rapidly establish and scale up treatment services in the state (PEPFAR, 2007). A team of three Nigerian military medical staff was dispatched to assist in establishing the services. They met extensively with local support groups to ensure that the planned services would meet local needs. In June 2006, free ART was launched at the Nigerian Air Force Hospital in Makurdi, the capital of Benue. Both the Minister of State for Defense and the Governor of Benue lent political support to the inaugural program (PEPFAR, 2007).
Academic twinning The twinning relationship must exist as a partnership with parity; new skills, processes, and knowledge should be exchanged by both partners through the process (AIHA, 2005; Einterz et al., 2007). The committee
|
BOX 5-2 AIDSRelief: A Faith-Based Program Combating HIV/AIDS in South Africa In South Africa, the Catholic Church has provided health care in areas of need since 1849. Today there are 2 hospitals, 31 clinics, 16 hospices, 10 multipurpose health centers, numerous home-based care organizations, and hundreds of HIV projects across the Catholic dioceses in South Africa (Stark, 2010). In 2000, an AIDS Office was established to coordinate the Church’s response to HIV; in 2004, the AIDS Office received PEPFAR funding through Catholic Relief Services (CRS) to provide ART and other HIV care and support services in 20 of the programs offered through the dioceses. The 5-year funding award was managed globally by CRS headquarters; the funds flowed from U.S. government channels through CRS to the implementing partners. The PEPFAR funding to CRS for ART was implemented through two local umbrella church organizations—the Institute for Youth Development South Africa (IYDSA) and the Southern African Catholic Bishops Conference (SACBC)—and became known as the AIDSRelief program. Through these programs, 73,293 people received HIV care and 35,038 were enrolled in ART over the course of 5 years (2004–2009) (Stark, 2010; Stark et al., 2010). Beginning in 2004, AIDSRelief worked in collaboration with IYDSA and SACBC to provide community-based care and clinical treatment to people affected by HIV. Treatment facilities were expanded and equipped. Financial compliance systems were instituted, and treatment sites were prepared to implement a new electronic database to assist with patient management. Throughout the project, hundreds of health workers were trained—296 in the 2008–2009 grant year alone (Stark et al., 2010). AIDSRelief committed to supporting activities that would ensure the sustainability of treatment for people living with HIV/AIDS when donor funds were no longer available. Linkages were established with local clinical experts, as well as with health training institutions and organizations. Relationships with South African government health and social services agencies were strengthened (Stark, 2010; Stark et al., 2010). Sustainability plans for some programs involved a variety of public–private partnership arrangements whereby government would cover the costs of certain services, including laboratory services, antiretroviral drugs, and even staff salaries. For other programs, sustaining people on ART involved the transfer of patients to South African government health services as they became available and accessible. Over the 5 years, 6,764 patients have been transferred to accredited government facilities where they will continue to receive lifelong treatment. The strong partnership with the local church, the commitment to collaborate with the local government, and the encouragement and support of the activity manager at the U.S. government mission in South Africa made the transfers possible (Stark, 2010; Stark et al., 2010). The program is currently embarking on a new direction, with local South African organizations taking the lead. The local organizations now receive their PEPFAR grant funds directly from the U.S. government and are responsible for managing all aspects of the program. AIDSRelief will serve its partners as a subgrantee in specified technical areas and will support partners as they assume their new role. South Africa’s is the first of the PEPFAR HIV/AIDS treatment programs to transition to local leadership (Stark, 2010; Stark et al., 2010). |
believes that parity is both a necessary and defining characteristic of a twinning relationship.
Formed in 1992, the American International Health Alliance (AIHA)7 broke ground for the establishment of large-scale twinning relationships aimed at building sustainable institutional and human resource capacity in nations with limited resources. AIHA was initially established by a consortium of major health care provider associations and professional medical education organizations to help the nations of the former Soviet Union build much-needed health system capacity (AIHA, 2010a). In 2004, AIHA established the HIV/AIDS Twinning Center, which creates peer-to-peer relationships between organizations working to improve services for people living with or affected by HIV/AIDS; the Twinning Center currently has programs in 11 countries in Africa and continues its program in Russia (AIHA, 2007).
An example of university twinning is the Academic Model for Providing Access to Healthcare (AMPATH), a partnership among Moi University School of Medicine, Moi Teaching and Referral Hospital, and other health centers and hospitals operated by Kenya’s Ministry of Health and a consortium of North American institutions led by Indiana University.8 AMPATH aims to deliver essential primary care services, control HIV/AIDS, and mitigate its economic and social consequences in a population of 2 million people in western Kenya (Einterz et al., 2007, 2010; Kimaiyo, 2010). In contrast with most academic twinning HIV/AIDS care programs, which partner with the private sector, delivery of care through AMPATH occurs through the public sector (Einterz et al., 2010; Kimaiyo, 2010).
AMPATH is supported by more than 1,000 staff members: 42 staff from Moi University; 447 staff from the Kenyan Ministry of Health; 665 direct AMPATH employees; and 8 North Americans (Kimaiyo, 2010), at least one of whom is an Indiana University general internal medicine faculty member committed on-site in Kenya (Einterz et al., 2007). In addition to care provided for patients, Indiana University School of Medicine helps educate and train Kenyan physicians in clinical care and research through a partnership called ASANTE (America/
sub-Saharan Africa Network for Training and Education in Medicine).9 More than 800 Kenyans and Americans have participated in exchanges of students, faculty, and postgraduates through this partnership.
AMPATH’s emphasis is not on the twinning relationship between two universities but on a triadic relationship among the two universities and the ministry of health (Einterz et al., 2007, 2010). Indiana University also ensures that there is Kenyan leadership at every level of the program; thus, Moi University is fully invested and shares equal ownership of the program (Kimaiyo, 2010).
Another example of twinning is the International Training and Education Center on Health (I-TECH),10 a global network that works with local partners to develop skilled health care workers and strong national health systems in resource-limited countries, promoting local ownership to sustain effective health systems (Holmes, 2004; I-TECH, 2010). Table 5-3 summarizes I-TECH’s principal programs and activities and the services they provide. The benefits of selected I-TECH programs are summarized later in the chapter.
Like AMPATH, I-TECH recognizes the importance of including local governing bodies and organizations to build a broad base of support among multiple stakeholders. I-TECH adapts each program to local preferences and resource constraints. To ensure the efficacy of each program, I-TECH invests in operations research and formal process evaluations. Ongoing monitoring allows for midstream corrections, as findings are communicated to program managers to improve decision making (I-TECH, 2009c).
Other Capacity-Building Programs
Other capacity-building programs include foundation programs and initiatives of civil society organizations.
Foundation programs Capacity-building efforts should target not only key health personnel in the health system, but also individuals in country governments who require capacity building for leadership. Governments act as stewards of the public interest and are responsible for ensuring conditions that allow their citizens to be as healthy as possible. Ministries of health and the ministers who lead them must be able to perform a set of core stewardship functions within the ministry and across the government. Ministers and ministries of health are currently
TABLE 5-3 I-TECH’s Principal Programs
|
Program |
Activities |
Services Provided |
|
Health System Strengthening |
Strengthening of clinical care and treatment systems |
|
|
|
Strengthening of health information systems |
|
|
|
Strengthening of laboratory systems |
|
|
|
Strengthening of training and education systems |
|
|
Health Workforce Development |
Health care worker education systems |
|
|
|
Training development |
|
|
|
Distance learning |
|
|
|
Clinical mentoring |
|
|
Operations Research and Evaluation |
Monitoring and evaluation |
|
|
Program |
Activities |
Services Provided |
|
Prevention, Care, and Treatment of Infectious Diseases |
Prevention |
|
|
|
Care and treatment |
|
|
SOURCE: I-TECH, 2009c. |
||
overlooked, however, when investments are made and initiatives are designed to strengthen health systems (Omaswa and Ivey Boufford, 2010).
The W.K. Kellogg Foundation was established in 1930 with the purpose of administering funds to promote the welfare, health, education, and safeguarding of children and youth. Over the years, the foundation’s programming has continued to evolve, striving to remain innovative and responsive to the ever-changing needs of society (W.K. Kellogg Foundation, 2010a). In 1989, the Kellogg International Leadership Program (KILP) was formed to promote the development of leadership capacity by connecting leaders in Latin America, the Caribbean, the United States, and Southern Africa. Through seminars, small study groups, and community-focused projects, KILP fellows obtain both didactic training and hands-on experience to refine their global leadership skills. Priority is given to leaders in the sectors most aligned with Kellogg’s four levers of change: civic responsibility, economic opportunity, skills and leadership, and health and wellbeing (W.K. Kellogg Foundation, 2010b).
Dr. Sheila Tlou, now UNAIDS Regional Support Team Director for East and Southern Africa (September 2010) and a former Minister of Health of Botswana (2004–2009), was the first recipient of the KILP grant. With the grant, she received her Ph.D. in the United States in community health nursing, with a concentration in gender and health issues, and she is now vice chair of a coalition of 20 women’s organizations that focus on issues of women’s political, health, and economic empowerment; violence; human rights; and education of girls. In addition, Tlou cofounded the Coping Centre for People Living with AIDS in Gabarone, Botswana, which rehabilitates HIV-positive women and develops their capacity to be leaders in the community. As a researcher, Tlou was instrumental in convincing Botswana’s government to invest in home care and treatment for HIV/AIDS patients. She served as HIV coordinator for the University of Botswana and is a highly regarded voice in the community, civic, and government sectors. Tlou is one of many successful public health and government leaders developed through this grant program (W.K. Kellogg Foundation, 2010b).
Additional government capacity-building programs include the Humphrey Fellowship Program and the Fogarty Fellowship Program. Sponsored by the U.S. Department of State, the Humphrey Fellowship Program provides midcareer
professionals from developing countries with 10 months of nondegree academic study and professional enrichment in the United States (Hubert H. Humphrey Fellowship Program, 2007). The program offers fellows valuable opportunities for leadership development and professional engagement. More than 3,700 men and women have been honored as Humphrey Fellows since the program began in 1978 (Hubert H. Humphrey Fellowship Program, 2007). The Fogarty Fellowship Program promotes productive reentry of National Institutes of Health (NIH)–trained foreign investigators into their home countries upon completion of their experiences with the fellowship program (NIH, 2010).
Civil society organization initiatives Throughout history, civil society organizations have been known to contribute to the good of the world. In keeping with this historical role, Rotary International formed Rotarians For Fighting AIDS, Inc. (RFFA) in 2003. RFFA’s mission is to improve the lives of orphans and vulnerable children affected by HIV/AIDS by mobilizing Rotarians and partners to provide care, nutrition, education, and life skills (RFFA, 2010a). RFFA works closely with the African Network for Children Orphaned and at Risk (ANCHOR), a partnership among four entities: RFFA, Project HOPE (Health Opportunities for People Everywhere), the Coca-Cola Africa Foundation, and Emory University’s School of Public Health (RFFA, 2010b).
RFFA’s current initiatives are focused on addressing issues related to HIV/AIDS orphans and vulnerable children. Through projects such as Orphan Rescue, RFFA has partnered with ANCHOR to build the capacity of families and local communities to cope with and respond to the needs of these children. The project provides vital educational support in the form of nutrition, uniforms, supplies, and mandatory school fees (RFFA, 2010c).
Another noteworthy project creates Kidz Clubs—community meeting places that provide children safe spaces to meet, play, and interact. RFFA and ANCHOR have successfully assisted communities in developing more than 250 Kidz Clubs across seven African countries, reaching and caring for more than 20,000 needy children affected by HIV/AIDS. In these clubs, children learn coping skills and build resilience. Counseling is provided to children dealing with grief, loss, violence, and other challenges resulting from HIV/AIDS (RFFA, 2010b).
Benefits of Partnerships and Other Capacity-Building Programs
As evidenced by the preceding examples of partnerships and training programs, many benefits are realized by participants. Among these benefits are increased program effectiveness and the opportunity to network and participate in the global health movement.
Increased program effectiveness The accomplishments of I-TECH’s HIV/ART Nurse Specialist (HANS) Training Program illustrate the benefits of capacity-
building initiatives. As a result of this program, for example, the number of Ethiopian nurse mentors who were once themselves HANS trainees has increased over time. This outcome reflects the expanded role of nurses as a result of the program, and indicates the program’s success in achieving the goal of building capacity within the Ethiopian health care system to train the nursing workforce in HIV/AIDS specialist care (I-TECH, 2009b). Participants’ pre- and posttests showed a significant increase in knowledge. More important, participants demonstrated consistent improvement in the performance of key competencies during their clinical practicum (I-TECH, 2009b).
Likewise, I-TECH’s Program Evaluation for the Implementation of the Revised Syndromic Management Algorithms for Sexually Transmitted Infections in Two Districts in Botswana found that, relative to patients at comparison clinics, a higher percentage of patients of trainees reported that the provider (1) offered an HIV test (87 percent versus 29 percent), (2) conducted a physical examination (98 percent versus 64 percent), (3) helped them develop a plan to avoid future acquisition of sexually transmitted infections (STIs) (95 percent versus 76 percent), and (4) provided patient-specific information about HIV risk (65 percent versus 32 percent) (I-TECH, 2009d; Weaver et al., 2008).
As a final example, at IDI in Uganda, a 4-week course on comprehensive management of HIV/AIDS, including ART, improved the clinical skills of doctors in 11 of 17 areas evaluated. Interactive methods, such as hands-on practice sessions, case discussions, and role-play, were effective in changing physician practices and in some cases the health outcomes of patients (I-TECH, 2009a; Weaver et al., 2006).
Opportunity to network and participate in the global health movement Twinning and partnering can contribute to greater networking by exposing partners to each other’s existing networks (ICAD, 1999). An unprecedented enthusiasm for global health currently exists among students and medical residents in U.S. universities (Drain et al., 2007; IOM, 2009). In 2008, the Consortium of Universities on Global Health created a formal alliance to build collaborations and foster the exchange of knowledge and experience among interdisciplinary university global health programs, working across education, research, and service (CUGH, 2010). The private sector and professional associations also have demonstrated an interest in sharing their business and technical acumen for the greater social good (IOM, 2009). In this context, participating in an international twinning relationship or partnership is beneficial to the Northern partner in that such programs attract faculty, students, and employees at the respective universities or organizations. Further, academic institutions are much more likely to be successful in both launching and sustaining global health programs if they work with international partners (Koplan and Baggett, 2008).
Challenges of Partnerships and Other Capacity-Building Programs
Although capacity-building programs have achieved many successes, they have faced challenges as well. Evaluations of twinning and other capacity-building programs reveal the following challenges to the future success or replication of such programs.
Financing WHO estimated that it would cost $254.8 billion in training and recurrent salary costs over 10 years to eliminate the global human resource gap (of 4.3 million health workers) (WHO, 2006). The question immediately arises of whether and how governments in low-income countries can finance such scale-up of human resources. Already, human resource spending can consume more than half of ministries’ recurrent health expenditures (WHO, 2008b). Expanded numbers of health workers require expanded resources to pay the costs of their employment, including wages and benefits, as well as the cost of their education and training, including teacher salaries; books, laboratories, and equipment; new buildings, classrooms, offices, and laboratories; maintenance and repair of facilities and equipment; and students’ living expenses. Scaling up of the health workforce also requires simultaneous increases in other health goods, such as drugs, supplies, functioning equipment, and adequate management and supervision (WHO, 2008b).
Given the extent of these costs, external support may be necessary to supplement domestic resources in scaling up the health workforce. To ensure the long-term sustainability of such a scale-up, donors must work within each country’s strategic plan, and a maximum amount of domestic resources must be mobilized. It has been noted that donors have been reluctant in the past to fund recurrent costs, such as employment costs of health workers (Vujicic, 2005), although some donors, such as the Global Fund, reportedly have begun to be more flexible in their policies concerning financing of public-sector recurrent costs (WHO, 2008b). The effect of external assistance on the ability of countries to scale up the health workforce is likely to be small, however; even a doubling of external assistance would not be as powerful as the combination of substantial economic growth and governments allocating larger shares of their spending to health (Preker et al., 2007). Ultimately, then, countries need to make choices about the scale-up of their health workforce that best suit their epidemiological profile and fiscal circumstances (WHO, 2008b).
Sustainability Sustaining twinning projects or other partnerships over time may be challenging, often because of insufficient funding and high administrative costs (ICAD, 1999). As noted earlier, for example, the AMPATH twin in Kenya maintains a staff that includes 665 direct employees and 8 North Americans (Kimaiyo, 2010), at least one of whom is an Indiana University general internal medicine faculty member committed on-site in Kenya (Einterz et al., 2007). The
cost of maintaining such numbers of staff may be prohibitive in some settings. In addition, stagnant funding is increasing the burden on the program to expand services while working with fewer resources (USAID-AMPATH, 2010).
More pressing priorities Some organizations involved in twinning or other partnership or training programs may need to devote all of their energies to the survival of their regular programs (ICAD, 1999). This pressure is bilateral; both partners have pressing priorities beyond the twinning project or partnership. In some countries, a program may not be seen as contributing to PEPFAR goals. Those goals call for reaching large numbers of people with services; some 85 percent of U.S. funds going to Africa have been for PEPFAR, so this is a high priority for U.S. missions in the region. Twinning projects are thought to contribute relatively little to the achievement of PEPFAR’s goals, and it is not always clear at the outset how such projects may fit into broader country plans. Hence it has sometimes been difficult to obtain buy-in for projects in Africa for which twinning would be appropriate, and some of the earliest twinning projects in the region could not fit readily into the existing programs of U.S. government teams (Conviser, 2009).
Time frame of results Relative to one-shot technical assistance programs, twinning programs take time to establish because they depend on the development of institutional and interpersonal relationships. Also, twinning programs require about the same amount of administrative oversight from in-country U.S. government agencies as larger-budget PEPFAR programs and may be slower to produce results. In-country U.S. government teams have often felt it was not worth the effort to fund relatively small projects that require roughly the same amount of attention as far larger PEPFAR initiatives (Conviser, 2009).
Lack of appropriate infrastructure Most African organizations lack an established infrastructure equipped to serve twinning or training projects (ICAD, 1999), and many of those evaluated have noted information technology challenges (Kangas et al., 2010). Several twinning projects (including projects in Botswana, Zambia, and Ethiopia) have reported that technology was a challenge in maintaining the twinning relationship. Fragile e-mail systems made it difficult to exchange information between partners. Limited access to electricity and telephone landlines was also cited as hampering communication between partners (Conviser, 2009). The AMPATH partnership in Kenya reported difficulties in encouraging patients’ continued compliance with ART (with a rate of loss to follow-up of 1.6 percent in the first quarter of 2010) as a result of several constraints, including limited access to program vehicles, a lack of reliable public transportation for both outreach staff and patients, and inadequacy of the electronic tracking system in locating patients. Some health care facilities
lacked supplies needed to provide STI care, such as patient education materials, condoms, and contact slips (I-TECH, 2009d; Weaver et al., 2008).
Extra strain on overburdened staff In low-resource countries, the human resource crisis leaves hospital staff members extremely busy, limiting their communication with twinning partners between visits. The amount of administrative work required for the relatively small-scale twinning projects does not differ significantly from the amount of work necessary for much larger projects, challenging small and already overburdened staff (Conviser, 2009). AMPATH’s outreach and follow-up with current patients, for example, were challenged by a shortage of staffing, as reported in the quarterly PEPFAR performance review for January–March 2010 (USAID-AMPATH, 2010).
Lack of an in-country coordinator The AIHA HIV/AIDS Twinning Center’s evaluation described one challenge particular to that organization. The absence of U.S. Health Resources and Services Administration (HRSA) representatives from U.S. government teams or an AIHA office in Africa makes it more administratively complex for other U.S. government agencies to fund twinning projects: U.S. government agencies must designate the funds for HRSA, which passes them on to AIHA, which provides them to the partners. The funding agencies also must do a substantial amount of administrative work on these small-ticket projects, whose impact in meeting PEPFAR goals, as noted above, may be both minor and delayed. There needs to be a single point of contact for both HRSA and the organization serving as its agent in overseeing twinning projects in Africa, with regular scheduled communication between them. This would help promote both advocacy and accountability in twinning projects, although it would come at the cost of increased work for HRSA’s agent(s) in Africa (Conviser, 2009).
RECOMMENDATIONS
Recommendation 5-1: Analyze and plan for meeting workforce requirements. African governments and international organizations should assess and plan for meeting national workforce requirements for responding to the long-term burden of HIV/AIDS.
-
Recommendation 5-1a: Through partnership programs and other investments, African governments and institutions, along with U.S. private companies, academic institutions, foundations, and civil society organizations, should establish national databases and information systems for health care worker statistics, as well as bolster the analytic capacity of national planners for determining human resource needs.
-
Recommendation 5-1b: African governments and institutions should create staffing models to optimize the impact of the health care work-
-
force. Such models should include developing cadres of managers and support staff outside the clinical health sector, encouraging needs-based training and task sharing within the health sector, focusing on retention through compensation and other incentives, utilizing information technologies, and harnessing the informal health sector.
-
Recommendation 5-1c: In Africa, governments and institutions should work together in planning the African health care workforce based on projected needs derived from national data and analyses of future human resource requirements. Such planning should involve ministries of health, education, finance, public service, and labor. The private sector and the academic and medical communities should also be brought to the table for such national human resource planning exercises.
Recommendation 5-2: Utilize existing African capacity. African governments and international donors should recognize, invest in, strengthen, and utilize currently existing capacity within African institutions and networks to provide local solutions for responding to the HIV/AIDS epidemic. This capacity includes South–South and regional partnerships, universities, African science academies, national public health institutes, and other networks within Africa.
Recommendation 5-3: Develop government leadership and management in health. U.S. government agencies and programs, foundations, and academic institutions should invest in the development of African leadership and management in the health sector.
-
Recommendation 5-3a: U.S. government agencies, such as the Health Resources and Service Administration (HRSA), the U.S. Agency for International Development (USAID), and the U.S. Centers for Disease Control and Prevention (CDC) and its global counterparts, should be actively engaged in leadership and management development, and the International Association of Public Health Institutes should be tapped as a resource for advancing these efforts.
-
Recommendation 5-3b: U.S. foundations and academic institutions should invest in African leadership and management development through programs that educate African scientists and scholars who may then take on leadership positions in their own countries.
Recommendation 5-4: Invest in innovative partnerships. Private-sector organizations, professional organizations, faith-based organizations, academic and research institutions, militaries, foundations, and civil society organizations should increase funding for and participation in meaningful,
effective, and innovative partnerships designed to build African capacity now to address the full extent of the HIV/AIDS burden over the next 10 years.
-
Recommendation 5-4a: New U.S.–African partnerships between local vocational or technical schools that train allied health professionals, laboratory technicians, informatics specialists, and/or health administrators should be explored and encouraged.
-
Recommendation 5-4b: Innovative North–South and South–South partnerships that build human resources for health should be developed. In North–South partnerships, African counterparts should take the lead in developing and controlling the partnership agenda.
As a final note, the committee emphasizes that a formidable gap exists between innovations in health (including vaccines, drugs, and strategies for care) and their delivery to communities in the developing world (Madon et al., 2007). Many of the recommendations in this chapter imply a need to perform operations research11 (OR) and implementation research12 (IR)—as well as ongoing evaluation—of programs, partnerships, and interventions aimed at combating HIV/AIDS in Africa. Such efforts can identify the optimal and most efficient approaches for carrying out the committee’s recommendations. Because HIV/AIDS is a mosaic of epidemics in Africa (see Chapter 1), programs and policies will require tailoring to local circumstances. There is a wide range of OR opportunities in capacity building for HIV/AIDS, including identifying the best methods for:
-
obtaining and delivering commodities in the health system;
-
making mass treatment more feasible;
-
managing patients on fewer doses of ART;
-
treating for a period of time and then stopping treatment, but monitoring the patient;
-
preventing infections and changing behavior in a particular context or risk group;
-
using new communication tools and social media to reach those in need of prevention messages;
-
scaling up information and communication technology;
-
employing task/responsibility sharing;
-
packaging together interventions for HIV/AIDS, TB, and other diseases;
-
training a new generation of researchers to bridge the implementation gap; and
-
strengthening research institutions in low-income countries (Madon et al., 2007).
The recommendations in this chapter, therefore, should be tested, evaluated, and tailored to specific country and regional contexts.
REFERENCES
Accordia Global Health Foundation. 2010. Return on investment: The long-term impact of building healthcare capacity in Africa. Washington, DC: Accordia Global Health Foundation.
AIHA (American International Health Alliance). 2005. HIV/AIDS twinning center frequently asked questions. http://www.twinningagainstaids.org/faq.html (accessed November 2, 2009).
———. 2007. HIV/AIDS twinning center: Overview. http://www.twinningagainstaids.org/overview.html (accessed August 16, 2010).
———. 2010a. History. http://www.aiha.com/en/WhoWeAre/History.asp (accessed August 12, 2010).
———. 2010b. Who we are. http://www.aiha.com/en/WhoweAre/ (accessed August 12, 2010).
Al Riyami, A., M. Afifi, and R. M. Mabry. 2004. Women’s autonomy, education and employment in Oman and their influence on contraceptive use. Reproductive Health Matters 12(23):144-154.
AMREF (African Medical and Research Foundation). 2010. Traditional healers, South Africa. http://www.amref.org/what-we-do/traditional-healers-south-africa/ (accessed July 31, 2010).
ASADI (African Science Academy Development Initiative). 2008. African science academy development intiative: Progress and promise. http://www.nationalacademies.org/asadi/progressreport.pdf (accessed December 20, 2010).
ASSAf (Academy of Science of South Africa). 2007. HIV, TB and nutrition: Scientific inquiry into the nutritional influences on human immunity with special reference to HIV infection and active TB in South Africa. Pretoria, South Africa: ASSAf.
August-Brady, M. 2010. Nursing and nursing education in Mozambique from Michele August-Brady. http://www.nursingsociety.org/VolunteerConnect/Pages/NursingMozambique.aspx (accessed October 28, 2010).
Avert. 2010. Why HIV and AIDS home based care? http://www.avert.org/aids-home-care.htm (accessed July 13, 2010).
Belhadj, H., and A. Touré. 2008. Gender equality and the right to health. The Lancet 372(9655): 2008-2009.
Buchan, J., and M. R. Del Poz. 2003. Role definitions, skill mix, multi-skilling and “new” workers. In Towards a global health workforce strategy, edited by P. Ferrinho and M. R. Del Poz. Antwerp, Belgium: ITGPress. Pp. 275-300.
CDC (Centers for Disease Control and Prevention). 2010. Public-private partnership strengthens global laboratory systems. http://www.cdc.gov/globalaids/Success-Stories/BD-Public-Private-Partnership.html (accessed August 9, 2010).
Chen, L., T. Evans, S. Anand, J. I. Boufford, H. Brown, M. Chowdhury, M. Cueto, L. Dare, G. Dussault, G. Elzinga, E. Fee, D. Habte, P. Hanvoravongchai, M. Jacobs, C. Kurowski, S. Michael, A. Pablos-Mendez, N. Sewankambo, G. Solimano, B. Stilwell, A. de Waal, and S. Wibulpolprasert. 2004. Human resources for health: Overcoming the crisis. The Lancet 364(9449):1984-1990.
Commission for Africa. 2005. Our common interest: Report of the Commission for Africa. 2005. London: Commission for Africa.
Conviser, R. 2009. Building capacity from within: AIHA’s twinning program in Africa. Missoula, MT: Global Health Policy Partners.
CUHG (Consortium of Universities for Global Health). 2010. Background. http://www.cugh.org/about/background (accessed August 23, 2010).
Dada, J., Fantsuam Foundation, V. Francis, Emerging Markets Group, M. Isaac, M. Mayson, Catholic Relief Services, T. Mensah, and Sinapi Aba Trust. 2009. Partnership models for successful microenterprise service delivery to HIV and AIDS-affected communities. Washington, DC: USAID.
Dare, L. 2010. Evaluating health systems. Presentation to the IOM committee on planning the evaluation of PEPFAR. http://www.iom.edu/~/media/Files/Activity%20Files/Global/PEPFAR2/Lola%20Dare.ashx (accessed September 22, 2010).
Dohrn, J., B. Nzama, and M. Murrman. 2009. The impact of HIV scale-up on the role of nurses in South Africa: Time for a new approach. Journal of Acquired Immune Deficiency Syndromes 52:S27-S29.
Dovlo, D. 2003. The brain drain and retention of health professionals in Africa. Paper presented at regional training conference on improving tertiary education in sub-Saharan Africa: Things that work!, Accra, Ghana, September 23-25.
Drain, P. K., A. Primack, D. D. Hunt, W. W. Fawzi, K. K. Holmes, and P. Gardner. 2007. Global health in medical education: A call for more training and opportunities. Academic Medicine 82(3):226-230.
Eckhert, N. L. 2002. The global pipeline: Too narrow, too wide or just right? Medical Education 36(7):606-613.
Einterz, R. M., S. Kimaiyo, H. N. K. Mengech, B. O. Khwa-Otsyula, F. Esamai, F. Quigley, and J. J. Mamlin. 2007. Responding to the HIV pandemic: The power of an academic medical partnership. Academic Medicine 82(8):812-818.
Einterz, R. M., J. Mamlin, W. Tierney, P. Biondich, D. Litzelman, M. Were, and T. Inui. 2010. AMPATH. Presentation to the IOM committee on envisioning a strategy to prepare for the long-term burden of HIV/AIDS: African needs and U.S. interests, Washington, DC, February 4, 2010.
eMOCHA (electronic Mobile Open-source Comprehensive Health Application). 2010. eMOCHA: Electronic mobile open-source comprehensive health application. http://emocha.org/ (accessed July 29, 2010).
Emory University School of Nursing. 2010. Health workforce information systems–Kenya project. http://www.nursing.emory.edu/lccin/research/health_workforce/project_kenya.html (accessed September 2, 2010).
Ferrinho, P., I. Fronteira, M. Sidat, F. da Sousa, and G. Dussault. 2010. Profile and professional expectations of medical students in Mozambique: A longitudinal study. Human Resources for Health 8(1):21.
Fox, S., C. Fawcett, K. Kelly, and P. Ntlabati. 2002. Integrated Community-based Home Care (ICHC) in South Africa: A review of the model implemented by the Hospice Association of South Africa. Capetown, South Africa: The Centre for AIDS Development, Research and Evaluation (Cadre) on behalf of The POLICY Project.
Glenngård, A. H., and A. Anell. 2003. Investment in human resources for health problems, approaches and donor experiences. Joint Learning Initiative on human resources for health and development. JLI working paper 2-6.
Hassan, M. H. A., and D. Schaffer. 2009. When less is more but still not enough: Managing academies of science in a globalised world. International Journal of Technology Management 46(1-2):71-82.
High-Level Forum on the Health MDGs. 2004. Addressing Africa’s health workforce crisis: An avenue for action. Abuja, Nigeria: World Bank and WHO.
Holmes, K. 2004. Model of training for grassroots work on HIV. Paper read at the December 1, 2004 workshop of the IOM committee on overseas placement of U.S. healthcare professionals, Washington, DC.
Hongoro, C., and B. McPake. 2004. How to bridge the gap in human resources for health. The Lancet 364(9443):1451-1456.
Hubert H. Humphrey Fellowship Program. 2007. About the program: The Hubert H. Humphrey Fellowship Program. http://humphreyfellowship.org/page/97565/index.v3page;jsessionid=2nd9knmmkdl00 (accessed August 13, 2010).
I-TECH (International Training & Education Center for Health). 2009a. Effectiveness of clinical training for HIV care in sub-Saharan Africa—The Infectious Disease Institute (IDI) training evaluation. http://www.go2itech.org/what-we-do/operations-research-and-evaluation/quality-improvement/qi-program-examples/effectiveness-of-clinical-training-for-hiv-care-in-sub-saharan-africa2014the-infectious-disease-institute-idi-training-evaluation (accessed July 28, 2010).
———. 2009b. Ethiopia HIV/ART Nurse Specialist (HANS) training program evaluation. http://www.go2itech.org/what-we-do/operations-research-and-evaluation/quality-improvement/qi-program-examples/ethiopia-hiv-art-nurse-specialist-hans-training-program-evaluation (accessed July 28, 2010).
———. 2009c. I-TECH. http://www.go2itech.org/ (accessed June 25, 2010).
———. 2009d. Program evaluation for the implementation of the revised syndromic management algorithms for sexually transmitted infections in two districts in Botswana. http://www.go2itech.org/what-we-do/operations-research-and-evaluation/quality-improvement/qi-program-examples/program-evaluation-for-the-implementation-of-the-revised-syndromic-management-algorithms-for-sexually-transmitted-infections-in-two-districts-in-botswana (accessed July 28, 2010).
———. 2010. I-TECH’s vision, mission, and principles. http://www.go2itech.org/who-we-are/visionmission-and-principles (accessed September 1, 2010).
IANPHI (The International Association of National Public Health Institutes). 2010. IANPHI: Public health institutes of the world. http://www.ianphi.org/ (accessed August 12, 2010).
ICAD (Interagency Coalition for AIDS and Development). 1999. Beyond our borders: A guide to twinning for HIV/AIDS organizations. Ottawa, Ontario: Canadian AIDS Clearinghouse.
———. 2002. Twinning against AIDS. http://www.comminit.com/pdf/twinning_against_AIDS_Final_Report.pdf (accessed November 10, 2009).
IOM (Institute of Medicine). 1986. Confronting AIDS: Directions for public health, health care, and research. Washington, DC: National Academy Press.
———. 1995. HIV and the blood supply: An analysis of crisis decision making. Washington, DC: National Academy Press.
———. 2005a. Healers abroad: Americans responding to the human resource crisis in HIV/AIDS. Washington, DC: The National Academies Press.
———. 2005b. Review of the HIVNET 012 perinatal HIV prevention study. Washington, DC: The National Academies Press.
———. 2005c. Scaling up treatment for the global AIDS pandemic: Challenges and opportunities. Washington, DC: The National Academies Press.
———. 2009. The U.S. commitment to global health: Recommendations for the public and private sectors. Edited by P. Subramanian. Washington, DC: The National Academies Press.
Ivers, L. C., J. S. Mukherjee, F. R. Leandre, J. Rigodon, K. A. Cullen, and J. Furin. 2010. South–south collaboration in scale-up of HIV care: Building human capacity for care. AIDS 24:S73-S78.
Jensen, M. B., Hjortso, C. N., Schipperijn, J., Nik, A., Nilsson, K. 2007. Research capacity building through twinning: Experiences from a Danish-Malaysian twinning project. Public Administration and Development 27:381-392.
JLI (Joint Learning Initiative). 2004. Human resources for health: Overcoming the crisis. Cambridge, MA: Global Equity Initiative, Harvard University.
Jones, M., and P. Blunt. 1999. “Twinning” as a method of sustainable institutional capacity building. Public Administration and Development 19:381-402.
Kangas, L., K. Fogg, L. Okoko, and G. Wein. 2010. Evaluation of Africa’s health in 2010. Washington, DC: Global Health Technical Assistance Project.
Kawasaki, E., and J. P. Patten. 2002 (unpublished). Drug supply systems of missionary organizations identifying factors affecting expansion and efficiency: Case studies from Uganda and Kenya.
Kelley, P. 2009. How science academies provide evidence-based advice. Paper presented at African Science Academy Development Initiative: Ghana’s 50th Anniversary Conference, Accra, Ghana.
Kenya Health Workforce Information System. 2010 (unpublished). HRH global forum award application. Kenya Health Workforce Information System.
Kimaiyo, S. 2010. University partnerships to build long-term capacity for HIV/AIDS in Africa. Presentation to the IOM committee on envisioning a strategy to prepare for the long-term burden of HIV/AIDS: African needs and U.S. interests. Pretoria, South Africa, April 13, 2010.
Koplan, J. P., and R. L. Baggett. 2008. The Emory Global Health Institute: Developing partnerships to improve health through research, training, and service. Academic Medicine 83(2):128-133.
LIPHEA (Leadership Initiative for Public Health in East Africa). 2010. About LIPHEA. http://halliance.org/groups/liphea/about-liphea.html (accessed July 8, 2010).
Littlefield, E., J. Morduch, and S. Hashemi. 2003. Is microfinance an effective strategy to reach the millenium development goals? Washington, DC: Consultative Group to Assist the Poor (CGAP).
Madon, T., K. J. Hofman, L. Kupfer, and R. I. Glass. 2007. Implementation science. Science 318(5857):1728-1729.
McCarthy, E. A., M. E. O’Brien, and W. R. Rodriguez. 2006. Training and HIV-Treatment scale-up: Establishing an implementation research agenda. PLoS Medicine 3(7):e304.
Merck Sharp & Dohme Corporation. 2010. African Comprehensive HIV/AIDS Partnerships (ACHAP): Advancing the dialogue toward a healthier future. http://www.merck.com/corporate-responsibility/access/access-hiv-aids/access-hiv-aids-ACHAP-botswana/approach.html (accessed August 24, 2010).
Michael, P., S. Ashlesh, M. Arthur, Q. Giulio, S. Philip, T. John, L. Brian, H. Mary Ann, R. Barbara, and S. Lakshminarayanan. 2009. The case for SmartTrack. Paper presented at proceedings of the 3rd international conference on information and communication technologies and development, Doha, Qatar.
Microsoft Corporation. 2008. Cell phone–based system could improve HIV/AIDS drug tracking. http://research.microsoft.com/en-us/collaboration/focus/health/smarttrack.pdf (accessed August 2, 2010).
Mills, E., S. Singh, K. Wilson, E. Peters, R. Onia, and I. Kanfer. 2006. The challenges of involving traditional healers in HIV/AIDS care. International Journal of STD and AIDS 17(6):360-363.
Morris, M., B. Chapula, B. Chi, A. Mwango, H. Chi, J. Mwanza, H. Manda, C. Bolton, D. Pankratz, J. Stringer, and S. Reid. 2009. Use of task-shifting to rapidly scale-up HIV treatment services: Experiences from Lusaka, Zambia. BMC Health Services Research 9(1):5.
Nature. 2006. It’s academic. Nature 439(7078):763-764.
———. 2010. The right kind of elitism. Nature 465(7301):986-986.
NIH (National Institutes of Health). 2010. Global Research Initiative Program for New Foreign Investigators (GRIP). http://www.fic.nih.gov/programs/research_grants/grip/index.htm#purpose (accessed August 16, 2010).
Nursing Sector Study Corporation. 2004. Building the future: An integrated strategy for nursing human resources in Canada. Immigration and emigration trends: A Canadian perspective. http://www.cna-nurses.ca/cna/documents/pdf/publications/immigration_emigration_trends_e.pdf (accessed February 22, 2010).
Ogden, J., S. Esim, and C. Grown. 2004. Expanding the care continuum for HIV/AIDS: Bringing carers into focus. Healthy Policy and Planning 21(5)333-342.
Omaswa, F. 2006. Informal health workers—To be encouraged or condemned? http://www.who.int/bulletin/volumes/84/2/editorial20206html/en/ (accessed August 5, 2010).
Omaswa, F., and J. Ivey Boufford. 2010. Strong ministries for strong health systems. New York: The New York Academy of Medicine.
Parfitt, B. 2010. Nurses—Making a difference in global health. http://www.2010iynurse.net/RNL_goal5.aspx (accessed July 7, 2010).
PEPFAR (U.S. President’s Emergency Plan for AIDS Relief). 2007. Nigeria: Military partnership extends life-saving antiretroviral treatment. http://www.pepfar.gov/press/83815.htm (accessed July 28, 2010).
———. 2009. Public-private partnerships. http://www.pepfar.gov/documents/organization/114616.pdf (accessed July 5, 2010).
Pfizer Inc. 2010. Infectious Disease Institute. http://www.pfizer.com/responsibility/global_health/infectious_diseases_institute.jsp (accessed August 24, 2010).
Preker, A. S., M. Vujicic, Y. Dukhan, C. Ly, H. Beciu, and P. N. Materu. 2007. Scaling up health education: Opportunities and challenges for Africa. Geneva: Global Health Workforce Alliance Task Force on Scaling Up Health Education.
RFFA (Rotarians For Fighting AIDS). 2010a. RFFA mission and brand. http://www.rffa.org/missionand-brand.php (accessed July 1, 2010).
———. 2010b. Rotary International: Kidz Clubs. 2010. http://www.rffa.org/kidz-clubs.php (accessed July 1, 2010).
———. 2010c. Rotary International: About Rotarians for fighting AIDS. http://www.rffa.org/aboutus.php (accessed July 1, 2010).
Riley, P. L., S. M. Vindigni, J. Arudo, A. N. Waudo, A. Kamenju, J. Ngoya, E. O. Oywer, C. P. Rakuom, M. E. Salmon, M. Kelley, M. Rogers, M. E. St. Louis, and L. H. Marum. 2007. Developing a nursing database system in Kenya. Health Services Research 42(3 II):1389-1405.
Rogers, B. L., and N. Youssef. 1988. The importance of women’s involvement in economic activities in the improvement of child nutrition and health. Food & Nutrition Bulletin 10(3):33-41.
Safe Blood for Africa Foundation. 2008. Safe blood programs. http://www.safebloodforafrica.org/programs.htm#nigeria (accessed August 24, 2010).
SAMSS (Sub-Saharan African Medical Schools). 2010. The SAMSS project. http://www.samss.org/display.aspx?project (accessed July 12, 2010).
Sanne, I., C. Orrell, M. P. Fox, F. Conradie, P. Ive, J. Zeinecker, M. Cornell, C. Heiberg, C. Ingram, R. Panchia, M. Rassool, R. Gonin, W. Stevens, H. Truter, M. Dehlinger, C. van der Horst, J. McIntyre, and R. Wood. 2010. Nurse versus doctor management of HIV-infected patients receiving antiretroviral therapy (CIPRA-SA): A randomised non-inferiority trial. The Lancet 376(9734):33-40.
South African Department of Health. 2006. Broad frame-work for HIV and AIDS and STI strategic plan for South Africa, 2007-2011. Pretoria, South Africa: South African Department of Health. http://www.doh.gov.za/docs/misc/aids.pdf (accessed September 24, 2010).
South African Nursing Council. 2010. Growth in students/pupils. http://www.sanc.co.za/stats/stat_ts/Growth%202000-2009_files/frame.htm (accessed October 27, 2010).
Stark, R. 2010. Presentation to the IOM committee on envisioning a strategy to prepare for the long-term burden of HIV/AIDS: African needs and U.S. interests, Pretoria, South Africa, April 13, 2010.
Stark, R., J. Donahue, S. Ford, and S. Senefeld. 2010. The AIDS relief South Africa partnership. Baltimore, MD.: Catholic Relief Services-United States Conference of Catholic Bishops.
Taché, S., E. Kaaya, S. Omer, C. A. Mkony, E. Lyamuya, K. Pallangyo, H. T. Debas, and S. B. MacFarlane. 2008. University partnership to address the shortage of healthcare professionals in Africa. Global Public Health 3(2):137-148.
Tettey, W. J. 2006. Staff retention in African universities: Elements of a sustainable strategy. Calgary, Alberta, Canada: University of Calgary (commissioned by the World Bank).
UNAIDS (The Joint United Nations Programme on HIV/AIDS). 2000. Collaboration with traditional healers in HIV/AIDS prevention and care in sub-Saharan Africa: A literature review. Geneva: UNAIDS.
———. 2008. Report on the global AIDS epidemic. Geneva: UNAIDS.
———. 2010a. Fact sheet: Treatment 2.0. Geneva: UNAIDS.
———. 2010b. Treatment 2.0: Is this the future of treatment? Geneva: UNAIDS.
UNCED (United Nations Conference on Environment and Development). 1992. Agenda 21: National mechanisms and international cooperation for capacity-building. Paper presented at UNCED, Conches, Switzerland.
UNFPA (United Nations Population Fund). 2005. Empowering women through education. http://www.unfpa.org/gender/empowerment2.htm (accessed September 13, 2010).
———. 2007. Women’s economic empowerment: Meeting the needs of impoverished women. http://www.unfpa.org/webdav/site/global/shared/documents/publications/2007/women_economic.pdf (accessed September 13, 2010).
University of KwaZulu-Natal. 2010. Undergraduate prospectus 2011. http://applications.ukzn.ac.za/Libraries/prospectus/2011_Undergraduate_Prospectus.sflb.ashx (accessed September 13, 2010).
U.S. Military HIV Research Program. 2010. Military–military PEPFAR programs. http://www.hivresearch.org/prevention.php?IndustryID=4 (accessed July 28, 2010).
USAID-AMPATH (United States Agency for International Development-Academic Model for Providing Access to Healthcare) (unpublished). 2010. PEPFAR quarterly performance report. IU-Moi Academic Model for Providing Access to Healthcare.
Uys, L. 2003. Guest editorial: Longer-term aid to combat AIDS. Journal of Advanced Nursing 1-2.
Vian, T., S. C. Richards, K. McCoy, P. Connelly, and F. Feeley. 2007. Public-private partnerships to build human capacity in low income countries: Findings from the Pfizer program. Human Resources for Health 5.
Vujicic, M. 2005. Macroeconomic and fiscal issues in scaling up human resources for health in low-income countries. Washington, DC: The World Bank.
W.K. Kellogg Foundation. 2010a. About the foundation. http://www.wkkf.org/who-we-are/who-weare.aspx (accessed August 23, 2010).
———. 2010b. Kellogg international leadership program in Africa. http://ww2.wkkf.org/default.aspx?tabid=55&CID=376&ProjCID=376&ProjID=15&NID=28&LanguageID=0 (accessed July 12, 2010).
Weaver, M. R., M. Myaya, K. Disasi, M. Regoeng, H. N. Matumo, M. Madisa, N. Puttkammer, F. Speilberg, P. H. Kilmarx, and J. M. Marrazzo. 2008. Routine HIV testing in the context of syndromic management of sexually transmitted infections: Outcomes of the first phase of a training programme in Botswana. Sexually Transmitted Infections 84(4):259-264.
Weaver, M. R., C. Nakitto, G. Schneider, M. R. Kamya, A. Kambugu, R. Lukwago, A. Ronald, K. McAdam, and M. A. Sande. 2006. Measuring the outcomes of a comprehensive HIV care course: Pilot test at the Infectious Diseases Institute, Kampala, Uganda. Journal of Acquired Immune Deficiency Syndromes 43(3):293-303.
WHO (World Health Organization). 2001. Strengthening nursing and midwifery progress and future directions: Summary document 1996–2000. Geneva: WHO.
———. 2004. WHO estimates of health personnel: Physicians, nurses, midwives, dentists, pharmacists. Geneva: WHO.
———. 2006. The world health report 2006: Working together for health. Geneva: WHO.
———. 2007a. Everybody’s business: Strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: WHO.
———. 2007b. Strategy 2004-2007: eHealth for health-care delivery. Geneva: WHO.
———. 2008a. The Kampala declaration and agenda for global action. Geneva: WHO.
———. 2008b. Task force on human resources for health financing: Global health workforce alliance. Geneva: WHO.
———. 2008c. Task shifting rational redistribution of tasks among health workforce teams: Global recommendations and guidelines. Geneva: WHO.
———. 2010a. Achieving the health-related MDGs. It takes a workforce! http://www.who.int/hrh/workforce_mdgs/en/index.html (accessed September 23, 2010).
———. 2010b. Análise dos recursos humanos da saúde (RHS) nos países africanos de língua oficial portuguesa (PALOP). Geneva: WHO.
———. 2010c. eHealth for health care delivery. http://www.who.int/eht/eHealthHCD/en/index.html (accessed August 5, 2010).
———. 2010d. International recruitment of health personnel: Draft global code of practice. Paper presented at sixty-third world health assembly, Geneva, Switzerland, May 20.
Zachariah, R., N. Ford, M. Philips, S. Lynch, M. Massaquoi, V. Janssens, and A. D. Harries. 2009. Task shifting in HIV/AIDS: Opportunities, challenges and proposed actions for sub-Saharan Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 103(6):549-558.










































