3
Measuring Health for Improved Decisions and Performance
In this chapter, the committee presents six recommendations to address the challenges described in Chapter 2: (1) improving coordination at the national level, beginning with the primary federal health statistics agency (the National Center for Health Statistics [NCHS]) and with federal health data and statistics activities in general1; (2) adopting the determinants of health perspective at a fundamental level (to complement the health system’s predominantly biomedical orientation); and (3) enhancing responsiveness of the population health information system to the needs of end users.
IMPROVING COORDINATION AT THE NATIONAL LEVEL
Critical to progress on these challenges is leadership at the federal level, largely by Department of Health and Human Services (HHS). While HHS has 30 statistical offices and programs, NCHS, which is located within the Centers for Disease Control and Prevention, is the nation’s lead health-statistics agency (NRC, 2009). Although the array of information produced by those multiple efforts is rich, its great fragmentation—and overlap, suboptimal coordination, and remaining unaddressed gaps (for example, in data elements and in research needed to improve the quality, usefulness,
and breadth of the information available)—makes the utility of the system’s combined efforts less than it should be.
Many of the data sets described in Chapter 2 are built from core data elements that have been static for many years and reflect the sum of the health of individuals with few data on measures of the health of a community. The committee’s vision of measurement includes both a reconsideration of the use of older measures that may be less amenable to local action and accountability and the building of new measures and potentially new measurement systems that report on more recently recognized loci for intervention.
NCHS’s current mission is “to provide statistical information that will guide actions and policies to improve the health of the American people. As the Nation’s principal health statistics agency, NCHS leads the way with accurate, relevant, and timely data” (CDC, 2009). Although recognizing the statutory underpinnings of its mission, the committee believes that the current implementation of the NCHS mission is too limited (e.g., to conducting surveys). The 2002 HHS document Developing a 21st Century Vision for Health Statistics states that the NCHS vision should (HHS, 2002)
-
Reflect all manifestations of health and health care delivery.
-
Encompass population health, transactions between the population and the health care delivery system, and the health care delivery system.
-
Address the relationship and potential synergy between public and private health data sets and national, state, and locally maintained data.
Those three points are congruent with the committee’s findings about the statistics and information system’s needs, gaps, and opportunities. NCHS’s current mission statement and the committee’s understanding of the agency’s scope of work suggest that its current role consists primarily of conducting several major surveys on population health, as well as managing the nation’s vital statistics system and managing surveys of nursing homes, hospitals, outpatient facilities, and other clinical care providers (NRC, 2009). The committee believes that NCHS can and should play a broader leadership role in the population health information system, expanding its analytic capabilities, its research activities, its ability to collaborate with those who use its data, and its ability to help to modernize and integrate the system. Transforming the way the mission of NCHS is implemented could broaden the array of activities in which NCHS engages beyond surveys and basic statistical work and toward activities that facilitate and provide guidance for the “translation” of data into information and knowledge that decision-makers and communities can use.
Facilitating a more highly integrated data system and a national popula-
tion health measurement strategy requires both governance and a high level of scientific guidance. In this chapter, the committee believes that NCHS, as the lead national health-statistics agency, must be strengthened to improve its ability to lead a system-wide effort toward better coordination and, as discussed below, enhanced information capacities for the health system. It is important to note here the roles of two federal advisory committees affiliated with NCHS: the Board of Scientific Counselors, which provides advice to NCHS, and the National Committee on Vital and Health Statistics (NCVHS), which is chartered to advise the secretary of HHS but is staffed in NCHS and closely identified with its work. NCVHS also has a population health subcommittee.2
The committee recognizes that two provisions of the Affordable Care Act (ACA)3 have potential pertinence to strengthening the nation’s population health information system. First, and most important, the new National Prevention, Health Promotion, and Public Health Council (NPHPPHC)—comprised of twelve cabinet secretaries and agency heads, under the leadership of the Surgeon General (Public Law 111-148)—offers an unprecedented opportunity for all sectors of government to come together around a de facto Health in All Policies effort. In recent years, there have been efforts around the country to examine the ramifications of all types of policy decisions on health outcomes, by using such tools as health impact assessments, as part of an approach called Health in All Policies, which calls for considering the health effects of all government policies and is internationally used (for example, in the European Union) (CDC, 2010b; Koivusalo, 2010). The council is to make “recommendations to the President and the Congress concerning the most pressing health issues confronting the United States and changes in Federal policy to achieve national wellness, health promotion, and public health goals, including the reduction of tobacco use, sedentary behavior, and poor nutrition” (Congressional Research Service, 2010).
The executive order establishing the council creates a forum for collaboration and coordination among twelve federal departments and agencies that have roles with implications for population health. For the purposes of enhancing the nation’s population health information system, the council’s composition (for example, the inclusion of other agencies) could provide an independent or fresh perspective from outside HHS that could be useful in supporting the department and NCHS (in addition to ensuring that the transformation of NCHS takes place as a primary requirement for meeting
the nation’s population health information needs). The council’s work could have ramifications for cross-department information and data efforts. For example, as discussed in Chapter 2 and below, data on determinants of health reside in many government agencies outside HHS, and linkages to make such data available to the public health community are not optimally developed or are in very early stages of development (the US Department of Agriculture Food Environment Atlas is an exception; see USDA, 2010). The council, under the leadership of the surgeon general, has been charged with preparing a national prevention strategy and an annual report on its progress in implementing the strategy.
Second, the act includes a provision to establish a Key National Indicators Initiative (Congressional Research Service, 2010). The initiative will develop and disseminate key indicators on health, education, the economy, agriculture, transportation, and other parts of American society in recognition of the cross-cutting information needs involved in forming a full picture of the status of American society. With respect to health, it could create a forum for integrating data from different levels of government and sectors.
A stronger and adequately resourced NCHS would be in a position to play a coordinating and leadership role in rationalizing, harmonizing, and integrating population health data collection, analysis, and reporting efforts and to provide scientific guidance on developing and selecting indicators and reflecting on the effects of various determinants of health. In continually reviewing the nation’s population health information system and its contributions to understanding health at the community and subpopulation level, NCHS could facilitate a move toward a more coherent system. In reviewing the major domains in which data are collected, the agency could call for new indicators to be added and for those of decreasing relevance to be culled. The process could be likened to those in other important societal arenas, such as changing the components of the consumer price index or the stocks included in the Dow Jones Industrial Average.
In its 2009 report Principles and Practices for a Federal Statistical Agency (Fourth Edition), the National Research Council’s Committee on National Statistics outlined the key characteristics and roles for such agencies as NCHS, including Practice 8 (an active research program intended to improve data content and the design and operation of data collection and to make information more useful to decision-makers) and Practice 11 (coordination and cooperation with other statistical agencies) (NRC, 2009). As noted in Chapter 2, two recent external reviews of NCHS’s National Health Interview Survey (NHIS) and its National Health and Nutrition Examination Survey have found that the agency needs greater financial and staff resources to undertake improvements in these major statistical activities, including methodologic and other research (NCHS, 2008, 2009). Three-fourths of NCHS’s estimated budget supports the purchase of data collec-
tion and reporting services from state and local governments, the Bureau of the Census, and private contractors (NRC, 2009), leaving few resources to support those other critical endeavors.
The committee has learned that others have examined the nation’s health statistics and information system and have suggested ways to enhance coordination and integration to serve the overarching objective of improving population health. Proposals have included a call, in the 2002 HHS document Shaping a Health Statistics Vision for the 21st Century, for an “integrating hub” to facilitate coordination of statistical activities within HHS (HHS et al., 2002) and a call for a population health record (Friedman and Parrish, 2010).
In its information-gathering sessions, the committee learned from public health practitioners that they often lack local-level data needed for fundamental planning and priority-setting and that federally produced statistics or measures meet only some of their information needs (IOM, 2010a,b). The committee heard repeatedly that the federal government’s own efforts to collect health-related data have historically occurred in silos (e.g., along vertical programmatic lines, with little or insufficient cross-cutting integration and collaboration) both within HHS and with other government departments and agencies. The population health information system as a whole is not ideally structured to facilitate interaction, collaboration, and data exchange and integration between the public and private sectors.
Another concern is minimizing inefficiencies to avoid burdensome procedures and costs for agencies and organizations, such as requests to provide the same data in different formats to different national, state, or local entities. Coordination is necessary to facilitate user access to data that originate from different government sources. That suggests the need for coordination to establish systems that maximize efficiency, streamline bureaucratic procedures, and expand the new HHS data warehouse (through the Community Health Data Initiative [CHDI] effort) while facilitating the integration of data from different sources on population health into an accessible, well-designed, and interactive interface to enable users to obtain relevant data at the geographic level of interest easily (see Chapter 2 and Appendix B discussion of CHDI, which represents a start).
Given the challenging nature of coordination and integration and the centrality of the need, the committee believes that a patchwork approach will not be adequate to meet the information needs of the health system. Comprehensive change, beginning at the core of federal work in this field, is needed to lead the way in addressing the gaps discussed in Chapter 2 and to support the development of a population health information system capable of responding to and forecasting the opportunities and meeting the challenges of the next decade and beyond.
Recommendation 1
The committee recommends that:
-
The Secretary of Health and Human Services transform the mission of the National Center for Health Statistics to provide leadership to a renewed population health information system through enhanced coordination, new capacities, and better integration of the determinants of health.
-
The National Prevention, Health Promotion, and Public Health Council include in its annual report to Congress on its national prevention and health-promotion strategy an update on the progress of the National Center for Health Statistics transformation.
The committee believes that NCHS is the right body to provide leadership in changing the nation’s population health information system because it is the nation’s main health-statistics entity, has a long history of work and accomplishment, and has many of the requisite connections with other federal agencies. Although federal agencies depend to a large extent on political realities and therefore have some limitations of independence, the committee was not able to envision a sustainable source of funding that would support a new public–private entity charged with playing the major coordinating role that it has described. The committee believes that the reporting structure laid out below, which includes an accountability mechanism, could help to buffer the agency against political vicissitudes that may affect its evolution to greater strength and capability.
The transformation of NCHS will require changes in the agency’s mission (or, more specifically, its implementation), capabilities, authority, and resources. Its current output is largely statistically analyzed data, but as described in this chapter, its role needs to be broadened to include capacities and activities to translate data into information and to conduct related research, such as research on the development and construction of indicators. Although “analysis by a statistical agency does not advocate policies or take partisan positions” (NRC, 2009), the committee believes that there is a substantial difference between advocacy and playing an active and central role in improving the quality and usefulness of indicators and other tools for disseminating population health information and enhancing the research infrastructure and agenda to support these activities.
An independent and influential external body will be necessary to oversee the progress of the transformation. Given the cross-cutting nature of the new NPHPPHC and the fundamental value and necessity of population health information for the prevention and health-promotion strategy that it is charged to develop, the committee believes that the council (with input from their Advisory Group on Prevention, Health Promotion, and Integrative and Public Health, which can provide input from other sectors) can play
an important role in monitoring changes in NCHS that can support or facilitate improvements in the nation’s population health information system as a whole. A considerable challenge is that NCHS will require continuing funding outside the political process. Although statistical agencies, such as NCHS, do not advocate, some of the information they produce could suggest or lead to action that is not consonant with particular political agendas. A possible solution would be to devote a portion of HHS funds to NCHS without requiring yearly appropriations.
The national prevention and health-promotion strategy is intended to include specific goals, and the NPHPPHC is asked to describe “corrective actions recommended by the Council and actions taken by relevant agencies and organizations to meet” the goals.4 The committee believes that NCVHS, working at the behest of the secretary of HHS, may serve as a technical resource to the NPHPPHC in evaluating the success of NCHS’s transformation (and the NCVHS Subcommittee on Population Health has additional expertise that would lend itself to this task, although it would need to include public health practice and community development). Although the executive order establishing the council does not explicitly refer to the centrality of statistics and measurement (and this is not one of the kinds of expertise listed in the charter of the advisory group of the council, which is still under development), the committee notes that the council’s first annual report lists eight principles that guide its work, including reviewing “data on the leading and underlying causes of death” as part of its focus on prevention (National Prevention Health Promotion and Public Health Council, 2010).
An adequately resourced and transformed NCHS would possess the mission, capabilities, resources, and authority to improve aspects of current activities and to undertake new activities. NCHS could
-
Coordinate research on and support the development of—within HHS and in collaboration with relevant stakeholders—several population health information tools and processes described in recommendations elsewhere in this chapter:
-
A standardized set of measures of community health (see Recommendation 2).
-
A standardized set of health-outcome indicators that can be used at the national, state, and local levels (see Recommendation 2).
-
A summary measure of population health (see Recommendation 2).
-
Modeling to elucidate the complex relationships between health and its determinants (see Recommendation 6).
-
|
4 |
Executive Order No. 13544, 75 Fed. Reg. 33983 (June 10, 2010). http://edocket.access.gpo.gov/2010/pdf/2010-14613.pdf (accessed June 14, 2010). |
-
Modernize national data sets to concentrate on indicators known to be pertinent to many conditions (for example, by combining NHIS, the Behavioral Risk Factor Surveillance System, and other questions about important social and environmental determinants not currently tracked in the data sets) and focus less on specific disease data sets.
-
Make recommendations about modern survey methods to collect more valid data efficiently. Modernizing could include better ways of performing household surveys, collecting responses electronically, and maximizing opportunities afforded by the shift from landline telephones to mobile phones.
-
Provide leadership in the uniform application of novel analytic tools.
-
Collaborate with other health-related government agencies, including on the collection of (and acting on) information on their user experience, their needs, and their use of available statistics.
NCHS already has strong or growing collaborative relationships with an array of federal departments and agencies, such as the Bureau of the Census and various HHS agencies and statistical units. NCHS could strengthen or cultivate additional linkages with other federal departments that produce statistics and information relevant to population health—such as the Departments of Agriculture, Transportation, Labor, and Education—and with external (private-sector) data organizations.
The committee acknowledges that calling for strengthening of a government agency does not address the fundamental need for coordination among public- and private-sector data sources. However, it is pleased to note (and endorses) the NPHPPHC’s guiding principle pertaining to public–private collaboration (National Prevention Health Promotion and Public Health Council, 2010), and believes that a federal advisory committee like NCVHS (which includes private-sector representatives, whose numbers could be expanded) can play a role in facilitating interactions between, for example, government and business.
Bringing Coherence to Indicators
Building an understanding of the forces that shape and create health requires development and testing of new and evolving indicators and continuing tests of their relationships to one another—for example, as facilitated by modeling. On the pages that follow, the committee describes indicators that are inadequately developed (community-health indicators), require rationalization and standardization (health-outcome indicators for national, state, and local data sets), or are in evolution (summary measures of population health).
A Standard Set of Community-Health Indicators
Chapter 2 summarized recent efforts to measure the health of communities and present the results as a ranking or in comparative fashion (Communities Count, 2008; Community Health Status Indicators, 2009; County Health Rankings, 2010; Saskatoon Regional Health Authority, 2007). Most of the indicators produced by such efforts are aggregations of various health and risk measures of individuals at specific times rather than measures of the overall health of communities in and of themselves (i.e., the health of the social and physical environments in a community). The current usage of the term community health indicators differs somewhat from the committee’s thinking about true measures of community health that convey information about characteristics of the community as opposed to aggregated data on its individual members.
Community-health indicators pertain largely to the local level. Consensus on the appropriate domains and indicators at this time is either impossible or extremely challenging. For example, there are different measures of “walkability” in a community—some that have been used in studies, such as pedestrian facilities (for example, sidewalk completeness and traffic-signal density) and street connectivity (street and intersection density), and some that have been included in municipal or community reports (for example, the ratio of sidewalks to roads in a community and the distance to such amenities as grocery stores, libraries, and parks; see, for example, Jakubowski and Frumkin, 2010; Zhu and Lee, 2008). Similarly, for healthy-food access or availability, there is no consensus about what indicators are best for different purposes—whether to select the ratio of convenience stores to grocery stores, the prevalence of fast-food outlets, or some other metric—and indicator validation has only recently begun (Glanz, 2009; Lytle, 2009). Social cohesion, trust, and support; health literacy; social vibrancy; and different types of environments all require consensus with respect to specific indicators (Lantz and Pritchard, 2010) that could be used and tested to further develop a balanced portfolio of community-health indicators. There also is no high-quality, widely accepted overarching measure of environmental health from an exposure perspective, although there are several focused measures, such as ozone and PM2.5 (Jakubowski and Frumkin, 2010). Both a more robust set of indicators and a set of criteria for selecting among them are needed (as an example, see Healthy People 2020 [HP 2020] criteria for selecting objectives [HHS, 2009a]).
Beyond their direct effects on the health of individuals, social, environmental, and economic factors rooted in communities also influence the overall health of communities, which in turn influences the health of individuals. (Chapter 1 summarizes some of the evidence on the determinants of health.) Community-health indicators are needed to capture, understand, and describe those factors to community members and to decision-makers.
Domains that require representation include aspects of the physical environment (such as sidewalks, pollution, green space, and housing), of social support (such as cohesion, social capital, and social efficacy and engagement), and of community vibrancy (such as participation in the arts and sports). The literature exploring the use of those indicators is developing. Some of the domains that may serve as examples include
-
Income and income distribution, education, unemployment and job security, employment and working conditions, early-childhood development, food insecurity, housing, social exclusion, social-safety network, sex, and race (Mikkonen and Raphael, 2010).
-
Scope of early-childhood development programs, education and skills, employment and good jobs, minimum income for healthy living, and healthy communities (community capital) (The Marmot Review, 2010).
-
Food and water, housing, a nonhazardous work environment, a nonhazardous physical environment, security in childhood, important primary relationships, economic security, physical security, and education (Doyle and Gough, 1991).
To track and understand those domains, public health agencies and their health-system partners at state and local levels require data from other sectors. For example, a local public health agency may have access to some indicators of the social determinants of health, such as educational attainment and income, but not to others, including more complex (or less well-understood or well-defined) community features or resources, such as social capital (Drukker et al., 2005; Prentice, 2006), the availability of healthy and fresh foods in the community, or the health literacy of its inhabitants. An employer or school planning department may need data on the community’s use of public recreational venues, such as parks, in developing physical-activity interventions.
The presence of smoking restrictions, requirements of menu labeling (before the ACA provision that pre-empted such local and state laws), pedistrian-friendly planning, and effective regulation of the clinical care system are all examples of regulatory and enforcement environments as good markers of aspects of community health (e.g., National Complete Streets Coalition, 2010).5 Communities that have higher levels of civic engagement
and similar characteristics are typically better equipped than others to enact policies that change environmental conditions to foster healthier behaviors (such as access to healthy foods and places for physical activity). Access to supermarkets and healthy food sources (and, conversely, the density of fast-food outlets, convenience stores, and liquor stores) is of established relevance to overweight and obesity and thus points to potentially important indicators of community health that could be routinely collected and shared.
In summary, although a number of national indicator sets include a few indicators of broad social determinants of health, the committee believes that unified guidance is needed to describe and build an evidence base for an actionable set of additional indicators that would support community decision-making with respect to local health-promoting initiatives. Data availability and research elucidating causal pathways may pose limitations, and the committee believes that galvanizing local partners to work in concert toward health gains will require a shared understanding of the factors that influence the health of communities. Developing that understanding rests on capturing new indicators and exploring their utility through experimental and observational studies and modeling.
The committee finds that many of the so-called community indicators that are in use focus largely on aggregates of individuals’ social risk factors, such as income and education, such health outcomes as mortality and disease-specific morbidity rates, and such individual risk factors as smoking. The committee recognizes that the evidence base available in many of the categories discussed here, including geographic relevance, is underdeveloped. It believes that knowing and communicating about the health of communities is essential for informing health-improvement efforts. Small area (community level) analysis is critical to identifying disparities, such as vulnerable subpopulations with considerably poorer health outcomes than those of the larger population (e.g., a metropolitan statistical area) within which they are embedded. The committee acknowledges the need for resources in capturing new information and understanding it.
A Standard Set of Health-Outcome Indicators
As discussed in Chapter 2, indicators of population health in the United States currently form a rich amalgam rather than a coherent whole that can be used in public health practice in a way that is considered and consistent over time. Although several existing measurement efforts described in Chapter 2 include a variety of health outcomes (i.e., distal outcomes such as disease rates and disease-specific mortality rates), and although such indicators are sometimes similar from one set to another and based on similar or identical sources of data, no standardized set of indicators has been vetted and found to be useful in serving population health planning at all levels.
The many sets of health indicators currently in use arose, understandably, to meet users’ varied needs. However, the existence of many indicator sets precludes gaining a single, coherent picture of population health in a consistent manner among communities and regions. Similarly, federal data sets and state and local efforts are not coordinated to the fullest extent to ensure efficiency and completeness, usefulness, and timeliness of the data. That can limit the ability of data-collection efforts to add relevant new indicators as the science develops and to discard indicators that are no longer useful. The committee believes that developing a core set of health-outcome indicators that identify priority health outcomes (aggregate distal individual health outcomes and indicators of behavioral risk) is a necessary step in a broader process to improve coordination and local-to-national relevance of data collection and indicator reporting efforts; however, such a set would not meet all needs, and it would need to evolve.
Indicators of health outcomes pertain to all geographic levels and refer to distal outcomes, such as disease and death. Such indicators are currently found in indicator sets like those described above. A core standardized set of indicators would ideally reflect a convergence of national, state, and local priorities, preferably embedded in a major national initiative, such as HP 2020 or the Key National Indicators Initiative. It would facilitate “apples to apples” comparisons of jurisdictions, allow the aggregation of local data to yield national figures, and support the linkage of national objectives, such as those in the Healthy People effort, to state and local objectives.
Summary Measures of Population Health
Because a summary measure of population health, described in detail below, would serve as a marker of the progress of the nation and its communities in improving health, it is important that it be implemented in data-collection and public communication efforts at the federal, state, and local levels. The committee believes that public officials need to take steps to educate Americans about the meaning of summary measures of population health and their linkage to determinants that are amenable to action at individual and societal levels.
Summary measures of population health that integrate information about mortality and morbidity are distal-outcomes measures that permit public health professionals, academicians, and decision-makers to understand trends in the health of populations and subpopulations. Referred to also as health-adjusted life years (HALYs), these measures have been used in local public health practice (Kominski et al., 2002) and in international settings (Ferrer et al., 2002; McIntosh et al., 2009; Murray et al., 2002) to establish distributions and burdens of disease, and they are routinely used in other nations to inform resource-allocation priorities in public health and
clinical care (for an Australian example, see Mitchell et al., 2009; for a British example, see Pearson and Rawlins, 2005; for an overview of use in other countries, see Neumann and Greenberg, 2009). Despite continuing development and validation by US and foreign academicians of the health-related quality-of-life measures on which HALYs are built, US health professionals and decision-makers have been slow to adopt them (Fryback et al., 2007).
In the United States and internationally, mortality-based indicators have functioned as the predominant final-outcome measure of the health of populations. Life expectancy and death rates provide important information about the different experience of nations, communities, and subpopulations. Disaggregated and presented by region and sociodemographic characteristic, they furnish critical information about health status and health inequalities that can be readily understood by decision-makers and members of the public. However, life expectancy is a blunt tool. It cannot capture the diminution in life experience and capacities that is associated with the chronic illnesses and injuries that are of increasing prevalence in modern society. Lessening of the burden of disease and attendant improvement in health-related quality of life are important objectives of population-based and clinical care delivery interventions. For example, use of life expectancy does not capture any information about the gains associated with the better dentition that accompanies fluoridated water or the better vision achieved with cataract surgery, and it only incompletely captures the effects of obesity and its sequelae (for example, arthritis and diabetes) on the health of Americans.
Representing the aggregate disease burden of a population requires a measurement system that captures the effects of morbidity as well as mortality. Over the last 35 years, there has been substantial development of measures of health status and of health-related quality of life. Some of the measures are specific to particular organ systems. For example, the Arthritis Impact Measurement Scale considers the quality of life of people who have arthritis (Meenan et al., 1982). The 25-item National Eye Institute Vision Functioning Questionnaire records the effect of visual disturbance on functioning and quality of life (Mangione et al., 2001). Those disease-specific measures are well validated and used clinically, but they do not allow assessments of the relative contributions of particular diseases or conditions to the overall health of populations. For example, effects on functional limitation on the basis of pain and on the basis of visual deficit cannot be captured with the same measure. In addition, comorbidities increase as a population ages, and disease-specific measures cannot chart the cumulative impact of arthritis, visual impairment, and obesity.
To address those limitations, generic measures that are not tied to any disease or condition have been developed. Under the umbrella of HALYs are quality-adjusted life years (QALYs) and disability-adjusted life years
(DALYs), both of which allow the quantification of effects of disease and social determinants on health and permit the study of how clinical care and population-based interventions can alter them. Although both QALYs and DALYs create combined estimates of morbidity and mortality, the functions they were originally envisioned as serving—DALYs to capture global burden of disease, and QALYs as an outcome measure in cost-effectiveness studies—led to different approaches to capturing their morbidity aspects (Gold et al., 2002). From a practical perspective, both are currently used to serve either function, but in the United States and in Canada, the dominant form of HALY in use is the QALY.
QALYs are built from descriptive systems that include dimensions of function and symptomatology that are widely understood (e.g., in different cultural contexts) to characterize the varying effects of disease and disability on functioning. Health-related quality of life (HRQL) measures combine two sources of information: health states and health weights. Health states categorize levels of functioning in domains that include physical activity, mobility, pain, cognition, and mental state. Once a particular health state is described with respect to levels of function in different domains, information is collected from a representative sample of the community to weight the value of the health state relative to others. The point of the weighting is to capture the desirability of the health state (composed of many domains at levels of function) with a single number that can allow comparisons among diseases and conditions. Different techniques are used to aggregate responses into a single number on a 0–1 scale (where 0 = death and 1 = perfect health) that represents the average value of that health state in a population. The weight associated with a particular health state is the average of the preferences for that state in a sample of people in the community (Gold et al., 1996).
As with life expectancy, the average HRQL of different populations and across all health conditions can be examined on the basis of geography, demography, and other environmental and social determinants of health. The HRQL of a representative sample of Americans has been shown to be higher in groups that have more education and income and is inversely related to age (Lubetkin et al., 2005).
In the final step in creating summary measures of population health, the life expectancy of a population is combined with its HRQL to create “health-adjusted life expectancy” (HALE). (For a more detailed accounting, see Asada, 2010; Erickson, 1998; Gold and Muennig, 2002; Gold et al., 1996; IOM, 1998; Murray and Lopez, 2000; Murray et al., 2000; Pearcy and Keppel, 2002; Stiefel et al., 2010.) The relationships of the different indicators are illustrated in Figure 3-1.
HALE and HALYs represent the effects of any health condition and allow aggregation across all the conditions that can affect a population.
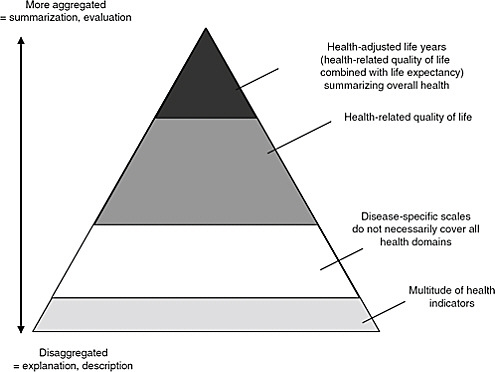
FIGURE 3-1 Data pyramid for population health.
SOURCE: Fryback, 2010, adapted from Wolfson.
They can provide information on the effects of particular illnesses, such as diabetes or cancer, on the health of a population (Boswell-Purdy et al., 2007; Manuel and Schultz, 2004). They can provide insight into regional differences associated with behavioral risk factors, such as smoking levels (Jia and Lubetkin, 2010). They can also allow examination of the health experiences of subpopulations by race and ethnicity and of exposure to different social and environmental risk factors. For example, using an HRQL measure from the Medical Expenditures Panel Survey and linked mortality data, Muennig and coauthors studied a number of social and behavioral risk factors and found that poverty, smoking, and high school dropout rates imposed the greatest burden of disease on Americans (Muennig et al., 2010). That study adds to the growing literature that has demonstrated the larger inequalities that race and socioeconomic status exact when measurement accounts for both health status and longevity (Franks et al., 2006; McIntosh et al., 2009; Muennig et al., 2005).
Over the last decade, use of the HALE and HALY summary measures has grown in both domestic and international clinical care and population
health (e.g., policy) settings. Because of their ability to paint an overall picture of the health of a community or a country, they have been referred to as a gross domestic product (GDP) for the health sector (see, for example, IOM, 1998; Wolfson, 1999).
Despite their versatility, HALYs and QALYs are not routinely used in health and health-system monitoring in the United States. Uptake has been slow in part because of the disparate approaches taken to measurement of the HRQL aspect of HALYs. However, recent work has shown relative concordance in outcomes of studies that compared existing measures, and a group of academics and policy-makers has called on the field to designate a measure that can be used in different types of population health and clinical care studies, as has been done in England and in Canada (Drummond et al., 2009). In addition, decision-makers have been leery of summary measures, largely because of the use of QALYs as an outcome measure for cost-effectiveness studies. In policy debates that date back to the Oregon Medicaid experiment (Kaplan, 1994), QALYs have been represented variously as discriminating against people who are disadvantaged on the basis of disability, age, and social position because they stand to gain fewer HALYs from life-saving interventions than would accrue to people who are in better health or have longer life expectancy (Harris, 1987; Rawles, 1989). That view has been countered by others who have noted that cost-effectiveness analyses that use QALYs as outcome indicators do so from the perspective of a general population and do not evaluate economic efficiency on the basis of subpopulation characteristics (Russell et al., 1996). In the ACA, however, the new Patient-Centered Outcomes Institute is prohibited from using a “dollars per quality adjusted life year (or similar measure that discounts the value of a life because of an individual’s disability) as a threshold to establish what type of health care is cost effective or recommended” (Garber and Sox, 2010; Neumann and Weinstein, 2010).
Although summary measures of population health like QALYs are prominent in discussions of rationing and the debate around the approach to curtailing clinical care costs, the uses of HALYs are far broader, permitting methods for monitoring health and for forecasting or directly studying the effects of different health and clinical interventions on communities and subpopulations. In public health settings, such as the Los Angeles County Health Department, DALYs have been used to provide information to support priority-setting (Kominski et al., 2002, 2010). More recently, Washington state has been using QALYs in priority-setting for population health (personal communication, A. Mokhdad, 2010).
In 1990, the HHS Healthy People initiative stated as its first goal “Improve Years of Healthy Life for all Americans”—a health-adjusted life expectancy indicator (HHS et al., 2001). Lacking an agreed-on measure with which to track years of healthy life, NCHS created a composite placeholder
measure with the intent of developing a more enduring approach for future use (Erickson et al., 1989; Gold et al., 2002).
Although this placeholder measure has not yet been replaced in national data sets, a growing understanding of the value of overall health measures has led to recent work by NCHS staff with international colleagues representing government and health organizations to identify and test concepts of health and function that are meaningful across countries and cultures (Taskforce on Health Status, 2005; The United Nations, 2010). The work of standing international committees (the Budapest Initiative and the Washington Group) has led to testing of measures that can be used to track progress and make comparisons internationally (see Box 3-1 for more details) (Madans, 2009; WHO et al., 2007). Questions on function—in domains that include vision, hearing, cognition, self-care, mobility, pain, fatigue, anxiety, and depression—are being tested on a sample from the 2010 NHIS, and the plan is to include a selected set on the full sample in 2011. The international working groups have identified the need to develop a “principled” weighting system derived from an empirical foundation or other agreed-on theory-based analytic technique that will unite the individual concepts of function into a summary measure. A measure arising from those efforts, which has been vetted by international and US measurement experts and is used at the national level, offers a model for building a
|
BOX 3-1 The Budapest Initiative and the Washington Group The Budapest Initiative (originally called the Task Force on Measuring Health Status) held its first meeting in 2005 and is a collaborative effort involving national statistics offices and other international organizations working in health statistics with the objective of developing internationally comparable measures of health states. The measures could be used to develop a core set of health indicators for use at the local, national, and international levels (Taskforce on Health Status, 2005). The purposes of the Washington Group (established in 2002) are to
|
standardized measure of population health that can eventually be deployed at all levels of community.
In addition to functioning as outcome variables that permit building an evidence base for programs and policies, summary measures of population health hold potential for capturing public attention with respect to the health of their communities. The 1998 Institute of Medicine (IOM) report Summarizing Population Health (IOM, 1998) suggested that a broader understanding of the meaning of the measures would be helpful in alerting all Americans to the health experience of the United States and their own communities. Because the HALYs of a community represent the combined health experiences of its members (rather than a disease-by-disease characterization, as many current measures do), clear differentials among communities provide an overall picture of the health fortunes of a region or a subpopulation. Concerted efforts that familiarize Americans with the meaning of the measures, such as portraying them in terms of the “GDP of health,” will be a key step in building the understanding that can galvanize action in and on behalf of populations and communities where health disparities are prominent.
The committee echoes the finding of prior work from IOM (IOM, 1998, 2003, 2006, 2009) and others that use of HALYs and life expectancy will markedly advance tools for tracking the health of populations and understanding what influences it. By embedding the building blocks with which to calculate HALE and HALYs in routine data-collection efforts at all geographic levels, the health system can gain a greater understanding of the effects of clinical care, population health interventions, and social policies on the health of the nation, its communities, and subpopulations that have been historically at higher risk for poorer health outcomes. As the most distal outcome measure (see Figure 3-2) in a coherent data system, HALE
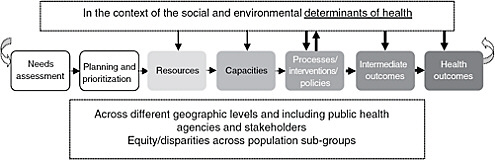
FIGURE 3-2 From inputs to outputs logic model.
NOTE: The thickness of some arrows denotes the present report’s focus on those interactions.
and HALYs allow the building of models that can inform predictions and assessments of how investments in different parts of the health system will contribute to the health of the nation.
Public health professionals would use summary measures of population health to track changes in their communities and evaluate the success of particular initiatives over the long term inasmuch as population health changes slowly. One way that a summary measure was used in the past was as one of the top three goals of the Healthy People 2000 initiative—to “increase years of healthy life for all Americans”—a goal that was tracked throughout the initiative’s implementation. Public health workers can also use summary measures, such as HALYs, to set priorities for resource expenditures by determining, for example, whether an obesity-related initiative that cost a given amount could improve HALYs by a particular percentage and would constitute a better investment than pursuing an injury-prevention (or other) program. Interventions that target different outcomes are not mutually exclusive, and the example provided is only an illustration of the type of use to which HALYs may be put. By conducting a “what if” analysis (for example, modeling with HALYs), a community might find that a particular type of investment in population-based initiatives could generate a particular number of HALYs at a particular cost and thus save money in the clinical care delivery system.
The committee finds that the nation’s health statistics and information system lacks the categories of measures that could support the information needs of policy-makers, public health officials, health-system partners, and communities. No category of measure tells the complete story or offers a complete picture of health in the nation and in the community, and they each have limitations (for example, HALE needs to be disaggregated to allow understanding of reasons for disparities among localities, nations, and subpopulations and identification of more specific, actionable factors). But HALE and HALYs, community-health indicators, and outcome indicators complement each other as tools to inform and to galvanize action.
Recommendation 2
The committee recommends that the Department of Health and Human Services support and implement the following to integrate, align, and standardize health data and health-outcome measurement at all geographic levels:
-
A core, standardized set of indicators that can be used to assess the health of communities.
-
A core, standardized set of health-outcome indicators for national, state, and local use.6
-
A summary measure of population health that can be used to estimate and track health-adjusted life expectancy for the United States.
Ideally, these activities will be conducted with advice from a fully resourced and strengthened NCHS (see Recommendation 1) and will include systematic, periodic review of indicators to ensure their sustained relevance and usefulness.
The committee was not constituted to and did not endeavor to develop lists of proposed indicators. The process of developing and reaching evidence-based consensus on standardized indicator sets will require considerable research, broad-based dialogue (involving all relevant parties), and prioritization to come up with a parsimonious set. Research would include modeling and other efforts to elucidate the linked nature of many determinants of health and intermediate indicators of health where provision of information can lead to actionable measures at all geographic levels. A national effort to accomplish this may initially require defining a modest core set that all localities would be encouraged to use (e.g., to support comparisons and allow “rolling up” from the local to the state and even the national level), additional optimal indicators could be identified for other outcomes or community characteristics of interest to some localities.
The process of developing and reaching evidence-based consensus on indicator sets will require considerable research (including modeling and other efforts to clarify the complex, overlapping pathways between the many determinants of health and population health outcomes and the interrelated effects of interventions), dialogue, and prioritization to come up with reasonably sized sets of indicators. As has been often noted, one of the challenges of the Healthy People process has been the lengthy list of objectives and indicators, which may contribute to the difficulties of communicating, tracking, and reporting on progress in meeting them. HHS has been examining ways to streamline Healthy People and make it a more useful tool for planning (see, for example, NORC, 2005). (See Table 3-1 for sample outcome indicators and indicators of community health.)
TABLE 3-1 Sample (Distal) Outcome Indicators and Indicators of Community Health
|
Categories of Indicators |
Examples |
|
Community health (indicators of the health of the community itself—refers partly to indicators of determinants of health in local contexts) |
Walkability Food insecurity Fresh-food availability Safety (gun-associated violence) Cohesion, social capital, social networks Inequity (e.g., data on distribution of clinical care, civic engagement, discrimination [real and perceived], education, and risk behaviors are accessible) Educational attainment, such as average years of schooling Physical environment (safe communities, diverse ecosystems, climate change, toxic exposures, health-promoting exposures) |
|
Health outcomes (mostly distal, but also behavioral risk factors; aggregate indicators of individual health or health risk and risky behavior) |
Smoking rates Cardiovascular disease Disease-specific mortality Infant mortality Life expectancy Asthma Health or functional status Health-adjusted life expectancy |
ADOPTING THE DETERMINANTS OF HEALTH PERSPECTIVE AT A FUNDAMENTAL LEVEL
The inputs-to-outputs logic model provided in Chapter 2 (see Figure 3-2), showing how steps in the population health improvement process are connected, illustrates the feedback loop between processes or interventions that modify determinants of health, which in turn become improved intermediate outcomes. The logic model also highlights the importance of understanding the causal relationships and interrelationships among the health outcomes, determinants, and evidence-based interventions.
Individual characteristics (e.g., genetics, sociodemographics, and health behaviors), community characteristics (physical and social environment), and clinical care all contribute to the total health of a community, a state, or a nation. The aggregated experience of individual people in health-related quality of life and longevity was viewed by the committee as the common distal health outcome that the health system works to maximize.
Chapter 2 described the categories on the far right of the logic model as having more indicators available (for example, on disease-specific out-
comes, data such as rates of cardiovascular disease [CVD] and cancer incidence) than those on the left. Also, some of the data that exist on the left side of the continuum (on capacities, performance) is found in the clinical care context—illustrating yet another reason for sharing and collaborating between the clinical care and public health communities. Those on the right side, however, typically draw on data from sources oriented toward the medical model and generally lack a determinants-of-health orientation in their reporting. Many categories of determinants of health are not measured by government-sponsored population health surveys, as this report has discussed in the section on the need for community health indicators. Information that is central to understanding health and promoting action to improve it often resides in government databases outside HHS or in the private sector. Examples of the former include information maintained by agencies in the US Department of Agriculture (the sources used in the department’s Food Environment Atlas), the Department of Commerce (Bureau of the Census data sets, such as the American Housing Survey and the American Community Survey), the Department of Transportation (the National Household Transportation Survey), the Bureau of Economic Analysis, and the Bureau of Labor Statistics (the Current Population Survey). Examples of the latter include data available from the food industry, retailers, local authorities, Web search engines, and other consumer- and industry-focused services (see, for example, Brownson et al., 2005). Making explicit the different contributions of many sectors to the social and environmental determinants of health demonstrates the need for sharing, linking, and integrating data that suggest opportunities and provide a more complete picture of the health of a community. That will require a broadening of the array of information available through public–public and public–private collaborations.
The committee believes that a national conversation is needed to transform how Americans conceptualize the factors that influence health outcomes and to demonstrate the potential contributions of moving beyond the medical model toward an ecologic, population-based approach to health improvement. It would afford clinical care the weight it merits as well as heighten understanding of the myriad other loci available for action. Other wealthy nations brief their populations on the social and environmental determinants of health, and such efforts are intended to heighten awareness and promote action that leads to improved health and health equity. International efforts that examine health status include the Human Development reports of the World Bank and the work of the World Health Organization.
National dialogue about health in such nations as Canada and the United Kingdom (UK) routinely includes references to determinants of health and to inequalities in health status that are related to socioeconomic status (for an overview of these issues, see Chapter 1). For example, the Canadian
Senate’s Subcommittee on Population Health released a report (2009) titled A Healthy, Productive Canada: A Determinant of Health Approach. The report listed the multiple determinants of the health of Canadians (housing, physical environment, early childhood environment, education, income and social status, employment and working conditions, and culture and sex) and showed that clinical care—on which Canada, like the United States, outspends many peer nations—alone cannot improve health outcomes. Other, older contributions to the higher profile of social and economic factors outside the United States include the UK’s Acheson report on inequalities in health and their causes (Lowdell et al., 1999) and the Canadian report by Evans and colleagues titled Why Are Some People Healthy and Others Not? The Determinants of Health of Populations (1990). Another relevant report was prepared by the Commission on the Measurement of Economic Performance and Social Progress at the request of French President Nicolas Sarkozy. In that report, Stiglitz and colleagues (2009) responded to the concern that France was overrelying on the GDP as an indicator of national well-being. Stiglitz et al. showed the need for and importance of other indicators both to inform the nation on its progress and to spur change, and they proposed new approaches, such as transforming statistical systems, to measure the dimensions of well-being, including health, and to complement what the GDP shows about a nation’s trajectory. The British report Fair Society, Healthy Lives: A Strategic Review of Health Inequalities in England Post (The Marmot Review, 2010) provides another example of a major government-commissioned report that is being rolled out throughout the UK and is intended to lead to “developing policies, building capacity and recommending practical steps to address the social determinants of health.”
A high-visibility annual report that describes the health of Americans on the basis of sociodemographics and other social and environmental determinants is a missing element in changing this nation’s narrative on health. As we gain further understanding of community-level indicators that directly influence the health of individuals, increasingly rich information on social and environmental determinants of health can be made available at national, state, and local levels. Wide dissemination of this sort would allow people everywhere to better understand the forces that create and detract from health in communities and thereby drive responses and actions appropriate to local conditions. Compilation of such data is resource-intensive, however, and some of the information is not available in many localities. An immediate and feasible first step would be to produce a national report that regularly updates and highlights the nation’s health, focusing on a determinants model.
Recommendation 3
The committee recommends that the Department of Health and Human Services produce an annual report to inform policy-makers, all health-system sectors, and the public about important trends and disparities in social and environmental determinants that affect health.
A strengthened and adequately resourced NCHS could play a central role in the development of such a report. The report would require some additional infrastructure to accomplish the secondary research, analyses, and other activities. In addition, although the report would presumably include state-level data, large metropolitan areas would ideally be included. Undertaking such an effort would require financial and human resources, but the committee was unable to examine these in any detail.
RESPONSIVENESS TO THE NEEDS OF END USERS
Some aspects of responsiveness to the need of decision-makers and communities would be addressed by implementation of Recommendations 1 and 2, pertaining to strengthening NCHS to play a greater leadership role in the nation’s population health information and statistics system, and to the development and implementation of a summary measure of population health and two standardized sets of indicators. Below, the committee provides rationale for and offers two recommendations that pertain both to the population health-clinical care interface and to the overarching need for modeling and related research to support information needs. The discussion of modeling also points back to the earlier discussion about the determinants of health; the field’s understanding of how these influence health could be greatly enhanced through modeling and related analyses.
One of the challenges facing the population health information system is intersectoral information exchange, coordination, and collaboration, including the interface between public health agencies and the clinical care delivery system but extending to education, transportation, and other fields in which public-sector and private-sector decisions can affect population health.
The interface between the clinical care system and public health agencies is a major potential source of valuable information on population health, but, as discussed below, various concerns must first be addressed. Some information pertinent to population health and not available from national population health data sets may be obtained from clinical care sources, including information on chronic-disease prevalence and prevention, prevalence of a wide array of diseases, and functional status (HHS et al., 2002; Luck et al., 2006; NCVHS, 2010). Public health agencies interact
with the clinical care system in various ways, in addition to providing some primary-care services themselves. The interactions may take the form of surveillance for reportable diseases, vital records, and statutorily established regulatory roles for selected state public health agencies, such as licensing and certification of hospitals and nursing homes. Some state and local public health agencies also perform the role of health-information stewards, analysts, and technical advisers, collecting population health–relevant data from providers in a community and conducting supporting activities to help providers to improve their performance and patient outcomes. It should be noted that some public health agencies are combined with or include departments that oversee clinical services, whereas others are separate from departments charged with clinical care assurance. One example of a clinically oriented public health program may be found in New York City, where the Department of Health and Mental Hygiene has established a hemoglobin A1C registry that mandates laboratory reporting of hemoglobin A1C test results, involves over 1,000 providers, and is designed to improve diabetes management in the city (Chamany et al., 2009). As another example, New York State has had a coronary-artery-bypass-surgery registry in place since 1989. Its intent is twofold: to provide information to clinical care teams and hospitals for quality improvement, and to alert the public about which centers are the best performers (Hannon and Beach, 1994). At the national level, the Centers for Medicare and Medicaid Services (CMS) began tracking “never” events (medical errors and untoward outcomes that should never occur, such as wrong-site surgery, bedsores, and hospital-associated infections) and began denying payment for any clinical services provided to address such events.
Immunization registries are an early form of a population health information system designed for a specific purpose and overseen by public health agencies of states and large cities. Immunization-information systems receive data from and provide data to the full array of immunization providers, including private clinical practices, federally qualified health centers, and public health clinics. In areas where health-information exchanges are operational—such as Indiana, Michigan, and Rhode Island—public health agencies become involved in the exchange. Regional health-information organizations have been organized in several areas to rationalize and facilitate secure health-information exchange among providers in a community or region, including public health agency clinic health-information systems.
In building a coherent data system that monitors health and evaluates interventions and policies that improve it, the clinical care system has much to contribute to the health-information system. Reporting of particular types of data from the clinical care delivery system to public health can accomplish two major functions:
-
Conducting population-based surveillance and assessment by providing information that can be uniquely and efficiently gathered in the clinical care system to form a more complete picture of the health of a community and the people in it.
-
Monitoring the quality and safety of clinical care services to provide information that can enhance performance and accountability of the clinical care system (this includes enhancing the use of clinical preventive services to address such risk factors as smoking and effective management of chronic diseases with the greatest population impact and preventing harm that can arise in the clinical care setting).
Population-Based Surveillance and the Clinical Care System
Population-based surveillance and information can be transmitted bidirectionally between the public health and clinical care delivery systems to help each fulfill its mission and target its activities better. For example, although it is financially daunting to mount a health-examination survey in every community, some key information already present in the clinical care system in many communities can be used to assess the prevalence and control of diabetes, hypertension, and hyperlipidemia and the use of clinical preventive services. The current state of data-sharing between public health agencies and medical care organizations varies greatly from one jurisdiction to another, and data-sharing is poorly standardized. For example, most state public health agencies use an immunization-information system (or registry), but participation of clinical care providers in the system may range from 100 percent to far smaller proportions, especially in communities that have many independent practices with little access to technology. Some 75 percent of public and 37 percent of private immunization providers participate in registries (Hinman and Ross, 2010). In addition to immunization registries, cancer registries and disease- and injury-reporting systems (such as the National Electronic Injury Surveillance System: Cooperative Adverse Drug Events Surveillance System) provide examples of the public health use of clinical data. Those systems serve important public health purposes, but they also present challenges. For example, because of the nature of their structure (organized in vertical programmatic “silos” without optimal coordination), they place additional reporting burdens on the clinical care system, requiring partially redundant data collection and reporting or requiring entry of different types of diagnoses into multiple databases rather than into an integrated, multipurpose database.
The increased emphasis on and support of electronically collected and stored information in the clinical care delivery system creates rich opportunities. For example, data obtainable from electronic health records (EHRs)
include claims for services and medications and laboratory data and could be integrated with or superimposed on information from population surveys that estimate prevalence on the basis of such questions as, “Has a doctor or a nurse ever told you that you have diabetes?”
The committee was mindful that use of electronic information creates procedural and logistical challenges. One logistical challenge arises because many people see a variety of providers who may not be electronically linked. Several other challenges arise from the ability of public health agencies to access medical care data for public health purposes. However, those data may not be accessible at the interface between providers and their patients, and there may be serious concerns related to privacy, right of access, and intended use of personal data. A different type of problem emerges from reporting of notifiable diseases. Such reporting has become markedly streamlined with direct reporting of results by laboratories and emergency rooms to the public health infrastructure. However, public health agencies and all partners in the health system must maintain caution to avoid the pitfalls of this more complete access, including the potential of spending more time and energy in collecting data than in using it thoughtfully.
Clinical care data can contribute substantially to public health agencies’ knowledge of population health and enhance their ability to identify and solve community health problems. This is also Essential Public Health Service #1—“monitor health status to identify and solve community health problems”—as described in Ten Essential Public Health Services developed by the Core Public Health Functions Steering Committee in 1994. Also, public health agencies can provide denominator data that can be helpful to clinicians. However, barriers exist to data-sharing and collaboration, and solutions must be identified. Although there are great hopes for the universal implementation of EHRs, their existence alone does not remove the obstacles to making needed population-based information widely available.7 Both thought and resources need to be put into defining what information is best harvested from the clinical system and how it should be obtained. Simply providing open-ended clinical care data to public health authorities will not be acceptable to the clinical care system or the public. Other considerations and barriers to unrestricted use and sharing of this information with the broader health system in a community include the following:
-
Health departments are, in general, authorized to receive confidential information from clinical sources for public health purposes. They are also generally required to keep such information confidential, so information released to other parties must be stripped of any potentially identifying information.
-
Public health surveillance is regarded as “practice,” not “research,” and so is not subject to consideration by institutional review boards or informed-consent requirements, although public health agencies recognize the importance of appropriate use and safeguards of the data to protect privacy and confidentiality. Analyses conducted by nongovernment entities are subject to different constraints.
-
Information that can be linked back to providers, clinical care systems, or insurance companies may be viewed as proprietary by those providers or systems and therefore less likely to be reported if released publicly in a way that maintains that link. Related concerns stem from the potential effects of data-sharing on reimbursement and medicolegal liability.
-
Key information useful for understanding population health—such as race, ethnicity, and educational achievement—might not be routinely collected by providers, and its collection might entail extra cost and effort. However, the Health Information Technology for Economic and Clinical Health Act requires the collection of demographic information for payment.
Great care will be needed to change the current state with legislation, funding, logistics, and technology and to define the attributes of the mechanisms for maximizing the use and usefulness of clinical care data to health-system stakeholders.
For data-sharing to be successful, it is critical that benefit flow from government public health agencies to clinical care stakeholders. For example, providers of clinical care need easier access to their own data that are submitted to government entities (federal, state, or local), access to analyses to help them benchmark and improve the appropriateness of the care they deliver, and access to other population health data (such as disparities and determinants) that are pertinent to the groups they serve so they can tailor their clinical care and community services to the population served to meet needs and improve outcomes.
The committee agrees with others who have commented on the actual and potential value of clinical care system data to inform population health efforts, including filling gaps in data available from other sources (NCVHS, 2010). The Office of the National Coordinator for Health Information Technology has emphasized the importance of including public health and population health goals in its various activities, and continued attention
from relevant groups will be needed to assure that investments in e-health initiatives do consider the population health and public health relevance of electronic health records and related efforts.
Recommendation 4
The committee recommends that governmental public health agencies partner with medical care organizations and providers in their jurisdictions to share information8 derived from clinical-data sources, when appropriate, to inform relevant population health priorities. Such information will support core health indicators that are otherwise unavailable at some or all geographic levels.
Indicators shared in that way may include prevalence data on traditional risk factors (such as smoking, lack of physical activity, and hypertension) and measures of preventive-service delivery and chronic-disease control. Other indicators that help in assessing the readiness of the community to interact with the clinical care delivery system in an informed manner might be added to the clinical data collected. They include measures of health literacy (Adams, 2010; DeWalt et al., 2004) and patient activation (Hibbard et al., 2004; Mancuso and Rincon, 2006; Paasche-Orlow and Wolf, 2007). Both health literacy and patient activation are known to influence outcomes in the clinical setting favorably (Adams, 2010; Hibbard et al., 2004).
The use of EHRs has accelerated in recent years, owing in part to such federal government initiatives as the creation of the Office of the National Coordinator of Health Information Technology in HHS and funding through the American Recovery and Reinvestment Act. At the state level, Minnesota has set deadlines for universal adoption of EHRs by all hospitals and clinical care providers (Mayberry and Hunkins, 2008). EHRs raise questions about equity, generalizability, and overreporting, and the use of clinical care data for population health purposes presents considerable concerns related to privacy and confidentiality (Safran, 2007). Although ample statutory protections are in place both for patients and for the public good, these related but discrete objectives (i.e., individual and societal needs) must be constantly held in balance, and all necessary actions to preserve this balance (and the credibility of all system components entrusted with personal identifying data) must be sustained with transparency and deliberation.
Clinical care data by definition include only information that is obtained in the clinical care system and are therefore not equivalent to population-based data. Although EHRs are limited in their ability to capture undetected
disease in the community, they can provide some insights into the descriptive epidemiology of disease (Califf and Ginsburg, 2008). A later report on law by the present committee will explore this more fully; any public health role in monitoring clinical care quality and outcomes through the use of personal health information requires a broader discussion about the role of government and the scope of government involvement.
Monitoring Outcomes of the Clinical Care System
Monitoring of the outcomes of the clinical care system by public health agencies can provide critical information about appropriate use, overuse, underuse, and misuse of medical technologies and can make the clinical care delivery system more efficient. However, different jurisdictions might make different decisions regarding whether this function is best housed in government public health agencies.
The American clinical care system has extraordinary capabilities, but it is also inefficient and is itself the cause of adverse events (IOM, 2000; Orszag, 2008). Policy-makers and clinical care system leaders in both the public and the private sector are increasingly recognizing and seeking to address those serious challenges. The American public is generally unfamiliar with the related notions of evidence-based medicine and comparative effectiveness (and the clinical field’s broader emphasis on improving quality, effectiveness, and efficiency). It is a sad testament both to the generally low levels of health literacy of the American public and to the unsuccessful efforts by the educational and clinical care systems and others to inform and educate the public (Clancy and Cronin, 2005; IOM, 2004). Many American patients assume that more clinical care is better care—for example, that care by specialists is generically better than that by primary-care providers, that more intensive treatments are more effective, or that the newest medical product is the best (Carman et al., 2010).
A variety of sources provide information on the quality and outcomes of clinical care in the United States. They include the Dartmouth Atlas Project, which “examines regional variations in the practice of medicine and in spending for health care, principally in the Medicare population” (Fisher et al., 2009); the National Healthcare Quality Report produced annually by the Agency for Healthcare Research and Quality; data sets and reports prepared by such clinical quality organizations as the National Committee for Quality Assurance, the National Quality Forum, and the Joint Commission; and a variety of reports produced by health plans and other medical-care organizations. However, much more (especially on the use of preventive care and on clinical care–associated harm) could be communicated to the public in an easy-to-understand format and in the context of a broader effort to inform and educate the public about effectiveness and efficiency in clinical
care and to support more informed decision-making by patients. The committee believes that public health agencies can play an important role in reporting to the public on local clinical care system performance.
Research on the effects of public reporting of clinical care system performance, including quality of care, shows that its effects on consumers are mixed. They depend on characteristics of consumers themselves, consumer awareness of the availability of such information, the presentation and clarity of the information, and its relevance to consumers’ own information needs, which are largely for information that is pertinent to their clinical needs and to their providers and information about errors and adverse events (Faber et al., 2009; Hibbard et al., 2005; Mosen et al., 2007; Schauffler and Mordavsky, 2001). Although consumers are not always well informed, often because available information is inaccessible to them, improving the clarity and completeness of public information about the performance of the clinical care system with respect to issues of appropriateness of care (underuse, overuse, and misuse), its quality, and its cost—with concerted efforts at public education—can inform consumer decision-making and enhance understanding of the strengths and limitations of clinical care. Most current indicators in the quality-improvement literature are “positive” indicators (for example, for interventions that are underused rather than overused or misused). That is understandable inasmuch as stakeholders can reach consensus on what needs to be done more easily than on what is currently done that should not be done.
Recommendation 5
The committee recommends that state and local public health agencies in each state collaborate with clinical care delivery systems to assure that the public has greater awareness of the appropriateness, quality, safety, and efficiency of clinical care services delivered in their state and community. Local performance reports about overuse, underuse, and misuse should be made available for selected interventions (including preventive and diagnostic tests, procedures, and treatment).
Such collaboration is needed to support continuous quality improvement among clinical care providers and alert the community to the effectiveness of the medical-care delivery system. Also, the collaborative convening of public health agencies and clinical care entities would likely include activities such as the joint development of evidence-based indicators and the development of a process to use data for system improvements, and will require a strong assurance of the privacy and confidentiality of clinical data to facilitate openness and collaboration. In settings where the public health agency is the quality assurer or regulator, establishing collaborative
relationships with the clinical care delivery system may be more challenging or complex.
Systems-Based Modeling and Simulation
There is still much to be understood about causal pathways in health and about which indicators are most useful for fostering understanding of health and for informing and mobilizing action to improve it. Systems-based modeling and simulation, although characterized by some limitations, are important tools that can advance this work.
Models are simplified representations of real-world systems—including biologic, environmental, behavioral, and organizational factors—that help us to understand these systems and answer questions about them. Models not only provide a way to understand what happened in the past but also provide an ability to explore what might happen under conditions that have not occurred, such as how a hypothetical system might behave, or to assess the benefits and harms of policy options. Models advance measurement in several ways. First, the process of building a model highlights in an explicit and systematic manner the relationships of model components and the data needed to implement the model. That can ensure that the major components are included in the model and can identify data elements that are needed. When those data are unavailable, the process points to the need to collect additional data elements or forces a model to be reconceptualized. Second, after a simulation model is run, a variety of what-if scenarios, formal sensitivity analysis9 (Fu, 2006), and factor-screening10 (Shen and Wan, 2009) can be used to identify the most critical factors that affect the model outputs and hence the most important data needed to focus on these factors. Modeling and simulation have long been used in many fields to maximize performance, productivity, and effectiveness, allowing system designers, planners, and managers to test a broad array of what-if scenarios and situations—for example, in flight simulators, weather forecasting, manufacturing and services systems, and computer-aided design (Law, 2007; Mass et al., 2002).
Statistical and simulation models are increasingly used in clinical care and in the study of population health. Statistical models relate such input variables as age, exercise level, and caloric intake to such output variables as glycated hemoglobin, body mass index (BMI), and adverse events (NavarroBarrientos et al., 2010). Public health agencies and investigators have used
modeling for numerous objectives, including prediction of the spread and control of infectious diseases and examination of the relationship of such behaviors and health outcomes as alcohol use and motor-vehicle injuries and such environmental exposures as air pollution and associated morbidity in people who have pulmonary diseases (Epstein, 2009; Kim and Neff, 2010; Peng et al., 2008; Pope et al., 2009). Modeling may serve as a tool for examining what-if scenarios when empirical outcome data are lacking or not generalizable. For example, if evidence of the effectiveness of an intervention in reducing obesity is lacking, the business community, health plans, or CMS may still wish to determine how much of a BMI reduction needs to be achieved by any intervention to produce a return on a hypothetical investment in 5 years under a given set of assumptions. A model could inform decision-makers that they will need the public health community to develop an intervention that might, for example, produce a 4 percent or greater reduction in BMI to offset their costs. Researchers could then be tasked with developing and testing strategies to reach that goal.
Modeling allows decision-makers to consider many aspects of the complex and interconnected causal pathways that lead to poor health outcomes, such as infant mortality or heart disease. As shown by the “problem tree”–style illustrations in Chapter 2 that highlight the difference between a largely clinical approach and a population and ecologic root-causes approach to CVD and infant mortality, intermediate outcomes (blood pressure decreases, smoking cessation, and amelioration or removal of other risk factors) and stakeholder actions that are intended to improve one outcome often have effects on multiple health outcomes. For example, increasing high school graduation rates is associated both with improvements in distal health outcomes (such as decreased infant mortality and decreased CVD) and with improvements in risk profiles (for example, decreased smoking rates and increased physical activity) that influence health-related quality of life, life expectancy, and, ultimately, HALYs. Models can consider health behaviors, social characteristics, and systems variables and suggest what can happen if variables change. As the evidence base grows, new variables and indicators can be introduced into models to continue to build understanding.
Statistical models can be useful for predictive purposes, but generally the underlying assumption of such models is that past trends and relationships can predict future behavior. That assumption may not be appropriate in trying to predict effects for a system like health, which receives inputs from an increasing array of sources and which evolves over time (Pearl, 2000). System-dynamics models have therefore been applied in health; they permit diverse variables in multiple sectors to change dynamically and to change each other. They have been used effectively in population health to optimize vaccination policies for HIV (Brandeau and Zaric, 2009) and for hepatitis B viruses (Hutton et al., 2007), to understand the effects of differ-
|
BOX 3-2 Health Impact Assessments (HIAs) A current IOM committee, the Committee on Health Impact Assessment, is developing a report that will explain the rationale of HIAs, enumerate their core elements and activities in the HIA process, describe the current practice, and provide guidance and provoke further exploration on effective HIA practice (expected to be released in 2011a). An overview of HIAs and a few examples are provided below. An HIA is commonly defined as “a combination of procedures, methods, and tools by which a policy, program, or project may be judged as to its potential effects on the health of a population, and the distribution of those effects within the population” (WHO and ECHP, 1999). An HIA is implemented before a project or policy is put into action to determine its potential health effects objectively. It brings together information from sectors beyond public health (such as transportation) to help in the decision-making process. It focuses on health outcomes, such as obesity, physical inactivity, asthma, injuries, and social equity (CDC, 2010b). The major steps in conducting an HIA include (CDC, 2010b):
|
ent interventions on pandemic outbreaks (Epstein, 2009; Ford et al., 2006), to study consumer eating behavior (Hammond, 2008), for cancer-screening optimization (Subramanian et al., 2010), and even for public health planning (Homer et al., 2007). Health impact assessments (HIAs) use a variety of modeling techniques to assess the benefits and harms of policy options—for example, the effects of living-wage laws, land use, and menu labeling (UCLA HIA-CLIC, 2010) (see Box 3-2 for more information on HIAs). Examining and leveraging existing simulation models would be useful. For example, the National Collaborative on Childhood Obesity Research has partnered with CDC, the National Institutes of Health (NIH), the Robert Wood Johnson Foundation, and the US Department of Agriculture to “forecast the impact of public health policies and interventions on childhood obesity on a population-wide level and among specific subpopulations” to simulate health
|
There are many ways in which an HIA can be implemented; depending on the method and tools used, they can be completed in a few days or take several months (Cole et al., 2005). HIA is used in Canada, Europe, Australia, and New Zealand; for some it is part of the regulatory process, for others it is voluntary (CDC, 2010b; Cole and Fielding, 2007; Cole et al., 2005). Several state legislatures—including those of California, Maryland, and Massachusetts—are considering bills that would implement HIA. The following are examples of HIA use in the United States:
For more information, see CDC Healthy Places (CDC, 2010a), Dannenberg et al. (2006), Health Impact Assessment Gateway (APHO, 2007), and the WHO Health Impact Assessment (WHO, 2010).
|
outcomes and potential cost savings from alternative health-promotion interventions (NCCOR, 2010).
In Canada, government health statisticians have been using simulation modeling to project the health-status trajectories of a longitudinal sample of people to inform health priorities and policy decisions (Wolfson, 1999) (see Box 3-3 for an example of some single outcome-specific uses of modeling). Various risk-behavior states in the population are interrelated to multiple outcomes—for example, smoking and multiple types of cancers and cardiovascular diseases. In the United States, the NIH Office of Behavioral and Social Sciences Research is leading efforts to accelerate the use of systems-based modeling in health (Mabry et al., 2010). CDC has also embraced systems-based modeling to advance community-based intervention strategies. This form of analysis can identify common causes of coexisting and synergistic conditions, such as substance abuse, violence, and sexually
|
BOX 3-3 Examples of the Use of Modeling by Statistics Canada The Population Health Model (POHEM) is a microsimulation model of diseases and risk factors in which the basic unit of analysis is the individual person. The simulation creates and ages a large sample population representative of Canada, one individual at a time, until death. The life trajectory of each simulated person unfolds by exposure to different life-like events, such as smoking initiation and cessation, changes in weight, and incidence and progression of such diseases as osteoarthritis, cancer, diabetes, and heart disease. POHEM combines data from a wide array of sources, including nationally representative cross-sectional and longitudinal surveys, cancer registries, hospitalization databases, vital statistics, census, and treatment-cost data. The model inputs may be altered at the user’s request to investigate what-if scenarios. The scenarios can be useful for policy-makers by providing information beyond what is available from retrospective population studies. Earlier versions of POHEM were used to estimate lifetime costs of breast and colorectal cancer and for assessments of health technology in cancer control, such as chemotherapy options for advanced lung cancer, the use of preventive tamoxifen in Canadian women, and the impact of population-based colorectal-cancer screening. More recent generations of POHEM models have been developed for other common diseases—such as osteoarthritis, acute myocardial infarction, and diabetes—and for disease risk factors, such as obesity and physical inactivity. The risk-factor modules enable users to simulate the effects of changes in obesity or physical activity on key health outcomes.a SOURCE: Statistics Canada, 2010. |
transmitted diseases (Milstein, 2008), that contribute to disease burdens in communities.
The complex, changing nature of the conditions (e.g., social, economic, environmental) that influence health, productivity, and the volume of patients flowing into the clinical care system requires increased use of analytic approaches that elucidate interactions and interdependences among differ-
ent systems and sectors, such as those between the traditional health sector (clinical care and government public health) and transportation, employment, and education (Collins et al., 2009). The success of the United States in dramatically reducing mortality from motor-vehicle collisions is a good illustration of the effects on health of actions taken in other sectors. Despite the meteoric rises in the numbers of motor vehicles and of miles driven per person, motor-vehicle fatality rates declined precipitously throughout the second half of the 20th century. That was a result of system-wide and mutually reinforcing interventions ranging from vehicle-safety design to traffic management, road construction design, alcohol regulation and enforcement, seat-belt laws and enforcement, workplace substance-abuse policies, and numerous community-based programs, including designated-driver and family-oriented engagement initiatives (Bolen et al., 1997). The transformation of the Department of Veterans Affairs health care system in the 1990s provides an example of dramatic system-wide improvement occurring in a short time through use of overlapping and reinforcing change strategies, including integrating and coordinating services and creation of an accountable management structure (Kizer and Dudley, 2009). “Bending the curve” of effects of chronic diseases and injury on functioning, productivity, clinical care use, and cost will require better information to support systemic improvements. Insights from modeling are essential for improved decision-making regarding priorities for intervention, collaboration among health-system sectors, and resource allocations. However, modeling itself will require further development and research.
Recommendation 6
The committee recommends that the Department of Health and Human Services (HHS) coordinate the development and evaluation and advance the use of predictive and system-based simulation models to understand the health consequences of underlying determinants of health. HHS should also use modeling to assess intended and unintended outcomes associated with policy, funding, investment, and resource options.
CONCLUDING OBSERVATIONS
The need for better and consistent measures at all levels to inform those who work to improve the health of the nation is great. This chapter makes recommendations that, if implemented, will lead to a more coherent population health information and statistics system. Advancing the timeliness and usefulness of data by creating standards, addressing inefficiencies, aligning health objectives, and improving coordination is key to meeting that goal. Communication of data to policy-makers and the public can help to create
a system in which decisions are made based on current information about the true health needs of the country, and actions are taken to confront health issues that will have the greatest impact.
REFERENCES
Adams, R. J. 2010. Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy 3:61-72.
APHO (Association of Public Health Observatories). 2007. The HIA Gateway. http://www.hiagateway.org.uk (September 8, 2010).
Asada, Y. 2010. A summary measure of health inequalities for a pay-for-population health performance system. Preventing Chronic Disease Public Health Research, Practice and Policy 7(4). http://www.cdc.gov/pcd/issues/2010/jul/09_0250.htm (July 4, 2010).
Bolen, J. R., D. A. Sleet, and T. Chorba. 1997. Overview of efforts to prevent motor vehicle-related injury. In Prevention of motor vehicle-related injuries: A compendium of articles from the morbidity and mortality weekly report, 1985-1996. Washington, DC: HHS and CDC.
Boswell-Purdy, J., W. M. Flanagan, H. Roberge, C. Le Petit, K. J. White, and J. M. Berthelot. 2007. Population health impact of cancer in Canada, 2001. Chronic Diseases in Canada 28(1-2):42-55.
Brandeau, M., and G. Zaric. 2009. Optimal investment in HIV prevention programs: More is not always better. Health Care Management Science 12(1):27-37.
Brownson, R. C., T. K. Boehmer, and D. A. Luke. 2005. Declining rates of physical activity in the United States: What are the contributors? Annual Review of Public Health 26:421-443.
Califf, R. M., and G. S. Ginsburg. 2008. Organizational improvements to enhance modern clinical epidemiology. Journal of the American Medical Association 300(19):2300-2302.
Canadian Senate Subcommittee on Population Health. 2009. A healthy, productive Canada: A determinant of health approach. Ottawa, Canada.
Carman, K. L., M. Maurer, J. M. Yegian, P. Dardess, J. McGee, M. Evers, and K. O. Marlo. 2010. Evidence that consumers are skeptical about evidence-based health care. Health Affairs 29(7):1400-1406.
CDC (Centers for Disease Control and Prevention). 2009. The NCHS Mission. http://www.cdc.gov/nchs/about/mission.htm (November 3, 2010).
CDC. 2010a. Designing and Building Healthy Places. http://www.cdc.gov/healthyplaces/ (September 8, 2010).
CDC. 2010b. Healthy Places: Health Impact Assessment. http://www.cdc.gov/healthyplaces/hia.htm (February 17, 2010).
Chamany, S., L. D. Silver, M. T. Bassett, C. R. Driver, D. K. Berger, C. E. Neuhaus, N. Kumar, and T. R. Frieden. 2009. Tracking diabetes: New York City’s A1C registry. Milbank Quarterly 87(3):547-570.
City and County of San Francisco Department of Public Health. 2010. Program on Health, Equity and Sustainability (October 7, 2010).
Clancy, C. M., and K. Cronin. 2005. Evidence-based decision making: Global evidence, local decisions. Health Affairs 24(1):151-162.
Cole, B. L., and J. E. Fielding. 2007. Health impact assessment: A tool to help policy makers understand health beyond health care. Annual Review of Public Health 28:393-412.
Cole, B. L., R. Shimkhada, J. E. Fielding, G. Kominski, and H. Morgenstern. 2005. Methodologies for realizing the potential of health impact assessment. American Journal of Preventive Medicine 28(4):382-389.
Collins, J. L., J. P. Koplanm, and J. S. Marks. 2009. Chronic disease prevention and control: Coming of age at the Centers for Disease Control and Prevention. Preventing Chronic Disease Public Health Research, Practice and Policy 6(3). http://www.cdc.gov/pcd/issues/2009/jul/08_0171.htm (August 20, 2010).
Communities Count. 2008. Introduction. In Communities Count 2008: Social and Health Indicators Across King County. Seattle, WA: Communities Count. Pp. ii-4.
Community Health Status Indicators. 2009. Community Health Status Indicators Report. http://www.communityhealth.hhs.gov/HomePage.aspx?GeogCD=&PeerStrat=&state=&county= (January 6, 2010).
Congressional Research Service. 2010. Public Health, Workforce, Quality, and Related Provisions in the Patient Protection and Affordable Care Act (P.L. 111-148). Washington, DC: Congressional Research Services.
County Health Rankings. 2010. How Healthy Is Your County? New County Health Rankings Give First County-by-County Snapshot of Health in Each State. http://www.countyhealthrankings.org/latest-news/healthday-county-county-report-sizes-americans-health (February 17, 2010).
Dannenberg, A. L., R. Bhatia, B. L. Cole, C. Dora, J. E. Fielding, K. Kraft, D. McClymont-Peace, J. Mindell, C. Onyekere, J. A. Roberts, C. L. Ross, C. D. Rutt, A. Scott-Samuel, and H. H. Tilson. 2006. Growing the field of health impact assessment in the United States: An agenda for research and practice. American Journal of Public Health 96(2):262-270.
DeWalt, D. A., N. D. Berkman, S. Sheridan, K. N. Lohr, and M. P. Pignone. 2004. Literacy and health outcomes. Journal of General Internal Medicine 19(12):1228-1239.
Doyle, L., and I. Gough. 1991. A Theory of Human Need. Hampshire, Bassingstoke: Macmillan.
Drukker, M., S. L. Buka, C. Kaplan, K. McKenzie, and J. Van Os. 2005. Social capital and young adolescents’ perceived health in different sociocultural settings. Social Science & Medicine 61(1):185-198.
Drummond, M., D. Brixner, M. R. Gold, P. Kind, A. McGuire, and E. Nord. 2009. Toward a consensus on the QALY. Value in Health 12(Suppl 1):S31-35.
Epstein, J. M. 2009. Modeling to contain pandemics. Nature 460(7256):687-687.
Erickson, P. 1998. Evaluation of a population-based measure of quality of life: The health and activity limitation index (HALex). Quality of Life Research 7(2):101-114.
Erickson, P., E. A. Kendall, J. P. Anderson, and R. M. Kaplan. 1989. Using composite health-status measures to assess the nations health. Medical Care 27(3):S66-S76.
Evans, R. G., M. L. Barer, and T. R. Marmor, eds. 1990. Why Are Some People Healthy and Others Not? The Determinants of Health of Populations. New York: Walter de Gruyter.
Faber, M., M. Bosch, H. Wollersheim, S. Leatherman, and R. Grol. 2009. Public reporting in health care: How do consumers use quality-of-care information? A systematic review. Medical Care 47(1):1-8.
Ferrer, M., C. Villasante, J. Alonso, V. Sobradillo, R. Gabriel, G. Vilagut, J. F. Masa, J. L. Viejo, C. A. Jiménez-Ruiz, and M. Miravitlles. 2002. Interpretation of quality of life scores from the St. George’s Respiratory Questionnaire. European Respiratory Journal 19(3):405-413.
Fisher, E., D. Goodman, J. Skinner, and K. Bronner. 2009. Health Care Spending, Quality, and Outcomes: More Isn’t Always Better. Lebanon, NH: The Dartmouth Institute for Health Policy and Clinical Practice.
Ford, D., J. Kaufman, and I. Eiron. 2006. An extensible spatial and temporal epidemiological modeling system. International Journal of Health Geographics 5(1):4.
Franks, P., P. Muennig, E. Lubetkin, and H. Jia. 2006. The burden of disease associated with being African-American in the United States and the contribution of socio-economic status. Social Science & Medicine 62(10):2469-2478.
Friedman, D. J., and R. G. Parrish. 2010. The population health record: Concepts, definition, design, and implementation. Journal of the American Medical Informatics Association 17:359-366.
Fryback, D. 2010. Summary Measures of Population Health: An Overview. Presentation to the IOM Committee on Public Health Strategies to Improve Health. Washington, DC: IOM.
Fryback, D. G., N. C. Dunham, M. Palta, J. Hanmer, J. Buechner, D. Cherepanov, S. A. Herrington, R. D. Hays, R. M. Kaplan, T. G. Ganiats, D. Feeny, and P. Kind. 2007. U.S. Norms for six generic health-related quality-of-life indexes from the national health measurement study. Medical Care 45(12):1162-1170.
Fu, M. C. 2006. Gradient Estimation. In Handbooks in Operations Research and Management Science. Vol. 13, edited by G. H. Shane and L. N. Barry. Boston, MA: Elsevier. Pp. 575-616.
Garber, A. M., and H. C. Sox. 2010. The role of costs in comparative effectiveness research. Health Affairs 29(10):1805-1811.
Glanz, K. 2009. Measuring food environments: A historical perspective. American Journal of Preventive Medicine 36(4):S93-S98.
Gold, M. R., and P. Muennig. 2002. Measure-dependent variation in burden of disease estimates: Implications for policy. Medical Care 40(3):260-266.
Gold, M. R., K. I. McCoy, and J. E. Siegel, eds. 1996. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press.
Gold, M. R., D. Stevenson, and D. G. Fryback. 2002. HALYS and QALYS and DALYS, oh my: Similarities and differences in summary measures of population health. Annual Review of Public Health 23:115-134.
Hammond, R. A. 2008. A Complex Systems Approach to Understanding and Combating the Obesity Epidemic. Washington, DC: The Brookings Institution.
Hannon, G. J., and D. Beach. 1994. P15INK4B is a potential effector of TGF-Beta-Induced cell cycle arrest. Nature 371(6494):257-261.
Harris, J. 1987. Qalyfying the value of life. Journal of Medical Ethics 13(3):117-123.
HHS (Department of Health and Human Services). 2002. Developing a 21st Century Vision for Health Statistics. http://www.ncvhs.hhs.gov/21stcent.htm (November 3, 2010).
HHS. 2009a. Healthy People 2020: Objective Selection Criteria. http://www.healthypeople. gov/hp2020/objectives/selectionCriteria.aspx (April 28, 2010).
HHS. 2009b. Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020: Data & IT, Implementation, Evidence-Based Actions, Process for Choosing National Priorities. http://www.healthypeople.gov/HP2020/Advisory/FACA14Minutes.htm (November 11, 2010).
HHS. 2010. HHS Gateway to Data and Statistics. http://www.hhs-stat.net/ (November 15, 2010).
HHS, CDC, and NCHS (National Center for Health Statistics). 2001. Healthy People 2000: Final Review. Hyattsville, MD: Public Health Services.
HHS, CDC, and NCVHS (National Committee on Vital and Health Statistics). 2002. Shaping a Health Statistics Vision for the 21st Century. Washington, DC: HHS.
Hibbard, J. H., J. Stockard, E. R. Mahoney, and M. Tusler. 2004. Development of the patient activation measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research 39(4p1):1005-1026.
Hibbard, J. H., J. Stockard, and M. Tusler. 2005. Hospital performance reports: Impact on quality, market share, and reputation. Health Affairs 24(4):1150-1160.
Hinman, A. R., and D. A. Ross. 2010. Immunization registries can be building blocks for national health information systems. Health Affairs 29(4):676-682.
Homer, J., G. Hirsch, and B. Milstein. 2007. Chronic illness in a complex health economy: The perils and promises of downstream and upstream reforms. System Dynamics Review 23(2-3):313-343.
Hutton, D. W., D. Tan, S. K. So, and M. L. Brandeau. 2007. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander adults for Hepatitis B. Annals of Internal Medicine 147(7):460-469.
IOM (Institute of Medicine). 1998. Summarizing Population Health: Directions for the Development and Application of Population Metrics. Washington, DC: National Academy Press.
IOM. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2003. Assuring America’s Health. In The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press.
IOM. 2004. Health Literacy: Prescription to End Confusion. Washington, DC: The National Academies Press.
IOM. 2006. Performance Measurement: Accelerating Improvement. Washington, DC: The National Academies Press.
IOM. 2009. State of the USA Health Indicators: Letter Report. Washington, DC: The National Academies Press.
IOM. 2010a. Transcript, Second Meeting of the IOM Committee on Public Health Strategies to Improve Health. Washington, DC: IOM.
IOM. 2010b. Transcript, Third Meeting of the IOM Committee on Public Health Strategies to Improve Health. Washington, DC: IOM.
Jakubowski, B., and H. Frumkin. 2010. Environmental metrics for community health improvement. Preventing Chronic Disease Public Health Research, Practice and Policy 7(4). http://www.cdc.gov/pcd/issues/2010/jul/09_0242.htm (July 4, 2010).
Jia, H., and E. I. Lubetkin. 2010. Trends in Quality-Adjusted Life-Years Lost Contributed by Smoking and Obesity. American Journal of Preventive Medicine 38(2):138-144.
Kaplan, R. M. 1994. Value judgment in the Oregon Medicaid experiment. Medical Care 32(10):975-988.
Kim, Y.-M., and J. A. Neff. 2010. Direct and indirect effects of parental influence upon adolescent alcohol use: A structural equation modeling analysis. Journal of Child & Adolescent Substance Abuse 19(3):244-260.
Kizer, K. W., and R. A. Dudley. 2009. Extreme makeover: Transformation of the veterans health care system. Annual Review of Public Health 30:313-339.
The Kohala Center. 2008. Current Events: Hawai’i County Agricultural Development Plan Health Impact Assessment. http://www.kohalacenter.org/agplan.html (October 7, 2010).
Koivusalo, M. 2010. The state of Health-in-all-Policies (HiAP) in the European Union: Potential and pitfalls. Journal of Epidemiology and Community Health 64:500-503.
Kominski, G. F., P. A. Simon, A. Ho, J. Luck, Y. W. Lim, and J. E. Fielding. 2002. Assessing the burden of disease and injury in Los Angeles County using Disability-Adjusted Life Years. Public Health Reports 117(2):185-191.
Kominski, G. F., P. A. Simon, A. Y. Ho, and J. E. Fielding. 2010. Financial burdens and disability-adjusted life years in Los Angeles County. In Handbook of Disease Burdens and Quality of Life Measures, edited by V. R. Preedy and R. R. Watson. New York: Springer. Pp. 473-482.
Lantz, P. M., and A. Pritchard. 2010. Socioeconomic indicators that matter for population health. Preventing Chronic Disease Public Health Research, Practice and Policy 7(4). http://www.cdc.gov/pcd/issues/2010/jul/09_0246.htm (July 4, 2010).
Law, A. M. 2007. Simulation Modeling and Analysis. 4th Edition. Boston, MA: McGraw-Hill.
Lowdell, C., M. Bardsley, and D. Morgan. 1999. Acheson Report: The Inquiry into Inequalities in Health, Implications for London. London, England: Health of Londoners Project.
Lubetkin, E., H. Jia, P. Franks, and M. Gold. 2005. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Quality of Life Research 14(10):2187-2196.
Luck, J., C. Chang, E. R. Brown, and J. Lumpkin. 2006. Using local health information to promote public health. Health Affairs 25(4):979-991.
Lytle, L. 2009. Measuring the food environment: State of the science. American Journal of Preventive Medicine 36(4): S134 -S144.
Mabry, P. L., S. E. Marcus, P. I. Clark, S. J. Leischow, and D. Mendez. 2010. Systems science: A revolution in public health policy research. American Journal of Public Health 100(7):1161-1163.
Madans, J. H. 2008. The Definition and Measurements of Disability: The Work of the Washington Group. Presentation to the Washington Group on Disability Statistics. Washington, DC.
Madans, J. H. 2009. Development of Internationally Comparable Disability Measures: The Washington Group on Disability Statistics. Presentation to the Washington Group on Disability Statistics. Washington, DC.
Mancuso, C. A., and M. Rincon. 2006. Impact of health literacy on longitudinal asthma outcomes. Journal of General Internal Medicine 21(8):813-817.
Mangione, C. M., P. P. Lee, P. R. Gutierrez, K. Spritzer, S. Berry, R. D. Hays, and the National Eye Institute Visual Function Questionnaire Field Test Investigators. 2001. Development of the 25-item National Eye Institute visual function questionnaire. Archives of Ophthalmology 119(7):1050-1058.
Manuel, D. G., and S. E. Schultz. 2004. Using linked data to calculate summary measures of population health: Health-adjusted life expectancy of people with diabetes mellitus. Population Health Metrics 2(1):4.
The Marmot Review. 2010. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010. London, England: The Marmot Review.
Mass, C. F., D. Ovens, K. Westrick, and B. A. Colle. 2002. Does increasing horizontal resolution produce more skillful forecasts? Bulletin of the American Meteorological Society 83(3):407-430.
Mayberry, D., and N. Hunkins. 2008. Health Information Technology (HIT) Report: 2008. MN: Minnesota Community Measures.
McIntosh, C. N., P. Finès, R. Wilkins, and M. C. Wolfson. 2009. Income disparities in health adjusted life expectancy for Canadian adults, 1991 to 2001. Statistics Canada 20(4):1-11.
Meenan, R. F., P. M. Gertman, J. H. Mason, and R. Dunaif. 1982. The Arthritis Impact Measurement Scales: Further investigations of a health status measure. Arthritis and Rheumatism 25(9):1048-1053.
Mikkonen, J., and D. Raphael. 2010. Social Determinants of Health: The Canadian Facts. Toronto, Canada: York University School of Health Policy and Management.
Milstein, B. 2008. Hygeia’s constellation: Navigating health futures in a dynamic and democratic world. Atlanta, CA: CDC, Syndemics Prevention Network.
Mitchell, R. J., R. J. McClure, J. Olivier, and W. L. Watson. 2009. Rational allocation of australia’s research dollars: Does the distribution of NHMRC funding by national health priority area reflect actual disease burden? Medical Journal of Australia 191(11-12):648-652.
Mosen, D., J. Hibbard, and C. Remmers. 2007. Is patient activation associated with outcomes of care for adults with chronic conditions. Journal of Ambulatory Care Management 30(1):21-29.
Muennig, P., P. Franks, H. Jiac, E. Lubetkind, and M. R. Gold. 2005. The income-associated burden of disease in the United States. Social Science and Medicine 61:2018-2026.
Muennig, P., K. Fiscella, D. Tancredi, and P. Franks. 2010. The relative health burden of selected social and behavioral risk factors in the United States: Implications for policy. American Journal of Public Health 100(9):1758-1764.
Murray, C. J., and A. D. Lopez. 2000. Progress and directions in refining the global burden of disease approach: A response to Williams. Health Economics 9(1):69-82.
Murray, C. J., J. A. Salomon, and C. Mathers. 2000. A critical examination of summary measures of population health. Bulletin of the World Health Organization 78(8):981-994.
Murray, C. J. L., J. A. Salomon, C. D. Mathers, and A. D. Lopez, eds. 2002. Summary measures of population health: Concepts, ethics, measurement and application. Geneva, Switzerland: World Health Organization.
National Complete Streets Coalition. 2010. Complete Streets: FAQ. http://www.completestreets.org/complete-streets-fundamentals/complete-streets-faq (November 19, 2010).
National Prevention Health Promotion and Public Health Council. 2010. 2010 Annual Status Report. Washington, DC: HHS.
Navarro-Barrientos, J., D. Rivera, and L. Collins. 2010. A dynamical systems model for understanding behavioral interventions for weight loss. Advances in Social Computing 6007:170-179.
NCCOR (National Collaborative on Childhood Obesity Research). 2010. Envision Project: Using Systems Models to Assess Public Health Policies and Interventions for Childhood Obesity Prevention and Control. http://www.nccor.org/projects_envision.html (September 8, 2010).
NCHS (National Center for Health Statistics). 2008. Final Report of the National Health Interview Survey Review Panel to the NCHS Board of Scientific Counselors: Executive Summary. Atlanta, GA: CDC.
NCHS. 2009. Report of the NHANES Review Panel to the NCHS Board of Scientific Counselors. Atlanta, GA: CDC.
NCVHS (National Committee on Vital and Health Statistics). 2008. Charge of the Subcommittee on Population Health. http://www.ncvhs.hhs.gov/popschrg.htm (June 17, 2010).
NCVHS. 2010. Toward Enhanced Information Capacities for Health: An NCVHS Concept Paper. Washington, DC: HHS.
Neumann, P. J., and D. Greenberg. 2009. Is the United States ready for QALYs? Health Affairs 28(5):1366-1371.
Neumann, P. J., and M. C. Weinstein. 2010. Legislating against use of cost-effectivness information. New England Journal of Medicine 363(16):1495-1497.
New York City Department of Health and Mental Hygiene. 2009. Primary Care Information Project. http://www.nyc.gov/html/doh/html/pcip/pcip.shtml (November 19, 2010).
NORC (National Opinion Research Center). 2005. Assessment of the Uses and Users of Healthier US and Healthy People 2010. Washington, DC: NORC.
NRC (National Research Council). 2009. Principles and Practices for a Federal Statistical Agency. 4th Edition. Washington, DC: The National Academies Press.
Orszag, P. 2008. The Overuse, Underuse, and Misuse of Health Care: Testimony Before the Committee on Finance, United States Senate. Washington, DC: Congressional Budget Office.
Paasche-Orlow, M. K., and M. S. Wolf. 2007. The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior 31(Supplement):S19-26.
Pearcy, J. N., and K. G. Keppel. 2002. A summary measure of health disparity. Public Health Report 117(3):273-280.
Pearl, J. 2000. Causality: Models, Reasoning, and Inference. Cambridge, United Kingdom: Cambridge University Press.
Pearson, S. D., and M. D. Rawlins. 2005. Quality, innovation, and value for money: NICE and the British National Health Service. Journal of the American Medical Association 294(20):2618-2622.
Peng, R. D., H. H. Chang, M. L. Bell, A. McDermott, S. L. Zeger, J. M. Samet, and F. Dominici. 2008. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. Journal of the American Medical Association 299(18):2172-2179.
Pope, C. A., III, M. Ezzati, and D. W. Dockery. 2009. Fine-particulate air pollution and life expectancy in the United States. New England Journal of Medicine 360(4):376-386.
Prentice, J. C. 2006. Neighborhood effects on primary care access in Los Angeles. Social Science and Medicine 62(5):1291-1303.
Rawles, J. 1989. Castigating QALYs. Journal of Medical Ethics 15(3):143-147.
Russell, L. B., M. R. Gold, J. E. Siegel, N. Daniels, and M. C. Weinstein. 1996. The role of cost-effectiveness analysis in health and medicine: Panel on cost-effectiveness in health and medicine. Journal of the American Medical Association 276(14):1172-1177.
Safran, C., M. Bloomrosen, W. Hammond, S. Labkoff, S. Markel-Fox, P. C. Tang, and D. E. Detmer. 2007. Toward a national framework for the secondary use of health data: An American Medical Informatics Association white paper. Journal of the American Medical Informatics Association 14(1):1-9.
Saskatoon Regional Health Authority. 2007. 2006-2007 Annual Report to the Minister of Health and the Minister of Healthy Living Services. Saskatoon, Canada: Saskatoon Regional Health Authority.
Schauffler, H. H., and J. K. Mordavsky. 2001. Consumer reports in health care: Do they make a difference? Annual Review of Public Health 22:69-89.
Shen, H., and H. Wan. 2009. Controlled sequential factorial design for simulation factor screening. European Journal of Operational Research 198(2):511-519.
Statistics Canada. 2010. Health Models. http://statcan.gc.ca/microsimulation/health-sante/health-sante-eng.htm (August 26, 2010).
Stiefel, M. C., R. J. Perla, and B. L. Zell. 2010. A healthy bottom line: Healthy life expectancy as an outcome measure for health improvement efforts. Milbank Quarterly 88(1):30-53.
Stiglitz, J. E., A. Sen, and J. P. Fitoussi. 2009. Report by the Commission on the Measurement of Economic Performance and Social Progress. French Republic: President of the French Republic.
Subramanian, S., G. Bobashev, and R. J. Morris. 2010. When budgets are tight, there are better options than colonoscopies for colorectal cancer screening. Health Affairs 29(9): 1734-1740.
Taskforce on Health Status. 2005 (November 14-16). Criteria for and Selection of Domains for the Measurement of Health Status. Presentation given at the Conference of European Statisticians, Budapest, Hungary.
UCLA HIA-CLIC (Health Impact Assessment-Clearinghouse Learning and Information Center). 2010. Completed HIAs. http://www.hiaguide.org/hias?page=1 (August 26, 2010).
The United Nations. 2010 (January). Brief Historical Overview of the Budapest Initiative and Testing Activities. Geneva, Switzerland: United Nations Conference.
USDA (United States Department of Agriculture). 2010. About the Food Environment Atlas. http://ers.usda.gov/FoodAtlas/about.htm (September 8, 2010).
White House Task Force on Childhood Obesity. 2010. Solving the Problem of Childhood Obesity Within a Generation. Washington, DC: Executive Office of the President of the United States.
WHO (World Health Organization). 2010. Health Impact Assessment. http://www.who.int/hia/en/ (September 8, 2010).
WHO and ECHP (European Center for Health Policy). 1999. Health Impact Assessment: Main Concepts and Suggested Approach. Brussels, Belgium: WHO.
WHO, UNECE (United Nations Economic Commission for Europe), and Eurostat. 2007. Rationale for the Budapest Initiative-Mark 1 Questionnaire. Geneva, Switzerland: United Nations Economic Commission for Europe.
Wolfson, M. C. 1999. Measuring health-visions and practicality. Statistical Journal of the United Nations Economic Commission for Europe 16:1-17.
Wolfson, M., and G. Rowe. 2009. Healthpaths Dynamics 2—Using Functional Health Trajectories to Quantify the Sources of Health Inequalities. Paper presented at International Microsimulation Association 2009, Ottawa, Ontario.
Zhu, X., and C. Lee. 2008. Walkability and safety around elementary schools: Economic and ethnic disparities. American Journal of Preventive Medicine 34(4):282-290.












































