II
Disease Threats
Our “war” on infectious microbes has restricted the spread of several pathogens and drastically reduced the burden of human disease, but we are a long way from conquering infectious diseases.
During the past three decades, 37 new human pathogens have been identified as disease threats. An estimated 12 percent of known human pathogens have been recognized as either emerging or re-emerging. Having fallen steadily since the turn of the 20th century, the number of deaths attributable to infection in the United States began to increase in the early 1980s due, in large part, to the HIV/AIDS pandemic and increases in deaths attributable to pneumonia and bloodstream infections. Infectious disease continues to cause high morbidity and mortality throughout the world, particularly in developing countries.
It accounts for about a quarter of deaths worldwide, and in 2008 caused more than two-thirds of the estimated 8.8 million deaths in children under the age of five. What are some of the most significant microbial threats we face?
Animal Carriers
Many of the diseases that afflict people today are caused by microbes whose ancestors came from animals first domesticated by early humans. Biologists believe that the measles virus stemmed from canine distemper and rinderpest, an affliction of cattle; that rhinoviruses, agents of the common cold, came to us from horses; and that smallpox is a close cousin of cowpox.
Infections transmitted from animals to humans are called zoonoses, or zoonotic diseases. Of the more than 1,700 known viruses, bacteria, and other pathogens that infect people, more than half either originated in or now come directly from animals;

Animals domesticated by early humans are believed to have been the source of microbes that eventually caused disease in people, as in the case of measles stemming from canine distemper and rinderpest.
the rest come from the environment around us, such as soil, water, and air. And of the 37 new infectious diseases identified in the past 30 years, more than two-thirds sprang from animals. The next deadly pandemic to sweep the world could very likely jump species in this way.
Direct Transmission
Some zoonotic infections move directly from animals to humans. In such cases, an animal is the natural host—or reservoir—for the pathogen, and through an evolutionary twist of fate, the pathogen moves from the natural host to humans. Severe Acute Respiratory Syndrome (SARS) is a recent example of this. In the spring of 2003 this new and deadly viral illness swept out from China’s Guangdong Province and spread rapidly around the world before it was contained that summer. SARS originated in Chinese horseshoe bats, animals that are used for food and medicine in many parts of Asia, and was then “amplified” through the infection of civet cats, a step leading to a mutation that makes the disease transmissible to humans. The virus infected 8,098 people, of which 774 died—a nearly 10 percent mortality rate. Fortunately, no human infections have been found since early 2004.
There are many other examples of direct transmission. Toxoplasmosis, a parasitic disease that typically causes mild flu-like symptoms in humans (but potentially more serious illness in individuals with compromised immune systems), infects many warmblooded animals. Cats play an important role in spreading the disease when they become infected by eating infected rodents or small birds and then pass the parasite to humans through their feces. Leptospirosis, a bacterial disease spread through the urine of infected animals, or through soil or water contaminated by infected urine, can cause a wide range of symptoms in humans, including high fever, vomiting, and even meningitis and liver failure. The Nipah virus, which can cause fatal encephalitis (inflammation of the brain), emerged in 1998 in Malaysia. Harbored in fruit bats, the virus afflicted slaughterhouse workers who had caught it from pigs.

Fruit bat, which can transmit the Nipah virus.
Indirect Transmission
Diseases that are transmitted to humans indirectly via an insect, an arthropod (animals with jointed appendages and exoskeletons, such as ticks), or another animal (such as snails, which deliver the parasite responsible for schistosomiasis) are called vector-borne diseases. Vectors carry disease-causing viruses, bacteria, or parasites from one host to another, delivering these pathogens to humans and other warmblooded hosts. The vectors themselves typically suffer no ill effects from the organisms they carry.

American dog tick, potential vector of Rocky Mountain spotted fever.
In 1999, for example, a mosquito-borne infection—West Nile virus—suddenly began targeting New Yorkers. Seven people died and 62 were hospitalized. Until then the virus had been confined to Africa, West Asia, and the Middle East. Today, the infection caused by West Nile virus has fully established itself in North America, flaring up in the summer and continuing into the fall. Since 1999 the virus has spread rapidly across North America and into Latin America. In 2009 there were 720 reported cases of West Nile virus in the United States, of which 32 were fatal.
Wild or domestic animals are natural reservoirs for many vector-borne diseases. The main reservoir host for West Nile virus is wild birds. The New York City strain of the virus was virtually identical to a strain taken the previous year from a dead goose in Israel. Scientists speculate that an infected mosquito, human, or bird may have brought the pathogen to this country on a plane or ship.

A vector ecologist tests crows for the West Nile virus in a lab in St. Paul, Minnesota. Dead crows were one of the early signs of the virus’s presence in North America.
Many other common infections, including malaria, yellow fever, Lyme disease, and typhus, are spread to humans from animals via the bites of insects and other arthropods. In fact, nearly half the world’s population is currently infected with a vector-borne disease.
Foodborne Pathogens
Each year an estimated 76 million Americans—about one in four—become infected by what they eat. Approximately 325,000 are hospitalized. More than 5,000 (14 a day) die. In April 2009 the U.S. Centers for Disease Control and Prevention (CDC) reported that progress in reducing foodborne infections had stalled, pointing to gaps in the existing food safety system and the need to develop improved food safety practices as products move from the farm to the table. The true magnitude of foodborne illness is likely to be much higher than even the official estimates because most people do not seek medical attention for its symptoms, such as abdominal cramps, vomiting, and diarrhea.
The Pathogens Behind Foodborne Illness
Foodborne disease occurs when a susceptible host consumes contaminated foods or beverages. Many different disease-causing microorganisms—bacteria, viruses, and parasites—can taint foods and liquids, each potentially associated with a different illness. The most common causes of foodborne illness
include the bacterial infections Campylobacter, the most frequently identified bacterial cause of diarrheal illness in the world; Salmonella, which spreads to humans through a variety of foods of animal origin, or through fecal contamination of plant-based foods, such as in the 2009 peanut-product outbreak; and E. coli O157:H7, the agent behind a serious and sometimes deadly complication called hemolytic-uremic syndrome (HUS). The most common viral cause of foodborne

Salad bars may harbor agents of foodborne illness, such as Salmonella bacteria (below), if the food has not been handled properly.

Outbreaks of norovirus (Calicivirus), the most common form of viral foodborne illness, spread easily in places where large numbers of people are gathered together, such as cruise ships.
Mangoes are sliced in preparation for exportation from South America. Global food distribution increases the risk of widespread epidemics if food becomes contaminated.

illness is Calicivirus, also referred to as Norwalk-like virus or norovirus. Unlike the previous three bacterial foodborne pathogens, noroviruses easily spread from one infected person to another and can contaminate an environment, making them extremely difficult to eradicate from hotels, hospitals, nursing homes, cruise ships, and similar establishments where large numbers of people congregate.
After you swallow a foodborne pathogen there may be a delay—the incubation period—before symptoms appear. This delay may range from hours to days. During the incubation period, the microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine; some, like cholera, produce a toxin that causes the body to secrete water, resulting in diarrhea. Others, like the typhoid bacillus, invade and replicate in the deeper body tissues.
Not all foodborne pathogens require an incubation period, however. Illness can result from toxins that form in the food before it is eaten—leading to true “food poisoning.” In such cases, bacteria do not need to replicate in the body at all and the onset of symptoms can be more rapid.
What Causes Outbreaks?
In the past few decades, food production and distribution for the developed world have increasingly involved vast and intricate global networks. This sprawling system produces food that, if contaminated, increases the potential for widespread epidemics. In this giant food economy
opportunities abound for food to come in contact with pathogens. Meat and poultry carcasses can become contaminated during slaughter by contact with small amounts of intestinal contents. Fresh fruits and vegetables become tainted if they are washed or irrigated with water contaminated with animal manure or human sewage. (Outbreaks related to fresh produce have increased eightfold in the United States during the past several decades.) And increasingly, we don’t cook our own meals, leaving food safety in the hands, literally, of others.
Raw foods of animal origin are the most likely to be contaminated—that is, raw meat and poultry, raw eggs, unpasteurized milk, and raw shellfish. Foods for which such products are pooled from many sources and batch processed are also hazardous, because a pathogen present in any one of the animals might contaminate the whole batch.
How to Protect Yourself
Consumers can reduce the risk of foodborne illness by adhering to the following safe food handling and preparation practices:
Wash hands thoroughly with soap and warm water before handling food.
Cook meat, poultry, and eggs thoroughly. Use a thermometer to measure the internal temperature of meat, to be sure that it is cooked sufficiently to kill bacteria. Ground beef, for example, should be cooked to an internal temperature of 160°F. Eggs should be cooked until the yolk is firm.
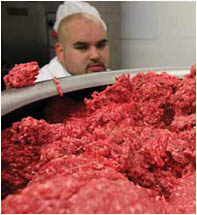
Foods pooled from many sources, such as batches of raw ground beef, can become tainted if any of the meat in the batch is contaminated with a human pathogen.
Separate: Avoid cross-contaminating foods by washing hands, utensils, and cutting boards after contact with raw meat or poultry and before they touch another food. Unless it is disinfected between each use, don’t use a “universal” cleanup tool such as a sponge. Place cooked meat on a clean platter, rather than back on the one that held the raw meat.
Chill: Bacteria can grow quickly at room temperature, so refrigerate leftover foods if they are not going to be eaten within 4 hours. A large volume of food will cool more quickly if divided into several shallow containers for refrigeration.
Clean: Rinse fresh fruits and vegetables in running tap water to remove visible dirt and grime. Remove and discard the outermost leaves from a head of lettuce or cabbage. Because bacteria can grow on the cut surface of fruits or vegetables, be careful not to contaminate these foods while slicing them on a cutting board, and avoid leaving cut produce at room temperature for many hours.
Report suspected foodborne illness to your local health department.
Global Killers
A handful of deadly infectious diseases claim millions of lives worldwide each year: lower respiratory tract infections, diarrheal diseases, HIV/AIDS, tuberculosis, and malaria. Together, they account for nearly one-fifth of deaths globally. Several of these diseases have plagued humankind throughout history, often decimating populations with greater efficiency than wars. In an age of vaccines, antibiotics, and dramatic scientific progress, these diseases should have been brought under control. Yet they continue to kill at an alarming rate, particularly in the developing world. In low-income countries the dominant causes of death are infectious and parasitic diseases (including malaria) and poor medical care surrounding childbirth. By contrast, in high-income countries the leading causes of death are noncommunicable diseases, such as heart disease and cancer. Infectious and parasitic causes of mortality are farther down on the list.
Lower respiratory tract infections (including pneumonia) account for more than 4 million deaths worldwide—the greatest global killer among infectious diseases. Pneumonia is also the leading cause of death of the very young, often striking children with low birth weight or those whose immune systems are weakened by malnutrition or other diseases. Most of these deaths occur in developing countries.
Diarrheal diseases are the second-leading cause of infectious disease deaths worldwide, accounting for more than 2 million deaths each year, and nearly one-fifth of all deaths of children under the age of five. These infections are so widespread in developing countries that parents often fail to recognize when symptoms become critical. Children die simply because their bodies are weakened—often through rapid loss of fluids and undernourishment. The burden of diarrheal diseases is highest in deprived areas where there is poor sanitation, inadequate hygiene, and unsafe drinking water.
HIV stands for human immunodeficiency virus, the virus that causes acquired immunodeficiency syndrome (AIDS), the final stage of HIV infection. HIV appears to have jumped to humans early in the 20th century from a type of chimpanzee in West Africa—most likely when humans hunted these animals for meat and came into contact with their infected blood. The virus slowly spread across Africa and later to other parts of the world.
In 2008 more than 33 million people worldwide were infected with HIV and an estimated 2 million died. Unlike most other viruses, HIV attacks the
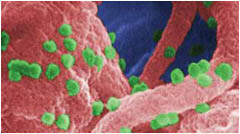
HIV particles (green spheres).
immune system, destroying a type of white blood cell (T cells or CD4 cells) that the immune system needs to fight disease. HIV is transmitted by having sex with someone infected with HIV, by sharing needles and syringes with an infected person, through blood or blood product transfusions, or by being exposed as a fetus or an infant to the virus before or during birth or through breastfeeding. HIV is not transmitted through casual contact, such as shaking hands, hugging, modest kissing, or drinking from the same glass.
Someone in the world is newly infected with the tuberculosis (TB) bacterium every second. In 2008 there were an estimated 9.4 million new cases of tuberculosis and 1.8 million deaths. The vast majority of TB deaths are in the developing world, and more than half of all deaths occur in Asia. In the United States, 12,904 TB cases were reported in 2008, a nearly 3 percent decline from the number reported in 2007.
TB, which is caused by the bacterium Mycobacterium tuberculosis, is a contagious disease that spreads through the air when an infected person coughs or sneezes and people nearby breathe in the bacteria. TB bacteria can live in the body without making an individual sick, a condition known as latent TB infection. More than 2 billion people—about one-third of the world’s population—are infected, many asymptomatically, with TB bacilli. A person with active TB can be treated by taking several drugs for 6 to 12 months.
Multidrug-resistant TB (MDR-TB) is a new threat. It is difficult and expensive to treat and fails to respond to the standard first-line drugs that are most easily tolerated and have historically worked best against the disease. Extensively drug-resistant TB (XDR-TB) occurs when resistance to second-line drugs, which are typically more toxic and less effective, develops on top of MDR-TB. Such infections are highly lethal.
On the global stage, HIV/AIDS and TB are tragically interconnected. Among HIV-infected people whose immune systems are weakened by the effects of the virus, the risk of developing TB is much higher than for persons with normal immune systems. Indeed, TB is the leading cause of death worldwide among people infected with HIV. Likewise, among people with latent (inactive) TB infection, HIV infection is the strongest known risk factor for progressing to active TB disease.
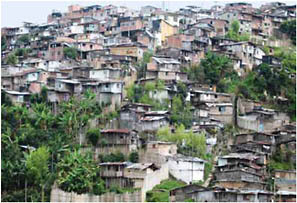
Crowded housing with poor sanitation may enable the rapid spread of disease within a community.
Like the other global killers, malaria occurs mostly in poor, tropical, and subtropical areas of the world. Each year as many as 300 million people are infected with malaria worldwide, and up to 1 million die, most of them young children in sub-Saharan Africa. Malaria is a mosquito-borne disease caused by several different protozoan parasites. Humans infected with malaria parasites, depending on the type, can develop a wide range of illnesses, from mild infection that does not produce symptoms to the classic symptoms of malaria (fever, chills, sweating, headaches, muscle pains) to severe complications (anemia, kidney failure, coma) that can lead to death.
Malaria serves as a particularly dramatic example of infectious disease re-emergence and illustrates the challenges of controlling human vector-borne diseases. Following the drastic depopulation of Anopheles mosquitoes in the first half of the 20th century due to liberal use of the pesticide DDT, malaria began its resurgence in Asia in the late 1960s. In Sri Lanka, where only 17 cases of malaria were reported in 1963, a major epidemic of more than 440,000 cases erupted 5 years later, after preventive vector control was replaced with a strategy of identifying and treating new cases of the illness. Similarly, by the mid-1970s millions of new cases had occurred in India after mosquito eradication efforts ceased. In Africa, where vector control programs were never initiated, a more recent upsurge in infections, including several explosive epidemics, has erupted in endemic areas. A number of factors appear to be driving this global resurgence, including the rapid spread of drug resistance among malarial parasites, changing rainfall patterns, and water development projects, such as dams, which create new mosquito breeding sites.

Villagers in sub-Saharan Africa learn how to set up a mosquito bednet for protection against malaria.
Yet despite today’s dire headlines, progress is being made against the world’s modern infectious scourges. The scale-up of antiretroviral therapy has reduced the number of AIDS deaths and mother-to-child transmissions, and has improved survival and productivity. Wider access to antiretroviral treatments has also been accompanied by a dramatic reduction in prices. The prevalence of TB has declined since 2000, partly because the WHO’s Directly Observed Therapy Short-Course strategy brought treatment and a cure to tens of millions of patients. And malaria deaths have fallen with the development of artemisinin-based drugs, distribution of insecticide-treated bed nets, and indoor residual spraying of insecticides. Alongside these efforts there have been major investments in health care systems—bolstering infrastructure, laboratories, and human resources.
Influenza
The “flu” has become a popular catch-all term to describe anything from a bad cold to stomach distress. But the real flu, influenza, is a defined illness that many public health officials dread most. Each year in the United States about 36,000 people die from flu-related complications, and more than 200,000 are hospitalized.
Of even greater concern is a flu pandemic—a worldwide epidemic of a new strain of influenza virus from which the human population has no immunity. Depending on its severity, an influenza pandemic could result in 200,000 to 2 million deaths in the United States alone. In 2009 the WHO declared the current H1N1 “swine flu” a pandemic, although its human mortality rate to date has been relatively modest, with about 18,000 confirmed deaths worldwide.

2009 H1N1 influenza virus.
How the Flu Spreads
Influenza viruses mainly spread when droplets from the cough or sneeze of an infected person are propelled through the air and land on the mouth or nose of someone nearby. Flu viruses may also spread when a person touches respiratory droplets on another person or on an object and then touches his or her own mouth or nose. The hardy influenza virus can survive on environmental surfaces, such as doorknobs and countertops, for 2 to 8 hours—one of the reasons that hand washing and surface hygiene is an important part of most flu control strategies.
Once the flu virus makes contact with mucous membranes in the eyes and nose, it heads to the cells along the upper respiratory tract, bronchial tubes, and trachea, where it swiftly multiplies. Scientists believe flu symptoms arise because growth of the virus damages the cells into which it has inserted itself and because the immune system, in trying to limit the damage, responds in ways that cause familiar discomfort: It sends out white blood cells, called cytokines, that cause muscle and joint pain, and it produces a fever, which is one of the body’s ways of mobilizing its defenses against invaders.
Seasonal Versus Pandemic Flu
The genius of the influenza virus lies in its ability to alter itself. The virus uses RNA rather than DNA as its genetic material. RNA viruses make frequent mistakes while copying themselves. Their high mutation rate means that RNA viruses evolve far more rapidly than DNA viruses, because every successive generation is a little different from the previous one. The flu virus’s surface proteins—hemagglutinin (H) and neuraminidase (N)—are also changeable. These proteins have a role in making it possible for a virus to invade and hijack cells. Hemagglutinin permits virus particles to gain access to the cell’s interior, and neuraminidase helps newly produced copies of the virus break free of the cell in quest of other cells to invade.
There are three types of influenza viruses: A, B, and C. Only influenza A viruses are further
classified by subtype on the basis of the H and N surface proteins. Influenza A subtypes and B viruses are further classified by strains. Among influenza A viruses, there are 16 known subtypes of hemagglutinin and 9 of neuraminidase. Many different combinations of these H and N proteins are possible, each representing a different subtype.
According to the CDC, the subtypes of influenza that are currently circulating among people worldwide include A H1N1, A H3N2, and B strains. Usually only one subtype predominates in a given flu season. Epidemics break out every year because of slight genetic mutations in a virus subtype’s surface proteins that result in a new strain of the virus—a process known as antigenic drift. New combination vaccines are formulated annually to protect against the three circulating strains of seasonal flu that experts predict will cause the most illness in the coming season.
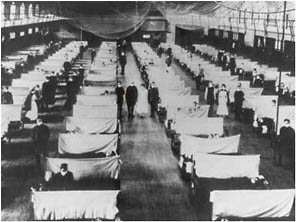
Sometimes the virus’s surface proteins undergo a radical change—a process known as antigenic shift—resulting in an altogether new influenza subtype against which most humans have no immunity. The result can be a pandemic. The extent and severity of a pandemic depend on the specific characteristics of the virus. While rare, pandemics sweep the world like wildfire. In addition to the recent H1N1 pandemic, three major pandemics broke out in the 20th century: an H1N1 in 1918 (the misnamed “Spanish” flu), an H2N2 in 1957 (the “Asian” flu), and an H3N2 in 1968 (the “Hong Kong” flu). Of these pandemics, the 1918–1919 virus was the most fearsome, killing 50 million to 100 million people worldwide (or between 0.5 and 1 percent of the global population at that time). Many of those deaths were due to the effects of pneumococcal pneumonia, a secondary complication of flu for which no antibiotics

During the 1918 flu pandemic, emergency hospitals were set up quickly for the huge influx of patients (left). A CDC microbiologist works carefully with a recreated 1918 virus to identify the characteristics that made this organism such a deadly pathogen (below).
existed in 1918. Diagnosis and treatment of this complication continue to be key to survival and recovery for flu patients.
Where Does the Flu Virus Come From?
The source of all flu strains is migrating aquatic birds, such as wild ducks, geese, and terns. Domestic birds—such as chickens, geese, and ducks—also carry a large variety of flu strains. New flu strains enter human populations in several ways. Sometimes genetic material is exchanged between human and avian flu viruses when a human or other mammal is infected with both viruses. Often this mixing and matching of viral genes happens in pigs, which are uniquely susceptible to both human and avian flu viruses. The process of swapping genes is called “reassortment.” Today’s H1N1, for example, is a triple reassortment virus containing genetic materials from avian, swine, and human viruses.

Sandpipers and other migrating aquatic birds are the source of all influenza strains.
Another process, known as adaptive mutation, is more gradual. In this case, the longer an avian flu virus infects humans, the more it is able to bind to human cells as the virus adapts to its new host. Recent investigations suggest that the 1918 flu virus was a bird virus that became a human virus by slowly accumulating genetic mutations that helped it survive in a human host.
On rare occasions, flu viruses leap directly from birds to humans. In 1997 a highly fatal H5N1 bird flu broke out in Hong Kong, infecting 18 individuals and causing 6 deaths—a potential pandemic that was averted when authorities ordered the slaughter of more than 1.5 million domestic birds. If H5N1 were to acquire the ability to spread easily from person to person, a new influenza pandemic could be possible.
Vaccines
Vaccines provide an effective means to prevent infection by the influenza virus. But as the world learned with the 2009 H1N1 “swine flu” pandemic, making vaccine is a time-consuming process that normally takes 5 to 6 months. For more than 50 years, flu vaccine has been produced by injecting the whole virus into fertilized hens’ eggs. The virus is harvested, purified, chemically treated, and then weakened (attenuated) so that it cannot trigger infections. Despite appeals from scientists, governments have been slow to invest in newer and faster methods of producing flu vaccines, such as recombinant technologies or tissue culture–based production methods that bypass the need to grow a whole virus in eggs or cells. However, recent moves by the U.S. government and vaccine manufacturers toward utilizing some of these new technologies
provide hopeful signs. Scientists are also exploring ways to make a vaccine that is effective against all flu strains—a so-called universal vaccine. Such a development could dramatically improve the public’s protection against influenza infection.
How to Protect Yourself
-
Consider getting vaccinated against influenza. Vaccines are one of the best ways to reduce the morbidity and mortality associated with the disease. They do not themselves cause influenza in any form.
-
Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
-
Wash your hands often with soap and water, especially after coughing or sneezing. Alcohol-based hand sanitizers are also effective.
Injecting eggs with the flu virus to develop vaccines.


Alcohol-based hand sanitizers are effective in preventing the transmission of many pathogens. The Food and Drug Administration recommends a concentration of at least 60 percent ethanol. In healthy households, the use of other antibacterial agents, such as triclosan (common in many soaps and detergents), may contribute to the problem of antibiotic resistance and should be used prudently.
-
Avoid touching your eyes, nose, or mouth, which can spread germs.
-
If you do get sick, stay home from work or school and limit your contact with others to keep from infecting them.
-
Ask your doctor whether you should take an anti-influenza drug, such as Tamiflu, which can be effective if taken within 48 hours of developing the symptoms of flu.
Antibiotic Resistance
Antibiotics—medicine’s “magic bullets”—save tens of thousands of lives annually in the United States. But these magic bullets are losing their power. The problem is growing antibiotic resistance—the ability of bacteria to resist the effects of an antibiotic. Antibiotic resistance occurs when bacteria undergo a genetic change that reduces or eliminates the
effectiveness of drugs or other agents designed to cure or prevent infection. Resistant bacterial infections have inevitably followed the widespread use of every new antibiotic introduced.

The more we use antibiotics, the more widespread bacterial resistance to these drugs becomes. Every time a person takes an antibiotic, sensitive bacteria are killed while resistant germs are left to grow and multiply—a classic case of natural selection. Too-frequent and improper uses of antibiotics are the main causes of today’s increase in drug-resistant bacteria.
Another source of antibiotic resistance originates with the way we raise livestock, fish, and orchard crops. Almost 70 percent of all the antibiotics produced in the United States are added to animal feeds—not to fend off disease but to boost growth. These non-therapeutic uses of antibiotics are a perfect way to cultivate resistant organisms, including Campylobacter and Salmonella, bacteria that can sicken people who eat meat and poultry products.
The Toll of Resistance
Antibiotic resistance has been called one of the world’s most pressing public health problems. Almost every type of bacteria has become less responsive to the antibiotic treatment designed to combat it. And antibiotic resistance affects everyone’s health in a way that no single disease does. It is a particularly serious problem for patients whose immune systems are compromised, such as people with HIV/AIDS and patients in critical care units. Resistant pathogens lead to higher health care costs because they often require more expensive drugs and extended hospital stays.
But healthy people are also at risk. A child with an ear infection that in the early 1990s would have been instantly cured by penicillin may now need two, three, or four courses of different drugs. A new mother may contract a drug-resistant urinary tract infection that keeps her in the hospital an extra day or more.
How Bacteria Become Drug Resistant
Bacteria are able to resist drugs through one of several mechanisms. Some develop the ability to inactivate or destroy the antibiotic before it can do harm. Others can rapidly pump the antibiotic out of bacterial cells. Still others can change the place in the cell that antibiotics target so that the drugs are ineffective. The more these resistant organisms spread, the more they add to the pool of resistance genes in all bacteria, raising the odds that these genes will jump to more and more disease-causing microbes.
The story of staph bacteria and antibiotics illustrates the perils of drug resistance. Scottish bacteriologist Alexander Fleming discovered the first antibiotic, penicillin, in 1927, an achievement for which he was co-awarded a Nobel Prize in 1945. By the early 1940s, the drug was used in patients. But

MRSA bacteria.
penicillin-resistant staph bacteria emerged as early as 1942. Today, virtually all Staphylococcus aureus are penicillin resistant.
Staph bacteria are commonly carried on the skin or in the nose of healthy people. MRSA—methicillin-resistant Staphylococcus aureus—is a type of staph that is resistant to antibiotics called beta-lactams. In the past the majority of MRSA infections occurred among patients in hospitals or other health care settings. But drug-resistant staph is also showing up in healthy people who have not been staying in a hospital. If common staph bacteria were to become resistant to all readily available antibiotics, the practice of medicine would change dramatically. Any surgery or invasive procedure could bring life-threatening complications. As was the case in the pre-antibiotic era, even the most minor cuts in the skin could prove fatal.
Though this discussion focuses on the evolving resistance of bacteria to antibiotics, the issue of antimicrobial resistance is actually much broader. The resistance of viruses such as HIV and influenza to antivirals and of protozoan parasites to antimalarial drugs is a huge problem around the globe. Microbes have the capacity to develop resistance, whether they are bacteria, viruses, or protozoa.
How to Protect Yourself
To avoid contracting an antibiotic-resistant infection:
-
Do not demand an antibiotic when a health care provider says it is not needed.
-
Do not take an antibiotic for a viral infection, such as the common cold.
-
If your health care provider prescribes an antibiotic for you, do not skip doses and do not save any for the next time you get sick. Complete the prescribed course of treatment, even if you are feeling better.
-
If you are a hospital patient or have a loved one in the hospital, make sure that you and the doctors, nurses, support staff, and all visitors wash their hands or use a hand sanitizer prior to touching the patient.
Chronic Illness and Cancer
In the United States, 70 percent of all deaths are due to chronic diseases. Until recently their biological causes were mostly unknown. Today, growing evidence suggests that infections are behind many chronic diseases once thought to be caused by genetic, environmental, or lifestyle factors.
The human papillomavirus (HPV), for instance, causes more than 90 percent of cervical cancer cases. The hepatitis B virus accounts for more than 60 percent of liver cancer cases. The hepatitis C virus causes cirrhosis, end-stage liver disease, and liver cancer. Human herpesvirus 8 causes Kaposi’s sarcoma, a malignant complication of AIDS. Helicobacter pylori, a spiral-shaped bacterium, is the agent of peptic ulcers and gastric cancer. These examples may be just the tip of the iceberg.

Helicobacter pylori.
Clues to Infection
For scientists there are tantalizing clues that a seemingly chronic disease may be infectious. When an illness arises mostly in people whose immune systems are weak, it suggests infection (such as in Kaposi’s sarcoma following organ transplants). When a disease gets better with antibiotics (as does strep-induced rheumatic fever), it’s likely to be infectious. Another sign of possible infection is chronic inflammation, which is a common denominator in such diseases as multiple sclerosis, rheumatoid arthritis, lupus, and other autoimmune diseases. It remains to be proven that any of these diseases have infectious origins, though the possibility certainly exists.
The traditional standards for establishing a microbial cause of disease were developed in the 19th century for acute infections such as tuberculosis and anthrax. When it comes to tracking down an infectious source of chronic disease, however, traditional standards may prove to be too restrictive. Sometimes the suspect bacteria or viruses are difficult to detect or grow in the lab. Or there may be long delays between infection and disease, so that by the time symptoms appear, the agents that caused the original infection may be gone. Some psychiatric illnesses, such as schizophrenia, may have been triggered by infections that occurred just before or after birth. Studies are in progress to address this possibility.
New Treatment Approaches
Proof that certain infections cause chronic diseases raises the promise of treatment with antibiotics or vaccines. The discovery that infection with H. pylori was associated with peptic ulcers is a well-known example. Doctors used to assume that stress and spicy foods caused ulcers—and recommended bland diets. Today they simply cure the condition by prescribing a pair of antibiotics.
Another advance in prevention is the hepatitis B vaccine. Liver cancer is one of the most common cancers in the world and the most common cancer in some parts of Asia. With the hepatitis B vaccine now included in universal childhood immunization programs, new cases of this cancer are expected to drop.
![]()
As even this brief survey of disease threats shows, trends in infectious disease are never stagnant. They reflect dynamic forces in the world, some of which are the subject of the next section. The microbe–human relationship continues to evolve in ways that may not always be predictable, especially as we exert ever-greater stresses on the planet in our endless quest to survive and prosper.
















