4
Research Needed to Improve Breastfeeding Protection, Promotion, and Support Within WIC
OPENING STATEMENT
Moderator: Miriam Labbok
Moderator Miriam Labbok opened the session with a series of slides covering research on the ways in which breastfeeding supports both maternal and infant health, the many adverse effects of any formula use (also called lack of breastfeeding), trends in the rate of breastfeeding initiation by the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participation status, and WIC participants’ much lower rates of exclusive breastfeeding at 3 and 6 months1 when compared with other WIC-eligible women and with non-eligible women, along with a list of areas where research is needed (Box 4-1). She emphasized the inverted pressure to formula-feed that is related to the formula provided by WIC food packages for infants whose mothers choose not to breastfeed exclusively or partially. During the session, the presenters (Karen Bonuck, Maya Bunik, and Cynthia Howard) focused on different aspects of breastfeeding research and provided suggestions related to surveillance, breastfeeding research involving the WIC food packages, staffing issues (especially peer counseling), and potential research designs. Discussant Larry Grummer-Strawn focused on research related to staffing for breastfeeding support.
|
BOX 4-1 Areas Where Breastfeeding Research Is Needed
|
A WIC AGENDA FOR BREASTFEEDING-PROMOTION RESEARCH
Presenter: Karen Bonuck
Lessons from Previous Research
Bonuck began by highlighting lessons for WIC that she had gleaned from a 2008 review by the U.S. Preventive Services Task Force (USPSTF, 2008) of the effects of breastfeeding interventions on initiation, duration, and exclusivity of breastfeeding. Those lessons include:
-
Study quality matters.
-
The continuity of care (breastfeeding interventions) over the prenatal and postnatal periods matters.
-
The focus should be on exclusive breastfeeding rather than any breastfeeding.
-
The effects of professional and lay support need to be compared.
Based on preliminary evidence from an ongoing study by her group, Bonuck identified a number of key elements of successful interventions to support breastfeeding:
-
Women need information and support across care settings, over time, and in a convenient manner. Information and support are needed as part of prenatal care, during WIC visits, in the hospital, and at home.
-
Rapport between the mother and the support person is a key factor determining the effectiveness of support, especially in assisting with such skills as latching on and positioning. Adequate time must be allowed to establish rapport, and cultural matching may be helpful for basic lactation support.
-
In-person care reduces the risk of such problems as dehydration and calorie deprivation in the infant, engorgement and mastitis in the mother, and the cessation of breastfeeding for the dyad. Phone calls, pamphlets, and videos should serve as adjuncts to rather than substitutions for face-to-face support.
-
Establishing links among health professionals leads to a recognition of the value of breastfeeding support.
Figure 4-1, taken from the WIC Breastfeeding Peer Counseling Study Final Implementation Report (USDA/FNS, 2010), shows the various locations where peer counseling occurs. It illustrates the need to take into
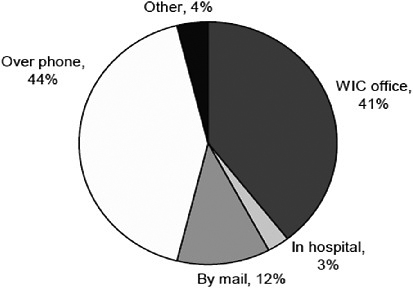
FIGURE 4-1 Location of contacts between WIC participants and peer counselors, fiscal year 2009 (n = 36 local WIC agencies, missing responses from 4).
SOURCE: USDA/FNS (2010).
account the above considerations regarding the location and timing of contacts between WIC participants and peer counselors. It is worth noting that a sizable percentage of WIC agencies prohibit peer counselors from providing guidance in the hospital or in the home, or both.
Challenges in Breastfeeding Support Research
The interpretation of studies of interventions intended to support breastfeeding (e.g., Gross et al., 2009; Olson et al., 2010) is often limited by a lack of data on breastfeeding intensity and sometimes by a lack of data on one or more of the following: actual client contacts, contacts outside of the home, duration of the contact, and problems solved and techniques used to solve them.
Research Suggestions
Based on recommendations from Chapman and Perez-Escamilla (2009), Bonuck provided the following suggestions for national breastfeeding surveillance:
-
Use standardized breastfeeding definitions: consider definitions from the Infant Feeding Practices Study II.
-
Reduce recall periods to obtain accurate information on the intensity of breastfeeding.
-
Collect data on relevant covariates.
Among the key covariates for studies of breastfeeding are prenatal breastfeeding intentions, past breastfeeding history/experience, early hospital experience, reasons for the feeding choice, and the WIC food package the mother has chosen. In addition, it would be useful to collect information on maternal and infant health outcomes, such as the body mass index of the mother and infant and, for the mother, data on cardiovascular disease and diabetes.
BREASTFEEDING ISSUES IN WIC PARTICIPANTS: FOCUS ON SUPPLEMENTATION AND STAFFING ISSUES
Presenter: Maya Bunik
In this presentation, Bunik summarized her perspective on general issues related to breastfeeding research in WIC, identified several attitudes that may interfere with breastfeeding, listed potential study questions, and briefly addressed methods and two types of intervention studies.
General Issues with Breastfeeding Research in WIC
Based on a review of selected studies related to breastfeeding in WIC, Bunik offered the following conclusions:
-
There is no need for another cross-sectional survey study on breastfeeding.
-
WIC sites vary widely in the way they deliver services.
-
The U.S. Department of Agriculture (USDA) does not allow randomization involving the food package.
-
Peer counselors seem to be the focus of funding.
Bunik added that WIC agencies need to partner with expert researchers when conducting studies, and WIC staff need time to enter data and develop meaningful databases.
Attitudes That May Interfere with Breastfeeding
According to Bunik, one of the biggest barriers for a mother may be the perception that her milk is insufficient for her infant. Combination feeding may be viewed as offering the infant “the best of both,” and there may be little recognition of the impact of supplementing mother’s milk with formula (Bunik et al., 2010). Many low-income women are concerned about pain and consider formula feeding to be an easy alternative (Alexander et al., 2010; Bunik et al., 2010). In the Latino culture, the reasons that women give for choosing combination feeding include the pain from breastfeeding, the modesty required in public places, and the need to return to work; parents and grandparents may give strong messages about cultural beliefs (Bunik et al., 2006); and the decision to formula feed may not be viewed with regret.
Study Questions
Bunik offered two sets of study questions for the research agenda.
-
The questions arising from the regulation that specifies that breastfeeding women receive no formula in the first month post partum are:
-
What are the rates in areas that truly practice this policy?
-
How universally is the policy enforced?
-
What is the role of the peer counselor in supporting and reporting on this?
-
-
-
Are there practices that couple with this policy to make it more effective (e.g., prenatal class, peer counselors, evaluation by an International Board Certified Lactation Consultant (IBCLC), breast pump access)?
-
-
The questions relating to the numbers and types of core WIC staff members, how they are used, and relationships among them are:
-
Which staff member schedules the “first visit,” and how is it done?
-
What WIC staff combinations offer the best outcomes for the breastfeeding dyad?
-
How often is an IBCLC on site?
-
Are WIC staff members empowered enough to “not give out formula”?
-
How do mothers get help early in the breastfeeding experience?
-
Is there communication with the hospital or primary care site?
-
Research Considerations
Bunik briefly addressed possible research designs, listed in Box 4-2, and then ended her presentation with two suggestions for studying interventions that combine a continuum of care with incentives:
-
Implement a series of prenatal sessions that provides preventive planning (among suggested topics were the possibilities of experiencing pain, barriers during the hospital stay, the need for access to early postpartum help for breastfeeding, and issues of unnecessary supplementation); and provide a blanket or a “hooter hider” as an incentive for attending the sessions.
-
For mothers who choose to breastfeed their newborns, provide no formula in the first month, but offer an early visit and an incentive of diapers to those who have continued to breastfeed at 1 month post partum.
PERSPECTIVES
Presenter: Cynthia R. Howard
Relevant Research Findings
Howard began her presentation by pointing out that research on awareness of and attitudes toward the breastfeeding food package is outdated.
|
BOX 4-2 Possible Research Designs
SOURCE: Szilagyi (2010). |
The previous package was not seen as valuable, whereas the formula package was seen as very valuable (Holmes et al., 2009; Murimi et al., 2010). Understanding is limited regarding the difference in the health benefits from exclusive breastfeeding and mixed feeding (Bunik et al., 2006; Holmes et al., 2009; Li et al., 2007; Vaaler et al., 2010). Barriers to breastfeeding include concerns about breastfeeding in public (even at home, depending on the household), the lack of availability of breast pumps, the difficulty of pumping, and the transition to work or school (Holmes et al., 2009).
When WIC participants are compared with non-participating WIC eligible women, the rates of exclusive breastfeeding are lower at 4 and 6 months among the WIC participants (Jacknowitz et al., 2007). Moreover, some investigators have found earlier entry into WIC to be associated with lower breastfeeding rates (Gross et al., 2009; Ziol-Guest and Hernandez, 2010). Other investigators (Bunik et al., 2009, Chatterji and Brooks-Gunn, 2004; Joyce et al., 2008; Yun et al., 2010) have reported non-significant or positive effects of WIC participation on breastfeeding outcomes. The conflicting data emphasize the importance of selecting an appropriate control group and gathering data regarding the mother’s infant feeding intentions when she enters the program.
Two Cochrane Reviews2 have addressed breastfeeding and provide information that may help in considering the WIC research agenda. The reviews found:
-
Needs-based, one-to-one, informal education or support sessions, delivered either (1) before or (2) before and after the birth by a trained breastfeeding professional or peer counselor, were the most effective intervention for promoting breastfeeding initiation among women of different ethnic backgrounds and feeding intentions (Dyson et al., 2005).
-
Trials of breastfeeding support for mothers should consider the timing and delivery of support interventions and the relative effectiveness of intervention components, and they should also report women’s views (Britton et al., 2007).
Suggested Research Priorities
Howard addressed research priorities in two topic areas: (1) the effects of the new food package, and (2) the effects of peer counseling. Studies related to the new food package would address breastfeeding initiation, exclusivity (use of the no-formula option), and duration of breastfeeding. Howard provided further detail on the proposed study to examine the effects of peer counseling on breastfeeding and other health outcomes:
-
Test components of peer counseling implemented by WIC agencies with high-performing programs, prioritizing exclusive breastfeeding and giving attention to ethnic background, race, and acculturation.
-
Test interventions that are feasible, replicable in many setting, and affordable, such as staffing and the supervision of peer counselors; the role of the WIC retailer in facilitating community partnerships; tools to facilitate referrals to WIC from medical care settings and social service agencies; and hospital rounding and collaborations.
-
Examine breastfeeding initiation, exclusivity, and duration as major outcomes, but also consider the introduction of solid food and of cow milk, maternal stress and self-confidence, parenting, and family diet.
-
Include a qualitative component to assess participant experiences, identify helpful aspects of the intervention, and help guide future processes and policies.
RESPONSE
Discussant: Larry M. Grummer-Strawn
In his response, Grummer-Strawn first introduced key breastfeeding initiatives in WIC and a few related research questions. His major focus,
however, was on peer counseling—the topic that was emphasized by the three presenters.
Overview of Key Breastfeeding Initiatives in WIC
The five key breastfeeding initiatives in WIC are: (1) mass media campaigns, (2) WIC food package changes, (3) breast pump distribution, (4) staff training (e.g., “Grow and Glow”), and (5) state incentives. Grummer-Strawn identified one research question related to each initiative:
-
Mass media What messages actually motivate behavior change with regard to breastfeeding?
-
Food packages What are the effects of the changes in the food packages on breastfeeding rates, especially the rate of exclusive breastfeeding?
-
Breast pump distribution Does breast pump distribution increase breastfeeding duration by enabling women to return to work or school, or does it reduce breastfeeding by mechanizing the process, as suggested earlier in the session?
-
Staff training Does general training of all WIC staff about breastfeeding make enough of a difference in breastfeeding rates to make it worth the additional cost?
-
State incentives Do financial incentives to states that provide more money for improvements resulting from breastfeeding promotion in WIC lead to changes in the planning and implementation of programs? Furthermore, what effects do the infant formula rebates have on program decisions?
Research Related to Staffing for Breastfeeding Support
Grummer-Strawn’s number one research priority was stronger effectiveness studies of peer counseling within WIC. Funding for peer counseling has grown to $80 million, but, as noted by earlier presenters, the U.S. Preventive Services Task Force found inconclusive evidence of its effectiveness, and there is limited information on the aspects that can improve effectiveness. Such research needs to examine the effects of peer counseling on breastfeeding rates for the entire clinic, not just for the women who choose to use a peer counselor. Moreover, studies need to examine the cost-effectiveness of peer counseling relative to other interventions.
The focus of the research, Grummer-Strawn said, should be on the following components of peer counseling support:
-
Peer counseling training: What competencies are needed?
-
The role of peer counselors: Breastfeeding advocates, or supporters of all infant feeding decisions
-
Peer counseling contacts: Relative importance of prenatal and postpartum contacts, number needed, duration, and type
-
Cultural competency: Matching of peer counselors with clients, structure in different communities, reaching women who do not want peer counselors
-
Roles of lactation consultants: Supervision versus individual support, ratio of clients to lactation consultants, relationship to peer counselors
-
Relationship of peer counseling to medical care: Connections with other providers and care sites, including in-hospital contacts and information flow
Study Design
Although very large sample sizes would be required in ecologic quasi-experimental studies, gathering information on the wide variety of ways in which peer counseling is implemented across the nation would make it possible to examine the differences in the impacts of the various sorts of programs. Given the long list of questions about different aspects of peer counseling, Grummer-Strawn argued for less emphasis on causality (that is, on group-randomized controlled trials, which can answer only one question at a time) and more on plausibility (relative effectiveness of different kinds of programs).
GROUP DISCUSSION
Moderator: Miriam Labbok
Presenters and many attendees participated in a discussion that covered the following topics:
-
Data quality The collection of accurate data on breastfeeding poses a number of challenges:
-
Exclusivity is determined from self-report and is more accurate if the question is asked about breastfeeding that day or at some time close to that day. Acceptance of the exclusive breastfeeding package does not mean that the mother is not obtaining formula from other sources (e.g., using manufacturers’ coupons to buy formula). The mother’s concern about answers that could change the mother-infant dyad’s WIC
-
-
-
food packages could contribute to biased responses. Answers obtained at different times from the same mother may be inconsistent.
-
Data are complicated in that the data must be collected longitudinally about a behavior that is changing over time.
-
Local agencies collect little data that are relevant to the impact of peer counseling.
-
Quality control is difficult to implement because tens of thousands of clerks across the nation collect, record, and process data for WIC.
-
Since WIC clinics are not set up to conduct research, researchers need to find an approach that allows a study to benefit the participating clinics or their clients, such as including money for WIC staff in the research budget.
-
-
Access to data Not all investigators have access to the data that are collected, because data sharing requires the Health Insurance Portability and Accountability Act (HIPAA) rules be followed.
-
Collaboration Considering that Medicaid covers the health care of many WIC families and that Medicaid has periodic contact with its clients, beneficial collaborations between WIC and Medicaid could include studies regarding the setting of reimbursement rates for specific services and studies regarding outreach. Data sharing between Medicaid and WIC could also be very valuable. Preliminary data suggest that collaboration is the weakest aspect of the Loving Support Peer Counseling Program,3 which is currently being evaluated. On the other hand, several workshop attendees encouraged a concerted effort to stay away from collaborations with the formula industry.
-
Preliminary findings According to Pat Gradziel,4 with the introduction of the new food package in the California state WIC program, the rate of exclusive breastfeeding jumped upward, the rate of partial breastfeeding decreased substantially, and these changes have persisted. Bonuck’s study has found that the trimester of entry into WIC is positively associated with the initiation and duration of breastfeeding but that the effects differ for first births versus higher-order births.
-
Baby Friendly Hospital Initiative (BFHI) Dr. Labbok reported that research she had done with Eugene Declercq demonstrated positive benefits on breastfeeding may result even if not all 10 steps to suc-
-
cessful breastfeeding cited by the BFHI are in place; implementation need not lead to increased costs.
One suggestion for improving the monitoring and surveillance of programs was to identify sentinel programs across the nation and support their efforts to improve the WIC electronic data. Income tiering (looking at incomes at different percentages [e.g., 25, 50, 75, 100, up to 185 percent] of the U.S. Poverty Income Guidelines) is a valuable approach when examining covariates in studies.
SUMMARY OF SUGGESTED RESEARCH TOPICS
The research suggestions made during this session focused mainly on the study of support services for breastfeeding, especially research related to staffing (e.g., roles of peer counselors and IBCLCs, where and when they provide care, and their collaboration with a variety of other care providers) and on the study of breastfeeding incentives and changes in the food packages for the mother-infant dyad. Considerable attention was given to research methods, including the need for (1) improved data collection, quality, and access; (2) feasible experimental designs that give careful attention to the selection of appropriate control groups; and (3) qualitative components of studies to gather data for guiding future efforts and for assessing the relative effectiveness of different kinds of programs.
REFERENCES
AAP (American Academy of Pediatrics). 2009. Pediatric Nutrition Handbook, 6th ed. Elk Grove Village, IL: American Academy of Pediatrics.
Alexander, A., D. Dowling, and L. Furman. 2010. What do pregnant low-income women say about breastfeeding? Breastfeeding Medicine 5(1):17–23.
Britton, C., F. M. McCormick, M. J. Renfrew, A. Wade, and S. E. King. 2007. Support for breastfeeding mothers. Cochrane Database of Systematic Reviews(1):CD001141.
Bunik, M., L. Clark, L. M. Zimmer, L. M. Jimenez, M. E. O’Connor, L. A. Crane, and A. Kempe. 2006. Early infant feeding decisions in low-income Latinas. Breastfeeding Medicine 1(4):225–235.
Bunik, M., N. F. Krebs, B. Beaty, M. McClatchey, and D. L. Olds. 2009. Breastfeeding and WIC enrollment in the nurse family partnership program. Breastfeeding Medicine 4(3):145–149.
Bunik, M., P. Shobe, M. E. O’Connor, B. Beaty, S. Langendoerfer, L. Crane, and A. Kempe. 2010. Are 2 weeks of daily breastfeeding support insufficient to overcome the influences of formula? Academic Pediatrics 10(1):21–28.
Chapman, D. J., and R. Perez-Escamilla. 2009. US national breastfeeding monitoring and surveillance: Current status and recommendations. Journal of Human Lactation 25(2): 139–150.
Chatterji, P., and J. Brooks-Gunn. 2004. WIC participation, breastfeeding practices, and well-child care among unmarried, low-income mothers. American Journal of Public Health 94(8):1324–1327.
Cochrane Reviews. 2010. What Are Cochrane Reviews? Oxford, UK: The Cochrane Collaboration. http://www.cochrane.org/cochrane-reviews (accessed October 15, 2010).
Dyson, L., F. McCormick, and M. J. Renfrew. 2005. Interventions for promoting the initiation of breastfeeding. Cochrane Database of Systematic Reviews (2):CD001688.
Gross, S. M., A. K. Resnik, C. Cross-Barnet, J. P. Nanda, M. Augustyn, and D. M. Paige. 2009. The differential impact of WIC peer counseling programs on breastfeeding initiation across the state of Maryland. Journal of Human Lactation 25(4):435–443.
Holmes, A. V., N. P. Chin, J. Kaczorowski, and C. R. Howard. 2009. A barrier to exclusive breastfeeding for WIC enrollees: Limited use of exclusive breastfeeding food package for mothers. Breastfeeding Medicine 4(1):25–30.
Jacknowitz, A., D. Novillo, and L. Tiehen. 2007. Special Supplemental Nutrition Program for Women, Infants, and Children and infant feeding practices. Pediatrics 119(2):281–289.
Joyce, T., A. Racine, and C. Yunzal-Butler. 2008. Reassessing the WIC effect: Evidence from the Pregnancy Nutrition Surveillance System. Journal of Policy Analysis and Management 27(2):277–303.
Li, R., V. J. Rock, and L. Grummer-Strawn. 2007. Changes in public attitudes toward breastfeeding in the United States, 1999–2003. Journal of the American Dietetic Association 107(1):122–127.
Murimi, M., C. M. Dodge, J. Pope, and D. Erickson. 2010. Factors that influence breastfeeding decisions among Special Supplemental Nutrition Program for Women, Infants, and Children participants from Central Louisiana. Journal of the American Dietetic Association 110(4):624–627.
Olson, B. H., S. J. Haider, L. Vangjel, T. A. Bolton, and J. G. Gold. 2010. A quasi-experimental evaluation of a breastfeeding support program for low income women in Michigan. Maternal and Child Health Journal 14(1):86–93.
Szilagyi, P. G. 2010. Crossing the Abyss: From Research to Dissemination/Implementation to Better Health. http://www.research-practice.org/pdfs/ConferencePresentations/Szilagyi_From_Research _to_Dossemination__Implementation.pdf (accessed September 16, 2010).
USDA/FNS (U.S. Department of Agriculture/Food and Nutrition Service). 2010. WIC Breastfeeding Peer Counseling Study Final Implementation Report. Alexandria, VA: USDA/FNS. http://www.fns.usda.gov/ora/menu/published/WIC/FILES/WICPeerCounseling.pdf (accessed September 7, 2010).
USPSTF (U.S. Preventive Services Task Force). 2008. Primary care interventions to promote breastfeeding: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine 149(8):560–564.
Vaaler, M. L., J. Stagg, S. E. Parks, T. Erickson, and B. C. Castrucci. 2010. Breast-feeding attitudes and behavior among WIC mothers in Texas. Journal of Nutrition Education and Behavior 42(3 Suppl.):S30–S38.
Yun, S., Q. Liu, K. Mertzlufft, C. Kruse, M. White, P. Fuller, and B. P. Zhu. 2010. Evaluation of the Missouri WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) breast-feeding peer counselling programme. Public Health Nutrition 13(2):229–237.
Ziol-Guest, K. M., and D. C. Hernandez. 2010. First- and second-trimester WIC participation is associated with lower rates of breastfeeding and early introduction of cow’s milk during infancy. Journal of the American Dietetic Association 110(5):702–709.














