8
Health Care and Systems Costs, Benefits, and Effectiveness
In opening this session, moderator Barbara Devaney noted that the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) might affect health care costs in two opposing ways and suggested that the speakers might address these effects. On one hand, WIC may lead to improved dietary and health behaviors that would lead to better health, fewer adverse health outcomes, and reduced health care costs. On the other hand, it is possible that WIC’s referrals and improved linkages to the health care system could lead to increased health care utilization and increased health care costs.
During the session, Sally Findley focused on research related to long-term health and system impacts associated with WIC, while Helen Jensen addressed elements of human health risk–benefit assessment and their implications for research.
SUGGESTIONS FOR ASSESSING THE LONG-TERM HEALTH AND SYSTEM IMPACTS ASSOCIATED WITH WIC
Presenter: Sally E. Findley
“Optimistic” Logic Model
Findley presented an “optimistic” logic model for assessing WIC’s impact on health care outcomes, an abbreviated version of which is shown in Figure 8-1. On the far right of the figure are the long-term impacts that
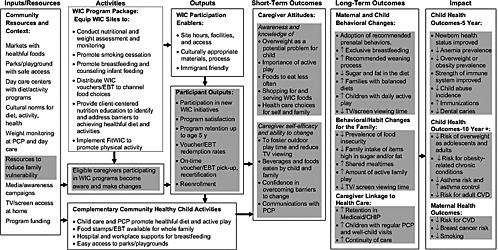
FIGURE 8-1 Abbreviated version of Findley’s optimistic logic model for assessing WIC’s impact on health care outcomes. Outcomes would be measured to determine the extent to which favorable results have occurred.
NOTE: ↑ = increased; ↓ = decreased; CHIP = Child Health Insurance Program; CVD = cardiovascular disease; EBT = electronic benefit transfer; PCP = primary care provider; TV = television. Fit WIC is a collection of social and environmental strategies to promote healthy weight among children enrolled in WIC.
SOURCE: Findley (2010).
can be anticipated from effective WIC services—in particular, impacts that could affect health care utilization and costs. One purpose of the logic model is to show the causal pathway that links WIC activities (box on left) with these impacts. The intermediary boxes show where changes occur through both short-term changes in caregiver attitudes, such as knowledge about the importance of low fat milk consumption, and increased caregiver self-efficacy. The subsequent long-term outcomes can include maternal and behavioral changes, some of which (e.g., reduced food insecurity) could affect the entire family’s health behaviors. The actual child health outcomes appear in the boxes at the far right and are listed as outcomes occurring after 5 years and after 10 or more years.
Considering Impacts Over Time
Rationale
According to Findley, WIC needs studies that document the different time frames over which effects take place. Currently, there are time-sensitive opportunities for 5-year WIC impact assessments that relate to the previous and current WIC food packages, effects of the recession and of changes in insurance coverage pursuant to the Affordable Health Care Act, and linkages with clinical programs seeking to promote patient-centered care. Findley found no studies that have looked at effects of WIC after 5 years. Child health studies, however, show evidence of possible long-term health outcomes of WIC for children, and maternal health studies suggest long-term health benefits for both women and their children (see Box 8-1). Even if the long-term benefits of WIC are fairly small, they could potentially be very large when multiplied over the entire population affected. Evidence of strong long-term consequences could provide additional details needed to extend cost–benefit and cost-effectiveness analyses.
Challenges
Long-term studies pose many challenges, including the tracking of WIC participants over time and difficulties obtaining accurate data on the intensity of and exposure to WIC services for a given mother-child dyad. The optimistic logic model can be used to tease out the possible mechanisms by which the WIC influence might be transmitted over time through sustained behavioral changes.
|
BOX 8-1 Evidence of Possible Long-Term Health Outcomes of WIC Children
Women
|
Potential Research Topics
Child Health
Findley suggested several high-priority research topics concerning the long-term impact of WIC on child health. These include WIC-related exclusive breastfeeding as protection from chronic disorders, the durability of any WIC-related reduction in body mass index through adolescence (e.g., does a decay model describe the findings, or is there evidence of positive synergistic interaction with subsequent interventions?), the effect of WIC participation on health care utilization and costs 5 to 15 years post WIC, and the effect of WIC to age 21 among a cohort followed through the National Children’s Study.
Maternal and Family Health
High-priority maternal-health-outcome studies include the effectiveness of WIC interventions during pregnancy to promote lasting behavioral
and diet changes among mothers, linkages between changes in the diets of mothers and the diets of their infants and children enrolled in WIC, effects of repeat WIC “doses” of counseling and checks on changes in family diet and activity patterns, changes in health care utilization and costs for WIC mothers (controlling for household economic security and prior chronic conditions), and the effects of co-locating WIC and Healthy Start and Healthy Families programs on maternal health behaviors and outcomes.
Changes in Health Care Utilization
An often overlooked behavioral component of WIC is change in health care utilization. Relatively little attention has been paid to the linkages between WIC and the primary health care system and continuity of care, even though there is much evidence that continuity of care has a positive effect on many preventive behaviors and on chronic disease management (Flores et al., 2005; Groner et al., 2009; Nelson et al., 2005). Kendal and colleagues (2002) have reported increased positive changes in health behavior when WIC is co-located with a managed-care organization.
Research Priorities
First Priority
Findley’s number one research priority is a long-term prospective study of WIC versus non-WIC children with a baseline and 5- and 10-year follow-ups, as indicated in Table 8-1.
The child health outcomes would include changes in body mass index, diet and physical activity, television viewing, and health care utilization. The same individuals would be evaluated at each time period. Co-variates to be tracked longitudinally would include the child’s family situation, maternal behaviors, participation in Head Start or parenting programs, continuity of care, and neighborhood factors that may contribute to obesity.
The National Children’s Study would be the best candidate data set for this research because the study is nationwide; centers will be located
TABLE 8-1 Proposed Design of Prospective Study of WIC Versus Non-WIC Children
|
|
WIC-High Exposure |
WIC-Low Exposure |
Non-WIC Exposure |
|
Baseline (2010–2011) |
|
|
|
|
5-Year Follow-Up |
|
|
|
|
10-Year Follow-Up |
|
|
|
in every state; vanguard sites are already recruiting cohorts; the study will collect extensive details regarding the prenatal situation, the mother’s situation, and the child’s situation at each point in time; and it will track neighborhood influences for each time period.
Second Priority
Findley’s second priority for WIC research is a study to determine the durability of the changes in behavior, food intake, and weight that are achieved among WIC participants with the new WIC package of foods and counseling. Such a study would use upcoming data from the new National Survey of Children’s Health (http://www.cdc.gov/nchs/slaits/nsch.htm). It may be possible to include WIC participation variables in the survey instrument, which is still in development. The multi-level and 5-year analysis would include the timing and intensity of WIC participation, qualitative interviews with selected WIC staff and participants, community characteristics, and primary care linkages. A particular focus would be maternal behaviors and maternal and child outcomes.
Third Priority
Findley’s third priority addresses the question “How is the WIC message enhanced through coordination with primary care providers?” She described a comparative effectiveness study that would be designed with multiple study arms, one for each type of linkage with a primary health care (PHC) provider: no PHC, PHC for maternal care, PHC for child health care, and joint linkage for maternal and child care. The design could also control for the style of PHC, such as whether the PHC provider offered patient-centered care, shared electronic medical records with WIC, or was co-located with WIC. This study would track WIC retention, behavioral and health outcomes, and health care utilization. Among the methodological concerns are issues relating to the measurement of WIC exposure, the time horizon for impact assessment, the key covariates, and the accurate description of the primary care structure and linkages.
Closing Comments
Findley emphasized that assessing the cost-effectiveness of WIC requires the careful identification of outcomes—both those that are targeted directly and those that may occur over the long term (such as the reduction of obesity, asthma, or diabetes).
PERSPECTIVES ON RISK–BENEFIT ASSESSMENT
Presenter: Helen H. Jensen
In opening her presentation, Jensen pointed out that WIC could be considered a bridge from the food programs to the health system. As shown in Table 8-2, WIC is one of several important food programs of the U.S. Department of Agriculture (USDA). Jensen took the perspective of looking at the risks and benefits relative to programs targeted to mothers, infants, and young children.
Elements of Human Health Risk-Benefit Assessment
The European Food Safety Authority gives the following definition of benefit, in the context of a health risk–benefit assessment: “The probability of a positive health effect and/or the probability of a reduction of an adverse health effect in an organism, system, or (sub) population, in reaction to exposure to an agent” (EFSA, 2010, p. 8). This broad definition indicates that WIC research into health benefits should aim to understand the context of the effect, the exposure, the intervention or policy, and the aspect of the program that is having the effect.
The risk–benefit assessment paradigm includes four elements: (1) identification of health effects, both positive and negative; (2) characterization of the health effect (the dose–response assessment; (3) exposure assessment; and (4) benefit characterization. The expected health effects would be examined for the target population. Health effects could be direct or indirect and would include the response to program participation; the response to program parameters, such as benefits and interventions; and the longevity of the response relative to differences in the intensity and duration of exposure and evidence of carryover. Exposure assessment addresses the populations that are reached, the extent of participation of at-risk populations, the duration and intensity of the exposure (e.g., breastfeeding) relative to those populations, and covariates (e.g., labor force participation issues relative to breastfeeding). Careful characterization of benefits is especially important
TABLE 8-2 Budgets for U.S. Department of Agriculture Food Programs, Federal Year 2011
|
Program |
2011 Budget (in millions) |
|
Supplemental Nutrition Assistance Program (SNAP) |
$68,207 |
|
Child Nutrition Programs |
$18,392 |
|
Special Supplemental Nutrition Program (WIC) |
$7,603 |
|
SOURCE: USDA (2010). |
|
for developing a more integrated understanding of relationships among WIC and health outcomes.
Jensen suggested that consideration be given to including three health risks in the WIC research agenda: low birth rate, obesity, and food insecurity. Human health benefits could result from interventions that reduce those adverse effects and enhance positive effects. Cost-effectiveness analysis could investigate the cost-effectiveness of program interventions relative to expenditures across various programs or else provide a comparative assessment of the three kinds of WIC interventions (supplemental food packages, nutrition education, and referrals to health services).
In conducting a comparative risk–benefit assessment, one must identify and consider multiple metrics and recognize that an increase in preventive services may increase health care costs. One also needs to consider the strength of the evidence and uncertainty. Uncertainties increase when examining longer-term associations. Combining risks and benefits in a systematic framework assists in setting priorities. A comparative assessment needs to distinguish substitute activities, complementary activities, and reinforcing activities and determine how best to build on the joint activities in the system.
To improve risk–benefit management decisions, one needs to understand key differences between treatment and prevention activities and determine how best to give value to prevention activities. A question for studies spanning the 1- to 5-year range might be, “What health care costs were saved by early interventions?” Effects need to be considered for individuals and for the household—both in terms of food and in terms of interactions with the health care system.
Implications for Research
In health care, the time horizon requires careful attention, as does the value of longer-term outcomes. The characterization of benefits for various program populations will differ considerably. Cross-program effects (such as concurrent participation in health care, immunizations, and prenatal care) make it especially challenging to distinguish among what is attributable to WIC, associated with WIC, or a product of other health care system interventions.
Jensen called for efforts to establish linkages between WIC interventions and health care utilization and outcomes. In the case of mothers, for example, how do incentives to breastfeed carry over in terms of improvements for the mother and for the household? Common metrics are needed that align with WIC and with related health programs. Finally, she suggested that data are needed on cross-program participation (including the diversity of participants and changing demographics) and the household’s exposure to the health care system.
RESPONSE
Discussant: Paul Buescher
In his response, Buescher commented on several issues related to cost studies that were raised during this and other sessions. In particular, he highlighted important types of evaluations, addressed some methodological challenges, and raised some new questions, as summarized below:
-
Evaluations linking administrative data from WIC, Medicaid, and birth certificates It would be useful to update such evaluations for time periods when the new WIC packages have become available, taking care to improve methods to reduce biases.
-
Linkages between WIC interventions and health care utilization and outcomes Perhaps many of the positive effects of WIC arise because of WIC’s success in helping its participants make use of other appropriate health and social services. Oral health care linkages may be important to address.
-
Long-term impacts of WIC for children, maternal health, and the interaction between WIC and health care A major challenge here will be accessing and developing appropriate data sources. One advantage of the longitudinal studies suggested earlier by Murphy and Findley would be the possibility of showing that later health care costs decrease substantially, overshadowing initial increases related to higher use of preventive care services.
-
Overcoming potential biases Huntington and Connell (1994) discuss several flaws in research methods used in studies of cost savings from prenatal care. Buescher said that it is essential to develop methods to address the problem of self-selection bias, for example, because WIC participants may differ from non-participants on unmeasured characteristics.
-
Benefits of WIC for children More research is needed on this topic, and new data sources are needed to conduct evaluations of this type. Buescher suggested that USDA staff contact the principal investigators of the National Children’s Study to ensure that appropriate data are collected to enable research on WIC, including the assessment of the long-term effects of prenatal and child WIC participation.
-
Criteria for judging WIC Is cost savings an appropriate criterion? WIC participants in North Carolina had higher use of preventive, diagnostic, and curative medical care services, and this was associated with higher costs for Medicaid (Buescher et al., 2003). This may not be a negative outcome, however, if the health care needs of the WIC children on Medicaid were being met better than were those of non-participants.
-
Consideration of income level Would it be advisable to stratify by income level in new studies of WIC in order to assess differential effects? The positive results of many of the earlier studies were from a time when the income level for Medicaid enrollment was 100 percent of the federal poverty level or less, in contrast to the current level of at least 185 percent of the poverty level.
GROUP DISCUSSION
Moderator: Barbara Devaney
Topics raised during the group discussion included the following:
-
One possible prenatal effect of WIC might be a decrease in the percentage of conceptuses lost before about 22 weeks of gestation accompanied by an increase in the number of very-low-birth-weight or preterm infants, for example.
-
Consideration of long-term outcomes requires information over a long period of time and is fraught with potential analytic traps. Methods need to be developed to deal with them.
-
Oral health care is an example of a primary care linkage with WIC—one that may merit more attention with regard to both maternal and child health.
-
A cost–benefit analysis might consider differences in lifetime earnings of WIC recipients; some data sets would allow examination of the issue. Because of the number of variables and the long timeframe, however, it may be more feasible to examine the relationship of WIC participation with early school performance.
-
Differences in the diagnosis and treatment of common childhood diseases for WIC and non-WIC children, as were seen in the North Carolina WIC–Medicaid study, could lead to big differences as the children enter school and beyond, and thus may merit study.
SUMMARY OF SUGGESTED RESEARCH TOPICS
The research suggestions made during this session centered on the investigation of long-term impacts of WIC for children, maternal health, and the interaction between WIC and health care. Among the suggested strategies was linking administrative data from WIC, Medicaid, and birth certificates. Methodological issues addressed included the consideration of risks and benefits, potential biases, and clear identification of WIC’s role relative to the health outcomes examined.
REFERENCES
Buescher, P. A., S. J. Horton, B. L. Devaney, S. J. Roholt, A. J. Lenihan, J. T. Whitmire, and J. B. Kotch. 2003. Child participation in WIC: Medicaid costs and use of health care services. American Journal of Public Health 93(1):145–150.
Chulada, P. C., S. J. Arbes, Jr., D. Dunson, and D. C. Zeldin. 2003. Breast-feeding and the prevalence of asthma and wheeze in children: Analyses from the third National Health and Nutrition Examination Survey, 1988–1994. Journal of Allergy and Clinical Immunology 111(2):328–336.
Dietert, R. R., and J. T. Zelikoff. 2008. Early-life environment, developmental immunotoxicology, and the risk of pediatric allergic disease including asthma. Birth Defects Research. Part B, Developmental and Reproductive Toxicology 83(6):547–560.
DiGiorgio, L. F., and N. Danoff. 2005. Promoting breastfeeding to mothers in the Special Supplemental Nutrition Program for Women, Infants, and Children. Journal of the American Dietetic Association 105(5):716–717.
EFSA (European Food Safety Authority Scientific Committee). 2010. Guidance on human health risk–benefit assessment of food. European Food Safety Authority Journal 8(7):1673. http://www.efsa.europa.eu/en/scdocs/doc/1673.pdf (accessed September 9, 2010).
Findley, S. E. 2010. Suggestions for assessing the long-term health and system impacts associated with the new WIC packages. Presented at the IOM workshop, Health Impacts: Planning a WIC Research Agenda. Washington, DC: The National Academies Press.
Fiorino, E. K., and L. J. Brooks. 2009. Obesity and respiratory diseases in childhood. Clinics in Chest Medicine 30(3):601–608, x.
Flores, G., L. Olson, and S. C. Tomany-Korman. 2005. Racial and ethnic disparities in early childhood health and health care. Pediatrics 115(2):e183–e193.
Franks, P. W., R. L. Hanson, W. C. Knowler, M. L. Sievers, P. H. Bennett, and H. C. Looker. 2010. Childhood obesity, other cardiovascular risk factors, and premature death. New England Journal of Medicine 362(6):485–493.
Gold, D. R., H. A. Burge, V. Carey, D. K. Milton, T. Platts-Mills, and S. T. Weiss. 1999. Predictors of repeated wheeze in the first year of life: The relative roles of cockroach, birth weight, acute lower respiratory illness, and maternal smoking. American Journal of Respiratory and Critical Care Medicine 160(1):227–236.
Goran, M. I., G. D. Ball, and M. L. Cruz. 2003. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. Journal of Clinical Endocrinology and Metabolism 88(4):1417–1427.
Groner, J. A., T. Skybo, L. Murray-Johnson, P. Schwirian, I. Eneli, A. Sternstein, E. Klein, and G. French. 2009. Anticipatory guidance for prevention of childhood obesity: Design of the MOMS project. Clinical Pediatrics 48(5):483–492.
Huang, J. S., T. A. Lee, and M. C. Lu. 2007. Prenatal programming of childhood overweight and obesity. Maternal and Child Health Journal 11(5):461–473.
Huntington, J., and F. A. Connell. 1994. For every dollar spent—The cost-savings argument for prenatal care. New England Journal of Medicine 331(19):1303–1307.
Hyppönen, E., S. M. Virtanen, M. G. Kenward, M. Knip, and H. K. Åkerblom. 2000. Obesity, increased linear growth, and risk of type 1 diabetes in children. Diabetes Care 23(12):1755–1760.
Kendal, A. P., A. Peterson, C. Manning, F. Xu, L. J. Neville, and C. Hogue. 2002. Improving the health of infants on Medicaid by collocating special supplemental nutrition clinics with managed care provider sites. American Journal of Public Health 92(3): 399–403.
Klohe-Lehman, D. M., J. Freeland-Graves, K. K. Clarke, G. Cai, V. S. Voruganti, T. J. Milani, H. J. Nuss, J. M. Proffitt, and T. M. Bohman. 2007. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. Journal of the American College of Nutrition 26(3):196–208.
Lamb, M. M., D. Dabelea, X. Yin, L. G. Ogden, G. J. Klingensmith, M. Rewers, and J. M. Norris. 2010. Early-life predictors of higher body mass index in healthy children. Annals of Nutrition and Metabolism 56(1):16–22.
Laraia, B. A., A. M. Siega–Riz, and C. Gundersen. 2010. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. Journal of the American Dietetic Association 110(5):692–701.
Lee, J. Y., R. G. Rozier, E. C. Norton, J. B. Kotch, and W. F. Vann, Jr. 2004. Effects of WIC participation on children’s use of oral health services. American Journal of Public Health 94(5):772–777.
McGillis Bindler, R. C. 2007. A cascade of events—Obesity, metabolic syndrome, and type 2 diabetes mellitus in youth. Nursing Clinics of North America 42(1):29–42, vi.
Morgan, W. J. 1998. Maternal smoking and infant lung function. Further evidence for an in utero effect. American Journal of Respiratory and Critical Care Medicine 158(3): 689–690.
Nelson, C. S., S. M. Higman, C. Sia, E. McFarlane, L. Fuddy, and A. K. Duggan. 2005. Medical homes for at-risk children: Parental reports of clinician–parent relationships, anticipatory guidance, and behavior changes. Pediatrics 115(1):48–56.
Nelson, S. M., P. Matthews, and L. Poston. 2010. Maternal metabolism and obesity: Modifiable determinants of pregnancy outcome. Human Reproduction Update 16(3):255–275.
Oddy, W. H., J. L. Sherriff, N. H. de Klerk, G. E. Kendall, P. D. Sly, L. J. Beilin, K. B. Blake, L. I. Landau, and F. J. Stanley. 2004. The relation of breastfeeding and body mass index to asthma and atopy in children: A prospective cohort study to age 6 years. American Journal of Public Health 94(9):1531–1537.
Papas, M. A., K. M. Hurley, A. M. Quigg, S. E. Oberlander, and M. M. Black. 2009. Low-income, African American adolescent mothers and their toddlers exhibit similar dietary variety patterns. Journal of Nutrition Education and Behavior 41(2):87–94.
Roelands, J., M. G. Jamison, A. D. Lyerly, and A. H. James. 2009. Consequences of smoking during pregnancy on maternal health. Journal of Women’s Health 18(6):867–872.
Serdula, M. K., D. Ivery, R. J. Coates, D. S. Freedman, D. F. Williamson, and T. Byers. 1993. Do obese children become obese adults? A review of the literature. Preventive Medicine 22(2):167–177.
Stuebe, A. M., W. C. Willett, F. Xue, and K. B. Michels. 2009. Lactation and incidence of premenopausal breast cancer: A longitudinal study. Archives of Internal Medicine 169(15):1364–1371.
USDA (U.S. Department of Agriculture). 2010. FY 2011 Budget Summary and Annual Performance Plan. Washington, DC: USDA. http://www.obpa.usda.gov/budsum/FY11budsum.pdf (accessed September 10, 2010).
Van Cleave, J., S. L. Gortmaker, and J. M. Perrin. 2010. Dynamics of obesity and chronic health conditions among children and youth. Journal of the American Medical Association 303(7):623–630.












