7
TB and Drug-Resistant TB in
Vulnerable Populations
Key Messages
- Pediatric TB is generally underreported since children can be difficult to diagnose and are often overlooked or slighted in TB statistics.
- Treatment of children calls for quality-assured pediatric formulations with standard regimens.
- Interventions in the lives of TB patients who suffer from alcohol or drug dependence can greatly reduce treatment default rates and the spread of drug-resistant strains.
- Despite an increase in HIV infection rates, the number of active TB patients in Russian prisons has fallen by more than half over the past decade, in part because of more effective diagnostic and treatment programs.
Speakers at the workshop addressed TB and drug-resistant TB among three particularly vulnerable populations: children, people with drug and alcohol dependencies, and the incarcerated.
DRUG-RESISTANT TB IN CHILDREN: THE HIDDEN EPIDEMIC1
Pérez-Vélez has been studying TB in the port city of Buenaventura, Colombia, since 2006. According to Pérez-Vélez, drug-susceptible and drug-resistant TB in children is underdiagnosed and underreported, and efforts to combat it are therefore underfunded. TB in children is a “hidden epidemic” and a major neglected child health problem he suggested, especially in communities that are ill equipped to address the problem adequately.
Data typically include only microbiologically confirmed and mainly smear-positive cases, yet children frequently have extrapulmonary TB, which can be difficult to diagnose clinically and confirm bacteriologically and carries its own set of complications. There are two additional reasons why accurate information on the epidemiology of TB in children is limited: (1) the criteria for defining a case of TB in a child vary, and (2) of the four WHO criteria for diagnosing TB in children, two (PPD-tuberculin test and radiography) often are not available in resource-limited settings—those with the highest burden of TB.
Furthermore, until 2007 WHO typically grouped all children in one age category—ages 0–14—rather than analyzing them in more precise subgroups. Even today, WHO reports results only for ages 0–4 and 5−14, even though children aged 5−10 tend to develop TB at much lower rates, thus confounding the latter grouping. In countries with an intermediate burden of TB, including many Latin American nations, many regions have high-burden pockets of TB; when averaged with the TB notifications from low-burden regions, however, the high-burden areas effectively disappear and consequently receive little attention. Native Indians (Amerindians) are an example of a highly vulnerable population, with some reservations having incidence rates as high as 1,000 per 100,000 population and high mortality. Another group underrepresented in surveillance reports consists of peasants, including many children, displaced by civil wars and often living in camps.
Children also have traditionally been excluded from surveillance of TB drug resistance. In the report series Anti-Tuberculosis Drug Resistance in the World (WHO, 2008), children originally were not included, and when they were, age groups between 0 and 14 were combined. In many health policy meetings and clinical training courses, pediatric TB is not even on the agenda.
Pérez-Vélez suggested that children be divided into different age groups and that a strong effort be made to eliminate underreporting. To advocate
![]()
1 This section is based on the presentations of Carlos Pérez-Vélez, National Jewish Health and University of Colorado School of Medicine, Denver, Colorado; Dr. Shin; and Gary Reubenson, Rahima Moosa Mother and Child Hospital, South Africa.
effectively for policy changes, supporting data must be available to decision makers. In addition, Pérez-Vélez noted, quality-assured pediatric formulations of both first-line and second-line anti-TB medications are needed for standard regimens.
Drug-Resistant TB in Children in Colombia
Limited data from several Latin American countries reveal widely varying pediatric resistance rates (Table 7-1). Bogota, the capital of Colombia, has 8 to 10 million inhabitants. The incidence of TB is reported as 25 per 100,000 population, compared with an estimated 200 per 100,000 in Buenaventura (which is near Cali, the center of the Colombian drug trade). According to data gathered from 2001 to 2009 in Colombia, about 70 percent of children have pulmonary TB, and about a quarter have extrapulmonary TB. These pediatric patients also have a variety of TB clinical syndromes, including pulmonary, central nervous system, and lymph node diseases. Pérez-Vélez shared a current pediatric case he is treating, a 2-year-old girl with MDR TB adopted from China. The girl’s strain of TB is resistant to a total of six drugs (although her case does not qualify as XDR TB). She has disseminated TB, including pulmonary disease (bronchopneumonia, endobronchial disease, bronchiectasis), with associated massive mediastinal
|
|
|||||
| Country | Year(s) of Survey | Patients Tested | Any Resistance (%) | Isoniazid Resistance (%) | MDR (%) |
|
|
|||||
| Argentina | 2005 | N = 683 P = 136 |
10.0 25.0 |
5.7 18.4 |
2.2 15.4 |
| Colombia | 2001−2009 | N = 26 P = 3 |
20.8 0.8 |
12.0 0.8 |
3.2 0.8 |
| Paraguay | 2001 | N = 235 P = 51 |
11.1 19.6 |
6.4 11.8 |
2.1 3.9 |
| Peru | 2006 | N = 1,809 P = 360 |
23.2 41.7 |
11.6 30.3 |
5.3 23.6 |
| Uruguay | 2005 | N = 335 P = 33 |
2.1 9.1 |
1.2 6.1 |
0 6.1 |
|
|
|||||
NOTE: N = new TB cases; P = previously treated TB cases.
SOURCES: Llerena et al., 2010; Wright et al., 2009.
lympohadenopathy (complicated by external compression of the trachea), two cervical lymphadenitis lesions, Pott’s spinal disease, and severe failure to thrive. The armamentarium for treating this child is, as one would expect, quite limited, said Pérez-Vélez.
In Colombia in 2007, 593 cases of TB were reported in children below age 15, representing just 5.3 percent of the total number of cases in the country. This is a low number for an intermediate-burden country and should probably be closer to 10 percent, Pérez-Vélez noted. As a general rule, said Pérez-Vélez, 5−10 percent of the caseload in low-burden countries would be children, 10−20 percent in intermediate-burden countries, and 20–40 percent in high-burden countries, although these proportions are gross estimates based on epidemiological studies that carried out both passive and active case finding. In Buenaventura, a high-burden TB setting, the pediatric caseload was almost zero in 2006 and is now at 23 percent (personal communication, Cesar A. Moreira, TB Controller of Buenaventura). Also, about 45 percent of pediatric cases in Colombia were smear positive, which suggests a late diagnosis since children are generally paucibacillary and therefore smear negative and culture negative. This finding also suggests a dependency on smear microscopy-based, as opposed to culture-based, diagnosis, which is quite common in developing countries. In some countries, children diagnosed with TB (i.e., fulfilling the recommended WHO criteria) are not treated because of the misconception that they, like adults, require bacteriological confirmation. Pérez-Vélez suggested that a solely smear-based program is inadequate for bacteriological confirmation in children and that a strengthening of laboratory capacity (especially for mycobacterial cultures and associated drug susceptibility testing) is necessary.
Of 128 pediatric TB cases in Colombia from 2001 to 2009—although this clearly is an underreported number, said Pérez-Vélez—3 had been treated previously, and 125 were new cases. Of the new cases, 99 were drug-susceptible, 14 exhibited monoresistance, 8 exhibited polyresistance, and 4 were MDR TB. The accuracy of these results depends on having both accurate bacteriological tests and good-quality samples, Pérez-Vélez emphasized. Even in very young children (including infants), who cannot undergo the conventional specimen collection method of gastric aspiration/lavage, bacteriological confirmation (and subsequent drug susceptibility testing) can be carried out through nasopharyngeal aspiration after sputum induction. Pérez-Vélez’s research group (Grupo Tuberculosis Valle-Colorado) is evaluating the bacteriological yield of alternative specimens to the gastric aspirate, including induced sputum, as well as a highly absorbent nylon string that absorbs the sputum swallowed by the pediatric patient over many hours while asleep or awake (known as the “string test”). Pérez-Vélez also stressed the importance of reducing the time elapsed between diagnos-
ing TB in children and obtaining results of drug susceptibility testing to guide the clinician in selecting an effective regimen of anti-TB medications.
Pediatric Drug-Resistant TB in Peru
Shin stated that in pediatric populations, patterns of drug resistance are often different from those in adults because pediatric TB infections are primary (i.e., transmitted from person to person). In these cases, excess morbidity and mortality are likely due to underdiagnosis. In Peru, a study examined 38 children with a median age of 11 who had experienced an average of more than 6 months from first TB diagnosis to MDR TB treatment. Rates of adverse events were much lower than for adults, and the children tolerated treatment very well despite the use of aggressive therapy. The median number of drugs in the regimen was six, and cure rates were 94 percent.
Pediatric Drug-Resistant TB in South Africa
An estimated 1 million cases of pediatric TB occur annually worldwide, three-quarters of which are in 22 high-burden countries, said Reubenson. Since the vast majority of these cases are smear negative, this figure is likely an underestimate. Pediatric TB has traditionally been neglected, suggested Reubenson. TB in children is difficult to diagnose and confirm, and from a public health perspective, children are less likely to transmit the disease. However, there is increasing awareness of the problem.
Children are especially important in assessing drug-resistant TB through surveillance programs because they represent patients that have recently been infected and therefore reflect circulating strains and prevalent drug susceptibility patterns. Yet international data on pediatric TB are extremely limited. In unpublished 2008 data, among 140 culture-confirmed pediatric cases in two Johannesburg academic hospitals, 49 percent were infected with HIV, 14.2 percent showed resistance to isoniazid, and 8.8 percent had MDR TB. Among this latter group, 85 percent had received no previous TB treatment, none had a history of contact with an adult with MDR TB, 30 percent had a history of contact with an adult with TB, 54 percent were infected with HIV, and the mortality rate was 30 percent (with a quarter of these deaths occurring prior to confirmation of MDR TB). Notably, none of those with confirmed MDR TB had a history of an adult MDR TB contact, and 85 percent had received no previous TB treatment. “These are the things we are taught to look for when trying to diagnose pediatric MDR TB,” said Reubenson, “and they would not have been helpful in these situations.”
Reubenson said he was aware of two confirmed cases of pediatric XDR
TB in Gauteng Province, where he works. Both had undergone multiple previous courses of TB therapy, and both were HIV-infected. One died, and one has had consistently negative sputa and is, it is hoped, cured.
Each South African province has its own treatment center for MDR TB, where cases are treated predominantly as inpatients. Isolates are tested for susceptibility to the second-line drugs ethambutol, ethionamide, streptomycin, amikacin, ofloxacin, and kanamycin, but not para-aminosalycylic acid, capreomycin, pyrazinamide, terizidone, or other quinolones. This series of tests largely follows national MDR TB treatment guidelines, but the Sizwe Hospital in Guateng Province does individualize therapy according to the specific isolates. Additional drugs used occasionally include high-dose isoniazid, clarithromycin, augmentin, moxifloxacin, para-aminosalycylic acid, and capreomycin. All HIV-infected children with drug-resistant TB receive ART, irrespective of clinical or immunological staging.
Almost no data are available on outcomes, although anecdotal experience indicates that outcomes are fairly good. As Reubenson suggested, however, patients who come to the hospital have in a sense “preselected” themselves for survival, so their prognosis would be expected to be better than that for the overall cohort.
MDR TB TREATMENT FOR PEOPLE WITH DRUG AND ALCOHOL DEPENDENCIES2
According to Shin, people who abuse alcohol have a higher risk of contracting TB, having drug-resistant TB, and experiencing excess morbidity and mortality. Researchers have looked at the ethnography of alcohol abuse in different settings, the role of alcohol in causes of death, and the effect of alcohol interventions on TB and alcohol dependency outcomes. One objective of these studies has been to integrate care for alcohol dependency into TB programs so that it is a part of TB management.
Shin noted that many patients who abuse alcohol are eager for treatment, despite the stereotype that they resist assistance. For example, two-thirds of eligible patients enrolled in a study of naltrexone therapy and counseling in Tomsk, even though the researchers initially suspected that alcoholic patients might not be willing or wish to receive care. Shin elaborated that these patients generally cannot afford counseling services through the private sector and are happy for the opportunity to receive treatment for their alcohol dependency during TB treatment. She suggested that, instead of viewing this population as untreatable, treatment programs must raise
![]()
2 This section is based on the presentations of Dr. Shin and Piotr Golubchikov, Tomsk Regional Tubercular Clinic.
the level of support for these patients and become more aggressive in diagnosing and treating them.
Golubchikov presented a case study of treatment for patients with TB and alcohol dependency. Tomsk Oblast lies within the Siberian Federal District of the Russian Federation. It has a population of about 1 million living in an area of 317,000 square kilometers. The DOTS program was piloted in the Tomsk region of Russia in 1994 to treat drug-susceptible TB, and in 2000 the DOTS-Plus program was launched to treat MDR TB. Beginning in 2000, Partners In Health began working in Tomsk Oblast, and in 2004 the region received a grant from the Global Fund to Fight AIDS, Tuberculosis, and Malaria.
With financial support from Partners In Health, a cohort of patients was enlisted in MDR TB treatment from 2000 to 2002. Of 244 patients, 191 were cured, 16 failed, 12 died, and 25 defaulted. When 75 patients were enrolled in a second cohort for treatment in 2004−2005, the results were much worse (Figure 7-1). According to Golubchikov, the main reasons for the high failure and default rates in the second cohort were higher rates of alcoholism and drug addiction. This is especially unfortunate, said Golubchikov, because these patients tend to leave treatment facilities and infect others.
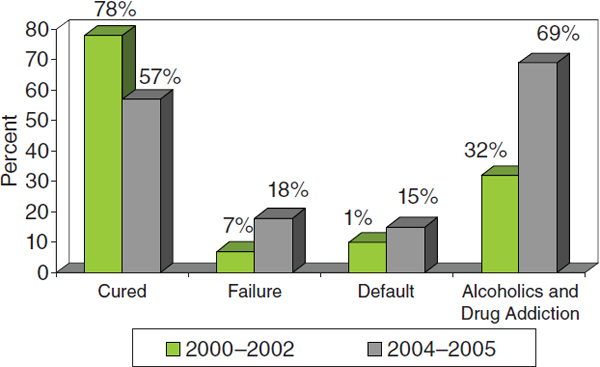
FIGURE 7-1 The 2004−2005 cohort had worse outcomes than the 2000−2002 cohort, largely because of alcoholism and drug addiction.
SOURCE: Golubchikov et al., 2010.
Golubchikov and his colleagues work mainly in the areas of alcohol harm reduction, narcotics harm reduction, social support for patients, development of patient-centered approaches, and training programs for staff and patients. All patients are tested for alcohol and drug dependence before beginning treatment.
If alcohol dependence is detected, patients receive counseling from a substance abuse professional and psychologist before they begin treatment, and this counseling is available throughout the course of therapy. The treatment program has been participating in research on the effectiveness of naltrexone to counter alcohol dependence. In addition, it provides separate counseling rooms for the substance abuse professional and the psychologist. Long-term communication with the psychologist is important to the treatment program, said Golubchikov.
For those dependent on drugs, counseling is available from a substance abuse professional and psychologist throughout the course of therapy. Outreach workers from Nasha Klinika, a nongovernmental organization, encourage intravenous drug users and MDR TB patients to receive treatment, and arrangements are made for patients to visit a drug abuse clinic to address their addiction or reduce their doses of drugs.
Patients receive a weekly distribution of food and other necessities, clothes, free travel to outpatient facilities, hot meals at local TB day-patient facilities, and the assistance of social workers for such tasks as applying for disability benefits. The development of patient-centered approaches included the expansion of day-patient facilities, with two hot meals served daily; home care for 60 patients; treatment at village health centers; and expansion of a network of volunteers in remote districts. The “Sputnik” program involves the provision of home visits for persistent or potential defaulters from TB treatment, with medical and psychological intervention and social support.
The Tomsk Oblast TB Service also has taken several administrative measures to counter MDR TB. A mobile default team visits the homes of patients who have missed their morning dose that day. A default committee consisting of a deputy head doctor, psychologist, substance abuse professional, and social worker meets to discuss patients who have missed their treatment for more than 3 days. A substance abuse professional, psychologist, and social worker conduct home visits. Improved case management and psychological support in the TB hospital have led to a decrease in early discharges of high-risk patients from inpatient clinics.
Health professionals receive training for clinical management of MDR TB, for detection and treatment of side effects, and for working with patients with alcohol and drug dependencies. Patients undergo their own health training, receive talks on TB, and have access to the management staff of TB facilities. Specialists from Alcoholics Anonymous and the Rus-
sian Orthodox Church are involved in the program to support TB patients. Also, patients who have successfully completed TB treatment programs talk with current patients.
These efforts have had a dramatic effect on the outcomes of MDR TB patients, said Golubchikov. In 2005, the year after the Global Fund grant was launched in Tomsk, defaults among civilian patients in the DOTS-Plus program dropped from 28.8 percent to 13.9 percent, and this percentage has continued to fall since then (Figure 7-2). The percentage of MDR TB among new bacteriologically proven cases of pulmonary TB investigated for drug susceptibility has fallen from a high of 16.8 percent earlier in the decade to slightly more than 13 percent. The level of XDR TB among all positive susceptibility tests has fallen from a high of 3.5 percent in 2006 to about 2.5 percent currently. TB mortality has declined more in Tomsk Oblast than in the Siberian Federal District and the Russian Federation (Figure 7-3). And the estimated reservoir of infectious MDR TB cases among the civilian sector has fallen from a high of more than 800 people in 2002 to fewer than 400 in 2009.
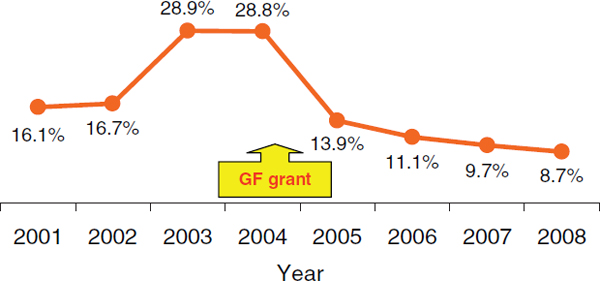
FIGURE 7-2 Default percentages among MDR TB patients dropped substantially after initiation of the DOTS-Plus program through a Global Fund grant.
SOURCE: Golubchikov et al., 2010.
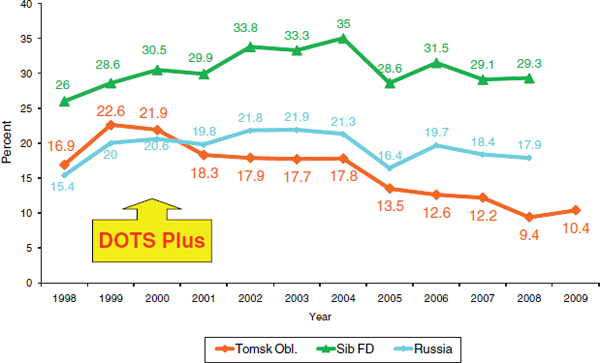
FIGURE 7-3 TB mortality in Tomsk Oblast has fallen at a greater rate than in the Siberian Federal District or the Russian Federation.
SOURCE: Golubchikov et al., 2010.
TB IN THE PRISON SYSTEM OF THE RUSSIAN FEDERATION3
Safonova reported that the number of active TB patients in Russia’s penal institutions has fallen by more than half over the past decade (Figure 7-4). Even greater reductions have occurred in TB incidence and mortality in Russia’s penal institutions. This decrease is due in part to shorter prison sentences following changes in criminal law, but it is also due to programs designed to detect and treat TB in the prison system. Financing from the Global Fund and The World Bank were used in part to create a laboratory network in the prison system, and 90 laboratories have been established. Drug sensitivity testing has allowed the detection of MDR TB cases followed by the introduction of second-line drugs. As a result, said Safonova, diagnostics are now quite good, with coverage rates of more than 97 percent, and prisons in 70 territories are now covered by second-line treatment.
During this same period, the number of HIV-infected patients in Russia’s penal institutions has increased, as has the number of prisoners coinfected with HIV and M.tb. (Figure 7-5). The number of drug-resistant and MDR TB patients in Russia’s penal institutions also has risen. In 2009, 54.4
![]()
3 This section is based on the presentation of Svetlana Safonova, Russia’s Federal Correction Service.
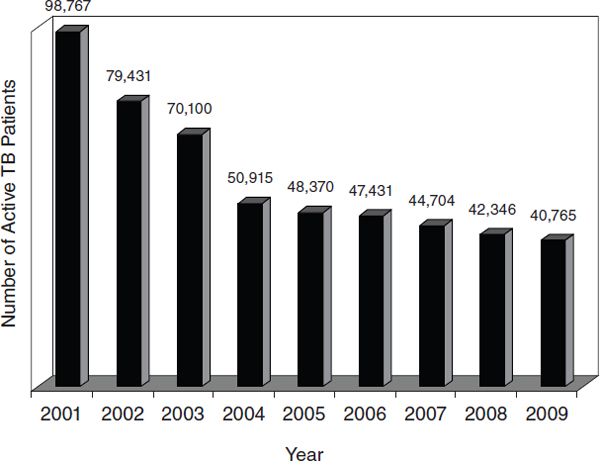
FIGURE 7-4 The number of active TB patients in Russia’s penal institutions has declined over the past decade.
SOURCE: Safonova, 2010.
percent of patients exhibited drug resistance, and 21.9 percent had MDR TB. Among relapse TB patients, these percentages were much higher—82.9 and 49.9 percent, respectively. Among those TB patients in Russia’s penal institutions that excreted M.tb., 2.5 percent of new cases and 7.2 percent of relapse cases in 2009 were XDR TB.
Many new cases of TB are discovered only in penal institutions, meaning that the patients would not have known they were infected with TB if they had not been incarcerated. Of all new TB cases appearing in Russia, only 12 percent appear in penal institutions. About 90 percent of those TB patients diagnosed in penitentiaries did not know about their infection prior to arrest.
About 68 percent of these cases are occupants of urban areas, and only about 2 percent are homeless, contrary to a common stereotype, said Safonova. Among these new cases, 76 percent are aged 20−29, and the majority are employed. About 80 percent are unmarried, and 41 percent of those sick were convicted for the first time.
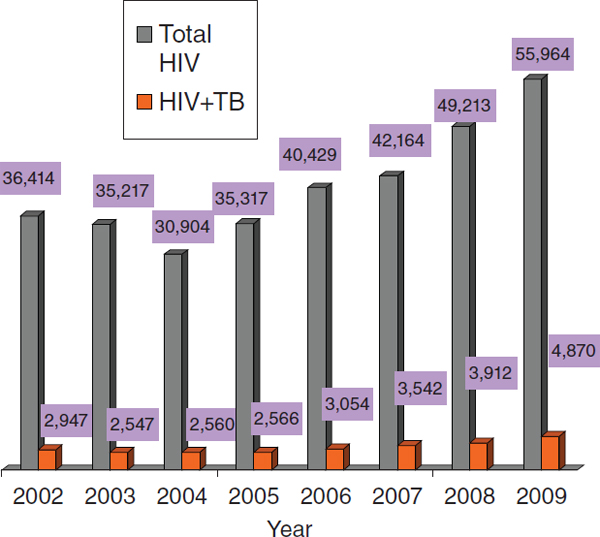
FIGURE 7-5 The number of patients infected with HIV and coinfected with HIV and M.tb. in Russia’s penal institutions has risen since 2004.
SOURCE: Safonova, 2010.
The Russian penitentiary service has several priorities, said Safonova:
- early diagnosis of TB through x-ray and microbiological investigation,
- continued development of the prison service’s laboratories and bacteriological investigation of all categories of TB patients,
- internal and external quality control of laboratories,
- continued development of the expertise of medical staff and provision of training, and
- continuing international cooperation.












