While the connections between oral health and overall health and well-being have been long established, oral health care and general health care are provided in almost entirely separate systems. Oral health is separated from overall health in terms of education and training, financing, workforce, service delivery, accreditation, and licensure. In the United States, medical and dental education and practice have been separated since the establishment of the first dental school in Baltimore in 1840 (University of Maryland, 2010). The financing of oral health care is characterized by a similar divide. For example, private health plans typically do not cover oral health care, and the benefits package for Medicare excludes oral health care almost entirely. These separations contribute to obstacles that impede the coordination of care for patients.
This chapter provides an overview of the oral health care system in America today—where services are provided, how those services are paid for, who delivers the services, how the workforce is educated and trained to provide these services, and how the workforce is regulated. The role of the U.S. Department of Health and Human Services (HHS) in oral health education and training, as well as in supporting the delivery of oral health care services, will be addressed in Chapter 4 of this report. Detailed examination of the role HHS plays in overseeing safety net providers such as Federally Qualified Health Centers (FQHCs1) was charged to the concurrent Institute of Medicine (IOM) Committee on Oral Health Access to
![]()
1 A Federally Qualified Health Center (FQHC) is any health center that receives a grant established by section 330 of the Public Health Service Act (42 U.S.C. §254b).
Services. Therefore, this committee limited its examination of the safety net in this current report.
The current oral health care system is composed of two basic parts—the private delivery system and the safety net—and there is little integration of either sector with wider health care services. The two systems function almost completely separately; they use different financing systems, serve different clientele, and provide care in different settings. In the private delivery system, care is usually provided in small, private dental offices and financed primarily through employer-based or privately purchased dental plans and out-of-pocket payments. This model of care has remained relatively unchanged throughout the history of dentistry. The safety net, in contrast, is made up of a diverse and fragmented group of providers who are financed primarily through Medicaid and the Children’s Health Insurance Program (CHIP), other government programs, private grants, as well as out-of-pocket payments.
In addition, some oral health care, especially for young children, has begun to be supplied by nondental providers in settings such as physicians’ offices, which is discussed later in this chapter. This section gives a brief overview of the basic settings of oral health care by dental professionals—namely, dentists, dental hygienists, and dental assistants. The professionals themselves will be discussed later in this chapter.
The Private Practice Model
The structure of private practice provides dentists with considerable autonomy in their practice decisions (Wendling, 2010). Private practices tend to be located in areas that have the population to support them; thus, there are more practices located in urban areas than in rural, and more practices in high-income than in low-income areas (ADA, 2009b; Solomon, 2007; Wall and Brown, 2007). About 92 percent of professionally active dentists work in the private practice model (ADA, 2009d) (see Box 3-1 for definitions of types of dentists). Among all active private practice dentists (whose primary occupation was private practice), about 84 percent are independent dentists, 13 percent are employed dentists, and 3 percent are independent contractors (ADA, 2009d). About 60 percent of private practice dentists are solo dentists (Wendling, 2010). In addition, 80 percent of all active private practitioners and 83 percent of new active private practitioners are in general practice, while the remainder work in one of many specialty areas (see Table 3-1).
Dentists in the private practice setting see a variety of patients. The
BOX 3-1
Types of Dentists
A professionally active dentist is primarily or secondarily occupied in a private practice, dental school faculty/staff, armed forces, or other federal service (e.g., Veterans Administration, U.S. Public Health Service); or is a state or local government employee, hospital staff dentist, graduate student/intern/resident, or other health/dental organization staff member.
An active private practitioner is someone whose primary and/or secondary occupation is private practice.
A new dentist is anyone who has graduated from dental school within the last 10 years.
An independent dentist is a dentist running a sole proprietorship or one who is involved in a partnership.
A solo dentist is an independent dentist working alone in the practice he or she owns.
A nonowner dentist does not share in ownership of the practice.
An employed dentist works on a salary, commission, percentage, or associate basis.
An independent contractor contracts with owner(s) for use of space and equipment.
A nonsolo dentist works with at least one other dentist and can be an independent or nonowner dentist.
NOTE: Each of these types can be either general or specialty practitioners.
SOURCES: ADA, 2009b,d.
patients of independent general practitioners are spread relatively evenly across the age spectrum and equally divided by gender (ADA, 2009b). About two-thirds (63 percent) of their patients have private insurance; only about 7 percent receive publicly supported dental coverage, and the remaining 30 percent are not covered by any dental insurance (ADA, 2009b). Similarly, independent dentists’ billings primarily are from private insurance and direct patient payments (44 percent and 39 percent, respectively) (ADA, 2009c). Nearly two-thirds of independent dentists (63 percent) and slightly more than half of new independent dentists (58 percent) do not have any patients in their practices covered by public sources (ADA, 2009b). However, in 2006, Bailit and colleagues estimated that 60 to 70 percent of underserved individuals who get care do so in the private care system (Bailit et al., 2006). While there is some disagreement as to whether dentists who care for patients with public coverage are considered part of
TABLE 3-1
Percentage Distribution of Active Private Practitioners by Practice, Research, or Administration Area, 2007
| Practice, Research, or Administration Area | All Active Private Practitioners | New Active Private Practitioners |
| General practice | 80.1 | 83.3 |
| Orthodontics and dentofacial orthopedics | 5.7 | 4.7 |
| Oral and maxillofacial surgery | 3.7 | 1.9 |
| Periodontics | 2.8 | 1.7 |
| Pediatric dentistry | 3.0 | 4.4 |
| Endodontics | 2.6 | 2.6 |
| Prosthodontics | 1.6 | 0.8 |
| Public health dentistry | 0.3 | 0.4 |
| Oral and maxillofacial pathology | 0.1 | 0.1 |
| Oral and maxillofacial radiology | 0.0 | 0.0 |
| Missing specialty area | 0.1 | 0.1 |
SOURCE: ADA, 2009d.
the safety net, opportunities to expand care for vulnerable and underserved populations in private settings cannot be overlooked.
The Oral Health Safety Net
Some segments of the American population, namely socioeconomically disadvantaged groups, have difficulty accessing the private dental system due to geographic, financial, or other access barriers and must rely on the dental safety net (if they are seeking care) (Bailit et al., 2006; Brown, 2005; Wendling, 2010). While the term safety net may give the impression of an organized group of providers, the dental safety net comprises a group of unrelated entities that both individually and collectively have very limited capacity (Bailit et al., 2006; Edelstein, 2010a). One estimate of the current capacity of the safety net suggests that 7 to 8 million people may be served in these settings annually, and approximately another 2.5 million could be served with improved efficiency (Bailit et al., 2006). However, the safety net as it exists simply does not have the capacity to serve all of the people in need of care, which is estimated to be as high as 80 to 100 million individu-
als (Bailit et al., 2006; HHS, 2000). While there is a perception that the care provided in safety net settings is somehow inferior to the care provided in the private practice setting, there are no data to support this assumption. In fact, there are very little data regarding the quality of oral health care provided in any setting (see later in this chapter for more on quality assessment in the oral health care system).
Common types of safety net providers include FQHCs, FQHC look-alikes,2 non-FQHC community health centers, dental schools, school-based clinics, state and local health departments, and community hospitals. Each type of provider offers some type of oral health care, but the extent of the services provided and the number of patients served varies widely and the safety net cannot care for everyone who needs it (Bailit et al., 2006; Edelstein, 2010a). Private sector efforts to supplement the safety net include the organization of single-day events to provide free dental care. In 2003, the ADA established the annual Give Kids a Smile Day; in 2011, the ADA estimated the event would involve about 45,000 volunteers providing care to nearly 400,000 children (ADA, 2011a). Another example includes the Missions of Mercy, which are often organized by state dental societies or private foundations. At these events, thousands of individuals have waited in lines for hours to receive care (Dickinson, 2010). These types of single-day events provide temporary relief to the access problem for some people, but they do not provide a regular source of care for people in need.
Multiple challenges exist in the financing of oral health care in the United States, including state budget crises, the relative lack of dental coverage, a payment system (like in general health care) that rewards treatment procedures rather than health promotion and disease prevention, and the high cost of dental services. Expenditures for dental services in the United States in 2009 were $102.2 billion, less than 5 percent of total spending on health care, a proportion that has remained fairly constant for the last two decades (CMS, 2011c).
Demand for dental care may vary with the economic climate of the country (Guay, 2005; Wendling, 2010). For example, the recent recession was identified as a key factor contributing to 2009 having the slowest rate of growth in health spending (4 percent) in the last 50 years (Martin et al., 2011). Notably, expenditures on dental services had a negative rate of
![]()
2 FQHC look-alikes must meet all of the statutory requirements of FQHCs, but they do not receive grant funding under section 330 and are eligible for many, but not all, of the benefits extended to FQHCs.
growth (–0.1 percent) in 2009, down from a positive rate of growth of 5.1 percent in 2008.
Typical sources of health care insurance—Medicare, Medicaid, CHIP, and employers of all sizes—often do not include dental coverage, especially for adults. Employment status of adults ages 51–64 is a strong predictor of dental coverage (Manski et al., 2010c), and “routine dental care” is specifically excluded from the traditional Medicare benefits package. High-income older adults are more likely to have dental coverage than are other older adults (Manski et al., 2010c). In any case, individuals with dental coverage often incur high out-of-pocket costs for oral health care (Bailit and Beazoglou, 2008). Estimates regarding the severity of uninsurance for dental care include the following:
• In 2000, the surgeon general’s report estimated that 108 million people (about 35 percent of the population) lacked dental coverage (HHS, 2000).
• A recent estimate based on enrollment in private dental plans found 130 million U.S. adults and children lack dental coverage (NADP, 2009).
• In 2004, 34 percent of adults ages 21–64 and about 70 percent of adults ages 65 and older lacked dental coverage (Manski and Brown, 2007).
• Nearly 25 percent of people who have private health insurance lack dental coverage (Bloom and Cohen, 2010).
Overall, rates of uninsurance for oral health care are almost three times the rates of uninsurance for medical care—34.6 percent (Manski and Brown, 2007) versus 14.7 percent (CDC, 2009).
Financing of oral health care greatly influences where and whether individuals receive care. For example, the national Medical Expenditure Panel Survey (MEPS) data show that in 2004, 57 percent of individuals with private dental coverage had at least one dental visit, compared to 32 percent of those with public dental coverage and 27 percent of uninsured individuals (Manski and Brown, 2007). At the individual level, insurance coverage and socioeconomic factors play a significant role in access to oral health care (Flores and Tomany-Korman, 2008; GAO, 2008; Isong et al., 2010; Liu et al., 2007). Financing also has an effect on providers’ practice patterns, in part due to the low reimbursement rates of public insurers. Previous studies have shown that like in medicine, dentists’ practice patterns are associated with financial incentives (Atchison and Schoen, 1990; Naegele et al., 2010; Porter et al., 1999). The following sections give a general overview of how care is financed in the United States.
Private Sources
As shown in Table 3-2, dental care is financed primarily through private sources, including individual out-of-pocket payments and private dental plans.
In 2008, dental services accounted for 22 percent of all out-of-pocket health care expenditures, ranking second only to prescription drug expenditures (see Figure 3-1).
Employers can add a separate oral health product to their overall coverage package, but often they do not. In 2006, 56 percent of all employers offered health insurance, but only 35 percent offered dental insurance (Manski and Cooper, 2010). The availability of dental coverage through one’s employer is associated with the size of the establishment; that is, the larger the number of employees overall, the higher the incidence of stand-alone dental plans available to employees (Barsky, 2004; Ford, 2009). Higher-paid workers are also more likely to have access to and participate in stand-alone dental plans (Barsky, 2004; Ford, 2009). Employees are more likely to be offered access to medical insurance than dental insurance, and a higher percentage of employees will take advantage of available dental benefits as compared with the percentage of employees who take advantage of available medical benefits (BLS, 2010b).
TABLE 3-2
National Health Expenditures by Type of Expenditure and Source of Funds, 2009
| Type of Expenditure | Total Spending (billions) | Percentage from Out-of-Pocket Payments (%) | Percentage from Private Insurance (%) | Percentage from Public Insurance (%) |
| Dental services | 102.2 | 41.6 | 48.9 | 9.1 |
| Physician and clinical services | 505.9 | 9.5 | 47.0 | 33.5 |
| Home health care | 68.3 | 8.8 | 7.4 | 80.2 |
| Nursing and continuing care | 137.0 | 29.1 | 7.7 | 56.2 |
| Prescription drugs | 249.9 | 21.2 | 43.4 | 33.9 |
| Hospital care | 759.1 | 3.2 | 35.0 | 53.2 |
NOTES: Public insurance includes Medicare, Medicaid, CHIP, the Department of Defense, and the Department of Veterans’ Affairs. Totals do not reach 100% as some expenditures were attributed to “Other Third Party Payers and Programs.”
SOURCE: CMS, 2011b.
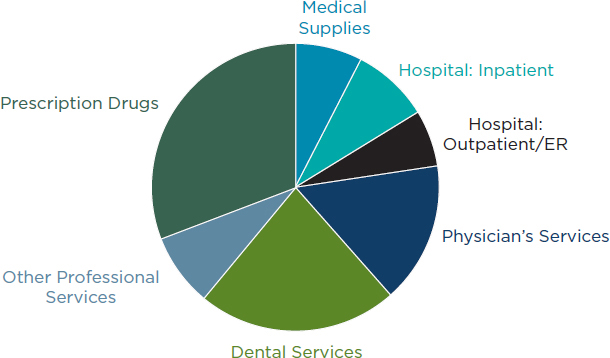
FIGURE 3-1
Out-of-pocket health care expenditures, 2008.
SOURCE: BLS, 2010a.
Public Sources
Of the $102.2 billion in dental expenditures, nearly 91 percent came from private funds (e.g., private insurance and out-of-pocket payments), and only 9 percent came from public funds (e.g., state and federal funds) (CMS, 2011b). In comparison, public funds account for about one-third of physician and clinical services (see Table 3-2). However, the reported national expenditure levels likely undercount the total public funds spent on improving oral health, because that total represents only the costs associated with direct services delivered by dentists (to the exclusion of the broader definition of oral health) and does not account for care provided in settings such as hospitals and nursing homes. While a much lower percentage of funds for dental services come from public sources as compared to the funding of many other services, the government may, in fact, have a very important role to play for those who cannot afford to pay for care.
Public sources are an important source of coverage for many vulnerable and underserved populations, but a recent report from the U.S. Government Accountability Office (GAO) found that finding providers to care for Medicaid populations “remains a challenge” (GAO, 2010). Low reimbursement by public programs is often cited as a disincentive for providers’ to participate in publicly funded programs (Damiano et al., 1990; GAO, 2000; Lang and Weintraub, 1986; McKnight-Hanes et al., 1992; Venezie et al., 1997). Studies have shown, though, that in order to significantly increase participation rates, increased reimbursement is necessary but often
requires additional efforts such as decreasing the administrative burdens of participation; changing provider perceptions of participating; and fostering relationships among state Medicaid staff, the state dental association, and local dentists (Borchgrevink et al., 2008; GAO, 2000; Greenberg et al., 2008; Wysen et al., 2004).
Medicaid and CHIP
Dental coverage is required for all Medicaid-enrolled children under age 21 (CMS, 2011a). This is a comprehensive benefit, including preventive, diagnostic, and treatment services. According to data from the Kaiser Family Foundation, Medicaid provides health care coverage to nearly 30 million children while CHIP covers an additional 6 million (KFF, 2011). Further, they note that together, Medicaid and CHIP provide health care coverage for one-third of children and over half (59 percent) of low-income children. However, exact documentation of these numbers may be challenging due to how enrollees are counted (e.g., at a point in time versus at any time in a given period).
Regarding the Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Program, by law,3 states must cover any Medicaid-covered service that would reasonably be considered medically necessary to prevent, correct, or ameliorate children’s physical (including oral) and mental conditions. In contrast, Medicaid dental benefits are not required for adults, and even among those states that offer dental coverage for adult Medicaid recipients, the benefits are often limited to emergency care (ASTDD, 2011c). In FY2008, Medicaid spending on dental services accounted for 1.3 percent of all Medicaid payments (CMS, 2010b).
CHIP is a federally funded grant program that provides resources to states to expand health coverage to uninsured, low-income children. Millions of children have received coverage for medical care, and a portion of those have also been covered for dental care (Brach et al., 2003). The Children’s Health Insurance Program Reauthorization Act (CHIPRA)4 enacted in February 2009 requires all states to provide dental coverage to children (but not including their parents) covered under CHIP.
Medicare
As increasing numbers of baby boomers become eligible for Medicare, considerable attention is being paid to how these aging adults will pay for
![]()
3 42 U.S.C. §1396d(r)(3).
4 Children’s Health Insurance Program Reauthorization Act of 2009, Public Law 3, 111th Cong., 1st sess. (February 4, 2009).
and obtain oral health care (Ferguson et al., 2010; Manski et al., 2010a,b,c; Moeller et al., 2010). In the year 2000, almost 77 percent of dental care for older adults was paid by out-of-pocket expenditures, and 0.4 percent was covered by Medicaid (Brown and Manski, 2004). Medicare explicitly excludes coverage for routine dental care, specifically “for services in connection with the care, treatment, filling, removal, or replacement of teeth or structures directly supporting the teeth.”5
In the initial Medicare program, “routine” physical checkups and routine foot care were excluded; comparatively, all dental services were excluded, not just “routine” dental services (CMS, 2010a). In 1980, Congress made an exception for “inpatient hospital services when the dental procedure itself made hospitalization necessary” (CMS, 2010a). Box 3-2 delineates the extent of the exclusion of oral health care from the Medicare program.
Federal Systems of Care
In addition to the public programs noted above, the federal government both directly provides and pays for the oral health care of several distinct segments of the U.S. population. This includes care provided both in public and private settings through the various branches of the military, the Bureau of Prisons, the Department of Homeland Security, and the Veterans Administration. The role of the federal government in providing care is discussed more fully in Chapter 4.
Impact of Health Care Reform
Between now and 2014, several provisions of the Patient Protection and Affordable Care Act (ACA)6 will affect dental coverage. For example, provisions address coverage of oral health services for children and the expansion of Medicaid eligibility. Table 4-4 in Chapter 4 highlights some of the key provisions that will affect dental coverage.
Traditionally, a combination of dentists, dental hygienists, and dental assistants directly provide oral health care. Dental laboratory technicians create bridges, dentures, and other dental prosthetics. In addition, new and evolving types of dental professionals (e.g., dental therapists) are being pro-
![]()
5 Social Security Act, §1862(a)(12).
6 Patient Protection and Affordable Care Act, Public Law 148, 111th Cong., 2nd sess. (March 23, 2010).
BOX 3-2
Exclusions (and Exceptions) to
Dental Coverage Under Medicare
Services Excluded Under Part B
A primary service (regardless of cause or complexity) provided for the care, treatment, removal, or replacement of teeth or structures directly supporting teeth (e.g., preparation of the mouth for dentures, removal of diseased teeth in an infected jaw).
A secondary service that is related to the teeth or structures directly supporting the teeth unless it is incident to and an integral part of a covered primary service that is necessary to treat a nondental condition (e.g., tumor removal) and it is performed at the same time as the covered primary service and by the same physician/dentist. In those cases in which these requirements are met and the secondary services are covered, Medicare does not make payment for the cost of dental appliances, such as dentures, even though the covered service resulted in the need for the teeth to be replaced, the cost of preparing the mouth for dentures, or the cost of directly repairing teeth or structures directly supporting teeth (e.g., alveolar process).
Exceptions to Services Excluded
Exceptions include the extraction of teeth to prepare the jaw for radiation treatment of neoplastic disease, as well as an oral or dental examination performed on an inpatient basis as part of comprehensive workup prior to renal transplant surgery or performed in a rural health clinic/FQHC prior to a heart valve replacement.
SOURCE: CMS, 2010a.
posed and, in some instances, used to provide some oral health care. The extent to which all of these professionals interact can vary greatly.
The surgeon general’s 2000 report expressed concerns about
a declining dentist-to population ratio, an inequitable distribution of oral health care professionals, a low number of underrepresented minorities applying to dental school, the effects of the costs of dental education and graduation debt on decisions to pursue a career in dentistry, the type and location of practice upon graduation, current and expected shortages in personnel for dental school faculties and oral health research, and an evolving curriculum with an ever-expanding knowledge base. (HHS, 2000)
Unfortunately, these concerns continue today.
The following section will focus on the traditional dental workforce in terms of its demographic profile, basic education and training, and racial
and ethnic diversity, as well as the role of new and emerging members of the dental team. Later sections in this chapter will describe the roles and skills of other types of health care professionals (e.g., nurses, physicians) in the provision of oral health care.
Basic Demographics
The adequacy of the current supply of oral health professionals, both in terms of its numbers and skills, is difficult to assess for a variety of reasons related to changes in employment status, differing measures (e.g., licensed vs. active professionals), the holding of more than one position per worker, part-time employment, and the presence of multiple job titles. Predicting the need for specific types of practitioners is always difficult because many factors can affect the need and demand for oral health care (Brown, 2005; Guthrie et al., 2009). For example, improvements in oral health of the population might limit future demand for restorative care.
While it is debatable whether the number of professionals is adequate, it is more certain that the oral health workforce is not well distributed, with distinct areas showing significant needs (Hart-Hester and Thomas, 2003; Mertz and Grumbach, 2001; Saman et al., 2010). Even with a sufficient supply, geographic maldistribution could still persist (Wall and Brown, 2007). For example, even with financial incentives such as loan repayment, dentists willing to locate in rural areas might be unable to sustain a practice in these locations (Allison and Manski, 2007). More attention may be needed to where students are recruited from, as 57 percent of graduates report plans to return to work in their home states after graduation (Okwuje et al., 2010).
Job growth during the next decade is projected to be above average for all the dental professions, particularly for dental hygienists and dental assistants (see Table 3-3). In fact, dental hygienists rank twelfth on the list of the fastest-growing occupations (of all occupations) and fifth among occupations directly related to health care (see Table 3-4). Dental assistants rank fourteenth on the list of the fastest-growing occupations and sixth among occupations directly related to health care.
Dentists
Estimates of the number of dentists in the workforce vary significantly, likely due to how they are counted. As shown in Table 3-3, the Bureau of Labor Statistics (BLS) estimates that dentists held approximately 141,900 jobs in 2008, 85 percent of which were in general dentistry. However, in 2007, the American Dental Association (ADA) estimated that there were 181,725 professionally active dentists; 79 percent were general dentists
TABLE 3-3
Employment of Dental Occupations, 2008 and Projected 2018
| Occupation | Number of Jobs | Percent Increase In Growth (%) | |
| 2008 | 2018 | ||
| Dentists | 141,900 | 164,000 | 16 |
| General dentists | 120,200 | 138,600 | 15 |
| Dental hygienists | 174,100 | 237,000 | 36 |
| Dental assistants | 295,300 | 400,900 | 36 |
| Dental laboratory technicians | 46,000 | 52,400 | 14 |
aThe Bureau of Labor Statistics calculates replacement needs based on estimates of job openings due to retirement or other reasons for permanently leaving an occupation.
bTotal job openings represent new positions due to both growth and replacement needs. Totals may not add precisely due to rounding.
SOURCES: BLS, 2010d,e,f,g.
(ADA, 2009d). The dentist-to-population ratio has remained relatively constant for nearly 20 years (about 60 dentists per 100,000 population) and is expected to decline in the coming decades (Wendling, 2010).
Among independent dentists in private practice, 43 percent are age 55 or older (ADA, 2009b). Like many other health care professions, concerns arise about replacement needs as these individuals retire. While most dentists are male, the proportion of female dentists is on the rise owing to the increased proportion of female dentists among younger dentists (see Figure 3-2). However, while dentistry is becoming increasingly gender diverse, the racial and ethnic profile of dentists has shown little change (see later in this section for a discussion of the racial and ethnic diversity of dental professions). Dentists’ income can vary depending on the type of employment, ranging from an average total net income of about $114,000 for new employed dentists to over $350,000 for independent specialists (ADA, 2009c).
As discussed previously, professionally active dentists overwhelmingly work in the private practice setting (92 percent). Among the remaining dentists, occupations include7
![]()
7 Does not total 100 percent due to rounding.
• Dental school faculty/staff member (1.7 percent),
• Armed forces (0.9 percent),
• Graduate student/intern/resident (1.3 percent),
• Hospital staff dentist (0.4 percent),
• State or local government employee (0.8 percent),
• Other federal service (0.8 percent), and
• Other health/dental organization staff (1.0 percent) (ADA, 2009d).
Among 2009 dental school graduates, 48 percent planned to enter private practice immediately, while 30 percent planned to go on to advanced education (e.g., residency), 11 percent planned to go into some form of government service, and less that one-half of 1 percent planned to enter teaching, research, or administration; the remainder were “other/undecided” (Okwuje et al., 2010).
TABLE 3-4
Top 15 Fastest-Growing Occupations, 2008 and Projected 2018
| Occupation | Percent Change, 2008–2018 |
| Biomedical engineers | 72.0 |
| Network systems and data communications analysts | 53.4 |
| Home health aides | 50.0 |
| Personal and home care aides | 46.0 |
| Financial examiners | 41.2 |
| Medical scientists, except epidemiologists | 40.4 |
| Physician assistants | 39.0 |
| Skin care specialists | 37.9 |
| Biochemists and biophysicists | 37.4 |
| Athletic trainers | 37.0 |
| Physical therapist aides | 36.3 |
| Dental hygienists | 36.1 |
| Veterinary technologists and technicians | 35.8 |
| Dental assistants | 35.8 |
| Computer software engineers, applications | 34.0 |
SOURCE: BLS, 2010c.
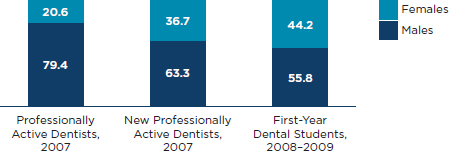
FIGURE 3-2
Percentage distribution of dentists by gender.
SOURCES: ADA, 2009d, 2010a.
Dental Hygienists
The dental hygiene profession began almost a century ago when a dentist trained his assistant to assist in preventive dental services (University of Bridgeport, 1998). Since then, dental hygiene has evolved to a licensed health care profession; dental hygienists, in concert with dentists, provide “preventive, educational, and therapeutic services supporting total health for the control of oral diseases and the promotion of oral health” (ADHA, 2010). In private dental practice, dental hygienists’ work is generally billed under the dentist’s provider number.
Dental hygienists are virtually all female (99 percent) (ADHA, 2009b). This is not changing dramatically: in 2008, only 2.8 percent of graduates of dental hygiene programs were male (ADA, 2009a). The mean age of dental hygienists is about 44 years of age (ADHA, 2009b), which, like dentists, may lend to concerns about the numbers nearing retirement. Dental hygienists are primarily employed in private dental practices but may also work in educational institutions and in public health settings such as school-based clinics, prisons, long-term care, and other institutional care facilities (ADHA, 2009b). In 2008, dental hygienists held about 174,100 jobs, with a median annual wage of about $66,500 (BLS, 2010e).8 Nearly 30 percent of dental hygienists do not receive any benefits (ADHA, 2009b).
In spite of BLS projections for a 36 percent growth in the employment of dental hygienists between 2008 and 2018 (see Table 3-4), the dental hygiene workforce may also be experiencing challenges due to geographic maldistribution. For example, a 2009 survey of dental hygienists showed that 68 percent of respondents reported finding employment was somewhat or very difficult in their geographic area (up from 31 percent in 2007), and
![]()
8 Because dental hygienists may hold more than one job, this is an overestimate of the number of practicing dental hygienists.
of these, 80 percent felt that there were too many hygienists living in the area (ADHA, 2009a,b).
Dental Assistants
Dental assistants primarily work in a clinical capacity, but other roles include administrative positions, practice management, and education (McDonough, 2007). Most dental assistants work in private practices and as assistants to general dentists, but many dental assistants work in specialty practices. Across the country, there are different job titles and categories for dental assistants in different states (ADAA/DANB Alliance, 2005). The BLS estimates that dental assistants held 295,000 jobs in 2008, with a median annual wage of about $32,000 (BLS, 2010d). Like dental hygienists, dental assistants are nearly all female (McDonough, 2007). Expanded function dental assistants (EFDAs) may perform some limited restorative functions under the supervision of a dentist (Skillman et al., 2010). Both the U.S. Army Dental Command and the Indian Health Service have programs to train and employ EFDAs (IHS, 2011; Luciano et al., 2006). While the title of EFDA is commonly used to describe all dental assistants who can perform extended duties, there are many other titles given to dental assistants with expanded duties (e.g., expanded duties dental assistant, advanced dental assistant, registered restorative assistant in extended functions), and many states permit dental assistants to perform specific extended functions (e.g., coronal polishing, administration or monitoring of sedation, pit and fissure sealants) (DANB, 2007). In fact, some states permit certified dental assistants to act at the level of an EFDA, even though titles such as certified dental assistant or registered dental assistant are used (DANB, 2007). As stated by the Dental Assistant National Board, “without a single, nationally-accepted set of guidelines that govern the practice of dental assisting in the country, it is difficult to execute a concise overview” of the profession (DANB, 2007).
Dental Laboratory Technicians
In 2008, dental laboratory technicians (or “dental technicians”) held about 46,000 jobs in 2008 with a median annual wage of about $34,000 (BLS, 2010g). Dental technicians work in a variety of settings, including dentists’ offices, their own private businesses, or small privately owned offices. Among all students enrolled during the 2008–2009 academic year, 40 percent were age 23 and younger and slightly more than half were female (ADA, 2009a).
Education and Training
Prior to the 20th century, dental and allied dental education occurred through apprenticeships and training in proprietary schools (Haden et al., 2001). The education of dental professionals evolved and formalized over time to take place in a variety of locations, including dental schools, 4-year colleges and universities, community colleges, and technical schools. The ADA’s Commission on Dental Accreditation (CODA) accredits predoctoral dental education programs; programs for dental hygienists, dental assistants, and dental laboratory technicians; and advanced dental educational programs (i.e., residencies) (Department of Education, 2010). While the number of programs is increasing, faculty recruitment, especially for dental schools and dental hygiene programs, is a persistent problem; this is often due to low salary (ADHA, 2006; Chmar et al., 2008; Walker et al., 2008). In addition, several efforts have emphasized the need to revise the way that dental students are educated and trained, including the need to provide care in a more patient-centered fashion, as well as for students to gain more clinical experiences in the community setting (Cohen et al., 1985; Formicola et al., 1999, 2006; HHS, 2010; IOM, 1995; Lamster et al., 2008). More effort is also needed to improve the health literacy and cultural competency of students.
The sections below provide some highlights as to the overall education and training of the dental professions. Chapter 4 provides more information on the role of HHS in education and training.
Dentists
U.S. dental schools typically offer a 4-year curriculum; students take 2 years of predominantly basic science classes followed by 2 years of predominantly clinical experience, after which they are awarded either a Doctor of Dental Medicine (DMD), or a Doctor of Dental Surgery (DDS). The number of dental schools in the United States is increasing, and more dentists are being produced. In 2009, there were 57 dental schools, of which 37 were public, 16 were private, and 4 were private, state-related institutions (ADA, 2010a). At that time, 8 new dental schools were in various stages of development (Guthrie et al., 2009). About 4,800 dentists graduate each year (ADA, 2010a). In 1999, there were 55 dental schools that graduated about 4,100 dentists annually (ADA, 2010a.)
The cost of dental education is a barrier to entry, especially for low-income and underrepresented minority students (IOM, 2004; Sullivan Commission, 2004; Walker et al., 2008). In 2008–2009, the average annual tuition for dental schools was $27,961 for state residents and $41,561 for nonresidents, similar to the tuition for medical students (AAMC, 2011;
ADA, 2010a); the difference is significant considering that many states do not have a single dental school. As this problem exists for several professions, the Western Interstate Commission for Higher Education created the Professional Student Exchange Program in which students from certain states may receive assistance to attend health professional schools (including dental schools) in other states (WICHE, 2011). There is also great variation between public and private institutions.
In 2009, average dental education debt was $164,000, and 77 percent of graduates had at least $100,000 in debt (Okwuje et al., 2010). Comparatively, the average educational debt for medical school graduates in 2009 was approximately $156,000, and 79 percent of graduates had at least $100,000 in debt (AMA, 2011). Debt among dental graduates varies widely; those with higher levels of debt are more likely to enter private practice immediately upon graduation and less likely to pursue advanced education as compared to those with no debt (Okwuje et al., 2010).
Dentists have the option of postgraduate education that provides further training in general dentistry or one of the nine recognized specialty areas. In 2008–2009, there were 723 specialty and postdoctoral general dentistry programs in the United States, including dental residencies and fellowship programs (ADA, 2010b). Currently, about 30 percent of graduating dental students plan to pursue postgraduate training (Okwuje et al., 2010). In the 2008–2009 academic year, there were nearly more than 44,500 applications9 for residency programs slots and about 3,000 first-year enrollees (ADA, 2010b).
Dental Hygienists
In the 2008–2009 academic year, there were 301 dental hygiene education programs accredited by CODA (ADA, 2009a). Most of these programs award associate degrees (82 percent), but others award baccalaureate degrees, diplomas, and certificates (ADA, 2009a). In 2008, there were about 6,700 dental hygiene graduates. In the early years of the profession, dental hygiene education programs were often colocated with dental education programs in schools of dentistry (Haden et al., 2001). Today, about two-thirds of dental hygiene education programs are located in community, junior, and technical colleges (ADHA, 2006), which may decrease the amount of interaction between dentists and dental hygienists during their training, and therefore not prepare them to work as a team. Annual tuition can vary widely. For example, community colleges have an average annual tuition of $3,154, while the average annual tuition for programs colocated with dentals schools is $12,659 (ADA, 2009a). While the educational admissions
![]()
9 This reflects the number of applications and not the unique number of applicants.
requirements for dental hygiene education programs vary widely, more than 80 percent of first-year students have completed at least 2 years of college (ADA, 2009a). Faculty in dental hygiene education programs are mostly dental hygienists (76 percent), and 21 percent are dentists (ADA, 2009a).
Dental Assistants
Dental assistants are trained on the job or in formal education programs. Education programs in dental assisting may be located in postsecondary institutions that are accredited by CODA, postsecondary institutions that are not accredited, high schools, vocational programs, and technical schools (ADAA/DANB Alliance, 2005). Dental assistants may also be trained on the job by their employers. Considering the numerous alternate pathways to working in dental assisting and the variability in state licensure and certification practices, as described previously, it is difficult to generalize a description of the workforce as a whole or to assess the impact of the various training alternatives (ADAA/DANB Alliance, 2005; Neumann, 2004). Little is known about the wide variety of programs that are not accredited by CODA.
In 2008–2009, CODA accredited 273 dental assisting programs, almost all of which (87 percent) were in public institutions (ADA, 2009a). Average cost for tuition and fees in a CODA-accredited dental assisting program in the 2008–2009 academic year for in-district students was $6,791 (ADA, 2009a). Among students enrolled in CODA-accredited dental assisting programs in the 2008–2009 academic year, 63 percent were age 23 and under, and less than 5 percent were male. In 2008, there were 6,110 graduates from CODA-accredited programs (ADA, 2009a).
Virtually all CODA-accredited programs require a high school diploma (or even higher level of education) for admission (ADA, 2009a). Most CODA-accredited programs are 1 year in length leading to a certificate or diploma. However, a few have a 2-year curriculum resulting in an associate degree. About 14 percent of faculty in CODA-accredited programs are dentists, 70 percent are dental assistants, and 28 percent are dental hygienists (ADA, 2009a).10
Dental Laboratory Technicians
There are no formal education or training requirements for dental technicians, and most learn required skills through on-the-job training; however, some formal programs exist in universities, community and junior
![]()
10 Some faculty members reported more than one discipline, so these numbers do not total 100 percent.
colleges, vocational schools, and the military (BLS, 2010g). In the 2008– 2009 academic year, there were 20 CODA-accredited programs (ADA, 2009a). Virtually all faculty (91 percent) are dental laboratory technicians (ADA, 2009a). Most accredited programs last 2 years, and 13 confer an associate’s degree. In the 5-year period from 2004–2009, applications to these programs decreased by nearly 13 percent (ADA, 2009a). Average total tuition and fees range from $7,838 for in-district students to $18,214 for out-of-state students (ADA, 2009a). In 2008, there were 234 total graduates from accredited dental laboratory technology programs (ADA, 2009a).
Racial and Ethnic Diversity
The racial and ethnic profile of the dental workforce is not representative of the overall population (see Table 3-5). While diversity among the dental professions students has increased in the previous decade (see Table 3-6), the numbers still are not significantly different. Evidence shows that a diverse health professions workforce (including race and ethnicity, gender, and geographic distribution) leads to improved access for underserved populations, greater patient satisfaction, and better communication (HRSA, 2006; IOM, 2004). Health care professionals from underrepresented minority (URM) populations, in part due to patient preference, often account for a disproportionate amount of the services provided to underserved populations (including both URM and low-income populations) (Brown et al., 2000; HRSA, 2006; IOM, 2003; Mitchell and Lassiter, 2006). For example, a 1996 survey by the ADA revealed that nearly 77 percent of white den-
TABLE 3-5
Dental Professions by Percentage of Race and Hispanic Ethnicity, 2000
| General Population | Dentists | Dental Hygienists | Dental Assistants | |
| Whitea | 75.1 | 82.8 | 90.9 | 75.8 |
| Black or African Americana | 12.3 | 3.3 | 2.3 | 5.6 |
| Asiana | 3.6 | 8.8 | 2.0 | 3.6 |
| Hispanic or Latino Origin | 12.5 | 3.6 | 3.7 | 12.6 |
aCategory excludes Hispanic origin.
SOURCES: U.S. Census Bureau, 2000, 2002.
TABLE 3-6
Percentage of Dental Professions School and Program Enrollment by Race and Hispanic Ethnicity, 2000–2001 and 2008–2009
| Enrolled Dental Students | Enrolled Dental Hygiene Students | Enrolled Dental Assistant Studentsa | ||||
| 2000–2001 | 2008–2009 | 2000–2001 | 2008–2009 | 2000–2001 | 2008–2009 | |
| White | 63.4 | 59.9 | 82.3 | 78.6 | 68.4 | 60.2 |
| Black | 4.8 | 5.8 | 4.2 | 4.4 | 12.5 | 15.1 |
| Asian | 24.8 | 23.4 | 4.6 | 7.0 | 2.9 | 4.8 |
| Hispanic | 5.3 | 6.2 | 5.7 | 7.3 | 9.7 | 11.1 |
aIncludes only dental assistant students enrolled in CODA-approved programs. Racial and ethnic diversity of entire dental assistant workforce may be different.
SOURCES: ADA, 2002, 2009a, 2010a.
tists’ patients were white, while 62 percent of African American dentists’ patients were African American and 27 percent were white (ADA, 1998). More recently, among dental students graduating in 2008, 80 percent of African American students and 75 percent of Hispanic students expected at least one-quarter of their patients would be from underserved racial and ethnic populations; nearly 37 percent of the African American students and 27 percent of the Hispanic students expected at least half their practice would come from these populations (Okwuje et al., 2009). In comparison, only 43.5 percent of white students expected at least one-quarter of their patients to come from underserved racial and ethnic populations, and only 6.5 percent expected at least half of their practice to be comprised from these populations (Okwuje et al., 2009). It is important to note that the recruitment of low-income students (regardless of race or ethnicity) may also be important in the future care of URM patients (Andersen et al., 2010).
Several factors complicate recruitment of underrepresented minorities into dentistry including lack of exposure to and knowledge of the dental profession, minimal opportunities for mentorship from dental professionals, and competition from other health professions for underrepresented minority students who are academically qualified (Haden et al., 2003).
Bridge and Pipeline Programs
Bridge and pipeline programs are two strategies used to attract and retain underrepresented minority, lower-income, and rural students to health care professions. Bridge programs primarily focus on elementary school
students through high school graduates while pipeline programs focus on undergraduate and preprofessional students. Both programs have a long history in health professions (e.g., dentistry, medicine, nursing, pharmacy) (Awé and Bauman, 2010; Brooks et al., 2002; Brunson et al., 2010; Cantor et al., 1998; Formicola et al., 2010; Grumbach and Chen, 2006; Hesser et al., 1996; Kim et al., 2009; Lewis, 1996; Rackley et al., 2003; Thomson et al., 2010).
Pipeline interventions for improving racial and ethnic diversity in the health professions in general have shown promise (HHS, 2009). In 2001, the Robert Wood Johnson Foundation, in collaboration with the California Endowment and the W.K. Kellogg Foundation, created the initiative Pipeline, Profession, and Practice: Community-Based Dental Education,11 which ended in July 2010. This project provided much insight into strategies for successful implementation (Lavizzo-Mourey, 2010; Leviton, 2009). Overall, dental pipeline programs show promise, but gains to date have been small and individual programs have had variable results regarding the ultimate enrollment and retention of students, dependent upon the program’s characteristics (Andersen et al., 2005; Markel et al., 2008; Price et al., 2007; Thind et al., 2008; Veal et al., 2004). Moreover, it has yet to be determined whether these programs will have a long-term effect on increasing diversity in dentistry. Evidence suggests that pipeline programs require a sustained commitment by participating schools and sufficient resources to maintain momentum (Brunson et al., 2010; Thind et al., 2009).
One example of an effort to increase the diversity of the dental workforce is the ADA Career Guidance and Diversity Committee, which sponsors the Student Ambassador Program. In this program, ambassadors reach out to high school and college students regarding careers in dentistry (ADA, 2011b). Strategies include increasing collaborations between dental schools and college prehealth advisors, providing shadowing opportunities, and linking to existing career guidance programs.
New and Emerging Members of the Dental Team
Many health care professions have become embroiled over the creation of new types of practitioners as well as over the expansion of scope of practice for existing practitioners. Within the dental professions, efforts to define or expand scopes of practice for dental professionals have been plagued by a decades-long, contentious history (Dunning, 1958; Edelstein, 2010b; Fales, 1958; Hammons and Jamison, 1967, 1968; Hammons et al., 1971; Nash, 2009; Nash and Willard, 2010). Early experiments to have dental
![]()
11 For information on participating schools, funding levels, activities, accomplishments, and community partners, see the RWJF project website at: http://www.dentalpipeline.org.
hygiene students perform discrete restorative procedures indicated that the quality of the care provided by these students was equal to that of dental students, but follow-up studies were not performed amidst the concerns of organized dentistry for patient safety (Dunning, 1958; Garcia et al., 2010; Lobene and Kerr, 1979; Sisty et al., 1978). Dental therapists and dental nurses have been used internationally for decades (Ambrose et al., 1976; Gallagher and Wright, 2003; GAO, 2010; Nash and Nagel, 2005b; Nash et al., 2008; Pew Center on the States and National Academy for State Health Policy, 2009; Sun et al., 2010). In particular, New Zealand and Australia have used these dental professionals since the early 20th century. Suggestions to perform a demonstration of the New Zealand school dental nurse in the United States occurred as early as 1947 (Dunning, 1958), but they were not acted upon, again due to the concerns of dentists for patient safety.
The use of dental therapists to provide basic educational, preventive, and restorative services in the United States has been especially contentious. Recently, the Indian Health Service (IHS) has used dental therapists to perform specific functions in order to address oral health access difficulties for American Indian communities (Bolin, 2008; Fiset, 2005; Nash and Nagel, 2005a,b; Wetterhall et al., 2010). In 2003, the Alaska Native Tribal Health Consortium first sent several Alaskan students to New Zealand to train as dental therapists, and the consortium is currently working with the University of Washington to train these students in Alaska (DENTEX, 2010; Nash and Nagel, 2005b). The first assessment of dental therapists in the United States indicated there was no significant difference between treatment provided by dental therapists and treatment provided by dentists (Bolin, 2008). A more recent evaluation indicates that the care provided by dental therapists in the United States is both effective and acceptable to patients (Wetterhall et al., 2010). Further, residents of communities served by dental therapists report that access to care has improved. It is important to note the narrow scope of this evaluation in that the authors examined the implementation of the dental therapist model in just five practice sites. In addition, they noted: “We undertook this challenging effort knowing that there are few, if any, widely accepted, evidence-based standards for assessing dental practice performance. Further, for the logical comparison group—that is, dentists in private practice—there are virtually no data for any of the outcomes that we undertook to observe and measure” (Wetterhall et al., 2010).
Aside from the dental therapist, several other workforce models have been recently proposed to either introduce new types of professionals or expand the scope of work of existing professionals. For example, in 2009, the Minnesota legislature approved the certification of a master’s
level “advanced dental therapist”12 to work in remote consultation with a dentist and provide some restorative procedures (GAO, 2010). The Community Dental Health Coordinator (CDHC), developed by the ADA, would provide oral health education and some limited preventive services under the supervision of a dentist (GAO, 2010; Pew Center on the States and National Academy for State Health Policy, 2009). The registered dental hygienist in alternative practice (RDHAP) started as a pilot project in the 1970s; the RDHAP is licensed (only in California) to provide care directly to patients but must have a documented relationship with a dentist for referral, consultation, and emergencies (Mertz and Glassman, 2011).
All of these new and emerging members of the dental team (and several others) have been targeted to reach populations that for a variety of reasons (e.g., transportation, geographic location, dental coverage issues) have difficulty accessing care. While there are differences, all depend on the practitioner being part of a larger health care team (Garcia et al., 2010). Many of these models remain controversial, with some arguing for their ability to increase access, and others voicing concerns for patient safety and the quality of care provided by these practitioners (ADA, 2007; AGD, 2008; Edelstein, 2010b; GDA, 2010; Pew Center on the States and National Academy for State Health Policy, 2009).
Lessons from Other Health Care Professions
Concerns have been raised in other fields when new types of practitioners were being developed or when existing professionals sought to extend their scopes of practice (Carson-Smith and Minarik, 2007; Daly, 2006; Huijbregts, 2007; RCHWS, 2003; Wing et al., 2004). While nurse practitioners and physician assistants are largely seen as well-accepted members of the health care team, their development was also resisted, and extension of their scopes of practice remains a sensitive issue. Professional tensions typically center around the quality of care provided by individuals with less training, but in many cases, evidence has not supported this. Advanced practice nurses are often involved in high-risk procedures such as childbirth and the administration of anesthesia, yet the evidence base continues to grow that the quality of their care is similar to that of physicians. For example, studies on certified nurse midwives have shown good maternal outcomes and cost savings in comparison with obstetricians (MacDorman and Singh, 1998; Oakley et al., 1996; Rosenblatt et al., 1997). Certified registered nurse anesthetists (CRNAs), like many nonphysician health care professionals, are an important source of care in rural populations: CRNAs are the sole providers of anesthesia in more than two-thirds of
![]()
12 2009 Minn. Laws Ch. 95, Art. 3.
all rural hospitals (AANA, 2011). In 2001, CMS ruled that states could opt out of requirements for physician supervision of CRNAs, a decision that was opposed by anesthesiologists due to concerns for quality of care (Dulisse and Cromwell, 2010). However, a study of the time period from 1996 until 2005 revealed that there was an increase in the number of procedures performed by CRNAs, but there was no concomittant increase in adverse events (Dulisse and Cromwell, 2010). These examples provide some evidence on the ability to use nonphysician health care professionals to provide quality care in some situations.
Conclusions
While dentists continue to raise concerns for the quality of care provided by individuals (apart from dentists) who might perform restorative care, there is a lack of evidence documenting poorer quality of the services performed by these individuals or poorer outcomes resulting from their care. There are many studies of the safety and quality of dental therapists and dental nurses around the world, but these models occur in different systems of care delivery and financing. Evaluations in the United States to date have been limited, and it is nearly impossible to compare their quality to that of existing dental professionals, since little evidence exists on the quality of care provided by traditional dental practitioners (see a discussion of quality of care later in this chapter). The committee considered the concerns raised by dentists, the unresolved needs of certain segments of the population (e.g., vulnerable and underserved populations), international evidence, and the experiences seen in developing new roles and responsibilities among other health care professions. In addition, the committee recognizes that there is little evidence to indicate which route would be best—developing new types of providers or expanding the scope of existing dental professionals. Due to the variety of challenges, the committee concludes that the exploration of new workforce models (including both new types of dental professionals as well as expansion of the role of existing professionals) is one part of a complex solution to improving oral health care. There may, in fact, be roles for different models depending on the needs of the population and sites of care. Without further research and evaluation, with monitoring for any concerns about the quality of care, better workforce models cannot be developed. Regardless of state laws, many factors will influence the ultimate success of new workforce models, including the support of dentists, the support of state Medicaid agencies, and a viable mechanism for paying the new types of practitioners (Nolan et al., 2003).
THE NONDENTAL ORAL HEALTH WORKFORCE
As oral health has increasingly become recognized as integral to overall health, nondental health care professionals have become increasingly involved in the prevention, diagnosis, and treatment of oral diseases. Studies show that training primary care clinicians in oral health leads to their increased ability to recognize oral disease and may help to increase their referrals to dentists (Dela Cruz et al., 2004; Mouradian et al., 2003; Pierce et al., 2002). In addition, practice changes resulting from this training can lead to increased access to preventive services and decreased dental disease (Chu et al., 2007; Douglass et al., 2009b; Kressin et al., 2009; Rozier et al., 2010). As discussed in Chapter 2, all types of health care professionals need improvements in their oral health literacy skills. In order to do so, educational programs will need to adapt curricula not only to teach basic oral health knowledge but also to impart a greater understanding of the importance of oral health to their individual disciplines. This section considers the education, training, and potential role of several nondental health care professions in the oral health care of the nation. At the end of the section, the role of nondental health care professionals as a whole in the delivery of preventive services for oral health is discussed.
Physicians
The need for physicians to learn about oral health has been recognized for nearly a century (Gies, 1926). Today, many physicians still do not receive education or training in oral health either during medical school, during residency training, or in continuing education programs (Krol, 2010; Mouradian et al., 2003). In addition, the breadth and depth of existing education and training efforts is highly variable (Douglass et al., 2009a; Ferullo et al., 2011). Even though many physicians recognize the importance of oral health (including their own role), they often do not feel prepared to provide oral health care. (See a discussion in Chapter 2 regarding health care professionals’ knowledge of oral health.) Dentists also express some hesitation about involving physicians in oral health care; while a large majority of directors of advanced general dentistry residencies supported physician inclusion of routine dental assessments (87.1 percent) and prevention counseling (83.3 percent) in well-child care, less than a third (31.2 percent) supported physicians applying fluoride varnish (Raybould et al., 2009).
Medical Schools
Very few medical schools include curriculum on oral health, despite the presence of oral health topics on medical licensing exams (Ferullo et
al., 2011; Krol, 2004; Mouradian et al., 2005; USMLE, 2010a,b). A recent survey indicated that almost 70 percent of medical schools include 4 hours or less of oral health in their curriculum; this includes the more than 10 percent of schools that have no oral health curriculum hours at all (Ferullo et al., 2011). The most frequently covered oral health topics include oral cancer, oral anatomy, and oral health and overall health; fewer than 50 percent of schools that teach oral health cover the risks of dental caries (Ferullo et al., 2011).
In 2004, the Josiah Macy, Jr. Foundation funded a 3-year grant to examine dental education, New Models of Dental Education (Formicola et al., 2005; Machen, 2008). As part of the project, three panels were convened to discuss different aspects of oral health education and each produced a report (Johnson et al., 2008; Lamster et al., 2008; Mouradian et al., 2008). One panel produced the report, Curriculum and Clinical Training in Oral Health for Physicians and Dentists, which emphasized the role for physicians in the identification and referral of patients with oral health needs (Mouradian et al., 2008). Subsequently, the American Association of Medical Colleges published learning objectives for oral health (AAMC, 2008). Courses that have incorporated these objectives have significantly increased students knowledge of oral health topics, even in a short time period (Silk et al., 2009). One medical school at the forefront of oral health education, the University of Washington Medical School, created and has started to implement a comprehensive oral health curriculum for medical students; results show students have more confidence in identification of oral disease and attitudes toward oral health care improved (Mouradian, 2010; Mouradian et al., 2005, 2006).
Pediatricians
A 2000 national survey of pediatricians found that more than 90 percent believed they had an important role in the recognition of oral diseases and the provision of counseling regarding the prevention of caries, and three-quarters expressed interest in the application of fluoride varnish in their practices (Lewis et al., 2000). However, half reported no oral health training in either medical school or residency. A 2006 survey found that two-thirds of graduating pediatrics residents thought they should be performing oral health assessments on their patients, but only about one-third of pediatrics residents receive any oral health training during their residencies, and of those that do, two-thirds get less than 3 hours of training. (Caspary et al., 2008). Only about 14 percent had clinical observation time with a dentist.
The American Academy of Pediatrics (AAP), the professional society for general pediatrics, has developed explicit educational guidelines for oral
health training in pediatric residency (AAP, 2011c). In addition, the pediatric board exam has questions about oral health (ABP, 2009). However, the residency review committee for pediatrics has not yet identified oral health as a required topic for pediatric residencies.
Family Medicine Physicians
Family medicine has taken a number of steps to incorporate oral health into residency curriculum. The Society of Teachers of Family Medicine Group on Oral Health published an oral health curriculum for family medicine in 2005 (it was updated in 2008), and the residency review committee for family medicine residencies added oral health as a requirement in 2006 (ACGME, 2007; Society of Teachers of Family Medicine Group on Oral Health, 2011). Yet, a recent survey showed only three-fourths of the residency directors knew of the oral health requirement, and only about two-thirds of the programs were actually including oral health content, with the most common training time being 2 hours per year (Douglass et al., 2009a).
Internal Medicine Physicians
Of the primary care specialties, internal medicine has done the least to incorporate oral health. Oral health education is not a requirement for internal medicine residencies, although the geriatrics subspecialty requires education in prevention of oral diseases, and the sleep medicine subspecialty requires residents to have experience receiving consults from oral maxillofacial surgeons (ACGME, 2008, 2009a,b). No specific curricula exist to educate internal medicine residents or physicians in oral health. In a survey of internal medicine trainees, 90 percent reported receiving no training on periodontal disease during medical school, and 23 percent said they never referred patients to dentists (Quijano et al., 2010).
Nurses
The nursing workforce is the largest workforce of health professionals in the nation, with 3.1 million registered nurses including over 141,000 nurse practitioners (NPs) (ANA, 2011a, 2011b). In a recent “call to action” to the nursing profession, Clemmens and Kerr (2008) noted that “oral health has not been a high nursing priority in the past” and urged the profession to “increase nursing’s awareness, knowledge, and skill about the significance that oral health holds.” However, as with other nondental health care professions, the training of nurses in oral health and hygiene is highly variable and often inadequate (Jablonski, 2010).
NPs in particular may have an important role to play in oral health
care. A recent study found that “substantial parallels exist in the education and practice of dentists and [NPs] including basic, social, and some clinical science education, practice models, research synergies, and community service” (Spielman et al., 2005). NPs have been defined as primary care providers (IOM, 1996) and can see patients independently and perform histories and physicals, perform lab tests, and diagnose and treat both acute and chronic conditions. NPs emphasize health promotion and disease prevention and especially focus on the health of individuals in the context of their families and communities. NPs commonly practice in rural areas and health professional shortage areas, and the growth of the profession, in part, is due to their role in caring for underserved populations (Grumbach et al., 2003; Harper and Johnson, 1998). As such, they may serve as a frontline screening source for oral diseases. NPs have been shown to provide high-quality care, be cost-effective, have high levels of patient satisfaction with their care, and contribute to increased productivity (Budzi et al., 2010; Hooker et al., 2005; Mezey et al., 2005; Todd et al., 2004).
Criteria set by the National Task Force on Quality Nurse Practitioner Education (2008) do not delineate any specific competencies for oral health. In 2006, the Arizona School of Health Sciences and the Arizona School of Dentistry and Oral Health developed a set of proposed oral health competencies for nurse practitioners and physician assistants (PAs) (Danielsen et al., 2006). As shown in Table 3-7, a subsequent survey of NPs and PAs revealed that many do not feel prepared for some of these basic competencies.
In addition to NPs, there are more than 3 million direct-care workers (e.g., nurse aides) who work in places where dental professionals typically do not provide care (e.g., assisted living facilities, home health agencies) (PHI, 2010). These nursing personnel also have the opportunity to be involved in the detection of oral diseases. In nursing home settings, certified nursing assistants are responsible for the provision of oral hygiene care for
TABLE 3-7
Perceived Competence of Nurse Practitioners and Physician Assistants (Percent)
| Nurse Practitioners | Physician Assistants | |
| Can perform an oral exam | 43 | 53 |
| Can recognize oral symptoms of systemic disease | 22 | 34 |
| Can discern “obvious pathology and conditions of the oral cavity” | 40 | 63 |
SOURCE: Danielsen et al., 2006.
residents, but they are often unprepared for this task and make it a low priority (Chalmers, 1996; Coleman and Watson, 2006; Jablonski et al., 2009).
Pharmacists
As health care professionals in community settings, the role of the pharmacist has expanded over time from merely dispensing medications to being an important partner with other health care professionals. Pharmacists are often involved in health promotion and disease prevention activities such as public health education, health screenings, and the provision of vaccines. In 2008, pharmacists held almost 270,000 jobs; about 65 percent worked in retail settings, and 22 percent worked in hospitals (BLS, 2009a). The BLS notes a likely increase in the need for pharmacists to provide services in settings such as doctors’ offices and nursing facilities as well as to increasingly offer patient care services, such as the administration of vaccines (BLS, 2009a).
Regarding oral health specifically, customers may approach pharmacists regarding the treatment of oral health conditions such as mouth ulcers, cold sores, and persistent pain (Cohen et al., 2009; Macleod et al., 2003; Sowter and Raynor, 1997; Weinberg and Maloney, 2007). Pharmacists can have an important role in the management and treatment of oral disease such as through education on selection and use of daily oral hygiene products as well as referrals to dentists as necessary. Pharmacists could also monitor the prescription of dietary fluoride supplements, especially as it might relate to the status of that community’s water fluoridation. No formal assessment has been done to evaluate the extent and depth of education and instruction that pharmacy students receive regarding oral health.
Physician Assistants
As primary care providers, PAs also have great opportunities and responsibilities to be involved in oral health care (Berg and Coniglio, 2006; Danielsen et al., 2006). PAs work under the supervision of a physician, but they can often work apart from the physician’s direct presence and can prescribe medications and bill for health care services. The BLS projects the PA profession to be the seventh fastest-growing occupation between 2008 and 2018 (see Table 3-4). In 2008, PAs held about 74,800 jobs; more than half of these jobs were located in physicians’ offices, and about one-quarter were in hospitals (BLS, 2009b).
About half of PAs work in primary care (Brugna et al., 2007; Hooker and Berlin, 2002). Like NPs, PAs are an especially important source of care for rural communities, for low-income and minority populations, and in health professional shortage areas (Grumbach et al., 2003), and they have
been shown to provide quality and cost-effective care (Ackermann and Kemle, 1998; Brugna et al., 2007; Jones and Cawley, 1994).
Very little is known about the extent of oral health education in the PA curricula. As in nurse practitioner programs, standards set by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA, 2010) do not delineate any specific competencies for oral health. In the previously mentioned survey performed by the Arizona School of Health Sciences and the Arizona School of Dentistry and Oral Health, many PAs feel unprepared for some basic oral health competencies (see Table 3-7). Interestingly, that survey showed that 10 percent of PAs did not think it was important for them to understand what the various dental specialties could do for their patients (compared to 2 percent of nurse practitioners) (Danielsen et al., 2006). A recent survey of PA program directors found “over 75 percent believed that dental disease prevention should be addressed in PA education, yet only 21 percent of programs actually did so” (Jacques et al., 2010). The number of curriculum hours dedicated to oral health ranged from 0 to 14 hours, with an average of 3.6 hours.
The Role of Nondental Health Care Professionals in Preventive Care
One solution for improving access to preventive care for oral health, especially for children, has been to expand the use of nondental health care professionals (Douglass et al., 2009b; Hallas and Shelley, 2009; Okunseri et al., 2009). Nondental health care professionals can incorporate oral health into their routine exams and wellness visits with basic risk assessments, oral exams, anticipatory guidance, and the provision of basic preventive services (Cantrell, 2008; Riter et al., 2008). The application of fluoride varnish is a prime example for the potential expanded role of nondental health care professionals. Fluoride varnish is increasingly being applied by nondental health care professionals and in community-based settings (AAP, 2011b; ASTDD, 2007). In spite of evidence on the effectiveness of fluoride varnish (see Chapter 2), it is not approved by the FDA for its use in the prevention of dental caries (ASTDD, 2007), which may deter some health care professionals from using it for this purpose.
In the past, nondental health care professionals could not be reimbursed for preventive care in oral health, but this is changing. As of 2010, 39 state Medicaid programs reimbursed primary medical care providers for preventive oral health services, 2 approved such reimbursement but did not have funding, and another 3 allowed reimbursement under certain circumstances (AAP, 2010). This is an increase from 2008, when only 25 states reimbursed physicians for these types of services, and 2009, when 34 states did so (Cantrell, 2008, 2009). In addition, some states also reimburse NPs and PAs for these services (Cantrell, 2008). The three types of services
typically reimbursed include oral examination, screening, and risk assessment; anticipatory guidance and caregiver education; and application of fluoride varnish (Cantrell, 2009). In 2009, 25 states required the health care professionals undergo training before they could be reimbursed (Cantrell, 2009). Aside from lack of reimbursement, other barriers to engaging nondental health care professionals in preventive care (both for oral health as well as other health conditions) can include the lack of familiarity with oral health issues, lack of confidence in their skills, skepticism on the efficacy of preventive services, and inadequate time in the patient visit (Lewis et al., 2000; Rozier et al., 2003; Sanchez et al., 1997).
Several individual state-based initiatives have arisen to help improve nondental health care professionals’ involvement in providing basic preventive services for oral health. One well-known example is North Carolina’s Into the Mouths of Babes (IMB) which targets children up to age 3 (Rozier et al., 2003, 2010). IMB stemmed from earlier work in the 1990s where poor oral health was identified as one of the most serious problems for children and their families in the Appalachian region of the state. With support from the North Carolina Medicaid program, CMS, the Health Resources and Services Administration (HRSA), and the Centers for Disease Control and Prevention, lessons learned from that work led to the statewide demonstration of IMB in 2001. The project aims to improve practitioners’ oral health knowledge, incorporate caregiver counseling and fluoride varnish application into primary care practices, and increase screenings and dental referrals for children with oral diseases or are at risk for diseases (Close et al., 2010). Reimbursement is provided for up to 6 visits for children up to age 3. Between 2001 and 2002, nearly 1,600 nondental health care professionals were trained (Rozier et al., 2003). About half of the participants were pediatricians or family physicians and another one-third were registered nurses; others included PAs, NPs, and a variety of other health care professionals. In 2006, almost one-third of all well-child visits for this age group included preventive care for oral health (Rozier et al., 2010). In 2009, the North Carolina Department of Health and Human Services reported a ten-fold increase in the number of preventive procedures since the inception of IMB (NC Department of Health and Human Services, 2009). Program successes have been attributed to a broad-based, collaborative coalition, support from the professions themselves, an active effort to improve awareness about oral diseases, and adequate resources (Rozier et al., 2003). A recent survey of participants in the program identified some of the barriers to success, including difficulty integrating the services into practices (reported by 42 percent), difficulty in applying fluoride varnish (29 percent), reluctance of other office personnel (26 percent), and difficulty in making dental referrals (21 percent) (Close et al., 2010). In order to better integrate the application of fluoride varnish into primary care setting, providers may
need to look to the model of immunization as an example of successfully integrating the delivery of preventive services in these settings.
HHS has also actively supported programs that seek to improve the use of nondental health care professionals in oral health care. For example, Bright Futures was initiated by HRSA’s Maternal and Child Health Bureau in 1990 to improve children’s health in general through health promotion and disease prevention (AAP, 2011a). The project includes a collaboration of many different organizations and includes information, guidance, and training on oral health issues from pregnancy through adolescence. Currently, the American Academy of Pediatrics (AAP) is MCHB’s lead collaborator; AAP has developed a new edition of the Bright Futures Guidelines, which focus on health promotion and disease prevention (MCHB, 2011). The website (www.brightfutures.org) includes online training modules for child health professionals in oral health management and risk assessment.
Public health workers include many of the professions previously mentioned, including both dental and nondental health care professionals. The 1988 IOM report The Future of Public Health defined the mission of public health as “fulfilling society’s interest in assuring conditions in which people can be healthy” (IOM, 1988). That committee went on to say:
[Public health’s] aim is to generate organized community effort to address the public interest in health by applying scientific and technical knowledge to prevent disease and promote health. The mission of public health is addressed by private organizations and individuals as well as by public agencies. But the governmental public health agency has a unique function: to see to it that vital elements are in place and that the mission is adequately addressed. (IOM, 1988)
As with other segments of the health care workforce, the public health workforce is difficult to enumerate due to the variety of professions involved, lack of a common taxonomy for job titles and duties, and a lack of a single comprehensive licensure or certification process for public health (HRSA, 2000). Both dental and nondental health care professionals may be involved in dental public health. Little is known about the extent of training in oral health among schools of public health, even though graduates may be involved in oral health issues during their careers. A 2001 survey of schools of public health showed that 60 percent of schools had no faculty with a degree in dentistry or dental hygiene (Tomar, 2006). In addition, only 15 percent of schools offered a Master of Public Health degree with a concentration in dental public health.
The predecessor to the present-day American Association of Public
Health Dentistry (AAPHD) was established in 1937 and represents a variety of public health professionals involved in oral health care (AAPHD, 2004). In 1948, the Association of State and Territorial Dental Directors was established to represent the directors and staff of state dental public health programs and is currently an affiliate of the Association of State and Territorial Health Officials (ASTDD, 2011a). In 1951, the American Dental Association (ADA) recognized dental public health as a specialty of dentistry (AAPHD, 2004). In 2005, estimates of the number of public health dentists ranged from 153 (the number of diplomats of the American Board of Public Health Dentistry) to 498 (the number of dentist members of the AAPHD) to 543 (the number of members in the ADA directory reporting a specialty of “dental public health”) (Tomar, 2005). HHS supports dental public health residency programs (see Chapter 4). Public health dentists often work for governments at the federal, state, county, and local levels (Tomar, 2006). While public health is a key part of the practice of dental hygiene, little is known about public health workers with specialty in dental hygiene.
While HHS is a key leader in establishing the general public health infrastructure of the country, much dental public health activity takes place at the state and local levels. Dental public health workers often are involved in state- and locally funded activities (e.g., sealant programs, fluoridation programs) that aim to assure access to services. Most states have established an oral health plan, whether as a part of the state’s direct dental public health activities, or as a part of a larger health plan (CDC, 2011). Such plans are usually developed and overseen by oral health directors or dental directors under the umbrella of state departments of (public) health. The range of services and activities provided under the auspices of state public health dentistry, vary considerably, however, and range from assessment (e.g., gathering oral health data through surveillance activities), to policy development (e.g., related to access), to assurance (e.g., providing clinical preventive and treatment services, supporting community-level water fluoridation) (ASTDD, 2011b).
Oral health data gathered through state and local public health dental programs allow state and federal agencies to identify trends in oral diseases (e.g., dental caries) and oral health professional shortage areas, and provide the basis for future planning. State-level dental public health programs provide both population and individual-level preventive, promotive, and restorative care. State public health dental programs, through county and city health departments, also provide fluoride varnish, mouth rinse, and fluoride tablets (ASTDD, 2011b).
In 2001, the ADA stated, “A formal dialogue among all health care professions should be established to develop a plan for greater cooperation and integration of knowledge in medical and dental predoctoral education, hospital settings, continuing education programs, and research facilities” (ADA, 2001). The importance of interaction between dentists and other health care professionals is a not new finding. In 1917, Sidney J. Rauh, Chairman of the Oral Hygiene Committee of the Ohio State Dental Society, noted,
It has been found imperative that physicians and surgeons possess at least a theoretical knowledge of disease-breeding conditions met with in the teeth and jaws, but it is even more important for the dentist to appreciate the close relationship between his profession and that of the physician, surgeon, bacteriologist, chemist, and public health official. (Rauh, 1917)
Still, health care professionals are typically trained separately by discipline. As a result, professionals may gain little understanding of or appreciation for the expertise of other professionals or the skills needed to effectively participate on a team, including how and when to refer patients to each other and how to best communicate with each other. The value of interprofessional care, especially to care for patients with complex care needs, and the importance of interprofessional education and training have been increasingly acknowledged in recent years (Baum and Axtell, 2005; Blue et al., 2010; Buelow et al., 2008; Dodds et al., 2010; Dyer, 2003; Fulmer et al., 2005; Hall and Weaver, 2001; Howe and Sherman, 2006; Lerner et al., 2009; Misra et al., 2009; O’Leary et al., 2010; Wilder et al., 2008; Williams et al., 2006). In particular, evidence is growing that interprofessional care leads to better care coordination, communication, and, ultimately, better patient outcomes, improved satisfaction, and cost savings (Hammick et al., 2007; HHS, 2010; McKinnon and Jorgenson, 2009; Reeves et al., 2008, 2010; Snyder et al., 2010). The AAP policy statement on the role of pediatricians in prevention calls for collaboration between primary care pediatricians and local dentists in order to establish a dental home (AAP, 2008). The newly formed Center for Medicare and Medicaid Innovation has several projects looking at the effectiveness of team care (Carey, 2010). (See Chapter 4 for more on the center.) While more professionals are gaining experience in interprofessional training, little evidence exists to determine which methods are best for imparting the knowledge and skills necessary to work as a team member, how such training affects patterns of practice, or how it affects patient outcomes (Cooper et al., 2001; Hall and Weaver, 2001; Remington et al., 2006; Thistlethwaite and Moran, 2010).
For oral health care, two levels of team care may exist—first among dental professionals and second among various health care professionals. As will be discussed in Chapter 4, the federal government has a history of training dental professionals to work together more effectively. More research will be needed for understanding the dynamics of the dental team as new types of dental professionals emerge. In addition, little research exists on the interprofessional education and training of dental professionals and nondental professionals together in caring for mutual patients who have complex oral health needs (Haden et al., 2010; Hallas and Shelley, 2009; Wilder et al., 2008). In 2005, New York University created a unique partnership in which a college of nursing was located within the college of dentistry. As part of the interdisciplinary educational model, pediatric nurse practitioner students work alongside dental students to provide care in school clinics and Head Start programs (Garcia et al., 2010; Hallas and Shelley, 2009). This allows the pediatric nurse practitioner students to learn about caries risk assessment and how to apply fluoride varnish while the dental students can become more familiar with the role of the nurse in oral health.
In January 2010, the Advisory Committee on Training in Primary Care Medicine and Dentistry recommended that “training grants should provide funds to develop, implement, and evaluate training programs that promote interprofessional practice in the patient-centered medical-dental home model of care” (HHS, 2010). They also stated that “funding should support clinical sites that prepare trainees for interprofessional practice by educating medical, dental, physician assistant, and other trainees together on health care teams.”
REGULATING THE ORAL HEALTH WORKFORCE
Regulation of the health care workforce in general occurs at several levels. The primary role of the federal government is to protect consumers and promote fair competition. The state has a legitimate interest in protecting the public as well, and each state develops their own scope of practice law for each health care profession that covers such things as who may enter a profession, what types of minimal competency requirements must be satisfied for licensure, and what services they may provide. Finally, the private sector is involved in the regulation of the health care workforce in that they often offer voluntary credentialing; sometimes these types of credentials are required for licensure. For professions and occupations without licensure requirements, credentialing may be one source of information for consumers. HHS has virtually no role in the regulation of health care professions, so this discussion is to provide an overview of the issues as they relate to the overall oral health care system.
The Role of the Federal Government
The Federal Trade Commission (FTC) is charged by Congress with preventing “unfair methods of competition in or affecting commerce, and unfair or deceptive acts or practices in or affecting commerce,”13 including the enforcement of antitrust laws and other basic consumer protection laws. Both the FTC and the Department of Justice advocate against the acts of professions that limit or prevent competition for the delivery of health care services by another profession (e.g., scope of practice laws or licensure restrictions) without providing counterveiling consumer benefit (Chiarello, 2009). In recent years, the FTC has been involved in two notable cases directly related to oral health. Beginning in 2003, the FTC intervened when the South Carolina Board of Dentistry amended state practice acts to override legislation that expanded the scope of practice of hygienists to allow preventive services to be provided in school settings without the direct presence of a dentist (FTC, 2004, 2010). More recently, the FTC became involved in actions surrounding a 2009 state bill (HB 687) supported by the Louisiana Dental Association to make it illegal for anyone to provide school-based oral health care for a fee (FTC, 2009; Moller, 2010). In both cases, the FTC said that the actions restricted care to underserved populations without evidence of counterveiling benefit.
The Role of States
While the education, training, and testing of most health care professionals and the accreditation of educational programs have national standards, the scope of practice for individual professions is established at the state level, often resulting in wide variability among states. As was briefly discussed earlier in this chapter, professional battles and controversy over expanding a profession’s scope of practice are not new to the health care professions or unique to oral health care (Carson-Smith and Minarik, 2007; Daly, 2006; Dulisse and Cromwell, 2010; Huijbregts, 2007; RCHWS, 2003; Wing et al., 2004). Several previous IOM reports have supported the idea of expanding scope of practice in alignment with professional competencies (IOM, 2008, 2010).
State health professions’ licensing boards tend to have an overrepresentation of the profession they are regulating (Dower, 2009; IOM, 1989). This is especially relevant in the dental professions, since boards of dentistry regulate the dental hygiene profession. When one class of professionals is regulated by a different group of professionals, practice may be restricted and it is often difficult to effect change in scope of practice (FTC and
![]()
13 15 U.S.C. §45.
DOJ, 2004; Nolan et al., 2003). Variations in permissible practice among the states are broad, especially for dental hygienists and dental assistants (ADAA/DANB Alliance, 2005; HRSA, 2004). As in medicine where physicians are given significant latitude to delegate to other health professions, in dentistry, dentists are provided with autonomy to delegate at their professional discretion. While part of the purpose of restricting scope of practice is to protect consumers from unsafe or untrained providers, some data suggest that overly restrictive licensure laws in oral health are not tied to better health outcomes; in fact, stringent laws have been tied to increased consumer costs, (IOM, 1989; Kleiner and Kudrle, 2000; Shepard, 1978).
The Role of the Private Sector
Certification is a process by which a private organization imposes a certain level of standards, either through testing or some other method, in order to become “certified.” Certification is often used as a measure of competence, especially in professions which do not have a formal licensure. The Dental Assisting National Board estimates that almost 12 percent of dental assistants in the United States are certified dental assistants (CDAs) by the Dental Assisting National Board (ADAA/DANB Alliance, 2005). As of 2011, 29 states recognize or require CDA certification to perform expanded duties, and a total of 38 states plus the District of Columbia recognize or require one or more of the components of the full CDA exam for particular expanded functions (e.g., Radiation Health and Safety Exam, Infection Control Exam) (DANB, 2011).
Dental technicians can voluntarily become certified dental technicians (CDTs) by the National Board for Certification in Dental Laboratory Technology, an independent board established by the National Association of Dental Laboratories (BLS, 2010g). Certification can occur in crowns and bridges, ceramics, partial dentures, complete dentures, and orthodontic appliances. Three states (Kentucky, South Carolina, and Texas) require dental laboratories to employ at least one CDT, and in Florida dental laboratories must register with the state, and at least one technician must meet requirements for continuing education (18 hours every 2 years) (BLS, 2010g).
ORAL HEALTH AND QUALITY MEASUREMENT
Despite the current interest in the quality of health care, little is known about the quality of oral health care provided in this country. Measurement and assessment of the quality of oral health care lag far behind similar work in the rest of health care (Stanton and Rutherford, 2003). For decades, significant research, resources, and expert opinion has focused on the quality and safety problems in health care, but oral health has largely been left
out of these discussions. In 1998, then President Clinton’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry (1998) found that “[a] key element of improving health care quality is the nation’s ability to measure the quality and provide easily understood, comparable information on the performance of the industry.” The National Quality Forum, a consensus-based entity responsible for endorsing quality measures, was formed as a result of that commission’s recommendations. In 2001, the IOM called for increasing national attention to the quality problems in American health care in Crossing the Quality Chasm (IOM, 2001). That report specifically highlighted the urgent need for more and better measures and other information about performance. It recommended that the field make that information widely and publicly available so the public and health professionals would have the necessary information to make informed health and health care decisions. In 2006, the IOM issued a related report, Performance Measures: Accelerating Improvement, that observed that measuring performance in health care is a critical step toward understanding and resolving health care quality problems (IOM, 2006). It also noted that “[t]here are many obstacles to rapid progress in improving the quality of health care, but none exceeds the fact that the nation still lacks a coherent, goal-oriented, consistent, and efficient system for assessing and reporting on the performance of the health care system.” Further, the report warned that “[f]ailure to establish a well-functioning national performance measurement and reporting system would severely compromise our ability to achieve the essential quality improvements called for in the Quality Chasm report.”
Efforts to develop, endorse, and implement a range of measures to understand the six aims of quality developed in the Crossing the Quality Chasm report (safety, timeliness, equity, effectiveness, efficiency, and patient-centeredness) are ongoing. The health care field has made some significant progress in the effort to measure health care quality (IOM, 2006). However, as the 2006 IOM report found, many significant gaps in health care quality measurement remain, particularly pertaining to measures of equity, efficiency, and patient centeredness. One ongoing significant challenge for health care quality measurement has been developing and implementing measures of significant outcomes relevant to patients. Cost metrics have also been challenging to develop and implement. Further creation of measures of outcomes and cost across the continuum of patient care or episode of care remain a challenge. The ACA directed the Centers for Medicare and Medicaid Services (CMS) to promote the development of these sorts of episode measures for health care, but that work is ongoing.
Arguably, none of this vast and expanding effort specifically includes attention to oral health care or measures of the quality (as defined by the six aims of quality) of oral health care. A quick review of measures cur-
rently endorsed by the National Quality Forum finds no measures related to oral health (NQF, 2010). Further, the most recent annual editions of the National Healthcare Quality Report and the National Healthcare Disparities Report only included information about access to dental services, and not about the state of quality in oral health care (AHRQ, 2010).
Current Oral Health Quality Measures
In oral health care, four types of quality measures are generally available: (1) measures of technical excellence, (2) patient satisfaction (as opposed to patient experience), (3) service use, and (4) structure and process measures (Bader, 2009a). The first type of measures, technical excellence in individual restorations, is not strongly associated with long-term outcomes or patient satisfaction (Bader, 2009a; Evans et al., 2005). The criteria for judgment of technical excellence tend to be subjective and therefore make standardization and comparison difficult. A second set of measures are measures of patient satisfaction. While many patient satisfaction instruments exist for oral health care, they tend to be short, are imprecise at determining the source of expressed dissatisfaction, and are also difficult to compare (Bader, 2009a). They also have not kept up with the movement in the broader health care field toward measuring a fuller range of patient experience.
Measures of service use, a third type of measures, may be used to answer specific access questions such as the proportion of a population that receives a dental service. These measures may also be used to evaluate adherence to evidence-based treatment guidelines; however, few guidelines exist, and the comparison of two practitioners is difficult because the service-use measures need to be risk- (and need-) adjusted for the possible differences in the patient populations being compared, but there are no well-accepted case mix adjustors in dentistry (Bader, 2009a).
The last group of measures in general use in private oral health care practice today includes some general structure and process measures (aside from service-use measures). Structural measures include evaluations of facilities, equipment, and personnel administration. While these are considered to reflect good practice and may have some basis in regulation (e.g., shielding around X-ray equipment), very little evidence supports their relative importance to specific treatment outcomes other than protection of patient health (Bader, 2009a). Process measures include assessment of such functions as infection control, imaging, diagnosis, and treatment planning. Again, very little evidence supports the importance of these measures to the outcomes of care, but they are assumed to reflect good practice (Bader, 2009a).
Overall, quality assessment in dentistry today is relatively weak and
does not assess either the appropriateness or the effectiveness of care. The only clinical outcome measure is technical excellence, which focuses on the provider’s intervention, not the patient’s long-term outcome (Bader, 2009a). The only patient-oriented outcome measure is patient satisfaction, which is inherently flawed as a clinical evaluation tool. In addition, there is no single source of oversight or reporting on any measures that are currently in use.
Limitations to Expanding Quality Measurement in Oral Health Care
The construction of quality measures depends on robust, timely, accurate, and reliable data sources. In health care, for instance, those data sources in the past have largely depended on administrative claims data. There is great hope in the future for more and better health care clinical data for cost and quality measurement from electronic sources (DesRoches and Jha, 2009). There is significant activity under way in health care to increase the adoption of electronic health records and to promote the meaningful use of those electronic tools to enhance the collection of clinical data for performance measurement. All that work to gather clinical data electronically is an ongoing significant challenge in health care. It is, however, largely nascent in oral health care (Langabeer et al., 2008).
Quality measurement in oral health care will also depend on administrative claims sources, at least in part, and until there is broad adoption and meaningful use of electronic formats in oral health care. Unfortunately, oral health care has an additional technical challenge: the absence of a universally accepted and used diagnosis code among dentists (Bader, 2009a; Garcia et al., 2010). Several code sets are available for oral health, but they have not been put into general use. Oral diseases are included in the International Statistical Classification of Diseases and Related Health Problems (ICD) codes, which have been almost universally adopted in medicine. The ICD oral health codes have been criticized, however, because they are interspersed with medically oriented diseases, and they do not distinguish between primary and permanent teeth (Leake, 2002). The ADA has developed a comprehensive system of diagnosis codes, the Systematized Nomenclature of Dentistry (SNODENT), but it has yet to be released (Bader, 2009a). Several closed-panel delivery systems have also developed oral health code sets for use inside their systems, but they are not available to the general public (Bader, 2009a).
The development of new measures depends on evidence-based standards and guidelines from which to create metrics. Quality measurement in oral health is hampered by the absence of a strong evidence base for most oral health treatments and, therefore, a lack of evidence-based guidelines (Bader, 2009b). In fact, a significant percentage of Cochrane reviews in dentistry did not have enough evidence to answer the research question
posed (Bader, 2009a,b). Dental research is challenged in part because with the typical small practice design, it can be difficult to obtain outcomes data due to the need to gather data from multiple practices as well as the variety of forms that are used to collect the same data. The practice design also makes it difficult to disseminate evidence when it exists; most dentists work alone, so information sharing is limited, and few have chairside access to journals or computers (Bader, 2009b).
Future Directions for Quality Measurement in Oral Health Care
Quality improvement in oral health is hampered by an insufficient evidence base for interventions, insufficient data sources, and a lack of quality measures. Based on and building from the logic of the extensive past work on quality and quality measurement by the IOM and many others in overall health care, HHS and others need to prioritize developing quality assessment in oral health. Oral health care needs better measures to understand the state of quality in oral health care, identify quality and disparities problems, and begin to develop appropriate solutions to address those problems. One of the first steps is promoting the development of measures of the quality of oral health care. Ideally, the effort to build oral health care measures could learn from and perhaps build upon the existing health care measurement enterprise.
In 2008, CMS called upon the ADA to take the lead in developing performance measures to assess the quality of dental care being provided to children across the country. The project, known as the Dental Quality Alliance (DQA), began with its first meeting in late 2010 and was scheduled to begin measures development in early 2011 (Rich, 2010). The mission of the DQA is “to advance performance measurement as a means to improve oral health, patient care, and safety through a consensus-building process” (Rich, 2010). The DQA will identify and develop evidence-based oral health care performance measures, advance the effectiveness and scientific basis of clinical performance measurement, and seek to foster greater professional accountability, transparency, and value in oral health care (Rich, 2010).
Beyond basic quality measurement, the development of better measures for the quality of oral health care is needed to perform comparative effectiveness research for many oral health interventions. For example, in 2009, the IOM produced a study that identified the 100 priority topics for comparative effectiveness research in all of health care. Two of the topics were related to oral health:
• ORAL-A: Compare the clinical and cost-effectiveness of surgical care and a medical model of prevention and care in managing
periodontal disease to increase tooth longevity and reduce systemic secondary effects in other organ systems, and
• ORAL-B: Compare the effectiveness of the various delivery models (e.g., primary care, dental offices, schools, mobile vans) in preventing dental caries in children (IOM, 2009).
The committee concluded that much more needs to be done to improve the quality assessment and improvement efforts in oral health to answer some of the basic questions regarding improving oral health and oral health access.
The committee noted the following key findings and conclusions:
Sites of Care
• Oral health is provided in two separate systems—private offices and the safety net—neither of which function adequately for vulnerable populations.
Financing Oral Health Care
• Out-of-pocket payments account for 44 percent of dental expenditures, and dental services account for 22 percent of all out-of-pocket health care expenditures.
• High out-of-pocket costs, lack of dental coverage, and limited financial means create barriers to receiving oral health care.
• Ideally, dental coverage would be included as part of health care coverage, but the cost of doing so makes this potential merger extraordinarily challenging.
• More research is needed on the economic and social impacts of increasing coverage (both in terms of numbers of individuals as well as the breadth of services).
• More research is needed on how different financing systems and the incentives therein might affect care delivery, including provider participation, cost-effectiveness, and efficiency.
Workforce
• Health care professionals from underrepresented minority groups often account for a disproportionate share of care for patients from those same populations.
• Although it is improving slowly, the racial and ethnic profile of the dental workforce does not reflect the population as a whole.
• Several models of new and emerging dental professionals have been developed, but little research exists on which type has the most promise to improve access or how they can best be integrated into the workforce and targeted to vulnerable populations.
• Interprofessional, team-based care has the potential to improve care-cooridination, patient outcomes, and produce cost savings, yet most health care professionals are not trained to work in either intra- or interdisciplinary teams.
• While the regulation of health care professions occurs at the state level, HHS has a role to play in the demonstration and testing of new workforce models.
Education and Training
• Many nondental health care professionals are well suited and willing to integrate oral health care into the primary care setting, but they are not trained to do so.
• Nondental health care professionals have a significant role to play in oral health promotion and disease prevention, especially for children. Key modalities include basic examinations and risk assessments, patient and caregiver counseling, and the application of topical fluorides.
Quality
• In general, dentists do not use a universally accepted diagnosis coding system.
• Oral health lags significantly behind the remainder of the health care system in developing quality measures, and as a result, little is known about the quality of oral health care.
• Much more needs to be done to improve the quality assessment, improvement, and reporting efforts in oral health in order to answer some of the basic questions regarding improving oral health and oral health access.
AAMC (Association of American Medical Colleges). 2008. Contemporary issues in medicine: Oral health education for medical and dental students. Washington, DC: American Association of Medical Colleges.
AAMC. 2011. Cost of a medical education. https://www.aamc.org/students/considering/financing/ (accessed February 23, 2011).
AANA (American Association of Nurse Anesthetists). 2011. AANA overview. http://www.aana.com/aboutaana.aspx?id=100&linkidentifier=id&itemid=100 (accessed February 26, 2011).
AAP (American Academy of Pediatrics). 2008. Policy statement: Preventive oral health intervention for pediatricians. Pediatrics 122(6):1387-1394.
AAP. 2010. Fluoride information by state. http://www.aap.org/commpeds/dochs/oralhealth/fluoride.cfm (accessed February 25, 2011).
AAP. 2011a. Bright futures: History. http://brightfutures.aap.org/history.html (accessed February 26, 2011).
AAP. 2011b. Oral health risk assessment: Training for pediatricians and other child health professionals. http://www.aap.org/oralhealth/cme/page46.htm (accessed February 25, 2011). AAP. 2011c. Protecting all children’s teeth: A pediatric oral health training program. http://www.aap.org/oralhealth/pact/index.cfm (accessed January 6, 2011).
AAPHD (American Association of Public Health Dentistry). 2004. History of the American Association of Public Health Dentistry. http://www.aaphd.org/default.asp?page=history.htm (accessed February 22, 2011).
ABP (American Board of Pediatrics). 2009. General pediatrics certification examination: Content outline. Chapel Hill, NC: American Board of Pediatrics.
ACGME (Accreditation Council for Graduate Medical Education). 2007. ACGME program requirements for graduate medical education in family medicine. Chicago, IL: Accreditation Council for Graduate Medical Education.
ACGME. 2008. ACGME program requirements for graduate medical education in sleep medicine. Chicago, IL: Accreditation Council for Graduate Medical Education.
ACGME. 2009a. ACGME program requirements for graduate medical education in geriatric medicine. Chicago, IL: Accreditation Council for Graduate Medical Education.
ACGME. 2009b. ACGME program requirements for graduate medical education in internal medicine. Chicago, IL: Accreditation Council for Graduate Medical Education.
Ackermann, R. J., and K. A. Kemle. 1998. The effect of a physician assistant on the hospitalization of nursing home residents. Journal of the American Geriatrics Society 46(5):610-614.
ADA (American Dental Association). 1998. 1996 dentist profile survey. Chilcago, IL: American Dental Association.
ADA. 2001. Future of dentistry. Chicago, IL: American Dental Association.
ADA. 2007. American Indian and Alaska Native oral health access summit: Summary report.
Santa Ana Pueblo, NM: American Dental Association.
ADA. 2009a. 2008-09 survey of allied dental education. Chicago, IL: American Dental Association.
ADA. 2009b. 2008 survey of dental practice: Characteristics of dentists in private practice and their patients. Chicago, IL: American Dental Association.
ADA. 2009c. 2008 survey of dental practice: Income from the private practice of dentistry.
Chicago, IL: American Dental Association.
ADA. 2009d. Distribution of dentists in the United States by region and state, 2007. Chicago, IL: American Dental Association.
ADA. 2010a. 2008-09 survey of dental education: Academic programs, enrollment, and graduates—volume 1. Chicago, IL: American Dental Association.
ADA. 2010b. 2008-2009 survey of advanced dental education. Chicago, IL: American Dental Association.
ADA. 2011a. Ninth GKAS Day a Success. http://www.ada.org/news/5416.aspx (accessed February 21, 2011).
ADA. 2011b. Students drive diversity initiatives. http://www.ada.org/news/5408.aspx (accessed August 30, 2011).
ADAA (American Dental Assistants Association)/DANB (Dental Assisting National Board) Alliance. 2005. Addressing a uniform national model for the dental assisting profession. Chicago, IL: Dental Assisting National Board.
ADHA (American Dental Hygienists’ Association). 2006. Dental hygiene education program director survey. Chicago, IL: American Dental Hygienists’ Association.
ADHA. 2009a. 2009 dental hygiene job market & employment survey. http://www.adha.org/downloads/Job_employment_survey_2009_exec_sum.pdf (accessed November 30, 2010).
ADHA. 2009b. Survey of dental hygienists in the United States: 2007. Chicago, IL: American Dental Hygienists’ Association.
ADHA. 2010. Frequently asked questions. http://www.adha.org/faqs/index.html (accessed November 23, 2010).
AGD (Academy of General Dentistry). 2008. White paper on increasing access to and utilization of oral health care services. Chicago, IL: Academy of General Dentistry.
AHRQ (Agency for Healthcare Research and Quality). 2010. National healthcare quality & disparities reports: NHQRDRnet. http://nhqrnet.ahrq.gov/nhqrdr/jsp/nhqrdr.jsp (accessed November 29, 2010).
Allison, R. A., and R. J. Manski. 2007. The supply of dentists and access to care in rural Kansas. Journal of Rural Health 23(3):198-206.
AMA (American Medical Association). 2011. Medical student debt. http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/medical-student-section/advocacy-policy/medical-student-debt.shtml (accessed January 5, 2011).
Ambrose, E. R., A. B. Hord, and W. J. Simpson. 1976. A quality evaluation of specific dental services provided by the Saskatchewan dental plan: Final report: Regina, Saskatchewan: Saskatchewan Dental Plan.
ANA (American Nurses Association). 2011a. More about RNs and advance practice RNs. http://www.nursingworld.org/EspeciallyForYou/StudentNurses/RNsAPNs.aspx (accessed September 1, 2011).
ANA. 2011b. Who we are. http://nursingworld.org/FunctionalMenuCategories/AboutANA/WhoWeAre.aspx (accessed February 21, 2011).
Andersen, R. M., P. L. Davidson, K. A. Atchison, E. Hewlett, J. R. Freed, J. A. Friedman, A. Thind, J. J. Gutierrez, T. T. Nakazono, and D. C. Carreon. 2005. Pipeline, profession, and practice program: Evaluating change in dental education. Journal of Dental Education 69(2):239-248.
Andersen, R. M., D. C. Carreon, P. L. Davidson, T. T. Nakazono, S. Shahedi, and J. J. Gutierrez. 2010. Who will serve? Assessing recruitment of underrepresented minority and low-income dental students to increase access to dental care. Journal of Dental Education 74(6):579-592.
ARC-PA (Accreditation Review Commission on Education for the Physician Assistant). 2010. Accreditation standards for physician assistant education, 4th ed. Johns Creek, GA: Accreditation Review Commission on Education for the Physician Assistant.
ASTDD (Association of State and Territorial Dental Directors). 2007. Fluoride varnish: An evidence-based approach. http://www.astdd.org/docs/Sept2007FINALFlvarnishpaper.pdf (accessed February 26, 2011).
ASTDD. 2011a. About ASTDD. http://www.astdd.org/about-us/ (accessed March 12, 2011).
ASTDD. 2011b. State & territorial dental public health activities: A collection of descriptive summaries. http://www.astdd.org/state-activities/ (accessed August 1, 2011).
ASTDD. 2011c. Synopses of state dental public health programs: Data for FY 2009-2010. http://www.astdd.org/docs/State_Synopsis_Report_SUMMARY_2011.pdf (accessed August 1, 2011).
Atchison, K. A., and M. H. Schoen. 1990. A comparison of quality in a dual-choice dental plan: Capitation versus fee-for-service. Journal of Public Health Dentistry 50(3):186-193.
Awé, C., and J. Bauman. 2010. Theoretical and conceptual framework for a high school pathway to pharmacy program. American Journal of Pharmaceutical Education 74(8): Article 149.
Bader, J. D. 2009a. Challenges in quality assessment of dental care. Journal of the American Dental Association 140(12):1456-1464.
Bader, J. D. 2009b. Stumbling into the age of evidence. Dental Clinics of North America 53(1):15-22.
Bailit, H., and T. Beazoglou. 2008. Financing dental care: Trends in public and private expenditures for dental services. Dental Clinics of North America 52(2):281-295.
Bailit, H., T. Beazoglou, N. Demby, J. McFarland, P. Robinson, and R. Weaver. 2006. Dental safety net: Current capacity and potential for expansion. Journal of the American Dental Association 137(6):807-815.
Barsky, C. B. 2004. Incidence benefits measures in the national compensation survey. Monthly Labor Review 127(8):21-28.
Baum, K. D., and S. Axtell. 2005. Trends in north american medical education. Keio Journal of Medicine 54(1):22-28.
Berg, P., and D. Coniglio. 2006. Oral health in children: Overlooked and undertreated. Journal of the American Academy of Physician Assistants 19(4):40.
Bloom, B., and R. A. Cohen. 2010. Dental insurance for persons under age 65 years with private health insurance: United States, 2008. Hyattsville, MD: National Center for Health Statistics.
BLS (Bureau of Labor Statistics). 2009a. Occupational outlook handbook, 2010-11 edition, pharmacists. http://www.bls.gov/oco/ocos079.htm (accessed December 28, 2010).
BLS. 2009b. Occupational outlook handbook, 2010-11 edition, physician assistants. http://www.bls.gov/oco/ocos081.htm (accessed December 28, 2010).
BLS. 2010a. Consumer out-of-pocket health care expenditures in 2008. http://www.bls.gov/opub/ted/2010/ted_20100325_data.htm (accessed January 9, 2011).
BLS. 2010b. Employee benefits survey: Health care benefits, March 2010. http://www.bls.gov/ncs/ebs/benefits/2010/benefits_health.htm (accessed December 28, 2010).
BLS. 2010c. Employment projections: Fastest growing occupations. http://www.bls.gov/emp/ep_table_103.htm (accessed December 28, 2010).
BLS. 2010d. Occupational outlook handbook 2010-11 edition, dental assistants. http://www.bls.gov/oco/ocos163.htm (accessed December 28, 2010).
BLS. 2010e. Occupational outlook handbook, 2010-11 edition, dental hygienists. http://www.bls.gov/oco/ocos097.htm (accessed December 28, 2010).
BLS. 2010f. Occupational outlook handbook, 2010-11 edition, dentists. http://www.bls.gov/oco/ocos072.htm (accessed January 5, 2011).
BLS. 2010g. Occupational outlook handbook, 2010-11 edition, medical, dental, and ophthalmic laboratory technicians. http://www.bls.gov/oco/ocos238.htm (accessed January 6, 2011).
Blue, A., B. F. Brandt, and M. H. Schmitt. 2010. American interprofessional health collaborative: Historical roots and organizational beginnings. Journal of Allied Health 39(Supp. 1):204-209.
Bolin, K. A. 2008. Assessment of treatment provided by dental health aide therapists in Alaska. Journal of the American Dental Association 139(11):1530-1535.
Borchgrevink, A., A. Snyder, and S. Gehshan. 2008. The effects of Medicaid reimbursement rates on access to dental care. Washington, DC: National Academy for State Health Policy.
Brach, C., E. M. Lewit, K. VanLandeghem, J. Bronstein, A. W. Dick, K. S. Kimminau, B. LaClair, E. Shenkman, L. P. Shone, N. Swigonski, and P. G. Szilagyi. 2003. Who’s enrolled in the state children’s health insurance program (SCHIP)? An overview of findings from the child health insurance research initiative (CHIRI). Pediatrics 112(6 Supp. 2): e499-e507.
Brooks, E. S., T. C. Gravely, S. A. Hornback, L. C. Cunningham, A. L. McCann, and J. L. Long. 2002. Bridge to dentistry: One dental school’s approach to improving its enrollment of underrepresented minorities. Journal of the American College of Dentists 69(1):23-30.
Brown, E., and R. J. Manski. 2004. Dental services: Use, expenses, and sources of payment, 1996-2000. Rockville, MD: Agency for Healthcare Research and Quality.
Brown, L. J. 2005. Adequacy of current and future dental workforce: Theory and analysis. Chicago, IL: American Dental Association.
Brown, L. J., K. S. Wagner, and B. Johns. 2000. Racial/ethnic variations of practicing dentists. Journal of the American Dental Association 131(12):1750-1754.
Brugna, R. A., J. F. Cawley, and M. D. Baker. 2007. Physician assistants in geriatric medicine. Clinical Geriatrics 15(10):22-29.
Brunson, W. D., D. L. Jackson, J. C. Sinkford, and R. W. Valachovic. 2010. Components of effective outreach and recruitment programs for underrepresented minority and low-income dental students. Journal of Dental Education 74(10 Supp.):S74-S86.
Budzi, D., S. Lurie, K. Singh, and R. Hooker. 2010. Veterans’ perceptions of care by nurse practitioners, physician assistants, and physicians: A comparison from satisfaction surveys. Journal of the American Academy of Nurse Practitioners 22(3):170-176.
Buelow, J. R., C. Rathsack, D. Downs, K. Jorgensen, J. R. Karges, and D. Nelson. 2008. Building interdisciplinary teamwork among allied health students through live clinical case simulations. Journal of Allied Health 37(2):e109-e123.
Cantor, J. C., L. Bergeisen, and L. C. Baker. 1998. Effect of an intensive educational program for minority college students and recent graduates on the probability of acceptance to medical school. Journal of the American Medical Association 280(9):772-776.
Cantrell, C. 2008. The role of physicians in children’s oral health. Portland, ME: National Association for State Health Policy.
Cantrell, C. 2009. Engaging primary care medical providers in children’s oral health. Portland, ME: National Academy for State Health Policy.
Carey, M. A. 2010. New Medicare/Medicaid projects aimed at cheaper, better care. http://www.kaiserhealthnews.org/Stories/2010/November/17/cms-innovation-center-berwick.aspx (accessed January 9, 2011).
Carson-Smith, W. Y., and P. A. Minarik. 2007. Advanced practice nurses: A new skirmish in the continuing battle over scope of practice. Clinical Nurse Specialist 21(1):52-54.
Caspary, G., D. M. Krol, S. Boulter, M. A. Keels, and G. R.C. 2008. Perceptions of oral health training and attitudes toward performing oral health screenings among graduating pediatric residents. Pediatrics 122(2):e465-e471.
CDC (Centers for Disease Control and Prevention). 2009. Lack of health insurance and type of coverage. http://www.cdc.gov/nchs/data/nhis/earlyrelease/200906_01.pdf (accessed August 19, 2010).
CDC. 2011. State oral health plans. http://www.cdc.gov/OralHealth/state_programs/OH_plans/index.htm (accessed September 8, 2011).
Chalmers, J. M. 1996. Factors influencing nurses’ aides’ provision of oral care for nursing facility residents. Special Care in Dentistry 16(2):71-79.
Chiarello, G. P. 2009. Regulating the professions: The intersection of competition and consumer protection policies. Paper presented at the IOM workshop The U.S. Oral Health Workforce in the Coming Decade, Washington, DC.
Chmar, J. E., R. G. Weaver, and R. W. Valachovic. 2008. Dental school vacant budgeted faculty positions, academic years 2005-06 and 2006-07. Journal of Dental Education 72(3):370-385.
Chu, M., L. E. Sweis, A. H. Guay, and R. J. Manski. 2007. The dental care of U.S. children: Access, use and referrals by nondentist providers, 2003. Journal of the American Dental Association 138(10):1324-1331.
Clemmens, D. A., and A. R. Kerr. 2008. Improving oral health in women: Nurses’ call to action. MCN American Journal of Maternal/Child Nursing 33(1):10-14.
Close, K., R. G. Rozier, L. P. Zeldin, and A. R. Gilbert. 2010. Barriers to the adoption and implementation of preventive dental services in primary medical care. Pediatrics 125(3):509-517.
CMS (Centers for Medicare and Medicaid Services). 2010a. Medicare dental coverage: Overview. http://www.cms.hhs.gov/MedicareDentalCoverage (accessed November 22, 2010).
CMS. 2010b. MSIS tables: Details for 2008. http://www.cms.gov/MedicaidDataSourcesGenInfo/MSIS/itemdetail.asp?filterType=dual,data2&filterValue=Medicaid Payments by Service Category&filterByDID=2&sortByDID=1&sortOrder=ascending&itemID=CMS1229918&intNumPerPage=10 (accessed February 23, 2011).
CMS. 2011a. Medicaid dental coverage. http://www.cms.gov/MedicaidDentalCoverage/ (accessed June 10, 2011).
CMS. 2011b. National health expenditures accounts: Definitions, sources, and methods, 2009. https://www.cms.gov/NationalHealthExpendData/downloads/dsm-09.pdf (accessed July 29, 2011).
CMS. 2011c. National health expenditures by type of service and source of funds: CY 1960-2009. http://www.cms.gov/NationalHealthExpendData/02_NationalHealthAccountsHistorical.asp (accessed June 14, 2011).
Cohen, D. W., P. P. Cormier, and J. L. Cohen. 1985. Educating the dentist of the future: the Pennsylvania Experiment. Philadelphia: University of Pennsylvania Press.
Cohen, L. A., A. J. Bonito, D. R. Akin, R. J. Manski, M. D. Macek, R. R. Edwards, and L. J. Cornelius. 2009. Role of pharmacists in consulting with the underserved regarding toothache pain. Journal of the American Pharmacists Association: JAPhA 49(1):38-42.
Coleman, P., and N. M. Watson. 2006. Oral care provided by certified nursing assistants in nursing homes. Journal of the American Geriatrics Society 54(1):138-143.
Cooper, H., C. Carlisle, T. Gibbs, and C. Watkins. 2001. Developing an evidence base for interdisciplinary learning: A systematic review. Journal of Advanced Nursing 35(2):228-237.
Daly, R. 2006. Physician coalition prepares for scope-of-practice battles. Psychiatric News 41(3):10.
Damiano, P. C., E. R. Brown, J. D. Johnson, and J. P. Scheetz. 1990. Factors affecting dentist participation in a state Medicaid program. Journal of Dental Education 54(11):638-643.
DANB (Dental Assisting National Board). 2007. Dental assisting job titles in the U.S. http://www.danb.org/PDFs/JobTitles.pdf (accessed February 23, 2011).
DANB. 2011. 2011 CDA exam application packet. http://www.danb.org/PDFs/CDAApplication.pdf (accessed September 8, 2011).
Danielsen, R., J. Dillenberg, and C. Bay. 2006. Oral health competencies for physician assistants and nurse practitioners. Journal of Physician Assistant Education 17(4):12-16.
Dela Cruz, G. G., R. G. Rozier, and G. Slade. 2004. Dental screening and referral of young children by pediatric primary care providers. Pediatrics 114(5).
DENTEX. 2010. Dental health aide training program. http://depts.washington.edu/dentexak/mission.html (accessed September 19, 2011).
Department of Education. 2010. College accreditation in the United States: Specialized accrediting agencies. http://www2.ed.gov/admins/finaid/accred/accreditation_pg7.html#health (accessed December 22, 2010).
DesRoches, C. M., and A. Jha. 2009. On the cusp of change: Health information technology in the United States, 2009. Princeton, NJ: Robert Wood Johnson Foundation.
Dickinson, T. D. 2010. The MOM experience: Pathways to collaboration and conversation. Presentation at meeting of the Committee on Oral Health Access to Services, Washington, DC. March 4, 2010.
Dodds, J., W. Vann, J. Lee, A. Rosenberg, K. Rounds, M. Roth, M. Wells, E. Evens, and L. H. Margolis. 2010. The UNC-CH MCH leadership training consortium: Building the capacity to develop interdisciplinary MCH leaders. Maternal and Child Health Journal 14(4):642-648.
Douglass, A. B., M. Deutchman, J. Douglass, W. Gonsalves, R. Maier, H. Silk, J. Tysinger, and A. S. Wrightson. 2009a. Incorporation of a national oral health curriculum into family medicine residency programs. Family Medicine 41(3):159-160.
Douglass, A. B., J. M. Douglass, and D. M. Krol. 2009b. Educating pediatricians and family physicians in children’s oral health. Academic Pediatrics 9(6):452-456.
Dower, C. 2009. Regulatory challenges to improving oral health care in the U.S. Presentation at the IOM workshop The U.S. Oral Health Workforce in the Coming Decade, Washington, DC. February 10, 2009.
Dulisse, B., and J. Cromwell. 2010. No harm found when nurse anesthetists work without supervision by physicians. Health Affairs 29(8):1469-1475.
Dunning, J. M. 1958. Extending the field for dental auxiliary personnel in the United States. American Journal of Public Health 48(8):1059-1064.
Dyer, J. A. 2003. Multidisciplinary, interdisciplinary, and transdisciplinary: Educational models and nursing education. Nursing Education Perspectives 24(4):186-188.
Edelstein, B. 2010a. The dental safety net, its workforce, and policy recommendations for its enhancement. Journal of Public Health Dentistry 70(Supp. 1):S32-S39.
Edelstein, B. 2010b. Training new dental health providers in the U.S. Battle Creek, MI: W.K. Kellogg Foundation.
Evans, A. W., R. M. A. Leeson, and A. Petrie. 2005. Correlation between a patient-centred outcome score and surgical skill in oral surgery. British Journal of Oral and Maxillofacial Surgery 43(6):505-510.
Fales, M. H. 1958. The potential role of the dental hygienist in public health programs. American Journal of Public Health 48(8):1054-1058.
Ferguson, D. A., B. J. Steinberg, and T. Schwien. 2010. Dental economics and the aging population. Compendium of continuing education in dentistry (Jamesburg, NJ : 1995) 31(6):418-420, 422, 424-425.
Ferullo, A., H. Silk, and J. A. Savageau. 2011. A national survey of oral health curriculum in all U.S. allopathic and osteopathic medical schools. Academic Medicine 86(2):252-825.
Fiset, L. 2005. A report on quality assessment of primary care provided by dental therapists to Alaska natives. Seattle, WA: University of Washington School of Dentistry.
Flores, G., and S. C. Tomany-Korman. 2008. The language spoken at home and disparities in medical and dental health, access to care, and use of services in U.S. children. Pediatrics 121(6):e1703-e1714.
Ford, J. L. 2009. The new health participation and access data from the National Compensation Survey. http://www.bls.gov/opub/cwc/cm20091022ar01p1.htm (accessed December 27, 2010).
Formicola, A. J., J. McIntosh, S. Marshall, D. Albert, D. Mitchell-Lewis, G. P. Zabos, and R. Garfield. 1999. Population-based primary care and dental education: A new role for dental schools. Journal of Dental Education 63(4):331-338.
Formicola, A J., H. Bailit, T. Beazoglou, and L. A. Tedesco. 2005. The Macy study: A framework for consensus. Journal of Dental Education 69(11): 1183-1185.
Formicola, A. J., R. Myers, J. F. Hasler, M. Peterson, W. Dodge, H. L. Bailit, T. Beazoglou, and L. A. Tedesco. 2006. Evolution of dental school clinics as patient care delivery centers. Journal of Dental Education 70(12):1271-1288.
Formicola, A. J., K. C. D’Abreu, and L. A. Tedesco. 2010. Underrepresented minority dental student recruitment and enrollment programs: An overview from the dental pipeline program. Journal of Dental Education 74(10 Supp.):S67-S73.
FTC (Federal Trade Commission). 2004. Opinion and order of the commission: Docket no. 9311. http://www.ftc.gov/os/adjpro/d9311/040728commissionopinion.pdf (accessed January 10, 2011).
FTC. 2009. FTC staff comment before the Louisiana House of Representatives concerning Louisiana House Bill 687 on the practice of in-school dentistry. http://www.ftc.gov/os/2009/05/V090009louisianahb687amendment.pdf (accessed September 8, 2011).
FTC. 2010. Overview of FTC antitrust actions in health care services and products. Washington, DC: Federal Trade Commission.
FTC and DOJ (Department of Justice). 2004. Improving health care: A dose of competition. Washington, DC: Federal Trade Commission and Department of Justice.
Fulmer, T., K. Hyer, E. Flaherty, M. Mezey, N. Whitelaw, M. Orry Jacobs, R. Luchi, J. C. Hansen, D. A. Evans, C. Cassel, E. Kotthoff-Burrell, R. Kane, and E. Pfeiffer. 2005. Geriatric interdisciplinary team training program: Evaluation results. Journal of Aging and Health 17(4):443-470.
Gallagher, J. L., and D. A. Wright. 2003. General dental practitioners’ knowledge of and attitudes towards the employment of dental therapists in general practice. British Dental Journal 194(1):37-41.
GAO (Government Accountability Office). 2000. Factors contributing to low use of dental services by low-income populations. Washington, DC: U.S. General Accounting Office.
GAO. 2008. Extent of dental disease in children has not decreased, and millions are estimated to have untreated tooth decay. Washington, DC: U.S. Government Accountability Office.
GAO. 2010. Efforts underway to improve children’s access to dental services, but sustained attention needed to address ongoing concerns. Washington, DC: U.S. Government Accountability Office.
Garcia, R. I., R. E. Inge, L. Niessen, and D. P. DePaola. 2010. Envisioning success: The future of the oral health care delivery system in the United States. Journal of Public Health Dentistry 70(Supp. 1):S58-S65.
GDA (Georgia Dental Association). 2010. White paper on Georgia’s oral health status, access to and utilization of oral health care services. Atlanta, GA: Georgia Dental Association.
Gies, W. J. 1926. Dental education in the United States and Canada. New York: Carnegie Foundation for the Advancement of Teaching.
Greenberg, B. J. S., J. V. Kumar, and H. Stevenson. 2008. Dental case management: Increasing access to oral health care for families and children with low incomes. Journal of the American Dental Association 139(8):1114-1121.
Grumbach, K., and E. Chen. 2006. Effectiveness of University of California postbaccalaureate premedical programs in increasing medical school matriculation for minority and disadvantaged students. Journal of the American Medical Association 296(9):1079-1085.
Grumbach, K., L. G. Hart, E. Mertz, J. Coffman, and L. Palazzo. 2003. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Annals of Family Medicine 1(2):97-104.
Guay, A. H. 2005. Dental practice: Prices, production and profits. Journal of the American Dental Association 136(3):357-361.
Guthrie, D., R. W. Valachovic, and L. J. Brown. 2009. The impact of new dental schools on the dental workforce through 2022. Journal of Dental Education 73(12):1353-1360.
Haden, N. K., K. E. Morr, and R. W. Valachovic. 2001. Trends in allied dental education: An analysis of the past and a look to the future. Journal of Dental Education 65(5):480-495.
Haden, N. K., F. A. Catalanotto, C. J. Alexander, H. Bailit, A. Battrell, J. Broussard Jr., J. Buchanan, C. W. Douglass, C. E. Fox 3rd, P. Glassman, R. I. Lugo, M. George, C. Meyerowitz, E. R. Scott 2nd, N. Yaple, J. Bresch, Z. Gutman-Betts, G. G. Luke, M. Moss, J. C. Sinkford, R. G. Weaver, and R. W. Valachovic. 2003. Improving the oral health status of all Americans: Roles and responsibilities of academic dental institutions: The report of the ADEA President’s Commission. Journal of Dental Education 67(5):563-583.
Haden, N. K., W. D. Hendricson, D. K. Kassebaum, R. R. Ranney, G. Weinstein, E. L. Anderson, and R. W. Valachovic. 2010. Curriculum change in dental education, 2003-09. Journal of Dental Education 74(5):539-557.
Hall, P., and L. Weaver. 2001. Interdisciplinary education and teamwork: A long and winding road. Medical Education 35(9):867-875.
Hallas, D., and D. Shelley. 2009. Role of pediatric nurse practitioners in oral health care. Academic Pediatrics 9(6):462-466.
Hammick, M., D. Freeth, I. Koppel, S. Reeves, and H. Barr. 2007. A best evidence systematic review of interprofessional education: BEME guide no. 9. Medical Teacher 29(8):735-751.
Hammons, P. E., and H. C. Jamison. 1967. Expanded functions for dental auxiliaries. Journal of the American Dental Association 75(3):658-672.
Hammons, P. E., and H. C. Jamison. 1968. New duties for dental auxiliaries—the Alabama experience. American Journal of Public Health and the Nation’s Health 58(5):882-886.
Hammons, P. E., H. C. Jamison, and L. L. Wilson. 1971. Quality of service provided by dental therapists in an experimental program at the University of Alabama. Journal of the American Dental Association 82(5):1060-1066.
Harper, D. C., and J. Johnson. 1998. The new generation of nurse practitioners: Is more enough? Health Affairs 17(5):158-164.
Hart-Hester, S., and C. Thomas. 2003. Access to health care professionals in rural Mississippi. Southern Medical Journal 96(2):149-154.
Hesser, A., E. Pond, L. Lewis, and B. Abbot. 1996. Evaluation of a supplementary retention program for African-American baccalaureate nursing students. Journal of Nursing Education 35(7):304-309.
HHS (Department of Health and Human Services). 2000. Oral health in America: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services.
HHS. 2009. Pipeline programs to improve racial and ethnic diversity in the health professions: An inventory of federal programs, assessment of evaluation approaches, and critical review of the research literature. Rockville, MD: U.S. Department of Health and Human Services.
HHS. 2010. Advisory committee on training in primary care medicine and dentistry: The redesign of primary care with implications for training. Rockville, MD: U.S. Department of Health and Human Services.
Hooker, R. S., and L. E. Berlin. 2002. Trends in the supply of physician assistants and nurse practitioners in the United States. Health Affairs 21(5):174-181.
Hooker, R. S., D. J. Cipher, and E. Sekscenski. 2005. Patient satisfaction with physician assistant, nurse practitioner, and physician care: A national survey of Medicare beneficiaries. Journal of Clinical Outcomes Management 12(2):88-92.
Howe, J. L., and D. W. Sherman. 2006. Interdisciplinary educational approaches to promote team-based geriatrics and palliative care. Gerontology and Geriatrics Education 26(3):1-16.
HRSA (Health Resources and Services Administration). 2000. The public health workforce: Enumeration 2000. ftp://ftp.hrsa.gov//bhpr/nationalcenter/phworkforce2000.pdf (accessed February 22, 2011).
HRSA. 2004. The professional practice environment of dental hygienists in the fifty states and the District of Columbia, 2001. http://bhpr.hrsa.gov/healthworkforce/reports/hygienists/dh1.htm (accessed January 10, 2011).
HRSA. 2006. The rationale for diversity in the health professions: A review of the evidence. Rockville, MD: Department of Health and Human Services.
Huijbregts, P. A. 2007. Chiropractic legal challenges to the physical therapy scope of practice: Anybody else taking the ethical high ground? Journal of Manual and Manipulative Therapy 15(2):69-80.
IHS (Indian Health Service). 2011. Indian health manual, part 3, Chapter 2, dental. http://www.ihs.gov/ihm/index.cfm?module=dsp_ihm_pc_p3c2 (accessed February 28, 2011).
IOM (Institute of Medicine). 1988. The future of public health. Washington, DC: National Academy Press.
IOM. 1989. Allied health services: Avoiding crises. Washington, DC: National Academy Press. IOM. 1995. Dental education at the crossroads: Challenges and change. Washington, DC: National Academy Press.
IOM. 1996. Primary care: America’s health in a new era. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2004. In the nation’s compelling interest: Ensuring diversity in the health-care workforce. Washington, DC: The National Academies Press.
IOM. 2006. Performance measures: Accelerating improvement. Washington, DC: The National Academies Press.
IOM. 2008. Retooling for an aging America. Washington, DC: The National Academies Press.
IOM. 2009. Initial national priorities for comparative effectiveness research. Washington, DC: The National Academies Press.
IOM. 2010. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies.
Isong, I. A., K. E. Zuckerman, S. R. Rao, K. A. Kuhlthau, J. P. Winickoff, and J. M. Perrin. 2010. Association between parents’ and children’s use of oral health services. Pediatrics 125(3):502-508.
Jablonski, R. 2010. Nursing education and research (geriatrics). Presentation at meeting of the Committee on an Oral Health Initiative, Washington, DC. June 28, 2010.
Jablonski, R. A., C. L. Munro, M. J. Grap, C. M. Schubert, M. Ligon, and P. Spigelmyer. 2009. Mouth care in nursing homes: Knowledge, beliefs, and practices of nursing assistants. Geriatric Nursing 30(2):99-107.
Jacques, P. F., C. Snow, M. Dowdle, N. Riley, K. Mao, and W. C. Gonsalves. 2010. Oral health curricula in physician assistant programs: A survey of physician assistant program directors. Journal of Physician Assistant Education 21(2):22-30.
Johnson, L., R. J. Genco, C. Damsky, N. K. Haden, S. Hart, T. C. Hart, C. F. Shuler, L. A. Tabak, and L. A. Tedesco. 2008. Genetics and its implications for clinical dental practice and education: Report of panel 3 of the Macy study. Journal of Dental Education 72(Supp. 2):86-94.
Jones, P. E., and J. F. Cawley. 1994. Physician assistants and health system reform: Clinical capabilities, practice activities, and potential roles. Journal of the American Medical Association 271(16):1266-1272.
KFF (Kaiser Family Foundation). 2011. Health coverage of children: The role of Medicaid and CHIP. http://www.kff.org/uninsured/upload/7698-05.pdf (accessed March 1, 2011).
Kim, M. J., K. Holm, P. Gerard, B. McElmurry, M. Foreman, S. Poslusny, and C. Dallas. 2009. Bridges to the doctorate: Mentored transition to successful completion of doctoral study for underrepresented minorities in nursing science. Nursing Outlook 57(3):166-171.
Kleiner, M. M., and R. T. Kudrle. 2000. Does regulation affect economic outcomes? The case of dentistry. Journal of Law and Economics 43(2):547-582.
Kressin, N., M. Nunn, H. Singh, M. Orner, L. Pbert, C. Hayes, C. Culler, S. Glicken, S. Palfrey, and P. Geltman. 2009. Pediatric clinicians can help reduce rates of early childhood caries: Effects of a practice-based intervention. Medical Care 47(11):1121-1128.
Krol, D. M. 2004. Educating pediatricians on children’s oral health: Past, present, and future. Pediatrics 113(5):e487-e492.
Krol, D. M. 2010. Children’s oral health and the role of the pediatrician. Current Opinion in Pediatrics 22(6):804-808.
Lamster, I. B., L. A. Tedesco, D. M. Fournier, J. M. Goodson, A. R. Gould, N. K. Haden, T. H. Howell, Jr., T. K. Schleyer, J. A. Ship, and D. T. W. Wong. 2008. New opportunities for dentistry in diagnosis and primary health care: Report of panel 1 of the Macy study. Journal of Dental Education 72(Supp. 2):66-72.
Lang, W. P., and J. A. Weintraub. 1986. Comparison of Medicaid and non-Medicaid dental providers. Journal of Public Health Dentistry 46(4):207-211.
Langabeer II, J. R., M. F. Walji, D. Taylor, and J. A. Valenza. 2008. Economic outcomes of a dental electronic patient record. Journal of Dental Education 72(10):1189-1200.
Lavizzo-Mourey, R. 2010. Foreword. Journal of Dental Education 74(Supp. 10):S7-S8.
Leake, J. 2002. Diagnostic codes in dentistry—Definition, utility and developments to date. Journal-Canadian Dental Association 68(7):403-407.
Lerner, S., D. Magrane, and E. Friedman. 2009. Teaching teamwork in medical education. Mount Sinai Journal of Medicine 76(4):318-329.
Leviton, L. C. 2009. Foreword. Journal of Dental Education 73(Supp. 2):S5-S7.
Lewis, C. L. 1996. A state university’s model program to increase the number of its disadvantaged students who matriculate into health professions schools. Academic Medicine 71(10):1050-1057.
Lewis, C. W., D. C. Grossman, P. K. Domoto, and R. A. Deyo. 2000. The role of the pediatrician in the oral health of children: A national survey. Pediatrics 106(6):e84.
Liu, J., J. C. Probst, A. B. Martin, J.-Y. Wang, and C. F. Salinas. 2007. Disparities in dental insurance coverage and dental care among U.S. children: The National Survey of Children’s Health. Pediatrics 119(Supp. 1):S12-S21.
Lobene, R. R., and A. Kerr. 1979. The Forsyth experiment: An alternative system for dental care. Cambridge, MA: Harvard University Press.
Luciano, W. J., L. G. Rothfuss, and A. S. v. Gonten. 2006. The expanded function dental assistant training program. Army Medical Department Journal January-March 2006:16-20.
MacDorman, M. F., and G. K. Singh. 1998. Midwifery care, social and medical risk factors, and birth outcomes in the USA. Journal of Epidemiology and Community Health 52(5):310-317.
Machen, J. B. 2008. Will we allow dentistry to be left behind? Principles underlying dental education and practice. Journal of Dental Education 72(2 Supp):10-13.
Macleod, I., G. Bell, and A. Lorimer. 2003. A role for pharmacists in cancer detection. Pharmaceutical Journal 270(7240):367.
Manski, R. J., and E. Brown. 2007. Dental use, expenses, private dental coverage, and changes, 1996 and 2004. Rockville, MD: Agency for Healthcare Research and Quality.
Manski, R. J., and P. F. Cooper. 2010. Characteristics of employers offering dental coverage in the United States. Journal of the American Dental Association 141(6):700-711.
Manski, R. J., J. Moeller, H. Chen, P. A. St. Clair, J. Schimmel, L. Magder, and J. V. Pepper. 2010a. Dental care expenditures and retirement. Journal of Public Health Dentistry 70(2):148-155.
Manski, R. J., J. Moeller, H. Chen, P. A. St. Clair, J. Schimmel, L. Magder, and J. V. Pepper. 2010b. Dental care utilization and retirement. Journal of Public Health Dentistry 70(1): 67-75.
Manski, R. J., J. Moeller, J. Schimmel, P. A. St. Clair, H. Chen, L. Magder, and J. V. Pepper. 2010c. Dental care coverage and retirement. Journal of Public Health Dentistry 70(1): 1-12.
Markel, G., M. Woolfolk, and M. R. Inglehart. 2008. Feeding the pipeline: Academic skills training for predental students. Journal of Dental Education 72(6):653-661.
Martin, A., D. Lassman, L. Whittle, A. Catlin, J. Benson, C. Cowan, B. Dickensheets, M. Hartman, P. McDonnell, O. Nuccio, and B. Washington. 2011. Recession contributes to slowest annual rate of increase in health spending in five decades. Health Affairs 30(1):11-20.
McDonough, D. 2007. What’s new in ADAA demographics. http://findarticles.com/p/articles/mi_m0MKX/is_1_76/ai_n18645509/ (accessed March 9, 2011).
MCHB (Maternal and Child Health Bureau). 2011. Bright Futures for Infants, Children, and Adolescents. http://mchb.hrsa.gov/programs/training/brightfutures.htm (accessed March 1, 2011).
McKinnon, A., and D. Jorgenson. 2009. Pharmacist and physician collaborative prescribing: For medication renewals within a primary health centre. Canadian Family Physician 55(12):e86-e91.
McKnight-Hanes, C., D. R. Myers, and J. C. Dushku. 1992. Method of payment for children’s dental services by practice type and geographic location. Pediatric Dentistry 14(5):338-341.
Mertz, E., and P. Glassman. 2011. Alternative practice dental hygiene in California: Past, present, and future. CDA Journal 39(1).
Mertz, E. A., and K. Grumbach. 2001. Identifying communities with low dentist supply in California. Journal of Public Health Dentistry 61(3):172-177.
Mezey, M., S. G. Burger, H. G. Bloom, A. Bonner, M. Bourbonniere, B. Bowers, J. B. Burl, E. Capezuti, D. Carter, J. Dimant, S. A. Jerro, S. C. Reinhard, and M. Ter Maat. 2005. Experts recommend strategies for strengthening the use of advanced practice nurses in nursing homes. Journal of the American Geriatrics Society 53(10):1790-1797.
Misra, S., R. H. Harvey, D. Stokols, K. H. Pine, J. Fuqua, S. M. Shokair, and J. M. Whiteley. 2009. Evaluating an interdisciplinary undergraduate training program in health promotion research. American Journal of Preventive Medicine 36(4):358-365.
Mitchell, D. A., and S. L. Lassiter. 2006. Addressing health care disparities and increasing workforce diversity: The next step for the dental, medical, and public health professions. American Journal of Public Health 96(12):2093-2097.
Moeller, J. F., H. Chen, and R. J. Manski. 2010. Investing in preventive dental care for the Medicare population: A preliminary analysis. American Journal of Public Health 100(11):2262-2269.
Moller, J. 2010. Mobile dental clinic rules endorsed by legislative committee. Times-Picayune, August 20. P. A02.
Mouradian, W. E. 2010. Wanted . . . physicians who understand oral health. Presentation at meeting of the Committee on an Oral Health Initiative, Washington, DC. June 28, 2010.
Mouradian, W. E., J. H. Berg, and M. J. Somerman. 2003. Addressing disparities through dental-medical collaborations, part 1. The role of cultural competency in health disparities: Training of primary care medical practitioners in children’s oral health. Journal of Dental Education 67(8):860-868.
Mouradian, W. E., A. Reeves, S. Kim, R. Evans, D. Schaad, S. G. Marshall, and R. Slayton. 2005. An oral health curriculum for medical students at the University of Washington. Academic Medicine 80(5):434-442.
Mouradian, W. E., A. Reeves, S. Kim, C. Lewis, A. Keerbs, R. L. Slayton, D. Gupta, R. Oskouian, D. Schaad, and T. Kalet. 2006. A new oral health elective for medical students at the University of Washington. Teaching and Learning in Medicine 18(4):336-342.
Mouradian, W., C. N. Bertolami, L. Tedesco, C. Aschenbrener, S. J. Crandall, R. M. Epstein, M. Da Fonseca, N. K. Haden, A. Ruffin, J. J. Sciubba, S. Silverton, and R. P. Strauss. 2008. Curriculum and clinical training in oral health for physicians and dentists: Report of panel 2 of the Macy study. Journal of Dental Education 72(Supp. 2):73-85.
NADP (National Association of Dental Plans). 2009. Dental benefits improve access to dental care. http://www.nadp.org/Libraries/HCR_Documents/nadphcr-dentalbenefitsimproveaccesstocare-3-28-09.sflb.ashx (accessed January 10, 2011).
Naegele, E. R., J. Cunha-Cruz, and P. Nadanovsky. 2010. Disparity between dental needs and dental treatment provided. Journal of Dental Research 89(9):975-979.
Nash, D. A. 2009. Adding dental therapists to the health care team to improve access to oral health care for children. Academic Pediatrics 9(6):446-451.
Nash, D. A., and R. J. Nagel. 2005a. A brief history and current status of a dental therapy initiative in the United States. Journal of Dental Education 69(8):857-859.
Nash, D. A., and R. J. Nagel. 2005b. Confronting oral health disparities among American Indian/Alaska Native children: The pediatric oral health therapist. American Journal of Public Health 95(8):1325-1329.
Nash, D. A., and W. R. Willard. 2010. On why the dental therapists’ “movement” in the United States should focus on children—not adults. Journal of Public Health Dentistry 70(4):259-261.
Nash, D. A., J. W. Friedman, T. B. Kardos, R. L. Kardos, E. Schwarz, J. Satur, D. G. Berg, J. Nasruddin, E. G. Mumghamba, E. S. Davenport, and R. Nagel. 2008. Dental therapists: A global perspective. International Dental Journal 58(2):61-70.
National Task Force on Quality Nurse Practitioner Education. 2008. Criteria for evaluation of nurse practitioner programs. Washington, DC: National Organization of Nurse Practitioner Faculties.
NC Department of Health and Human Services. 2009. 2008-2009 annual report: North Carolina oral health section. http://www.ncdhhs.gov/dph/oralhealth/library/includes/08-09%20OHS%20Annual%20Report.pdf (accessed February 26, 2011).
Neumann, L. M. 2004. Trends in dental and allied dental education. Journal of the American Dental Association 135(9):1253-1259.
Nolan, L., B. Kamoie, J. Harvey, L. Vaquerano, S. Blake, S. Chawla, J. Levi, and S. Rosenbaum. 2003. The effects of state dental practice laws allowing alternative models of preventive oral health care delivery to low-income children. Washington, DC: Center for Health Services Research and Policy, School of Public Health and Health Services, The George Washington University.
NQF (National Quality Forum). 2010. NQF-endorsed standards. http://www.qualityforum.org/Measures_List.aspx (accessed November 29, 2010).
Oakley, D., M. E. Murray, T. Murtland, R. Hayashi, H. F. Andersen, F. Mayes, and J. Rooks. 1996. Comparisons of outcomes of maternity care by obstetricians and certified nurse midwives. Obstetrics and Gynecology 88(5):823-829.
Okunseri, C., A. Szabo, S. Jackson, N. M. Pajewski, and R. I. Garcia. 2009. Increased children’s access to fluoride varnish treatment by involving medical care providers: Effect of a Medicaid policy change. Health Services Research 44(4):1144-1156.
Okwuje, I., E. Anderson, and R. W. Valachovic. 2009. Annual ADEA survey of dental school seniors: 2008 graduating class. Journal of Dental Education 73(8):1009-1032.
Okwuje, I., E. Anderson, and R. W. Valachovic. 2010. Annual ADEA survey of dental school seniors: 2009 graduating class. Journal of Dental Education 74(9):1024-1045.
O’Leary, K. J., D. B. Wayne, C. Haviley, M. E. Slade, J. Lee, and M. V. Williams. 2010. Improving teamwork: Impact of structured interdisciplinary rounds on a medical teaching unit. Journal of General Internal Medicine 25(8):826-832.
Pew Center on the States and National Academy for State Health Policy. 2009. Help wanted: A policy maker’s guide to new dental providers. Washington, DC: Pew Center on the States, National Academy for State Health Policy.
PHI. 2010. Facts 3: Who are direct care workers? http://www.directcareclearinghouse.org/download/PHI%20FactSheet3_singles.pdf (accessed September 27, 2010).
Pierce, K. M., R. G. Rozier, and W. F. Vann. 2002. Accuracy of pediatric primary care providers’ screening and referral for early childhood caries. Pediatrics 109(5):e82.
Porter, J., P. C. Coyte, J. Barnsley, and R. Croxford. 1999. The effects of fee bundling on dental utilization. Health Services Research 34(4):901-921.
President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry. 1998. Quality first: Better health care for all Americans. http://www.hcqualitycommission.gov/final/ (accessed November 29, 2010).
Price, S. S., W. D. Brunson, D. A. Mitchell, C. J. Alexander, and D. L. Jackson. 2007. Increasing the enrollment of underrepresented minority dental students: Experiences from the dental pipeline program. Journal of Dental Education 71(3):339-347.
Quijano, A., A. J. Shah, A. I. Schwarcz, E. Lalla, and R. J. Ostfeld. 2010. Knowledge and orientations of internal medicine trainees toward periodontal disease. Journal of Periodontology 81(3):359-363.
Rackley, B., J. Wheat, C. Moore, R. Garner, and B. Harrell. 2003. The southern rural access program and Alabama’s rural health leaders pipeline: A partnership to develop needed minority health care professionals. Journal of Rural Health 19(5):354-360.
Rauh, S. J. 1917. The present status of and necessity for mouth hygiene. American Journal of Public Health 7:631-636.
Raybould, T. P., A. S. Wrightson, C. S. Massey, T. A. Smith, and J. Skelton. 2009. Advanced general dentistry program directors’ attitudes on physician involvement in pediatric oral health care. Special Care in Dentistry 29(6):232-236.
RCHWS (Regional Center for Health Workforce Studies). 2003. Changes in the scope of practice and the supply of non-physician clinicians in Texas. San Antonio, TX: Regional Center for Health Workforce Studies, Center for Health Economics and Policy, The University of Texas Health Science Center at San Antonio.
Reeves, S., M. Zwarenstein, J. Goldman, H. Barr, D. Freeth, M. Hammick, and I. Koppel. 2008. Interprofessional education: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews(1). Issue 1. Art. No.: CD002213. DOI: 10.1002/14651858.CD002213.pub2.
Reeves, S., M. Zwarenstein, J. Goldman, H. Barr, D. Freeth, I. Koppel, and M. Hammick. 2010. The effectiveness of interprofessional education: Key findings from a new systematic review. Journal of Interprofessional Care 24(3):230-241.
Remington, T. L., M. A. Foulk, and B. C. Williams. 2006. Evaluation of evidence for interprofessional education. American Journal of Pharmaceutical Education 70(3).
Rich, K. 2010. Dental quality alliance. http://www.medicaiddental.org/Docs/2010/Rich_Quality.pdf (accessed February 18, 2011).
Riter, D., R. Maier, and D. Grossman. 2008. Delivering preventive oral health services in pediatric primary care: A case study. Health Affairs 27(6):1728-1732.
Rosenblatt, R. A., S. A. Dobie, L. G. Hart, R. Schneeweiss, D. Gould, T. R. Raine, T. J. Benedetti, M. J. Pirani, and E. B. Perrin. 1997. Interspecialty differences in the obstetric care of low-risk women. American Journal of Public Health 87(3):344-351.
Rozier, R. G., B. K. Sutton, J. W. Bawden, K. Haupt, G. D. Slade, and R. S. King. 2003. Prevention of early childhood caries in north carolina medical practices: Implications for research and practice. Journal of Dental Education 67(8):876-885.
Rozier, R. G., S. C. Stearns, B. T. Pahel, R. B. Quinonez, and J. Park. 2010. How a North Carolina program boosted preventive oral health services for low-income children. Health Affairs 29(12):2278-2285.
Saman, D. M., O. Arevalo, and A. O. Johnson. 2010. The dental workforce in Kentucky: Current status and future needs. Journal of Public Health Dentistry 70(3):188-196.
Sanchez, O., N. Childers, L. Fox, and E. Bradley. 1997. Physicians’ views on pediatric preventive dental care. Pediatric Dentistry 19(6):377-383.
Shepard, L. 1978. Licensing restrictions and the cost of dental care. Journal of Law and Economics 21(1):187-201.
Silk, H., S. O. G. Stille, R. Baldor, and E. Joseph. 2009. Implementation of STFM’s “Smiles for Life” oral health curriculum in a medical school interclerkship. Family Medicine 41(7):487-491.
Sisty, N. L., W. G. Henderson, C. L. Paule, and J. F. Martin. 1978. Evaluation of student performance in the four-year study of expanded functions for dental hygienists at the University of Iowa. Journal of the American Dental Association 97(4):613-627.
Skillman, S. M., M. P. Doescher, W. E. Mouradian, and D. K. Brunson. 2010. The challenge to delivering oral health services in rural America. Journal of Public Health Dentistry 70(Supp. 1):S49-S57.
Snyder, M. E., A. J. Zillich, B. A. Primack, K. R. Rice, M. A. Somma McGivney, J. L. Pringle, and R. B. Smith. 2010. Exploring successful community pharmacist-physician collaborative working relationships using mixed methods. Research in Social and Administrative Pharmacy 6(4):307-321.
Society of Teachers of Family Medicine Group on Oral Health. 2011. Smiles for life: A national oral health curriculum. http://www.smilesforlife2.org (accessed January 6, 2011).
Solomon, E. S. 2007. Demographic characteristics of general dental practice sites. General Dentistry 55(6):552-558.
Sowter, J. R., and D. K. Raynor. 1997. The management of oral health problems in community pharmacies. Pharmaceutical Journal 259(6957):308-310.
Spielman, A. I., T. Fulmer, E. S. Eisenberg, and M. C. Alfano. 2005. Dentistry, nursing, and medicine: A comparison of core competencies. Journal of Dental Education. 69(11): 1257-1271.
Stanton, M. W., and M. K. Rutherford. 2003. Dental care: Improving access and quality. Rockville, MD: Agency for Healthcare Research and Quality.
Sullivan Commission. 2004. Missing persons: Minorities in the health professions, a report of the Sullivan Commission on diversity in the healthcare workforce. http://www.aacn.nche.edu/Media/pdf/SullivanReport.pdf (accessed January 24, 2011).
Sun, N., G. Burnside, and R. Harris. 2010. Patient satisfaction with care by dental therapists. British Dental Journal 208(5):E9.
Thind, A., K. A. Atchison, R. M. Andersen, T. T. Nakazono, and J. J. Gutierrez. 2008. Reforming dental education: Faculty members’ perceptions on the continuation of pipeline program changes. Journal of Dental Education 72(12):1472-1480.
Thind, A., K. A. Atchison, T. T. Nakazono, J. J. Gutierrez, D. C. Carreon, and J. Bai. 2009. Sustainability of dental school recruitment, curriculum, and community-based pipeline initiatives. Journal of Dental Education 73(Supp. 2):S297-S307.
Thistlethwaite, J., and M. Moran. 2010. Learning outcomes for interprofessional education (IPE): Literature review and synthesis. Journal of interprofessional care 24(5):503-513.
Thomson, W. A., P. Ferry, J. King, C. M. Wedig, and G. B. Villarreal. 2010. A baccalaureate-MD program for students from medically underserved communities: 15-year outcomes. Academic Medicine 85(4):668-674.
Todd, B. A., A. Resnick, R. Stuhlemmer, J. B. Morris, and J. Mullen. 2004. Challenges of the 80-hour resident work rules: Collaboration between surgeons and nonphysician practitioners. Surgical Clinics of North America 84(6):1573-1586.
Tomar, S. L. 2005. Dental public health training: Time for new models? Presentation at the National Oral Health Conference, Pittsburgh, PA. May 3, 2005.
Tomar, S. L. 2006. An assessment of the dental public health infrastructure in the United States. Journal of Public Health Dentistry 66(1):5-16.
University of Bridgeport. 1998. History of Fones School. http://www1bpt.bridgeport.edu/dental/history.html (accessed November 3, 2010).
University of Maryland. 2010. About the Baltimore College of Dental Surgery. http://www.dental.umaryland.edu/z_dental_archives/aboutBCDS_old/ (accessed December 27, 2010).
U.S. Census Bureau. 2000. Census 2000 EEO data tool. http://www.census.gov/eeo2000/index.html (accessed January 7, 2011).
U.S. Census Bureau. 2002. United States census 2000: U.S. Summary. http://www.census.gov/prod/2002pubs/c2kprof00-us.pdf (accessed January 7, 2011).
USMLE (U.S. Medical Licensing Exam). 2010a. 2011 step 2 clinical knowledge: Content description and general information. Philadelphia, PA: Federation of State Medical Boards of the United States and National Board of Medical Examiners.
USMLE. 2010b. 2011 step 3: Content description and general information. Philadelphia, PA: Federation of State Medical Boards of the United States and National Board of Medical Examiners.
Veal, K., M. Perry, J. Stavisky, and K. D. Herbert. 2004. The pathway to dentistry for minority students: From their perspective. Journal of Dental Education 68(9):938-946.
Venezie, R., W. Vann, Jr., S. Cashion, and R. Rozier. 1997. Pediatric and general dentists’ participation in the North Carolina Medicaid program: Trends from 1986 to 1992. Pediatric Dentistry 19(2):114-117.
Walker, M. P., S. I. Duley, M. M. Beach, L. Deem, R. Pileggi, N. Samet, A. Segura, and J. N. Williams. 2008. Dental education economics: Challenges and innovative strategies. Journal of Dental Education. 72(12):1440-1449.
Wall, T. P., and L. J. Brown. 2007. The urban and rural distribution of dentists, 2000. Journal of the American Dental Association 138(7):1003-1011.
Weinberg, M. A., and W. J. Maloney. 2007. Treatment of common oral lesions. U.S. Pharmacist 32(3):82-88.
Wendling, W. R. 2010. Private sector approaches to workforce enhancement. Journal of Public Health Dentistry 70(Supp. 1):S24-S31.
Wetterhall, S., J. D. Bader, B. B. Burrus, J. Y. Lee, and D. A. Shugars. 2010. Evaluation of the dental health aide therapist workforce model in Alaska. Research Triangle Park, NC: W.K. Kellogg Foundation, Rasmuson Foundation, Bethel Community Services Foundation.
WICHE (Western Interstate Commission for Higher Education). 2011. Professional student exchange program (PSEP). http://wiche.edu/psep (accessed January 11, 2011).
Wilder, R. S., J. A. O’Donnell, J. M. Barry, D. M. Galli, F. F. Hakim, L. J. Holyfield, and M. R. Robbins. 2008. Is dentistry at risk? A case for interprofessional education. Journal of Dental Education 72(11):1231-1237.
Williams, B. C., T. L. Remington, M. A. Foulk, and A. L. Whall. 2006. Teaching interdisciplinary geriatrics ambulatory care: A case study. Gerontology and Geriatrics Education 26(3):29-45.
Wing, P., M. H. Langelier, E. S. Salsberg, and R. S. Hooker. 2004. The changing professional practice of physician assistants: 1992 to 2000. Journal of the American Academy of Physician Assistants 17(1):37-40, 42, 45.
Wysen, K. H., P. M. Hennessy, M. I. Lieberman, T. E. Garland, and S. M. Johnson. 2004. Kids get care: Integrating preventive dental and medical care using a public health case management model. Journal of Dental Education 68(5):522-530.




























































